User login
Metabolic/bariatric surgery reduces CVD risk in teens
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipedemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that, with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
AGA Resource
GIs are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide provides a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management.
SOURCE: Michalsky M et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipedemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that, with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
AGA Resource
GIs are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide provides a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management.
SOURCE: Michalsky M et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipedemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that, with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, elevated blood pressure, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
AGA Resource
GIs are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide provides a comprehensive, multidisciplinary process to personalize innovative obesity care for safe and effective weight management.
SOURCE: Michalsky M et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Metabolic and bariatric surgery reduces CVD risk in severely obese adolescents
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
FROM PEDIATRICS
Key clinical point:
Major finding: With every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, elevated BP, hyperinsulinemia, diabetes and elevated high-sensitivity C-reactive protein, respectively.
Study details: This study was a longitudinal, multicenter prospective study of 242 severely obese adolescents undergoing metabolic and bariatric surgery between February 28, 2007 and December 30, 2011.
Disclosures: Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various healthcare groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
Source: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485
Acne evaluations using photos with digital tool comparable to in-person exams
Dermatologist evaluation of photographs of acne taken by patients using a telemedicine and mobile data collection tool produced similar Investigator’s Global Assessment (IGA) findings and lesion counts, compared with traditional in-person examinations, in a pilot study sponsored by the tool’s manufacturer.
, the Network Oriented Research Assistant (NORA), Hannah Singer, a medical student at Columbia University, New York, and her coinvestigators concluded. The study was published online Dec. 20 in JAMA Dermatology.
To determine the effectiveness of the tool, investigators compared in-person evaluations of acne patients with digital evaluations in 60 patients in one dermatology practice. The “intraclass correlation coefficient (ICC)” was used to compare the in-person exam and the digital photo assessments of the IGA score and acne lesion counts; ICC scores ranged from 0 to 1, with 0 indicating no agreement and 1 indicating perfect agreement.
Study participants, who were aged 12-54 years (mean age 23 years) were trained to use NORA on an iPhone 6 and were instructed to take five photographs of different facial regions: the forehead, chin, right cheek, left cheek, and the whole face. The evaluation of patient-photographed acne and the in-person evaluation were separated by 1 week.
The ICC for IGA scores was 0.75, and the ICC for total lesion count was 0.81. Inflammatory lesion count and noninflammatory lesion count both had an ICC score of 0.72, while cyst count had the highest ICC score of 0.82. The ICC results demonstrated “strong agreement” between assessment scores from in-person examinations and the patient-taken digital photos, the authors wrote.
The study had several limitations, including the small patient sample size and limited geographic area, and although there was a 1- to 2-week gap between the digital and in-person evaluations, there may have been recall bias because the same physicians conducted both evaluations, they added.
Future studies should collect data from multiple centers, with a longer follow-up, and cost analysis and patient-reported measures, the researchers wrote.
The NORA technology platform is currently being evaluated in studies of patients with diagnoses including atopic dermatitis, pemphigus vulgaris, and liver disease. “Use of the NORA platform in telemedicine-based clinical trials will allow for increased access, a broader diversity of patients, and improved adherence among participants in trials for acne vulgaris and other therapeutic areas,” the researchers noted.
The study was sponsored by Science 37, a mobile technology and clinical trial company that developed NORA, the software used in this study. Other than Ms. Singer, who had no disclosures, the remaining 10 authors are Science 37 employees and have stock options in the company.
SOURCE: M. Singer, JAMA Dermatol 2017 Dec 20; doi:10.1001/jamadermatol.2017.5141.
Dermatologist evaluation of photographs of acne taken by patients using a telemedicine and mobile data collection tool produced similar Investigator’s Global Assessment (IGA) findings and lesion counts, compared with traditional in-person examinations, in a pilot study sponsored by the tool’s manufacturer.
, the Network Oriented Research Assistant (NORA), Hannah Singer, a medical student at Columbia University, New York, and her coinvestigators concluded. The study was published online Dec. 20 in JAMA Dermatology.
To determine the effectiveness of the tool, investigators compared in-person evaluations of acne patients with digital evaluations in 60 patients in one dermatology practice. The “intraclass correlation coefficient (ICC)” was used to compare the in-person exam and the digital photo assessments of the IGA score and acne lesion counts; ICC scores ranged from 0 to 1, with 0 indicating no agreement and 1 indicating perfect agreement.
Study participants, who were aged 12-54 years (mean age 23 years) were trained to use NORA on an iPhone 6 and were instructed to take five photographs of different facial regions: the forehead, chin, right cheek, left cheek, and the whole face. The evaluation of patient-photographed acne and the in-person evaluation were separated by 1 week.
The ICC for IGA scores was 0.75, and the ICC for total lesion count was 0.81. Inflammatory lesion count and noninflammatory lesion count both had an ICC score of 0.72, while cyst count had the highest ICC score of 0.82. The ICC results demonstrated “strong agreement” between assessment scores from in-person examinations and the patient-taken digital photos, the authors wrote.
The study had several limitations, including the small patient sample size and limited geographic area, and although there was a 1- to 2-week gap between the digital and in-person evaluations, there may have been recall bias because the same physicians conducted both evaluations, they added.
Future studies should collect data from multiple centers, with a longer follow-up, and cost analysis and patient-reported measures, the researchers wrote.
The NORA technology platform is currently being evaluated in studies of patients with diagnoses including atopic dermatitis, pemphigus vulgaris, and liver disease. “Use of the NORA platform in telemedicine-based clinical trials will allow for increased access, a broader diversity of patients, and improved adherence among participants in trials for acne vulgaris and other therapeutic areas,” the researchers noted.
The study was sponsored by Science 37, a mobile technology and clinical trial company that developed NORA, the software used in this study. Other than Ms. Singer, who had no disclosures, the remaining 10 authors are Science 37 employees and have stock options in the company.
SOURCE: M. Singer, JAMA Dermatol 2017 Dec 20; doi:10.1001/jamadermatol.2017.5141.
Dermatologist evaluation of photographs of acne taken by patients using a telemedicine and mobile data collection tool produced similar Investigator’s Global Assessment (IGA) findings and lesion counts, compared with traditional in-person examinations, in a pilot study sponsored by the tool’s manufacturer.
, the Network Oriented Research Assistant (NORA), Hannah Singer, a medical student at Columbia University, New York, and her coinvestigators concluded. The study was published online Dec. 20 in JAMA Dermatology.
To determine the effectiveness of the tool, investigators compared in-person evaluations of acne patients with digital evaluations in 60 patients in one dermatology practice. The “intraclass correlation coefficient (ICC)” was used to compare the in-person exam and the digital photo assessments of the IGA score and acne lesion counts; ICC scores ranged from 0 to 1, with 0 indicating no agreement and 1 indicating perfect agreement.
Study participants, who were aged 12-54 years (mean age 23 years) were trained to use NORA on an iPhone 6 and were instructed to take five photographs of different facial regions: the forehead, chin, right cheek, left cheek, and the whole face. The evaluation of patient-photographed acne and the in-person evaluation were separated by 1 week.
The ICC for IGA scores was 0.75, and the ICC for total lesion count was 0.81. Inflammatory lesion count and noninflammatory lesion count both had an ICC score of 0.72, while cyst count had the highest ICC score of 0.82. The ICC results demonstrated “strong agreement” between assessment scores from in-person examinations and the patient-taken digital photos, the authors wrote.
The study had several limitations, including the small patient sample size and limited geographic area, and although there was a 1- to 2-week gap between the digital and in-person evaluations, there may have been recall bias because the same physicians conducted both evaluations, they added.
Future studies should collect data from multiple centers, with a longer follow-up, and cost analysis and patient-reported measures, the researchers wrote.
The NORA technology platform is currently being evaluated in studies of patients with diagnoses including atopic dermatitis, pemphigus vulgaris, and liver disease. “Use of the NORA platform in telemedicine-based clinical trials will allow for increased access, a broader diversity of patients, and improved adherence among participants in trials for acne vulgaris and other therapeutic areas,” the researchers noted.
The study was sponsored by Science 37, a mobile technology and clinical trial company that developed NORA, the software used in this study. Other than Ms. Singer, who had no disclosures, the remaining 10 authors are Science 37 employees and have stock options in the company.
SOURCE: M. Singer, JAMA Dermatol 2017 Dec 20; doi:10.1001/jamadermatol.2017.5141.
FROM JAMA DERMATOLOGY
Key clinical point: In-person evaluations and digital evaluations of self-photographed acne produced comparable results.
Major finding: There was “strong agreement” in the Investigator’s Global Assessment scores and acne lesion counts between assessments of digital photos and in-person exams.
Study details: A pilot study of 60 acne patients at a dermatology office compared assessments with digital photos and in-person exams.
Disclosures: The study was sponsored by Science 37, a mobile technology and clinical trial company that developed NORA, the software used in this study. Other than the lead author, who had no disclosures, the 10 remaining authors are Science 37 employees and have stock options in the company.
Source: M Singer, JAMA Dermatol. 2017 Dec 20; doi: 10.1001/jamadermatol.2017.5141.
Laparoscopic nerve-sparing approach is effective in deep infiltrating endometriosis
NATIONAL HARBOR, MD. – Laparoscopic retroperitoneal nerve-sparing surgery is a safe approach that relieves pain in women with deep infiltrating endometriosis, according to findings presented by Giovanni Roviglione, MD, at the AAGL Global Congress.
The prospective case series study with a single gynecologic surgeon in Verona, Italy, involved 382 women who had deep infiltrating endometriosis with sciatica and anogenital pain. All of the women had some level of nervous compression of somatic structures and infiltration of their fascial envelope.
The surgery involved whole decompression and partial neurolysis of nervous structures for most patients, while nearly 20% of women required complete neurolysis based on their level of infiltration. Most women (64%) had severe enough infiltration that a concomitant bowel resection was also necessary.
The surgeon performed a medial approach for deep pelvic endometriosis with rectal and/or parametrial involvement extending to the pelvic wall and somatic nerve, or a lateral approach for isolated endometriosis of the pelvic wall and somatic nerves.
At 6 months after surgery, all patients reported complete relief from pain. However, 77 women (20%) experienced postoperative neuritis, which was successfully treated with corticosteroids, antiepileptics, and opioids.
Endometriosis that extends into somatic nerves and the sacral roots is a common cause of pelvic pain, Dr. Roviglione said.
“This kind of endometriosis is resistant to opioids and drugs,” he said. The difficulty in treating deep infiltrating endometriosis is compounded by the often long delay in diagnosis, he added.
Using laparoscopy for neurolysis and decompression of somatic nerves affected by endometriosis is a “more accurate and effective treatment” for providing pain relief, Dr. Roviglione said. But laparoscopic retroperitoneal nerve-sparing surgery should be performed only by skilled neuroanatomy surgeons at referral centers because of the complex nature of the procedure, he noted.
Dr. Roviglione reported having no relevant financial disclosures.
SOURCE: Ceccaroni M et al. AAGL 2017 Abstract 166.
NATIONAL HARBOR, MD. – Laparoscopic retroperitoneal nerve-sparing surgery is a safe approach that relieves pain in women with deep infiltrating endometriosis, according to findings presented by Giovanni Roviglione, MD, at the AAGL Global Congress.
The prospective case series study with a single gynecologic surgeon in Verona, Italy, involved 382 women who had deep infiltrating endometriosis with sciatica and anogenital pain. All of the women had some level of nervous compression of somatic structures and infiltration of their fascial envelope.
The surgery involved whole decompression and partial neurolysis of nervous structures for most patients, while nearly 20% of women required complete neurolysis based on their level of infiltration. Most women (64%) had severe enough infiltration that a concomitant bowel resection was also necessary.
The surgeon performed a medial approach for deep pelvic endometriosis with rectal and/or parametrial involvement extending to the pelvic wall and somatic nerve, or a lateral approach for isolated endometriosis of the pelvic wall and somatic nerves.
At 6 months after surgery, all patients reported complete relief from pain. However, 77 women (20%) experienced postoperative neuritis, which was successfully treated with corticosteroids, antiepileptics, and opioids.
Endometriosis that extends into somatic nerves and the sacral roots is a common cause of pelvic pain, Dr. Roviglione said.
“This kind of endometriosis is resistant to opioids and drugs,” he said. The difficulty in treating deep infiltrating endometriosis is compounded by the often long delay in diagnosis, he added.
Using laparoscopy for neurolysis and decompression of somatic nerves affected by endometriosis is a “more accurate and effective treatment” for providing pain relief, Dr. Roviglione said. But laparoscopic retroperitoneal nerve-sparing surgery should be performed only by skilled neuroanatomy surgeons at referral centers because of the complex nature of the procedure, he noted.
Dr. Roviglione reported having no relevant financial disclosures.
SOURCE: Ceccaroni M et al. AAGL 2017 Abstract 166.
NATIONAL HARBOR, MD. – Laparoscopic retroperitoneal nerve-sparing surgery is a safe approach that relieves pain in women with deep infiltrating endometriosis, according to findings presented by Giovanni Roviglione, MD, at the AAGL Global Congress.
The prospective case series study with a single gynecologic surgeon in Verona, Italy, involved 382 women who had deep infiltrating endometriosis with sciatica and anogenital pain. All of the women had some level of nervous compression of somatic structures and infiltration of their fascial envelope.
The surgery involved whole decompression and partial neurolysis of nervous structures for most patients, while nearly 20% of women required complete neurolysis based on their level of infiltration. Most women (64%) had severe enough infiltration that a concomitant bowel resection was also necessary.
The surgeon performed a medial approach for deep pelvic endometriosis with rectal and/or parametrial involvement extending to the pelvic wall and somatic nerve, or a lateral approach for isolated endometriosis of the pelvic wall and somatic nerves.
At 6 months after surgery, all patients reported complete relief from pain. However, 77 women (20%) experienced postoperative neuritis, which was successfully treated with corticosteroids, antiepileptics, and opioids.
Endometriosis that extends into somatic nerves and the sacral roots is a common cause of pelvic pain, Dr. Roviglione said.
“This kind of endometriosis is resistant to opioids and drugs,” he said. The difficulty in treating deep infiltrating endometriosis is compounded by the often long delay in diagnosis, he added.
Using laparoscopy for neurolysis and decompression of somatic nerves affected by endometriosis is a “more accurate and effective treatment” for providing pain relief, Dr. Roviglione said. But laparoscopic retroperitoneal nerve-sparing surgery should be performed only by skilled neuroanatomy surgeons at referral centers because of the complex nature of the procedure, he noted.
Dr. Roviglione reported having no relevant financial disclosures.
SOURCE: Ceccaroni M et al. AAGL 2017 Abstract 166.
REPORTING FROM AAGL 2017
Key clinical point:
Major finding: All patients reported complete relief of neurologic symptoms at 6 months after surgery.
Study details: Single center, prospective case series of 382 women who underwent laparoscopic retroperitoneal nerve-sparing surgery to treat pain associated with deep infiltrating endometriosis.
Disclosures: Dr. Roviglione reported having no relevant financial disclosures.
Source: Ceccaroni M et al. AAGL 2017 Abstract 166.
FDA approves angiotensin II for shock patients
Angiotensin II has been approved for use in intravenous infusions to increase blood pressure in adults with septic or other distributive shock, the Food and Drug Administration announced.
Shock-related drops in blood pressure can restrict blood flow to vital organs and can result in organ failure and death. “There is a need for treatment options for critically ill hypotensive patients who do not adequately respond to available therapies,” Norman Stockbridge, MD, PhD, director of the division of cardiovascular and renal products in the FDA’s Center for Drug Evaluation and Research, said in a written statement.
The effectiveness of angiotensin II for treating critically low blood pressure was confirmed in a clinical trial of 321 patients who were in shock. A significant number of patients responded to angiotensin II treatment, compared with those given placebo. In combination with conventional treatments, angiotensin II increased blood pressure safely and effectively, according to the FDA statement.
Angiotensin II can cause serious blood clots, and prophylactic treatment for such issues is recommended.
The application for angiontensin II was received under Priority Review. The goal of Priority Review is for the FDA to take action on the application within 6 months if the agency determines that an approved drug would improve the safety and effectiveness of treating a serious medical condition.
Angiotensin II injections will be marketed as Giapreza by La Jolla Pharmaceutical Company.
Angiotensin II has been approved for use in intravenous infusions to increase blood pressure in adults with septic or other distributive shock, the Food and Drug Administration announced.
Shock-related drops in blood pressure can restrict blood flow to vital organs and can result in organ failure and death. “There is a need for treatment options for critically ill hypotensive patients who do not adequately respond to available therapies,” Norman Stockbridge, MD, PhD, director of the division of cardiovascular and renal products in the FDA’s Center for Drug Evaluation and Research, said in a written statement.
The effectiveness of angiotensin II for treating critically low blood pressure was confirmed in a clinical trial of 321 patients who were in shock. A significant number of patients responded to angiotensin II treatment, compared with those given placebo. In combination with conventional treatments, angiotensin II increased blood pressure safely and effectively, according to the FDA statement.
Angiotensin II can cause serious blood clots, and prophylactic treatment for such issues is recommended.
The application for angiontensin II was received under Priority Review. The goal of Priority Review is for the FDA to take action on the application within 6 months if the agency determines that an approved drug would improve the safety and effectiveness of treating a serious medical condition.
Angiotensin II injections will be marketed as Giapreza by La Jolla Pharmaceutical Company.
Angiotensin II has been approved for use in intravenous infusions to increase blood pressure in adults with septic or other distributive shock, the Food and Drug Administration announced.
Shock-related drops in blood pressure can restrict blood flow to vital organs and can result in organ failure and death. “There is a need for treatment options for critically ill hypotensive patients who do not adequately respond to available therapies,” Norman Stockbridge, MD, PhD, director of the division of cardiovascular and renal products in the FDA’s Center for Drug Evaluation and Research, said in a written statement.
The effectiveness of angiotensin II for treating critically low blood pressure was confirmed in a clinical trial of 321 patients who were in shock. A significant number of patients responded to angiotensin II treatment, compared with those given placebo. In combination with conventional treatments, angiotensin II increased blood pressure safely and effectively, according to the FDA statement.
Angiotensin II can cause serious blood clots, and prophylactic treatment for such issues is recommended.
The application for angiontensin II was received under Priority Review. The goal of Priority Review is for the FDA to take action on the application within 6 months if the agency determines that an approved drug would improve the safety and effectiveness of treating a serious medical condition.
Angiotensin II injections will be marketed as Giapreza by La Jolla Pharmaceutical Company.
FDA updates nilotinib product label outlining criteria for discontinuation
for patients who meet certain criteria. Nilotinib, a kinase inhibitor that blocks the BCR-ABL protein that promotes abnormal cell growth, was originally approved in 2007 and was indicated for use in patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML). In accordance with the new label update, patients who have early phase CML, have been using nilotinib for 3 years or more, and whose leukemia has responded to treatment according to a test that has received FDA marketing authorization, may be eligible to discontinue use of nilotinib.
The information that led to the FDA approved label update was based on two single-arm trials of patients with chronic phase Ph+ CML. The trial measured the length of time patients were able to discontinue use of nilotinib without leukemia returning, and who had entered treatment-free remission (TFR). In the first trial, among 190 newly diagnosed CML patients who discontinued taking nilotinib after using the drug for 3 or more years, 51.6% were still in TFR after about 1 year (48 weeks) and 48.9% were still in TFR after nearly 2 years (96 weeks). Similar results were seen in the second trial, among 126 patients, with 57.9% in TFR after about a year (48 weeks) and 53.2% in TFR after approximately 2 years (96 weeks).
An important element of these trials was regular monitoring of specific RNA information that specifies the level of BCR-ABL protein in the blood using a diagnostic test that has received FDA marketing authorization. Monitoring with a test that accurately detects the reductions of RNA information in the blood with accuracy and precision is critical in discontinuing the use of nilotinib. This monitoring will allow physicians to detect the first signs of relapse.
“Patients diagnosed with CML generally face a lifetime of treatment to keep their leukemia from growing or recurring,” said Richard Pazdur, MD, acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval shows that some patients may be able to stop treatment with Tasigna altogether if they are showing a strong response to therapy. While we welcome this progress in patient care, it’s important to note that any discontinuation of treatment still means patients must be regularly monitored for disease recurrence,” Dr. Pazdur said in the FDA statement.
Common side effects after discontinuing use of nilotinib include body aches and pain in the bones and extremities. Severe side effects of taking nilotinib can include myelosuppression, blockages in the heart and arteries, and inflammation of the pancreas. Severe liver damage can also occur.
Severe side effects typically associated with nilotinib administration occurred less frequently in patients who discontinued the drug. However, the long-term outcomes of patients discontinuing versus continuing treatment are unknown at this time, the FDA noted.
for patients who meet certain criteria. Nilotinib, a kinase inhibitor that blocks the BCR-ABL protein that promotes abnormal cell growth, was originally approved in 2007 and was indicated for use in patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML). In accordance with the new label update, patients who have early phase CML, have been using nilotinib for 3 years or more, and whose leukemia has responded to treatment according to a test that has received FDA marketing authorization, may be eligible to discontinue use of nilotinib.
The information that led to the FDA approved label update was based on two single-arm trials of patients with chronic phase Ph+ CML. The trial measured the length of time patients were able to discontinue use of nilotinib without leukemia returning, and who had entered treatment-free remission (TFR). In the first trial, among 190 newly diagnosed CML patients who discontinued taking nilotinib after using the drug for 3 or more years, 51.6% were still in TFR after about 1 year (48 weeks) and 48.9% were still in TFR after nearly 2 years (96 weeks). Similar results were seen in the second trial, among 126 patients, with 57.9% in TFR after about a year (48 weeks) and 53.2% in TFR after approximately 2 years (96 weeks).
An important element of these trials was regular monitoring of specific RNA information that specifies the level of BCR-ABL protein in the blood using a diagnostic test that has received FDA marketing authorization. Monitoring with a test that accurately detects the reductions of RNA information in the blood with accuracy and precision is critical in discontinuing the use of nilotinib. This monitoring will allow physicians to detect the first signs of relapse.
“Patients diagnosed with CML generally face a lifetime of treatment to keep their leukemia from growing or recurring,” said Richard Pazdur, MD, acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval shows that some patients may be able to stop treatment with Tasigna altogether if they are showing a strong response to therapy. While we welcome this progress in patient care, it’s important to note that any discontinuation of treatment still means patients must be regularly monitored for disease recurrence,” Dr. Pazdur said in the FDA statement.
Common side effects after discontinuing use of nilotinib include body aches and pain in the bones and extremities. Severe side effects of taking nilotinib can include myelosuppression, blockages in the heart and arteries, and inflammation of the pancreas. Severe liver damage can also occur.
Severe side effects typically associated with nilotinib administration occurred less frequently in patients who discontinued the drug. However, the long-term outcomes of patients discontinuing versus continuing treatment are unknown at this time, the FDA noted.
for patients who meet certain criteria. Nilotinib, a kinase inhibitor that blocks the BCR-ABL protein that promotes abnormal cell growth, was originally approved in 2007 and was indicated for use in patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML). In accordance with the new label update, patients who have early phase CML, have been using nilotinib for 3 years or more, and whose leukemia has responded to treatment according to a test that has received FDA marketing authorization, may be eligible to discontinue use of nilotinib.
The information that led to the FDA approved label update was based on two single-arm trials of patients with chronic phase Ph+ CML. The trial measured the length of time patients were able to discontinue use of nilotinib without leukemia returning, and who had entered treatment-free remission (TFR). In the first trial, among 190 newly diagnosed CML patients who discontinued taking nilotinib after using the drug for 3 or more years, 51.6% were still in TFR after about 1 year (48 weeks) and 48.9% were still in TFR after nearly 2 years (96 weeks). Similar results were seen in the second trial, among 126 patients, with 57.9% in TFR after about a year (48 weeks) and 53.2% in TFR after approximately 2 years (96 weeks).
An important element of these trials was regular monitoring of specific RNA information that specifies the level of BCR-ABL protein in the blood using a diagnostic test that has received FDA marketing authorization. Monitoring with a test that accurately detects the reductions of RNA information in the blood with accuracy and precision is critical in discontinuing the use of nilotinib. This monitoring will allow physicians to detect the first signs of relapse.
“Patients diagnosed with CML generally face a lifetime of treatment to keep their leukemia from growing or recurring,” said Richard Pazdur, MD, acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval shows that some patients may be able to stop treatment with Tasigna altogether if they are showing a strong response to therapy. While we welcome this progress in patient care, it’s important to note that any discontinuation of treatment still means patients must be regularly monitored for disease recurrence,” Dr. Pazdur said in the FDA statement.
Common side effects after discontinuing use of nilotinib include body aches and pain in the bones and extremities. Severe side effects of taking nilotinib can include myelosuppression, blockages in the heart and arteries, and inflammation of the pancreas. Severe liver damage can also occur.
Severe side effects typically associated with nilotinib administration occurred less frequently in patients who discontinued the drug. However, the long-term outcomes of patients discontinuing versus continuing treatment are unknown at this time, the FDA noted.
FDA approves raltegravir for newborns at risk for HIV-1 infection
The Food and Drug Administration has approved the use of raltegravir (Isentress), in combination with other antiretrovirals, for HIV-1 exposed newborns who weigh at least 2 kg and are at high risk for acquiring HIV-1 infection from their mothers, according to a press release from Merck, the manufacturer of Isentress.
“With this FDA approval, Isentress becomes the only integrase inhibitor approved in the U.S. for the treatment of HIV-1, in combination with other antiretroviral agents, for neonates weighing at least 2 kg,” Eliav Barr, MD, senior vice president, global clinical development, infectious diseases and vaccines, Merck Research Laboratories, said in a statement.
The study, IMPAACT P1110, was composed of two cohorts receiving different doses of raltegravir at different time intervals. The first cohort, of 16 newborns, received two single doses of raltegravir: the first within 48 hours of birth and the second between 7 and 10 days of age. The second cohort of 26 newborns received daily doses based on weight for 6 weeks. After observation for 24 weeks, all infants were HIV-1 negative.
Raltegravir does not cure HIV-1 infection or AIDS and severe side effects have been reported, including hypersensitivity reaction and toxic epidermal necrolysis, according to the Merck release.
Raltegravir should not be used in newborns and infants weighing under 2 kg. If raltegravir has been administered to the mother 2-24 hours before delivery, the first dose for the newborn should be given between 24 and 48 hours after birth.
The Food and Drug Administration has approved the use of raltegravir (Isentress), in combination with other antiretrovirals, for HIV-1 exposed newborns who weigh at least 2 kg and are at high risk for acquiring HIV-1 infection from their mothers, according to a press release from Merck, the manufacturer of Isentress.
“With this FDA approval, Isentress becomes the only integrase inhibitor approved in the U.S. for the treatment of HIV-1, in combination with other antiretroviral agents, for neonates weighing at least 2 kg,” Eliav Barr, MD, senior vice president, global clinical development, infectious diseases and vaccines, Merck Research Laboratories, said in a statement.
The study, IMPAACT P1110, was composed of two cohorts receiving different doses of raltegravir at different time intervals. The first cohort, of 16 newborns, received two single doses of raltegravir: the first within 48 hours of birth and the second between 7 and 10 days of age. The second cohort of 26 newborns received daily doses based on weight for 6 weeks. After observation for 24 weeks, all infants were HIV-1 negative.
Raltegravir does not cure HIV-1 infection or AIDS and severe side effects have been reported, including hypersensitivity reaction and toxic epidermal necrolysis, according to the Merck release.
Raltegravir should not be used in newborns and infants weighing under 2 kg. If raltegravir has been administered to the mother 2-24 hours before delivery, the first dose for the newborn should be given between 24 and 48 hours after birth.
The Food and Drug Administration has approved the use of raltegravir (Isentress), in combination with other antiretrovirals, for HIV-1 exposed newborns who weigh at least 2 kg and are at high risk for acquiring HIV-1 infection from their mothers, according to a press release from Merck, the manufacturer of Isentress.
“With this FDA approval, Isentress becomes the only integrase inhibitor approved in the U.S. for the treatment of HIV-1, in combination with other antiretroviral agents, for neonates weighing at least 2 kg,” Eliav Barr, MD, senior vice president, global clinical development, infectious diseases and vaccines, Merck Research Laboratories, said in a statement.
The study, IMPAACT P1110, was composed of two cohorts receiving different doses of raltegravir at different time intervals. The first cohort, of 16 newborns, received two single doses of raltegravir: the first within 48 hours of birth and the second between 7 and 10 days of age. The second cohort of 26 newborns received daily doses based on weight for 6 weeks. After observation for 24 weeks, all infants were HIV-1 negative.
Raltegravir does not cure HIV-1 infection or AIDS and severe side effects have been reported, including hypersensitivity reaction and toxic epidermal necrolysis, according to the Merck release.
Raltegravir should not be used in newborns and infants weighing under 2 kg. If raltegravir has been administered to the mother 2-24 hours before delivery, the first dose for the newborn should be given between 24 and 48 hours after birth.
FDA approves hydroxyurea for pediatric patients with sickle cell anemia
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
to reduce the frequency of painful crises and the need for blood transfusions, the Food and Drug Administration announced on Dec. 21.
This is the first FDA approval of hydroxyurea for use in pediatric sickle cell patients. The recommended initial dose is 20 mg/kg once daily but can be changed based on blood count levels, the agency said in a press release.
The most common adverse reactions to hydroxyurea, infections and neutropenia, occurred in less than 10% of patients. Hydroxyurea causes severe myelosuppression and should not be administered to patients with depressed bone marrow function.
Hydroxyurea is manufactured as Siklos by Addmedica. More information concerning hydroxyurea indications, dosing, and precautions can be found here.
SOURCE: FDA press release.
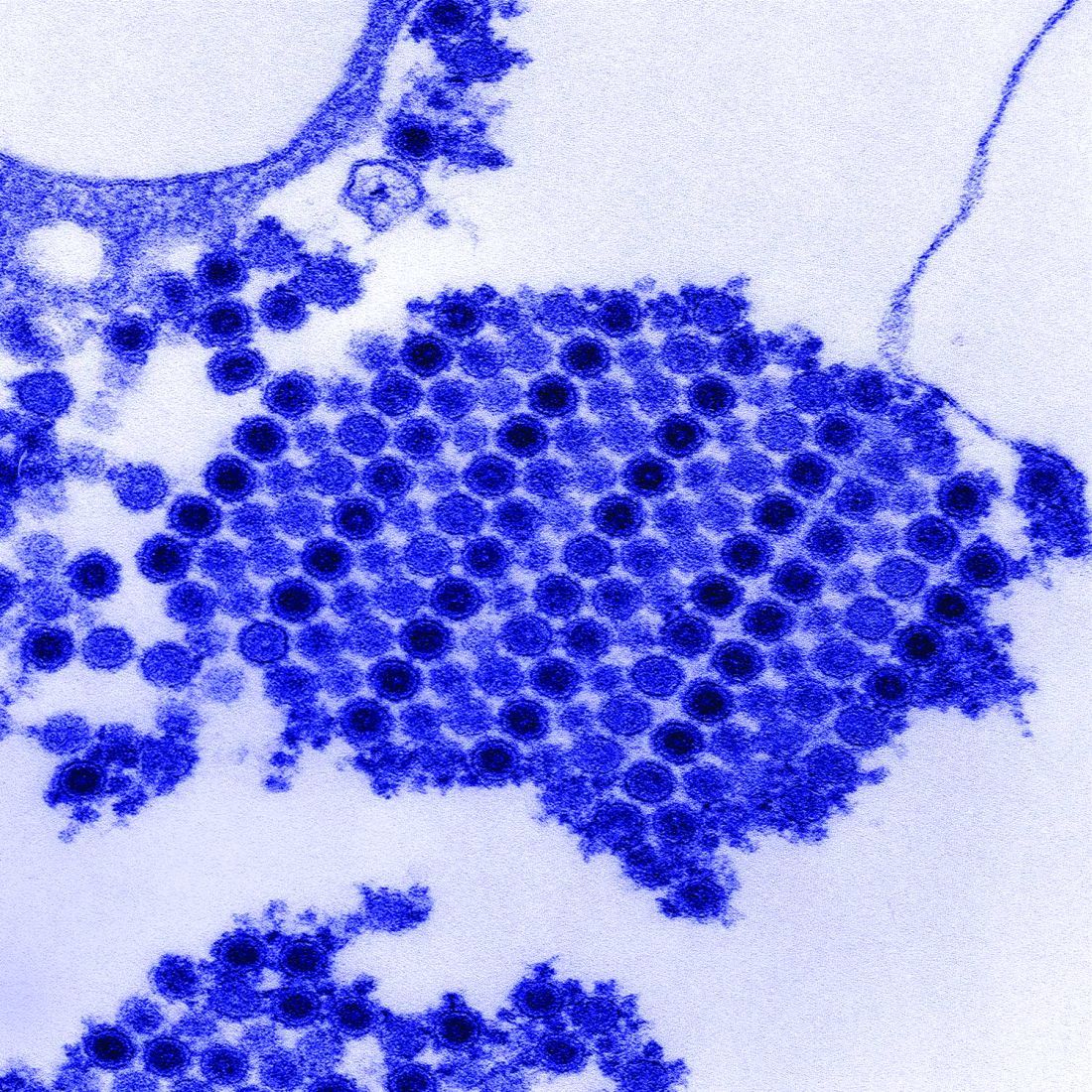
Chikungunya virus goes undetected despite chronic arthritis in 25% of patients after 20 months
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
Up to a quarter of patients infected with chikungunya virus who reported joint pain as one of their initial symptoms continue to have joint pain after 20 months of follow-up, and evidence suggests that the persistent joint symptoms are not related to the continued presence of the virus in synovial fluid, according to two studies of patients infected during the 2014-2015 Colombian epidemic.
In the first large-scale, cross-sectional follow-up of a prospective cohort from the Colombian epidemic, Aileen Chang, MD, of George Washington University, Washington, and her colleagues at multiple other institutions reported persistent joint pain and multiple swollen and/or tender joints after 20 months in 123 of 485 Colombian patients who initially had joint pain with their Chikungunya virus infection (CHIKV) diagnosis. In their report in Arthritis & Rheumatology, they said that increased initial viral load and severe initial joint pain were predictors of persistent arthritis, which is consistent with the work of other researchers.
Dr. Chang worked with a variety of coinvestigators, some of whom were also involved in the larger symptom follow-up study, to conduct this Study of Chikungunya Arthritis Mechanisms in the Americas (CAMA). They collected synovial fluid and blood plasma from these 38 patients as well as 10 healthy controls who were serologically negative for CHIKV and never had arthritis, and analyzed the fluid and plasma for signs of CHIKV. They assessed viral RNA via quantitative reverse transcription polymerase chain reaction (qRT-PCR) testing, looked at viral proteins via mass spectrometry, and did viral cultures.
All samples from the 38 patients in the study were negative for CHIKV in two separate qRT-PCR assays. To determine if low-level viremia was present in synovial fluid samples, the samples were added to cell cultures to expand viral replication. No viral growth was found after three attempts and 10 days of culture. Conversely, controls with low quantities of virus (about 1 plaque-forming unit per well) yielded growth and detection of the virus.
Patients with CHIKV-associated arthritis also had no significant increase in rheumatoid arthritis markers or C-reactive protein. In fact, plasma markers for rheumatoid arthritis were found in only a fraction of patients with CHIKV arthritis: rheumatoid factor (RF) IgM antibody in 9%, RF IgG antibody in 12%, and anti–cyclic citrullinated peptide in 0%.
The more probable potential mechanisms through which CHIKV could cause persistent arthritis symptoms is through the presence of persistent CHIKV or viral antigens at low enough levels in the synovial tissue that it is undetectable in the synovial fluid, Dr. Chang and her associates suggested. There is also a possibility of epigenetic changes to the host DNA, altering host gene transcription. Other epigenetic changes, like epigenetic imprinting, could be possible in macrophages, leading to more aggressive cell behavior, they said. Unlikelier scenarios would be the presence of seronegative RA in these patients or, alternatively, the presence of seronegative RA indicating prior infection with CHIKV or other arthritogenic viruses.
Whatever mechanisms are causing CHIKV-associated arthritis, “these study findings may have important clinical relevance for CHIKV in the Americas. Since there is no current standard of care guidance for the treatment of CHIKV arthritis, some patients are currently being treated with immunosuppressant medications such as methotrexate, hydroxychloroquine, etanercept, adalimumab, sulfasalazine, fingolimod, abatacept, and tofacitinib,” Dr. Chang and her colleagues wrote. “This practice could be potentially harmful in the setting of replicating virus in the synovium as it could permit reemergence of a systemic viral infection.”
The CAMA study has several important limitations , the investigators said, the first being that during collection of synovial fluid, 0-20 mL of saline solution were used to flush the joints, which could have affected the ability to detect virus in the samples. In an attempt to mitigate this, the researchers cultured 0.5-1.5 mL of sampled synovial fluid to expand any replication-competent virus present in the sample, used two complementary PCR assays to detect nucleic acids, and a proteomic approach to look for viral proteins.
The researchers acknowledged that despite these measures, “proving the absence of a target is difficult, and we recognize that it is possible that our approach failed to detect low-level viral antigen; however, our orthogonal approach clearly demonstrates that if viral antigen exists in the synovial fluid, it is at extremely low levels.” They advised that future studies may want to use synovial biopsies rather than extracted fluid.
The investigators also did not include patients who had previously been infected by CHIKV without chronic arthritis. This issue was compounded by the lack of age- and sex-matched healthy controls.
All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
SOURCE: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: No signs of persistent CHIKV infection can be found in synovial fluid or blood plasma from patients with chronic arthritis after CHIKV.
Study details: Cross-sectional studies of 485 Colombian patients who had clinical CHIKV and associated arthritis symptoms in 2014-2015 and another 38 patients who underwent further synovial fluid and blood plasma testing after a median of 22 months.
Disclosures: All researchers involved in the studies reported no financial conflicts of interest. The studies were supported by various grants from the National Institutes of Health and the Rheumatology Research Foundation.
Source: Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40383 and Chang A et al. Arthritis Rheumatol. 2017 Dec 20. doi: 10.1002/art.40384.
FDA okays dosing software for hemophilia A
The Food and Drug Administration has granted 510(k) clearance to myPKFiT for ADVATE (Antihemophilic Factor, Recombinant), pharmokinetic dosing software used for tailoring prophylaxis regimens for hemophilia A patients.
The software can be used for hemophilia A patients aged 16 years or older who weigh at least 45 kilograms (about 99 pounds) and are treated with ADVATE.
The free, web-based software estimates a patient’s pharmokinetic curve using age, body weight, and local laboratory FVIII one-stage clotting activity measurements and allows physicians to estimate a full pharmokinetic curve with just two measurable blood samples, according to Shire, the software’s manufacturer. That’s much lower than the 9-11 blood samples recommendation from the International Society on Thrombosis and Haemostasis.
The software is expected to be available in the United States by the end of the first quarter of 2018. A version of the software is already marketed in Europe.
The Food and Drug Administration has granted 510(k) clearance to myPKFiT for ADVATE (Antihemophilic Factor, Recombinant), pharmokinetic dosing software used for tailoring prophylaxis regimens for hemophilia A patients.
The software can be used for hemophilia A patients aged 16 years or older who weigh at least 45 kilograms (about 99 pounds) and are treated with ADVATE.
The free, web-based software estimates a patient’s pharmokinetic curve using age, body weight, and local laboratory FVIII one-stage clotting activity measurements and allows physicians to estimate a full pharmokinetic curve with just two measurable blood samples, according to Shire, the software’s manufacturer. That’s much lower than the 9-11 blood samples recommendation from the International Society on Thrombosis and Haemostasis.
The software is expected to be available in the United States by the end of the first quarter of 2018. A version of the software is already marketed in Europe.
The Food and Drug Administration has granted 510(k) clearance to myPKFiT for ADVATE (Antihemophilic Factor, Recombinant), pharmokinetic dosing software used for tailoring prophylaxis regimens for hemophilia A patients.
The software can be used for hemophilia A patients aged 16 years or older who weigh at least 45 kilograms (about 99 pounds) and are treated with ADVATE.
The free, web-based software estimates a patient’s pharmokinetic curve using age, body weight, and local laboratory FVIII one-stage clotting activity measurements and allows physicians to estimate a full pharmokinetic curve with just two measurable blood samples, according to Shire, the software’s manufacturer. That’s much lower than the 9-11 blood samples recommendation from the International Society on Thrombosis and Haemostasis.
The software is expected to be available in the United States by the end of the first quarter of 2018. A version of the software is already marketed in Europe.