User login
FDA investigating potential sex differences in LAAO adverse outcomes
The agency said it is evaluating a real-world study, published in JAMA Cardiology, of 49,357 patients in the National Cardiovascular Data Registry LAAO Registry that suggested women might be at greater risk than men for procedural outcomes, including major adverse events after device implant.
“The FDA recognizes the limitations of these data, including that the study was not randomized, only included one LAAO device (the first-generation Watchman device), and did not include longer-term outcomes beyond in-hospital events. However, the analysis provides results from a large registry of patients treated with LAAO implants in the U.S.,” the agency said in its letter to health care providers Sept. 27.
As reported last month, the study by Darden et al showed a significantly higher rate of adverse procedural events in women than in men, including any adverse events (6.3% vs. 3.9%; P < .001), any major adverse events (4.1% vs. 2.0%; P < .001), and hospital stay longer than 1 day (16.0% vs. 11.6%; P < .001). Procedure-associated death was 0.3% in women and 0.1% in men.
The agency noted that the number of patients in the LAAO Registry analysis was much larger than the number of patients in the premarket studies of the Watchman device that supported its approval and in the premarket studies for the other approved LAAO devices.
LAAO devices are indicated to reduce the risk for thromboembolism from the left atrial appendage in patients with nonvalvular atrial fibrillation who are not good candidates for long-term anticoagulation. LAAO devices currently marketed in the United States are Boston Scientific’s Watchman and Watchman FLX devices and Abbott Medical’s Amplatzer Amulet device.
“Currently, the FDA believes the benefits continue to outweigh the risks for approved LAAO devices when used in accordance with their instructions for use,” the letter states.
The FDA will work with device manufacturers to evaluate the potential issue, including a review of available premarket and postapproval study data and other available real-world, postmarket datasets, the letter notes.
The agency will also work with device manufacturers, investigators, and the LAAO Registry to try to identify the causes of procedural outcome differences between women and men.
In the letter, the FDA recommends health care providers continue monitoring patients who have been treated with LAAO devices in accordance with the current standard of care. They should also discuss the risks and benefits of all available options for stroke prevention in patients with atrial fibrillation as part of shared clinical decision-making.
Any adverse events or suspected adverse events experienced by patients with LAAO devices should also be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
The agency said it is evaluating a real-world study, published in JAMA Cardiology, of 49,357 patients in the National Cardiovascular Data Registry LAAO Registry that suggested women might be at greater risk than men for procedural outcomes, including major adverse events after device implant.
“The FDA recognizes the limitations of these data, including that the study was not randomized, only included one LAAO device (the first-generation Watchman device), and did not include longer-term outcomes beyond in-hospital events. However, the analysis provides results from a large registry of patients treated with LAAO implants in the U.S.,” the agency said in its letter to health care providers Sept. 27.
As reported last month, the study by Darden et al showed a significantly higher rate of adverse procedural events in women than in men, including any adverse events (6.3% vs. 3.9%; P < .001), any major adverse events (4.1% vs. 2.0%; P < .001), and hospital stay longer than 1 day (16.0% vs. 11.6%; P < .001). Procedure-associated death was 0.3% in women and 0.1% in men.
The agency noted that the number of patients in the LAAO Registry analysis was much larger than the number of patients in the premarket studies of the Watchman device that supported its approval and in the premarket studies for the other approved LAAO devices.
LAAO devices are indicated to reduce the risk for thromboembolism from the left atrial appendage in patients with nonvalvular atrial fibrillation who are not good candidates for long-term anticoagulation. LAAO devices currently marketed in the United States are Boston Scientific’s Watchman and Watchman FLX devices and Abbott Medical’s Amplatzer Amulet device.
“Currently, the FDA believes the benefits continue to outweigh the risks for approved LAAO devices when used in accordance with their instructions for use,” the letter states.
The FDA will work with device manufacturers to evaluate the potential issue, including a review of available premarket and postapproval study data and other available real-world, postmarket datasets, the letter notes.
The agency will also work with device manufacturers, investigators, and the LAAO Registry to try to identify the causes of procedural outcome differences between women and men.
In the letter, the FDA recommends health care providers continue monitoring patients who have been treated with LAAO devices in accordance with the current standard of care. They should also discuss the risks and benefits of all available options for stroke prevention in patients with atrial fibrillation as part of shared clinical decision-making.
Any adverse events or suspected adverse events experienced by patients with LAAO devices should also be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
The agency said it is evaluating a real-world study, published in JAMA Cardiology, of 49,357 patients in the National Cardiovascular Data Registry LAAO Registry that suggested women might be at greater risk than men for procedural outcomes, including major adverse events after device implant.
“The FDA recognizes the limitations of these data, including that the study was not randomized, only included one LAAO device (the first-generation Watchman device), and did not include longer-term outcomes beyond in-hospital events. However, the analysis provides results from a large registry of patients treated with LAAO implants in the U.S.,” the agency said in its letter to health care providers Sept. 27.
As reported last month, the study by Darden et al showed a significantly higher rate of adverse procedural events in women than in men, including any adverse events (6.3% vs. 3.9%; P < .001), any major adverse events (4.1% vs. 2.0%; P < .001), and hospital stay longer than 1 day (16.0% vs. 11.6%; P < .001). Procedure-associated death was 0.3% in women and 0.1% in men.
The agency noted that the number of patients in the LAAO Registry analysis was much larger than the number of patients in the premarket studies of the Watchman device that supported its approval and in the premarket studies for the other approved LAAO devices.
LAAO devices are indicated to reduce the risk for thromboembolism from the left atrial appendage in patients with nonvalvular atrial fibrillation who are not good candidates for long-term anticoagulation. LAAO devices currently marketed in the United States are Boston Scientific’s Watchman and Watchman FLX devices and Abbott Medical’s Amplatzer Amulet device.
“Currently, the FDA believes the benefits continue to outweigh the risks for approved LAAO devices when used in accordance with their instructions for use,” the letter states.
The FDA will work with device manufacturers to evaluate the potential issue, including a review of available premarket and postapproval study data and other available real-world, postmarket datasets, the letter notes.
The agency will also work with device manufacturers, investigators, and the LAAO Registry to try to identify the causes of procedural outcome differences between women and men.
In the letter, the FDA recommends health care providers continue monitoring patients who have been treated with LAAO devices in accordance with the current standard of care. They should also discuss the risks and benefits of all available options for stroke prevention in patients with atrial fibrillation as part of shared clinical decision-making.
Any adverse events or suspected adverse events experienced by patients with LAAO devices should also be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
Cardiogenic shock teams again tied to lower mortality
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
Cavernous gender gap in Medicare payments to cardiologists
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Feds slap UPMC, lead cardiothoracic surgeon with fraud lawsuit
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
Two swings, two misses with colchicine, Vascepa in COVID-19
The anti-inflammatory agents colchicine and icosapent ethyl (Vascepa; Amarin) failed to provide substantial benefits in separate randomized COVID-19 trials.
Both were reported at the European Society of Cardiology (ESC) Congress 2021.
The open-label ECLA PHRI COLCOVID trial randomized 1,277 hospitalized adults (mean age 62 years) to usual care alone or with colchicine at a loading dose of 1.5 mg for 2 hours followed by 0.5 mg on day 1 and then 0.5 mg twice daily for 14 days or until discharge.
The investigators hypothesized that colchicine, which is widely used to treat gout and other inflammatory conditions, might modulate the hyperinflammatory syndrome, or cytokine storm, associated with COVID-19.
Results showed that the need for mechanical ventilation or death occurred in 25.0% of patients receiving colchicine and 28.8% with usual care (P = .08).
The coprimary endpoint of death at 28 days was also not significantly different between groups (20.5% vs. 22.2%), principal investigator Rafael Diaz, MD, said in a late-breaking COVID-19 trials session at the congress.
Among the secondary outcomes at 28 days, colchicine significantly reduced the incidence of new intubation or death from respiratory failure from 27.0% to 22.3% (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99) but not mortality from respiratory failure (19.5% vs. 16.8%).
The only important adverse effect was severe diarrhea, which was reported in 11.3% of the colchicine group vs. 4.5% in the control group, said Dr. Diaz, director of Estudios Clínicos Latinoamérica (ECLA), Rosario, Argentina.
The results are consistent with those from the massive RECOVERY trial, which earlier this year stopped enrollment in the colchicine arm for lack of efficacy in patients hospitalized with COVID-19, and COLCORONA, which missed its primary endpoint using colchicine among nonhospitalized adults with COVID-19.
Session chair and COLCORONA principal investigator Jean-Claude Tardif, MD, pointed out that, as clinicians, it’s fairly uncommon to combine systemic steroids with colchicine, which was the case in 92% of patients in ECLA PHRI COLCOVID.
“I think it is an inherent limitation of testing colchicine on top of steroids,” said Dr. Tardif, of the Montreal Heart Institute.
Icosapent ethyl in PREPARE-IT
Dr. Diaz returned in the ESC session to present the results of the PREPARE-IT trial, which tested whether icosapent ethyl – at a loading dose of 8 grams (4 capsules) for the first 3 days and 4 g/d on days 4-60 – could reduce the risk for SARS-CoV-2 infection in 2,041 health care and other public workers in Argentina at high risk for infection (mean age 40.5 years).
Vascepa was approved by the Food and Drug Administration in 2012 for the reduction of elevated triglyceride levels, with an added indication in 2019 to reduce cardiovascular (CV) events in people with elevated triglycerides and established CV disease or diabetes with other CV risk factors.
The rationale for using the high-dose prescription eicosapentaenoic acid (EPA) preparation includes its anti-inflammatory and antithrombotic effects, and that unsaturated fatty acids, especially EPA, might inactivate the enveloped virus, he explained.
Among 1,712 participants followed for up to 60 days, however, the SARS-CoV-2 infection rate was 7.9% with icosapent ethyl vs. 7.1% with a mineral oil placebo (P = .58).
There were also no significant changes from baseline in the icosapent ethyl and placebo groups for the secondary outcomes of high-sensitivity C-reactive protein (0 vs. 0), triglycerides (median –2 mg/dL vs. 7 mg/dL), or Influenza Patient-Reported Outcome (FLU-PRO) questionnaire scores (median 0.01 vs. 0.03).
The use of a mineral oil placebo has been the subject of controversy in previous fish oil trials, but, Dr. Diaz noted, it did not have a significant proinflammatory effect or cause any excess adverse events.
Overall, adverse events were similar between the active and placebo groups, including atrial fibrillation (none), major bleeding (none), minor bleeding (7 events vs. 10 events), gastrointestinal symptoms (6.8% vs. 7.0%), and diarrhea (8.6% vs. 7.7%).
Although it missed the primary endpoint, Dr. Diaz said, “this is the first large, randomized blinded trial to demonstrate excellent safety and tolerability of an 8-gram-per-day loading dose of icosapent ethyl, opening up the potential for acute use in randomized trials of myocardial infarction, acute coronary syndromes, strokes, and revascularization.”
During a discussion of the results, Dr. Diaz said the Delta variant was not present at the time of the analysis and that the second half of the trial will report on whether icosapent ethyl can reduce the risk for hospitalization or death in participants diagnosed with COVID-19.
ECLA PHRI COLCOVID was supported by the Estudios Clínicos Latinoamérica Population Health Research Institute. PREPARE-IT was supported by Estudios Clínicos Latinoamérica with collaboration from Amarin. Dr. Diaz reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The anti-inflammatory agents colchicine and icosapent ethyl (Vascepa; Amarin) failed to provide substantial benefits in separate randomized COVID-19 trials.
Both were reported at the European Society of Cardiology (ESC) Congress 2021.
The open-label ECLA PHRI COLCOVID trial randomized 1,277 hospitalized adults (mean age 62 years) to usual care alone or with colchicine at a loading dose of 1.5 mg for 2 hours followed by 0.5 mg on day 1 and then 0.5 mg twice daily for 14 days or until discharge.
The investigators hypothesized that colchicine, which is widely used to treat gout and other inflammatory conditions, might modulate the hyperinflammatory syndrome, or cytokine storm, associated with COVID-19.
Results showed that the need for mechanical ventilation or death occurred in 25.0% of patients receiving colchicine and 28.8% with usual care (P = .08).
The coprimary endpoint of death at 28 days was also not significantly different between groups (20.5% vs. 22.2%), principal investigator Rafael Diaz, MD, said in a late-breaking COVID-19 trials session at the congress.
Among the secondary outcomes at 28 days, colchicine significantly reduced the incidence of new intubation or death from respiratory failure from 27.0% to 22.3% (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99) but not mortality from respiratory failure (19.5% vs. 16.8%).
The only important adverse effect was severe diarrhea, which was reported in 11.3% of the colchicine group vs. 4.5% in the control group, said Dr. Diaz, director of Estudios Clínicos Latinoamérica (ECLA), Rosario, Argentina.
The results are consistent with those from the massive RECOVERY trial, which earlier this year stopped enrollment in the colchicine arm for lack of efficacy in patients hospitalized with COVID-19, and COLCORONA, which missed its primary endpoint using colchicine among nonhospitalized adults with COVID-19.
Session chair and COLCORONA principal investigator Jean-Claude Tardif, MD, pointed out that, as clinicians, it’s fairly uncommon to combine systemic steroids with colchicine, which was the case in 92% of patients in ECLA PHRI COLCOVID.
“I think it is an inherent limitation of testing colchicine on top of steroids,” said Dr. Tardif, of the Montreal Heart Institute.
Icosapent ethyl in PREPARE-IT
Dr. Diaz returned in the ESC session to present the results of the PREPARE-IT trial, which tested whether icosapent ethyl – at a loading dose of 8 grams (4 capsules) for the first 3 days and 4 g/d on days 4-60 – could reduce the risk for SARS-CoV-2 infection in 2,041 health care and other public workers in Argentina at high risk for infection (mean age 40.5 years).
Vascepa was approved by the Food and Drug Administration in 2012 for the reduction of elevated triglyceride levels, with an added indication in 2019 to reduce cardiovascular (CV) events in people with elevated triglycerides and established CV disease or diabetes with other CV risk factors.
The rationale for using the high-dose prescription eicosapentaenoic acid (EPA) preparation includes its anti-inflammatory and antithrombotic effects, and that unsaturated fatty acids, especially EPA, might inactivate the enveloped virus, he explained.
Among 1,712 participants followed for up to 60 days, however, the SARS-CoV-2 infection rate was 7.9% with icosapent ethyl vs. 7.1% with a mineral oil placebo (P = .58).
There were also no significant changes from baseline in the icosapent ethyl and placebo groups for the secondary outcomes of high-sensitivity C-reactive protein (0 vs. 0), triglycerides (median –2 mg/dL vs. 7 mg/dL), or Influenza Patient-Reported Outcome (FLU-PRO) questionnaire scores (median 0.01 vs. 0.03).
The use of a mineral oil placebo has been the subject of controversy in previous fish oil trials, but, Dr. Diaz noted, it did not have a significant proinflammatory effect or cause any excess adverse events.
Overall, adverse events were similar between the active and placebo groups, including atrial fibrillation (none), major bleeding (none), minor bleeding (7 events vs. 10 events), gastrointestinal symptoms (6.8% vs. 7.0%), and diarrhea (8.6% vs. 7.7%).
Although it missed the primary endpoint, Dr. Diaz said, “this is the first large, randomized blinded trial to demonstrate excellent safety and tolerability of an 8-gram-per-day loading dose of icosapent ethyl, opening up the potential for acute use in randomized trials of myocardial infarction, acute coronary syndromes, strokes, and revascularization.”
During a discussion of the results, Dr. Diaz said the Delta variant was not present at the time of the analysis and that the second half of the trial will report on whether icosapent ethyl can reduce the risk for hospitalization or death in participants diagnosed with COVID-19.
ECLA PHRI COLCOVID was supported by the Estudios Clínicos Latinoamérica Population Health Research Institute. PREPARE-IT was supported by Estudios Clínicos Latinoamérica with collaboration from Amarin. Dr. Diaz reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The anti-inflammatory agents colchicine and icosapent ethyl (Vascepa; Amarin) failed to provide substantial benefits in separate randomized COVID-19 trials.
Both were reported at the European Society of Cardiology (ESC) Congress 2021.
The open-label ECLA PHRI COLCOVID trial randomized 1,277 hospitalized adults (mean age 62 years) to usual care alone or with colchicine at a loading dose of 1.5 mg for 2 hours followed by 0.5 mg on day 1 and then 0.5 mg twice daily for 14 days or until discharge.
The investigators hypothesized that colchicine, which is widely used to treat gout and other inflammatory conditions, might modulate the hyperinflammatory syndrome, or cytokine storm, associated with COVID-19.
Results showed that the need for mechanical ventilation or death occurred in 25.0% of patients receiving colchicine and 28.8% with usual care (P = .08).
The coprimary endpoint of death at 28 days was also not significantly different between groups (20.5% vs. 22.2%), principal investigator Rafael Diaz, MD, said in a late-breaking COVID-19 trials session at the congress.
Among the secondary outcomes at 28 days, colchicine significantly reduced the incidence of new intubation or death from respiratory failure from 27.0% to 22.3% (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99) but not mortality from respiratory failure (19.5% vs. 16.8%).
The only important adverse effect was severe diarrhea, which was reported in 11.3% of the colchicine group vs. 4.5% in the control group, said Dr. Diaz, director of Estudios Clínicos Latinoamérica (ECLA), Rosario, Argentina.
The results are consistent with those from the massive RECOVERY trial, which earlier this year stopped enrollment in the colchicine arm for lack of efficacy in patients hospitalized with COVID-19, and COLCORONA, which missed its primary endpoint using colchicine among nonhospitalized adults with COVID-19.
Session chair and COLCORONA principal investigator Jean-Claude Tardif, MD, pointed out that, as clinicians, it’s fairly uncommon to combine systemic steroids with colchicine, which was the case in 92% of patients in ECLA PHRI COLCOVID.
“I think it is an inherent limitation of testing colchicine on top of steroids,” said Dr. Tardif, of the Montreal Heart Institute.
Icosapent ethyl in PREPARE-IT
Dr. Diaz returned in the ESC session to present the results of the PREPARE-IT trial, which tested whether icosapent ethyl – at a loading dose of 8 grams (4 capsules) for the first 3 days and 4 g/d on days 4-60 – could reduce the risk for SARS-CoV-2 infection in 2,041 health care and other public workers in Argentina at high risk for infection (mean age 40.5 years).
Vascepa was approved by the Food and Drug Administration in 2012 for the reduction of elevated triglyceride levels, with an added indication in 2019 to reduce cardiovascular (CV) events in people with elevated triglycerides and established CV disease or diabetes with other CV risk factors.
The rationale for using the high-dose prescription eicosapentaenoic acid (EPA) preparation includes its anti-inflammatory and antithrombotic effects, and that unsaturated fatty acids, especially EPA, might inactivate the enveloped virus, he explained.
Among 1,712 participants followed for up to 60 days, however, the SARS-CoV-2 infection rate was 7.9% with icosapent ethyl vs. 7.1% with a mineral oil placebo (P = .58).
There were also no significant changes from baseline in the icosapent ethyl and placebo groups for the secondary outcomes of high-sensitivity C-reactive protein (0 vs. 0), triglycerides (median –2 mg/dL vs. 7 mg/dL), or Influenza Patient-Reported Outcome (FLU-PRO) questionnaire scores (median 0.01 vs. 0.03).
The use of a mineral oil placebo has been the subject of controversy in previous fish oil trials, but, Dr. Diaz noted, it did not have a significant proinflammatory effect or cause any excess adverse events.
Overall, adverse events were similar between the active and placebo groups, including atrial fibrillation (none), major bleeding (none), minor bleeding (7 events vs. 10 events), gastrointestinal symptoms (6.8% vs. 7.0%), and diarrhea (8.6% vs. 7.7%).
Although it missed the primary endpoint, Dr. Diaz said, “this is the first large, randomized blinded trial to demonstrate excellent safety and tolerability of an 8-gram-per-day loading dose of icosapent ethyl, opening up the potential for acute use in randomized trials of myocardial infarction, acute coronary syndromes, strokes, and revascularization.”
During a discussion of the results, Dr. Diaz said the Delta variant was not present at the time of the analysis and that the second half of the trial will report on whether icosapent ethyl can reduce the risk for hospitalization or death in participants diagnosed with COVID-19.
ECLA PHRI COLCOVID was supported by the Estudios Clínicos Latinoamérica Population Health Research Institute. PREPARE-IT was supported by Estudios Clínicos Latinoamérica with collaboration from Amarin. Dr. Diaz reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dapagliflozin in HFrEF may cut arrhythmias, sudden death: DAPA-HF
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).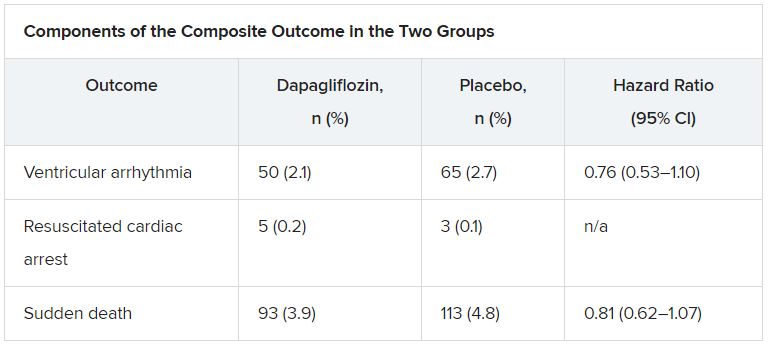
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).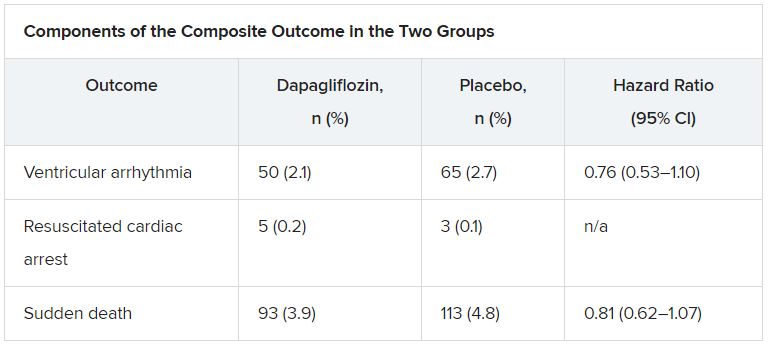
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).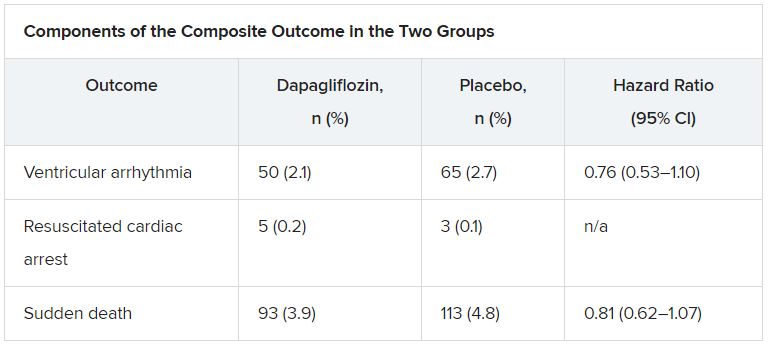
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2021
Colchicine effective regardless of ACS history, timing: LoDoCo2
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
Chronic kidney disease tied to worse LAAO outcomes
The presence of chronic kidney disease (CKD) or end-stage renal disease (ESRD) is associated with worse in-hospital and short-term outcomes after left atrial appendage (LAA) closure, a nationwide study shows.
Patients with ESRD were particularly vulnerable, having about 6.5-fold higher odds of in-hospital mortality than those without CKD and about 11.5-fold higher odds than those with CKD, even after adjustment for potential confounders.
Patients with CKD had higher rates of stroke or transient ischemic attack (TIA) and more short-term readmissions for bleeding, Keerat Rai Ahuja, MD, Reading Hospital-Tower Health, West Reading, Pennsylvania, and colleagues reported August 16 in JACC: Cardiovascular Interventions.
CKD and ESRD are known to be associated with an increased risk for stroke and bleeding in patients with atrial fibrillation (AFib), yet data are limited on the safety and efficacy of LAA closure for stroke prevention in AFib patients with CKD or ESRD, they note.
“It’s important to know about CKD and understand that there may be an association with worse levels of CKD and worse outcomes, but the data that strikes me is really that for end-stage renal disease,” Matthew Sherwood, MD, MHS, who was not involved with the study, said in an interview.
He noted that data have not been published for patients with CKD and ESRD enrolled in the pivotal PROTECT-AF and PREVAIL trials of Boston Scientific’s Watchman device or from large clinical registries such as EWOLUTION and the company’s continued access protocol registries.
Further, it’s not well understood what the best strategy is to prevent stroke in AFib patients with ESRD and whether they benefit from anticoagulation with warfarin or any of the newer agents. “Thus, it’s hard to then say: ‘Well they have worse outcomes with Watchman,’ which is true as shown in this study, but they may not have any other options based upon the lack of data for oral anticoagulants in end-stage kidney disease patients,” said Dr. Sherwood, from the Inova Heart and Vascular Institute, Falls Church, Virginia.
The lack of clarity is concerning, given rising atrial fibrillation cases and the prevalence of abnormal renal function in everyday practice. In the present study – involving 21,274 patients undergoing LAA closure between 2016 and 2017 in the Nationwide Readmissions Database – 18.6% of patients had CKD stages I to V and 2.7% had ESRD based on ICD-10 codes.
In-hospital mortality was increased only in patients with ESRD. In all, 3.3% of patients with ESRD and 0.4% of those with no CKD died in hospital (adjusted odds ratio [aOR], 6.48), as did 0.5% of patients with CKD (aOR, 11.43; both P <.001).
“These patients represent a sicker population at baseline and have an inherent greater risk for mortality in cardiac interventions, as noted in other studies of structural heart interventions,” Dr. Ahuja and colleagues write.
Patients with CKD had a higher risk for in-hospital stroke or TIA than patients with no CKD (1.8% vs. 1.3%; aOR, 1.35; P = .038) and this risk continued up to 90 days after discharge (1.7% vs. 1.0%; aOR, 1.67; P = .007).
The in-hospital stroke rate was numerically higher in patients with ESRD compared with no CKD (aOR, 1.18; P = .62).
The authors point out that previous LAA closure and CKD studies have reported no differences in in-hospital or subsequent stroke/TIA rates in patients with and without CKD. Possible explanations are that patients with CKD in the present study had higher CHA2DS2-VASc scores than those without CKD (4.18 vs. 3.62) and, second, patients with CKD and AFib are known to have higher risk for thromboembolic events than those with AFib without CKD.
CKD patients were also more likely than those without CKD to experience in-hospital acute kidney injury or hemodialysis (aOR, 5.02; P <.001).
CKD has been shown to be independently associated with acute kidney injury (AKI) after LAA closure. AKI may have long-term thromboembolic consequences, the authors suggest, with one study reporting higher stroke risk at midterm follow-up in patients with AKI.
“As with other cardiac interventions in patients with CKD, efforts should be made to optimize preoperative renal function, minimize contrast volume, and avoid abrupt hemodynamic changes such as hypotension during the procedure to prevent AKI,” Dr. Ahuja and colleagues write.
Patients with CKD and ESRD had longer index length of stay than those without CKD but had similar rates of other in-hospital complications, such as systemic embolization, bleeding/transfusion, vascular complications, and pericardial tamponade requiring intervention.
Among the short-term outcomes, 30- and 90-day all-cause readmissions were increased in patients with CKD and ESRD compared with those without CKD, and 30-day bleeding readmissions were increased within the CKD cohort.
“With Watchman and left atrial appendage closure, what we see is that they have higher rates of readmission and other problems,” Dr. Sherwood said. “I think we understand that that’s probably related not to the procedure itself, not because the Watchman doesn’t work for end-stage kidney disease, but because the patients themselves are likely higher risk.”
Commonly used risk scores for atrial fibrillation, however, don’t take into account advanced kidney disease, he added.
Besides the inherent limitations of observational studies, Dr. Sherwood and the authors point to the lack of laboratory variables and procedural variables in the database, the fact that CKD was defined using ICD-10 codes, that outcomes were not clinically adjudicated, that unmeasured confounders likely still exist, and that long-term follow-up is lacking.
Dr. Sherwood, who wrote an editorial accompanying the study, said that the release of outcomes data from CKD and ESRD patients in the major clinical trials would be helpful going forward, as would possible involvement with the Kidney Disease Improving Global Outcomes organization.
“One of the main points of this study is that we just need a lot more research diving into this patient population,” he said.
The authors report no relevant financial relationships. Dr. Sherwood reports honoraria from Janssen and Medtronic. Editorial coauthor Sean Pokorney reports research grant support from Gilead, Boston Scientific, Pfizer, Bristol Myers Squibb, Janssen, and the Food and Drug Administration; and advisory board, consulting, and honoraria supports from Medtronic, Boston Scientific, Pfizer, Bristol Myers Squibb, Philips, and Zoll.
A version of this article first appeared on Medscape.com.
The presence of chronic kidney disease (CKD) or end-stage renal disease (ESRD) is associated with worse in-hospital and short-term outcomes after left atrial appendage (LAA) closure, a nationwide study shows.
Patients with ESRD were particularly vulnerable, having about 6.5-fold higher odds of in-hospital mortality than those without CKD and about 11.5-fold higher odds than those with CKD, even after adjustment for potential confounders.
Patients with CKD had higher rates of stroke or transient ischemic attack (TIA) and more short-term readmissions for bleeding, Keerat Rai Ahuja, MD, Reading Hospital-Tower Health, West Reading, Pennsylvania, and colleagues reported August 16 in JACC: Cardiovascular Interventions.
CKD and ESRD are known to be associated with an increased risk for stroke and bleeding in patients with atrial fibrillation (AFib), yet data are limited on the safety and efficacy of LAA closure for stroke prevention in AFib patients with CKD or ESRD, they note.
“It’s important to know about CKD and understand that there may be an association with worse levels of CKD and worse outcomes, but the data that strikes me is really that for end-stage renal disease,” Matthew Sherwood, MD, MHS, who was not involved with the study, said in an interview.
He noted that data have not been published for patients with CKD and ESRD enrolled in the pivotal PROTECT-AF and PREVAIL trials of Boston Scientific’s Watchman device or from large clinical registries such as EWOLUTION and the company’s continued access protocol registries.
Further, it’s not well understood what the best strategy is to prevent stroke in AFib patients with ESRD and whether they benefit from anticoagulation with warfarin or any of the newer agents. “Thus, it’s hard to then say: ‘Well they have worse outcomes with Watchman,’ which is true as shown in this study, but they may not have any other options based upon the lack of data for oral anticoagulants in end-stage kidney disease patients,” said Dr. Sherwood, from the Inova Heart and Vascular Institute, Falls Church, Virginia.
The lack of clarity is concerning, given rising atrial fibrillation cases and the prevalence of abnormal renal function in everyday practice. In the present study – involving 21,274 patients undergoing LAA closure between 2016 and 2017 in the Nationwide Readmissions Database – 18.6% of patients had CKD stages I to V and 2.7% had ESRD based on ICD-10 codes.
In-hospital mortality was increased only in patients with ESRD. In all, 3.3% of patients with ESRD and 0.4% of those with no CKD died in hospital (adjusted odds ratio [aOR], 6.48), as did 0.5% of patients with CKD (aOR, 11.43; both P <.001).
“These patients represent a sicker population at baseline and have an inherent greater risk for mortality in cardiac interventions, as noted in other studies of structural heart interventions,” Dr. Ahuja and colleagues write.
Patients with CKD had a higher risk for in-hospital stroke or TIA than patients with no CKD (1.8% vs. 1.3%; aOR, 1.35; P = .038) and this risk continued up to 90 days after discharge (1.7% vs. 1.0%; aOR, 1.67; P = .007).
The in-hospital stroke rate was numerically higher in patients with ESRD compared with no CKD (aOR, 1.18; P = .62).
The authors point out that previous LAA closure and CKD studies have reported no differences in in-hospital or subsequent stroke/TIA rates in patients with and without CKD. Possible explanations are that patients with CKD in the present study had higher CHA2DS2-VASc scores than those without CKD (4.18 vs. 3.62) and, second, patients with CKD and AFib are known to have higher risk for thromboembolic events than those with AFib without CKD.
CKD patients were also more likely than those without CKD to experience in-hospital acute kidney injury or hemodialysis (aOR, 5.02; P <.001).
CKD has been shown to be independently associated with acute kidney injury (AKI) after LAA closure. AKI may have long-term thromboembolic consequences, the authors suggest, with one study reporting higher stroke risk at midterm follow-up in patients with AKI.
“As with other cardiac interventions in patients with CKD, efforts should be made to optimize preoperative renal function, minimize contrast volume, and avoid abrupt hemodynamic changes such as hypotension during the procedure to prevent AKI,” Dr. Ahuja and colleagues write.
Patients with CKD and ESRD had longer index length of stay than those without CKD but had similar rates of other in-hospital complications, such as systemic embolization, bleeding/transfusion, vascular complications, and pericardial tamponade requiring intervention.
Among the short-term outcomes, 30- and 90-day all-cause readmissions were increased in patients with CKD and ESRD compared with those without CKD, and 30-day bleeding readmissions were increased within the CKD cohort.
“With Watchman and left atrial appendage closure, what we see is that they have higher rates of readmission and other problems,” Dr. Sherwood said. “I think we understand that that’s probably related not to the procedure itself, not because the Watchman doesn’t work for end-stage kidney disease, but because the patients themselves are likely higher risk.”
Commonly used risk scores for atrial fibrillation, however, don’t take into account advanced kidney disease, he added.
Besides the inherent limitations of observational studies, Dr. Sherwood and the authors point to the lack of laboratory variables and procedural variables in the database, the fact that CKD was defined using ICD-10 codes, that outcomes were not clinically adjudicated, that unmeasured confounders likely still exist, and that long-term follow-up is lacking.
Dr. Sherwood, who wrote an editorial accompanying the study, said that the release of outcomes data from CKD and ESRD patients in the major clinical trials would be helpful going forward, as would possible involvement with the Kidney Disease Improving Global Outcomes organization.
“One of the main points of this study is that we just need a lot more research diving into this patient population,” he said.
The authors report no relevant financial relationships. Dr. Sherwood reports honoraria from Janssen and Medtronic. Editorial coauthor Sean Pokorney reports research grant support from Gilead, Boston Scientific, Pfizer, Bristol Myers Squibb, Janssen, and the Food and Drug Administration; and advisory board, consulting, and honoraria supports from Medtronic, Boston Scientific, Pfizer, Bristol Myers Squibb, Philips, and Zoll.
A version of this article first appeared on Medscape.com.
The presence of chronic kidney disease (CKD) or end-stage renal disease (ESRD) is associated with worse in-hospital and short-term outcomes after left atrial appendage (LAA) closure, a nationwide study shows.
Patients with ESRD were particularly vulnerable, having about 6.5-fold higher odds of in-hospital mortality than those without CKD and about 11.5-fold higher odds than those with CKD, even after adjustment for potential confounders.
Patients with CKD had higher rates of stroke or transient ischemic attack (TIA) and more short-term readmissions for bleeding, Keerat Rai Ahuja, MD, Reading Hospital-Tower Health, West Reading, Pennsylvania, and colleagues reported August 16 in JACC: Cardiovascular Interventions.
CKD and ESRD are known to be associated with an increased risk for stroke and bleeding in patients with atrial fibrillation (AFib), yet data are limited on the safety and efficacy of LAA closure for stroke prevention in AFib patients with CKD or ESRD, they note.
“It’s important to know about CKD and understand that there may be an association with worse levels of CKD and worse outcomes, but the data that strikes me is really that for end-stage renal disease,” Matthew Sherwood, MD, MHS, who was not involved with the study, said in an interview.
He noted that data have not been published for patients with CKD and ESRD enrolled in the pivotal PROTECT-AF and PREVAIL trials of Boston Scientific’s Watchman device or from large clinical registries such as EWOLUTION and the company’s continued access protocol registries.
Further, it’s not well understood what the best strategy is to prevent stroke in AFib patients with ESRD and whether they benefit from anticoagulation with warfarin or any of the newer agents. “Thus, it’s hard to then say: ‘Well they have worse outcomes with Watchman,’ which is true as shown in this study, but they may not have any other options based upon the lack of data for oral anticoagulants in end-stage kidney disease patients,” said Dr. Sherwood, from the Inova Heart and Vascular Institute, Falls Church, Virginia.
The lack of clarity is concerning, given rising atrial fibrillation cases and the prevalence of abnormal renal function in everyday practice. In the present study – involving 21,274 patients undergoing LAA closure between 2016 and 2017 in the Nationwide Readmissions Database – 18.6% of patients had CKD stages I to V and 2.7% had ESRD based on ICD-10 codes.
In-hospital mortality was increased only in patients with ESRD. In all, 3.3% of patients with ESRD and 0.4% of those with no CKD died in hospital (adjusted odds ratio [aOR], 6.48), as did 0.5% of patients with CKD (aOR, 11.43; both P <.001).
“These patients represent a sicker population at baseline and have an inherent greater risk for mortality in cardiac interventions, as noted in other studies of structural heart interventions,” Dr. Ahuja and colleagues write.
Patients with CKD had a higher risk for in-hospital stroke or TIA than patients with no CKD (1.8% vs. 1.3%; aOR, 1.35; P = .038) and this risk continued up to 90 days after discharge (1.7% vs. 1.0%; aOR, 1.67; P = .007).
The in-hospital stroke rate was numerically higher in patients with ESRD compared with no CKD (aOR, 1.18; P = .62).
The authors point out that previous LAA closure and CKD studies have reported no differences in in-hospital or subsequent stroke/TIA rates in patients with and without CKD. Possible explanations are that patients with CKD in the present study had higher CHA2DS2-VASc scores than those without CKD (4.18 vs. 3.62) and, second, patients with CKD and AFib are known to have higher risk for thromboembolic events than those with AFib without CKD.
CKD patients were also more likely than those without CKD to experience in-hospital acute kidney injury or hemodialysis (aOR, 5.02; P <.001).
CKD has been shown to be independently associated with acute kidney injury (AKI) after LAA closure. AKI may have long-term thromboembolic consequences, the authors suggest, with one study reporting higher stroke risk at midterm follow-up in patients with AKI.
“As with other cardiac interventions in patients with CKD, efforts should be made to optimize preoperative renal function, minimize contrast volume, and avoid abrupt hemodynamic changes such as hypotension during the procedure to prevent AKI,” Dr. Ahuja and colleagues write.
Patients with CKD and ESRD had longer index length of stay than those without CKD but had similar rates of other in-hospital complications, such as systemic embolization, bleeding/transfusion, vascular complications, and pericardial tamponade requiring intervention.
Among the short-term outcomes, 30- and 90-day all-cause readmissions were increased in patients with CKD and ESRD compared with those without CKD, and 30-day bleeding readmissions were increased within the CKD cohort.
“With Watchman and left atrial appendage closure, what we see is that they have higher rates of readmission and other problems,” Dr. Sherwood said. “I think we understand that that’s probably related not to the procedure itself, not because the Watchman doesn’t work for end-stage kidney disease, but because the patients themselves are likely higher risk.”
Commonly used risk scores for atrial fibrillation, however, don’t take into account advanced kidney disease, he added.
Besides the inherent limitations of observational studies, Dr. Sherwood and the authors point to the lack of laboratory variables and procedural variables in the database, the fact that CKD was defined using ICD-10 codes, that outcomes were not clinically adjudicated, that unmeasured confounders likely still exist, and that long-term follow-up is lacking.
Dr. Sherwood, who wrote an editorial accompanying the study, said that the release of outcomes data from CKD and ESRD patients in the major clinical trials would be helpful going forward, as would possible involvement with the Kidney Disease Improving Global Outcomes organization.
“One of the main points of this study is that we just need a lot more research diving into this patient population,” he said.
The authors report no relevant financial relationships. Dr. Sherwood reports honoraria from Janssen and Medtronic. Editorial coauthor Sean Pokorney reports research grant support from Gilead, Boston Scientific, Pfizer, Bristol Myers Squibb, Janssen, and the Food and Drug Administration; and advisory board, consulting, and honoraria supports from Medtronic, Boston Scientific, Pfizer, Bristol Myers Squibb, Philips, and Zoll.
A version of this article first appeared on Medscape.com.
Connecticut chapter of ACC at center of Twitter dustup
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
FDA approves Abbott’s Amplatzer Amulet for AFib
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.



