User login
Study: Shared decision-making in lung cancer screening needs work
Shared decision-making is an integral step in lung cancer screening with low-dose CT (LDCT) in high-risk patients, but a cross-sectional study at two academic medical centers in Texas has found wide variability in the quality of shared decision-making encounters and that nearly a third of patients reported being conflicted about their decisions to pursue screening.
Lead author Shawn P.E. Nishi, MD, associate professor in the division of pulmonary critical care and sleep medicine, department of internal medicine, of the University of Texas Medical Branch, Galveston, noted two striking findings of the study, published in Chest: that physicians rarely used decision aids according to Centers for Medicare & Medicaid Services direction, and that a “considerable imbalance” exists in the way physicians present management choices to patients. “As physicians, we want to focus on the positive,” she said, “but in shared decision-making (SDM) there needs to be a better balance between presentation and understanding of the risks and the benefits of lung cancer screening (LCS).”
Since 2015, CMS has reimbursed for LCS counseling and an shared decision-making visit before a patient has the screening.
The study analyzed self-reported survey results of 266 patients who had been through SDM at UTMB Galveston and MD Anderson Cancer Center in Houston in 2017. They completed patient surveys the following year. The study population was 87% White, 38% had a family history of lung cancer, and 39% were current smokers. The mean pack-year history was 40.4 years.
A high percentage – 86.6% – said they were satisfied with the level in which they were involved in their screening decision. Patients reported that their doctors talked to them about the benefits of LCS far more frequently than the potential harms, 68.3% to 20.8%. And 12.5% said they understood that an abnormal scan was likely to result in a negative finding. Only 30.7% said they’d received educational materials about LCS during the screening process.
A year after completing the SDM process, their knowledge of LCS was variable at best; on average, they answered 41.4% of the questions correctly, and almost one-third (31%) indicated that screening, rather than quitting smoking, was the best way reduce their lung cancer risk.
The study noted that, for patients who derive a small benefit from LCS, the absolute risk reduction is only 0.3%, which may not be enough to offset the potential harms of LDCT.
“The LCS exam itself is a simple noninvasive procedure; you get a scan and go about your day once it’s read,” Dr. Nishi said. “However there is a high false-positive rate, and the question really becomes that, as you start to work up those false positives and even true positives, however small, there is a risk associated with every procedure or evaluation thereafter. So the shared decision-making process is really there to ensure that patients value finding their lung cancer early if they do have it versus the potential harms down the line.”
However, as this study points out, there aren’t many parameters for what SDM entails. “It’s more than just an information exchange back and forth,” Dr. Nishi said. “It’s about having good-quality communication between the provider and patients so that the right decision can ultimately be made for each patient. It takes a very dedicated person that can commit the time and expertise to it. I don’t think that it should be taken lightly.”
As Dr. Nishi and colleagues pointed out in their study, SDM incorporates three essential elements: recognizing and acknowledging that a decision has to be made, knowing and understanding the best available evidence, and incorporating the patient’s own values and preferences in the decision.
CMS outlines specific components of SDM. It includes, beyond a discussion of the potential benefits and harms and use of a decision aid, education on the need for adherence to annual screening, and counseling on either stopping smoking or continued abstinence.
For physicians, dedicating the time and energy SDM needs can be a challenge, Dr. Nishi noted, “Health care doesn’t have a lot of support to perform shared decision-making,” she said. “In a very busy practice it’s very hard to make sure you have a good process where you can sit down and take all the time you need with a patient to open up a dialog about the risks and benefits.”
After they completed the screening process, 33.6% of patients said they had some conflicting feelings about their decision. Non-White patients were about four times more likely than White patients to feel conflicted about their choices (odds ratio, 4.31; 95% confidence interval, 1.36-13.70), as were former smokers, compared with current smokers (OR, 1.93; 95% CI, 1.04-3.55).
Future studies of SDM in LCS should focus on outcomes, said Dr. Nishi. “Hopefully then we can focus on those things that benefit patients the most.”
Abbie Begnaud, MD, FCCP, a pulmonologist at the University of Minnesota, Minneapolis, said this study confirmed what other studies found about shortcomings of SDM, with one difference. “We already knew we were not doing a great job at shared decision-making,” she said. “To me, the difference in this study is that most of the patients were pretty satisfied with their degree of involvement.”
She noted the low percentage of patients who understood that abnormal scans may be noncancerous. “This is one area that I think is an important place for us to improve,” Dr. Begnaud said.
The findings about non-White patients and former smokers are also telling, Dr. Begnaud said. “This highlights that we need to pay close attention to these two groups – people who have traditionally, historically been marginalized in medical care – and provide them the support they need to make a decision.”
Dr. Nishi and colleagues have no relevant disclosures. The study was supported by the Cancer Prevention and Research Institute of Texas and received grants from the National Cancer Institute and the University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. Dr. Begnaud has no relevant relationships to disclose.
Shared decision-making is an integral step in lung cancer screening with low-dose CT (LDCT) in high-risk patients, but a cross-sectional study at two academic medical centers in Texas has found wide variability in the quality of shared decision-making encounters and that nearly a third of patients reported being conflicted about their decisions to pursue screening.
Lead author Shawn P.E. Nishi, MD, associate professor in the division of pulmonary critical care and sleep medicine, department of internal medicine, of the University of Texas Medical Branch, Galveston, noted two striking findings of the study, published in Chest: that physicians rarely used decision aids according to Centers for Medicare & Medicaid Services direction, and that a “considerable imbalance” exists in the way physicians present management choices to patients. “As physicians, we want to focus on the positive,” she said, “but in shared decision-making (SDM) there needs to be a better balance between presentation and understanding of the risks and the benefits of lung cancer screening (LCS).”
Since 2015, CMS has reimbursed for LCS counseling and an shared decision-making visit before a patient has the screening.
The study analyzed self-reported survey results of 266 patients who had been through SDM at UTMB Galveston and MD Anderson Cancer Center in Houston in 2017. They completed patient surveys the following year. The study population was 87% White, 38% had a family history of lung cancer, and 39% were current smokers. The mean pack-year history was 40.4 years.
A high percentage – 86.6% – said they were satisfied with the level in which they were involved in their screening decision. Patients reported that their doctors talked to them about the benefits of LCS far more frequently than the potential harms, 68.3% to 20.8%. And 12.5% said they understood that an abnormal scan was likely to result in a negative finding. Only 30.7% said they’d received educational materials about LCS during the screening process.
A year after completing the SDM process, their knowledge of LCS was variable at best; on average, they answered 41.4% of the questions correctly, and almost one-third (31%) indicated that screening, rather than quitting smoking, was the best way reduce their lung cancer risk.
The study noted that, for patients who derive a small benefit from LCS, the absolute risk reduction is only 0.3%, which may not be enough to offset the potential harms of LDCT.
“The LCS exam itself is a simple noninvasive procedure; you get a scan and go about your day once it’s read,” Dr. Nishi said. “However there is a high false-positive rate, and the question really becomes that, as you start to work up those false positives and even true positives, however small, there is a risk associated with every procedure or evaluation thereafter. So the shared decision-making process is really there to ensure that patients value finding their lung cancer early if they do have it versus the potential harms down the line.”
However, as this study points out, there aren’t many parameters for what SDM entails. “It’s more than just an information exchange back and forth,” Dr. Nishi said. “It’s about having good-quality communication between the provider and patients so that the right decision can ultimately be made for each patient. It takes a very dedicated person that can commit the time and expertise to it. I don’t think that it should be taken lightly.”
As Dr. Nishi and colleagues pointed out in their study, SDM incorporates three essential elements: recognizing and acknowledging that a decision has to be made, knowing and understanding the best available evidence, and incorporating the patient’s own values and preferences in the decision.
CMS outlines specific components of SDM. It includes, beyond a discussion of the potential benefits and harms and use of a decision aid, education on the need for adherence to annual screening, and counseling on either stopping smoking or continued abstinence.
For physicians, dedicating the time and energy SDM needs can be a challenge, Dr. Nishi noted, “Health care doesn’t have a lot of support to perform shared decision-making,” she said. “In a very busy practice it’s very hard to make sure you have a good process where you can sit down and take all the time you need with a patient to open up a dialog about the risks and benefits.”
After they completed the screening process, 33.6% of patients said they had some conflicting feelings about their decision. Non-White patients were about four times more likely than White patients to feel conflicted about their choices (odds ratio, 4.31; 95% confidence interval, 1.36-13.70), as were former smokers, compared with current smokers (OR, 1.93; 95% CI, 1.04-3.55).
Future studies of SDM in LCS should focus on outcomes, said Dr. Nishi. “Hopefully then we can focus on those things that benefit patients the most.”
Abbie Begnaud, MD, FCCP, a pulmonologist at the University of Minnesota, Minneapolis, said this study confirmed what other studies found about shortcomings of SDM, with one difference. “We already knew we were not doing a great job at shared decision-making,” she said. “To me, the difference in this study is that most of the patients were pretty satisfied with their degree of involvement.”
She noted the low percentage of patients who understood that abnormal scans may be noncancerous. “This is one area that I think is an important place for us to improve,” Dr. Begnaud said.
The findings about non-White patients and former smokers are also telling, Dr. Begnaud said. “This highlights that we need to pay close attention to these two groups – people who have traditionally, historically been marginalized in medical care – and provide them the support they need to make a decision.”
Dr. Nishi and colleagues have no relevant disclosures. The study was supported by the Cancer Prevention and Research Institute of Texas and received grants from the National Cancer Institute and the University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. Dr. Begnaud has no relevant relationships to disclose.
Shared decision-making is an integral step in lung cancer screening with low-dose CT (LDCT) in high-risk patients, but a cross-sectional study at two academic medical centers in Texas has found wide variability in the quality of shared decision-making encounters and that nearly a third of patients reported being conflicted about their decisions to pursue screening.
Lead author Shawn P.E. Nishi, MD, associate professor in the division of pulmonary critical care and sleep medicine, department of internal medicine, of the University of Texas Medical Branch, Galveston, noted two striking findings of the study, published in Chest: that physicians rarely used decision aids according to Centers for Medicare & Medicaid Services direction, and that a “considerable imbalance” exists in the way physicians present management choices to patients. “As physicians, we want to focus on the positive,” she said, “but in shared decision-making (SDM) there needs to be a better balance between presentation and understanding of the risks and the benefits of lung cancer screening (LCS).”
Since 2015, CMS has reimbursed for LCS counseling and an shared decision-making visit before a patient has the screening.
The study analyzed self-reported survey results of 266 patients who had been through SDM at UTMB Galveston and MD Anderson Cancer Center in Houston in 2017. They completed patient surveys the following year. The study population was 87% White, 38% had a family history of lung cancer, and 39% were current smokers. The mean pack-year history was 40.4 years.
A high percentage – 86.6% – said they were satisfied with the level in which they were involved in their screening decision. Patients reported that their doctors talked to them about the benefits of LCS far more frequently than the potential harms, 68.3% to 20.8%. And 12.5% said they understood that an abnormal scan was likely to result in a negative finding. Only 30.7% said they’d received educational materials about LCS during the screening process.
A year after completing the SDM process, their knowledge of LCS was variable at best; on average, they answered 41.4% of the questions correctly, and almost one-third (31%) indicated that screening, rather than quitting smoking, was the best way reduce their lung cancer risk.
The study noted that, for patients who derive a small benefit from LCS, the absolute risk reduction is only 0.3%, which may not be enough to offset the potential harms of LDCT.
“The LCS exam itself is a simple noninvasive procedure; you get a scan and go about your day once it’s read,” Dr. Nishi said. “However there is a high false-positive rate, and the question really becomes that, as you start to work up those false positives and even true positives, however small, there is a risk associated with every procedure or evaluation thereafter. So the shared decision-making process is really there to ensure that patients value finding their lung cancer early if they do have it versus the potential harms down the line.”
However, as this study points out, there aren’t many parameters for what SDM entails. “It’s more than just an information exchange back and forth,” Dr. Nishi said. “It’s about having good-quality communication between the provider and patients so that the right decision can ultimately be made for each patient. It takes a very dedicated person that can commit the time and expertise to it. I don’t think that it should be taken lightly.”
As Dr. Nishi and colleagues pointed out in their study, SDM incorporates three essential elements: recognizing and acknowledging that a decision has to be made, knowing and understanding the best available evidence, and incorporating the patient’s own values and preferences in the decision.
CMS outlines specific components of SDM. It includes, beyond a discussion of the potential benefits and harms and use of a decision aid, education on the need for adherence to annual screening, and counseling on either stopping smoking or continued abstinence.
For physicians, dedicating the time and energy SDM needs can be a challenge, Dr. Nishi noted, “Health care doesn’t have a lot of support to perform shared decision-making,” she said. “In a very busy practice it’s very hard to make sure you have a good process where you can sit down and take all the time you need with a patient to open up a dialog about the risks and benefits.”
After they completed the screening process, 33.6% of patients said they had some conflicting feelings about their decision. Non-White patients were about four times more likely than White patients to feel conflicted about their choices (odds ratio, 4.31; 95% confidence interval, 1.36-13.70), as were former smokers, compared with current smokers (OR, 1.93; 95% CI, 1.04-3.55).
Future studies of SDM in LCS should focus on outcomes, said Dr. Nishi. “Hopefully then we can focus on those things that benefit patients the most.”
Abbie Begnaud, MD, FCCP, a pulmonologist at the University of Minnesota, Minneapolis, said this study confirmed what other studies found about shortcomings of SDM, with one difference. “We already knew we were not doing a great job at shared decision-making,” she said. “To me, the difference in this study is that most of the patients were pretty satisfied with their degree of involvement.”
She noted the low percentage of patients who understood that abnormal scans may be noncancerous. “This is one area that I think is an important place for us to improve,” Dr. Begnaud said.
The findings about non-White patients and former smokers are also telling, Dr. Begnaud said. “This highlights that we need to pay close attention to these two groups – people who have traditionally, historically been marginalized in medical care – and provide them the support they need to make a decision.”
Dr. Nishi and colleagues have no relevant disclosures. The study was supported by the Cancer Prevention and Research Institute of Texas and received grants from the National Cancer Institute and the University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. Dr. Begnaud has no relevant relationships to disclose.
FROM CHEST
Study clarifies who gets post–COVID-19 interstitial lung disease
A study of post–COVID-19 patients in the United Kingdom who developed severe lung inflammation after they left the hospital may provide greater clarity on which patients are most likely to have persistent lung dysfunction.
In addition to pinpointing those most at risk, the findings showed that conventional corticosteroid treatment is highly effective in improving lung function and reducing symptoms.
Researchers from Guy’s and St. Thomas’ National Health Foundation Trust in London reported that a small percentage of patients – 4.8%, or 35 of 837 patients in the study – had severe persistent interstitial lung disease (ILD), mostly organizing pneumonia, 4 weeks after discharge. Of these patients, 30 received steroid treatment, all of whom showed improvement in lung function.
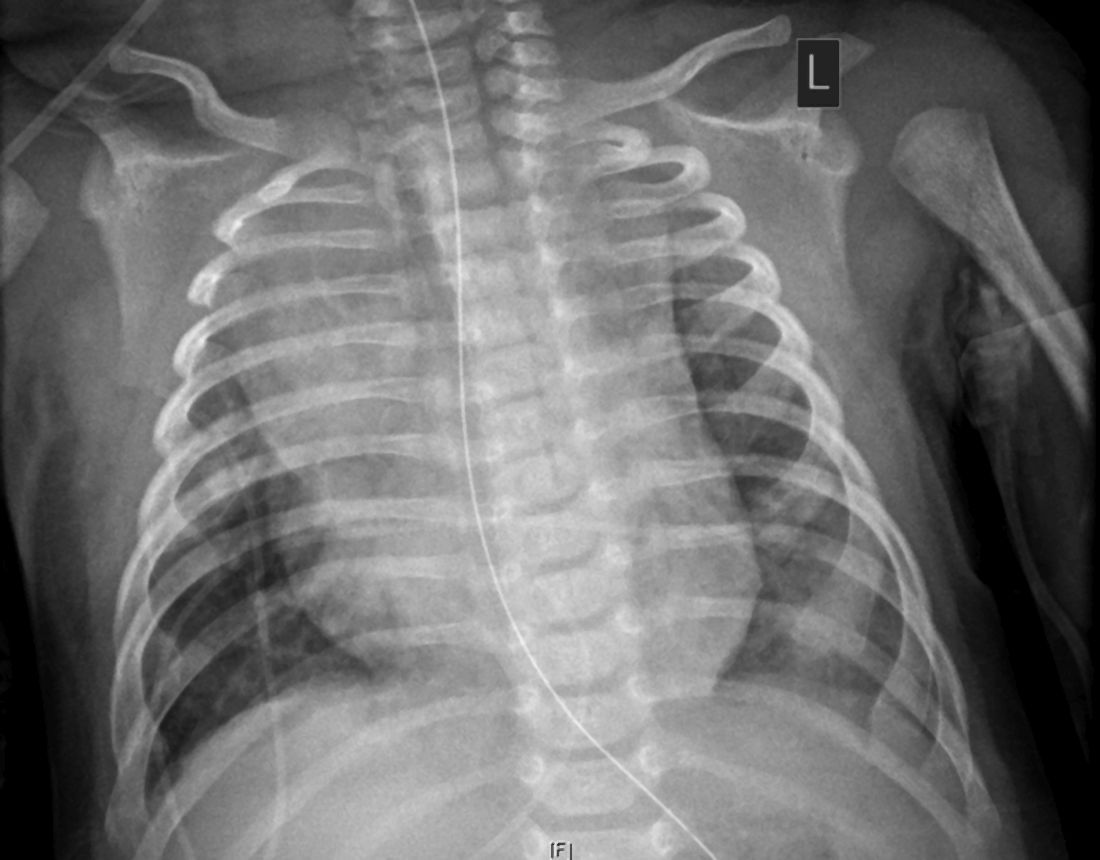
Lead author Katherine Jane Myall, MRCP, and colleagues wrote that the most common radiologic finding in acute COVID-19 is bilateral ground-glass opacification, and findings of organizing pneumonia are common. However, no reports exist of the role of inflammatory infiltrates during recovery from COVID-19 or of the effectiveness of treatments for persistent ILD. “The long-term respiratory morbidity remains unclear,” Dr. Myall and colleagues wrote.
The study findings are significant because they quantify the degree of lung disease that patients have after COVID-19, said Sachin Gupta, MD, FCCP, a pulmonologist and critical care specialist at Alameda Health System in Oakland, Calif. He added that the disease course and presentation followed the pattern of organizing pneumonia in some patients, and traditional corticosteroid therapy seemed to resolve symptoms and improve lung function.
“This is a really important piece to get out there because it describes what a lot of us are worried about in patients with post-COVID lung disease and about what type of lung disease they have. It offers a potential treatment,” he said.
Dr. Myall and colleagues noted that even a “relatively small proportion” of patients with persistent, severe ILD – as reported in this study – pose “a significant disease burden.” They added: “Prompt therapy may avoid potentially permanent fibrosis and functional impairment.”
The single-center, prospective, observational study followed discharged patients with telephone calls 4 weeks after discharge to determine their status. At that point, 39% of the study cohort (n = 325) reported ongoing symptoms.
The patients had outpatient examinations at 6 weeks post discharge, at which time 42.9% (n = 138) had no signs or symptoms of persistent disease; 33.8% (n = 110) had symptoms but no radiologic findings and received referrals to other departments; and 24% (n = 77) were referred to the post-COVID lung disease multidisciplinary team. A total of 59 were diagnosed with persistent post-COVID interstitial change, 35 of whom had organizing pneumonia, hence the rationale for using steroids in this group, Dr. Myall and colleagues stated.
The 30 patients treated with corticosteroids received a maximum initial dose of 0.5 mg/kg prednisolone, which was rapidly weaned over 3 weeks. Some patients received lower doses depending on their comorbidities.
Treatment resulted in an average relative increase in transfer factor of 31.6% (P < .001) and forced vital capacity of 9.6% (P = .014), along with significant improvement in symptoms and x-ray signs.
The study identified some key characteristics of the patients who had persistent post–COVID-19 inflammatory ILD. They were mostly male (71.5%) and overweight with an average body mass index of 28.3, but only 26% were obese. Most had at least one comorbidity, with the most common being diabetes and asthma (22.9%). Their average hospital stay was 16.9 days, 82.9% required oxygen, 55% were in the ICU, and 46% needed invasive mechanical ventilation.
The patients most vulnerable to ILD and organizing pneumonia were the “sicker” of the whole cohort, Dr. Gupta said. “In one sense, it’s reassuring that this is not just happening in anyone; this is happening in patients who had the worst course and were hospitalized in the ICU for the most part.”
The study shows that identifying these patients early on and initiating steroid therapy could avoid persistent lung injury and scarring, Dr. Gupta said.
The London researchers noted that theirs wasn’t a radiologic study, so CT scans weren’t formally scored before and after treatment. They also acknowledged vagueness about imaging and clinical findings representing “nothing other than slow ongoing recovery.”
Patients with post–COVID-19 ILD will require ongoing follow-up to better understand the disease course, Dr. Myall and colleagues stated, although they predicted organizing pneumonia is unlikely to recur once it resolves.
Dr. Myall and coauthors had no relevant relationships to disclose. Dr. Gupta disclosed he is also an employee and shareholder at Genentech.
A study of post–COVID-19 patients in the United Kingdom who developed severe lung inflammation after they left the hospital may provide greater clarity on which patients are most likely to have persistent lung dysfunction.
In addition to pinpointing those most at risk, the findings showed that conventional corticosteroid treatment is highly effective in improving lung function and reducing symptoms.
Researchers from Guy’s and St. Thomas’ National Health Foundation Trust in London reported that a small percentage of patients – 4.8%, or 35 of 837 patients in the study – had severe persistent interstitial lung disease (ILD), mostly organizing pneumonia, 4 weeks after discharge. Of these patients, 30 received steroid treatment, all of whom showed improvement in lung function.
Lead author Katherine Jane Myall, MRCP, and colleagues wrote that the most common radiologic finding in acute COVID-19 is bilateral ground-glass opacification, and findings of organizing pneumonia are common. However, no reports exist of the role of inflammatory infiltrates during recovery from COVID-19 or of the effectiveness of treatments for persistent ILD. “The long-term respiratory morbidity remains unclear,” Dr. Myall and colleagues wrote.
The study findings are significant because they quantify the degree of lung disease that patients have after COVID-19, said Sachin Gupta, MD, FCCP, a pulmonologist and critical care specialist at Alameda Health System in Oakland, Calif. He added that the disease course and presentation followed the pattern of organizing pneumonia in some patients, and traditional corticosteroid therapy seemed to resolve symptoms and improve lung function.
“This is a really important piece to get out there because it describes what a lot of us are worried about in patients with post-COVID lung disease and about what type of lung disease they have. It offers a potential treatment,” he said.
Dr. Myall and colleagues noted that even a “relatively small proportion” of patients with persistent, severe ILD – as reported in this study – pose “a significant disease burden.” They added: “Prompt therapy may avoid potentially permanent fibrosis and functional impairment.”
The single-center, prospective, observational study followed discharged patients with telephone calls 4 weeks after discharge to determine their status. At that point, 39% of the study cohort (n = 325) reported ongoing symptoms.
The patients had outpatient examinations at 6 weeks post discharge, at which time 42.9% (n = 138) had no signs or symptoms of persistent disease; 33.8% (n = 110) had symptoms but no radiologic findings and received referrals to other departments; and 24% (n = 77) were referred to the post-COVID lung disease multidisciplinary team. A total of 59 were diagnosed with persistent post-COVID interstitial change, 35 of whom had organizing pneumonia, hence the rationale for using steroids in this group, Dr. Myall and colleagues stated.
The 30 patients treated with corticosteroids received a maximum initial dose of 0.5 mg/kg prednisolone, which was rapidly weaned over 3 weeks. Some patients received lower doses depending on their comorbidities.
Treatment resulted in an average relative increase in transfer factor of 31.6% (P < .001) and forced vital capacity of 9.6% (P = .014), along with significant improvement in symptoms and x-ray signs.
The study identified some key characteristics of the patients who had persistent post–COVID-19 inflammatory ILD. They were mostly male (71.5%) and overweight with an average body mass index of 28.3, but only 26% were obese. Most had at least one comorbidity, with the most common being diabetes and asthma (22.9%). Their average hospital stay was 16.9 days, 82.9% required oxygen, 55% were in the ICU, and 46% needed invasive mechanical ventilation.
The patients most vulnerable to ILD and organizing pneumonia were the “sicker” of the whole cohort, Dr. Gupta said. “In one sense, it’s reassuring that this is not just happening in anyone; this is happening in patients who had the worst course and were hospitalized in the ICU for the most part.”
The study shows that identifying these patients early on and initiating steroid therapy could avoid persistent lung injury and scarring, Dr. Gupta said.
The London researchers noted that theirs wasn’t a radiologic study, so CT scans weren’t formally scored before and after treatment. They also acknowledged vagueness about imaging and clinical findings representing “nothing other than slow ongoing recovery.”
Patients with post–COVID-19 ILD will require ongoing follow-up to better understand the disease course, Dr. Myall and colleagues stated, although they predicted organizing pneumonia is unlikely to recur once it resolves.
Dr. Myall and coauthors had no relevant relationships to disclose. Dr. Gupta disclosed he is also an employee and shareholder at Genentech.
A study of post–COVID-19 patients in the United Kingdom who developed severe lung inflammation after they left the hospital may provide greater clarity on which patients are most likely to have persistent lung dysfunction.
In addition to pinpointing those most at risk, the findings showed that conventional corticosteroid treatment is highly effective in improving lung function and reducing symptoms.
Researchers from Guy’s and St. Thomas’ National Health Foundation Trust in London reported that a small percentage of patients – 4.8%, or 35 of 837 patients in the study – had severe persistent interstitial lung disease (ILD), mostly organizing pneumonia, 4 weeks after discharge. Of these patients, 30 received steroid treatment, all of whom showed improvement in lung function.
Lead author Katherine Jane Myall, MRCP, and colleagues wrote that the most common radiologic finding in acute COVID-19 is bilateral ground-glass opacification, and findings of organizing pneumonia are common. However, no reports exist of the role of inflammatory infiltrates during recovery from COVID-19 or of the effectiveness of treatments for persistent ILD. “The long-term respiratory morbidity remains unclear,” Dr. Myall and colleagues wrote.
The study findings are significant because they quantify the degree of lung disease that patients have after COVID-19, said Sachin Gupta, MD, FCCP, a pulmonologist and critical care specialist at Alameda Health System in Oakland, Calif. He added that the disease course and presentation followed the pattern of organizing pneumonia in some patients, and traditional corticosteroid therapy seemed to resolve symptoms and improve lung function.
“This is a really important piece to get out there because it describes what a lot of us are worried about in patients with post-COVID lung disease and about what type of lung disease they have. It offers a potential treatment,” he said.
Dr. Myall and colleagues noted that even a “relatively small proportion” of patients with persistent, severe ILD – as reported in this study – pose “a significant disease burden.” They added: “Prompt therapy may avoid potentially permanent fibrosis and functional impairment.”
The single-center, prospective, observational study followed discharged patients with telephone calls 4 weeks after discharge to determine their status. At that point, 39% of the study cohort (n = 325) reported ongoing symptoms.
The patients had outpatient examinations at 6 weeks post discharge, at which time 42.9% (n = 138) had no signs or symptoms of persistent disease; 33.8% (n = 110) had symptoms but no radiologic findings and received referrals to other departments; and 24% (n = 77) were referred to the post-COVID lung disease multidisciplinary team. A total of 59 were diagnosed with persistent post-COVID interstitial change, 35 of whom had organizing pneumonia, hence the rationale for using steroids in this group, Dr. Myall and colleagues stated.
The 30 patients treated with corticosteroids received a maximum initial dose of 0.5 mg/kg prednisolone, which was rapidly weaned over 3 weeks. Some patients received lower doses depending on their comorbidities.
Treatment resulted in an average relative increase in transfer factor of 31.6% (P < .001) and forced vital capacity of 9.6% (P = .014), along with significant improvement in symptoms and x-ray signs.
The study identified some key characteristics of the patients who had persistent post–COVID-19 inflammatory ILD. They were mostly male (71.5%) and overweight with an average body mass index of 28.3, but only 26% were obese. Most had at least one comorbidity, with the most common being diabetes and asthma (22.9%). Their average hospital stay was 16.9 days, 82.9% required oxygen, 55% were in the ICU, and 46% needed invasive mechanical ventilation.
The patients most vulnerable to ILD and organizing pneumonia were the “sicker” of the whole cohort, Dr. Gupta said. “In one sense, it’s reassuring that this is not just happening in anyone; this is happening in patients who had the worst course and were hospitalized in the ICU for the most part.”
The study shows that identifying these patients early on and initiating steroid therapy could avoid persistent lung injury and scarring, Dr. Gupta said.
The London researchers noted that theirs wasn’t a radiologic study, so CT scans weren’t formally scored before and after treatment. They also acknowledged vagueness about imaging and clinical findings representing “nothing other than slow ongoing recovery.”
Patients with post–COVID-19 ILD will require ongoing follow-up to better understand the disease course, Dr. Myall and colleagues stated, although they predicted organizing pneumonia is unlikely to recur once it resolves.
Dr. Myall and coauthors had no relevant relationships to disclose. Dr. Gupta disclosed he is also an employee and shareholder at Genentech.
FROM ANNALS OF THE AMERICAN THORACIC SOCIETY
Telemedicine models show some benefit in OA
Remote interventions using an Internet-based app and telephone outreach to engage patients with osteoarthritis to self-manage their disease have demonstrated the potential to improve some symptoms, at least in the short term, showing the potential for tools to interact with OA patients without having them come into an office or clinic.
Remote interaction using these two forms of telemedicine – one a sophisticated digital platform, the other using a device that’s been around for almost 150 years – may have greater utility for keeping physicians connected with their OA patients during the COVID-19 pandemic, OA experts said in an interview.
“This is certainly relevant during the pandemic, but this has been of high interest for years as well, as researchers and clinicians have been seeking the best ways to reach patients with these types of programs,” said Kelli Allen, PhD, a research health scientist at the University of North Carolina at Chapel Hill.
Two separate studies evaluated the telemedicine platforms. In JAMA Internal Medicine, researchers reported that telephone-based cognitive-behavioral therapy (CBT) for patients aged 60 and older with OA and insomnia led to improved sleep, fatigue and, to a lesser extent, pain, in a randomized, controlled trial with 327 patients.
A separate randomized, controlled trial of 105 OA patients at the University of Nottingham (England), published in JAMA Network Open, reported that users of a smartphone-based exercise intervention app had greater improvements in pain and function than did controls.
“I think these two studies represent a first step in terms of moving forward, and certainly the interventions could be refined and potentially combined together for patients in the future,” said C. Kent Kwoh, MD, director of the University of Arizona Arthritis Center in Tucson.
Phone-based CBT study
The telephone-based CBT study consisted of two groups: the CBT group (n = 163) who completed six 20- to 30-minute telephone calls over 8 weeks, kept daily diaries, and received tailored educational materials and an education-only group (n = 164). At 2 months after treatment, Insomnia Severity Index scores decreased 8.1 points on average in the CBT group versus 4.8 points in the education-only patients (P < .001).
That variation between the intervention group and controls was sustained out to a year: 7.7 points lower than baseline versus 4.7 points lower. At the same time point, 56.3% of the CBT group remained in remission with Insomnia Severity Index scores less than 7 versus 25.8% of controls. Fatigue outcomes were similarly disparate between the groups.
Pain outcomes were a different story, however. “Post treatment, significant differences were observed for pain, but these differences were not sustained at 12-month follow-up,” first author Susan M. McCurry, PhD, a clinical psychologist and faculty member at the University of Washington, Seattle, and colleagues wrote.
“I think their positive findings illustrate that remotely delivered interventions can be ‘low tech’ and still effective,” Dr. Allen said of the CBT phone study. She noted that complete case data were available for 282 of 327 patients. “The high rate of session attendance suggests that they chose a delivery modality appropriate for their target patient group.”
The scalability of the telephone model is noteworthy, Dr. Kwoh said. “Having a telemedicine intervention that could be scaled a little more easily rather than an in-person intervention, and having individualized treatment, that’s beneficial, as is targeting two symptoms that are very bothersome and burdensome to patients with OA: insomnia and fatigue.” Following patients out to 12 months is a strength of the study, he added.
Smartphone app–based exercise study
The U.K. study evaluated 6-week outcomes of 48 patients with knee OA who used a proprietary app-based exercise program (Joint Academy) and 57 controls who used traditional self-management. The app provided daily exercises and texts, along with email and smartphone reminders. The app was derived from the Better Management of Patients with OA program initiated in Sweden in 2008 that used OA treatment guidelines for education and exercise in person in primary care clinics.
App users showed a 1.5-point reduction in numeric rating scale (NRS) pain score at 6 weeks versus virtually no change in controls (P < .001). In terms of secondary outcomes, pain scores improved 2.2 points on average for app users versus 1.2 for controls (P = .02), with similar improvements recorded in both stiffness and physical function.
Average change in the 30-second sit-to-stand test measured 4.5 for the app users and 1.2 for the usual-care group (P < .001). The study found no difference between the two groups in changes in temporal summation, conditional pain modulation, or Arthritis Research UK Musculoskeletal Health Questionnaire scores.
First author Sameer Akram Gohir, MSc, PhD, and colleagues wrote that the reasons for differences in outcomes between app users and controls aren’t clear. “The superior outcome in the intervention group may depend on the content and context in the app, including a combination of standardized exercises and information, as well as using a digital delivery system.”
Data gathering was cut short because of COVID-19 restrictions in the United Kingdom, as 27 patients missed their in-person follow-up visits. That was one shortcoming of the study, Dr. Kwoh noted.
“Given the caveats certainly they were able to show robust changes in terms of decreased pain, and also improvement in a variety of performance measures. Certainly this may be beneficial – we don’t know – in terms of cost-effectiveness, but it may be beneficial for insurance companies to adapt such a program,” he said, adding that future studies into the cost effectiveness of the digital platform would be in order.
“Certainly, if this program were to decrease physician visits or postpone the need for joint replacement for individuals, then it could be certainly very cost effective,” Dr. Kwoh said.
The completion rate among patients in the study – almost 90% – was “impressive,” Dr. Allen said. “However, this is a relatively short-term study, and I think an important question for future research is whether patients continue with this level of engagement for a longer period of time.”
Dr. McCurry had no relevant financial relationships to disclose. The CBT phone study received funding from the Public Health Service and the National Institute on Aging. Coauthors disclosed relationships with Campbell Alliance Group, Mapi Research Trust, and Pfizer. Dr. Gohir reported no relevant financial relationships. The study received funding from the Versus Arthritis UK Plan Center, the National Institute for Health Research Nottingham Biomedical Research Center, and Pfizer Global. The Joint Academy provided software for the study. A coauthor reported a financial relationships with Pfizer. Dr. Kwoh said that in the past year he has consulted for Express Scripts, Kolon Tissue Gene, LG Chem, and Regeneron. In the past year, he also received institutional grants for clinical trials from AbbVie, Cumberland, Eicos, Eli Lilly, GlaxoSmithKline, Mitsubishi, and Pfizer. Dr. Allen had no relevant financial relationships to disclose.
Remote interventions using an Internet-based app and telephone outreach to engage patients with osteoarthritis to self-manage their disease have demonstrated the potential to improve some symptoms, at least in the short term, showing the potential for tools to interact with OA patients without having them come into an office or clinic.
Remote interaction using these two forms of telemedicine – one a sophisticated digital platform, the other using a device that’s been around for almost 150 years – may have greater utility for keeping physicians connected with their OA patients during the COVID-19 pandemic, OA experts said in an interview.
“This is certainly relevant during the pandemic, but this has been of high interest for years as well, as researchers and clinicians have been seeking the best ways to reach patients with these types of programs,” said Kelli Allen, PhD, a research health scientist at the University of North Carolina at Chapel Hill.
Two separate studies evaluated the telemedicine platforms. In JAMA Internal Medicine, researchers reported that telephone-based cognitive-behavioral therapy (CBT) for patients aged 60 and older with OA and insomnia led to improved sleep, fatigue and, to a lesser extent, pain, in a randomized, controlled trial with 327 patients.
A separate randomized, controlled trial of 105 OA patients at the University of Nottingham (England), published in JAMA Network Open, reported that users of a smartphone-based exercise intervention app had greater improvements in pain and function than did controls.
“I think these two studies represent a first step in terms of moving forward, and certainly the interventions could be refined and potentially combined together for patients in the future,” said C. Kent Kwoh, MD, director of the University of Arizona Arthritis Center in Tucson.
Phone-based CBT study
The telephone-based CBT study consisted of two groups: the CBT group (n = 163) who completed six 20- to 30-minute telephone calls over 8 weeks, kept daily diaries, and received tailored educational materials and an education-only group (n = 164). At 2 months after treatment, Insomnia Severity Index scores decreased 8.1 points on average in the CBT group versus 4.8 points in the education-only patients (P < .001).
That variation between the intervention group and controls was sustained out to a year: 7.7 points lower than baseline versus 4.7 points lower. At the same time point, 56.3% of the CBT group remained in remission with Insomnia Severity Index scores less than 7 versus 25.8% of controls. Fatigue outcomes were similarly disparate between the groups.
Pain outcomes were a different story, however. “Post treatment, significant differences were observed for pain, but these differences were not sustained at 12-month follow-up,” first author Susan M. McCurry, PhD, a clinical psychologist and faculty member at the University of Washington, Seattle, and colleagues wrote.
“I think their positive findings illustrate that remotely delivered interventions can be ‘low tech’ and still effective,” Dr. Allen said of the CBT phone study. She noted that complete case data were available for 282 of 327 patients. “The high rate of session attendance suggests that they chose a delivery modality appropriate for their target patient group.”
The scalability of the telephone model is noteworthy, Dr. Kwoh said. “Having a telemedicine intervention that could be scaled a little more easily rather than an in-person intervention, and having individualized treatment, that’s beneficial, as is targeting two symptoms that are very bothersome and burdensome to patients with OA: insomnia and fatigue.” Following patients out to 12 months is a strength of the study, he added.
Smartphone app–based exercise study
The U.K. study evaluated 6-week outcomes of 48 patients with knee OA who used a proprietary app-based exercise program (Joint Academy) and 57 controls who used traditional self-management. The app provided daily exercises and texts, along with email and smartphone reminders. The app was derived from the Better Management of Patients with OA program initiated in Sweden in 2008 that used OA treatment guidelines for education and exercise in person in primary care clinics.
App users showed a 1.5-point reduction in numeric rating scale (NRS) pain score at 6 weeks versus virtually no change in controls (P < .001). In terms of secondary outcomes, pain scores improved 2.2 points on average for app users versus 1.2 for controls (P = .02), with similar improvements recorded in both stiffness and physical function.
Average change in the 30-second sit-to-stand test measured 4.5 for the app users and 1.2 for the usual-care group (P < .001). The study found no difference between the two groups in changes in temporal summation, conditional pain modulation, or Arthritis Research UK Musculoskeletal Health Questionnaire scores.
First author Sameer Akram Gohir, MSc, PhD, and colleagues wrote that the reasons for differences in outcomes between app users and controls aren’t clear. “The superior outcome in the intervention group may depend on the content and context in the app, including a combination of standardized exercises and information, as well as using a digital delivery system.”
Data gathering was cut short because of COVID-19 restrictions in the United Kingdom, as 27 patients missed their in-person follow-up visits. That was one shortcoming of the study, Dr. Kwoh noted.
“Given the caveats certainly they were able to show robust changes in terms of decreased pain, and also improvement in a variety of performance measures. Certainly this may be beneficial – we don’t know – in terms of cost-effectiveness, but it may be beneficial for insurance companies to adapt such a program,” he said, adding that future studies into the cost effectiveness of the digital platform would be in order.
“Certainly, if this program were to decrease physician visits or postpone the need for joint replacement for individuals, then it could be certainly very cost effective,” Dr. Kwoh said.
The completion rate among patients in the study – almost 90% – was “impressive,” Dr. Allen said. “However, this is a relatively short-term study, and I think an important question for future research is whether patients continue with this level of engagement for a longer period of time.”
Dr. McCurry had no relevant financial relationships to disclose. The CBT phone study received funding from the Public Health Service and the National Institute on Aging. Coauthors disclosed relationships with Campbell Alliance Group, Mapi Research Trust, and Pfizer. Dr. Gohir reported no relevant financial relationships. The study received funding from the Versus Arthritis UK Plan Center, the National Institute for Health Research Nottingham Biomedical Research Center, and Pfizer Global. The Joint Academy provided software for the study. A coauthor reported a financial relationships with Pfizer. Dr. Kwoh said that in the past year he has consulted for Express Scripts, Kolon Tissue Gene, LG Chem, and Regeneron. In the past year, he also received institutional grants for clinical trials from AbbVie, Cumberland, Eicos, Eli Lilly, GlaxoSmithKline, Mitsubishi, and Pfizer. Dr. Allen had no relevant financial relationships to disclose.
Remote interventions using an Internet-based app and telephone outreach to engage patients with osteoarthritis to self-manage their disease have demonstrated the potential to improve some symptoms, at least in the short term, showing the potential for tools to interact with OA patients without having them come into an office or clinic.
Remote interaction using these two forms of telemedicine – one a sophisticated digital platform, the other using a device that’s been around for almost 150 years – may have greater utility for keeping physicians connected with their OA patients during the COVID-19 pandemic, OA experts said in an interview.
“This is certainly relevant during the pandemic, but this has been of high interest for years as well, as researchers and clinicians have been seeking the best ways to reach patients with these types of programs,” said Kelli Allen, PhD, a research health scientist at the University of North Carolina at Chapel Hill.
Two separate studies evaluated the telemedicine platforms. In JAMA Internal Medicine, researchers reported that telephone-based cognitive-behavioral therapy (CBT) for patients aged 60 and older with OA and insomnia led to improved sleep, fatigue and, to a lesser extent, pain, in a randomized, controlled trial with 327 patients.
A separate randomized, controlled trial of 105 OA patients at the University of Nottingham (England), published in JAMA Network Open, reported that users of a smartphone-based exercise intervention app had greater improvements in pain and function than did controls.
“I think these two studies represent a first step in terms of moving forward, and certainly the interventions could be refined and potentially combined together for patients in the future,” said C. Kent Kwoh, MD, director of the University of Arizona Arthritis Center in Tucson.
Phone-based CBT study
The telephone-based CBT study consisted of two groups: the CBT group (n = 163) who completed six 20- to 30-minute telephone calls over 8 weeks, kept daily diaries, and received tailored educational materials and an education-only group (n = 164). At 2 months after treatment, Insomnia Severity Index scores decreased 8.1 points on average in the CBT group versus 4.8 points in the education-only patients (P < .001).
That variation between the intervention group and controls was sustained out to a year: 7.7 points lower than baseline versus 4.7 points lower. At the same time point, 56.3% of the CBT group remained in remission with Insomnia Severity Index scores less than 7 versus 25.8% of controls. Fatigue outcomes were similarly disparate between the groups.
Pain outcomes were a different story, however. “Post treatment, significant differences were observed for pain, but these differences were not sustained at 12-month follow-up,” first author Susan M. McCurry, PhD, a clinical psychologist and faculty member at the University of Washington, Seattle, and colleagues wrote.
“I think their positive findings illustrate that remotely delivered interventions can be ‘low tech’ and still effective,” Dr. Allen said of the CBT phone study. She noted that complete case data were available for 282 of 327 patients. “The high rate of session attendance suggests that they chose a delivery modality appropriate for their target patient group.”
The scalability of the telephone model is noteworthy, Dr. Kwoh said. “Having a telemedicine intervention that could be scaled a little more easily rather than an in-person intervention, and having individualized treatment, that’s beneficial, as is targeting two symptoms that are very bothersome and burdensome to patients with OA: insomnia and fatigue.” Following patients out to 12 months is a strength of the study, he added.
Smartphone app–based exercise study
The U.K. study evaluated 6-week outcomes of 48 patients with knee OA who used a proprietary app-based exercise program (Joint Academy) and 57 controls who used traditional self-management. The app provided daily exercises and texts, along with email and smartphone reminders. The app was derived from the Better Management of Patients with OA program initiated in Sweden in 2008 that used OA treatment guidelines for education and exercise in person in primary care clinics.
App users showed a 1.5-point reduction in numeric rating scale (NRS) pain score at 6 weeks versus virtually no change in controls (P < .001). In terms of secondary outcomes, pain scores improved 2.2 points on average for app users versus 1.2 for controls (P = .02), with similar improvements recorded in both stiffness and physical function.
Average change in the 30-second sit-to-stand test measured 4.5 for the app users and 1.2 for the usual-care group (P < .001). The study found no difference between the two groups in changes in temporal summation, conditional pain modulation, or Arthritis Research UK Musculoskeletal Health Questionnaire scores.
First author Sameer Akram Gohir, MSc, PhD, and colleagues wrote that the reasons for differences in outcomes between app users and controls aren’t clear. “The superior outcome in the intervention group may depend on the content and context in the app, including a combination of standardized exercises and information, as well as using a digital delivery system.”
Data gathering was cut short because of COVID-19 restrictions in the United Kingdom, as 27 patients missed their in-person follow-up visits. That was one shortcoming of the study, Dr. Kwoh noted.
“Given the caveats certainly they were able to show robust changes in terms of decreased pain, and also improvement in a variety of performance measures. Certainly this may be beneficial – we don’t know – in terms of cost-effectiveness, but it may be beneficial for insurance companies to adapt such a program,” he said, adding that future studies into the cost effectiveness of the digital platform would be in order.
“Certainly, if this program were to decrease physician visits or postpone the need for joint replacement for individuals, then it could be certainly very cost effective,” Dr. Kwoh said.
The completion rate among patients in the study – almost 90% – was “impressive,” Dr. Allen said. “However, this is a relatively short-term study, and I think an important question for future research is whether patients continue with this level of engagement for a longer period of time.”
Dr. McCurry had no relevant financial relationships to disclose. The CBT phone study received funding from the Public Health Service and the National Institute on Aging. Coauthors disclosed relationships with Campbell Alliance Group, Mapi Research Trust, and Pfizer. Dr. Gohir reported no relevant financial relationships. The study received funding from the Versus Arthritis UK Plan Center, the National Institute for Health Research Nottingham Biomedical Research Center, and Pfizer Global. The Joint Academy provided software for the study. A coauthor reported a financial relationships with Pfizer. Dr. Kwoh said that in the past year he has consulted for Express Scripts, Kolon Tissue Gene, LG Chem, and Regeneron. In the past year, he also received institutional grants for clinical trials from AbbVie, Cumberland, Eicos, Eli Lilly, GlaxoSmithKline, Mitsubishi, and Pfizer. Dr. Allen had no relevant financial relationships to disclose.
FROM JAMA INTERNAL MEDICINE AND JAMA NETWORK OPEN
Coffee lowers heart failure risk in unique study
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
FROM CIRCULATION: HEART FAILURE
Gestational diabetes carries CVD risk years later
Women who’ve had gestational diabetes are 40% more likely to develop coronary artery calcification later in life than are women haven’t, and attaining normal glycemic levels doesn’t diminish their midlife risk for atherosclerotic cardiovascular disease.
“The new finding from this study is that women with gestational diabetes had twice the risk of coronary artery calcium, compared to women who never had gestational diabetes, even though both groups attained normal blood sugar levels many years after pregnancy,” lead author Erica P. Gunderson, PhD, MS, MPH, said in an interview about a community-based prospective cohort study of young adults followed for up to 25 years, which was published in Circulation (2021 Feb 1. doi: 10.1161/CIRCULATIONAHA.120.047320).
Previous studies have reported a higher risk of heart disease in women who had gestational diabetes (GD) and later developed type 2 diabetes, but they didn’t elucidate whether that risk carried over in GD patients whose glycemic levels were normal after pregnancy. In 2018, the American College of Cardiology/American Heart Association Cholesterol Clinical Practice Guidelines specified that a history of GD increases women’s risk for coronary artery calcification (CAC).
This study analyzed data of 1,133 women ages 18-30 enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study who had no diabetes in the baseline years of 1985-1986 and had given birth at least once in the ensuing 25 years. They had glucose tolerance testing at baseline and up to five times through the study period, along with evaluation for GD status and coronary artery calcification CAC measurements at least once at years 15, 20 and 25 (2001-2011).
CARDIA enrolled 5,155 young Black and White men and women ages 18-30 from four distinct geographic areas: Birmingham, Ala.; Chicago; Minneapolis; and Oakland, Calif. About 52% of the study population was Black.
Of the women who’d given birth, 139 (12%) had GD. Their average age at follow-up was 47.6 years, and 25% of the GD patients (34) had CAC, compared with 15% (149/994) in the non-GD group.
Dr. Gunderson noted that the same relative risk for CAC applied to women who had GD and went on to develop prediabetes or were diagnosed with type 2 diabetes during follow-up.
Risks persist even in normoglycemia
In the GD group, the adjusted hazard ratio for having CAC with normoglycemia was 2.3 (95% confidence interval, 1.34-4.09). The researchers also calculated HRs for prediabetes and incident diabetes: 1.5 (95% CI, 1.06-2.24) in no-GD and 2.1 (95% CI, 1.09-4.17) for GD for prediabetes; and 2.2 (95% CI, 1.3-3.62) and 2.02 (95% CI, 0.98-4.19), respectively, for incident diabetes (P = .003).
“This means the risk of heart disease may be increased substantially in women with a history of gestational diabetes and may not diminish even if their blood-sugar levels remain normal for years later,” said Dr. Gunderson, an epidemiologist and senior research scientist at the Kaiser Permanente Northern California Division of Research in Oakland.
“The clinical implications of our findings are that women with previous GD may benefit from enhanced traditional CVD [cardiovascular disease] risk factor testing – i.e., for hypertension, dyslipidemia, and hyperinsulinemia,” Dr. Gunderson said. “Our findings also suggest that it could be beneficial to incorporate history of GD into risk calculators to improve CVD risk stratification and prevention.”
Strong findings argue for more frequent CVD screening
These study results may be the strongest data to date on the long-term effects of GD, said Prakash Deedwania, MD, professor of cardiology at the University of California, San Francisco. “It’s the strongest in the sense in that it’s sponsored, involved four different communities in different parts of the United States, enrolled individuals when they were young and followed them, and saw very few patients drop out for such a long-term study.” The study reported follow-up data on 72% of patients at 25 years, a rate Dr. Deedwania noted was “excellent.”
“Patients who have had GD should be screened aggressively – for not only diabetes, but other cardiovascular risk factors – early on to minimize the subsequent risk of cardiovascular disease is a very important point of this study,” he added. In the absence of a clinical guideline, Dr. Deedwania suggested women with GD might have screening for CV risk factors every 5-7 years depending on their risk profile, but emphasized that parameter isn’t settled.
Future research should focus on the link between GD and CVD risk, Dr. Gunderson said. “Research is needed to better characterize the severity of GD in relation to CVD outcomes, and to identify critical pregnancy-related periods to modify cardiometabolic risk.” The latter would include life-course studies across the full pregnancy continuum from preconception to lactation. “Interventions for primary prevention of CVD and the importance of modifiable lifestyle behaviors with the highest relevance to reduce both diabetes and CVD risks during the first year post partum merit increased research investigation,” she added.
Future studies might also explore the role of inflammation in the GD-CVD relationship, Dr. Deedwania said. “My hypothesis is, and it’s purely a hypothesis, that perhaps the presence of coronary artery calcification scores score in these individuals who were described as having normal glucose but who could be at risk could very well be related to the beginning of inflammation.”
Dr. Gunderson and Dr. Deedwania have no financial relationships to disclose. The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute.
Women who’ve had gestational diabetes are 40% more likely to develop coronary artery calcification later in life than are women haven’t, and attaining normal glycemic levels doesn’t diminish their midlife risk for atherosclerotic cardiovascular disease.
“The new finding from this study is that women with gestational diabetes had twice the risk of coronary artery calcium, compared to women who never had gestational diabetes, even though both groups attained normal blood sugar levels many years after pregnancy,” lead author Erica P. Gunderson, PhD, MS, MPH, said in an interview about a community-based prospective cohort study of young adults followed for up to 25 years, which was published in Circulation (2021 Feb 1. doi: 10.1161/CIRCULATIONAHA.120.047320).
Previous studies have reported a higher risk of heart disease in women who had gestational diabetes (GD) and later developed type 2 diabetes, but they didn’t elucidate whether that risk carried over in GD patients whose glycemic levels were normal after pregnancy. In 2018, the American College of Cardiology/American Heart Association Cholesterol Clinical Practice Guidelines specified that a history of GD increases women’s risk for coronary artery calcification (CAC).
This study analyzed data of 1,133 women ages 18-30 enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study who had no diabetes in the baseline years of 1985-1986 and had given birth at least once in the ensuing 25 years. They had glucose tolerance testing at baseline and up to five times through the study period, along with evaluation for GD status and coronary artery calcification CAC measurements at least once at years 15, 20 and 25 (2001-2011).
CARDIA enrolled 5,155 young Black and White men and women ages 18-30 from four distinct geographic areas: Birmingham, Ala.; Chicago; Minneapolis; and Oakland, Calif. About 52% of the study population was Black.
Of the women who’d given birth, 139 (12%) had GD. Their average age at follow-up was 47.6 years, and 25% of the GD patients (34) had CAC, compared with 15% (149/994) in the non-GD group.
Dr. Gunderson noted that the same relative risk for CAC applied to women who had GD and went on to develop prediabetes or were diagnosed with type 2 diabetes during follow-up.
Risks persist even in normoglycemia
In the GD group, the adjusted hazard ratio for having CAC with normoglycemia was 2.3 (95% confidence interval, 1.34-4.09). The researchers also calculated HRs for prediabetes and incident diabetes: 1.5 (95% CI, 1.06-2.24) in no-GD and 2.1 (95% CI, 1.09-4.17) for GD for prediabetes; and 2.2 (95% CI, 1.3-3.62) and 2.02 (95% CI, 0.98-4.19), respectively, for incident diabetes (P = .003).
“This means the risk of heart disease may be increased substantially in women with a history of gestational diabetes and may not diminish even if their blood-sugar levels remain normal for years later,” said Dr. Gunderson, an epidemiologist and senior research scientist at the Kaiser Permanente Northern California Division of Research in Oakland.
“The clinical implications of our findings are that women with previous GD may benefit from enhanced traditional CVD [cardiovascular disease] risk factor testing – i.e., for hypertension, dyslipidemia, and hyperinsulinemia,” Dr. Gunderson said. “Our findings also suggest that it could be beneficial to incorporate history of GD into risk calculators to improve CVD risk stratification and prevention.”
Strong findings argue for more frequent CVD screening
These study results may be the strongest data to date on the long-term effects of GD, said Prakash Deedwania, MD, professor of cardiology at the University of California, San Francisco. “It’s the strongest in the sense in that it’s sponsored, involved four different communities in different parts of the United States, enrolled individuals when they were young and followed them, and saw very few patients drop out for such a long-term study.” The study reported follow-up data on 72% of patients at 25 years, a rate Dr. Deedwania noted was “excellent.”
“Patients who have had GD should be screened aggressively – for not only diabetes, but other cardiovascular risk factors – early on to minimize the subsequent risk of cardiovascular disease is a very important point of this study,” he added. In the absence of a clinical guideline, Dr. Deedwania suggested women with GD might have screening for CV risk factors every 5-7 years depending on their risk profile, but emphasized that parameter isn’t settled.
Future research should focus on the link between GD and CVD risk, Dr. Gunderson said. “Research is needed to better characterize the severity of GD in relation to CVD outcomes, and to identify critical pregnancy-related periods to modify cardiometabolic risk.” The latter would include life-course studies across the full pregnancy continuum from preconception to lactation. “Interventions for primary prevention of CVD and the importance of modifiable lifestyle behaviors with the highest relevance to reduce both diabetes and CVD risks during the first year post partum merit increased research investigation,” she added.
Future studies might also explore the role of inflammation in the GD-CVD relationship, Dr. Deedwania said. “My hypothesis is, and it’s purely a hypothesis, that perhaps the presence of coronary artery calcification scores score in these individuals who were described as having normal glucose but who could be at risk could very well be related to the beginning of inflammation.”
Dr. Gunderson and Dr. Deedwania have no financial relationships to disclose. The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute.
Women who’ve had gestational diabetes are 40% more likely to develop coronary artery calcification later in life than are women haven’t, and attaining normal glycemic levels doesn’t diminish their midlife risk for atherosclerotic cardiovascular disease.
“The new finding from this study is that women with gestational diabetes had twice the risk of coronary artery calcium, compared to women who never had gestational diabetes, even though both groups attained normal blood sugar levels many years after pregnancy,” lead author Erica P. Gunderson, PhD, MS, MPH, said in an interview about a community-based prospective cohort study of young adults followed for up to 25 years, which was published in Circulation (2021 Feb 1. doi: 10.1161/CIRCULATIONAHA.120.047320).
Previous studies have reported a higher risk of heart disease in women who had gestational diabetes (GD) and later developed type 2 diabetes, but they didn’t elucidate whether that risk carried over in GD patients whose glycemic levels were normal after pregnancy. In 2018, the American College of Cardiology/American Heart Association Cholesterol Clinical Practice Guidelines specified that a history of GD increases women’s risk for coronary artery calcification (CAC).
This study analyzed data of 1,133 women ages 18-30 enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study who had no diabetes in the baseline years of 1985-1986 and had given birth at least once in the ensuing 25 years. They had glucose tolerance testing at baseline and up to five times through the study period, along with evaluation for GD status and coronary artery calcification CAC measurements at least once at years 15, 20 and 25 (2001-2011).
CARDIA enrolled 5,155 young Black and White men and women ages 18-30 from four distinct geographic areas: Birmingham, Ala.; Chicago; Minneapolis; and Oakland, Calif. About 52% of the study population was Black.
Of the women who’d given birth, 139 (12%) had GD. Their average age at follow-up was 47.6 years, and 25% of the GD patients (34) had CAC, compared with 15% (149/994) in the non-GD group.
Dr. Gunderson noted that the same relative risk for CAC applied to women who had GD and went on to develop prediabetes or were diagnosed with type 2 diabetes during follow-up.
Risks persist even in normoglycemia
In the GD group, the adjusted hazard ratio for having CAC with normoglycemia was 2.3 (95% confidence interval, 1.34-4.09). The researchers also calculated HRs for prediabetes and incident diabetes: 1.5 (95% CI, 1.06-2.24) in no-GD and 2.1 (95% CI, 1.09-4.17) for GD for prediabetes; and 2.2 (95% CI, 1.3-3.62) and 2.02 (95% CI, 0.98-4.19), respectively, for incident diabetes (P = .003).
“This means the risk of heart disease may be increased substantially in women with a history of gestational diabetes and may not diminish even if their blood-sugar levels remain normal for years later,” said Dr. Gunderson, an epidemiologist and senior research scientist at the Kaiser Permanente Northern California Division of Research in Oakland.
“The clinical implications of our findings are that women with previous GD may benefit from enhanced traditional CVD [cardiovascular disease] risk factor testing – i.e., for hypertension, dyslipidemia, and hyperinsulinemia,” Dr. Gunderson said. “Our findings also suggest that it could be beneficial to incorporate history of GD into risk calculators to improve CVD risk stratification and prevention.”
Strong findings argue for more frequent CVD screening
These study results may be the strongest data to date on the long-term effects of GD, said Prakash Deedwania, MD, professor of cardiology at the University of California, San Francisco. “It’s the strongest in the sense in that it’s sponsored, involved four different communities in different parts of the United States, enrolled individuals when they were young and followed them, and saw very few patients drop out for such a long-term study.” The study reported follow-up data on 72% of patients at 25 years, a rate Dr. Deedwania noted was “excellent.”
“Patients who have had GD should be screened aggressively – for not only diabetes, but other cardiovascular risk factors – early on to minimize the subsequent risk of cardiovascular disease is a very important point of this study,” he added. In the absence of a clinical guideline, Dr. Deedwania suggested women with GD might have screening for CV risk factors every 5-7 years depending on their risk profile, but emphasized that parameter isn’t settled.
Future research should focus on the link between GD and CVD risk, Dr. Gunderson said. “Research is needed to better characterize the severity of GD in relation to CVD outcomes, and to identify critical pregnancy-related periods to modify cardiometabolic risk.” The latter would include life-course studies across the full pregnancy continuum from preconception to lactation. “Interventions for primary prevention of CVD and the importance of modifiable lifestyle behaviors with the highest relevance to reduce both diabetes and CVD risks during the first year post partum merit increased research investigation,” she added.
Future studies might also explore the role of inflammation in the GD-CVD relationship, Dr. Deedwania said. “My hypothesis is, and it’s purely a hypothesis, that perhaps the presence of coronary artery calcification scores score in these individuals who were described as having normal glucose but who could be at risk could very well be related to the beginning of inflammation.”
Dr. Gunderson and Dr. Deedwania have no financial relationships to disclose. The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute.
FROM CIRCULATION
Left atrial appendage occlusion, DOAC comparable for AFib
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
FROM JACC CARDIOVASCULAR INTERVENTION
Asthma guidelines update FeNO, intermittent ICS use
The updated guidelines address six priority topics, including refined recommendations for the use of fractional exhaled nitric oxide (FeNO) testing, intermittent inhaled corticosteroids (ICS), long-acting muscarinic antagonists (LAMA), and bronchial thermoplasty, but notably exclude any recommendations for the use of fast-emerging biological therapy.
“Biological therapy is the major step forward,” said William W. Busse, MD, professor of allergy and immunology at the University of Wisconsin–Madison, and lead author of the previous guidelines (Bethesda, Md.: NHLBI, 2007). “It wasn’t within the scope of work, so it’s not a criticism, but it is an important shortcoming,” he said. The omission identifies the need for the next update. “This is an area that has to be dealt with,” Dr. Busse stated in an interview.
Including biologic agents would have delayed the release of the recommendations for another year or 2, wrote the expert panel working group of the NHLBI, “and this was felt to be unacceptable.” The working group, overseen by the National Asthma Education and Prevention Program Coordinating Committee, also acknowledged the update is “not a complete revision” of the 2007 guidelines.
The update provides an evidenced-based review of six key topics in asthma care, as Mary Cataletto, MD, FCCP, professor of pediatrics at New York University Long Island, Mineola, pointed out: use of FeNO, indoor allergen mitigation, use of intermittent ICS and LAMA for asthma, role of subcutaneous and sublingual immunotherapy in the treatment of allergic asthma, and the use of bronchial thermoplasty.
“It has been 13 years since the last update and substantial progress has been made since then in understanding how to best treat children and adults with asthma,” said working group member Michael Schatz, MD, MS, FCCP, an allergy specialist at Kaiser Permanente Medical Center in San Diego.
According to Dr. Schatz, the most important updated recommendations are:
- Conditional recommendation for the use of ICS in children aged infant to 4 years with recurrent wheezing with respiratory infections.
- Use of combination ICS-formoterol for maintenance and to relieve flares in patients with moderate to severe asthma.
- Addition of the LAMA inhaled bronchodilator as add-on therapy for severe asthma not controlled by long-acting beta-agonist (LABA)/ICS combination medications.
Another important update, Dr. Cataletto said, is “shared decision-making among members of asthma teams in order to improve asthma care across all age groups.”
In all, the update includes 19 recommendations in the six subject areas. Each recommendation is notated with two values: its strength, either strong or conditional, and the certainty of evidence behind it, either low, moderate, or high. For example, the recommendation for ICS in young children that Dr. Schatz referred to has a conditional strength of recommendation with moderate certainty of evidence.
Using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) methodology to determine strength of recommendation is a notable innovation of the latest guidelines, Dr. Busse noted.
Recommendations (strength of recommendation/certainty of evidence) include:
- Use of FeNO in children and adults when the asthma diagnosis is uncertain (conditional/moderate) or in those with allergic asthma and an uncertain course of management (conditional/low).
- Avoid standalone FeNO to evaluate asthma control or the likelihood or severity of future exacerbations, or for in infants to 4-year-olds with recurrent wheezing (strong/low for both).
- Avoid allergen mitigation in routine asthma management for patients who don’t have sensitivity to specific indoor allergens (conditional/low).
- Multicomponent allergen-specific mitigation when specific allergen sensitivity has been identified and pest management alone for symptoms related to specific pest exposure (conditional/low for both).
- Impermeable bedding covers should be part of a multicomponent mitigation strategy, not as a standalone tool, for patients with asthma and dust mite sensitivity (conditional/moderate).
- Daily ICS at onset of a respiratory tract infection along with as-needed short-acting beta-agonists in children aged 4 years and younger with recurrent wheezing but no wheezing between infections rather than as-needed standalone SABA (conditional/high).
- For adults and children aged 12 years and older with mild persistent asthma, either daily low-dose ICS with as-needed SABA or as-needed ICS and SABA concomitantly (conditional/moderate).
- Avoid short-course increased ICS dosing for patients aged 4 years and older with good adherence to daily ICS therapy (conditional/low).
- For patients aged 4 years and older with moderate to severe persistent asthma, a preference for combined ICS-formoterol inhaler over higher dose ICS daily and intermittent SABA or daily ICS-LABA with intermittent SABA (strong/high [aged 12 years and older]; moderate [aged 4-11 years]).
- A preference for combined ICS-formoterol for both daily and relief therapy for patients 12 years and older with severe persistent asthma over higher-dose ICS-LABA daily and intermittent SABA (conditional/high).
- A preference for adding LABA rather than LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma (conditional/moderate).
- If LABA isn’t used, add LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma rather than continuing the same dose of ICS alone (conditional/moderate).
- In those same patients already on combined ICS-LABA therapy, add LAMA rather than continuing the same dose of ICS-LABA (conditional/moderate).
- Use subcutaneous immunotherapy as a potential adjunct to standard drug therapy in patients aged 5 years and older with mild to moderate allergic asthma when their asthma is controlled on immunotherapy (conditional/moderate).
- Avoid sublingual immunotherapy in patients with persistent allergic asthma (conditional/moderate).
- Avoid bronchial thermoplasty in those 18 years and older with persistent asthma, but consider it in patients who can accept the short-term worsening symptoms or unknown long-term side effects in exchange for the potential benefits (conditional/moderate).
One of the key elements of the guidelines is the use of the SMART (single maintenance and reliever therapy) approach to evaluate the comparative effectiveness of intermittent ICS with formoterol, Dr. Busse noted. “I think that’s a very significant advance. The literature is replete with evidence to support this. Secondly, it really makes life convenient for patients; you have one inhaler.”
The recommendation on SABA use is also significant, Dr. Busse said. “Data have emerged to suggest that if you’re having a need for one of these rescue medications, it’s due to an increase in inflammation in the lower airway, and you want to give an ICS which will act on the inflammation along with the bronchodilator. That’s a new concept, and it’s a very significant step forward.”
Dr. Schatz disclosed financial relationships with Merck, Teva, and ALK-Abello, but was recused from the writing, discussion, and voting related to the immunotherapy recommendation. Dr. Cataletto and Dr. Busse have no relevant relationships to disclose.
SOURCE: Schatz M et al. J Allergy Clin Immunol. 2020;146:1217-70.
The updated guidelines address six priority topics, including refined recommendations for the use of fractional exhaled nitric oxide (FeNO) testing, intermittent inhaled corticosteroids (ICS), long-acting muscarinic antagonists (LAMA), and bronchial thermoplasty, but notably exclude any recommendations for the use of fast-emerging biological therapy.
“Biological therapy is the major step forward,” said William W. Busse, MD, professor of allergy and immunology at the University of Wisconsin–Madison, and lead author of the previous guidelines (Bethesda, Md.: NHLBI, 2007). “It wasn’t within the scope of work, so it’s not a criticism, but it is an important shortcoming,” he said. The omission identifies the need for the next update. “This is an area that has to be dealt with,” Dr. Busse stated in an interview.
Including biologic agents would have delayed the release of the recommendations for another year or 2, wrote the expert panel working group of the NHLBI, “and this was felt to be unacceptable.” The working group, overseen by the National Asthma Education and Prevention Program Coordinating Committee, also acknowledged the update is “not a complete revision” of the 2007 guidelines.
The update provides an evidenced-based review of six key topics in asthma care, as Mary Cataletto, MD, FCCP, professor of pediatrics at New York University Long Island, Mineola, pointed out: use of FeNO, indoor allergen mitigation, use of intermittent ICS and LAMA for asthma, role of subcutaneous and sublingual immunotherapy in the treatment of allergic asthma, and the use of bronchial thermoplasty.
“It has been 13 years since the last update and substantial progress has been made since then in understanding how to best treat children and adults with asthma,” said working group member Michael Schatz, MD, MS, FCCP, an allergy specialist at Kaiser Permanente Medical Center in San Diego.
According to Dr. Schatz, the most important updated recommendations are:
- Conditional recommendation for the use of ICS in children aged infant to 4 years with recurrent wheezing with respiratory infections.
- Use of combination ICS-formoterol for maintenance and to relieve flares in patients with moderate to severe asthma.
- Addition of the LAMA inhaled bronchodilator as add-on therapy for severe asthma not controlled by long-acting beta-agonist (LABA)/ICS combination medications.
Another important update, Dr. Cataletto said, is “shared decision-making among members of asthma teams in order to improve asthma care across all age groups.”
In all, the update includes 19 recommendations in the six subject areas. Each recommendation is notated with two values: its strength, either strong or conditional, and the certainty of evidence behind it, either low, moderate, or high. For example, the recommendation for ICS in young children that Dr. Schatz referred to has a conditional strength of recommendation with moderate certainty of evidence.
Using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) methodology to determine strength of recommendation is a notable innovation of the latest guidelines, Dr. Busse noted.
Recommendations (strength of recommendation/certainty of evidence) include:
- Use of FeNO in children and adults when the asthma diagnosis is uncertain (conditional/moderate) or in those with allergic asthma and an uncertain course of management (conditional/low).
- Avoid standalone FeNO to evaluate asthma control or the likelihood or severity of future exacerbations, or for in infants to 4-year-olds with recurrent wheezing (strong/low for both).
- Avoid allergen mitigation in routine asthma management for patients who don’t have sensitivity to specific indoor allergens (conditional/low).
- Multicomponent allergen-specific mitigation when specific allergen sensitivity has been identified and pest management alone for symptoms related to specific pest exposure (conditional/low for both).
- Impermeable bedding covers should be part of a multicomponent mitigation strategy, not as a standalone tool, for patients with asthma and dust mite sensitivity (conditional/moderate).
- Daily ICS at onset of a respiratory tract infection along with as-needed short-acting beta-agonists in children aged 4 years and younger with recurrent wheezing but no wheezing between infections rather than as-needed standalone SABA (conditional/high).
- For adults and children aged 12 years and older with mild persistent asthma, either daily low-dose ICS with as-needed SABA or as-needed ICS and SABA concomitantly (conditional/moderate).
- Avoid short-course increased ICS dosing for patients aged 4 years and older with good adherence to daily ICS therapy (conditional/low).
- For patients aged 4 years and older with moderate to severe persistent asthma, a preference for combined ICS-formoterol inhaler over higher dose ICS daily and intermittent SABA or daily ICS-LABA with intermittent SABA (strong/high [aged 12 years and older]; moderate [aged 4-11 years]).
- A preference for combined ICS-formoterol for both daily and relief therapy for patients 12 years and older with severe persistent asthma over higher-dose ICS-LABA daily and intermittent SABA (conditional/high).
- A preference for adding LABA rather than LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma (conditional/moderate).
- If LABA isn’t used, add LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma rather than continuing the same dose of ICS alone (conditional/moderate).
- In those same patients already on combined ICS-LABA therapy, add LAMA rather than continuing the same dose of ICS-LABA (conditional/moderate).
- Use subcutaneous immunotherapy as a potential adjunct to standard drug therapy in patients aged 5 years and older with mild to moderate allergic asthma when their asthma is controlled on immunotherapy (conditional/moderate).
- Avoid sublingual immunotherapy in patients with persistent allergic asthma (conditional/moderate).
- Avoid bronchial thermoplasty in those 18 years and older with persistent asthma, but consider it in patients who can accept the short-term worsening symptoms or unknown long-term side effects in exchange for the potential benefits (conditional/moderate).
One of the key elements of the guidelines is the use of the SMART (single maintenance and reliever therapy) approach to evaluate the comparative effectiveness of intermittent ICS with formoterol, Dr. Busse noted. “I think that’s a very significant advance. The literature is replete with evidence to support this. Secondly, it really makes life convenient for patients; you have one inhaler.”
The recommendation on SABA use is also significant, Dr. Busse said. “Data have emerged to suggest that if you’re having a need for one of these rescue medications, it’s due to an increase in inflammation in the lower airway, and you want to give an ICS which will act on the inflammation along with the bronchodilator. That’s a new concept, and it’s a very significant step forward.”
Dr. Schatz disclosed financial relationships with Merck, Teva, and ALK-Abello, but was recused from the writing, discussion, and voting related to the immunotherapy recommendation. Dr. Cataletto and Dr. Busse have no relevant relationships to disclose.
SOURCE: Schatz M et al. J Allergy Clin Immunol. 2020;146:1217-70.
The updated guidelines address six priority topics, including refined recommendations for the use of fractional exhaled nitric oxide (FeNO) testing, intermittent inhaled corticosteroids (ICS), long-acting muscarinic antagonists (LAMA), and bronchial thermoplasty, but notably exclude any recommendations for the use of fast-emerging biological therapy.
“Biological therapy is the major step forward,” said William W. Busse, MD, professor of allergy and immunology at the University of Wisconsin–Madison, and lead author of the previous guidelines (Bethesda, Md.: NHLBI, 2007). “It wasn’t within the scope of work, so it’s not a criticism, but it is an important shortcoming,” he said. The omission identifies the need for the next update. “This is an area that has to be dealt with,” Dr. Busse stated in an interview.
Including biologic agents would have delayed the release of the recommendations for another year or 2, wrote the expert panel working group of the NHLBI, “and this was felt to be unacceptable.” The working group, overseen by the National Asthma Education and Prevention Program Coordinating Committee, also acknowledged the update is “not a complete revision” of the 2007 guidelines.
The update provides an evidenced-based review of six key topics in asthma care, as Mary Cataletto, MD, FCCP, professor of pediatrics at New York University Long Island, Mineola, pointed out: use of FeNO, indoor allergen mitigation, use of intermittent ICS and LAMA for asthma, role of subcutaneous and sublingual immunotherapy in the treatment of allergic asthma, and the use of bronchial thermoplasty.
“It has been 13 years since the last update and substantial progress has been made since then in understanding how to best treat children and adults with asthma,” said working group member Michael Schatz, MD, MS, FCCP, an allergy specialist at Kaiser Permanente Medical Center in San Diego.
According to Dr. Schatz, the most important updated recommendations are:
- Conditional recommendation for the use of ICS in children aged infant to 4 years with recurrent wheezing with respiratory infections.
- Use of combination ICS-formoterol for maintenance and to relieve flares in patients with moderate to severe asthma.
- Addition of the LAMA inhaled bronchodilator as add-on therapy for severe asthma not controlled by long-acting beta-agonist (LABA)/ICS combination medications.
Another important update, Dr. Cataletto said, is “shared decision-making among members of asthma teams in order to improve asthma care across all age groups.”
In all, the update includes 19 recommendations in the six subject areas. Each recommendation is notated with two values: its strength, either strong or conditional, and the certainty of evidence behind it, either low, moderate, or high. For example, the recommendation for ICS in young children that Dr. Schatz referred to has a conditional strength of recommendation with moderate certainty of evidence.
Using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) methodology to determine strength of recommendation is a notable innovation of the latest guidelines, Dr. Busse noted.
Recommendations (strength of recommendation/certainty of evidence) include:
- Use of FeNO in children and adults when the asthma diagnosis is uncertain (conditional/moderate) or in those with allergic asthma and an uncertain course of management (conditional/low).
- Avoid standalone FeNO to evaluate asthma control or the likelihood or severity of future exacerbations, or for in infants to 4-year-olds with recurrent wheezing (strong/low for both).
- Avoid allergen mitigation in routine asthma management for patients who don’t have sensitivity to specific indoor allergens (conditional/low).
- Multicomponent allergen-specific mitigation when specific allergen sensitivity has been identified and pest management alone for symptoms related to specific pest exposure (conditional/low for both).
- Impermeable bedding covers should be part of a multicomponent mitigation strategy, not as a standalone tool, for patients with asthma and dust mite sensitivity (conditional/moderate).
- Daily ICS at onset of a respiratory tract infection along with as-needed short-acting beta-agonists in children aged 4 years and younger with recurrent wheezing but no wheezing between infections rather than as-needed standalone SABA (conditional/high).
- For adults and children aged 12 years and older with mild persistent asthma, either daily low-dose ICS with as-needed SABA or as-needed ICS and SABA concomitantly (conditional/moderate).
- Avoid short-course increased ICS dosing for patients aged 4 years and older with good adherence to daily ICS therapy (conditional/low).
- For patients aged 4 years and older with moderate to severe persistent asthma, a preference for combined ICS-formoterol inhaler over higher dose ICS daily and intermittent SABA or daily ICS-LABA with intermittent SABA (strong/high [aged 12 years and older]; moderate [aged 4-11 years]).
- A preference for combined ICS-formoterol for both daily and relief therapy for patients 12 years and older with severe persistent asthma over higher-dose ICS-LABA daily and intermittent SABA (conditional/high).
- A preference for adding LABA rather than LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma (conditional/moderate).
- If LABA isn’t used, add LAMA to ICS in patients aged 12 years and older with uncontrolled persistent asthma rather than continuing the same dose of ICS alone (conditional/moderate).
- In those same patients already on combined ICS-LABA therapy, add LAMA rather than continuing the same dose of ICS-LABA (conditional/moderate).
- Use subcutaneous immunotherapy as a potential adjunct to standard drug therapy in patients aged 5 years and older with mild to moderate allergic asthma when their asthma is controlled on immunotherapy (conditional/moderate).
- Avoid sublingual immunotherapy in patients with persistent allergic asthma (conditional/moderate).
- Avoid bronchial thermoplasty in those 18 years and older with persistent asthma, but consider it in patients who can accept the short-term worsening symptoms or unknown long-term side effects in exchange for the potential benefits (conditional/moderate).
One of the key elements of the guidelines is the use of the SMART (single maintenance and reliever therapy) approach to evaluate the comparative effectiveness of intermittent ICS with formoterol, Dr. Busse noted. “I think that’s a very significant advance. The literature is replete with evidence to support this. Secondly, it really makes life convenient for patients; you have one inhaler.”
The recommendation on SABA use is also significant, Dr. Busse said. “Data have emerged to suggest that if you’re having a need for one of these rescue medications, it’s due to an increase in inflammation in the lower airway, and you want to give an ICS which will act on the inflammation along with the bronchodilator. That’s a new concept, and it’s a very significant step forward.”
Dr. Schatz disclosed financial relationships with Merck, Teva, and ALK-Abello, but was recused from the writing, discussion, and voting related to the immunotherapy recommendation. Dr. Cataletto and Dr. Busse have no relevant relationships to disclose.
SOURCE: Schatz M et al. J Allergy Clin Immunol. 2020;146:1217-70.
FROM THE JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY
Sac/val heart failure benefit extends to diabetes patients
The beneficial effects of sacubitril/valsartan on reverse cardiac remodeling in patients with heart failure and reduced ejection fraction have been well established, but those benefits haven’t been as clearly demonstrated to carry over to HFrEF patients who also have type 2 diabetes mellitus (T2DM).
Now, a post-hoc analysis of a pivotal clinical trial reports that those benefits do extend to patients with HFrEF and T2DM.
“It’s really not about a Sophie’s choice of whether you give this or that drug in these patients,” said corresponding author Javed Butler, MD, MPH, MBA. “We really ought to be giving all of these drugs – the angiotensin receptor neprilysin inhibitors (ARNIs) and sodium-glucose transporter 2 (SGLT-2) inhibitors – to our patients for the best outcomes.”
The post-hoc analysis, published in JACC: Heart Failure, evaluated 361 patients with T2DM who were enrolled in the PROVE-HF trial of sac/val therapy for HF, published in JAMA.
PROVE-HF evaluated biomarkers, myocardial remodeling, and outcomes through a year of treatment with sac/val. The primary endpoint was the level of changes in natriuretic peptide (NT-proBNP) concentrations, left-ventricle ejection fraction (LVEF) and overall Kansas City Cardiomyopathy Questionnaire (KCCQ)-23 scores through 12 months of treatment.
The post hoc study reported that baseline NT-proBNP concentrations were higher in the DM patients (854 pg/mL vs. 706 pg/mL), but at 12 months those levels were 513 and 441 pg/mL, respectively.
LVEF changed similarly from baseline to 12 months in both groups: from 28.3% to 37% in the DM patients and from 28.1% to 38.34% in non-DM patients. Overall KCCQ-23 scores improved similarly in both groups, but longitudinal analyses found modestly higher gains in the T2DM group, 9.3 vs. 8.6 points (P = .07).
“The real reason I wanted to do this study is that I’m a huge fan of all the SGLT-2 inhibitors, and I’m very involved in those trials, and there is right now so much momentum behind SGLT-2 inhibitors that I don’t want people to forget that ARNI is still the base therapy for HF,” said Dr. Butler, chair of cardiovascular research and the department of medicine at the University of Mississippi in Jackson.
He noted that the size of the diabetes cohort in PROVE-HF “is a nonissue” for evaluating power of the post hoc analysis because it tracked key measures in the study population continuously at eight intervals over the 12 months.
The analysis further demonstrates the synergistic effects of ARNI and SGLT-2 inhibitors in patients with T2DM and HF that were also reported in the PARADIGM-HF study, Dr. Butler said.
“We have sort of moved on, saying that SGLT-2 inhibitors have a benefit on the heart, but the reverse is also true: ARNIs are still heart failure drugs, and we don’t think of them as diabetes drugs, but the PARADIGM-HF data showed that there was a substantial reduction in hemoglobin A1c in those who had diabetes,” he said.
The researchers noted that an absence of a control group may contribute to an overestimation of reverse cardiac remodeling in the T2DM patients, and that the PROVE-HF study wasn’t prospectively powered to delineate differences in how sac/val therapy affected patients with or without diabetes. “Future investigations seeking to evaluate differences by T2DM status after sacubitril/valsartan initiation may use our findings to plan prospective sample sizes,” the researchers wrote.
Dr. Butler disclosed financial relationships with Abbott, Amgen, Array, AstraZeneca, Bayer, Boehringer Ingelheim, CVRx, Eli Lilly, G3 Pharmaceutical, Impulse Dynamics, Innolife, Janssen, Luitpold, Medtronic, Merck, Novartis, Novo Nordisk, Relypsa, Sequana, StealthPeptide and Vifor. Lead author Muhammad Shahzeb Khan, MD, MSc, a professor at the University of Mississippi, has no relevant financial relationships to disclose.
SOURCE: Kahn MS et al. JACC: HF. 2020 Dec 9. doi: 10.1016/j.jchf.2020.09.014.
The beneficial effects of sacubitril/valsartan on reverse cardiac remodeling in patients with heart failure and reduced ejection fraction have been well established, but those benefits haven’t been as clearly demonstrated to carry over to HFrEF patients who also have type 2 diabetes mellitus (T2DM).
Now, a post-hoc analysis of a pivotal clinical trial reports that those benefits do extend to patients with HFrEF and T2DM.
“It’s really not about a Sophie’s choice of whether you give this or that drug in these patients,” said corresponding author Javed Butler, MD, MPH, MBA. “We really ought to be giving all of these drugs – the angiotensin receptor neprilysin inhibitors (ARNIs) and sodium-glucose transporter 2 (SGLT-2) inhibitors – to our patients for the best outcomes.”
The post-hoc analysis, published in JACC: Heart Failure, evaluated 361 patients with T2DM who were enrolled in the PROVE-HF trial of sac/val therapy for HF, published in JAMA.
PROVE-HF evaluated biomarkers, myocardial remodeling, and outcomes through a year of treatment with sac/val. The primary endpoint was the level of changes in natriuretic peptide (NT-proBNP) concentrations, left-ventricle ejection fraction (LVEF) and overall Kansas City Cardiomyopathy Questionnaire (KCCQ)-23 scores through 12 months of treatment.
The post hoc study reported that baseline NT-proBNP concentrations were higher in the DM patients (854 pg/mL vs. 706 pg/mL), but at 12 months those levels were 513 and 441 pg/mL, respectively.
LVEF changed similarly from baseline to 12 months in both groups: from 28.3% to 37% in the DM patients and from 28.1% to 38.34% in non-DM patients. Overall KCCQ-23 scores improved similarly in both groups, but longitudinal analyses found modestly higher gains in the T2DM group, 9.3 vs. 8.6 points (P = .07).
“The real reason I wanted to do this study is that I’m a huge fan of all the SGLT-2 inhibitors, and I’m very involved in those trials, and there is right now so much momentum behind SGLT-2 inhibitors that I don’t want people to forget that ARNI is still the base therapy for HF,” said Dr. Butler, chair of cardiovascular research and the department of medicine at the University of Mississippi in Jackson.
He noted that the size of the diabetes cohort in PROVE-HF “is a nonissue” for evaluating power of the post hoc analysis because it tracked key measures in the study population continuously at eight intervals over the 12 months.
The analysis further demonstrates the synergistic effects of ARNI and SGLT-2 inhibitors in patients with T2DM and HF that were also reported in the PARADIGM-HF study, Dr. Butler said.
“We have sort of moved on, saying that SGLT-2 inhibitors have a benefit on the heart, but the reverse is also true: ARNIs are still heart failure drugs, and we don’t think of them as diabetes drugs, but the PARADIGM-HF data showed that there was a substantial reduction in hemoglobin A1c in those who had diabetes,” he said.
The researchers noted that an absence of a control group may contribute to an overestimation of reverse cardiac remodeling in the T2DM patients, and that the PROVE-HF study wasn’t prospectively powered to delineate differences in how sac/val therapy affected patients with or without diabetes. “Future investigations seeking to evaluate differences by T2DM status after sacubitril/valsartan initiation may use our findings to plan prospective sample sizes,” the researchers wrote.
Dr. Butler disclosed financial relationships with Abbott, Amgen, Array, AstraZeneca, Bayer, Boehringer Ingelheim, CVRx, Eli Lilly, G3 Pharmaceutical, Impulse Dynamics, Innolife, Janssen, Luitpold, Medtronic, Merck, Novartis, Novo Nordisk, Relypsa, Sequana, StealthPeptide and Vifor. Lead author Muhammad Shahzeb Khan, MD, MSc, a professor at the University of Mississippi, has no relevant financial relationships to disclose.
SOURCE: Kahn MS et al. JACC: HF. 2020 Dec 9. doi: 10.1016/j.jchf.2020.09.014.
The beneficial effects of sacubitril/valsartan on reverse cardiac remodeling in patients with heart failure and reduced ejection fraction have been well established, but those benefits haven’t been as clearly demonstrated to carry over to HFrEF patients who also have type 2 diabetes mellitus (T2DM).
Now, a post-hoc analysis of a pivotal clinical trial reports that those benefits do extend to patients with HFrEF and T2DM.
“It’s really not about a Sophie’s choice of whether you give this or that drug in these patients,” said corresponding author Javed Butler, MD, MPH, MBA. “We really ought to be giving all of these drugs – the angiotensin receptor neprilysin inhibitors (ARNIs) and sodium-glucose transporter 2 (SGLT-2) inhibitors – to our patients for the best outcomes.”
The post-hoc analysis, published in JACC: Heart Failure, evaluated 361 patients with T2DM who were enrolled in the PROVE-HF trial of sac/val therapy for HF, published in JAMA.
PROVE-HF evaluated biomarkers, myocardial remodeling, and outcomes through a year of treatment with sac/val. The primary endpoint was the level of changes in natriuretic peptide (NT-proBNP) concentrations, left-ventricle ejection fraction (LVEF) and overall Kansas City Cardiomyopathy Questionnaire (KCCQ)-23 scores through 12 months of treatment.
The post hoc study reported that baseline NT-proBNP concentrations were higher in the DM patients (854 pg/mL vs. 706 pg/mL), but at 12 months those levels were 513 and 441 pg/mL, respectively.
LVEF changed similarly from baseline to 12 months in both groups: from 28.3% to 37% in the DM patients and from 28.1% to 38.34% in non-DM patients. Overall KCCQ-23 scores improved similarly in both groups, but longitudinal analyses found modestly higher gains in the T2DM group, 9.3 vs. 8.6 points (P = .07).
“The real reason I wanted to do this study is that I’m a huge fan of all the SGLT-2 inhibitors, and I’m very involved in those trials, and there is right now so much momentum behind SGLT-2 inhibitors that I don’t want people to forget that ARNI is still the base therapy for HF,” said Dr. Butler, chair of cardiovascular research and the department of medicine at the University of Mississippi in Jackson.
He noted that the size of the diabetes cohort in PROVE-HF “is a nonissue” for evaluating power of the post hoc analysis because it tracked key measures in the study population continuously at eight intervals over the 12 months.
The analysis further demonstrates the synergistic effects of ARNI and SGLT-2 inhibitors in patients with T2DM and HF that were also reported in the PARADIGM-HF study, Dr. Butler said.
“We have sort of moved on, saying that SGLT-2 inhibitors have a benefit on the heart, but the reverse is also true: ARNIs are still heart failure drugs, and we don’t think of them as diabetes drugs, but the PARADIGM-HF data showed that there was a substantial reduction in hemoglobin A1c in those who had diabetes,” he said.
The researchers noted that an absence of a control group may contribute to an overestimation of reverse cardiac remodeling in the T2DM patients, and that the PROVE-HF study wasn’t prospectively powered to delineate differences in how sac/val therapy affected patients with or without diabetes. “Future investigations seeking to evaluate differences by T2DM status after sacubitril/valsartan initiation may use our findings to plan prospective sample sizes,” the researchers wrote.
Dr. Butler disclosed financial relationships with Abbott, Amgen, Array, AstraZeneca, Bayer, Boehringer Ingelheim, CVRx, Eli Lilly, G3 Pharmaceutical, Impulse Dynamics, Innolife, Janssen, Luitpold, Medtronic, Merck, Novartis, Novo Nordisk, Relypsa, Sequana, StealthPeptide and Vifor. Lead author Muhammad Shahzeb Khan, MD, MSc, a professor at the University of Mississippi, has no relevant financial relationships to disclose.
SOURCE: Kahn MS et al. JACC: HF. 2020 Dec 9. doi: 10.1016/j.jchf.2020.09.014.
FROM JACC: HEART FAILURE
Infant’s COVID-19–related myocardial injury reversed
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
FROM JACC CASE REPORTS
Key clinical point: Children presenting with COVID-19 should be tested for heart failure.
Major finding: A 2-month-old infant with COVID-19 had acute but reversible myocardial injury.
Study details: Single case report.
Disclosures: Dr. Sharma, MD, has no relevant financial relationships to disclose.
Source: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
New HCM guidelines make shared decision-making top priority
Greater involvement of the patient and family in decision-making, clarity on the role of genetic testing and parameters for team-oriented care, and use of high-volume specialty centers are cornerstones of the first update in almost a decade of the American Heart Association/American College of Cardiology guideline for patients with hypertrophic cardiomyopathy (HCM).
The update lists 133 recommendations for HCM care in six categories: shared decision-making; role of high-volume HCM centers; diagnosis, initial evaluation, and follow-up; risk assessment and prevention of sudden cardiac death (SCD); management of HCM; and lifestyle considerations for patients.
“The guideline puts the patient front and center in the shared decision-making process and emphasizes the importance of incorporating patient’s lifestyle choices and preferences when making complex, life-altering decisions,” writing committee vice chair Seema Mital, MD, of the University of Toronto and the Hospital for Sick Children, also in Toronto, said in an interview.
The fully updated guideline, authored by a joint committee of the AHA and ACC with input from other specialty societies, has been published online in the Journal of the American College of Cardiology. It replaces the 2011 guideline.
Another key component of the update is the strong recommendation to utilize multidisciplinary care, said Matthew W. Martinez, MD, a writing committee member and sports cardiologists at Morristown (N.J.) Medical Center. “This is not only as a part of shared decision-making, but really in care for the patients,” he said, “that there’s a level of expertise that is provided by centers of excellence who handle HCM, and we did lay out some recommendations with regards to surgery, imaging, interventionists, and management with electrophysiology, and the care of athletes with potential for HCM and pregnant women.”
The update ranks recommendations by class of recommendation (COR), ranging from strong benefit much greater than risk to harm with risk exceeding benefit, and level of evidence (LOE). The recommendation for shared decision making, for example, carries at COR of 1, the highest rating, and a mid-level LOE of B-NR, meaning from nonrandomized studies. Patients who need septal reduction therapy (SRT) should be referred to a comprehensive or primary HCM center – a recommendation with a COR of 1 but an LOE of C-LD, meaning there are limited data.
From diagnosis to follow-up
The most extensive list of recommendations falls under the category covering diagnosis, initial evaluation and follow-up. They include a three-generation family history as part of the initial diagnostic assessment (COR, 1; LOE, B-NR), high-level recommendations for use of transthoracic echocardiogram in the initial work-up, every 1 or 2 years or when the patient’s status changes in confirmed cases, as well as parameters for using other imaging and diagnostic tests. Cardiovascular MRI, for example, is indicated when echocardiography is inconclusive (COR, 1; LOE, B-NR) and in other scenarios. When echocardiography is inconclusive but cardiac MRI isn’t available, cardiac CT is an option, albeit at a lower level of evidence (COR, 2b; LOE, C-LD).
Heart rhythm assessment has a high level of recommendation in multiple scenarios, even in first-degree relatives of HCM patients. Invasive hemodynamic assessment is in order for candidates of SRT whose left ventricular (LV) outflow tract obstruction status is unknown. This category also sets parameters for angiography, and exercise stress testing.
The most extensive recommendations for diagnosis and follow-up cover genetic testing; it consists of nine high-level recommendations.
“The guideline highlights not only the importance of genetic testing of an affected patient and genetic screening of family members, but also emphasizes ongoing reassessment of variant classification as this may evolve with time and change how we recommend ongoing family screening,” Dr. Mital noted.
“The guideline proposes initiating screening of family members at the earliest regardless of age given HCM can manifest at any age in affected families,” she added.
The guideline notes that the usefulness of genetic testing to evaluate the risk of sudden cardiac death (SCD) is uncertain. There’s even guidance for implementing those test results. Further testing is recommended for patients who are genotype positive and phenotype negative for HCM (COR, 1; LOE, B-NR). Those same patients may participate in competitive sports (COR, 2a; LOE, C-LD), but a pacemaker isn’t recommended as a primary prevention (COR, 3 [no benefit]; LOE, B-NR).
Risk evaluation and prevention
For SCD risk evaluation and prevention, the guideline spells out five components for the initial and follow-up evaluations (COR, 1; LOE, B-NR). That includes maximal LV wall thickness, ejection fraction, and LV apical aneurysm. The section include multiple recommendations for patient selection for placement of an implantable cardioverter-defibrillator (ICD). For example, it’s recommended for patient’s who’ve had a heart attack or sustained ventricular tachycardia (COR, 1; LOE, B-NR), but not so much for patients without risk factors or for participating in sports (COR, 3 [harm]; LOE, B-NR). The guideline even provides recommendations for selecting an ICD.
Management recommendations address when medical therapy is indicated, including which therapies are indicated for specific scenarios, as well as higher level interventions such as SRT for severely symptomatic patients with obstructive HCM (COR, 2b; LOE, C-LD) and surgical myectomy with ablation in patients with HCM and atrial fibrillation (COR, 2a; LOE, B-NR). This section also provides recommendations for managing patients with HCM and ventricular arrhythmias or advanced heart failure.
The guideline also includes a host of lifestyle considerations. Mild to moderate exercise is beneficial (COR, 1; LOE, B-NR), but athletes with HCM should consult with an “expert provider” (COR, 1; LOE, C, meaning based on expert opinion). Truck drivers, pilots and people who do strenuous physical labor with HCM should meet specific standards.
These recommendations again emphasize the role of shared decision-making, said Dr. Martinez. “It’s not a cookie-cutter discussion. It is taking all of the information, incorporating what the patient’s needs are, and then making sure you appropriately tell them what are the risks of exercising and not exercising. I have as many discussions through the day about what the risks of exercise are as I do the risks of not exercising.”
Refining nomenclature, pathophysiology
The writing committee addressed the nomenclature for HCM. The use of HCM to describe increased LV wall thickness linked to systemic diseases or secondary to LV hypertrophy “can lead to confusion,” the committee stated, so other cardiac or systemic causes of LV hypertrophy shouldn’t be labeled HCM. Other etiologies can cause secondary LV hypertrophy that can overlap with HCM; clinical markers and testing can help differentiate these mimickers from HCM. When echocardiography is inconclusive, cardiovascular MRI is indicated (COR, 1; LOE, B-NR).
The guideline update also provides clarity on the pathophysiology of HCM: It consists of dynamic LV outflow tract obstruction, mitral regurgitation, diastolic dysfunction, myocardial ischemia, arrhythmias, or autonomic dysfunction. “For a given patient with HCM, the clinical outcome may be dominated by one of these components or may be the result of a complex interplay,” the guideline states. The clinical evaluation should consider all these conditions.
This update also provides “clear separation” between care of HCM with and without obstruction, Dr. Martinez said. “The role of advanced therapies and referrals with advanced treatment options such as heart transplantation or CRT therapy in this group is different than before, recognizing that people with obstruction have symptoms that may be similar to those without obstruction, and the individual should be [thoroughly] investigated to make sure that you can discern between those two groups to make appropriate recommendations.”
The guideline was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, American Society of Echocardiography, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society for Cardiovascular Magnetic Resonance. It’s also been endorsed by the Pediatric & Congenital Electrophysiology Society.
Dr. Mital and Dr. Martinez have no relevant financial relationships to disclose.
SOURCE: Mital S et al. J Am Coll Cardiol. 2020 Nov 20. doi: 10.1016/j.jacc.2020.08.044.
Greater involvement of the patient and family in decision-making, clarity on the role of genetic testing and parameters for team-oriented care, and use of high-volume specialty centers are cornerstones of the first update in almost a decade of the American Heart Association/American College of Cardiology guideline for patients with hypertrophic cardiomyopathy (HCM).
The update lists 133 recommendations for HCM care in six categories: shared decision-making; role of high-volume HCM centers; diagnosis, initial evaluation, and follow-up; risk assessment and prevention of sudden cardiac death (SCD); management of HCM; and lifestyle considerations for patients.
“The guideline puts the patient front and center in the shared decision-making process and emphasizes the importance of incorporating patient’s lifestyle choices and preferences when making complex, life-altering decisions,” writing committee vice chair Seema Mital, MD, of the University of Toronto and the Hospital for Sick Children, also in Toronto, said in an interview.
The fully updated guideline, authored by a joint committee of the AHA and ACC with input from other specialty societies, has been published online in the Journal of the American College of Cardiology. It replaces the 2011 guideline.
Another key component of the update is the strong recommendation to utilize multidisciplinary care, said Matthew W. Martinez, MD, a writing committee member and sports cardiologists at Morristown (N.J.) Medical Center. “This is not only as a part of shared decision-making, but really in care for the patients,” he said, “that there’s a level of expertise that is provided by centers of excellence who handle HCM, and we did lay out some recommendations with regards to surgery, imaging, interventionists, and management with electrophysiology, and the care of athletes with potential for HCM and pregnant women.”
The update ranks recommendations by class of recommendation (COR), ranging from strong benefit much greater than risk to harm with risk exceeding benefit, and level of evidence (LOE). The recommendation for shared decision making, for example, carries at COR of 1, the highest rating, and a mid-level LOE of B-NR, meaning from nonrandomized studies. Patients who need septal reduction therapy (SRT) should be referred to a comprehensive or primary HCM center – a recommendation with a COR of 1 but an LOE of C-LD, meaning there are limited data.
From diagnosis to follow-up
The most extensive list of recommendations falls under the category covering diagnosis, initial evaluation and follow-up. They include a three-generation family history as part of the initial diagnostic assessment (COR, 1; LOE, B-NR), high-level recommendations for use of transthoracic echocardiogram in the initial work-up, every 1 or 2 years or when the patient’s status changes in confirmed cases, as well as parameters for using other imaging and diagnostic tests. Cardiovascular MRI, for example, is indicated when echocardiography is inconclusive (COR, 1; LOE, B-NR) and in other scenarios. When echocardiography is inconclusive but cardiac MRI isn’t available, cardiac CT is an option, albeit at a lower level of evidence (COR, 2b; LOE, C-LD).
Heart rhythm assessment has a high level of recommendation in multiple scenarios, even in first-degree relatives of HCM patients. Invasive hemodynamic assessment is in order for candidates of SRT whose left ventricular (LV) outflow tract obstruction status is unknown. This category also sets parameters for angiography, and exercise stress testing.
The most extensive recommendations for diagnosis and follow-up cover genetic testing; it consists of nine high-level recommendations.
“The guideline highlights not only the importance of genetic testing of an affected patient and genetic screening of family members, but also emphasizes ongoing reassessment of variant classification as this may evolve with time and change how we recommend ongoing family screening,” Dr. Mital noted.
“The guideline proposes initiating screening of family members at the earliest regardless of age given HCM can manifest at any age in affected families,” she added.
The guideline notes that the usefulness of genetic testing to evaluate the risk of sudden cardiac death (SCD) is uncertain. There’s even guidance for implementing those test results. Further testing is recommended for patients who are genotype positive and phenotype negative for HCM (COR, 1; LOE, B-NR). Those same patients may participate in competitive sports (COR, 2a; LOE, C-LD), but a pacemaker isn’t recommended as a primary prevention (COR, 3 [no benefit]; LOE, B-NR).
Risk evaluation and prevention
For SCD risk evaluation and prevention, the guideline spells out five components for the initial and follow-up evaluations (COR, 1; LOE, B-NR). That includes maximal LV wall thickness, ejection fraction, and LV apical aneurysm. The section include multiple recommendations for patient selection for placement of an implantable cardioverter-defibrillator (ICD). For example, it’s recommended for patient’s who’ve had a heart attack or sustained ventricular tachycardia (COR, 1; LOE, B-NR), but not so much for patients without risk factors or for participating in sports (COR, 3 [harm]; LOE, B-NR). The guideline even provides recommendations for selecting an ICD.
Management recommendations address when medical therapy is indicated, including which therapies are indicated for specific scenarios, as well as higher level interventions such as SRT for severely symptomatic patients with obstructive HCM (COR, 2b; LOE, C-LD) and surgical myectomy with ablation in patients with HCM and atrial fibrillation (COR, 2a; LOE, B-NR). This section also provides recommendations for managing patients with HCM and ventricular arrhythmias or advanced heart failure.
The guideline also includes a host of lifestyle considerations. Mild to moderate exercise is beneficial (COR, 1; LOE, B-NR), but athletes with HCM should consult with an “expert provider” (COR, 1; LOE, C, meaning based on expert opinion). Truck drivers, pilots and people who do strenuous physical labor with HCM should meet specific standards.
These recommendations again emphasize the role of shared decision-making, said Dr. Martinez. “It’s not a cookie-cutter discussion. It is taking all of the information, incorporating what the patient’s needs are, and then making sure you appropriately tell them what are the risks of exercising and not exercising. I have as many discussions through the day about what the risks of exercise are as I do the risks of not exercising.”
Refining nomenclature, pathophysiology
The writing committee addressed the nomenclature for HCM. The use of HCM to describe increased LV wall thickness linked to systemic diseases or secondary to LV hypertrophy “can lead to confusion,” the committee stated, so other cardiac or systemic causes of LV hypertrophy shouldn’t be labeled HCM. Other etiologies can cause secondary LV hypertrophy that can overlap with HCM; clinical markers and testing can help differentiate these mimickers from HCM. When echocardiography is inconclusive, cardiovascular MRI is indicated (COR, 1; LOE, B-NR).
The guideline update also provides clarity on the pathophysiology of HCM: It consists of dynamic LV outflow tract obstruction, mitral regurgitation, diastolic dysfunction, myocardial ischemia, arrhythmias, or autonomic dysfunction. “For a given patient with HCM, the clinical outcome may be dominated by one of these components or may be the result of a complex interplay,” the guideline states. The clinical evaluation should consider all these conditions.
This update also provides “clear separation” between care of HCM with and without obstruction, Dr. Martinez said. “The role of advanced therapies and referrals with advanced treatment options such as heart transplantation or CRT therapy in this group is different than before, recognizing that people with obstruction have symptoms that may be similar to those without obstruction, and the individual should be [thoroughly] investigated to make sure that you can discern between those two groups to make appropriate recommendations.”
The guideline was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, American Society of Echocardiography, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society for Cardiovascular Magnetic Resonance. It’s also been endorsed by the Pediatric & Congenital Electrophysiology Society.
Dr. Mital and Dr. Martinez have no relevant financial relationships to disclose.
SOURCE: Mital S et al. J Am Coll Cardiol. 2020 Nov 20. doi: 10.1016/j.jacc.2020.08.044.
Greater involvement of the patient and family in decision-making, clarity on the role of genetic testing and parameters for team-oriented care, and use of high-volume specialty centers are cornerstones of the first update in almost a decade of the American Heart Association/American College of Cardiology guideline for patients with hypertrophic cardiomyopathy (HCM).
The update lists 133 recommendations for HCM care in six categories: shared decision-making; role of high-volume HCM centers; diagnosis, initial evaluation, and follow-up; risk assessment and prevention of sudden cardiac death (SCD); management of HCM; and lifestyle considerations for patients.
“The guideline puts the patient front and center in the shared decision-making process and emphasizes the importance of incorporating patient’s lifestyle choices and preferences when making complex, life-altering decisions,” writing committee vice chair Seema Mital, MD, of the University of Toronto and the Hospital for Sick Children, also in Toronto, said in an interview.
The fully updated guideline, authored by a joint committee of the AHA and ACC with input from other specialty societies, has been published online in the Journal of the American College of Cardiology. It replaces the 2011 guideline.
Another key component of the update is the strong recommendation to utilize multidisciplinary care, said Matthew W. Martinez, MD, a writing committee member and sports cardiologists at Morristown (N.J.) Medical Center. “This is not only as a part of shared decision-making, but really in care for the patients,” he said, “that there’s a level of expertise that is provided by centers of excellence who handle HCM, and we did lay out some recommendations with regards to surgery, imaging, interventionists, and management with electrophysiology, and the care of athletes with potential for HCM and pregnant women.”
The update ranks recommendations by class of recommendation (COR), ranging from strong benefit much greater than risk to harm with risk exceeding benefit, and level of evidence (LOE). The recommendation for shared decision making, for example, carries at COR of 1, the highest rating, and a mid-level LOE of B-NR, meaning from nonrandomized studies. Patients who need septal reduction therapy (SRT) should be referred to a comprehensive or primary HCM center – a recommendation with a COR of 1 but an LOE of C-LD, meaning there are limited data.
From diagnosis to follow-up
The most extensive list of recommendations falls under the category covering diagnosis, initial evaluation and follow-up. They include a three-generation family history as part of the initial diagnostic assessment (COR, 1; LOE, B-NR), high-level recommendations for use of transthoracic echocardiogram in the initial work-up, every 1 or 2 years or when the patient’s status changes in confirmed cases, as well as parameters for using other imaging and diagnostic tests. Cardiovascular MRI, for example, is indicated when echocardiography is inconclusive (COR, 1; LOE, B-NR) and in other scenarios. When echocardiography is inconclusive but cardiac MRI isn’t available, cardiac CT is an option, albeit at a lower level of evidence (COR, 2b; LOE, C-LD).
Heart rhythm assessment has a high level of recommendation in multiple scenarios, even in first-degree relatives of HCM patients. Invasive hemodynamic assessment is in order for candidates of SRT whose left ventricular (LV) outflow tract obstruction status is unknown. This category also sets parameters for angiography, and exercise stress testing.
The most extensive recommendations for diagnosis and follow-up cover genetic testing; it consists of nine high-level recommendations.
“The guideline highlights not only the importance of genetic testing of an affected patient and genetic screening of family members, but also emphasizes ongoing reassessment of variant classification as this may evolve with time and change how we recommend ongoing family screening,” Dr. Mital noted.
“The guideline proposes initiating screening of family members at the earliest regardless of age given HCM can manifest at any age in affected families,” she added.
The guideline notes that the usefulness of genetic testing to evaluate the risk of sudden cardiac death (SCD) is uncertain. There’s even guidance for implementing those test results. Further testing is recommended for patients who are genotype positive and phenotype negative for HCM (COR, 1; LOE, B-NR). Those same patients may participate in competitive sports (COR, 2a; LOE, C-LD), but a pacemaker isn’t recommended as a primary prevention (COR, 3 [no benefit]; LOE, B-NR).
Risk evaluation and prevention
For SCD risk evaluation and prevention, the guideline spells out five components for the initial and follow-up evaluations (COR, 1; LOE, B-NR). That includes maximal LV wall thickness, ejection fraction, and LV apical aneurysm. The section include multiple recommendations for patient selection for placement of an implantable cardioverter-defibrillator (ICD). For example, it’s recommended for patient’s who’ve had a heart attack or sustained ventricular tachycardia (COR, 1; LOE, B-NR), but not so much for patients without risk factors or for participating in sports (COR, 3 [harm]; LOE, B-NR). The guideline even provides recommendations for selecting an ICD.
Management recommendations address when medical therapy is indicated, including which therapies are indicated for specific scenarios, as well as higher level interventions such as SRT for severely symptomatic patients with obstructive HCM (COR, 2b; LOE, C-LD) and surgical myectomy with ablation in patients with HCM and atrial fibrillation (COR, 2a; LOE, B-NR). This section also provides recommendations for managing patients with HCM and ventricular arrhythmias or advanced heart failure.
The guideline also includes a host of lifestyle considerations. Mild to moderate exercise is beneficial (COR, 1; LOE, B-NR), but athletes with HCM should consult with an “expert provider” (COR, 1; LOE, C, meaning based on expert opinion). Truck drivers, pilots and people who do strenuous physical labor with HCM should meet specific standards.
These recommendations again emphasize the role of shared decision-making, said Dr. Martinez. “It’s not a cookie-cutter discussion. It is taking all of the information, incorporating what the patient’s needs are, and then making sure you appropriately tell them what are the risks of exercising and not exercising. I have as many discussions through the day about what the risks of exercise are as I do the risks of not exercising.”
Refining nomenclature, pathophysiology
The writing committee addressed the nomenclature for HCM. The use of HCM to describe increased LV wall thickness linked to systemic diseases or secondary to LV hypertrophy “can lead to confusion,” the committee stated, so other cardiac or systemic causes of LV hypertrophy shouldn’t be labeled HCM. Other etiologies can cause secondary LV hypertrophy that can overlap with HCM; clinical markers and testing can help differentiate these mimickers from HCM. When echocardiography is inconclusive, cardiovascular MRI is indicated (COR, 1; LOE, B-NR).
The guideline update also provides clarity on the pathophysiology of HCM: It consists of dynamic LV outflow tract obstruction, mitral regurgitation, diastolic dysfunction, myocardial ischemia, arrhythmias, or autonomic dysfunction. “For a given patient with HCM, the clinical outcome may be dominated by one of these components or may be the result of a complex interplay,” the guideline states. The clinical evaluation should consider all these conditions.
This update also provides “clear separation” between care of HCM with and without obstruction, Dr. Martinez said. “The role of advanced therapies and referrals with advanced treatment options such as heart transplantation or CRT therapy in this group is different than before, recognizing that people with obstruction have symptoms that may be similar to those without obstruction, and the individual should be [thoroughly] investigated to make sure that you can discern between those two groups to make appropriate recommendations.”
The guideline was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, American Society of Echocardiography, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society for Cardiovascular Magnetic Resonance. It’s also been endorsed by the Pediatric & Congenital Electrophysiology Society.
Dr. Mital and Dr. Martinez have no relevant financial relationships to disclose.
SOURCE: Mital S et al. J Am Coll Cardiol. 2020 Nov 20. doi: 10.1016/j.jacc.2020.08.044.