User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Australian apocalypse essentials and bacterial evolution stoppers
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
Irony 1, Council on Foreign Relations 0
It’s not a great time to be a business owner right now. People everywhere are feeling nervous, thanks to our old friend COVID-19, and it can be difficult to actually sell things when half the population is staying indoors hoarding toilet paper.
So if you are a business owner, you’re probably thinking: “Gee, it sure would be nice to meet up with my fellow business owners to come up with a plan on how to operate in a world dealing with a potential pandemic.” Right?
That’s the idea behind the Council on Foreign Relations’ roundtable discussion called “Doing Business Under Coronavirus,” scheduled for March 13, 2020, in New York. Or at least, it was the idea, because the conference has been canceled. And you’ll never guess why.
Okay, it was coronavirus. Uh, you probably did guess that. We’re not entirely sure what that means for business owners, but come on, there’s no need to worry, at least the infectious disease physicians had their meeting this past weekend ... oh wait. Hmm, maybe it’s time to start searching Amazon for some toilet paper.
Wipe away coronavirus fear
People now have smartphones to read the news while on the toilet, but at one point or another, having a newspaper to read in the john was probably pretty essential to combat boredom. Our friends down under, however, seem to have found another essential way to use a newspaper in the bathroom.
The coronavirus is slowly making its way around the world, and in Australia, people are stocking up on toilet paper. Toilet paper companies are working extra hard to keep a steady supply of toilet paper in supermarkets. A newspaper has tried to help by adding extra pages to its newspapers that could potentially be used as toilet paper. This seems like a good time to swap out your smartphone for one of these newspapers as it would not be wise to use your smartphone for toilet paper.
No one is sure why everyone in Australia is in a frenzy over toilet paper since it’s not a very big necessity in a large coronavirus outbreak. Are Aussies preparing to hide out in their homes just in case those affected by coronavirus turn into zombies, thus creating a zombie apocalypse? In that case, yeah, toilet paper, among other things, is probably essential.
Resistance meets resistance
As our planet moves from zombie apocalypse to coronapocalypse, even the business news has gone full COVID-19. So, it would be pointless for us to cover any other topic, right?
Well, welcome to the Bureau of Missing the Point. Ladies and gentleman, we give you [drum roll, please] bacteria.
That’s right, we said bacteria. In a world ruled by coronavirus, LOTME dares to bring you the latest edition of Bacteria vs. the World.
This week, we’re talking antibiotic resistance. The problem is that bacteria have the ability to pick up DNA from their surroundings to create resistance. That ability, known as competence, could be considered a form of evolution, and scientists are trying to stop it.
Investigators at the University of Groningen in the Netherlands and the Swiss University of Lausanne “developed a high-throughput assay to simultaneously test cells for competence and growth,” lead investigator Arnau Domenech, PhD, said in a written statement. Of the 1,366 approved drugs that they tested against Streptococcus pneumoniae, 46 blocked bacterial competence.
“When cells are under growth stress, for instance in the presence of antibiotics, they try to find a solution and become resistant to these drugs,” Dr. Domenech explained. “Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress.”
The drug concentrations used to block competence may be too high to be safe for humans, but the results suggest that competence blockers are, indeed, anti-evolution drugs. As we go bacteria to the future, it seems, the ghost of Charles Darwin is working for the humans. Thanks, Chuck.
Oh, one more thing … CORONAVIRUS!
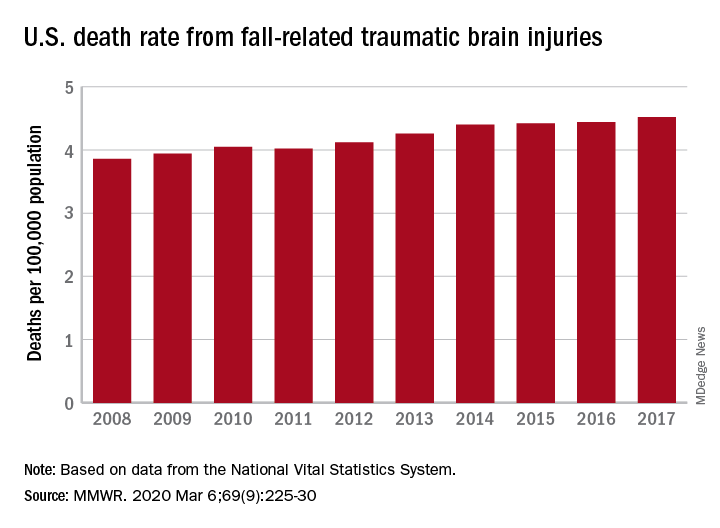
TBI deaths from falls on the rise
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
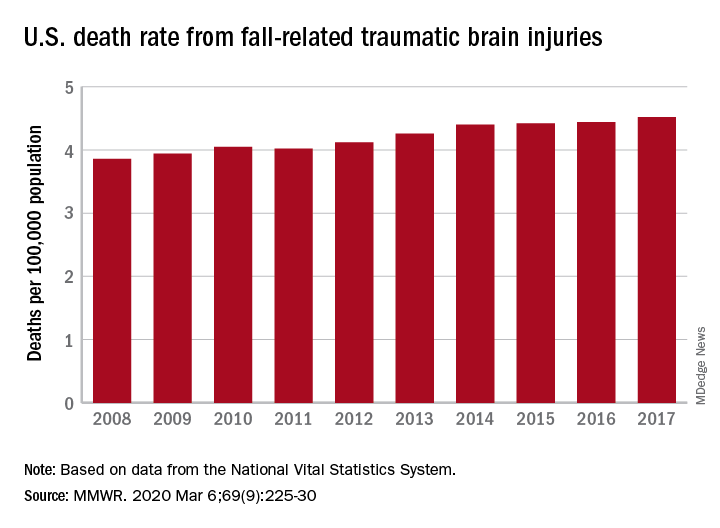
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
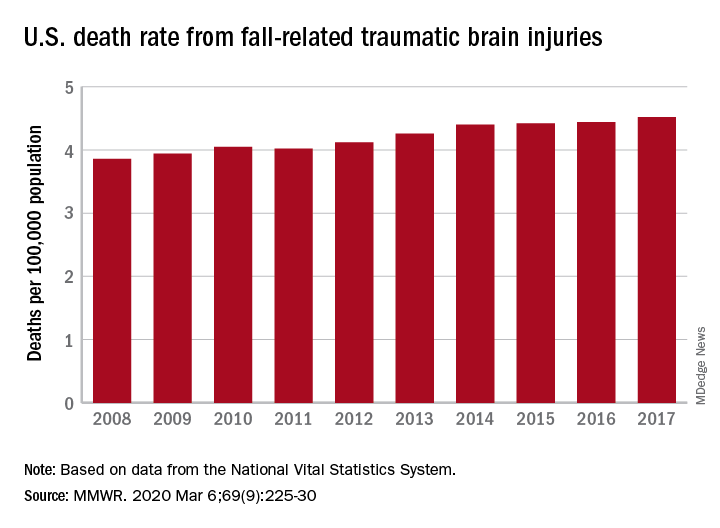
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
A 17% surge in mortality from fall-related traumatic brain injuries from 2008 to 2017 was driven largely by increases among those aged 75 years and older, according to investigators from the Centers for Disease Control and Prevention.
Nationally, the rate of deaths from traumatic brain injuries (TBIs) caused by unintentional falls rose from 3.86 per 100,000 population in 2008 to 4.52 per 100,000 in 2017, as the number of deaths went from 12,311 to 17,408, said Alexis B. Peterson, PhD, and Scott R. Kegler, PhD, of the CDC’s National Center for Injury Prevention and Control in Atlanta.
“This increase might be explained by longer survival following the onset of common diseases such as stroke, cancer, and heart disease or be attributable to the increasing population of older adults in the United States,” they suggested in the Mortality and Morbidity Weekly Report.
The rate of fall-related TBI among Americans aged 75 years and older increased by an average of 2.6% per year from 2008 to 2017, compared with 1.8% in those aged 55-74. Over that same time, death rates dropped for those aged 35-44 (–0.3%), 18-34 (–1.1%), and 0-17 (–4.3%), they said, based on data from the National Vital Statistics System’s multiple cause-of-death database.
The death rate increased fastest in residents of rural areas (2.9% per year), but deaths from fall-related TBI were up at all levels of urbanization. The largest central cities and fringe metro areas were up by 1.4% a year, with larger annual increases seen in medium-size cities (2.1%), small cities (2.2%), and small towns (2.1%), Dr. Peterson and Dr. Kegler said.
Rates of TBI-related mortality in general are higher in rural areas, they noted, and “heterogeneity in the availability and accessibility of resources (e.g., access to high-level trauma centers and rehabilitative services) can result in disparities in postinjury outcomes.”
State-specific rates increased in 45 states, although Alaska was excluded from the analysis because of its small number of cases (less than 20). Increases were significant in 29 states, but none of the changes were significant in the 4 states with lower rates at the end of the study period, the investigators reported.
“In older adults, evidence-based fall prevention strategies can prevent falls and avert costly medical expenditures,” Dr. Peterson and Dr. Kegler said, suggesting that health care providers “consider prescribing exercises that incorporate balance, strength and gait activities, such as tai chi, and reviewing and managing medications linked to falls.”
SOURCE: Peterson AB, Kegler SR. MMWR. 2019 Mar 6;69(9):225-30.
FROM MMWR
Flu activity declines again but remains high
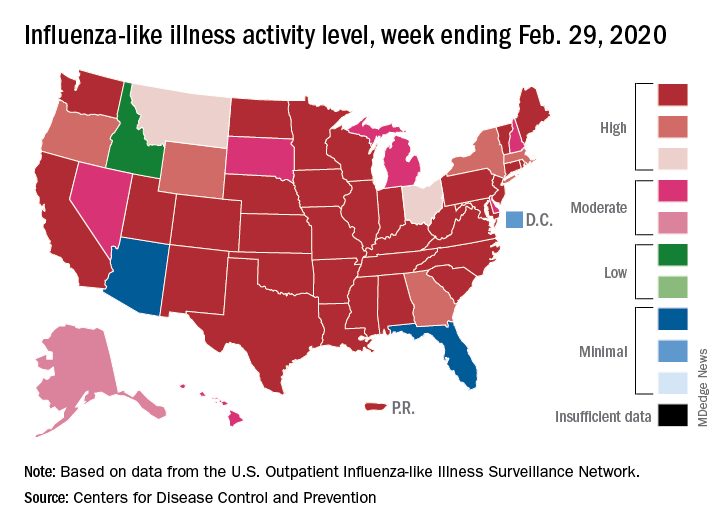
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Survey: 2020 will see more attacks on ACA
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
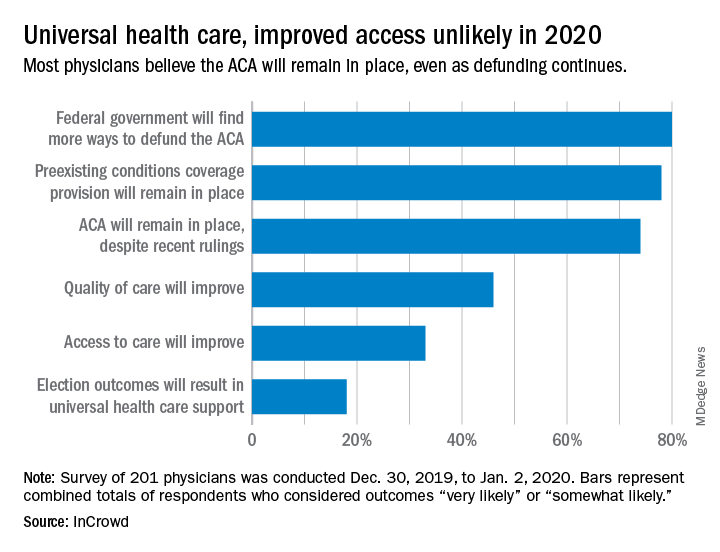
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
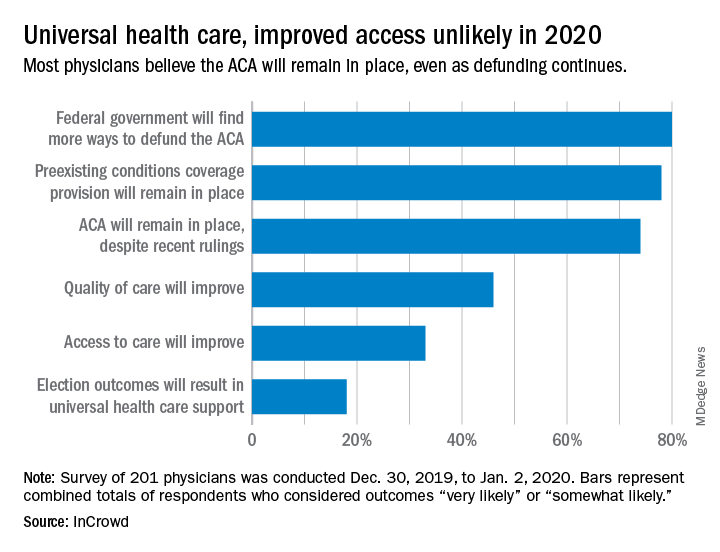
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
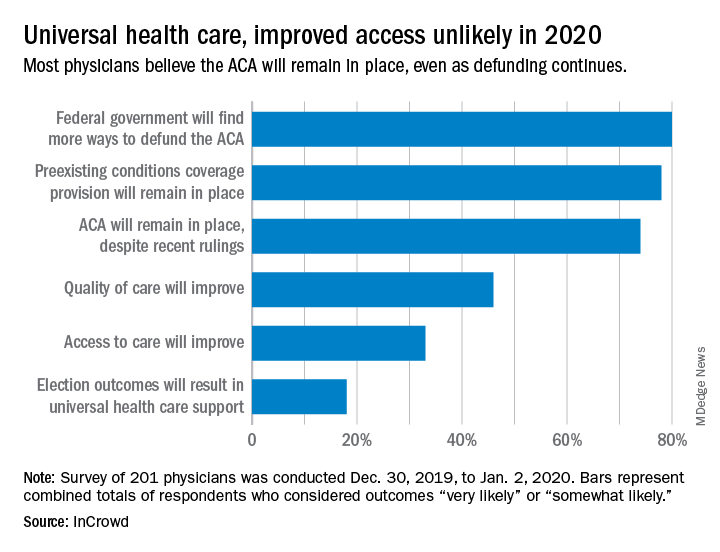
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
COVID-19’s hairy conspiracy, and a Kardashian Kolonoscopy
Coronavirus conspiracy gets hairy
It was inevitable, of course. The government’s response to COVID-19 and the novel coronavirus has become an issue, and the increased scrutiny has now turned up a conspiracy.
This particular plot, recently uncovered by the Twitterverse and reported by Newsweek, is being perpetuated by the CDC against the American patriots who make up the bearded wings of the Men-ocratic and Republi-man parties.
Our story begins on Nov. 2, 2017, when the National Institute for Occupational Safety and Health posted “To Beard or not to Beard? That’s a good Question!” on its science blog, which was aimed at “workers who wear tight-fitting respirators.” Like the N95 face mask. More than 2 years before the coronavirus was “discovered” in China. Hmmm, interesting.
The NIOSH post claimed that beards, sideburns, and some mustaches “will interfere with respirators that rely on a tight facepiece seal to achieve maximum protection.” The agency further alleged that “research tells us that the presence of facial hair under the sealing surface causes 20 to 1,000 times more leakage, compared to clean-shaven individuals.” As if research ever proved anything.
The post’s pièce de résistance, however, was an infograph illustrating 36 types of facial hairstyles and whether they worked with a face mask/respirator. Did you know that beard styles such as the chin curtain, French fork, Garibaldi, and Hulihee get a thumbs down? Did you know there are beard styles called the chin curtain, French fork, Garibaldi, and Hulihee? [What? No ZZ Top beard?]
Most mustaches are okay, though, and therein lies the proof of a conspiracy. Among the approved mustache styles is the toothbrush. You’ll find it on the bottom row of the graph, third from the left. Notice anything?
It’s a Hitler mustache! The CDC put its seal of approval on a Hitler mustache!
Thus, by the transfollicular property of the High Castle corollary to the Boys from Brazil theorem, a government conspiracy must exist.
The coronavirus will now proceed to take over the world. Have a nice day.
Keeping up with the Kolonoscopies
Imagine owing your life to the Kardashians. It’s a bit tough to swallow, but a man from Ohio owes Kim and her Krew a life debt.
Gary Paine was just passing the time, watching some daytime “Keeping Up With the Kardashians” television in the doctor’s waiting room while his wife was getting a colonoscopy. We’ve all been there – we in the Bureau of LOTME have watched more waiting-room “Judge Judy” than we care to admit.
And just like us, Gary said he was getting bored while watching the Kardashians’ TV travails. Although he felt relatively healthy, he decided to distract himself the best way he knew how: making his own colonoscopy appointment. Anything’s better than getting sucked into an 8-hour Kardashian marathon, right?
During Gary’s Kim K–inspired colonoscopy, it was discovered that he had an irregularity in his heart. Eventually, doctors found two severely blocked arteries. Paine underwent immediate, lifesaving quadruple-bypass surgery.
He now urges people to be aware that checkups are essential, whether you’re showing symptoms of poor health or not.
Which leads us to wonder: Do Kris Jenner and her clan know they’re now officially more painful than a colonoscopy appointment?
(Crosswalks) Don’t stop me now
There’s always that one guy. You’re stuck in a long line behind a big slow tractor trailer going 10 under the speed limit, and there’s a flashy BMW practically living inside your trunk. A brief passing zone approaches, but there’s no point ... oh, of course they swerve around and cut you off, what did they even gain from doing that?
Point is, people who drive expensive cars have a bit of a reputation for being less than courteous behind the wheel, and thanks to a study published in the Journal of Transport & Health, there’s some science to back that up.
A group of four presumably well-paid volunteers were sent out to crosswalks and crossed in front of cars to see how many would yield. Results were less than encouraging: Only 28% of 461 cars yielded. The only factor that significantly predicted whether or not a car would yield was how expensive it was; for every $1,000 increase in the value of the car, the driver was 3% less likely to stop.
It’s not looking good for owners of expensive cars, especially when even the study authors suggest that these drivers were displaying increased entitlement and narcissism through their lack of yielding behavior.
Our suggestion? Clearly rich people are sick and need intensive psychotherapy, and the offending vehicles should be removed and redistributed to the rest of us. We wouldn’t mind a nice slightly used Corvette, in red preferably. Nope, no ulterior motive here.
Coronavirus conspiracy gets hairy
It was inevitable, of course. The government’s response to COVID-19 and the novel coronavirus has become an issue, and the increased scrutiny has now turned up a conspiracy.
This particular plot, recently uncovered by the Twitterverse and reported by Newsweek, is being perpetuated by the CDC against the American patriots who make up the bearded wings of the Men-ocratic and Republi-man parties.
Our story begins on Nov. 2, 2017, when the National Institute for Occupational Safety and Health posted “To Beard or not to Beard? That’s a good Question!” on its science blog, which was aimed at “workers who wear tight-fitting respirators.” Like the N95 face mask. More than 2 years before the coronavirus was “discovered” in China. Hmmm, interesting.
The NIOSH post claimed that beards, sideburns, and some mustaches “will interfere with respirators that rely on a tight facepiece seal to achieve maximum protection.” The agency further alleged that “research tells us that the presence of facial hair under the sealing surface causes 20 to 1,000 times more leakage, compared to clean-shaven individuals.” As if research ever proved anything.
The post’s pièce de résistance, however, was an infograph illustrating 36 types of facial hairstyles and whether they worked with a face mask/respirator. Did you know that beard styles such as the chin curtain, French fork, Garibaldi, and Hulihee get a thumbs down? Did you know there are beard styles called the chin curtain, French fork, Garibaldi, and Hulihee? [What? No ZZ Top beard?]
Most mustaches are okay, though, and therein lies the proof of a conspiracy. Among the approved mustache styles is the toothbrush. You’ll find it on the bottom row of the graph, third from the left. Notice anything?
It’s a Hitler mustache! The CDC put its seal of approval on a Hitler mustache!
Thus, by the transfollicular property of the High Castle corollary to the Boys from Brazil theorem, a government conspiracy must exist.
The coronavirus will now proceed to take over the world. Have a nice day.
Keeping up with the Kolonoscopies
Imagine owing your life to the Kardashians. It’s a bit tough to swallow, but a man from Ohio owes Kim and her Krew a life debt.
Gary Paine was just passing the time, watching some daytime “Keeping Up With the Kardashians” television in the doctor’s waiting room while his wife was getting a colonoscopy. We’ve all been there – we in the Bureau of LOTME have watched more waiting-room “Judge Judy” than we care to admit.
And just like us, Gary said he was getting bored while watching the Kardashians’ TV travails. Although he felt relatively healthy, he decided to distract himself the best way he knew how: making his own colonoscopy appointment. Anything’s better than getting sucked into an 8-hour Kardashian marathon, right?
During Gary’s Kim K–inspired colonoscopy, it was discovered that he had an irregularity in his heart. Eventually, doctors found two severely blocked arteries. Paine underwent immediate, lifesaving quadruple-bypass surgery.
He now urges people to be aware that checkups are essential, whether you’re showing symptoms of poor health or not.
Which leads us to wonder: Do Kris Jenner and her clan know they’re now officially more painful than a colonoscopy appointment?
(Crosswalks) Don’t stop me now
There’s always that one guy. You’re stuck in a long line behind a big slow tractor trailer going 10 under the speed limit, and there’s a flashy BMW practically living inside your trunk. A brief passing zone approaches, but there’s no point ... oh, of course they swerve around and cut you off, what did they even gain from doing that?
Point is, people who drive expensive cars have a bit of a reputation for being less than courteous behind the wheel, and thanks to a study published in the Journal of Transport & Health, there’s some science to back that up.
A group of four presumably well-paid volunteers were sent out to crosswalks and crossed in front of cars to see how many would yield. Results were less than encouraging: Only 28% of 461 cars yielded. The only factor that significantly predicted whether or not a car would yield was how expensive it was; for every $1,000 increase in the value of the car, the driver was 3% less likely to stop.
It’s not looking good for owners of expensive cars, especially when even the study authors suggest that these drivers were displaying increased entitlement and narcissism through their lack of yielding behavior.
Our suggestion? Clearly rich people are sick and need intensive psychotherapy, and the offending vehicles should be removed and redistributed to the rest of us. We wouldn’t mind a nice slightly used Corvette, in red preferably. Nope, no ulterior motive here.
Coronavirus conspiracy gets hairy
It was inevitable, of course. The government’s response to COVID-19 and the novel coronavirus has become an issue, and the increased scrutiny has now turned up a conspiracy.
This particular plot, recently uncovered by the Twitterverse and reported by Newsweek, is being perpetuated by the CDC against the American patriots who make up the bearded wings of the Men-ocratic and Republi-man parties.
Our story begins on Nov. 2, 2017, when the National Institute for Occupational Safety and Health posted “To Beard or not to Beard? That’s a good Question!” on its science blog, which was aimed at “workers who wear tight-fitting respirators.” Like the N95 face mask. More than 2 years before the coronavirus was “discovered” in China. Hmmm, interesting.
The NIOSH post claimed that beards, sideburns, and some mustaches “will interfere with respirators that rely on a tight facepiece seal to achieve maximum protection.” The agency further alleged that “research tells us that the presence of facial hair under the sealing surface causes 20 to 1,000 times more leakage, compared to clean-shaven individuals.” As if research ever proved anything.
The post’s pièce de résistance, however, was an infograph illustrating 36 types of facial hairstyles and whether they worked with a face mask/respirator. Did you know that beard styles such as the chin curtain, French fork, Garibaldi, and Hulihee get a thumbs down? Did you know there are beard styles called the chin curtain, French fork, Garibaldi, and Hulihee? [What? No ZZ Top beard?]
Most mustaches are okay, though, and therein lies the proof of a conspiracy. Among the approved mustache styles is the toothbrush. You’ll find it on the bottom row of the graph, third from the left. Notice anything?
It’s a Hitler mustache! The CDC put its seal of approval on a Hitler mustache!
Thus, by the transfollicular property of the High Castle corollary to the Boys from Brazil theorem, a government conspiracy must exist.
The coronavirus will now proceed to take over the world. Have a nice day.
Keeping up with the Kolonoscopies
Imagine owing your life to the Kardashians. It’s a bit tough to swallow, but a man from Ohio owes Kim and her Krew a life debt.
Gary Paine was just passing the time, watching some daytime “Keeping Up With the Kardashians” television in the doctor’s waiting room while his wife was getting a colonoscopy. We’ve all been there – we in the Bureau of LOTME have watched more waiting-room “Judge Judy” than we care to admit.
And just like us, Gary said he was getting bored while watching the Kardashians’ TV travails. Although he felt relatively healthy, he decided to distract himself the best way he knew how: making his own colonoscopy appointment. Anything’s better than getting sucked into an 8-hour Kardashian marathon, right?
During Gary’s Kim K–inspired colonoscopy, it was discovered that he had an irregularity in his heart. Eventually, doctors found two severely blocked arteries. Paine underwent immediate, lifesaving quadruple-bypass surgery.
He now urges people to be aware that checkups are essential, whether you’re showing symptoms of poor health or not.
Which leads us to wonder: Do Kris Jenner and her clan know they’re now officially more painful than a colonoscopy appointment?
(Crosswalks) Don’t stop me now
There’s always that one guy. You’re stuck in a long line behind a big slow tractor trailer going 10 under the speed limit, and there’s a flashy BMW practically living inside your trunk. A brief passing zone approaches, but there’s no point ... oh, of course they swerve around and cut you off, what did they even gain from doing that?
Point is, people who drive expensive cars have a bit of a reputation for being less than courteous behind the wheel, and thanks to a study published in the Journal of Transport & Health, there’s some science to back that up.
A group of four presumably well-paid volunteers were sent out to crosswalks and crossed in front of cars to see how many would yield. Results were less than encouraging: Only 28% of 461 cars yielded. The only factor that significantly predicted whether or not a car would yield was how expensive it was; for every $1,000 increase in the value of the car, the driver was 3% less likely to stop.
It’s not looking good for owners of expensive cars, especially when even the study authors suggest that these drivers were displaying increased entitlement and narcissism through their lack of yielding behavior.
Our suggestion? Clearly rich people are sick and need intensive psychotherapy, and the offending vehicles should be removed and redistributed to the rest of us. We wouldn’t mind a nice slightly used Corvette, in red preferably. Nope, no ulterior motive here.
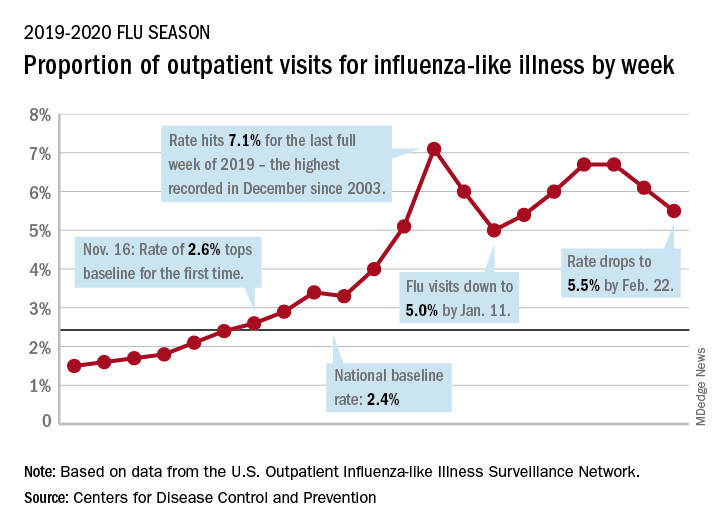
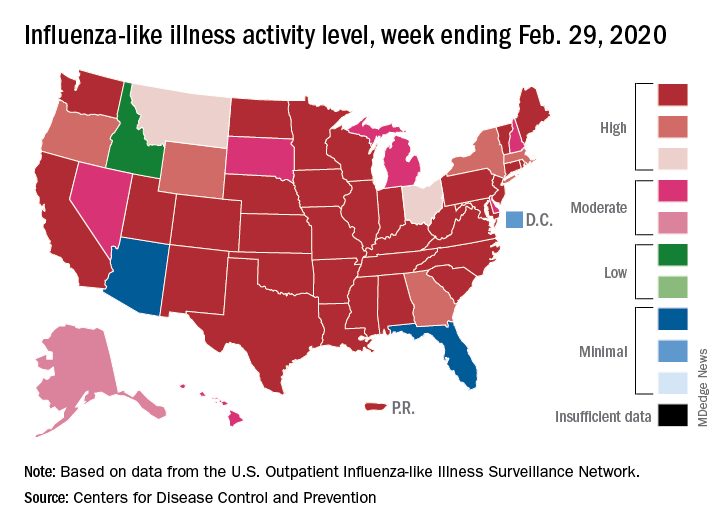
Children bearing the brunt of declining flu activity
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”
A bladder brewery and a neurosurgical violin solo
One bikram, one shakti, one beer
Novelty yoga is a thing, and there’s no stopping it now.
There’s cat yoga, aerial yoga (performed in a harness or hammock suspended above the ground), karaoke yoga, laughter yoga (done while listening to the LOTME podcast, no doubt), snake yoga, toega (yoga for toes), and, of course, goat yoga. So what’s next, beer yoga?
Why, yes, it is beer yoga.
In our travels around the dark, deserted corners of the Internet, we came across an article on Educatedbox.com that said a beer yoga class “involves picking up a beer, drinking it, and putting it back down again, in many different ways.”
Pretty straightforward. Then we saw a photo on Germany’s Bieryoga.de that showed all of the participants doing the tree pose while balancing a beer bottle on their heads. Not so straightforward. Trust us, we tried.
Bieryoga explains that “the exuberance that comes with drinking beer and the body awareness of yoga can be combined into an energizing experience. In the beer and now.”
How can we say no to “in the beer and now”? Well, we can’t, but we do have one teeny tiny problem: We’ve gotten into “downward-facing dog with IPA on rump,” and now we can’t get up.
Little help … anyone?
A surgical symphony
A patient playing the violin during her own brain surgery? That sounds way more interesting than paying hundreds of dollars to attend any old normal concert.
Violinist Dagmar Turner found out in 2013 that she had a brain tumor that was gradually advancing in size. After learning the tumor needed to be removed, Ms. Turner worried she might lose her talents if the parts of her brain crucial to playing the violin were destroyed.
Luckily, her well-orchestrated surgical team composed a plan to ensure they spared the vital parts of the brain used when playing the violin: They would wake their patient during brain surgery and have her play her violin. Yes, you read that right – she played the violin during surgery to help her surgeons make certain there was no damage to the violin-related areas of her brain.
Personally, we here at the profit-minded Bureau of LOTME believe the surgical team missed a perfect opportunity to sell tickets to this event. Ms. Turner successfully made it through the surgery both 90% tumor free and fully able to play her violin. We love a happy ending! Bravo! Though maybe not “Encore!”
Belly up to the bar, boys
Quick, what would be the worst superpower? No doubt your head is flooding with ideas, each more comical than the last. But did you think of “able to pee beer?”
That’s right, it’s the return of an old LOTME favorite – auto-brewery syndrome. But this time, there’s a twist.
Our daring hero in today’s exciting case report from Annals of Internal Medicine is a 61-year-old woman from Pittsburgh who presented with liver damage and poorly controlled diabetes, and who sought placement on the liver transplant list.
But hang on, the woman’s history seemed to indicate her liver problems stemmed from alcohol addiction, because her urine tests were always positive for alcohol, and the current tests said the same. Hmm, this is sounding slightly villainous!
There were, however, some discrepancies. The woman didn’t appear to be intoxicated during clinic visits, tests for ethanol metabolites were negative while urine tests for ethanol were positive, and there were large quantities of glucose and budding yeast in the urine. Something strange was going on, so the doctors decided to dig deeper.
The yeast in question was Candida glabrata, which is closely related to brewer’s yeast. The doctors found high levels of ethanol production in the urine, suggesting that the yeast was fermenting sugar inside the bladder. The patient was quite literally urinating alcohol, becoming the first documented case in a living person of what the doctors dubbed “urinary auto-brewery syndrome.”
As much as we love a good drink here at LOTME world headquarters, we’ll have to pass on the urine cocktail. Just don’t tell all the beer yoga enthusiasts, this seems right up their alley. You know, positive natural energy flow or something like that.
One bikram, one shakti, one beer
Novelty yoga is a thing, and there’s no stopping it now.
There’s cat yoga, aerial yoga (performed in a harness or hammock suspended above the ground), karaoke yoga, laughter yoga (done while listening to the LOTME podcast, no doubt), snake yoga, toega (yoga for toes), and, of course, goat yoga. So what’s next, beer yoga?
Why, yes, it is beer yoga.
In our travels around the dark, deserted corners of the Internet, we came across an article on Educatedbox.com that said a beer yoga class “involves picking up a beer, drinking it, and putting it back down again, in many different ways.”
Pretty straightforward. Then we saw a photo on Germany’s Bieryoga.de that showed all of the participants doing the tree pose while balancing a beer bottle on their heads. Not so straightforward. Trust us, we tried.
Bieryoga explains that “the exuberance that comes with drinking beer and the body awareness of yoga can be combined into an energizing experience. In the beer and now.”
How can we say no to “in the beer and now”? Well, we can’t, but we do have one teeny tiny problem: We’ve gotten into “downward-facing dog with IPA on rump,” and now we can’t get up.
Little help … anyone?
A surgical symphony
A patient playing the violin during her own brain surgery? That sounds way more interesting than paying hundreds of dollars to attend any old normal concert.
Violinist Dagmar Turner found out in 2013 that she had a brain tumor that was gradually advancing in size. After learning the tumor needed to be removed, Ms. Turner worried she might lose her talents if the parts of her brain crucial to playing the violin were destroyed.
Luckily, her well-orchestrated surgical team composed a plan to ensure they spared the vital parts of the brain used when playing the violin: They would wake their patient during brain surgery and have her play her violin. Yes, you read that right – she played the violin during surgery to help her surgeons make certain there was no damage to the violin-related areas of her brain.
Personally, we here at the profit-minded Bureau of LOTME believe the surgical team missed a perfect opportunity to sell tickets to this event. Ms. Turner successfully made it through the surgery both 90% tumor free and fully able to play her violin. We love a happy ending! Bravo! Though maybe not “Encore!”
Belly up to the bar, boys
Quick, what would be the worst superpower? No doubt your head is flooding with ideas, each more comical than the last. But did you think of “able to pee beer?”
That’s right, it’s the return of an old LOTME favorite – auto-brewery syndrome. But this time, there’s a twist.
Our daring hero in today’s exciting case report from Annals of Internal Medicine is a 61-year-old woman from Pittsburgh who presented with liver damage and poorly controlled diabetes, and who sought placement on the liver transplant list.
But hang on, the woman’s history seemed to indicate her liver problems stemmed from alcohol addiction, because her urine tests were always positive for alcohol, and the current tests said the same. Hmm, this is sounding slightly villainous!
There were, however, some discrepancies. The woman didn’t appear to be intoxicated during clinic visits, tests for ethanol metabolites were negative while urine tests for ethanol were positive, and there were large quantities of glucose and budding yeast in the urine. Something strange was going on, so the doctors decided to dig deeper.
The yeast in question was Candida glabrata, which is closely related to brewer’s yeast. The doctors found high levels of ethanol production in the urine, suggesting that the yeast was fermenting sugar inside the bladder. The patient was quite literally urinating alcohol, becoming the first documented case in a living person of what the doctors dubbed “urinary auto-brewery syndrome.”
As much as we love a good drink here at LOTME world headquarters, we’ll have to pass on the urine cocktail. Just don’t tell all the beer yoga enthusiasts, this seems right up their alley. You know, positive natural energy flow or something like that.
One bikram, one shakti, one beer
Novelty yoga is a thing, and there’s no stopping it now.
There’s cat yoga, aerial yoga (performed in a harness or hammock suspended above the ground), karaoke yoga, laughter yoga (done while listening to the LOTME podcast, no doubt), snake yoga, toega (yoga for toes), and, of course, goat yoga. So what’s next, beer yoga?
Why, yes, it is beer yoga.
In our travels around the dark, deserted corners of the Internet, we came across an article on Educatedbox.com that said a beer yoga class “involves picking up a beer, drinking it, and putting it back down again, in many different ways.”
Pretty straightforward. Then we saw a photo on Germany’s Bieryoga.de that showed all of the participants doing the tree pose while balancing a beer bottle on their heads. Not so straightforward. Trust us, we tried.
Bieryoga explains that “the exuberance that comes with drinking beer and the body awareness of yoga can be combined into an energizing experience. In the beer and now.”
How can we say no to “in the beer and now”? Well, we can’t, but we do have one teeny tiny problem: We’ve gotten into “downward-facing dog with IPA on rump,” and now we can’t get up.
Little help … anyone?
A surgical symphony
A patient playing the violin during her own brain surgery? That sounds way more interesting than paying hundreds of dollars to attend any old normal concert.
Violinist Dagmar Turner found out in 2013 that she had a brain tumor that was gradually advancing in size. After learning the tumor needed to be removed, Ms. Turner worried she might lose her talents if the parts of her brain crucial to playing the violin were destroyed.
Luckily, her well-orchestrated surgical team composed a plan to ensure they spared the vital parts of the brain used when playing the violin: They would wake their patient during brain surgery and have her play her violin. Yes, you read that right – she played the violin during surgery to help her surgeons make certain there was no damage to the violin-related areas of her brain.
Personally, we here at the profit-minded Bureau of LOTME believe the surgical team missed a perfect opportunity to sell tickets to this event. Ms. Turner successfully made it through the surgery both 90% tumor free and fully able to play her violin. We love a happy ending! Bravo! Though maybe not “Encore!”
Belly up to the bar, boys
Quick, what would be the worst superpower? No doubt your head is flooding with ideas, each more comical than the last. But did you think of “able to pee beer?”
That’s right, it’s the return of an old LOTME favorite – auto-brewery syndrome. But this time, there’s a twist.
Our daring hero in today’s exciting case report from Annals of Internal Medicine is a 61-year-old woman from Pittsburgh who presented with liver damage and poorly controlled diabetes, and who sought placement on the liver transplant list.
But hang on, the woman’s history seemed to indicate her liver problems stemmed from alcohol addiction, because her urine tests were always positive for alcohol, and the current tests said the same. Hmm, this is sounding slightly villainous!
There were, however, some discrepancies. The woman didn’t appear to be intoxicated during clinic visits, tests for ethanol metabolites were negative while urine tests for ethanol were positive, and there were large quantities of glucose and budding yeast in the urine. Something strange was going on, so the doctors decided to dig deeper.
The yeast in question was Candida glabrata, which is closely related to brewer’s yeast. The doctors found high levels of ethanol production in the urine, suggesting that the yeast was fermenting sugar inside the bladder. The patient was quite literally urinating alcohol, becoming the first documented case in a living person of what the doctors dubbed “urinary auto-brewery syndrome.”
As much as we love a good drink here at LOTME world headquarters, we’ll have to pass on the urine cocktail. Just don’t tell all the beer yoga enthusiasts, this seems right up their alley. You know, positive natural energy flow or something like that.
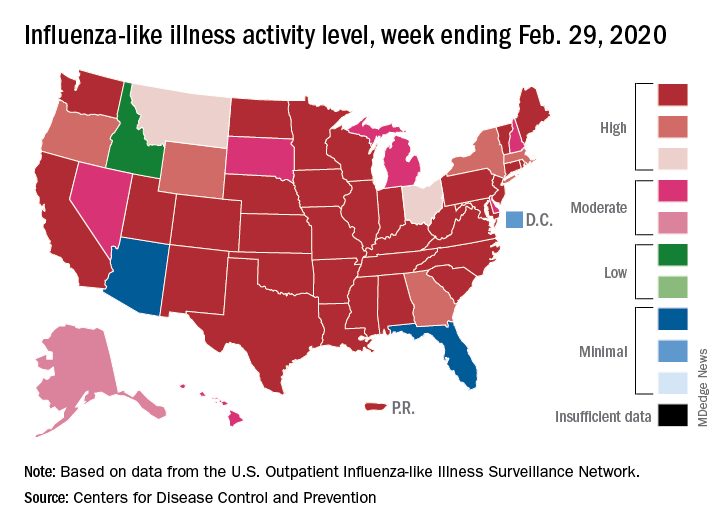
Drop in flu activity suggests season may have peaked
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
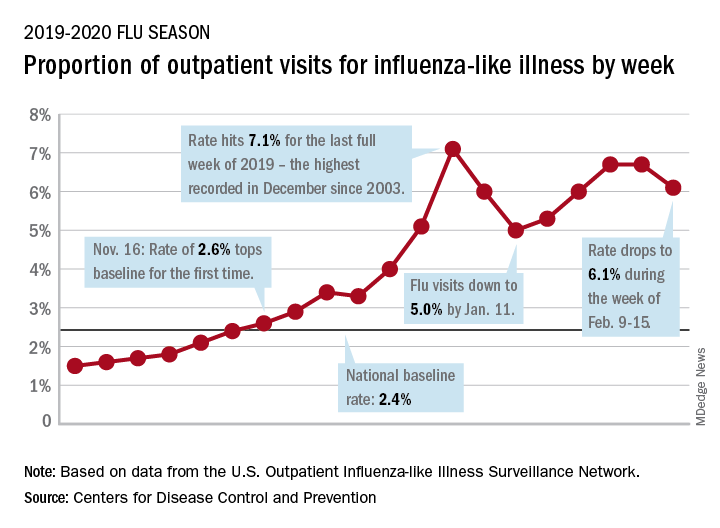
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.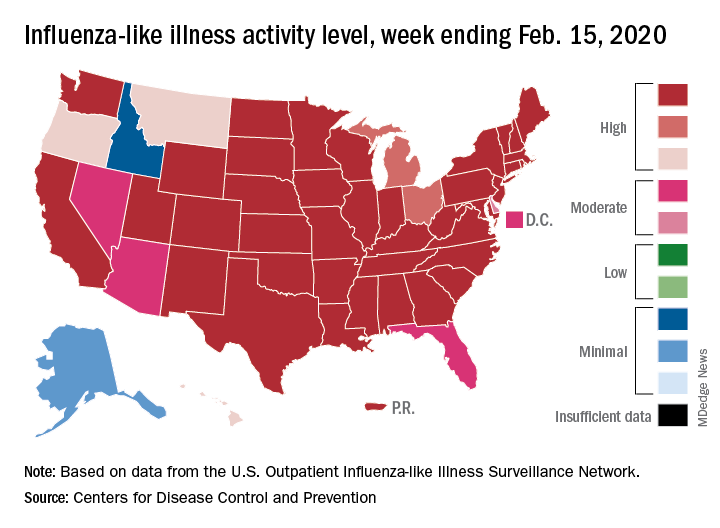
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
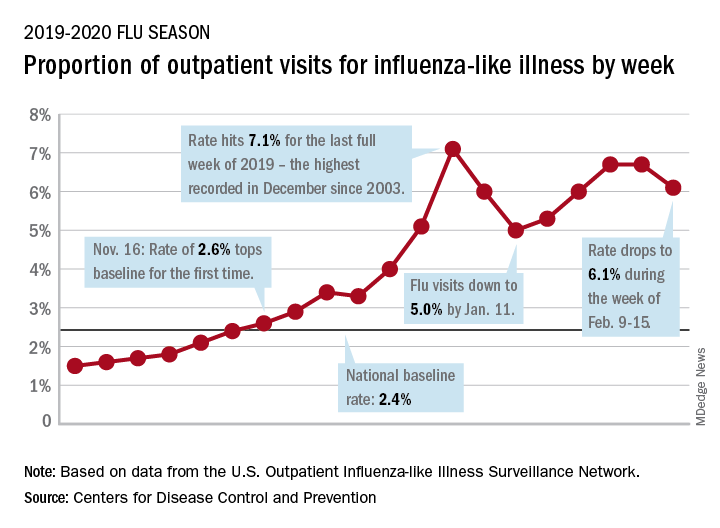
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.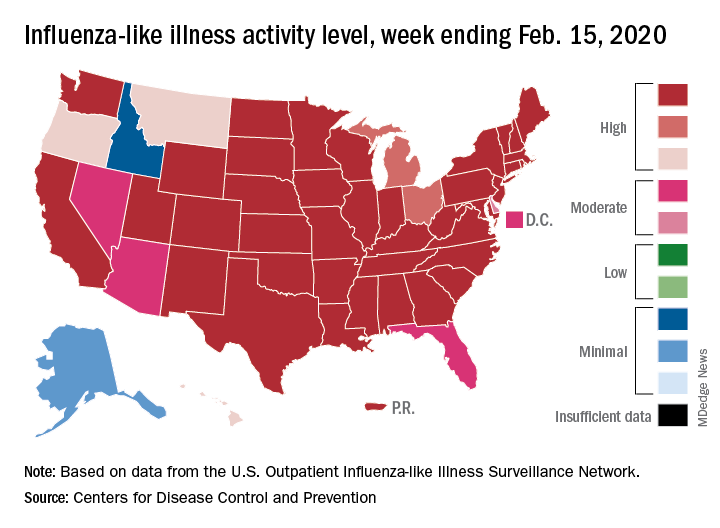
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
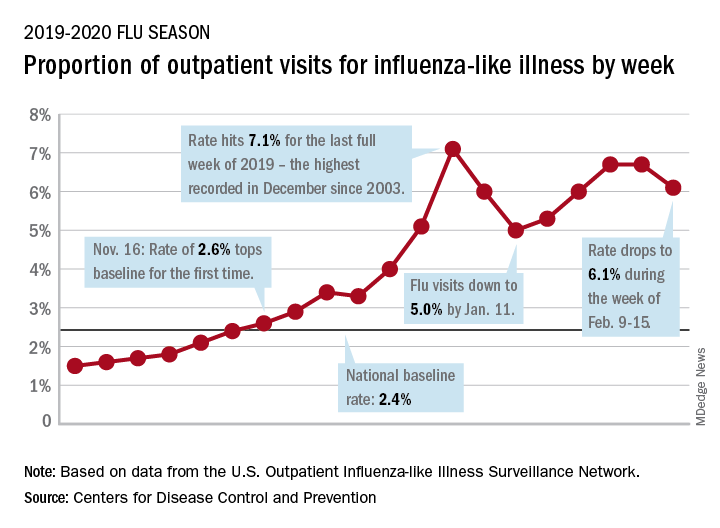
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.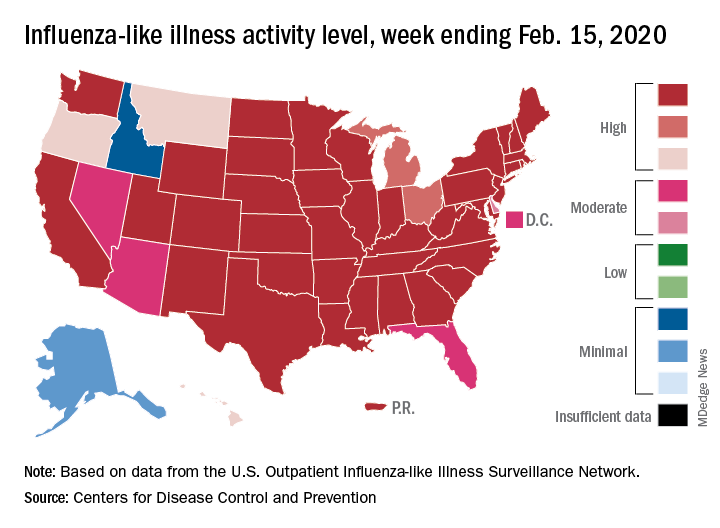
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
FROM THE CDC
Texas’ tasty heart cake and Gotham’s coronavirus robot
Make dialysis great again!
Now, you’re probably thinking that Mr. Nelson tried to bring in his dog or some other animal, and that’s surely an issue of hygiene. But no, Mr. Gibson wasn’t bringing in a dog or cat, or even a squirrel or turkey, but a president.
Specifically, Mr. Nelson’s emotional support was one President Donald J. Trump.
Okay, it wasn’t actually Mr. Trump himself, but a life-sized (bigly?) cardboard cutout of the president smiling and offering two thumbs up. This, um, unusual choice was based on the president’s signing of an executive order in July 2019 launching an initiative promoting kidney disease awareness.
Mr. Nelson had previously been bringing in smaller images of the president. But when he brought in the large cutout – made by his son – a social worker at the center told him that the president couldn’t stay, adding that “this is not a Trump rally,” according to Mr. Nelson.
Naturally, this has caused quite a rift. Mr. Nelson feels that his freedom of expression and speech has been violated, and Fresenius says they can’t allow a support item so big because of those pesky health and safety regulations. Typical doctors.
The actual President Trump has yet to respond to this odd situation, but no doubt he’ll offer Fresenius a hearty “you’re fired!”
Your friendly neighborhood pandemic robot
Robots, of course!
A shiny new robot in Times Square not only can recognize symptoms of the coronavirus, it also can provide information to promote prevention and stop the spread. And if you look like a tourist, it’ll try to sell you half-priced tickets for a Big Apple bus tour. Move over, smartphones; having a robot analyze my symptoms sounds way more fun than frantically googling them.
The “Promobot” was designed with a friendly face and welcoming smile – that’s how you know the robot isn’t a local.
Interested users can interact with the Promobot’s iPad, which has a questionnaire regarding signs and symptoms of the coronavirus. Promobot doesn’t actually physically detect the virus (it’s a robot, not a blood test), but the questionnaire asks about general symptoms of coronavirus. At the end, the robot gives advice on how to proceed if the answers indicate the virus is present (hopefully without any panic-inducing fanfare).
Ah, New York: Where even the robots are friendlier than the residents.
Beating? No. Delicious? Yes
No, it’s a cake!
Heart!
Cake!
Wait, you’re both right. It’s two treats in one! It’s a heart and a cake. It’s the cake that looks like a heart.
Seriously, it really looks like a heart. It looks like it should still be beating. We’re talking anatomically correct and glistening with just-pulled-from-the-body freshness.
This latest wonder of the baking world comes from Crabby Cakes in Portland, Tex., just across the Nueces Bay Causeway from Corpus Christi. Just get on West Broadway Avenue from the I-181 frontage road, then make a right onto Wildcat Drive and a left at Maple Drive.
Crabby Cakes owner Jessica Wolfe is a big fan of horror movies and has even visited some of the sites where scenes were shot for “The Texas Chain Saw Massacre.” She told the Dallas Morning News that she “was trying to do something different for Valentine’s Day, cake-wise.”
She posted a video of the cake on the bakery’s Facebook page and it went viral, gobbling up over a million views in less than a week, the Morning News reported. Each cake costs $70 and will feed about five people, but the bakery cannot ship them out of state.
Among the cake-generated surprises was the attention she got from the health care industry. “Nurses, doctor’s offices, and graduates want the hearts,” Ms. Wolfe told the Morning News. “But they also want livers, kidneys, and lungs.”
Let’s just hope there aren’t any transplant surgeons calling.
Make dialysis great again!
Now, you’re probably thinking that Mr. Nelson tried to bring in his dog or some other animal, and that’s surely an issue of hygiene. But no, Mr. Gibson wasn’t bringing in a dog or cat, or even a squirrel or turkey, but a president.
Specifically, Mr. Nelson’s emotional support was one President Donald J. Trump.
Okay, it wasn’t actually Mr. Trump himself, but a life-sized (bigly?) cardboard cutout of the president smiling and offering two thumbs up. This, um, unusual choice was based on the president’s signing of an executive order in July 2019 launching an initiative promoting kidney disease awareness.
Mr. Nelson had previously been bringing in smaller images of the president. But when he brought in the large cutout – made by his son – a social worker at the center told him that the president couldn’t stay, adding that “this is not a Trump rally,” according to Mr. Nelson.
Naturally, this has caused quite a rift. Mr. Nelson feels that his freedom of expression and speech has been violated, and Fresenius says they can’t allow a support item so big because of those pesky health and safety regulations. Typical doctors.
The actual President Trump has yet to respond to this odd situation, but no doubt he’ll offer Fresenius a hearty “you’re fired!”
Your friendly neighborhood pandemic robot
Robots, of course!
A shiny new robot in Times Square not only can recognize symptoms of the coronavirus, it also can provide information to promote prevention and stop the spread. And if you look like a tourist, it’ll try to sell you half-priced tickets for a Big Apple bus tour. Move over, smartphones; having a robot analyze my symptoms sounds way more fun than frantically googling them.
The “Promobot” was designed with a friendly face and welcoming smile – that’s how you know the robot isn’t a local.
Interested users can interact with the Promobot’s iPad, which has a questionnaire regarding signs and symptoms of the coronavirus. Promobot doesn’t actually physically detect the virus (it’s a robot, not a blood test), but the questionnaire asks about general symptoms of coronavirus. At the end, the robot gives advice on how to proceed if the answers indicate the virus is present (hopefully without any panic-inducing fanfare).
Ah, New York: Where even the robots are friendlier than the residents.
Beating? No. Delicious? Yes
No, it’s a cake!
Heart!
Cake!
Wait, you’re both right. It’s two treats in one! It’s a heart and a cake. It’s the cake that looks like a heart.
Seriously, it really looks like a heart. It looks like it should still be beating. We’re talking anatomically correct and glistening with just-pulled-from-the-body freshness.
This latest wonder of the baking world comes from Crabby Cakes in Portland, Tex., just across the Nueces Bay Causeway from Corpus Christi. Just get on West Broadway Avenue from the I-181 frontage road, then make a right onto Wildcat Drive and a left at Maple Drive.
Crabby Cakes owner Jessica Wolfe is a big fan of horror movies and has even visited some of the sites where scenes were shot for “The Texas Chain Saw Massacre.” She told the Dallas Morning News that she “was trying to do something different for Valentine’s Day, cake-wise.”
She posted a video of the cake on the bakery’s Facebook page and it went viral, gobbling up over a million views in less than a week, the Morning News reported. Each cake costs $70 and will feed about five people, but the bakery cannot ship them out of state.
Among the cake-generated surprises was the attention she got from the health care industry. “Nurses, doctor’s offices, and graduates want the hearts,” Ms. Wolfe told the Morning News. “But they also want livers, kidneys, and lungs.”
Let’s just hope there aren’t any transplant surgeons calling.
Make dialysis great again!
Now, you’re probably thinking that Mr. Nelson tried to bring in his dog or some other animal, and that’s surely an issue of hygiene. But no, Mr. Gibson wasn’t bringing in a dog or cat, or even a squirrel or turkey, but a president.
Specifically, Mr. Nelson’s emotional support was one President Donald J. Trump.
Okay, it wasn’t actually Mr. Trump himself, but a life-sized (bigly?) cardboard cutout of the president smiling and offering two thumbs up. This, um, unusual choice was based on the president’s signing of an executive order in July 2019 launching an initiative promoting kidney disease awareness.
Mr. Nelson had previously been bringing in smaller images of the president. But when he brought in the large cutout – made by his son – a social worker at the center told him that the president couldn’t stay, adding that “this is not a Trump rally,” according to Mr. Nelson.
Naturally, this has caused quite a rift. Mr. Nelson feels that his freedom of expression and speech has been violated, and Fresenius says they can’t allow a support item so big because of those pesky health and safety regulations. Typical doctors.
The actual President Trump has yet to respond to this odd situation, but no doubt he’ll offer Fresenius a hearty “you’re fired!”
Your friendly neighborhood pandemic robot
Robots, of course!
A shiny new robot in Times Square not only can recognize symptoms of the coronavirus, it also can provide information to promote prevention and stop the spread. And if you look like a tourist, it’ll try to sell you half-priced tickets for a Big Apple bus tour. Move over, smartphones; having a robot analyze my symptoms sounds way more fun than frantically googling them.
The “Promobot” was designed with a friendly face and welcoming smile – that’s how you know the robot isn’t a local.
Interested users can interact with the Promobot’s iPad, which has a questionnaire regarding signs and symptoms of the coronavirus. Promobot doesn’t actually physically detect the virus (it’s a robot, not a blood test), but the questionnaire asks about general symptoms of coronavirus. At the end, the robot gives advice on how to proceed if the answers indicate the virus is present (hopefully without any panic-inducing fanfare).
Ah, New York: Where even the robots are friendlier than the residents.
Beating? No. Delicious? Yes
No, it’s a cake!
Heart!
Cake!
Wait, you’re both right. It’s two treats in one! It’s a heart and a cake. It’s the cake that looks like a heart.
Seriously, it really looks like a heart. It looks like it should still be beating. We’re talking anatomically correct and glistening with just-pulled-from-the-body freshness.
This latest wonder of the baking world comes from Crabby Cakes in Portland, Tex., just across the Nueces Bay Causeway from Corpus Christi. Just get on West Broadway Avenue from the I-181 frontage road, then make a right onto Wildcat Drive and a left at Maple Drive.
Crabby Cakes owner Jessica Wolfe is a big fan of horror movies and has even visited some of the sites where scenes were shot for “The Texas Chain Saw Massacre.” She told the Dallas Morning News that she “was trying to do something different for Valentine’s Day, cake-wise.”
She posted a video of the cake on the bakery’s Facebook page and it went viral, gobbling up over a million views in less than a week, the Morning News reported. Each cake costs $70 and will feed about five people, but the bakery cannot ship them out of state.
Among the cake-generated surprises was the attention she got from the health care industry. “Nurses, doctor’s offices, and graduates want the hearts,” Ms. Wolfe told the Morning News. “But they also want livers, kidneys, and lungs.”
Let’s just hope there aren’t any transplant surgeons calling.
50 years of growth: More dermatologists, more demand
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
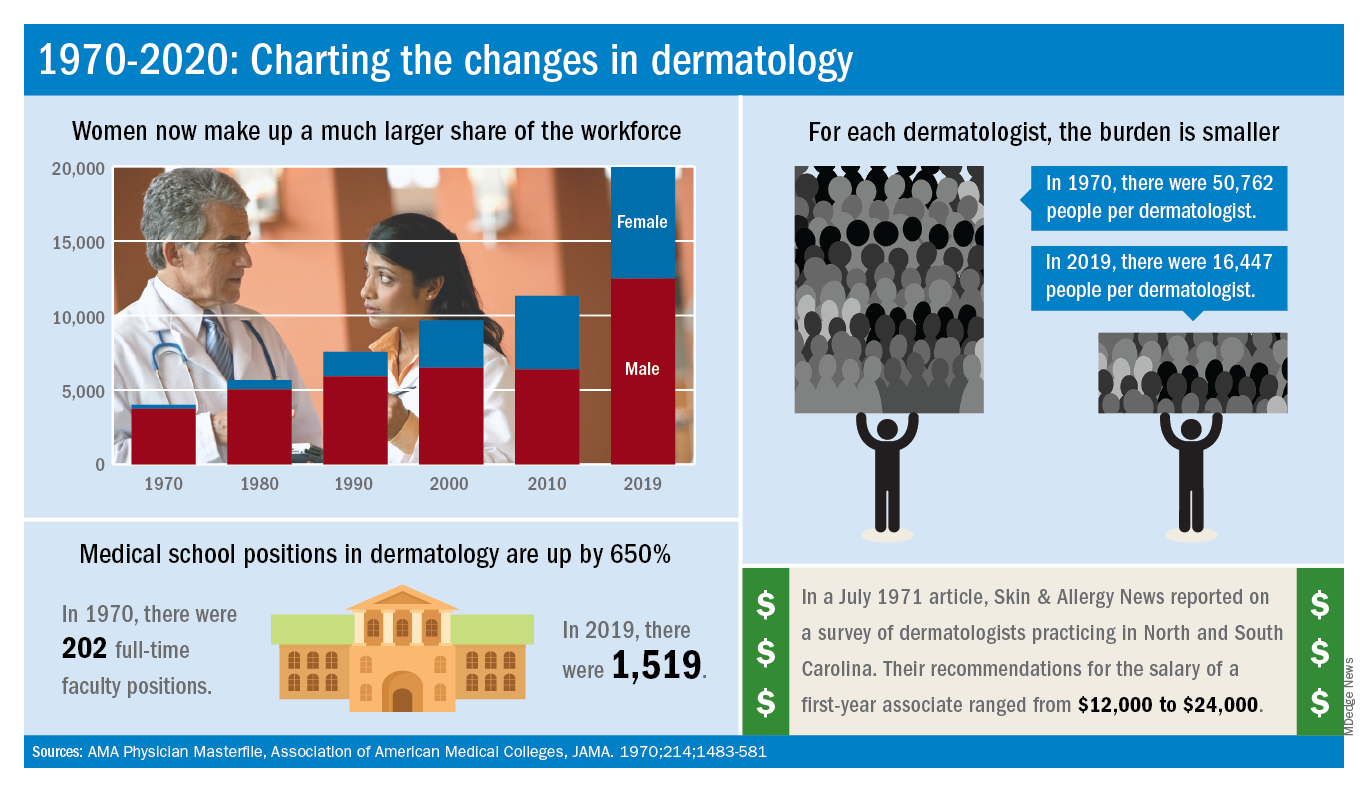
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
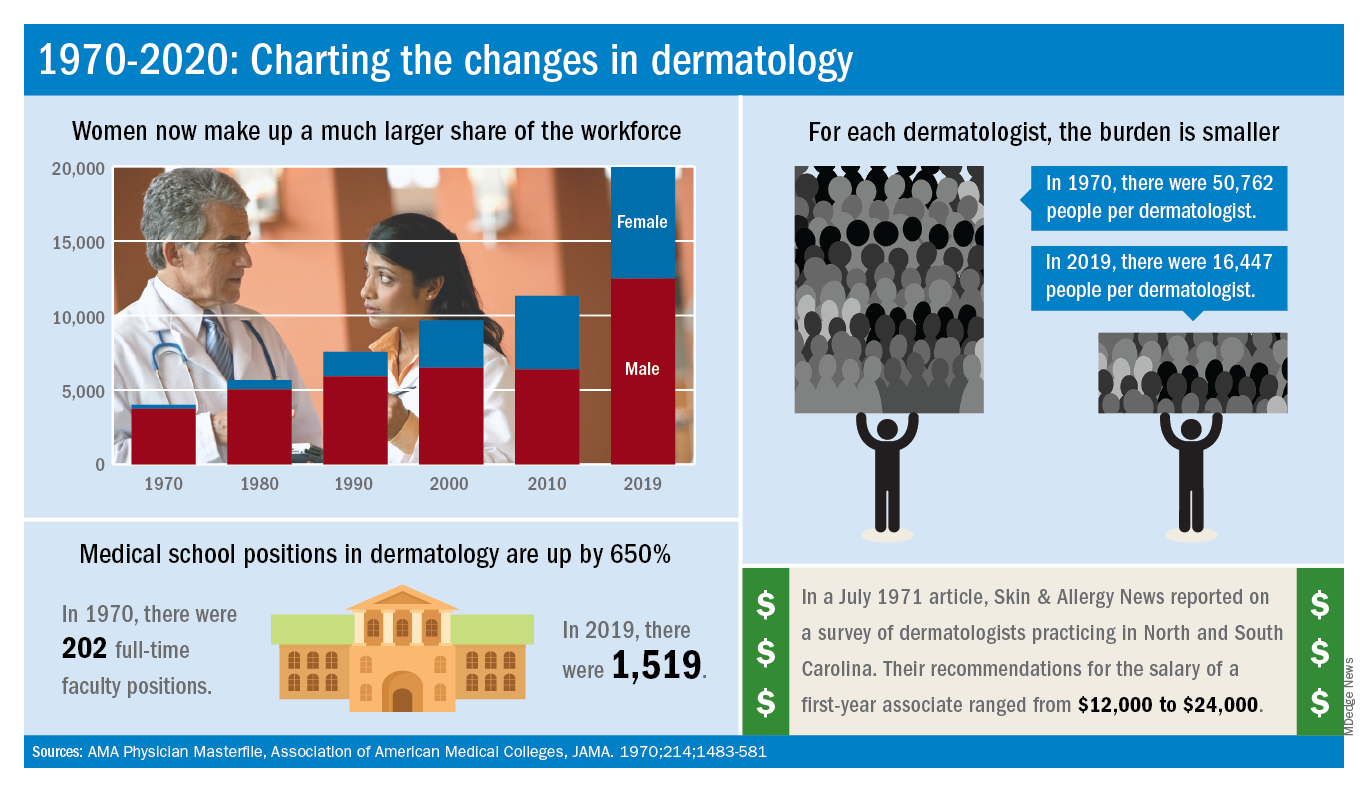
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
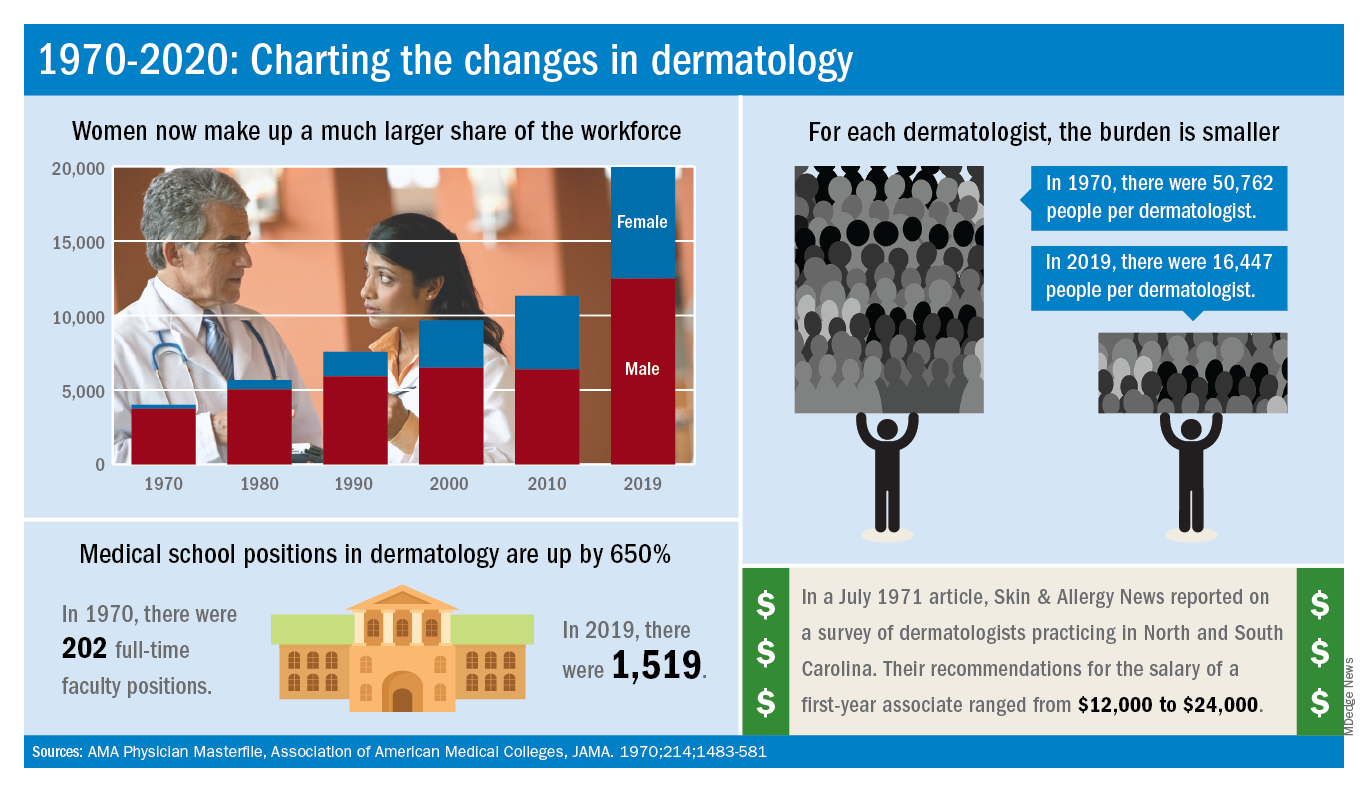
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.