User login
Neutrophils may decline in patients on fingolimod
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
SEATTLE –
A decrease in neutrophils over 6 months in a cohort of fingolimod treatment–experienced patients “was a surprise, at least to me,” said study investigator Bruce Cree, MD, PhD, professor of neurology at UCSF Weill Institute for Neurosciences, University of California, San Francisco. Why levels of these innate immune cells decreased in patients who had been on the drug for years “remains to be understood,” Dr. Cree said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “This is something that deserves further investigation ... to understand if that neutrophil count will continue to drop down over time or whether it ultimately plateaus.”
The decline in neutrophils in this cohort of patients continuously treated for at least 2 years was “only about 9%,” from an average of 3,698.56 cells per microliter at study baseline to 3,336.13 cells per microliter at 6 months.
Among fingolimod-naive patients who initiated treatment during the study, neutrophils decreased from 4,058.48 cells per microliter at baseline to 3,475.09 cells per microliter at 6 months, about 14%.
In the treatment-experienced patients, other immune cell subsets remained relatively stable over the 6-month period.
“If we are trying to understand the impact of fingolimod ultimately on propensity for development of opportunistic infection, of course we are focused almost exclusively on adaptive immunity,” Dr. Cree said. “But perhaps we are forgetting that innate immunity might be also extremely important for protecting ourselves against infection.”
The FLUENT study
Dr. Cree presented interim, 6-month data from the ongoing, open-label FLUENT study, which is a 12-month, prospective, multicenter, nonrandomized study to assess changes in the immune cell profiles of patients with relapsing MS who receive fingolimod. The study includes a cohort of treatment-experienced patients and a cohort of treatment-naive patients.
Fingolimod is a once-daily oral sphingosine 1–phosphate receptor modulator that prevents egress of lymphocytes from lymph nodes. Since its FDA approval in 2010, rare opportunistic infections, including progressive multifocal leukoencephalopathy (PML), have been reported in patients taking fingolimod.
Investigators did not assess changes in innate and adaptive components of the immune system during fingolimod treatment in the pivotal clinical trials, and the relationship between anti-JCV antibody index and immune cell subsets during fingolimod treatment is not known. Immunologic profiling may help gauge patients’ treatment response and risk of infection.
The FLUENT study’s primary outcome is change from baseline to month 6 in peripheral blood cellular components of the innate and adaptive immune system. Secondary endpoints include change in the immune cell subtype profile at months 3 and 12; anti-JCV antibody status at months 3, 6, and 12; change in anti-JCV antibody index at months 3, 6, and 12; and clinical variables. In addition, the investigators plan to examine changes in serum neurofilament light chain (NfL) levels at months 3, 6, and 12.
FLUENT includes a cohort of fingolimod-naive patients and a cohort of patients who have received continuous, commercially available fingolimod 0.5 mg/day for at least 2 years and plan to continue the drug during the 1-year study. The interim analysis included data from 166 fingolimod-naive patients (median age, 41 years; 77.7% female) and 216 fingolimod-experienced patients (median age, 50 years; 73.1% female). About 70% of patients in the fingolimod-naive cohort had had a relapse in the past 2 years, compared with about 22% of patients in the treatment-experienced cohort. Investigators began enrolling patients in September 2017.
Immune cell subsets
In the fingolimod-naive cohort, changes in immune cell subsets were expected and characteristic. Overall CD4+ count declined from baseline to month 6, and the decrease was “driven primarily by a decline in CD4+ naive T cells and CD4+ central memory T cells.” CD4+ effector memory cells, CD4+ Th1 cells, CD4+ Th2 cells, and CD4+ Th17 cells were less affected. “The effector cells do not have an expression of CCR7 [C-C chemokine receptor type 7] so they tend not to hone to the lymph nodes anyway,” Dr. Cree said.
CD8+ cells followed a similar pattern. “The overall count goes down, but perhaps not as much as with the CD4+ cells. The central memory and naive cells are affected a little bit more than the effector memory cells,” Dr. Cree said. “Then we see a comparable pattern with B cells. The absolute CD19+ counts go down. They’re driven by a decline in the naive cells. ... with less of a decline in memory cells and almost no decline in regulatory cells.”
Among innate immune cells, monocytes increased slightly, neutrophils declined, as expected, and natural killer cells declined slightly.
“When you turn your attention to ... those patients who have been on fingolimod, you do not see these changes for the lymphocytes,” Dr. Cree said. “Those lymphocytes are already sequestered, and we are really not seeing much of a change over time at all.”
A measure of CNS injury
In the treatment-naive cohort, serum neurofilament light chain (NfL) declined, but this measure did not change by much in the treatment-experienced cohort.
Among patients already on fingolimod, the serum NfL reduction “that would be anticipated as a therapeutic benefit from fingolimod is already being realized,” he said.
The serum NfL levels in the treatment-naive cohort at 6 months were similar to those of the treatment-experienced cohort at baseline, which indicates that “the impact of fingolimod in reducing circulating neurofilament – a marker of central nervous system injury – is seen within 6 months of treatment and likely persists as patients continue on fingolimod therapy,” Dr. Cree said.
Baseline anti-JCV antibody index was about the same for the treatment-naive and treatment-experienced cohorts (1.28 vs. 1.39, respectively), and this measure did not meaningfully change over 6 months in either cohort.
Adverse events
No new adverse events were identified in this interim analysis. Most common adverse events occurred more frequently in the treatment-naive cohort than in the treatment-experienced cohort, including headache (7.2% vs. 1.9%), upper respiratory tract infection (4.2% vs. 1.9%), pain in extremity (4.2% vs. 1.4%), lymphopenia (4.8% vs. 0.5%), anxiety (3.6% vs. 1.4%), fatigue (3.6% vs. 1.4%), nausea (3.0% vs. 0.9%), dizziness (3.0% vs. 0.5%), hypoesthesia (3.0% vs. 0.5%), and tremor (3.0% vs. 0%). An exception was falls, which occurred in 3.0% of the treatment-naive cohort and 4.6% of the treatment-experienced cohort.
Serious adverse events were about equal between the two groups (4.2% of the treatment-naive group and 5.1% of the treatment-experienced group), and adverse events leading to treatment discontinuation were more common in the fingolimod-naive cohort (10.2% vs. 5.6%).
Novartis funded the study, and four of the authors are Novartis employees. Dr. Cree disclosed consulting fees from Novartis and other pharmaceutical companies. His coauthors disclosed consulting fees, speaking fees, research support, and serving on advisory boards for pharmaceutical companies, including Novartis.
SOURCE: Mao-Draayer Y et al. CMSC 2019. Abstract DXM03.
REPORTING FROM CMSC 2019
FDA approves first treatment for neuromyelitis optica spectrum disorder
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
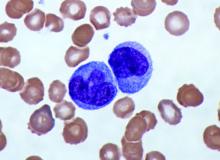
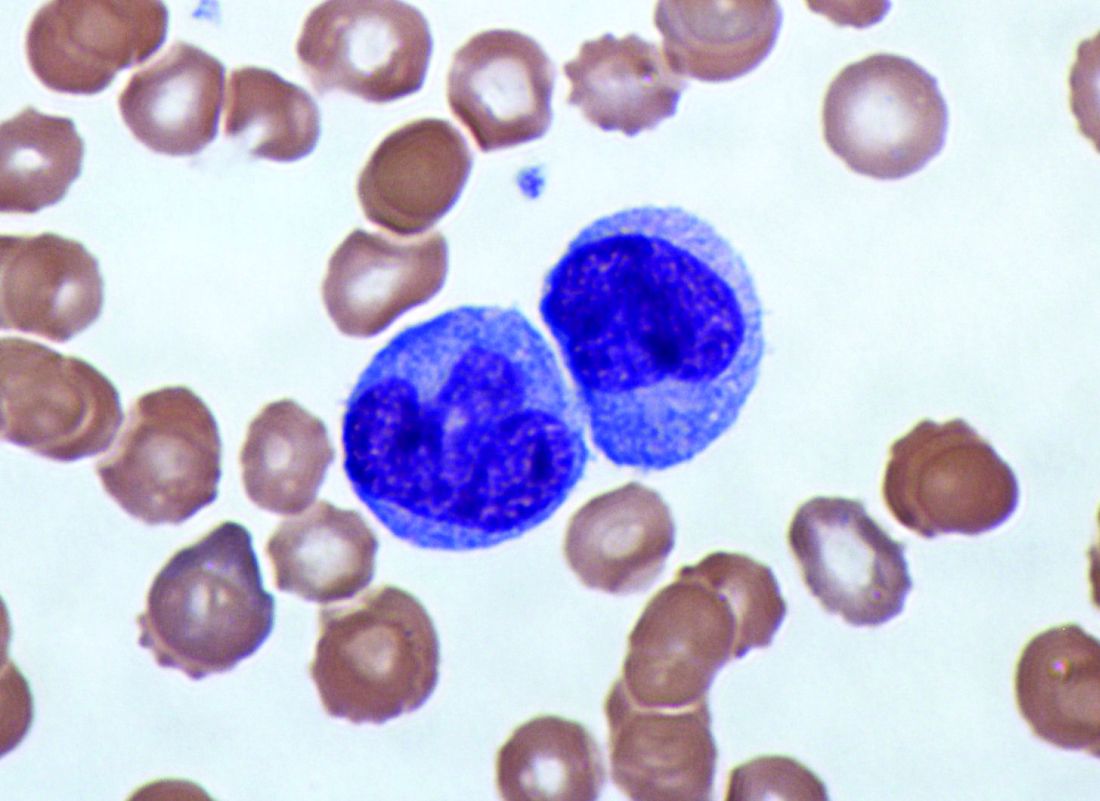
Elevated monocyte count predicts poor outcomes in idiopathic pulmonary fibrosis
, including hypertrophic cardiomyopathy, systemic sclerosis, and myelofibrosis, according to research published in The Lancet Respiratory Medicine.
The data indicate that “a single threshold value of absolute monocyte counts of 0.95 K/mcL could be used to identify high-risk patients with a fibrotic disease,” said Madeleine K. D. Scott, a researcher at Stanford (Calif.) University, and coauthors. The results “suggest that monocyte count should be incorporated into the clinical assessment” and may “enable more conscientious allocation of scarce resources, including lung transplantations,” they said.
While other published biomarkers – including gene panels and multicytokine signatures – may be expensive and not readily available, “absolute monocyte count is routinely measured as part of a complete blood count, an inexpensive test used in clinical practice worldwide,” the authors said.
Further study of monocytes’ mechanistic role in fibrosis ultimately could point to new treatment approaches.
A retrospective multicenter cohort study
To assess whether immune cells may identify patients with idiopathic pulmonary fibrosis at greater risk of poor outcomes, Ms. Scott and her collaborators conducted a retrospective multicenter cohort study.
They first analyzed transcriptome data from 120 peripheral blood mononuclear cell samples of patients with idiopathic pulmonary fibrosis, which they obtained from the Gene Expression Omnibus at the National Center for Biotechnology Information. They used statistical deconvolution to estimate percentages of 13 immune cell types and examined their associations with transplant-free survival. Their discovery analysis found that estimated CD14+ classical monocyte percentages above the mean correlated with shorter transplant-free survival times (hazard ratio, 1.82), but percentages of T cells and B cells did not.
The researchers then validated these results using samples from patients with idiopathic pulmonary fibrosis in two independent cohorts. In the COMET validation cohort, which included 45 patients with idiopathic pulmonary fibrosis whose monocyte counts were measured using flow cytometry, higher monocyte counts were significantly associated with greater risk of disease progression. In the Yale cohort, which included 15 patients with idiopathic pulmonary fibrosis, the 6 patients who were classified as high risk on the basis of a 52-gene signature had more CD14+ monocytes than the 9 low-risk patients did.
In addition, Ms. Scott and her collaborators looked at complete blood count values in the electronic health records of 45,068 patients with idiopathic pulmonary fibrosis, systemic sclerosis, hypertrophic cardiomyopathy, or myelofibrosis in Stanford, Northwestern, Vanderbilt, and Optum Clinformatics Data Mart cohorts.
Among patients in the COMET, Stanford, and Northwestern datasets, monocyte counts of 0.95 K/mcL or greater were associated with mortality after adjustment for forced vital capacity (HR, 2.47) and the gender, age, and physiology index (HR, 2.06). Data from 7,459 patients with idiopathic pulmonary fibrosis “showed that patients with monocyte counts of 0.95 K/mcL or greater were at increased risk of mortality with lung transplantation as a censoring event, after adjusting for age at diagnosis and sex” in the Stanford (HR, 2.30), Vanderbilt (HR, 1.52), and Optum (HR, 1.74) cohorts. “Likewise, higher absolute monocyte count was associated with shortened survival in patients with hypertrophic cardiomyopathy across all three cohorts, and in patients with systemic sclerosis or myelofibrosis in two of the three cohorts,” the researchers said.
The study was funded by grants from the Bill & Melinda Gates Foundation, U.S. National Institute of Allergy and Infectious Diseases, and U.S. National Library of Medicine. Ms. Scott had no competing interests. Coauthors disclosed grants, compensation, and support from foundations, agencies, and companies.
SOURCE: Scott MKD et al. Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600(18)30508-3.
The study by Scott et al. provides evidence that monocyte count may be a “novel, simple, and inexpensive prognostic biomarker in idiopathic pulmonary fibrosis,” according to an accompanying editorial.
Progress has been made in the treatment of idiopathic pulmonary fibrosis, but patient prognosis remains “challenging to predict,” wrote Michael Kreuter, MD, of University of Heidelberg, Germany, and Toby M. Maher, MB, MSc, PhD, of Royal Brompton Hospital in London and Imperial College London. “One lesson that can be learned from other respiratory disorders is that routinely measured cellular biomarkers, such as blood eosinophil counts in chronic obstructive pulmonary disease (COPD), can predict treatment responses” (Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600[19]30050-5).
Increased blood monocyte counts in idiopathic pulmonary fibrosis may reflect disease activity, which “could explain the outcome differences,” said Dr. Kreuter and Dr. Maher. “As highlighted by the investigators themselves, before introducing assessment of monocyte counts as part of routine clinical care for individuals with idiopathic pulmonary fibrosis, the limitations of this research should be taken into account. These include uncertainty around diagnosis and disease severity in a substantial subset of the patients, and the unknown effect of medical therapies (including corticosteroids and immunosuppressant and antifibrotic drugs) on monocyte counts and prognosis.” Researchers should validate the clinical value of blood monocyte counts in existing and future cohorts and evaluate the biomarker in clinical trials.
The editorialists have received compensation and funding from various pharmaceutical companies.
The study by Scott et al. provides evidence that monocyte count may be a “novel, simple, and inexpensive prognostic biomarker in idiopathic pulmonary fibrosis,” according to an accompanying editorial.
Progress has been made in the treatment of idiopathic pulmonary fibrosis, but patient prognosis remains “challenging to predict,” wrote Michael Kreuter, MD, of University of Heidelberg, Germany, and Toby M. Maher, MB, MSc, PhD, of Royal Brompton Hospital in London and Imperial College London. “One lesson that can be learned from other respiratory disorders is that routinely measured cellular biomarkers, such as blood eosinophil counts in chronic obstructive pulmonary disease (COPD), can predict treatment responses” (Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600[19]30050-5).
Increased blood monocyte counts in idiopathic pulmonary fibrosis may reflect disease activity, which “could explain the outcome differences,” said Dr. Kreuter and Dr. Maher. “As highlighted by the investigators themselves, before introducing assessment of monocyte counts as part of routine clinical care for individuals with idiopathic pulmonary fibrosis, the limitations of this research should be taken into account. These include uncertainty around diagnosis and disease severity in a substantial subset of the patients, and the unknown effect of medical therapies (including corticosteroids and immunosuppressant and antifibrotic drugs) on monocyte counts and prognosis.” Researchers should validate the clinical value of blood monocyte counts in existing and future cohorts and evaluate the biomarker in clinical trials.
The editorialists have received compensation and funding from various pharmaceutical companies.
The study by Scott et al. provides evidence that monocyte count may be a “novel, simple, and inexpensive prognostic biomarker in idiopathic pulmonary fibrosis,” according to an accompanying editorial.
Progress has been made in the treatment of idiopathic pulmonary fibrosis, but patient prognosis remains “challenging to predict,” wrote Michael Kreuter, MD, of University of Heidelberg, Germany, and Toby M. Maher, MB, MSc, PhD, of Royal Brompton Hospital in London and Imperial College London. “One lesson that can be learned from other respiratory disorders is that routinely measured cellular biomarkers, such as blood eosinophil counts in chronic obstructive pulmonary disease (COPD), can predict treatment responses” (Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600[19]30050-5).
Increased blood monocyte counts in idiopathic pulmonary fibrosis may reflect disease activity, which “could explain the outcome differences,” said Dr. Kreuter and Dr. Maher. “As highlighted by the investigators themselves, before introducing assessment of monocyte counts as part of routine clinical care for individuals with idiopathic pulmonary fibrosis, the limitations of this research should be taken into account. These include uncertainty around diagnosis and disease severity in a substantial subset of the patients, and the unknown effect of medical therapies (including corticosteroids and immunosuppressant and antifibrotic drugs) on monocyte counts and prognosis.” Researchers should validate the clinical value of blood monocyte counts in existing and future cohorts and evaluate the biomarker in clinical trials.
The editorialists have received compensation and funding from various pharmaceutical companies.
, including hypertrophic cardiomyopathy, systemic sclerosis, and myelofibrosis, according to research published in The Lancet Respiratory Medicine.
The data indicate that “a single threshold value of absolute monocyte counts of 0.95 K/mcL could be used to identify high-risk patients with a fibrotic disease,” said Madeleine K. D. Scott, a researcher at Stanford (Calif.) University, and coauthors. The results “suggest that monocyte count should be incorporated into the clinical assessment” and may “enable more conscientious allocation of scarce resources, including lung transplantations,” they said.
While other published biomarkers – including gene panels and multicytokine signatures – may be expensive and not readily available, “absolute monocyte count is routinely measured as part of a complete blood count, an inexpensive test used in clinical practice worldwide,” the authors said.
Further study of monocytes’ mechanistic role in fibrosis ultimately could point to new treatment approaches.
A retrospective multicenter cohort study
To assess whether immune cells may identify patients with idiopathic pulmonary fibrosis at greater risk of poor outcomes, Ms. Scott and her collaborators conducted a retrospective multicenter cohort study.
They first analyzed transcriptome data from 120 peripheral blood mononuclear cell samples of patients with idiopathic pulmonary fibrosis, which they obtained from the Gene Expression Omnibus at the National Center for Biotechnology Information. They used statistical deconvolution to estimate percentages of 13 immune cell types and examined their associations with transplant-free survival. Their discovery analysis found that estimated CD14+ classical monocyte percentages above the mean correlated with shorter transplant-free survival times (hazard ratio, 1.82), but percentages of T cells and B cells did not.
The researchers then validated these results using samples from patients with idiopathic pulmonary fibrosis in two independent cohorts. In the COMET validation cohort, which included 45 patients with idiopathic pulmonary fibrosis whose monocyte counts were measured using flow cytometry, higher monocyte counts were significantly associated with greater risk of disease progression. In the Yale cohort, which included 15 patients with idiopathic pulmonary fibrosis, the 6 patients who were classified as high risk on the basis of a 52-gene signature had more CD14+ monocytes than the 9 low-risk patients did.
In addition, Ms. Scott and her collaborators looked at complete blood count values in the electronic health records of 45,068 patients with idiopathic pulmonary fibrosis, systemic sclerosis, hypertrophic cardiomyopathy, or myelofibrosis in Stanford, Northwestern, Vanderbilt, and Optum Clinformatics Data Mart cohorts.
Among patients in the COMET, Stanford, and Northwestern datasets, monocyte counts of 0.95 K/mcL or greater were associated with mortality after adjustment for forced vital capacity (HR, 2.47) and the gender, age, and physiology index (HR, 2.06). Data from 7,459 patients with idiopathic pulmonary fibrosis “showed that patients with monocyte counts of 0.95 K/mcL or greater were at increased risk of mortality with lung transplantation as a censoring event, after adjusting for age at diagnosis and sex” in the Stanford (HR, 2.30), Vanderbilt (HR, 1.52), and Optum (HR, 1.74) cohorts. “Likewise, higher absolute monocyte count was associated with shortened survival in patients with hypertrophic cardiomyopathy across all three cohorts, and in patients with systemic sclerosis or myelofibrosis in two of the three cohorts,” the researchers said.
The study was funded by grants from the Bill & Melinda Gates Foundation, U.S. National Institute of Allergy and Infectious Diseases, and U.S. National Library of Medicine. Ms. Scott had no competing interests. Coauthors disclosed grants, compensation, and support from foundations, agencies, and companies.
SOURCE: Scott MKD et al. Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600(18)30508-3.
, including hypertrophic cardiomyopathy, systemic sclerosis, and myelofibrosis, according to research published in The Lancet Respiratory Medicine.
The data indicate that “a single threshold value of absolute monocyte counts of 0.95 K/mcL could be used to identify high-risk patients with a fibrotic disease,” said Madeleine K. D. Scott, a researcher at Stanford (Calif.) University, and coauthors. The results “suggest that monocyte count should be incorporated into the clinical assessment” and may “enable more conscientious allocation of scarce resources, including lung transplantations,” they said.
While other published biomarkers – including gene panels and multicytokine signatures – may be expensive and not readily available, “absolute monocyte count is routinely measured as part of a complete blood count, an inexpensive test used in clinical practice worldwide,” the authors said.
Further study of monocytes’ mechanistic role in fibrosis ultimately could point to new treatment approaches.
A retrospective multicenter cohort study
To assess whether immune cells may identify patients with idiopathic pulmonary fibrosis at greater risk of poor outcomes, Ms. Scott and her collaborators conducted a retrospective multicenter cohort study.
They first analyzed transcriptome data from 120 peripheral blood mononuclear cell samples of patients with idiopathic pulmonary fibrosis, which they obtained from the Gene Expression Omnibus at the National Center for Biotechnology Information. They used statistical deconvolution to estimate percentages of 13 immune cell types and examined their associations with transplant-free survival. Their discovery analysis found that estimated CD14+ classical monocyte percentages above the mean correlated with shorter transplant-free survival times (hazard ratio, 1.82), but percentages of T cells and B cells did not.
The researchers then validated these results using samples from patients with idiopathic pulmonary fibrosis in two independent cohorts. In the COMET validation cohort, which included 45 patients with idiopathic pulmonary fibrosis whose monocyte counts were measured using flow cytometry, higher monocyte counts were significantly associated with greater risk of disease progression. In the Yale cohort, which included 15 patients with idiopathic pulmonary fibrosis, the 6 patients who were classified as high risk on the basis of a 52-gene signature had more CD14+ monocytes than the 9 low-risk patients did.
In addition, Ms. Scott and her collaborators looked at complete blood count values in the electronic health records of 45,068 patients with idiopathic pulmonary fibrosis, systemic sclerosis, hypertrophic cardiomyopathy, or myelofibrosis in Stanford, Northwestern, Vanderbilt, and Optum Clinformatics Data Mart cohorts.
Among patients in the COMET, Stanford, and Northwestern datasets, monocyte counts of 0.95 K/mcL or greater were associated with mortality after adjustment for forced vital capacity (HR, 2.47) and the gender, age, and physiology index (HR, 2.06). Data from 7,459 patients with idiopathic pulmonary fibrosis “showed that patients with monocyte counts of 0.95 K/mcL or greater were at increased risk of mortality with lung transplantation as a censoring event, after adjusting for age at diagnosis and sex” in the Stanford (HR, 2.30), Vanderbilt (HR, 1.52), and Optum (HR, 1.74) cohorts. “Likewise, higher absolute monocyte count was associated with shortened survival in patients with hypertrophic cardiomyopathy across all three cohorts, and in patients with systemic sclerosis or myelofibrosis in two of the three cohorts,” the researchers said.
The study was funded by grants from the Bill & Melinda Gates Foundation, U.S. National Institute of Allergy and Infectious Diseases, and U.S. National Library of Medicine. Ms. Scott had no competing interests. Coauthors disclosed grants, compensation, and support from foundations, agencies, and companies.
SOURCE: Scott MKD et al. Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600(18)30508-3.
FROM THE LANCET RESPIRATORY MEDICINE
Key clinical point: An increased monocyte count predicts poor outcomes among patients with idiopathic pulmonary fibrosis and other fibrotic diseases.
Major finding: Among patients in three cohorts, monocyte counts of 0.95 K/mcL or greater were associated with mortality after adjustment for forced vital capacity (hazard ratio, 2.47) and the gender, age, and physiology index (HR, 2.06).
Study details: A retrospective analysis of data from 7,000 patients with idiopathic pulmonary fibrosis from five independent cohorts.
Disclosures: The study was funded by grants from the Bill & Melinda Gates Foundation, U.S. National Institute of Allergy and Infectious Diseases, and U.S. National Library of Medicine. Ms. Scott had no competing interests. Coauthors disclosed grants, compensation, and support from foundations, agencies, and companies.
Source: Scott MKD et al. Lancet Respir Med. 2019 Jun. doi: 10.1016/S2213-2600(18)30508-3.
Hippocampal cerebral blood flow upped with antihypertensive use in Alzheimer’s
according to a new study.
Cerebral blood flow in other regions of the brain did not significantly change in patients who took the antihypertensive drug nilvadipine, according to a report on the trial published in Hypertension. Reduced cerebral blood flow is an early marker of Alzheimer’s disease, and the SPRINT MIND study suggests that intensive blood pressure control may reduce the risk of cognitive impairment.
“These findings [of the new study] not only indicate preserved cerebral autoregulation in Alzheimer’s disease but also point toward beneficial cerebrovascular effects of antihypertensive treatment,” said Jurgen A.H.R. Claassen, MD, PhD of Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. “An important question is whether this observed increase in [cerebral blood flow] translates to clinical benefits. Unfortunately, sample sizes were too small and follow-up time too short to reliably study the effects ... on structural brain measures and cognitive measures.”
Nilvadipine is a dihydropyridine calcium antagonist used to treat hypertension. In the NILVAD trial, investigators assessed the effects of nilvadipine versus placebo in approximately 500 patients with Alzheimer’s disease. The 18-month trial found no beneficial effects of nilvadipine on cognitive function, but subgroup analyses suggested a potential benefit among patients in the early stages of the disease (PLoS Med. 2018 Sep 24;15[9]:e1002660.).
The cerebral blood flow analysis was a preplanned substudy of NILVAD designed to assess how 6 months of treatment with the drug affects cerebral blood flow as measured using MRI arterial spin labeling. The researchers looked at cerebral blood flow in whole-brain gray matter and in specific regions such as the hippocampus.
The substudy analysis included 22 patients who received nilvadipine and 22 who received placebo during the randomized, double-blind study. Participants had a mean age of 72.8 years and a mean Mini-Mental State Examination score of 20.4.
At 6 months, nilvadipine lowered systolic BP by 11.5 mm Hg, and whole-brain gray matter cerebral blood flow remained stable. Blood flow to the hippocampus increased by approximately 20% among patients treated with nilvadipine – by 24.4 mL/100 g per minute to the left hippocampus and by 20.1 mL/100 g per minute to the right hippocampus.
The increased hippocampal cerebral blood flow could be related to nilvadipine’s antihypertensive effects or its effects on amyloid-beta, the authors noted.
“These findings indicate that the known decrease in [cerebral blood flow] in patients with [Alzheimer’s disease] can in some regions be reversed,” they wrote.
“Even though no medical treatment is without risk, getting treatment for high blood pressure could be important to maintain brain health in patients with Alzheimer’s disease,” Dr. Claassen said in a statement. “In the future, we need to find out whether the improvement in blood flow, especially in the hippocampus, can be used as a supportive treatment to slow down progression of Alzheimer’s disease, especially in earlier states of disease.”
The researchers wrote they lacked biomarkers to confirm Alzheimer’s disease pathology. Most of the study participants were white Europeans, which “limits extrapolation [of the findings] to other populations,” they added.
The Alzheimer’s Drug Discovery Foundation and the Dutch Alzheimer Society funded the NILVAD cerebral blood flow substudy. NILVAD was funded by the European Commission Framework 7 Program Health Theme. Dr. Claassen had no disclosures; one coauthor disclosed a pending patent for nilvadipine.
SOURCE: Claassen JAHR et al. Hypertension. 2019 Jun 17. doi: 10.1161/HYPERTENSIONAHA.119.12892.
according to a new study.
Cerebral blood flow in other regions of the brain did not significantly change in patients who took the antihypertensive drug nilvadipine, according to a report on the trial published in Hypertension. Reduced cerebral blood flow is an early marker of Alzheimer’s disease, and the SPRINT MIND study suggests that intensive blood pressure control may reduce the risk of cognitive impairment.
“These findings [of the new study] not only indicate preserved cerebral autoregulation in Alzheimer’s disease but also point toward beneficial cerebrovascular effects of antihypertensive treatment,” said Jurgen A.H.R. Claassen, MD, PhD of Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. “An important question is whether this observed increase in [cerebral blood flow] translates to clinical benefits. Unfortunately, sample sizes were too small and follow-up time too short to reliably study the effects ... on structural brain measures and cognitive measures.”
Nilvadipine is a dihydropyridine calcium antagonist used to treat hypertension. In the NILVAD trial, investigators assessed the effects of nilvadipine versus placebo in approximately 500 patients with Alzheimer’s disease. The 18-month trial found no beneficial effects of nilvadipine on cognitive function, but subgroup analyses suggested a potential benefit among patients in the early stages of the disease (PLoS Med. 2018 Sep 24;15[9]:e1002660.).
The cerebral blood flow analysis was a preplanned substudy of NILVAD designed to assess how 6 months of treatment with the drug affects cerebral blood flow as measured using MRI arterial spin labeling. The researchers looked at cerebral blood flow in whole-brain gray matter and in specific regions such as the hippocampus.
The substudy analysis included 22 patients who received nilvadipine and 22 who received placebo during the randomized, double-blind study. Participants had a mean age of 72.8 years and a mean Mini-Mental State Examination score of 20.4.
At 6 months, nilvadipine lowered systolic BP by 11.5 mm Hg, and whole-brain gray matter cerebral blood flow remained stable. Blood flow to the hippocampus increased by approximately 20% among patients treated with nilvadipine – by 24.4 mL/100 g per minute to the left hippocampus and by 20.1 mL/100 g per minute to the right hippocampus.
The increased hippocampal cerebral blood flow could be related to nilvadipine’s antihypertensive effects or its effects on amyloid-beta, the authors noted.
“These findings indicate that the known decrease in [cerebral blood flow] in patients with [Alzheimer’s disease] can in some regions be reversed,” they wrote.
“Even though no medical treatment is without risk, getting treatment for high blood pressure could be important to maintain brain health in patients with Alzheimer’s disease,” Dr. Claassen said in a statement. “In the future, we need to find out whether the improvement in blood flow, especially in the hippocampus, can be used as a supportive treatment to slow down progression of Alzheimer’s disease, especially in earlier states of disease.”
The researchers wrote they lacked biomarkers to confirm Alzheimer’s disease pathology. Most of the study participants were white Europeans, which “limits extrapolation [of the findings] to other populations,” they added.
The Alzheimer’s Drug Discovery Foundation and the Dutch Alzheimer Society funded the NILVAD cerebral blood flow substudy. NILVAD was funded by the European Commission Framework 7 Program Health Theme. Dr. Claassen had no disclosures; one coauthor disclosed a pending patent for nilvadipine.
SOURCE: Claassen JAHR et al. Hypertension. 2019 Jun 17. doi: 10.1161/HYPERTENSIONAHA.119.12892.
according to a new study.
Cerebral blood flow in other regions of the brain did not significantly change in patients who took the antihypertensive drug nilvadipine, according to a report on the trial published in Hypertension. Reduced cerebral blood flow is an early marker of Alzheimer’s disease, and the SPRINT MIND study suggests that intensive blood pressure control may reduce the risk of cognitive impairment.
“These findings [of the new study] not only indicate preserved cerebral autoregulation in Alzheimer’s disease but also point toward beneficial cerebrovascular effects of antihypertensive treatment,” said Jurgen A.H.R. Claassen, MD, PhD of Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. “An important question is whether this observed increase in [cerebral blood flow] translates to clinical benefits. Unfortunately, sample sizes were too small and follow-up time too short to reliably study the effects ... on structural brain measures and cognitive measures.”
Nilvadipine is a dihydropyridine calcium antagonist used to treat hypertension. In the NILVAD trial, investigators assessed the effects of nilvadipine versus placebo in approximately 500 patients with Alzheimer’s disease. The 18-month trial found no beneficial effects of nilvadipine on cognitive function, but subgroup analyses suggested a potential benefit among patients in the early stages of the disease (PLoS Med. 2018 Sep 24;15[9]:e1002660.).
The cerebral blood flow analysis was a preplanned substudy of NILVAD designed to assess how 6 months of treatment with the drug affects cerebral blood flow as measured using MRI arterial spin labeling. The researchers looked at cerebral blood flow in whole-brain gray matter and in specific regions such as the hippocampus.
The substudy analysis included 22 patients who received nilvadipine and 22 who received placebo during the randomized, double-blind study. Participants had a mean age of 72.8 years and a mean Mini-Mental State Examination score of 20.4.
At 6 months, nilvadipine lowered systolic BP by 11.5 mm Hg, and whole-brain gray matter cerebral blood flow remained stable. Blood flow to the hippocampus increased by approximately 20% among patients treated with nilvadipine – by 24.4 mL/100 g per minute to the left hippocampus and by 20.1 mL/100 g per minute to the right hippocampus.
The increased hippocampal cerebral blood flow could be related to nilvadipine’s antihypertensive effects or its effects on amyloid-beta, the authors noted.
“These findings indicate that the known decrease in [cerebral blood flow] in patients with [Alzheimer’s disease] can in some regions be reversed,” they wrote.
“Even though no medical treatment is without risk, getting treatment for high blood pressure could be important to maintain brain health in patients with Alzheimer’s disease,” Dr. Claassen said in a statement. “In the future, we need to find out whether the improvement in blood flow, especially in the hippocampus, can be used as a supportive treatment to slow down progression of Alzheimer’s disease, especially in earlier states of disease.”
The researchers wrote they lacked biomarkers to confirm Alzheimer’s disease pathology. Most of the study participants were white Europeans, which “limits extrapolation [of the findings] to other populations,” they added.
The Alzheimer’s Drug Discovery Foundation and the Dutch Alzheimer Society funded the NILVAD cerebral blood flow substudy. NILVAD was funded by the European Commission Framework 7 Program Health Theme. Dr. Claassen had no disclosures; one coauthor disclosed a pending patent for nilvadipine.
SOURCE: Claassen JAHR et al. Hypertension. 2019 Jun 17. doi: 10.1161/HYPERTENSIONAHA.119.12892.
FROM HYPERTENSION
Gabapentinoids associated with suicidal behavior, overdose
Young patients might be at increased risk of suicidal behavior, unintentional overdose, injuries, and traffic incidents during treatment periods with gabapentinoids, compared with periods without treatment with those medications, a cohort study of almost 200,000 people shows. Pregabalin is associated with higher hazards of those outcomes than is gabapentin, and the associations are strongest in patients aged 15-24 years, the researchers reported.
“If our findings are triangulated with other forms of evidence, ,” wrote Yasmina Molero, PhD, and associates. “Further restrictions for off-label prescription may need consideration.” The study was published in BMJ.
The use of gabapentinoids has risen in the United States (JAMA Intern Med. 2018;178[2]:292-4), and overdose deaths tied to gabapentin have led some states to explore reclassification of the drug as a controlled substance (Risk Manag Healthc Policy. 2018;11:109-16). In the United Kingdom, gabapentinoids are being reclassified as a class C controlled drug because of concerns about the risk of addiction, overdose, and safety, wrote Dr. Molero of the department of psychiatry at Warneford Hospital at the University of Oxford, England, and associates.
To study associations between gabapentinoids and adverse outcomes related to coordination, mental health, and criminality, Dr. Molero and her associates analyzed data from 191,973 people from the Swedish Prescribed Drug Register who collected prescriptions for pregabalin or gabapentin between 2006 and 2013. The researchers included patients aged 15 years and older in their analyses.
They examined suicidal behavior, unintentional overdoses, head or body injuries, road traffic incidents and offenses, and arrests for violent crime using the Swedish Patient Register and the National Crime Register. In addition, they defined suicidal behavior as emergency hospital visits attributable to self-injurious behavior or suicide attempt, or death by suicide. Unintentional overdoses were defined as emergency hospital visits or death attributable to poisoning by illicit drugs, medications, or biologic substances; accidental poisoning by noxious substances; or acute intoxications and overdoses by alcohol and illicit drugs, excluding intentional self-poisoning, wrote Dr. Molero, who is affiliated with the Karolinska Institute in Stockholm, and her associates.
Of the nearly 192,000 participants who collected prescriptions of gabapentinoids on at least two consecutive occasions, 120,664 received pregabalin, and 85,360 received gabapentin; 14,051 of the participants received both drugs. Fifty-nine percent were women, and most patients were aged 45 or older.
During the study period, 10,026 participants (5.2%) were treated for suicidal behavior or died from suicide, 17,144 participants (8.9%) experienced an unintentional overdose, and 12,070 participants (6.3%) had a road traffic incident or offense. In addition, 70,522 participants (36.7%) had head or body injuries, and 7,984 participants (4.1%) were arrested for a violent crime.
The study used a within-individual design that compared when a person was taking a gabapentinoid with when he or she was not. During treatment periods, participants were at increased risk of suicidal behavior or death from suicide (age-adjusted hazard ratio, 1.26), unintentional overdose (1.24), head or body injuries (1.22), and road traffic incidents or offenses (1.13). Associations with arrests for violent crime were not significant.
Gabapentinoid treatment was associated with increased hazards of suicidal behavior in people young than 55 years, but hazards were reduced or not significant in participants aged 55 years and older. Participants aged 15-24 years had the highest hazards of suicidal behavior (1.67).
In a sensitivity analysis, the researchers examined participants who had a diagnosis of comorbid epilepsy, psychiatric disorders, or musculoskeletal disorders before the start of gabapentinoid treatment. Among patients with comorbid epilepsy, gabapentinoids were not significantly associated with suicidal behavior and were associated with reduced hazards for all other outcomes.
“In comorbid psychiatric disorders, gabapentinoids were associated with lower risk for all outcomes,” the researchers said. Among patients with comorbid musculoskeletal disorders, gabapentinoids were associated with reductions in head or body injuries, traffic incidents, and arrests for violent crime.
Dr. Molero and her associates noted that they lacked information about alcohol and drug use, as well as treatment adherence and the conditions for which gabapentinoids had been prescribed. Furthermore, differences in prescription practices and outcome rates might affect the generalizability of the results to other countries.
The different results for pregabalin and gabapentin “could be due to their different pharmacodynamic and pharmacokinetic profiles; pregabalin has a higher potency, greater bioavailability, and quicker absorption than gabapentin. Pregabalin also has been associated with withdrawal symptoms following rapid discontinuation, which could be related to suicidal behavior,” Dr. Molero and colleagues said. “The reduced hazards in older people could reflect pharmacodynamic differences related to age, less concurrent use of alcohol or drugs, different indications for treatment, or reduced symptom severity of underlying conditions.”
The Wellcome Trust, Swedish Research Council, and Karolinska Institute supported the study. The authors had no disclosures relevant to the study. One author reported grants from Shire and Evolan and has served as a speaker for Shire.
SOURCE: Molero Y et al. BMJ. 2019 Jun 12. doi: 10.1136/bmj.l2147.
The findings by Molero et al. advance clinical knowledge about the drug class of gabapentinoids, wrote Derek K. Tracy, MB BCh. Though the study does not establish causality, it does rely on a solid, large dataset. The study shows the importance of uncoupling pregabalin and gabapentin. Both drugs are indeed gabapentinoids, but their use can lead to different outcomes, depending on the age of patients. For example, pregabalin – not gabapentin – appears tied to higher risks of harm. The demographic group that is most vulnerable is patients aged 15-24, the researchers found. Factors driving those age-related differences in risks tied to the drugs need to be understood.
Dr. Tracy is a consultant psychiatrist at Queen Mary’s Hospital in London. He is a trustee of the charity Mentor and has received honoraria from Janssen for delivering educational talks on novel psychoactive substances. His comments were adapted from an editorial (BMJ. 2019 Jun 12. doi: 10.1136/bmj.14021 ).
The findings by Molero et al. advance clinical knowledge about the drug class of gabapentinoids, wrote Derek K. Tracy, MB BCh. Though the study does not establish causality, it does rely on a solid, large dataset. The study shows the importance of uncoupling pregabalin and gabapentin. Both drugs are indeed gabapentinoids, but their use can lead to different outcomes, depending on the age of patients. For example, pregabalin – not gabapentin – appears tied to higher risks of harm. The demographic group that is most vulnerable is patients aged 15-24, the researchers found. Factors driving those age-related differences in risks tied to the drugs need to be understood.
Dr. Tracy is a consultant psychiatrist at Queen Mary’s Hospital in London. He is a trustee of the charity Mentor and has received honoraria from Janssen for delivering educational talks on novel psychoactive substances. His comments were adapted from an editorial (BMJ. 2019 Jun 12. doi: 10.1136/bmj.14021 ).
The findings by Molero et al. advance clinical knowledge about the drug class of gabapentinoids, wrote Derek K. Tracy, MB BCh. Though the study does not establish causality, it does rely on a solid, large dataset. The study shows the importance of uncoupling pregabalin and gabapentin. Both drugs are indeed gabapentinoids, but their use can lead to different outcomes, depending on the age of patients. For example, pregabalin – not gabapentin – appears tied to higher risks of harm. The demographic group that is most vulnerable is patients aged 15-24, the researchers found. Factors driving those age-related differences in risks tied to the drugs need to be understood.
Dr. Tracy is a consultant psychiatrist at Queen Mary’s Hospital in London. He is a trustee of the charity Mentor and has received honoraria from Janssen for delivering educational talks on novel psychoactive substances. His comments were adapted from an editorial (BMJ. 2019 Jun 12. doi: 10.1136/bmj.14021 ).
Young patients might be at increased risk of suicidal behavior, unintentional overdose, injuries, and traffic incidents during treatment periods with gabapentinoids, compared with periods without treatment with those medications, a cohort study of almost 200,000 people shows. Pregabalin is associated with higher hazards of those outcomes than is gabapentin, and the associations are strongest in patients aged 15-24 years, the researchers reported.
“If our findings are triangulated with other forms of evidence, ,” wrote Yasmina Molero, PhD, and associates. “Further restrictions for off-label prescription may need consideration.” The study was published in BMJ.
The use of gabapentinoids has risen in the United States (JAMA Intern Med. 2018;178[2]:292-4), and overdose deaths tied to gabapentin have led some states to explore reclassification of the drug as a controlled substance (Risk Manag Healthc Policy. 2018;11:109-16). In the United Kingdom, gabapentinoids are being reclassified as a class C controlled drug because of concerns about the risk of addiction, overdose, and safety, wrote Dr. Molero of the department of psychiatry at Warneford Hospital at the University of Oxford, England, and associates.
To study associations between gabapentinoids and adverse outcomes related to coordination, mental health, and criminality, Dr. Molero and her associates analyzed data from 191,973 people from the Swedish Prescribed Drug Register who collected prescriptions for pregabalin or gabapentin between 2006 and 2013. The researchers included patients aged 15 years and older in their analyses.
They examined suicidal behavior, unintentional overdoses, head or body injuries, road traffic incidents and offenses, and arrests for violent crime using the Swedish Patient Register and the National Crime Register. In addition, they defined suicidal behavior as emergency hospital visits attributable to self-injurious behavior or suicide attempt, or death by suicide. Unintentional overdoses were defined as emergency hospital visits or death attributable to poisoning by illicit drugs, medications, or biologic substances; accidental poisoning by noxious substances; or acute intoxications and overdoses by alcohol and illicit drugs, excluding intentional self-poisoning, wrote Dr. Molero, who is affiliated with the Karolinska Institute in Stockholm, and her associates.
Of the nearly 192,000 participants who collected prescriptions of gabapentinoids on at least two consecutive occasions, 120,664 received pregabalin, and 85,360 received gabapentin; 14,051 of the participants received both drugs. Fifty-nine percent were women, and most patients were aged 45 or older.
During the study period, 10,026 participants (5.2%) were treated for suicidal behavior or died from suicide, 17,144 participants (8.9%) experienced an unintentional overdose, and 12,070 participants (6.3%) had a road traffic incident or offense. In addition, 70,522 participants (36.7%) had head or body injuries, and 7,984 participants (4.1%) were arrested for a violent crime.
The study used a within-individual design that compared when a person was taking a gabapentinoid with when he or she was not. During treatment periods, participants were at increased risk of suicidal behavior or death from suicide (age-adjusted hazard ratio, 1.26), unintentional overdose (1.24), head or body injuries (1.22), and road traffic incidents or offenses (1.13). Associations with arrests for violent crime were not significant.
Gabapentinoid treatment was associated with increased hazards of suicidal behavior in people young than 55 years, but hazards were reduced or not significant in participants aged 55 years and older. Participants aged 15-24 years had the highest hazards of suicidal behavior (1.67).
In a sensitivity analysis, the researchers examined participants who had a diagnosis of comorbid epilepsy, psychiatric disorders, or musculoskeletal disorders before the start of gabapentinoid treatment. Among patients with comorbid epilepsy, gabapentinoids were not significantly associated with suicidal behavior and were associated with reduced hazards for all other outcomes.
“In comorbid psychiatric disorders, gabapentinoids were associated with lower risk for all outcomes,” the researchers said. Among patients with comorbid musculoskeletal disorders, gabapentinoids were associated with reductions in head or body injuries, traffic incidents, and arrests for violent crime.
Dr. Molero and her associates noted that they lacked information about alcohol and drug use, as well as treatment adherence and the conditions for which gabapentinoids had been prescribed. Furthermore, differences in prescription practices and outcome rates might affect the generalizability of the results to other countries.
The different results for pregabalin and gabapentin “could be due to their different pharmacodynamic and pharmacokinetic profiles; pregabalin has a higher potency, greater bioavailability, and quicker absorption than gabapentin. Pregabalin also has been associated with withdrawal symptoms following rapid discontinuation, which could be related to suicidal behavior,” Dr. Molero and colleagues said. “The reduced hazards in older people could reflect pharmacodynamic differences related to age, less concurrent use of alcohol or drugs, different indications for treatment, or reduced symptom severity of underlying conditions.”
The Wellcome Trust, Swedish Research Council, and Karolinska Institute supported the study. The authors had no disclosures relevant to the study. One author reported grants from Shire and Evolan and has served as a speaker for Shire.
SOURCE: Molero Y et al. BMJ. 2019 Jun 12. doi: 10.1136/bmj.l2147.
Young patients might be at increased risk of suicidal behavior, unintentional overdose, injuries, and traffic incidents during treatment periods with gabapentinoids, compared with periods without treatment with those medications, a cohort study of almost 200,000 people shows. Pregabalin is associated with higher hazards of those outcomes than is gabapentin, and the associations are strongest in patients aged 15-24 years, the researchers reported.
“If our findings are triangulated with other forms of evidence, ,” wrote Yasmina Molero, PhD, and associates. “Further restrictions for off-label prescription may need consideration.” The study was published in BMJ.
The use of gabapentinoids has risen in the United States (JAMA Intern Med. 2018;178[2]:292-4), and overdose deaths tied to gabapentin have led some states to explore reclassification of the drug as a controlled substance (Risk Manag Healthc Policy. 2018;11:109-16). In the United Kingdom, gabapentinoids are being reclassified as a class C controlled drug because of concerns about the risk of addiction, overdose, and safety, wrote Dr. Molero of the department of psychiatry at Warneford Hospital at the University of Oxford, England, and associates.
To study associations between gabapentinoids and adverse outcomes related to coordination, mental health, and criminality, Dr. Molero and her associates analyzed data from 191,973 people from the Swedish Prescribed Drug Register who collected prescriptions for pregabalin or gabapentin between 2006 and 2013. The researchers included patients aged 15 years and older in their analyses.
They examined suicidal behavior, unintentional overdoses, head or body injuries, road traffic incidents and offenses, and arrests for violent crime using the Swedish Patient Register and the National Crime Register. In addition, they defined suicidal behavior as emergency hospital visits attributable to self-injurious behavior or suicide attempt, or death by suicide. Unintentional overdoses were defined as emergency hospital visits or death attributable to poisoning by illicit drugs, medications, or biologic substances; accidental poisoning by noxious substances; or acute intoxications and overdoses by alcohol and illicit drugs, excluding intentional self-poisoning, wrote Dr. Molero, who is affiliated with the Karolinska Institute in Stockholm, and her associates.
Of the nearly 192,000 participants who collected prescriptions of gabapentinoids on at least two consecutive occasions, 120,664 received pregabalin, and 85,360 received gabapentin; 14,051 of the participants received both drugs. Fifty-nine percent were women, and most patients were aged 45 or older.
During the study period, 10,026 participants (5.2%) were treated for suicidal behavior or died from suicide, 17,144 participants (8.9%) experienced an unintentional overdose, and 12,070 participants (6.3%) had a road traffic incident or offense. In addition, 70,522 participants (36.7%) had head or body injuries, and 7,984 participants (4.1%) were arrested for a violent crime.
The study used a within-individual design that compared when a person was taking a gabapentinoid with when he or she was not. During treatment periods, participants were at increased risk of suicidal behavior or death from suicide (age-adjusted hazard ratio, 1.26), unintentional overdose (1.24), head or body injuries (1.22), and road traffic incidents or offenses (1.13). Associations with arrests for violent crime were not significant.
Gabapentinoid treatment was associated with increased hazards of suicidal behavior in people young than 55 years, but hazards were reduced or not significant in participants aged 55 years and older. Participants aged 15-24 years had the highest hazards of suicidal behavior (1.67).
In a sensitivity analysis, the researchers examined participants who had a diagnosis of comorbid epilepsy, psychiatric disorders, or musculoskeletal disorders before the start of gabapentinoid treatment. Among patients with comorbid epilepsy, gabapentinoids were not significantly associated with suicidal behavior and were associated with reduced hazards for all other outcomes.
“In comorbid psychiatric disorders, gabapentinoids were associated with lower risk for all outcomes,” the researchers said. Among patients with comorbid musculoskeletal disorders, gabapentinoids were associated with reductions in head or body injuries, traffic incidents, and arrests for violent crime.
Dr. Molero and her associates noted that they lacked information about alcohol and drug use, as well as treatment adherence and the conditions for which gabapentinoids had been prescribed. Furthermore, differences in prescription practices and outcome rates might affect the generalizability of the results to other countries.
The different results for pregabalin and gabapentin “could be due to their different pharmacodynamic and pharmacokinetic profiles; pregabalin has a higher potency, greater bioavailability, and quicker absorption than gabapentin. Pregabalin also has been associated with withdrawal symptoms following rapid discontinuation, which could be related to suicidal behavior,” Dr. Molero and colleagues said. “The reduced hazards in older people could reflect pharmacodynamic differences related to age, less concurrent use of alcohol or drugs, different indications for treatment, or reduced symptom severity of underlying conditions.”
The Wellcome Trust, Swedish Research Council, and Karolinska Institute supported the study. The authors had no disclosures relevant to the study. One author reported grants from Shire and Evolan and has served as a speaker for Shire.
SOURCE: Molero Y et al. BMJ. 2019 Jun 12. doi: 10.1136/bmj.l2147.
FROM BMJ
Key clinical point: Patients might be at increased risk of suicidal behavior, unintentional overdose, head and body injuries, and traffic incidents during periods of treatment with gabapentinoids. Pregabalin is associated with higher hazards of these outcomes than is gabapentin, and the associations are strongest in patients aged 15-24 years.
Major finding: During treatment periods, patients were at increased risk of suicidal behavior or death from suicide (age-adjusted hazard ratio, 1.26), unintentional overdose (1.24), head or body injuries (1.22), and road traffic incidents or offenses (1.13).
Study details: An analysis of data from 191,973 people from the Swedish Prescribed Drug Register, which collected prescriptions for pregabalin or gabapentin between 2006 and 2013.
Disclosures: The Wellcome Trust, Swedish Research Council, and Karolinska Institute supported the study. The authors had no relevant disclosures. One author reported grants from Shire and Evolan, and has served as a speaker for Shire.
Source: Molero Y et al. BMJ. 2019 Jun 12. doi: 10.1136/bmj.l2147.
Pediatric-onset MS may slow information processing in adulthood
independent of age or disease duration, according to a study published in JAMA Neurology.
Information-processing efficiency as measured by the Symbol Digit Modalities Test (SDMT) may decrease more rapidly in patients with pediatric-onset multiple sclerosis (MS).
“Children and adolescents who develop [MS] should be monitored closely for cognitive changes and helped to manage the potential challenges that early-onset multiple sclerosis poses for cognitive abilities later in life,” Kyla A. McKay, PhD, a researcher at Karolinska Institutet in Stockholm, and colleagues wrote.
Prior research has found that an SDMT score of 55 may be a point at which a person with MS is “employed but work challenged.” In the present study, patients with pediatric-onset MS reached this threshold at about age 34 years, whereas patients with adult-onset MS reached it at approximately 50 years. These findings suggest that the groups’ different cognitive outcomes “may be meaningful,” the researchers wrote.
Onset of MS before age 18 years occurs in 2%-10% of cases, but few studies have looked at cognitive outcomes of patients with pediatric-onset MS in adulthood. Cognitive impairment is common in patients with MS and may affect quality of life, social functioning, and employment.
To compare changes in cognitive function over time in adults with pediatric-onset MS versus adults with adult-onset MS, Dr. McKay and colleagues conducted a population-based, longitudinal cohort study using data from more than 5,700 patients in the Swedish Multiple Sclerosis Registry. The registry includes information from all neurology clinics in Sweden, and the researchers examined data collected between April 2006 and April 2018.
SDMT scores range from 0 to 120, and higher scores indicate greater information-processing efficiency.
The researchers classified patients with MS onset at younger than 18 years as pediatric-onset MS. The researchers excluded patients with fewer than two SDMT scores, patients younger than 18 years or older than 55 years at the time of testing, and patients with disease duration of 30 years or more.
The researchers included 5,704 patients, 300 of whom had pediatric-onset MS (5.3%). About 70% of the patients were female, and 98% had a relapsing-onset disease course. The pediatric-onset MS group had a younger median age at baseline than the adult-onset group did (26 years vs. 38 years). The patients had more than 46,000 SDMT scores, with an average baseline SDMT of 51; the median follow-up time was 3 years.
Patients with pediatric-onset MS had significantly lower SDMT scores (beta coefficient, –3.59), after adjusting for sex, age, disease duration, disease course, total number of SDMTs completed, oral or visual SDMT form, and exposure to disease-modifying therapy. Their scores also declined faster than those of patients with adult-onset MS (beta coefficient, –0.30; 95% confidence interval, –5.56 to –1.54), and they were more likely to ever have cognitive impairment (odds ratio, 1.44).
“At younger than 30 years, SDMT scores between the ... groups were comparable; but after 30 years of age the trajectories began to diverge,” Dr. McKay and associates wrote. At age 35 years, the mean SDMT score for patients with adult-onset MS was 61, whereas for patients with pediatric-onset MS it was 51. By age 40 years, the mean score was 58 for adult-onset MS versus 46 for pediatric-onset MS.
The study was supported by the Swedish Research Council and the Swedish Brain Foundation and by postdoctoral awards from the Canadian Institutes of Health Research to Dr. McKay and European Committee for Treatment and Research in Multiple Sclerosis to Dr. McKay. Coauthors reported receiving honoraria for speaking and serving on advisory boards for various pharmaceutical companies, as well as receiving research funding from agencies, foundations, and pharmaceutical companies.
SOURCE: McKay KA et al. JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546.
The study by McKay et al. indicates that onset of multiple sclerosis (MS) during childhood or adolescence has long-term effects, Lauren B. Krupp, MD, and Leigh E. Charvet, PhD, wrote in an accompanying editorial.
In early adulthood, patients with pediatric-onset MS initially may perform better on the Symbol Digit Modalities Test, compared with patients with adult-onset MS. “However, the two groups diverged by the time the [pediatric-onset MS] patients reached 30 years of age, with slower performance in the [pediatric-onset MS] group relative to the [adult-onset MS] group, a difference that persisted over time,” Dr. Krupp and Dr. Charvet wrote. The findings remained even when the researchers adjusted for disease duration.
“Despite initial resiliency and age-based advantages, the study’s findings suggest greater deleterious long-term consequences from developing MS during a period of ongoing brain development,” they wrote.
The effect of slowed cognitive processing on quality of life is unclear, however. “The key question for future research is whether those with [pediatric-onset MS] attain their anticipated educational and occupational achievements in a manner comparable to those with [adult-onset MS],” Dr. Krupp and Dr. Charvet concluded.
Dr. Krupp and Dr. Charvet are affiliated with the Multiple Sclerosis Comprehensive Care Center at New York University. These comments are adapted from an editorial accompanying the article by McKay et al. ( JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546 ). Dr. Krupp reported receiving grants from the National Multiple Sclerosis Society; grants and personal fees from Biogen; and personal fees from Novartis, Sanofi Aventis, Sanofi Genzyme, Shire Pharmaceuticals, Roche, and RedHill Biopharma outside the submitted work. Dr. Charvet reported receiving grants and personal fees from Biogen, grants from the National Multiple Sclerosis Society, and research funding from Novartis and Biogen outside the submitted work.
The study by McKay et al. indicates that onset of multiple sclerosis (MS) during childhood or adolescence has long-term effects, Lauren B. Krupp, MD, and Leigh E. Charvet, PhD, wrote in an accompanying editorial.
In early adulthood, patients with pediatric-onset MS initially may perform better on the Symbol Digit Modalities Test, compared with patients with adult-onset MS. “However, the two groups diverged by the time the [pediatric-onset MS] patients reached 30 years of age, with slower performance in the [pediatric-onset MS] group relative to the [adult-onset MS] group, a difference that persisted over time,” Dr. Krupp and Dr. Charvet wrote. The findings remained even when the researchers adjusted for disease duration.
“Despite initial resiliency and age-based advantages, the study’s findings suggest greater deleterious long-term consequences from developing MS during a period of ongoing brain development,” they wrote.
The effect of slowed cognitive processing on quality of life is unclear, however. “The key question for future research is whether those with [pediatric-onset MS] attain their anticipated educational and occupational achievements in a manner comparable to those with [adult-onset MS],” Dr. Krupp and Dr. Charvet concluded.
Dr. Krupp and Dr. Charvet are affiliated with the Multiple Sclerosis Comprehensive Care Center at New York University. These comments are adapted from an editorial accompanying the article by McKay et al. ( JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546 ). Dr. Krupp reported receiving grants from the National Multiple Sclerosis Society; grants and personal fees from Biogen; and personal fees from Novartis, Sanofi Aventis, Sanofi Genzyme, Shire Pharmaceuticals, Roche, and RedHill Biopharma outside the submitted work. Dr. Charvet reported receiving grants and personal fees from Biogen, grants from the National Multiple Sclerosis Society, and research funding from Novartis and Biogen outside the submitted work.
The study by McKay et al. indicates that onset of multiple sclerosis (MS) during childhood or adolescence has long-term effects, Lauren B. Krupp, MD, and Leigh E. Charvet, PhD, wrote in an accompanying editorial.
In early adulthood, patients with pediatric-onset MS initially may perform better on the Symbol Digit Modalities Test, compared with patients with adult-onset MS. “However, the two groups diverged by the time the [pediatric-onset MS] patients reached 30 years of age, with slower performance in the [pediatric-onset MS] group relative to the [adult-onset MS] group, a difference that persisted over time,” Dr. Krupp and Dr. Charvet wrote. The findings remained even when the researchers adjusted for disease duration.
“Despite initial resiliency and age-based advantages, the study’s findings suggest greater deleterious long-term consequences from developing MS during a period of ongoing brain development,” they wrote.
The effect of slowed cognitive processing on quality of life is unclear, however. “The key question for future research is whether those with [pediatric-onset MS] attain their anticipated educational and occupational achievements in a manner comparable to those with [adult-onset MS],” Dr. Krupp and Dr. Charvet concluded.
Dr. Krupp and Dr. Charvet are affiliated with the Multiple Sclerosis Comprehensive Care Center at New York University. These comments are adapted from an editorial accompanying the article by McKay et al. ( JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546 ). Dr. Krupp reported receiving grants from the National Multiple Sclerosis Society; grants and personal fees from Biogen; and personal fees from Novartis, Sanofi Aventis, Sanofi Genzyme, Shire Pharmaceuticals, Roche, and RedHill Biopharma outside the submitted work. Dr. Charvet reported receiving grants and personal fees from Biogen, grants from the National Multiple Sclerosis Society, and research funding from Novartis and Biogen outside the submitted work.
independent of age or disease duration, according to a study published in JAMA Neurology.
Information-processing efficiency as measured by the Symbol Digit Modalities Test (SDMT) may decrease more rapidly in patients with pediatric-onset multiple sclerosis (MS).
“Children and adolescents who develop [MS] should be monitored closely for cognitive changes and helped to manage the potential challenges that early-onset multiple sclerosis poses for cognitive abilities later in life,” Kyla A. McKay, PhD, a researcher at Karolinska Institutet in Stockholm, and colleagues wrote.
Prior research has found that an SDMT score of 55 may be a point at which a person with MS is “employed but work challenged.” In the present study, patients with pediatric-onset MS reached this threshold at about age 34 years, whereas patients with adult-onset MS reached it at approximately 50 years. These findings suggest that the groups’ different cognitive outcomes “may be meaningful,” the researchers wrote.
Onset of MS before age 18 years occurs in 2%-10% of cases, but few studies have looked at cognitive outcomes of patients with pediatric-onset MS in adulthood. Cognitive impairment is common in patients with MS and may affect quality of life, social functioning, and employment.
To compare changes in cognitive function over time in adults with pediatric-onset MS versus adults with adult-onset MS, Dr. McKay and colleagues conducted a population-based, longitudinal cohort study using data from more than 5,700 patients in the Swedish Multiple Sclerosis Registry. The registry includes information from all neurology clinics in Sweden, and the researchers examined data collected between April 2006 and April 2018.
SDMT scores range from 0 to 120, and higher scores indicate greater information-processing efficiency.
The researchers classified patients with MS onset at younger than 18 years as pediatric-onset MS. The researchers excluded patients with fewer than two SDMT scores, patients younger than 18 years or older than 55 years at the time of testing, and patients with disease duration of 30 years or more.
The researchers included 5,704 patients, 300 of whom had pediatric-onset MS (5.3%). About 70% of the patients were female, and 98% had a relapsing-onset disease course. The pediatric-onset MS group had a younger median age at baseline than the adult-onset group did (26 years vs. 38 years). The patients had more than 46,000 SDMT scores, with an average baseline SDMT of 51; the median follow-up time was 3 years.
Patients with pediatric-onset MS had significantly lower SDMT scores (beta coefficient, –3.59), after adjusting for sex, age, disease duration, disease course, total number of SDMTs completed, oral or visual SDMT form, and exposure to disease-modifying therapy. Their scores also declined faster than those of patients with adult-onset MS (beta coefficient, –0.30; 95% confidence interval, –5.56 to –1.54), and they were more likely to ever have cognitive impairment (odds ratio, 1.44).
“At younger than 30 years, SDMT scores between the ... groups were comparable; but after 30 years of age the trajectories began to diverge,” Dr. McKay and associates wrote. At age 35 years, the mean SDMT score for patients with adult-onset MS was 61, whereas for patients with pediatric-onset MS it was 51. By age 40 years, the mean score was 58 for adult-onset MS versus 46 for pediatric-onset MS.
The study was supported by the Swedish Research Council and the Swedish Brain Foundation and by postdoctoral awards from the Canadian Institutes of Health Research to Dr. McKay and European Committee for Treatment and Research in Multiple Sclerosis to Dr. McKay. Coauthors reported receiving honoraria for speaking and serving on advisory boards for various pharmaceutical companies, as well as receiving research funding from agencies, foundations, and pharmaceutical companies.
SOURCE: McKay KA et al. JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546.
independent of age or disease duration, according to a study published in JAMA Neurology.
Information-processing efficiency as measured by the Symbol Digit Modalities Test (SDMT) may decrease more rapidly in patients with pediatric-onset multiple sclerosis (MS).
“Children and adolescents who develop [MS] should be monitored closely for cognitive changes and helped to manage the potential challenges that early-onset multiple sclerosis poses for cognitive abilities later in life,” Kyla A. McKay, PhD, a researcher at Karolinska Institutet in Stockholm, and colleagues wrote.
Prior research has found that an SDMT score of 55 may be a point at which a person with MS is “employed but work challenged.” In the present study, patients with pediatric-onset MS reached this threshold at about age 34 years, whereas patients with adult-onset MS reached it at approximately 50 years. These findings suggest that the groups’ different cognitive outcomes “may be meaningful,” the researchers wrote.
Onset of MS before age 18 years occurs in 2%-10% of cases, but few studies have looked at cognitive outcomes of patients with pediatric-onset MS in adulthood. Cognitive impairment is common in patients with MS and may affect quality of life, social functioning, and employment.
To compare changes in cognitive function over time in adults with pediatric-onset MS versus adults with adult-onset MS, Dr. McKay and colleagues conducted a population-based, longitudinal cohort study using data from more than 5,700 patients in the Swedish Multiple Sclerosis Registry. The registry includes information from all neurology clinics in Sweden, and the researchers examined data collected between April 2006 and April 2018.
SDMT scores range from 0 to 120, and higher scores indicate greater information-processing efficiency.
The researchers classified patients with MS onset at younger than 18 years as pediatric-onset MS. The researchers excluded patients with fewer than two SDMT scores, patients younger than 18 years or older than 55 years at the time of testing, and patients with disease duration of 30 years or more.
The researchers included 5,704 patients, 300 of whom had pediatric-onset MS (5.3%). About 70% of the patients were female, and 98% had a relapsing-onset disease course. The pediatric-onset MS group had a younger median age at baseline than the adult-onset group did (26 years vs. 38 years). The patients had more than 46,000 SDMT scores, with an average baseline SDMT of 51; the median follow-up time was 3 years.
Patients with pediatric-onset MS had significantly lower SDMT scores (beta coefficient, –3.59), after adjusting for sex, age, disease duration, disease course, total number of SDMTs completed, oral or visual SDMT form, and exposure to disease-modifying therapy. Their scores also declined faster than those of patients with adult-onset MS (beta coefficient, –0.30; 95% confidence interval, –5.56 to –1.54), and they were more likely to ever have cognitive impairment (odds ratio, 1.44).
“At younger than 30 years, SDMT scores between the ... groups were comparable; but after 30 years of age the trajectories began to diverge,” Dr. McKay and associates wrote. At age 35 years, the mean SDMT score for patients with adult-onset MS was 61, whereas for patients with pediatric-onset MS it was 51. By age 40 years, the mean score was 58 for adult-onset MS versus 46 for pediatric-onset MS.
The study was supported by the Swedish Research Council and the Swedish Brain Foundation and by postdoctoral awards from the Canadian Institutes of Health Research to Dr. McKay and European Committee for Treatment and Research in Multiple Sclerosis to Dr. McKay. Coauthors reported receiving honoraria for speaking and serving on advisory boards for various pharmaceutical companies, as well as receiving research funding from agencies, foundations, and pharmaceutical companies.
SOURCE: McKay KA et al. JAMA Neurol. 2019 Jun 17. doi: 10.1001/jamaneurol.2019.1546.
FROM JAMA NEUROLOGY
Deaths from drugs, alcohol, and suicide increase among millennials
The number of Americans who die each year from alcohol, drugs, or suicide increased to an all-time high in 2017, and the increase was especially pronounced among young adults, according a June 13 report from two public health policy and advocacy organizations. A separate report found that rates of these “deaths of despair” vary widely by state.
The report by Trust for America’s Health and Well Being Trust examined Centers for Disease Control and Prevention (CDC) data with a focus on adults aged 18-34 years. Between 2007 and 2017, alcohol-induced deaths increased by 69%, drug-related deaths by 108%, and suicide by 35% in this age group. These deaths increased in other age groups, too, but often to a lesser extent.
In 1999, there were 7 drug deaths per 100,000 people across age groups, which increased to 22.7 drug deaths per 100,000 people in 2017. Among adults aged 18-34, however, the rate was nearly 31 drug overdose deaths per 100,000 people. Opioid overdoses are largely responsible for the increase in drug-related deaths, and synthetic opioid death rates increased by 6,000% between 1999 and 2017, the report said.
... including the opioid crisis, the skyrocketing costs of education and housing, and entering the job market during the great recession,” according to the report, which was funded with grants from Well Being Trust and the Robert Wood Johnson Foundation.
Screening, treatment, and addressing risk and protective factors are among the measures that the groups recommend to reduce “deaths of despair.”
On June 12, the Commonwealth Fund released a report that examines how drug, alcohol, and suicide death rates across age groups may vary widely by state.
“In Pennsylvania, Maryland, and Ohio, mortality rates from drug overdoses were at least five times higher than rates for alcohol-related deaths and about three times higher than suicide rates,” according to the Commonwealth Fund analysis. “In other states, deaths from suicide and alcohol dominate. In 2017, Montana, Nebraska, the Dakotas, Oregon, and Wyoming saw higher rates of death from suicide and alcohol than from drugs.”
Substance use disorders and suicide might be related, and researchers have suggested that many overdoses may be suicide attempts.
“We assumed that overdoses were accidental ... only to find that many users were actively suicidal, others were playing a version of Russian roulette, and others had passive suicidal ideation,” said Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis, in an interview. Opioid use disorders often are treated as “simply opioid deficiency syndromes,” and physicians may miss when patients have physical, sexual, or emotional trauma, anxiety disorders, or major depression, he said.
The number of Americans who die each year from alcohol, drugs, or suicide increased to an all-time high in 2017, and the increase was especially pronounced among young adults, according a June 13 report from two public health policy and advocacy organizations. A separate report found that rates of these “deaths of despair” vary widely by state.
The report by Trust for America’s Health and Well Being Trust examined Centers for Disease Control and Prevention (CDC) data with a focus on adults aged 18-34 years. Between 2007 and 2017, alcohol-induced deaths increased by 69%, drug-related deaths by 108%, and suicide by 35% in this age group. These deaths increased in other age groups, too, but often to a lesser extent.
In 1999, there were 7 drug deaths per 100,000 people across age groups, which increased to 22.7 drug deaths per 100,000 people in 2017. Among adults aged 18-34, however, the rate was nearly 31 drug overdose deaths per 100,000 people. Opioid overdoses are largely responsible for the increase in drug-related deaths, and synthetic opioid death rates increased by 6,000% between 1999 and 2017, the report said.
... including the opioid crisis, the skyrocketing costs of education and housing, and entering the job market during the great recession,” according to the report, which was funded with grants from Well Being Trust and the Robert Wood Johnson Foundation.
Screening, treatment, and addressing risk and protective factors are among the measures that the groups recommend to reduce “deaths of despair.”
On June 12, the Commonwealth Fund released a report that examines how drug, alcohol, and suicide death rates across age groups may vary widely by state.
“In Pennsylvania, Maryland, and Ohio, mortality rates from drug overdoses were at least five times higher than rates for alcohol-related deaths and about three times higher than suicide rates,” according to the Commonwealth Fund analysis. “In other states, deaths from suicide and alcohol dominate. In 2017, Montana, Nebraska, the Dakotas, Oregon, and Wyoming saw higher rates of death from suicide and alcohol than from drugs.”
Substance use disorders and suicide might be related, and researchers have suggested that many overdoses may be suicide attempts.
“We assumed that overdoses were accidental ... only to find that many users were actively suicidal, others were playing a version of Russian roulette, and others had passive suicidal ideation,” said Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis, in an interview. Opioid use disorders often are treated as “simply opioid deficiency syndromes,” and physicians may miss when patients have physical, sexual, or emotional trauma, anxiety disorders, or major depression, he said.
The number of Americans who die each year from alcohol, drugs, or suicide increased to an all-time high in 2017, and the increase was especially pronounced among young adults, according a June 13 report from two public health policy and advocacy organizations. A separate report found that rates of these “deaths of despair” vary widely by state.
The report by Trust for America’s Health and Well Being Trust examined Centers for Disease Control and Prevention (CDC) data with a focus on adults aged 18-34 years. Between 2007 and 2017, alcohol-induced deaths increased by 69%, drug-related deaths by 108%, and suicide by 35% in this age group. These deaths increased in other age groups, too, but often to a lesser extent.
In 1999, there were 7 drug deaths per 100,000 people across age groups, which increased to 22.7 drug deaths per 100,000 people in 2017. Among adults aged 18-34, however, the rate was nearly 31 drug overdose deaths per 100,000 people. Opioid overdoses are largely responsible for the increase in drug-related deaths, and synthetic opioid death rates increased by 6,000% between 1999 and 2017, the report said.
... including the opioid crisis, the skyrocketing costs of education and housing, and entering the job market during the great recession,” according to the report, which was funded with grants from Well Being Trust and the Robert Wood Johnson Foundation.
Screening, treatment, and addressing risk and protective factors are among the measures that the groups recommend to reduce “deaths of despair.”
On June 12, the Commonwealth Fund released a report that examines how drug, alcohol, and suicide death rates across age groups may vary widely by state.
“In Pennsylvania, Maryland, and Ohio, mortality rates from drug overdoses were at least five times higher than rates for alcohol-related deaths and about three times higher than suicide rates,” according to the Commonwealth Fund analysis. “In other states, deaths from suicide and alcohol dominate. In 2017, Montana, Nebraska, the Dakotas, Oregon, and Wyoming saw higher rates of death from suicide and alcohol than from drugs.”
Substance use disorders and suicide might be related, and researchers have suggested that many overdoses may be suicide attempts.
“We assumed that overdoses were accidental ... only to find that many users were actively suicidal, others were playing a version of Russian roulette, and others had passive suicidal ideation,” said Mark S. Gold, MD, adjunct professor of psychiatry at Washington University in St. Louis, in an interview. Opioid use disorders often are treated as “simply opioid deficiency syndromes,” and physicians may miss when patients have physical, sexual, or emotional trauma, anxiety disorders, or major depression, he said.
Chronic opioid use may be common in patients with ankylosing spondylitis
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
FROM THE JOURNAL OF RHEUMATOLOGY
Pediatric MS often goes untreated in the year after diagnosis
SEATTLE – Females may be more likely than males to receive DMT during this time, said Chinmay Deshpande, PhD, at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pediatric onset of MS occurs in 3-5% of patients with the disease, and the median age of pediatric onset is 15 years. This population tends to have a high relapse rate and may develop disability at a younger age, said Dr. Deshpande, associate director of health economics and outcomes research at Novartis. “There have been very few studies done on this population, especially in the clinical trial setting. ... Physicians face considerable uncertainty in how to treat these patients.”
Observational data
To assess the proportion of patients with pediatric MS who receive DMT in the year after diagnosis, Dr. Deshpande and colleagues analyzed retrospective observational data from the Truven Health Marketscan Commercial and Encounters administrative claims databases. They studied patients who received an MS diagnosis between Jan. 1, 2010, and Dec. 31, 2016. In addition, they examined which DMTs were used as first-line therapies, whether prescribing patterns changed between 2010 and 2017, and time to treatment discontinuation or switch.
The databases included data from more than 182,000 patients with two or more claims of MS diagnosis. After including only patients age 17 years or younger at the index diagnosis date who had insurance during the 6 months prior to the index date and 12 months after the index date and who did not use DMT during the 6 months prior to the index date, 288 patients remained in the analysis. Patients had an average age of about 14 years.
The primary outcome was the proportion of patients who started DMT in the year after MS diagnosis. “The proportion of untreated patients within their first year of diagnosis was around 65%,” said Dr. Deshpande. On average, treated patients were slightly older than untreated patients (15.0 years vs. 13.3 years). Among treated patients, 75% were female, and 25% were male. Overall, however, 61% were female and 39% were male. The difference in treatment by gender was surprising and the reason for it is not understood, Dr. Deshpande said. One possibility is that the difference relates to earlier maturation in females, but that is only a hypothesis, he said.
Glatiramer acetate and interferon beta-1a were first-line DMTs for 48% and 30.6% of the treated patients, respectively. Dimethyl fumarate (7.1%), natalizumab (5.1%), fingolimod (4.1%), interferon beta-1b (4.1%), and peginterferon beta-1a (1%) also were used as first-line therapy.
Twenty percent of patients who received DMT switched to another medication during the follow-up period. The median time of switching was within 6 months of starting first-line therapy. Most patients who discontinued DMT – that is, they did not have any DMT for 60 days after stopping their first DMT – did so within 10 months of diagnosis.
Use of newer medications
Overall, the use of glatiramer acetate and interferons has decreased over time, and while the use of newer DMTs has increased, the trend is not consistent. “With the growing uptake of newer oral and infusible DMTs over the recent years, there is a need to increase treatment awareness in the pediatric MS population and to inform currently approved treatment options to the prescribers,” Dr. Deshpande and colleagues said.
The claims database is generalizable and nationally representative, but it does not include clinical or MRI data. “It’s hard to understand the reasoning why they discontinued or why they are switching,” Dr. Deshpande said. In addition, the sample size was relatively small, and the results should be interpreted accordingly, he said.
Novartis funded the study, and Dr. Deshpande and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
SOURCE: Greenberg B et al. CMSC 2019, Abstract DXM02.
SEATTLE – Females may be more likely than males to receive DMT during this time, said Chinmay Deshpande, PhD, at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pediatric onset of MS occurs in 3-5% of patients with the disease, and the median age of pediatric onset is 15 years. This population tends to have a high relapse rate and may develop disability at a younger age, said Dr. Deshpande, associate director of health economics and outcomes research at Novartis. “There have been very few studies done on this population, especially in the clinical trial setting. ... Physicians face considerable uncertainty in how to treat these patients.”
Observational data
To assess the proportion of patients with pediatric MS who receive DMT in the year after diagnosis, Dr. Deshpande and colleagues analyzed retrospective observational data from the Truven Health Marketscan Commercial and Encounters administrative claims databases. They studied patients who received an MS diagnosis between Jan. 1, 2010, and Dec. 31, 2016. In addition, they examined which DMTs were used as first-line therapies, whether prescribing patterns changed between 2010 and 2017, and time to treatment discontinuation or switch.
The databases included data from more than 182,000 patients with two or more claims of MS diagnosis. After including only patients age 17 years or younger at the index diagnosis date who had insurance during the 6 months prior to the index date and 12 months after the index date and who did not use DMT during the 6 months prior to the index date, 288 patients remained in the analysis. Patients had an average age of about 14 years.
The primary outcome was the proportion of patients who started DMT in the year after MS diagnosis. “The proportion of untreated patients within their first year of diagnosis was around 65%,” said Dr. Deshpande. On average, treated patients were slightly older than untreated patients (15.0 years vs. 13.3 years). Among treated patients, 75% were female, and 25% were male. Overall, however, 61% were female and 39% were male. The difference in treatment by gender was surprising and the reason for it is not understood, Dr. Deshpande said. One possibility is that the difference relates to earlier maturation in females, but that is only a hypothesis, he said.
Glatiramer acetate and interferon beta-1a were first-line DMTs for 48% and 30.6% of the treated patients, respectively. Dimethyl fumarate (7.1%), natalizumab (5.1%), fingolimod (4.1%), interferon beta-1b (4.1%), and peginterferon beta-1a (1%) also were used as first-line therapy.
Twenty percent of patients who received DMT switched to another medication during the follow-up period. The median time of switching was within 6 months of starting first-line therapy. Most patients who discontinued DMT – that is, they did not have any DMT for 60 days after stopping their first DMT – did so within 10 months of diagnosis.
Use of newer medications
Overall, the use of glatiramer acetate and interferons has decreased over time, and while the use of newer DMTs has increased, the trend is not consistent. “With the growing uptake of newer oral and infusible DMTs over the recent years, there is a need to increase treatment awareness in the pediatric MS population and to inform currently approved treatment options to the prescribers,” Dr. Deshpande and colleagues said.
The claims database is generalizable and nationally representative, but it does not include clinical or MRI data. “It’s hard to understand the reasoning why they discontinued or why they are switching,” Dr. Deshpande said. In addition, the sample size was relatively small, and the results should be interpreted accordingly, he said.
Novartis funded the study, and Dr. Deshpande and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
SOURCE: Greenberg B et al. CMSC 2019, Abstract DXM02.
SEATTLE – Females may be more likely than males to receive DMT during this time, said Chinmay Deshpande, PhD, at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pediatric onset of MS occurs in 3-5% of patients with the disease, and the median age of pediatric onset is 15 years. This population tends to have a high relapse rate and may develop disability at a younger age, said Dr. Deshpande, associate director of health economics and outcomes research at Novartis. “There have been very few studies done on this population, especially in the clinical trial setting. ... Physicians face considerable uncertainty in how to treat these patients.”
Observational data
To assess the proportion of patients with pediatric MS who receive DMT in the year after diagnosis, Dr. Deshpande and colleagues analyzed retrospective observational data from the Truven Health Marketscan Commercial and Encounters administrative claims databases. They studied patients who received an MS diagnosis between Jan. 1, 2010, and Dec. 31, 2016. In addition, they examined which DMTs were used as first-line therapies, whether prescribing patterns changed between 2010 and 2017, and time to treatment discontinuation or switch.
The databases included data from more than 182,000 patients with two or more claims of MS diagnosis. After including only patients age 17 years or younger at the index diagnosis date who had insurance during the 6 months prior to the index date and 12 months after the index date and who did not use DMT during the 6 months prior to the index date, 288 patients remained in the analysis. Patients had an average age of about 14 years.
The primary outcome was the proportion of patients who started DMT in the year after MS diagnosis. “The proportion of untreated patients within their first year of diagnosis was around 65%,” said Dr. Deshpande. On average, treated patients were slightly older than untreated patients (15.0 years vs. 13.3 years). Among treated patients, 75% were female, and 25% were male. Overall, however, 61% were female and 39% were male. The difference in treatment by gender was surprising and the reason for it is not understood, Dr. Deshpande said. One possibility is that the difference relates to earlier maturation in females, but that is only a hypothesis, he said.
Glatiramer acetate and interferon beta-1a were first-line DMTs for 48% and 30.6% of the treated patients, respectively. Dimethyl fumarate (7.1%), natalizumab (5.1%), fingolimod (4.1%), interferon beta-1b (4.1%), and peginterferon beta-1a (1%) also were used as first-line therapy.
Twenty percent of patients who received DMT switched to another medication during the follow-up period. The median time of switching was within 6 months of starting first-line therapy. Most patients who discontinued DMT – that is, they did not have any DMT for 60 days after stopping their first DMT – did so within 10 months of diagnosis.
Use of newer medications
Overall, the use of glatiramer acetate and interferons has decreased over time, and while the use of newer DMTs has increased, the trend is not consistent. “With the growing uptake of newer oral and infusible DMTs over the recent years, there is a need to increase treatment awareness in the pediatric MS population and to inform currently approved treatment options to the prescribers,” Dr. Deshpande and colleagues said.
The claims database is generalizable and nationally representative, but it does not include clinical or MRI data. “It’s hard to understand the reasoning why they discontinued or why they are switching,” Dr. Deshpande said. In addition, the sample size was relatively small, and the results should be interpreted accordingly, he said.
Novartis funded the study, and Dr. Deshpande and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
SOURCE: Greenberg B et al. CMSC 2019, Abstract DXM02.
REPORTING FROM CMSC 2019
Which interventions can treat cognitive fatigue?
SEATTLE – Cognitive fatigue in patients with neurologic disease is a common problem with few objectively studied treatments, according to a systematic review presented at the annual meeting of the Consortium of Multiple Sclerosis Centers., the review authors said.
One other objective trial found that Fampridine-SR (Ampyra) did not reduce cognitive fatigue in patients with multiple sclerosis (MS).
The researchers screened for studies across various neurologic conditions, and found that both trials were in patients with MS, “suggesting that more emphasis is given to this issue in this population,” said review author Alyssa Lindsay-Brown, a researcher at Ottawa Hospital Research Institute, and her collaborators. “This review highlighted the paucity of interventions designed to target objectively measured cognitive fatigability and demonstrates the need for further research in this area.”
Investigators have examined self-reported fatigue in patients with neurologic disease, but objective cognitive fatigability, the inability to maintain optimal task performance during a sustained cognitive task, is not well understood, and the best approach to treating cognitive fatigue is unclear, said Ms. Lindsay-Brown and colleagues. To determine how researchers objectively measure cognitive fatigability and summarize currently available treatments, they conducted a systematic literature review.
The researchers registered the review protocol with the PROSPERO international prospective register of systematic reviews and searched databases for studies that objectively measured cognitive fatigability in patients with neurologic disorders aged 18-65 years. They searched for randomized controlled trials, case-control studies, and case reports and case series published in English between 1980 and February 2019.
The authors reviewed the studies using a modified Cochrane Data Extraction Template and assessed their quality and risk of bias. They decided in advance to group studies according to whether they evaluated pharmacologic, procedural, or behavioral interventions.
The search initially yielded 431 records, and the authors assessed 28 full-text articles for possible inclusion. They ultimately included 2 studies in their qualitative synthesis.
A 2017 pharmacologic study by Morrow et al. sought to determine whether Fampridine-SR objectively improves cognitive fatigability in 60 patients with MS (Mult Scler Relat Disord. 2017 Jan;11:4-9.). This study compared the number of responses from the last third to the first third on the Paced Auditory Serial Addition Test (PASAT). Patients performed better with placebo than with Fampridine-SR.
A 2018 procedural study by Fiene at al. assessed tDCS over the prefrontal cortex in 15 patients with MS (J Neurol. 2018 Mar;265[3]:607-17.). The investigators objectively measured P300 event-related potential and reaction times on an alertness test. Compared with sham, anodal tDCS increased P300 amplitude and reduced fatigue-related decrements in reaction time.
The search did not identify any behavioral interventions for objective cognitive fatigability. “Given the known benefit of behavioral interventions at improving subjectively measured fatigue, future research should investigate whether these effects are transferable to objectively measured cognitive fatigability,” the review authors concluded. “If behavioral interventions demonstrate promise, then future studies should evaluate these against the beneficial, but preliminary, outcomes from tDCS.”
The authors had no disclosures.
SOURCE: Lindsay-Brown A et al. CMSC 2019, Abstract NNN10.
SEATTLE – Cognitive fatigue in patients with neurologic disease is a common problem with few objectively studied treatments, according to a systematic review presented at the annual meeting of the Consortium of Multiple Sclerosis Centers., the review authors said.
One other objective trial found that Fampridine-SR (Ampyra) did not reduce cognitive fatigue in patients with multiple sclerosis (MS).
The researchers screened for studies across various neurologic conditions, and found that both trials were in patients with MS, “suggesting that more emphasis is given to this issue in this population,” said review author Alyssa Lindsay-Brown, a researcher at Ottawa Hospital Research Institute, and her collaborators. “This review highlighted the paucity of interventions designed to target objectively measured cognitive fatigability and demonstrates the need for further research in this area.”
Investigators have examined self-reported fatigue in patients with neurologic disease, but objective cognitive fatigability, the inability to maintain optimal task performance during a sustained cognitive task, is not well understood, and the best approach to treating cognitive fatigue is unclear, said Ms. Lindsay-Brown and colleagues. To determine how researchers objectively measure cognitive fatigability and summarize currently available treatments, they conducted a systematic literature review.
The researchers registered the review protocol with the PROSPERO international prospective register of systematic reviews and searched databases for studies that objectively measured cognitive fatigability in patients with neurologic disorders aged 18-65 years. They searched for randomized controlled trials, case-control studies, and case reports and case series published in English between 1980 and February 2019.
The authors reviewed the studies using a modified Cochrane Data Extraction Template and assessed their quality and risk of bias. They decided in advance to group studies according to whether they evaluated pharmacologic, procedural, or behavioral interventions.
The search initially yielded 431 records, and the authors assessed 28 full-text articles for possible inclusion. They ultimately included 2 studies in their qualitative synthesis.
A 2017 pharmacologic study by Morrow et al. sought to determine whether Fampridine-SR objectively improves cognitive fatigability in 60 patients with MS (Mult Scler Relat Disord. 2017 Jan;11:4-9.). This study compared the number of responses from the last third to the first third on the Paced Auditory Serial Addition Test (PASAT). Patients performed better with placebo than with Fampridine-SR.
A 2018 procedural study by Fiene at al. assessed tDCS over the prefrontal cortex in 15 patients with MS (J Neurol. 2018 Mar;265[3]:607-17.). The investigators objectively measured P300 event-related potential and reaction times on an alertness test. Compared with sham, anodal tDCS increased P300 amplitude and reduced fatigue-related decrements in reaction time.
The search did not identify any behavioral interventions for objective cognitive fatigability. “Given the known benefit of behavioral interventions at improving subjectively measured fatigue, future research should investigate whether these effects are transferable to objectively measured cognitive fatigability,” the review authors concluded. “If behavioral interventions demonstrate promise, then future studies should evaluate these against the beneficial, but preliminary, outcomes from tDCS.”
The authors had no disclosures.
SOURCE: Lindsay-Brown A et al. CMSC 2019, Abstract NNN10.
SEATTLE – Cognitive fatigue in patients with neurologic disease is a common problem with few objectively studied treatments, according to a systematic review presented at the annual meeting of the Consortium of Multiple Sclerosis Centers., the review authors said.
One other objective trial found that Fampridine-SR (Ampyra) did not reduce cognitive fatigue in patients with multiple sclerosis (MS).
The researchers screened for studies across various neurologic conditions, and found that both trials were in patients with MS, “suggesting that more emphasis is given to this issue in this population,” said review author Alyssa Lindsay-Brown, a researcher at Ottawa Hospital Research Institute, and her collaborators. “This review highlighted the paucity of interventions designed to target objectively measured cognitive fatigability and demonstrates the need for further research in this area.”
Investigators have examined self-reported fatigue in patients with neurologic disease, but objective cognitive fatigability, the inability to maintain optimal task performance during a sustained cognitive task, is not well understood, and the best approach to treating cognitive fatigue is unclear, said Ms. Lindsay-Brown and colleagues. To determine how researchers objectively measure cognitive fatigability and summarize currently available treatments, they conducted a systematic literature review.
The researchers registered the review protocol with the PROSPERO international prospective register of systematic reviews and searched databases for studies that objectively measured cognitive fatigability in patients with neurologic disorders aged 18-65 years. They searched for randomized controlled trials, case-control studies, and case reports and case series published in English between 1980 and February 2019.
The authors reviewed the studies using a modified Cochrane Data Extraction Template and assessed their quality and risk of bias. They decided in advance to group studies according to whether they evaluated pharmacologic, procedural, or behavioral interventions.
The search initially yielded 431 records, and the authors assessed 28 full-text articles for possible inclusion. They ultimately included 2 studies in their qualitative synthesis.
A 2017 pharmacologic study by Morrow et al. sought to determine whether Fampridine-SR objectively improves cognitive fatigability in 60 patients with MS (Mult Scler Relat Disord. 2017 Jan;11:4-9.). This study compared the number of responses from the last third to the first third on the Paced Auditory Serial Addition Test (PASAT). Patients performed better with placebo than with Fampridine-SR.
A 2018 procedural study by Fiene at al. assessed tDCS over the prefrontal cortex in 15 patients with MS (J Neurol. 2018 Mar;265[3]:607-17.). The investigators objectively measured P300 event-related potential and reaction times on an alertness test. Compared with sham, anodal tDCS increased P300 amplitude and reduced fatigue-related decrements in reaction time.
The search did not identify any behavioral interventions for objective cognitive fatigability. “Given the known benefit of behavioral interventions at improving subjectively measured fatigue, future research should investigate whether these effects are transferable to objectively measured cognitive fatigability,” the review authors concluded. “If behavioral interventions demonstrate promise, then future studies should evaluate these against the beneficial, but preliminary, outcomes from tDCS.”
The authors had no disclosures.
SOURCE: Lindsay-Brown A et al. CMSC 2019, Abstract NNN10.
REPORTING FROM CMSC 2019