User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Physicians pessimistic despite increased COVID-19 test kits
according to a survey.
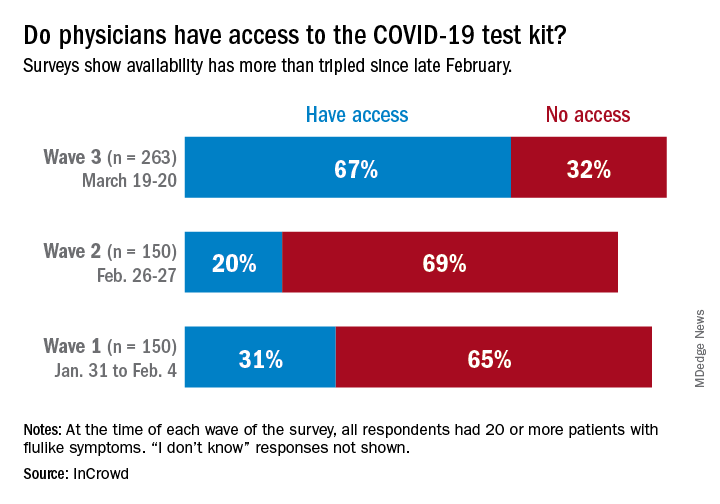
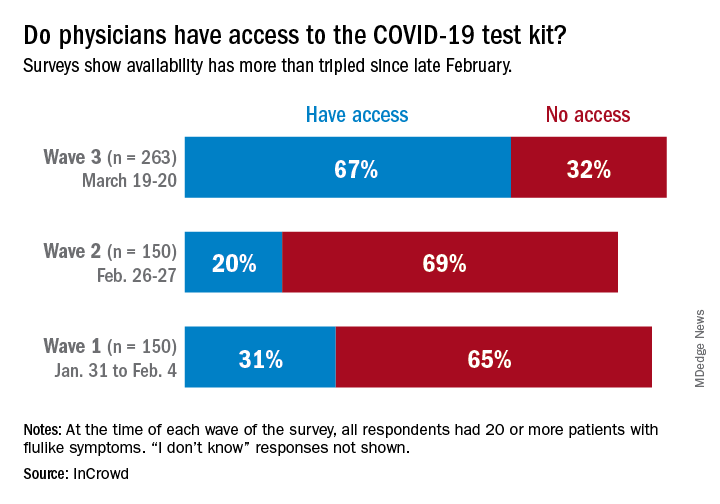
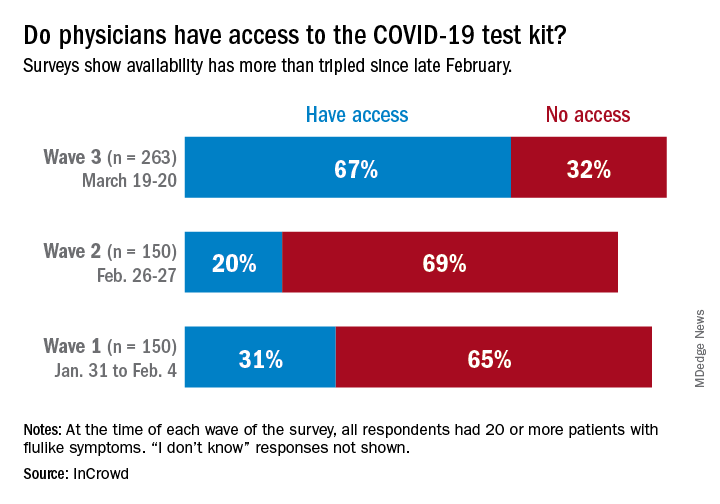
One positive finding from the physicians who participated in this survey March 19-20 was that the availability of COVID-19 test kits has more than doubled since late February.
Reported access to test kits went from 31% in the first wave of a series of surveys (Jan. 31–Feb. 4), down to 20% in the second (Feb. 26-27), and then jumped to 67% by the third wave (March 19-20), InCrowd reported March 26.
Views on several other COVID-related topics were negative among the majority of responding physicians – all of whom had or were currently treating 20 or more patients with flu-like symptoms at the time of the survey.
“Their frustrations and concerns about their ability to protect themselves while meeting upcoming patient care levels has increased significantly in the last 3 months,” Daniel S. Fitzgerald, CEO and president of InCrowd, said in a written statement.
In the third wave, 78% of respondents were “concerned for the safety of loved ones due to my exposure as a physician to COVID-19” and only 16% believed that their facility was “staffed adequately to treat the influx of patients anticipated in the next 30 days,” InCrowd said.
One primary care physician from California elaborated on the issue of safety equipment: “First, [the CDC] said we need N95 masks and other masks would not protect us. As those are running out then they said just use regular surgical masks. Now they are saying use bandannas and scarves! It’s like they don’t care about the safety of the people who will be treating the ill! We don’t want to bring it home to our families!”
“Overall, morale appears low, with few optimistic about the efficacy of public-private collaboration (21%), their own safety given current PPE [personal protective equipment] supply (13%), and the U.S.’s ability to ‘flatten the curve’ (12%),” InCrowd noted in the report.
The first two waves each had 150 respondents, but the number increased to 263 for wave 3, with similar proportions – about 50% emergency medicine or critical care specialists, 25% pediatricians, and 25% primary care physicians – in all three.
according to a survey.
One positive finding from the physicians who participated in this survey March 19-20 was that the availability of COVID-19 test kits has more than doubled since late February.
Reported access to test kits went from 31% in the first wave of a series of surveys (Jan. 31–Feb. 4), down to 20% in the second (Feb. 26-27), and then jumped to 67% by the third wave (March 19-20), InCrowd reported March 26.
Views on several other COVID-related topics were negative among the majority of responding physicians – all of whom had or were currently treating 20 or more patients with flu-like symptoms at the time of the survey.
“Their frustrations and concerns about their ability to protect themselves while meeting upcoming patient care levels has increased significantly in the last 3 months,” Daniel S. Fitzgerald, CEO and president of InCrowd, said in a written statement.
In the third wave, 78% of respondents were “concerned for the safety of loved ones due to my exposure as a physician to COVID-19” and only 16% believed that their facility was “staffed adequately to treat the influx of patients anticipated in the next 30 days,” InCrowd said.
One primary care physician from California elaborated on the issue of safety equipment: “First, [the CDC] said we need N95 masks and other masks would not protect us. As those are running out then they said just use regular surgical masks. Now they are saying use bandannas and scarves! It’s like they don’t care about the safety of the people who will be treating the ill! We don’t want to bring it home to our families!”
“Overall, morale appears low, with few optimistic about the efficacy of public-private collaboration (21%), their own safety given current PPE [personal protective equipment] supply (13%), and the U.S.’s ability to ‘flatten the curve’ (12%),” InCrowd noted in the report.
The first two waves each had 150 respondents, but the number increased to 263 for wave 3, with similar proportions – about 50% emergency medicine or critical care specialists, 25% pediatricians, and 25% primary care physicians – in all three.
according to a survey.
One positive finding from the physicians who participated in this survey March 19-20 was that the availability of COVID-19 test kits has more than doubled since late February.
Reported access to test kits went from 31% in the first wave of a series of surveys (Jan. 31–Feb. 4), down to 20% in the second (Feb. 26-27), and then jumped to 67% by the third wave (March 19-20), InCrowd reported March 26.
Views on several other COVID-related topics were negative among the majority of responding physicians – all of whom had or were currently treating 20 or more patients with flu-like symptoms at the time of the survey.
“Their frustrations and concerns about their ability to protect themselves while meeting upcoming patient care levels has increased significantly in the last 3 months,” Daniel S. Fitzgerald, CEO and president of InCrowd, said in a written statement.
In the third wave, 78% of respondents were “concerned for the safety of loved ones due to my exposure as a physician to COVID-19” and only 16% believed that their facility was “staffed adequately to treat the influx of patients anticipated in the next 30 days,” InCrowd said.
One primary care physician from California elaborated on the issue of safety equipment: “First, [the CDC] said we need N95 masks and other masks would not protect us. As those are running out then they said just use regular surgical masks. Now they are saying use bandannas and scarves! It’s like they don’t care about the safety of the people who will be treating the ill! We don’t want to bring it home to our families!”
“Overall, morale appears low, with few optimistic about the efficacy of public-private collaboration (21%), their own safety given current PPE [personal protective equipment] supply (13%), and the U.S.’s ability to ‘flatten the curve’ (12%),” InCrowd noted in the report.
The first two waves each had 150 respondents, but the number increased to 263 for wave 3, with similar proportions – about 50% emergency medicine or critical care specialists, 25% pediatricians, and 25% primary care physicians – in all three.
Elderly Americans carry heavier opioid burden
according to the Agency for Healthcare Quality and Research.

Elderly adults with chronic and acute pain obtained an average of 774 morphine milligram equivalents (MMEs) of prescription opioids annually during 2015-2016 from outpatient clinicians, compared with 376 MMEs a year for nonelderly adults, said Asako S. Moriya, PhD, and G. Edward Miller, PhD, of the AHRQ.
Narrowing the age groups shows that opioid MMEs increased with age, starting at 49 MMEs for 18- to 26-year-olds and rising to a high of 856 MMEs in the 65- to 74-year-old group, before dropping off in the oldest adults, the investigators said in a Medical Expenditure Panel Survey (MEPS) research findings report.
The analysis included “all opioid medications that are commonly used to treat pain” and excluded respiratory agents, antitussives, and drugs used for medication-assisted treatment, they noted. The MEPS data cover prescriptions purchased or obtained in outpatient settings but not those administered in inpatient settings or in clinics or physician offices.
according to the Agency for Healthcare Quality and Research.

Elderly adults with chronic and acute pain obtained an average of 774 morphine milligram equivalents (MMEs) of prescription opioids annually during 2015-2016 from outpatient clinicians, compared with 376 MMEs a year for nonelderly adults, said Asako S. Moriya, PhD, and G. Edward Miller, PhD, of the AHRQ.
Narrowing the age groups shows that opioid MMEs increased with age, starting at 49 MMEs for 18- to 26-year-olds and rising to a high of 856 MMEs in the 65- to 74-year-old group, before dropping off in the oldest adults, the investigators said in a Medical Expenditure Panel Survey (MEPS) research findings report.
The analysis included “all opioid medications that are commonly used to treat pain” and excluded respiratory agents, antitussives, and drugs used for medication-assisted treatment, they noted. The MEPS data cover prescriptions purchased or obtained in outpatient settings but not those administered in inpatient settings or in clinics or physician offices.
according to the Agency for Healthcare Quality and Research.

Elderly adults with chronic and acute pain obtained an average of 774 morphine milligram equivalents (MMEs) of prescription opioids annually during 2015-2016 from outpatient clinicians, compared with 376 MMEs a year for nonelderly adults, said Asako S. Moriya, PhD, and G. Edward Miller, PhD, of the AHRQ.
Narrowing the age groups shows that opioid MMEs increased with age, starting at 49 MMEs for 18- to 26-year-olds and rising to a high of 856 MMEs in the 65- to 74-year-old group, before dropping off in the oldest adults, the investigators said in a Medical Expenditure Panel Survey (MEPS) research findings report.
The analysis included “all opioid medications that are commonly used to treat pain” and excluded respiratory agents, antitussives, and drugs used for medication-assisted treatment, they noted. The MEPS data cover prescriptions purchased or obtained in outpatient settings but not those administered in inpatient settings or in clinics or physician offices.
High rate of asymptomatic COVID-19 seen in cruise ship passengers
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
FROM MMWR
Flu now riding on COVID-19’s coattails
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
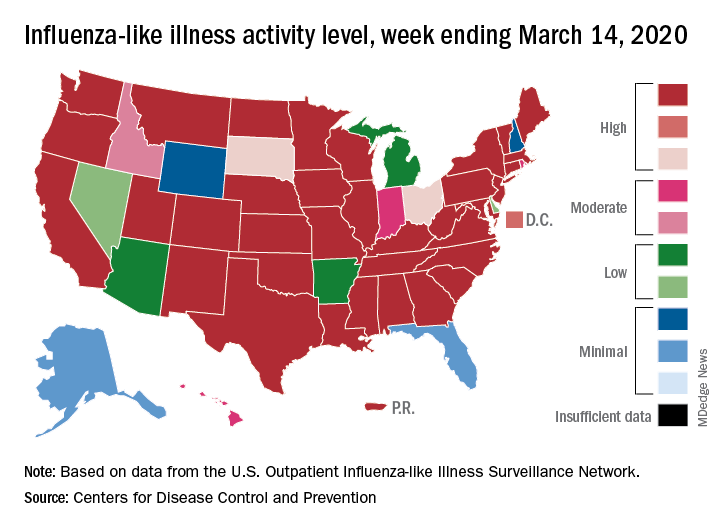
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
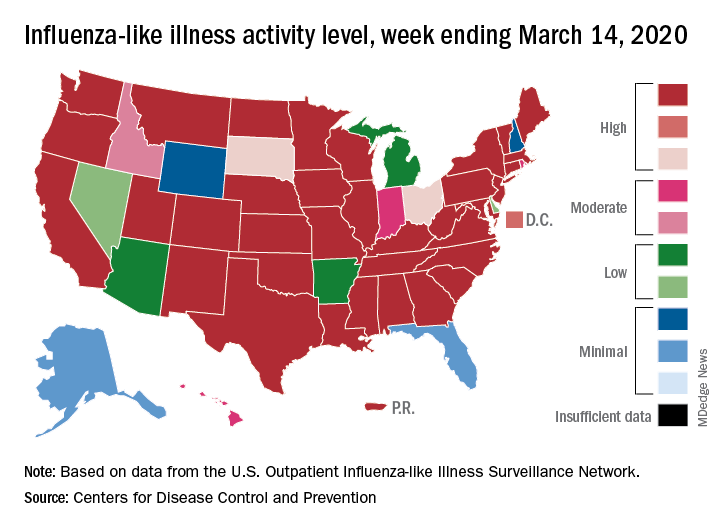
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
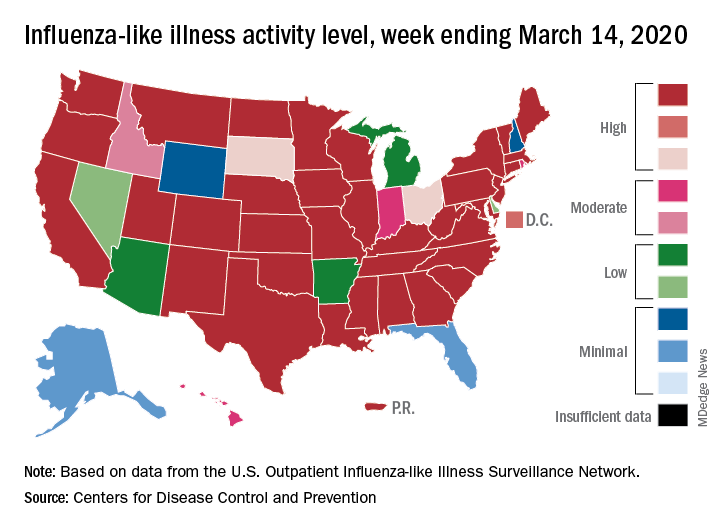
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
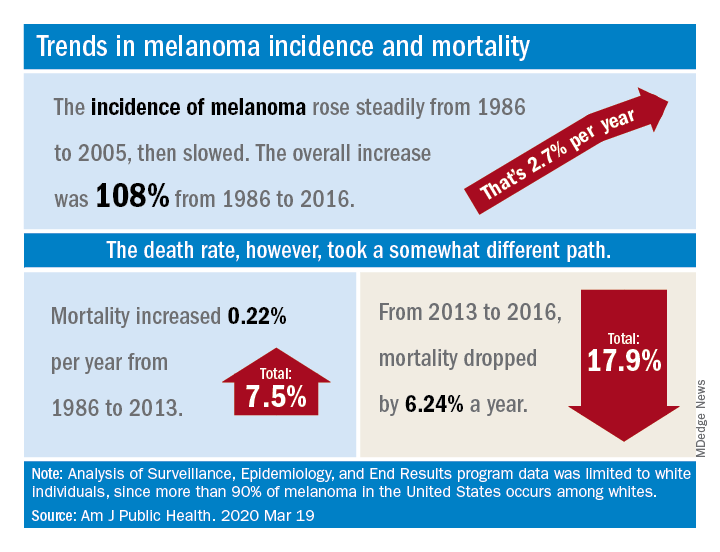
New melanoma treatments linked to mortality decline
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
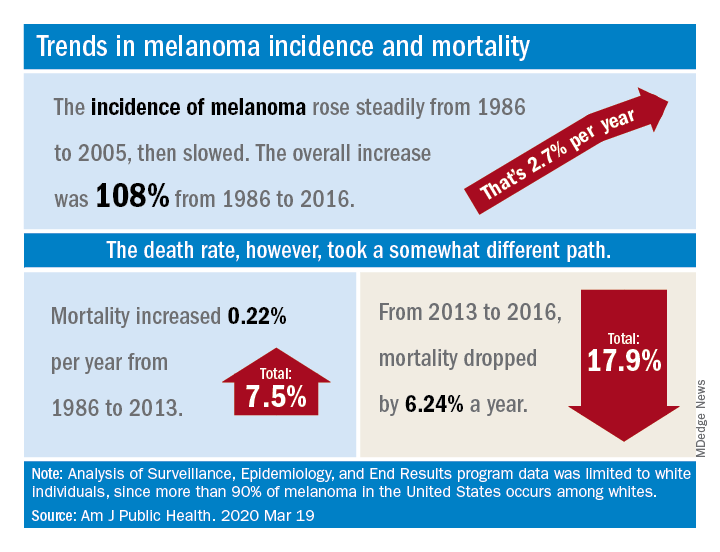
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
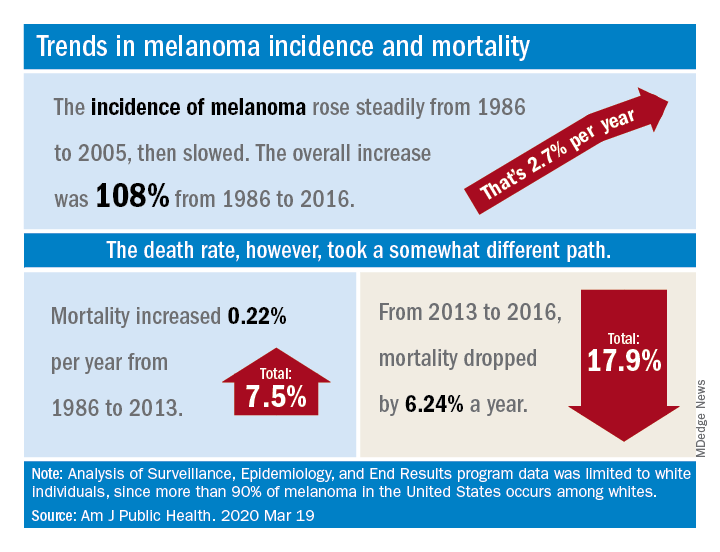
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
FROM THE AMERICAN JOURNAL OF PUBLIC HEALTH
Earthworm lollipops and Monty Python peer review
So you think you can pandemic?
What’s that? You say you’ve got an idea for the next great pandemic? Well, if your pandemic is going to beat coronavirus/COVID-19, it’s going to have to top this:
Sex: Porn star Lola Taylor (real name, Iyubov Bushueva) is currently in COVID-related isolation in Moscow and has offered to “have sex with the first scientist who finds a cure for coronavirus,” the Daily Star reported.
Sensible terrorists: “Islamic State has adopted a safety-first approach to the coronavirus pandemic and advised its members not to travel to Europe,” Politico reported. The terrorist group’s latest newsletter recommends that followers “stay away from the land of the epidemic” for the time being.
Drugs: Michigan is doing its part to keep the cannabis flowing. The state is temporarily lifting its ban against curbside pickup at marijuana stores as a way to limit exposure to coronavirus. “There has been an increase of customers who are stockpiling both medical and recreational cannabis, and sales are definitely up, just like other essentials,” Michigan Cannabis Industry Association Director Robin Schneider told mLive.com.
Sewage gridlock: Please don’t feed the fatbergs. That’s the message from the United Kingdom’s largest water and sewage authority. Thames Water is warning customers that flushing paper towels and wet wipes will add to the nonbiodegradable sewage blobs known as fatbergs, the Guardian reported. Thames Water’s position: “The only things that should be flushed are the 3 P’s: poo, pee and (toilet) paper,” the Guardian said.
Airship hospitals: China built two hospitals in response to the coronavirus epidemic, but can either of them fly? No. Science writer Bill Gourgey suggests that it’s time to revisit an idea proposed 100 years ago during a tuberculosis epidemic. Airships equipped as hospitals “could offer all of the resources – staff and equipment – to extract, quarantine, and treat patients. And a fleet could deliver at scale,” he wrote on OneZero.
The Governator: His royal Arnold-ness, along with this his pony Whiskey and donkey Lulu, has taken to Twitter to try to convince folks to stay inside and eat carrots together. Happily, Mr. Schwarzenegger did not go all Terminator when Whiskey tried to bite Lulu, instead offering a gentle, “You’ve got to get along.”
If your pandemic doesn’t have all of this, then you’re just not trying hard enough.
Earthworm Surprise
If you watched the Rugrats as a kid – or if your kids did, nonmillennials – you may remember how Phil and Lil used to eat bugs and worms whenever they played outside. We used to think it was gross, but now we think it may be time to follow their lead.
A Latvian scientist has unearthed (sorry) ways to make bread, muffins, lollipops, and so on using earthworms, claiming that earthworms are full of protein. Next time your children are crying for candy or sweets, why not hand them an earthworm lollipop to appease them? You’ll be making sure they’re getting their daily dose of protein!
The scientist, Ilga Gedrovica of the Latvian University of Life Science and Technologies, reported that earthworms not only contain just as much protein as meat, but they are also cheaper to produce. She also explained that, when dried, earthworms contain about three times more protein than meat.
Research is now underway to determine the safety of eating earthworms, fried or otherwise.
Just think: In a post–COVID-19 future, instead of a steak dinner, we could be making earthworm casseroles! Which, of course, kids won’t eat. Not because of the earthworms, of course. But because, ewwww, casseroles.
It’s ... Monty Python’s Flying Study!
It’s one of life’s most haunting questions, asked by one of our best philosophers: What is the velocity of an unladen swallow?
Sadly, Nathaniel Dominy and Erin Butler of Dartmouth University did not tackle this conundrum, but they did address another issue raised by Monty Python: Just how silly are the walks displayed by the Ministry of Silly Walks?
As you might expect, the minister himself is a masterclass of inefficiency, moving with 6.7 times more variability than someone walking in a nonhumorous fashion. Mr. Pudey, the man applying for the government grant to develop his own silly walk, is noticeably more efficient, merely displaying a rate of variability 3.3 times that of a normal walk. However, the researchers agreed with the minister that Mr. Pudey was well deserving of a government grant.
While we feel answering that question alone was worth a study, the researchers did have a larger point to make: comparing the bureaucratic inefficiency of the Ministry of Silly Walks to today’s peer-review process within the health field, particularly when researchers seek funding.
Grants take months to be approved and often involve researchers flying back and forth. A streamlined process could save huge amounts of both time and money, they noted.
The LOTME team would like to salute these two researchers for their excellent choice of metaphor, and hope they use Monty Python to make further points about health care. The swallow problem is just begging to be made into a metaphor.
So you think you can pandemic?
What’s that? You say you’ve got an idea for the next great pandemic? Well, if your pandemic is going to beat coronavirus/COVID-19, it’s going to have to top this:
Sex: Porn star Lola Taylor (real name, Iyubov Bushueva) is currently in COVID-related isolation in Moscow and has offered to “have sex with the first scientist who finds a cure for coronavirus,” the Daily Star reported.
Sensible terrorists: “Islamic State has adopted a safety-first approach to the coronavirus pandemic and advised its members not to travel to Europe,” Politico reported. The terrorist group’s latest newsletter recommends that followers “stay away from the land of the epidemic” for the time being.
Drugs: Michigan is doing its part to keep the cannabis flowing. The state is temporarily lifting its ban against curbside pickup at marijuana stores as a way to limit exposure to coronavirus. “There has been an increase of customers who are stockpiling both medical and recreational cannabis, and sales are definitely up, just like other essentials,” Michigan Cannabis Industry Association Director Robin Schneider told mLive.com.
Sewage gridlock: Please don’t feed the fatbergs. That’s the message from the United Kingdom’s largest water and sewage authority. Thames Water is warning customers that flushing paper towels and wet wipes will add to the nonbiodegradable sewage blobs known as fatbergs, the Guardian reported. Thames Water’s position: “The only things that should be flushed are the 3 P’s: poo, pee and (toilet) paper,” the Guardian said.
Airship hospitals: China built two hospitals in response to the coronavirus epidemic, but can either of them fly? No. Science writer Bill Gourgey suggests that it’s time to revisit an idea proposed 100 years ago during a tuberculosis epidemic. Airships equipped as hospitals “could offer all of the resources – staff and equipment – to extract, quarantine, and treat patients. And a fleet could deliver at scale,” he wrote on OneZero.
The Governator: His royal Arnold-ness, along with this his pony Whiskey and donkey Lulu, has taken to Twitter to try to convince folks to stay inside and eat carrots together. Happily, Mr. Schwarzenegger did not go all Terminator when Whiskey tried to bite Lulu, instead offering a gentle, “You’ve got to get along.”
If your pandemic doesn’t have all of this, then you’re just not trying hard enough.
Earthworm Surprise
If you watched the Rugrats as a kid – or if your kids did, nonmillennials – you may remember how Phil and Lil used to eat bugs and worms whenever they played outside. We used to think it was gross, but now we think it may be time to follow their lead.
A Latvian scientist has unearthed (sorry) ways to make bread, muffins, lollipops, and so on using earthworms, claiming that earthworms are full of protein. Next time your children are crying for candy or sweets, why not hand them an earthworm lollipop to appease them? You’ll be making sure they’re getting their daily dose of protein!
The scientist, Ilga Gedrovica of the Latvian University of Life Science and Technologies, reported that earthworms not only contain just as much protein as meat, but they are also cheaper to produce. She also explained that, when dried, earthworms contain about three times more protein than meat.
Research is now underway to determine the safety of eating earthworms, fried or otherwise.
Just think: In a post–COVID-19 future, instead of a steak dinner, we could be making earthworm casseroles! Which, of course, kids won’t eat. Not because of the earthworms, of course. But because, ewwww, casseroles.
It’s ... Monty Python’s Flying Study!
It’s one of life’s most haunting questions, asked by one of our best philosophers: What is the velocity of an unladen swallow?
Sadly, Nathaniel Dominy and Erin Butler of Dartmouth University did not tackle this conundrum, but they did address another issue raised by Monty Python: Just how silly are the walks displayed by the Ministry of Silly Walks?
As you might expect, the minister himself is a masterclass of inefficiency, moving with 6.7 times more variability than someone walking in a nonhumorous fashion. Mr. Pudey, the man applying for the government grant to develop his own silly walk, is noticeably more efficient, merely displaying a rate of variability 3.3 times that of a normal walk. However, the researchers agreed with the minister that Mr. Pudey was well deserving of a government grant.
While we feel answering that question alone was worth a study, the researchers did have a larger point to make: comparing the bureaucratic inefficiency of the Ministry of Silly Walks to today’s peer-review process within the health field, particularly when researchers seek funding.
Grants take months to be approved and often involve researchers flying back and forth. A streamlined process could save huge amounts of both time and money, they noted.
The LOTME team would like to salute these two researchers for their excellent choice of metaphor, and hope they use Monty Python to make further points about health care. The swallow problem is just begging to be made into a metaphor.
So you think you can pandemic?
What’s that? You say you’ve got an idea for the next great pandemic? Well, if your pandemic is going to beat coronavirus/COVID-19, it’s going to have to top this:
Sex: Porn star Lola Taylor (real name, Iyubov Bushueva) is currently in COVID-related isolation in Moscow and has offered to “have sex with the first scientist who finds a cure for coronavirus,” the Daily Star reported.
Sensible terrorists: “Islamic State has adopted a safety-first approach to the coronavirus pandemic and advised its members not to travel to Europe,” Politico reported. The terrorist group’s latest newsletter recommends that followers “stay away from the land of the epidemic” for the time being.
Drugs: Michigan is doing its part to keep the cannabis flowing. The state is temporarily lifting its ban against curbside pickup at marijuana stores as a way to limit exposure to coronavirus. “There has been an increase of customers who are stockpiling both medical and recreational cannabis, and sales are definitely up, just like other essentials,” Michigan Cannabis Industry Association Director Robin Schneider told mLive.com.
Sewage gridlock: Please don’t feed the fatbergs. That’s the message from the United Kingdom’s largest water and sewage authority. Thames Water is warning customers that flushing paper towels and wet wipes will add to the nonbiodegradable sewage blobs known as fatbergs, the Guardian reported. Thames Water’s position: “The only things that should be flushed are the 3 P’s: poo, pee and (toilet) paper,” the Guardian said.
Airship hospitals: China built two hospitals in response to the coronavirus epidemic, but can either of them fly? No. Science writer Bill Gourgey suggests that it’s time to revisit an idea proposed 100 years ago during a tuberculosis epidemic. Airships equipped as hospitals “could offer all of the resources – staff and equipment – to extract, quarantine, and treat patients. And a fleet could deliver at scale,” he wrote on OneZero.
The Governator: His royal Arnold-ness, along with this his pony Whiskey and donkey Lulu, has taken to Twitter to try to convince folks to stay inside and eat carrots together. Happily, Mr. Schwarzenegger did not go all Terminator when Whiskey tried to bite Lulu, instead offering a gentle, “You’ve got to get along.”
If your pandemic doesn’t have all of this, then you’re just not trying hard enough.
Earthworm Surprise
If you watched the Rugrats as a kid – or if your kids did, nonmillennials – you may remember how Phil and Lil used to eat bugs and worms whenever they played outside. We used to think it was gross, but now we think it may be time to follow their lead.
A Latvian scientist has unearthed (sorry) ways to make bread, muffins, lollipops, and so on using earthworms, claiming that earthworms are full of protein. Next time your children are crying for candy or sweets, why not hand them an earthworm lollipop to appease them? You’ll be making sure they’re getting their daily dose of protein!
The scientist, Ilga Gedrovica of the Latvian University of Life Science and Technologies, reported that earthworms not only contain just as much protein as meat, but they are also cheaper to produce. She also explained that, when dried, earthworms contain about three times more protein than meat.
Research is now underway to determine the safety of eating earthworms, fried or otherwise.
Just think: In a post–COVID-19 future, instead of a steak dinner, we could be making earthworm casseroles! Which, of course, kids won’t eat. Not because of the earthworms, of course. But because, ewwww, casseroles.
It’s ... Monty Python’s Flying Study!
It’s one of life’s most haunting questions, asked by one of our best philosophers: What is the velocity of an unladen swallow?
Sadly, Nathaniel Dominy and Erin Butler of Dartmouth University did not tackle this conundrum, but they did address another issue raised by Monty Python: Just how silly are the walks displayed by the Ministry of Silly Walks?
As you might expect, the minister himself is a masterclass of inefficiency, moving with 6.7 times more variability than someone walking in a nonhumorous fashion. Mr. Pudey, the man applying for the government grant to develop his own silly walk, is noticeably more efficient, merely displaying a rate of variability 3.3 times that of a normal walk. However, the researchers agreed with the minister that Mr. Pudey was well deserving of a government grant.
While we feel answering that question alone was worth a study, the researchers did have a larger point to make: comparing the bureaucratic inefficiency of the Ministry of Silly Walks to today’s peer-review process within the health field, particularly when researchers seek funding.
Grants take months to be approved and often involve researchers flying back and forth. A streamlined process could save huge amounts of both time and money, they noted.
The LOTME team would like to salute these two researchers for their excellent choice of metaphor, and hope they use Monty Python to make further points about health care. The swallow problem is just begging to be made into a metaphor.
Here’s what ICUs are putting up against COVID-19
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
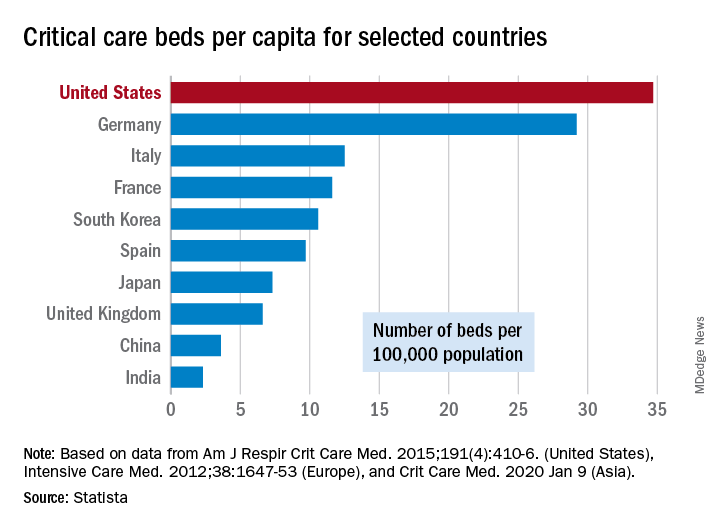
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
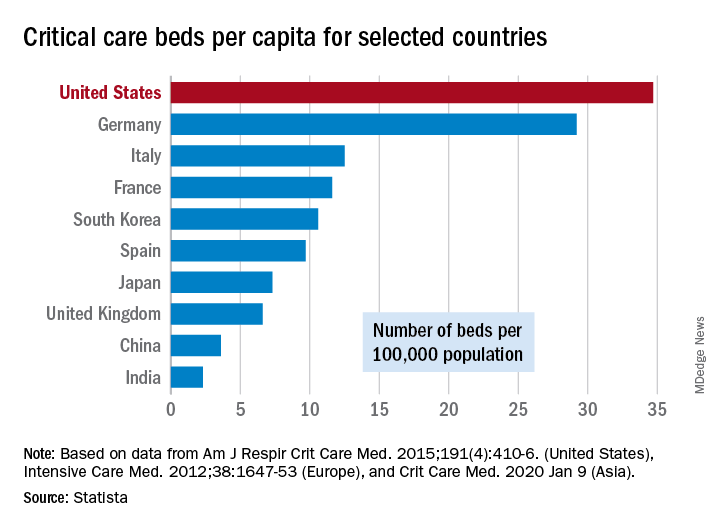
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
As COVID-19 spreads across the United States, it is important to understand the extent of the nation’s ICU resources, according to the Society of Critical Care Medicine. The SCCM has updated its statistics on the resources available to care for what could become “an overwhelming number of critically ill patients, many of whom may require mechanical ventilation,” the society said in a blog post on March 13.
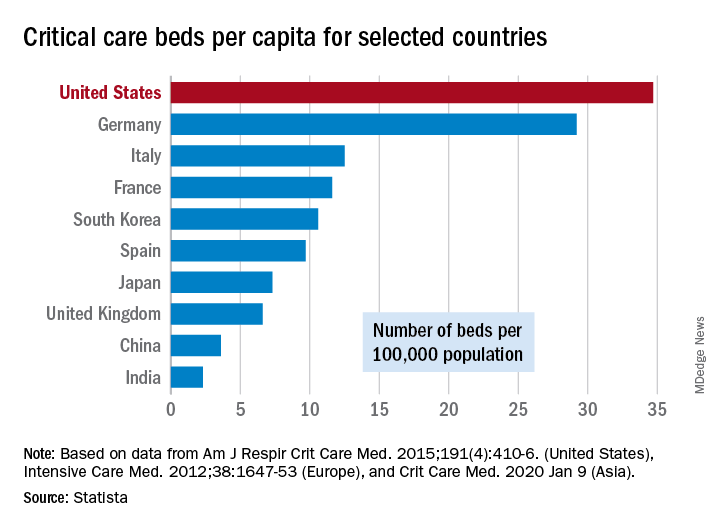
That overwhelming number was considered at an American Hospital Association webinar in February: Investigators projected that 4.8 million patients could be hospitalized with COVID-19, of whom 1.9 million would be admitted to ICUs and 960,000 would require ventilator support, Neil A. Halpern, MD, director of the critical care center at Memorial Sloan Kettering Cancer Center, New York, and Kay See Tan, PhD, of the hospital’s department of epidemiology and biostatistics, reported in that post.
As far as critical care beds are concerned, the United States is in better shape than are other countries dealing with the coronavirus. The United States’ 34.7 critical care beds per 100,000 population put it a good bit ahead of Germany, which has 29.2 beds per 100,000, while other countries in both Europe and Asia are well behind, Dr. Halpern and Dr. Tan noted.
More recent data from the AHA show that just over half of its registered community hospitals deliver ICU services and have at least 10 acute care beds and one ICU bed, they reported.
Those 2,704 hospitals have nearly 535,000 acute care beds, of which almost 97,000 are ICU beds. Almost 71% of those ICU beds are for adults, with the rest located in neonatal and pediatric units, data from an AHA 2018 survey show.
Since patients with COVID-19 are most often admitted to ICUs with severe hypoxic respiratory failure, the nation’s supply of ventilators also may be tested. U.S. acute care hospitals own about 62,000 full-featured mechanical ventilators and almost 99,000 older ventilators that “may not be capable of adequately supporting patients with severe acute respiratory failure,” Dr. Halpern and Dr. Tan said.
As U.S. hospitals reach the crisis levels anticipated in the COVID-19 pandemic, staffing shortages can be expected as well. Almost half (48%) of acute care hospitals have no intensivists, so “other physicians (e.g., pulmonologists, surgeons, anesthesiologists, etc) may be pressed into service as outpatient clinics and elective surgery are suspended,” they wrote.
The blog post includes a tiered staffing strategy that the SCCM “encourages hospitals to adopt in pandemic situations such as COVID-19.”
After weeks of decline, influenza activity increases slightly
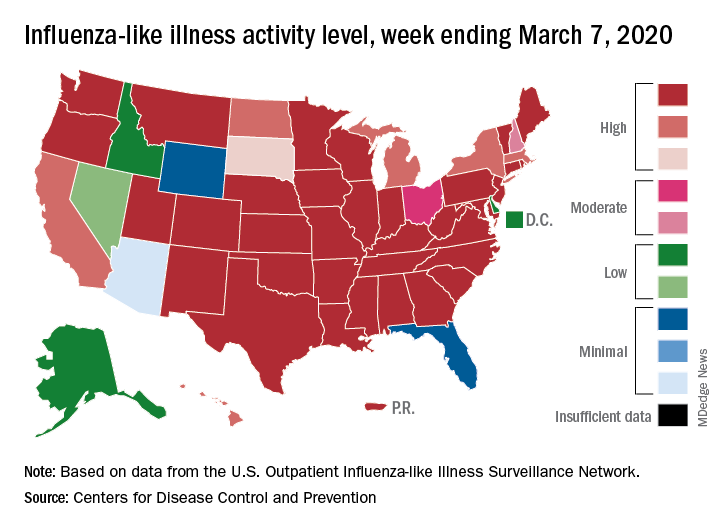
The two leading measures of influenza activity – the percentage of respiratory specimens testing positive for influenza and the proportion of visits to health care providers for influenza-like illness (ILI) – had been following a similar downward path since mid-February. But during the week ending March 7, their paths diverged, according to the Centers for Disease Control and Prevention.
The percentage of respiratory specimens testing positive for influenza dropped for the fourth consecutive week, falling from 26.1% to 21.5%, while the proportion of visits to health care providers for ILI increased from 5.1% to 5.2%, the CDC’s influenza division reported.
One possible explanation for that rise: “The largest increases in ILI activity occurred in areas of the country where COVID-19 is most prevalent. More people may be seeking care for respiratory illness than usual at this time,” the influenza division said March 13 in its weekly Fluview report.
This week’s map puts 34 states and Puerto Rico at level 10 on the CDC’s 1-10 scale of ILI activity, one more state than the week before, and 43 jurisdictions in the “high” range of 8-10, compared with 42 the previous week, the CDC said.
Rates of hospitalizations associated with influenza “remain moderate compared to recent seasons, but rates for children 0-4 years and adults 18-49 years are now the highest CDC has on record for these age groups, surpassing rates reported during the 2009 H1N1 pandemic,” the Fluview report said. Rates for children aged 5-17 years “are higher than any recent regular season but remain lower than rates experienced by this age group during the pandemic.”
The number of pediatric deaths this season is now up to 144, equaling the total for all of the 2018-2019 season. This year’s count led the CDC to invoke 2009 again, since it “is higher for the same time period than in every season since reporting began in 2004-2005, except for the 2009 pandemic.”
For the 2019-2020 season so far there have been 36 million flu illnesses, 370,000 hospitalizations, and 22,000 deaths from flu and pneumonia, the CDC estimated.
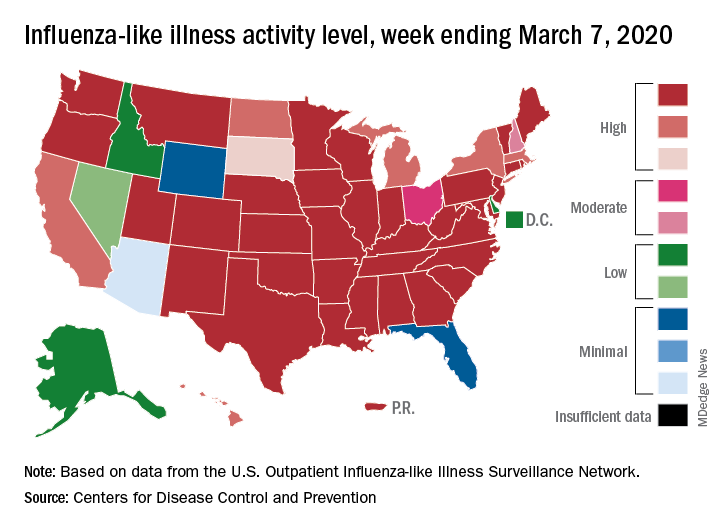
The two leading measures of influenza activity – the percentage of respiratory specimens testing positive for influenza and the proportion of visits to health care providers for influenza-like illness (ILI) – had been following a similar downward path since mid-February. But during the week ending March 7, their paths diverged, according to the Centers for Disease Control and Prevention.
The percentage of respiratory specimens testing positive for influenza dropped for the fourth consecutive week, falling from 26.1% to 21.5%, while the proportion of visits to health care providers for ILI increased from 5.1% to 5.2%, the CDC’s influenza division reported.
One possible explanation for that rise: “The largest increases in ILI activity occurred in areas of the country where COVID-19 is most prevalent. More people may be seeking care for respiratory illness than usual at this time,” the influenza division said March 13 in its weekly Fluview report.
This week’s map puts 34 states and Puerto Rico at level 10 on the CDC’s 1-10 scale of ILI activity, one more state than the week before, and 43 jurisdictions in the “high” range of 8-10, compared with 42 the previous week, the CDC said.
Rates of hospitalizations associated with influenza “remain moderate compared to recent seasons, but rates for children 0-4 years and adults 18-49 years are now the highest CDC has on record for these age groups, surpassing rates reported during the 2009 H1N1 pandemic,” the Fluview report said. Rates for children aged 5-17 years “are higher than any recent regular season but remain lower than rates experienced by this age group during the pandemic.”
The number of pediatric deaths this season is now up to 144, equaling the total for all of the 2018-2019 season. This year’s count led the CDC to invoke 2009 again, since it “is higher for the same time period than in every season since reporting began in 2004-2005, except for the 2009 pandemic.”
For the 2019-2020 season so far there have been 36 million flu illnesses, 370,000 hospitalizations, and 22,000 deaths from flu and pneumonia, the CDC estimated.
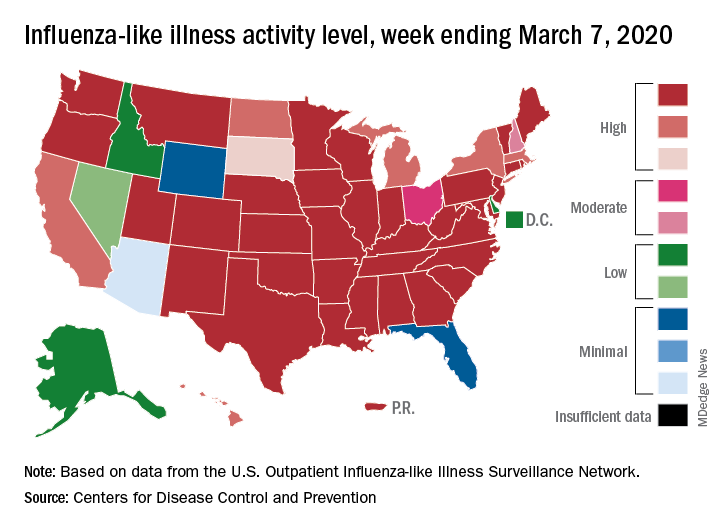
The two leading measures of influenza activity – the percentage of respiratory specimens testing positive for influenza and the proportion of visits to health care providers for influenza-like illness (ILI) – had been following a similar downward path since mid-February. But during the week ending March 7, their paths diverged, according to the Centers for Disease Control and Prevention.
The percentage of respiratory specimens testing positive for influenza dropped for the fourth consecutive week, falling from 26.1% to 21.5%, while the proportion of visits to health care providers for ILI increased from 5.1% to 5.2%, the CDC’s influenza division reported.
One possible explanation for that rise: “The largest increases in ILI activity occurred in areas of the country where COVID-19 is most prevalent. More people may be seeking care for respiratory illness than usual at this time,” the influenza division said March 13 in its weekly Fluview report.
This week’s map puts 34 states and Puerto Rico at level 10 on the CDC’s 1-10 scale of ILI activity, one more state than the week before, and 43 jurisdictions in the “high” range of 8-10, compared with 42 the previous week, the CDC said.
Rates of hospitalizations associated with influenza “remain moderate compared to recent seasons, but rates for children 0-4 years and adults 18-49 years are now the highest CDC has on record for these age groups, surpassing rates reported during the 2009 H1N1 pandemic,” the Fluview report said. Rates for children aged 5-17 years “are higher than any recent regular season but remain lower than rates experienced by this age group during the pandemic.”
The number of pediatric deaths this season is now up to 144, equaling the total for all of the 2018-2019 season. This year’s count led the CDC to invoke 2009 again, since it “is higher for the same time period than in every season since reporting began in 2004-2005, except for the 2009 pandemic.”
For the 2019-2020 season so far there have been 36 million flu illnesses, 370,000 hospitalizations, and 22,000 deaths from flu and pneumonia, the CDC estimated.
Age divide seen in colorectal cancer screening use
Roughly 79% of adults aged 65-75 years were up to date with their colorectal cancer (CRC) screening in 2018, compared with a significantly lower 63% of those aged 50-64, according to the Centers for Disease Control and Prevention.
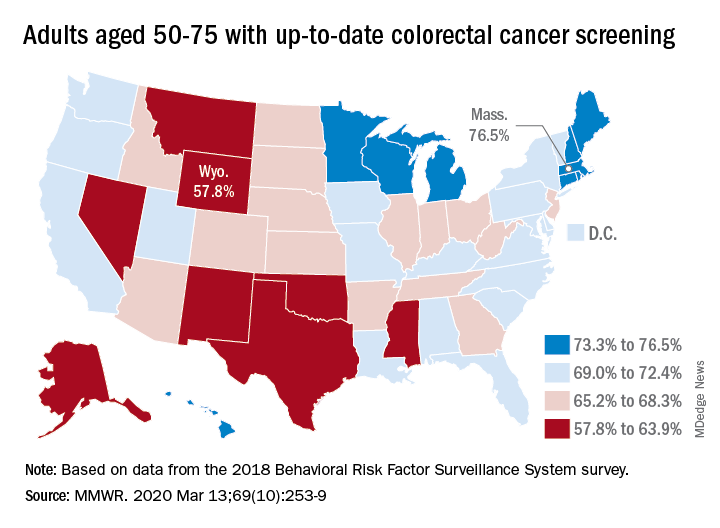
That works out to almost 69% of Americans aged 50-75 years with up-to-date CRC screening, which was defined as a blood stool test in the past year, sigmoidoscopy in the past 5 years, and/or colonoscopy in the past 10 years, Djenaba A. Joseph, MD, and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion wrote in the Morbidity and Mortality Weekly Report.
“CRC screening has increased steadily among adults over the past 20 years,” the authors noted. However, they observed a lower rate of screening in the 50-64 age group (vs. the 65-75 age group) that was consistent and significant across all demographic groups studied: sex, race/ethnicity, education, annual income, residence location, health insurance status, and regular health care provider status.
The range of screening rates in those groups went from a low of 32.6% (in 50- to 64-year-olds who had no health insurance) to a high of 87.1% (in 65- to 75-year-olds who had annual household incomes of $75,000 and over).
Up-to-date CRC screening rates were higher for the 65-75 age group in every state. The highest screening rate was observed in Rhode Island, at 84.9% in the 65-75 age group. Massachusetts had the highest rate for 50- to 64-year-olds, at 72.1%, and the highest rate for all ages studied (50-75 years), at 76.5%. Wyoming was lowest in all three categories: 51.5% in the 50-64 age group, 68.5% in the 65-75 age group, and 57.8% in the 50-75 age group.
“To achieve further increases in CRC screening to maximize benefit, specific efforts to increase screening in persons aged 50-64 years are needed,” Dr. Joseph and colleagues wrote. They added that efforts might include “providing education about insurance coverage for preventive services, providing clear communication about test options, and conducting research to identify and understand barriers and facilitators to CRC screening specific to this younger age group to inform effective interventions to increase screening.”
SOURCE: Joseph DA et al. MMWR. 2020 Mar 13;69(10):253-9.
Roughly 79% of adults aged 65-75 years were up to date with their colorectal cancer (CRC) screening in 2018, compared with a significantly lower 63% of those aged 50-64, according to the Centers for Disease Control and Prevention.
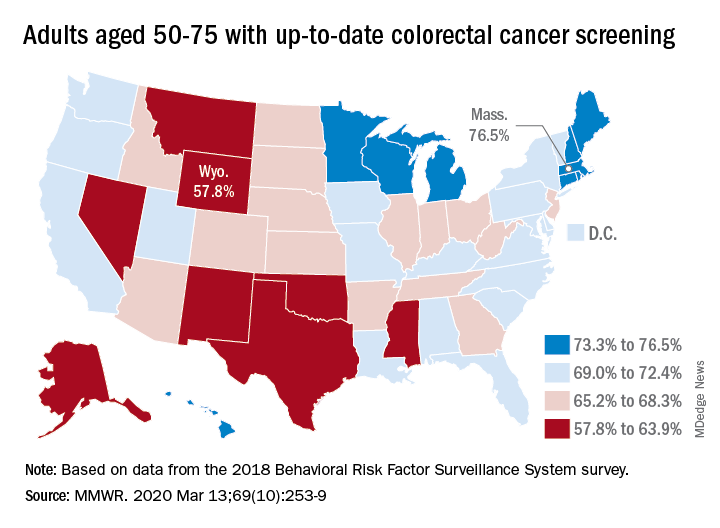
That works out to almost 69% of Americans aged 50-75 years with up-to-date CRC screening, which was defined as a blood stool test in the past year, sigmoidoscopy in the past 5 years, and/or colonoscopy in the past 10 years, Djenaba A. Joseph, MD, and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion wrote in the Morbidity and Mortality Weekly Report.
“CRC screening has increased steadily among adults over the past 20 years,” the authors noted. However, they observed a lower rate of screening in the 50-64 age group (vs. the 65-75 age group) that was consistent and significant across all demographic groups studied: sex, race/ethnicity, education, annual income, residence location, health insurance status, and regular health care provider status.
The range of screening rates in those groups went from a low of 32.6% (in 50- to 64-year-olds who had no health insurance) to a high of 87.1% (in 65- to 75-year-olds who had annual household incomes of $75,000 and over).
Up-to-date CRC screening rates were higher for the 65-75 age group in every state. The highest screening rate was observed in Rhode Island, at 84.9% in the 65-75 age group. Massachusetts had the highest rate for 50- to 64-year-olds, at 72.1%, and the highest rate for all ages studied (50-75 years), at 76.5%. Wyoming was lowest in all three categories: 51.5% in the 50-64 age group, 68.5% in the 65-75 age group, and 57.8% in the 50-75 age group.
“To achieve further increases in CRC screening to maximize benefit, specific efforts to increase screening in persons aged 50-64 years are needed,” Dr. Joseph and colleagues wrote. They added that efforts might include “providing education about insurance coverage for preventive services, providing clear communication about test options, and conducting research to identify and understand barriers and facilitators to CRC screening specific to this younger age group to inform effective interventions to increase screening.”
SOURCE: Joseph DA et al. MMWR. 2020 Mar 13;69(10):253-9.
Roughly 79% of adults aged 65-75 years were up to date with their colorectal cancer (CRC) screening in 2018, compared with a significantly lower 63% of those aged 50-64, according to the Centers for Disease Control and Prevention.
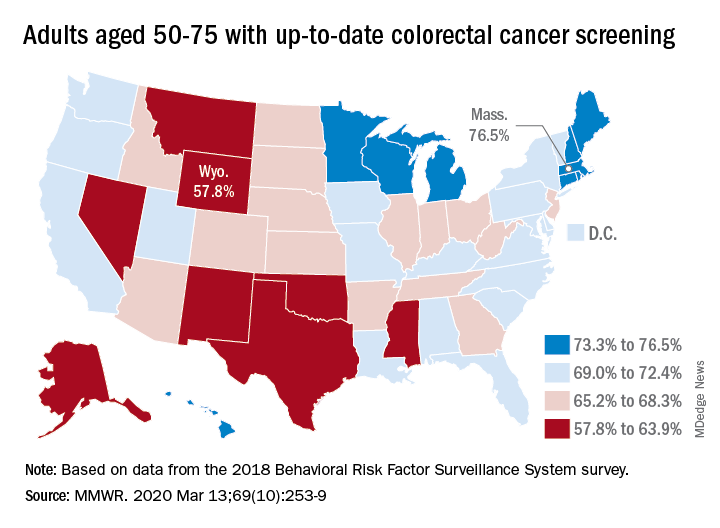
That works out to almost 69% of Americans aged 50-75 years with up-to-date CRC screening, which was defined as a blood stool test in the past year, sigmoidoscopy in the past 5 years, and/or colonoscopy in the past 10 years, Djenaba A. Joseph, MD, and associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion wrote in the Morbidity and Mortality Weekly Report.
“CRC screening has increased steadily among adults over the past 20 years,” the authors noted. However, they observed a lower rate of screening in the 50-64 age group (vs. the 65-75 age group) that was consistent and significant across all demographic groups studied: sex, race/ethnicity, education, annual income, residence location, health insurance status, and regular health care provider status.
The range of screening rates in those groups went from a low of 32.6% (in 50- to 64-year-olds who had no health insurance) to a high of 87.1% (in 65- to 75-year-olds who had annual household incomes of $75,000 and over).
Up-to-date CRC screening rates were higher for the 65-75 age group in every state. The highest screening rate was observed in Rhode Island, at 84.9% in the 65-75 age group. Massachusetts had the highest rate for 50- to 64-year-olds, at 72.1%, and the highest rate for all ages studied (50-75 years), at 76.5%. Wyoming was lowest in all three categories: 51.5% in the 50-64 age group, 68.5% in the 65-75 age group, and 57.8% in the 50-75 age group.
“To achieve further increases in CRC screening to maximize benefit, specific efforts to increase screening in persons aged 50-64 years are needed,” Dr. Joseph and colleagues wrote. They added that efforts might include “providing education about insurance coverage for preventive services, providing clear communication about test options, and conducting research to identify and understand barriers and facilitators to CRC screening specific to this younger age group to inform effective interventions to increase screening.”
SOURCE: Joseph DA et al. MMWR. 2020 Mar 13;69(10):253-9.
FROM MMWR
Cancer mortality continues to decline while cancer incidence rises in women
according to the Annual Report to the Nation on the Status of Cancer.
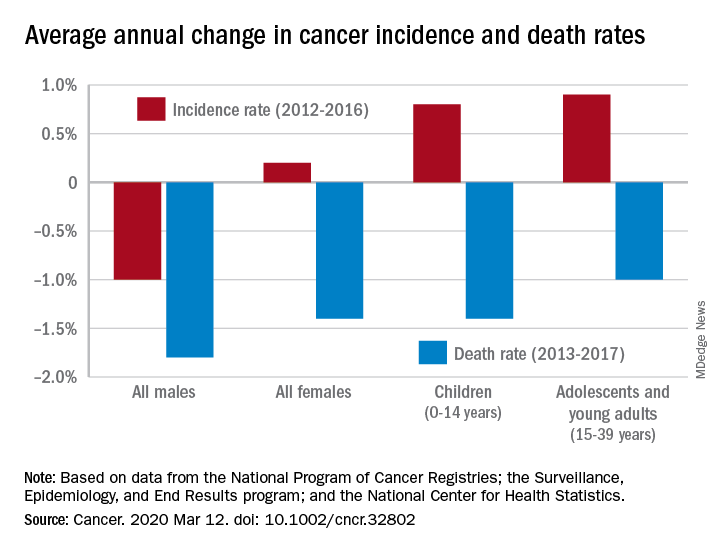
During 2013-2017, the overall age-standardized death rate for all cancers was 158.2 per 100,000 population, and the average decline over that period was 1.5% per year. The average annual change was greater for men (–1.8%) than women (–1.4%) for 2013-2017, but the death rate was higher for men (189.3 per 100,000 vs. 135.5 per 100,000) for those years, S. Jane Henley of the Centers for Disease Control and Prevention and associates reported in Cancer.
“The drops in mortality we’re seeing are real, sustained, and a strong indication of what we can do when we work to prevent and treat cancer,” William G. Cance, MD, chief medical and scientific officer of the America Cancer Society, said in a written statement accompanying the report.
Overall cancer incidence for the most recent 5-year period (2012-2016) was 447.9 per 100,000, with rates of 487.9 for men and 421.4 for women, the investigators said.
Incidence dropped by 0.6% per year overall, but that hides a major difference between men, who saw a decrease of 1.0% a year, and women, who experienced an annual increase of 0.2%.
Over those 5 years, cancer incidence also increased by 0.8% annually among children aged 0-14 years and by 0.9% in adolescents and young adults aged 15-39 years, Ms. Henley and associates said in the report, which is a collaborative effort between the CDC, the National Cancer Institute, the American Cancer Society, and the North American Association of Central Cancer Registries.
“[W]e must not be complacent. The cancer incidence data – especially the increase in cancer among women – is a clear reminder that there is more work ahead,” Norman E. Sharpless, MD, director of the National Cancer Institute, said in the accompanying statement.
SOURCE: Henley SJ et al. Cancer. 2020 Mar 12. doi: 10.1002/cncr.32802.
according to the Annual Report to the Nation on the Status of Cancer.
During 2013-2017, the overall age-standardized death rate for all cancers was 158.2 per 100,000 population, and the average decline over that period was 1.5% per year. The average annual change was greater for men (–1.8%) than women (–1.4%) for 2013-2017, but the death rate was higher for men (189.3 per 100,000 vs. 135.5 per 100,000) for those years, S. Jane Henley of the Centers for Disease Control and Prevention and associates reported in Cancer.
“The drops in mortality we’re seeing are real, sustained, and a strong indication of what we can do when we work to prevent and treat cancer,” William G. Cance, MD, chief medical and scientific officer of the America Cancer Society, said in a written statement accompanying the report.
Overall cancer incidence for the most recent 5-year period (2012-2016) was 447.9 per 100,000, with rates of 487.9 for men and 421.4 for women, the investigators said.
Incidence dropped by 0.6% per year overall, but that hides a major difference between men, who saw a decrease of 1.0% a year, and women, who experienced an annual increase of 0.2%.
Over those 5 years, cancer incidence also increased by 0.8% annually among children aged 0-14 years and by 0.9% in adolescents and young adults aged 15-39 years, Ms. Henley and associates said in the report, which is a collaborative effort between the CDC, the National Cancer Institute, the American Cancer Society, and the North American Association of Central Cancer Registries.
“[W]e must not be complacent. The cancer incidence data – especially the increase in cancer among women – is a clear reminder that there is more work ahead,” Norman E. Sharpless, MD, director of the National Cancer Institute, said in the accompanying statement.
SOURCE: Henley SJ et al. Cancer. 2020 Mar 12. doi: 10.1002/cncr.32802.
according to the Annual Report to the Nation on the Status of Cancer.
During 2013-2017, the overall age-standardized death rate for all cancers was 158.2 per 100,000 population, and the average decline over that period was 1.5% per year. The average annual change was greater for men (–1.8%) than women (–1.4%) for 2013-2017, but the death rate was higher for men (189.3 per 100,000 vs. 135.5 per 100,000) for those years, S. Jane Henley of the Centers for Disease Control and Prevention and associates reported in Cancer.
“The drops in mortality we’re seeing are real, sustained, and a strong indication of what we can do when we work to prevent and treat cancer,” William G. Cance, MD, chief medical and scientific officer of the America Cancer Society, said in a written statement accompanying the report.
Overall cancer incidence for the most recent 5-year period (2012-2016) was 447.9 per 100,000, with rates of 487.9 for men and 421.4 for women, the investigators said.
Incidence dropped by 0.6% per year overall, but that hides a major difference between men, who saw a decrease of 1.0% a year, and women, who experienced an annual increase of 0.2%.
Over those 5 years, cancer incidence also increased by 0.8% annually among children aged 0-14 years and by 0.9% in adolescents and young adults aged 15-39 years, Ms. Henley and associates said in the report, which is a collaborative effort between the CDC, the National Cancer Institute, the American Cancer Society, and the North American Association of Central Cancer Registries.
“[W]e must not be complacent. The cancer incidence data – especially the increase in cancer among women – is a clear reminder that there is more work ahead,” Norman E. Sharpless, MD, director of the National Cancer Institute, said in the accompanying statement.
SOURCE: Henley SJ et al. Cancer. 2020 Mar 12. doi: 10.1002/cncr.32802.
FROM CANCER



