User login
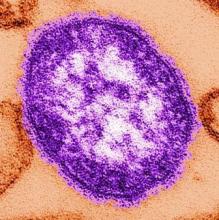
Lessons from largest measles outbreak in 20 years
The largest measles outbreak in the United States in more than 2 decades, with an attack rate several orders of magnitude larger than the usual annual nationwide incidence of the disease, could have been better controlled if clinicians had recognized the index cases sooner, according to a report published online Oct. 6 in the New England Journal of Medicine.
At 4 months’ duration, the 2014 measles outbreak in undervaccinated Amish communities across Ohio was also the longest-lasting one on record since the disease was eliminated in the United States, said Paul A. Gastañaduy, MD, of the division of viral diseases, Centers for Disease Control and Prevention, and his associates.
Two index cases developed in young Amish men (aged 22 and 23 years) who had just returned from a church-sponsored trip to the Philippines to perform charitable work among victims of a typhoon. They had not received any guidance about contagious diseases before their trip. Both developed prodromal symptoms (cough, coryza, or conjunctivitis) the day after their return, then a generalized red maculopapular rash 2 days later. They were then admitted to a local hospital and found to have thrombocytopenia and were diagnosed as having dengue fever. Only after a febrile illness with rash developed in 2 more returning relief workers, then in 12 additional contacts within the Amish community, was measles recognized and reported to the health department a full 30 days later. “Health care providers should maintain a high awareness of measles when returning unvaccinated travelers present with a fever and rash,” Dr. Gastañaduy and his associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1602295).
A total of 383 people developed measles in this outbreak; 380 were Amish, and the other 3 were epidemiologically linked to the Amish community. The Amish sect doesn’t specifically prohibit vaccination, but immunization rates are low because the people’s personal and cultural beliefs limit participation in preventive health care. The fact that this outbreak was confined almost exclusively to the Amish indicates that high vaccine coverage in the general Ohio population probably prevented further spread of measles, the investigators noted. A total of 52% of the cases occurred among children and adolescents aged 5-17 years and 25% among persons aged 18-39 years.
After the outbreak was recognized, “engagement of local leaders, isolation of infectious persons, quarantine of those exposed, and vaccination of susceptible persons” allowed it to be contained. Local health departments implemented enhanced surveillance and met with community leaders to encourage case reporting, emphasize the importance of vaccination, inform residents about testing, and alert health care providers statewide about the outbreak. A total of 120 free vaccination clinics were held and 10,644 people were immunized.
This study was supported by the Ohio Department of Health and the CDC. Dr. Gastañaduy and his associates reported having no relevant financial disclosures.
The largest measles outbreak in the United States in more than 2 decades, with an attack rate several orders of magnitude larger than the usual annual nationwide incidence of the disease, could have been better controlled if clinicians had recognized the index cases sooner, according to a report published online Oct. 6 in the New England Journal of Medicine.
At 4 months’ duration, the 2014 measles outbreak in undervaccinated Amish communities across Ohio was also the longest-lasting one on record since the disease was eliminated in the United States, said Paul A. Gastañaduy, MD, of the division of viral diseases, Centers for Disease Control and Prevention, and his associates.
Two index cases developed in young Amish men (aged 22 and 23 years) who had just returned from a church-sponsored trip to the Philippines to perform charitable work among victims of a typhoon. They had not received any guidance about contagious diseases before their trip. Both developed prodromal symptoms (cough, coryza, or conjunctivitis) the day after their return, then a generalized red maculopapular rash 2 days later. They were then admitted to a local hospital and found to have thrombocytopenia and were diagnosed as having dengue fever. Only after a febrile illness with rash developed in 2 more returning relief workers, then in 12 additional contacts within the Amish community, was measles recognized and reported to the health department a full 30 days later. “Health care providers should maintain a high awareness of measles when returning unvaccinated travelers present with a fever and rash,” Dr. Gastañaduy and his associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1602295).
A total of 383 people developed measles in this outbreak; 380 were Amish, and the other 3 were epidemiologically linked to the Amish community. The Amish sect doesn’t specifically prohibit vaccination, but immunization rates are low because the people’s personal and cultural beliefs limit participation in preventive health care. The fact that this outbreak was confined almost exclusively to the Amish indicates that high vaccine coverage in the general Ohio population probably prevented further spread of measles, the investigators noted. A total of 52% of the cases occurred among children and adolescents aged 5-17 years and 25% among persons aged 18-39 years.
After the outbreak was recognized, “engagement of local leaders, isolation of infectious persons, quarantine of those exposed, and vaccination of susceptible persons” allowed it to be contained. Local health departments implemented enhanced surveillance and met with community leaders to encourage case reporting, emphasize the importance of vaccination, inform residents about testing, and alert health care providers statewide about the outbreak. A total of 120 free vaccination clinics were held and 10,644 people were immunized.
This study was supported by the Ohio Department of Health and the CDC. Dr. Gastañaduy and his associates reported having no relevant financial disclosures.
The largest measles outbreak in the United States in more than 2 decades, with an attack rate several orders of magnitude larger than the usual annual nationwide incidence of the disease, could have been better controlled if clinicians had recognized the index cases sooner, according to a report published online Oct. 6 in the New England Journal of Medicine.
At 4 months’ duration, the 2014 measles outbreak in undervaccinated Amish communities across Ohio was also the longest-lasting one on record since the disease was eliminated in the United States, said Paul A. Gastañaduy, MD, of the division of viral diseases, Centers for Disease Control and Prevention, and his associates.
Two index cases developed in young Amish men (aged 22 and 23 years) who had just returned from a church-sponsored trip to the Philippines to perform charitable work among victims of a typhoon. They had not received any guidance about contagious diseases before their trip. Both developed prodromal symptoms (cough, coryza, or conjunctivitis) the day after their return, then a generalized red maculopapular rash 2 days later. They were then admitted to a local hospital and found to have thrombocytopenia and were diagnosed as having dengue fever. Only after a febrile illness with rash developed in 2 more returning relief workers, then in 12 additional contacts within the Amish community, was measles recognized and reported to the health department a full 30 days later. “Health care providers should maintain a high awareness of measles when returning unvaccinated travelers present with a fever and rash,” Dr. Gastañaduy and his associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1602295).
A total of 383 people developed measles in this outbreak; 380 were Amish, and the other 3 were epidemiologically linked to the Amish community. The Amish sect doesn’t specifically prohibit vaccination, but immunization rates are low because the people’s personal and cultural beliefs limit participation in preventive health care. The fact that this outbreak was confined almost exclusively to the Amish indicates that high vaccine coverage in the general Ohio population probably prevented further spread of measles, the investigators noted. A total of 52% of the cases occurred among children and adolescents aged 5-17 years and 25% among persons aged 18-39 years.
After the outbreak was recognized, “engagement of local leaders, isolation of infectious persons, quarantine of those exposed, and vaccination of susceptible persons” allowed it to be contained. Local health departments implemented enhanced surveillance and met with community leaders to encourage case reporting, emphasize the importance of vaccination, inform residents about testing, and alert health care providers statewide about the outbreak. A total of 120 free vaccination clinics were held and 10,644 people were immunized.
This study was supported by the Ohio Department of Health and the CDC. Dr. Gastañaduy and his associates reported having no relevant financial disclosures.
Key clinical point: The largest measles outbreak in the U.S. in more than 2 decades could have been better controlled if clinicians had recognized the index cases earlier.
Major finding: Only after a febrile illness with rash developed in 2 more returning relief workers, then in 12 additional contacts within the Amish community, was measles recognized and reported to the health department – a full 30 days after the 2 index patients presented.
Data source: A descriptive analysis of the epidemiologic features of a measles outbreak affecting 383 patients in nine counties in Ohio.
Disclosures: This study was supported by the Ohio Department of Health and the CDC. Dr. Gastañaduy and his associates reported having no relevant financial disclosures.
High-performing hospitals yield longer life expectancy after MI
Patients treated for acute MI at high-performing hospitals – those with the best performance on 30-day mortality quality measures assessed by the Centers for Medicare & Medicaid Services – had longer life expectancies than did patients treated at low-performing hospitals, according to a report published online Oct. 6 in the New England Journal of Medicine.
This survival benefit persisted through 17 years of follow-up, said Emily Bucholz, MD, of Boston Children’s Hospital, and her associates.
Until now, researchers didn’t know whether the short-term survival benefit at high-performing hospitals would wane over time, which “would lend support to the theory that these hospitals discharge more patients alive but with higher subsequent mortality.” The results of this secondary analysis of data from a nationally representative cohort study indicate that, instead, the superior quality of care delivered at high-performing hospitals appears to “produce an early benefit that endures over time,” Dr. Bucholz and her associates noted. The investigators assessed long-term life expectancy using data from the Cooperative Cardiovascular Project, which enrolled Medicare beneficiaries aged 65 years and older treated for acute MI in 1994-1996. They focused on 119,735 patients admitted to 1,824 hospitals. They grouped the hospitals according to their case mixes (a measure of patients’ severity of illness) and calculated risk-standardized mortality rates according to CMS criteria.
“We found that patients treated at high-performing hospitals ... lived, on average, between 0.74 and 1.14 years longer after acute MI than [did] those treated at low-performing hospitals. These findings were consistent across case-mix strata, which indicates that the relationship between hospital performance and long-term patient outcomes is independent of hospital case mix,” Dr. Bucholz and her associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1513223).
These findings show that the early survival advantage achieved by high-performing hospitals is durable, and that “investing in initiatives to improve short-term hospital performance may also improve patient outcomes over the long term,” they added.
Patients treated for acute MI at high-performing hospitals – those with the best performance on 30-day mortality quality measures assessed by the Centers for Medicare & Medicaid Services – had longer life expectancies than did patients treated at low-performing hospitals, according to a report published online Oct. 6 in the New England Journal of Medicine.
This survival benefit persisted through 17 years of follow-up, said Emily Bucholz, MD, of Boston Children’s Hospital, and her associates.
Until now, researchers didn’t know whether the short-term survival benefit at high-performing hospitals would wane over time, which “would lend support to the theory that these hospitals discharge more patients alive but with higher subsequent mortality.” The results of this secondary analysis of data from a nationally representative cohort study indicate that, instead, the superior quality of care delivered at high-performing hospitals appears to “produce an early benefit that endures over time,” Dr. Bucholz and her associates noted. The investigators assessed long-term life expectancy using data from the Cooperative Cardiovascular Project, which enrolled Medicare beneficiaries aged 65 years and older treated for acute MI in 1994-1996. They focused on 119,735 patients admitted to 1,824 hospitals. They grouped the hospitals according to their case mixes (a measure of patients’ severity of illness) and calculated risk-standardized mortality rates according to CMS criteria.
“We found that patients treated at high-performing hospitals ... lived, on average, between 0.74 and 1.14 years longer after acute MI than [did] those treated at low-performing hospitals. These findings were consistent across case-mix strata, which indicates that the relationship between hospital performance and long-term patient outcomes is independent of hospital case mix,” Dr. Bucholz and her associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1513223).
These findings show that the early survival advantage achieved by high-performing hospitals is durable, and that “investing in initiatives to improve short-term hospital performance may also improve patient outcomes over the long term,” they added.
Patients treated for acute MI at high-performing hospitals – those with the best performance on 30-day mortality quality measures assessed by the Centers for Medicare & Medicaid Services – had longer life expectancies than did patients treated at low-performing hospitals, according to a report published online Oct. 6 in the New England Journal of Medicine.
This survival benefit persisted through 17 years of follow-up, said Emily Bucholz, MD, of Boston Children’s Hospital, and her associates.
Until now, researchers didn’t know whether the short-term survival benefit at high-performing hospitals would wane over time, which “would lend support to the theory that these hospitals discharge more patients alive but with higher subsequent mortality.” The results of this secondary analysis of data from a nationally representative cohort study indicate that, instead, the superior quality of care delivered at high-performing hospitals appears to “produce an early benefit that endures over time,” Dr. Bucholz and her associates noted. The investigators assessed long-term life expectancy using data from the Cooperative Cardiovascular Project, which enrolled Medicare beneficiaries aged 65 years and older treated for acute MI in 1994-1996. They focused on 119,735 patients admitted to 1,824 hospitals. They grouped the hospitals according to their case mixes (a measure of patients’ severity of illness) and calculated risk-standardized mortality rates according to CMS criteria.
“We found that patients treated at high-performing hospitals ... lived, on average, between 0.74 and 1.14 years longer after acute MI than [did] those treated at low-performing hospitals. These findings were consistent across case-mix strata, which indicates that the relationship between hospital performance and long-term patient outcomes is independent of hospital case mix,” Dr. Bucholz and her associates said (N Engl J Med. 2016 Oct 6. doi: 10.1056/NEJMoa1513223).
These findings show that the early survival advantage achieved by high-performing hospitals is durable, and that “investing in initiatives to improve short-term hospital performance may also improve patient outcomes over the long term,” they added.
Key clinical point: Patients treated for MI at high-performing hospitals have longer life expectancies than those treated at low-performing hospitals.
Major finding: Patients treated at high-performing hospitals lived, on average, 0.74-1.14 years longer after acute MI than those treated at low-performing hospitals.
Data source: A secondary analysis of data in a nationally representative cohort study involving 119,735 MI patients treated at 1,824 hospitals and followed for 17 years.
Disclosures: This study was supported by the National Heart, Lung, and Blood Institute and the National Institute of General Medical Sciences. Dr. Bucholz reported having no relevant financial disclosures; one of her associates reported ties to Medtronic, Johnson & Johnson, and UnitedHealth.
Rivaroxaban linked to more bleeding compared with dabigatran in elderly patients with nonvalvular AF
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Key clinical point: Rivaroxaban is associated with significantly more intra- and extracranial bleeding than dabigatran in patients aged 75 and older with nonvalvular atrial fibrillation.
Major finding: Rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment.
Data source: A retrospective cohort study of 118,891 patients aged 65 and older who initiated anticoagulation therapy for AF during a 2.5-year period.
Disclosures: This study was conducted by employees or contractors of the Centers for Medicare & Medicaid Services and the Food and Drug Administration. Dr. Graham and his associates reported having no relevant financial disclosures.
Cerebral protection in TAVI reduces ischemic brain lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Key clinical point: In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions.
Major finding: At 2 days, the number of new brain lesions was markedly lower in the filter group than in the control group (8 vs. 16), as was the lesion volume (466 mm vs. 800 mm).
Data source: A prospective single-center randomized clinical trial involving 100 patients undergoing TAVI for severe aortic stenosis.
Disclosures: This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Meta-analysis links NPC1L1 variants to diabetes risk
Naturally occurring variations on or near the NPC1L1 gene, which is linked to lower LDL-cholesterol levels, were associated with a higher risk of type 2 diabetes in a meta-analysis reported online Oct. 4 in JAMA.
Some cholesterol-lowering medications, notably ezetimibe, work by inhibiting the action of the NPC1L1 gene. The findings of this meta-analysis suggest that by doing so, these cholesterol-lowering agents may raise the risk of type 2 diabetes, said Luca A. Lotta, MD, PhD, of the Medical Research Council Epidemiology Unit, University of Cambridge (U.K.), and his associates. The investigators examined gene-association analyses in several studies and databases covering 50,775 adults with type 2 diabetes and 270,269 control subjects in Europe and the United States during 1991-2016. They found that alleles at the NPC1L1 locus that are known to be associated with lower LDL-cholesterol levels also were strongly associated with higher rates of diabetes. For every genetically predicted reduction in LDL-C of 1 mmol/L, the risk for type 2 diabetes increased (odds ratio, 2.42).
The estimated absolute risk difference was 5.3 incident cases/1,000 person-years for every genetically predicted 1-mmol/L reduction in LDL-C, Dr. Lotta and his associates said (JAMA. 2016 Oct. 4. doi: 10.1001/jama.2016.14568).
These findings are consistent with reports that link cholesterol-lowering medications with weight gain and a higher incidence of new-onset type 2 diabetes, as well as with the clinical observation that patients with familial hypercholesterolemia carry a lower risk for diabetes. “These results warrant the continued monitoring of the glycemic effects of ezetimibe in clinical trials and in clinical practice,” the researchers noted.
Naturally occurring variations on or near the NPC1L1 gene, which is linked to lower LDL-cholesterol levels, were associated with a higher risk of type 2 diabetes in a meta-analysis reported online Oct. 4 in JAMA.
Some cholesterol-lowering medications, notably ezetimibe, work by inhibiting the action of the NPC1L1 gene. The findings of this meta-analysis suggest that by doing so, these cholesterol-lowering agents may raise the risk of type 2 diabetes, said Luca A. Lotta, MD, PhD, of the Medical Research Council Epidemiology Unit, University of Cambridge (U.K.), and his associates. The investigators examined gene-association analyses in several studies and databases covering 50,775 adults with type 2 diabetes and 270,269 control subjects in Europe and the United States during 1991-2016. They found that alleles at the NPC1L1 locus that are known to be associated with lower LDL-cholesterol levels also were strongly associated with higher rates of diabetes. For every genetically predicted reduction in LDL-C of 1 mmol/L, the risk for type 2 diabetes increased (odds ratio, 2.42).
The estimated absolute risk difference was 5.3 incident cases/1,000 person-years for every genetically predicted 1-mmol/L reduction in LDL-C, Dr. Lotta and his associates said (JAMA. 2016 Oct. 4. doi: 10.1001/jama.2016.14568).
These findings are consistent with reports that link cholesterol-lowering medications with weight gain and a higher incidence of new-onset type 2 diabetes, as well as with the clinical observation that patients with familial hypercholesterolemia carry a lower risk for diabetes. “These results warrant the continued monitoring of the glycemic effects of ezetimibe in clinical trials and in clinical practice,” the researchers noted.
Naturally occurring variations on or near the NPC1L1 gene, which is linked to lower LDL-cholesterol levels, were associated with a higher risk of type 2 diabetes in a meta-analysis reported online Oct. 4 in JAMA.
Some cholesterol-lowering medications, notably ezetimibe, work by inhibiting the action of the NPC1L1 gene. The findings of this meta-analysis suggest that by doing so, these cholesterol-lowering agents may raise the risk of type 2 diabetes, said Luca A. Lotta, MD, PhD, of the Medical Research Council Epidemiology Unit, University of Cambridge (U.K.), and his associates. The investigators examined gene-association analyses in several studies and databases covering 50,775 adults with type 2 diabetes and 270,269 control subjects in Europe and the United States during 1991-2016. They found that alleles at the NPC1L1 locus that are known to be associated with lower LDL-cholesterol levels also were strongly associated with higher rates of diabetes. For every genetically predicted reduction in LDL-C of 1 mmol/L, the risk for type 2 diabetes increased (odds ratio, 2.42).
The estimated absolute risk difference was 5.3 incident cases/1,000 person-years for every genetically predicted 1-mmol/L reduction in LDL-C, Dr. Lotta and his associates said (JAMA. 2016 Oct. 4. doi: 10.1001/jama.2016.14568).
These findings are consistent with reports that link cholesterol-lowering medications with weight gain and a higher incidence of new-onset type 2 diabetes, as well as with the clinical observation that patients with familial hypercholesterolemia carry a lower risk for diabetes. “These results warrant the continued monitoring of the glycemic effects of ezetimibe in clinical trials and in clinical practice,” the researchers noted.
Key clinical point:
Major finding: The estimated difference in absolute risk was 5.3 incident cases of diabetes per 1,000 person-years for every genetically predicted 1-mmol/L reduction in LDL-C.
Data source: A meta-analysis of gene-association analyses in several studies and databases covering 50,775 adults with diabetes and 270,269 control subjects.
Disclosures: This study was supported by the U.K. Medical Research Council, the National Institute of Health Research Biomedical Research Centre, and Wellcome Trust. Dr. Lotta reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Simple interventions markedly improve hepatitis care
Several simple, inexpensive operational interventions substantially improve care for viral hepatitis, according to a report published in the Lancet.
Recent advances in treatment for chronic hepatitis B and chronic hepatitis C have the potential to halt or even reverse the progression of associated liver disease and to reduce related mortality, reported Kali Zhou, MD, of the division of gastroenterology, University of California, San Francisco, and her associates. But they can do so only if affected individuals are engaged and retained in the relatively long continuum of care, from diagnosis through viral suppression or cure.
To assess the usefulness of interventions that promote such patient engagement and retention, Dr. Zhou and her colleagues reviewed the scientific literature and performed a meta-analysis of 56 studies. They examined 15 studies on HBV care, 38 on HCV care, and 3 on both types of hepatitis (Lancet Infect Dis. 2016 Sep 5. doi: 10.1016/S1473-3099[16]30208-0).
Among their findings:
• Educating a single lay health worker to improve knowledge about the disease in his or her community and to promote diagnostic testing nearly tripled the testing rate (relative risk, 2.68), compared with no such intervention.
• Clinician reminders during regular office visits to consider hepatitis testing – such as prompts in the patients’ electronic medical records or stickers on their charts – nearly quadrupled the testing rate (RR, 3.70), compared with no clinician reminders.
• Providing guided referral to a hepatitis specialist for people at risk for the disorder markedly improved the rate of visits to such specialists (RR, 1.57), compared with no such referrals.
• Providing psychological counseling and motivational therapy for mental health and/or substance misuse problems along with medical care for hepatitis dramatically increased the number of patients treated (OR, 3.42) and raised the rate of treatment completion (RR, 1.14).
• Combining mental health, substance misuse, and hepatitis treatment services at one location increased the rate of treatment initiation (RR, 1.36), treatment adherence (RR, 1.22), and cure as measured by sustained virologic response rate (RR, 1.21), compared with usual care.These interventions might be useful in augmenting hepatitis treatment programs worldwide, Dr. Zhou and her associates said.
The World Health Organization and the U.S. Fulbright Program supported the study. Dr. Zhou and her associates reported having no relevant financial disclosures.
This meta-analysis identified proven strategies that can be adopted widely and can become standard components of a package of health care services for viral hepatitis.
But it also revealed the need for additional high-quality data to guide the development of even more such strategies. Reducing the burden of hepatitis depends on helping patients navigate through diagnosis; referral to specialist care; completion of complex, long-term treatment; and linkages to related clinical services such as mental health or substance misuse counseling.
John W. Ward, MD, is director of the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta. He reported having no relevant financial disclosures. Dr. Ward made these remarks in a comment accompanying Dr. Zhou’s report (Lancet. 2016 Sep 5; doi: 10.1016/S1473-3099[16]30272-9).
AGA Resource
Through the HCV Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards, and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
This meta-analysis identified proven strategies that can be adopted widely and can become standard components of a package of health care services for viral hepatitis.
But it also revealed the need for additional high-quality data to guide the development of even more such strategies. Reducing the burden of hepatitis depends on helping patients navigate through diagnosis; referral to specialist care; completion of complex, long-term treatment; and linkages to related clinical services such as mental health or substance misuse counseling.
John W. Ward, MD, is director of the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta. He reported having no relevant financial disclosures. Dr. Ward made these remarks in a comment accompanying Dr. Zhou’s report (Lancet. 2016 Sep 5; doi: 10.1016/S1473-3099[16]30272-9).
AGA Resource
Through the HCV Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards, and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
This meta-analysis identified proven strategies that can be adopted widely and can become standard components of a package of health care services for viral hepatitis.
But it also revealed the need for additional high-quality data to guide the development of even more such strategies. Reducing the burden of hepatitis depends on helping patients navigate through diagnosis; referral to specialist care; completion of complex, long-term treatment; and linkages to related clinical services such as mental health or substance misuse counseling.
John W. Ward, MD, is director of the division of viral hepatitis at the Centers for Disease Control and Prevention, Atlanta. He reported having no relevant financial disclosures. Dr. Ward made these remarks in a comment accompanying Dr. Zhou’s report (Lancet. 2016 Sep 5; doi: 10.1016/S1473-3099[16]30272-9).
AGA Resource
Through the HCV Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards, and improve the process of care for patients. Learn more at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
Several simple, inexpensive operational interventions substantially improve care for viral hepatitis, according to a report published in the Lancet.
Recent advances in treatment for chronic hepatitis B and chronic hepatitis C have the potential to halt or even reverse the progression of associated liver disease and to reduce related mortality, reported Kali Zhou, MD, of the division of gastroenterology, University of California, San Francisco, and her associates. But they can do so only if affected individuals are engaged and retained in the relatively long continuum of care, from diagnosis through viral suppression or cure.
To assess the usefulness of interventions that promote such patient engagement and retention, Dr. Zhou and her colleagues reviewed the scientific literature and performed a meta-analysis of 56 studies. They examined 15 studies on HBV care, 38 on HCV care, and 3 on both types of hepatitis (Lancet Infect Dis. 2016 Sep 5. doi: 10.1016/S1473-3099[16]30208-0).
Among their findings:
• Educating a single lay health worker to improve knowledge about the disease in his or her community and to promote diagnostic testing nearly tripled the testing rate (relative risk, 2.68), compared with no such intervention.
• Clinician reminders during regular office visits to consider hepatitis testing – such as prompts in the patients’ electronic medical records or stickers on their charts – nearly quadrupled the testing rate (RR, 3.70), compared with no clinician reminders.
• Providing guided referral to a hepatitis specialist for people at risk for the disorder markedly improved the rate of visits to such specialists (RR, 1.57), compared with no such referrals.
• Providing psychological counseling and motivational therapy for mental health and/or substance misuse problems along with medical care for hepatitis dramatically increased the number of patients treated (OR, 3.42) and raised the rate of treatment completion (RR, 1.14).
• Combining mental health, substance misuse, and hepatitis treatment services at one location increased the rate of treatment initiation (RR, 1.36), treatment adherence (RR, 1.22), and cure as measured by sustained virologic response rate (RR, 1.21), compared with usual care.These interventions might be useful in augmenting hepatitis treatment programs worldwide, Dr. Zhou and her associates said.
The World Health Organization and the U.S. Fulbright Program supported the study. Dr. Zhou and her associates reported having no relevant financial disclosures.
Several simple, inexpensive operational interventions substantially improve care for viral hepatitis, according to a report published in the Lancet.
Recent advances in treatment for chronic hepatitis B and chronic hepatitis C have the potential to halt or even reverse the progression of associated liver disease and to reduce related mortality, reported Kali Zhou, MD, of the division of gastroenterology, University of California, San Francisco, and her associates. But they can do so only if affected individuals are engaged and retained in the relatively long continuum of care, from diagnosis through viral suppression or cure.
To assess the usefulness of interventions that promote such patient engagement and retention, Dr. Zhou and her colleagues reviewed the scientific literature and performed a meta-analysis of 56 studies. They examined 15 studies on HBV care, 38 on HCV care, and 3 on both types of hepatitis (Lancet Infect Dis. 2016 Sep 5. doi: 10.1016/S1473-3099[16]30208-0).
Among their findings:
• Educating a single lay health worker to improve knowledge about the disease in his or her community and to promote diagnostic testing nearly tripled the testing rate (relative risk, 2.68), compared with no such intervention.
• Clinician reminders during regular office visits to consider hepatitis testing – such as prompts in the patients’ electronic medical records or stickers on their charts – nearly quadrupled the testing rate (RR, 3.70), compared with no clinician reminders.
• Providing guided referral to a hepatitis specialist for people at risk for the disorder markedly improved the rate of visits to such specialists (RR, 1.57), compared with no such referrals.
• Providing psychological counseling and motivational therapy for mental health and/or substance misuse problems along with medical care for hepatitis dramatically increased the number of patients treated (OR, 3.42) and raised the rate of treatment completion (RR, 1.14).
• Combining mental health, substance misuse, and hepatitis treatment services at one location increased the rate of treatment initiation (RR, 1.36), treatment adherence (RR, 1.22), and cure as measured by sustained virologic response rate (RR, 1.21), compared with usual care.These interventions might be useful in augmenting hepatitis treatment programs worldwide, Dr. Zhou and her associates said.
The World Health Organization and the U.S. Fulbright Program supported the study. Dr. Zhou and her associates reported having no relevant financial disclosures.
Key clinical point: Several simple, inexpensive operational interventions substantially improve care for viral hepatitis.
Major finding: Clinician reminders during regular office visits to consider hepatitis testing – such as prompts in the patients’ electronic medical records or stickers on their charts – nearly quadrupled the testing rate (relative risk, 3.70).
Data source: A meta-analysis of 56 studies worldwide assessing interventions to improve HBV and HCV care.
Disclosures: The World Health Organization and the U.S. Fulbright Program supported the study. Dr. Zhou and her associates reported having no relevant financial disclosures.
Incontinence trial finds small advantage for Botox over sacral neuromodulation
OnabotulinumtoxinA decreased daily episodes of urinary incontinence by a small amount, compared with sacral neuromodulation, but did not appear to impact several quality of life measures and raised the rates of urinary tract infection and self-catheterization, according to findings from a comparative effectiveness study.
In an open-label randomized trial directly comparing the two approaches for refractory urgency incontinence, onabotulinumtoxinA showed a statistically significant advantage over sacral neuromodulation, but whether this translates into a clinically significant difference is unclear.
“Overall, these findings make it uncertain whether onabotulinumtoxinA provides a clinically important net benefit, compared with sacral neuromodulation,” said Cindy L. Amundsen, MD, of Duke University, Durham N.C., and her associates.
Noting that a recent systematic review of the literature found insufficient evidence to recommend one of these treatments over the other, the investigators performed their study at nine medical centers participating in the National Institutes of Health’s Pelvic Floor Disorder Network. Study participants included 386 women who had a minimum of six urgency incontinence episodes per day and whose symptoms persisted despite treatment with at least one behavioral or physical therapy intervention and at least two medical therapies. They were followed up at 6 months.
In the intention-to-treat analysis, the 190 women who received a single injection of onabotulinumtoxinA showed a mean reduction of 3.9 daily episodes of urinary incontinence, compared with a reduction of 3.3 episodes for the 174 women who underwent sacral neuromodulation. The onabotulinumtoxinA group also showed slightly greater improvement on the Overactive Bladder Short Form score for symptom bother and on the Overactive Bladder Satisfaction of Treatment questionnaire, Dr. Amundsen and her associates reported (JAMA. 2016;316[13]:1366-1374).
However, there were no significant differences between the two study groups in measures of convenience, adverse effects, treatment preference, or other quality of life factors. And onabotulinumtoxinA was associated with a higher rate of urinary tract infection (35% vs. 11%) and of intermittent self-catheterization (8% vs. 0% at 1 month).
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the NIH Office of Research on Women’s Health. Dr. Amundsen reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, Medtronic (maker of the InterStim sacral neuromodulation device), Allergan (maker of Botox), and Axonics.
OnabotulinumtoxinA decreased daily episodes of urinary incontinence by a small amount, compared with sacral neuromodulation, but did not appear to impact several quality of life measures and raised the rates of urinary tract infection and self-catheterization, according to findings from a comparative effectiveness study.
In an open-label randomized trial directly comparing the two approaches for refractory urgency incontinence, onabotulinumtoxinA showed a statistically significant advantage over sacral neuromodulation, but whether this translates into a clinically significant difference is unclear.
“Overall, these findings make it uncertain whether onabotulinumtoxinA provides a clinically important net benefit, compared with sacral neuromodulation,” said Cindy L. Amundsen, MD, of Duke University, Durham N.C., and her associates.
Noting that a recent systematic review of the literature found insufficient evidence to recommend one of these treatments over the other, the investigators performed their study at nine medical centers participating in the National Institutes of Health’s Pelvic Floor Disorder Network. Study participants included 386 women who had a minimum of six urgency incontinence episodes per day and whose symptoms persisted despite treatment with at least one behavioral or physical therapy intervention and at least two medical therapies. They were followed up at 6 months.
In the intention-to-treat analysis, the 190 women who received a single injection of onabotulinumtoxinA showed a mean reduction of 3.9 daily episodes of urinary incontinence, compared with a reduction of 3.3 episodes for the 174 women who underwent sacral neuromodulation. The onabotulinumtoxinA group also showed slightly greater improvement on the Overactive Bladder Short Form score for symptom bother and on the Overactive Bladder Satisfaction of Treatment questionnaire, Dr. Amundsen and her associates reported (JAMA. 2016;316[13]:1366-1374).
However, there were no significant differences between the two study groups in measures of convenience, adverse effects, treatment preference, or other quality of life factors. And onabotulinumtoxinA was associated with a higher rate of urinary tract infection (35% vs. 11%) and of intermittent self-catheterization (8% vs. 0% at 1 month).
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the NIH Office of Research on Women’s Health. Dr. Amundsen reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, Medtronic (maker of the InterStim sacral neuromodulation device), Allergan (maker of Botox), and Axonics.
OnabotulinumtoxinA decreased daily episodes of urinary incontinence by a small amount, compared with sacral neuromodulation, but did not appear to impact several quality of life measures and raised the rates of urinary tract infection and self-catheterization, according to findings from a comparative effectiveness study.
In an open-label randomized trial directly comparing the two approaches for refractory urgency incontinence, onabotulinumtoxinA showed a statistically significant advantage over sacral neuromodulation, but whether this translates into a clinically significant difference is unclear.
“Overall, these findings make it uncertain whether onabotulinumtoxinA provides a clinically important net benefit, compared with sacral neuromodulation,” said Cindy L. Amundsen, MD, of Duke University, Durham N.C., and her associates.
Noting that a recent systematic review of the literature found insufficient evidence to recommend one of these treatments over the other, the investigators performed their study at nine medical centers participating in the National Institutes of Health’s Pelvic Floor Disorder Network. Study participants included 386 women who had a minimum of six urgency incontinence episodes per day and whose symptoms persisted despite treatment with at least one behavioral or physical therapy intervention and at least two medical therapies. They were followed up at 6 months.
In the intention-to-treat analysis, the 190 women who received a single injection of onabotulinumtoxinA showed a mean reduction of 3.9 daily episodes of urinary incontinence, compared with a reduction of 3.3 episodes for the 174 women who underwent sacral neuromodulation. The onabotulinumtoxinA group also showed slightly greater improvement on the Overactive Bladder Short Form score for symptom bother and on the Overactive Bladder Satisfaction of Treatment questionnaire, Dr. Amundsen and her associates reported (JAMA. 2016;316[13]:1366-1374).
However, there were no significant differences between the two study groups in measures of convenience, adverse effects, treatment preference, or other quality of life factors. And onabotulinumtoxinA was associated with a higher rate of urinary tract infection (35% vs. 11%) and of intermittent self-catheterization (8% vs. 0% at 1 month).
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the NIH Office of Research on Women’s Health. Dr. Amundsen reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, Medtronic (maker of the InterStim sacral neuromodulation device), Allergan (maker of Botox), and Axonics.
Key clinical point:
Major finding: The 190 women who received a single injection of onabotulinumtoxinA showed a mean reduction of 3.9 daily episodes of urinary incontinence, compared with a reduction of 3.3 episodes for the 174 women who underwent sacral neuromodulation.
Data source: A multicenter open-label randomized trial involving 386 women followed for 6 months.
Disclosures: This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the NIH Office of Research on Women’s Health. Dr. Amundsen reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, Medtronic (maker of the InterStim sacral neuromodulation device), Allergan (maker of Botox), and Axonics.
Psoriasis not consistently linked to adverse pregnancy outcomes
Psoriasis was not consistently associated with adverse pregnancy outcomes across nine studies in a systematic review of the literature, but four of the studies reported significant increases in at least one adverse outcome among women with psoriasis, according to a report in the British Journal of Dermatology.
Many women with psoriasis develop the disorder during their reproductive years, and more than 100,000 births to such patients are estimated to occur in the United States each year. Other autoimmune diseases are known to adversely affect pregnancy outcomes, but the issue has not been well studied among women with psoriasis, said Robert Bobotsis, a medical student at Western University, London (Ont.), and his associates.
They performed a systematic review of the literature to examine a possible link, but were only able to find nine fair- or good-quality studies involving a total of 4,756 pregnancies from which to extract data concerning a possible association. This small sample size may have been underpowered to detect the uncommon adverse pregnancy outcomes being assessed. Moreover, the investigators were unable to conduct a meta-analysis pooling the data because the effect measures were inconsistent across the nine studies, Mr. Bobotsis and his associates noted.
The review included a retrospective case series, a retrospective case control study, three retrospective cohort studies, two prospective cohort studies, one cross-sectional study, and one study combining prospective and retrospective cohorts. It “did not demonstrate an increased risk of poor outcomes in pregnant women with psoriasis” (Br J Dermatol. 2016 Jul 24;175:464-72).
However, four studies showed that compared with women who didn’t have psoriasis, those who did were at significantly increased risk for spontaneous abortion, cesarean delivery, low birth weight, macrosomia, large for gestational age, and prematurity, with odds ratios as high as 5.6. “Our results should be viewed as an opportunity to further research pregnancy outcomes in psoriasis,” the investigators said.
Psoriasis was not consistently associated with adverse pregnancy outcomes across nine studies in a systematic review of the literature, but four of the studies reported significant increases in at least one adverse outcome among women with psoriasis, according to a report in the British Journal of Dermatology.
Many women with psoriasis develop the disorder during their reproductive years, and more than 100,000 births to such patients are estimated to occur in the United States each year. Other autoimmune diseases are known to adversely affect pregnancy outcomes, but the issue has not been well studied among women with psoriasis, said Robert Bobotsis, a medical student at Western University, London (Ont.), and his associates.
They performed a systematic review of the literature to examine a possible link, but were only able to find nine fair- or good-quality studies involving a total of 4,756 pregnancies from which to extract data concerning a possible association. This small sample size may have been underpowered to detect the uncommon adverse pregnancy outcomes being assessed. Moreover, the investigators were unable to conduct a meta-analysis pooling the data because the effect measures were inconsistent across the nine studies, Mr. Bobotsis and his associates noted.
The review included a retrospective case series, a retrospective case control study, three retrospective cohort studies, two prospective cohort studies, one cross-sectional study, and one study combining prospective and retrospective cohorts. It “did not demonstrate an increased risk of poor outcomes in pregnant women with psoriasis” (Br J Dermatol. 2016 Jul 24;175:464-72).
However, four studies showed that compared with women who didn’t have psoriasis, those who did were at significantly increased risk for spontaneous abortion, cesarean delivery, low birth weight, macrosomia, large for gestational age, and prematurity, with odds ratios as high as 5.6. “Our results should be viewed as an opportunity to further research pregnancy outcomes in psoriasis,” the investigators said.
Psoriasis was not consistently associated with adverse pregnancy outcomes across nine studies in a systematic review of the literature, but four of the studies reported significant increases in at least one adverse outcome among women with psoriasis, according to a report in the British Journal of Dermatology.
Many women with psoriasis develop the disorder during their reproductive years, and more than 100,000 births to such patients are estimated to occur in the United States each year. Other autoimmune diseases are known to adversely affect pregnancy outcomes, but the issue has not been well studied among women with psoriasis, said Robert Bobotsis, a medical student at Western University, London (Ont.), and his associates.
They performed a systematic review of the literature to examine a possible link, but were only able to find nine fair- or good-quality studies involving a total of 4,756 pregnancies from which to extract data concerning a possible association. This small sample size may have been underpowered to detect the uncommon adverse pregnancy outcomes being assessed. Moreover, the investigators were unable to conduct a meta-analysis pooling the data because the effect measures were inconsistent across the nine studies, Mr. Bobotsis and his associates noted.
The review included a retrospective case series, a retrospective case control study, three retrospective cohort studies, two prospective cohort studies, one cross-sectional study, and one study combining prospective and retrospective cohorts. It “did not demonstrate an increased risk of poor outcomes in pregnant women with psoriasis” (Br J Dermatol. 2016 Jul 24;175:464-72).
However, four studies showed that compared with women who didn’t have psoriasis, those who did were at significantly increased risk for spontaneous abortion, cesarean delivery, low birth weight, macrosomia, large for gestational age, and prematurity, with odds ratios as high as 5.6. “Our results should be viewed as an opportunity to further research pregnancy outcomes in psoriasis,” the investigators said.
Key clinical point: Psoriasis is not consistently associated with adverse pregnancy outcomes across studies, but individual studies reported such links.
Major finding: Four of nine studies showed that compared with women who did not have psoriasis, those who did were at significantly increased risk for spontaneous abortion, cesarean delivery, low birth weight, macrosomia, large for gestational age, and prematurity, with odds ratios as high as 5.6.
Data source: A systematic review of nine reports in the literature concerning adverse outcomes in 4,756 pregnancies among women with psoriasis.
Disclosures: The authors reported that this work had no funding sources. Mr. Bobotsis reported having no relevant financial disclosures; two of his associates reported ties to AbbVie, Actelion, Amgen, Bio-K, Celgene, Eli Lilly, Galderma, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Roche, and Valeant.
Seven days of antibiotics sufficient for most hospital-acquired pneumonia
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
Key clinical point: A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology.
Major finding: The joint IDSA/ATS Guidelines include 25 recommendations regarding diagnosis, empiric therapy, and pathogen-targeted antibiotics for HAP and VAP.
Data source: An update to the 2005 Clinical Practice Guidelines for managing adults with HAP or VAP.
Disclosures: The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
October 2016: Click for Credit
Here are 5 articles in the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Autism Follow-up Screening by PCPs Yields High Accuracy
To take the posttest, go to: http://bit.ly/2bTLhFS
Expires August 19, 2017
VITALS
Key clinical point:
Primary care providers can conduct the M-CHAT/F following a positive M-CHAT screening for autism spectrum disorders.
Major finding:
Primary care providers and trained interviewers agreed 86.6% of the time on the screening results of the M-CHAT/F for ASDs.
Data source:
A cohort study of 5,071 children, mean age 23 months, screened with the M-CHAT, and a subsequent 197 children screened with the M-CHAT/F in 22 Maryland primary care practices.
Disclosures:
The National Institutes of Mental Health funded the research. Dr. Sturner is director of Total Child Health (TCH), a for-profit subsidiary of the Center for Promotion of Child Development through Primary Care, which conducted the study. Barbara Howard, MD, is president of TCH. Tanya Morrel, PhD, is an employee of and stockholder in TCH, and Paul Bergmann has consulted for the company. The remaining authors had no relevant disclosures.
2. Gallstone Disease Boosts Heart Risk
To take the posttest, go to: http://bit.ly/2c7TP7D
Expires August 18, 2017
VITALS
Key clinical point:
Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding:
A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source:
A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures:
Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States-Israel Binational Science Foundation. The authors had no relevant financial disclosures.
3. New HER2-testing Guidelines Result in More Women Eligible for Directed Treatment
To take the posttest, go to: http://bit.ly/2cd9llO
Expires July 25, 2017
VITALS
Key clinical point:
New IHC and FISH pathology guidelines categorize more breast cancers as "equivocal" regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive.
Major finding:
By using 2013 guidelines, 358 additional tumors were interpreted as positive, compared with the 2007 guidelines and 298 additional tumors were considered positive, compared with the FDA criteria.
Data source:
A cohort study involving 2,851 breast cancer samples analyzed according to three different pathology guidelines during a 1-year period.
Disclosures:
This study was supported by the Mayo Clinic. Dr. Shah reported having no relevant financial disclosures; his associates reported ties to Merck, Hospira, Ariad Pharmaceuticals, Abbott Molecular, and Genome Diagnostics.
4. Extreme Alcohol Use Worsens HIV Disease
To take the posttest, go to: http://bit.ly/2coIzG3
Expires August 14, 2017
VITALS
Key clinical point:
A pattern of heavy alcohol use over time in HIV-infected patients was associated with accelerated HIV disease progression.
Major finding:
Long-term heavy alcohol use by middle-aged, HIV-infected military veterans was associated with a 1.83-fold increased likelihood of also being in the highest-risk group for accelerated progression of HIV disease.
Data source:
This study included 3,539 U.S. military veterans receiving care for HIV infection at eight VA centers. The impact of their long-term pattern of alcohol use on HIV disease progression was assessed over an 8-year period by annual assessments using validated instruments.
Disclosures:
The presenter reported having no financial conflicts of interest regarding the study, funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute of Allergy and Infectious Diseases.
5. Weight Loss Boosts TNFis' Psoriatic Arthritis Efficacy
To take the posttest, go to: http://bit.ly/2chD4M1
Expires July 23, 2017
Here are 5 articles in the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Autism Follow-up Screening by PCPs Yields High Accuracy
To take the posttest, go to: http://bit.ly/2bTLhFS
Expires August 19, 2017
VITALS
Key clinical point:
Primary care providers can conduct the M-CHAT/F following a positive M-CHAT screening for autism spectrum disorders.
Major finding:
Primary care providers and trained interviewers agreed 86.6% of the time on the screening results of the M-CHAT/F for ASDs.
Data source:
A cohort study of 5,071 children, mean age 23 months, screened with the M-CHAT, and a subsequent 197 children screened with the M-CHAT/F in 22 Maryland primary care practices.
Disclosures:
The National Institutes of Mental Health funded the research. Dr. Sturner is director of Total Child Health (TCH), a for-profit subsidiary of the Center for Promotion of Child Development through Primary Care, which conducted the study. Barbara Howard, MD, is president of TCH. Tanya Morrel, PhD, is an employee of and stockholder in TCH, and Paul Bergmann has consulted for the company. The remaining authors had no relevant disclosures.
2. Gallstone Disease Boosts Heart Risk
To take the posttest, go to: http://bit.ly/2c7TP7D
Expires August 18, 2017
VITALS
Key clinical point:
Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding:
A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source:
A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures:
Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States-Israel Binational Science Foundation. The authors had no relevant financial disclosures.
3. New HER2-testing Guidelines Result in More Women Eligible for Directed Treatment
To take the posttest, go to: http://bit.ly/2cd9llO
Expires July 25, 2017
VITALS
Key clinical point:
New IHC and FISH pathology guidelines categorize more breast cancers as "equivocal" regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive.
Major finding:
By using 2013 guidelines, 358 additional tumors were interpreted as positive, compared with the 2007 guidelines and 298 additional tumors were considered positive, compared with the FDA criteria.
Data source:
A cohort study involving 2,851 breast cancer samples analyzed according to three different pathology guidelines during a 1-year period.
Disclosures:
This study was supported by the Mayo Clinic. Dr. Shah reported having no relevant financial disclosures; his associates reported ties to Merck, Hospira, Ariad Pharmaceuticals, Abbott Molecular, and Genome Diagnostics.
4. Extreme Alcohol Use Worsens HIV Disease
To take the posttest, go to: http://bit.ly/2coIzG3
Expires August 14, 2017
VITALS
Key clinical point:
A pattern of heavy alcohol use over time in HIV-infected patients was associated with accelerated HIV disease progression.
Major finding:
Long-term heavy alcohol use by middle-aged, HIV-infected military veterans was associated with a 1.83-fold increased likelihood of also being in the highest-risk group for accelerated progression of HIV disease.
Data source:
This study included 3,539 U.S. military veterans receiving care for HIV infection at eight VA centers. The impact of their long-term pattern of alcohol use on HIV disease progression was assessed over an 8-year period by annual assessments using validated instruments.
Disclosures:
The presenter reported having no financial conflicts of interest regarding the study, funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute of Allergy and Infectious Diseases.
5. Weight Loss Boosts TNFis' Psoriatic Arthritis Efficacy
To take the posttest, go to: http://bit.ly/2chD4M1
Expires July 23, 2017
Here are 5 articles in the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Autism Follow-up Screening by PCPs Yields High Accuracy
To take the posttest, go to: http://bit.ly/2bTLhFS
Expires August 19, 2017
VITALS
Key clinical point:
Primary care providers can conduct the M-CHAT/F following a positive M-CHAT screening for autism spectrum disorders.
Major finding:
Primary care providers and trained interviewers agreed 86.6% of the time on the screening results of the M-CHAT/F for ASDs.
Data source:
A cohort study of 5,071 children, mean age 23 months, screened with the M-CHAT, and a subsequent 197 children screened with the M-CHAT/F in 22 Maryland primary care practices.
Disclosures:
The National Institutes of Mental Health funded the research. Dr. Sturner is director of Total Child Health (TCH), a for-profit subsidiary of the Center for Promotion of Child Development through Primary Care, which conducted the study. Barbara Howard, MD, is president of TCH. Tanya Morrel, PhD, is an employee of and stockholder in TCH, and Paul Bergmann has consulted for the company. The remaining authors had no relevant disclosures.
2. Gallstone Disease Boosts Heart Risk
To take the posttest, go to: http://bit.ly/2c7TP7D
Expires August 18, 2017
VITALS
Key clinical point:
Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding:
A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source:
A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures:
Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States-Israel Binational Science Foundation. The authors had no relevant financial disclosures.
3. New HER2-testing Guidelines Result in More Women Eligible for Directed Treatment
To take the posttest, go to: http://bit.ly/2cd9llO
Expires July 25, 2017
VITALS
Key clinical point:
New IHC and FISH pathology guidelines categorize more breast cancers as "equivocal" regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive.
Major finding:
By using 2013 guidelines, 358 additional tumors were interpreted as positive, compared with the 2007 guidelines and 298 additional tumors were considered positive, compared with the FDA criteria.
Data source:
A cohort study involving 2,851 breast cancer samples analyzed according to three different pathology guidelines during a 1-year period.
Disclosures:
This study was supported by the Mayo Clinic. Dr. Shah reported having no relevant financial disclosures; his associates reported ties to Merck, Hospira, Ariad Pharmaceuticals, Abbott Molecular, and Genome Diagnostics.
4. Extreme Alcohol Use Worsens HIV Disease
To take the posttest, go to: http://bit.ly/2coIzG3
Expires August 14, 2017
VITALS
Key clinical point:
A pattern of heavy alcohol use over time in HIV-infected patients was associated with accelerated HIV disease progression.
Major finding:
Long-term heavy alcohol use by middle-aged, HIV-infected military veterans was associated with a 1.83-fold increased likelihood of also being in the highest-risk group for accelerated progression of HIV disease.
Data source:
This study included 3,539 U.S. military veterans receiving care for HIV infection at eight VA centers. The impact of their long-term pattern of alcohol use on HIV disease progression was assessed over an 8-year period by annual assessments using validated instruments.
Disclosures:
The presenter reported having no financial conflicts of interest regarding the study, funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute of Allergy and Infectious Diseases.
5. Weight Loss Boosts TNFis' Psoriatic Arthritis Efficacy
To take the posttest, go to: http://bit.ly/2chD4M1
Expires July 23, 2017