User login
UCSF Hospitalist Mini‐College
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
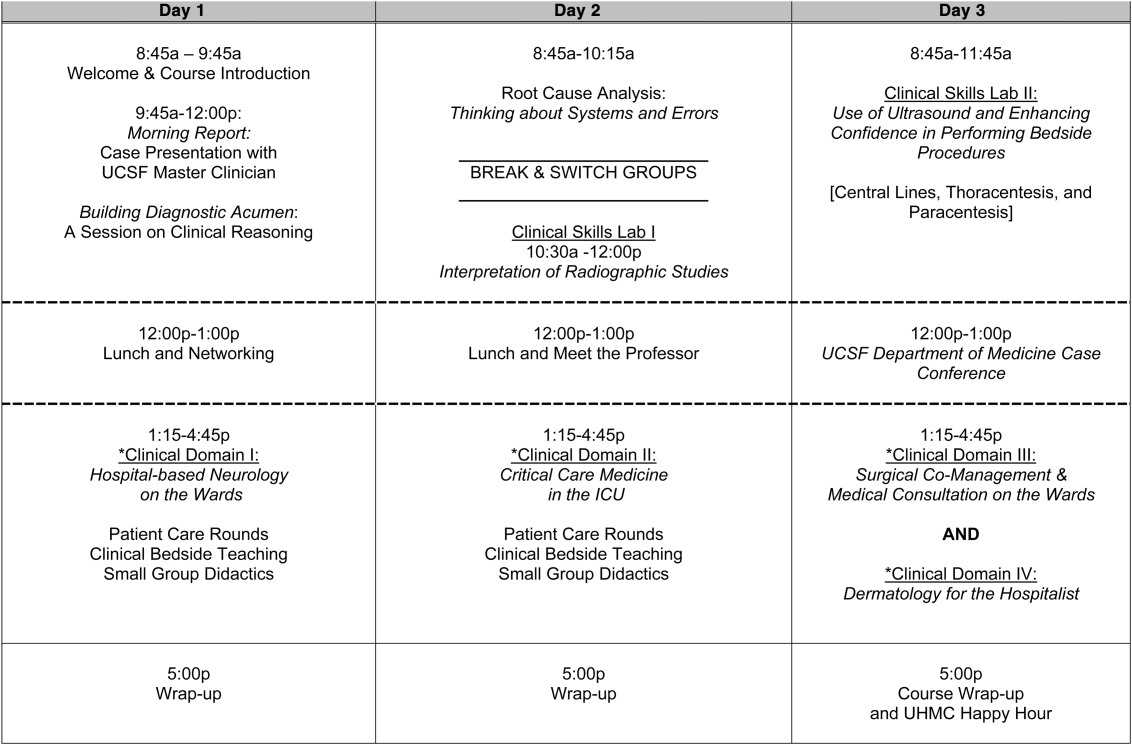
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
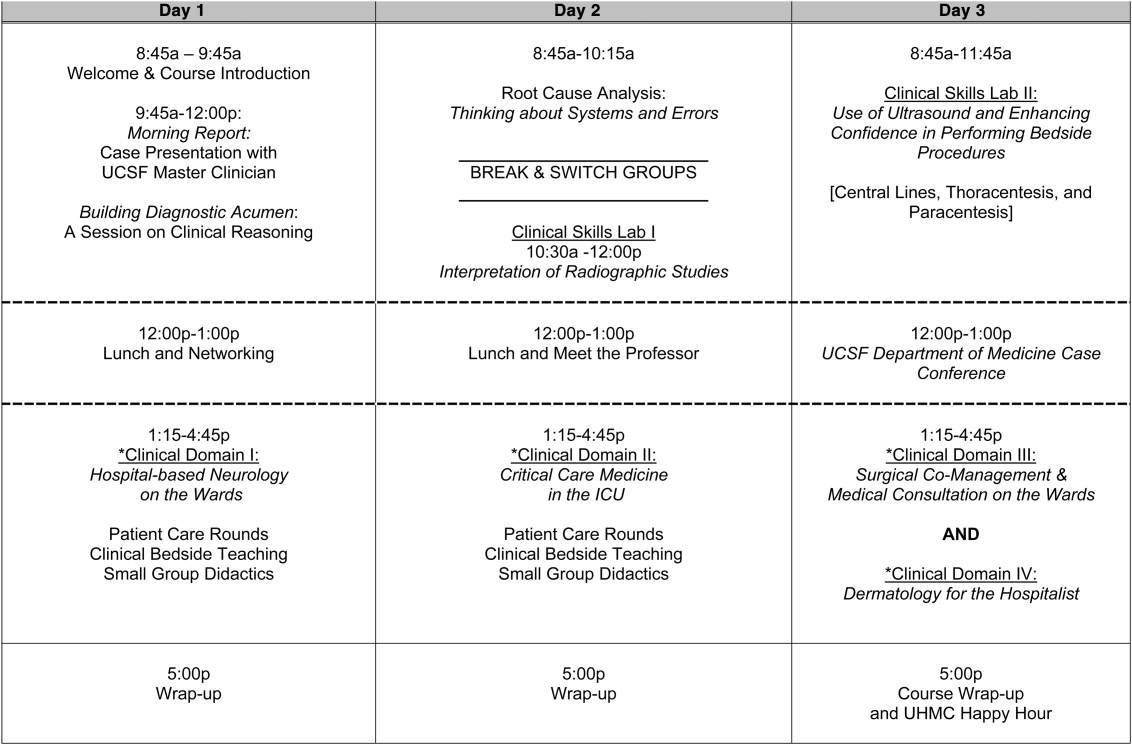
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
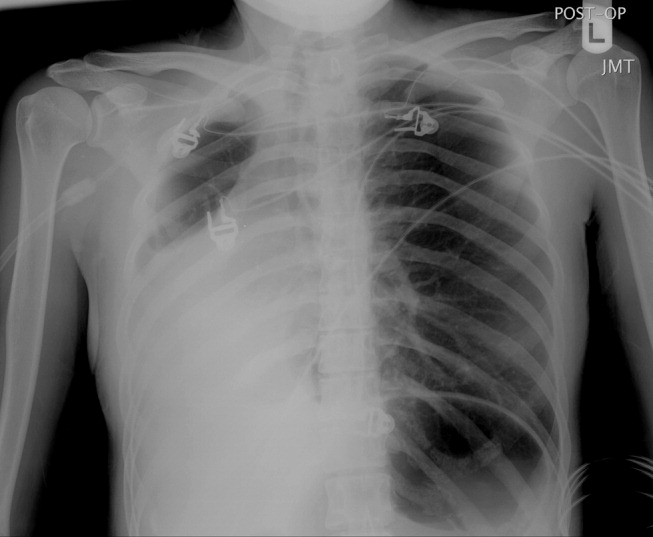
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
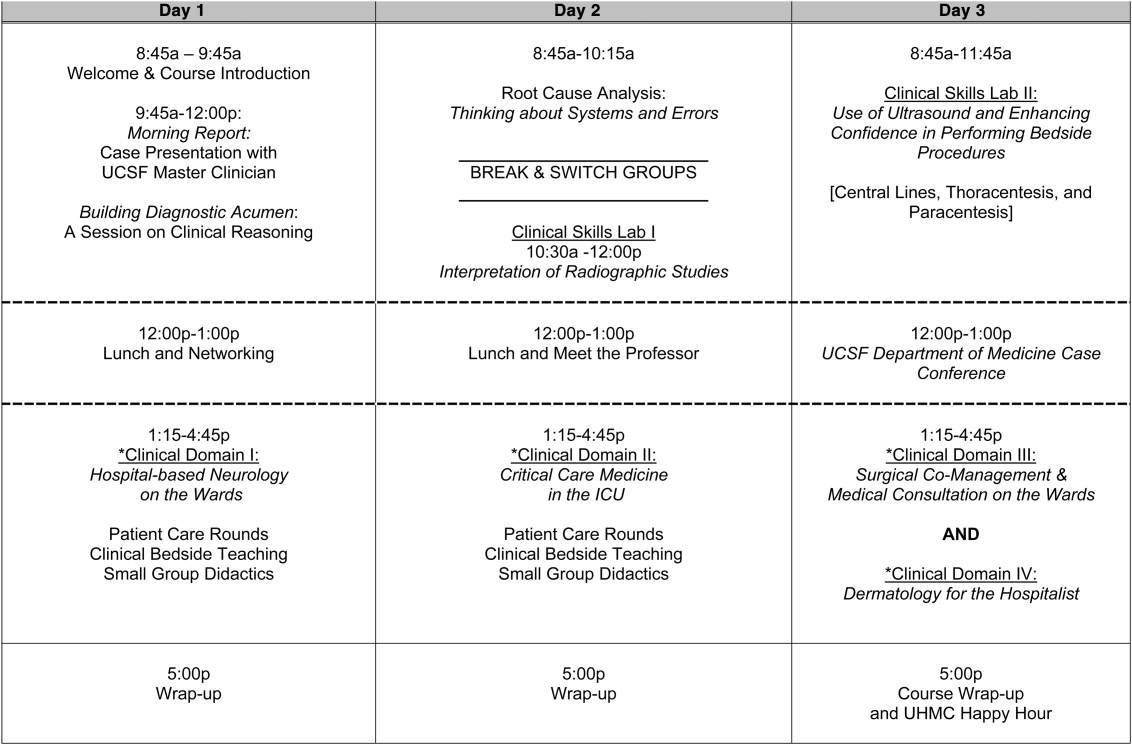
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
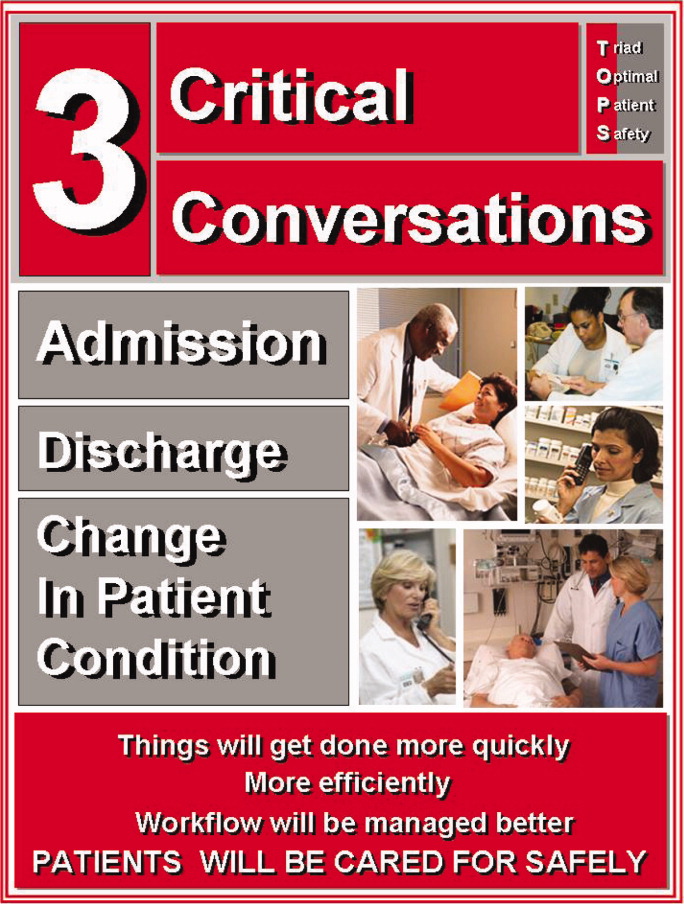
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
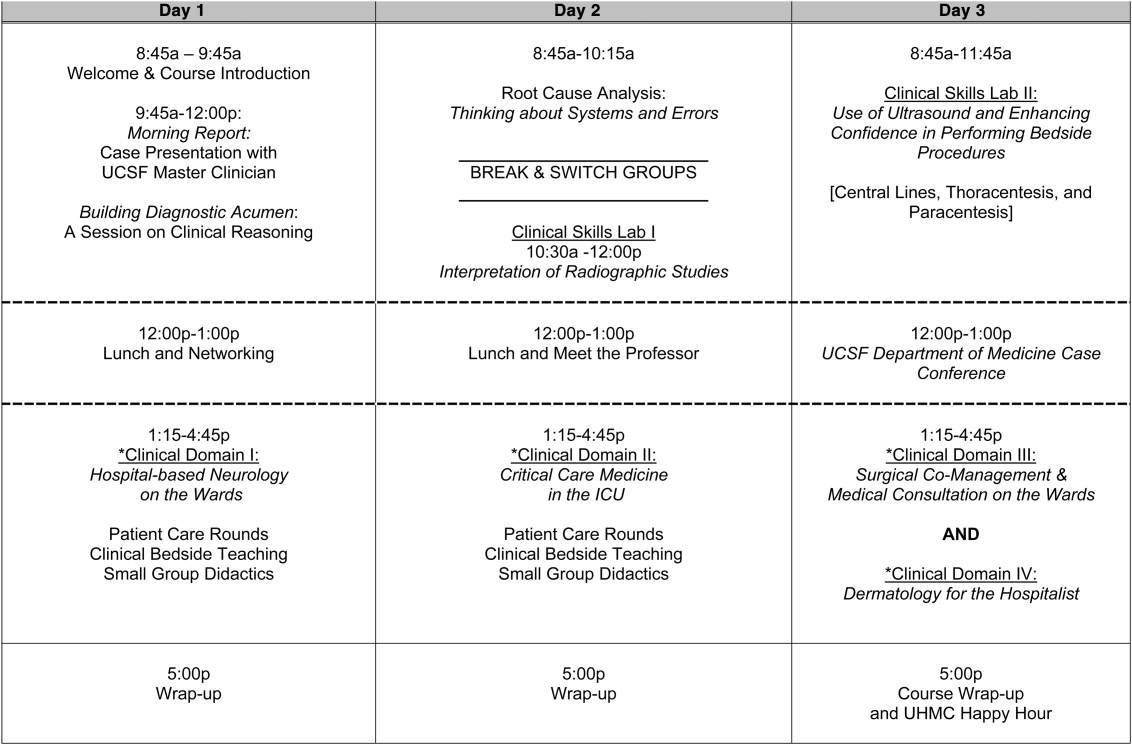
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
Teamwork in Hospitals
Teamwork is important in providing high‐quality hospital care. Despite tremendous efforts in the 10 years since publication of the Institute of Medicine's To Err is Human report,1 hospitalized patients remain at risk for adverse events (AEs).2 Although many AEs are not preventable, a large portion of those which are identified as preventable can be attributed to communication and teamwork failures.35 A Joint Commission study indicated that communication failures were the root cause for two‐thirds of the 3548 sentinel events reported from 1995 to 2005.6 Another study, involving interviews of resident physicians about recent medical mishaps, found that communication failures contributed to 91% of the AEs they reported.5
Teamwork also plays an important role in other aspects of hospital care delivery. Patients' ratings of nurse‐physician coordination correlate with their overall perception of the quality of care received.7, 8 A study of Veterans Health Administration (VHA) hospitals found that teamwork culture was significantly and positively associated with overall patient satisfaction.9 Another VHA study found that hospitals with higher teamwork culture ratings had lower nurse resignations rates.10 Furthermore, poor teamwork within hospitals may have an adverse effect on financial performance, as a result of inefficiencies in physician and nurse workflow.11
Some organizations are capable of operating in complex, hazardous environments while maintaining exceptional performance over long periods of time. These high reliability organizations (HRO) include aircraft carriers, air traffic control systems, and nuclear power plants, and are characterized by their preoccupation with failure, reluctance to simplify interpretations, sensitivity to operations, commitment to resilience, and deference to expertise.12, 13 Preoccupation with failure is manifested by an organization's efforts to avoid complacency and persist in the search for additional risks. Reluctance to simplify interpretations is exemplified by an interest in pursuing a deep understanding of the issues that arise. Sensitivity to operations is the close attention paid to input from front‐line personnel and processes. Commitment to resilience relates to an organization's ability to contain errors once they occur and mitigate harm. Deference to expertise describes the practice of having authority migrate to the people with the most expertise, regardless of rank. Collectively, these qualities produce a state of mindfulness, allowing teams to anticipate and become aware of unexpected events, yet also quickly contain and learn from them. Recent publications have highlighted the need for hospitals to learn from HROs and the teams within them.14, 15
Recognizing the importance of teamwork in hospitals, senior leadership from the American College of Physician Executives (ACPE), the American Hospital Association (AHA), the American Organization of Nurse Executives (AONE), and the Society of Hospital Medicine (SHM) established the High Performance Teams and the Hospital of the Future project. This collaborative learning effort aims to redesign care delivery to provide optimal value to hospitalized patients. As an initial step, the High Performance Teams and the Hospital of the Future project team completed a literature review related to teamwork in hospitals. The purpose of this report is to summarize the current understanding of teamwork, describe interventions designed to improve teamwork, and make practical recommendations for hospitals to assess and improve teamwork‐related performance. We approach teamwork from the hospitalized patient's perspective, and restrict our discussion to interactions occurring among healthcare professionals within the hospital. We recognize the importance of teamwork at all points in the continuum of patient care. Highly functional inpatient teams should be integrated into an overall system of coordinated and collaborative care.
TEAMWORK: DEFINITION AND CONSTRUCTS
Physicians, nurses, and other healthcare professionals spend a great deal of their time on communication and coordination of care activities.1618 In spite of this and the patient safety concerns previously noted, interpersonal communication skills and teamwork have been historically underemphasized in professional training.1922 A team is defined as 2 or more individuals with specified roles interacting adaptively, interdependently, and dynamically toward a shared and common goal.23 Elements of effective teamwork have been identified through research conducted in aviation, the military, and more recently, healthcare. Salas and colleagues have synthesized this research into 5 core components: team leadership, mutual performance monitoring, backup behavior, adaptability, and team orientation (see Table 1).23 Additionally, 3 supporting and coordinating mechanisms are essential for effective teamwork: shared mental model, closed‐loop communication, and mutual trust (see Table 1).23 High‐performing teams use these elements to develop a culture for speaking up, and situational awareness among team members. Situational awareness refers to a person's perception and understanding of their dynamic environment, and human errors often result from a lack of such awareness.24 These teamwork constructs provide the foundational basis for understanding how hospitals can identify teamwork challenges, assess team performance, and design effective interventions.
| Teamwork | Definition | Behavioral Examples |
|---|---|---|
| ||
| Component | ||
| Team leadership | The leader directs and coordinates team members activities | Facilitate team problem solving; |
| Provide performance expectations; | ||
| Clarify team member roles; | ||
| Assist in conflict resolution | ||
| Mutual performance monitoring | Team members are able to monitor one another's performance | Identify mistakes and lapses in other team member actions; |
| Provide feedback to fellow team members to facilitate self‐correction | ||
| Backup behavior | Team members anticipate and respond to one another's needs | Recognize workload distribution problem; |
| Shift work responsibilities to underutilized members | ||
| Adaptability | The team adjusts strategies based on new information | Identify cues that change has occurred and develop plan to deal with changes; |
| Remain vigilant to change in internal and external environment | ||
| Team orientation | Team members prioritize team goals above individual goals | Take into account alternate solutions by teammates; |
| Increased task involvement, information sharing, and participatory goal setting | ||
| Coordinating mechanism | ||
| Shared mental model | An organizing knowledge of the task of the team and how members will interact to achieve their goal | Anticipate and predict each other's needs; |
| Identify changes in team, task, or teammates | ||
| Closed‐loop communication | Acknowledgement and confirmation of information received | Follow up with team members to ensure message received; |
| Acknowledge that message was received; | ||
| Clarify information received | ||
| Mutual trust | Shared belief that team members will perform their roles | Share information; |
| Willingly admit mistakes and accept feedback | ||
CHALLENGES TO EFFECTIVE TEAMWORK
Several important and unique barriers to teamwork exist in hospitals. Teams are large and formed in an ad hoc fashion. On a given day, a patient's hospital team might include a hospitalist, a nurse, a case manager, a pharmacist, and 1 or more consulting physicians and therapists. Team members in each respective discipline care for multiple patients at the same time, yet few hospitals align team membership (ie, patient assignment). Therefore, a nurse caring for 4 patients may interact with 4 different hospitalists. Similarly, a hospitalist caring for 14 patients may interact with multiple nurses in a given day. Team membership is ever changing because hospital professionals work in shifts and rotations. Finally, team members are seldom in the same place at the same time because physicians often care for patients on multiple units and floors, while nurses and other team members are often unit‐based. Salas and others have noted that team size, instability, and geographic dispersion of membership serve as important barriers to improving teamwork.25, 26 As a result of these barriers, nurses and physicians do not communicate consistently, and often disagree on the daily plan of care for their patients.27, 28 When communication does occur, clinicians may overestimate how well their messages are understood by other team members, reflecting a phenomenon well known in communication psychology related to egocentric thought processes.29, 30
The traditionally steep hierarchy within medicine may also serve as a barrier to teamwork. Studies in intensive care units (ICUs), operating rooms, and general medical units reveal widely discrepant views on the quality of collaboration and communication between healthcare professionals.3133 Although physicians generally give high ratings to the quality of collaboration with nurses, nurses consistently rate the quality of collaboration with physicians as poor. Similarly, specialist physicians rate collaboration with hospitalists higher than hospitalists rate collaboration with specialists.33 Effective teams in other high‐risk industries, like aviation, strive to flatten hierarchy so that team members feel comfortable raising concerns and engaging in open and respectful communications.34
The effect of technology on communication practices and teamwork is complex and incompletely understood. The implementation of electronic heath records and computerized provider order entry systems fundamentally changes work‐flow, and may result in less synchronization and feedback during nurse‐physician collaboration.35 Similarly, the expanded use of text messages delivered via alphanumeric paging or mobile phone results in a transition toward asynchronous modes of communication. These asynchronous modes allow healthcare professionals to review and respond to messages at their convenience, and may reduce unnecessary interruptions. Research shows that these systems are popular among clinicians.3638 However, receipt and understanding of the intended message may not be confirmed with the use of asynchronous modes of communication. Moreover, important face‐to‐face communication elements (tone of voice, expression, gesture, eye contract)39, 40 are lacking. One promising approach is a system which sends low‐priority messages to a Web‐based task list for periodic review, while allowing higher priority messages to pass through to an alphanumeric pager and interrupt the intended recipient.41 Another common frustration in hospitals, despite advancing technology, is difficulty identifying the correct physician(s) and nurse(s) caring for a particular patient at a given point in time.33 Wong and colleagues found that 14% of pages in their hospital were initially sent to the wrong physician.42
ASSESSMENT OF TEAMWORK
One of the challenges in improving teamwork is the difficulty in measuring it. Teamwork assessment entails measuring the performance of teams composed of multiple individuals. Methods of teamwork assessment can be broadly categorized as self assessment, peer assessment, direct observation, survey of team climate or culture, and measurement of the outcome of effective teamwork. While self‐report tools are easy to administer and can capture affective components influencing team performance, they may not reflect actual skills on the part of individuals or teams. Peer assessment includes the use of 360‐degree evaluations or multisource feedback, and provides an evaluation of individual performance.4347
Direct observation provides a more accurate assessment of team‐related behaviors using trained observers. Observers use checklists and/or behaviorally anchored rating scales (BARS) to evaluate individual and team performance. A number of BARS have been developed and validated for the evaluation of team performance.4852 Of note, direct observation may be difficult in settings in which team members are not in the same place at the same time. An alternative method, which may be better suited for general medical units, is the use of survey instruments designed to assess attitudes and teamwork climate.5355 Importantly, higher survey ratings of collaboration and teamwork have been associated with better patient outcomes in observational studies.5658
The ultimate goal of teamwork efforts is to improve patient outcomes. Because patient outcomes are affected by a number of factors and because hospitals frequently engage in multiple, simultaneous efforts to improve care, it is often difficult to clearly link improved outcomes with teamwork interventions. Continued efforts to rigorously evaluate teamwork interventions should remain a priority, particularly as the cost of these interventions must be weighed against other interventions and investments.
EXAMPLES OF SUCCESSFUL INTERVENTIONS
A number of interventions have been used to improve teamwork in hospitals (see Table 2).
| Intervention | Advantages | Disadvantages |
|---|---|---|
| Localization of physicians | Increases frequency of nurse‐physician communication; provides foundation for additional interventions | Insufficient in creating a shared mental model; does not specifically enhance communication skills |
| Daily goals‐of‐care forms and checklists | Provides structure to interdisciplinary discussions and ensures input from all team members | May be completed in a perfunctory manner and may not be updated as plans of care evolve |
| Teamwork training | Emphasizes improved communication behaviors relevant across a range of team member interactions | Requires time and deliberate practice of new skills; effect may be attenuated if members are dispersed. |
| Interdisciplinary rounds | Provides a forum for regular interdisciplinary communication | Requires leadership to organize discussion and does not address need for updates as plans of care evolve |
Geographic Localization of Physicians
As mentioned earlier, physicians in large hospitals may care for patients on multiple units or floors. Designating certain physicians to care for patients admitted to specific units may improve efficiency and communication among healthcare professionals. One study recently reported on the effect of localization of hospital physicians to specific patient care units. Localization resulted in an increase in the rate of nurse‐physician communication, but did not improve providers' shared understanding of the plan of care.56 Notably, localizing physicians may improve the feasibility of additional interventions, like teamwork training and interdisciplinary rounds.
Daily Goals of Care and Surgery Safety Checklists
In ICU and operating room settings, physicians and nurses work in proximity, allowing interdisciplinary discussions to occur at the bedside. The finding that professionals in ICUs and operating rooms have widely discrepant views on the quality of collaboration31, 32 indicates that proximity, alone, is not sufficient for effective communication. Pronovost et al. used a daily goals form for bedside ICU rounds in an effort to standardize communication about the daily plan of care.57 The form defined essential goals of care for patients, and its use resulted in a significant improvement in the team's understanding of the daily goals. Narasimhan et al. performed a similar study using a daily goals worksheet during ICU rounds,58 and also found a significant improvement in physicians' and nurses' ratings of their understanding of the goals of care. The forms used in these studies provided structure to the interdisciplinary conversations during rounds to create a shared understanding of patients' plans of care.
Haynes and colleagues recently reported on the use of a surgical safety checklist in a large, multicenter pre‐post study.59 The checklist consisted of verbal confirmation of the completion of basic steps essential to safe care in the operating room, and provided structure to communication among surgical team members to ensure a shared understanding of the operative plan. The intervention resulted in a significant reduction in inpatient complications and mortality.
Team Training
Formalized team training, based on crew resource management, has been studied as a potential method to improve teamwork in a variety of medical settings.6062 Training emphasizes the core components of successful teamwork and essential coordinating mechanisms previously mentioned.23 Team training appears to positively influence culture, as assessed by teamwork and patient safety climate survey instruments.60 Based on these findings and extensive research demonstrating the success of teamwork training in aviation,63 the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD) have partnered in offering the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) program, designed to improve teamwork skills for healthcare professionals.64, 65
Only a handful of studies have evaluated the effectiveness of teamwork training programs on patient outcomes, and the results are mixed.66 Morey et al. found a reduction in the rate of observed errors as a result of teamwork training in emergency departments, but observers in the study were not blinded with regard to whether teams had undergone training.61 A research group in the United Kingdom evaluated the benefit of simulation‐based team training on outcomes in an obstetrical setting.67, 68 Training included management of specific complications, including shoulder dystocia and uterine cord prolapse. Using retrospective chart review, the investigators found a significant reduction in the proportion of babies born with an obstetric brachial palsy injury and a reduction in the time from diagnosis of uterine cord prolapse to infant delivery. Nielsen and colleagues also evaluated the use of teamwork training in an obstetric setting.62 In a cluster randomized controlled trial, the investigators found no reduction in the rate of adverse outcomes. Differences in the duration of teamwork training and the degree of emphasis on deliberate practice of new skills (eg, with the use of simulation‐based training) likely explains the lack of consistent results.
Very little research has evaluated teamwork training in the general medical environment.69, 70 Sehgal and colleagues recently published an evaluation of the effect of teamwork training delivered to internal medicine residents, hospitalists, nurses, pharmacists, case managers, and social workers on medical services in 3 Northern California hospitals.69 The 4‐hour training sessions covered topical areas of safety culture, teamwork, and communication through didactics, videos, facilitated discussions, and small group role plays to practice new skills and behaviors. The intervention was rated highly among participants,69 and the training along with subsequent follow‐up interventions resulted in improved patient perceptions of teamwork and communication but had no impact on key patient outcomes.71
Interdisciplinary Rounds
Interdisciplinary rounds (IDR) have been used for many years as a means to assemble team members in a single location,7275 and the use of IDR has been associated with lower mortality among ICU patients.76 Interdisciplinary rounds may be particularly useful for clinical settings in which team members are traditionally dispersed in time and place, such as medical‐surgical units. Recent studies have evaluated the effect of structured inter‐disciplinary rounds (SIDR),77, 78 which combine a structured format for communication, similar to a daily goals‐of‐care form, with a forum for daily interdisciplinary meetings. Though no effect was seen on length of stay or cost, SIDR resulted in significantly higher ratings of the quality of collaboration and teamwork climate, and a reduction in the rate of AEs.79 Importantly, the majority of clinicians in the studies agreed that SIDR improved the efficiency of their work day, and expressed a desire that SIDR continue indefinitely. Many investigators have emphasized the importance of leadership during IDR, often by a medical director, nurse manager, or both.74, 77, 78
Summary of Interventions to Improve Teamwork
Localization of physicians increases the frequency of nurse‐physician communication, but is insufficient in creating a shared understanding of patients' plans of care. Providing structure for the discussion among team members (eg, daily goals of care forms and checklists) ensures that critical elements of the plan of care are communicated. Teamwork training is based upon a strong foundation of research both inside and outside of healthcare, and has demonstrated improved knowledge of teamwork principles, attitudes about the importance of teamwork, and overall safety climate. Creating a forum for team members to assemble and discuss their patients (eg, IDR) can overcome some of the unique barriers to collaboration in settings where members are dispersed in time and space. Leaders wishing to improve interdisciplinary teamwork should consider implementing a combination of complementary interventions. For example, localization may increase the frequency of team member interactions, the quality of which may be enhanced with teamwork training and reinforced with the use of structured communication tools and IDR. Future research should evaluate the effect of these combined interventions.
CONCLUSIONS
In summary, teamwork is critically important to provide safe and effective care. Important and unique barriers to teamwork exist in hospitals. We recommend the use of survey instruments, such as those mentioned earlier, as the most feasible method to assess teamwork in the general medical setting. Because each intervention addresses only a portion of the barriers to optimal teamwork, we encourage leaders to use a multifaceted approach. We recommend the implementation of a combination of interventions with adaptations to fit unique clinical settings and local culture.
Acknowledgements
This manuscript was prepared as part of the High Performance Teams and the Hospital of the Future project, a collaborative effort including senior leadership from the American College of Physician Executives, the American Hospital Association, the American Organization of Nurse Executives, and the Society of Hospital Medicine. The authors thank Taylor Marsh for her administrative support and help in coordinating project meetings.
- To Err Is Human: Building a Safer Health System.Washington, DC:Institute of Medicine;1999.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,.Exploring the causes of adverse events in NHS hospital practice.J R Soc Med.2001;94(7):322–330.
- ,,,,,.The Quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety 2007. Available at: http://www.jointcommissionreport.org. Accessed November2007.
- ,,.Patient perceptions of coordinated care: the importance of organized communication in hospitals.J Healthc Qual.1999;21(5):18–23.
- ,,.Am I safe here? Improving patients' perceptions of safety in hospitals.J Nurs Care Qual.2006;21(1):30–40.
- ,,.Teamwork culture and patient satisfaction in hospitals.Med Care.2004;42(5):492–498.
- ,,.The influence of teamwork culture on physician and nurse resignation rates in hospitals.Health Serv Manage Res.2008;21(1):23–31.
- ,,.Quantifying the economic impact of communication inefficiencies in U.S. hospitals.J Healthc Manag.2010;55(4):265–282.
- ,.Managing the Unexpected: Assuring High Performance in an Age of Complexity.San Francisco, CA:Jossey‐Bass;2001.
- .Some characteristics of high reliability organizations.Organization Science.1990;1(2):160–177.
- ,,.Teamwork as an essential component of high‐reliability organizations.Health Serv Res.2006;41(4 pt 2):1576–1598.
- ,,,.Promoting health care safety through training high reliability teams.Qual Saf Health Care.2005;14(4):303–309.
- ,,,,,.Analyzing the time and value of housestaff inpatient work.J Gen Intern Med.1998;13(8):534–540.
- ,,, et al.Quantifying nursing workflow in medication administration.J Nurs Adm.2008;38(1):19–26.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.The role of teamwork in the professional education of physicians: current status and assessment recommendations.Jt Comm J Qual Patient Saf.2005;31(4):185–202.
- ,,.Is there a “big five” in teamwork?Small Group Research.2005;36:555–599.
- ,,.Objective measures of situation awareness in a simulated medical environment.Qual Saf Health Care.2004;13(suppl 1):i65–i71.
- ,.What do we know about health care team effectiveness? A review of the literature.Med Care Res Rev.2006;63(3):263–300.
- ,,, et al.Does team training improve team performance? A meta‐analysis.Hum Factors.2008;50(6):903–933.
- ,,,,,.Can we talk? Priorities for patient care differed among health care providers. AHRQ Publication No. 05–0021‐1.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,, et al.Patterns of nurse–physicians communication and agreement on the plan of care.Qual Saf Health Care.2010;19:195–199.
- ,,,,.Interns overestimate the effectiveness of their hand‐off communication.Pediatrics.2010;125(3):491–496.
- ,.Speakers' overestimation of their effectiveness.Psychol Sci.2002;13(3):207–212.
- ,,, et al.Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- ,,.Discrepant attitudes about teamwork among critical care nurses and physicians.Crit Care Med.2003;31(3):956–959.
- ,,,,,.Teamwork on inpatient medical units: assessing attitudes and barriers.Qual Saf Health Care.2010;19(2):117–121.
- ,,.Error, stress, and teamwork in medicine and aviation: cross sectional surveys.BMJ.2000;320(7237):745–749.
- ,,,,.Impact of a computerized physician order entry system on nurse‐physician collaboration in the medication process.Int J Med Inform.2008;77(11):735–744.
- ,,,,.Alphanumeric paging in an academic hospital setting.Am J Surg.2006;191(4):561–565.
- ,,,.Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service.J Hosp Med.2009;4(8):E34–E40.
- ,,, et al.The use of smartphones for clinical communication on internal medicine wards.J Hosp Med.2010;5(9):553–559.
- ,.Organizational information requirements, media richness, and structural design.Management Science.1986;32(5):554–571.
- ,.Decoding of inconsistent communications of personality and social psychology.J Pers Soc Psychol.1967;6(1):109–114.
- ,,,,.Beyond paging: building a Web‐based communication tool for nurses and physicians.J Gen Intern Med.2009;24(1):105–110.
- ,,, et al.Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Evaluation of resident communication skills and professionalism: a matter of perspective?Pediatrics.2006;118(4):1371–1379.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- .Multisource feedback in the assessment of physician competencies.J Contin Educ Health Prof.2003;23(1):4–12.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' Non‐Technical Skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,,.Using the Communication and Teamwork Skills (CATS) Assessment to measure health care team performance.Jt Comm J Qual Patient Saf.2007;33(9):549–558.
- ,,, et al.The Mayo High Performance Teamwork Scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,, et al.The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research.BMC Health Serv Res.2006;6:44.
- .Development of an instrument to measure collaboration and satisfaction about care decisions.J Adv Nurs.1994;20(1):176–182.
- ,,,,,.Psychometric properties of an attitude scale measuring physician‐nurse collaboration.Eval Health Prof.1999;22(2):208–220.
- ,,, et al.Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care.J Gen Intern Med.2009;24(11):1223–1227.
- ,,,,,.Improving communication in the ICU using daily goals.J Crit Care.2003;18(2):71–75.
- ,,,,.Improving nurse‐physician communication and satisfaction in the intensive care unit with a daily goals worksheet.Am J Crit Care.2006;15(2):217–222.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,, et al.Effect of crew resource management training in a multidisciplinary obstetrical setting.Int J Qual Health Care.2008;20(4):254–263.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial.Obstet Gynecol.2007;109(1):48–55.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- Agency for Healthcare Research and Quality. TeamSTEPPS Home. Available at: http://teamstepps.ahrq.gov/index.htm. Accessed January 18,2010.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48(2):392–412.
- ,,, et al.Improving neonatal outcome through practical shoulder dystocia training.Obstet Gynecol.2008;112(1):14–20.
- ,,, et al.Retrospective cohort study of diagnosis‐delivery interval with umbilical cord prolapse: the effect of team training.Br J Obstet Gynaecol.2009;116(8):1089–1096.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,,,.Teambuilding and leadership training in an internal medicine residency training program.J Gen Intern Med.2004;19(6):692–697.
- ,,, et al. Effects of a multicenter teamwork and communication program on patient outcomes: results from the Triad for Optimal Patient Safety (TOPS) project. In press.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,.A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement.Med Care.1998;36(8 suppl):AS4–A12.
- ,,,,.Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay.J Gen Intern Med.2007;22(8):1073–1079.
- ,,,.Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses.Am J Crit Care.2005;14(1):71–77.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit.J Hosp Med.2011;6(2):88–93.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit.J Gen Intern Med.2010;25(8):826–832.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
Teamwork is important in providing high‐quality hospital care. Despite tremendous efforts in the 10 years since publication of the Institute of Medicine's To Err is Human report,1 hospitalized patients remain at risk for adverse events (AEs).2 Although many AEs are not preventable, a large portion of those which are identified as preventable can be attributed to communication and teamwork failures.35 A Joint Commission study indicated that communication failures were the root cause for two‐thirds of the 3548 sentinel events reported from 1995 to 2005.6 Another study, involving interviews of resident physicians about recent medical mishaps, found that communication failures contributed to 91% of the AEs they reported.5
Teamwork also plays an important role in other aspects of hospital care delivery. Patients' ratings of nurse‐physician coordination correlate with their overall perception of the quality of care received.7, 8 A study of Veterans Health Administration (VHA) hospitals found that teamwork culture was significantly and positively associated with overall patient satisfaction.9 Another VHA study found that hospitals with higher teamwork culture ratings had lower nurse resignations rates.10 Furthermore, poor teamwork within hospitals may have an adverse effect on financial performance, as a result of inefficiencies in physician and nurse workflow.11
Some organizations are capable of operating in complex, hazardous environments while maintaining exceptional performance over long periods of time. These high reliability organizations (HRO) include aircraft carriers, air traffic control systems, and nuclear power plants, and are characterized by their preoccupation with failure, reluctance to simplify interpretations, sensitivity to operations, commitment to resilience, and deference to expertise.12, 13 Preoccupation with failure is manifested by an organization's efforts to avoid complacency and persist in the search for additional risks. Reluctance to simplify interpretations is exemplified by an interest in pursuing a deep understanding of the issues that arise. Sensitivity to operations is the close attention paid to input from front‐line personnel and processes. Commitment to resilience relates to an organization's ability to contain errors once they occur and mitigate harm. Deference to expertise describes the practice of having authority migrate to the people with the most expertise, regardless of rank. Collectively, these qualities produce a state of mindfulness, allowing teams to anticipate and become aware of unexpected events, yet also quickly contain and learn from them. Recent publications have highlighted the need for hospitals to learn from HROs and the teams within them.14, 15
Recognizing the importance of teamwork in hospitals, senior leadership from the American College of Physician Executives (ACPE), the American Hospital Association (AHA), the American Organization of Nurse Executives (AONE), and the Society of Hospital Medicine (SHM) established the High Performance Teams and the Hospital of the Future project. This collaborative learning effort aims to redesign care delivery to provide optimal value to hospitalized patients. As an initial step, the High Performance Teams and the Hospital of the Future project team completed a literature review related to teamwork in hospitals. The purpose of this report is to summarize the current understanding of teamwork, describe interventions designed to improve teamwork, and make practical recommendations for hospitals to assess and improve teamwork‐related performance. We approach teamwork from the hospitalized patient's perspective, and restrict our discussion to interactions occurring among healthcare professionals within the hospital. We recognize the importance of teamwork at all points in the continuum of patient care. Highly functional inpatient teams should be integrated into an overall system of coordinated and collaborative care.
TEAMWORK: DEFINITION AND CONSTRUCTS
Physicians, nurses, and other healthcare professionals spend a great deal of their time on communication and coordination of care activities.1618 In spite of this and the patient safety concerns previously noted, interpersonal communication skills and teamwork have been historically underemphasized in professional training.1922 A team is defined as 2 or more individuals with specified roles interacting adaptively, interdependently, and dynamically toward a shared and common goal.23 Elements of effective teamwork have been identified through research conducted in aviation, the military, and more recently, healthcare. Salas and colleagues have synthesized this research into 5 core components: team leadership, mutual performance monitoring, backup behavior, adaptability, and team orientation (see Table 1).23 Additionally, 3 supporting and coordinating mechanisms are essential for effective teamwork: shared mental model, closed‐loop communication, and mutual trust (see Table 1).23 High‐performing teams use these elements to develop a culture for speaking up, and situational awareness among team members. Situational awareness refers to a person's perception and understanding of their dynamic environment, and human errors often result from a lack of such awareness.24 These teamwork constructs provide the foundational basis for understanding how hospitals can identify teamwork challenges, assess team performance, and design effective interventions.
| Teamwork | Definition | Behavioral Examples |
|---|---|---|
| ||
| Component | ||
| Team leadership | The leader directs and coordinates team members activities | Facilitate team problem solving; |
| Provide performance expectations; | ||
| Clarify team member roles; | ||
| Assist in conflict resolution | ||
| Mutual performance monitoring | Team members are able to monitor one another's performance | Identify mistakes and lapses in other team member actions; |
| Provide feedback to fellow team members to facilitate self‐correction | ||
| Backup behavior | Team members anticipate and respond to one another's needs | Recognize workload distribution problem; |
| Shift work responsibilities to underutilized members | ||
| Adaptability | The team adjusts strategies based on new information | Identify cues that change has occurred and develop plan to deal with changes; |
| Remain vigilant to change in internal and external environment | ||
| Team orientation | Team members prioritize team goals above individual goals | Take into account alternate solutions by teammates; |
| Increased task involvement, information sharing, and participatory goal setting | ||
| Coordinating mechanism | ||
| Shared mental model | An organizing knowledge of the task of the team and how members will interact to achieve their goal | Anticipate and predict each other's needs; |
| Identify changes in team, task, or teammates | ||
| Closed‐loop communication | Acknowledgement and confirmation of information received | Follow up with team members to ensure message received; |
| Acknowledge that message was received; | ||
| Clarify information received | ||
| Mutual trust | Shared belief that team members will perform their roles | Share information; |
| Willingly admit mistakes and accept feedback | ||
CHALLENGES TO EFFECTIVE TEAMWORK
Several important and unique barriers to teamwork exist in hospitals. Teams are large and formed in an ad hoc fashion. On a given day, a patient's hospital team might include a hospitalist, a nurse, a case manager, a pharmacist, and 1 or more consulting physicians and therapists. Team members in each respective discipline care for multiple patients at the same time, yet few hospitals align team membership (ie, patient assignment). Therefore, a nurse caring for 4 patients may interact with 4 different hospitalists. Similarly, a hospitalist caring for 14 patients may interact with multiple nurses in a given day. Team membership is ever changing because hospital professionals work in shifts and rotations. Finally, team members are seldom in the same place at the same time because physicians often care for patients on multiple units and floors, while nurses and other team members are often unit‐based. Salas and others have noted that team size, instability, and geographic dispersion of membership serve as important barriers to improving teamwork.25, 26 As a result of these barriers, nurses and physicians do not communicate consistently, and often disagree on the daily plan of care for their patients.27, 28 When communication does occur, clinicians may overestimate how well their messages are understood by other team members, reflecting a phenomenon well known in communication psychology related to egocentric thought processes.29, 30
The traditionally steep hierarchy within medicine may also serve as a barrier to teamwork. Studies in intensive care units (ICUs), operating rooms, and general medical units reveal widely discrepant views on the quality of collaboration and communication between healthcare professionals.3133 Although physicians generally give high ratings to the quality of collaboration with nurses, nurses consistently rate the quality of collaboration with physicians as poor. Similarly, specialist physicians rate collaboration with hospitalists higher than hospitalists rate collaboration with specialists.33 Effective teams in other high‐risk industries, like aviation, strive to flatten hierarchy so that team members feel comfortable raising concerns and engaging in open and respectful communications.34
The effect of technology on communication practices and teamwork is complex and incompletely understood. The implementation of electronic heath records and computerized provider order entry systems fundamentally changes work‐flow, and may result in less synchronization and feedback during nurse‐physician collaboration.35 Similarly, the expanded use of text messages delivered via alphanumeric paging or mobile phone results in a transition toward asynchronous modes of communication. These asynchronous modes allow healthcare professionals to review and respond to messages at their convenience, and may reduce unnecessary interruptions. Research shows that these systems are popular among clinicians.3638 However, receipt and understanding of the intended message may not be confirmed with the use of asynchronous modes of communication. Moreover, important face‐to‐face communication elements (tone of voice, expression, gesture, eye contract)39, 40 are lacking. One promising approach is a system which sends low‐priority messages to a Web‐based task list for periodic review, while allowing higher priority messages to pass through to an alphanumeric pager and interrupt the intended recipient.41 Another common frustration in hospitals, despite advancing technology, is difficulty identifying the correct physician(s) and nurse(s) caring for a particular patient at a given point in time.33 Wong and colleagues found that 14% of pages in their hospital were initially sent to the wrong physician.42
ASSESSMENT OF TEAMWORK
One of the challenges in improving teamwork is the difficulty in measuring it. Teamwork assessment entails measuring the performance of teams composed of multiple individuals. Methods of teamwork assessment can be broadly categorized as self assessment, peer assessment, direct observation, survey of team climate or culture, and measurement of the outcome of effective teamwork. While self‐report tools are easy to administer and can capture affective components influencing team performance, they may not reflect actual skills on the part of individuals or teams. Peer assessment includes the use of 360‐degree evaluations or multisource feedback, and provides an evaluation of individual performance.4347
Direct observation provides a more accurate assessment of team‐related behaviors using trained observers. Observers use checklists and/or behaviorally anchored rating scales (BARS) to evaluate individual and team performance. A number of BARS have been developed and validated for the evaluation of team performance.4852 Of note, direct observation may be difficult in settings in which team members are not in the same place at the same time. An alternative method, which may be better suited for general medical units, is the use of survey instruments designed to assess attitudes and teamwork climate.5355 Importantly, higher survey ratings of collaboration and teamwork have been associated with better patient outcomes in observational studies.5658
The ultimate goal of teamwork efforts is to improve patient outcomes. Because patient outcomes are affected by a number of factors and because hospitals frequently engage in multiple, simultaneous efforts to improve care, it is often difficult to clearly link improved outcomes with teamwork interventions. Continued efforts to rigorously evaluate teamwork interventions should remain a priority, particularly as the cost of these interventions must be weighed against other interventions and investments.
EXAMPLES OF SUCCESSFUL INTERVENTIONS
A number of interventions have been used to improve teamwork in hospitals (see Table 2).
| Intervention | Advantages | Disadvantages |
|---|---|---|
| Localization of physicians | Increases frequency of nurse‐physician communication; provides foundation for additional interventions | Insufficient in creating a shared mental model; does not specifically enhance communication skills |
| Daily goals‐of‐care forms and checklists | Provides structure to interdisciplinary discussions and ensures input from all team members | May be completed in a perfunctory manner and may not be updated as plans of care evolve |
| Teamwork training | Emphasizes improved communication behaviors relevant across a range of team member interactions | Requires time and deliberate practice of new skills; effect may be attenuated if members are dispersed. |
| Interdisciplinary rounds | Provides a forum for regular interdisciplinary communication | Requires leadership to organize discussion and does not address need for updates as plans of care evolve |
Geographic Localization of Physicians
As mentioned earlier, physicians in large hospitals may care for patients on multiple units or floors. Designating certain physicians to care for patients admitted to specific units may improve efficiency and communication among healthcare professionals. One study recently reported on the effect of localization of hospital physicians to specific patient care units. Localization resulted in an increase in the rate of nurse‐physician communication, but did not improve providers' shared understanding of the plan of care.56 Notably, localizing physicians may improve the feasibility of additional interventions, like teamwork training and interdisciplinary rounds.
Daily Goals of Care and Surgery Safety Checklists
In ICU and operating room settings, physicians and nurses work in proximity, allowing interdisciplinary discussions to occur at the bedside. The finding that professionals in ICUs and operating rooms have widely discrepant views on the quality of collaboration31, 32 indicates that proximity, alone, is not sufficient for effective communication. Pronovost et al. used a daily goals form for bedside ICU rounds in an effort to standardize communication about the daily plan of care.57 The form defined essential goals of care for patients, and its use resulted in a significant improvement in the team's understanding of the daily goals. Narasimhan et al. performed a similar study using a daily goals worksheet during ICU rounds,58 and also found a significant improvement in physicians' and nurses' ratings of their understanding of the goals of care. The forms used in these studies provided structure to the interdisciplinary conversations during rounds to create a shared understanding of patients' plans of care.
Haynes and colleagues recently reported on the use of a surgical safety checklist in a large, multicenter pre‐post study.59 The checklist consisted of verbal confirmation of the completion of basic steps essential to safe care in the operating room, and provided structure to communication among surgical team members to ensure a shared understanding of the operative plan. The intervention resulted in a significant reduction in inpatient complications and mortality.
Team Training
Formalized team training, based on crew resource management, has been studied as a potential method to improve teamwork in a variety of medical settings.6062 Training emphasizes the core components of successful teamwork and essential coordinating mechanisms previously mentioned.23 Team training appears to positively influence culture, as assessed by teamwork and patient safety climate survey instruments.60 Based on these findings and extensive research demonstrating the success of teamwork training in aviation,63 the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD) have partnered in offering the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) program, designed to improve teamwork skills for healthcare professionals.64, 65
Only a handful of studies have evaluated the effectiveness of teamwork training programs on patient outcomes, and the results are mixed.66 Morey et al. found a reduction in the rate of observed errors as a result of teamwork training in emergency departments, but observers in the study were not blinded with regard to whether teams had undergone training.61 A research group in the United Kingdom evaluated the benefit of simulation‐based team training on outcomes in an obstetrical setting.67, 68 Training included management of specific complications, including shoulder dystocia and uterine cord prolapse. Using retrospective chart review, the investigators found a significant reduction in the proportion of babies born with an obstetric brachial palsy injury and a reduction in the time from diagnosis of uterine cord prolapse to infant delivery. Nielsen and colleagues also evaluated the use of teamwork training in an obstetric setting.62 In a cluster randomized controlled trial, the investigators found no reduction in the rate of adverse outcomes. Differences in the duration of teamwork training and the degree of emphasis on deliberate practice of new skills (eg, with the use of simulation‐based training) likely explains the lack of consistent results.
Very little research has evaluated teamwork training in the general medical environment.69, 70 Sehgal and colleagues recently published an evaluation of the effect of teamwork training delivered to internal medicine residents, hospitalists, nurses, pharmacists, case managers, and social workers on medical services in 3 Northern California hospitals.69 The 4‐hour training sessions covered topical areas of safety culture, teamwork, and communication through didactics, videos, facilitated discussions, and small group role plays to practice new skills and behaviors. The intervention was rated highly among participants,69 and the training along with subsequent follow‐up interventions resulted in improved patient perceptions of teamwork and communication but had no impact on key patient outcomes.71
Interdisciplinary Rounds
Interdisciplinary rounds (IDR) have been used for many years as a means to assemble team members in a single location,7275 and the use of IDR has been associated with lower mortality among ICU patients.76 Interdisciplinary rounds may be particularly useful for clinical settings in which team members are traditionally dispersed in time and place, such as medical‐surgical units. Recent studies have evaluated the effect of structured inter‐disciplinary rounds (SIDR),77, 78 which combine a structured format for communication, similar to a daily goals‐of‐care form, with a forum for daily interdisciplinary meetings. Though no effect was seen on length of stay or cost, SIDR resulted in significantly higher ratings of the quality of collaboration and teamwork climate, and a reduction in the rate of AEs.79 Importantly, the majority of clinicians in the studies agreed that SIDR improved the efficiency of their work day, and expressed a desire that SIDR continue indefinitely. Many investigators have emphasized the importance of leadership during IDR, often by a medical director, nurse manager, or both.74, 77, 78
Summary of Interventions to Improve Teamwork
Localization of physicians increases the frequency of nurse‐physician communication, but is insufficient in creating a shared understanding of patients' plans of care. Providing structure for the discussion among team members (eg, daily goals of care forms and checklists) ensures that critical elements of the plan of care are communicated. Teamwork training is based upon a strong foundation of research both inside and outside of healthcare, and has demonstrated improved knowledge of teamwork principles, attitudes about the importance of teamwork, and overall safety climate. Creating a forum for team members to assemble and discuss their patients (eg, IDR) can overcome some of the unique barriers to collaboration in settings where members are dispersed in time and space. Leaders wishing to improve interdisciplinary teamwork should consider implementing a combination of complementary interventions. For example, localization may increase the frequency of team member interactions, the quality of which may be enhanced with teamwork training and reinforced with the use of structured communication tools and IDR. Future research should evaluate the effect of these combined interventions.
CONCLUSIONS
In summary, teamwork is critically important to provide safe and effective care. Important and unique barriers to teamwork exist in hospitals. We recommend the use of survey instruments, such as those mentioned earlier, as the most feasible method to assess teamwork in the general medical setting. Because each intervention addresses only a portion of the barriers to optimal teamwork, we encourage leaders to use a multifaceted approach. We recommend the implementation of a combination of interventions with adaptations to fit unique clinical settings and local culture.
Acknowledgements
This manuscript was prepared as part of the High Performance Teams and the Hospital of the Future project, a collaborative effort including senior leadership from the American College of Physician Executives, the American Hospital Association, the American Organization of Nurse Executives, and the Society of Hospital Medicine. The authors thank Taylor Marsh for her administrative support and help in coordinating project meetings.
Teamwork is important in providing high‐quality hospital care. Despite tremendous efforts in the 10 years since publication of the Institute of Medicine's To Err is Human report,1 hospitalized patients remain at risk for adverse events (AEs).2 Although many AEs are not preventable, a large portion of those which are identified as preventable can be attributed to communication and teamwork failures.35 A Joint Commission study indicated that communication failures were the root cause for two‐thirds of the 3548 sentinel events reported from 1995 to 2005.6 Another study, involving interviews of resident physicians about recent medical mishaps, found that communication failures contributed to 91% of the AEs they reported.5
Teamwork also plays an important role in other aspects of hospital care delivery. Patients' ratings of nurse‐physician coordination correlate with their overall perception of the quality of care received.7, 8 A study of Veterans Health Administration (VHA) hospitals found that teamwork culture was significantly and positively associated with overall patient satisfaction.9 Another VHA study found that hospitals with higher teamwork culture ratings had lower nurse resignations rates.10 Furthermore, poor teamwork within hospitals may have an adverse effect on financial performance, as a result of inefficiencies in physician and nurse workflow.11
Some organizations are capable of operating in complex, hazardous environments while maintaining exceptional performance over long periods of time. These high reliability organizations (HRO) include aircraft carriers, air traffic control systems, and nuclear power plants, and are characterized by their preoccupation with failure, reluctance to simplify interpretations, sensitivity to operations, commitment to resilience, and deference to expertise.12, 13 Preoccupation with failure is manifested by an organization's efforts to avoid complacency and persist in the search for additional risks. Reluctance to simplify interpretations is exemplified by an interest in pursuing a deep understanding of the issues that arise. Sensitivity to operations is the close attention paid to input from front‐line personnel and processes. Commitment to resilience relates to an organization's ability to contain errors once they occur and mitigate harm. Deference to expertise describes the practice of having authority migrate to the people with the most expertise, regardless of rank. Collectively, these qualities produce a state of mindfulness, allowing teams to anticipate and become aware of unexpected events, yet also quickly contain and learn from them. Recent publications have highlighted the need for hospitals to learn from HROs and the teams within them.14, 15
Recognizing the importance of teamwork in hospitals, senior leadership from the American College of Physician Executives (ACPE), the American Hospital Association (AHA), the American Organization of Nurse Executives (AONE), and the Society of Hospital Medicine (SHM) established the High Performance Teams and the Hospital of the Future project. This collaborative learning effort aims to redesign care delivery to provide optimal value to hospitalized patients. As an initial step, the High Performance Teams and the Hospital of the Future project team completed a literature review related to teamwork in hospitals. The purpose of this report is to summarize the current understanding of teamwork, describe interventions designed to improve teamwork, and make practical recommendations for hospitals to assess and improve teamwork‐related performance. We approach teamwork from the hospitalized patient's perspective, and restrict our discussion to interactions occurring among healthcare professionals within the hospital. We recognize the importance of teamwork at all points in the continuum of patient care. Highly functional inpatient teams should be integrated into an overall system of coordinated and collaborative care.
TEAMWORK: DEFINITION AND CONSTRUCTS
Physicians, nurses, and other healthcare professionals spend a great deal of their time on communication and coordination of care activities.1618 In spite of this and the patient safety concerns previously noted, interpersonal communication skills and teamwork have been historically underemphasized in professional training.1922 A team is defined as 2 or more individuals with specified roles interacting adaptively, interdependently, and dynamically toward a shared and common goal.23 Elements of effective teamwork have been identified through research conducted in aviation, the military, and more recently, healthcare. Salas and colleagues have synthesized this research into 5 core components: team leadership, mutual performance monitoring, backup behavior, adaptability, and team orientation (see Table 1).23 Additionally, 3 supporting and coordinating mechanisms are essential for effective teamwork: shared mental model, closed‐loop communication, and mutual trust (see Table 1).23 High‐performing teams use these elements to develop a culture for speaking up, and situational awareness among team members. Situational awareness refers to a person's perception and understanding of their dynamic environment, and human errors often result from a lack of such awareness.24 These teamwork constructs provide the foundational basis for understanding how hospitals can identify teamwork challenges, assess team performance, and design effective interventions.
| Teamwork | Definition | Behavioral Examples |
|---|---|---|
| ||
| Component | ||
| Team leadership | The leader directs and coordinates team members activities | Facilitate team problem solving; |
| Provide performance expectations; | ||
| Clarify team member roles; | ||
| Assist in conflict resolution | ||
| Mutual performance monitoring | Team members are able to monitor one another's performance | Identify mistakes and lapses in other team member actions; |
| Provide feedback to fellow team members to facilitate self‐correction | ||
| Backup behavior | Team members anticipate and respond to one another's needs | Recognize workload distribution problem; |
| Shift work responsibilities to underutilized members | ||
| Adaptability | The team adjusts strategies based on new information | Identify cues that change has occurred and develop plan to deal with changes; |
| Remain vigilant to change in internal and external environment | ||
| Team orientation | Team members prioritize team goals above individual goals | Take into account alternate solutions by teammates; |
| Increased task involvement, information sharing, and participatory goal setting | ||
| Coordinating mechanism | ||
| Shared mental model | An organizing knowledge of the task of the team and how members will interact to achieve their goal | Anticipate and predict each other's needs; |
| Identify changes in team, task, or teammates | ||
| Closed‐loop communication | Acknowledgement and confirmation of information received | Follow up with team members to ensure message received; |
| Acknowledge that message was received; | ||
| Clarify information received | ||
| Mutual trust | Shared belief that team members will perform their roles | Share information; |
| Willingly admit mistakes and accept feedback | ||
CHALLENGES TO EFFECTIVE TEAMWORK
Several important and unique barriers to teamwork exist in hospitals. Teams are large and formed in an ad hoc fashion. On a given day, a patient's hospital team might include a hospitalist, a nurse, a case manager, a pharmacist, and 1 or more consulting physicians and therapists. Team members in each respective discipline care for multiple patients at the same time, yet few hospitals align team membership (ie, patient assignment). Therefore, a nurse caring for 4 patients may interact with 4 different hospitalists. Similarly, a hospitalist caring for 14 patients may interact with multiple nurses in a given day. Team membership is ever changing because hospital professionals work in shifts and rotations. Finally, team members are seldom in the same place at the same time because physicians often care for patients on multiple units and floors, while nurses and other team members are often unit‐based. Salas and others have noted that team size, instability, and geographic dispersion of membership serve as important barriers to improving teamwork.25, 26 As a result of these barriers, nurses and physicians do not communicate consistently, and often disagree on the daily plan of care for their patients.27, 28 When communication does occur, clinicians may overestimate how well their messages are understood by other team members, reflecting a phenomenon well known in communication psychology related to egocentric thought processes.29, 30
The traditionally steep hierarchy within medicine may also serve as a barrier to teamwork. Studies in intensive care units (ICUs), operating rooms, and general medical units reveal widely discrepant views on the quality of collaboration and communication between healthcare professionals.3133 Although physicians generally give high ratings to the quality of collaboration with nurses, nurses consistently rate the quality of collaboration with physicians as poor. Similarly, specialist physicians rate collaboration with hospitalists higher than hospitalists rate collaboration with specialists.33 Effective teams in other high‐risk industries, like aviation, strive to flatten hierarchy so that team members feel comfortable raising concerns and engaging in open and respectful communications.34
The effect of technology on communication practices and teamwork is complex and incompletely understood. The implementation of electronic heath records and computerized provider order entry systems fundamentally changes work‐flow, and may result in less synchronization and feedback during nurse‐physician collaboration.35 Similarly, the expanded use of text messages delivered via alphanumeric paging or mobile phone results in a transition toward asynchronous modes of communication. These asynchronous modes allow healthcare professionals to review and respond to messages at their convenience, and may reduce unnecessary interruptions. Research shows that these systems are popular among clinicians.3638 However, receipt and understanding of the intended message may not be confirmed with the use of asynchronous modes of communication. Moreover, important face‐to‐face communication elements (tone of voice, expression, gesture, eye contract)39, 40 are lacking. One promising approach is a system which sends low‐priority messages to a Web‐based task list for periodic review, while allowing higher priority messages to pass through to an alphanumeric pager and interrupt the intended recipient.41 Another common frustration in hospitals, despite advancing technology, is difficulty identifying the correct physician(s) and nurse(s) caring for a particular patient at a given point in time.33 Wong and colleagues found that 14% of pages in their hospital were initially sent to the wrong physician.42
ASSESSMENT OF TEAMWORK
One of the challenges in improving teamwork is the difficulty in measuring it. Teamwork assessment entails measuring the performance of teams composed of multiple individuals. Methods of teamwork assessment can be broadly categorized as self assessment, peer assessment, direct observation, survey of team climate or culture, and measurement of the outcome of effective teamwork. While self‐report tools are easy to administer and can capture affective components influencing team performance, they may not reflect actual skills on the part of individuals or teams. Peer assessment includes the use of 360‐degree evaluations or multisource feedback, and provides an evaluation of individual performance.4347
Direct observation provides a more accurate assessment of team‐related behaviors using trained observers. Observers use checklists and/or behaviorally anchored rating scales (BARS) to evaluate individual and team performance. A number of BARS have been developed and validated for the evaluation of team performance.4852 Of note, direct observation may be difficult in settings in which team members are not in the same place at the same time. An alternative method, which may be better suited for general medical units, is the use of survey instruments designed to assess attitudes and teamwork climate.5355 Importantly, higher survey ratings of collaboration and teamwork have been associated with better patient outcomes in observational studies.5658
The ultimate goal of teamwork efforts is to improve patient outcomes. Because patient outcomes are affected by a number of factors and because hospitals frequently engage in multiple, simultaneous efforts to improve care, it is often difficult to clearly link improved outcomes with teamwork interventions. Continued efforts to rigorously evaluate teamwork interventions should remain a priority, particularly as the cost of these interventions must be weighed against other interventions and investments.
EXAMPLES OF SUCCESSFUL INTERVENTIONS
A number of interventions have been used to improve teamwork in hospitals (see Table 2).
| Intervention | Advantages | Disadvantages |
|---|---|---|
| Localization of physicians | Increases frequency of nurse‐physician communication; provides foundation for additional interventions | Insufficient in creating a shared mental model; does not specifically enhance communication skills |
| Daily goals‐of‐care forms and checklists | Provides structure to interdisciplinary discussions and ensures input from all team members | May be completed in a perfunctory manner and may not be updated as plans of care evolve |
| Teamwork training | Emphasizes improved communication behaviors relevant across a range of team member interactions | Requires time and deliberate practice of new skills; effect may be attenuated if members are dispersed. |
| Interdisciplinary rounds | Provides a forum for regular interdisciplinary communication | Requires leadership to organize discussion and does not address need for updates as plans of care evolve |
Geographic Localization of Physicians
As mentioned earlier, physicians in large hospitals may care for patients on multiple units or floors. Designating certain physicians to care for patients admitted to specific units may improve efficiency and communication among healthcare professionals. One study recently reported on the effect of localization of hospital physicians to specific patient care units. Localization resulted in an increase in the rate of nurse‐physician communication, but did not improve providers' shared understanding of the plan of care.56 Notably, localizing physicians may improve the feasibility of additional interventions, like teamwork training and interdisciplinary rounds.
Daily Goals of Care and Surgery Safety Checklists
In ICU and operating room settings, physicians and nurses work in proximity, allowing interdisciplinary discussions to occur at the bedside. The finding that professionals in ICUs and operating rooms have widely discrepant views on the quality of collaboration31, 32 indicates that proximity, alone, is not sufficient for effective communication. Pronovost et al. used a daily goals form for bedside ICU rounds in an effort to standardize communication about the daily plan of care.57 The form defined essential goals of care for patients, and its use resulted in a significant improvement in the team's understanding of the daily goals. Narasimhan et al. performed a similar study using a daily goals worksheet during ICU rounds,58 and also found a significant improvement in physicians' and nurses' ratings of their understanding of the goals of care. The forms used in these studies provided structure to the interdisciplinary conversations during rounds to create a shared understanding of patients' plans of care.
Haynes and colleagues recently reported on the use of a surgical safety checklist in a large, multicenter pre‐post study.59 The checklist consisted of verbal confirmation of the completion of basic steps essential to safe care in the operating room, and provided structure to communication among surgical team members to ensure a shared understanding of the operative plan. The intervention resulted in a significant reduction in inpatient complications and mortality.
Team Training
Formalized team training, based on crew resource management, has been studied as a potential method to improve teamwork in a variety of medical settings.6062 Training emphasizes the core components of successful teamwork and essential coordinating mechanisms previously mentioned.23 Team training appears to positively influence culture, as assessed by teamwork and patient safety climate survey instruments.60 Based on these findings and extensive research demonstrating the success of teamwork training in aviation,63 the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD) have partnered in offering the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) program, designed to improve teamwork skills for healthcare professionals.64, 65
Only a handful of studies have evaluated the effectiveness of teamwork training programs on patient outcomes, and the results are mixed.66 Morey et al. found a reduction in the rate of observed errors as a result of teamwork training in emergency departments, but observers in the study were not blinded with regard to whether teams had undergone training.61 A research group in the United Kingdom evaluated the benefit of simulation‐based team training on outcomes in an obstetrical setting.67, 68 Training included management of specific complications, including shoulder dystocia and uterine cord prolapse. Using retrospective chart review, the investigators found a significant reduction in the proportion of babies born with an obstetric brachial palsy injury and a reduction in the time from diagnosis of uterine cord prolapse to infant delivery. Nielsen and colleagues also evaluated the use of teamwork training in an obstetric setting.62 In a cluster randomized controlled trial, the investigators found no reduction in the rate of adverse outcomes. Differences in the duration of teamwork training and the degree of emphasis on deliberate practice of new skills (eg, with the use of simulation‐based training) likely explains the lack of consistent results.
Very little research has evaluated teamwork training in the general medical environment.69, 70 Sehgal and colleagues recently published an evaluation of the effect of teamwork training delivered to internal medicine residents, hospitalists, nurses, pharmacists, case managers, and social workers on medical services in 3 Northern California hospitals.69 The 4‐hour training sessions covered topical areas of safety culture, teamwork, and communication through didactics, videos, facilitated discussions, and small group role plays to practice new skills and behaviors. The intervention was rated highly among participants,69 and the training along with subsequent follow‐up interventions resulted in improved patient perceptions of teamwork and communication but had no impact on key patient outcomes.71
Interdisciplinary Rounds
Interdisciplinary rounds (IDR) have been used for many years as a means to assemble team members in a single location,7275 and the use of IDR has been associated with lower mortality among ICU patients.76 Interdisciplinary rounds may be particularly useful for clinical settings in which team members are traditionally dispersed in time and place, such as medical‐surgical units. Recent studies have evaluated the effect of structured inter‐disciplinary rounds (SIDR),77, 78 which combine a structured format for communication, similar to a daily goals‐of‐care form, with a forum for daily interdisciplinary meetings. Though no effect was seen on length of stay or cost, SIDR resulted in significantly higher ratings of the quality of collaboration and teamwork climate, and a reduction in the rate of AEs.79 Importantly, the majority of clinicians in the studies agreed that SIDR improved the efficiency of their work day, and expressed a desire that SIDR continue indefinitely. Many investigators have emphasized the importance of leadership during IDR, often by a medical director, nurse manager, or both.74, 77, 78
Summary of Interventions to Improve Teamwork
Localization of physicians increases the frequency of nurse‐physician communication, but is insufficient in creating a shared understanding of patients' plans of care. Providing structure for the discussion among team members (eg, daily goals of care forms and checklists) ensures that critical elements of the plan of care are communicated. Teamwork training is based upon a strong foundation of research both inside and outside of healthcare, and has demonstrated improved knowledge of teamwork principles, attitudes about the importance of teamwork, and overall safety climate. Creating a forum for team members to assemble and discuss their patients (eg, IDR) can overcome some of the unique barriers to collaboration in settings where members are dispersed in time and space. Leaders wishing to improve interdisciplinary teamwork should consider implementing a combination of complementary interventions. For example, localization may increase the frequency of team member interactions, the quality of which may be enhanced with teamwork training and reinforced with the use of structured communication tools and IDR. Future research should evaluate the effect of these combined interventions.
CONCLUSIONS
In summary, teamwork is critically important to provide safe and effective care. Important and unique barriers to teamwork exist in hospitals. We recommend the use of survey instruments, such as those mentioned earlier, as the most feasible method to assess teamwork in the general medical setting. Because each intervention addresses only a portion of the barriers to optimal teamwork, we encourage leaders to use a multifaceted approach. We recommend the implementation of a combination of interventions with adaptations to fit unique clinical settings and local culture.
Acknowledgements
This manuscript was prepared as part of the High Performance Teams and the Hospital of the Future project, a collaborative effort including senior leadership from the American College of Physician Executives, the American Hospital Association, the American Organization of Nurse Executives, and the Society of Hospital Medicine. The authors thank Taylor Marsh for her administrative support and help in coordinating project meetings.
- To Err Is Human: Building a Safer Health System.Washington, DC:Institute of Medicine;1999.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,.Exploring the causes of adverse events in NHS hospital practice.J R Soc Med.2001;94(7):322–330.
- ,,,,,.The Quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety 2007. Available at: http://www.jointcommissionreport.org. Accessed November2007.
- ,,.Patient perceptions of coordinated care: the importance of organized communication in hospitals.J Healthc Qual.1999;21(5):18–23.
- ,,.Am I safe here? Improving patients' perceptions of safety in hospitals.J Nurs Care Qual.2006;21(1):30–40.
- ,,.Teamwork culture and patient satisfaction in hospitals.Med Care.2004;42(5):492–498.
- ,,.The influence of teamwork culture on physician and nurse resignation rates in hospitals.Health Serv Manage Res.2008;21(1):23–31.
- ,,.Quantifying the economic impact of communication inefficiencies in U.S. hospitals.J Healthc Manag.2010;55(4):265–282.
- ,.Managing the Unexpected: Assuring High Performance in an Age of Complexity.San Francisco, CA:Jossey‐Bass;2001.
- .Some characteristics of high reliability organizations.Organization Science.1990;1(2):160–177.
- ,,.Teamwork as an essential component of high‐reliability organizations.Health Serv Res.2006;41(4 pt 2):1576–1598.
- ,,,.Promoting health care safety through training high reliability teams.Qual Saf Health Care.2005;14(4):303–309.
- ,,,,,.Analyzing the time and value of housestaff inpatient work.J Gen Intern Med.1998;13(8):534–540.
- ,,, et al.Quantifying nursing workflow in medication administration.J Nurs Adm.2008;38(1):19–26.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.The role of teamwork in the professional education of physicians: current status and assessment recommendations.Jt Comm J Qual Patient Saf.2005;31(4):185–202.
- ,,.Is there a “big five” in teamwork?Small Group Research.2005;36:555–599.
- ,,.Objective measures of situation awareness in a simulated medical environment.Qual Saf Health Care.2004;13(suppl 1):i65–i71.
- ,.What do we know about health care team effectiveness? A review of the literature.Med Care Res Rev.2006;63(3):263–300.
- ,,, et al.Does team training improve team performance? A meta‐analysis.Hum Factors.2008;50(6):903–933.
- ,,,,,.Can we talk? Priorities for patient care differed among health care providers. AHRQ Publication No. 05–0021‐1.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,, et al.Patterns of nurse–physicians communication and agreement on the plan of care.Qual Saf Health Care.2010;19:195–199.
- ,,,,.Interns overestimate the effectiveness of their hand‐off communication.Pediatrics.2010;125(3):491–496.
- ,.Speakers' overestimation of their effectiveness.Psychol Sci.2002;13(3):207–212.
- ,,, et al.Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- ,,.Discrepant attitudes about teamwork among critical care nurses and physicians.Crit Care Med.2003;31(3):956–959.
- ,,,,,.Teamwork on inpatient medical units: assessing attitudes and barriers.Qual Saf Health Care.2010;19(2):117–121.
- ,,.Error, stress, and teamwork in medicine and aviation: cross sectional surveys.BMJ.2000;320(7237):745–749.
- ,,,,.Impact of a computerized physician order entry system on nurse‐physician collaboration in the medication process.Int J Med Inform.2008;77(11):735–744.
- ,,,,.Alphanumeric paging in an academic hospital setting.Am J Surg.2006;191(4):561–565.
- ,,,.Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service.J Hosp Med.2009;4(8):E34–E40.
- ,,, et al.The use of smartphones for clinical communication on internal medicine wards.J Hosp Med.2010;5(9):553–559.
- ,.Organizational information requirements, media richness, and structural design.Management Science.1986;32(5):554–571.
- ,.Decoding of inconsistent communications of personality and social psychology.J Pers Soc Psychol.1967;6(1):109–114.
- ,,,,.Beyond paging: building a Web‐based communication tool for nurses and physicians.J Gen Intern Med.2009;24(1):105–110.
- ,,, et al.Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Evaluation of resident communication skills and professionalism: a matter of perspective?Pediatrics.2006;118(4):1371–1379.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- .Multisource feedback in the assessment of physician competencies.J Contin Educ Health Prof.2003;23(1):4–12.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' Non‐Technical Skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,,.Using the Communication and Teamwork Skills (CATS) Assessment to measure health care team performance.Jt Comm J Qual Patient Saf.2007;33(9):549–558.
- ,,, et al.The Mayo High Performance Teamwork Scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,, et al.The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research.BMC Health Serv Res.2006;6:44.
- .Development of an instrument to measure collaboration and satisfaction about care decisions.J Adv Nurs.1994;20(1):176–182.
- ,,,,,.Psychometric properties of an attitude scale measuring physician‐nurse collaboration.Eval Health Prof.1999;22(2):208–220.
- ,,, et al.Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care.J Gen Intern Med.2009;24(11):1223–1227.
- ,,,,,.Improving communication in the ICU using daily goals.J Crit Care.2003;18(2):71–75.
- ,,,,.Improving nurse‐physician communication and satisfaction in the intensive care unit with a daily goals worksheet.Am J Crit Care.2006;15(2):217–222.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,, et al.Effect of crew resource management training in a multidisciplinary obstetrical setting.Int J Qual Health Care.2008;20(4):254–263.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial.Obstet Gynecol.2007;109(1):48–55.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- Agency for Healthcare Research and Quality. TeamSTEPPS Home. Available at: http://teamstepps.ahrq.gov/index.htm. Accessed January 18,2010.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48(2):392–412.
- ,,, et al.Improving neonatal outcome through practical shoulder dystocia training.Obstet Gynecol.2008;112(1):14–20.
- ,,, et al.Retrospective cohort study of diagnosis‐delivery interval with umbilical cord prolapse: the effect of team training.Br J Obstet Gynaecol.2009;116(8):1089–1096.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,,,.Teambuilding and leadership training in an internal medicine residency training program.J Gen Intern Med.2004;19(6):692–697.
- ,,, et al. Effects of a multicenter teamwork and communication program on patient outcomes: results from the Triad for Optimal Patient Safety (TOPS) project. In press.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,.A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement.Med Care.1998;36(8 suppl):AS4–A12.
- ,,,,.Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay.J Gen Intern Med.2007;22(8):1073–1079.
- ,,,.Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses.Am J Crit Care.2005;14(1):71–77.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit.J Hosp Med.2011;6(2):88–93.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit.J Gen Intern Med.2010;25(8):826–832.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- To Err Is Human: Building a Safer Health System.Washington, DC:Institute of Medicine;1999.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,.Exploring the causes of adverse events in NHS hospital practice.J R Soc Med.2001;94(7):322–330.
- ,,,,,.The Quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety 2007. Available at: http://www.jointcommissionreport.org. Accessed November2007.
- ,,.Patient perceptions of coordinated care: the importance of organized communication in hospitals.J Healthc Qual.1999;21(5):18–23.
- ,,.Am I safe here? Improving patients' perceptions of safety in hospitals.J Nurs Care Qual.2006;21(1):30–40.
- ,,.Teamwork culture and patient satisfaction in hospitals.Med Care.2004;42(5):492–498.
- ,,.The influence of teamwork culture on physician and nurse resignation rates in hospitals.Health Serv Manage Res.2008;21(1):23–31.
- ,,.Quantifying the economic impact of communication inefficiencies in U.S. hospitals.J Healthc Manag.2010;55(4):265–282.
- ,.Managing the Unexpected: Assuring High Performance in an Age of Complexity.San Francisco, CA:Jossey‐Bass;2001.
- .Some characteristics of high reliability organizations.Organization Science.1990;1(2):160–177.
- ,,.Teamwork as an essential component of high‐reliability organizations.Health Serv Res.2006;41(4 pt 2):1576–1598.
- ,,,.Promoting health care safety through training high reliability teams.Qual Saf Health Care.2005;14(4):303–309.
- ,,,,,.Analyzing the time and value of housestaff inpatient work.J Gen Intern Med.1998;13(8):534–540.
- ,,, et al.Quantifying nursing workflow in medication administration.J Nurs Adm.2008;38(1):19–26.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.The role of teamwork in the professional education of physicians: current status and assessment recommendations.Jt Comm J Qual Patient Saf.2005;31(4):185–202.
- ,,.Is there a “big five” in teamwork?Small Group Research.2005;36:555–599.
- ,,.Objective measures of situation awareness in a simulated medical environment.Qual Saf Health Care.2004;13(suppl 1):i65–i71.
- ,.What do we know about health care team effectiveness? A review of the literature.Med Care Res Rev.2006;63(3):263–300.
- ,,, et al.Does team training improve team performance? A meta‐analysis.Hum Factors.2008;50(6):903–933.
- ,,,,,.Can we talk? Priorities for patient care differed among health care providers. AHRQ Publication No. 05–0021‐1.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,, et al.Patterns of nurse–physicians communication and agreement on the plan of care.Qual Saf Health Care.2010;19:195–199.
- ,,,,.Interns overestimate the effectiveness of their hand‐off communication.Pediatrics.2010;125(3):491–496.
- ,.Speakers' overestimation of their effectiveness.Psychol Sci.2002;13(3):207–212.
- ,,, et al.Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- ,,.Discrepant attitudes about teamwork among critical care nurses and physicians.Crit Care Med.2003;31(3):956–959.
- ,,,,,.Teamwork on inpatient medical units: assessing attitudes and barriers.Qual Saf Health Care.2010;19(2):117–121.
- ,,.Error, stress, and teamwork in medicine and aviation: cross sectional surveys.BMJ.2000;320(7237):745–749.
- ,,,,.Impact of a computerized physician order entry system on nurse‐physician collaboration in the medication process.Int J Med Inform.2008;77(11):735–744.
- ,,,,.Alphanumeric paging in an academic hospital setting.Am J Surg.2006;191(4):561–565.
- ,,,.Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service.J Hosp Med.2009;4(8):E34–E40.
- ,,, et al.The use of smartphones for clinical communication on internal medicine wards.J Hosp Med.2010;5(9):553–559.
- ,.Organizational information requirements, media richness, and structural design.Management Science.1986;32(5):554–571.
- ,.Decoding of inconsistent communications of personality and social psychology.J Pers Soc Psychol.1967;6(1):109–114.
- ,,,,.Beyond paging: building a Web‐based communication tool for nurses and physicians.J Gen Intern Med.2009;24(1):105–110.
- ,,, et al.Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Evaluation of resident communication skills and professionalism: a matter of perspective?Pediatrics.2006;118(4):1371–1379.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- .Multisource feedback in the assessment of physician competencies.J Contin Educ Health Prof.2003;23(1):4–12.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' Non‐Technical Skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,,.Using the Communication and Teamwork Skills (CATS) Assessment to measure health care team performance.Jt Comm J Qual Patient Saf.2007;33(9):549–558.
- ,,, et al.The Mayo High Performance Teamwork Scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,, et al.The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research.BMC Health Serv Res.2006;6:44.
- .Development of an instrument to measure collaboration and satisfaction about care decisions.J Adv Nurs.1994;20(1):176–182.
- ,,,,,.Psychometric properties of an attitude scale measuring physician‐nurse collaboration.Eval Health Prof.1999;22(2):208–220.
- ,,, et al.Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care.J Gen Intern Med.2009;24(11):1223–1227.
- ,,,,,.Improving communication in the ICU using daily goals.J Crit Care.2003;18(2):71–75.
- ,,,,.Improving nurse‐physician communication and satisfaction in the intensive care unit with a daily goals worksheet.Am J Crit Care.2006;15(2):217–222.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,, et al.Effect of crew resource management training in a multidisciplinary obstetrical setting.Int J Qual Health Care.2008;20(4):254–263.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial.Obstet Gynecol.2007;109(1):48–55.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- Agency for Healthcare Research and Quality. TeamSTEPPS Home. Available at: http://teamstepps.ahrq.gov/index.htm. Accessed January 18,2010.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48(2):392–412.
- ,,, et al.Improving neonatal outcome through practical shoulder dystocia training.Obstet Gynecol.2008;112(1):14–20.
- ,,, et al.Retrospective cohort study of diagnosis‐delivery interval with umbilical cord prolapse: the effect of team training.Br J Obstet Gynaecol.2009;116(8):1089–1096.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,,,.Teambuilding and leadership training in an internal medicine residency training program.J Gen Intern Med.2004;19(6):692–697.
- ,,, et al. Effects of a multicenter teamwork and communication program on patient outcomes: results from the Triad for Optimal Patient Safety (TOPS) project. In press.
- ,,, et al.The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs.J Nurs Adm.2006;36(2):79–85.
- ,,.A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement.Med Care.1998;36(8 suppl):AS4–A12.
- ,,,,.Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay.J Gen Intern Med.2007;22(8):1073–1079.
- ,,,.Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses.Am J Crit Care.2005;14(1):71–77.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit.J Hosp Med.2011;6(2):88–93.
- ,,,,,.Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit.J Gen Intern Med.2010;25(8):826–832.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
Erratum: Investing in the future: Building an academic hospitalist faculty development program
The disclosure statement for the following article, Investing in the Future: Building an Academic Hospitalist Faculty Development Program, by Niraj L. Sehgal, MD, MPH, Bradley A. Sharpe, MD, Andrew A. Auerbach, MD, MPH, Robert M. Wachter, MD, that published in Volume 6, Issue 3 pages 161166 of the Journal of Hospital Medicine, was incorrect. The correct disclosure statement is: All authors report no relevant conflicts of interest. The publisher regrets this error.
The disclosure statement for the following article, Investing in the Future: Building an Academic Hospitalist Faculty Development Program, by Niraj L. Sehgal, MD, MPH, Bradley A. Sharpe, MD, Andrew A. Auerbach, MD, MPH, Robert M. Wachter, MD, that published in Volume 6, Issue 3 pages 161166 of the Journal of Hospital Medicine, was incorrect. The correct disclosure statement is: All authors report no relevant conflicts of interest. The publisher regrets this error.
The disclosure statement for the following article, Investing in the Future: Building an Academic Hospitalist Faculty Development Program, by Niraj L. Sehgal, MD, MPH, Bradley A. Sharpe, MD, Andrew A. Auerbach, MD, MPH, Robert M. Wachter, MD, that published in Volume 6, Issue 3 pages 161166 of the Journal of Hospital Medicine, was incorrect. The correct disclosure statement is: All authors report no relevant conflicts of interest. The publisher regrets this error.
Nonprocedural “Time Out”
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
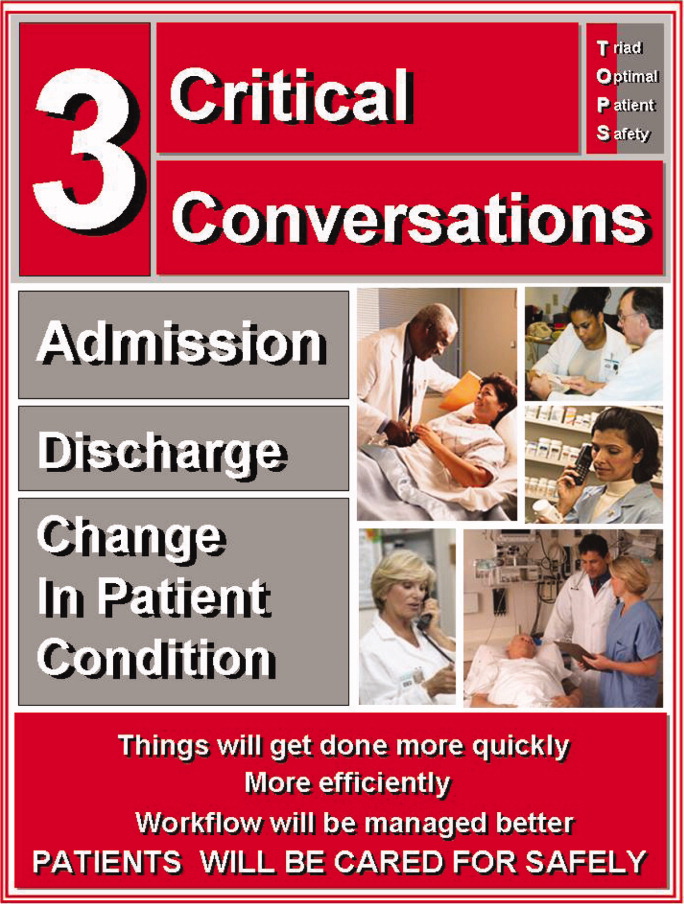
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
Copyright © 2011 Society of Hospital Medicine
Faculty Development for Hospitalists
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
Copyright © 2011 Society of Hospital Medicine
Patient Whiteboards in the Hospital Setting
Communication failures are a frequent cause of adverse events14; the Joint Commission (TJC) reports that such failures contributed to 65% of reported sentinel events.5 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.613 While these strategies largely address communication between healthcare providers, there is a growing emphasis on developing strategies to engage patients in their care, and improving communication with them and their families.
In 2007, TJC announced a new National Patient Safety Goal (NPSG) that encourage(s) patients' active involvement in their own care as a patient safety strategy.14 This builds upon a landmark Institute of Medicine report that highlighted patient‐centeredness as 1 of the 6 domains for delivering high‐quality care.15 Current literature on developing such patient‐centered strategies enumerates several approaches, including better access to health information, use of innovative technology solutions, and focused efforts at improving communication.1618
The placement of whiteboards in patient rooms is an increasingly common strategy to improve communication. These boards, typically placed on a wall near a patient's hospital bed, allow any number of providers to communicate a wide range of information. Both Kaiser Permanente's Nurse Knowledge Exchange program and the Institute for Healthcare Improvement's Transforming Care at the Bedside promote whiteboard use, though with little specific guidance about practical implementation.19,20 Despite their growing prevalence, there is no published literature guiding the most effective uses of whiteboards, or describing their impact on communication, teamwork, or patient satisfaction and care. We present findings from a survey of patient whiteboard use on an academic medical service, and offer a series of recommendations based on our findings and experiences.
Methods
We anonymously surveyed bedside nurses from 3 inpatient medical units, internal medicine housestaff, and faculty from the Division of Hospital Medicine at the University of California, San Francisco (UCSF). We solicited experiences of physician and nursing leaders who were engaged in whiteboard interventions over the past 2 years to identify relevant topics for study. Their experiences were based on isolated unit‐based efforts to implement whiteboards through a variety of strategies (eg, whiteboard templates, simple identification of provider teams, goals for the day). Their input guided the survey development and the suggested recommendations. The topics identified were then translated into multiple‐choice questions, and further edited for clarity by the authors. A Likert scale was used that measured frequency of use, usefulness, and attitudes toward patient whiteboards. An open‐ended question seeking additional comments about patient whiteboards was also asked. The survey was administered to nurses at staff meetings and through physical mailboxes on their respective patient care units with a 1‐month collection period. The survey was administered to housestaff and attendings via e‐mail listserves using an online commercial survey administration tool.21 The nursing surveys were later entered into the same online survey administration tool, which ultimately provided summary reports and descriptive findings to meet the study objectives. Our project was reviewed and approved by the UCSF Committee on Human Research.
Results
Survey responses were collected from 104 nurse respondents (81% response rate), 118 internal medicine housestaff (74% response rate), and 31 hospitalists (86% response rate). Nurses were far more likely to write on whiteboards, read what was written on them, and find the related information useful (Figure 1A‐C). Nurses, housestaff, and attendings all believed the bedside nurse was the single most important provider name listed on a whiteboard. However, the respondents differed in their rated value of other providers listed on the whiteboard (Figure 2). Nurses gave higher ratings to the utility of having patient care assistants (PCAs) listed as compared to housestaff and attendings. Overall, respondents felt it would be less useful to list consultants and pharmacists than the nurse, attending, and housestaff. All of the respondents believed family contact information was the most useful information on a whiteboard, whereas more nurses rated a goal for the day and anticipated discharge date as more useful than housestaff and attendings (Figure 3).



From an operational standpoint, the majority of respondents felt that nurses should be responsible for the information on a whiteboard, nurses and physicians together should create goals for the day, and the greatest barrier to using whiteboards was not having pens easily available (Figure 4A‐C). Most respondents also agreed that using templated whiteboards (with predefined fields) to guide content would increase their use (Figure 4D). All respondents believed that whiteboard use could improve teamwork and communication as well as patient care (Figure 5). Respondents also offered a variety of specific comments in response to an open‐ended question about whiteboard use (Table 1).


| From nurses | If MDs were engaged in using (or reviewing the information on) whiteboards more, it might reduce the number of times we page them to clarify care plans |
| It might be helpful to have a dedicated section on the whiteboard where families can write questions that are separate from other information that the nurse writes on them | |
| Part of the bedside nurse role is to be a patient advocate and the whiteboard can be a tool to assist in this important responsibility | |
| Nothing is worse than a patient (or family member) asking me, What's the plan for the day?and being unable to do so because a goal (or scheduled procedure) hasn't been communicated to me by the MD or written on the whiteboard | |
| I would use [whiteboards] more if they were clearly being used as a patient‐centered communication tool rather than trying to improve communication between us and the MDs. | |
| From physicians | The boards need to be kept simple for success. |
| There needs to be specific training to make this a cultural norm across care providers and reinforced on a regular basis. If it's a priority, there should be audits, tracking for performance (accuracy and updated info), and feedback to providers. I would also ask patients what info they would like to see, as [whiteboards] should be patient‐centered, not provider‐centered. | |
| Having providers intermittently write on whiteboards should not be considered a substitute for communication. In fact, this would likely only further display our lack of cohesive communication to patients and families. | |
| I have been skeptical that the goals for the day for an ill patient can be satisfactorily reduced to a statement that fits on a whiteboard and that forecasting a day of discharge well in advance is frequently wrong and may create more confusion than it alleviates. I am also concerned that if a goal for the day on a whiteboard is intended for the nurse, this is substituting for richer channels of communications, such as the nurse reading the progress notes, speaking with the physicians, or communicating through the charge nurse who attends our case management rounds. | |
| Whiteboards are frequently not accurate, underused, and they require patients to have visual acuity, cognition, and speak Englishall challenges depending on your patient population. |
Discussion
Our findings demonstrate the potential value of patient whiteboards, which is supported by the vast majority of respondents, who agreed their use may improve patient care and teamwork. It is also clear that whiteboard use is not achieving this potential or being used as a patient‐centered tool. This is best illustrated by findings of their low rate of use and completion among attendings and housestaff (Figure 1A, B) and the lack of consensus as to what information on the whiteboards is useful. Patient whiteboards require defined goals, thoughtful planning, regular monitoring, and ongoing evaluation. The challenges around effective adoption and implementation is perhaps more about ensuring compliance and completion rather than simply gaining buy‐in and engagement for their value.
While the differential use of whiteboards between nurses and physicians was not surprising, a few specific findings warrant further discussion. First, it is interesting that nurses rated their own names and that of PCAs as the most useful, while physicians rated the nurse's name as being of equal value to their own. This may speak to the role PCAs play for nurses in helping the latter provide bedside care, rather than a reflection of the nurses' perception of the value of PCAs for patients. Second, while all respondents rated highly the value of family contact information on the whiteboard, nurses valued a goal for the day and anticipated discharge date more highly than did physicians. These findings likely reflect that nurses desire an understanding about plans of care and if they are not communicated face‐to‐face as the most effective strategy,22 they should at least be spelled out clearly on a whiteboard. This is supported by evidence that better collaboration between nurses and physicians improves patient outcomes.23 It may also be that physicians place more value on their own progress notes (rather than whiteboards) as a vehicle for communicating daily goals and discharge planning.
Other practical considerations involve who owns it and, if we do create goals for the day, whose goals should they represent? The majority of nurse and physician responses advocated for nurses to be responsible for accurate and complete information being updated on whiteboards. A larger percentage of attendings favored shared responsibility of the whiteboard, which was reinforced by their support of having goals for the day created jointly by nurses and physicians. Interestingly, a much smaller percentage of respondents felt goals for the day should be driven by patients (or family members). These data may point to the different perspectives that each individual provider bringsphysician, nurse, pharmacist, discharge plannerwith their respective goals differing in nature. Finally, it is also interesting that while attendings and housestaff believed that whiteboards can improve patient care teamwork/communication (Figure 5), a much smaller percentage actually read what is on them (Figure 1B). This may reflect the unclear goals of whiteboards, its absence as part of daily workflow, the infrequency of updated information on them, or perhaps an institution‐specific phenomenon that we will use to drive further improvement strategies.
Selected respondent comments (Table 1) highlight important messages about whiteboard use and provide helpful context to the survey responses. We found that the goal of whiteboard use is not always clear; is it to improve communication among providers, to improve communication with patients, a tool to engage patients in their care, or some combination of the above? Without a clear goal, providers are left to wonder whether whiteboard use is simply another task or really an intervention to improve care. This may in part, or perhaps fully, explain the differences discovered in whiteboard use and practices among our surveyed providers.
If, however, one were to make clear that the goal of patient whiteboards is to engage patients in their care and help achieve an important NPSG, methods to implement their use become better guided. A limitation of our study is that we did not survey patients about their perceptions of whiteboards use, an important needs assessment that would further drive this patient‐centered intervention. Regardless, we can draw a number of lessons from our findings and devise a set of reasonable recommendations.
Recommendations
We provide the following set of recommendations for hospitals adopting patient whiteboards, drawing on our survey findings and experiences with implementation at our own institution. We also acknowledge the role that local hospital cultures may play in adopting whiteboard use, and our recommendations are simply guidelines that can be applied or used in planning efforts. We believe effective use of a patient whiteboard requires a patient‐centered approach and the following:
-
Whiteboards should be placed in clear view of patients from their hospital bed
A simple yet critical issue as placing a whiteboard behind a patient's bed or off to the side fails to provide them with a constant visual cue to engage in the information.
-
Buy and fasten erasable pens to the whiteboards themselves
In our institution, purchasing pens for each provider was a less effective strategy than simply affixing the pen to the whiteboard itself. A supply of erasable pens must be available at the nursing station to quickly replace those with fading ink.
-
Create whiteboard templates
Our findings and experience suggest that structured formats for whiteboards may be more effective in ensuring both important and accurate information gets included. Blank whiteboards lead to less standardization in practice and fail to create prompts for providers to both write and review the content available. Anecdotally, we created a number of whiteboards with templated information, and this did seem to increase the consistency, standardization, and ease of use.
-
Whiteboard templates should include the following items:
-
Day and Date
This serves to orient patients (and their families) as well as providers with the date of information written on the whiteboard. It is also an important mechanism to ensure information is updated daily.
-
Patient's name (or initials)
With bed turnover (or patient transfers to different beds and units) commonplace in hospital care, we believe that listing the patient's name on the board prevents the potential for patients (and their families) or providers to mistakenly take information from a previous patient's care on the whiteboard for their own.
-
Bedside nurse
This was noted as the most useful provider listed on a patient whiteboard, which is quite logical given the role bedside nurses play for hospitalized patients.
-
Primary physician(s) (attending, resident, and intern, if applicable)
This was noted as the next most important provider(s) and perhaps increasingly important both in teaching and nonteaching settings where shift‐work and signouts are growing in frequency among physicians.
-
Goal for the day
While this was not a consensus from our survey respondents, we believe patients (rather than providers) should ultimately guide determination of their goal for the day as this engages them directly with the planachieving a patient‐centered initiative. In our experience, an effective strategy was having the bedside nurse directly engage patients each morning to help place a goal for the day on their whiteboard.
-
Anticipated discharge date
While understanding the potential for this date to change, we believe the benefits of having patients (and their families) thinking about discharge, rather than feeling surprised by it on the morning of discharge, serves as an important mechanism to bridge communication about the discharge process.24
-
Family member's contact information (phone number)
-
Questions for providers
This last entry allows a space for families to engage the healthcare team and, once again, create an opportunity for clarification of treatment and discharge plans.
-
Bedside nurses should facilitate writing and updating information on the whiteboard
Without our survey findings, this might have generated debate or controversy over whether nurses should be burdened with one more task to their responsibilities. However, our nurse respondents embraced this responsibility with spontaneous comments about their patient advocate role, and stated that whiteboards can serve as a tool to assist in that responsibility. Furthermore, not a single nurse respondent stated as barrier to use that I didn't think it was my responsibility. Nonetheless, whiteboard use must be a shared communication tool and not simply a tool between nurse and patient. Practically, we would recommend that bedside nurses facilitate updating whiteboards each morning, at a time when they are already helping patients create a goal for the day. Other providers must be trained to review information on the whiteboard, engage patients about their specific goal, and share the responsibility of keeping the information on the whiteboard updated.
-
Create a system for auditing utilization and providing feedback early during rollout
We found that adoption was very slow at the outset. One strategy to consider is having designated auditors check whiteboards in each room, measuring weekly compliance and providing this feedback to nurse managers. This auditing process may help identify barriers that can be addressed quickly (eg, unavailability of pens).
Finally, it is important to comment on the confidentiality concerns often raised in the context of whiteboard use. Confidentiality concerns largely arise from personal health information being used without a patient's explicit consent. If our recommendations are adopted, they require whiteboard use to be a patient‐centered and patient‐driven initiative. The type of information on the whiteboard should be determined with sensitivity but also with consent of the patient. We have not experienced any concerns by patients or providers in this regard because patients are told about the goals of the whiteboard initiative with our above principles in mind.
Conclusions
Patient whiteboards may improve communication among members of the healthcare team (eg, nurses, physicians, and others) and between providers and their patients (and family members). Further investigation is warranted to determine if adopting our recommendations leads to improved communication, teamwork, or patient satisfaction and care. In the meantime, as many hospitals continue to install and implement whiteboards, we hope our recommendations, accompanied by an emphasis on creating a patient‐centered communication tool, offer a roadmap for considering best practices in their use.
Acknowledgements
This study of patient whiteboards developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. The authors thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204(4):533–540.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- The Joint Commission: Sentinel Event Statistics, March 31,2009. Available at: http://www.jointcommission.org/SentinelEvents/Statistics. Accessed October 2009.
- ,,, et al.Bridging the communication gap in the operating room with medical team training.Am J Surg.2005;190(5):770–774.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,.Enhancing patient safety through teamwork training.J Healthc Risk Manag.2001;21(4):57–65.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- The Joint Commission's National Patient Safety Goals 2007 for Hospital/Critical Access Hospital. Available at:http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_hap_cah_npsgs.htm. Accessed October 2009.
- Institute of Medicine (U.S.). Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.A systems approach to patient‐centered care.JAMA.2006;296(23):2848–2851.
- ,,,,.Microsystems in health care: Part 4. Planning patient‐centered care.Jt Comm J Qual Saf.2003;29(5):227–237.
- Gerteis M, Edgman‐Levitan S, Daley J, Delbanco TL, eds.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,.Transforming Care at the Bedside. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement;2004. Available at: http://www.ihi.org. Accessed October 2009.
- ..Nurse Knowledge Exchange: Patient Hand Offs. American Academy of Ambulatory Care Nursing (AAACN) Viewpoint. Sep/Oct 2007. Available at: http://findarticles.com/p/articles/mi_qa4022/is_200709/ai_n21137476. Accessed October 2009.
- Survey Console. Available at: http://www.surveyconsole.com. Accessed October 2009.
- How do we communicate?Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed October 2009.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
Communication failures are a frequent cause of adverse events14; the Joint Commission (TJC) reports that such failures contributed to 65% of reported sentinel events.5 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.613 While these strategies largely address communication between healthcare providers, there is a growing emphasis on developing strategies to engage patients in their care, and improving communication with them and their families.
In 2007, TJC announced a new National Patient Safety Goal (NPSG) that encourage(s) patients' active involvement in their own care as a patient safety strategy.14 This builds upon a landmark Institute of Medicine report that highlighted patient‐centeredness as 1 of the 6 domains for delivering high‐quality care.15 Current literature on developing such patient‐centered strategies enumerates several approaches, including better access to health information, use of innovative technology solutions, and focused efforts at improving communication.1618
The placement of whiteboards in patient rooms is an increasingly common strategy to improve communication. These boards, typically placed on a wall near a patient's hospital bed, allow any number of providers to communicate a wide range of information. Both Kaiser Permanente's Nurse Knowledge Exchange program and the Institute for Healthcare Improvement's Transforming Care at the Bedside promote whiteboard use, though with little specific guidance about practical implementation.19,20 Despite their growing prevalence, there is no published literature guiding the most effective uses of whiteboards, or describing their impact on communication, teamwork, or patient satisfaction and care. We present findings from a survey of patient whiteboard use on an academic medical service, and offer a series of recommendations based on our findings and experiences.
Methods
We anonymously surveyed bedside nurses from 3 inpatient medical units, internal medicine housestaff, and faculty from the Division of Hospital Medicine at the University of California, San Francisco (UCSF). We solicited experiences of physician and nursing leaders who were engaged in whiteboard interventions over the past 2 years to identify relevant topics for study. Their experiences were based on isolated unit‐based efforts to implement whiteboards through a variety of strategies (eg, whiteboard templates, simple identification of provider teams, goals for the day). Their input guided the survey development and the suggested recommendations. The topics identified were then translated into multiple‐choice questions, and further edited for clarity by the authors. A Likert scale was used that measured frequency of use, usefulness, and attitudes toward patient whiteboards. An open‐ended question seeking additional comments about patient whiteboards was also asked. The survey was administered to nurses at staff meetings and through physical mailboxes on their respective patient care units with a 1‐month collection period. The survey was administered to housestaff and attendings via e‐mail listserves using an online commercial survey administration tool.21 The nursing surveys were later entered into the same online survey administration tool, which ultimately provided summary reports and descriptive findings to meet the study objectives. Our project was reviewed and approved by the UCSF Committee on Human Research.
Results
Survey responses were collected from 104 nurse respondents (81% response rate), 118 internal medicine housestaff (74% response rate), and 31 hospitalists (86% response rate). Nurses were far more likely to write on whiteboards, read what was written on them, and find the related information useful (Figure 1A‐C). Nurses, housestaff, and attendings all believed the bedside nurse was the single most important provider name listed on a whiteboard. However, the respondents differed in their rated value of other providers listed on the whiteboard (Figure 2). Nurses gave higher ratings to the utility of having patient care assistants (PCAs) listed as compared to housestaff and attendings. Overall, respondents felt it would be less useful to list consultants and pharmacists than the nurse, attending, and housestaff. All of the respondents believed family contact information was the most useful information on a whiteboard, whereas more nurses rated a goal for the day and anticipated discharge date as more useful than housestaff and attendings (Figure 3).



From an operational standpoint, the majority of respondents felt that nurses should be responsible for the information on a whiteboard, nurses and physicians together should create goals for the day, and the greatest barrier to using whiteboards was not having pens easily available (Figure 4A‐C). Most respondents also agreed that using templated whiteboards (with predefined fields) to guide content would increase their use (Figure 4D). All respondents believed that whiteboard use could improve teamwork and communication as well as patient care (Figure 5). Respondents also offered a variety of specific comments in response to an open‐ended question about whiteboard use (Table 1).


| From nurses | If MDs were engaged in using (or reviewing the information on) whiteboards more, it might reduce the number of times we page them to clarify care plans |
| It might be helpful to have a dedicated section on the whiteboard where families can write questions that are separate from other information that the nurse writes on them | |
| Part of the bedside nurse role is to be a patient advocate and the whiteboard can be a tool to assist in this important responsibility | |
| Nothing is worse than a patient (or family member) asking me, What's the plan for the day?and being unable to do so because a goal (or scheduled procedure) hasn't been communicated to me by the MD or written on the whiteboard | |
| I would use [whiteboards] more if they were clearly being used as a patient‐centered communication tool rather than trying to improve communication between us and the MDs. | |
| From physicians | The boards need to be kept simple for success. |
| There needs to be specific training to make this a cultural norm across care providers and reinforced on a regular basis. If it's a priority, there should be audits, tracking for performance (accuracy and updated info), and feedback to providers. I would also ask patients what info they would like to see, as [whiteboards] should be patient‐centered, not provider‐centered. | |
| Having providers intermittently write on whiteboards should not be considered a substitute for communication. In fact, this would likely only further display our lack of cohesive communication to patients and families. | |
| I have been skeptical that the goals for the day for an ill patient can be satisfactorily reduced to a statement that fits on a whiteboard and that forecasting a day of discharge well in advance is frequently wrong and may create more confusion than it alleviates. I am also concerned that if a goal for the day on a whiteboard is intended for the nurse, this is substituting for richer channels of communications, such as the nurse reading the progress notes, speaking with the physicians, or communicating through the charge nurse who attends our case management rounds. | |
| Whiteboards are frequently not accurate, underused, and they require patients to have visual acuity, cognition, and speak Englishall challenges depending on your patient population. |
Discussion
Our findings demonstrate the potential value of patient whiteboards, which is supported by the vast majority of respondents, who agreed their use may improve patient care and teamwork. It is also clear that whiteboard use is not achieving this potential or being used as a patient‐centered tool. This is best illustrated by findings of their low rate of use and completion among attendings and housestaff (Figure 1A, B) and the lack of consensus as to what information on the whiteboards is useful. Patient whiteboards require defined goals, thoughtful planning, regular monitoring, and ongoing evaluation. The challenges around effective adoption and implementation is perhaps more about ensuring compliance and completion rather than simply gaining buy‐in and engagement for their value.
While the differential use of whiteboards between nurses and physicians was not surprising, a few specific findings warrant further discussion. First, it is interesting that nurses rated their own names and that of PCAs as the most useful, while physicians rated the nurse's name as being of equal value to their own. This may speak to the role PCAs play for nurses in helping the latter provide bedside care, rather than a reflection of the nurses' perception of the value of PCAs for patients. Second, while all respondents rated highly the value of family contact information on the whiteboard, nurses valued a goal for the day and anticipated discharge date more highly than did physicians. These findings likely reflect that nurses desire an understanding about plans of care and if they are not communicated face‐to‐face as the most effective strategy,22 they should at least be spelled out clearly on a whiteboard. This is supported by evidence that better collaboration between nurses and physicians improves patient outcomes.23 It may also be that physicians place more value on their own progress notes (rather than whiteboards) as a vehicle for communicating daily goals and discharge planning.
Other practical considerations involve who owns it and, if we do create goals for the day, whose goals should they represent? The majority of nurse and physician responses advocated for nurses to be responsible for accurate and complete information being updated on whiteboards. A larger percentage of attendings favored shared responsibility of the whiteboard, which was reinforced by their support of having goals for the day created jointly by nurses and physicians. Interestingly, a much smaller percentage of respondents felt goals for the day should be driven by patients (or family members). These data may point to the different perspectives that each individual provider bringsphysician, nurse, pharmacist, discharge plannerwith their respective goals differing in nature. Finally, it is also interesting that while attendings and housestaff believed that whiteboards can improve patient care teamwork/communication (Figure 5), a much smaller percentage actually read what is on them (Figure 1B). This may reflect the unclear goals of whiteboards, its absence as part of daily workflow, the infrequency of updated information on them, or perhaps an institution‐specific phenomenon that we will use to drive further improvement strategies.
Selected respondent comments (Table 1) highlight important messages about whiteboard use and provide helpful context to the survey responses. We found that the goal of whiteboard use is not always clear; is it to improve communication among providers, to improve communication with patients, a tool to engage patients in their care, or some combination of the above? Without a clear goal, providers are left to wonder whether whiteboard use is simply another task or really an intervention to improve care. This may in part, or perhaps fully, explain the differences discovered in whiteboard use and practices among our surveyed providers.
If, however, one were to make clear that the goal of patient whiteboards is to engage patients in their care and help achieve an important NPSG, methods to implement their use become better guided. A limitation of our study is that we did not survey patients about their perceptions of whiteboards use, an important needs assessment that would further drive this patient‐centered intervention. Regardless, we can draw a number of lessons from our findings and devise a set of reasonable recommendations.
Recommendations
We provide the following set of recommendations for hospitals adopting patient whiteboards, drawing on our survey findings and experiences with implementation at our own institution. We also acknowledge the role that local hospital cultures may play in adopting whiteboard use, and our recommendations are simply guidelines that can be applied or used in planning efforts. We believe effective use of a patient whiteboard requires a patient‐centered approach and the following:
-
Whiteboards should be placed in clear view of patients from their hospital bed
A simple yet critical issue as placing a whiteboard behind a patient's bed or off to the side fails to provide them with a constant visual cue to engage in the information.
-
Buy and fasten erasable pens to the whiteboards themselves
In our institution, purchasing pens for each provider was a less effective strategy than simply affixing the pen to the whiteboard itself. A supply of erasable pens must be available at the nursing station to quickly replace those with fading ink.
-
Create whiteboard templates
Our findings and experience suggest that structured formats for whiteboards may be more effective in ensuring both important and accurate information gets included. Blank whiteboards lead to less standardization in practice and fail to create prompts for providers to both write and review the content available. Anecdotally, we created a number of whiteboards with templated information, and this did seem to increase the consistency, standardization, and ease of use.
-
Whiteboard templates should include the following items:
-
Day and Date
This serves to orient patients (and their families) as well as providers with the date of information written on the whiteboard. It is also an important mechanism to ensure information is updated daily.
-
Patient's name (or initials)
With bed turnover (or patient transfers to different beds and units) commonplace in hospital care, we believe that listing the patient's name on the board prevents the potential for patients (and their families) or providers to mistakenly take information from a previous patient's care on the whiteboard for their own.
-
Bedside nurse
This was noted as the most useful provider listed on a patient whiteboard, which is quite logical given the role bedside nurses play for hospitalized patients.
-
Primary physician(s) (attending, resident, and intern, if applicable)
This was noted as the next most important provider(s) and perhaps increasingly important both in teaching and nonteaching settings where shift‐work and signouts are growing in frequency among physicians.
-
Goal for the day
While this was not a consensus from our survey respondents, we believe patients (rather than providers) should ultimately guide determination of their goal for the day as this engages them directly with the planachieving a patient‐centered initiative. In our experience, an effective strategy was having the bedside nurse directly engage patients each morning to help place a goal for the day on their whiteboard.
-
Anticipated discharge date
While understanding the potential for this date to change, we believe the benefits of having patients (and their families) thinking about discharge, rather than feeling surprised by it on the morning of discharge, serves as an important mechanism to bridge communication about the discharge process.24
-
Family member's contact information (phone number)
-
Questions for providers
This last entry allows a space for families to engage the healthcare team and, once again, create an opportunity for clarification of treatment and discharge plans.
-
Bedside nurses should facilitate writing and updating information on the whiteboard
Without our survey findings, this might have generated debate or controversy over whether nurses should be burdened with one more task to their responsibilities. However, our nurse respondents embraced this responsibility with spontaneous comments about their patient advocate role, and stated that whiteboards can serve as a tool to assist in that responsibility. Furthermore, not a single nurse respondent stated as barrier to use that I didn't think it was my responsibility. Nonetheless, whiteboard use must be a shared communication tool and not simply a tool between nurse and patient. Practically, we would recommend that bedside nurses facilitate updating whiteboards each morning, at a time when they are already helping patients create a goal for the day. Other providers must be trained to review information on the whiteboard, engage patients about their specific goal, and share the responsibility of keeping the information on the whiteboard updated.
-
Create a system for auditing utilization and providing feedback early during rollout
We found that adoption was very slow at the outset. One strategy to consider is having designated auditors check whiteboards in each room, measuring weekly compliance and providing this feedback to nurse managers. This auditing process may help identify barriers that can be addressed quickly (eg, unavailability of pens).
Finally, it is important to comment on the confidentiality concerns often raised in the context of whiteboard use. Confidentiality concerns largely arise from personal health information being used without a patient's explicit consent. If our recommendations are adopted, they require whiteboard use to be a patient‐centered and patient‐driven initiative. The type of information on the whiteboard should be determined with sensitivity but also with consent of the patient. We have not experienced any concerns by patients or providers in this regard because patients are told about the goals of the whiteboard initiative with our above principles in mind.
Conclusions
Patient whiteboards may improve communication among members of the healthcare team (eg, nurses, physicians, and others) and between providers and their patients (and family members). Further investigation is warranted to determine if adopting our recommendations leads to improved communication, teamwork, or patient satisfaction and care. In the meantime, as many hospitals continue to install and implement whiteboards, we hope our recommendations, accompanied by an emphasis on creating a patient‐centered communication tool, offer a roadmap for considering best practices in their use.
Acknowledgements
This study of patient whiteboards developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. The authors thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
Communication failures are a frequent cause of adverse events14; the Joint Commission (TJC) reports that such failures contributed to 65% of reported sentinel events.5 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.613 While these strategies largely address communication between healthcare providers, there is a growing emphasis on developing strategies to engage patients in their care, and improving communication with them and their families.
In 2007, TJC announced a new National Patient Safety Goal (NPSG) that encourage(s) patients' active involvement in their own care as a patient safety strategy.14 This builds upon a landmark Institute of Medicine report that highlighted patient‐centeredness as 1 of the 6 domains for delivering high‐quality care.15 Current literature on developing such patient‐centered strategies enumerates several approaches, including better access to health information, use of innovative technology solutions, and focused efforts at improving communication.1618
The placement of whiteboards in patient rooms is an increasingly common strategy to improve communication. These boards, typically placed on a wall near a patient's hospital bed, allow any number of providers to communicate a wide range of information. Both Kaiser Permanente's Nurse Knowledge Exchange program and the Institute for Healthcare Improvement's Transforming Care at the Bedside promote whiteboard use, though with little specific guidance about practical implementation.19,20 Despite their growing prevalence, there is no published literature guiding the most effective uses of whiteboards, or describing their impact on communication, teamwork, or patient satisfaction and care. We present findings from a survey of patient whiteboard use on an academic medical service, and offer a series of recommendations based on our findings and experiences.
Methods
We anonymously surveyed bedside nurses from 3 inpatient medical units, internal medicine housestaff, and faculty from the Division of Hospital Medicine at the University of California, San Francisco (UCSF). We solicited experiences of physician and nursing leaders who were engaged in whiteboard interventions over the past 2 years to identify relevant topics for study. Their experiences were based on isolated unit‐based efforts to implement whiteboards through a variety of strategies (eg, whiteboard templates, simple identification of provider teams, goals for the day). Their input guided the survey development and the suggested recommendations. The topics identified were then translated into multiple‐choice questions, and further edited for clarity by the authors. A Likert scale was used that measured frequency of use, usefulness, and attitudes toward patient whiteboards. An open‐ended question seeking additional comments about patient whiteboards was also asked. The survey was administered to nurses at staff meetings and through physical mailboxes on their respective patient care units with a 1‐month collection period. The survey was administered to housestaff and attendings via e‐mail listserves using an online commercial survey administration tool.21 The nursing surveys were later entered into the same online survey administration tool, which ultimately provided summary reports and descriptive findings to meet the study objectives. Our project was reviewed and approved by the UCSF Committee on Human Research.
Results
Survey responses were collected from 104 nurse respondents (81% response rate), 118 internal medicine housestaff (74% response rate), and 31 hospitalists (86% response rate). Nurses were far more likely to write on whiteboards, read what was written on them, and find the related information useful (Figure 1A‐C). Nurses, housestaff, and attendings all believed the bedside nurse was the single most important provider name listed on a whiteboard. However, the respondents differed in their rated value of other providers listed on the whiteboard (Figure 2). Nurses gave higher ratings to the utility of having patient care assistants (PCAs) listed as compared to housestaff and attendings. Overall, respondents felt it would be less useful to list consultants and pharmacists than the nurse, attending, and housestaff. All of the respondents believed family contact information was the most useful information on a whiteboard, whereas more nurses rated a goal for the day and anticipated discharge date as more useful than housestaff and attendings (Figure 3).



From an operational standpoint, the majority of respondents felt that nurses should be responsible for the information on a whiteboard, nurses and physicians together should create goals for the day, and the greatest barrier to using whiteboards was not having pens easily available (Figure 4A‐C). Most respondents also agreed that using templated whiteboards (with predefined fields) to guide content would increase their use (Figure 4D). All respondents believed that whiteboard use could improve teamwork and communication as well as patient care (Figure 5). Respondents also offered a variety of specific comments in response to an open‐ended question about whiteboard use (Table 1).


| From nurses | If MDs were engaged in using (or reviewing the information on) whiteboards more, it might reduce the number of times we page them to clarify care plans |
| It might be helpful to have a dedicated section on the whiteboard where families can write questions that are separate from other information that the nurse writes on them | |
| Part of the bedside nurse role is to be a patient advocate and the whiteboard can be a tool to assist in this important responsibility | |
| Nothing is worse than a patient (or family member) asking me, What's the plan for the day?and being unable to do so because a goal (or scheduled procedure) hasn't been communicated to me by the MD or written on the whiteboard | |
| I would use [whiteboards] more if they were clearly being used as a patient‐centered communication tool rather than trying to improve communication between us and the MDs. | |
| From physicians | The boards need to be kept simple for success. |
| There needs to be specific training to make this a cultural norm across care providers and reinforced on a regular basis. If it's a priority, there should be audits, tracking for performance (accuracy and updated info), and feedback to providers. I would also ask patients what info they would like to see, as [whiteboards] should be patient‐centered, not provider‐centered. | |
| Having providers intermittently write on whiteboards should not be considered a substitute for communication. In fact, this would likely only further display our lack of cohesive communication to patients and families. | |
| I have been skeptical that the goals for the day for an ill patient can be satisfactorily reduced to a statement that fits on a whiteboard and that forecasting a day of discharge well in advance is frequently wrong and may create more confusion than it alleviates. I am also concerned that if a goal for the day on a whiteboard is intended for the nurse, this is substituting for richer channels of communications, such as the nurse reading the progress notes, speaking with the physicians, or communicating through the charge nurse who attends our case management rounds. | |
| Whiteboards are frequently not accurate, underused, and they require patients to have visual acuity, cognition, and speak Englishall challenges depending on your patient population. |
Discussion
Our findings demonstrate the potential value of patient whiteboards, which is supported by the vast majority of respondents, who agreed their use may improve patient care and teamwork. It is also clear that whiteboard use is not achieving this potential or being used as a patient‐centered tool. This is best illustrated by findings of their low rate of use and completion among attendings and housestaff (Figure 1A, B) and the lack of consensus as to what information on the whiteboards is useful. Patient whiteboards require defined goals, thoughtful planning, regular monitoring, and ongoing evaluation. The challenges around effective adoption and implementation is perhaps more about ensuring compliance and completion rather than simply gaining buy‐in and engagement for their value.
While the differential use of whiteboards between nurses and physicians was not surprising, a few specific findings warrant further discussion. First, it is interesting that nurses rated their own names and that of PCAs as the most useful, while physicians rated the nurse's name as being of equal value to their own. This may speak to the role PCAs play for nurses in helping the latter provide bedside care, rather than a reflection of the nurses' perception of the value of PCAs for patients. Second, while all respondents rated highly the value of family contact information on the whiteboard, nurses valued a goal for the day and anticipated discharge date more highly than did physicians. These findings likely reflect that nurses desire an understanding about plans of care and if they are not communicated face‐to‐face as the most effective strategy,22 they should at least be spelled out clearly on a whiteboard. This is supported by evidence that better collaboration between nurses and physicians improves patient outcomes.23 It may also be that physicians place more value on their own progress notes (rather than whiteboards) as a vehicle for communicating daily goals and discharge planning.
Other practical considerations involve who owns it and, if we do create goals for the day, whose goals should they represent? The majority of nurse and physician responses advocated for nurses to be responsible for accurate and complete information being updated on whiteboards. A larger percentage of attendings favored shared responsibility of the whiteboard, which was reinforced by their support of having goals for the day created jointly by nurses and physicians. Interestingly, a much smaller percentage of respondents felt goals for the day should be driven by patients (or family members). These data may point to the different perspectives that each individual provider bringsphysician, nurse, pharmacist, discharge plannerwith their respective goals differing in nature. Finally, it is also interesting that while attendings and housestaff believed that whiteboards can improve patient care teamwork/communication (Figure 5), a much smaller percentage actually read what is on them (Figure 1B). This may reflect the unclear goals of whiteboards, its absence as part of daily workflow, the infrequency of updated information on them, or perhaps an institution‐specific phenomenon that we will use to drive further improvement strategies.
Selected respondent comments (Table 1) highlight important messages about whiteboard use and provide helpful context to the survey responses. We found that the goal of whiteboard use is not always clear; is it to improve communication among providers, to improve communication with patients, a tool to engage patients in their care, or some combination of the above? Without a clear goal, providers are left to wonder whether whiteboard use is simply another task or really an intervention to improve care. This may in part, or perhaps fully, explain the differences discovered in whiteboard use and practices among our surveyed providers.
If, however, one were to make clear that the goal of patient whiteboards is to engage patients in their care and help achieve an important NPSG, methods to implement their use become better guided. A limitation of our study is that we did not survey patients about their perceptions of whiteboards use, an important needs assessment that would further drive this patient‐centered intervention. Regardless, we can draw a number of lessons from our findings and devise a set of reasonable recommendations.
Recommendations
We provide the following set of recommendations for hospitals adopting patient whiteboards, drawing on our survey findings and experiences with implementation at our own institution. We also acknowledge the role that local hospital cultures may play in adopting whiteboard use, and our recommendations are simply guidelines that can be applied or used in planning efforts. We believe effective use of a patient whiteboard requires a patient‐centered approach and the following:
-
Whiteboards should be placed in clear view of patients from their hospital bed
A simple yet critical issue as placing a whiteboard behind a patient's bed or off to the side fails to provide them with a constant visual cue to engage in the information.
-
Buy and fasten erasable pens to the whiteboards themselves
In our institution, purchasing pens for each provider was a less effective strategy than simply affixing the pen to the whiteboard itself. A supply of erasable pens must be available at the nursing station to quickly replace those with fading ink.
-
Create whiteboard templates
Our findings and experience suggest that structured formats for whiteboards may be more effective in ensuring both important and accurate information gets included. Blank whiteboards lead to less standardization in practice and fail to create prompts for providers to both write and review the content available. Anecdotally, we created a number of whiteboards with templated information, and this did seem to increase the consistency, standardization, and ease of use.
-
Whiteboard templates should include the following items:
-
Day and Date
This serves to orient patients (and their families) as well as providers with the date of information written on the whiteboard. It is also an important mechanism to ensure information is updated daily.
-
Patient's name (or initials)
With bed turnover (or patient transfers to different beds and units) commonplace in hospital care, we believe that listing the patient's name on the board prevents the potential for patients (and their families) or providers to mistakenly take information from a previous patient's care on the whiteboard for their own.
-
Bedside nurse
This was noted as the most useful provider listed on a patient whiteboard, which is quite logical given the role bedside nurses play for hospitalized patients.
-
Primary physician(s) (attending, resident, and intern, if applicable)
This was noted as the next most important provider(s) and perhaps increasingly important both in teaching and nonteaching settings where shift‐work and signouts are growing in frequency among physicians.
-
Goal for the day
While this was not a consensus from our survey respondents, we believe patients (rather than providers) should ultimately guide determination of their goal for the day as this engages them directly with the planachieving a patient‐centered initiative. In our experience, an effective strategy was having the bedside nurse directly engage patients each morning to help place a goal for the day on their whiteboard.
-
Anticipated discharge date
While understanding the potential for this date to change, we believe the benefits of having patients (and their families) thinking about discharge, rather than feeling surprised by it on the morning of discharge, serves as an important mechanism to bridge communication about the discharge process.24
-
Family member's contact information (phone number)
-
Questions for providers
This last entry allows a space for families to engage the healthcare team and, once again, create an opportunity for clarification of treatment and discharge plans.
-
Bedside nurses should facilitate writing and updating information on the whiteboard
Without our survey findings, this might have generated debate or controversy over whether nurses should be burdened with one more task to their responsibilities. However, our nurse respondents embraced this responsibility with spontaneous comments about their patient advocate role, and stated that whiteboards can serve as a tool to assist in that responsibility. Furthermore, not a single nurse respondent stated as barrier to use that I didn't think it was my responsibility. Nonetheless, whiteboard use must be a shared communication tool and not simply a tool between nurse and patient. Practically, we would recommend that bedside nurses facilitate updating whiteboards each morning, at a time when they are already helping patients create a goal for the day. Other providers must be trained to review information on the whiteboard, engage patients about their specific goal, and share the responsibility of keeping the information on the whiteboard updated.
-
Create a system for auditing utilization and providing feedback early during rollout
We found that adoption was very slow at the outset. One strategy to consider is having designated auditors check whiteboards in each room, measuring weekly compliance and providing this feedback to nurse managers. This auditing process may help identify barriers that can be addressed quickly (eg, unavailability of pens).
Finally, it is important to comment on the confidentiality concerns often raised in the context of whiteboard use. Confidentiality concerns largely arise from personal health information being used without a patient's explicit consent. If our recommendations are adopted, they require whiteboard use to be a patient‐centered and patient‐driven initiative. The type of information on the whiteboard should be determined with sensitivity but also with consent of the patient. We have not experienced any concerns by patients or providers in this regard because patients are told about the goals of the whiteboard initiative with our above principles in mind.
Conclusions
Patient whiteboards may improve communication among members of the healthcare team (eg, nurses, physicians, and others) and between providers and their patients (and family members). Further investigation is warranted to determine if adopting our recommendations leads to improved communication, teamwork, or patient satisfaction and care. In the meantime, as many hospitals continue to install and implement whiteboards, we hope our recommendations, accompanied by an emphasis on creating a patient‐centered communication tool, offer a roadmap for considering best practices in their use.
Acknowledgements
This study of patient whiteboards developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. The authors thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204(4):533–540.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- The Joint Commission: Sentinel Event Statistics, March 31,2009. Available at: http://www.jointcommission.org/SentinelEvents/Statistics. Accessed October 2009.
- ,,, et al.Bridging the communication gap in the operating room with medical team training.Am J Surg.2005;190(5):770–774.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,.Enhancing patient safety through teamwork training.J Healthc Risk Manag.2001;21(4):57–65.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- The Joint Commission's National Patient Safety Goals 2007 for Hospital/Critical Access Hospital. Available at:http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_hap_cah_npsgs.htm. Accessed October 2009.
- Institute of Medicine (U.S.). Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.A systems approach to patient‐centered care.JAMA.2006;296(23):2848–2851.
- ,,,,.Microsystems in health care: Part 4. Planning patient‐centered care.Jt Comm J Qual Saf.2003;29(5):227–237.
- Gerteis M, Edgman‐Levitan S, Daley J, Delbanco TL, eds.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,.Transforming Care at the Bedside. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement;2004. Available at: http://www.ihi.org. Accessed October 2009.
- ..Nurse Knowledge Exchange: Patient Hand Offs. American Academy of Ambulatory Care Nursing (AAACN) Viewpoint. Sep/Oct 2007. Available at: http://findarticles.com/p/articles/mi_qa4022/is_200709/ai_n21137476. Accessed October 2009.
- Survey Console. Available at: http://www.surveyconsole.com. Accessed October 2009.
- How do we communicate?Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed October 2009.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204(4):533–540.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- The Joint Commission: Sentinel Event Statistics, March 31,2009. Available at: http://www.jointcommission.org/SentinelEvents/Statistics. Accessed October 2009.
- ,,, et al.Bridging the communication gap in the operating room with medical team training.Am J Surg.2005;190(5):770–774.
- ,,, et al.Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project.Health Serv Res.2002;37(6):1553–1581.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,.Enhancing patient safety through teamwork training.J Healthc Risk Manag.2001;21(4):57–65.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- ,,, et al.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) experience.J Gen Intern Med.2008;23(12):2053–2057.
- The Joint Commission's National Patient Safety Goals 2007 for Hospital/Critical Access Hospital. Available at:http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_hap_cah_npsgs.htm. Accessed October 2009.
- Institute of Medicine (U.S.). Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.A systems approach to patient‐centered care.JAMA.2006;296(23):2848–2851.
- ,,,,.Microsystems in health care: Part 4. Planning patient‐centered care.Jt Comm J Qual Saf.2003;29(5):227–237.
- Gerteis M, Edgman‐Levitan S, Daley J, Delbanco TL, eds.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,.Transforming Care at the Bedside. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement;2004. Available at: http://www.ihi.org. Accessed October 2009.
- ..Nurse Knowledge Exchange: Patient Hand Offs. American Academy of Ambulatory Care Nursing (AAACN) Viewpoint. Sep/Oct 2007. Available at: http://findarticles.com/p/articles/mi_qa4022/is_200709/ai_n21137476. Accessed October 2009.
- Survey Console. Available at: http://www.surveyconsole.com. Accessed October 2009.
- How do we communicate?Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed October 2009.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
Engaging Patients at Hospital Discharge
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
Non–Housestaff Medicine Services in Academic Centers
Many academic medical centers (AMCs) have developed nonhousestaff services to provide clinical care once provided by physicians‐in‐training. These services, often staffed by hospitalists and/or midlevel providers, have experienced tremendous growth in the past few years, yet very little exists in the literature about their development, structure, efficacy, or impact on hospitals, patients, and hospital medicine programs. The primary forces driving this growth include Accreditation Council for Graduate Medical Education (ACGME) resident duty hour restrictions,1 growth of the hospitalist movement,2 and the emphasis on simultaneously improving financial performance and quality of care in AMCs.3
Resident Duty Hour Restrictions
In 2003, the ACGME mandated restrictions on resident work hours, limiting trainees to 80 hours per week.1 Many training programs struggled with how to provide important clinical services while complying with the new restrictionscreating numerous models that bridged care between different shifts of residents.45 Implementation of day floats (a dedicated resident who rounds with the postcall team), night floats (a dedicated overnight resident who admits and cross‐covers patients), or some variation of both was common.6 No guidelines accompanied the ACGME mandate, leaving institutions to independently structure their programs without a known best practice.
Subsequent literature carefully addressed how the duty hour restrictions affect residents' lives and education but failed to discuss models for providing care.711 Training programs began to institute necessary changes but in doing so, created greater patient discontinuity and increased handoffs between residents, elevating the potential for adverse patient outcomes.12 Recent large‐scale studies indicate that inpatient care is the same or improved since adoption of the duty hour restrictions,1316 but controversy continues, with several editorials debating the issue.1719
Because increasing the volume of patients on housestaff services was not a viable option,20 many AMCs created nonhousestaff services and hired midlevel providers (nurse practitioners and physician assistants) to offset resident workloads and comply with the new restrictions. However, this strategy represented a very expensive alternative.21 Moreover, the current 80‐hour work limits may be revised downward, particularly given the lower restrictions in other countries,22 and this will further drive the demand for nonhousestaff services. Hospitalists, with their documented impact on efficiency and return on investment,23 represent a solution to fill these needs and have quickly become the predominant approach at AMCs.
The Hospitalist Movement
Since the term hospitalist was first coined in 1996,24 the remarkable growth of the number of practicing hospitalists emphasizes how first community hospitals and now AMCs have embraced this approach.25 With more than 20,000 nationwide and projections that the field will grow to 30,000 by 2010,26 hospitalists are becoming the primary providers for in‐patients.2 This growth was further catalyzed when widely expressed concerns about safety and quality became public,2728 and hospitalists incorporated patient safety and quality improvement activities into their efforts.3 The confluence of these factors also prompted emergence of hospital medicine programs at AMCs, a growth that came with anticipated dangers.29 Reflecting the recognition that hospital medicine is becoming a separate specialty30 and is integral to the functioning of an AMC, institutions now operate dedicated divisions of hospital medicine.
AMCs and Hospital Performance
AMCs operate 3 related enterprises: a medical school that trains future physicians, a research arena that promotes basic and clinical investigation, and health care services that often encompass both hospitals and clinics. The financial viability of AMCs has always been a topic of debate, largely because of the different missions they pursue and the financial means by which they survive.3133 Over the past decade, cuts in Medicare reimbursement, challenges in balancing bed availability with occupancy rates, and a growing emphasis on cost reduction have created a more competitive health care environment, but without the predicted demise of AMCs.34 Because education and research generally fail to bolster the bottom line, AMCs have focused on optimizing clinical services to promote financial viability.
Hospitalists are uniquely positioned to help this bottom line, just as they do at community hospitals. Their involvement in patient care may produce reductions in length of stay, greater efficiency in discharge planning, and significant cost savings.3537 Hospitalists may also improve throughput in emergency departments and decrease wait times, leading to more efficient bed utilization.38 This leads to a potential for greater hospital revenue by increasing both the number of admissions, particularly surgical cases, and staffed inpatient beds, the latter a premium, as AMCs continue to expand their bed capacity almost annually. Finally, hospitalists may serve as change agents in improving the quality and safety of care delivered, an increasingly important metric given the desire for and expansion of publicly reported measures.
From a financial standpoint, Medicare support to AMCs for training residents now subsidizes fewer clinical care hours. Hospitalist‐driven nonhousestaff services will continue to fulfill a need created by this marked change in residency training. The tension of who pays for nonhousestaff servicesincreased federal support, financial backing from AMCs, or academic department fundsposes an ongoing struggle. In fact, this may be the most important issue currently debated among hospital administrators and department chairs. Regardless, AMCs continue to view hospitalists as a mechanism (or even solution) to maintaining their financial bottom line through improving care delivery systems, adhering to resident work hour restrictions, leading quality and safety improvement initiatives, and improving clinical patient outcomes.
MODELS FOR NONHOUSESTAFF MEDICAL SERVICES
For AMCs developing nonhousestaff services, the process begins by addressing a series of important questions (Table 1). How these questions are answered is often driven by local factors such as the vision of local leadership and the availability of important resources. Nonetheless, it is important for hospitals to share their experiences because best practices remain unclear. Table 2 provides a tabular snapshot of nonhousestaff medicine services at 5 AMCs to highlight similarities and differences. Data in the table were compiled by having a representative from each AMC report the different attributes, which reflects each program as of July 2007. Table 2 provides no data on the quality or efficiency of housestaff versus nonhousestaff services, though this type of investigation is underway and will be critical in future planning.3940
| Questions | Potential options |
|---|---|
| Who will provide care on nonhousestaff services? | Physicians seeking a 1‐year position |
| Physicians committed to a purely clinical career | |
| Physicians committed to an academic career in hospital medicine | |
| Will hospitalists share nonhousestaff service time, or will there be dedicated nonhousestaff hospitalists? | Hybrid positions |
| Dedicated nonhousestaff hospitalists | |
| Use of PGY‐4s1‐year positions (often individuals planning a fellowship) | |
| How should staffing be organized? | Hospitalist‐only services |
| Use of midlevel providers | |
| Will there be 24‐7 coverage, and if so, how will nights be staffed? | Dedicated nocturnists |
| Shared among daytime hospitalists | |
| Midlevel providers | |
| Moonlighters (fellows or residents) | |
| What type of schedule will provide blocks of clinical time to ensure continuity of care but also ensure adequate nonclinical time to prevent physician burnout and turnover? | 7 on/7 off sequences |
| 45 day sequences | |
| Longer shifts with fewer shifts per month | |
| Shorter shifts with more shifts per month | |
| Where will patients on a nonhousestaff service receive care? | Geographically designed serviced |
| ○ Different floor | |
| ○ Different hospital | |
| Mixed among housestaff service | |
| What patient population will be cared for on the nonhousestaff service? | Same as on housestaff service |
| Based on bed availability if nonhousestaff service is geographic (a unit) | |
| Based on triage guidelines (lower acuity, observation patients, specific diagnoses) | |
| What volume of patients will be cared for on the nonhousestaff service? | Fixed census cap based on staffing |
| Flexible census depending on activity of housestaff service (above their cap) | |
| Will compensation for providing nonhousestaff services differ from that on housestaff services? | Higher base salary |
| Incentives tied to nonhousestaff time | |
| Different incentive structures |
| Attributes | BWH | Emory | University of Michigan | Northwestern | UCSF |
|---|---|---|---|---|---|
| Description of staffing model | Mon.‐Sun.: 1 daytime Hospitalist | Mon.‐Sun.: 4 daytime hospitalists, 2 swing shift admitters | Weekdays: 7 daytime hospitalists, 1 swing shift hospitalist | Mon.‐Sun.: 8 daytime hospitalists, 1 triage hospitalist | Weekdays: 2 daytime hospitalists, 1 swing shift hospitalist |
| Nights: 1 MD | Nights: 1 MDs | Weekends: 7 daytime hospitalists | Nights: 2 MDs | Weekends: 2 daytime hospitalists | |
| Nights: 2 MDs | Nights: 1 MD | ||||
| Location of service | In same university hospital | In same university hospital | In same university hospital | In same university hospital | Physically separate hospital affiliate (UCSF Medical Center at Mount Zion) |
| Nonhousestaff FTEs/total hospitalist group | 3/15 | 10/14 | 20/30 | 25/34 | 6/36 |
| What hospitalists provide care on nonhous estaff services? | Core of 3 hospitalists (also do month on housestaff service) | Hospitalist group shares nonhousestaff services | Core of 14 FTEs dedicated to nonhousestaff services | Hospitalist group shares nonhousestaff services | Core of 6 Mount Zionbased hospitalists (also spend 23 months on housestaff service at university hospital) |
| Other 6 FTEs consist of 10 faculty with mixed roles | |||||
| Age of service | 2 years | 4 years | 3 years | 5 years | 3 years |
| How patients get assigned to non‐housestaff service? | 1. Only ED admissions with no transfers from ICU or other services | Assigned by rotation | 1. Alternating admissions with housestaff services during afternoon | 1. Alternating admissions with housestaff services during day | 1. Lower‐acuity admissions from ED |
| 2. Admit whenever bed open on service (geographic) | 2. Observation cases triaged directly to service | 2. Lower‐acuity patients and direct admissions | 2. Lower‐acuity admissions from clinics | ||
| 3. Once housestaff cap, all subsequent admits until midnight to nonhousestaff service | 3. Nonhousestaff service admits all patients once resident caps reached | 3. Transfers from housestaff service no longer requiring tertiary services (or with complex discharge planning) | |||
| Average daily census of nonhousestaff service | 12 | 56 | 70 (75 cap) | 8595 | 2026 |
| Number of shifts per month/shift duration | 15/1012 hours | 15/12 hours | 1517 (depending on number of nights covered)/812 hours (swing = 8 hours, day = 1012 hours, night = 12 hours) | 20/1012 hours | 1617/1012 hours |
| Shift sequences | 710 days consecutive | Variable | 67 days consecutive followed by 1 night for those who cover nights | 7 days consecutive | 4‐ to 6‐day variable sequences |
| Total clinical days worked/year | 168 | 182.5 | 185202 (depending on number of nights covered) | 212 | 196 |
| Weekend clinical time | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends |
| Night coverage/by whom? | Yes/exclusively moonlighters | Yes/shared (50% covered by 1 dedicated nocturnist) | Yes/66% of nights staffed by dedicated nocturnists with remainder shared | Yes/exclusively by six 1‐year nocturnists | Yes/exclusively by moonlighters |
| Presence of midlevel providers | Yes 6 FTE PAs Mon.‐Sun. | No | Yes 8 FTE PAs weekdays | No | No |
| Presence of dedicated case manager | Yes | Yes | Yes | No | Yes |
| Presence of medical students for patient care | No | No | Yes, 4th‐year subinterns or students on elective rotation | No | No |
| Compensation model | Salary + weekend bonus beyond 10 | Salary + incentive | Base + shift‐based incentive + quality incentive | Salary + incentive | Salary |
| Pay differential compared to housestaff service compensation | 10% Higher because of weekend bonus | None | About 20% higher base compensation; loan forgiveness program tied to nonhousestaff time | None | About 20% higher compensation |
| Hospital financial support | Yes | Yes | Yes | Yes | Yes |
Table 2 does illustrate several important considerations in structuring nonhousestaff services. For example, if a nonhousestaff service operates at a different physical location, careful triage of patients is necessary. Resources, including the availability of subspecialty and surgical consultants, may differ, and thus patient complexity and acuity may dictate whether a patient gets admitted to the nonhousestaff service. These triage factors were a major challenge in the design of UCSF's nonhousestaff service. The other nonhousestaff services handle overflow admissions after the housestaff service reaches a census or admission cap; transfers between services rarely occur, and resources are similar.
Other observations include that hospitalists work a similar number of hours each year and cover 50% of weekends but with differing shift lengths and sequences. Each service also provides night coverage but only Emory, the University of Michigan, and Northwestern utilize dedicated nocturnists. The University of Michigan and Brigham & Women's Hospital are the only sites that employ midlevel providers who work closely with hospitalists. In terms of group structure, Northwestern's hospitalists are the most integrated, with each hospitalist sharing equal responsibility for nonhousestaff coverage. In contrast, the other programs use selected hospitalists or a dedicated core of hospitalists to provide nonhousestaff services. Compensation models also vary, with certain groups salaried and others having incentive systems, although all receive hospital‐based funding support. Hospital‐based funding support ranges from 40% to 100% of total program costs across sites, creating similar variance in a given program's deficit risk. Finally, most programs do compensate nonhousestaff services at higher rates.
All the decisions captured in Table 2 have implications for costs, recruitment, and service structure. Furthermore, the striking variations demonstrate how different academic hospitalist positions can occur both within a hospital medicine group and across institutions. Of note, Table 2 only characterizes nonhousestaff medicine services, not the growing number of comanagement (eg, orthopedics, neurosurgery, or hematology/oncology) and other clinical services (eg, observation unit or preoperative medicine clinic) also staffed by hospitalists at AMCs.
CHALLENGES
Hospital medicine programs and AMCs face several challenges in building non‐housestaff services, but these will likely become less daunting as programs learn from their own experiences, from those of colleagues at other institutions, and from future investigations of these care models. We highlight a few issues below that warrant important consideration.
The Equities of the System
Prior to developing nonhousestaff services, our academic hospitalist programs scheduled teaching service time in month or half‐month blocks, balancing holidays and weekends. Equity in scheduling became a function of required clinical time, sources of non‐clinical funding (eg, grants, educational or administrative roles), and expectations for scholarship, attributes typical of most subspecialty academic divisions. Given the differing clinical missions that have stimulated academic hospital medicine programs to form, concerns of scheduling equity have grown, posing challenges not experienced in other divisions.
Institutions that choose to divide housestaff and nonhousestaff duties among distinct groups of hospitalists create the potential for a 2‐tiered system, one in which those with housestaff roles are more valued and respected by the institution. Hospitalists working on nonhousestaff services admit patients, write orders, and field direct patient calls, a role rarely undertaken by subspecialty attendings or hospitalists on housestaff services. Our collective experiences provide evidence of the danger of this second‐class‐citizen status, one that requires attention to ensure job satisfaction, retention, and necessary career development.
Institutions have accentuated the second‐class‐citizen concern by staffing nonhousestaff roles with 1‐year hospitalistsPGY‐4s. Most of these hires in our institutions are individuals just out of residency and intent on pursuing a fellowship. We speculate that they enjoy the comforts of the AMC where they often trained and accept purely nonhousestaff positions because of what they view as an appealing work schedule and salary. Although this approach addresses the growing need for hospitalists on nonhousestaff services in the short term, these positions must remain attractive enough (both financially and professionally) to encourage residency graduates to pursue an academic hospitalist career instead of a 1‐year position as a transition to fellowship. Otherwise, the approach conveys a message that relatively inexperienced physicians are good enough to be hospitalists.
Developing a cadre of clinically focused hospitalists who provide outstanding patient care and also garner respect as successful academicians is a difficult task. Although 1 group in our sample (Northwestern) shares nonhousestaff responsibilities equally, others may find this impractical, particularly where faculty members were hired before nonhousestaff services were established. Redefining such clinical positions several years into a career may be challenging, as it forces faculty members into roles they didn't sign up for or grandfathers them out of such roles, adding to the risk of a 2‐tiered system. Alternatively, groups may focus on building academic activities into nonhousestaff services, including medical student teaching, quality improvement, or clinical research activities. In this article, we deliberately classified these services as nonhousestaff rather than non‐teaching because the latter fails to acknowledge that these hospitalists often serve as teachers (eg, housestaff conferences, supervision of midlevel providers, and/or rotating medical students)an important if not symbolic distinction. It is imperative that planning for nonhousestaff services balance the larger academic mission of hospital medicine groups with creating equitable, valued, and sustainable job descriptions.
Defining the Patient Mix
Developing an optimal patient mix on nonhousestaff services also carries important implications. For services that work in parallel with the housestaff service and simply take extra patients above the resident cap, this concern may be less significant. However, other nonhousestaff services have been structured to care for lower‐acuity patients (eg, cellulitis, asthma, pneumonia) or select patient populations (eg, sickle cell or inflammatory bowel disease). This distribution system potentially changes the educational experience on the housestaff servicedecreasing the bread‐and‐butter admissionsbut also may affect the job satisfaction of hospitalists and midlevel providers on nonhousestaff services. Building triage criteria, working with emergency department leadership, and avoiding patients being turfed between different services is critical. We strongly recommend a regular process to review admissions to each service and determine when the triage process requires further calibration.
Recruitment and Retention
Traditionally, graduates of residency or fellowship training programs chose academic positions because of an interest in teaching, a desire for scholarship, or a commitment to research. Those interested in primarily clinical roles typically pursued positions in nonacademic settings. The development of nonhousestaff services challenges this paradigm because the objective for academic hospitalist leadership now becomes recruiting pure clinicians as well as academicians. These might be the same individual, a hospitalist who provides both housestaff and nonhousestaff services, or 2 different individuals if the nonhousestaff service is covered by dedicated hospitalists. In addition, with the current promotion structure in academia, a purely clinical position may be less attractive, as it provides fewer opportunities for advancement.
Therefore, recruitment and retention of academic hospitalists will require job descriptions that provide dedicated teaching opportunities, time for participation in quality and safety improvement projects, or pursuit of a scholarly interest in non‐clinical timethe diastole of an academic hospitalist.41 Hospital medicine leadership will also need to better distinguish off‐time from non‐clinical time, as many young hospitalists struggle to balance professional and personal commitmentsa recipe for burnout.42 Regardless of how clinical responsibilities differ between 2 hospitalists, providing them with similar academic resources is what will distinguish their positions from that in the community. Furthermore, many groups have chosen to pay faculty a premium for their nonhousestaff roles or to use specific recruitment incentives such as educational loan forgiveness programs.
With the expected growth of nonhousestaff services and surgical comanagement, hospital medicine programs will also need to determine if new hires will focus on a specific service (eg, orthopedic hospitalist) or whether job descriptions will include a mix of activities (eg, 3 months' teaching service, 3 months' nonhousestaff medical service, and 3 months' surgical comanagement service). A second and equally important question is where does the hospitalist live? If cardiology wants hospitalists to care for their patients, should they be hired and mentored by cardiologists or by hospitalists in a division of general or hospital medicine? In many cases, a graduating resident with plans to pursue a fellowship (eg, cardiology or hematology/oncology) may be a perfect candidate for a 1‐year position on his or her future specialty service. However, in the long term, maintaining all the academic hospitalists under the same umbrella will provide greater mentorship, professional development, opportunities for collaboration, clinical diversity, and sense of belonging to a group, rather than being a token hospitalist for another division.
Compensation and Financial Relationships with AMCs
Salaries for hospitalists working on nonhousestaff services are typically higher at AMCs, which are competing with community standards given the similar level of clinical hours worked. However, although pay for nonhousestaff activities should reflect the nature of the work, compensation models based on clinical productivity alone may prove inadequate. It appears hospitalists working in academic facilities spend significant time on indirect patient care because of these hospitals' inefficiencies, usually not found in community settings.43 Devising compensation for an academic hospitalist requires careful attention and must balance a number of factors because these hospitalists will not generate their entire salary from clinical services. Financial support must come from either the division or medical center, an annual negotiation at AMCs.
Several methods exist to structure hospitalist compensation. A hospitalist's salary may be fixed, may have a base salary with incentives, or may be derived based on clinical productivity. For example, if a hospital medicine program provides both housestaff and nonhousestaff services and employs a fixed‐salary approach, it may choose a menu‐style method to determine compensation (eg, 6 months on nonhousestaff service at x dollars/month + 3 months on housestaff service at x dollars/month = annual salary). If a hospitalist takes on a funded nonclinical role or secures extramural funding, the salary menu gets adjusted accordingly as the clinical time is bought out. Critics of the fixed‐salary approach argue that paying each hospitalist the same salary regardless of the specific job description yields an inequitable system in which some are rewarded with less clinical time.
Compensation should probably have a guaranteed base salary with incentives, which could be determined by a formula that weighs clinical productivity, quality improvement efforts, scholarly activity, and teaching excellence. This model provides financial incentives to develop both clinically and academically but introduces complexity in determining a fair incentive structure. Finally, compensation can be structured without salary guarantee and putting compensation fully at risk based on clinical productivity, although this is an unlikely strategy for any hospital medicine group. This approach does disproportionately reward high volume providers, potentially at the risk of quality and safety, but also creates significant incentives to improve efficiency.
With respect to AMC relationships, hospital medicine programs must ensure the positive return on investment that drives financial support at their institutions. This fundamental economic dynamic makes AMCs dependent on their hospital medicine groups and vice versa. We caution programs from solely relying on measures such as reduced hospital costs or length of stay as a basis of funding unless there is a reward for maintaining performance once it inevitably plateaus. Moreover, explicitly tying utilization efficiency (ie, length of stay) to salary violates Stark rules44 and carries potential malpractice implications should patient care errors be attributable to premature hospital discharge. Over time hospitalists will need to maintain clinical benchmarks but also provide additional and valued services to their institutions, including quality and safety improvement activities and compliance with residency work hour restrictions.
Defining the Academic Hospitalist
The question is simple and perhaps philosophical: Are hospitalists who work at an AMC academic hospitalists? And what job description truly defines an academic hospitalist? Currently, there are no standards for the clinical activity of an academic hospitalist position (eg, number of weeks, weekends, and hours) or for assessment of nonclinical productivity. Hospital medicine programs face the challenge of defining positions that fulfill the growing clinical mission at AMCs but have little experience or guidance in ensuring they will lead to advancing the academic mission. Specifically, how do hospitalists who provide mostly clinical care, particularly on nonhousestaff services, achieve promotion? Hospital medicine program leadership must create enough opportunity and time for the development of skills in research, education, and quality or systems improvement if academic hospitalists are to succeed.
The Association of Chiefs of General Internal Medicine (ACGIM), the Society of General Internal Medicine (SGIM), and the Society of Hospital Medicine (SHM) are currently collaborating to develop consensus guidelines in this area. Ultimately, through the efforts of these important governing bodies, the specialty of hospital medicine will be able to demonstrate the unique skills and services they provide and move toward advocating for academic promotion criteria that recognize their value and accomplishments.
FUTURE DIRECTIONS
Many lament that the milieu for academic hospitalists raises more challenges than solutions, but we believe the current era is one of excitement and opportunity. In the coming years, we will experience continued growth of nonhousestaff services, including greater comanagement with our surgical and medical specialty colleagues. These opportunities will create new relationships and increase our visibility in AMCs. However, we must remain committed to studying nonhousestaff services and determine if and how they differ from their housestaff and community counterparts, as this will be an important step toward addressing current challenges.
As hospitalists take on increasingly diverse roles,45 we must also lead initiatives to better train, recruit, and retain those interested in our specialty. Promoting our field and recruiting future faculty should occur through local hospitalist career nights, events at national meetings (targeting students, housestaff, and fellows), and other mechanisms utilized by our subspecialty colleagues. For housestaff interested in fellowship training, the growing number of hospitalist fellowships can provide skills in teaching and quality improvement.46 For trainees committed to research, we should work with existing general medicine research fellowships and partner to provide hospitalist mentorship.
Hospitalists are in a unique position to influence the delivery of clinical services, shape the future of residency training, guide quality and safety improvement initiatives, and take on leadership roles through our departments, universities, and medical centers. With the growing number of clinical services being added to our portfolio, we will need careful planning and evaluation of our efforts to build successful partnerships and develop faculty roles that balance clinical and academic pursuits to sustain long‐term and satisfying hospitalist careers.
- Accreditation Council for Graduate Medical Education. Information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp Accessed May 28,2007.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- .Duty hours for resident physicians—tough choices for teaching hospitals.N Engl J Med.2002;347:1275–1278.
- ,.Resident work hours, hospitalist programs and academic medical centers.The Hospitalist.2005;Jan/Feb:30–33.
- .Adapting to duty‐hour limits—four years on.N Engl J Med.2007;356:2668–2670.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,,, et al.Effect of Residency Duty‐Hour Limits. Views of Key Clinical Faculty.Arch Intern Med.2007;167:1487–1492.
- ,,,.Perceived impact of duty hours regulation: a survey of residents and program directors.Am J Med.2007;120:644–648.
- ,,,.The impact of duty hours on resident self reports of errors.J Gen Intern Med.2007;22:205–209.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,.Changes in hospital mortality associated with residency work‐hour regulations.Ann Intern Med.2007;147:73–80.
- ,,,.Changes in outcomes for internal medicine inpatients after work‐hour regulations.Ann Intern Med.2007;147:97–103.
- ,,, et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:975–983.
- ,,, et al.Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:984–991.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356:2665–2667.
- ,.Hippocrates affirmed? Limiting residents' work hours does no harm to patients.Ann Intern Med.2007;356:143–144.
- ,.Evaluating resident duty hour reforms.JAMA.2007;298:1055–1057.
- ,,,,.Housestaff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167:47–52.
- ,,,.Predicting future staffing needs at teaching hospitals: use of an analytical program with multiple variables.Arch Surg.2007;142:329–334.
- . A primer on: resident work hours. American Medical Student Association. 6th ed. 2005. Available at: http://www.amsa.org/rwh/RWHprimer_6thEdition.pdf. Accessed May 28,2007.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- Society of Hospital Medicine. Media Center link: Growth of hospital medicine nationwide. Available at www.hospitalmedicine.org. Accessed May 28,2007.
- Kohn L,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington DC:Committee on Quality of Health Care in America, Institute of Medicine, National Academy Press;2000.
- Committee on Quality of Health Care in America, Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- .What will board certification be‐and mean‐for hospitalists?J Hosp Med.2007;2:102–104.
- .Academic medical centers under siege.N Engl J Med.1994;331:1370–1371.
- ,.Academic medicine meets managed care: a high impact collision.Acad Med.1996;71:839–845.
- .Preventing the academic medical center from becoming an oxymoron.Acad Med.1996;71:117–120.
- ,,.Why have academic medical center survived?JAMA.2005:293;1495–1500.
- ,,,.Comparison of hospitalist and nonhospitalists in inpatient length of stay adjusting for patient and physician characteristics.J Gen Intern Med.2004;19:1127–1132.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22;662–667.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,.Hospitalists and an innovative emergency department admissions process.J Gen Intern Med.2004;19:266–268.
- ,,,,.Comparison of resource utilization and clinical outcomes between teaching and nonteaching medical services.J Hosp Med.2007;2:150–157.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22:662–667.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1:368–377.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction. 2006;1–45. Available at: http://www.hospitalmedicine.org. Accessed August 11,2007.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1:88–93.
- A Guide to Complying with Stark Self‐Referral Rules.Washington, DC:Atlantic Information Services, Inc.; 2004. Available at: http://www.aispub.com/. Accessed September 9, 2007.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72e71–e77.
Many academic medical centers (AMCs) have developed nonhousestaff services to provide clinical care once provided by physicians‐in‐training. These services, often staffed by hospitalists and/or midlevel providers, have experienced tremendous growth in the past few years, yet very little exists in the literature about their development, structure, efficacy, or impact on hospitals, patients, and hospital medicine programs. The primary forces driving this growth include Accreditation Council for Graduate Medical Education (ACGME) resident duty hour restrictions,1 growth of the hospitalist movement,2 and the emphasis on simultaneously improving financial performance and quality of care in AMCs.3
Resident Duty Hour Restrictions
In 2003, the ACGME mandated restrictions on resident work hours, limiting trainees to 80 hours per week.1 Many training programs struggled with how to provide important clinical services while complying with the new restrictionscreating numerous models that bridged care between different shifts of residents.45 Implementation of day floats (a dedicated resident who rounds with the postcall team), night floats (a dedicated overnight resident who admits and cross‐covers patients), or some variation of both was common.6 No guidelines accompanied the ACGME mandate, leaving institutions to independently structure their programs without a known best practice.
Subsequent literature carefully addressed how the duty hour restrictions affect residents' lives and education but failed to discuss models for providing care.711 Training programs began to institute necessary changes but in doing so, created greater patient discontinuity and increased handoffs between residents, elevating the potential for adverse patient outcomes.12 Recent large‐scale studies indicate that inpatient care is the same or improved since adoption of the duty hour restrictions,1316 but controversy continues, with several editorials debating the issue.1719
Because increasing the volume of patients on housestaff services was not a viable option,20 many AMCs created nonhousestaff services and hired midlevel providers (nurse practitioners and physician assistants) to offset resident workloads and comply with the new restrictions. However, this strategy represented a very expensive alternative.21 Moreover, the current 80‐hour work limits may be revised downward, particularly given the lower restrictions in other countries,22 and this will further drive the demand for nonhousestaff services. Hospitalists, with their documented impact on efficiency and return on investment,23 represent a solution to fill these needs and have quickly become the predominant approach at AMCs.
The Hospitalist Movement
Since the term hospitalist was first coined in 1996,24 the remarkable growth of the number of practicing hospitalists emphasizes how first community hospitals and now AMCs have embraced this approach.25 With more than 20,000 nationwide and projections that the field will grow to 30,000 by 2010,26 hospitalists are becoming the primary providers for in‐patients.2 This growth was further catalyzed when widely expressed concerns about safety and quality became public,2728 and hospitalists incorporated patient safety and quality improvement activities into their efforts.3 The confluence of these factors also prompted emergence of hospital medicine programs at AMCs, a growth that came with anticipated dangers.29 Reflecting the recognition that hospital medicine is becoming a separate specialty30 and is integral to the functioning of an AMC, institutions now operate dedicated divisions of hospital medicine.
AMCs and Hospital Performance
AMCs operate 3 related enterprises: a medical school that trains future physicians, a research arena that promotes basic and clinical investigation, and health care services that often encompass both hospitals and clinics. The financial viability of AMCs has always been a topic of debate, largely because of the different missions they pursue and the financial means by which they survive.3133 Over the past decade, cuts in Medicare reimbursement, challenges in balancing bed availability with occupancy rates, and a growing emphasis on cost reduction have created a more competitive health care environment, but without the predicted demise of AMCs.34 Because education and research generally fail to bolster the bottom line, AMCs have focused on optimizing clinical services to promote financial viability.
Hospitalists are uniquely positioned to help this bottom line, just as they do at community hospitals. Their involvement in patient care may produce reductions in length of stay, greater efficiency in discharge planning, and significant cost savings.3537 Hospitalists may also improve throughput in emergency departments and decrease wait times, leading to more efficient bed utilization.38 This leads to a potential for greater hospital revenue by increasing both the number of admissions, particularly surgical cases, and staffed inpatient beds, the latter a premium, as AMCs continue to expand their bed capacity almost annually. Finally, hospitalists may serve as change agents in improving the quality and safety of care delivered, an increasingly important metric given the desire for and expansion of publicly reported measures.
From a financial standpoint, Medicare support to AMCs for training residents now subsidizes fewer clinical care hours. Hospitalist‐driven nonhousestaff services will continue to fulfill a need created by this marked change in residency training. The tension of who pays for nonhousestaff servicesincreased federal support, financial backing from AMCs, or academic department fundsposes an ongoing struggle. In fact, this may be the most important issue currently debated among hospital administrators and department chairs. Regardless, AMCs continue to view hospitalists as a mechanism (or even solution) to maintaining their financial bottom line through improving care delivery systems, adhering to resident work hour restrictions, leading quality and safety improvement initiatives, and improving clinical patient outcomes.
MODELS FOR NONHOUSESTAFF MEDICAL SERVICES
For AMCs developing nonhousestaff services, the process begins by addressing a series of important questions (Table 1). How these questions are answered is often driven by local factors such as the vision of local leadership and the availability of important resources. Nonetheless, it is important for hospitals to share their experiences because best practices remain unclear. Table 2 provides a tabular snapshot of nonhousestaff medicine services at 5 AMCs to highlight similarities and differences. Data in the table were compiled by having a representative from each AMC report the different attributes, which reflects each program as of July 2007. Table 2 provides no data on the quality or efficiency of housestaff versus nonhousestaff services, though this type of investigation is underway and will be critical in future planning.3940
| Questions | Potential options |
|---|---|
| Who will provide care on nonhousestaff services? | Physicians seeking a 1‐year position |
| Physicians committed to a purely clinical career | |
| Physicians committed to an academic career in hospital medicine | |
| Will hospitalists share nonhousestaff service time, or will there be dedicated nonhousestaff hospitalists? | Hybrid positions |
| Dedicated nonhousestaff hospitalists | |
| Use of PGY‐4s1‐year positions (often individuals planning a fellowship) | |
| How should staffing be organized? | Hospitalist‐only services |
| Use of midlevel providers | |
| Will there be 24‐7 coverage, and if so, how will nights be staffed? | Dedicated nocturnists |
| Shared among daytime hospitalists | |
| Midlevel providers | |
| Moonlighters (fellows or residents) | |
| What type of schedule will provide blocks of clinical time to ensure continuity of care but also ensure adequate nonclinical time to prevent physician burnout and turnover? | 7 on/7 off sequences |
| 45 day sequences | |
| Longer shifts with fewer shifts per month | |
| Shorter shifts with more shifts per month | |
| Where will patients on a nonhousestaff service receive care? | Geographically designed serviced |
| ○ Different floor | |
| ○ Different hospital | |
| Mixed among housestaff service | |
| What patient population will be cared for on the nonhousestaff service? | Same as on housestaff service |
| Based on bed availability if nonhousestaff service is geographic (a unit) | |
| Based on triage guidelines (lower acuity, observation patients, specific diagnoses) | |
| What volume of patients will be cared for on the nonhousestaff service? | Fixed census cap based on staffing |
| Flexible census depending on activity of housestaff service (above their cap) | |
| Will compensation for providing nonhousestaff services differ from that on housestaff services? | Higher base salary |
| Incentives tied to nonhousestaff time | |
| Different incentive structures |
| Attributes | BWH | Emory | University of Michigan | Northwestern | UCSF |
|---|---|---|---|---|---|
| Description of staffing model | Mon.‐Sun.: 1 daytime Hospitalist | Mon.‐Sun.: 4 daytime hospitalists, 2 swing shift admitters | Weekdays: 7 daytime hospitalists, 1 swing shift hospitalist | Mon.‐Sun.: 8 daytime hospitalists, 1 triage hospitalist | Weekdays: 2 daytime hospitalists, 1 swing shift hospitalist |
| Nights: 1 MD | Nights: 1 MDs | Weekends: 7 daytime hospitalists | Nights: 2 MDs | Weekends: 2 daytime hospitalists | |
| Nights: 2 MDs | Nights: 1 MD | ||||
| Location of service | In same university hospital | In same university hospital | In same university hospital | In same university hospital | Physically separate hospital affiliate (UCSF Medical Center at Mount Zion) |
| Nonhousestaff FTEs/total hospitalist group | 3/15 | 10/14 | 20/30 | 25/34 | 6/36 |
| What hospitalists provide care on nonhous estaff services? | Core of 3 hospitalists (also do month on housestaff service) | Hospitalist group shares nonhousestaff services | Core of 14 FTEs dedicated to nonhousestaff services | Hospitalist group shares nonhousestaff services | Core of 6 Mount Zionbased hospitalists (also spend 23 months on housestaff service at university hospital) |
| Other 6 FTEs consist of 10 faculty with mixed roles | |||||
| Age of service | 2 years | 4 years | 3 years | 5 years | 3 years |
| How patients get assigned to non‐housestaff service? | 1. Only ED admissions with no transfers from ICU or other services | Assigned by rotation | 1. Alternating admissions with housestaff services during afternoon | 1. Alternating admissions with housestaff services during day | 1. Lower‐acuity admissions from ED |
| 2. Admit whenever bed open on service (geographic) | 2. Observation cases triaged directly to service | 2. Lower‐acuity patients and direct admissions | 2. Lower‐acuity admissions from clinics | ||
| 3. Once housestaff cap, all subsequent admits until midnight to nonhousestaff service | 3. Nonhousestaff service admits all patients once resident caps reached | 3. Transfers from housestaff service no longer requiring tertiary services (or with complex discharge planning) | |||
| Average daily census of nonhousestaff service | 12 | 56 | 70 (75 cap) | 8595 | 2026 |
| Number of shifts per month/shift duration | 15/1012 hours | 15/12 hours | 1517 (depending on number of nights covered)/812 hours (swing = 8 hours, day = 1012 hours, night = 12 hours) | 20/1012 hours | 1617/1012 hours |
| Shift sequences | 710 days consecutive | Variable | 67 days consecutive followed by 1 night for those who cover nights | 7 days consecutive | 4‐ to 6‐day variable sequences |
| Total clinical days worked/year | 168 | 182.5 | 185202 (depending on number of nights covered) | 212 | 196 |
| Weekend clinical time | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends |
| Night coverage/by whom? | Yes/exclusively moonlighters | Yes/shared (50% covered by 1 dedicated nocturnist) | Yes/66% of nights staffed by dedicated nocturnists with remainder shared | Yes/exclusively by six 1‐year nocturnists | Yes/exclusively by moonlighters |
| Presence of midlevel providers | Yes 6 FTE PAs Mon.‐Sun. | No | Yes 8 FTE PAs weekdays | No | No |
| Presence of dedicated case manager | Yes | Yes | Yes | No | Yes |
| Presence of medical students for patient care | No | No | Yes, 4th‐year subinterns or students on elective rotation | No | No |
| Compensation model | Salary + weekend bonus beyond 10 | Salary + incentive | Base + shift‐based incentive + quality incentive | Salary + incentive | Salary |
| Pay differential compared to housestaff service compensation | 10% Higher because of weekend bonus | None | About 20% higher base compensation; loan forgiveness program tied to nonhousestaff time | None | About 20% higher compensation |
| Hospital financial support | Yes | Yes | Yes | Yes | Yes |
Table 2 does illustrate several important considerations in structuring nonhousestaff services. For example, if a nonhousestaff service operates at a different physical location, careful triage of patients is necessary. Resources, including the availability of subspecialty and surgical consultants, may differ, and thus patient complexity and acuity may dictate whether a patient gets admitted to the nonhousestaff service. These triage factors were a major challenge in the design of UCSF's nonhousestaff service. The other nonhousestaff services handle overflow admissions after the housestaff service reaches a census or admission cap; transfers between services rarely occur, and resources are similar.
Other observations include that hospitalists work a similar number of hours each year and cover 50% of weekends but with differing shift lengths and sequences. Each service also provides night coverage but only Emory, the University of Michigan, and Northwestern utilize dedicated nocturnists. The University of Michigan and Brigham & Women's Hospital are the only sites that employ midlevel providers who work closely with hospitalists. In terms of group structure, Northwestern's hospitalists are the most integrated, with each hospitalist sharing equal responsibility for nonhousestaff coverage. In contrast, the other programs use selected hospitalists or a dedicated core of hospitalists to provide nonhousestaff services. Compensation models also vary, with certain groups salaried and others having incentive systems, although all receive hospital‐based funding support. Hospital‐based funding support ranges from 40% to 100% of total program costs across sites, creating similar variance in a given program's deficit risk. Finally, most programs do compensate nonhousestaff services at higher rates.
All the decisions captured in Table 2 have implications for costs, recruitment, and service structure. Furthermore, the striking variations demonstrate how different academic hospitalist positions can occur both within a hospital medicine group and across institutions. Of note, Table 2 only characterizes nonhousestaff medicine services, not the growing number of comanagement (eg, orthopedics, neurosurgery, or hematology/oncology) and other clinical services (eg, observation unit or preoperative medicine clinic) also staffed by hospitalists at AMCs.
CHALLENGES
Hospital medicine programs and AMCs face several challenges in building non‐housestaff services, but these will likely become less daunting as programs learn from their own experiences, from those of colleagues at other institutions, and from future investigations of these care models. We highlight a few issues below that warrant important consideration.
The Equities of the System
Prior to developing nonhousestaff services, our academic hospitalist programs scheduled teaching service time in month or half‐month blocks, balancing holidays and weekends. Equity in scheduling became a function of required clinical time, sources of non‐clinical funding (eg, grants, educational or administrative roles), and expectations for scholarship, attributes typical of most subspecialty academic divisions. Given the differing clinical missions that have stimulated academic hospital medicine programs to form, concerns of scheduling equity have grown, posing challenges not experienced in other divisions.
Institutions that choose to divide housestaff and nonhousestaff duties among distinct groups of hospitalists create the potential for a 2‐tiered system, one in which those with housestaff roles are more valued and respected by the institution. Hospitalists working on nonhousestaff services admit patients, write orders, and field direct patient calls, a role rarely undertaken by subspecialty attendings or hospitalists on housestaff services. Our collective experiences provide evidence of the danger of this second‐class‐citizen status, one that requires attention to ensure job satisfaction, retention, and necessary career development.
Institutions have accentuated the second‐class‐citizen concern by staffing nonhousestaff roles with 1‐year hospitalistsPGY‐4s. Most of these hires in our institutions are individuals just out of residency and intent on pursuing a fellowship. We speculate that they enjoy the comforts of the AMC where they often trained and accept purely nonhousestaff positions because of what they view as an appealing work schedule and salary. Although this approach addresses the growing need for hospitalists on nonhousestaff services in the short term, these positions must remain attractive enough (both financially and professionally) to encourage residency graduates to pursue an academic hospitalist career instead of a 1‐year position as a transition to fellowship. Otherwise, the approach conveys a message that relatively inexperienced physicians are good enough to be hospitalists.
Developing a cadre of clinically focused hospitalists who provide outstanding patient care and also garner respect as successful academicians is a difficult task. Although 1 group in our sample (Northwestern) shares nonhousestaff responsibilities equally, others may find this impractical, particularly where faculty members were hired before nonhousestaff services were established. Redefining such clinical positions several years into a career may be challenging, as it forces faculty members into roles they didn't sign up for or grandfathers them out of such roles, adding to the risk of a 2‐tiered system. Alternatively, groups may focus on building academic activities into nonhousestaff services, including medical student teaching, quality improvement, or clinical research activities. In this article, we deliberately classified these services as nonhousestaff rather than non‐teaching because the latter fails to acknowledge that these hospitalists often serve as teachers (eg, housestaff conferences, supervision of midlevel providers, and/or rotating medical students)an important if not symbolic distinction. It is imperative that planning for nonhousestaff services balance the larger academic mission of hospital medicine groups with creating equitable, valued, and sustainable job descriptions.
Defining the Patient Mix
Developing an optimal patient mix on nonhousestaff services also carries important implications. For services that work in parallel with the housestaff service and simply take extra patients above the resident cap, this concern may be less significant. However, other nonhousestaff services have been structured to care for lower‐acuity patients (eg, cellulitis, asthma, pneumonia) or select patient populations (eg, sickle cell or inflammatory bowel disease). This distribution system potentially changes the educational experience on the housestaff servicedecreasing the bread‐and‐butter admissionsbut also may affect the job satisfaction of hospitalists and midlevel providers on nonhousestaff services. Building triage criteria, working with emergency department leadership, and avoiding patients being turfed between different services is critical. We strongly recommend a regular process to review admissions to each service and determine when the triage process requires further calibration.
Recruitment and Retention
Traditionally, graduates of residency or fellowship training programs chose academic positions because of an interest in teaching, a desire for scholarship, or a commitment to research. Those interested in primarily clinical roles typically pursued positions in nonacademic settings. The development of nonhousestaff services challenges this paradigm because the objective for academic hospitalist leadership now becomes recruiting pure clinicians as well as academicians. These might be the same individual, a hospitalist who provides both housestaff and nonhousestaff services, or 2 different individuals if the nonhousestaff service is covered by dedicated hospitalists. In addition, with the current promotion structure in academia, a purely clinical position may be less attractive, as it provides fewer opportunities for advancement.
Therefore, recruitment and retention of academic hospitalists will require job descriptions that provide dedicated teaching opportunities, time for participation in quality and safety improvement projects, or pursuit of a scholarly interest in non‐clinical timethe diastole of an academic hospitalist.41 Hospital medicine leadership will also need to better distinguish off‐time from non‐clinical time, as many young hospitalists struggle to balance professional and personal commitmentsa recipe for burnout.42 Regardless of how clinical responsibilities differ between 2 hospitalists, providing them with similar academic resources is what will distinguish their positions from that in the community. Furthermore, many groups have chosen to pay faculty a premium for their nonhousestaff roles or to use specific recruitment incentives such as educational loan forgiveness programs.
With the expected growth of nonhousestaff services and surgical comanagement, hospital medicine programs will also need to determine if new hires will focus on a specific service (eg, orthopedic hospitalist) or whether job descriptions will include a mix of activities (eg, 3 months' teaching service, 3 months' nonhousestaff medical service, and 3 months' surgical comanagement service). A second and equally important question is where does the hospitalist live? If cardiology wants hospitalists to care for their patients, should they be hired and mentored by cardiologists or by hospitalists in a division of general or hospital medicine? In many cases, a graduating resident with plans to pursue a fellowship (eg, cardiology or hematology/oncology) may be a perfect candidate for a 1‐year position on his or her future specialty service. However, in the long term, maintaining all the academic hospitalists under the same umbrella will provide greater mentorship, professional development, opportunities for collaboration, clinical diversity, and sense of belonging to a group, rather than being a token hospitalist for another division.
Compensation and Financial Relationships with AMCs
Salaries for hospitalists working on nonhousestaff services are typically higher at AMCs, which are competing with community standards given the similar level of clinical hours worked. However, although pay for nonhousestaff activities should reflect the nature of the work, compensation models based on clinical productivity alone may prove inadequate. It appears hospitalists working in academic facilities spend significant time on indirect patient care because of these hospitals' inefficiencies, usually not found in community settings.43 Devising compensation for an academic hospitalist requires careful attention and must balance a number of factors because these hospitalists will not generate their entire salary from clinical services. Financial support must come from either the division or medical center, an annual negotiation at AMCs.
Several methods exist to structure hospitalist compensation. A hospitalist's salary may be fixed, may have a base salary with incentives, or may be derived based on clinical productivity. For example, if a hospital medicine program provides both housestaff and nonhousestaff services and employs a fixed‐salary approach, it may choose a menu‐style method to determine compensation (eg, 6 months on nonhousestaff service at x dollars/month + 3 months on housestaff service at x dollars/month = annual salary). If a hospitalist takes on a funded nonclinical role or secures extramural funding, the salary menu gets adjusted accordingly as the clinical time is bought out. Critics of the fixed‐salary approach argue that paying each hospitalist the same salary regardless of the specific job description yields an inequitable system in which some are rewarded with less clinical time.
Compensation should probably have a guaranteed base salary with incentives, which could be determined by a formula that weighs clinical productivity, quality improvement efforts, scholarly activity, and teaching excellence. This model provides financial incentives to develop both clinically and academically but introduces complexity in determining a fair incentive structure. Finally, compensation can be structured without salary guarantee and putting compensation fully at risk based on clinical productivity, although this is an unlikely strategy for any hospital medicine group. This approach does disproportionately reward high volume providers, potentially at the risk of quality and safety, but also creates significant incentives to improve efficiency.
With respect to AMC relationships, hospital medicine programs must ensure the positive return on investment that drives financial support at their institutions. This fundamental economic dynamic makes AMCs dependent on their hospital medicine groups and vice versa. We caution programs from solely relying on measures such as reduced hospital costs or length of stay as a basis of funding unless there is a reward for maintaining performance once it inevitably plateaus. Moreover, explicitly tying utilization efficiency (ie, length of stay) to salary violates Stark rules44 and carries potential malpractice implications should patient care errors be attributable to premature hospital discharge. Over time hospitalists will need to maintain clinical benchmarks but also provide additional and valued services to their institutions, including quality and safety improvement activities and compliance with residency work hour restrictions.
Defining the Academic Hospitalist
The question is simple and perhaps philosophical: Are hospitalists who work at an AMC academic hospitalists? And what job description truly defines an academic hospitalist? Currently, there are no standards for the clinical activity of an academic hospitalist position (eg, number of weeks, weekends, and hours) or for assessment of nonclinical productivity. Hospital medicine programs face the challenge of defining positions that fulfill the growing clinical mission at AMCs but have little experience or guidance in ensuring they will lead to advancing the academic mission. Specifically, how do hospitalists who provide mostly clinical care, particularly on nonhousestaff services, achieve promotion? Hospital medicine program leadership must create enough opportunity and time for the development of skills in research, education, and quality or systems improvement if academic hospitalists are to succeed.
The Association of Chiefs of General Internal Medicine (ACGIM), the Society of General Internal Medicine (SGIM), and the Society of Hospital Medicine (SHM) are currently collaborating to develop consensus guidelines in this area. Ultimately, through the efforts of these important governing bodies, the specialty of hospital medicine will be able to demonstrate the unique skills and services they provide and move toward advocating for academic promotion criteria that recognize their value and accomplishments.
FUTURE DIRECTIONS
Many lament that the milieu for academic hospitalists raises more challenges than solutions, but we believe the current era is one of excitement and opportunity. In the coming years, we will experience continued growth of nonhousestaff services, including greater comanagement with our surgical and medical specialty colleagues. These opportunities will create new relationships and increase our visibility in AMCs. However, we must remain committed to studying nonhousestaff services and determine if and how they differ from their housestaff and community counterparts, as this will be an important step toward addressing current challenges.
As hospitalists take on increasingly diverse roles,45 we must also lead initiatives to better train, recruit, and retain those interested in our specialty. Promoting our field and recruiting future faculty should occur through local hospitalist career nights, events at national meetings (targeting students, housestaff, and fellows), and other mechanisms utilized by our subspecialty colleagues. For housestaff interested in fellowship training, the growing number of hospitalist fellowships can provide skills in teaching and quality improvement.46 For trainees committed to research, we should work with existing general medicine research fellowships and partner to provide hospitalist mentorship.
Hospitalists are in a unique position to influence the delivery of clinical services, shape the future of residency training, guide quality and safety improvement initiatives, and take on leadership roles through our departments, universities, and medical centers. With the growing number of clinical services being added to our portfolio, we will need careful planning and evaluation of our efforts to build successful partnerships and develop faculty roles that balance clinical and academic pursuits to sustain long‐term and satisfying hospitalist careers.
Many academic medical centers (AMCs) have developed nonhousestaff services to provide clinical care once provided by physicians‐in‐training. These services, often staffed by hospitalists and/or midlevel providers, have experienced tremendous growth in the past few years, yet very little exists in the literature about their development, structure, efficacy, or impact on hospitals, patients, and hospital medicine programs. The primary forces driving this growth include Accreditation Council for Graduate Medical Education (ACGME) resident duty hour restrictions,1 growth of the hospitalist movement,2 and the emphasis on simultaneously improving financial performance and quality of care in AMCs.3
Resident Duty Hour Restrictions
In 2003, the ACGME mandated restrictions on resident work hours, limiting trainees to 80 hours per week.1 Many training programs struggled with how to provide important clinical services while complying with the new restrictionscreating numerous models that bridged care between different shifts of residents.45 Implementation of day floats (a dedicated resident who rounds with the postcall team), night floats (a dedicated overnight resident who admits and cross‐covers patients), or some variation of both was common.6 No guidelines accompanied the ACGME mandate, leaving institutions to independently structure their programs without a known best practice.
Subsequent literature carefully addressed how the duty hour restrictions affect residents' lives and education but failed to discuss models for providing care.711 Training programs began to institute necessary changes but in doing so, created greater patient discontinuity and increased handoffs between residents, elevating the potential for adverse patient outcomes.12 Recent large‐scale studies indicate that inpatient care is the same or improved since adoption of the duty hour restrictions,1316 but controversy continues, with several editorials debating the issue.1719
Because increasing the volume of patients on housestaff services was not a viable option,20 many AMCs created nonhousestaff services and hired midlevel providers (nurse practitioners and physician assistants) to offset resident workloads and comply with the new restrictions. However, this strategy represented a very expensive alternative.21 Moreover, the current 80‐hour work limits may be revised downward, particularly given the lower restrictions in other countries,22 and this will further drive the demand for nonhousestaff services. Hospitalists, with their documented impact on efficiency and return on investment,23 represent a solution to fill these needs and have quickly become the predominant approach at AMCs.
The Hospitalist Movement
Since the term hospitalist was first coined in 1996,24 the remarkable growth of the number of practicing hospitalists emphasizes how first community hospitals and now AMCs have embraced this approach.25 With more than 20,000 nationwide and projections that the field will grow to 30,000 by 2010,26 hospitalists are becoming the primary providers for in‐patients.2 This growth was further catalyzed when widely expressed concerns about safety and quality became public,2728 and hospitalists incorporated patient safety and quality improvement activities into their efforts.3 The confluence of these factors also prompted emergence of hospital medicine programs at AMCs, a growth that came with anticipated dangers.29 Reflecting the recognition that hospital medicine is becoming a separate specialty30 and is integral to the functioning of an AMC, institutions now operate dedicated divisions of hospital medicine.
AMCs and Hospital Performance
AMCs operate 3 related enterprises: a medical school that trains future physicians, a research arena that promotes basic and clinical investigation, and health care services that often encompass both hospitals and clinics. The financial viability of AMCs has always been a topic of debate, largely because of the different missions they pursue and the financial means by which they survive.3133 Over the past decade, cuts in Medicare reimbursement, challenges in balancing bed availability with occupancy rates, and a growing emphasis on cost reduction have created a more competitive health care environment, but without the predicted demise of AMCs.34 Because education and research generally fail to bolster the bottom line, AMCs have focused on optimizing clinical services to promote financial viability.
Hospitalists are uniquely positioned to help this bottom line, just as they do at community hospitals. Their involvement in patient care may produce reductions in length of stay, greater efficiency in discharge planning, and significant cost savings.3537 Hospitalists may also improve throughput in emergency departments and decrease wait times, leading to more efficient bed utilization.38 This leads to a potential for greater hospital revenue by increasing both the number of admissions, particularly surgical cases, and staffed inpatient beds, the latter a premium, as AMCs continue to expand their bed capacity almost annually. Finally, hospitalists may serve as change agents in improving the quality and safety of care delivered, an increasingly important metric given the desire for and expansion of publicly reported measures.
From a financial standpoint, Medicare support to AMCs for training residents now subsidizes fewer clinical care hours. Hospitalist‐driven nonhousestaff services will continue to fulfill a need created by this marked change in residency training. The tension of who pays for nonhousestaff servicesincreased federal support, financial backing from AMCs, or academic department fundsposes an ongoing struggle. In fact, this may be the most important issue currently debated among hospital administrators and department chairs. Regardless, AMCs continue to view hospitalists as a mechanism (or even solution) to maintaining their financial bottom line through improving care delivery systems, adhering to resident work hour restrictions, leading quality and safety improvement initiatives, and improving clinical patient outcomes.
MODELS FOR NONHOUSESTAFF MEDICAL SERVICES
For AMCs developing nonhousestaff services, the process begins by addressing a series of important questions (Table 1). How these questions are answered is often driven by local factors such as the vision of local leadership and the availability of important resources. Nonetheless, it is important for hospitals to share their experiences because best practices remain unclear. Table 2 provides a tabular snapshot of nonhousestaff medicine services at 5 AMCs to highlight similarities and differences. Data in the table were compiled by having a representative from each AMC report the different attributes, which reflects each program as of July 2007. Table 2 provides no data on the quality or efficiency of housestaff versus nonhousestaff services, though this type of investigation is underway and will be critical in future planning.3940
| Questions | Potential options |
|---|---|
| Who will provide care on nonhousestaff services? | Physicians seeking a 1‐year position |
| Physicians committed to a purely clinical career | |
| Physicians committed to an academic career in hospital medicine | |
| Will hospitalists share nonhousestaff service time, or will there be dedicated nonhousestaff hospitalists? | Hybrid positions |
| Dedicated nonhousestaff hospitalists | |
| Use of PGY‐4s1‐year positions (often individuals planning a fellowship) | |
| How should staffing be organized? | Hospitalist‐only services |
| Use of midlevel providers | |
| Will there be 24‐7 coverage, and if so, how will nights be staffed? | Dedicated nocturnists |
| Shared among daytime hospitalists | |
| Midlevel providers | |
| Moonlighters (fellows or residents) | |
| What type of schedule will provide blocks of clinical time to ensure continuity of care but also ensure adequate nonclinical time to prevent physician burnout and turnover? | 7 on/7 off sequences |
| 45 day sequences | |
| Longer shifts with fewer shifts per month | |
| Shorter shifts with more shifts per month | |
| Where will patients on a nonhousestaff service receive care? | Geographically designed serviced |
| ○ Different floor | |
| ○ Different hospital | |
| Mixed among housestaff service | |
| What patient population will be cared for on the nonhousestaff service? | Same as on housestaff service |
| Based on bed availability if nonhousestaff service is geographic (a unit) | |
| Based on triage guidelines (lower acuity, observation patients, specific diagnoses) | |
| What volume of patients will be cared for on the nonhousestaff service? | Fixed census cap based on staffing |
| Flexible census depending on activity of housestaff service (above their cap) | |
| Will compensation for providing nonhousestaff services differ from that on housestaff services? | Higher base salary |
| Incentives tied to nonhousestaff time | |
| Different incentive structures |
| Attributes | BWH | Emory | University of Michigan | Northwestern | UCSF |
|---|---|---|---|---|---|
| Description of staffing model | Mon.‐Sun.: 1 daytime Hospitalist | Mon.‐Sun.: 4 daytime hospitalists, 2 swing shift admitters | Weekdays: 7 daytime hospitalists, 1 swing shift hospitalist | Mon.‐Sun.: 8 daytime hospitalists, 1 triage hospitalist | Weekdays: 2 daytime hospitalists, 1 swing shift hospitalist |
| Nights: 1 MD | Nights: 1 MDs | Weekends: 7 daytime hospitalists | Nights: 2 MDs | Weekends: 2 daytime hospitalists | |
| Nights: 2 MDs | Nights: 1 MD | ||||
| Location of service | In same university hospital | In same university hospital | In same university hospital | In same university hospital | Physically separate hospital affiliate (UCSF Medical Center at Mount Zion) |
| Nonhousestaff FTEs/total hospitalist group | 3/15 | 10/14 | 20/30 | 25/34 | 6/36 |
| What hospitalists provide care on nonhous estaff services? | Core of 3 hospitalists (also do month on housestaff service) | Hospitalist group shares nonhousestaff services | Core of 14 FTEs dedicated to nonhousestaff services | Hospitalist group shares nonhousestaff services | Core of 6 Mount Zionbased hospitalists (also spend 23 months on housestaff service at university hospital) |
| Other 6 FTEs consist of 10 faculty with mixed roles | |||||
| Age of service | 2 years | 4 years | 3 years | 5 years | 3 years |
| How patients get assigned to non‐housestaff service? | 1. Only ED admissions with no transfers from ICU or other services | Assigned by rotation | 1. Alternating admissions with housestaff services during afternoon | 1. Alternating admissions with housestaff services during day | 1. Lower‐acuity admissions from ED |
| 2. Admit whenever bed open on service (geographic) | 2. Observation cases triaged directly to service | 2. Lower‐acuity patients and direct admissions | 2. Lower‐acuity admissions from clinics | ||
| 3. Once housestaff cap, all subsequent admits until midnight to nonhousestaff service | 3. Nonhousestaff service admits all patients once resident caps reached | 3. Transfers from housestaff service no longer requiring tertiary services (or with complex discharge planning) | |||
| Average daily census of nonhousestaff service | 12 | 56 | 70 (75 cap) | 8595 | 2026 |
| Number of shifts per month/shift duration | 15/1012 hours | 15/12 hours | 1517 (depending on number of nights covered)/812 hours (swing = 8 hours, day = 1012 hours, night = 12 hours) | 20/1012 hours | 1617/1012 hours |
| Shift sequences | 710 days consecutive | Variable | 67 days consecutive followed by 1 night for those who cover nights | 7 days consecutive | 4‐ to 6‐day variable sequences |
| Total clinical days worked/year | 168 | 182.5 | 185202 (depending on number of nights covered) | 212 | 196 |
| Weekend clinical time | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends | 50% of weekends |
| Night coverage/by whom? | Yes/exclusively moonlighters | Yes/shared (50% covered by 1 dedicated nocturnist) | Yes/66% of nights staffed by dedicated nocturnists with remainder shared | Yes/exclusively by six 1‐year nocturnists | Yes/exclusively by moonlighters |
| Presence of midlevel providers | Yes 6 FTE PAs Mon.‐Sun. | No | Yes 8 FTE PAs weekdays | No | No |
| Presence of dedicated case manager | Yes | Yes | Yes | No | Yes |
| Presence of medical students for patient care | No | No | Yes, 4th‐year subinterns or students on elective rotation | No | No |
| Compensation model | Salary + weekend bonus beyond 10 | Salary + incentive | Base + shift‐based incentive + quality incentive | Salary + incentive | Salary |
| Pay differential compared to housestaff service compensation | 10% Higher because of weekend bonus | None | About 20% higher base compensation; loan forgiveness program tied to nonhousestaff time | None | About 20% higher compensation |
| Hospital financial support | Yes | Yes | Yes | Yes | Yes |
Table 2 does illustrate several important considerations in structuring nonhousestaff services. For example, if a nonhousestaff service operates at a different physical location, careful triage of patients is necessary. Resources, including the availability of subspecialty and surgical consultants, may differ, and thus patient complexity and acuity may dictate whether a patient gets admitted to the nonhousestaff service. These triage factors were a major challenge in the design of UCSF's nonhousestaff service. The other nonhousestaff services handle overflow admissions after the housestaff service reaches a census or admission cap; transfers between services rarely occur, and resources are similar.
Other observations include that hospitalists work a similar number of hours each year and cover 50% of weekends but with differing shift lengths and sequences. Each service also provides night coverage but only Emory, the University of Michigan, and Northwestern utilize dedicated nocturnists. The University of Michigan and Brigham & Women's Hospital are the only sites that employ midlevel providers who work closely with hospitalists. In terms of group structure, Northwestern's hospitalists are the most integrated, with each hospitalist sharing equal responsibility for nonhousestaff coverage. In contrast, the other programs use selected hospitalists or a dedicated core of hospitalists to provide nonhousestaff services. Compensation models also vary, with certain groups salaried and others having incentive systems, although all receive hospital‐based funding support. Hospital‐based funding support ranges from 40% to 100% of total program costs across sites, creating similar variance in a given program's deficit risk. Finally, most programs do compensate nonhousestaff services at higher rates.
All the decisions captured in Table 2 have implications for costs, recruitment, and service structure. Furthermore, the striking variations demonstrate how different academic hospitalist positions can occur both within a hospital medicine group and across institutions. Of note, Table 2 only characterizes nonhousestaff medicine services, not the growing number of comanagement (eg, orthopedics, neurosurgery, or hematology/oncology) and other clinical services (eg, observation unit or preoperative medicine clinic) also staffed by hospitalists at AMCs.
CHALLENGES
Hospital medicine programs and AMCs face several challenges in building non‐housestaff services, but these will likely become less daunting as programs learn from their own experiences, from those of colleagues at other institutions, and from future investigations of these care models. We highlight a few issues below that warrant important consideration.
The Equities of the System
Prior to developing nonhousestaff services, our academic hospitalist programs scheduled teaching service time in month or half‐month blocks, balancing holidays and weekends. Equity in scheduling became a function of required clinical time, sources of non‐clinical funding (eg, grants, educational or administrative roles), and expectations for scholarship, attributes typical of most subspecialty academic divisions. Given the differing clinical missions that have stimulated academic hospital medicine programs to form, concerns of scheduling equity have grown, posing challenges not experienced in other divisions.
Institutions that choose to divide housestaff and nonhousestaff duties among distinct groups of hospitalists create the potential for a 2‐tiered system, one in which those with housestaff roles are more valued and respected by the institution. Hospitalists working on nonhousestaff services admit patients, write orders, and field direct patient calls, a role rarely undertaken by subspecialty attendings or hospitalists on housestaff services. Our collective experiences provide evidence of the danger of this second‐class‐citizen status, one that requires attention to ensure job satisfaction, retention, and necessary career development.
Institutions have accentuated the second‐class‐citizen concern by staffing nonhousestaff roles with 1‐year hospitalistsPGY‐4s. Most of these hires in our institutions are individuals just out of residency and intent on pursuing a fellowship. We speculate that they enjoy the comforts of the AMC where they often trained and accept purely nonhousestaff positions because of what they view as an appealing work schedule and salary. Although this approach addresses the growing need for hospitalists on nonhousestaff services in the short term, these positions must remain attractive enough (both financially and professionally) to encourage residency graduates to pursue an academic hospitalist career instead of a 1‐year position as a transition to fellowship. Otherwise, the approach conveys a message that relatively inexperienced physicians are good enough to be hospitalists.
Developing a cadre of clinically focused hospitalists who provide outstanding patient care and also garner respect as successful academicians is a difficult task. Although 1 group in our sample (Northwestern) shares nonhousestaff responsibilities equally, others may find this impractical, particularly where faculty members were hired before nonhousestaff services were established. Redefining such clinical positions several years into a career may be challenging, as it forces faculty members into roles they didn't sign up for or grandfathers them out of such roles, adding to the risk of a 2‐tiered system. Alternatively, groups may focus on building academic activities into nonhousestaff services, including medical student teaching, quality improvement, or clinical research activities. In this article, we deliberately classified these services as nonhousestaff rather than non‐teaching because the latter fails to acknowledge that these hospitalists often serve as teachers (eg, housestaff conferences, supervision of midlevel providers, and/or rotating medical students)an important if not symbolic distinction. It is imperative that planning for nonhousestaff services balance the larger academic mission of hospital medicine groups with creating equitable, valued, and sustainable job descriptions.
Defining the Patient Mix
Developing an optimal patient mix on nonhousestaff services also carries important implications. For services that work in parallel with the housestaff service and simply take extra patients above the resident cap, this concern may be less significant. However, other nonhousestaff services have been structured to care for lower‐acuity patients (eg, cellulitis, asthma, pneumonia) or select patient populations (eg, sickle cell or inflammatory bowel disease). This distribution system potentially changes the educational experience on the housestaff servicedecreasing the bread‐and‐butter admissionsbut also may affect the job satisfaction of hospitalists and midlevel providers on nonhousestaff services. Building triage criteria, working with emergency department leadership, and avoiding patients being turfed between different services is critical. We strongly recommend a regular process to review admissions to each service and determine when the triage process requires further calibration.
Recruitment and Retention
Traditionally, graduates of residency or fellowship training programs chose academic positions because of an interest in teaching, a desire for scholarship, or a commitment to research. Those interested in primarily clinical roles typically pursued positions in nonacademic settings. The development of nonhousestaff services challenges this paradigm because the objective for academic hospitalist leadership now becomes recruiting pure clinicians as well as academicians. These might be the same individual, a hospitalist who provides both housestaff and nonhousestaff services, or 2 different individuals if the nonhousestaff service is covered by dedicated hospitalists. In addition, with the current promotion structure in academia, a purely clinical position may be less attractive, as it provides fewer opportunities for advancement.
Therefore, recruitment and retention of academic hospitalists will require job descriptions that provide dedicated teaching opportunities, time for participation in quality and safety improvement projects, or pursuit of a scholarly interest in non‐clinical timethe diastole of an academic hospitalist.41 Hospital medicine leadership will also need to better distinguish off‐time from non‐clinical time, as many young hospitalists struggle to balance professional and personal commitmentsa recipe for burnout.42 Regardless of how clinical responsibilities differ between 2 hospitalists, providing them with similar academic resources is what will distinguish their positions from that in the community. Furthermore, many groups have chosen to pay faculty a premium for their nonhousestaff roles or to use specific recruitment incentives such as educational loan forgiveness programs.
With the expected growth of nonhousestaff services and surgical comanagement, hospital medicine programs will also need to determine if new hires will focus on a specific service (eg, orthopedic hospitalist) or whether job descriptions will include a mix of activities (eg, 3 months' teaching service, 3 months' nonhousestaff medical service, and 3 months' surgical comanagement service). A second and equally important question is where does the hospitalist live? If cardiology wants hospitalists to care for their patients, should they be hired and mentored by cardiologists or by hospitalists in a division of general or hospital medicine? In many cases, a graduating resident with plans to pursue a fellowship (eg, cardiology or hematology/oncology) may be a perfect candidate for a 1‐year position on his or her future specialty service. However, in the long term, maintaining all the academic hospitalists under the same umbrella will provide greater mentorship, professional development, opportunities for collaboration, clinical diversity, and sense of belonging to a group, rather than being a token hospitalist for another division.
Compensation and Financial Relationships with AMCs
Salaries for hospitalists working on nonhousestaff services are typically higher at AMCs, which are competing with community standards given the similar level of clinical hours worked. However, although pay for nonhousestaff activities should reflect the nature of the work, compensation models based on clinical productivity alone may prove inadequate. It appears hospitalists working in academic facilities spend significant time on indirect patient care because of these hospitals' inefficiencies, usually not found in community settings.43 Devising compensation for an academic hospitalist requires careful attention and must balance a number of factors because these hospitalists will not generate their entire salary from clinical services. Financial support must come from either the division or medical center, an annual negotiation at AMCs.
Several methods exist to structure hospitalist compensation. A hospitalist's salary may be fixed, may have a base salary with incentives, or may be derived based on clinical productivity. For example, if a hospital medicine program provides both housestaff and nonhousestaff services and employs a fixed‐salary approach, it may choose a menu‐style method to determine compensation (eg, 6 months on nonhousestaff service at x dollars/month + 3 months on housestaff service at x dollars/month = annual salary). If a hospitalist takes on a funded nonclinical role or secures extramural funding, the salary menu gets adjusted accordingly as the clinical time is bought out. Critics of the fixed‐salary approach argue that paying each hospitalist the same salary regardless of the specific job description yields an inequitable system in which some are rewarded with less clinical time.
Compensation should probably have a guaranteed base salary with incentives, which could be determined by a formula that weighs clinical productivity, quality improvement efforts, scholarly activity, and teaching excellence. This model provides financial incentives to develop both clinically and academically but introduces complexity in determining a fair incentive structure. Finally, compensation can be structured without salary guarantee and putting compensation fully at risk based on clinical productivity, although this is an unlikely strategy for any hospital medicine group. This approach does disproportionately reward high volume providers, potentially at the risk of quality and safety, but also creates significant incentives to improve efficiency.
With respect to AMC relationships, hospital medicine programs must ensure the positive return on investment that drives financial support at their institutions. This fundamental economic dynamic makes AMCs dependent on their hospital medicine groups and vice versa. We caution programs from solely relying on measures such as reduced hospital costs or length of stay as a basis of funding unless there is a reward for maintaining performance once it inevitably plateaus. Moreover, explicitly tying utilization efficiency (ie, length of stay) to salary violates Stark rules44 and carries potential malpractice implications should patient care errors be attributable to premature hospital discharge. Over time hospitalists will need to maintain clinical benchmarks but also provide additional and valued services to their institutions, including quality and safety improvement activities and compliance with residency work hour restrictions.
Defining the Academic Hospitalist
The question is simple and perhaps philosophical: Are hospitalists who work at an AMC academic hospitalists? And what job description truly defines an academic hospitalist? Currently, there are no standards for the clinical activity of an academic hospitalist position (eg, number of weeks, weekends, and hours) or for assessment of nonclinical productivity. Hospital medicine programs face the challenge of defining positions that fulfill the growing clinical mission at AMCs but have little experience or guidance in ensuring they will lead to advancing the academic mission. Specifically, how do hospitalists who provide mostly clinical care, particularly on nonhousestaff services, achieve promotion? Hospital medicine program leadership must create enough opportunity and time for the development of skills in research, education, and quality or systems improvement if academic hospitalists are to succeed.
The Association of Chiefs of General Internal Medicine (ACGIM), the Society of General Internal Medicine (SGIM), and the Society of Hospital Medicine (SHM) are currently collaborating to develop consensus guidelines in this area. Ultimately, through the efforts of these important governing bodies, the specialty of hospital medicine will be able to demonstrate the unique skills and services they provide and move toward advocating for academic promotion criteria that recognize their value and accomplishments.
FUTURE DIRECTIONS
Many lament that the milieu for academic hospitalists raises more challenges than solutions, but we believe the current era is one of excitement and opportunity. In the coming years, we will experience continued growth of nonhousestaff services, including greater comanagement with our surgical and medical specialty colleagues. These opportunities will create new relationships and increase our visibility in AMCs. However, we must remain committed to studying nonhousestaff services and determine if and how they differ from their housestaff and community counterparts, as this will be an important step toward addressing current challenges.
As hospitalists take on increasingly diverse roles,45 we must also lead initiatives to better train, recruit, and retain those interested in our specialty. Promoting our field and recruiting future faculty should occur through local hospitalist career nights, events at national meetings (targeting students, housestaff, and fellows), and other mechanisms utilized by our subspecialty colleagues. For housestaff interested in fellowship training, the growing number of hospitalist fellowships can provide skills in teaching and quality improvement.46 For trainees committed to research, we should work with existing general medicine research fellowships and partner to provide hospitalist mentorship.
Hospitalists are in a unique position to influence the delivery of clinical services, shape the future of residency training, guide quality and safety improvement initiatives, and take on leadership roles through our departments, universities, and medical centers. With the growing number of clinical services being added to our portfolio, we will need careful planning and evaluation of our efforts to build successful partnerships and develop faculty roles that balance clinical and academic pursuits to sustain long‐term and satisfying hospitalist careers.
- Accreditation Council for Graduate Medical Education. Information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp Accessed May 28,2007.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- .Duty hours for resident physicians—tough choices for teaching hospitals.N Engl J Med.2002;347:1275–1278.
- ,.Resident work hours, hospitalist programs and academic medical centers.The Hospitalist.2005;Jan/Feb:30–33.
- .Adapting to duty‐hour limits—four years on.N Engl J Med.2007;356:2668–2670.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,,, et al.Effect of Residency Duty‐Hour Limits. Views of Key Clinical Faculty.Arch Intern Med.2007;167:1487–1492.
- ,,,.Perceived impact of duty hours regulation: a survey of residents and program directors.Am J Med.2007;120:644–648.
- ,,,.The impact of duty hours on resident self reports of errors.J Gen Intern Med.2007;22:205–209.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,.Changes in hospital mortality associated with residency work‐hour regulations.Ann Intern Med.2007;147:73–80.
- ,,,.Changes in outcomes for internal medicine inpatients after work‐hour regulations.Ann Intern Med.2007;147:97–103.
- ,,, et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:975–983.
- ,,, et al.Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:984–991.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356:2665–2667.
- ,.Hippocrates affirmed? Limiting residents' work hours does no harm to patients.Ann Intern Med.2007;356:143–144.
- ,.Evaluating resident duty hour reforms.JAMA.2007;298:1055–1057.
- ,,,,.Housestaff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167:47–52.
- ,,,.Predicting future staffing needs at teaching hospitals: use of an analytical program with multiple variables.Arch Surg.2007;142:329–334.
- . A primer on: resident work hours. American Medical Student Association. 6th ed. 2005. Available at: http://www.amsa.org/rwh/RWHprimer_6thEdition.pdf. Accessed May 28,2007.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- Society of Hospital Medicine. Media Center link: Growth of hospital medicine nationwide. Available at www.hospitalmedicine.org. Accessed May 28,2007.
- Kohn L,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington DC:Committee on Quality of Health Care in America, Institute of Medicine, National Academy Press;2000.
- Committee on Quality of Health Care in America, Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- .What will board certification be‐and mean‐for hospitalists?J Hosp Med.2007;2:102–104.
- .Academic medical centers under siege.N Engl J Med.1994;331:1370–1371.
- ,.Academic medicine meets managed care: a high impact collision.Acad Med.1996;71:839–845.
- .Preventing the academic medical center from becoming an oxymoron.Acad Med.1996;71:117–120.
- ,,.Why have academic medical center survived?JAMA.2005:293;1495–1500.
- ,,,.Comparison of hospitalist and nonhospitalists in inpatient length of stay adjusting for patient and physician characteristics.J Gen Intern Med.2004;19:1127–1132.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22;662–667.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,.Hospitalists and an innovative emergency department admissions process.J Gen Intern Med.2004;19:266–268.
- ,,,,.Comparison of resource utilization and clinical outcomes between teaching and nonteaching medical services.J Hosp Med.2007;2:150–157.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22:662–667.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1:368–377.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction. 2006;1–45. Available at: http://www.hospitalmedicine.org. Accessed August 11,2007.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1:88–93.
- A Guide to Complying with Stark Self‐Referral Rules.Washington, DC:Atlantic Information Services, Inc.; 2004. Available at: http://www.aispub.com/. Accessed September 9, 2007.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72e71–e77.
- Accreditation Council for Graduate Medical Education. Information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp Accessed May 28,2007.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- .Duty hours for resident physicians—tough choices for teaching hospitals.N Engl J Med.2002;347:1275–1278.
- ,.Resident work hours, hospitalist programs and academic medical centers.The Hospitalist.2005;Jan/Feb:30–33.
- .Adapting to duty‐hour limits—four years on.N Engl J Med.2007;356:2668–2670.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,,, et al.Effect of Residency Duty‐Hour Limits. Views of Key Clinical Faculty.Arch Intern Med.2007;167:1487–1492.
- ,,,.Perceived impact of duty hours regulation: a survey of residents and program directors.Am J Med.2007;120:644–648.
- ,,,.The impact of duty hours on resident self reports of errors.J Gen Intern Med.2007;22:205–209.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,.Changes in hospital mortality associated with residency work‐hour regulations.Ann Intern Med.2007;147:73–80.
- ,,,.Changes in outcomes for internal medicine inpatients after work‐hour regulations.Ann Intern Med.2007;147:97–103.
- ,,, et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:975–983.
- ,,, et al.Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform.JAMA.2007;298:984–991.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356:2665–2667.
- ,.Hippocrates affirmed? Limiting residents' work hours does no harm to patients.Ann Intern Med.2007;356:143–144.
- ,.Evaluating resident duty hour reforms.JAMA.2007;298:1055–1057.
- ,,,,.Housestaff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167:47–52.
- ,,,.Predicting future staffing needs at teaching hospitals: use of an analytical program with multiple variables.Arch Surg.2007;142:329–334.
- . A primer on: resident work hours. American Medical Student Association. 6th ed. 2005. Available at: http://www.amsa.org/rwh/RWHprimer_6thEdition.pdf. Accessed May 28,2007.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- Society of Hospital Medicine. Media Center link: Growth of hospital medicine nationwide. Available at www.hospitalmedicine.org. Accessed May 28,2007.
- Kohn L,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington DC:Committee on Quality of Health Care in America, Institute of Medicine, National Academy Press;2000.
- Committee on Quality of Health Care in America, Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- .What will board certification be‐and mean‐for hospitalists?J Hosp Med.2007;2:102–104.
- .Academic medical centers under siege.N Engl J Med.1994;331:1370–1371.
- ,.Academic medicine meets managed care: a high impact collision.Acad Med.1996;71:839–845.
- .Preventing the academic medical center from becoming an oxymoron.Acad Med.1996;71:117–120.
- ,,.Why have academic medical center survived?JAMA.2005:293;1495–1500.
- ,,,.Comparison of hospitalist and nonhospitalists in inpatient length of stay adjusting for patient and physician characteristics.J Gen Intern Med.2004;19:1127–1132.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22;662–667.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,.Hospitalists and an innovative emergency department admissions process.J Gen Intern Med.2004;19:266–268.
- ,,,,.Comparison of resource utilization and clinical outcomes between teaching and nonteaching medical services.J Hosp Med.2007;2:150–157.
- ,,.Comparison of hospital costs and length of stay for community internists, hospitalists, and academicians.J Gen Intern Med.2007;22:662–667.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1:368–377.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction. 2006;1–45. Available at: http://www.hospitalmedicine.org. Accessed August 11,2007.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1:88–93.
- A Guide to Complying with Stark Self‐Referral Rules.Washington, DC:Atlantic Information Services, Inc.; 2004. Available at: http://www.aispub.com/. Accessed September 9, 2007.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72e71–e77.
Tuberculosis: In and out of the airways
A 23‐year‐old Chinese woman presented with worsening exertional dyspnea. Her medical history was notable for pulmonary tuberculosis treated at the age of 16. Over the past 3 years, she reported progressive respiratory symptoms resulting in marked exercise intolerance. She denied any fevers, cough, or weight loss. On examination, she had right‐sided tracheal deviation but spoke comfortably. Her heart sounds were displaced and right‐sided breath sounds nearly absent. Chest x‐ray (Fig. 1) and subsequent CT revealed complete collapse of the right lung with associated hyperexpansion of the left lung and left‐to‐right mediastinal shift (Fig. 2, with an asterisk denoting the aortic arch; an arrow, the right main‐stem bronchus, which would soon terminate; and arrowheads, the collapsed right lung). No lung masses or effusions were noted; active TB had been ruled out with AFB sputums. Bronchoscopy revealed a fibrotic and stenotic right main‐stem bronchus (Fig. 3, with an asterisk denoting a patent left main‐stem bronchus and an arrow denoting a stenotic right main‐stem bronchus). Pulmonary manifestations of TB include parenchymal and endobronchial disease. Patients more likely to develop endobronchial disease include those with extensive pulmonary involvement, particularly cavitary lesions. Between 10% and 20% of patients with endobronchial disease will have normal CXRs, though CT scans may reveal endobronchial lesions or narrowing. Complications of endobronchial disease include obstruction, bronchiectasis, and tracheal or bronchial stenosis. Some airway obstructions may be associated with enlarging peribronchial nodes, which may erode into the airways as broncholiths. Steroids have been used to prevent long‐term complications, but their efficacy is still unclear. Repeated dilation, stenting, and resection all serve as management options for advanced endobronchial disease. In our patient, the extensive bronchial scarring and stenosis were most likely complications from past endobronchial infection. Unfortunately, attempts at balloon dilatation of her right main‐stem bronchus were unsuccessful, and she continues to have considerable exercise limitation. More prompt recognition of the disease may have allowed for an earlier and more successful intervention.
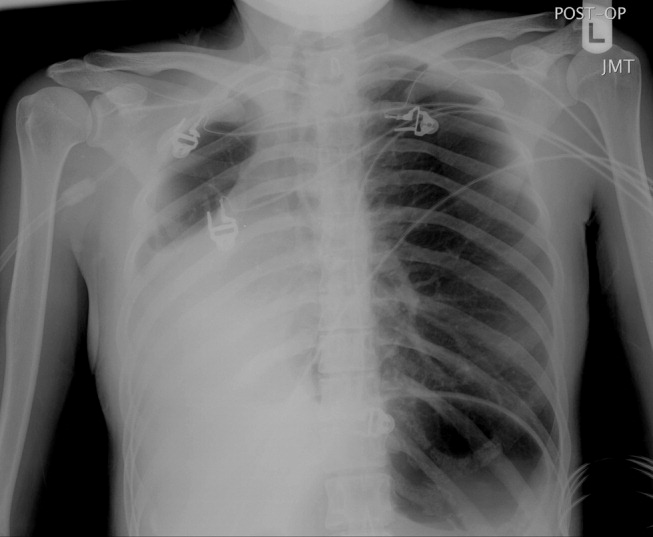
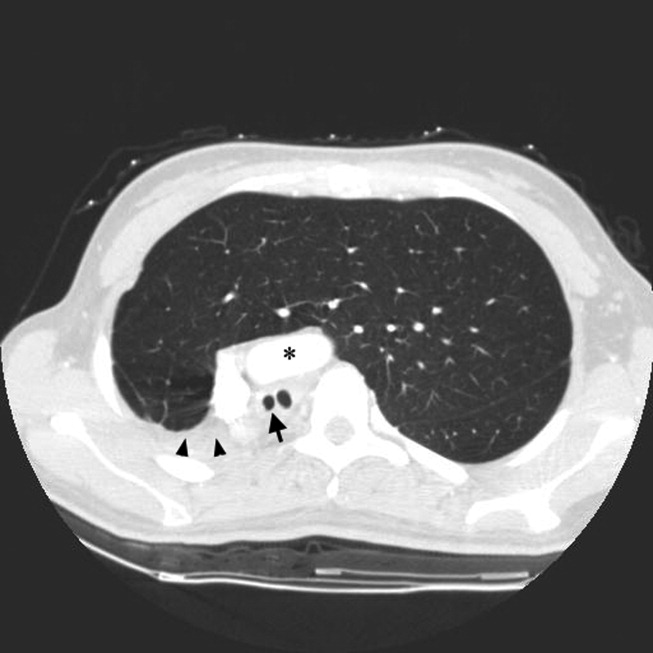
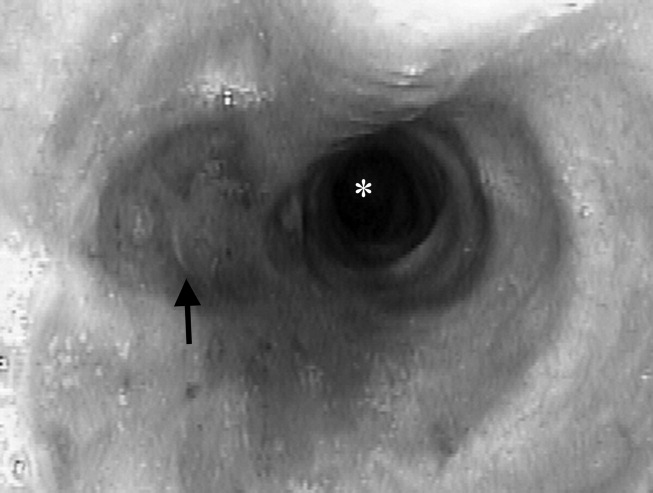
A 23‐year‐old Chinese woman presented with worsening exertional dyspnea. Her medical history was notable for pulmonary tuberculosis treated at the age of 16. Over the past 3 years, she reported progressive respiratory symptoms resulting in marked exercise intolerance. She denied any fevers, cough, or weight loss. On examination, she had right‐sided tracheal deviation but spoke comfortably. Her heart sounds were displaced and right‐sided breath sounds nearly absent. Chest x‐ray (Fig. 1) and subsequent CT revealed complete collapse of the right lung with associated hyperexpansion of the left lung and left‐to‐right mediastinal shift (Fig. 2, with an asterisk denoting the aortic arch; an arrow, the right main‐stem bronchus, which would soon terminate; and arrowheads, the collapsed right lung). No lung masses or effusions were noted; active TB had been ruled out with AFB sputums. Bronchoscopy revealed a fibrotic and stenotic right main‐stem bronchus (Fig. 3, with an asterisk denoting a patent left main‐stem bronchus and an arrow denoting a stenotic right main‐stem bronchus). Pulmonary manifestations of TB include parenchymal and endobronchial disease. Patients more likely to develop endobronchial disease include those with extensive pulmonary involvement, particularly cavitary lesions. Between 10% and 20% of patients with endobronchial disease will have normal CXRs, though CT scans may reveal endobronchial lesions or narrowing. Complications of endobronchial disease include obstruction, bronchiectasis, and tracheal or bronchial stenosis. Some airway obstructions may be associated with enlarging peribronchial nodes, which may erode into the airways as broncholiths. Steroids have been used to prevent long‐term complications, but their efficacy is still unclear. Repeated dilation, stenting, and resection all serve as management options for advanced endobronchial disease. In our patient, the extensive bronchial scarring and stenosis were most likely complications from past endobronchial infection. Unfortunately, attempts at balloon dilatation of her right main‐stem bronchus were unsuccessful, and she continues to have considerable exercise limitation. More prompt recognition of the disease may have allowed for an earlier and more successful intervention.
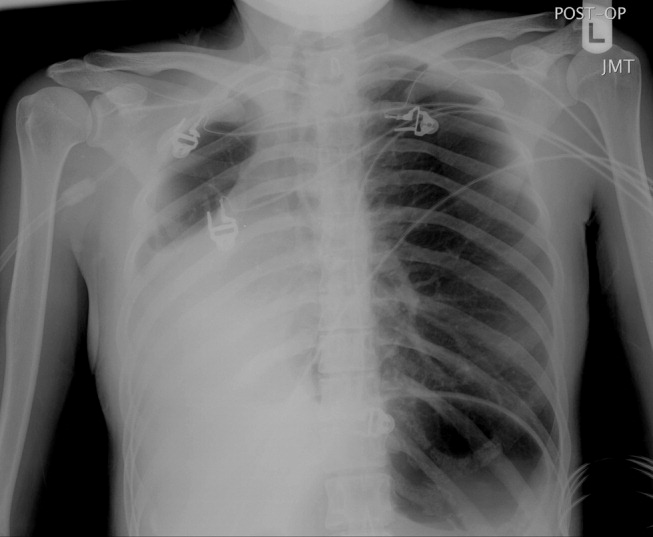
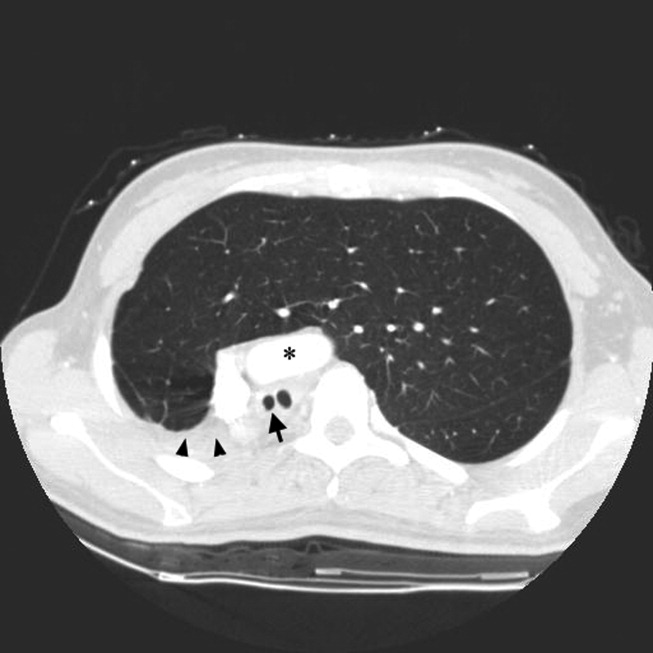
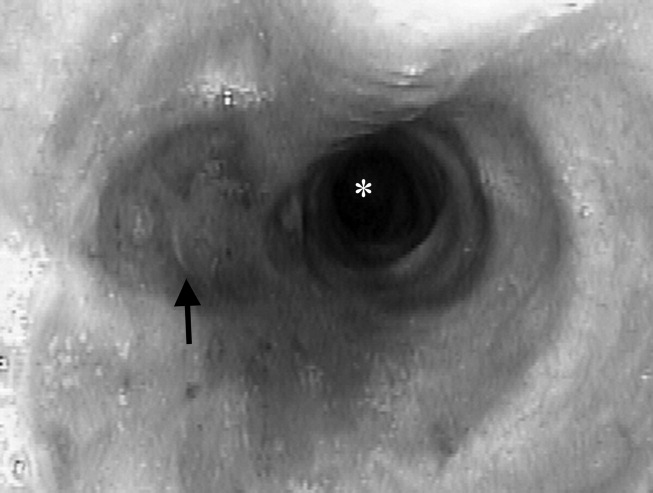
A 23‐year‐old Chinese woman presented with worsening exertional dyspnea. Her medical history was notable for pulmonary tuberculosis treated at the age of 16. Over the past 3 years, she reported progressive respiratory symptoms resulting in marked exercise intolerance. She denied any fevers, cough, or weight loss. On examination, she had right‐sided tracheal deviation but spoke comfortably. Her heart sounds were displaced and right‐sided breath sounds nearly absent. Chest x‐ray (Fig. 1) and subsequent CT revealed complete collapse of the right lung with associated hyperexpansion of the left lung and left‐to‐right mediastinal shift (Fig. 2, with an asterisk denoting the aortic arch; an arrow, the right main‐stem bronchus, which would soon terminate; and arrowheads, the collapsed right lung). No lung masses or effusions were noted; active TB had been ruled out with AFB sputums. Bronchoscopy revealed a fibrotic and stenotic right main‐stem bronchus (Fig. 3, with an asterisk denoting a patent left main‐stem bronchus and an arrow denoting a stenotic right main‐stem bronchus). Pulmonary manifestations of TB include parenchymal and endobronchial disease. Patients more likely to develop endobronchial disease include those with extensive pulmonary involvement, particularly cavitary lesions. Between 10% and 20% of patients with endobronchial disease will have normal CXRs, though CT scans may reveal endobronchial lesions or narrowing. Complications of endobronchial disease include obstruction, bronchiectasis, and tracheal or bronchial stenosis. Some airway obstructions may be associated with enlarging peribronchial nodes, which may erode into the airways as broncholiths. Steroids have been used to prevent long‐term complications, but their efficacy is still unclear. Repeated dilation, stenting, and resection all serve as management options for advanced endobronchial disease. In our patient, the extensive bronchial scarring and stenosis were most likely complications from past endobronchial infection. Unfortunately, attempts at balloon dilatation of her right main‐stem bronchus were unsuccessful, and she continues to have considerable exercise limitation. More prompt recognition of the disease may have allowed for an earlier and more successful intervention.
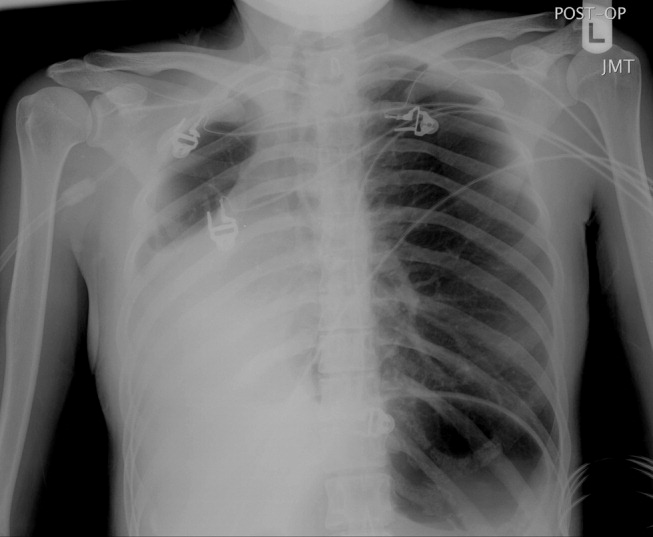
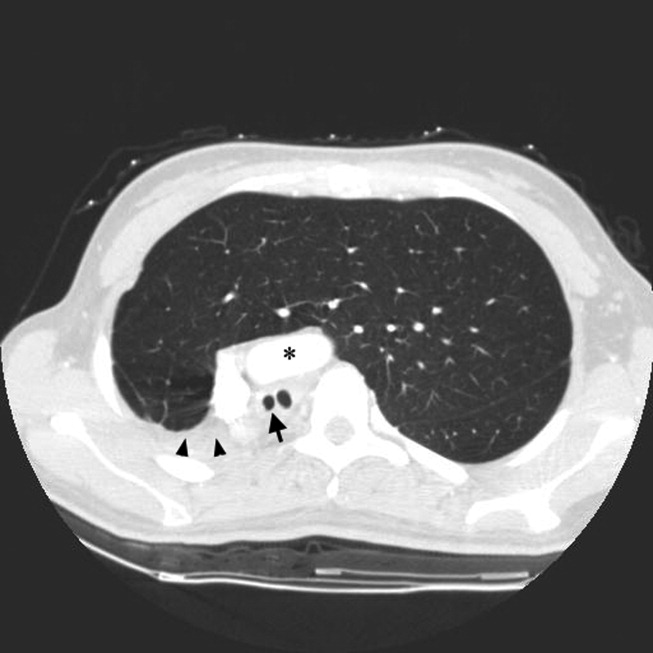
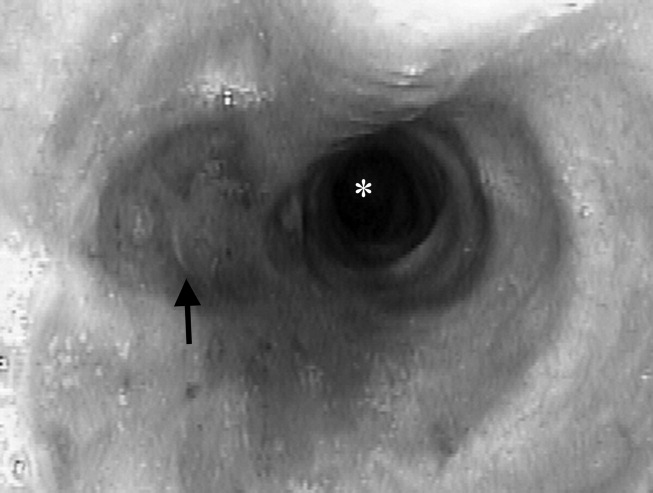
Color‐coded wristbands: Promoting safety or confusion?
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.