User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
HealthCare.gov enrollment ends with unexpected extension
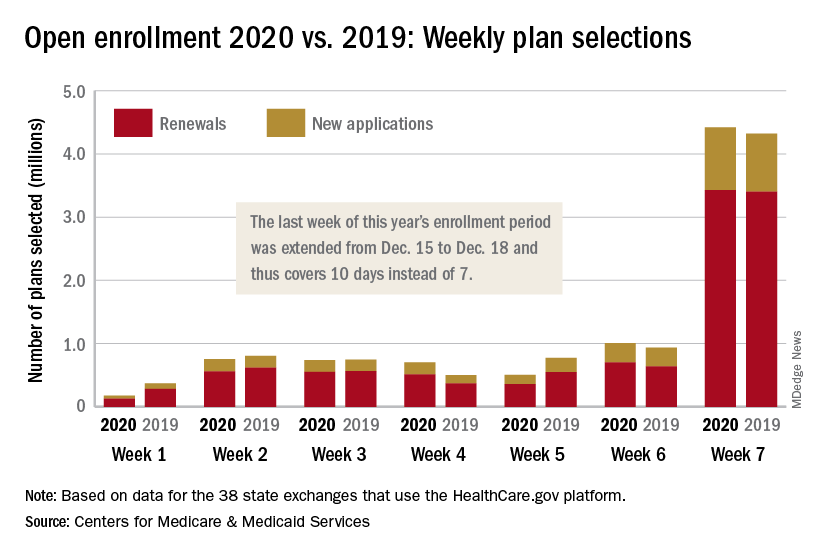
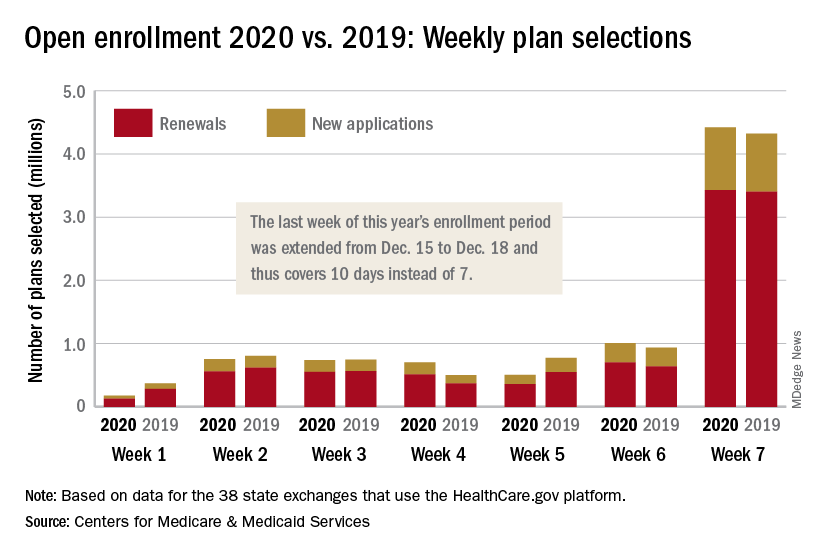
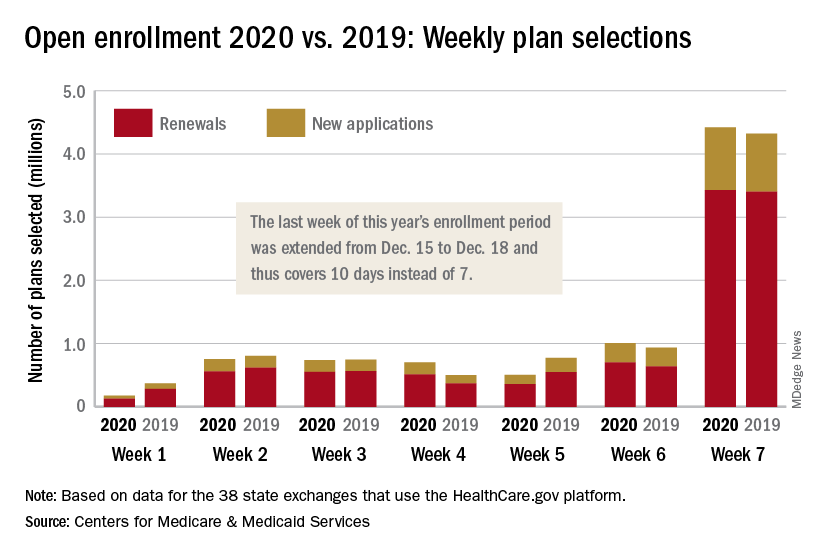
The 2020 open enrollment period on HealthCare.gov ended on Dec. 18 after an unplanned extension, but Centers for Medicare & Medicaid Services Administrator Seema Verma touted the system’s stability.
“We are reporting that for the third year in a row enrollment in the Federal Exchange remained stable,” she said in a statement. “For all our successes, too many Americans who do not qualify for subsidies still cannot afford premiums that remain in the stratosphere – constituting a new class of uninsured. The Affordable Care Act remains fundamentally broken and nothing less than wholesale reforms can fix it.”
The open enrollment period was scheduled to end on Dec. 15, but some individuals had problems signing up for coverage that day so the CMS extended the deadline to Dec. 18. During that last “week,” consumers selected over 4.4 million plans – 3.4 million were renewals and just under 1 million were new – bringing the cumulative total for the 2020 enrollment period to 8.3 million plans selected from Nov. 1 to Dec. 17, CMS reported.
Plans selected during the last 3 hours of open enrollment – 12:00 a.m. to 3:00 a.m. on Dec. 18 – are not included in the weekly or final counts, so it’s still possible that the 2020 enrollment could surpass last year’s total of 8.45 million plan selections. The fully updated enrollment data will be released during the second week of January, CMS said.
The 2020 open enrollment period on HealthCare.gov ended on Dec. 18 after an unplanned extension, but Centers for Medicare & Medicaid Services Administrator Seema Verma touted the system’s stability.
“We are reporting that for the third year in a row enrollment in the Federal Exchange remained stable,” she said in a statement. “For all our successes, too many Americans who do not qualify for subsidies still cannot afford premiums that remain in the stratosphere – constituting a new class of uninsured. The Affordable Care Act remains fundamentally broken and nothing less than wholesale reforms can fix it.”
The open enrollment period was scheduled to end on Dec. 15, but some individuals had problems signing up for coverage that day so the CMS extended the deadline to Dec. 18. During that last “week,” consumers selected over 4.4 million plans – 3.4 million were renewals and just under 1 million were new – bringing the cumulative total for the 2020 enrollment period to 8.3 million plans selected from Nov. 1 to Dec. 17, CMS reported.
Plans selected during the last 3 hours of open enrollment – 12:00 a.m. to 3:00 a.m. on Dec. 18 – are not included in the weekly or final counts, so it’s still possible that the 2020 enrollment could surpass last year’s total of 8.45 million plan selections. The fully updated enrollment data will be released during the second week of January, CMS said.
The 2020 open enrollment period on HealthCare.gov ended on Dec. 18 after an unplanned extension, but Centers for Medicare & Medicaid Services Administrator Seema Verma touted the system’s stability.
“We are reporting that for the third year in a row enrollment in the Federal Exchange remained stable,” she said in a statement. “For all our successes, too many Americans who do not qualify for subsidies still cannot afford premiums that remain in the stratosphere – constituting a new class of uninsured. The Affordable Care Act remains fundamentally broken and nothing less than wholesale reforms can fix it.”
The open enrollment period was scheduled to end on Dec. 15, but some individuals had problems signing up for coverage that day so the CMS extended the deadline to Dec. 18. During that last “week,” consumers selected over 4.4 million plans – 3.4 million were renewals and just under 1 million were new – bringing the cumulative total for the 2020 enrollment period to 8.3 million plans selected from Nov. 1 to Dec. 17, CMS reported.
Plans selected during the last 3 hours of open enrollment – 12:00 a.m. to 3:00 a.m. on Dec. 18 – are not included in the weekly or final counts, so it’s still possible that the 2020 enrollment could surpass last year’s total of 8.45 million plan selections. The fully updated enrollment data will be released during the second week of January, CMS said.
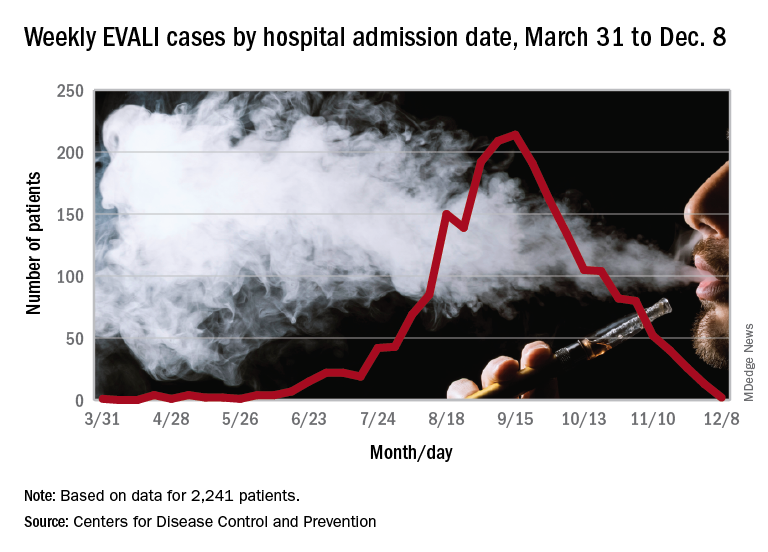
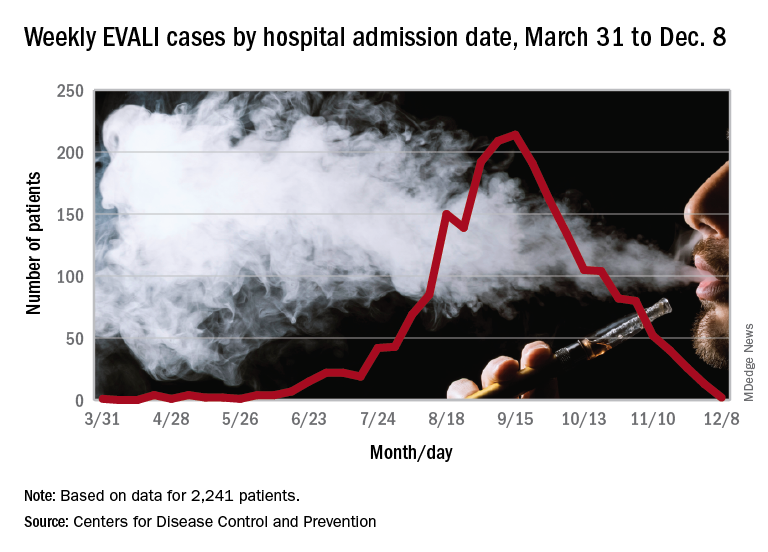
EVALI readmissions and deaths prompt guideline change
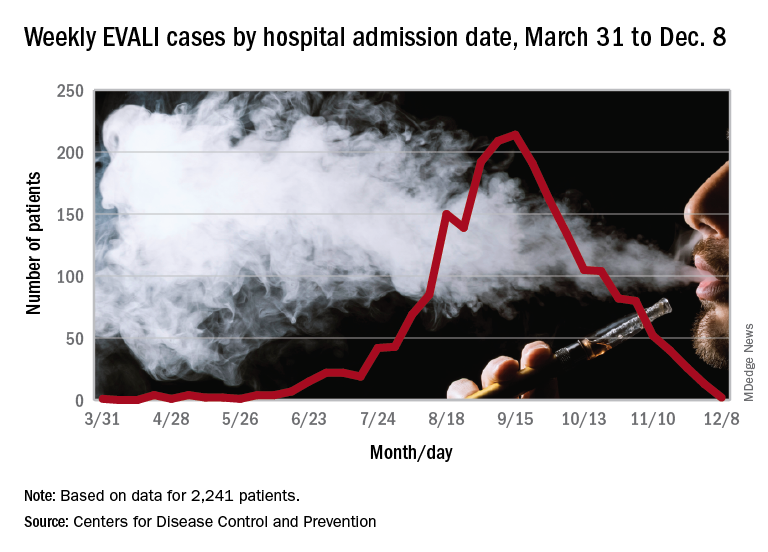
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
FROM MMWR
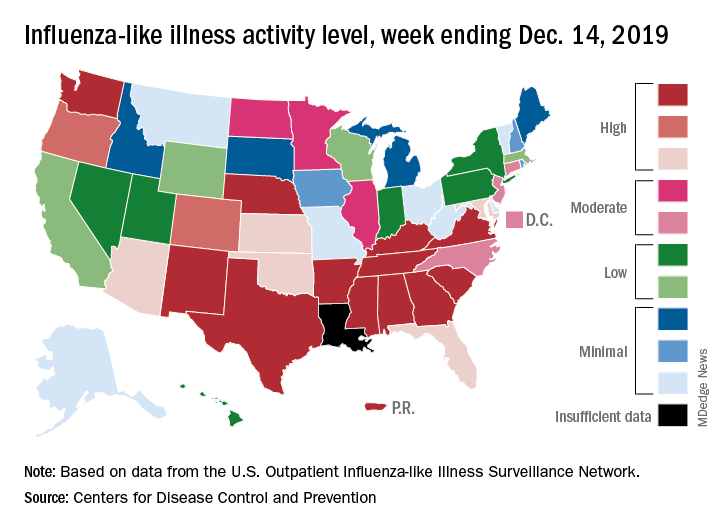
Influenza activity continues to be unusually high
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
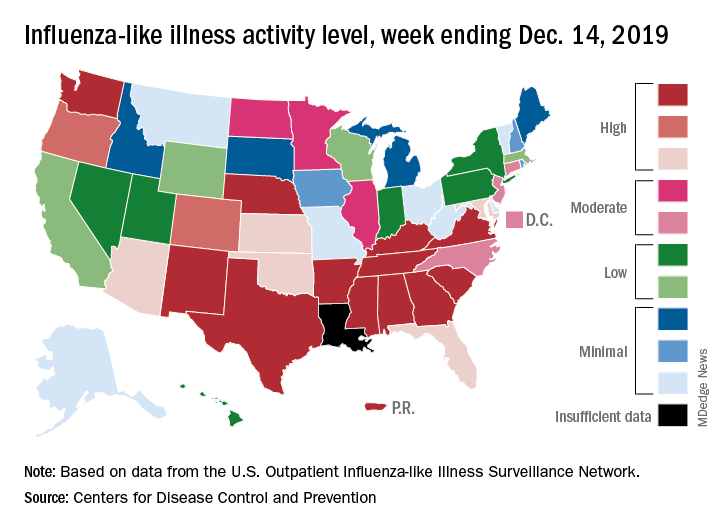
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
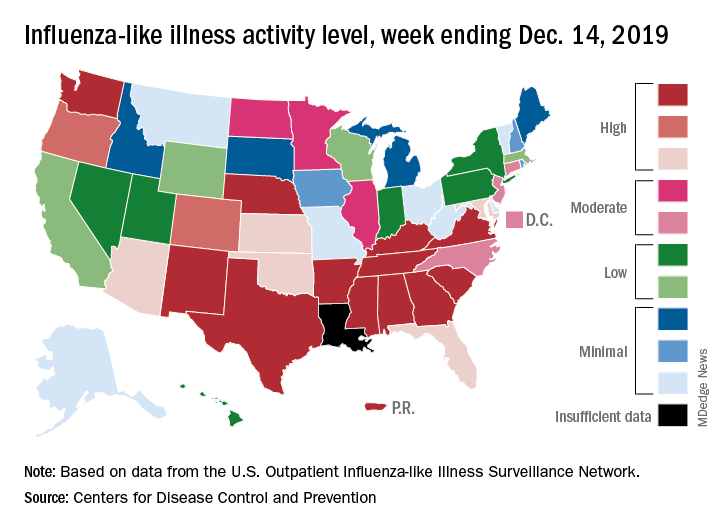
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.
Human hair’s super strength and boiled diabetes
Stop us if you’ve heard this one
An elephant, a capybara, and a horse walk into a bar …
What? You’ve heard it? Really? … No, not really? You were just pulling our leg. Very funny.
Can we go on now? You’re sure? Because if there’s one thing we love, it’s reader participation.
Anyway, there’s this bar, and a bunch of researchers from the University of California’s San Diego and Berkeley campuses are hanging out with a bear, a boar, a javelina (looks and sounds like a pig, about the size of a border collie), and a giraffe when the aforementioned trio shows up.
They see all these mammals together and get an idea. Why not compare the tensile strength of their hair with that of a human adult and child? The next day, after sobering up, they started collecting hair samples.[Legal note: The situation at the bar is a literary device. At no time did the investigators conduct any of their work in such a place.]
Once that was done, uniaxial tension tests were conducted, as you would expect, using an Instron 3342 universal testing system equipped with a 500-N load cell at a strain rate of 10–2s–1.
The results, however, were not expected. Thin hairs are stronger than thick hairs. Hair from a human, with an average diameter of about 60 mcm, is stronger than hair from a boar (average diameter, 235 mcm) or a horse (average diameter, 200 mcm), and the weakest hair of all came from an elephant (diameter of 345 mcm) and a giraffe (diameter of 370 mcm). Also, the hair from the 9-year-old child is stronger than the thicker hair of the 30-year-old adult.
The results show that the inherent strength of human hair’s hierarchical structure – an outer layer, or cuticle, “wraps around an inner cortex made of many small fibers linked by chemical bonds” – makes it resistant to deformation, the investigators explained. They hope that synthetic materials with a similar structure could become lighter and stronger in the future.
Now what? The punchline? All this valuable hair information isn’t enough? Fine.
The shocked bartender, who’s already got the makings of a small zoo in his establishment, points a finger in alarm at the latest arrivals and yells, “Hey!” The horse says, “You read my mind, buddy.”
Boiled type 2 diabetes
Ah, coffee. Is there anything it can’t do? From speeding up delivery of this tardy column (if not boosting its comedy quotient) to reducing the risk of type 2 diabetes, the magic bean seems nearly omnipotent. But java’s magical metabolic properties may be entirely dependent on how you brew your brown elixir.
Coffee-fueled Scandinavians have determined that the stimulating liquid’s antidiabetes effect is only possible when you don’t boil your beans. For those eager to ward off type 2 diabetes, filtered coffee – not boiled coffee – is the ticket to lower insulin resistance.
Researchers at Chalmers University of Technology in Gothenburg, Sweden, and Umeå (Sweden) University identified biomarkers that distinguished the consumption of filtered coffee from its boiled cousin. They found that people who drank two to three cups of filtered coffee a day enjoyed a 60% lower risk of type 2 diabetes than did those who subsisted on less than one cup of filtered coffee per day. But drinking boiled coffee did nothing to dent drinkers’ diabetes risk.
Why the difference? The coffee-sipping Swedish investigators say boiled coffee contains diterpenes, which don’t make it past a coffee filter. Other studies have shown diterpenes inflate the risk of heart and vascular diseases. And the researchers say those unfiltered diterpenes may sap your morning cuppa joe’s antidiabetes powers.
We know what you’re thinking: Who boils powdered coffee? Is Sanka even a thing anymore? It’s an approach that’s unfamiliar to most Mr. Coffee–owning Scandinavians and American java junkies alike. But before you, like us, take another smug sip from that cup you just made in the Keurig machine, know this: Coffee pod machines deal out hot, unfiltered brew.
Maybe just add two sugar packets next time. Your beta cells will thank you.
Let my people poop!
This is the way the world ends, this is the way the world ends: Not with a bang, but a tilted toilet.
The latest piece of late-stage capitalistic horror comes from Great Britain, and has lovingly been called the “StandardToilet.” No dystopian overtones there, absolutely not. The toilet’s “genius” lies in the seat’s 13-degree downward slope, which increases strain on the legs just like a squat thrust would. Sit on one for more than 5 minutes, and the pain becomes too much to handle.
The inventor of the StandardToilet claims that his product will cut time employees spend on the toilet by 25%, saving businesses as much as 4.8 billion pounds sterling a year. Not only that, he suggests that there are numerous health benefits, such as reduced hemorrhoid risk and a reduction of musculoskeletal disorders.
Critics were quick to point out that people with disabilities would likely have accessibility issues (and let’s not forget people with GI diseases), and a bathroom space expert (yes, that’s a thing) suggested that, if employees are spending too much time on the toilet, the issue is likely not laziness but the poor state of affairs in the workplace itself.
As purveyors of quality toilet- and poop-themed humor, we here at Livin’ on the MDedge world headquarters think it would be a shame if the giant corporations of the world took away normal toilets. So we say to the downtrodden proletariat: Workers of the world, unite! You have nothing to lose but your toilets!
Livin’ on the MDedge will be taking a holiday break, but we’ll be back to advance medical science in January!
Stop us if you’ve heard this one
An elephant, a capybara, and a horse walk into a bar …
What? You’ve heard it? Really? … No, not really? You were just pulling our leg. Very funny.
Can we go on now? You’re sure? Because if there’s one thing we love, it’s reader participation.
Anyway, there’s this bar, and a bunch of researchers from the University of California’s San Diego and Berkeley campuses are hanging out with a bear, a boar, a javelina (looks and sounds like a pig, about the size of a border collie), and a giraffe when the aforementioned trio shows up.
They see all these mammals together and get an idea. Why not compare the tensile strength of their hair with that of a human adult and child? The next day, after sobering up, they started collecting hair samples.[Legal note: The situation at the bar is a literary device. At no time did the investigators conduct any of their work in such a place.]
Once that was done, uniaxial tension tests were conducted, as you would expect, using an Instron 3342 universal testing system equipped with a 500-N load cell at a strain rate of 10–2s–1.
The results, however, were not expected. Thin hairs are stronger than thick hairs. Hair from a human, with an average diameter of about 60 mcm, is stronger than hair from a boar (average diameter, 235 mcm) or a horse (average diameter, 200 mcm), and the weakest hair of all came from an elephant (diameter of 345 mcm) and a giraffe (diameter of 370 mcm). Also, the hair from the 9-year-old child is stronger than the thicker hair of the 30-year-old adult.
The results show that the inherent strength of human hair’s hierarchical structure – an outer layer, or cuticle, “wraps around an inner cortex made of many small fibers linked by chemical bonds” – makes it resistant to deformation, the investigators explained. They hope that synthetic materials with a similar structure could become lighter and stronger in the future.
Now what? The punchline? All this valuable hair information isn’t enough? Fine.
The shocked bartender, who’s already got the makings of a small zoo in his establishment, points a finger in alarm at the latest arrivals and yells, “Hey!” The horse says, “You read my mind, buddy.”
Boiled type 2 diabetes
Ah, coffee. Is there anything it can’t do? From speeding up delivery of this tardy column (if not boosting its comedy quotient) to reducing the risk of type 2 diabetes, the magic bean seems nearly omnipotent. But java’s magical metabolic properties may be entirely dependent on how you brew your brown elixir.
Coffee-fueled Scandinavians have determined that the stimulating liquid’s antidiabetes effect is only possible when you don’t boil your beans. For those eager to ward off type 2 diabetes, filtered coffee – not boiled coffee – is the ticket to lower insulin resistance.
Researchers at Chalmers University of Technology in Gothenburg, Sweden, and Umeå (Sweden) University identified biomarkers that distinguished the consumption of filtered coffee from its boiled cousin. They found that people who drank two to three cups of filtered coffee a day enjoyed a 60% lower risk of type 2 diabetes than did those who subsisted on less than one cup of filtered coffee per day. But drinking boiled coffee did nothing to dent drinkers’ diabetes risk.
Why the difference? The coffee-sipping Swedish investigators say boiled coffee contains diterpenes, which don’t make it past a coffee filter. Other studies have shown diterpenes inflate the risk of heart and vascular diseases. And the researchers say those unfiltered diterpenes may sap your morning cuppa joe’s antidiabetes powers.
We know what you’re thinking: Who boils powdered coffee? Is Sanka even a thing anymore? It’s an approach that’s unfamiliar to most Mr. Coffee–owning Scandinavians and American java junkies alike. But before you, like us, take another smug sip from that cup you just made in the Keurig machine, know this: Coffee pod machines deal out hot, unfiltered brew.
Maybe just add two sugar packets next time. Your beta cells will thank you.
Let my people poop!
This is the way the world ends, this is the way the world ends: Not with a bang, but a tilted toilet.
The latest piece of late-stage capitalistic horror comes from Great Britain, and has lovingly been called the “StandardToilet.” No dystopian overtones there, absolutely not. The toilet’s “genius” lies in the seat’s 13-degree downward slope, which increases strain on the legs just like a squat thrust would. Sit on one for more than 5 minutes, and the pain becomes too much to handle.
The inventor of the StandardToilet claims that his product will cut time employees spend on the toilet by 25%, saving businesses as much as 4.8 billion pounds sterling a year. Not only that, he suggests that there are numerous health benefits, such as reduced hemorrhoid risk and a reduction of musculoskeletal disorders.
Critics were quick to point out that people with disabilities would likely have accessibility issues (and let’s not forget people with GI diseases), and a bathroom space expert (yes, that’s a thing) suggested that, if employees are spending too much time on the toilet, the issue is likely not laziness but the poor state of affairs in the workplace itself.
As purveyors of quality toilet- and poop-themed humor, we here at Livin’ on the MDedge world headquarters think it would be a shame if the giant corporations of the world took away normal toilets. So we say to the downtrodden proletariat: Workers of the world, unite! You have nothing to lose but your toilets!
Livin’ on the MDedge will be taking a holiday break, but we’ll be back to advance medical science in January!
Stop us if you’ve heard this one
An elephant, a capybara, and a horse walk into a bar …
What? You’ve heard it? Really? … No, not really? You were just pulling our leg. Very funny.
Can we go on now? You’re sure? Because if there’s one thing we love, it’s reader participation.
Anyway, there’s this bar, and a bunch of researchers from the University of California’s San Diego and Berkeley campuses are hanging out with a bear, a boar, a javelina (looks and sounds like a pig, about the size of a border collie), and a giraffe when the aforementioned trio shows up.
They see all these mammals together and get an idea. Why not compare the tensile strength of their hair with that of a human adult and child? The next day, after sobering up, they started collecting hair samples.[Legal note: The situation at the bar is a literary device. At no time did the investigators conduct any of their work in such a place.]
Once that was done, uniaxial tension tests were conducted, as you would expect, using an Instron 3342 universal testing system equipped with a 500-N load cell at a strain rate of 10–2s–1.
The results, however, were not expected. Thin hairs are stronger than thick hairs. Hair from a human, with an average diameter of about 60 mcm, is stronger than hair from a boar (average diameter, 235 mcm) or a horse (average diameter, 200 mcm), and the weakest hair of all came from an elephant (diameter of 345 mcm) and a giraffe (diameter of 370 mcm). Also, the hair from the 9-year-old child is stronger than the thicker hair of the 30-year-old adult.
The results show that the inherent strength of human hair’s hierarchical structure – an outer layer, or cuticle, “wraps around an inner cortex made of many small fibers linked by chemical bonds” – makes it resistant to deformation, the investigators explained. They hope that synthetic materials with a similar structure could become lighter and stronger in the future.
Now what? The punchline? All this valuable hair information isn’t enough? Fine.
The shocked bartender, who’s already got the makings of a small zoo in his establishment, points a finger in alarm at the latest arrivals and yells, “Hey!” The horse says, “You read my mind, buddy.”
Boiled type 2 diabetes
Ah, coffee. Is there anything it can’t do? From speeding up delivery of this tardy column (if not boosting its comedy quotient) to reducing the risk of type 2 diabetes, the magic bean seems nearly omnipotent. But java’s magical metabolic properties may be entirely dependent on how you brew your brown elixir.
Coffee-fueled Scandinavians have determined that the stimulating liquid’s antidiabetes effect is only possible when you don’t boil your beans. For those eager to ward off type 2 diabetes, filtered coffee – not boiled coffee – is the ticket to lower insulin resistance.
Researchers at Chalmers University of Technology in Gothenburg, Sweden, and Umeå (Sweden) University identified biomarkers that distinguished the consumption of filtered coffee from its boiled cousin. They found that people who drank two to three cups of filtered coffee a day enjoyed a 60% lower risk of type 2 diabetes than did those who subsisted on less than one cup of filtered coffee per day. But drinking boiled coffee did nothing to dent drinkers’ diabetes risk.
Why the difference? The coffee-sipping Swedish investigators say boiled coffee contains diterpenes, which don’t make it past a coffee filter. Other studies have shown diterpenes inflate the risk of heart and vascular diseases. And the researchers say those unfiltered diterpenes may sap your morning cuppa joe’s antidiabetes powers.
We know what you’re thinking: Who boils powdered coffee? Is Sanka even a thing anymore? It’s an approach that’s unfamiliar to most Mr. Coffee–owning Scandinavians and American java junkies alike. But before you, like us, take another smug sip from that cup you just made in the Keurig machine, know this: Coffee pod machines deal out hot, unfiltered brew.
Maybe just add two sugar packets next time. Your beta cells will thank you.
Let my people poop!
This is the way the world ends, this is the way the world ends: Not with a bang, but a tilted toilet.
The latest piece of late-stage capitalistic horror comes from Great Britain, and has lovingly been called the “StandardToilet.” No dystopian overtones there, absolutely not. The toilet’s “genius” lies in the seat’s 13-degree downward slope, which increases strain on the legs just like a squat thrust would. Sit on one for more than 5 minutes, and the pain becomes too much to handle.
The inventor of the StandardToilet claims that his product will cut time employees spend on the toilet by 25%, saving businesses as much as 4.8 billion pounds sterling a year. Not only that, he suggests that there are numerous health benefits, such as reduced hemorrhoid risk and a reduction of musculoskeletal disorders.
Critics were quick to point out that people with disabilities would likely have accessibility issues (and let’s not forget people with GI diseases), and a bathroom space expert (yes, that’s a thing) suggested that, if employees are spending too much time on the toilet, the issue is likely not laziness but the poor state of affairs in the workplace itself.
As purveyors of quality toilet- and poop-themed humor, we here at Livin’ on the MDedge world headquarters think it would be a shame if the giant corporations of the world took away normal toilets. So we say to the downtrodden proletariat: Workers of the world, unite! You have nothing to lose but your toilets!
Livin’ on the MDedge will be taking a holiday break, but we’ll be back to advance medical science in January!
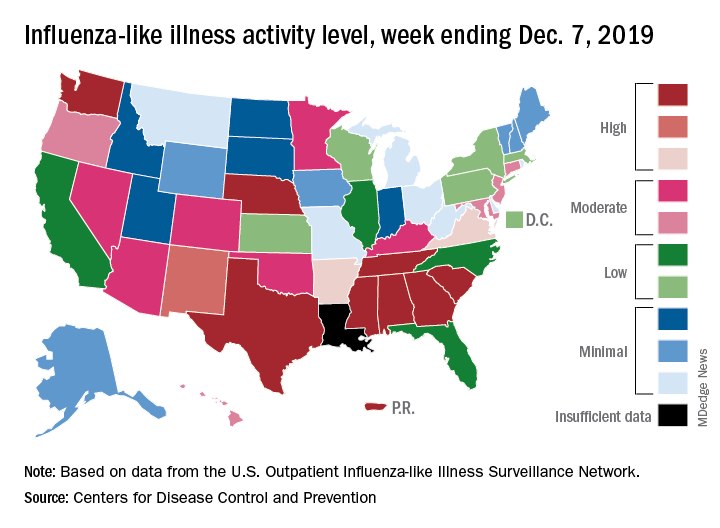
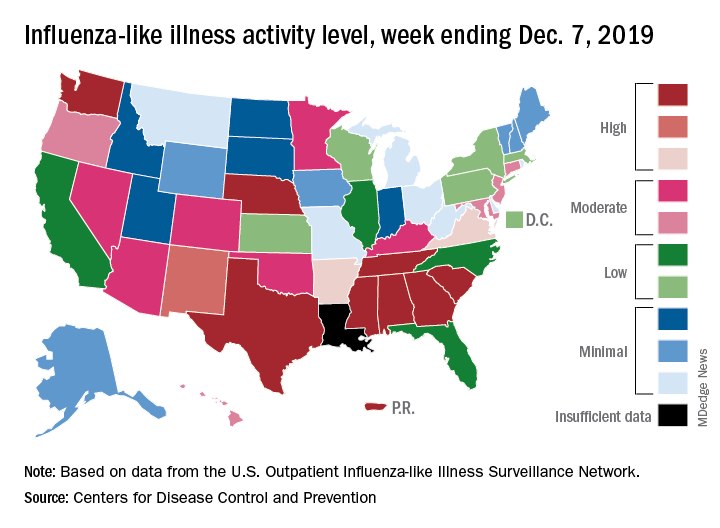
Flu activity dropped in early December
according to the Centers for Disease Control and Prevention.
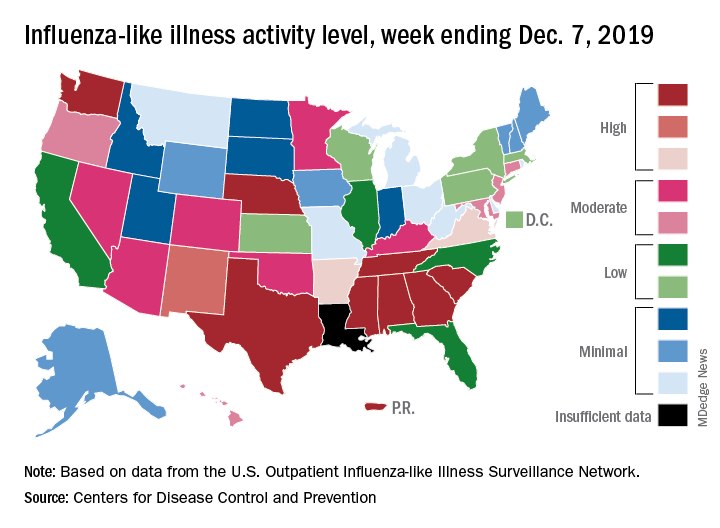
Nationally, 3.2% of outpatient visits were for influenza-like illness (ILI) during the week of Dec. 1-7, the CDC reported. That is down from 3.4% the week before, which was the highest November rate in 10 years. The national baseline rate is 2.4%, and the current 3.2% marks the fifth consecutive week that the outpatient ILI rate has been at or above the baseline level, the CDC report noted.
The drop in activity “may be influenced in part by a reduction in routine healthcare visits surrounding the Thanksgiving holiday. … as has occurred during previous seasons,” the CDC influenza division said Dec. 13 in its weekly flu report.
The early spike in “activity is being caused mostly by influenza B/Victoria viruses, which is unusual for this time of year,” the report said. Since the beginning of the 2019-2020 season a little over 2 months ago, almost 70% of specimens that have been positive for influenza have been identified as type B.
The nationwide decline in activity doesn’t, however, show up at the state level. For the week ending Dec. 7, there were eight states along with Puerto Rico at level 10 on the CDC’s 1-10 scale of flu activity, as there were the previous week. Washington state moved up from 9 to 10, but Louisiana, which was at level 10 last week, had insufficient data to be included this week, the CDC data show.
There were four flu-related pediatric deaths reported to the CDC during the week ending Dec. 7, all occurring in previous weeks, which brings the total to 10 for the season. In 2018-2019, there were 143 pediatric deaths caused by influenza, the CDC said.
according to the Centers for Disease Control and Prevention.
Nationally, 3.2% of outpatient visits were for influenza-like illness (ILI) during the week of Dec. 1-7, the CDC reported. That is down from 3.4% the week before, which was the highest November rate in 10 years. The national baseline rate is 2.4%, and the current 3.2% marks the fifth consecutive week that the outpatient ILI rate has been at or above the baseline level, the CDC report noted.
The drop in activity “may be influenced in part by a reduction in routine healthcare visits surrounding the Thanksgiving holiday. … as has occurred during previous seasons,” the CDC influenza division said Dec. 13 in its weekly flu report.
The early spike in “activity is being caused mostly by influenza B/Victoria viruses, which is unusual for this time of year,” the report said. Since the beginning of the 2019-2020 season a little over 2 months ago, almost 70% of specimens that have been positive for influenza have been identified as type B.
The nationwide decline in activity doesn’t, however, show up at the state level. For the week ending Dec. 7, there were eight states along with Puerto Rico at level 10 on the CDC’s 1-10 scale of flu activity, as there were the previous week. Washington state moved up from 9 to 10, but Louisiana, which was at level 10 last week, had insufficient data to be included this week, the CDC data show.
There were four flu-related pediatric deaths reported to the CDC during the week ending Dec. 7, all occurring in previous weeks, which brings the total to 10 for the season. In 2018-2019, there were 143 pediatric deaths caused by influenza, the CDC said.
according to the Centers for Disease Control and Prevention.
Nationally, 3.2% of outpatient visits were for influenza-like illness (ILI) during the week of Dec. 1-7, the CDC reported. That is down from 3.4% the week before, which was the highest November rate in 10 years. The national baseline rate is 2.4%, and the current 3.2% marks the fifth consecutive week that the outpatient ILI rate has been at or above the baseline level, the CDC report noted.
The drop in activity “may be influenced in part by a reduction in routine healthcare visits surrounding the Thanksgiving holiday. … as has occurred during previous seasons,” the CDC influenza division said Dec. 13 in its weekly flu report.
The early spike in “activity is being caused mostly by influenza B/Victoria viruses, which is unusual for this time of year,” the report said. Since the beginning of the 2019-2020 season a little over 2 months ago, almost 70% of specimens that have been positive for influenza have been identified as type B.
The nationwide decline in activity doesn’t, however, show up at the state level. For the week ending Dec. 7, there were eight states along with Puerto Rico at level 10 on the CDC’s 1-10 scale of flu activity, as there were the previous week. Washington state moved up from 9 to 10, but Louisiana, which was at level 10 last week, had insufficient data to be included this week, the CDC data show.
There were four flu-related pediatric deaths reported to the CDC during the week ending Dec. 7, all occurring in previous weeks, which brings the total to 10 for the season. In 2018-2019, there were 143 pediatric deaths caused by influenza, the CDC said.
2020 open enrollment: HealthCare.gov heats up in week 6
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
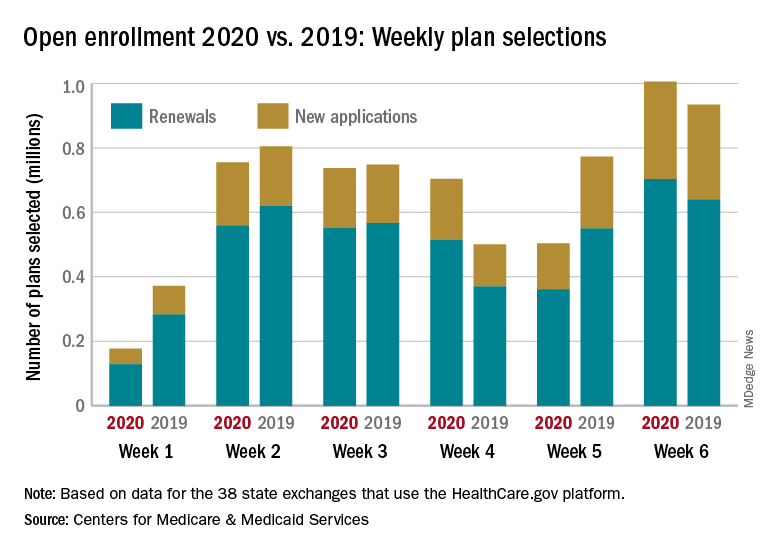
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
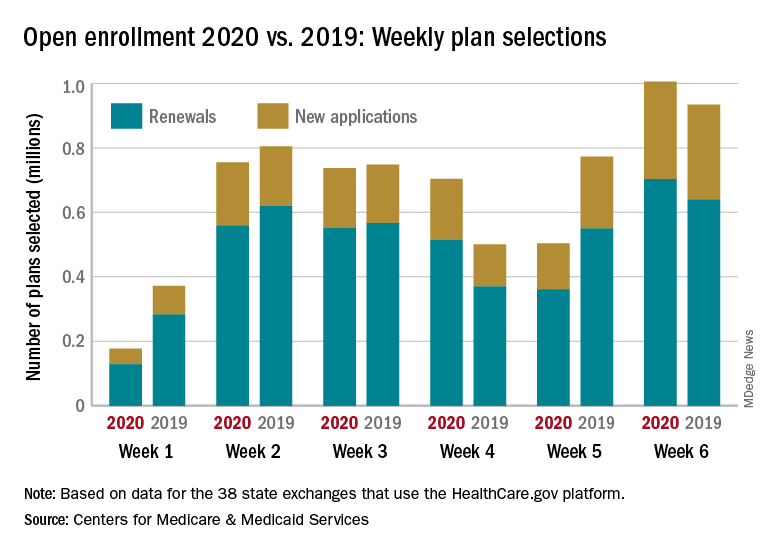
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
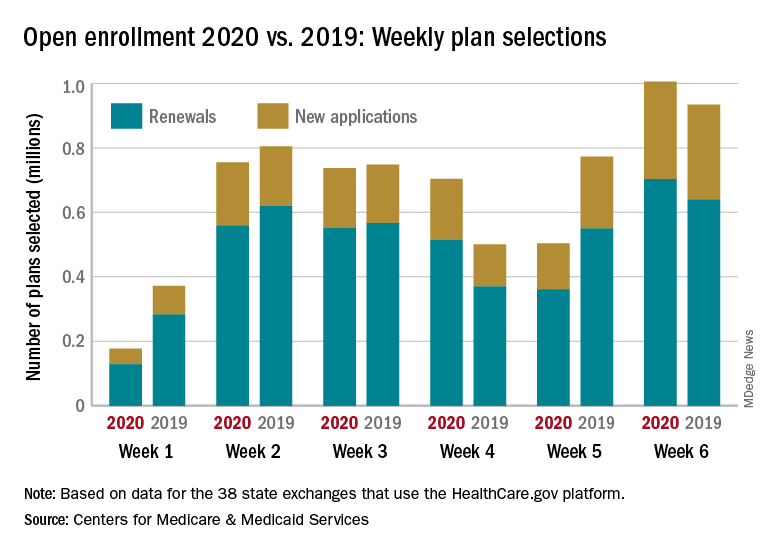
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.
Tales of nasal terror, and dental hoverboarding
A cure for nosiness
Christmas may be just around the corner, but is there ever really a wrong time to huddle around a campfire and swap scary stories? So bundle up, get the fire going, and prepare yourselves for a pair of nasal-based horror stories that will frighten your Jingle Bells off!
Our first tale of nostril terror comes all the way from southern India, where a 13-year-old boy jumped into a water well to cool off. Hey, southern India gets hot, even in November. But like something out of a bad sci-fi movie, his peaceful swim was interrupted when something swam up his nose, causing him extreme pain. After a 30-minute procedure, the doctor pulled out the culprit: A horrific alien parasite! Okay, we’re lying; it was a fish. But we had you going, didn’t we?
Well, maybe that didn’t get you frightened. But we have more rhinal dread to share! A young girl in Las Vegas stuck a pair of plastic doll shoes up her nose, one in each nostril. Her mother removed one shoe, but neither she nor urgent care could reach the second. A trip to the hospital was in order, and once there, the doctors were able to remove the foreign object in seconds.
But as with all things in U.S. medicine, a reckoning would soon come. You feel it now, the dread in this woman’s heart when the hospital bill came.
She takes the envelope, and opens it slowly.
The paper unfolds, rough and heavy in her hands.
Her eyes scan the page, looking for the number, where is it, where is it? It must be here, it must be ...
$3,000.
That’s right, for this simple procedure, performed with a pair of fancy tweezers, the hospital saw fit to charge the hapless mother $3,000! AHHHHHHHHHHHH!
Some say that the mother’s high-deductible insurance policy reduced the cost to $1,700. But we ask you, does that make the story any less spooky? We think not.
Hoverboarding down the root canal
Time spent in the dentist’s chair is among the most anxiety-inducing in anyone’s life. The needles. The grinding. The drilling. The rinsing. The spitting. The throbbing copays.
But you know what might inject a few cc’s of fun into your oral hygiene visits?
Did you guess ... a hoverboard?
If you did, well, you’re probably dentist Steve Martin in “Little Shop of Horrors.” Or perhaps Alaska dentist Seth Lookhart, who authorities say performed a tooth extraction on a sedated patient while Dr. Lookhart also rode a hoverboard. There are also charges of felony Medicaid fraud and reckless endangerment. And allegations of hefty theft from his practice partners. Oh, and a state board apparently suspended Dr. Lookhart’s dental license in 2017.
But hey, pulling teeth while taming a hoverboard? Photos or it didn’t happen, right?
Unfortunately for the well-balanced dentist, there are photos. Actually, there’s an entire video. And when prosecutors showed it to Dr. Lookhart’s unwitting and horrified costar, she was about as happy as the impacted wisdom teeth your teen kid’s still toting around.
Dr. Lookhart denied the felony fraud charges. But he did cop to the hoverboard. Which puts him one up on his cinematic “Wild and Crazy Guy” doppelganger. Even as a neurosurgeon in “The Man With Two Brains,” Mr. Martin never attempted to hoverboard while performing double “cranial screw-top” brain surgeries.
CSI: Quebec
They may live in that eternally polite land on the other side of our northern border, but they know where the bodies are buried. Lots of bodies. Some of them in shallow graves. Some of them in vehicles.
No, we are not talking about Gil Grissom and the gang at CSI. We’re talking about the Secure Site for Research in Thanatology, also known as the “body farm,” which is scheduled to open this spring in Becancour, Quebec.
It’s the first such outdoor forensic facility in Canada and the first in the world – there are also body farms in the United States, Australia, and the Netherlands – to be located in a northern climate.
“We’re particularly interested in understanding what happens when a body is in subzero temperatures, when there’s a lot of snow on the ground, and how that freeze and then the thaw process might actually change the rate of decomposition,” Shari Forbes, the farm’s director, told CTV News recently.
The science team will be out on the farm every day, meticulously checking each body – talk about making a list and checking it twice – for all the important CSI stuff: how long fingerprints and DNA evidence last, the effects of insect feeding and egg-laying, and the ability of dogs to detect scents.
The decomposition process in a cold climate will be a strange and wondrous journey, and the body farm’s work can, perhaps, best be summed up by none other than Mr. Grissom, who once said that getting to the evidence means having to destroy the evidence.
Then again, he also said that “dead men don’t ride roller coasters,” so the analogy only goes so far.
A cure for nosiness
Christmas may be just around the corner, but is there ever really a wrong time to huddle around a campfire and swap scary stories? So bundle up, get the fire going, and prepare yourselves for a pair of nasal-based horror stories that will frighten your Jingle Bells off!
Our first tale of nostril terror comes all the way from southern India, where a 13-year-old boy jumped into a water well to cool off. Hey, southern India gets hot, even in November. But like something out of a bad sci-fi movie, his peaceful swim was interrupted when something swam up his nose, causing him extreme pain. After a 30-minute procedure, the doctor pulled out the culprit: A horrific alien parasite! Okay, we’re lying; it was a fish. But we had you going, didn’t we?
Well, maybe that didn’t get you frightened. But we have more rhinal dread to share! A young girl in Las Vegas stuck a pair of plastic doll shoes up her nose, one in each nostril. Her mother removed one shoe, but neither she nor urgent care could reach the second. A trip to the hospital was in order, and once there, the doctors were able to remove the foreign object in seconds.
But as with all things in U.S. medicine, a reckoning would soon come. You feel it now, the dread in this woman’s heart when the hospital bill came.
She takes the envelope, and opens it slowly.
The paper unfolds, rough and heavy in her hands.
Her eyes scan the page, looking for the number, where is it, where is it? It must be here, it must be ...
$3,000.
That’s right, for this simple procedure, performed with a pair of fancy tweezers, the hospital saw fit to charge the hapless mother $3,000! AHHHHHHHHHHHH!
Some say that the mother’s high-deductible insurance policy reduced the cost to $1,700. But we ask you, does that make the story any less spooky? We think not.
Hoverboarding down the root canal
Time spent in the dentist’s chair is among the most anxiety-inducing in anyone’s life. The needles. The grinding. The drilling. The rinsing. The spitting. The throbbing copays.
But you know what might inject a few cc’s of fun into your oral hygiene visits?
Did you guess ... a hoverboard?
If you did, well, you’re probably dentist Steve Martin in “Little Shop of Horrors.” Or perhaps Alaska dentist Seth Lookhart, who authorities say performed a tooth extraction on a sedated patient while Dr. Lookhart also rode a hoverboard. There are also charges of felony Medicaid fraud and reckless endangerment. And allegations of hefty theft from his practice partners. Oh, and a state board apparently suspended Dr. Lookhart’s dental license in 2017.
But hey, pulling teeth while taming a hoverboard? Photos or it didn’t happen, right?
Unfortunately for the well-balanced dentist, there are photos. Actually, there’s an entire video. And when prosecutors showed it to Dr. Lookhart’s unwitting and horrified costar, she was about as happy as the impacted wisdom teeth your teen kid’s still toting around.
Dr. Lookhart denied the felony fraud charges. But he did cop to the hoverboard. Which puts him one up on his cinematic “Wild and Crazy Guy” doppelganger. Even as a neurosurgeon in “The Man With Two Brains,” Mr. Martin never attempted to hoverboard while performing double “cranial screw-top” brain surgeries.
CSI: Quebec
They may live in that eternally polite land on the other side of our northern border, but they know where the bodies are buried. Lots of bodies. Some of them in shallow graves. Some of them in vehicles.
No, we are not talking about Gil Grissom and the gang at CSI. We’re talking about the Secure Site for Research in Thanatology, also known as the “body farm,” which is scheduled to open this spring in Becancour, Quebec.
It’s the first such outdoor forensic facility in Canada and the first in the world – there are also body farms in the United States, Australia, and the Netherlands – to be located in a northern climate.
“We’re particularly interested in understanding what happens when a body is in subzero temperatures, when there’s a lot of snow on the ground, and how that freeze and then the thaw process might actually change the rate of decomposition,” Shari Forbes, the farm’s director, told CTV News recently.
The science team will be out on the farm every day, meticulously checking each body – talk about making a list and checking it twice – for all the important CSI stuff: how long fingerprints and DNA evidence last, the effects of insect feeding and egg-laying, and the ability of dogs to detect scents.
The decomposition process in a cold climate will be a strange and wondrous journey, and the body farm’s work can, perhaps, best be summed up by none other than Mr. Grissom, who once said that getting to the evidence means having to destroy the evidence.
Then again, he also said that “dead men don’t ride roller coasters,” so the analogy only goes so far.
A cure for nosiness
Christmas may be just around the corner, but is there ever really a wrong time to huddle around a campfire and swap scary stories? So bundle up, get the fire going, and prepare yourselves for a pair of nasal-based horror stories that will frighten your Jingle Bells off!
Our first tale of nostril terror comes all the way from southern India, where a 13-year-old boy jumped into a water well to cool off. Hey, southern India gets hot, even in November. But like something out of a bad sci-fi movie, his peaceful swim was interrupted when something swam up his nose, causing him extreme pain. After a 30-minute procedure, the doctor pulled out the culprit: A horrific alien parasite! Okay, we’re lying; it was a fish. But we had you going, didn’t we?
Well, maybe that didn’t get you frightened. But we have more rhinal dread to share! A young girl in Las Vegas stuck a pair of plastic doll shoes up her nose, one in each nostril. Her mother removed one shoe, but neither she nor urgent care could reach the second. A trip to the hospital was in order, and once there, the doctors were able to remove the foreign object in seconds.
But as with all things in U.S. medicine, a reckoning would soon come. You feel it now, the dread in this woman’s heart when the hospital bill came.
She takes the envelope, and opens it slowly.
The paper unfolds, rough and heavy in her hands.
Her eyes scan the page, looking for the number, where is it, where is it? It must be here, it must be ...
$3,000.
That’s right, for this simple procedure, performed with a pair of fancy tweezers, the hospital saw fit to charge the hapless mother $3,000! AHHHHHHHHHHHH!
Some say that the mother’s high-deductible insurance policy reduced the cost to $1,700. But we ask you, does that make the story any less spooky? We think not.
Hoverboarding down the root canal
Time spent in the dentist’s chair is among the most anxiety-inducing in anyone’s life. The needles. The grinding. The drilling. The rinsing. The spitting. The throbbing copays.
But you know what might inject a few cc’s of fun into your oral hygiene visits?
Did you guess ... a hoverboard?
If you did, well, you’re probably dentist Steve Martin in “Little Shop of Horrors.” Or perhaps Alaska dentist Seth Lookhart, who authorities say performed a tooth extraction on a sedated patient while Dr. Lookhart also rode a hoverboard. There are also charges of felony Medicaid fraud and reckless endangerment. And allegations of hefty theft from his practice partners. Oh, and a state board apparently suspended Dr. Lookhart’s dental license in 2017.
But hey, pulling teeth while taming a hoverboard? Photos or it didn’t happen, right?
Unfortunately for the well-balanced dentist, there are photos. Actually, there’s an entire video. And when prosecutors showed it to Dr. Lookhart’s unwitting and horrified costar, she was about as happy as the impacted wisdom teeth your teen kid’s still toting around.
Dr. Lookhart denied the felony fraud charges. But he did cop to the hoverboard. Which puts him one up on his cinematic “Wild and Crazy Guy” doppelganger. Even as a neurosurgeon in “The Man With Two Brains,” Mr. Martin never attempted to hoverboard while performing double “cranial screw-top” brain surgeries.
CSI: Quebec
They may live in that eternally polite land on the other side of our northern border, but they know where the bodies are buried. Lots of bodies. Some of them in shallow graves. Some of them in vehicles.
No, we are not talking about Gil Grissom and the gang at CSI. We’re talking about the Secure Site for Research in Thanatology, also known as the “body farm,” which is scheduled to open this spring in Becancour, Quebec.
It’s the first such outdoor forensic facility in Canada and the first in the world – there are also body farms in the United States, Australia, and the Netherlands – to be located in a northern climate.
“We’re particularly interested in understanding what happens when a body is in subzero temperatures, when there’s a lot of snow on the ground, and how that freeze and then the thaw process might actually change the rate of decomposition,” Shari Forbes, the farm’s director, told CTV News recently.
The science team will be out on the farm every day, meticulously checking each body – talk about making a list and checking it twice – for all the important CSI stuff: how long fingerprints and DNA evidence last, the effects of insect feeding and egg-laying, and the ability of dogs to detect scents.
The decomposition process in a cold climate will be a strange and wondrous journey, and the body farm’s work can, perhaps, best be summed up by none other than Mr. Grissom, who once said that getting to the evidence means having to destroy the evidence.
Then again, he also said that “dead men don’t ride roller coasters,” so the analogy only goes so far.
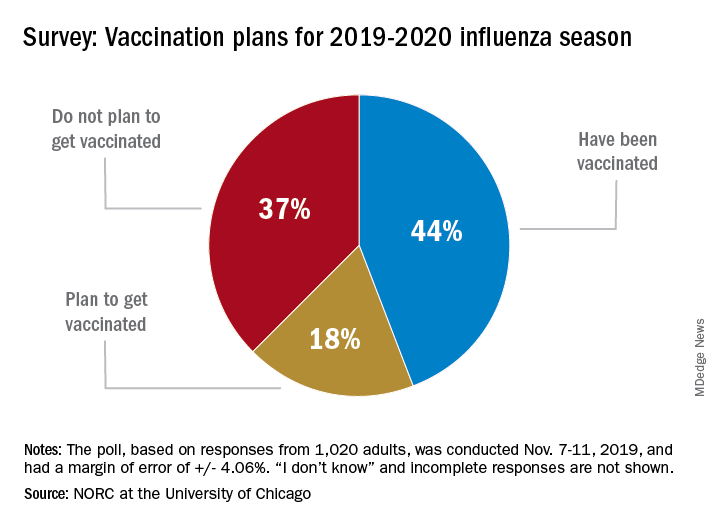
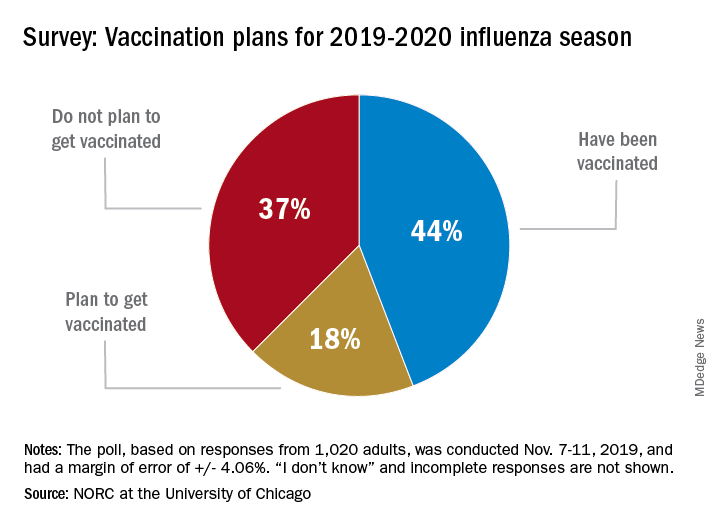
Many Americans planning to avoid flu vaccination
As the 2019-20 flu season got underway, more than half of American adults had not yet been vaccinated, according to a survey from the research organization NORC at the University of Chicago.
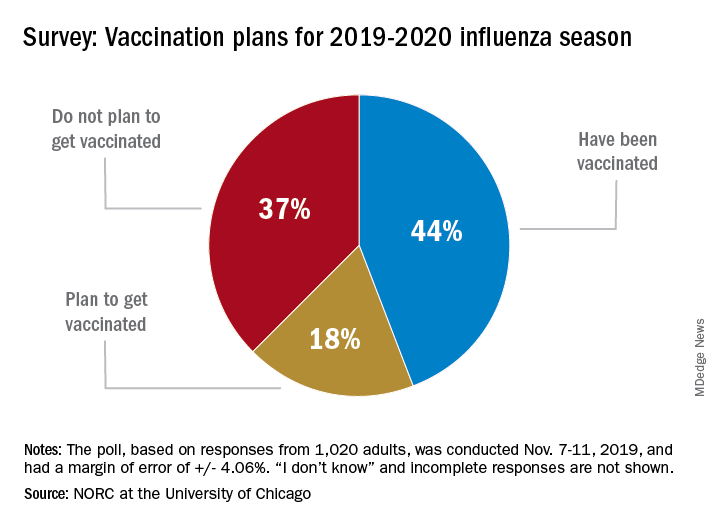
Only 44% of the 1,020 adults surveyed said that they had already received the vaccine as of Nov. 7-11, when the poll was conducted. Another the NORC reported. About 1% of those surveyed said they didn’t know or skipped the question.
Age was a strong determinant of vaccination status: 35% of those aged 18-29 years had gotten their flu shot, along with 36% of respondents aged 30-44 years and 34% of those aged 45- 59 years, compared with 65% of those aged 60 years and older. Of the respondents with children under age 18 years, 43% said that they were not planning to have the children vaccinated, the NORC said.
Concern about side effects, mentioned by 37% of those who were not planning to get vaccinated, was the most common reason given to avoid a flu shot, followed by belief that the vaccine doesn’t work very well (36%) and “never get the flu” (26%), the survey results showed.
“Widespread misconceptions exist regarding the safety and efficacy of flu shots. Because of the way the flu spreads in a community, failing to get a vaccination not only puts you at risk but also others for whom the consequences of the flu can be severe. Policymakers should focus on changing erroneous beliefs about immunizing against the flu,” said Caitlin Oppenheimer, who is senior vice president of public health research for the NORC, which has conducted the National Immunization Survey for the Centers for Disease Control and Prevention since 2005.
As the 2019-20 flu season got underway, more than half of American adults had not yet been vaccinated, according to a survey from the research organization NORC at the University of Chicago.
Only 44% of the 1,020 adults surveyed said that they had already received the vaccine as of Nov. 7-11, when the poll was conducted. Another the NORC reported. About 1% of those surveyed said they didn’t know or skipped the question.
Age was a strong determinant of vaccination status: 35% of those aged 18-29 years had gotten their flu shot, along with 36% of respondents aged 30-44 years and 34% of those aged 45- 59 years, compared with 65% of those aged 60 years and older. Of the respondents with children under age 18 years, 43% said that they were not planning to have the children vaccinated, the NORC said.
Concern about side effects, mentioned by 37% of those who were not planning to get vaccinated, was the most common reason given to avoid a flu shot, followed by belief that the vaccine doesn’t work very well (36%) and “never get the flu” (26%), the survey results showed.
“Widespread misconceptions exist regarding the safety and efficacy of flu shots. Because of the way the flu spreads in a community, failing to get a vaccination not only puts you at risk but also others for whom the consequences of the flu can be severe. Policymakers should focus on changing erroneous beliefs about immunizing against the flu,” said Caitlin Oppenheimer, who is senior vice president of public health research for the NORC, which has conducted the National Immunization Survey for the Centers for Disease Control and Prevention since 2005.
As the 2019-20 flu season got underway, more than half of American adults had not yet been vaccinated, according to a survey from the research organization NORC at the University of Chicago.
Only 44% of the 1,020 adults surveyed said that they had already received the vaccine as of Nov. 7-11, when the poll was conducted. Another the NORC reported. About 1% of those surveyed said they didn’t know or skipped the question.
Age was a strong determinant of vaccination status: 35% of those aged 18-29 years had gotten their flu shot, along with 36% of respondents aged 30-44 years and 34% of those aged 45- 59 years, compared with 65% of those aged 60 years and older. Of the respondents with children under age 18 years, 43% said that they were not planning to have the children vaccinated, the NORC said.
Concern about side effects, mentioned by 37% of those who were not planning to get vaccinated, was the most common reason given to avoid a flu shot, followed by belief that the vaccine doesn’t work very well (36%) and “never get the flu” (26%), the survey results showed.
“Widespread misconceptions exist regarding the safety and efficacy of flu shots. Because of the way the flu spreads in a community, failing to get a vaccination not only puts you at risk but also others for whom the consequences of the flu can be severe. Policymakers should focus on changing erroneous beliefs about immunizing against the flu,” said Caitlin Oppenheimer, who is senior vice president of public health research for the NORC, which has conducted the National Immunization Survey for the Centers for Disease Control and Prevention since 2005.
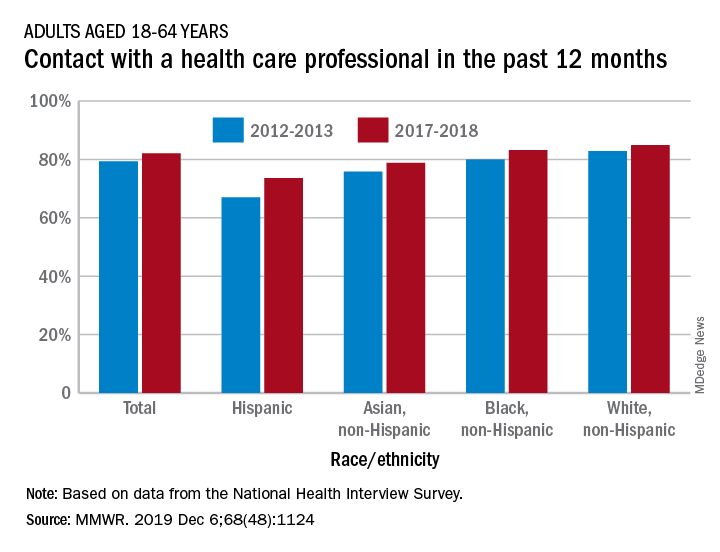
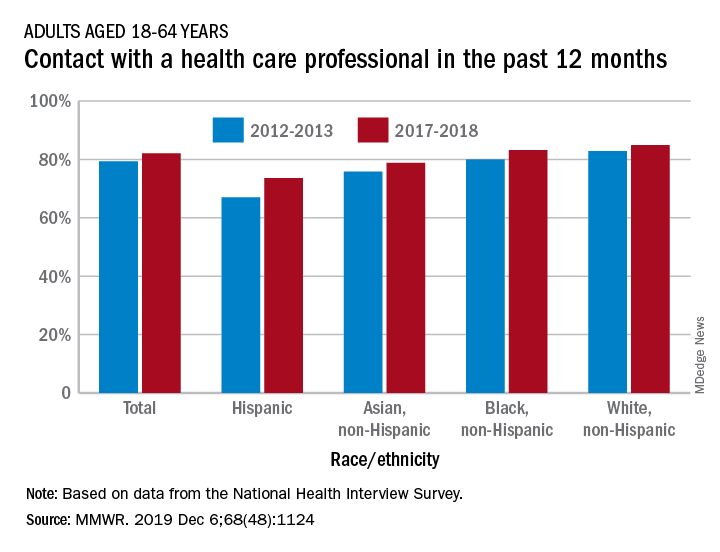
Contacts with health care professionals increased among adults
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
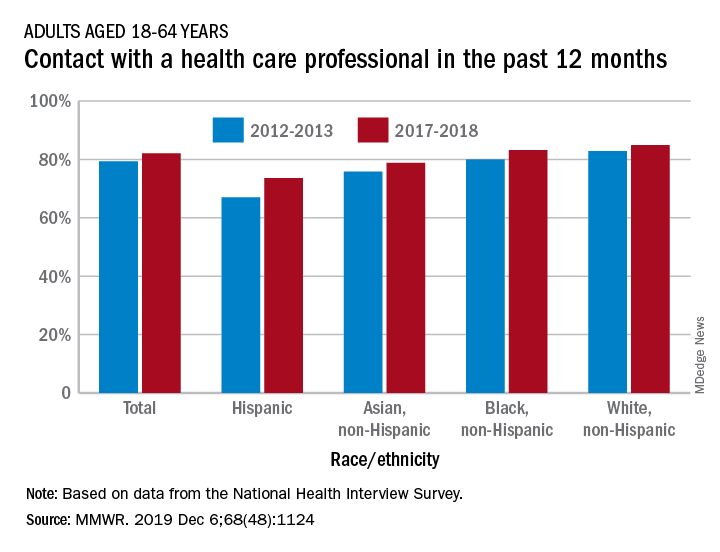
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Influenza already in midseason form
It’s been a decade since flu activity levels were this high this early in the season.

For the week ending Nov. 30, outpatient visits for influenza-like illness reached 3.5% of all visits to health care providers, the Centers for Disease Control and Prevention reported Dec. 6. That is the highest pre-December rate since the pandemic of 2009-2010, when the rate peaked at 7.7% in mid-October, CDC data show.
For the last week of November, eight states and Puerto Rico reported activity levels at the high point of the CDC’s 1-10 scale, which is at least five more states than any of the past five flu seasons. Three of the last five seasons had no states at level 10 this early in the season.
Another 4 states at levels 8 and 9 put a total of 13 jurisdictions in the “high” range of flu activity, with another 14 states in the “moderate” range of levels 6 and 7. Geographically speaking, 24 jurisdictions are experiencing regional or widespread activity, which is up from the 15 reported last week, the CDC’s influenza division said.
The hospitalization rate to date for the 2019-2020 season – 2.7 per 100,000 population – is “similar to what has been seen at this time during other recent seasons,” the CDC said.
One influenza-related pediatric death was reported during the week ending Nov. 30, which brings the total for the season to six, according to the CDC report.
It’s been a decade since flu activity levels were this high this early in the season.

For the week ending Nov. 30, outpatient visits for influenza-like illness reached 3.5% of all visits to health care providers, the Centers for Disease Control and Prevention reported Dec. 6. That is the highest pre-December rate since the pandemic of 2009-2010, when the rate peaked at 7.7% in mid-October, CDC data show.
For the last week of November, eight states and Puerto Rico reported activity levels at the high point of the CDC’s 1-10 scale, which is at least five more states than any of the past five flu seasons. Three of the last five seasons had no states at level 10 this early in the season.
Another 4 states at levels 8 and 9 put a total of 13 jurisdictions in the “high” range of flu activity, with another 14 states in the “moderate” range of levels 6 and 7. Geographically speaking, 24 jurisdictions are experiencing regional or widespread activity, which is up from the 15 reported last week, the CDC’s influenza division said.
The hospitalization rate to date for the 2019-2020 season – 2.7 per 100,000 population – is “similar to what has been seen at this time during other recent seasons,” the CDC said.
One influenza-related pediatric death was reported during the week ending Nov. 30, which brings the total for the season to six, according to the CDC report.
It’s been a decade since flu activity levels were this high this early in the season.

For the week ending Nov. 30, outpatient visits for influenza-like illness reached 3.5% of all visits to health care providers, the Centers for Disease Control and Prevention reported Dec. 6. That is the highest pre-December rate since the pandemic of 2009-2010, when the rate peaked at 7.7% in mid-October, CDC data show.
For the last week of November, eight states and Puerto Rico reported activity levels at the high point of the CDC’s 1-10 scale, which is at least five more states than any of the past five flu seasons. Three of the last five seasons had no states at level 10 this early in the season.
Another 4 states at levels 8 and 9 put a total of 13 jurisdictions in the “high” range of flu activity, with another 14 states in the “moderate” range of levels 6 and 7. Geographically speaking, 24 jurisdictions are experiencing regional or widespread activity, which is up from the 15 reported last week, the CDC’s influenza division said.
The hospitalization rate to date for the 2019-2020 season – 2.7 per 100,000 population – is “similar to what has been seen at this time during other recent seasons,” the CDC said.
One influenza-related pediatric death was reported during the week ending Nov. 30, which brings the total for the season to six, according to the CDC report.







