User login
FDA grants priority review to multiple myeloma treatment
, a monoclonal antibody treatment for newly diagnosed multiple myeloma patients who are ineligible for autologous stem cell transplant.
The current application is based on the randomized, multicenter, phase 3 ALCYONE study of daratumumab in combination with bortezomib (Velcade), melphalan, and prednisone (VMP) in de novo multiple myeloma patients.
Priority review is an FDA designation for drugs that treat a serious condition and may provide a significant improvement in safety or efficacy. The agency has assigned the drug a Prescription Drug User Fee Act date of May 21, which is a target date for an approval decision.
Daratumumab is being developed by Janssen Biotech, in partnership with Genmab.
, a monoclonal antibody treatment for newly diagnosed multiple myeloma patients who are ineligible for autologous stem cell transplant.
The current application is based on the randomized, multicenter, phase 3 ALCYONE study of daratumumab in combination with bortezomib (Velcade), melphalan, and prednisone (VMP) in de novo multiple myeloma patients.
Priority review is an FDA designation for drugs that treat a serious condition and may provide a significant improvement in safety or efficacy. The agency has assigned the drug a Prescription Drug User Fee Act date of May 21, which is a target date for an approval decision.
Daratumumab is being developed by Janssen Biotech, in partnership with Genmab.
, a monoclonal antibody treatment for newly diagnosed multiple myeloma patients who are ineligible for autologous stem cell transplant.
The current application is based on the randomized, multicenter, phase 3 ALCYONE study of daratumumab in combination with bortezomib (Velcade), melphalan, and prednisone (VMP) in de novo multiple myeloma patients.
Priority review is an FDA designation for drugs that treat a serious condition and may provide a significant improvement in safety or efficacy. The agency has assigned the drug a Prescription Drug User Fee Act date of May 21, which is a target date for an approval decision.
Daratumumab is being developed by Janssen Biotech, in partnership with Genmab.
Written exposure therapy rivals cognitive processing therapy for PTSD
Cognitive processing therapy may offer a greater benefit over time for posttraumatic stress disorder, but writing therapy offers a viable treatment in fewer sessions.
“Our results add to mounting research showing that the dose of therapy needed for beneficial outcomes for individuals with PTSD is not as large as what was once previously thought,” wrote Denise M. Sloan, PhD, of the National Center for PTSD, Boston, and her colleagues. “Our findings extend those prior studies by demonstrating that not only can PTSD symptoms be reduced significantly with less therapeutic exposure but that not as many therapy sessions are required.”
In a 1:1 randomized clinical trial, Dr. Sloan and her colleagues compared the effectiveness of written exposure therapy (WET) and cognitive processing therapy (CPT) in treating PTSD in 126 veteran and nonveteran adults, split evenly into the two therapy groups. and focused on details of the event, including thoughts and feelings associated with it. The CPT intervention was a 12-session trauma-focused therapy with a limited take-home writing component. It focused on helping patients recognize and challenge dysfunctional cognitions associated with traumatic events, the investigators wrote in JAMA Psychiatry.
When Dr. Sloan and her colleagues looked at the patients’ mean Clinician Administered PTSD Scale for DSM-5, or CAPS-5 score, a measure of PTSD symptom severity, they found that the WET and CPT groups’ scores were similar at 6 weeks, 12, weeks, and 36 weeks. At the 24-week assessment, the CAPS-5 score for those in the CPT group (20.92) was significantly lower than it was for those in the WET group (25.23) (mean difference, 4.31 points; 95% confidence interval, –1.37 to 9.99).
In addition, the CPT group had a higher dropout rate (31.7%) than did the WET group (6.3%). The investigators concluded, however, that both therapies are effective. “Written exposure therapy should be considered by clinicians to be a viable treatment option that can address some of the barriers to receiving and implementing CPT and prolonged exposure that have been noted in health care settings,” Dr. Sloan and her colleagues wrote.
This study was funded by a grant from the National Institute of Mental Health. None of the authors had financial conflicts to report. Further details on this information can be found here.
SOURCE: Sloan DM. 2018 Jan 17. doi: 10.1001/jamapsychiatry.2017.4249.
Cognitive processing therapy may offer a greater benefit over time for posttraumatic stress disorder, but writing therapy offers a viable treatment in fewer sessions.
“Our results add to mounting research showing that the dose of therapy needed for beneficial outcomes for individuals with PTSD is not as large as what was once previously thought,” wrote Denise M. Sloan, PhD, of the National Center for PTSD, Boston, and her colleagues. “Our findings extend those prior studies by demonstrating that not only can PTSD symptoms be reduced significantly with less therapeutic exposure but that not as many therapy sessions are required.”
In a 1:1 randomized clinical trial, Dr. Sloan and her colleagues compared the effectiveness of written exposure therapy (WET) and cognitive processing therapy (CPT) in treating PTSD in 126 veteran and nonveteran adults, split evenly into the two therapy groups. and focused on details of the event, including thoughts and feelings associated with it. The CPT intervention was a 12-session trauma-focused therapy with a limited take-home writing component. It focused on helping patients recognize and challenge dysfunctional cognitions associated with traumatic events, the investigators wrote in JAMA Psychiatry.
When Dr. Sloan and her colleagues looked at the patients’ mean Clinician Administered PTSD Scale for DSM-5, or CAPS-5 score, a measure of PTSD symptom severity, they found that the WET and CPT groups’ scores were similar at 6 weeks, 12, weeks, and 36 weeks. At the 24-week assessment, the CAPS-5 score for those in the CPT group (20.92) was significantly lower than it was for those in the WET group (25.23) (mean difference, 4.31 points; 95% confidence interval, –1.37 to 9.99).
In addition, the CPT group had a higher dropout rate (31.7%) than did the WET group (6.3%). The investigators concluded, however, that both therapies are effective. “Written exposure therapy should be considered by clinicians to be a viable treatment option that can address some of the barriers to receiving and implementing CPT and prolonged exposure that have been noted in health care settings,” Dr. Sloan and her colleagues wrote.
This study was funded by a grant from the National Institute of Mental Health. None of the authors had financial conflicts to report. Further details on this information can be found here.
SOURCE: Sloan DM. 2018 Jan 17. doi: 10.1001/jamapsychiatry.2017.4249.
Cognitive processing therapy may offer a greater benefit over time for posttraumatic stress disorder, but writing therapy offers a viable treatment in fewer sessions.
“Our results add to mounting research showing that the dose of therapy needed for beneficial outcomes for individuals with PTSD is not as large as what was once previously thought,” wrote Denise M. Sloan, PhD, of the National Center for PTSD, Boston, and her colleagues. “Our findings extend those prior studies by demonstrating that not only can PTSD symptoms be reduced significantly with less therapeutic exposure but that not as many therapy sessions are required.”
In a 1:1 randomized clinical trial, Dr. Sloan and her colleagues compared the effectiveness of written exposure therapy (WET) and cognitive processing therapy (CPT) in treating PTSD in 126 veteran and nonveteran adults, split evenly into the two therapy groups. and focused on details of the event, including thoughts and feelings associated with it. The CPT intervention was a 12-session trauma-focused therapy with a limited take-home writing component. It focused on helping patients recognize and challenge dysfunctional cognitions associated with traumatic events, the investigators wrote in JAMA Psychiatry.
When Dr. Sloan and her colleagues looked at the patients’ mean Clinician Administered PTSD Scale for DSM-5, or CAPS-5 score, a measure of PTSD symptom severity, they found that the WET and CPT groups’ scores were similar at 6 weeks, 12, weeks, and 36 weeks. At the 24-week assessment, the CAPS-5 score for those in the CPT group (20.92) was significantly lower than it was for those in the WET group (25.23) (mean difference, 4.31 points; 95% confidence interval, –1.37 to 9.99).
In addition, the CPT group had a higher dropout rate (31.7%) than did the WET group (6.3%). The investigators concluded, however, that both therapies are effective. “Written exposure therapy should be considered by clinicians to be a viable treatment option that can address some of the barriers to receiving and implementing CPT and prolonged exposure that have been noted in health care settings,” Dr. Sloan and her colleagues wrote.
This study was funded by a grant from the National Institute of Mental Health. None of the authors had financial conflicts to report. Further details on this information can be found here.
SOURCE: Sloan DM. 2018 Jan 17. doi: 10.1001/jamapsychiatry.2017.4249.
FROM JAMA Psychiatry
FDA: LifeVest wearable defibrillator has safety issue
The Zoll LifeVest 4000, a wearable defibrillator, could fail to deliver a treatment shock after displaying the message “Call for service: Device has a problem that may require service. Call ZOLL for service, Message Code 102,” according to the FDA.
“Failure to contact Zoll and immediately replace the device after Message Code 102 appears on the device screen may result in serious patient harm or death of the patient because the device may fail to deliver therapy appropriately when needed” according to an FDA press release.
Only one death associated with “Message Code 102” malfunction of LifeVest has been reported, but about 0.1% of devices have displayed the “Message Code 102” error. According to Zoll, roughly 33,670 devices have been distributed as of Nov. 14, 2017, with nearly 75% of them distributed in the United States.
The FDA has indicated that it will continue to work with Zoll to monitor adverse events associated with the “Message Code 102” error and work on finding a permanent solution to this problem. Recommendations for physicians, caregivers, and patients regarding how to respond to error messages can be found here.
The Zoll LifeVest 4000, a wearable defibrillator, could fail to deliver a treatment shock after displaying the message “Call for service: Device has a problem that may require service. Call ZOLL for service, Message Code 102,” according to the FDA.
“Failure to contact Zoll and immediately replace the device after Message Code 102 appears on the device screen may result in serious patient harm or death of the patient because the device may fail to deliver therapy appropriately when needed” according to an FDA press release.
Only one death associated with “Message Code 102” malfunction of LifeVest has been reported, but about 0.1% of devices have displayed the “Message Code 102” error. According to Zoll, roughly 33,670 devices have been distributed as of Nov. 14, 2017, with nearly 75% of them distributed in the United States.
The FDA has indicated that it will continue to work with Zoll to monitor adverse events associated with the “Message Code 102” error and work on finding a permanent solution to this problem. Recommendations for physicians, caregivers, and patients regarding how to respond to error messages can be found here.
The Zoll LifeVest 4000, a wearable defibrillator, could fail to deliver a treatment shock after displaying the message “Call for service: Device has a problem that may require service. Call ZOLL for service, Message Code 102,” according to the FDA.
“Failure to contact Zoll and immediately replace the device after Message Code 102 appears on the device screen may result in serious patient harm or death of the patient because the device may fail to deliver therapy appropriately when needed” according to an FDA press release.
Only one death associated with “Message Code 102” malfunction of LifeVest has been reported, but about 0.1% of devices have displayed the “Message Code 102” error. According to Zoll, roughly 33,670 devices have been distributed as of Nov. 14, 2017, with nearly 75% of them distributed in the United States.
The FDA has indicated that it will continue to work with Zoll to monitor adverse events associated with the “Message Code 102” error and work on finding a permanent solution to this problem. Recommendations for physicians, caregivers, and patients regarding how to respond to error messages can be found here.
Antiseizure medication tied to improved deficits in schizophrenia
Altered glutamate signaling tied to variants of a protein called Thorase has been associated with schizophrenia, and the antiseizure medication perampanel might help regulate such deficits, a study showed.
“Perampanel treatment … could offer a potential therapeutic opportunity for treating disorders associated with abnormal AMPAR-mediated neurotransmission,” wrote George K.E. Umanah, PhD, of Johns Hopkins University, Baltimore, and his associates. AMPARs, or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors, mediate rapid synaptic transmission in the brain.
The conclusions are based on bidirectional sequence data from a group of adults with schizophrenia and controls, and a murine study.
In the human portion of the study, the researchers analyzed bidirectional sequence data for ATAD1, a protein that codes for Thorase in an Ashkenazi Jewish population. In 712 schizophrenia patients and 649 healthy patients, Dr. Umanah and his associates found three rare gene variants in five individuals. The variants, R9H and D221H, were present only in the patients with schizophrenia. Another variant, E290K, was present in schizophrenia patients as well as in unscreened individuals. The researchers said that the variants found in this analysis might be implicated in schizophrenia.
Building on the observations from the human portion of the study, Dr. Umanah and his colleagues conducted a battery of tests to see whether the observed Thorase variants had any psychological effects on mice that were heterozygous for these variants. The researchers found that these heterozygous Thorase mice were sensitive to psychostimulants, and exhibited impaired memory and social behaviors. Heterozygous Thorase mice also displayed long-term memory and associative learning deficits. Those deficits improved, however, after perampanel was administered.
This study was supported in part by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. The authors declared that they have no conflicts of interest.
Read the full study in Science Translational Medicine (2017 Dec 13;9[420]. doi: 10.1126/scitranslmed.aah4985).
[email protected]
Altered glutamate signaling tied to variants of a protein called Thorase has been associated with schizophrenia, and the antiseizure medication perampanel might help regulate such deficits, a study showed.
“Perampanel treatment … could offer a potential therapeutic opportunity for treating disorders associated with abnormal AMPAR-mediated neurotransmission,” wrote George K.E. Umanah, PhD, of Johns Hopkins University, Baltimore, and his associates. AMPARs, or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors, mediate rapid synaptic transmission in the brain.
The conclusions are based on bidirectional sequence data from a group of adults with schizophrenia and controls, and a murine study.
In the human portion of the study, the researchers analyzed bidirectional sequence data for ATAD1, a protein that codes for Thorase in an Ashkenazi Jewish population. In 712 schizophrenia patients and 649 healthy patients, Dr. Umanah and his associates found three rare gene variants in five individuals. The variants, R9H and D221H, were present only in the patients with schizophrenia. Another variant, E290K, was present in schizophrenia patients as well as in unscreened individuals. The researchers said that the variants found in this analysis might be implicated in schizophrenia.
Building on the observations from the human portion of the study, Dr. Umanah and his colleagues conducted a battery of tests to see whether the observed Thorase variants had any psychological effects on mice that were heterozygous for these variants. The researchers found that these heterozygous Thorase mice were sensitive to psychostimulants, and exhibited impaired memory and social behaviors. Heterozygous Thorase mice also displayed long-term memory and associative learning deficits. Those deficits improved, however, after perampanel was administered.
This study was supported in part by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. The authors declared that they have no conflicts of interest.
Read the full study in Science Translational Medicine (2017 Dec 13;9[420]. doi: 10.1126/scitranslmed.aah4985).
[email protected]
Altered glutamate signaling tied to variants of a protein called Thorase has been associated with schizophrenia, and the antiseizure medication perampanel might help regulate such deficits, a study showed.
“Perampanel treatment … could offer a potential therapeutic opportunity for treating disorders associated with abnormal AMPAR-mediated neurotransmission,” wrote George K.E. Umanah, PhD, of Johns Hopkins University, Baltimore, and his associates. AMPARs, or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors, mediate rapid synaptic transmission in the brain.
The conclusions are based on bidirectional sequence data from a group of adults with schizophrenia and controls, and a murine study.
In the human portion of the study, the researchers analyzed bidirectional sequence data for ATAD1, a protein that codes for Thorase in an Ashkenazi Jewish population. In 712 schizophrenia patients and 649 healthy patients, Dr. Umanah and his associates found three rare gene variants in five individuals. The variants, R9H and D221H, were present only in the patients with schizophrenia. Another variant, E290K, was present in schizophrenia patients as well as in unscreened individuals. The researchers said that the variants found in this analysis might be implicated in schizophrenia.
Building on the observations from the human portion of the study, Dr. Umanah and his colleagues conducted a battery of tests to see whether the observed Thorase variants had any psychological effects on mice that were heterozygous for these variants. The researchers found that these heterozygous Thorase mice were sensitive to psychostimulants, and exhibited impaired memory and social behaviors. Heterozygous Thorase mice also displayed long-term memory and associative learning deficits. Those deficits improved, however, after perampanel was administered.
This study was supported in part by grants from the National Institutes of Health and the Simons Foundation Autism Research Initiative. The authors declared that they have no conflicts of interest.
Read the full study in Science Translational Medicine (2017 Dec 13;9[420]. doi: 10.1126/scitranslmed.aah4985).
[email protected]
FROM SCIENCE TRANSLATIONAL MEDICINE
Novel herpes zoster vaccine is more cost effective than old vaccine
The novel herpes zoster subunit vaccine (HZ/su) is more effective and less expensive than the currently used live attenuated virus (ZVL), according to a study from the Center for Value-Based Research.
Phuc Le, PhD, of the Cleveland Clinic and her colleague Michael Rothberg, MD, conducted an economic analysis of vaccine strategies from the societal perspective. This included the direct medical costs and productivity losses associated with HZ disease and complications.
The one-, two-, and three-way sensitivity analyses examined how different variables affected the cost-effectiveness of different vaccine strategies. The one-way analysis examined the association of input variables and cost-effectiveness. This included HZ/su prices, waning rate and initial efficacy of a dose of HZ/su, and the adherence rate. This analysis revealed that, compared with no vaccination, HZ/su would provide cost savings up to a price of $160, or $80 per dose.
Regardless of circumstance, HZ/su was always more effective than ZVL according to the two-way sensitivity analysis. This analysis took into account the joint effect of price, adherence to two doses of HZ/su, efficacy, and the waning rate of one dose and two doses of HZ/su and ZVL. Compared with ZVL, HZ/su would be less costly up to a price of $350 per series.
Adherence rates to vaccination schedules were important in determining the efficacy and waning rate which ultimately effected cost-effectiveness. The three-way sensitivity analysis found that, if HZ/su adherence to the second dose was greater than 56.8%, results were insensitive to the variation of single-dose efficacy and waning rate of HZ/su. But if adherence rates fell below 40%, combinations of waning rate and lower efficacy made HZ/su cost ineffective. Most importantly, ZVL was never cost effective for 60-year-old patients.
Despite a projected price of $280 per series, HZ/su is still more effective and less expensive than ZVL for adults 60 years or older. According to Dr. Le and Dr. Rothberg, the assumptions about the vaccine’s efficacy duration and price were reasonable. But, if the vaccine price were to rise in the future, or a single dose becomes much less effective than reported by GlaxoSmithKline, or if adherence to the second dose was remarkably low, the results of the study would be changed.
“An ACIP recommendation stating a preference for HZ/su over ZVL could lead to future price increases, which would render the vaccine no longer cost effective” wrote Dr. Le and Dr. Rothberg. “Therefore, a recommendation linked to periodic reassessment of cost-effectiveness based on the vaccine price might help to mitigate the effect of the recommendation on vaccine affordability.”
Dr. Le and Dr. Rothberg reported having no conflicts of interest.
The HZ/su vaccine is not yet approved by the U.S. Food and Drug Administration, but in 2017, the FDA Advisory Committee unanimously voted in favor of its use in adults age 50 years and older.
SOURCE: Phuc L et al. JAMA Intern Med. 2018 Jan 2. doi: 10.1001/jamainternmed.2017.7431. Najafzadeh M. JAMA Intern Med. 2018. doi: 10.1001/jamainternmed.2017.7442.
The herpes zoster (HZ) virus disproportionately affects elderly populations. As the U.S. population ages, tools and mechanisms to reduce the clinical and economic burden of HZ will be needed in the coming years.
The work of Dr. Le and Dr. Rothberg presents the results of an economic evaluation on randomized clinical trials of a yet-to-be-approved novel HZ subunit vaccine (HZ/su) to determine the economic and clinical benefit of the new vaccine, compared with the currently used vaccine. Although HZ/su is intended to be a two-dose vaccine, the study focused on a one-time vaccine strategy because booster vaccines are unpopular and not recommended by the Advisory Committee on Immunization Practices.
“If priced at $280 per two required doses, HZ/su appears to be a cost-saving option, compared with ZVL and a cost-effective option, compared with no-vaccine strategies,” wrote Dr. Najafzadeh. “However, the value of HZ/su vaccine would be even higher if it could be marketed at a price comparable to that of ZVL.” An added benefit of the HZ/su vaccine is that it can be used in immunocompromised patients.
Mehdi Najafzadeh, PhD , is an instructor in medicine at Harvard Medical School, Boston. He also serves as an associate statistician/epidemiologist in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
The herpes zoster (HZ) virus disproportionately affects elderly populations. As the U.S. population ages, tools and mechanisms to reduce the clinical and economic burden of HZ will be needed in the coming years.
The work of Dr. Le and Dr. Rothberg presents the results of an economic evaluation on randomized clinical trials of a yet-to-be-approved novel HZ subunit vaccine (HZ/su) to determine the economic and clinical benefit of the new vaccine, compared with the currently used vaccine. Although HZ/su is intended to be a two-dose vaccine, the study focused on a one-time vaccine strategy because booster vaccines are unpopular and not recommended by the Advisory Committee on Immunization Practices.
“If priced at $280 per two required doses, HZ/su appears to be a cost-saving option, compared with ZVL and a cost-effective option, compared with no-vaccine strategies,” wrote Dr. Najafzadeh. “However, the value of HZ/su vaccine would be even higher if it could be marketed at a price comparable to that of ZVL.” An added benefit of the HZ/su vaccine is that it can be used in immunocompromised patients.
Mehdi Najafzadeh, PhD , is an instructor in medicine at Harvard Medical School, Boston. He also serves as an associate statistician/epidemiologist in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
The herpes zoster (HZ) virus disproportionately affects elderly populations. As the U.S. population ages, tools and mechanisms to reduce the clinical and economic burden of HZ will be needed in the coming years.
The work of Dr. Le and Dr. Rothberg presents the results of an economic evaluation on randomized clinical trials of a yet-to-be-approved novel HZ subunit vaccine (HZ/su) to determine the economic and clinical benefit of the new vaccine, compared with the currently used vaccine. Although HZ/su is intended to be a two-dose vaccine, the study focused on a one-time vaccine strategy because booster vaccines are unpopular and not recommended by the Advisory Committee on Immunization Practices.
“If priced at $280 per two required doses, HZ/su appears to be a cost-saving option, compared with ZVL and a cost-effective option, compared with no-vaccine strategies,” wrote Dr. Najafzadeh. “However, the value of HZ/su vaccine would be even higher if it could be marketed at a price comparable to that of ZVL.” An added benefit of the HZ/su vaccine is that it can be used in immunocompromised patients.
Mehdi Najafzadeh, PhD , is an instructor in medicine at Harvard Medical School, Boston. He also serves as an associate statistician/epidemiologist in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
The novel herpes zoster subunit vaccine (HZ/su) is more effective and less expensive than the currently used live attenuated virus (ZVL), according to a study from the Center for Value-Based Research.
Phuc Le, PhD, of the Cleveland Clinic and her colleague Michael Rothberg, MD, conducted an economic analysis of vaccine strategies from the societal perspective. This included the direct medical costs and productivity losses associated with HZ disease and complications.
The one-, two-, and three-way sensitivity analyses examined how different variables affected the cost-effectiveness of different vaccine strategies. The one-way analysis examined the association of input variables and cost-effectiveness. This included HZ/su prices, waning rate and initial efficacy of a dose of HZ/su, and the adherence rate. This analysis revealed that, compared with no vaccination, HZ/su would provide cost savings up to a price of $160, or $80 per dose.
Regardless of circumstance, HZ/su was always more effective than ZVL according to the two-way sensitivity analysis. This analysis took into account the joint effect of price, adherence to two doses of HZ/su, efficacy, and the waning rate of one dose and two doses of HZ/su and ZVL. Compared with ZVL, HZ/su would be less costly up to a price of $350 per series.
Adherence rates to vaccination schedules were important in determining the efficacy and waning rate which ultimately effected cost-effectiveness. The three-way sensitivity analysis found that, if HZ/su adherence to the second dose was greater than 56.8%, results were insensitive to the variation of single-dose efficacy and waning rate of HZ/su. But if adherence rates fell below 40%, combinations of waning rate and lower efficacy made HZ/su cost ineffective. Most importantly, ZVL was never cost effective for 60-year-old patients.
Despite a projected price of $280 per series, HZ/su is still more effective and less expensive than ZVL for adults 60 years or older. According to Dr. Le and Dr. Rothberg, the assumptions about the vaccine’s efficacy duration and price were reasonable. But, if the vaccine price were to rise in the future, or a single dose becomes much less effective than reported by GlaxoSmithKline, or if adherence to the second dose was remarkably low, the results of the study would be changed.
“An ACIP recommendation stating a preference for HZ/su over ZVL could lead to future price increases, which would render the vaccine no longer cost effective” wrote Dr. Le and Dr. Rothberg. “Therefore, a recommendation linked to periodic reassessment of cost-effectiveness based on the vaccine price might help to mitigate the effect of the recommendation on vaccine affordability.”
Dr. Le and Dr. Rothberg reported having no conflicts of interest.
The HZ/su vaccine is not yet approved by the U.S. Food and Drug Administration, but in 2017, the FDA Advisory Committee unanimously voted in favor of its use in adults age 50 years and older.
SOURCE: Phuc L et al. JAMA Intern Med. 2018 Jan 2. doi: 10.1001/jamainternmed.2017.7431. Najafzadeh M. JAMA Intern Med. 2018. doi: 10.1001/jamainternmed.2017.7442.
The novel herpes zoster subunit vaccine (HZ/su) is more effective and less expensive than the currently used live attenuated virus (ZVL), according to a study from the Center for Value-Based Research.
Phuc Le, PhD, of the Cleveland Clinic and her colleague Michael Rothberg, MD, conducted an economic analysis of vaccine strategies from the societal perspective. This included the direct medical costs and productivity losses associated with HZ disease and complications.
The one-, two-, and three-way sensitivity analyses examined how different variables affected the cost-effectiveness of different vaccine strategies. The one-way analysis examined the association of input variables and cost-effectiveness. This included HZ/su prices, waning rate and initial efficacy of a dose of HZ/su, and the adherence rate. This analysis revealed that, compared with no vaccination, HZ/su would provide cost savings up to a price of $160, or $80 per dose.
Regardless of circumstance, HZ/su was always more effective than ZVL according to the two-way sensitivity analysis. This analysis took into account the joint effect of price, adherence to two doses of HZ/su, efficacy, and the waning rate of one dose and two doses of HZ/su and ZVL. Compared with ZVL, HZ/su would be less costly up to a price of $350 per series.
Adherence rates to vaccination schedules were important in determining the efficacy and waning rate which ultimately effected cost-effectiveness. The three-way sensitivity analysis found that, if HZ/su adherence to the second dose was greater than 56.8%, results were insensitive to the variation of single-dose efficacy and waning rate of HZ/su. But if adherence rates fell below 40%, combinations of waning rate and lower efficacy made HZ/su cost ineffective. Most importantly, ZVL was never cost effective for 60-year-old patients.
Despite a projected price of $280 per series, HZ/su is still more effective and less expensive than ZVL for adults 60 years or older. According to Dr. Le and Dr. Rothberg, the assumptions about the vaccine’s efficacy duration and price were reasonable. But, if the vaccine price were to rise in the future, or a single dose becomes much less effective than reported by GlaxoSmithKline, or if adherence to the second dose was remarkably low, the results of the study would be changed.
“An ACIP recommendation stating a preference for HZ/su over ZVL could lead to future price increases, which would render the vaccine no longer cost effective” wrote Dr. Le and Dr. Rothberg. “Therefore, a recommendation linked to periodic reassessment of cost-effectiveness based on the vaccine price might help to mitigate the effect of the recommendation on vaccine affordability.”
Dr. Le and Dr. Rothberg reported having no conflicts of interest.
The HZ/su vaccine is not yet approved by the U.S. Food and Drug Administration, but in 2017, the FDA Advisory Committee unanimously voted in favor of its use in adults age 50 years and older.
SOURCE: Phuc L et al. JAMA Intern Med. 2018 Jan 2. doi: 10.1001/jamainternmed.2017.7431. Najafzadeh M. JAMA Intern Med. 2018. doi: 10.1001/jamainternmed.2017.7442.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Cost-effectiveness can be an important factor in considering patient treatment for herpes zoster.
Major finding:
Study details: The study was based on U.S. medical literature. Data were derived from adults 60 years or older in patient groups of 100-30,000 from July 1 to July 31, 2017.
Disclosures: None of the researchers had conflicts of interest to report.
Source: L. Phuc et al. JAMA Intern Med. 2018 Jan 2. doi: 10.1001/jamainternmed.2017.7431; Najafzadeh M. JAMA Intern Med. 2018. doi: 10.1001/jamainternmed.2017.7442.
FDA panel doesn’t back inhaled ciprofloxacin for chronic lung infections
HYATTSVILLE, MD – A Food and Drug Administration advisory panel voted against recommending Linhaliq, ciprofloxacin dispersion for inhalation, to treat adult non-cystic fibrosis bronchiectasis (NCFBE) patients who have chronic lung infections with Pseudomonas aeruginosa.
“Two trials that have two very different outcomes – and no matter how we try and explain what the difference was, there was something really missing there,” said advisory committee member Peter Weina, MD, chief of the department of research programs at Walter Reed National Military Medical Center, Bethesda, Md.
NCFBE is often treated with antibacterial drugs, which temporarily reduce inflammation and bacterial load. One of the most common colonizing bacteria in NCFBE infections is P. aeruginosa, which is often associated with increased risk of death and hospital admission.
Prior studies involving inhaled bacterial drugs such as gentamicin and colistin to treat NCFBE have yielded mixed results, and none has been approved for that indication by the FDA.
The FDA granted cipro DI orphan drug status in June 2011 and fast-track approval in August 2014. Cipro DI’s developer, Aradigm, conducted two phase 3 clinical trials to support inhaled ciprofloxacin for the NCFBE indication.
The two phase 3 clinical trials, ORBIT-3 and ORBIT-4, were nearly identical in design. Patients in both were randomized 2:1 to receive cipro DI or placebo once daily for six cycles of 56 days each.
The efficacy results of the ORBIT-3 and ORBIT-4 trials were mixed. In ORBIT-3, there was very little difference between the treatment and placebo arms, with a median difference of 78 days for the primary endpoint of time to first pulmonary exacerbation (PE) (hazard ratio, 0.99; P = .974). ORBIT-3 also showed no difference between treatment and placebo in the frequency of PEs by week 48 of the study (incidence ratio, 0.852).
In contrast, a marginal treatment effect was observed in ORBIT-4, with a median time difference to first PE of 72 days between the placebo and treatment arms (HR, 0.71; P = .032). ORBIT-4 also demonstrated an ability to reduce the number of PEs (incidence ratio, 0.631) by approximately 36.9% by week 48.
Adverse events were the most common reason leading to patient discontinuation in both studies, accounting for 13.1% and 5.3% in the treatment arms of ORBIT-3 and ORBIT-4, respectively.
Despite some of the positive findings in ORBIT-4, FDA presenter LaRee Tracy, PhD, of the FDA’s office of biostatistics, voiced concerns about the trial data – specifically, the failure to reach the primary endpoint in ORBIT-3.
“If I were to be a [statistically speaking] ‘strict’ person, I wouldn’t be looking at the frequency of the [secondary] endpoints, because the primary [endpoint] failed,” Dr. Tracy noted. She also voiced concerns about a re-analysis Aradigm conducted after the trial data were unblinded, stating that the changes made to the original analysis plan “lend a lot of concerns for me.”
Both ORBIT-3 and ORBIT-4 presented uncertainties related to the long-term use of cipro DI. The durability of efficacy and safety findings did not extend beyond a year, leaving some committee members wondering about the development of antibiotic resistance in cipro DI-treated patients. In addition, members were concerned that long-term use of cipro DI could limit the utility of systemic fluoroquinolones to treat severe bacterial and pneumonia infections in NCFBE patients.
The FDA usually follows the recommendations of its advisory panels, which are not binding.
This article was updated 1/11/18.
HYATTSVILLE, MD – A Food and Drug Administration advisory panel voted against recommending Linhaliq, ciprofloxacin dispersion for inhalation, to treat adult non-cystic fibrosis bronchiectasis (NCFBE) patients who have chronic lung infections with Pseudomonas aeruginosa.
“Two trials that have two very different outcomes – and no matter how we try and explain what the difference was, there was something really missing there,” said advisory committee member Peter Weina, MD, chief of the department of research programs at Walter Reed National Military Medical Center, Bethesda, Md.
NCFBE is often treated with antibacterial drugs, which temporarily reduce inflammation and bacterial load. One of the most common colonizing bacteria in NCFBE infections is P. aeruginosa, which is often associated with increased risk of death and hospital admission.
Prior studies involving inhaled bacterial drugs such as gentamicin and colistin to treat NCFBE have yielded mixed results, and none has been approved for that indication by the FDA.
The FDA granted cipro DI orphan drug status in June 2011 and fast-track approval in August 2014. Cipro DI’s developer, Aradigm, conducted two phase 3 clinical trials to support inhaled ciprofloxacin for the NCFBE indication.
The two phase 3 clinical trials, ORBIT-3 and ORBIT-4, were nearly identical in design. Patients in both were randomized 2:1 to receive cipro DI or placebo once daily for six cycles of 56 days each.
The efficacy results of the ORBIT-3 and ORBIT-4 trials were mixed. In ORBIT-3, there was very little difference between the treatment and placebo arms, with a median difference of 78 days for the primary endpoint of time to first pulmonary exacerbation (PE) (hazard ratio, 0.99; P = .974). ORBIT-3 also showed no difference between treatment and placebo in the frequency of PEs by week 48 of the study (incidence ratio, 0.852).
In contrast, a marginal treatment effect was observed in ORBIT-4, with a median time difference to first PE of 72 days between the placebo and treatment arms (HR, 0.71; P = .032). ORBIT-4 also demonstrated an ability to reduce the number of PEs (incidence ratio, 0.631) by approximately 36.9% by week 48.
Adverse events were the most common reason leading to patient discontinuation in both studies, accounting for 13.1% and 5.3% in the treatment arms of ORBIT-3 and ORBIT-4, respectively.
Despite some of the positive findings in ORBIT-4, FDA presenter LaRee Tracy, PhD, of the FDA’s office of biostatistics, voiced concerns about the trial data – specifically, the failure to reach the primary endpoint in ORBIT-3.
“If I were to be a [statistically speaking] ‘strict’ person, I wouldn’t be looking at the frequency of the [secondary] endpoints, because the primary [endpoint] failed,” Dr. Tracy noted. She also voiced concerns about a re-analysis Aradigm conducted after the trial data were unblinded, stating that the changes made to the original analysis plan “lend a lot of concerns for me.”
Both ORBIT-3 and ORBIT-4 presented uncertainties related to the long-term use of cipro DI. The durability of efficacy and safety findings did not extend beyond a year, leaving some committee members wondering about the development of antibiotic resistance in cipro DI-treated patients. In addition, members were concerned that long-term use of cipro DI could limit the utility of systemic fluoroquinolones to treat severe bacterial and pneumonia infections in NCFBE patients.
The FDA usually follows the recommendations of its advisory panels, which are not binding.
This article was updated 1/11/18.
HYATTSVILLE, MD – A Food and Drug Administration advisory panel voted against recommending Linhaliq, ciprofloxacin dispersion for inhalation, to treat adult non-cystic fibrosis bronchiectasis (NCFBE) patients who have chronic lung infections with Pseudomonas aeruginosa.
“Two trials that have two very different outcomes – and no matter how we try and explain what the difference was, there was something really missing there,” said advisory committee member Peter Weina, MD, chief of the department of research programs at Walter Reed National Military Medical Center, Bethesda, Md.
NCFBE is often treated with antibacterial drugs, which temporarily reduce inflammation and bacterial load. One of the most common colonizing bacteria in NCFBE infections is P. aeruginosa, which is often associated with increased risk of death and hospital admission.
Prior studies involving inhaled bacterial drugs such as gentamicin and colistin to treat NCFBE have yielded mixed results, and none has been approved for that indication by the FDA.
The FDA granted cipro DI orphan drug status in June 2011 and fast-track approval in August 2014. Cipro DI’s developer, Aradigm, conducted two phase 3 clinical trials to support inhaled ciprofloxacin for the NCFBE indication.
The two phase 3 clinical trials, ORBIT-3 and ORBIT-4, were nearly identical in design. Patients in both were randomized 2:1 to receive cipro DI or placebo once daily for six cycles of 56 days each.
The efficacy results of the ORBIT-3 and ORBIT-4 trials were mixed. In ORBIT-3, there was very little difference between the treatment and placebo arms, with a median difference of 78 days for the primary endpoint of time to first pulmonary exacerbation (PE) (hazard ratio, 0.99; P = .974). ORBIT-3 also showed no difference between treatment and placebo in the frequency of PEs by week 48 of the study (incidence ratio, 0.852).
In contrast, a marginal treatment effect was observed in ORBIT-4, with a median time difference to first PE of 72 days between the placebo and treatment arms (HR, 0.71; P = .032). ORBIT-4 also demonstrated an ability to reduce the number of PEs (incidence ratio, 0.631) by approximately 36.9% by week 48.
Adverse events were the most common reason leading to patient discontinuation in both studies, accounting for 13.1% and 5.3% in the treatment arms of ORBIT-3 and ORBIT-4, respectively.
Despite some of the positive findings in ORBIT-4, FDA presenter LaRee Tracy, PhD, of the FDA’s office of biostatistics, voiced concerns about the trial data – specifically, the failure to reach the primary endpoint in ORBIT-3.
“If I were to be a [statistically speaking] ‘strict’ person, I wouldn’t be looking at the frequency of the [secondary] endpoints, because the primary [endpoint] failed,” Dr. Tracy noted. She also voiced concerns about a re-analysis Aradigm conducted after the trial data were unblinded, stating that the changes made to the original analysis plan “lend a lot of concerns for me.”
Both ORBIT-3 and ORBIT-4 presented uncertainties related to the long-term use of cipro DI. The durability of efficacy and safety findings did not extend beyond a year, leaving some committee members wondering about the development of antibiotic resistance in cipro DI-treated patients. In addition, members were concerned that long-term use of cipro DI could limit the utility of systemic fluoroquinolones to treat severe bacterial and pneumonia infections in NCFBE patients.
The FDA usually follows the recommendations of its advisory panels, which are not binding.
This article was updated 1/11/18.
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
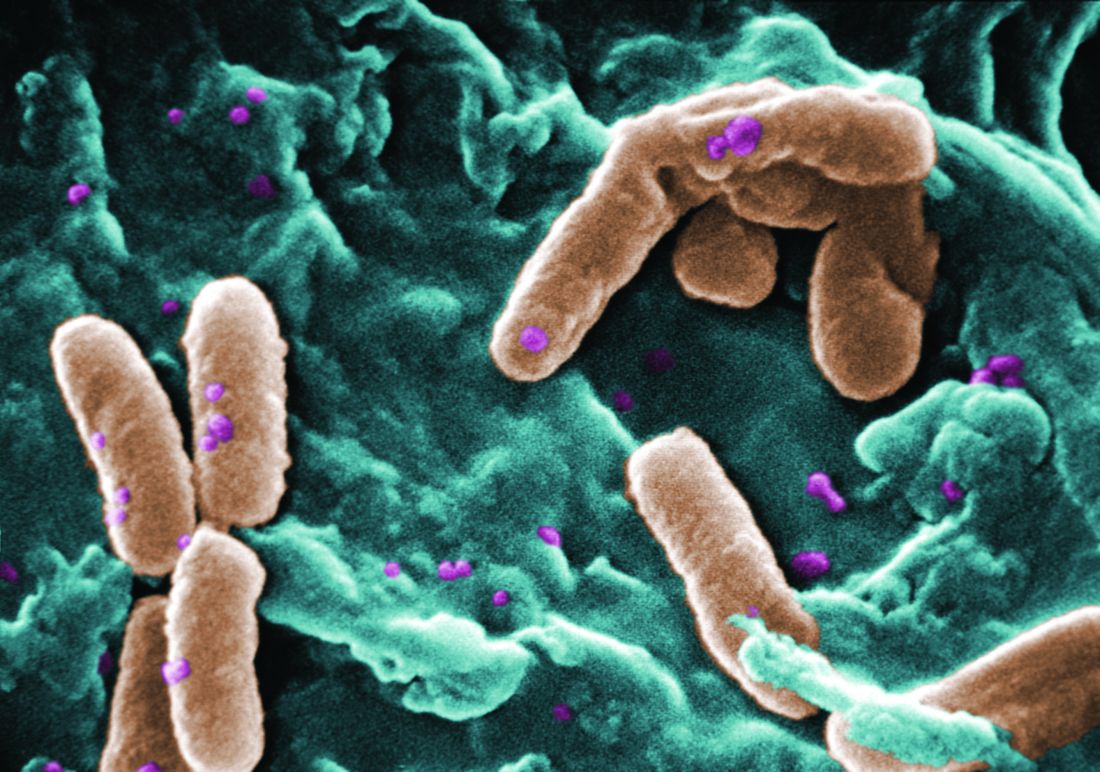
Common food additive makes C. difficile more virulent
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
Fecal microbiota transplantation (FMT) is a promising new treatment for recurring C. diff infections. The AGA FMT National Registry — conducted in collaboration with the Crohn’s and Colitis Foundation, the Infectious Diseases Society of America, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition — will allow physicians and patients to report back on outcomes of the FMT procedure. This data will help answer critical questions about the longer-term health effects of FMT and guide future use. Learn more at www.gastro.org/FMTRegistry.
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
Fecal microbiota transplantation (FMT) is a promising new treatment for recurring C. diff infections. The AGA FMT National Registry — conducted in collaboration with the Crohn’s and Colitis Foundation, the Infectious Diseases Society of America, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition — will allow physicians and patients to report back on outcomes of the FMT procedure. This data will help answer critical questions about the longer-term health effects of FMT and guide future use. Learn more at www.gastro.org/FMTRegistry.
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
Fecal microbiota transplantation (FMT) is a promising new treatment for recurring C. diff infections. The AGA FMT National Registry — conducted in collaboration with the Crohn’s and Colitis Foundation, the Infectious Diseases Society of America, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition — will allow physicians and patients to report back on outcomes of the FMT procedure. This data will help answer critical questions about the longer-term health effects of FMT and guide future use. Learn more at www.gastro.org/FMTRegistry.
FROM NATURE
Key clinical point: Metabolizing trehalose increases the virulence and mortality of C. difficile ribotype 027 (RT027).
Major finding: The ability to metabolize trehalose with the phosphotrehalase enzyme (TreA) increases mortality in RT027.
Study details: Experimental mouse models and an analysis of ileostomy effluent from three anonymous donors.
Disclosures: All authors had no financial disclosures to report.
Source: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
Common food additive makes C. difficile more virulent
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
, a study showed.
“Out of several carbon sources identified that supported CD2015 growth [epidemic RT027 isolate], we found the disaccharide trehalose increased the growth yield of CD2015 by approximately fivefold, compared with a non-RT027 strain,” according to James Collins, PhD, of Baylor University, Houston, and his colleagues. The increased growth of the epidemic strain of C. difficile observed by Dr. Collins and his team demonstrates that trehalose is a robust carbon source for C. difficile bacterium.
In one experiment, mice with humanized microbiota were infected with two strains of RT027, either R20291 (n = 27) or R20291-delta treA (n = 28), a phosphotrehalase enzyme (TreA) deletion mutant that cannot metabolize trehalose. Mice were then given 5 mM of trehalose ad libitum in their drinking water. Researchers observed that the mice infected with R20291-delta treA had much lower mortality rates than the R20291 group (33.3% vs.78.6%). These findings were then reinforced with a second experiment using mice with humanized microbiota, in which trehalose addition increased mortality in RT027 mice, compared with RT027-infected mice that were not given dietary trehalose.
While Dr. Collins and his team demonstrated the effect of trehalose on C. difficile in mice, they also conducted a limited analysis of ileostomy effluent from three human donors. The researchers found that in two of three samples, treA was strongly induced in CD2015, but not in another ribotype, CD2048. This demonstrates that amounts of trehalose found in food are high enough to be metabolized by certain epidemic strains of C. difficile in humans.
Prior to 2000, trehalose use was limited by a relatively high cost of production, approximately $700 per kilogram. A production innovation that utilized a novel enzymatic method that yielded trehalose from starch brought the price of trehalose to approximately $3 per kilogram, making it a commercially viable food supplement. After being considered “generally recognized as safe” by the U.S. Food and Drug Administration in 2000 and approved for use in Europe, the trehalose concentrations in food skyrocketed from around 2% to 11.25%, and trehalose became widely used in several foods, including ice cream, pasta, and ground beef.
Dr. Collins and his associates said that there is considerable evidence that the widespread use of dietary trehalose has contributed to the spread of epidemic C. difficile ribotypes. First, strains RT027 and RT078 have always had the ability to metabolize trehalose, as evidenced by outbreaks of nonepidemic C. difficile in the 1980s. But no epidemic outbreaks were reported until after 2003, several years after trehalose was approved by the FDA. Second, RT027 and RT078 are phylogenetically distant, but independently evolved the ability to metabolize low levels of trehalose. Third, increased severity of the RT027 strain, which metabolizes trehalose in mice, is consistent with increased virulence of RT078 and RT027 in human patients. Fourth, a competitive advantage is conferred to C. difficile being able to metabolize trehalose in low concentrations in a diverse intestinal setting. Finally, the levels of trehalose in ileostomy fluid from patients who eat a normal diet are high enough to be utilized by RT027 strains.
“On the basis of these observations, we propose that the widespread adoption and use of the disaccharide trehalose in the human diet has played a significant role in the emergence of these epidemic and hypervirulent strains,” Dr. Collins and his colleagues wrote in their article in Nature.
The authors of the study had no relevant financial disclosures to report.
SOURCE: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
FROM NATURE
Key clinical point: Metabolizing trehalose increases the virulence and mortality of C. difficile ribotype 027 (RT027).
Major finding: The ability to metabolize trehalose with the phosphotrehalase enzyme (TreA) increases mortality in RT027.
Study details: Experimental mouse models and an analysis of ileostomy effluent from three anonymous donors.
Disclosures: All authors had no financial disclosures to report.
Source: Collins J et al. Nature. 2018 Jan 3. doi: 10.1038/nature25178.
Biologic mesh safe, effective for prevention of parastomal hernia recurrence
at 18.9%.
Theadore Hufford, MD, of the University of Illinois at Chicago and his colleagues conducted a study to look at the effects of placement and type of mesh on postop morbidity and recurrence of parastomal hernia (PSH). The study was a retrospective analysis of 58 patients who had undergone local PSH repair with biological mesh between July 2006 and July 2015 at a single medical center.
All procedures were conducted by three board-certified surgeons at a tertiary medical center, and decisions such as the mesh type, placement and incision type were determined by the attending surgeon’s operative preferences.
In the study group, mesh placement (overlay, underlay, or sandwich technique) was found to have a statistically significant effect on recurrence. Of the patients who received an underlay of biologic mesh, 33% had a recurrence, compared with 25% of those who had overlays. The sandwich technique (a combination of overlay and underlay) was found to have the lowest rate of recurrence at 6.7%. The type of mesh (human origin, bovine, or porcine) and type of stoma (colostomy vs. ileostomy) had no statistically significant effect on the rate of recurrence.
Total recurrences in the study patients was 18.9%, a figure consistent with the current literature on parastomal hernia repair, the investigators wrote.
A key factor in recurrence was type of incision. Keyhole incisions had a much lower rate of recurrence than did circular incisions (32% vs. 9.1%; P = .042).
In the study group, “one patient was readmitted for mesh infection within 30 days of the repair and required mesh removal. Even with the biologic mesh in place there was an overlying skin infection that warranted reoperation that resulted in the stoma being moved to a new site altogether,” the investigators wrote.
The limitations of this study include the retrospective nature of the research and the difficulty in diagnosing PSH, which is often asymptomatic, the investigators mentioned. In addition, the techniques for local PSH repair with biologic mesh are not fully standardized. Mesh type and location decisions are often made on a case-by-case basis which limits the applicability of the study data for general PSH repairs.
Dr. Hufford and his associates wrote, “Our results suggest local parastomal hernia repair with biological mesh is both a safe and effective method, especially when used with the sandwich technique for mesh placement, for definitive treatment of parastomal hernias with very low morbidity, and acceptable recurrence rate.”
The investigators reported no disclosures.
at 18.9%.
Theadore Hufford, MD, of the University of Illinois at Chicago and his colleagues conducted a study to look at the effects of placement and type of mesh on postop morbidity and recurrence of parastomal hernia (PSH). The study was a retrospective analysis of 58 patients who had undergone local PSH repair with biological mesh between July 2006 and July 2015 at a single medical center.
All procedures were conducted by three board-certified surgeons at a tertiary medical center, and decisions such as the mesh type, placement and incision type were determined by the attending surgeon’s operative preferences.
In the study group, mesh placement (overlay, underlay, or sandwich technique) was found to have a statistically significant effect on recurrence. Of the patients who received an underlay of biologic mesh, 33% had a recurrence, compared with 25% of those who had overlays. The sandwich technique (a combination of overlay and underlay) was found to have the lowest rate of recurrence at 6.7%. The type of mesh (human origin, bovine, or porcine) and type of stoma (colostomy vs. ileostomy) had no statistically significant effect on the rate of recurrence.
Total recurrences in the study patients was 18.9%, a figure consistent with the current literature on parastomal hernia repair, the investigators wrote.
A key factor in recurrence was type of incision. Keyhole incisions had a much lower rate of recurrence than did circular incisions (32% vs. 9.1%; P = .042).
In the study group, “one patient was readmitted for mesh infection within 30 days of the repair and required mesh removal. Even with the biologic mesh in place there was an overlying skin infection that warranted reoperation that resulted in the stoma being moved to a new site altogether,” the investigators wrote.
The limitations of this study include the retrospective nature of the research and the difficulty in diagnosing PSH, which is often asymptomatic, the investigators mentioned. In addition, the techniques for local PSH repair with biologic mesh are not fully standardized. Mesh type and location decisions are often made on a case-by-case basis which limits the applicability of the study data for general PSH repairs.
Dr. Hufford and his associates wrote, “Our results suggest local parastomal hernia repair with biological mesh is both a safe and effective method, especially when used with the sandwich technique for mesh placement, for definitive treatment of parastomal hernias with very low morbidity, and acceptable recurrence rate.”
The investigators reported no disclosures.
at 18.9%.
Theadore Hufford, MD, of the University of Illinois at Chicago and his colleagues conducted a study to look at the effects of placement and type of mesh on postop morbidity and recurrence of parastomal hernia (PSH). The study was a retrospective analysis of 58 patients who had undergone local PSH repair with biological mesh between July 2006 and July 2015 at a single medical center.
All procedures were conducted by three board-certified surgeons at a tertiary medical center, and decisions such as the mesh type, placement and incision type were determined by the attending surgeon’s operative preferences.
In the study group, mesh placement (overlay, underlay, or sandwich technique) was found to have a statistically significant effect on recurrence. Of the patients who received an underlay of biologic mesh, 33% had a recurrence, compared with 25% of those who had overlays. The sandwich technique (a combination of overlay and underlay) was found to have the lowest rate of recurrence at 6.7%. The type of mesh (human origin, bovine, or porcine) and type of stoma (colostomy vs. ileostomy) had no statistically significant effect on the rate of recurrence.
Total recurrences in the study patients was 18.9%, a figure consistent with the current literature on parastomal hernia repair, the investigators wrote.
A key factor in recurrence was type of incision. Keyhole incisions had a much lower rate of recurrence than did circular incisions (32% vs. 9.1%; P = .042).
In the study group, “one patient was readmitted for mesh infection within 30 days of the repair and required mesh removal. Even with the biologic mesh in place there was an overlying skin infection that warranted reoperation that resulted in the stoma being moved to a new site altogether,” the investigators wrote.
The limitations of this study include the retrospective nature of the research and the difficulty in diagnosing PSH, which is often asymptomatic, the investigators mentioned. In addition, the techniques for local PSH repair with biologic mesh are not fully standardized. Mesh type and location decisions are often made on a case-by-case basis which limits the applicability of the study data for general PSH repairs.
Dr. Hufford and his associates wrote, “Our results suggest local parastomal hernia repair with biological mesh is both a safe and effective method, especially when used with the sandwich technique for mesh placement, for definitive treatment of parastomal hernias with very low morbidity, and acceptable recurrence rate.”
The investigators reported no disclosures.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: In a comparison of the biologic meshes and placement techniques, the sandwich technique was most successful in preventing recurrence.
Major finding: Rate of recurrence of parastomal hernia was 33% with underlay surgical mesh placement, 25% with overlay placement, and 6.7% with sandwich placement.
Study details: A retrospective analysis of 58 patients who had undergone local parastomal hernia repair with biological mesh at a single medical center.
Disclosures: The investigators reported no disclosures.
Source: Hufford T et al. Am J Surg. 2018 Jan. 215(1):88-90.
Systemic corticosteroids not recommended for long-term treatment of eczema
Systemic corticosteroids (SCSs) should be limited to short courses as a transition to steroid-sparing therapies in patients with atopic dermatitis because of the potential for adverse effects, reported Sherry Yu, MD, of Massachusetts General Hospital, Boston, and her associates.
Another AE is adrenal insufficiency, defined as a cortisol level less than or equal to 500 nmol/L. In a meta-analysis of 74 articles with 3,753 participants, there was a significant increase in absolute risk of adrenal insufficiency with medium term use (1 month to less than 1 year) and long term use (more than 1 year) of SCSs, as well as medium and high doses of SCSs. Adrenal insufficiency can occur in as little as 4 weeks and may be subclinical. This can leave patients vulnerable to infection and stress from surgery. Adrenal insufficiency also can manifest itself as weakness, fatigue, and shock in more severe cases.
Dr. Yu and her colleagues noted that tapering may minimize the risk of adrenal insufficiency and that a single morning dose or alternate dosing strategy may minimize this risk.
Another finding from this study was the adverse effects the SCSs have on pediatric patients. One study showed that 7 of 10 (70%) of children taking maintenance doses of beclomethasone dipropionate had growth impairment after 6 months of therapy. Significant growth disruption also was observed in children who had taken beclomethasone dipropionate only 4 weeks.
Dr. Yu and her colleagues warned that SCS should not be used to treat pediatric AD “because of growth retardation and other AEs.”
In conclusion, Dr. Yu and her colleagues said, “the literature supports short-term use of short courses of oral corticosteroids (less than 3 weeks) to interrupt acute flares, but rebound flaring is commonly observed after discontinuation. If SCSs are used at all, their use should be short term when bridging to other systemic therapies or phototherapy.” Despite the support for short-term courses of SCSs, the “duration of an optimal short course is not well defined” in the literature.
Dr. Yu reported no relevant financial disclosures. The other three authors reported relationships with various companies in the industry.
SOURCE: Yu S et al. J Am Acad Dermatol. 2017 Oct 13. doi: 10.1016/j.jaad.2017.09.074.
Systemic corticosteroids (SCSs) should be limited to short courses as a transition to steroid-sparing therapies in patients with atopic dermatitis because of the potential for adverse effects, reported Sherry Yu, MD, of Massachusetts General Hospital, Boston, and her associates.
Another AE is adrenal insufficiency, defined as a cortisol level less than or equal to 500 nmol/L. In a meta-analysis of 74 articles with 3,753 participants, there was a significant increase in absolute risk of adrenal insufficiency with medium term use (1 month to less than 1 year) and long term use (more than 1 year) of SCSs, as well as medium and high doses of SCSs. Adrenal insufficiency can occur in as little as 4 weeks and may be subclinical. This can leave patients vulnerable to infection and stress from surgery. Adrenal insufficiency also can manifest itself as weakness, fatigue, and shock in more severe cases.
Dr. Yu and her colleagues noted that tapering may minimize the risk of adrenal insufficiency and that a single morning dose or alternate dosing strategy may minimize this risk.
Another finding from this study was the adverse effects the SCSs have on pediatric patients. One study showed that 7 of 10 (70%) of children taking maintenance doses of beclomethasone dipropionate had growth impairment after 6 months of therapy. Significant growth disruption also was observed in children who had taken beclomethasone dipropionate only 4 weeks.
Dr. Yu and her colleagues warned that SCS should not be used to treat pediatric AD “because of growth retardation and other AEs.”
In conclusion, Dr. Yu and her colleagues said, “the literature supports short-term use of short courses of oral corticosteroids (less than 3 weeks) to interrupt acute flares, but rebound flaring is commonly observed after discontinuation. If SCSs are used at all, their use should be short term when bridging to other systemic therapies or phototherapy.” Despite the support for short-term courses of SCSs, the “duration of an optimal short course is not well defined” in the literature.
Dr. Yu reported no relevant financial disclosures. The other three authors reported relationships with various companies in the industry.
SOURCE: Yu S et al. J Am Acad Dermatol. 2017 Oct 13. doi: 10.1016/j.jaad.2017.09.074.
Systemic corticosteroids (SCSs) should be limited to short courses as a transition to steroid-sparing therapies in patients with atopic dermatitis because of the potential for adverse effects, reported Sherry Yu, MD, of Massachusetts General Hospital, Boston, and her associates.
Another AE is adrenal insufficiency, defined as a cortisol level less than or equal to 500 nmol/L. In a meta-analysis of 74 articles with 3,753 participants, there was a significant increase in absolute risk of adrenal insufficiency with medium term use (1 month to less than 1 year) and long term use (more than 1 year) of SCSs, as well as medium and high doses of SCSs. Adrenal insufficiency can occur in as little as 4 weeks and may be subclinical. This can leave patients vulnerable to infection and stress from surgery. Adrenal insufficiency also can manifest itself as weakness, fatigue, and shock in more severe cases.
Dr. Yu and her colleagues noted that tapering may minimize the risk of adrenal insufficiency and that a single morning dose or alternate dosing strategy may minimize this risk.
Another finding from this study was the adverse effects the SCSs have on pediatric patients. One study showed that 7 of 10 (70%) of children taking maintenance doses of beclomethasone dipropionate had growth impairment after 6 months of therapy. Significant growth disruption also was observed in children who had taken beclomethasone dipropionate only 4 weeks.
Dr. Yu and her colleagues warned that SCS should not be used to treat pediatric AD “because of growth retardation and other AEs.”
In conclusion, Dr. Yu and her colleagues said, “the literature supports short-term use of short courses of oral corticosteroids (less than 3 weeks) to interrupt acute flares, but rebound flaring is commonly observed after discontinuation. If SCSs are used at all, their use should be short term when bridging to other systemic therapies or phototherapy.” Despite the support for short-term courses of SCSs, the “duration of an optimal short course is not well defined” in the literature.
Dr. Yu reported no relevant financial disclosures. The other three authors reported relationships with various companies in the industry.
SOURCE: Yu S et al. J Am Acad Dermatol. 2017 Oct 13. doi: 10.1016/j.jaad.2017.09.074.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point:
Major finding: Growth impairment was seen after 6 months in 7 out of 10 children with eczema taking maintenance doses of oral beclomethasone dipropionate.
Study details: A systematic review of 52 reviews and 12 studies concerning systemic corticosteroid use in atopic dermatitis patients from journal databases including PubMed and Medline
Disclosures: Dr. Yu reported no relevant financial disclosures. The other three authors reported relationships with various companies in the industry.
Source: Yu S et al. J Am Acad Dermatol. 2017 Oct 13. doi: 10.1016/j.jaad.2017.09.074.