User login
Ibudilast’s efficacy differs in primary and secondary progressive MS
PHILADELPHIA – researchers reported at the annual meeting of the American Academy of Neurology.
The difference may be related to faster atrophy rates among patients with primary progressive MS who received placebo, compared with those with secondary progressive MS who received placebo.
The finding was surprising, said Andrew Goodman, MD, professor of neurology, chief of the neuroimmunology unit, and director of the multiple sclerosis center at the University of Rochester (N.Y.). “Going into the trial, it was my bias and expectation that both primary and secondary progressive MS would behave more similarly than different.”
The trial, SPRINT-MS, included more than 250 patients with progressive MS at 28 sites. Patients were aged 18-65 years and were followed for 96 weeks. Patients had primary progressive MS (n = 134) or secondary progressive MS (n = 121) and were randomized 1:1 to ibudilast or placebo.
Ibudilast is an orally administered small molecule that has been used in Japan for approximately 30 years for asthma and other indications, Dr. Goodman said. Preclinical models suggested that the drug may have neuroprotective effects.
The trial’s primary result – a 48% slowing in the rate of whole brain atrophy as measured by brain parenchymal fraction with ibudilast – was reported last year (N Engl J Med. 2018 Aug 30;379[9]:846-55).
The present study examined whether the treatment effect of ibudilast was similar by progressive disease type using a linear mixed model analytic approach.
The group with primary progressive MS included a smaller percentage of women. Patients with secondary progressive MS had longer disease duration and more brain atrophy at baseline.
“The overall benefit which we previously reported appears to be driven by subjects with primary progressive rather than secondary progressive MS,” Dr. Goodman said. Accounting for baseline covariates did not affect this result.
Among patients who received placebo, brain atrophy in those with secondary progressive MS was 57% slower than in those with primary progressive MS. The rate of atrophy for untreated patients with primary progressive MS “was roughly twice as fast as that in the secondary progressive MS group, which we think may explain in part the differential in efficacy,” Dr. Goodman said. “These findings may impact future trial design for progressive MS.”
The SPRINT-MS trial was funded by the National Institute of Neurological Disorders and Stroke. The National Multiple Sclerosis Society and MediciNova also supported the study. Dr. Goodman reported receiving research support from pharmaceutical companies, as well as personal compensation from companies for consulting, serving on a scientific advisory board, and speaking.
SOURCE: Goodman A et al. AAN 2019, Abstract S12.007.
PHILADELPHIA – researchers reported at the annual meeting of the American Academy of Neurology.
The difference may be related to faster atrophy rates among patients with primary progressive MS who received placebo, compared with those with secondary progressive MS who received placebo.
The finding was surprising, said Andrew Goodman, MD, professor of neurology, chief of the neuroimmunology unit, and director of the multiple sclerosis center at the University of Rochester (N.Y.). “Going into the trial, it was my bias and expectation that both primary and secondary progressive MS would behave more similarly than different.”
The trial, SPRINT-MS, included more than 250 patients with progressive MS at 28 sites. Patients were aged 18-65 years and were followed for 96 weeks. Patients had primary progressive MS (n = 134) or secondary progressive MS (n = 121) and were randomized 1:1 to ibudilast or placebo.
Ibudilast is an orally administered small molecule that has been used in Japan for approximately 30 years for asthma and other indications, Dr. Goodman said. Preclinical models suggested that the drug may have neuroprotective effects.
The trial’s primary result – a 48% slowing in the rate of whole brain atrophy as measured by brain parenchymal fraction with ibudilast – was reported last year (N Engl J Med. 2018 Aug 30;379[9]:846-55).
The present study examined whether the treatment effect of ibudilast was similar by progressive disease type using a linear mixed model analytic approach.
The group with primary progressive MS included a smaller percentage of women. Patients with secondary progressive MS had longer disease duration and more brain atrophy at baseline.
“The overall benefit which we previously reported appears to be driven by subjects with primary progressive rather than secondary progressive MS,” Dr. Goodman said. Accounting for baseline covariates did not affect this result.
Among patients who received placebo, brain atrophy in those with secondary progressive MS was 57% slower than in those with primary progressive MS. The rate of atrophy for untreated patients with primary progressive MS “was roughly twice as fast as that in the secondary progressive MS group, which we think may explain in part the differential in efficacy,” Dr. Goodman said. “These findings may impact future trial design for progressive MS.”
The SPRINT-MS trial was funded by the National Institute of Neurological Disorders and Stroke. The National Multiple Sclerosis Society and MediciNova also supported the study. Dr. Goodman reported receiving research support from pharmaceutical companies, as well as personal compensation from companies for consulting, serving on a scientific advisory board, and speaking.
SOURCE: Goodman A et al. AAN 2019, Abstract S12.007.
PHILADELPHIA – researchers reported at the annual meeting of the American Academy of Neurology.
The difference may be related to faster atrophy rates among patients with primary progressive MS who received placebo, compared with those with secondary progressive MS who received placebo.
The finding was surprising, said Andrew Goodman, MD, professor of neurology, chief of the neuroimmunology unit, and director of the multiple sclerosis center at the University of Rochester (N.Y.). “Going into the trial, it was my bias and expectation that both primary and secondary progressive MS would behave more similarly than different.”
The trial, SPRINT-MS, included more than 250 patients with progressive MS at 28 sites. Patients were aged 18-65 years and were followed for 96 weeks. Patients had primary progressive MS (n = 134) or secondary progressive MS (n = 121) and were randomized 1:1 to ibudilast or placebo.
Ibudilast is an orally administered small molecule that has been used in Japan for approximately 30 years for asthma and other indications, Dr. Goodman said. Preclinical models suggested that the drug may have neuroprotective effects.
The trial’s primary result – a 48% slowing in the rate of whole brain atrophy as measured by brain parenchymal fraction with ibudilast – was reported last year (N Engl J Med. 2018 Aug 30;379[9]:846-55).
The present study examined whether the treatment effect of ibudilast was similar by progressive disease type using a linear mixed model analytic approach.
The group with primary progressive MS included a smaller percentage of women. Patients with secondary progressive MS had longer disease duration and more brain atrophy at baseline.
“The overall benefit which we previously reported appears to be driven by subjects with primary progressive rather than secondary progressive MS,” Dr. Goodman said. Accounting for baseline covariates did not affect this result.
Among patients who received placebo, brain atrophy in those with secondary progressive MS was 57% slower than in those with primary progressive MS. The rate of atrophy for untreated patients with primary progressive MS “was roughly twice as fast as that in the secondary progressive MS group, which we think may explain in part the differential in efficacy,” Dr. Goodman said. “These findings may impact future trial design for progressive MS.”
The SPRINT-MS trial was funded by the National Institute of Neurological Disorders and Stroke. The National Multiple Sclerosis Society and MediciNova also supported the study. Dr. Goodman reported receiving research support from pharmaceutical companies, as well as personal compensation from companies for consulting, serving on a scientific advisory board, and speaking.
SOURCE: Goodman A et al. AAN 2019, Abstract S12.007.
REPORTING FROM AAN 2019
Rimegepant dissolving tablets treat acute migraine in phase 3 trial
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
REPORTING FROM AAN 2019
Can an antisense oligonucleotide benefit patients with SOD1-ALS?
PHILADELPHIA – In patients with amyotrophic lateral sclerosis (ALS) caused by gain-of-toxic function mutations in the SOD1 gene, according to phase 1/2 trial results presented at the annual meeting of the American Academy of Neurology. Exploratory analyses suggest that the drug, known as tofersen (also known as BIIB067), may lessen declines in function, respiratory function, and strength. The treatment generally was safe and well tolerated, researchers said.
Most ALS cases are sporadic, but about 10% are genetic, of which approximately 20% are caused by SOD1 mutations. “Although SOD1-ALS disease progression is heterogeneous, the underlying pathophysiology, attributable to mutant SOD1 toxicity, is thought to be consistent across SOD1 mutation types,” said Timothy M. Miller, MD, PhD, of Washington University, St. Louis, and colleagues. “As such, effective reduction of SOD1 protein, irrespective of mutation, has the potential to alter the disease course of people with SOD1-ALS.”
Tofersen is an antisense oligonucleotide ribonuclease H1-mediated inhibitor of SOD1 messenger RNA. To study its safety, tolerability, pharmacokinetics, pharmacodynamics, and exploratory efficacy in patients with SOD1-ALS, investigators conducted a double-blind study. The investigators randomized 50 patients with ALS with a SOD1 mutation to 20 mg (n = 10), 40 mg (n = 9), 60 mg (n = 9), or 100 mg (n = 10) of tofersen or placebo (n = 12).
Patients received tofersen by intrathecal bolus over 1-3 minutes. They received a loading regimen on days 1, 15, and 29 and maintenance dosing on days 57 and 85. After the dosing period, patients completed a 12-week follow-up period.
Adverse events
All patients received at least one dose of the study treatment, and 48 received all treatments. Three patients died during the study. One patient in the 20-mg group died of pulmonary embolism, and one patient in both the 60-mg group and placebo group died of respiratory failure. Investigators considered the deaths secondary to ALS or other conditions and not drug related.
Most adverse events were mild or moderate. The most common adverse events among tofersen-treated patients were headache (n = 16), procedural pain (n = 14), and post–lumbar puncture syndrome (n = 13). Five patients who received tofersen and two who received placebo experienced serious adverse events; no serious adverse events occurred in the 100-mg dose group.
“A reduction from baseline in CSF SOD1 concentrations was observed in the tofersen 40-, 60-, and 100-mg cohorts with the maximal reduction observed in the 100 mg–treated group [37% vs. no reduction in the placebo group; P less than 0.002] at day 85,” the investigators reported.
Possible efficacy
In exploratory analyses, the 100-mg dose slowed decline on the Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised (ASLFRS-R), compared with placebo. Mean change in ASLFRS-R from baseline to day 85 was –1.1 in patients who received 100 mg of tofersen, compared with –5.3 for patients who received placebo. Declines on measures of respiratory function and muscle strength also slowed. “Across clinical measures, separation from placebo was most apparent in participants with fast progressing disease,” the researchers said.
“Lower concentrations of the protein in the spinal fluid suggest that there were also lower concentrations in the brain and spinal cord,” Dr. Miller said in a news release. “Such reductions could lead to preservation of motor neurons and slow progression of the disease, but more study is needed to examine this further.”
The study was sponsored by Biogen, which is developing tofersen. Some of the study authors are Biogen employees. Dr. Miller is on Biogen’s medical advisory board and receives clinical research support from Biogen. In addition, he consults, has licensing agreements with, and is a principal investigator for other companies.
PHILADELPHIA – In patients with amyotrophic lateral sclerosis (ALS) caused by gain-of-toxic function mutations in the SOD1 gene, according to phase 1/2 trial results presented at the annual meeting of the American Academy of Neurology. Exploratory analyses suggest that the drug, known as tofersen (also known as BIIB067), may lessen declines in function, respiratory function, and strength. The treatment generally was safe and well tolerated, researchers said.
Most ALS cases are sporadic, but about 10% are genetic, of which approximately 20% are caused by SOD1 mutations. “Although SOD1-ALS disease progression is heterogeneous, the underlying pathophysiology, attributable to mutant SOD1 toxicity, is thought to be consistent across SOD1 mutation types,” said Timothy M. Miller, MD, PhD, of Washington University, St. Louis, and colleagues. “As such, effective reduction of SOD1 protein, irrespective of mutation, has the potential to alter the disease course of people with SOD1-ALS.”
Tofersen is an antisense oligonucleotide ribonuclease H1-mediated inhibitor of SOD1 messenger RNA. To study its safety, tolerability, pharmacokinetics, pharmacodynamics, and exploratory efficacy in patients with SOD1-ALS, investigators conducted a double-blind study. The investigators randomized 50 patients with ALS with a SOD1 mutation to 20 mg (n = 10), 40 mg (n = 9), 60 mg (n = 9), or 100 mg (n = 10) of tofersen or placebo (n = 12).
Patients received tofersen by intrathecal bolus over 1-3 minutes. They received a loading regimen on days 1, 15, and 29 and maintenance dosing on days 57 and 85. After the dosing period, patients completed a 12-week follow-up period.
Adverse events
All patients received at least one dose of the study treatment, and 48 received all treatments. Three patients died during the study. One patient in the 20-mg group died of pulmonary embolism, and one patient in both the 60-mg group and placebo group died of respiratory failure. Investigators considered the deaths secondary to ALS or other conditions and not drug related.
Most adverse events were mild or moderate. The most common adverse events among tofersen-treated patients were headache (n = 16), procedural pain (n = 14), and post–lumbar puncture syndrome (n = 13). Five patients who received tofersen and two who received placebo experienced serious adverse events; no serious adverse events occurred in the 100-mg dose group.
“A reduction from baseline in CSF SOD1 concentrations was observed in the tofersen 40-, 60-, and 100-mg cohorts with the maximal reduction observed in the 100 mg–treated group [37% vs. no reduction in the placebo group; P less than 0.002] at day 85,” the investigators reported.
Possible efficacy
In exploratory analyses, the 100-mg dose slowed decline on the Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised (ASLFRS-R), compared with placebo. Mean change in ASLFRS-R from baseline to day 85 was –1.1 in patients who received 100 mg of tofersen, compared with –5.3 for patients who received placebo. Declines on measures of respiratory function and muscle strength also slowed. “Across clinical measures, separation from placebo was most apparent in participants with fast progressing disease,” the researchers said.
“Lower concentrations of the protein in the spinal fluid suggest that there were also lower concentrations in the brain and spinal cord,” Dr. Miller said in a news release. “Such reductions could lead to preservation of motor neurons and slow progression of the disease, but more study is needed to examine this further.”
The study was sponsored by Biogen, which is developing tofersen. Some of the study authors are Biogen employees. Dr. Miller is on Biogen’s medical advisory board and receives clinical research support from Biogen. In addition, he consults, has licensing agreements with, and is a principal investigator for other companies.
PHILADELPHIA – In patients with amyotrophic lateral sclerosis (ALS) caused by gain-of-toxic function mutations in the SOD1 gene, according to phase 1/2 trial results presented at the annual meeting of the American Academy of Neurology. Exploratory analyses suggest that the drug, known as tofersen (also known as BIIB067), may lessen declines in function, respiratory function, and strength. The treatment generally was safe and well tolerated, researchers said.
Most ALS cases are sporadic, but about 10% are genetic, of which approximately 20% are caused by SOD1 mutations. “Although SOD1-ALS disease progression is heterogeneous, the underlying pathophysiology, attributable to mutant SOD1 toxicity, is thought to be consistent across SOD1 mutation types,” said Timothy M. Miller, MD, PhD, of Washington University, St. Louis, and colleagues. “As such, effective reduction of SOD1 protein, irrespective of mutation, has the potential to alter the disease course of people with SOD1-ALS.”
Tofersen is an antisense oligonucleotide ribonuclease H1-mediated inhibitor of SOD1 messenger RNA. To study its safety, tolerability, pharmacokinetics, pharmacodynamics, and exploratory efficacy in patients with SOD1-ALS, investigators conducted a double-blind study. The investigators randomized 50 patients with ALS with a SOD1 mutation to 20 mg (n = 10), 40 mg (n = 9), 60 mg (n = 9), or 100 mg (n = 10) of tofersen or placebo (n = 12).
Patients received tofersen by intrathecal bolus over 1-3 minutes. They received a loading regimen on days 1, 15, and 29 and maintenance dosing on days 57 and 85. After the dosing period, patients completed a 12-week follow-up period.
Adverse events
All patients received at least one dose of the study treatment, and 48 received all treatments. Three patients died during the study. One patient in the 20-mg group died of pulmonary embolism, and one patient in both the 60-mg group and placebo group died of respiratory failure. Investigators considered the deaths secondary to ALS or other conditions and not drug related.
Most adverse events were mild or moderate. The most common adverse events among tofersen-treated patients were headache (n = 16), procedural pain (n = 14), and post–lumbar puncture syndrome (n = 13). Five patients who received tofersen and two who received placebo experienced serious adverse events; no serious adverse events occurred in the 100-mg dose group.
“A reduction from baseline in CSF SOD1 concentrations was observed in the tofersen 40-, 60-, and 100-mg cohorts with the maximal reduction observed in the 100 mg–treated group [37% vs. no reduction in the placebo group; P less than 0.002] at day 85,” the investigators reported.
Possible efficacy
In exploratory analyses, the 100-mg dose slowed decline on the Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised (ASLFRS-R), compared with placebo. Mean change in ASLFRS-R from baseline to day 85 was –1.1 in patients who received 100 mg of tofersen, compared with –5.3 for patients who received placebo. Declines on measures of respiratory function and muscle strength also slowed. “Across clinical measures, separation from placebo was most apparent in participants with fast progressing disease,” the researchers said.
“Lower concentrations of the protein in the spinal fluid suggest that there were also lower concentrations in the brain and spinal cord,” Dr. Miller said in a news release. “Such reductions could lead to preservation of motor neurons and slow progression of the disease, but more study is needed to examine this further.”
The study was sponsored by Biogen, which is developing tofersen. Some of the study authors are Biogen employees. Dr. Miller is on Biogen’s medical advisory board and receives clinical research support from Biogen. In addition, he consults, has licensing agreements with, and is a principal investigator for other companies.
REPORTING FROM AAN 2019
Females with acne stay on spironolactone longer than antibiotics in real-world usage study
according to a retrospective study of women with acne published in the Journal of the American Academy of Dermatology.
Among those treated for at least a year, patients continued spironolactone for about 90 days longer on average, than those on antibiotic therapy, reported John S. Barbieri, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and associates. “The extended drug usage survival of spironolactone suggests that, in routine clinical practice, spironolactone may have good long-term effectiveness and tolerability,” they wrote. “Since female patients often have persistent acne into adulthood and given concerns regarding antibiotic overuse among acne patients, it is possible that using spironolactone as a first-line agent before oral antibiotics could improve outcomes for female patients with acne,” they added.
In the study, they pointed out that spironolactone is emerging as a possible alternative to oral antibiotic therapy, but “little is known about long-term outcomes with spironolactone for those who have an initial positive response and how it compares to other alternatives.”
To examine the duration of acne treatment with spironolactone versus oral antibiotics, the researchers analyzed data during 2010-2016 in the Optum Clinformatics Data Mart. They included data on female patients aged 12-40 years, with at least two diagnosis codes for acne, who received spironolactone or oral antibiotics for at least 12 months. They used multivariate Cox proportional hazard models to assess differences in duration of therapy for spironolactone, compared with oral antibiotics.
The mean duration of a treatment course was significantly longer among the 4,321 patients treated with spironolactone than among the 7,517 patients treated with oral tetracycline-class antibiotics (697.8 days vs. 604.4 days; P less than .001). Compared with treatment with oral tetracyclines, the hazard ratio for discontinuing spironolactone treatment was 0.74, after researchers controlled for the age at diagnosis and treatment, history of polycystic ovarian syndrome, and history of combined oral contraceptive or topical retinoid treatment.
Patients who receive spironolactone and patients who receive oral antibiotics may represent different populations, the authors noted. In addition, guidelines advise limiting antibiotic treatment to 3-6 months, and antibiotic discontinuations may have been related to these recommendations. “It is not possible to determine whether medication discontinuation occurred due to lack of efficacy, cost, side effects, resolution of acne, or other factors,” they said, adding that prospective studies are needed “to identify the optimal treatment approaches for female patients with moderate to severe acne.”
The study was funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Barbieri is supported by NIAMS and receives partial salary support through a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania.
SOURCE: Barbieri JS et al. J Am Acad Dermatol. 2019 Mar 21. doi: 10.1016/j.jaad.2019.03.036.
according to a retrospective study of women with acne published in the Journal of the American Academy of Dermatology.
Among those treated for at least a year, patients continued spironolactone for about 90 days longer on average, than those on antibiotic therapy, reported John S. Barbieri, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and associates. “The extended drug usage survival of spironolactone suggests that, in routine clinical practice, spironolactone may have good long-term effectiveness and tolerability,” they wrote. “Since female patients often have persistent acne into adulthood and given concerns regarding antibiotic overuse among acne patients, it is possible that using spironolactone as a first-line agent before oral antibiotics could improve outcomes for female patients with acne,” they added.
In the study, they pointed out that spironolactone is emerging as a possible alternative to oral antibiotic therapy, but “little is known about long-term outcomes with spironolactone for those who have an initial positive response and how it compares to other alternatives.”
To examine the duration of acne treatment with spironolactone versus oral antibiotics, the researchers analyzed data during 2010-2016 in the Optum Clinformatics Data Mart. They included data on female patients aged 12-40 years, with at least two diagnosis codes for acne, who received spironolactone or oral antibiotics for at least 12 months. They used multivariate Cox proportional hazard models to assess differences in duration of therapy for spironolactone, compared with oral antibiotics.
The mean duration of a treatment course was significantly longer among the 4,321 patients treated with spironolactone than among the 7,517 patients treated with oral tetracycline-class antibiotics (697.8 days vs. 604.4 days; P less than .001). Compared with treatment with oral tetracyclines, the hazard ratio for discontinuing spironolactone treatment was 0.74, after researchers controlled for the age at diagnosis and treatment, history of polycystic ovarian syndrome, and history of combined oral contraceptive or topical retinoid treatment.
Patients who receive spironolactone and patients who receive oral antibiotics may represent different populations, the authors noted. In addition, guidelines advise limiting antibiotic treatment to 3-6 months, and antibiotic discontinuations may have been related to these recommendations. “It is not possible to determine whether medication discontinuation occurred due to lack of efficacy, cost, side effects, resolution of acne, or other factors,” they said, adding that prospective studies are needed “to identify the optimal treatment approaches for female patients with moderate to severe acne.”
The study was funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Barbieri is supported by NIAMS and receives partial salary support through a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania.
SOURCE: Barbieri JS et al. J Am Acad Dermatol. 2019 Mar 21. doi: 10.1016/j.jaad.2019.03.036.
according to a retrospective study of women with acne published in the Journal of the American Academy of Dermatology.
Among those treated for at least a year, patients continued spironolactone for about 90 days longer on average, than those on antibiotic therapy, reported John S. Barbieri, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and associates. “The extended drug usage survival of spironolactone suggests that, in routine clinical practice, spironolactone may have good long-term effectiveness and tolerability,” they wrote. “Since female patients often have persistent acne into adulthood and given concerns regarding antibiotic overuse among acne patients, it is possible that using spironolactone as a first-line agent before oral antibiotics could improve outcomes for female patients with acne,” they added.
In the study, they pointed out that spironolactone is emerging as a possible alternative to oral antibiotic therapy, but “little is known about long-term outcomes with spironolactone for those who have an initial positive response and how it compares to other alternatives.”
To examine the duration of acne treatment with spironolactone versus oral antibiotics, the researchers analyzed data during 2010-2016 in the Optum Clinformatics Data Mart. They included data on female patients aged 12-40 years, with at least two diagnosis codes for acne, who received spironolactone or oral antibiotics for at least 12 months. They used multivariate Cox proportional hazard models to assess differences in duration of therapy for spironolactone, compared with oral antibiotics.
The mean duration of a treatment course was significantly longer among the 4,321 patients treated with spironolactone than among the 7,517 patients treated with oral tetracycline-class antibiotics (697.8 days vs. 604.4 days; P less than .001). Compared with treatment with oral tetracyclines, the hazard ratio for discontinuing spironolactone treatment was 0.74, after researchers controlled for the age at diagnosis and treatment, history of polycystic ovarian syndrome, and history of combined oral contraceptive or topical retinoid treatment.
Patients who receive spironolactone and patients who receive oral antibiotics may represent different populations, the authors noted. In addition, guidelines advise limiting antibiotic treatment to 3-6 months, and antibiotic discontinuations may have been related to these recommendations. “It is not possible to determine whether medication discontinuation occurred due to lack of efficacy, cost, side effects, resolution of acne, or other factors,” they said, adding that prospective studies are needed “to identify the optimal treatment approaches for female patients with moderate to severe acne.”
The study was funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Barbieri is supported by NIAMS and receives partial salary support through a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania.
SOURCE: Barbieri JS et al. J Am Acad Dermatol. 2019 Mar 21. doi: 10.1016/j.jaad.2019.03.036.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
The art of selecting an MS therapy
DALLAS – , said Mark Freedman, MD, MSc, in a presentation at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Right now, we are probably dealing with more of an imprecise medicine,” said Dr. Freedman.
Information such as a patient’s ability to recover from relapses may indicate MS severity or the likelihood of disease progression, but selecting a therapy remains “an art of medicine,” said Dr. Freedman, professor of neurology at the University of Ottawa, director of the multiple sclerosis research unit at Ottawa Hospital, and senior scientist at the Ottawa Hospital Research Institute.
When prescribing a DMT, neurologists tend to consider three key elements: the disease, the treatment, and patient expectations. “Focus on these three aspects,” Dr. Freedman said.
It is no longer sufficient for neurologists to diagnose MS, hand the patient a drug, and “expect that things are going to go the way you want them to go,” he said.
Immunomodulating, anti–cell trafficking, or cell-depleting therapy?
Genetics, sex, types of relapses, recovery from relapses, response to therapy, MRI burden, and other biomarkers such as oligoclonal bands and neurofilaments may indicate which patients have severe disease and should receive aggressive treatment.
Determining the phase of the disease is a crucial first step “that is going to drive your choice of therapy,” he said.
Dr. Freedman likened the development of progressive MS to approaching the edge of a cliff. If patients appear to be nearing the progressive phase, “then your choice of therapy has to be an aggressive one – one that will hopefully hold them back from falling,” he said. In the earlier phases of MS, on the other hand, “you are looking at a long-term treatment that should probably be safe and still able to contain the disease,” such as an immunomodulator. If a patient is “about to fall off, you may want to go for temporary use of an antitrafficker to control things, and then eventually deplete the cells that are going to be causing the patient to fall off the cliff.”
Prognostic factors
Disease activity over time, and whether the disease is progressing faster or slower than would be expected, may be important prognostic factors. A patient’s sex also may be a factor because women tend to have more attacks and to have their attacks at a younger age, Dr. Freedman said.
The types of relapses and a patient’s ability to recover from them may provide important information. “Some attacks are quite mild. Others tend to build up disease,” Dr. Freedman said. “Some people are better healers than others. We have all seen people who have been quadriplegic in an ICU on a ventilator walk out of the hospital without even a numb toe. And other people who have a little bit of weakness in one leg seem to never be able to recover from that. Exactly what drives repair is still not clear.” Most patients do recover, however, “and the inability to recover early on is a bad omen,” Dr. Freedman said.
When researchers examined the relationship between functional components of the Expanded Disability Status Scale (EDSS) and disability progression, “not surprisingly ... pyramidal and spinal cord and cerebellar [functioning] are more associated with earlier progression” (Neuroepidemiology. 2015;44[1]:16-23).
A study by Lublin et al. found that patients with MS whose attacks left them with residual deficits had more EDSS accumulation over time (Neurology. 2003 Dec 9;61[11]:1528-32.).
Response to immunomodulators
“The inability to control the disease with an immunomodulator is a bad sign,” Dr. Freedman said. He pointed to data from a trial of teriflunomide that included patients who had had suboptimal responses to first-line therapy as well as patients who were treatment naive (Mult Scler. 2018 Apr;24[4]:535-9.). Some of the patients who had received prior MS therapy were randomized to placebo, which “is not something that would happen today,” he said.
“If you just focus on the [patients who received placebo] and look at the rate of attack in patients who had no prior DMT, at least one prior DMT, or two or more prior DMTs, the attack rates are much higher in those individuals who tried and failed first-line therapies,” Dr. Freedman said. These patients also had more EDSS progression. “The majority of people do respond [to first-line treatment], but those who do not you need to worry about a little bit more than those who do respond.”
MRI lesions and brain reserve
MRI activity over time tends to predict disease progression, and lesion location is important. One cohort study found that the likelihood of developing secondary progressive MS was lower among patients who did not develop new spinal cord or brainstem lesions in the first three years of the disease, compared with those who did.
In addition, patients who presented with more lesions were more likely to reach an EDSS score 3 or 6 over 10 years (Brain. 2008 Mar;131[Pt 3]:808-17.).
Brain reserve also may be important. Among 52 treatment-naive Serbian adults with MS, Sumowski et al. found that maximal lifetime brain growth as estimated with intracranial volume was associated with risk of disability progression over 5 years (Neurology. 2016 May 24;86[21]:2006-9.). “Those who had a greater reserve had a much lower risk of disease progression,” Dr. Freedman said. The results suggest that patients with more brain reserve may be better able to sustain damage as the disease progresses and they age, he said.
Comorbidities
In the past, neurologists may have left it up to general practitioners “to sort out the rest of the patient’s health,” Dr. Freedman said. “But we now recognize that having certain comorbidities already puts a higher burden onto the disease. And those patients who have more comorbidities ... are going to do worse. But not only are they going to do worse ... it turns out that patients who have more comorbidities are going to have less of a response to your various therapies.” Vascular comorbidities, in particular, may affect treatment response (Neurology. 2017 Nov 28;89[22]:2222-9.).
If hypertension or diabetes clinics can help control those conditions in patients with MS, “it will help us a lot in getting what we are expecting from the [MS] medications,” Dr. Freedman said.
Adherence, expectations, and symptomatic treatment
Ultimately, selecting an MS therapy is a decision that doctors share with their patients. “You’re going to have a discussion with them,” he said. “You can see what fits their lifestyle.” For example, a world traveler might not be a good candidate for a drug that requires regular monitoring. A patient’s risk averseness also may influence treatment choice.
If you involve patients in the selection process, it may improve medication adherence. In addition, patients need to understand what you aim to accomplish with a DMT, said Dr. Freedman. “That may sound like a trivial thing. But how many times has the patient come in and said, ‘The drug is not working. ... My eye is not better’” when that was not the goal of treatment to begin with. Let patients know that symptomatic treatments may address problems apart from MS DMT. This personalized but imprecise approach to treatment is “probably the best we can do for now,” Dr. Freedman said.
Dr. Freedman has received a research grant from Genzyme and is on the company’s speakers bureau. He has received honoraria and consulting fees from various pharmaceutical companies and serves on companies’ advisory boards.
SOURCE: Freedman MS. ACTRIMS Forum 2019, Session 2.
DALLAS – , said Mark Freedman, MD, MSc, in a presentation at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Right now, we are probably dealing with more of an imprecise medicine,” said Dr. Freedman.
Information such as a patient’s ability to recover from relapses may indicate MS severity or the likelihood of disease progression, but selecting a therapy remains “an art of medicine,” said Dr. Freedman, professor of neurology at the University of Ottawa, director of the multiple sclerosis research unit at Ottawa Hospital, and senior scientist at the Ottawa Hospital Research Institute.
When prescribing a DMT, neurologists tend to consider three key elements: the disease, the treatment, and patient expectations. “Focus on these three aspects,” Dr. Freedman said.
It is no longer sufficient for neurologists to diagnose MS, hand the patient a drug, and “expect that things are going to go the way you want them to go,” he said.
Immunomodulating, anti–cell trafficking, or cell-depleting therapy?
Genetics, sex, types of relapses, recovery from relapses, response to therapy, MRI burden, and other biomarkers such as oligoclonal bands and neurofilaments may indicate which patients have severe disease and should receive aggressive treatment.
Determining the phase of the disease is a crucial first step “that is going to drive your choice of therapy,” he said.
Dr. Freedman likened the development of progressive MS to approaching the edge of a cliff. If patients appear to be nearing the progressive phase, “then your choice of therapy has to be an aggressive one – one that will hopefully hold them back from falling,” he said. In the earlier phases of MS, on the other hand, “you are looking at a long-term treatment that should probably be safe and still able to contain the disease,” such as an immunomodulator. If a patient is “about to fall off, you may want to go for temporary use of an antitrafficker to control things, and then eventually deplete the cells that are going to be causing the patient to fall off the cliff.”
Prognostic factors
Disease activity over time, and whether the disease is progressing faster or slower than would be expected, may be important prognostic factors. A patient’s sex also may be a factor because women tend to have more attacks and to have their attacks at a younger age, Dr. Freedman said.
The types of relapses and a patient’s ability to recover from them may provide important information. “Some attacks are quite mild. Others tend to build up disease,” Dr. Freedman said. “Some people are better healers than others. We have all seen people who have been quadriplegic in an ICU on a ventilator walk out of the hospital without even a numb toe. And other people who have a little bit of weakness in one leg seem to never be able to recover from that. Exactly what drives repair is still not clear.” Most patients do recover, however, “and the inability to recover early on is a bad omen,” Dr. Freedman said.
When researchers examined the relationship between functional components of the Expanded Disability Status Scale (EDSS) and disability progression, “not surprisingly ... pyramidal and spinal cord and cerebellar [functioning] are more associated with earlier progression” (Neuroepidemiology. 2015;44[1]:16-23).
A study by Lublin et al. found that patients with MS whose attacks left them with residual deficits had more EDSS accumulation over time (Neurology. 2003 Dec 9;61[11]:1528-32.).
Response to immunomodulators
“The inability to control the disease with an immunomodulator is a bad sign,” Dr. Freedman said. He pointed to data from a trial of teriflunomide that included patients who had had suboptimal responses to first-line therapy as well as patients who were treatment naive (Mult Scler. 2018 Apr;24[4]:535-9.). Some of the patients who had received prior MS therapy were randomized to placebo, which “is not something that would happen today,” he said.
“If you just focus on the [patients who received placebo] and look at the rate of attack in patients who had no prior DMT, at least one prior DMT, or two or more prior DMTs, the attack rates are much higher in those individuals who tried and failed first-line therapies,” Dr. Freedman said. These patients also had more EDSS progression. “The majority of people do respond [to first-line treatment], but those who do not you need to worry about a little bit more than those who do respond.”
MRI lesions and brain reserve
MRI activity over time tends to predict disease progression, and lesion location is important. One cohort study found that the likelihood of developing secondary progressive MS was lower among patients who did not develop new spinal cord or brainstem lesions in the first three years of the disease, compared with those who did.
In addition, patients who presented with more lesions were more likely to reach an EDSS score 3 or 6 over 10 years (Brain. 2008 Mar;131[Pt 3]:808-17.).
Brain reserve also may be important. Among 52 treatment-naive Serbian adults with MS, Sumowski et al. found that maximal lifetime brain growth as estimated with intracranial volume was associated with risk of disability progression over 5 years (Neurology. 2016 May 24;86[21]:2006-9.). “Those who had a greater reserve had a much lower risk of disease progression,” Dr. Freedman said. The results suggest that patients with more brain reserve may be better able to sustain damage as the disease progresses and they age, he said.
Comorbidities
In the past, neurologists may have left it up to general practitioners “to sort out the rest of the patient’s health,” Dr. Freedman said. “But we now recognize that having certain comorbidities already puts a higher burden onto the disease. And those patients who have more comorbidities ... are going to do worse. But not only are they going to do worse ... it turns out that patients who have more comorbidities are going to have less of a response to your various therapies.” Vascular comorbidities, in particular, may affect treatment response (Neurology. 2017 Nov 28;89[22]:2222-9.).
If hypertension or diabetes clinics can help control those conditions in patients with MS, “it will help us a lot in getting what we are expecting from the [MS] medications,” Dr. Freedman said.
Adherence, expectations, and symptomatic treatment
Ultimately, selecting an MS therapy is a decision that doctors share with their patients. “You’re going to have a discussion with them,” he said. “You can see what fits their lifestyle.” For example, a world traveler might not be a good candidate for a drug that requires regular monitoring. A patient’s risk averseness also may influence treatment choice.
If you involve patients in the selection process, it may improve medication adherence. In addition, patients need to understand what you aim to accomplish with a DMT, said Dr. Freedman. “That may sound like a trivial thing. But how many times has the patient come in and said, ‘The drug is not working. ... My eye is not better’” when that was not the goal of treatment to begin with. Let patients know that symptomatic treatments may address problems apart from MS DMT. This personalized but imprecise approach to treatment is “probably the best we can do for now,” Dr. Freedman said.
Dr. Freedman has received a research grant from Genzyme and is on the company’s speakers bureau. He has received honoraria and consulting fees from various pharmaceutical companies and serves on companies’ advisory boards.
SOURCE: Freedman MS. ACTRIMS Forum 2019, Session 2.
DALLAS – , said Mark Freedman, MD, MSc, in a presentation at ACTRIMS Forum 2019, the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “Right now, we are probably dealing with more of an imprecise medicine,” said Dr. Freedman.
Information such as a patient’s ability to recover from relapses may indicate MS severity or the likelihood of disease progression, but selecting a therapy remains “an art of medicine,” said Dr. Freedman, professor of neurology at the University of Ottawa, director of the multiple sclerosis research unit at Ottawa Hospital, and senior scientist at the Ottawa Hospital Research Institute.
When prescribing a DMT, neurologists tend to consider three key elements: the disease, the treatment, and patient expectations. “Focus on these three aspects,” Dr. Freedman said.
It is no longer sufficient for neurologists to diagnose MS, hand the patient a drug, and “expect that things are going to go the way you want them to go,” he said.
Immunomodulating, anti–cell trafficking, or cell-depleting therapy?
Genetics, sex, types of relapses, recovery from relapses, response to therapy, MRI burden, and other biomarkers such as oligoclonal bands and neurofilaments may indicate which patients have severe disease and should receive aggressive treatment.
Determining the phase of the disease is a crucial first step “that is going to drive your choice of therapy,” he said.
Dr. Freedman likened the development of progressive MS to approaching the edge of a cliff. If patients appear to be nearing the progressive phase, “then your choice of therapy has to be an aggressive one – one that will hopefully hold them back from falling,” he said. In the earlier phases of MS, on the other hand, “you are looking at a long-term treatment that should probably be safe and still able to contain the disease,” such as an immunomodulator. If a patient is “about to fall off, you may want to go for temporary use of an antitrafficker to control things, and then eventually deplete the cells that are going to be causing the patient to fall off the cliff.”
Prognostic factors
Disease activity over time, and whether the disease is progressing faster or slower than would be expected, may be important prognostic factors. A patient’s sex also may be a factor because women tend to have more attacks and to have their attacks at a younger age, Dr. Freedman said.
The types of relapses and a patient’s ability to recover from them may provide important information. “Some attacks are quite mild. Others tend to build up disease,” Dr. Freedman said. “Some people are better healers than others. We have all seen people who have been quadriplegic in an ICU on a ventilator walk out of the hospital without even a numb toe. And other people who have a little bit of weakness in one leg seem to never be able to recover from that. Exactly what drives repair is still not clear.” Most patients do recover, however, “and the inability to recover early on is a bad omen,” Dr. Freedman said.
When researchers examined the relationship between functional components of the Expanded Disability Status Scale (EDSS) and disability progression, “not surprisingly ... pyramidal and spinal cord and cerebellar [functioning] are more associated with earlier progression” (Neuroepidemiology. 2015;44[1]:16-23).
A study by Lublin et al. found that patients with MS whose attacks left them with residual deficits had more EDSS accumulation over time (Neurology. 2003 Dec 9;61[11]:1528-32.).
Response to immunomodulators
“The inability to control the disease with an immunomodulator is a bad sign,” Dr. Freedman said. He pointed to data from a trial of teriflunomide that included patients who had had suboptimal responses to first-line therapy as well as patients who were treatment naive (Mult Scler. 2018 Apr;24[4]:535-9.). Some of the patients who had received prior MS therapy were randomized to placebo, which “is not something that would happen today,” he said.
“If you just focus on the [patients who received placebo] and look at the rate of attack in patients who had no prior DMT, at least one prior DMT, or two or more prior DMTs, the attack rates are much higher in those individuals who tried and failed first-line therapies,” Dr. Freedman said. These patients also had more EDSS progression. “The majority of people do respond [to first-line treatment], but those who do not you need to worry about a little bit more than those who do respond.”
MRI lesions and brain reserve
MRI activity over time tends to predict disease progression, and lesion location is important. One cohort study found that the likelihood of developing secondary progressive MS was lower among patients who did not develop new spinal cord or brainstem lesions in the first three years of the disease, compared with those who did.
In addition, patients who presented with more lesions were more likely to reach an EDSS score 3 or 6 over 10 years (Brain. 2008 Mar;131[Pt 3]:808-17.).
Brain reserve also may be important. Among 52 treatment-naive Serbian adults with MS, Sumowski et al. found that maximal lifetime brain growth as estimated with intracranial volume was associated with risk of disability progression over 5 years (Neurology. 2016 May 24;86[21]:2006-9.). “Those who had a greater reserve had a much lower risk of disease progression,” Dr. Freedman said. The results suggest that patients with more brain reserve may be better able to sustain damage as the disease progresses and they age, he said.
Comorbidities
In the past, neurologists may have left it up to general practitioners “to sort out the rest of the patient’s health,” Dr. Freedman said. “But we now recognize that having certain comorbidities already puts a higher burden onto the disease. And those patients who have more comorbidities ... are going to do worse. But not only are they going to do worse ... it turns out that patients who have more comorbidities are going to have less of a response to your various therapies.” Vascular comorbidities, in particular, may affect treatment response (Neurology. 2017 Nov 28;89[22]:2222-9.).
If hypertension or diabetes clinics can help control those conditions in patients with MS, “it will help us a lot in getting what we are expecting from the [MS] medications,” Dr. Freedman said.
Adherence, expectations, and symptomatic treatment
Ultimately, selecting an MS therapy is a decision that doctors share with their patients. “You’re going to have a discussion with them,” he said. “You can see what fits their lifestyle.” For example, a world traveler might not be a good candidate for a drug that requires regular monitoring. A patient’s risk averseness also may influence treatment choice.
If you involve patients in the selection process, it may improve medication adherence. In addition, patients need to understand what you aim to accomplish with a DMT, said Dr. Freedman. “That may sound like a trivial thing. But how many times has the patient come in and said, ‘The drug is not working. ... My eye is not better’” when that was not the goal of treatment to begin with. Let patients know that symptomatic treatments may address problems apart from MS DMT. This personalized but imprecise approach to treatment is “probably the best we can do for now,” Dr. Freedman said.
Dr. Freedman has received a research grant from Genzyme and is on the company’s speakers bureau. He has received honoraria and consulting fees from various pharmaceutical companies and serves on companies’ advisory boards.
SOURCE: Freedman MS. ACTRIMS Forum 2019, Session 2.
EXPERT ANALYSIS FROM ACTRIMS
Guideline issued for treating Tourette syndrome and chronic tics
PHILADELPHIA – Approaches to managing tics in patients with Tourette syndrome or chronic tic disorders “should be individualized, and the choice should be the result of a collaborative decision among patient, caregiver, and clinician, during which the benefits and harms of individual treatments as well as the presence of comorbid disorders are considered,” according to Tamara Pringsheim, MD, lead author of a practice guideline published May 6, 2019, by the American Academy of Neurology, and her collaborators.
The panel of nine physicians, two psychologists, and two patient representatives developed the recommendations based on a comprehensive systematic literature review. They concluded that treatments may decrease the frequency and severity of tics but rarely eliminate them.
The guideline was endorsed by the Child Neurology Society and the European Academy of Neurology and is the first such guideline for American neurologists, said Dr. Pringsheim of the University of Calgary (Alta.). Like recent Canadian and European guidelines, it strongly supports the Comprehensive Behavioral Intervention for Tics (CBIT) as a treatment option for tics.
After examining which medical, behavioral, and neurostimulation interventions, compared with placebo or other active interventions, improve tic severity and tic-related impairment in children and adults with Tourette syndrome or a chronic tic disorder, the guideline writers recommended that the evidence was strongest for CBIT as a first-line treatment, relative to other behavioral treatments and medications.
If symptoms affect a patient’s daily life, doctors should consider CBIT, said guideline author John Piacentini, PhD, of the University of California, Los Angeles, at the annual meeting of the American Academy of Neurology. “This treatment combines habit-reversal training, which teaches patients how to control their urges to tic, with other behavioral strategies to reduce stress and other factors that often make tics worse.”
Patients typically see results from CBIT in 8-12 weeks. More CBIT providers are needed, however, to make the treatment readily available to all patients, he said.
The guideline panel members said that there was moderate confidence in the evidence for reduced tic severity for the following therapeutic approaches, compared with placebo: haloperidol, risperidone, aripiprazole (children only), tiapride (children only), clonidine, onabotulinumtoxinA injections, ningdong granule (as formulated by Zhao), (children only), and ling granule (children only). There was low or very low confidence in the evidence for all other therapies for reducing tic severity.
Comorbid conditions
Many people with tic disorders have neurodevelopmental or psychiatric conditions such as ADHD, obsessive-compulsive disorder, and mood and anxiety disorders. The guideline recommends that people with tics be evaluated for these conditions.
Alpha2-adrenergic agonists may improve symptoms of tic disorders and ADHD, the authors said. There was moderate confidence in the evidence for reduced tic severity for people with a comorbid diagnosis of ADHD with clonidine plus methylphenidate (children only) and methylphenidate alone (children only), compared with placebo.
Adults with severe Tourette syndrome who are resistant to medical and behavioral therapy may benefit from deep brain stimulation (DBS), the guideline states. There was moderate confidence in the evidence for reduced tic severity for DBS of the globus pallidus, compared with sham DBS, as an option for adults with severe tics who have failed CBIT and drugs. These patients first must be screened by a mental health professional and continue to be monitored throughout DBS treatment.
Adults with Tourette syndrome who self-treat their tics with cannabis in states where cannabis is legal should see a doctor who can monitor the use of cannabis for efficacy and adverse effects, the guideline says.
Adverse effects of therapy
The panel also examined the risks of harm, including weight gain, elevated prolactin levels, sedation, drug-induced movement disorders, hypotension, bradycardia, and ECG changes with medical treatments, compared with placebo or other active interventions. In regard to weight gain, the panel concluded with moderate confidence that people with tics receiving risperidone or aripiprazole (children only) are probably more likely to gain weight than people receiving placebo. There was low confidence for associations between specific therapies and elevated prolactin levels.
Compared with people receiving placebo, there was moderate confidence that tiapride is probably associated with higher rates of physical tiredness and sleep disturbances (children only), that clonidine is probably associated with sedation, and that guanfacine is probably associated with drowsiness (children only). There was moderate evidence that pimozide is probably associated with extrapyramidal symptoms. There was low confidence that any specific treatment led to hypotension, bradycardia, or ECG changes.
Additional guideline specifics
The guideline’s practice recommendations include explaining the natural history of tic disorders to patients and caregivers and evaluating patients for functional impairment. Watchful waiting is an acceptable approach in people who do not experience functional impairment, and patients receiving medications for tics must have periodic reevaluations for the need for ongoing medical treatment. People with Tourette syndrome should be referred to resources for psychoeducation for teachers and peers, such as the Tourette Association of America.
Comorbid ADHD occurs in 30%-50% of patients with tics. If screening for ADHD is positive, the burden of ADHD symptoms should be assessed and those with functionally impairing ADHD should be treated for the disorder. Similarly, obsessive-compulsive behaviors occur in 10%-50% of those with Tourette syndrome. If an assessment finds comorbid obsessive-compulsive disorder, it should be treated.
Other psychiatric comorbidities with Tourette syndrome include anxiety disorders, oppositional defiant disorder, and mood disorders. When screening for these conditions, one must inquire about suicidal thoughts and suicide attempts and refer to appropriate resources if present, according to the guidelines.
Individuals with tics and comorbid ADHD should be advised that alpha2-adrenergic agonists may provide benefit for both conditions. Alpha2-adrenergic agonists should be prescribed for the treatment of tics when the benefits of treatment outweigh the risks and patients must be counseled regarding common side effects of alpha2-adrenergic agonists, including sedation. Heart rate and blood pressure must be monitored in patients with tics treated with alpha2-adrenergic agonists. If prescribing extended-release guanfacine, one must monitor the QTc interval in patients with a history of cardiac conditions, patients taking other QT-prolonging agents, or patients with a family history of long QT syndrome. If discontinuing alpha2-adrenergic agonists, they must gradually be tapered to avoid rebound hypertension.
If considering antipsychotic therapies, patients must be counseled on the relative risk for extrapyramidal, hormonal, and metabolic adverse effects to inform decision making on which antipsychotic should be prescribed. Before prescribing antipsychotics for tics, ECGs must be performed. The QTc interval must be measured before and after starting pimozide or ziprasidone, or if antipsychotics are coadministered with other drugs that can prolong the QT interval. The lowest effective dose should be prescribed to decrease the risk of adverse effects, and patients should be monitored for drug-induced movement disorders and for metabolic and hormonal adverse effects of antipsychotics. When attempting to discontinue antipsychotics for tics, the medications should be gradually tapered over weeks to months to avoid withdrawal dyskinesias.
If topiramate is prescribed, patients must be counseled regarding common adverse effects, including cognitive and language problems, somnolence, weight loss, and an increased risk of renal stones.
Some patients with Tourette syndrome use cannabis as a self-medication for tics and comorbidities. Because of the risks associated with cannabis use and widespread self-medication with cannabis for tics, where regional legislation and resources allow, physicians must offer to direct patients to appropriate medical supervision when cannabis is used as self-medication for tics. Appropriate medical supervision would entail education and monitoring for efficacy and adverse effects, according to the guidelines.
Where regional legislation allows, physicians prescribing cannabis-based medication must prescribe the lowest effective dose to decrease the risk of adverse effects. Physicians prescribing cannabis-based medication must inform patients that medication may impair driving ability. Physicians prescribing cannabis-based medication to patients with Tourette syndrome must periodically reevaluate the need for ongoing treatment.
A multidisciplinary evaluation is needed to establish when the benefits of treatment outweigh the risks for prescribing DBS for medication-resistant motor and phonic tics. The DSM-5 diagnosis of Tourette syndrome must be confirmed and exclude secondary and functional tic-like movements when considering DBS for medication-resistant tics. A mental health professional must screen patients preoperatively and follow patients postoperatively for psychiatric disorders that may impede the long-term success of the therapy. Physicians must confirm that multiple classes of medication (antipsychotics, dopamine depleters, alpha1 agonists) and behavioral therapy have been administered (or are contraindicated) before prescribing DBS for tics.
The practice guideline was developed with financial support from AAN. Dr. Pringsheim reported no disclosures. Dr. Piacentini reported receiving funding for travel and speaking from foundations and universities and has received royalties from publishers. In addition, he has performed behavior therapy for tics for approximately 50% of his clinical time and has received financial or material support from Pfizer, the National Institute of Mental Health, and foundations.
SOURCE: Pringsheim T et al. Neurology. 2019 May 6. doi: 10.1212/WNL.0000000000007466.
PHILADELPHIA – Approaches to managing tics in patients with Tourette syndrome or chronic tic disorders “should be individualized, and the choice should be the result of a collaborative decision among patient, caregiver, and clinician, during which the benefits and harms of individual treatments as well as the presence of comorbid disorders are considered,” according to Tamara Pringsheim, MD, lead author of a practice guideline published May 6, 2019, by the American Academy of Neurology, and her collaborators.
The panel of nine physicians, two psychologists, and two patient representatives developed the recommendations based on a comprehensive systematic literature review. They concluded that treatments may decrease the frequency and severity of tics but rarely eliminate them.
The guideline was endorsed by the Child Neurology Society and the European Academy of Neurology and is the first such guideline for American neurologists, said Dr. Pringsheim of the University of Calgary (Alta.). Like recent Canadian and European guidelines, it strongly supports the Comprehensive Behavioral Intervention for Tics (CBIT) as a treatment option for tics.
After examining which medical, behavioral, and neurostimulation interventions, compared with placebo or other active interventions, improve tic severity and tic-related impairment in children and adults with Tourette syndrome or a chronic tic disorder, the guideline writers recommended that the evidence was strongest for CBIT as a first-line treatment, relative to other behavioral treatments and medications.
If symptoms affect a patient’s daily life, doctors should consider CBIT, said guideline author John Piacentini, PhD, of the University of California, Los Angeles, at the annual meeting of the American Academy of Neurology. “This treatment combines habit-reversal training, which teaches patients how to control their urges to tic, with other behavioral strategies to reduce stress and other factors that often make tics worse.”
Patients typically see results from CBIT in 8-12 weeks. More CBIT providers are needed, however, to make the treatment readily available to all patients, he said.
The guideline panel members said that there was moderate confidence in the evidence for reduced tic severity for the following therapeutic approaches, compared with placebo: haloperidol, risperidone, aripiprazole (children only), tiapride (children only), clonidine, onabotulinumtoxinA injections, ningdong granule (as formulated by Zhao), (children only), and ling granule (children only). There was low or very low confidence in the evidence for all other therapies for reducing tic severity.
Comorbid conditions
Many people with tic disorders have neurodevelopmental or psychiatric conditions such as ADHD, obsessive-compulsive disorder, and mood and anxiety disorders. The guideline recommends that people with tics be evaluated for these conditions.
Alpha2-adrenergic agonists may improve symptoms of tic disorders and ADHD, the authors said. There was moderate confidence in the evidence for reduced tic severity for people with a comorbid diagnosis of ADHD with clonidine plus methylphenidate (children only) and methylphenidate alone (children only), compared with placebo.
Adults with severe Tourette syndrome who are resistant to medical and behavioral therapy may benefit from deep brain stimulation (DBS), the guideline states. There was moderate confidence in the evidence for reduced tic severity for DBS of the globus pallidus, compared with sham DBS, as an option for adults with severe tics who have failed CBIT and drugs. These patients first must be screened by a mental health professional and continue to be monitored throughout DBS treatment.
Adults with Tourette syndrome who self-treat their tics with cannabis in states where cannabis is legal should see a doctor who can monitor the use of cannabis for efficacy and adverse effects, the guideline says.
Adverse effects of therapy
The panel also examined the risks of harm, including weight gain, elevated prolactin levels, sedation, drug-induced movement disorders, hypotension, bradycardia, and ECG changes with medical treatments, compared with placebo or other active interventions. In regard to weight gain, the panel concluded with moderate confidence that people with tics receiving risperidone or aripiprazole (children only) are probably more likely to gain weight than people receiving placebo. There was low confidence for associations between specific therapies and elevated prolactin levels.
Compared with people receiving placebo, there was moderate confidence that tiapride is probably associated with higher rates of physical tiredness and sleep disturbances (children only), that clonidine is probably associated with sedation, and that guanfacine is probably associated with drowsiness (children only). There was moderate evidence that pimozide is probably associated with extrapyramidal symptoms. There was low confidence that any specific treatment led to hypotension, bradycardia, or ECG changes.
Additional guideline specifics
The guideline’s practice recommendations include explaining the natural history of tic disorders to patients and caregivers and evaluating patients for functional impairment. Watchful waiting is an acceptable approach in people who do not experience functional impairment, and patients receiving medications for tics must have periodic reevaluations for the need for ongoing medical treatment. People with Tourette syndrome should be referred to resources for psychoeducation for teachers and peers, such as the Tourette Association of America.
Comorbid ADHD occurs in 30%-50% of patients with tics. If screening for ADHD is positive, the burden of ADHD symptoms should be assessed and those with functionally impairing ADHD should be treated for the disorder. Similarly, obsessive-compulsive behaviors occur in 10%-50% of those with Tourette syndrome. If an assessment finds comorbid obsessive-compulsive disorder, it should be treated.
Other psychiatric comorbidities with Tourette syndrome include anxiety disorders, oppositional defiant disorder, and mood disorders. When screening for these conditions, one must inquire about suicidal thoughts and suicide attempts and refer to appropriate resources if present, according to the guidelines.
Individuals with tics and comorbid ADHD should be advised that alpha2-adrenergic agonists may provide benefit for both conditions. Alpha2-adrenergic agonists should be prescribed for the treatment of tics when the benefits of treatment outweigh the risks and patients must be counseled regarding common side effects of alpha2-adrenergic agonists, including sedation. Heart rate and blood pressure must be monitored in patients with tics treated with alpha2-adrenergic agonists. If prescribing extended-release guanfacine, one must monitor the QTc interval in patients with a history of cardiac conditions, patients taking other QT-prolonging agents, or patients with a family history of long QT syndrome. If discontinuing alpha2-adrenergic agonists, they must gradually be tapered to avoid rebound hypertension.
If considering antipsychotic therapies, patients must be counseled on the relative risk for extrapyramidal, hormonal, and metabolic adverse effects to inform decision making on which antipsychotic should be prescribed. Before prescribing antipsychotics for tics, ECGs must be performed. The QTc interval must be measured before and after starting pimozide or ziprasidone, or if antipsychotics are coadministered with other drugs that can prolong the QT interval. The lowest effective dose should be prescribed to decrease the risk of adverse effects, and patients should be monitored for drug-induced movement disorders and for metabolic and hormonal adverse effects of antipsychotics. When attempting to discontinue antipsychotics for tics, the medications should be gradually tapered over weeks to months to avoid withdrawal dyskinesias.
If topiramate is prescribed, patients must be counseled regarding common adverse effects, including cognitive and language problems, somnolence, weight loss, and an increased risk of renal stones.
Some patients with Tourette syndrome use cannabis as a self-medication for tics and comorbidities. Because of the risks associated with cannabis use and widespread self-medication with cannabis for tics, where regional legislation and resources allow, physicians must offer to direct patients to appropriate medical supervision when cannabis is used as self-medication for tics. Appropriate medical supervision would entail education and monitoring for efficacy and adverse effects, according to the guidelines.
Where regional legislation allows, physicians prescribing cannabis-based medication must prescribe the lowest effective dose to decrease the risk of adverse effects. Physicians prescribing cannabis-based medication must inform patients that medication may impair driving ability. Physicians prescribing cannabis-based medication to patients with Tourette syndrome must periodically reevaluate the need for ongoing treatment.
A multidisciplinary evaluation is needed to establish when the benefits of treatment outweigh the risks for prescribing DBS for medication-resistant motor and phonic tics. The DSM-5 diagnosis of Tourette syndrome must be confirmed and exclude secondary and functional tic-like movements when considering DBS for medication-resistant tics. A mental health professional must screen patients preoperatively and follow patients postoperatively for psychiatric disorders that may impede the long-term success of the therapy. Physicians must confirm that multiple classes of medication (antipsychotics, dopamine depleters, alpha1 agonists) and behavioral therapy have been administered (or are contraindicated) before prescribing DBS for tics.
The practice guideline was developed with financial support from AAN. Dr. Pringsheim reported no disclosures. Dr. Piacentini reported receiving funding for travel and speaking from foundations and universities and has received royalties from publishers. In addition, he has performed behavior therapy for tics for approximately 50% of his clinical time and has received financial or material support from Pfizer, the National Institute of Mental Health, and foundations.
SOURCE: Pringsheim T et al. Neurology. 2019 May 6. doi: 10.1212/WNL.0000000000007466.
PHILADELPHIA – Approaches to managing tics in patients with Tourette syndrome or chronic tic disorders “should be individualized, and the choice should be the result of a collaborative decision among patient, caregiver, and clinician, during which the benefits and harms of individual treatments as well as the presence of comorbid disorders are considered,” according to Tamara Pringsheim, MD, lead author of a practice guideline published May 6, 2019, by the American Academy of Neurology, and her collaborators.
The panel of nine physicians, two psychologists, and two patient representatives developed the recommendations based on a comprehensive systematic literature review. They concluded that treatments may decrease the frequency and severity of tics but rarely eliminate them.
The guideline was endorsed by the Child Neurology Society and the European Academy of Neurology and is the first such guideline for American neurologists, said Dr. Pringsheim of the University of Calgary (Alta.). Like recent Canadian and European guidelines, it strongly supports the Comprehensive Behavioral Intervention for Tics (CBIT) as a treatment option for tics.
After examining which medical, behavioral, and neurostimulation interventions, compared with placebo or other active interventions, improve tic severity and tic-related impairment in children and adults with Tourette syndrome or a chronic tic disorder, the guideline writers recommended that the evidence was strongest for CBIT as a first-line treatment, relative to other behavioral treatments and medications.
If symptoms affect a patient’s daily life, doctors should consider CBIT, said guideline author John Piacentini, PhD, of the University of California, Los Angeles, at the annual meeting of the American Academy of Neurology. “This treatment combines habit-reversal training, which teaches patients how to control their urges to tic, with other behavioral strategies to reduce stress and other factors that often make tics worse.”
Patients typically see results from CBIT in 8-12 weeks. More CBIT providers are needed, however, to make the treatment readily available to all patients, he said.
The guideline panel members said that there was moderate confidence in the evidence for reduced tic severity for the following therapeutic approaches, compared with placebo: haloperidol, risperidone, aripiprazole (children only), tiapride (children only), clonidine, onabotulinumtoxinA injections, ningdong granule (as formulated by Zhao), (children only), and ling granule (children only). There was low or very low confidence in the evidence for all other therapies for reducing tic severity.
Comorbid conditions
Many people with tic disorders have neurodevelopmental or psychiatric conditions such as ADHD, obsessive-compulsive disorder, and mood and anxiety disorders. The guideline recommends that people with tics be evaluated for these conditions.
Alpha2-adrenergic agonists may improve symptoms of tic disorders and ADHD, the authors said. There was moderate confidence in the evidence for reduced tic severity for people with a comorbid diagnosis of ADHD with clonidine plus methylphenidate (children only) and methylphenidate alone (children only), compared with placebo.
Adults with severe Tourette syndrome who are resistant to medical and behavioral therapy may benefit from deep brain stimulation (DBS), the guideline states. There was moderate confidence in the evidence for reduced tic severity for DBS of the globus pallidus, compared with sham DBS, as an option for adults with severe tics who have failed CBIT and drugs. These patients first must be screened by a mental health professional and continue to be monitored throughout DBS treatment.
Adults with Tourette syndrome who self-treat their tics with cannabis in states where cannabis is legal should see a doctor who can monitor the use of cannabis for efficacy and adverse effects, the guideline says.
Adverse effects of therapy
The panel also examined the risks of harm, including weight gain, elevated prolactin levels, sedation, drug-induced movement disorders, hypotension, bradycardia, and ECG changes with medical treatments, compared with placebo or other active interventions. In regard to weight gain, the panel concluded with moderate confidence that people with tics receiving risperidone or aripiprazole (children only) are probably more likely to gain weight than people receiving placebo. There was low confidence for associations between specific therapies and elevated prolactin levels.
Compared with people receiving placebo, there was moderate confidence that tiapride is probably associated with higher rates of physical tiredness and sleep disturbances (children only), that clonidine is probably associated with sedation, and that guanfacine is probably associated with drowsiness (children only). There was moderate evidence that pimozide is probably associated with extrapyramidal symptoms. There was low confidence that any specific treatment led to hypotension, bradycardia, or ECG changes.
Additional guideline specifics
The guideline’s practice recommendations include explaining the natural history of tic disorders to patients and caregivers and evaluating patients for functional impairment. Watchful waiting is an acceptable approach in people who do not experience functional impairment, and patients receiving medications for tics must have periodic reevaluations for the need for ongoing medical treatment. People with Tourette syndrome should be referred to resources for psychoeducation for teachers and peers, such as the Tourette Association of America.
Comorbid ADHD occurs in 30%-50% of patients with tics. If screening for ADHD is positive, the burden of ADHD symptoms should be assessed and those with functionally impairing ADHD should be treated for the disorder. Similarly, obsessive-compulsive behaviors occur in 10%-50% of those with Tourette syndrome. If an assessment finds comorbid obsessive-compulsive disorder, it should be treated.
Other psychiatric comorbidities with Tourette syndrome include anxiety disorders, oppositional defiant disorder, and mood disorders. When screening for these conditions, one must inquire about suicidal thoughts and suicide attempts and refer to appropriate resources if present, according to the guidelines.
Individuals with tics and comorbid ADHD should be advised that alpha2-adrenergic agonists may provide benefit for both conditions. Alpha2-adrenergic agonists should be prescribed for the treatment of tics when the benefits of treatment outweigh the risks and patients must be counseled regarding common side effects of alpha2-adrenergic agonists, including sedation. Heart rate and blood pressure must be monitored in patients with tics treated with alpha2-adrenergic agonists. If prescribing extended-release guanfacine, one must monitor the QTc interval in patients with a history of cardiac conditions, patients taking other QT-prolonging agents, or patients with a family history of long QT syndrome. If discontinuing alpha2-adrenergic agonists, they must gradually be tapered to avoid rebound hypertension.
If considering antipsychotic therapies, patients must be counseled on the relative risk for extrapyramidal, hormonal, and metabolic adverse effects to inform decision making on which antipsychotic should be prescribed. Before prescribing antipsychotics for tics, ECGs must be performed. The QTc interval must be measured before and after starting pimozide or ziprasidone, or if antipsychotics are coadministered with other drugs that can prolong the QT interval. The lowest effective dose should be prescribed to decrease the risk of adverse effects, and patients should be monitored for drug-induced movement disorders and for metabolic and hormonal adverse effects of antipsychotics. When attempting to discontinue antipsychotics for tics, the medications should be gradually tapered over weeks to months to avoid withdrawal dyskinesias.
If topiramate is prescribed, patients must be counseled regarding common adverse effects, including cognitive and language problems, somnolence, weight loss, and an increased risk of renal stones.
Some patients with Tourette syndrome use cannabis as a self-medication for tics and comorbidities. Because of the risks associated with cannabis use and widespread self-medication with cannabis for tics, where regional legislation and resources allow, physicians must offer to direct patients to appropriate medical supervision when cannabis is used as self-medication for tics. Appropriate medical supervision would entail education and monitoring for efficacy and adverse effects, according to the guidelines.
Where regional legislation allows, physicians prescribing cannabis-based medication must prescribe the lowest effective dose to decrease the risk of adverse effects. Physicians prescribing cannabis-based medication must inform patients that medication may impair driving ability. Physicians prescribing cannabis-based medication to patients with Tourette syndrome must periodically reevaluate the need for ongoing treatment.
A multidisciplinary evaluation is needed to establish when the benefits of treatment outweigh the risks for prescribing DBS for medication-resistant motor and phonic tics. The DSM-5 diagnosis of Tourette syndrome must be confirmed and exclude secondary and functional tic-like movements when considering DBS for medication-resistant tics. A mental health professional must screen patients preoperatively and follow patients postoperatively for psychiatric disorders that may impede the long-term success of the therapy. Physicians must confirm that multiple classes of medication (antipsychotics, dopamine depleters, alpha1 agonists) and behavioral therapy have been administered (or are contraindicated) before prescribing DBS for tics.
The practice guideline was developed with financial support from AAN. Dr. Pringsheim reported no disclosures. Dr. Piacentini reported receiving funding for travel and speaking from foundations and universities and has received royalties from publishers. In addition, he has performed behavior therapy for tics for approximately 50% of his clinical time and has received financial or material support from Pfizer, the National Institute of Mental Health, and foundations.
SOURCE: Pringsheim T et al. Neurology. 2019 May 6. doi: 10.1212/WNL.0000000000007466.
REPORTING FROM AAN 2019
Depressive symptoms are associated with stroke risk
PHILADELPHIA – according to preliminary data from a prospective cohort study presented at the annual meeting of the American Academy of Neurology.
Prior research has found that depression may increase the likelihood of hypertension, cardiac morbidity and mortality, and stroke mortality. How depression affects the risk of incident stroke, however, “is underexplored, especially among Latinos and African Americans,” said study author Marialaura Simonetto, MD, of the University of Miami and associates.
To assess the relationship between depressive symptoms and risk of incident ischemic stroke, the researchers analyzed data from more than 1,100 participants in the MRI substudy of the Northern Manhattan Study. The cohort includes older adults who were clinically stroke free at baseline.
Researchers assessed depressive symptoms at baseline using the Center for Epidemiological Studies–Depression Scale (CES-D). Scores range from 0-60, and they considered CES-D scores of 16 or greater to be elevated.
The investigators used Cox proportional hazards models to estimate hazard ratios of incident ischemic stroke after adjusting for age, sex, race, ethnicity, years of education, smoking, physical activity, alcohol consumption, diabetes, and hypertension.
In all, 1,104 participants were included in the analysis. Participants had an average age of 70 years, 61% were women, and 69% were Hispanic. At baseline, 198 participants (18%) had elevated depressive symptoms.
During 14 years of follow-up, 101 participants had incident strokes, 87 of which were ischemic strokes. In adjusted models, participants with elevated depressive symptoms had a significantly greater risk of ischemic stroke (HR, 1.75; 95% confidence interval, 1.06-2.88). “Every 5-point increase in CES-D score conferred a 12% greater risk of ischemic stroke,” the researchers reported.
“Depression is common and often goes untreated,” Dr. Simonetto said in a news release. “If people with depression are at elevated risk of stroke, early detection and treatment will be even more important.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Simonetto reported no disclosures. Coauthors disclosed personal compensation and research support from pharmaceutical and medical device companies.
SOURCE: Simonetto M et al. AAN 2019, Abstract S1.003.
PHILADELPHIA – according to preliminary data from a prospective cohort study presented at the annual meeting of the American Academy of Neurology.
Prior research has found that depression may increase the likelihood of hypertension, cardiac morbidity and mortality, and stroke mortality. How depression affects the risk of incident stroke, however, “is underexplored, especially among Latinos and African Americans,” said study author Marialaura Simonetto, MD, of the University of Miami and associates.
To assess the relationship between depressive symptoms and risk of incident ischemic stroke, the researchers analyzed data from more than 1,100 participants in the MRI substudy of the Northern Manhattan Study. The cohort includes older adults who were clinically stroke free at baseline.
Researchers assessed depressive symptoms at baseline using the Center for Epidemiological Studies–Depression Scale (CES-D). Scores range from 0-60, and they considered CES-D scores of 16 or greater to be elevated.
The investigators used Cox proportional hazards models to estimate hazard ratios of incident ischemic stroke after adjusting for age, sex, race, ethnicity, years of education, smoking, physical activity, alcohol consumption, diabetes, and hypertension.
In all, 1,104 participants were included in the analysis. Participants had an average age of 70 years, 61% were women, and 69% were Hispanic. At baseline, 198 participants (18%) had elevated depressive symptoms.
During 14 years of follow-up, 101 participants had incident strokes, 87 of which were ischemic strokes. In adjusted models, participants with elevated depressive symptoms had a significantly greater risk of ischemic stroke (HR, 1.75; 95% confidence interval, 1.06-2.88). “Every 5-point increase in CES-D score conferred a 12% greater risk of ischemic stroke,” the researchers reported.
“Depression is common and often goes untreated,” Dr. Simonetto said in a news release. “If people with depression are at elevated risk of stroke, early detection and treatment will be even more important.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Simonetto reported no disclosures. Coauthors disclosed personal compensation and research support from pharmaceutical and medical device companies.
SOURCE: Simonetto M et al. AAN 2019, Abstract S1.003.
PHILADELPHIA – according to preliminary data from a prospective cohort study presented at the annual meeting of the American Academy of Neurology.
Prior research has found that depression may increase the likelihood of hypertension, cardiac morbidity and mortality, and stroke mortality. How depression affects the risk of incident stroke, however, “is underexplored, especially among Latinos and African Americans,” said study author Marialaura Simonetto, MD, of the University of Miami and associates.
To assess the relationship between depressive symptoms and risk of incident ischemic stroke, the researchers analyzed data from more than 1,100 participants in the MRI substudy of the Northern Manhattan Study. The cohort includes older adults who were clinically stroke free at baseline.
Researchers assessed depressive symptoms at baseline using the Center for Epidemiological Studies–Depression Scale (CES-D). Scores range from 0-60, and they considered CES-D scores of 16 or greater to be elevated.
The investigators used Cox proportional hazards models to estimate hazard ratios of incident ischemic stroke after adjusting for age, sex, race, ethnicity, years of education, smoking, physical activity, alcohol consumption, diabetes, and hypertension.
In all, 1,104 participants were included in the analysis. Participants had an average age of 70 years, 61% were women, and 69% were Hispanic. At baseline, 198 participants (18%) had elevated depressive symptoms.
During 14 years of follow-up, 101 participants had incident strokes, 87 of which were ischemic strokes. In adjusted models, participants with elevated depressive symptoms had a significantly greater risk of ischemic stroke (HR, 1.75; 95% confidence interval, 1.06-2.88). “Every 5-point increase in CES-D score conferred a 12% greater risk of ischemic stroke,” the researchers reported.
“Depression is common and often goes untreated,” Dr. Simonetto said in a news release. “If people with depression are at elevated risk of stroke, early detection and treatment will be even more important.”
The study was supported by the National Institute of Neurological Disorders and Stroke. Dr. Simonetto reported no disclosures. Coauthors disclosed personal compensation and research support from pharmaceutical and medical device companies.
SOURCE: Simonetto M et al. AAN 2019, Abstract S1.003.
REPORTING FROM AAN 2019
Multiple sclerosis may not flare up after pregnancy
PHILADELPHIA – according to a study to be presented at the annual meeting of the American Academy of Neurology.
“We did not observe any rebound disease activity,” said Annette Langer-Gould, MD, PhD, and her research colleagues in their report.
The findings contrast with those of 20-year-old studies that first identified a lower risk of relapse during pregnancy but signficant rebound disease activity in the early postpartum period. The initial studies were conducted before disease-modifying treatments (DMTs) were available and before neurologists used MRI to help diagnose MS after one attack, noted Dr. Langer-Gould in a statement.
In the large, contemporary cohort of patients with MS, the annualized relapse rate was 0.39 pre-pregnancy, 0.07-0.14 during pregnancy, 0.27 in the first 3 months postpartum, and 0.37 at 4-6 months postpartum. Exclusive breastfeeding significantly reduced the risk of postpartum relapses by 42% (adjusted hazard ratio = 0.58). Women who supplemented breast milk with formula within 2 months of delivery had the same risk of relapse as women who did not breastfeed, however.
“These results are exciting, as MS is more common among women of childbearing age than in any other group,” said Dr. Langer-Gould, who is regional lead for clinical and translational neuroscience at Kaiser Permanente Southern California in Pasadena, in the statement. “This shows us that women with MS today can have children, breastfeed, and resume their treatment without experiencing an increased risk of relapses during the postpartum period.”
To describe the risk of postpartum relapses and identify potential risk factors for relapse the investigators analyzed prospectively collected data from 466 pregnancies among 375 women with MS from the complete electronic health record at Kaiser Permanente Southern and Northern California between 2008 and 2016. The researchers also used surveys to collect information about treatment history, breastfeeding, and relapses. They used multivariable models to account for intraclass clustering and disease severity.
In 38% of the pregnancies, the mother had not received treatment in the year before conception. In 14.6%, the mother had a clinically isolated syndrome; in 8.4%, the mother had a relapse during pregnancy.
Resuming modestly effective DMTs such as interferon-betas and glatiramer acetate did not affect relapse risk.
In the postpartum year, 26.4% of mothers relapsed, 87% breastfed, 35% breastfed exclusively, and 41.2% resumed using DMT.
The lack of rebound disease activity in this cohort could be related to the high rate of exclusive breastfeeding, as well as the inclusion of women from a population-based setting and the inclusion of women who had incorrectly been diagnosed with MS after a single relapse. Few patients in this cohort had been treated with natalizumab or fingolimod prior to pregnancy, so the study does not address the potential harms of stopping these drugs or the potential benefits of breastfeeding among patients treated with these drugs.
The study was supported by the National Multiple Sclerosis Society. The researchers had no disclosures.
SOURCE: Langer-Gould A et al. AAN 2019, Abstract S6.007.
PHILADELPHIA – according to a study to be presented at the annual meeting of the American Academy of Neurology.
“We did not observe any rebound disease activity,” said Annette Langer-Gould, MD, PhD, and her research colleagues in their report.
The findings contrast with those of 20-year-old studies that first identified a lower risk of relapse during pregnancy but signficant rebound disease activity in the early postpartum period. The initial studies were conducted before disease-modifying treatments (DMTs) were available and before neurologists used MRI to help diagnose MS after one attack, noted Dr. Langer-Gould in a statement.
In the large, contemporary cohort of patients with MS, the annualized relapse rate was 0.39 pre-pregnancy, 0.07-0.14 during pregnancy, 0.27 in the first 3 months postpartum, and 0.37 at 4-6 months postpartum. Exclusive breastfeeding significantly reduced the risk of postpartum relapses by 42% (adjusted hazard ratio = 0.58). Women who supplemented breast milk with formula within 2 months of delivery had the same risk of relapse as women who did not breastfeed, however.
“These results are exciting, as MS is more common among women of childbearing age than in any other group,” said Dr. Langer-Gould, who is regional lead for clinical and translational neuroscience at Kaiser Permanente Southern California in Pasadena, in the statement. “This shows us that women with MS today can have children, breastfeed, and resume their treatment without experiencing an increased risk of relapses during the postpartum period.”
To describe the risk of postpartum relapses and identify potential risk factors for relapse the investigators analyzed prospectively collected data from 466 pregnancies among 375 women with MS from the complete electronic health record at Kaiser Permanente Southern and Northern California between 2008 and 2016. The researchers also used surveys to collect information about treatment history, breastfeeding, and relapses. They used multivariable models to account for intraclass clustering and disease severity.
In 38% of the pregnancies, the mother had not received treatment in the year before conception. In 14.6%, the mother had a clinically isolated syndrome; in 8.4%, the mother had a relapse during pregnancy.
Resuming modestly effective DMTs such as interferon-betas and glatiramer acetate did not affect relapse risk.
In the postpartum year, 26.4% of mothers relapsed, 87% breastfed, 35% breastfed exclusively, and 41.2% resumed using DMT.
The lack of rebound disease activity in this cohort could be related to the high rate of exclusive breastfeeding, as well as the inclusion of women from a population-based setting and the inclusion of women who had incorrectly been diagnosed with MS after a single relapse. Few patients in this cohort had been treated with natalizumab or fingolimod prior to pregnancy, so the study does not address the potential harms of stopping these drugs or the potential benefits of breastfeeding among patients treated with these drugs.
The study was supported by the National Multiple Sclerosis Society. The researchers had no disclosures.
SOURCE: Langer-Gould A et al. AAN 2019, Abstract S6.007.
PHILADELPHIA – according to a study to be presented at the annual meeting of the American Academy of Neurology.
“We did not observe any rebound disease activity,” said Annette Langer-Gould, MD, PhD, and her research colleagues in their report.
The findings contrast with those of 20-year-old studies that first identified a lower risk of relapse during pregnancy but signficant rebound disease activity in the early postpartum period. The initial studies were conducted before disease-modifying treatments (DMTs) were available and before neurologists used MRI to help diagnose MS after one attack, noted Dr. Langer-Gould in a statement.
In the large, contemporary cohort of patients with MS, the annualized relapse rate was 0.39 pre-pregnancy, 0.07-0.14 during pregnancy, 0.27 in the first 3 months postpartum, and 0.37 at 4-6 months postpartum. Exclusive breastfeeding significantly reduced the risk of postpartum relapses by 42% (adjusted hazard ratio = 0.58). Women who supplemented breast milk with formula within 2 months of delivery had the same risk of relapse as women who did not breastfeed, however.
“These results are exciting, as MS is more common among women of childbearing age than in any other group,” said Dr. Langer-Gould, who is regional lead for clinical and translational neuroscience at Kaiser Permanente Southern California in Pasadena, in the statement. “This shows us that women with MS today can have children, breastfeed, and resume their treatment without experiencing an increased risk of relapses during the postpartum period.”
To describe the risk of postpartum relapses and identify potential risk factors for relapse the investigators analyzed prospectively collected data from 466 pregnancies among 375 women with MS from the complete electronic health record at Kaiser Permanente Southern and Northern California between 2008 and 2016. The researchers also used surveys to collect information about treatment history, breastfeeding, and relapses. They used multivariable models to account for intraclass clustering and disease severity.
In 38% of the pregnancies, the mother had not received treatment in the year before conception. In 14.6%, the mother had a clinically isolated syndrome; in 8.4%, the mother had a relapse during pregnancy.
Resuming modestly effective DMTs such as interferon-betas and glatiramer acetate did not affect relapse risk.
In the postpartum year, 26.4% of mothers relapsed, 87% breastfed, 35% breastfed exclusively, and 41.2% resumed using DMT.
The lack of rebound disease activity in this cohort could be related to the high rate of exclusive breastfeeding, as well as the inclusion of women from a population-based setting and the inclusion of women who had incorrectly been diagnosed with MS after a single relapse. Few patients in this cohort had been treated with natalizumab or fingolimod prior to pregnancy, so the study does not address the potential harms of stopping these drugs or the potential benefits of breastfeeding among patients treated with these drugs.
The study was supported by the National Multiple Sclerosis Society. The researchers had no disclosures.
SOURCE: Langer-Gould A et al. AAN 2019, Abstract S6.007.
FROM AAN 2019
Out-of-pocket costs for neurologic medications rise sharply
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
The out-of-pocket cost of multiple sclerosis (MS) treatments increased the most, with a 20-fold increase during that time. The average out-of-pocket cost for MS therapy was $15/month in 2004, compared with $309/month in 2016. Patients also had to pay more for brand name medications for peripheral neuropathy, dementia, and Parkinson’s disease, researchers said.
“Out-of-pocket costs vary widely both across and within conditions,” said study author Brian C. Callaghan, MD, an assistant professor of neurology at the University of Michigan in Ann Arbor, and research colleagues. “To minimize patient financial burden, neurologists require access to precise cost information when making treatment decisions.”
Prior studies have found that high drug costs “can create burdens such as medical debt, skipping food or other essentials, or even not taking drugs as often as necessary,” Dr. Callaghan said in a news release.
To assess how out-of-pocket costs affect patients with neurologic conditions, the investigators analyzed data from a large, privately insured health care claims database. They determined medication costs for patients with MS, peripheral neuropathy, epilepsy, dementia, and Parkinson’s disease who were seen by outpatient neurologists. They also compared costs for high-deductible and traditional plans and explored cumulative out-of-pocket costs during the first 2 years after diagnosis.
The analysis examined the five most commonly prescribed drugs by neurologists for each condition based on Medicare data. In addition, the researchers included in their analysis all approved MS medications, lacosamide as a brand name epilepsy drug, and venlafaxine, a peripheral neuropathy medication that transitioned from brand to generic.
In all, the study population included 105,355 patients with MS, 314,530 with peripheral neuropathy, 281,073 with epilepsy, 120,720 with dementia, and 90,801 with Parkinson’s disease.
In 2016, patients in high-deductible health plans had an average monthly out-of-pocket expense that was approximately twice that of patients not in those plans – $661 versus $246 among patients with MS, and $40 versus $18 among patients with epilepsy.
In the 2 years after diagnosis in 2012 or 2013, cumulative out-of-pocket costs for patients with MS were a mean of $2,238, but costs varied widely. Cumulative costs were no more than $90 for patients in the bottom 5% of expenses, whereas they exceeded $9,800 for patients in the top 5% of expenses. Among patients with epilepsy, cumulative out-of-pocket costs were $230 in the 2 years after diagnosis.
“In 2004, out-of-pocket costs were of such low magnitude that physicians could typically ignore these costs for most patients and not adversely affect the financial status of patients or their adherence to medications. However, by 2016, out-of-pockets costs have risen to the point where neurologists should consider out-of-pocket costs for most medications and for most patients,” Dr. Callaghan and colleagues wrote.
Ralph L. Sacco, MD, president of the American Academy of Neurology (AAN), said in a news release that the AAN has created a Neurology Drug Pricing Task Force and is advocating for better drug-pricing policies. “This study provides important information to help us better understand how these problems can directly affect our patients,” Dr. Sacco said.
“Everyone deserves affordable access to the medications that will be most beneficial, but if the drugs are too expensive, people may simply not take them, possibly leading to medical complications and higher costs later,” Dr. Sacco said.
The study was supported by the AAN. Several authors are supported by National Institutes of Health grants. Dr. Callaghan receives research support from Impeto Medical and performs consulting work.
SOURCE: Callaghan BC et al. Neurology. 2019 May 1. doi: 10.1212/WNL.0000000000007564.
FROM NEUROLOGY
Most measles cases in 25 years prompts government pleas to vaccinate
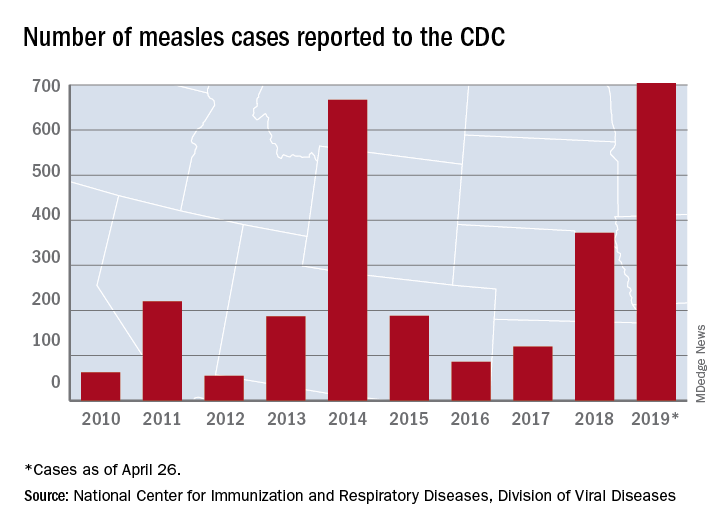
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
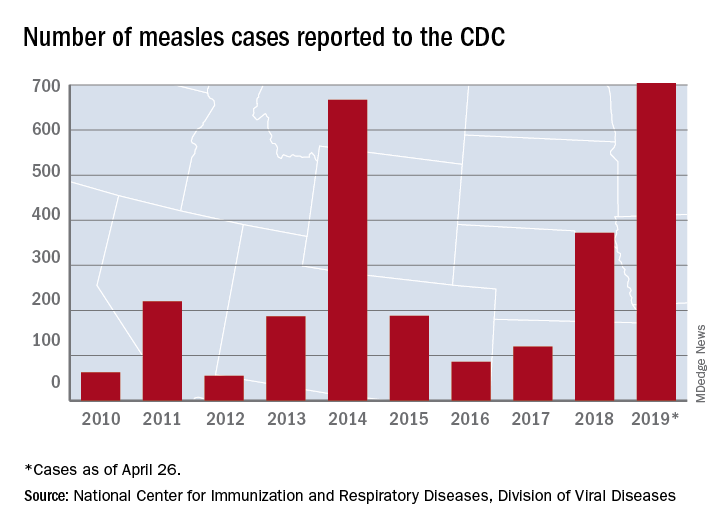
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
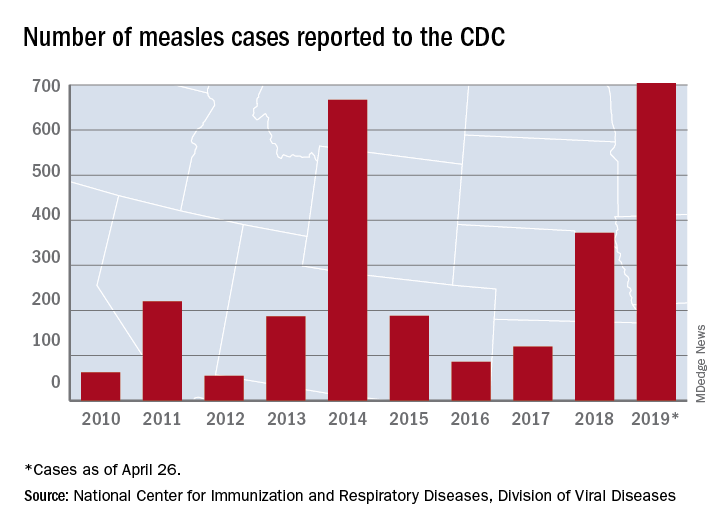
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
FROM A CDC TELEBRIEFING