User login
Low baseline heart rate may not increase cardiac risk when starting fingolimod
SEATTLE – , according to data presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In addition, the data “provide further evidence that first-dose cardiac events with fingolimod are rare,” regardless of whether the first dose is given in a clinic or a patient’s home, the study researchers said.
Transient heart rate decreases are an anticipated effect of starting fingolimod, and the U.S. prescribing information for the drug requires first-dose observation of heart rate and blood pressure for at least 6 hours. Heart rate and blood pressure may be monitored in a clinic or at home via the Gilenya@Home program.
To examine whether low baseline heart rate is associated with the likelihood of certain cardiac events during the first-dose observation period, John Osborne, MD, of State of the Heart Cardiology in Grapevine, Tex., and colleagues analyzed retrospective, first-dose observation data from Gilenya@Home between October 2014 and July 2017 and from Gilenya Assessment Network clinics between July 2010 and December 2016.
The investigators sought to determine whether baseline heart rate predicts the risk of documented bradycardia, new-onset second-degree atrioventricular block, or ED transfer for additional monitoring. In addition, they examined whether patients with heart rates above a certain threshold may be at risk of first-dose cardiac events.
Dr. Osborne and colleagues reviewed data from 5,572 in-home and 15,025 in-clinic first-dose observation procedures. They classified patients as having marked bradycardia (under 50 beats per minute), mild bradycardia (50-59 bpm), or a normal heart rate (at least 60 bpm) at baseline. During the 20,001 procedures with available data, 182 cardiac events occurred, including 28 instances of documented bradycardia, 13 instances of second-degree atrioventricular block, and 141 instances of ED transfer for extended monitoring; 40 events occurred during at-home monitoring, and 142 events occurred in clinic.
About 87.0% of the cardiac events occurred in patients with a normal baseline heart rate, 11.5% occurred in patients with mild bradycardia, and 1.1% occurred in patients with marked bradycardia. The two cardiac events in patients with marked bradycardia at baseline were ED transfers of patients whose first-dose observations occurred in clinics. “The threshold heart rate above which patients did not experience a cardiac event was 80 bpm, well within the normal range of 60-100 bpm,” the authors said.
“These data suggest that patients with a low baseline heart rate may be at no more risk of cardiac events than patients with a heart rate in the normal range, nor is there a baseline heart rate threshold below which a patient is at greater risk of cardiac events,” Dr. Osborne and colleagues concluded.
Dr. Osborne reporting receiving a consulting fee from Novartis, which markets Gilenya (fingolimod), and his coauthors are employees of Novartis.
SEATTLE – , according to data presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In addition, the data “provide further evidence that first-dose cardiac events with fingolimod are rare,” regardless of whether the first dose is given in a clinic or a patient’s home, the study researchers said.
Transient heart rate decreases are an anticipated effect of starting fingolimod, and the U.S. prescribing information for the drug requires first-dose observation of heart rate and blood pressure for at least 6 hours. Heart rate and blood pressure may be monitored in a clinic or at home via the Gilenya@Home program.
To examine whether low baseline heart rate is associated with the likelihood of certain cardiac events during the first-dose observation period, John Osborne, MD, of State of the Heart Cardiology in Grapevine, Tex., and colleagues analyzed retrospective, first-dose observation data from Gilenya@Home between October 2014 and July 2017 and from Gilenya Assessment Network clinics between July 2010 and December 2016.
The investigators sought to determine whether baseline heart rate predicts the risk of documented bradycardia, new-onset second-degree atrioventricular block, or ED transfer for additional monitoring. In addition, they examined whether patients with heart rates above a certain threshold may be at risk of first-dose cardiac events.
Dr. Osborne and colleagues reviewed data from 5,572 in-home and 15,025 in-clinic first-dose observation procedures. They classified patients as having marked bradycardia (under 50 beats per minute), mild bradycardia (50-59 bpm), or a normal heart rate (at least 60 bpm) at baseline. During the 20,001 procedures with available data, 182 cardiac events occurred, including 28 instances of documented bradycardia, 13 instances of second-degree atrioventricular block, and 141 instances of ED transfer for extended monitoring; 40 events occurred during at-home monitoring, and 142 events occurred in clinic.
About 87.0% of the cardiac events occurred in patients with a normal baseline heart rate, 11.5% occurred in patients with mild bradycardia, and 1.1% occurred in patients with marked bradycardia. The two cardiac events in patients with marked bradycardia at baseline were ED transfers of patients whose first-dose observations occurred in clinics. “The threshold heart rate above which patients did not experience a cardiac event was 80 bpm, well within the normal range of 60-100 bpm,” the authors said.
“These data suggest that patients with a low baseline heart rate may be at no more risk of cardiac events than patients with a heart rate in the normal range, nor is there a baseline heart rate threshold below which a patient is at greater risk of cardiac events,” Dr. Osborne and colleagues concluded.
Dr. Osborne reporting receiving a consulting fee from Novartis, which markets Gilenya (fingolimod), and his coauthors are employees of Novartis.
SEATTLE – , according to data presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In addition, the data “provide further evidence that first-dose cardiac events with fingolimod are rare,” regardless of whether the first dose is given in a clinic or a patient’s home, the study researchers said.
Transient heart rate decreases are an anticipated effect of starting fingolimod, and the U.S. prescribing information for the drug requires first-dose observation of heart rate and blood pressure for at least 6 hours. Heart rate and blood pressure may be monitored in a clinic or at home via the Gilenya@Home program.
To examine whether low baseline heart rate is associated with the likelihood of certain cardiac events during the first-dose observation period, John Osborne, MD, of State of the Heart Cardiology in Grapevine, Tex., and colleagues analyzed retrospective, first-dose observation data from Gilenya@Home between October 2014 and July 2017 and from Gilenya Assessment Network clinics between July 2010 and December 2016.
The investigators sought to determine whether baseline heart rate predicts the risk of documented bradycardia, new-onset second-degree atrioventricular block, or ED transfer for additional monitoring. In addition, they examined whether patients with heart rates above a certain threshold may be at risk of first-dose cardiac events.
Dr. Osborne and colleagues reviewed data from 5,572 in-home and 15,025 in-clinic first-dose observation procedures. They classified patients as having marked bradycardia (under 50 beats per minute), mild bradycardia (50-59 bpm), or a normal heart rate (at least 60 bpm) at baseline. During the 20,001 procedures with available data, 182 cardiac events occurred, including 28 instances of documented bradycardia, 13 instances of second-degree atrioventricular block, and 141 instances of ED transfer for extended monitoring; 40 events occurred during at-home monitoring, and 142 events occurred in clinic.
About 87.0% of the cardiac events occurred in patients with a normal baseline heart rate, 11.5% occurred in patients with mild bradycardia, and 1.1% occurred in patients with marked bradycardia. The two cardiac events in patients with marked bradycardia at baseline were ED transfers of patients whose first-dose observations occurred in clinics. “The threshold heart rate above which patients did not experience a cardiac event was 80 bpm, well within the normal range of 60-100 bpm,” the authors said.
“These data suggest that patients with a low baseline heart rate may be at no more risk of cardiac events than patients with a heart rate in the normal range, nor is there a baseline heart rate threshold below which a patient is at greater risk of cardiac events,” Dr. Osborne and colleagues concluded.
Dr. Osborne reporting receiving a consulting fee from Novartis, which markets Gilenya (fingolimod), and his coauthors are employees of Novartis.
REPORTING FROM CMSC 2019
Group creates three-step algorithm for the management of MS relapse
SEATTLE –
“Acute clinical relapses are a defining feature of MS with highly variable symptoms and potentially disabling effects,” said first author Amy Perrin Ross, APN, an MS certified nurse at Loyola University Chicago in Maywood, Ill., and coauthors. “Although clinicians have several management options for MS relapses, including several therapeutic interventions or observation, these options vary in terms of clinical evidence of efficacy, safety, cost, and tolerability. No consensus statements currently exist to help clinicians approach patients with acute MS relapse.”
To offer an algorithm for the management of MS relapses based on evidence and clinical experience, a work group of MS clinicians reviewed published literature on MS relapses and shared their clinical experiences managing relapses. They sought to develop a standardized and optimized approach to management.
The group reached consensus on an iterative management algorithm that consists of evaluation of symptoms to distinguish an MS relapse from a pseudorelapse; treatment, if necessary; and assessment of treatment response.
“Timely and careful evaluation of new symptoms in patients with MS is paramount, and distinguishing an MS relapse from a pseudorelapse is essential,” the authors said. “This evaluation is primarily clinical, and imaging findings may not be necessary for confirmation.”
Corticosteroid therapy is the mainstay of MS relapse management. For patients who cannot tolerate corticosteroids or in whom corticosteroids have been ineffective, clinicians may consider adrenocorticotropic hormone (ACTH). In patients with fulminant demyelination, plasma exchange therapy may be considered. In mild cases, observation may be reasonable, the authors said.
The group recommends that, between 3 and 5 weeks after the initial evaluation, a clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire should be undertaken.
If a patient’s response to treatment has been suboptimal – that is, symptoms have worsened despite treatment or there has been a lack of functional recovery – “reevaluation of the relapse and treatment with an alternative option should be considered,” they said.
The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
SEATTLE –
“Acute clinical relapses are a defining feature of MS with highly variable symptoms and potentially disabling effects,” said first author Amy Perrin Ross, APN, an MS certified nurse at Loyola University Chicago in Maywood, Ill., and coauthors. “Although clinicians have several management options for MS relapses, including several therapeutic interventions or observation, these options vary in terms of clinical evidence of efficacy, safety, cost, and tolerability. No consensus statements currently exist to help clinicians approach patients with acute MS relapse.”
To offer an algorithm for the management of MS relapses based on evidence and clinical experience, a work group of MS clinicians reviewed published literature on MS relapses and shared their clinical experiences managing relapses. They sought to develop a standardized and optimized approach to management.
The group reached consensus on an iterative management algorithm that consists of evaluation of symptoms to distinguish an MS relapse from a pseudorelapse; treatment, if necessary; and assessment of treatment response.
“Timely and careful evaluation of new symptoms in patients with MS is paramount, and distinguishing an MS relapse from a pseudorelapse is essential,” the authors said. “This evaluation is primarily clinical, and imaging findings may not be necessary for confirmation.”
Corticosteroid therapy is the mainstay of MS relapse management. For patients who cannot tolerate corticosteroids or in whom corticosteroids have been ineffective, clinicians may consider adrenocorticotropic hormone (ACTH). In patients with fulminant demyelination, plasma exchange therapy may be considered. In mild cases, observation may be reasonable, the authors said.
The group recommends that, between 3 and 5 weeks after the initial evaluation, a clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire should be undertaken.
If a patient’s response to treatment has been suboptimal – that is, symptoms have worsened despite treatment or there has been a lack of functional recovery – “reevaluation of the relapse and treatment with an alternative option should be considered,” they said.
The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
SEATTLE –
“Acute clinical relapses are a defining feature of MS with highly variable symptoms and potentially disabling effects,” said first author Amy Perrin Ross, APN, an MS certified nurse at Loyola University Chicago in Maywood, Ill., and coauthors. “Although clinicians have several management options for MS relapses, including several therapeutic interventions or observation, these options vary in terms of clinical evidence of efficacy, safety, cost, and tolerability. No consensus statements currently exist to help clinicians approach patients with acute MS relapse.”
To offer an algorithm for the management of MS relapses based on evidence and clinical experience, a work group of MS clinicians reviewed published literature on MS relapses and shared their clinical experiences managing relapses. They sought to develop a standardized and optimized approach to management.
The group reached consensus on an iterative management algorithm that consists of evaluation of symptoms to distinguish an MS relapse from a pseudorelapse; treatment, if necessary; and assessment of treatment response.
“Timely and careful evaluation of new symptoms in patients with MS is paramount, and distinguishing an MS relapse from a pseudorelapse is essential,” the authors said. “This evaluation is primarily clinical, and imaging findings may not be necessary for confirmation.”
Corticosteroid therapy is the mainstay of MS relapse management. For patients who cannot tolerate corticosteroids or in whom corticosteroids have been ineffective, clinicians may consider adrenocorticotropic hormone (ACTH). In patients with fulminant demyelination, plasma exchange therapy may be considered. In mild cases, observation may be reasonable, the authors said.
The group recommends that, between 3 and 5 weeks after the initial evaluation, a clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire should be undertaken.
If a patient’s response to treatment has been suboptimal – that is, symptoms have worsened despite treatment or there has been a lack of functional recovery – “reevaluation of the relapse and treatment with an alternative option should be considered,” they said.
The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
REPORTING FROM CMSC 2019
Association between cytomegalovirus and MS varies by region
SEATTLE – presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In the United States, the association between CMV seropositivity and MS is not statistically significant, whereas combined data from all regions show a significant positive association, researchers said.
“To our knowledge, this is the largest meta-analysis evaluation of the association between CMV seropositivity and MS,” said Smathorn Thakolwiboon, MD, a neurology resident at Texas Tech University, Lubbock, and colleagues. Understanding the reasons for the geographic heterogeneity will require further research, they said.
Researchers have hypothesized that increased incidence of autoimmune conditions may be linked to the prevention or delay of common infections, but studies have been inconclusive (Neurology. 2017 Sep 26;89[13]:1330-7.).
To evaluate the association between CMV seropositivity and MS, Dr. Thakolwiboon and colleagues searched databases, including PubMed/MEDLINE, Embase, and Web of Science, from inception through Dec. 2018. They included in their analysis observational studies that evaluated the seroprevalence of CMV immunoglobulin G (IgG) in adults with MS and healthy controls. They estimated the odds ratio (OR) for CMV seropositivity and MS.
An initial search yielded 982 articles, 56 of which underwent full review. The researchers ultimately included 13 articles in their quantitative analysis. The studies included data from 3,049 patients with MS and 3,604 controls.
Overall, CMV seropositivity was significantly associated with MS (OR, 1.58; 95% confidence interval, 1.04-2.39; P = .031), but the relationship varied by region. In five U.S. studies, the association was not statistically significant (OR, 1.57; 95% CI, 0.83-2.99; P = .168). CMV seropositivity was negatively associated with MS in Europe (OR, 0.81; 95% CI, 0.68-0.96; P less than .001), but positively associated with MS in the Middle East (OR, 5.42; 95% CI, 1.06-27.89; P less than .001). “The meta-analysis showed a heterogeneity of the association between CMV seropositivity and MS,” the researchers concluded. “More genetic and environmental studies are needed for better understanding this geographic heterogeneity.”
Dr. Thakolwiboon had no disclosures. A coauthor disclosed speaking and advisory board roles with EMD Serono, Genzyme, Novartis, and Teva.
SOURCE: Thakolwiboon S et al. CMSC 2019. Abstract EPI01.
SEATTLE – presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In the United States, the association between CMV seropositivity and MS is not statistically significant, whereas combined data from all regions show a significant positive association, researchers said.
“To our knowledge, this is the largest meta-analysis evaluation of the association between CMV seropositivity and MS,” said Smathorn Thakolwiboon, MD, a neurology resident at Texas Tech University, Lubbock, and colleagues. Understanding the reasons for the geographic heterogeneity will require further research, they said.
Researchers have hypothesized that increased incidence of autoimmune conditions may be linked to the prevention or delay of common infections, but studies have been inconclusive (Neurology. 2017 Sep 26;89[13]:1330-7.).
To evaluate the association between CMV seropositivity and MS, Dr. Thakolwiboon and colleagues searched databases, including PubMed/MEDLINE, Embase, and Web of Science, from inception through Dec. 2018. They included in their analysis observational studies that evaluated the seroprevalence of CMV immunoglobulin G (IgG) in adults with MS and healthy controls. They estimated the odds ratio (OR) for CMV seropositivity and MS.
An initial search yielded 982 articles, 56 of which underwent full review. The researchers ultimately included 13 articles in their quantitative analysis. The studies included data from 3,049 patients with MS and 3,604 controls.
Overall, CMV seropositivity was significantly associated with MS (OR, 1.58; 95% confidence interval, 1.04-2.39; P = .031), but the relationship varied by region. In five U.S. studies, the association was not statistically significant (OR, 1.57; 95% CI, 0.83-2.99; P = .168). CMV seropositivity was negatively associated with MS in Europe (OR, 0.81; 95% CI, 0.68-0.96; P less than .001), but positively associated with MS in the Middle East (OR, 5.42; 95% CI, 1.06-27.89; P less than .001). “The meta-analysis showed a heterogeneity of the association between CMV seropositivity and MS,” the researchers concluded. “More genetic and environmental studies are needed for better understanding this geographic heterogeneity.”
Dr. Thakolwiboon had no disclosures. A coauthor disclosed speaking and advisory board roles with EMD Serono, Genzyme, Novartis, and Teva.
SOURCE: Thakolwiboon S et al. CMSC 2019. Abstract EPI01.
SEATTLE – presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. In the United States, the association between CMV seropositivity and MS is not statistically significant, whereas combined data from all regions show a significant positive association, researchers said.
“To our knowledge, this is the largest meta-analysis evaluation of the association between CMV seropositivity and MS,” said Smathorn Thakolwiboon, MD, a neurology resident at Texas Tech University, Lubbock, and colleagues. Understanding the reasons for the geographic heterogeneity will require further research, they said.
Researchers have hypothesized that increased incidence of autoimmune conditions may be linked to the prevention or delay of common infections, but studies have been inconclusive (Neurology. 2017 Sep 26;89[13]:1330-7.).
To evaluate the association between CMV seropositivity and MS, Dr. Thakolwiboon and colleagues searched databases, including PubMed/MEDLINE, Embase, and Web of Science, from inception through Dec. 2018. They included in their analysis observational studies that evaluated the seroprevalence of CMV immunoglobulin G (IgG) in adults with MS and healthy controls. They estimated the odds ratio (OR) for CMV seropositivity and MS.
An initial search yielded 982 articles, 56 of which underwent full review. The researchers ultimately included 13 articles in their quantitative analysis. The studies included data from 3,049 patients with MS and 3,604 controls.
Overall, CMV seropositivity was significantly associated with MS (OR, 1.58; 95% confidence interval, 1.04-2.39; P = .031), but the relationship varied by region. In five U.S. studies, the association was not statistically significant (OR, 1.57; 95% CI, 0.83-2.99; P = .168). CMV seropositivity was negatively associated with MS in Europe (OR, 0.81; 95% CI, 0.68-0.96; P less than .001), but positively associated with MS in the Middle East (OR, 5.42; 95% CI, 1.06-27.89; P less than .001). “The meta-analysis showed a heterogeneity of the association between CMV seropositivity and MS,” the researchers concluded. “More genetic and environmental studies are needed for better understanding this geographic heterogeneity.”
Dr. Thakolwiboon had no disclosures. A coauthor disclosed speaking and advisory board roles with EMD Serono, Genzyme, Novartis, and Teva.
SOURCE: Thakolwiboon S et al. CMSC 2019. Abstract EPI01.
REPORTING FROM CMSC 2019
Key clinical point: Cytomegalovirus seropositivity may be associated with increased likelihood of multiple sclerosis in the Middle East and decreased likelihood in Europe.
Major finding: Overall, cytomegalovirus seropositivity was significantly associated with multiple sclerosis (OR, 1.58), but the relationship varied by region.
Study details: A meta-analysis of 13 studies that included data from 3,049 patients with MS and 3,604 controls.
Disclosures: Dr. Thakolwiboon had no disclosures. A coauthor disclosed speaking and advisory board roles with EMD Serono, Genzyme, Novartis, and Teva.
Source: Thakolwiboon S et al. CMSC 2019. Abstract EPI01.
Pain, fatigue, depression, and anxiety are common in the year after MS diagnosis
SEATTLE – researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. In a novel study, about half of patients with MS reported clinically significant symptoms of depression or pain, and approximately 60% reported fatigue during that time.
Pain, fatigue, depression, and anxiety are common in MS, but their prevalence in the first year after diagnosis is not well understood. To examine the rates of these conditions and how often they co-occur during that period, Anna L. Kratz, PhD, associate professor of physical medicine and rehabilitation at the University of Michigan in Ann Arbor, and her research colleagues had 231 adults with MS complete validated surveys at 1, 2, 3, 6, 9, and 12 months after diagnosis to assess symptoms of these conditions.
Overall, 47.2% of patients reported clinically significant levels of depression, 38.5% reported clinically significant levels of anxiety, 50.4% reported clinically significant pain, and 62.2% reported clinically significant fatigue at any point during the year after diagnosis. “Of those who did not have clinically significant symptoms at time of diagnosis, 21.3% went on to develop clinically significant depression, 17.0% anxiety, 30.9% pain, and 34.1% fatigue,” the authors reported.
About 23% of patients did not have clinically significant symptoms for any condition, while 20% had clinically significant symptoms for one condition, 21% for two, 19% for three, and 17% for all four.
Depression and fatigue had the highest rate of comorbidity, whereas pain and anxiety had the lowest rate of comorbidity.
“Important clinical symptoms associated with MS are present at high levels in the first year post diagnosis,” Dr. Kratz and colleagues concluded. “While the rates and severity are marginally lower than have been identified in studies of individuals farther into the MS disease course, this study is a reminder that early MS intervention should incorporate interventions for these symptoms that are known to have strong associations with quality of life.”
The researchers had no disclosures.
SEATTLE – researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. In a novel study, about half of patients with MS reported clinically significant symptoms of depression or pain, and approximately 60% reported fatigue during that time.
Pain, fatigue, depression, and anxiety are common in MS, but their prevalence in the first year after diagnosis is not well understood. To examine the rates of these conditions and how often they co-occur during that period, Anna L. Kratz, PhD, associate professor of physical medicine and rehabilitation at the University of Michigan in Ann Arbor, and her research colleagues had 231 adults with MS complete validated surveys at 1, 2, 3, 6, 9, and 12 months after diagnosis to assess symptoms of these conditions.
Overall, 47.2% of patients reported clinically significant levels of depression, 38.5% reported clinically significant levels of anxiety, 50.4% reported clinically significant pain, and 62.2% reported clinically significant fatigue at any point during the year after diagnosis. “Of those who did not have clinically significant symptoms at time of diagnosis, 21.3% went on to develop clinically significant depression, 17.0% anxiety, 30.9% pain, and 34.1% fatigue,” the authors reported.
About 23% of patients did not have clinically significant symptoms for any condition, while 20% had clinically significant symptoms for one condition, 21% for two, 19% for three, and 17% for all four.
Depression and fatigue had the highest rate of comorbidity, whereas pain and anxiety had the lowest rate of comorbidity.
“Important clinical symptoms associated with MS are present at high levels in the first year post diagnosis,” Dr. Kratz and colleagues concluded. “While the rates and severity are marginally lower than have been identified in studies of individuals farther into the MS disease course, this study is a reminder that early MS intervention should incorporate interventions for these symptoms that are known to have strong associations with quality of life.”
The researchers had no disclosures.
SEATTLE – researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. In a novel study, about half of patients with MS reported clinically significant symptoms of depression or pain, and approximately 60% reported fatigue during that time.
Pain, fatigue, depression, and anxiety are common in MS, but their prevalence in the first year after diagnosis is not well understood. To examine the rates of these conditions and how often they co-occur during that period, Anna L. Kratz, PhD, associate professor of physical medicine and rehabilitation at the University of Michigan in Ann Arbor, and her research colleagues had 231 adults with MS complete validated surveys at 1, 2, 3, 6, 9, and 12 months after diagnosis to assess symptoms of these conditions.
Overall, 47.2% of patients reported clinically significant levels of depression, 38.5% reported clinically significant levels of anxiety, 50.4% reported clinically significant pain, and 62.2% reported clinically significant fatigue at any point during the year after diagnosis. “Of those who did not have clinically significant symptoms at time of diagnosis, 21.3% went on to develop clinically significant depression, 17.0% anxiety, 30.9% pain, and 34.1% fatigue,” the authors reported.
About 23% of patients did not have clinically significant symptoms for any condition, while 20% had clinically significant symptoms for one condition, 21% for two, 19% for three, and 17% for all four.
Depression and fatigue had the highest rate of comorbidity, whereas pain and anxiety had the lowest rate of comorbidity.
“Important clinical symptoms associated with MS are present at high levels in the first year post diagnosis,” Dr. Kratz and colleagues concluded. “While the rates and severity are marginally lower than have been identified in studies of individuals farther into the MS disease course, this study is a reminder that early MS intervention should incorporate interventions for these symptoms that are known to have strong associations with quality of life.”
The researchers had no disclosures.
REPORTING FROM CMSC 2019
Key clinical point: Pain, fatigue, depression, and anxiety are common among patients with multiple sclerosis in the 12 months after diagnosis.
Major finding: About half of patients with multiple sclerosis reported clinically significant symptoms of depression or pain, and approximately 60% reported fatigue.
Study details: An analysis of data from 231 adults with multiple sclerosis who completed validated surveys at 1, 2, 3, 6, 9, and 12 months after diagnosis to assess symptoms of pain, fatigue, depression, and anxiety.
Disclosures: The researchers had no disclosures.
More patients than ever receive DMT within 1 year of MS disease onset
SEATTLE – The proportion of patients with multiple sclerosis (MS) who start a disease-modifying therapy (DMT) within 1 year of MS onset has increased in Southern Alberta, researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. , said Jamie Greenfield, MPH, an epidemiologist at the University of Calgary, Alta., and colleagues.
Studies suggest that early initiation of DMT may change the course of MS, but diagnostic delays and barriers to treatment “often impede this opportunity,” the investigators said at the annual meeting of the Consortium of Multiple Sclerosis Centers. To assess time to treatment initiation among patients with relapsing-remitting MS, the researchers analyzed administrative data from the Calgary MS Clinic. They determined the time to initiation of an approved first-line DMT from MS onset, first MS clinic appointment, MS diagnosis, and most recent prior MS clinic appointment. They excluded patients who started a second-line DMT, started a DMT before an MS clinic appointment, or started a DMT during a clinical trial. In addition, they excluded patients with MS onset before 1999, when government reimbursements for DMTs became available.
In all, 1,462 eligible patients started DMTs during August 1999–March 2018; 57.2% started glatiramer acetate, 28.2% interferon-beta, 12.5% dimethyl fumarate, and 2.1% teriflunomide. Average age at treatment initiation was 36 years, and 71.3% were women. Median Expanded Disability Status Scale (EDSS) score was 2.0, and about 90% were urban residents. Approximately 23% had MS diagnosed before their first visit, 37% at their first visit, and 40% after their first visit.
Median time to DMT initiations was 20.3 months from MS onset, 5.4 months from first appointment, 4.1 months from MS diagnosis, and 1.6 months from most recent prior appointment. During 2015-2017, a greater percentage of patients started a DMT within 1 year of MS onset, compared with 1999-2004 (60.9% vs. 20.4%). During 2015-2017, patients also were more likely to start DMTs within 1 year of their first appointment (88.4% vs. 65.7%), within 1 year of MS diagnosis (92.8% vs. 81.3%), and within 3 months of their most recent prior appointment (89.2% vs. 59.5%), compared with 1999-2004.
The investigators used Spearman rank correlations or Kruskal-Wallis tests to evaluate associations between baseline characteristics and time to DMT initiation. A diagnosis of MS or a relapsing-remitting MS course at the first appointment, older age at MS onset, longer MS duration at the first appointment, higher EDSS scores at the first or most recent prior appointment, and shorter time between diagnosis and first appointment, regardless of whether diagnosis occurred before or after the appointment, were associated with earlier DMT initiation.
“Treatment delays are improving. Better understanding of these delays will guide development of additional early-initiation strategies,” the authors concluded.
Ms. Greenfield had no disclosures. A coauthor reported consulting fees from Biogen, Roche, Sanofi Genzyme, and Serono.
SOURCE: Greenfield J et al. CMSC 2019, Abstract DXT25.
SEATTLE – The proportion of patients with multiple sclerosis (MS) who start a disease-modifying therapy (DMT) within 1 year of MS onset has increased in Southern Alberta, researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. , said Jamie Greenfield, MPH, an epidemiologist at the University of Calgary, Alta., and colleagues.
Studies suggest that early initiation of DMT may change the course of MS, but diagnostic delays and barriers to treatment “often impede this opportunity,” the investigators said at the annual meeting of the Consortium of Multiple Sclerosis Centers. To assess time to treatment initiation among patients with relapsing-remitting MS, the researchers analyzed administrative data from the Calgary MS Clinic. They determined the time to initiation of an approved first-line DMT from MS onset, first MS clinic appointment, MS diagnosis, and most recent prior MS clinic appointment. They excluded patients who started a second-line DMT, started a DMT before an MS clinic appointment, or started a DMT during a clinical trial. In addition, they excluded patients with MS onset before 1999, when government reimbursements for DMTs became available.
In all, 1,462 eligible patients started DMTs during August 1999–March 2018; 57.2% started glatiramer acetate, 28.2% interferon-beta, 12.5% dimethyl fumarate, and 2.1% teriflunomide. Average age at treatment initiation was 36 years, and 71.3% were women. Median Expanded Disability Status Scale (EDSS) score was 2.0, and about 90% were urban residents. Approximately 23% had MS diagnosed before their first visit, 37% at their first visit, and 40% after their first visit.
Median time to DMT initiations was 20.3 months from MS onset, 5.4 months from first appointment, 4.1 months from MS diagnosis, and 1.6 months from most recent prior appointment. During 2015-2017, a greater percentage of patients started a DMT within 1 year of MS onset, compared with 1999-2004 (60.9% vs. 20.4%). During 2015-2017, patients also were more likely to start DMTs within 1 year of their first appointment (88.4% vs. 65.7%), within 1 year of MS diagnosis (92.8% vs. 81.3%), and within 3 months of their most recent prior appointment (89.2% vs. 59.5%), compared with 1999-2004.
The investigators used Spearman rank correlations or Kruskal-Wallis tests to evaluate associations between baseline characteristics and time to DMT initiation. A diagnosis of MS or a relapsing-remitting MS course at the first appointment, older age at MS onset, longer MS duration at the first appointment, higher EDSS scores at the first or most recent prior appointment, and shorter time between diagnosis and first appointment, regardless of whether diagnosis occurred before or after the appointment, were associated with earlier DMT initiation.
“Treatment delays are improving. Better understanding of these delays will guide development of additional early-initiation strategies,” the authors concluded.
Ms. Greenfield had no disclosures. A coauthor reported consulting fees from Biogen, Roche, Sanofi Genzyme, and Serono.
SOURCE: Greenfield J et al. CMSC 2019, Abstract DXT25.
SEATTLE – The proportion of patients with multiple sclerosis (MS) who start a disease-modifying therapy (DMT) within 1 year of MS onset has increased in Southern Alberta, researchers reported at the annual meeting of the Consortium of Multiple Sclerosis Centers. , said Jamie Greenfield, MPH, an epidemiologist at the University of Calgary, Alta., and colleagues.
Studies suggest that early initiation of DMT may change the course of MS, but diagnostic delays and barriers to treatment “often impede this opportunity,” the investigators said at the annual meeting of the Consortium of Multiple Sclerosis Centers. To assess time to treatment initiation among patients with relapsing-remitting MS, the researchers analyzed administrative data from the Calgary MS Clinic. They determined the time to initiation of an approved first-line DMT from MS onset, first MS clinic appointment, MS diagnosis, and most recent prior MS clinic appointment. They excluded patients who started a second-line DMT, started a DMT before an MS clinic appointment, or started a DMT during a clinical trial. In addition, they excluded patients with MS onset before 1999, when government reimbursements for DMTs became available.
In all, 1,462 eligible patients started DMTs during August 1999–March 2018; 57.2% started glatiramer acetate, 28.2% interferon-beta, 12.5% dimethyl fumarate, and 2.1% teriflunomide. Average age at treatment initiation was 36 years, and 71.3% were women. Median Expanded Disability Status Scale (EDSS) score was 2.0, and about 90% were urban residents. Approximately 23% had MS diagnosed before their first visit, 37% at their first visit, and 40% after their first visit.
Median time to DMT initiations was 20.3 months from MS onset, 5.4 months from first appointment, 4.1 months from MS diagnosis, and 1.6 months from most recent prior appointment. During 2015-2017, a greater percentage of patients started a DMT within 1 year of MS onset, compared with 1999-2004 (60.9% vs. 20.4%). During 2015-2017, patients also were more likely to start DMTs within 1 year of their first appointment (88.4% vs. 65.7%), within 1 year of MS diagnosis (92.8% vs. 81.3%), and within 3 months of their most recent prior appointment (89.2% vs. 59.5%), compared with 1999-2004.
The investigators used Spearman rank correlations or Kruskal-Wallis tests to evaluate associations between baseline characteristics and time to DMT initiation. A diagnosis of MS or a relapsing-remitting MS course at the first appointment, older age at MS onset, longer MS duration at the first appointment, higher EDSS scores at the first or most recent prior appointment, and shorter time between diagnosis and first appointment, regardless of whether diagnosis occurred before or after the appointment, were associated with earlier DMT initiation.
“Treatment delays are improving. Better understanding of these delays will guide development of additional early-initiation strategies,” the authors concluded.
Ms. Greenfield had no disclosures. A coauthor reported consulting fees from Biogen, Roche, Sanofi Genzyme, and Serono.
SOURCE: Greenfield J et al. CMSC 2019, Abstract DXT25.
REPORTING FROM CMSC 2019
Key clinical point: The proportion of patients with multiple sclerosis who start disease-modifying therapies within 1 year of disease onset may be increasing.
Major finding: During 1999-2004, about 20% of patients with MS started treatment within 1 year of disease onset, compared with 60% of patients during 2015-2017, at a center in Southern Alberta.
Study details: An analysis of administrative data from 1,462 patients from the Calgary MS Clinic between 1999 and 2018.
Disclosures: Ms. Greenfield had no disclosures. A coauthor reported consulting fees from Biogen, Roche, Sanofi Genzyme, and Serono.
Source: Greenfield J et al. CMSC 2019, Abstract DXT25.
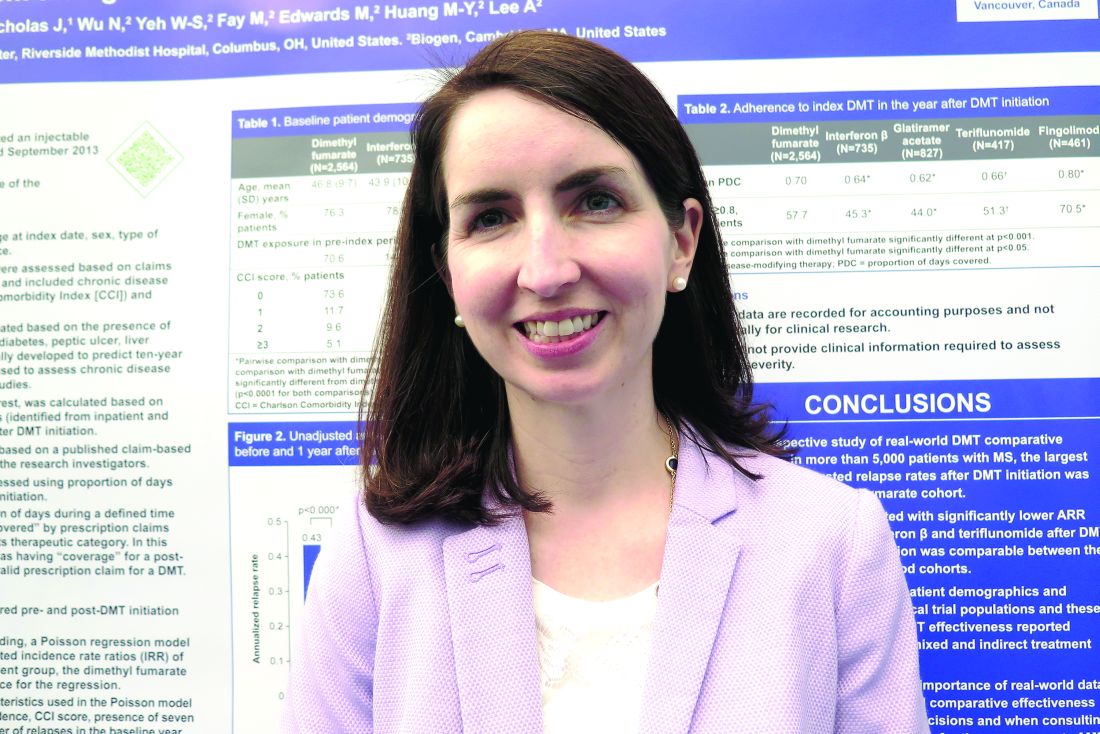
What other drugs do patients take when they start MS therapy?
SEATTLE – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. The likelihood of particular comorbidities and concomitant medications varies by age and sex, researchers reported.
“This may have implications for MS treatment,” said study author Jacqueline Nicholas, MD, MPH, of Ohio Multiple Sclerosis Center in Columbus and her research colleagues. “A better understanding of the effects of comorbidities and concomitant medications on the effectiveness and safety of DMDs is needed to support clinical decision making.”
Researchers have examined comorbidities in patients with MS, but concomitant medication use among patients starting DMDs is poorly understood, the authors said.
To study this question, Dr. Nicholas and colleagues analyzed retrospective administrative claims data from IQVIA’s Real-World Data Adjudicated Claims–U.S. database from Jan. 1, 2010, to June 30, 2017. Their analysis included patients with two or more MS diagnosis claims and at least one DMD claim between Jan. 1, 2011, and June 30, 2015. Eligible patients were aged 18-63 years and had continuous eligibility with commercial insurance 1 year before and 2 years after DMD initiation. In addition, patients had no evidence of DMD use during the 1-year baseline period.
The investigators used International Classification of Diseases, 9th and 10th Revision, Clinical Modification codes and claims to evaluate patients’ comorbidities and concomitant medications during the study period.
The researchers identified 8,251 eligible patients. Patients had a mean age of 43.2 years, and 75.5% were female. Average baseline Charlson comorbidity score was 0.41. In the 2 years after DMD initiation, common comorbid diagnoses were hyperlipidemia (30.0%), hypertension (28.2%), gastrointestinal disorders (26.2%), depression (25.5%), and anxiety (20.1%).
Common concomitant medications included antibiotics (70.6%); analgesics (57.0%); corticosteroids (52.0%); antidepressants (47.7%); anticonvulsants (46.7%); anxiolytics, sedatives, or hypnotics (43.2%); spasticity medications (36.2%); and muscle relaxants (35.4%).
Most comorbidities and many medications, including bladder and antifatigue medications, were more common among patients aged 55 years and older. Hyperlipidemia, hypertension, and diabetes were more likely in males than in females. Females were more likely to have gastrointestinal disease, depression, thyroid disease, anxiety, lung disease, and arthritis. In addition, females were more likely than males to use many of the concomitant medications.
Dr. Nicholas disclosed grant support from EMD Serono. A coauthor is an employee of Health Services Consulting Corporation and received funding from EMD Serono to conduct the study. Other coauthors are employees of EMD Serono.
SEATTLE – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. The likelihood of particular comorbidities and concomitant medications varies by age and sex, researchers reported.
“This may have implications for MS treatment,” said study author Jacqueline Nicholas, MD, MPH, of Ohio Multiple Sclerosis Center in Columbus and her research colleagues. “A better understanding of the effects of comorbidities and concomitant medications on the effectiveness and safety of DMDs is needed to support clinical decision making.”
Researchers have examined comorbidities in patients with MS, but concomitant medication use among patients starting DMDs is poorly understood, the authors said.
To study this question, Dr. Nicholas and colleagues analyzed retrospective administrative claims data from IQVIA’s Real-World Data Adjudicated Claims–U.S. database from Jan. 1, 2010, to June 30, 2017. Their analysis included patients with two or more MS diagnosis claims and at least one DMD claim between Jan. 1, 2011, and June 30, 2015. Eligible patients were aged 18-63 years and had continuous eligibility with commercial insurance 1 year before and 2 years after DMD initiation. In addition, patients had no evidence of DMD use during the 1-year baseline period.
The investigators used International Classification of Diseases, 9th and 10th Revision, Clinical Modification codes and claims to evaluate patients’ comorbidities and concomitant medications during the study period.
The researchers identified 8,251 eligible patients. Patients had a mean age of 43.2 years, and 75.5% were female. Average baseline Charlson comorbidity score was 0.41. In the 2 years after DMD initiation, common comorbid diagnoses were hyperlipidemia (30.0%), hypertension (28.2%), gastrointestinal disorders (26.2%), depression (25.5%), and anxiety (20.1%).
Common concomitant medications included antibiotics (70.6%); analgesics (57.0%); corticosteroids (52.0%); antidepressants (47.7%); anticonvulsants (46.7%); anxiolytics, sedatives, or hypnotics (43.2%); spasticity medications (36.2%); and muscle relaxants (35.4%).
Most comorbidities and many medications, including bladder and antifatigue medications, were more common among patients aged 55 years and older. Hyperlipidemia, hypertension, and diabetes were more likely in males than in females. Females were more likely to have gastrointestinal disease, depression, thyroid disease, anxiety, lung disease, and arthritis. In addition, females were more likely than males to use many of the concomitant medications.
Dr. Nicholas disclosed grant support from EMD Serono. A coauthor is an employee of Health Services Consulting Corporation and received funding from EMD Serono to conduct the study. Other coauthors are employees of EMD Serono.
SEATTLE – , according to research presented at the annual meeting of the Consortium of Multiple Sclerosis Centers. The likelihood of particular comorbidities and concomitant medications varies by age and sex, researchers reported.
“This may have implications for MS treatment,” said study author Jacqueline Nicholas, MD, MPH, of Ohio Multiple Sclerosis Center in Columbus and her research colleagues. “A better understanding of the effects of comorbidities and concomitant medications on the effectiveness and safety of DMDs is needed to support clinical decision making.”
Researchers have examined comorbidities in patients with MS, but concomitant medication use among patients starting DMDs is poorly understood, the authors said.
To study this question, Dr. Nicholas and colleagues analyzed retrospective administrative claims data from IQVIA’s Real-World Data Adjudicated Claims–U.S. database from Jan. 1, 2010, to June 30, 2017. Their analysis included patients with two or more MS diagnosis claims and at least one DMD claim between Jan. 1, 2011, and June 30, 2015. Eligible patients were aged 18-63 years and had continuous eligibility with commercial insurance 1 year before and 2 years after DMD initiation. In addition, patients had no evidence of DMD use during the 1-year baseline period.
The investigators used International Classification of Diseases, 9th and 10th Revision, Clinical Modification codes and claims to evaluate patients’ comorbidities and concomitant medications during the study period.
The researchers identified 8,251 eligible patients. Patients had a mean age of 43.2 years, and 75.5% were female. Average baseline Charlson comorbidity score was 0.41. In the 2 years after DMD initiation, common comorbid diagnoses were hyperlipidemia (30.0%), hypertension (28.2%), gastrointestinal disorders (26.2%), depression (25.5%), and anxiety (20.1%).
Common concomitant medications included antibiotics (70.6%); analgesics (57.0%); corticosteroids (52.0%); antidepressants (47.7%); anticonvulsants (46.7%); anxiolytics, sedatives, or hypnotics (43.2%); spasticity medications (36.2%); and muscle relaxants (35.4%).
Most comorbidities and many medications, including bladder and antifatigue medications, were more common among patients aged 55 years and older. Hyperlipidemia, hypertension, and diabetes were more likely in males than in females. Females were more likely to have gastrointestinal disease, depression, thyroid disease, anxiety, lung disease, and arthritis. In addition, females were more likely than males to use many of the concomitant medications.
Dr. Nicholas disclosed grant support from EMD Serono. A coauthor is an employee of Health Services Consulting Corporation and received funding from EMD Serono to conduct the study. Other coauthors are employees of EMD Serono.
REPORTING FROM CMSC 2019
Key clinical point: The effect of comorbidities and concomitant medications on the effectiveness and safety of disease-modifying drugs for multiple sclerosis requires further study.
Major finding: In one analysis, common concomitant medications included antibiotics (70.6%), analgesics (57.0%), corticosteroids (52.0%), antidepressants (47.7%), and anticonvulsants (46.7%).
Study details: An analysis of retrospective administrative claims data from 8,251 patients with MS.
Disclosures: Dr. Nicholas disclosed grant support from EMD Serono. A coauthor is an employee of Health Services Consulting Corporation and received funding from EMD Serono to conduct the study. Other coauthors are employees of EMD Serono.
FDA approves midazolam nasal spray for seizure clusters
The Food and Drug Administration has approved midazolam (Nayzilam) nasal spray for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity – seizure clusters or acute repetitive seizures – that are distinct from a patient’s usual seizure pattern. The treatment is approved for patients with epilepsy aged 12 years and older, according to a news release from UCB, the company that markets the drug.
Nayzilam is the first FDA-approved nasal option for treating seizure clusters, and the nasally administered formulation may allow for people other than healthcare professionals to administer the benzodiazepine in patients who are actively seizing when a seizure cluster occurs, according to the news release.
Nayzilam is designed as a single-use treatment that can be carried with a patient. The drug is a Schedule IV controlled substance.
Nayzilam’s efficacy was studied in a randomized, double-blind, placebo-controlled trial that enrolled patients with epilepsy who had intermittent, stereotypic episodes of frequent seizure activity that were distinct from the patient’s usual seizure pattern.
During an open-label phase, 292 patients in the absence of seizure received two 5-mg doses of Nayzilam 10 minutes apart. During the randomized, double-blind, placebo-controlled phase, 201 patients treated a single seizure cluster episode in an outpatient setting with Nayzilam (134 patients) or placebo (67 patients). If the seizure activity persisted or recurred, patients in both groups had the option to receive a subsequent unblinded dose of Nayzilam between 10 minutes and 6 hours after the initial blinded dose of study drug.
Compared with patients who received placebo, significantly more patients who received Nayzilam had termination of seizures within 10 minutes after the initial blinded dose of study drug (80.6% vs. 70.1%) and the absence of a recurrence of seizures within 6 hours of the initial blinded dose of study drug (58.2% vs. 37.3%). Adverse reactions that occurred in 5% or more of patients who received Nayzilam were somnolence, headache, nasal discomfort, throat irritation, and rhinorrhea.
Respiratory depression was observed with the administration of Nayzilam during clinical trials. Cardiac or respiratory arrest have occurred after administration of midazolam, and midazolam is associated with a high incidence of partial or complete impairment of recall for several hours following an administered dose. Nayzilam is contraindicated in patients with acute narrow-angle glaucoma. In addition, concomitant use of opioids, moderate or strong CYP3A4 inhibitors, or other CNS depressants entails risks. Antiepileptic drugs, including Nayzilam, increase the risk of suicidal thoughts or behavior, according to the announcement.
The Food and Drug Administration has approved midazolam (Nayzilam) nasal spray for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity – seizure clusters or acute repetitive seizures – that are distinct from a patient’s usual seizure pattern. The treatment is approved for patients with epilepsy aged 12 years and older, according to a news release from UCB, the company that markets the drug.
Nayzilam is the first FDA-approved nasal option for treating seizure clusters, and the nasally administered formulation may allow for people other than healthcare professionals to administer the benzodiazepine in patients who are actively seizing when a seizure cluster occurs, according to the news release.
Nayzilam is designed as a single-use treatment that can be carried with a patient. The drug is a Schedule IV controlled substance.
Nayzilam’s efficacy was studied in a randomized, double-blind, placebo-controlled trial that enrolled patients with epilepsy who had intermittent, stereotypic episodes of frequent seizure activity that were distinct from the patient’s usual seizure pattern.
During an open-label phase, 292 patients in the absence of seizure received two 5-mg doses of Nayzilam 10 minutes apart. During the randomized, double-blind, placebo-controlled phase, 201 patients treated a single seizure cluster episode in an outpatient setting with Nayzilam (134 patients) or placebo (67 patients). If the seizure activity persisted or recurred, patients in both groups had the option to receive a subsequent unblinded dose of Nayzilam between 10 minutes and 6 hours after the initial blinded dose of study drug.
Compared with patients who received placebo, significantly more patients who received Nayzilam had termination of seizures within 10 minutes after the initial blinded dose of study drug (80.6% vs. 70.1%) and the absence of a recurrence of seizures within 6 hours of the initial blinded dose of study drug (58.2% vs. 37.3%). Adverse reactions that occurred in 5% or more of patients who received Nayzilam were somnolence, headache, nasal discomfort, throat irritation, and rhinorrhea.
Respiratory depression was observed with the administration of Nayzilam during clinical trials. Cardiac or respiratory arrest have occurred after administration of midazolam, and midazolam is associated with a high incidence of partial or complete impairment of recall for several hours following an administered dose. Nayzilam is contraindicated in patients with acute narrow-angle glaucoma. In addition, concomitant use of opioids, moderate or strong CYP3A4 inhibitors, or other CNS depressants entails risks. Antiepileptic drugs, including Nayzilam, increase the risk of suicidal thoughts or behavior, according to the announcement.
The Food and Drug Administration has approved midazolam (Nayzilam) nasal spray for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity – seizure clusters or acute repetitive seizures – that are distinct from a patient’s usual seizure pattern. The treatment is approved for patients with epilepsy aged 12 years and older, according to a news release from UCB, the company that markets the drug.
Nayzilam is the first FDA-approved nasal option for treating seizure clusters, and the nasally administered formulation may allow for people other than healthcare professionals to administer the benzodiazepine in patients who are actively seizing when a seizure cluster occurs, according to the news release.
Nayzilam is designed as a single-use treatment that can be carried with a patient. The drug is a Schedule IV controlled substance.
Nayzilam’s efficacy was studied in a randomized, double-blind, placebo-controlled trial that enrolled patients with epilepsy who had intermittent, stereotypic episodes of frequent seizure activity that were distinct from the patient’s usual seizure pattern.
During an open-label phase, 292 patients in the absence of seizure received two 5-mg doses of Nayzilam 10 minutes apart. During the randomized, double-blind, placebo-controlled phase, 201 patients treated a single seizure cluster episode in an outpatient setting with Nayzilam (134 patients) or placebo (67 patients). If the seizure activity persisted or recurred, patients in both groups had the option to receive a subsequent unblinded dose of Nayzilam between 10 minutes and 6 hours after the initial blinded dose of study drug.
Compared with patients who received placebo, significantly more patients who received Nayzilam had termination of seizures within 10 minutes after the initial blinded dose of study drug (80.6% vs. 70.1%) and the absence of a recurrence of seizures within 6 hours of the initial blinded dose of study drug (58.2% vs. 37.3%). Adverse reactions that occurred in 5% or more of patients who received Nayzilam were somnolence, headache, nasal discomfort, throat irritation, and rhinorrhea.
Respiratory depression was observed with the administration of Nayzilam during clinical trials. Cardiac or respiratory arrest have occurred after administration of midazolam, and midazolam is associated with a high incidence of partial or complete impairment of recall for several hours following an administered dose. Nayzilam is contraindicated in patients with acute narrow-angle glaucoma. In addition, concomitant use of opioids, moderate or strong CYP3A4 inhibitors, or other CNS depressants entails risks. Antiepileptic drugs, including Nayzilam, increase the risk of suicidal thoughts or behavior, according to the announcement.
Stroke policy recommendations incorporate advances in endovascular therapy
Stroke centers need to collaborate within their regions to assure best practices and optimal access to comprehensive stroke centers as well as newly-designated thrombectomy-capable stroke centers, according to an updated policy statement from the American Stroke Association published in Stroke.
Opeolu Adeoye, MD, associate professor of emergency medicine and neurosurgery at the University of Cincinnati – and chair of the policy statement writing group – and coauthors updated the ASA’s 2005 recommendations for policy makers and public health care agencies to reflect current evidence, the increased availability of endovascular therapy, and new stroke center certifications.
“We have seen monumental advancements in acute stroke care over the past 14 years, and our concept of a comprehensive stroke system of care has evolved as a result,” Dr. Adeoye said in a news release.
While a recommendation to support the initiation of stroke prevention regimens remains unchanged from the 2005 recommendations, the 2019 update emphasizes a need to support long-term adherence to such regimens. To that end, researchers should examine the potential benefits of stroke prevention efforts that incorporate social media, gamification, and other technologies and principles to promote healthy behavior, the authors suggested. Furthermore, technology may allow for the passive surveillance of baseline behaviors and enable researchers to track changes in behavior over time.
Thrombectomy-capable centers
Thrombectomy-capable stroke centers, which have capabilities between those of primary stroke centers and comprehensive stroke centers, provide a relatively new level of acute stroke care. In communities that do not otherwise have access to thrombectomy, these centers play a clear role. In communities with comprehensive stroke centers, their role “is more controversial, and routing plans for patients with a suspected LVO [large vessel occlusion] should always seek the center of highest capability when travel time differences are short,” the statement says.
Timely parenchymal and arterial imaging via CT or MRI are needed to identify the subset of patients who may benefit from thrombectomy. All centers managing stroke patients should develop a plan for the definitive identification and treatment of these patients. Imaging techniques that assess penumbral patterns to identify candidates for endovascular therapy between 6 and 24 hours after patients were last known to be normal “merit broader adoption,” the statement says.
Hospitals without thrombectomy capability should have transfer protocols to allow the rapid treatment of these patients to hospitals with the appropriate level of care. In rural facilities that lack 24/7 imaging and radiology capabilities, this may mean rapid transfer of patients with clinically suspected LVO to hospitals where their work-up may be expedited.
To improve process, centers providing thrombectomy should rigorously track patient flow at all time points from presentation to imaging to intervention. Reperfusion rates, procedural complications, and patient clinical outcomes must be tracked and reported.
Travel times
Triage paradigms and protocols should be developed to ensure that emergency medical service (EMS) providers are able to rapidly identify all patients with a known or suspected stroke and to assess them with a validated and standardized instrument for stroke screening such as FAST (Face, Arm, Speech, Time), Los Angeles Prehospital Stroke Screen, or Cincinnati Prehospital Stroke Scale.
In prehospital patients who screen positive for suspected stroke, a standard prehospital stroke severity assessment tool such as the Cincinnati Stroke Triage Assessment Tool, Rapid Arterial Occlusion Evaluation, Los Angeles Motor Scale, or Field Assessment Stroke Triage for Emergency Destination should be used. “Further research is needed to establish the most effective prehospital stroke severity triage scale,” the authors noted. In all cases, EMS should notify hospitals that a stroke patient is en route.
“When there are several intravenous alteplase–capable hospitals in a well-defined geographic region, extra transportation times to reach a facility capable of endovascular thrombectomy should be limited to no more than 15 minutes in patients with a prehospital stroke severity score suggestive of LVO,” according to the recommendations. “When several hospital options exist within similar travel times, EMS should seek care at the facility capable of offering the highest level of stroke care. Further research is needed to establish travel time parameters for hospital bypass in cases of prehospital suspicion of LVO.”
Outcomes and discharge
Centers should track various treatment and patient outcomes, and all patients discharged to their homes should have appropriate follow-up with specialized stroke services and primary care and be screened for postacute complications.
Government institutions should standardize the organization of stroke care, ensure that stroke patients receive timely care at appropriate hospitals, and facilitate access to secondary prevention and rehabilitation resources after stroke, the authors wrote.
“Programs geared at further improving the knowledge of the public, encouraging primordial and primary prevention, advancing and facilitating acute therapy, improving secondary prevention and recovery from stroke, and reducing disparities in stroke care should be actively developed in a coordinated and collaborative fashion by providers and policymakers at the local, state, and national levels,” the authors concluded. “Such efforts will continue to mitigate the effects of stroke on society.”
Dr. Adeoye had no disclosures. Some coauthors reported research grants and consultant or advisory board positions.
SOURCE: Adeoye O et al. Stroke. 2019 May 20. doi: 10.1161/STR.0000000000000173.
When determining where to transport a patient with stroke, uncertainty about the patient’s diagnosis and eligibility for thrombectomy is a necessary consideration, said Robert A. Harrington, MD, of Stanford University (Calif.), in an accompanying editorial.
In lieu of better data, stroke systems should follow the recommendation of the Mission: Lifeline Severity-based Stroke Triage Algorithm for emergency medical services to avoid more than 15 minutes of additional travel time to transport a patient to a center that can perform endovascular therapy when the patient may be eligible for intravenous tissue plasminogen activator (tPA), said Dr. Harrington.
Delays in initiating tPA could lead to some patients not receiving treatment. “Some patients with suspected LVO [large vessel occlusion] either will not have thrombectomy or will not be eligible for it, and they also run the risk of not receiving any acute reperfusion therapy. Consequently, transport algorithms and models must take into account the uncertainty in prehospital diagnosis when considering the most appropriate facility,” he said.
Forthcoming acute stroke guidelines “will recommend intravenous tPA for all eligible subjects” because administration of tPA before endovascular thrombectomy does not appear to be harmful, Dr. Harrington noted.
Ultimately, approaches to routing patients may vary by region. “It is up to local and regional communities ... to define how best to implement these elements into a stroke system of care that meets their needs and resources and to define the types of hospitals that should qualify as points of entry for patients with suspected LVO strokes,” Dr. Harrington said.
A group convened by the American Heart Association and American Stroke Association is drafting further guiding principles for stroke systems of care in various regional settings.
Dr. Harrington is president-elect of the American Heart Association. He reported receiving research grants from AstraZeneca and Bristol-Myers Squibb.
When determining where to transport a patient with stroke, uncertainty about the patient’s diagnosis and eligibility for thrombectomy is a necessary consideration, said Robert A. Harrington, MD, of Stanford University (Calif.), in an accompanying editorial.
In lieu of better data, stroke systems should follow the recommendation of the Mission: Lifeline Severity-based Stroke Triage Algorithm for emergency medical services to avoid more than 15 minutes of additional travel time to transport a patient to a center that can perform endovascular therapy when the patient may be eligible for intravenous tissue plasminogen activator (tPA), said Dr. Harrington.
Delays in initiating tPA could lead to some patients not receiving treatment. “Some patients with suspected LVO [large vessel occlusion] either will not have thrombectomy or will not be eligible for it, and they also run the risk of not receiving any acute reperfusion therapy. Consequently, transport algorithms and models must take into account the uncertainty in prehospital diagnosis when considering the most appropriate facility,” he said.
Forthcoming acute stroke guidelines “will recommend intravenous tPA for all eligible subjects” because administration of tPA before endovascular thrombectomy does not appear to be harmful, Dr. Harrington noted.
Ultimately, approaches to routing patients may vary by region. “It is up to local and regional communities ... to define how best to implement these elements into a stroke system of care that meets their needs and resources and to define the types of hospitals that should qualify as points of entry for patients with suspected LVO strokes,” Dr. Harrington said.
A group convened by the American Heart Association and American Stroke Association is drafting further guiding principles for stroke systems of care in various regional settings.
Dr. Harrington is president-elect of the American Heart Association. He reported receiving research grants from AstraZeneca and Bristol-Myers Squibb.
When determining where to transport a patient with stroke, uncertainty about the patient’s diagnosis and eligibility for thrombectomy is a necessary consideration, said Robert A. Harrington, MD, of Stanford University (Calif.), in an accompanying editorial.
In lieu of better data, stroke systems should follow the recommendation of the Mission: Lifeline Severity-based Stroke Triage Algorithm for emergency medical services to avoid more than 15 minutes of additional travel time to transport a patient to a center that can perform endovascular therapy when the patient may be eligible for intravenous tissue plasminogen activator (tPA), said Dr. Harrington.
Delays in initiating tPA could lead to some patients not receiving treatment. “Some patients with suspected LVO [large vessel occlusion] either will not have thrombectomy or will not be eligible for it, and they also run the risk of not receiving any acute reperfusion therapy. Consequently, transport algorithms and models must take into account the uncertainty in prehospital diagnosis when considering the most appropriate facility,” he said.
Forthcoming acute stroke guidelines “will recommend intravenous tPA for all eligible subjects” because administration of tPA before endovascular thrombectomy does not appear to be harmful, Dr. Harrington noted.
Ultimately, approaches to routing patients may vary by region. “It is up to local and regional communities ... to define how best to implement these elements into a stroke system of care that meets their needs and resources and to define the types of hospitals that should qualify as points of entry for patients with suspected LVO strokes,” Dr. Harrington said.
A group convened by the American Heart Association and American Stroke Association is drafting further guiding principles for stroke systems of care in various regional settings.
Dr. Harrington is president-elect of the American Heart Association. He reported receiving research grants from AstraZeneca and Bristol-Myers Squibb.
Stroke centers need to collaborate within their regions to assure best practices and optimal access to comprehensive stroke centers as well as newly-designated thrombectomy-capable stroke centers, according to an updated policy statement from the American Stroke Association published in Stroke.
Opeolu Adeoye, MD, associate professor of emergency medicine and neurosurgery at the University of Cincinnati – and chair of the policy statement writing group – and coauthors updated the ASA’s 2005 recommendations for policy makers and public health care agencies to reflect current evidence, the increased availability of endovascular therapy, and new stroke center certifications.
“We have seen monumental advancements in acute stroke care over the past 14 years, and our concept of a comprehensive stroke system of care has evolved as a result,” Dr. Adeoye said in a news release.
While a recommendation to support the initiation of stroke prevention regimens remains unchanged from the 2005 recommendations, the 2019 update emphasizes a need to support long-term adherence to such regimens. To that end, researchers should examine the potential benefits of stroke prevention efforts that incorporate social media, gamification, and other technologies and principles to promote healthy behavior, the authors suggested. Furthermore, technology may allow for the passive surveillance of baseline behaviors and enable researchers to track changes in behavior over time.
Thrombectomy-capable centers
Thrombectomy-capable stroke centers, which have capabilities between those of primary stroke centers and comprehensive stroke centers, provide a relatively new level of acute stroke care. In communities that do not otherwise have access to thrombectomy, these centers play a clear role. In communities with comprehensive stroke centers, their role “is more controversial, and routing plans for patients with a suspected LVO [large vessel occlusion] should always seek the center of highest capability when travel time differences are short,” the statement says.
Timely parenchymal and arterial imaging via CT or MRI are needed to identify the subset of patients who may benefit from thrombectomy. All centers managing stroke patients should develop a plan for the definitive identification and treatment of these patients. Imaging techniques that assess penumbral patterns to identify candidates for endovascular therapy between 6 and 24 hours after patients were last known to be normal “merit broader adoption,” the statement says.
Hospitals without thrombectomy capability should have transfer protocols to allow the rapid treatment of these patients to hospitals with the appropriate level of care. In rural facilities that lack 24/7 imaging and radiology capabilities, this may mean rapid transfer of patients with clinically suspected LVO to hospitals where their work-up may be expedited.
To improve process, centers providing thrombectomy should rigorously track patient flow at all time points from presentation to imaging to intervention. Reperfusion rates, procedural complications, and patient clinical outcomes must be tracked and reported.
Travel times
Triage paradigms and protocols should be developed to ensure that emergency medical service (EMS) providers are able to rapidly identify all patients with a known or suspected stroke and to assess them with a validated and standardized instrument for stroke screening such as FAST (Face, Arm, Speech, Time), Los Angeles Prehospital Stroke Screen, or Cincinnati Prehospital Stroke Scale.
In prehospital patients who screen positive for suspected stroke, a standard prehospital stroke severity assessment tool such as the Cincinnati Stroke Triage Assessment Tool, Rapid Arterial Occlusion Evaluation, Los Angeles Motor Scale, or Field Assessment Stroke Triage for Emergency Destination should be used. “Further research is needed to establish the most effective prehospital stroke severity triage scale,” the authors noted. In all cases, EMS should notify hospitals that a stroke patient is en route.
“When there are several intravenous alteplase–capable hospitals in a well-defined geographic region, extra transportation times to reach a facility capable of endovascular thrombectomy should be limited to no more than 15 minutes in patients with a prehospital stroke severity score suggestive of LVO,” according to the recommendations. “When several hospital options exist within similar travel times, EMS should seek care at the facility capable of offering the highest level of stroke care. Further research is needed to establish travel time parameters for hospital bypass in cases of prehospital suspicion of LVO.”
Outcomes and discharge
Centers should track various treatment and patient outcomes, and all patients discharged to their homes should have appropriate follow-up with specialized stroke services and primary care and be screened for postacute complications.
Government institutions should standardize the organization of stroke care, ensure that stroke patients receive timely care at appropriate hospitals, and facilitate access to secondary prevention and rehabilitation resources after stroke, the authors wrote.
“Programs geared at further improving the knowledge of the public, encouraging primordial and primary prevention, advancing and facilitating acute therapy, improving secondary prevention and recovery from stroke, and reducing disparities in stroke care should be actively developed in a coordinated and collaborative fashion by providers and policymakers at the local, state, and national levels,” the authors concluded. “Such efforts will continue to mitigate the effects of stroke on society.”
Dr. Adeoye had no disclosures. Some coauthors reported research grants and consultant or advisory board positions.
SOURCE: Adeoye O et al. Stroke. 2019 May 20. doi: 10.1161/STR.0000000000000173.
Stroke centers need to collaborate within their regions to assure best practices and optimal access to comprehensive stroke centers as well as newly-designated thrombectomy-capable stroke centers, according to an updated policy statement from the American Stroke Association published in Stroke.
Opeolu Adeoye, MD, associate professor of emergency medicine and neurosurgery at the University of Cincinnati – and chair of the policy statement writing group – and coauthors updated the ASA’s 2005 recommendations for policy makers and public health care agencies to reflect current evidence, the increased availability of endovascular therapy, and new stroke center certifications.
“We have seen monumental advancements in acute stroke care over the past 14 years, and our concept of a comprehensive stroke system of care has evolved as a result,” Dr. Adeoye said in a news release.
While a recommendation to support the initiation of stroke prevention regimens remains unchanged from the 2005 recommendations, the 2019 update emphasizes a need to support long-term adherence to such regimens. To that end, researchers should examine the potential benefits of stroke prevention efforts that incorporate social media, gamification, and other technologies and principles to promote healthy behavior, the authors suggested. Furthermore, technology may allow for the passive surveillance of baseline behaviors and enable researchers to track changes in behavior over time.
Thrombectomy-capable centers
Thrombectomy-capable stroke centers, which have capabilities between those of primary stroke centers and comprehensive stroke centers, provide a relatively new level of acute stroke care. In communities that do not otherwise have access to thrombectomy, these centers play a clear role. In communities with comprehensive stroke centers, their role “is more controversial, and routing plans for patients with a suspected LVO [large vessel occlusion] should always seek the center of highest capability when travel time differences are short,” the statement says.
Timely parenchymal and arterial imaging via CT or MRI are needed to identify the subset of patients who may benefit from thrombectomy. All centers managing stroke patients should develop a plan for the definitive identification and treatment of these patients. Imaging techniques that assess penumbral patterns to identify candidates for endovascular therapy between 6 and 24 hours after patients were last known to be normal “merit broader adoption,” the statement says.
Hospitals without thrombectomy capability should have transfer protocols to allow the rapid treatment of these patients to hospitals with the appropriate level of care. In rural facilities that lack 24/7 imaging and radiology capabilities, this may mean rapid transfer of patients with clinically suspected LVO to hospitals where their work-up may be expedited.
To improve process, centers providing thrombectomy should rigorously track patient flow at all time points from presentation to imaging to intervention. Reperfusion rates, procedural complications, and patient clinical outcomes must be tracked and reported.
Travel times
Triage paradigms and protocols should be developed to ensure that emergency medical service (EMS) providers are able to rapidly identify all patients with a known or suspected stroke and to assess them with a validated and standardized instrument for stroke screening such as FAST (Face, Arm, Speech, Time), Los Angeles Prehospital Stroke Screen, or Cincinnati Prehospital Stroke Scale.
In prehospital patients who screen positive for suspected stroke, a standard prehospital stroke severity assessment tool such as the Cincinnati Stroke Triage Assessment Tool, Rapid Arterial Occlusion Evaluation, Los Angeles Motor Scale, or Field Assessment Stroke Triage for Emergency Destination should be used. “Further research is needed to establish the most effective prehospital stroke severity triage scale,” the authors noted. In all cases, EMS should notify hospitals that a stroke patient is en route.
“When there are several intravenous alteplase–capable hospitals in a well-defined geographic region, extra transportation times to reach a facility capable of endovascular thrombectomy should be limited to no more than 15 minutes in patients with a prehospital stroke severity score suggestive of LVO,” according to the recommendations. “When several hospital options exist within similar travel times, EMS should seek care at the facility capable of offering the highest level of stroke care. Further research is needed to establish travel time parameters for hospital bypass in cases of prehospital suspicion of LVO.”
Outcomes and discharge
Centers should track various treatment and patient outcomes, and all patients discharged to their homes should have appropriate follow-up with specialized stroke services and primary care and be screened for postacute complications.
Government institutions should standardize the organization of stroke care, ensure that stroke patients receive timely care at appropriate hospitals, and facilitate access to secondary prevention and rehabilitation resources after stroke, the authors wrote.
“Programs geared at further improving the knowledge of the public, encouraging primordial and primary prevention, advancing and facilitating acute therapy, improving secondary prevention and recovery from stroke, and reducing disparities in stroke care should be actively developed in a coordinated and collaborative fashion by providers and policymakers at the local, state, and national levels,” the authors concluded. “Such efforts will continue to mitigate the effects of stroke on society.”
Dr. Adeoye had no disclosures. Some coauthors reported research grants and consultant or advisory board positions.
SOURCE: Adeoye O et al. Stroke. 2019 May 20. doi: 10.1161/STR.0000000000000173.
FROM STROKE
Sugary drink intake may be associated with MS severity
PHILADELPHIA – presented at the annual meeting of the American Academy of Neurology. Overall diet quality, however, is not associated with disability, the study showed.
The results do not establish that sugary drinks cause disability, and the potential association needs to be confirmed in larger, longitudinal studies, the researchers said. Nevertheless, “we do know that sodas have no nutritional value, and people with MS may want to consider reducing or eliminating them from their diet,” study lead author Elisa Meier-Gerdingh, MD, of St. Josef Hospital in Bochum, Germany, said in a written statement.
Diet may influence metabolic comorbidities, immune function, oxidative stress, and gut microbiota in patients with MS, but data about diet’s effects on MS progression are limited, the researchers said.
To examine dietary intake and disability in patients with MS, Dr. Meier-Gerdingh and her colleagues conducted a cross-sectional study of 135 participants with MS who were treated at a large referral center in Germany. Participants had a mean age of 44.6 years and mean body mass index of 24.5. Mean disease duration was 13.8 years, and 73% were women. Participants completed a 102-item food frequency questionnaire, which the investigators used to calculate each participant’s Dietary Approaches to Stop Hypertension (DASH) score. The score is a composite measure of dietary quality that favorably scores intake of fruits, vegetables, nuts and legumes, whole grains, and dairy and unfavorably scores intake of sodium, sugar-sweetened beverages, and red and processed meats.
“We chose to study the DASH diet because adherence to the DASH diet is associated with lower risk of other chronic diseases like high blood pressure, diabetes, and cardiovascular diseases,” Dr. Meier-Gerdingh said.
The researchers considered severe disability to be an Expanded Disability Status Scale (EDSS) score of 6 or greater. They assessed the association between overall DASH scores and disability status using logistic regression models that adjusted for age, sex, body mass index, smoking, and symptom duration. They also assessed the association between disability and each nutritional component of the DASH score.
In all, 30 participants had severe disability. “Overall DASH scores were not associated with disability status,” Dr. Meier-Gerdingh and her colleagues said. When they looked at individual DASH score components, patients with higher intakes of sugar-sweetened beverages had a higher risk of severe disability (P for trend = .01). Participants in the highest quartile consumed about 290 calories of sugar-sweetened beverages per day on average, compared with 7 calories per day for patients in the lowest quartile. The top quartile had an average EDSS of 4.1, and the bottom quartile had an average EDSS of 3.4. Other DASH score components were not associated with disability status.
Dr. Meier-Gerdingh had no disclosures. Her coauthors reported research support and personal compensation from pharmaceutical companies.
SOURCE: Meier-Gerdingh E et al. AAN 2019, Abstract P4.2-063.
PHILADELPHIA – presented at the annual meeting of the American Academy of Neurology. Overall diet quality, however, is not associated with disability, the study showed.
The results do not establish that sugary drinks cause disability, and the potential association needs to be confirmed in larger, longitudinal studies, the researchers said. Nevertheless, “we do know that sodas have no nutritional value, and people with MS may want to consider reducing or eliminating them from their diet,” study lead author Elisa Meier-Gerdingh, MD, of St. Josef Hospital in Bochum, Germany, said in a written statement.
Diet may influence metabolic comorbidities, immune function, oxidative stress, and gut microbiota in patients with MS, but data about diet’s effects on MS progression are limited, the researchers said.
To examine dietary intake and disability in patients with MS, Dr. Meier-Gerdingh and her colleagues conducted a cross-sectional study of 135 participants with MS who were treated at a large referral center in Germany. Participants had a mean age of 44.6 years and mean body mass index of 24.5. Mean disease duration was 13.8 years, and 73% were women. Participants completed a 102-item food frequency questionnaire, which the investigators used to calculate each participant’s Dietary Approaches to Stop Hypertension (DASH) score. The score is a composite measure of dietary quality that favorably scores intake of fruits, vegetables, nuts and legumes, whole grains, and dairy and unfavorably scores intake of sodium, sugar-sweetened beverages, and red and processed meats.
“We chose to study the DASH diet because adherence to the DASH diet is associated with lower risk of other chronic diseases like high blood pressure, diabetes, and cardiovascular diseases,” Dr. Meier-Gerdingh said.
The researchers considered severe disability to be an Expanded Disability Status Scale (EDSS) score of 6 or greater. They assessed the association between overall DASH scores and disability status using logistic regression models that adjusted for age, sex, body mass index, smoking, and symptom duration. They also assessed the association between disability and each nutritional component of the DASH score.
In all, 30 participants had severe disability. “Overall DASH scores were not associated with disability status,” Dr. Meier-Gerdingh and her colleagues said. When they looked at individual DASH score components, patients with higher intakes of sugar-sweetened beverages had a higher risk of severe disability (P for trend = .01). Participants in the highest quartile consumed about 290 calories of sugar-sweetened beverages per day on average, compared with 7 calories per day for patients in the lowest quartile. The top quartile had an average EDSS of 4.1, and the bottom quartile had an average EDSS of 3.4. Other DASH score components were not associated with disability status.
Dr. Meier-Gerdingh had no disclosures. Her coauthors reported research support and personal compensation from pharmaceutical companies.
SOURCE: Meier-Gerdingh E et al. AAN 2019, Abstract P4.2-063.
PHILADELPHIA – presented at the annual meeting of the American Academy of Neurology. Overall diet quality, however, is not associated with disability, the study showed.
The results do not establish that sugary drinks cause disability, and the potential association needs to be confirmed in larger, longitudinal studies, the researchers said. Nevertheless, “we do know that sodas have no nutritional value, and people with MS may want to consider reducing or eliminating them from their diet,” study lead author Elisa Meier-Gerdingh, MD, of St. Josef Hospital in Bochum, Germany, said in a written statement.
Diet may influence metabolic comorbidities, immune function, oxidative stress, and gut microbiota in patients with MS, but data about diet’s effects on MS progression are limited, the researchers said.
To examine dietary intake and disability in patients with MS, Dr. Meier-Gerdingh and her colleagues conducted a cross-sectional study of 135 participants with MS who were treated at a large referral center in Germany. Participants had a mean age of 44.6 years and mean body mass index of 24.5. Mean disease duration was 13.8 years, and 73% were women. Participants completed a 102-item food frequency questionnaire, which the investigators used to calculate each participant’s Dietary Approaches to Stop Hypertension (DASH) score. The score is a composite measure of dietary quality that favorably scores intake of fruits, vegetables, nuts and legumes, whole grains, and dairy and unfavorably scores intake of sodium, sugar-sweetened beverages, and red and processed meats.
“We chose to study the DASH diet because adherence to the DASH diet is associated with lower risk of other chronic diseases like high blood pressure, diabetes, and cardiovascular diseases,” Dr. Meier-Gerdingh said.
The researchers considered severe disability to be an Expanded Disability Status Scale (EDSS) score of 6 or greater. They assessed the association between overall DASH scores and disability status using logistic regression models that adjusted for age, sex, body mass index, smoking, and symptom duration. They also assessed the association between disability and each nutritional component of the DASH score.
In all, 30 participants had severe disability. “Overall DASH scores were not associated with disability status,” Dr. Meier-Gerdingh and her colleagues said. When they looked at individual DASH score components, patients with higher intakes of sugar-sweetened beverages had a higher risk of severe disability (P for trend = .01). Participants in the highest quartile consumed about 290 calories of sugar-sweetened beverages per day on average, compared with 7 calories per day for patients in the lowest quartile. The top quartile had an average EDSS of 4.1, and the bottom quartile had an average EDSS of 3.4. Other DASH score components were not associated with disability status.
Dr. Meier-Gerdingh had no disclosures. Her coauthors reported research support and personal compensation from pharmaceutical companies.
SOURCE: Meier-Gerdingh E et al. AAN 2019, Abstract P4.2-063.
REPORTING FROM AAN 2019
Insomnia symptoms correlate with seizure frequency
PHILADELPHIA – . Insomnia symptoms are not associated with epilepsy type, number of antiepileptic drugs (AEDs), or AED standardized dose, however.
“Given the potential benefits of sleep therapies on epilepsy outcomes, routine screening of insomnia symptoms is warranted,” said lead study author Thapanee Somboon, MD, a researcher at the sleep disorders center at Cleveland Clinic Neurological Institute in Ohio and at Prasat Neurological Institute in Bangkok.
Insomnia is common and associated with depression in patients with epilepsy, but prior studies that looked at the relationship between insomnia and epilepsy-related characteristics yielded limited and conflicting results, according to Dr. Somboon.
To evaluate potential associations between insomnia and epilepsy, Dr. Somboon and colleagues conducted a prospective analysis of data from 270 patients with epilepsy who presented to the Cleveland Clinic Epilepsy Center for an initial evaluation between January and August 2018. The patients completed the Insomnia Severity Index (ISI). An ISI score of 8 or greater indicated clinical insomnia symptoms, and an ISI score of 15 or greater indicated moderate or severe insomnia symptoms.
The researchers used Spearman’s correlation and the Kruskal-Wallis test to evaluate associations among insomnia symptoms and AED standardized dose, monthly seizure frequency, Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Questionnaire (GAD-7), and Quality of Life in Epilepsy-10 (QOLIE10).
Among the 270 patients, the average age was 43.5 years, 58% were female, 74% had focal epilepsy, and 26% had one or more seizures per month. The population’s median ISI score was 7. Nearly half had an ISI score of 8 or greater, and 23% had an ISI score of 15 or greater.
“A positive correlation was found between ISI and PHQ-9 (r = 0.64, P less than .001), GAD-7 (r = 0.68, P less than .001), QOLIE (r = 0.55, P less than .001), and monthly seizure frequency (r = 0.31, P less than .001),” the researchers reported. Insomnia symptoms had a significantly stronger correlation with PHQ-9 and GAD-7 than with seizure frequency.
Dr. Somboon had no disclosures. A coinvestigator has received research support from Jazz Pharmaceuticals.
SOURCE: Somboon T et al. AAN 2019, Abstract P3.6-026.
PHILADELPHIA – . Insomnia symptoms are not associated with epilepsy type, number of antiepileptic drugs (AEDs), or AED standardized dose, however.
“Given the potential benefits of sleep therapies on epilepsy outcomes, routine screening of insomnia symptoms is warranted,” said lead study author Thapanee Somboon, MD, a researcher at the sleep disorders center at Cleveland Clinic Neurological Institute in Ohio and at Prasat Neurological Institute in Bangkok.
Insomnia is common and associated with depression in patients with epilepsy, but prior studies that looked at the relationship between insomnia and epilepsy-related characteristics yielded limited and conflicting results, according to Dr. Somboon.
To evaluate potential associations between insomnia and epilepsy, Dr. Somboon and colleagues conducted a prospective analysis of data from 270 patients with epilepsy who presented to the Cleveland Clinic Epilepsy Center for an initial evaluation between January and August 2018. The patients completed the Insomnia Severity Index (ISI). An ISI score of 8 or greater indicated clinical insomnia symptoms, and an ISI score of 15 or greater indicated moderate or severe insomnia symptoms.
The researchers used Spearman’s correlation and the Kruskal-Wallis test to evaluate associations among insomnia symptoms and AED standardized dose, monthly seizure frequency, Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Questionnaire (GAD-7), and Quality of Life in Epilepsy-10 (QOLIE10).
Among the 270 patients, the average age was 43.5 years, 58% were female, 74% had focal epilepsy, and 26% had one or more seizures per month. The population’s median ISI score was 7. Nearly half had an ISI score of 8 or greater, and 23% had an ISI score of 15 or greater.
“A positive correlation was found between ISI and PHQ-9 (r = 0.64, P less than .001), GAD-7 (r = 0.68, P less than .001), QOLIE (r = 0.55, P less than .001), and monthly seizure frequency (r = 0.31, P less than .001),” the researchers reported. Insomnia symptoms had a significantly stronger correlation with PHQ-9 and GAD-7 than with seizure frequency.
Dr. Somboon had no disclosures. A coinvestigator has received research support from Jazz Pharmaceuticals.
SOURCE: Somboon T et al. AAN 2019, Abstract P3.6-026.
PHILADELPHIA – . Insomnia symptoms are not associated with epilepsy type, number of antiepileptic drugs (AEDs), or AED standardized dose, however.
“Given the potential benefits of sleep therapies on epilepsy outcomes, routine screening of insomnia symptoms is warranted,” said lead study author Thapanee Somboon, MD, a researcher at the sleep disorders center at Cleveland Clinic Neurological Institute in Ohio and at Prasat Neurological Institute in Bangkok.
Insomnia is common and associated with depression in patients with epilepsy, but prior studies that looked at the relationship between insomnia and epilepsy-related characteristics yielded limited and conflicting results, according to Dr. Somboon.
To evaluate potential associations between insomnia and epilepsy, Dr. Somboon and colleagues conducted a prospective analysis of data from 270 patients with epilepsy who presented to the Cleveland Clinic Epilepsy Center for an initial evaluation between January and August 2018. The patients completed the Insomnia Severity Index (ISI). An ISI score of 8 or greater indicated clinical insomnia symptoms, and an ISI score of 15 or greater indicated moderate or severe insomnia symptoms.
The researchers used Spearman’s correlation and the Kruskal-Wallis test to evaluate associations among insomnia symptoms and AED standardized dose, monthly seizure frequency, Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Questionnaire (GAD-7), and Quality of Life in Epilepsy-10 (QOLIE10).
Among the 270 patients, the average age was 43.5 years, 58% were female, 74% had focal epilepsy, and 26% had one or more seizures per month. The population’s median ISI score was 7. Nearly half had an ISI score of 8 or greater, and 23% had an ISI score of 15 or greater.
“A positive correlation was found between ISI and PHQ-9 (r = 0.64, P less than .001), GAD-7 (r = 0.68, P less than .001), QOLIE (r = 0.55, P less than .001), and monthly seizure frequency (r = 0.31, P less than .001),” the researchers reported. Insomnia symptoms had a significantly stronger correlation with PHQ-9 and GAD-7 than with seizure frequency.
Dr. Somboon had no disclosures. A coinvestigator has received research support from Jazz Pharmaceuticals.
SOURCE: Somboon T et al. AAN 2019, Abstract P3.6-026.
REPORTING FROM AAN 2019