User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Suicide rate higher than average for female clinicians
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
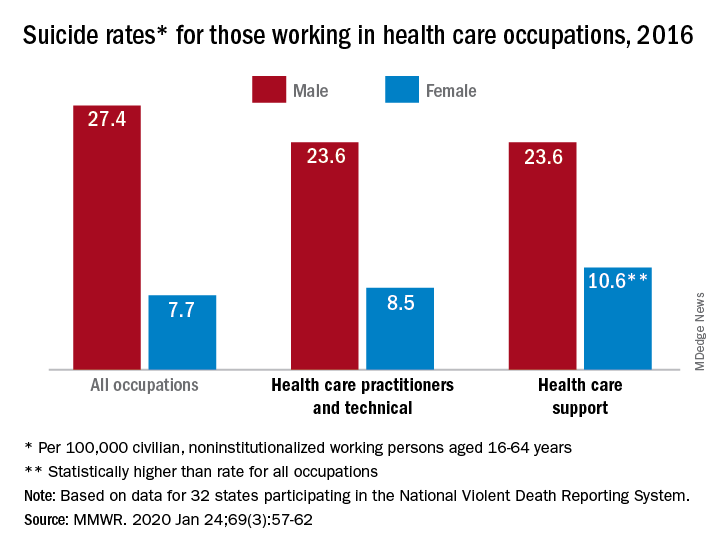
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
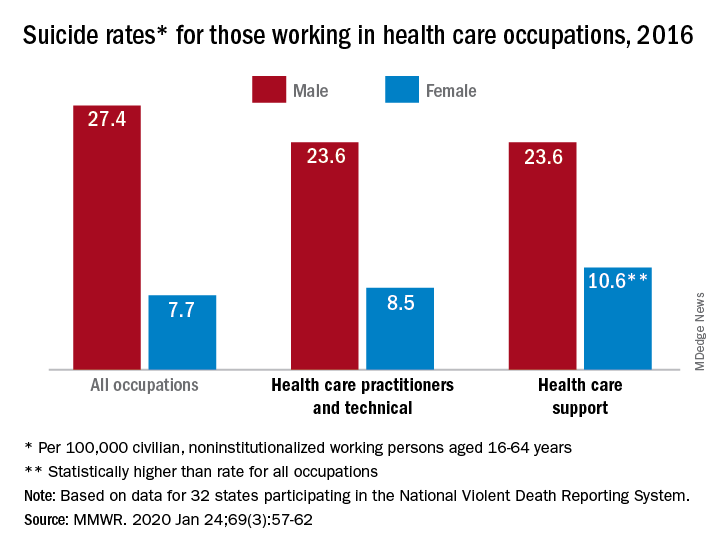
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
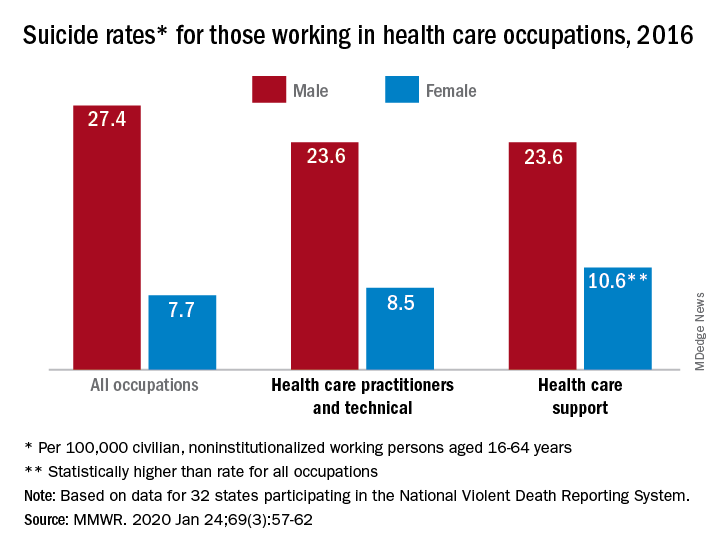
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
FROM MMWR
The age of maximum misery, and why Marcus Welby was gray
A year to forget
47.2. Just another number, right? Nothing too special about it. But this innocent number is hiding a deep, dark secret. It is the number of misery.
More specifically, 47.2 is the age when human misery hits its peak, according to a study distributed by the National Bureau of Economic Research.
The data, collected from 132 countries, show that human happiness is actually U-shaped. We all start out pretty happy, you know, being infants and all. Sadly, life takes a pretty sharp downhill turn when we’re born, and that slide doesn’t abate until the magic age of 47.2. That’s the point in our lives when we’re at our most unhappy.
We do have some good news if you happen to have been born in early November 1972 and you’re having a rough time of things lately. That U-shaped curve will be your friend from now on, as your happiness will, according to the data at least, grow constantly from this point forward. Once you get past 70, at least in the United States, you’ll be as happy as you’ve ever been in your adult life.
Of course, that’s not much comfort for those of us who’ve yet to hit that magic number. So if you thought the daily existential crises were bad now, just wait: Apparently, they’ll only get worse. Won’t that be fun?
Why Marcus Welby was gray
Stress is a key ingredient in the Bureau of LOTME’s recipe for success. The deadlines. The office coffee. The serial commas. And what do we get for all that stress? Other than fan mail (thanks, Mom) and cease-and-desist orders?
Gray hair.
Is the correlation coefficient between stress and our silvering LOTME coifs truly zero? We think not. And now science agrees: Stress may indeed be gray hair’s follicular fertilizer.
Harvard University scientists say they’ve mapped the path from after-hours EHR data entry to premature silver fox status. Specifically, like a pharma rep with a new drug to detail, stress wears on nerves, which help spew norepinephrine and deplete the stem cells that regenerate your hair follicles’ pigment cells. Presto! You’ve got gray hair and a med closet bursting with more drug samples.
More accurately, the Harvard researchers found that stress damages the color-restorative function in the hair of mice. Which means 92-year-old Mickey Mouse is clearly hiding a dye job. (Ed. note: C’mon, people – another Disney cease-and-desist letter?)
We know no one knows stress as intimately as physicians. That’s why we’re planning a complete line of hair coloring products we call “Just for Docs,” featuring colors like “Pre-Auth Platinum Blonde,” “MOC Magenta,” and “EHR Red.” And, of course, “Burnout Brunette.”
Mr. Bedbug goes to Washington
You’ve heard it a million times: The old good news/bad news delivery.
Well, make that a million and one, because it’s time to play “Good news is bad news!”
Good news: Baltimore is no longer the bedbug capital of the United States. Bad news: It only dropped from first to second place on Orkin’s Top 50 Bed Bug Cities list. More bad news: Washington, D.C., the capital of the United States, is now the bedbug capital as well. [Insert joke about Congress here.]
Good news: Kids in England are getting less sugar and salt in their packed school lunches than they did a decade ago. Bad news: They are also getting less vitamin A, vitamin C, and fruit, according to a study in BMJ Open.
Good news: Drinking skim or 1% milk instead of 2% can add more than 4 years to your life, and the reduction in lifespan is even greater for whole milk. Bad news: “Children who drink whole milk are actually 40% less likely to be obese or overweight than kids drinking reduced-fat milk,” Study Finds reported.
Wait a second. That’s not exactly bad news, is it? Maybe for those who are drinking low-fat milk to add a few years to their lives. They will live longer, but they’ll be overweight while they’re doing it.
Thank you for watching “Good news is bad news.” Remember, if you’re not confused, you haven’t been paying attention.
A year to forget
47.2. Just another number, right? Nothing too special about it. But this innocent number is hiding a deep, dark secret. It is the number of misery.
More specifically, 47.2 is the age when human misery hits its peak, according to a study distributed by the National Bureau of Economic Research.
The data, collected from 132 countries, show that human happiness is actually U-shaped. We all start out pretty happy, you know, being infants and all. Sadly, life takes a pretty sharp downhill turn when we’re born, and that slide doesn’t abate until the magic age of 47.2. That’s the point in our lives when we’re at our most unhappy.
We do have some good news if you happen to have been born in early November 1972 and you’re having a rough time of things lately. That U-shaped curve will be your friend from now on, as your happiness will, according to the data at least, grow constantly from this point forward. Once you get past 70, at least in the United States, you’ll be as happy as you’ve ever been in your adult life.
Of course, that’s not much comfort for those of us who’ve yet to hit that magic number. So if you thought the daily existential crises were bad now, just wait: Apparently, they’ll only get worse. Won’t that be fun?
Why Marcus Welby was gray
Stress is a key ingredient in the Bureau of LOTME’s recipe for success. The deadlines. The office coffee. The serial commas. And what do we get for all that stress? Other than fan mail (thanks, Mom) and cease-and-desist orders?
Gray hair.
Is the correlation coefficient between stress and our silvering LOTME coifs truly zero? We think not. And now science agrees: Stress may indeed be gray hair’s follicular fertilizer.
Harvard University scientists say they’ve mapped the path from after-hours EHR data entry to premature silver fox status. Specifically, like a pharma rep with a new drug to detail, stress wears on nerves, which help spew norepinephrine and deplete the stem cells that regenerate your hair follicles’ pigment cells. Presto! You’ve got gray hair and a med closet bursting with more drug samples.
More accurately, the Harvard researchers found that stress damages the color-restorative function in the hair of mice. Which means 92-year-old Mickey Mouse is clearly hiding a dye job. (Ed. note: C’mon, people – another Disney cease-and-desist letter?)
We know no one knows stress as intimately as physicians. That’s why we’re planning a complete line of hair coloring products we call “Just for Docs,” featuring colors like “Pre-Auth Platinum Blonde,” “MOC Magenta,” and “EHR Red.” And, of course, “Burnout Brunette.”
Mr. Bedbug goes to Washington
You’ve heard it a million times: The old good news/bad news delivery.
Well, make that a million and one, because it’s time to play “Good news is bad news!”
Good news: Baltimore is no longer the bedbug capital of the United States. Bad news: It only dropped from first to second place on Orkin’s Top 50 Bed Bug Cities list. More bad news: Washington, D.C., the capital of the United States, is now the bedbug capital as well. [Insert joke about Congress here.]
Good news: Kids in England are getting less sugar and salt in their packed school lunches than they did a decade ago. Bad news: They are also getting less vitamin A, vitamin C, and fruit, according to a study in BMJ Open.
Good news: Drinking skim or 1% milk instead of 2% can add more than 4 years to your life, and the reduction in lifespan is even greater for whole milk. Bad news: “Children who drink whole milk are actually 40% less likely to be obese or overweight than kids drinking reduced-fat milk,” Study Finds reported.
Wait a second. That’s not exactly bad news, is it? Maybe for those who are drinking low-fat milk to add a few years to their lives. They will live longer, but they’ll be overweight while they’re doing it.
Thank you for watching “Good news is bad news.” Remember, if you’re not confused, you haven’t been paying attention.
A year to forget
47.2. Just another number, right? Nothing too special about it. But this innocent number is hiding a deep, dark secret. It is the number of misery.
More specifically, 47.2 is the age when human misery hits its peak, according to a study distributed by the National Bureau of Economic Research.
The data, collected from 132 countries, show that human happiness is actually U-shaped. We all start out pretty happy, you know, being infants and all. Sadly, life takes a pretty sharp downhill turn when we’re born, and that slide doesn’t abate until the magic age of 47.2. That’s the point in our lives when we’re at our most unhappy.
We do have some good news if you happen to have been born in early November 1972 and you’re having a rough time of things lately. That U-shaped curve will be your friend from now on, as your happiness will, according to the data at least, grow constantly from this point forward. Once you get past 70, at least in the United States, you’ll be as happy as you’ve ever been in your adult life.
Of course, that’s not much comfort for those of us who’ve yet to hit that magic number. So if you thought the daily existential crises were bad now, just wait: Apparently, they’ll only get worse. Won’t that be fun?
Why Marcus Welby was gray
Stress is a key ingredient in the Bureau of LOTME’s recipe for success. The deadlines. The office coffee. The serial commas. And what do we get for all that stress? Other than fan mail (thanks, Mom) and cease-and-desist orders?
Gray hair.
Is the correlation coefficient between stress and our silvering LOTME coifs truly zero? We think not. And now science agrees: Stress may indeed be gray hair’s follicular fertilizer.
Harvard University scientists say they’ve mapped the path from after-hours EHR data entry to premature silver fox status. Specifically, like a pharma rep with a new drug to detail, stress wears on nerves, which help spew norepinephrine and deplete the stem cells that regenerate your hair follicles’ pigment cells. Presto! You’ve got gray hair and a med closet bursting with more drug samples.
More accurately, the Harvard researchers found that stress damages the color-restorative function in the hair of mice. Which means 92-year-old Mickey Mouse is clearly hiding a dye job. (Ed. note: C’mon, people – another Disney cease-and-desist letter?)
We know no one knows stress as intimately as physicians. That’s why we’re planning a complete line of hair coloring products we call “Just for Docs,” featuring colors like “Pre-Auth Platinum Blonde,” “MOC Magenta,” and “EHR Red.” And, of course, “Burnout Brunette.”
Mr. Bedbug goes to Washington
You’ve heard it a million times: The old good news/bad news delivery.
Well, make that a million and one, because it’s time to play “Good news is bad news!”
Good news: Baltimore is no longer the bedbug capital of the United States. Bad news: It only dropped from first to second place on Orkin’s Top 50 Bed Bug Cities list. More bad news: Washington, D.C., the capital of the United States, is now the bedbug capital as well. [Insert joke about Congress here.]
Good news: Kids in England are getting less sugar and salt in their packed school lunches than they did a decade ago. Bad news: They are also getting less vitamin A, vitamin C, and fruit, according to a study in BMJ Open.
Good news: Drinking skim or 1% milk instead of 2% can add more than 4 years to your life, and the reduction in lifespan is even greater for whole milk. Bad news: “Children who drink whole milk are actually 40% less likely to be obese or overweight than kids drinking reduced-fat milk,” Study Finds reported.
Wait a second. That’s not exactly bad news, is it? Maybe for those who are drinking low-fat milk to add a few years to their lives. They will live longer, but they’ll be overweight while they’re doing it.
Thank you for watching “Good news is bad news.” Remember, if you’re not confused, you haven’t been paying attention.
Flu activity declines for second straight week
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
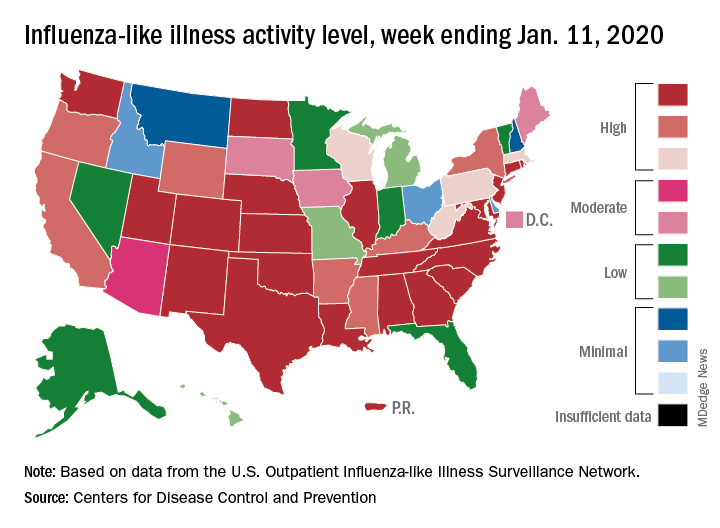
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
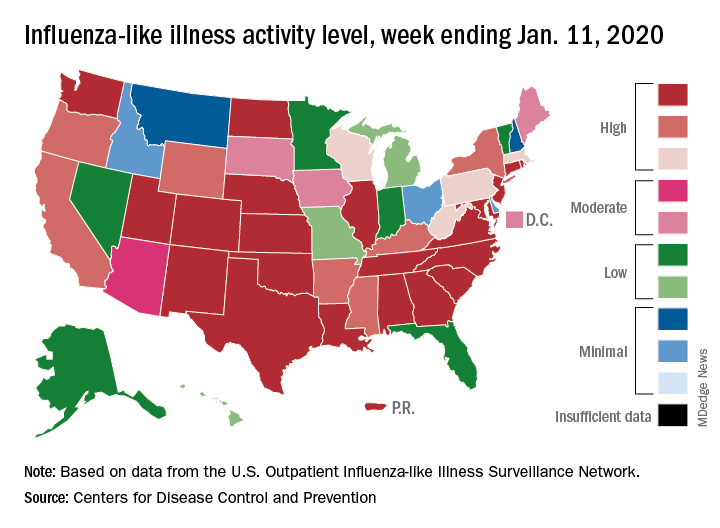
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
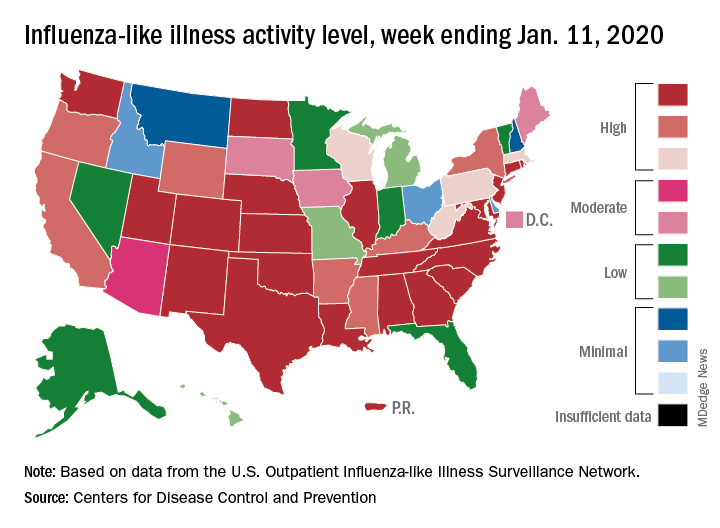
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Sleep apnea’s got your tongue, and singin’ in the kerosene rain
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
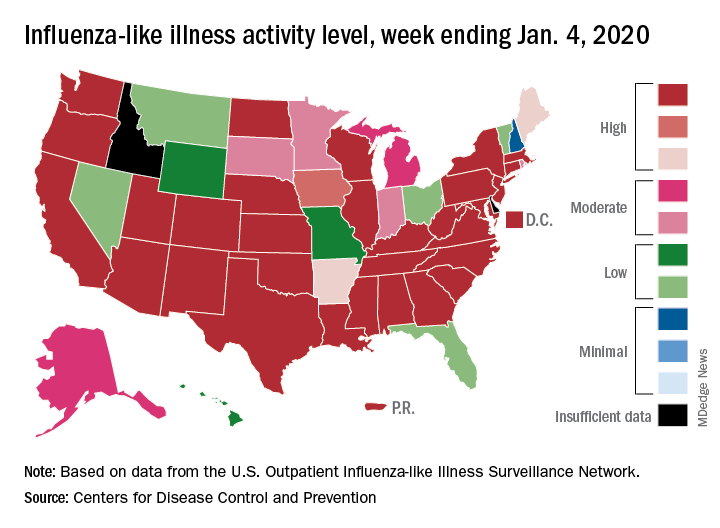
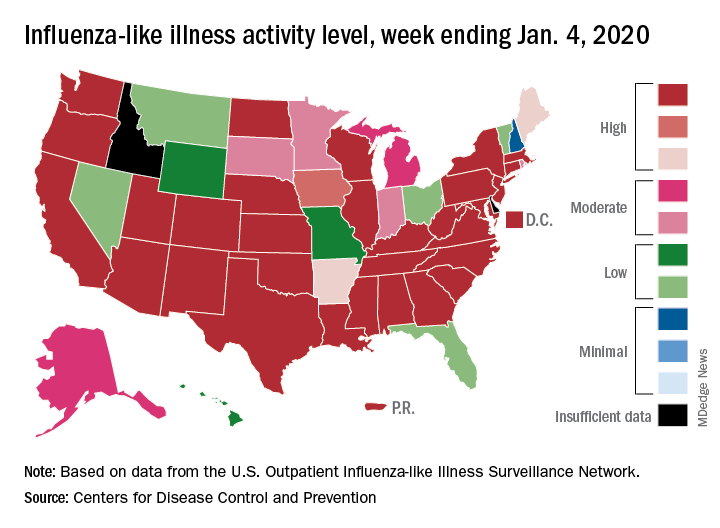
Drop in flu activity may not signal seasonal peak
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
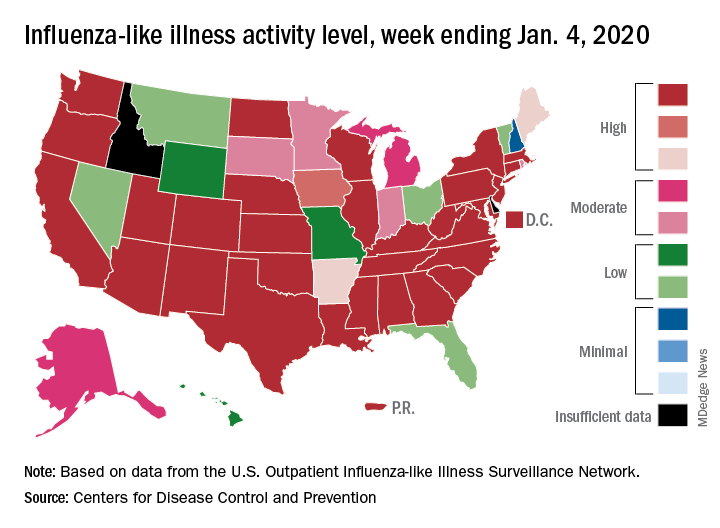
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
Oral lichen planus prevalence estimates go global
for the general population and 0.98% among clinical patients.
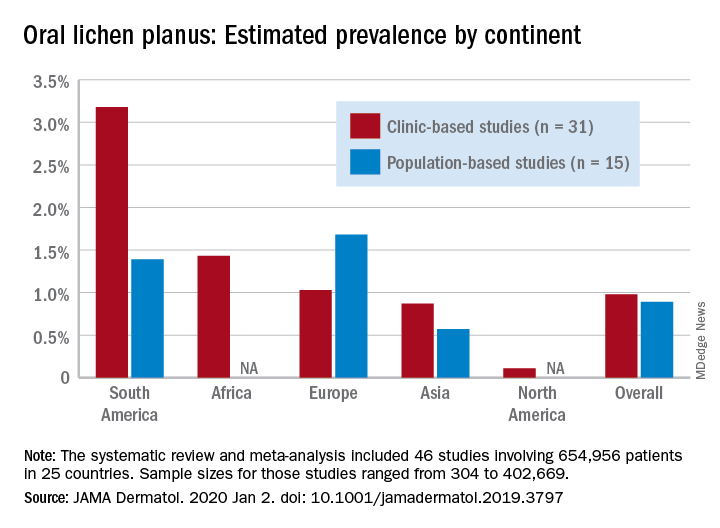
Globally, oral lichen planus (OLP) appears to be more prevalent in women than men (1.55% vs. 1.11% in population-based studies; 1.69% vs. 1.09% in clinic-based), in those aged 40 years and older (1.90% vs. 0.62% in clinic-based studies), and in non-Asian countries (see graph), Changchang Li, MD, and associates reported in JAMA Dermatology.
Of the 25 countries represented among the 46 included studies, Brazil had the highest OLP prevalence at 6.04% and India had the lowest at 0.02%. “Smokers and patients who abuse alcohol have a higher prevalence of OLP. This factor may explain why the highest prevalence … was found in Brazil, where 18.18% of residents report being smokers and 29.09% report consumption of alcoholic beverages,” wrote Dr. Li of the department of dermatology at Zhejiang University of Traditional Chinese Medicine, Wenzhou, China, and associates.
The difference in OLP prevalence by sex may be related to fluctuating female hormone levels, “especially during menstruation or menopause, and that different social roles may lead to the body being in a state of stress,” the investigators suggested.
The age-related difference in OLP could be the result of “longstanding oral habits” or changes to the oral mucosa over time, such as mucosal thinning, decreased elasticity, less saliva secretion, and greater tissue permeability. The higher prevalence among those aged 40 years and older also may be “associated with metabolic changes during aging or with decreased immunity, nutritional deficiencies, medication use, or denture wear,” they wrote.
The review and meta-analysis involved 15 studies (n = 462,993) that included general population data and 31 (n = 191,963) that used information from clinical patients. Sample sizes for those studies ranged from 308 to 402,669.
Statistically significant publication bias was seen among the clinic-based studies but not those that were population based, Dr. Li and associates wrote, adding that “our findings should be considered with caution because of the high heterogeneity of the included studies.”
The study was funded by the First-Class Discipline Construction Foundation of Guangzhou University of Chinese Medicine, the Young Top Talent Project of Scientific and Technological Innovation in Special Support Plan for Training High-level Talents, and the Youth Research and Cultivation Project of Guangzhou University of Chinese Medicine. The investigators did not report any conflicts of interest.
SOURCE: C Li et al. JAMA Dermatol. 2020 Jan 2. doi: 10.1001/jamadermatol.2019.3797.
for the general population and 0.98% among clinical patients.
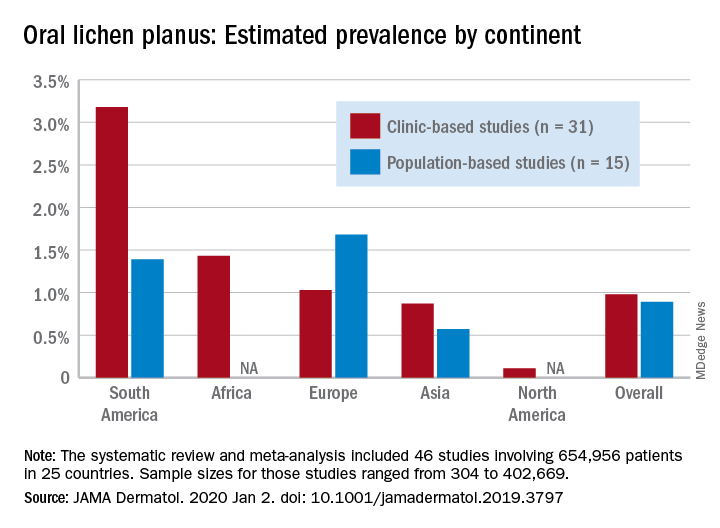
Globally, oral lichen planus (OLP) appears to be more prevalent in women than men (1.55% vs. 1.11% in population-based studies; 1.69% vs. 1.09% in clinic-based), in those aged 40 years and older (1.90% vs. 0.62% in clinic-based studies), and in non-Asian countries (see graph), Changchang Li, MD, and associates reported in JAMA Dermatology.
Of the 25 countries represented among the 46 included studies, Brazil had the highest OLP prevalence at 6.04% and India had the lowest at 0.02%. “Smokers and patients who abuse alcohol have a higher prevalence of OLP. This factor may explain why the highest prevalence … was found in Brazil, where 18.18% of residents report being smokers and 29.09% report consumption of alcoholic beverages,” wrote Dr. Li of the department of dermatology at Zhejiang University of Traditional Chinese Medicine, Wenzhou, China, and associates.
The difference in OLP prevalence by sex may be related to fluctuating female hormone levels, “especially during menstruation or menopause, and that different social roles may lead to the body being in a state of stress,” the investigators suggested.
The age-related difference in OLP could be the result of “longstanding oral habits” or changes to the oral mucosa over time, such as mucosal thinning, decreased elasticity, less saliva secretion, and greater tissue permeability. The higher prevalence among those aged 40 years and older also may be “associated with metabolic changes during aging or with decreased immunity, nutritional deficiencies, medication use, or denture wear,” they wrote.
The review and meta-analysis involved 15 studies (n = 462,993) that included general population data and 31 (n = 191,963) that used information from clinical patients. Sample sizes for those studies ranged from 308 to 402,669.
Statistically significant publication bias was seen among the clinic-based studies but not those that were population based, Dr. Li and associates wrote, adding that “our findings should be considered with caution because of the high heterogeneity of the included studies.”
The study was funded by the First-Class Discipline Construction Foundation of Guangzhou University of Chinese Medicine, the Young Top Talent Project of Scientific and Technological Innovation in Special Support Plan for Training High-level Talents, and the Youth Research and Cultivation Project of Guangzhou University of Chinese Medicine. The investigators did not report any conflicts of interest.
SOURCE: C Li et al. JAMA Dermatol. 2020 Jan 2. doi: 10.1001/jamadermatol.2019.3797.
for the general population and 0.98% among clinical patients.
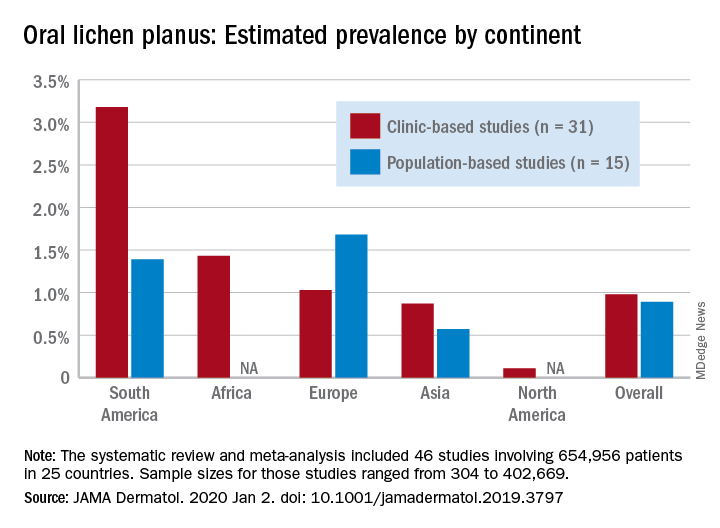
Globally, oral lichen planus (OLP) appears to be more prevalent in women than men (1.55% vs. 1.11% in population-based studies; 1.69% vs. 1.09% in clinic-based), in those aged 40 years and older (1.90% vs. 0.62% in clinic-based studies), and in non-Asian countries (see graph), Changchang Li, MD, and associates reported in JAMA Dermatology.
Of the 25 countries represented among the 46 included studies, Brazil had the highest OLP prevalence at 6.04% and India had the lowest at 0.02%. “Smokers and patients who abuse alcohol have a higher prevalence of OLP. This factor may explain why the highest prevalence … was found in Brazil, where 18.18% of residents report being smokers and 29.09% report consumption of alcoholic beverages,” wrote Dr. Li of the department of dermatology at Zhejiang University of Traditional Chinese Medicine, Wenzhou, China, and associates.
The difference in OLP prevalence by sex may be related to fluctuating female hormone levels, “especially during menstruation or menopause, and that different social roles may lead to the body being in a state of stress,” the investigators suggested.
The age-related difference in OLP could be the result of “longstanding oral habits” or changes to the oral mucosa over time, such as mucosal thinning, decreased elasticity, less saliva secretion, and greater tissue permeability. The higher prevalence among those aged 40 years and older also may be “associated with metabolic changes during aging or with decreased immunity, nutritional deficiencies, medication use, or denture wear,” they wrote.
The review and meta-analysis involved 15 studies (n = 462,993) that included general population data and 31 (n = 191,963) that used information from clinical patients. Sample sizes for those studies ranged from 308 to 402,669.
Statistically significant publication bias was seen among the clinic-based studies but not those that were population based, Dr. Li and associates wrote, adding that “our findings should be considered with caution because of the high heterogeneity of the included studies.”
The study was funded by the First-Class Discipline Construction Foundation of Guangzhou University of Chinese Medicine, the Young Top Talent Project of Scientific and Technological Innovation in Special Support Plan for Training High-level Talents, and the Youth Research and Cultivation Project of Guangzhou University of Chinese Medicine. The investigators did not report any conflicts of interest.
SOURCE: C Li et al. JAMA Dermatol. 2020 Jan 2. doi: 10.1001/jamadermatol.2019.3797.
FROM JAMA DERMATOLOGY
Invasion of the body-snatcher DNA, and pediatric ‘La Niña’s revenge’
A place for everything
Our editor – imagine a combination of Mitch McConnell and SpongeBob SquarePants – is a big fan of the year-in-review list and said we should do one. But he turned down our idea for “Top 10 reasons not to do a year-in-review list,” so we’re doing the next-best thing: reporting on someone else’s.
We came across a list on Vice.com that was right up our alley, so to speak: “What did we get stuck in our rectums last year?”
It’s the latest edition of an annual list compiled by Barry Petchesky, who says he’s “been chronicling our country’s cavity misadventures” for a decade using data from the U.S. Consumer Product Safety Commission’s National Electronic Injury Surveillance System (NEISS) database.
After you’re done here, we strongly urge you to check out Mr. Petchesky’s full list, which covers all of the major bodily orifices and is not limited to rectums. In the meantime, here are a few highlights, with quotes from the actual NEISS reports when necessary:
- Christmas ornament (ear).
- Egg timer (rectum).
- “Jumped off couch landed on spoon” (vagina).
- Christmas ornament (nose).
- Small shampoo bottle (rectum).
- Large shampoo bottle (rectum).
- Christmas ornament (throat).
- “Was using prostate massager & it got ‘sucked in’ ” (rectum).
- Coaxial cable (penis).
- Christmas ornament (rectum).
The weather stinks today
On the surface, the El Niño–Southern Oscillation isn’t the most impressive phenomenon in the world. The tropical eastern Pacific Ocean isn’t a small area, but there’s a lot of ocean out there, and the temperature difference from the norm during El Niño and its less well-known sister, La Niña, is only a few degrees.
But that blob of water can have massive effects on the world’s climate, causing drought and heat waves in some areas while being responsible for increased storms and massive amounts of rainfall and diarrhea in others.
“Wait, hang on – what was that last one?” you’re probably asking.
Yes, we’re going from “things stuck in our rectums” to “things very much not stuck in our rectums” thanks to a study published in Nature Communications. According to the researchers from Columbia University, La Niña (cooler water) is linked to increased diarrhea in young children in Botswana. During La Niña years, incidence of diarrhea in children aged 5 years or younger is 30% higher than in non–La Niña years.
It does make sense when you think about it. In southern Africa, La Niña is associated with cooler weather, increased rainfall, and more flooding during the rainy season. The aftermath of extreme rainfall events is often a breeding ground for waterborne pathogens. And so the diarrhea flows.
So, if you happen to be reading this from Botswana, pay attention to the news. If the meteorologists start talking about La Niña, you may want to stock up on oral rehydration salts and zinc.
Are two DNAs better than one?
Before you read any further, you need to find the X-Files theme to set the mood, so use this link and get it started.
Okay, is it on? No? That’s fine, we can wait.
Now are you ready? Good, here goes.
What happens after you receive a bone marrow transplant to treat acute myeloid leukemia? Many years of life, hopefully. But what if you survived and then started to turn into someone else? What if the DNA from the bone marrow donor started to replace your DNA?
Now you know why we needed the X-Files music.
Chris Long, who works at the Washoe County (Nev.) Sheriff’s Department, underwent a bone marrow transplant several years ago. Just before the procedure, a friend and colleague in the department, who just happened to run the crime lab, asked him for DNA samples.
Say, isn’t Area 51 in Nevada? Hmm, interesting.
A few months later, the lab determined that all of the DNA in his blood had been replaced by that of the bone marrow donor, the New York Times reported. And over the years, “swabs collected from his lip, cheek and tongue showed that these also contained his donor’s DNA, with the percentages rising and falling.”
Even more surprising? After 4 years, Mr. Long’s colleagues in the crime lab found that all of the DNA in his semen belonged to the donor, the Times said.
Mr. Long, it seems, has become a chimera, a combination of two people.
Guess what? There was an X-Files episode called “Chimera.”
Now, we’re not saying that all this proves aliens were involved, but … well … you know.
A place for everything
Our editor – imagine a combination of Mitch McConnell and SpongeBob SquarePants – is a big fan of the year-in-review list and said we should do one. But he turned down our idea for “Top 10 reasons not to do a year-in-review list,” so we’re doing the next-best thing: reporting on someone else’s.
We came across a list on Vice.com that was right up our alley, so to speak: “What did we get stuck in our rectums last year?”
It’s the latest edition of an annual list compiled by Barry Petchesky, who says he’s “been chronicling our country’s cavity misadventures” for a decade using data from the U.S. Consumer Product Safety Commission’s National Electronic Injury Surveillance System (NEISS) database.
After you’re done here, we strongly urge you to check out Mr. Petchesky’s full list, which covers all of the major bodily orifices and is not limited to rectums. In the meantime, here are a few highlights, with quotes from the actual NEISS reports when necessary:
- Christmas ornament (ear).
- Egg timer (rectum).
- “Jumped off couch landed on spoon” (vagina).
- Christmas ornament (nose).
- Small shampoo bottle (rectum).
- Large shampoo bottle (rectum).
- Christmas ornament (throat).
- “Was using prostate massager & it got ‘sucked in’ ” (rectum).
- Coaxial cable (penis).
- Christmas ornament (rectum).
The weather stinks today
On the surface, the El Niño–Southern Oscillation isn’t the most impressive phenomenon in the world. The tropical eastern Pacific Ocean isn’t a small area, but there’s a lot of ocean out there, and the temperature difference from the norm during El Niño and its less well-known sister, La Niña, is only a few degrees.
But that blob of water can have massive effects on the world’s climate, causing drought and heat waves in some areas while being responsible for increased storms and massive amounts of rainfall and diarrhea in others.
“Wait, hang on – what was that last one?” you’re probably asking.
Yes, we’re going from “things stuck in our rectums” to “things very much not stuck in our rectums” thanks to a study published in Nature Communications. According to the researchers from Columbia University, La Niña (cooler water) is linked to increased diarrhea in young children in Botswana. During La Niña years, incidence of diarrhea in children aged 5 years or younger is 30% higher than in non–La Niña years.
It does make sense when you think about it. In southern Africa, La Niña is associated with cooler weather, increased rainfall, and more flooding during the rainy season. The aftermath of extreme rainfall events is often a breeding ground for waterborne pathogens. And so the diarrhea flows.
So, if you happen to be reading this from Botswana, pay attention to the news. If the meteorologists start talking about La Niña, you may want to stock up on oral rehydration salts and zinc.
Are two DNAs better than one?
Before you read any further, you need to find the X-Files theme to set the mood, so use this link and get it started.
Okay, is it on? No? That’s fine, we can wait.
Now are you ready? Good, here goes.
What happens after you receive a bone marrow transplant to treat acute myeloid leukemia? Many years of life, hopefully. But what if you survived and then started to turn into someone else? What if the DNA from the bone marrow donor started to replace your DNA?
Now you know why we needed the X-Files music.
Chris Long, who works at the Washoe County (Nev.) Sheriff’s Department, underwent a bone marrow transplant several years ago. Just before the procedure, a friend and colleague in the department, who just happened to run the crime lab, asked him for DNA samples.
Say, isn’t Area 51 in Nevada? Hmm, interesting.
A few months later, the lab determined that all of the DNA in his blood had been replaced by that of the bone marrow donor, the New York Times reported. And over the years, “swabs collected from his lip, cheek and tongue showed that these also contained his donor’s DNA, with the percentages rising and falling.”
Even more surprising? After 4 years, Mr. Long’s colleagues in the crime lab found that all of the DNA in his semen belonged to the donor, the Times said.
Mr. Long, it seems, has become a chimera, a combination of two people.
Guess what? There was an X-Files episode called “Chimera.”
Now, we’re not saying that all this proves aliens were involved, but … well … you know.
A place for everything
Our editor – imagine a combination of Mitch McConnell and SpongeBob SquarePants – is a big fan of the year-in-review list and said we should do one. But he turned down our idea for “Top 10 reasons not to do a year-in-review list,” so we’re doing the next-best thing: reporting on someone else’s.
We came across a list on Vice.com that was right up our alley, so to speak: “What did we get stuck in our rectums last year?”
It’s the latest edition of an annual list compiled by Barry Petchesky, who says he’s “been chronicling our country’s cavity misadventures” for a decade using data from the U.S. Consumer Product Safety Commission’s National Electronic Injury Surveillance System (NEISS) database.
After you’re done here, we strongly urge you to check out Mr. Petchesky’s full list, which covers all of the major bodily orifices and is not limited to rectums. In the meantime, here are a few highlights, with quotes from the actual NEISS reports when necessary:
- Christmas ornament (ear).
- Egg timer (rectum).
- “Jumped off couch landed on spoon” (vagina).
- Christmas ornament (nose).
- Small shampoo bottle (rectum).
- Large shampoo bottle (rectum).
- Christmas ornament (throat).
- “Was using prostate massager & it got ‘sucked in’ ” (rectum).
- Coaxial cable (penis).
- Christmas ornament (rectum).
The weather stinks today
On the surface, the El Niño–Southern Oscillation isn’t the most impressive phenomenon in the world. The tropical eastern Pacific Ocean isn’t a small area, but there’s a lot of ocean out there, and the temperature difference from the norm during El Niño and its less well-known sister, La Niña, is only a few degrees.
But that blob of water can have massive effects on the world’s climate, causing drought and heat waves in some areas while being responsible for increased storms and massive amounts of rainfall and diarrhea in others.
“Wait, hang on – what was that last one?” you’re probably asking.
Yes, we’re going from “things stuck in our rectums” to “things very much not stuck in our rectums” thanks to a study published in Nature Communications. According to the researchers from Columbia University, La Niña (cooler water) is linked to increased diarrhea in young children in Botswana. During La Niña years, incidence of diarrhea in children aged 5 years or younger is 30% higher than in non–La Niña years.
It does make sense when you think about it. In southern Africa, La Niña is associated with cooler weather, increased rainfall, and more flooding during the rainy season. The aftermath of extreme rainfall events is often a breeding ground for waterborne pathogens. And so the diarrhea flows.
So, if you happen to be reading this from Botswana, pay attention to the news. If the meteorologists start talking about La Niña, you may want to stock up on oral rehydration salts and zinc.
Are two DNAs better than one?
Before you read any further, you need to find the X-Files theme to set the mood, so use this link and get it started.
Okay, is it on? No? That’s fine, we can wait.
Now are you ready? Good, here goes.
What happens after you receive a bone marrow transplant to treat acute myeloid leukemia? Many years of life, hopefully. But what if you survived and then started to turn into someone else? What if the DNA from the bone marrow donor started to replace your DNA?
Now you know why we needed the X-Files music.
Chris Long, who works at the Washoe County (Nev.) Sheriff’s Department, underwent a bone marrow transplant several years ago. Just before the procedure, a friend and colleague in the department, who just happened to run the crime lab, asked him for DNA samples.
Say, isn’t Area 51 in Nevada? Hmm, interesting.
A few months later, the lab determined that all of the DNA in his blood had been replaced by that of the bone marrow donor, the New York Times reported. And over the years, “swabs collected from his lip, cheek and tongue showed that these also contained his donor’s DNA, with the percentages rising and falling.”
Even more surprising? After 4 years, Mr. Long’s colleagues in the crime lab found that all of the DNA in his semen belonged to the donor, the Times said.
Mr. Long, it seems, has become a chimera, a combination of two people.
Guess what? There was an X-Files episode called “Chimera.”
Now, we’re not saying that all this proves aliens were involved, but … well … you know.
Flu records most active December since 2003
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
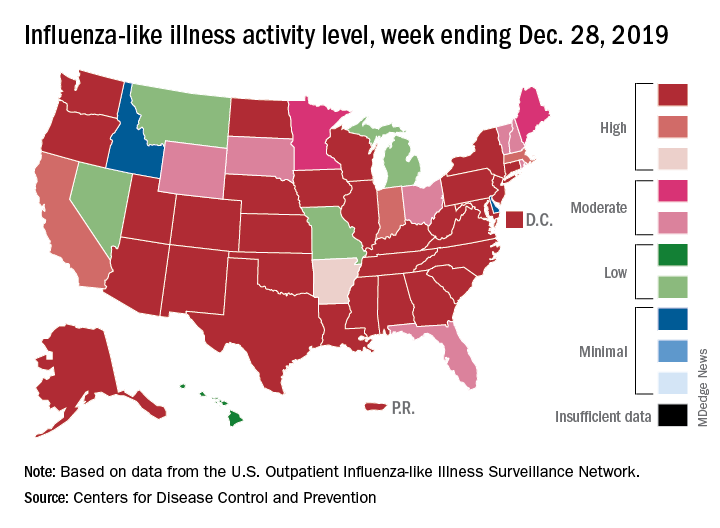
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
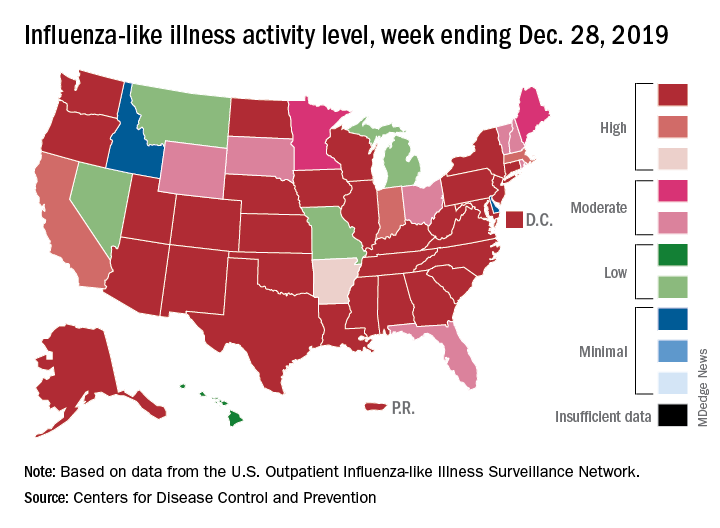
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
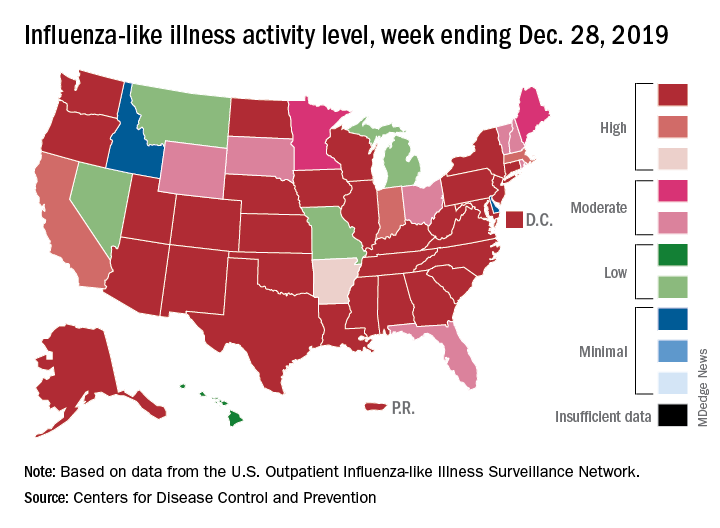
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
Vermont tops America’s Health Rankings for 2019
The award for healthiest state goes to Vermont in 2019, marking the fifth time the Green Mountain State has taken the top spot in the 30-year span of America’s Health Rankings.

The New England states took 3 of the top 5 spots and 4 of the top 10, while last year’s winner, Hawaii, dropped to third and missed out on the title for only the second time in the last 8 years, according to the America’s Heath Rankings annual report.
Another rankings tradition lived on, however, as Mississippi and Louisiana continued their battle to be the state with the “greatest opportunity for improvement.” In 2019, Mississippi managed to take that dishonor away from Louisiana, which had finished 50th in 2018. The two states have occupied the 49th and 50th spots in the rankings for the last 5 years, with Mississippi ahead 3-2 on 50th-place finishes, based on data from the AHR website.
Alaska (2019 rank, 27th), Virginia (15th), and Wyoming (19th) made the largest improvements, each moving up five spots since 2018, while Maine dropped from 16th to 21st for the largest decline among the states. A look back to the original rankings from 1990 puts New York on top of the list of improvers with a +29 over 30 years and shows Kansas to be the largest decliner with a change of –21, the report said.
At the national level, the report noted some key long-term health improvements and challenges:
- Smoking among adults is down 45% since 1990.
- Infant mortality declined by 43% and decreased in all 50 states.
- Diabetes prevalence has risen by 166% in adults since 1996.
- Obesity has increased by 166% since 1990.
The model used by AHR ranks states using 35 measures of public health in five broad categories: behaviors (Utah, 1st; La., 50th), community and environment (N.H., 1st; La. 50th), policy (Mass., 1st; Tex., 50th), clinical care (Mass., 1st; Miss. 50th), and health outcomes (Hawaii, 1st; Ala., 50th). Health measures include rates of excessive drinking, occupational fatalities, uninsured, preventable hospitalizations, and infant mortality.
America’s Health Rankings are produced by the American Public Health Association and the private, not-for-profit United Health Foundation, which was founded by UnitedHealth Group, operator of UnitedHealthcare.
The award for healthiest state goes to Vermont in 2019, marking the fifth time the Green Mountain State has taken the top spot in the 30-year span of America’s Health Rankings.

The New England states took 3 of the top 5 spots and 4 of the top 10, while last year’s winner, Hawaii, dropped to third and missed out on the title for only the second time in the last 8 years, according to the America’s Heath Rankings annual report.
Another rankings tradition lived on, however, as Mississippi and Louisiana continued their battle to be the state with the “greatest opportunity for improvement.” In 2019, Mississippi managed to take that dishonor away from Louisiana, which had finished 50th in 2018. The two states have occupied the 49th and 50th spots in the rankings for the last 5 years, with Mississippi ahead 3-2 on 50th-place finishes, based on data from the AHR website.
Alaska (2019 rank, 27th), Virginia (15th), and Wyoming (19th) made the largest improvements, each moving up five spots since 2018, while Maine dropped from 16th to 21st for the largest decline among the states. A look back to the original rankings from 1990 puts New York on top of the list of improvers with a +29 over 30 years and shows Kansas to be the largest decliner with a change of –21, the report said.
At the national level, the report noted some key long-term health improvements and challenges:
- Smoking among adults is down 45% since 1990.
- Infant mortality declined by 43% and decreased in all 50 states.
- Diabetes prevalence has risen by 166% in adults since 1996.
- Obesity has increased by 166% since 1990.
The model used by AHR ranks states using 35 measures of public health in five broad categories: behaviors (Utah, 1st; La., 50th), community and environment (N.H., 1st; La. 50th), policy (Mass., 1st; Tex., 50th), clinical care (Mass., 1st; Miss. 50th), and health outcomes (Hawaii, 1st; Ala., 50th). Health measures include rates of excessive drinking, occupational fatalities, uninsured, preventable hospitalizations, and infant mortality.
America’s Health Rankings are produced by the American Public Health Association and the private, not-for-profit United Health Foundation, which was founded by UnitedHealth Group, operator of UnitedHealthcare.
The award for healthiest state goes to Vermont in 2019, marking the fifth time the Green Mountain State has taken the top spot in the 30-year span of America’s Health Rankings.

The New England states took 3 of the top 5 spots and 4 of the top 10, while last year’s winner, Hawaii, dropped to third and missed out on the title for only the second time in the last 8 years, according to the America’s Heath Rankings annual report.
Another rankings tradition lived on, however, as Mississippi and Louisiana continued their battle to be the state with the “greatest opportunity for improvement.” In 2019, Mississippi managed to take that dishonor away from Louisiana, which had finished 50th in 2018. The two states have occupied the 49th and 50th spots in the rankings for the last 5 years, with Mississippi ahead 3-2 on 50th-place finishes, based on data from the AHR website.
Alaska (2019 rank, 27th), Virginia (15th), and Wyoming (19th) made the largest improvements, each moving up five spots since 2018, while Maine dropped from 16th to 21st for the largest decline among the states. A look back to the original rankings from 1990 puts New York on top of the list of improvers with a +29 over 30 years and shows Kansas to be the largest decliner with a change of –21, the report said.
At the national level, the report noted some key long-term health improvements and challenges:
- Smoking among adults is down 45% since 1990.
- Infant mortality declined by 43% and decreased in all 50 states.
- Diabetes prevalence has risen by 166% in adults since 1996.
- Obesity has increased by 166% since 1990.
The model used by AHR ranks states using 35 measures of public health in five broad categories: behaviors (Utah, 1st; La., 50th), community and environment (N.H., 1st; La. 50th), policy (Mass., 1st; Tex., 50th), clinical care (Mass., 1st; Miss. 50th), and health outcomes (Hawaii, 1st; Ala., 50th). Health measures include rates of excessive drinking, occupational fatalities, uninsured, preventable hospitalizations, and infant mortality.
America’s Health Rankings are produced by the American Public Health Association and the private, not-for-profit United Health Foundation, which was founded by UnitedHealth Group, operator of UnitedHealthcare.
Early increase in flu activity shows no signs of slowing
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
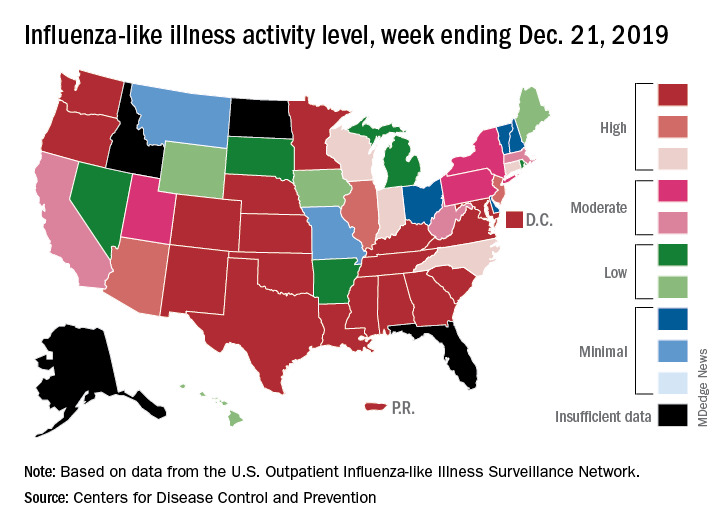
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.