User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
CDC: Five confirmed 2019-nCoV cases in the U.S.
Five cases of the new infectious coronavirus, 2019-nCoV, have been confirmed in the United States, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during a Jan. 27 press briefing.
A total of 110 individuals are under investigation in 26 states, she said. While five cases have been confirmed positive for the virus, 32 cases were confirmed negative. There have been no new cases overnight.
Last week, CDC scientists developed a real-time polymerase chain reaction (PCR) test that can diagnose the virus in respiratory and serum samples from clinical specimens. On Jan. 24, the protocol for this test was publicly posted. “This is essentially a blueprint to make the test,” Dr. Messonnier explained. “Currently, we are refining the use of the test so that it can provide optimal guidance to states and labs on how to use it. We are working on a plan so that priority states get these test kits as soon as possible. In the coming weeks, we will share these tests with domestic and international partners so they can test for this virus themselves.”
The CDC uploaded the entire genome of the virus from the first two cases in the United States to GenBank. It was similar to the one that China had previously posted. “Right now, based on CDC’s analysis of the available data, it doesn’t look like the virus has mutated,” she said. “And we are growing the virus in cell culture, which is necessary for further studies, including the additional genetic characterization.”
As of today, 16 international locations, including the United States, have identified cases of the virus. CDC officials are continuing to screen passengers from Wuhan, China, at five designated airports. “This serves two purposes: first to detect the illness and rapidly respond to [affected] people entering the country,” Dr. Messonnier said. “The second purpose is to educate travelers about the symptoms of this new virus, and what to do if they develop symptoms. I expect that in the coming days, our travel recommendations will change. Risk depends on exposure. Right now, we have an handful of new patients with this new virus here in the U.S. However, at this time in the U.S., this virus is not spreading in the community. For that reason, we believe that the immediate health risk of the new virus to the general American public is low.”
The CDC is asking its clinical lab partners to send virus samples to the CDC to ensure that results are analyzed as accurately as possible.
Five cases of the new infectious coronavirus, 2019-nCoV, have been confirmed in the United States, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during a Jan. 27 press briefing.
A total of 110 individuals are under investigation in 26 states, she said. While five cases have been confirmed positive for the virus, 32 cases were confirmed negative. There have been no new cases overnight.
Last week, CDC scientists developed a real-time polymerase chain reaction (PCR) test that can diagnose the virus in respiratory and serum samples from clinical specimens. On Jan. 24, the protocol for this test was publicly posted. “This is essentially a blueprint to make the test,” Dr. Messonnier explained. “Currently, we are refining the use of the test so that it can provide optimal guidance to states and labs on how to use it. We are working on a plan so that priority states get these test kits as soon as possible. In the coming weeks, we will share these tests with domestic and international partners so they can test for this virus themselves.”
The CDC uploaded the entire genome of the virus from the first two cases in the United States to GenBank. It was similar to the one that China had previously posted. “Right now, based on CDC’s analysis of the available data, it doesn’t look like the virus has mutated,” she said. “And we are growing the virus in cell culture, which is necessary for further studies, including the additional genetic characterization.”
As of today, 16 international locations, including the United States, have identified cases of the virus. CDC officials are continuing to screen passengers from Wuhan, China, at five designated airports. “This serves two purposes: first to detect the illness and rapidly respond to [affected] people entering the country,” Dr. Messonnier said. “The second purpose is to educate travelers about the symptoms of this new virus, and what to do if they develop symptoms. I expect that in the coming days, our travel recommendations will change. Risk depends on exposure. Right now, we have an handful of new patients with this new virus here in the U.S. However, at this time in the U.S., this virus is not spreading in the community. For that reason, we believe that the immediate health risk of the new virus to the general American public is low.”
The CDC is asking its clinical lab partners to send virus samples to the CDC to ensure that results are analyzed as accurately as possible.
Five cases of the new infectious coronavirus, 2019-nCoV, have been confirmed in the United States, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during a Jan. 27 press briefing.
A total of 110 individuals are under investigation in 26 states, she said. While five cases have been confirmed positive for the virus, 32 cases were confirmed negative. There have been no new cases overnight.
Last week, CDC scientists developed a real-time polymerase chain reaction (PCR) test that can diagnose the virus in respiratory and serum samples from clinical specimens. On Jan. 24, the protocol for this test was publicly posted. “This is essentially a blueprint to make the test,” Dr. Messonnier explained. “Currently, we are refining the use of the test so that it can provide optimal guidance to states and labs on how to use it. We are working on a plan so that priority states get these test kits as soon as possible. In the coming weeks, we will share these tests with domestic and international partners so they can test for this virus themselves.”
The CDC uploaded the entire genome of the virus from the first two cases in the United States to GenBank. It was similar to the one that China had previously posted. “Right now, based on CDC’s analysis of the available data, it doesn’t look like the virus has mutated,” she said. “And we are growing the virus in cell culture, which is necessary for further studies, including the additional genetic characterization.”
As of today, 16 international locations, including the United States, have identified cases of the virus. CDC officials are continuing to screen passengers from Wuhan, China, at five designated airports. “This serves two purposes: first to detect the illness and rapidly respond to [affected] people entering the country,” Dr. Messonnier said. “The second purpose is to educate travelers about the symptoms of this new virus, and what to do if they develop symptoms. I expect that in the coming days, our travel recommendations will change. Risk depends on exposure. Right now, we have an handful of new patients with this new virus here in the U.S. However, at this time in the U.S., this virus is not spreading in the community. For that reason, we believe that the immediate health risk of the new virus to the general American public is low.”
The CDC is asking its clinical lab partners to send virus samples to the CDC to ensure that results are analyzed as accurately as possible.
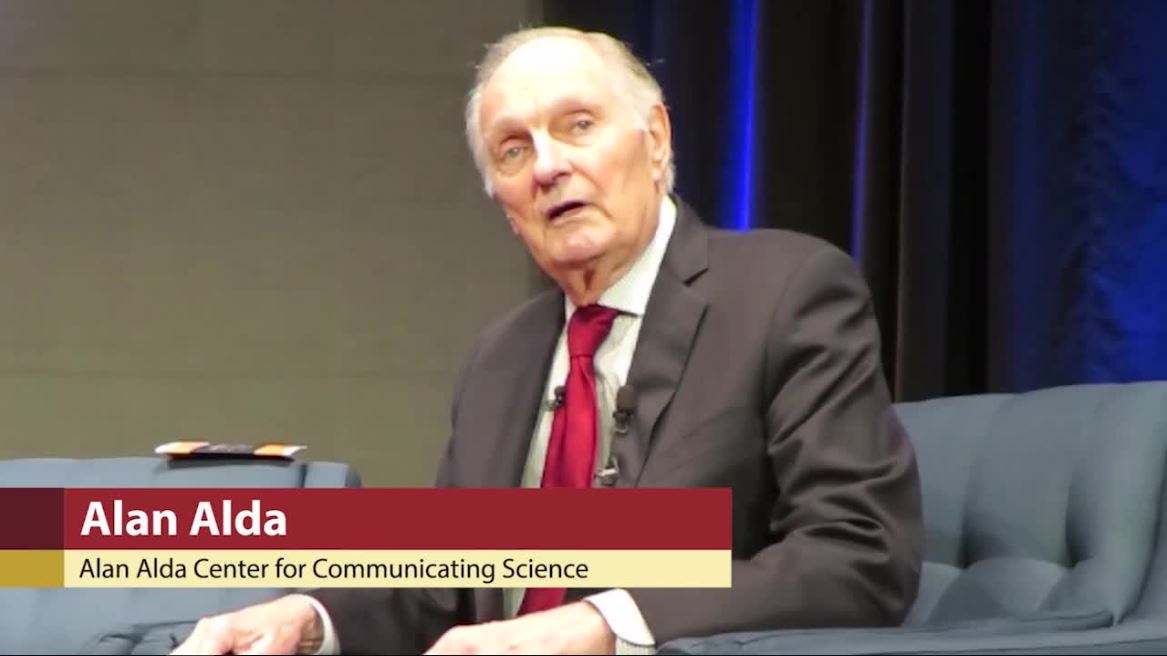
Actor Alan Alda discusses using empathy as an antidote to burnout
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
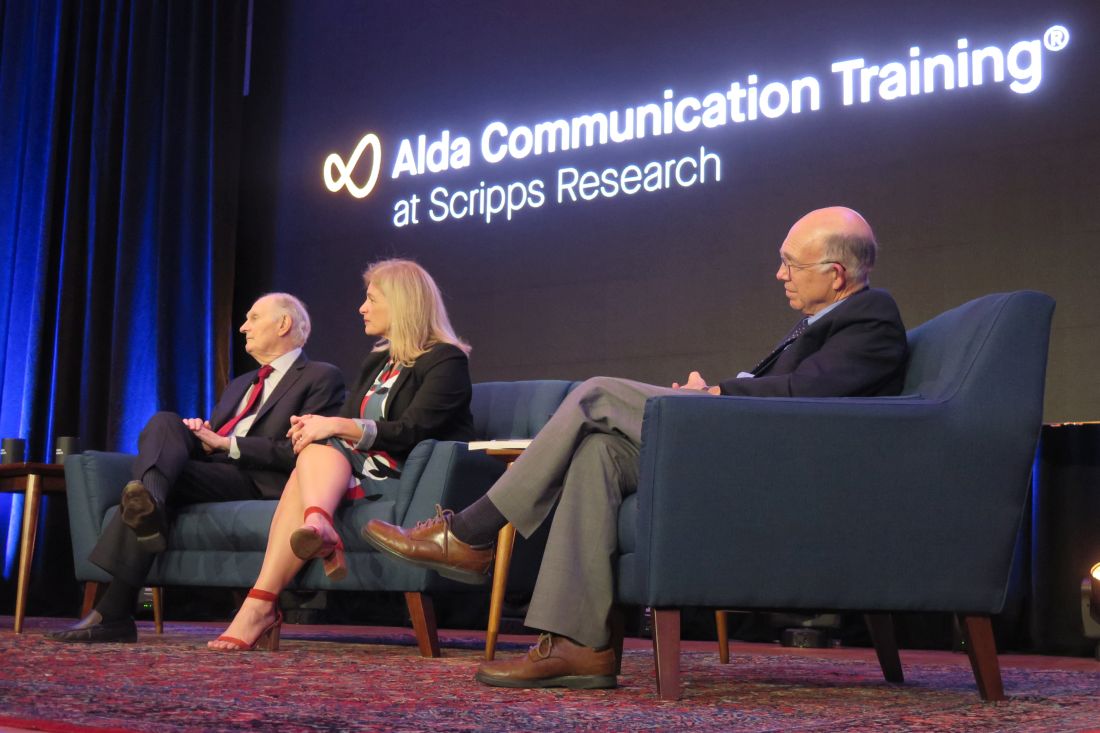
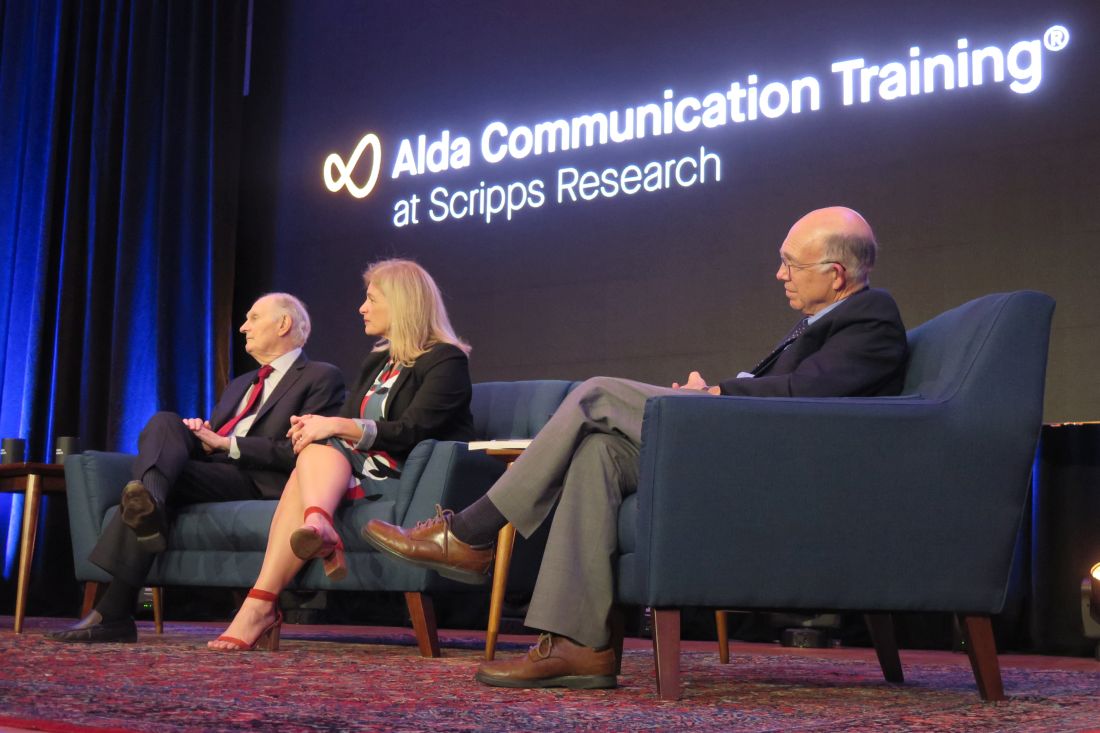
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
Alan Alda, Scripps Research join forces to improve science communication
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
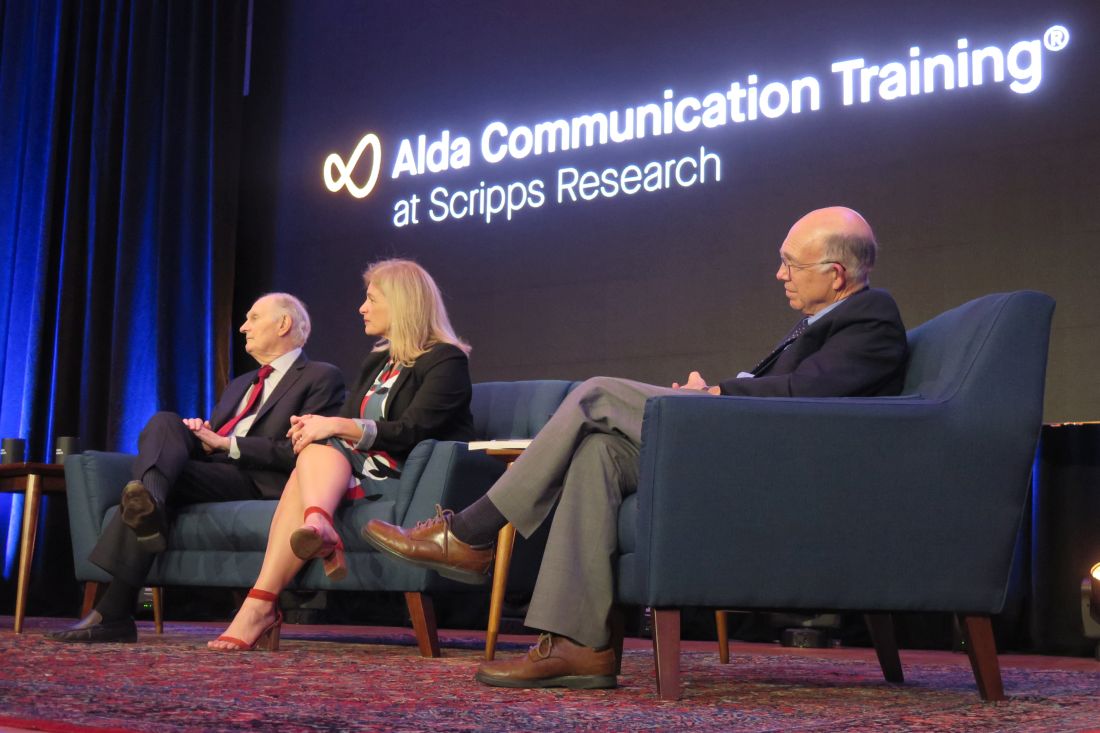
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
Sarcopenia associated with increased cardiometabolic risk
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019
Bariatric surgery is most effective early in the diabetes trajectory
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019
Treatment of heart failure with preserved ejection fraction is a work in progress
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019
Carbohydrate restriction a viable choice for reversal of type 2 diabetes, expert says
LOS ANGELES – according to Sarah Hallberg, DO.
“Nutritional ketosis supports diabetes reversal by reducing insulin resistance while providing an alternative fuel to glucose with favorable signaling properties,” she said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease.
Low-carbohydrate nutritional patterns including ketosis have extensive clinical trial evidence for improvement of type 2 diabetes, including preliminary results from a 5-year study of 465 patients enrolled in the Indiana Type 2 Diabetes Reversal Trial that Dr. Hallberg is overseeing in her role as medical director and founder of the medically supervised weight-loss program at Indiana University Health Arnett, Lafayette.
“The ketogenic diet is not a fad diet, it’s what we used to treat people with before the advent of insulin,” said Dr. Hallberg, who has been recommending and counseling patients with type 2 diabetes to follow a ketogenic diet for nearly 10 years. “Of course, insulin has been wonderful. It’s saved so many people with type 1 diabetes. But we also misused it in type 2 diabetes. Instead of counseling people the way we used to about the food that they’re taking in to control their blood sugar, we’ve just been putting [them] on medication, including insulin.”
The American Diabetes Association and other organizations have updated their guidelines to include low-carbohydrate eating patterns for type 2 diabetes treatment, she continued. Veterans Affairs/Department of Defense recommend carbohydrate levels as low as 14%.
Dr. Hallberg, who is also medical director for Virta Health, defined a very-low-carbohydrate or ketogenic diet as less than 50 g of carbohydrates per day, or fewer than 10% of calories consumed. A low-carbohydrate diet is 51-130 g of carbohydrates per day, or 25% or fewer calories consumed, whereas anything above 25% calories consumed is a not a low-carbohydrate diet. A well-formulated ketogenic diet, she continued, consists of 5%-10% carbohydrates (or less than 50 g), 15%-20% protein, and 70%-80% fat. The carbohydrates include 5-10 g per day of protein-based food, 10-15 g of vegetables, 5-10 g of nuts/seeds, 5-10 g of fruits, and 5-10 g of miscellaneous nutrients. “When we’re talking about a total carbohydrate intake per day of under 50 g, you can get a lot of vegetables and nuts in,” she said. “I like to tell my patients they’re not eating GPS: no grains, no potatoes, and no sugar.”
Recently, Dr. Hallberg and colleagues published a review in which they sought to evaluate the appropriateness of sources cited in the ADA’s guidelines on eating patterns for the management of type 2 diabetes, identify additional relevant sources, and evaluate the evidence (Diabetes Obes Metab. 2019;21[8]:1769-79). “We looked at how much evidence there is for the low-carb diet, the Mediterranean diet, the DASH [Dietary Approaches to Stop Hypertension] diet, and a plant-based diet,” she said. “We found a wide variation in the evidence for each eating pattern, but the low-carb eating pattern for diabetes has so much more evidence than any of the other eating patterns.”
In an earlier study, researchers followed 10 inpatients with diabetes in a metabolic ward for 3 weeks. Their mean age was 51 years, and their mean body mass index was 40.3 kg/m2. The patients were fed a standard diet for 7 days, then a low-carbohydrate diet (21 g per day) for 14 days (Ann Intern Med 2005; 142[6]:403-11). After 2 weeks of the low-carbohydrate diet, their mean fasting blood glucose dropped from 7.5 to 6.3 mmol/L, and their mean hemoglobin A1c (HbA1c) fell from 7.3% to 6.8%. “The levels came down very fast,” said Dr. Hallberg, who was not involved with the study. “This is an important part of the intervention, because when you get a patient who’s tried everything, who’s injecting hundreds of units of insulin every day, you can make a huge difference in the first couple of weeks. It is not unusual for us to pull patients off of 200-plus units of insulin. This is as motivating as all get out. It also affects their pocketbook right away. This is one of the reasons our patients are able to sustain a ketogenic diet along with support: early motivation and satisfaction.”
In a longer-term trial, researchers evaluated the impact of a ketogenic diet in 64 obese patients with diabetes over the course of 56 weeks (Moll Cell Biochem. 2007;302[1-2]:249-56). The body weight, body mass index, and levels of blood glucose, total cholesterol, LDL cholesterol, triglycerides, and urea showed a significant decrease from week 1 to week 56 (P less than .0001), while the level of HDL cholesterol increased significantly (P less than .0001).
A separate trial conducted in Israel evaluated the effects of a low-carbohydrate diet, compared with a Mediterranean or low-fat diet in 322 moderately obese patients over the course of 2 years (N Engl J Med. 2008;359:229-41). The rate of adherence to a study diet was 85% at 2 years. The mean weight change was greatest for those on the low-carbohydrate diet, followed by the Mediterranean and low-fat diets. Fasting glucose was best for those on the Mediterranean diet at the end of 2 years, whereas change in HbA1c was best among those on the low-carbohydrate diet.
Another study randomized patients to a low-carbohydrate ketogenic diet (less than 20 g per day with no calorie restriction) or to a low–glycemic index diet (55% carbohydrate restriction of 500 kcal from baseline) over the course of 24 weeks (Nutr Metab [Lond]. 2008 Dec 19. doi:10.1186/1743-7075-5-36). Between baseline and week 24, the mean HbA1c fell from 8.8% to 7.3% in the very-low-carbohydrate diet group, and from 8.3% to 7.8% in the low–glycemic diet group, for a between-group comparison P value of .03. In addition, 95% of patients in the low-carbohydrate diet group were able to reduce or eliminate the number of medications they were taking, compared with 62% of patients in the low–glycemic diet group (P less than .01).
Dr. Hallberg and colleagues are currently in year 4 of the 5-year Indiana Type 2 Diabetes Reversal Study, a prospective, nonrandomized, controlled trial of carbohydrate restriction in 465 patients, making it the largest and longest study of its kind. Of the 465 patients, 387 are in the continuous-care arm, which consists of a diet from Virta Health based on principles of nutritional ketosis, and 87 patients in a usual care arm who are followed for 2 years. The trial includes patients who have been prescribed insulin and who have been diagnosed with diabetes for an average of 8 years.
At the meeting, Dr. Hallberg presented preliminary results based on 2 years of data collection. The retention rate was 83% at 1 year and 74% at 2 years. In the treatment arm, the researchers observed that the level of beta hydroxybutyrate, or evidence of ketogenesis, was the same at 2 years as it had been at 1 year. “So, people were still following the diet, as well as being engaged,” she said.
At the end of 2 years, the mean HbA1c reduction was 0.9, the mean reduction for the Homeostatic Model Assessment of Insulin Resistance was 32%, and 55% of completers experienced reversal of their diabetes. Overall, 91% of insulin users reduced or eliminated their use of insulin, and the average weight loss was 10% of baseline weight. “Medication reduction was across the board,” she added. “This is huge from a cost-savings and a patient-satisfaction standpoint. We were improving A1c levels in patients who have had diabetes for an average of over 8 years while we were getting [them] off medication, including insulin. Low carb is now the standard of care.”
Even patients who did not experience a reversal of their diabetes were conferred a benefit. They had an average reduction of 1.2 in HbA1c level, to 7%; their average weight loss was 9.8%; 45% of patients eliminated their diabetes prescriptions; 81% reduced or eliminated their use of insulin; there was an average reduction of 27% in triglyceride levels; and they had a 17% reduction in their 10-year risk score for atherosclerotic cardiovascular disease.
In the overall cohort, the 10-year Atherosclerotic Cardiovascular Disease risk score improved by 12%; almost all markers for cardiovascular disease improved at 1 year. “We were giving these patients appropriate support, which I think is key,” Dr. Hallberg said. “No matter what you do, you have to have a high-touch intervention, and supply that through technology. We do better than medication adherence. Putting patients on a carbohydrate-restricted diet with the appropriate support works for sustainability.”
Dr. Hallberg disclosed that she is an employee of Virta Health and that she is an adviser for Simply Good Foods.
LOS ANGELES – according to Sarah Hallberg, DO.
“Nutritional ketosis supports diabetes reversal by reducing insulin resistance while providing an alternative fuel to glucose with favorable signaling properties,” she said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease.
Low-carbohydrate nutritional patterns including ketosis have extensive clinical trial evidence for improvement of type 2 diabetes, including preliminary results from a 5-year study of 465 patients enrolled in the Indiana Type 2 Diabetes Reversal Trial that Dr. Hallberg is overseeing in her role as medical director and founder of the medically supervised weight-loss program at Indiana University Health Arnett, Lafayette.
“The ketogenic diet is not a fad diet, it’s what we used to treat people with before the advent of insulin,” said Dr. Hallberg, who has been recommending and counseling patients with type 2 diabetes to follow a ketogenic diet for nearly 10 years. “Of course, insulin has been wonderful. It’s saved so many people with type 1 diabetes. But we also misused it in type 2 diabetes. Instead of counseling people the way we used to about the food that they’re taking in to control their blood sugar, we’ve just been putting [them] on medication, including insulin.”
The American Diabetes Association and other organizations have updated their guidelines to include low-carbohydrate eating patterns for type 2 diabetes treatment, she continued. Veterans Affairs/Department of Defense recommend carbohydrate levels as low as 14%.
Dr. Hallberg, who is also medical director for Virta Health, defined a very-low-carbohydrate or ketogenic diet as less than 50 g of carbohydrates per day, or fewer than 10% of calories consumed. A low-carbohydrate diet is 51-130 g of carbohydrates per day, or 25% or fewer calories consumed, whereas anything above 25% calories consumed is a not a low-carbohydrate diet. A well-formulated ketogenic diet, she continued, consists of 5%-10% carbohydrates (or less than 50 g), 15%-20% protein, and 70%-80% fat. The carbohydrates include 5-10 g per day of protein-based food, 10-15 g of vegetables, 5-10 g of nuts/seeds, 5-10 g of fruits, and 5-10 g of miscellaneous nutrients. “When we’re talking about a total carbohydrate intake per day of under 50 g, you can get a lot of vegetables and nuts in,” she said. “I like to tell my patients they’re not eating GPS: no grains, no potatoes, and no sugar.”
Recently, Dr. Hallberg and colleagues published a review in which they sought to evaluate the appropriateness of sources cited in the ADA’s guidelines on eating patterns for the management of type 2 diabetes, identify additional relevant sources, and evaluate the evidence (Diabetes Obes Metab. 2019;21[8]:1769-79). “We looked at how much evidence there is for the low-carb diet, the Mediterranean diet, the DASH [Dietary Approaches to Stop Hypertension] diet, and a plant-based diet,” she said. “We found a wide variation in the evidence for each eating pattern, but the low-carb eating pattern for diabetes has so much more evidence than any of the other eating patterns.”
In an earlier study, researchers followed 10 inpatients with diabetes in a metabolic ward for 3 weeks. Their mean age was 51 years, and their mean body mass index was 40.3 kg/m2. The patients were fed a standard diet for 7 days, then a low-carbohydrate diet (21 g per day) for 14 days (Ann Intern Med 2005; 142[6]:403-11). After 2 weeks of the low-carbohydrate diet, their mean fasting blood glucose dropped from 7.5 to 6.3 mmol/L, and their mean hemoglobin A1c (HbA1c) fell from 7.3% to 6.8%. “The levels came down very fast,” said Dr. Hallberg, who was not involved with the study. “This is an important part of the intervention, because when you get a patient who’s tried everything, who’s injecting hundreds of units of insulin every day, you can make a huge difference in the first couple of weeks. It is not unusual for us to pull patients off of 200-plus units of insulin. This is as motivating as all get out. It also affects their pocketbook right away. This is one of the reasons our patients are able to sustain a ketogenic diet along with support: early motivation and satisfaction.”
In a longer-term trial, researchers evaluated the impact of a ketogenic diet in 64 obese patients with diabetes over the course of 56 weeks (Moll Cell Biochem. 2007;302[1-2]:249-56). The body weight, body mass index, and levels of blood glucose, total cholesterol, LDL cholesterol, triglycerides, and urea showed a significant decrease from week 1 to week 56 (P less than .0001), while the level of HDL cholesterol increased significantly (P less than .0001).
A separate trial conducted in Israel evaluated the effects of a low-carbohydrate diet, compared with a Mediterranean or low-fat diet in 322 moderately obese patients over the course of 2 years (N Engl J Med. 2008;359:229-41). The rate of adherence to a study diet was 85% at 2 years. The mean weight change was greatest for those on the low-carbohydrate diet, followed by the Mediterranean and low-fat diets. Fasting glucose was best for those on the Mediterranean diet at the end of 2 years, whereas change in HbA1c was best among those on the low-carbohydrate diet.
Another study randomized patients to a low-carbohydrate ketogenic diet (less than 20 g per day with no calorie restriction) or to a low–glycemic index diet (55% carbohydrate restriction of 500 kcal from baseline) over the course of 24 weeks (Nutr Metab [Lond]. 2008 Dec 19. doi:10.1186/1743-7075-5-36). Between baseline and week 24, the mean HbA1c fell from 8.8% to 7.3% in the very-low-carbohydrate diet group, and from 8.3% to 7.8% in the low–glycemic diet group, for a between-group comparison P value of .03. In addition, 95% of patients in the low-carbohydrate diet group were able to reduce or eliminate the number of medications they were taking, compared with 62% of patients in the low–glycemic diet group (P less than .01).
Dr. Hallberg and colleagues are currently in year 4 of the 5-year Indiana Type 2 Diabetes Reversal Study, a prospective, nonrandomized, controlled trial of carbohydrate restriction in 465 patients, making it the largest and longest study of its kind. Of the 465 patients, 387 are in the continuous-care arm, which consists of a diet from Virta Health based on principles of nutritional ketosis, and 87 patients in a usual care arm who are followed for 2 years. The trial includes patients who have been prescribed insulin and who have been diagnosed with diabetes for an average of 8 years.
At the meeting, Dr. Hallberg presented preliminary results based on 2 years of data collection. The retention rate was 83% at 1 year and 74% at 2 years. In the treatment arm, the researchers observed that the level of beta hydroxybutyrate, or evidence of ketogenesis, was the same at 2 years as it had been at 1 year. “So, people were still following the diet, as well as being engaged,” she said.
At the end of 2 years, the mean HbA1c reduction was 0.9, the mean reduction for the Homeostatic Model Assessment of Insulin Resistance was 32%, and 55% of completers experienced reversal of their diabetes. Overall, 91% of insulin users reduced or eliminated their use of insulin, and the average weight loss was 10% of baseline weight. “Medication reduction was across the board,” she added. “This is huge from a cost-savings and a patient-satisfaction standpoint. We were improving A1c levels in patients who have had diabetes for an average of over 8 years while we were getting [them] off medication, including insulin. Low carb is now the standard of care.”
Even patients who did not experience a reversal of their diabetes were conferred a benefit. They had an average reduction of 1.2 in HbA1c level, to 7%; their average weight loss was 9.8%; 45% of patients eliminated their diabetes prescriptions; 81% reduced or eliminated their use of insulin; there was an average reduction of 27% in triglyceride levels; and they had a 17% reduction in their 10-year risk score for atherosclerotic cardiovascular disease.
In the overall cohort, the 10-year Atherosclerotic Cardiovascular Disease risk score improved by 12%; almost all markers for cardiovascular disease improved at 1 year. “We were giving these patients appropriate support, which I think is key,” Dr. Hallberg said. “No matter what you do, you have to have a high-touch intervention, and supply that through technology. We do better than medication adherence. Putting patients on a carbohydrate-restricted diet with the appropriate support works for sustainability.”
Dr. Hallberg disclosed that she is an employee of Virta Health and that she is an adviser for Simply Good Foods.
LOS ANGELES – according to Sarah Hallberg, DO.
“Nutritional ketosis supports diabetes reversal by reducing insulin resistance while providing an alternative fuel to glucose with favorable signaling properties,” she said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease.
Low-carbohydrate nutritional patterns including ketosis have extensive clinical trial evidence for improvement of type 2 diabetes, including preliminary results from a 5-year study of 465 patients enrolled in the Indiana Type 2 Diabetes Reversal Trial that Dr. Hallberg is overseeing in her role as medical director and founder of the medically supervised weight-loss program at Indiana University Health Arnett, Lafayette.
“The ketogenic diet is not a fad diet, it’s what we used to treat people with before the advent of insulin,” said Dr. Hallberg, who has been recommending and counseling patients with type 2 diabetes to follow a ketogenic diet for nearly 10 years. “Of course, insulin has been wonderful. It’s saved so many people with type 1 diabetes. But we also misused it in type 2 diabetes. Instead of counseling people the way we used to about the food that they’re taking in to control their blood sugar, we’ve just been putting [them] on medication, including insulin.”
The American Diabetes Association and other organizations have updated their guidelines to include low-carbohydrate eating patterns for type 2 diabetes treatment, she continued. Veterans Affairs/Department of Defense recommend carbohydrate levels as low as 14%.
Dr. Hallberg, who is also medical director for Virta Health, defined a very-low-carbohydrate or ketogenic diet as less than 50 g of carbohydrates per day, or fewer than 10% of calories consumed. A low-carbohydrate diet is 51-130 g of carbohydrates per day, or 25% or fewer calories consumed, whereas anything above 25% calories consumed is a not a low-carbohydrate diet. A well-formulated ketogenic diet, she continued, consists of 5%-10% carbohydrates (or less than 50 g), 15%-20% protein, and 70%-80% fat. The carbohydrates include 5-10 g per day of protein-based food, 10-15 g of vegetables, 5-10 g of nuts/seeds, 5-10 g of fruits, and 5-10 g of miscellaneous nutrients. “When we’re talking about a total carbohydrate intake per day of under 50 g, you can get a lot of vegetables and nuts in,” she said. “I like to tell my patients they’re not eating GPS: no grains, no potatoes, and no sugar.”
Recently, Dr. Hallberg and colleagues published a review in which they sought to evaluate the appropriateness of sources cited in the ADA’s guidelines on eating patterns for the management of type 2 diabetes, identify additional relevant sources, and evaluate the evidence (Diabetes Obes Metab. 2019;21[8]:1769-79). “We looked at how much evidence there is for the low-carb diet, the Mediterranean diet, the DASH [Dietary Approaches to Stop Hypertension] diet, and a plant-based diet,” she said. “We found a wide variation in the evidence for each eating pattern, but the low-carb eating pattern for diabetes has so much more evidence than any of the other eating patterns.”
In an earlier study, researchers followed 10 inpatients with diabetes in a metabolic ward for 3 weeks. Their mean age was 51 years, and their mean body mass index was 40.3 kg/m2. The patients were fed a standard diet for 7 days, then a low-carbohydrate diet (21 g per day) for 14 days (Ann Intern Med 2005; 142[6]:403-11). After 2 weeks of the low-carbohydrate diet, their mean fasting blood glucose dropped from 7.5 to 6.3 mmol/L, and their mean hemoglobin A1c (HbA1c) fell from 7.3% to 6.8%. “The levels came down very fast,” said Dr. Hallberg, who was not involved with the study. “This is an important part of the intervention, because when you get a patient who’s tried everything, who’s injecting hundreds of units of insulin every day, you can make a huge difference in the first couple of weeks. It is not unusual for us to pull patients off of 200-plus units of insulin. This is as motivating as all get out. It also affects their pocketbook right away. This is one of the reasons our patients are able to sustain a ketogenic diet along with support: early motivation and satisfaction.”
In a longer-term trial, researchers evaluated the impact of a ketogenic diet in 64 obese patients with diabetes over the course of 56 weeks (Moll Cell Biochem. 2007;302[1-2]:249-56). The body weight, body mass index, and levels of blood glucose, total cholesterol, LDL cholesterol, triglycerides, and urea showed a significant decrease from week 1 to week 56 (P less than .0001), while the level of HDL cholesterol increased significantly (P less than .0001).
A separate trial conducted in Israel evaluated the effects of a low-carbohydrate diet, compared with a Mediterranean or low-fat diet in 322 moderately obese patients over the course of 2 years (N Engl J Med. 2008;359:229-41). The rate of adherence to a study diet was 85% at 2 years. The mean weight change was greatest for those on the low-carbohydrate diet, followed by the Mediterranean and low-fat diets. Fasting glucose was best for those on the Mediterranean diet at the end of 2 years, whereas change in HbA1c was best among those on the low-carbohydrate diet.
Another study randomized patients to a low-carbohydrate ketogenic diet (less than 20 g per day with no calorie restriction) or to a low–glycemic index diet (55% carbohydrate restriction of 500 kcal from baseline) over the course of 24 weeks (Nutr Metab [Lond]. 2008 Dec 19. doi:10.1186/1743-7075-5-36). Between baseline and week 24, the mean HbA1c fell from 8.8% to 7.3% in the very-low-carbohydrate diet group, and from 8.3% to 7.8% in the low–glycemic diet group, for a between-group comparison P value of .03. In addition, 95% of patients in the low-carbohydrate diet group were able to reduce or eliminate the number of medications they were taking, compared with 62% of patients in the low–glycemic diet group (P less than .01).
Dr. Hallberg and colleagues are currently in year 4 of the 5-year Indiana Type 2 Diabetes Reversal Study, a prospective, nonrandomized, controlled trial of carbohydrate restriction in 465 patients, making it the largest and longest study of its kind. Of the 465 patients, 387 are in the continuous-care arm, which consists of a diet from Virta Health based on principles of nutritional ketosis, and 87 patients in a usual care arm who are followed for 2 years. The trial includes patients who have been prescribed insulin and who have been diagnosed with diabetes for an average of 8 years.
At the meeting, Dr. Hallberg presented preliminary results based on 2 years of data collection. The retention rate was 83% at 1 year and 74% at 2 years. In the treatment arm, the researchers observed that the level of beta hydroxybutyrate, or evidence of ketogenesis, was the same at 2 years as it had been at 1 year. “So, people were still following the diet, as well as being engaged,” she said.
At the end of 2 years, the mean HbA1c reduction was 0.9, the mean reduction for the Homeostatic Model Assessment of Insulin Resistance was 32%, and 55% of completers experienced reversal of their diabetes. Overall, 91% of insulin users reduced or eliminated their use of insulin, and the average weight loss was 10% of baseline weight. “Medication reduction was across the board,” she added. “This is huge from a cost-savings and a patient-satisfaction standpoint. We were improving A1c levels in patients who have had diabetes for an average of over 8 years while we were getting [them] off medication, including insulin. Low carb is now the standard of care.”
Even patients who did not experience a reversal of their diabetes were conferred a benefit. They had an average reduction of 1.2 in HbA1c level, to 7%; their average weight loss was 9.8%; 45% of patients eliminated their diabetes prescriptions; 81% reduced or eliminated their use of insulin; there was an average reduction of 27% in triglyceride levels; and they had a 17% reduction in their 10-year risk score for atherosclerotic cardiovascular disease.
In the overall cohort, the 10-year Atherosclerotic Cardiovascular Disease risk score improved by 12%; almost all markers for cardiovascular disease improved at 1 year. “We were giving these patients appropriate support, which I think is key,” Dr. Hallberg said. “No matter what you do, you have to have a high-touch intervention, and supply that through technology. We do better than medication adherence. Putting patients on a carbohydrate-restricted diet with the appropriate support works for sustainability.”
Dr. Hallberg disclosed that she is an employee of Virta Health and that she is an adviser for Simply Good Foods.
EXPERT ANALYSIS FROM WCIRDC 2019
End ‘therapeutic nihilism’ in care of older diabetic patients, says expert
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
LOS ANGELES – In the opinion of Richard Pratley, MD, it’s time for diabetes treatment guidelines to evolve in light of accumulating data from cardiovascular outcome trials in type 2 diabetes.
“They have evolved for the general patient population, and this should apply to older individuals as well,” Dr. Pratley said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “My fear is, there is therapeutic nihilism, the idea that by the time someone is 75 years old, the horse is out of the barn and you’re not going to be able to impact outcomes with directed therapy. I don’t think that’s true. Our current treatment guidelines for the treatment of diabetes in older individuals remain focused on glycemic control. It’s not hyperglycemia that’s killing people; it’s heart disease and renal disease.”
According to data from the United Nations, about 12% of the global population is older than 60. By 2050, that number is expected to reach 20%, which will continue to drive an epidemic of diabetes in the near future. Dr. Pratley, medical director of AdventHealth Diabetes Institute in Orlando, pointed out that diabetes in older individuals is not a homogeneous condition. “There are many people in my clinic who had type 1 diabetes diagnosed as kids, but I also have patients who have adult-onset type 1 diabetes,” he said. “We also have type 2 patients who can be diagnosed in their 20s, 30s, or 40s, and there are people who are diagnosed in their 70s and 80s. Now we are learning that there are different subtypes of diabetes; so even type 2 diabetes is not a homogeneous condition. There are people who are more insulin resistant or have more of an insulin secretory defect, and there’s a special type of older-onset type 2 diabetes. When you consider all this in talking about diabetes treatments, about 30% of patients in the United States are diagnosed [when they are] over the age of 60, so this is an ongoing issue.”
Older adults with diabetes may have longstanding diabetes with associated microvascular and macrovascular complications, he continued, or they may have newly diagnosed diabetes with evidence of end organ complications at the time of presentation. Or, they may have newly diagnosed diabetes without evidence of complications. “Does this matter? It does,” Dr. Pratley said. “The things we worry about with all patients with diabetes are the microvascular complications, but I would argue that the macrovascular complications, particularly diabetic nephropathy, are things we should have a laser focus on, because they have high morbidity and mortality, especially in older individuals.”
There are more than 28 cardiovascular outcomes trials in patients with type 2 diabetes ongoing or completed, and involving eight classes of medications, with more than 200,000 planned participants, Dr. Pratley said. Of those participants, 90,000 are older than 65 years, and 30,000 are older than 75 years. “This is great,” he said. “Not only do these cardiovascular outcome studies give us a lot of information about the safety and efficacy of these drugs in the general population, we can now dig in to this specific patient population.” For example, in cardiovascular outcomes trials with dipeptidyl peptidase–4 (DPP-4) inhibitors, the mean age of patients was 65. About half of the patients were older than 65, and 10%-14% were older than 75.
Investigators in the SAVOR-TIMI 53 trial examined age in one of their subgroup analyses (Diabetes Care. 2015;38:1145-53). In that study with saxagliptin, among people older than 65 who received the study drug, the hazard ratio for major adverse cardiac events (MACE) was 0.92, compared with 1.15 for those younger than 65 (P value for interaction = .058). “So older people did great [on this drug],” Dr. Pratley said. “In fact, they had a bit of a decreased risk.” A similar association was seen in adults aged 75 years and older (HR, 1.01 in those younger than 75 years, vs. 0.95 in those aged 75 years and older; P value for interaction = .673). “This is telling us that saxagliptin is safe in the older population.”
In the EXAMINE trial, in which patients with type 2 diabetes who had had a recent acute coronary syndrome received either alogliptin or placebo, researchers conducted an analysis of patients older and younger than 65 (N Engl J Med. 2013;369:1327-35). They observed no significant interactions on the primary composite cardiovascular outcome in those younger than 65 (HR, 0.91) and those aged 65 and older (HR, 0.98).
Dr. Pratley noted that in cardiovascular outcome trials with sodium-glucose transporter 2 (SGLT2) inhibitors, the mean age of patients was 64, and 48%-50% of them were older than 65. In the EMPA-REG OUTCOME trial of empagliflozin, the hazard ratio for the primary cardiovascular outcome was 1.04 in patients younger than 65 and 0.71 in those aged 65 and older (P = .01; N Engl J Med, 2015;373:2117-28). “That was a significant interaction,” he said. In addition, the hazard ratio for cardiovascular death was 0.72 in those younger than 65, and 0.54 in those aged 65 and older (P = .21). “There was not a significant interaction here, but clearly there was some trending in the older patient population,” Dr. Pratley said.
In the LEADER study of liraglutide in patients with diabetes, the hazard ratio for the primary composite cardiovascular outcome was 0.87 in the overall population, 0.78 in patients younger than 60, and 0.90 in those aged 60 and older (P = 0.27; N Engl J Med. 2016;375:311-22). In a post hoc analysis that stratified LEADER patients into younger than 75 and 75 and older, the researchers observed a 31% reduction in the 75 and older population, compared with a 10% reduction in the younger population (P for interaction = .09; Ann Intern Med. 2019;170[6]:423-6). “This was driven largely by a decrease in nonfatal [myocardial infarction],” said Dr. Pratley, who was one of the study investigators. “But in patients who were 75 years and older, there was a 30% reduction in all-cause mortality in those treated with liraglutide, compared with 12% in those younger than 75 (P for interaction = .22). That interaction is not significant, but the theme here is that older populations do quite well.”
Based on such evidence, he said, In particular, SGLT2 inhibitors and certain GLP-1 receptor agonists may be associated with an additional benefit in older individuals with cardiovascular disease, “perhaps because they’re the ones at highest risk,” Dr. Pratley said. “But we need further studies to better identify those older individuals who may be at highest risk of adverse cardiovascular complications from diabetes and who might benefit from targeted therapies.”
Many questions remain unanswered in efforts to provide optimal care to older adults with diabetes. “One of the problems is being inclusive in the older patient population,” Dr. Pratley said. “We tried to do a study of frail older individuals looking at different treatments and policies. It was difficult to recruit frail older individuals, even though they routinely are treated with the drugs we study in healthier populations. We need to know how to enroll patients, and which investigators are going to do these trials. Who is going to support these trials? Pharma? The NIH?”
Then there’s the question of what appropriate outcomes are in older individuals. “I think we can agree that hemoglobin A1c is a surrogate of microvascular complications,” he said. “Do we need to be looking at outcomes like MACE, hospitalization for heart failure, death, progression of [chronic kidney disease], and perhaps cognitive function, physical function, sarcopenia, and quality of life?”
Dr. Pratley called for the development of a personalized approach to diabetes management that takes into account heterogeneity in disease pathogenesis, comorbidities, and patient preference.
“We need to change the focus to patient-important outcomes: dying, heart attack, strokes, and avoid therapeutic nihilism, which is still pervasive among many practitioners,” he said. “We also need to partner with primary care, because they take care of the majority of older individuals, and they need to understand how we’re evolving the goals of therapy. We need to educate them about the new guidelines and try to get them on board with some of the latest data that will help improve outcomes in our patients. We also need to understand the cost of diabetes and the cost effectiveness of interventions.”
He also recommends the development of a comprehensive evidence base for the use of drugs in older individuals. “I suggest pooled analyses within clinical development programs,” he said. “That’s been done for most development programs, but the phase 3 studies tend to enroll younger, healthier individuals. It would be good to do a meta-analysis across CVOTs [cardiovascular outcome trials] within different classes of medications.”
Dr. Pratley disclosed that all honoraria and fees he receives are directed to AdventHealth. These include serving on the advisory board or as consultant to AstraZeneca, GlaxoSmithKline, Glytec, Janssen, Ligand, Lilly, Merck, Mundipharma, Novo Nordisk, and Sanofi. He also has served as a speaker for AstraZeneca and Novo Nordisk, and has received research support from Lexicon, Ligand, Lilly, Merck, Novo Nordisk, and Sanofi. He receives no direct or indirect compensation.
EXPERT ANALYSIS FROM WCIRDC 2019
ENGAGE AF-TIMI: Insulin linked to greater risk for stroke, CV death, bleeding
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
REPORTING FROM THE WCIRDC 2019
Clinic goes to bat for bullied kids
NEW ORLEANS – After Massachusetts passed antibullying legislation in 2009, Peter C. Raffalli, MD, saw an opportunity to improve care for the increasing numbers of children presenting to his neurology practice at Boston Children’s Hospital who were victims of bullying – especially those with developmental disabilities.
“I had been thinking of a clinic to help kids with these issues, aside from just helping them deal with the fallout: the depression, anxiety, et cetera, that comes with being bullied,” Dr. Raffalli recalled at the annual meeting of the American Academy of Pediatrics. “I wanted to do something to help present to families the evidence-based strategies regarding bullying prevention, detection, and intervention that might help to stop the bullying.”
This led him to launch the Bullying and Cyberbullying Prevention and Advocacy Collaborative (BACPAC) at Boston Children’s Hospital, which began in 2009 as an educational resource for families, medical colleagues, and schools. Dr. Raffalli also formed an alliance with the Massachusetts Aggression Reduction Center at Bridgewater State University (Ann Neurol. 2016;79[2]:167-8).
Two years later in 2011, BACPAC became a formal clinic at Boston Children’s that serves as a subspecialty consult service for victims of bullying and their families. The clinic team consists of a child neurologist, a social worker, and an education resource specialist who meet with the bullying victim and his/her family in initial consultation for 90 minutes. The goal is to develop an evidence-based plan for bullying prevention, detection, and intervention that is individualized to the patient’s developmental and social needs.
“We tell families that bullying is recognized medically and legally as a form of abuse,” said Dr. Raffalli. “The medical and psychological consequences are similar to other forms of abuse. You’d be surprised how often patients do think the bullying is their fault.”
The extent of the problem
Researchers estimate that 25%-30% of children will experience some form of bullying between kindergarten and grade 12, and about 8% will engage in bullying themselves. When BACPAC began in 2009, Dr. Raffalli conducted an informal search of peer-reviewed literature on bullying in children with special needs; it yielded just four articles. “Since then, there’s been an exponential explosion of literature on various aspects of bullying,” he said. Now there is ample evidence in the peer-reviewed literature to show the increased risk for bullying/cyberbullying in children/teens, not just with neurodevelopmental disorders, but also for kids with other medical disorders such as obesity, asthma, and allergies.
“We’ve had a good number of kids over the years with peanut allergy who were literally threatened physically with peanut butter at school,” he said. “It’s incredible how callous some kids can be. Kids with oppositional defiant disorder, impulse control disorder, and callous/unemotional traits from a psychological standpoint are hardest to reach when it comes to getting them to stop bullying. You’d be surprised how frequently bullies use the phrase [to their victims], ‘You should kill yourself.’ They don’t realize the damage they’re doing to people. Bullying can lead to severe psychological but also long-term medical problems, including suicidal ideation.”
Published studies show that the highest incidences of bullying occur in children with neurodevelopmental conditions such as ADHD, autistic spectrum disorders, Tourette syndrome, and other learning disabilities (Eur J Spec Needs Ed. 2010;25[1]:77-91). This population of children is overrepresented in bullying “because the services they receive at school make their disabilities more visible,” explained Dr. Raffalli, who is also an assistant professor of neurology at Harvard Medical School, Boston. “They stand out, and they have social information–processing deficits or distortions that exacerbate bullying involvement. They also have difficulty interpreting social cues or attributing hostile characteristics to their peer’s behavior.”
The consequences of bullying
The psychological and educational consequences of bullying among children in general include being more likely to develop depression, loneliness, low self-esteem, alcohol and drug abuse, sleeping difficulties, self-harm, and suicidal ideation and attempts. “We’re social creatures, and when we don’t have those social connections, we get very depressed.”
Bullying victims also are more likely to develop school avoidance and absence, decreased school performance, poor concentration, high anxiety, and social withdrawal – all of which limit their opportunities to learn. “The No. 1 thing you can do to help these kids is to believe their story – to explain to them that it’s not their fault, and to explain that you are there for them and that you support them,” he said. “When a kid gets the feeling that someone is willing to listen to them and believe them, it does an enormous good for their emotional state.”
Dr. Raffalli added that a toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity – such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship – without adequate adult support. This kind of prolonged activation of the stress response systems can disrupt the development of brain architecture and other organ systems, and increase the risk for stress-related disease and cognitive impairment well into the adult years.
In the Harvard Review of Psychiatry, researchers set out to investigate what’s known about the long-term health effects of childhood bullying. They found that bullying can induce “aspects of the stress response, via epigenetic, inflammatory, and metabolic mediators [that] have the capacity to compromise mental and physical health, and to increase the risk of disease.” The researchers advised clinicians who care for children to assess the mental and physical health effects of bullying (Harv Rev Psychiatry. 2017;25[2]:89-95).
Additional vulnerabilities for bullying victims include parents and children whose primary language is not English, as well as parents with mental illness or substance abuse and families living in poverty. “We have to keep in mind how much additional stress they may be dealing with. This can make it harder for them to cope. Bullies also are shown to be at higher risk for psychological and legal trouble into adulthood, so we should be trying to help them too. We have to keep in mind that these are all developing kids.”
Cyberbullying
In Dr. Raffalli’s clinical experience, cyberbullying has become the bully’s weapon of choice. “I call it the stealth bomber of bullying,” he said. “Cyberbullying can start as early as the second or third grade. Most parents are not giving phones to second-graders. I’m worried that it’s going to get worse, though, with the excuse that ‘I feel safer if they have a cell phone so they can call me.’ I tell parents that they still make flip phones. You don’t have to get a smartphone for a second- or third-grader, or even for a sixth-grader.”
By the time kids reach fourth and fifth grade, he continued, they begin to form their opinion “about what they believe is cool and not cool, and they begin to get into cliques that have similar beliefs, and support each other, and may break off from old friends.” He added that, while adult predation “makes the news and is certainly something we should all be concerned about, the incidence of being harassed and bullied by someone in your own age group at school is actually much higher and still has serious outcomes, including the possibility of death.”
The Massachusetts antibullying law stipulates that all teachers and all school personnel have to participate in mandatory bullying training. Schools also are required to draft and follow a bullying investigative protocol.
“Apparently the schools have all done this, yet the number of times that schools use interventions that are not advisable, such as mediation, is incredible to me,” Dr. Raffalli said. “Bringing the bully and the victim together for a ‘cup of coffee and a handshake’ is not advisable. Mediation has been shown in a number of studies to be detrimental in bullying situations. Things can easily get worse.”
Often, family members who bring their child to the BACPAC “feel that their child’s school is not helping them,” he said. “We should try to figure out why those schools are having such a hard time and see if we can help them.”
Dr. Raffalli reported having no financial disclosures.
NEW ORLEANS – After Massachusetts passed antibullying legislation in 2009, Peter C. Raffalli, MD, saw an opportunity to improve care for the increasing numbers of children presenting to his neurology practice at Boston Children’s Hospital who were victims of bullying – especially those with developmental disabilities.
“I had been thinking of a clinic to help kids with these issues, aside from just helping them deal with the fallout: the depression, anxiety, et cetera, that comes with being bullied,” Dr. Raffalli recalled at the annual meeting of the American Academy of Pediatrics. “I wanted to do something to help present to families the evidence-based strategies regarding bullying prevention, detection, and intervention that might help to stop the bullying.”
This led him to launch the Bullying and Cyberbullying Prevention and Advocacy Collaborative (BACPAC) at Boston Children’s Hospital, which began in 2009 as an educational resource for families, medical colleagues, and schools. Dr. Raffalli also formed an alliance with the Massachusetts Aggression Reduction Center at Bridgewater State University (Ann Neurol. 2016;79[2]:167-8).
Two years later in 2011, BACPAC became a formal clinic at Boston Children’s that serves as a subspecialty consult service for victims of bullying and their families. The clinic team consists of a child neurologist, a social worker, and an education resource specialist who meet with the bullying victim and his/her family in initial consultation for 90 minutes. The goal is to develop an evidence-based plan for bullying prevention, detection, and intervention that is individualized to the patient’s developmental and social needs.
“We tell families that bullying is recognized medically and legally as a form of abuse,” said Dr. Raffalli. “The medical and psychological consequences are similar to other forms of abuse. You’d be surprised how often patients do think the bullying is their fault.”
The extent of the problem
Researchers estimate that 25%-30% of children will experience some form of bullying between kindergarten and grade 12, and about 8% will engage in bullying themselves. When BACPAC began in 2009, Dr. Raffalli conducted an informal search of peer-reviewed literature on bullying in children with special needs; it yielded just four articles. “Since then, there’s been an exponential explosion of literature on various aspects of bullying,” he said. Now there is ample evidence in the peer-reviewed literature to show the increased risk for bullying/cyberbullying in children/teens, not just with neurodevelopmental disorders, but also for kids with other medical disorders such as obesity, asthma, and allergies.
“We’ve had a good number of kids over the years with peanut allergy who were literally threatened physically with peanut butter at school,” he said. “It’s incredible how callous some kids can be. Kids with oppositional defiant disorder, impulse control disorder, and callous/unemotional traits from a psychological standpoint are hardest to reach when it comes to getting them to stop bullying. You’d be surprised how frequently bullies use the phrase [to their victims], ‘You should kill yourself.’ They don’t realize the damage they’re doing to people. Bullying can lead to severe psychological but also long-term medical problems, including suicidal ideation.”
Published studies show that the highest incidences of bullying occur in children with neurodevelopmental conditions such as ADHD, autistic spectrum disorders, Tourette syndrome, and other learning disabilities (Eur J Spec Needs Ed. 2010;25[1]:77-91). This population of children is overrepresented in bullying “because the services they receive at school make their disabilities more visible,” explained Dr. Raffalli, who is also an assistant professor of neurology at Harvard Medical School, Boston. “They stand out, and they have social information–processing deficits or distortions that exacerbate bullying involvement. They also have difficulty interpreting social cues or attributing hostile characteristics to their peer’s behavior.”
The consequences of bullying
The psychological and educational consequences of bullying among children in general include being more likely to develop depression, loneliness, low self-esteem, alcohol and drug abuse, sleeping difficulties, self-harm, and suicidal ideation and attempts. “We’re social creatures, and when we don’t have those social connections, we get very depressed.”
Bullying victims also are more likely to develop school avoidance and absence, decreased school performance, poor concentration, high anxiety, and social withdrawal – all of which limit their opportunities to learn. “The No. 1 thing you can do to help these kids is to believe their story – to explain to them that it’s not their fault, and to explain that you are there for them and that you support them,” he said. “When a kid gets the feeling that someone is willing to listen to them and believe them, it does an enormous good for their emotional state.”
Dr. Raffalli added that a toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity – such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship – without adequate adult support. This kind of prolonged activation of the stress response systems can disrupt the development of brain architecture and other organ systems, and increase the risk for stress-related disease and cognitive impairment well into the adult years.
In the Harvard Review of Psychiatry, researchers set out to investigate what’s known about the long-term health effects of childhood bullying. They found that bullying can induce “aspects of the stress response, via epigenetic, inflammatory, and metabolic mediators [that] have the capacity to compromise mental and physical health, and to increase the risk of disease.” The researchers advised clinicians who care for children to assess the mental and physical health effects of bullying (Harv Rev Psychiatry. 2017;25[2]:89-95).
Additional vulnerabilities for bullying victims include parents and children whose primary language is not English, as well as parents with mental illness or substance abuse and families living in poverty. “We have to keep in mind how much additional stress they may be dealing with. This can make it harder for them to cope. Bullies also are shown to be at higher risk for psychological and legal trouble into adulthood, so we should be trying to help them too. We have to keep in mind that these are all developing kids.”
Cyberbullying
In Dr. Raffalli’s clinical experience, cyberbullying has become the bully’s weapon of choice. “I call it the stealth bomber of bullying,” he said. “Cyberbullying can start as early as the second or third grade. Most parents are not giving phones to second-graders. I’m worried that it’s going to get worse, though, with the excuse that ‘I feel safer if they have a cell phone so they can call me.’ I tell parents that they still make flip phones. You don’t have to get a smartphone for a second- or third-grader, or even for a sixth-grader.”
By the time kids reach fourth and fifth grade, he continued, they begin to form their opinion “about what they believe is cool and not cool, and they begin to get into cliques that have similar beliefs, and support each other, and may break off from old friends.” He added that, while adult predation “makes the news and is certainly something we should all be concerned about, the incidence of being harassed and bullied by someone in your own age group at school is actually much higher and still has serious outcomes, including the possibility of death.”
The Massachusetts antibullying law stipulates that all teachers and all school personnel have to participate in mandatory bullying training. Schools also are required to draft and follow a bullying investigative protocol.
“Apparently the schools have all done this, yet the number of times that schools use interventions that are not advisable, such as mediation, is incredible to me,” Dr. Raffalli said. “Bringing the bully and the victim together for a ‘cup of coffee and a handshake’ is not advisable. Mediation has been shown in a number of studies to be detrimental in bullying situations. Things can easily get worse.”
Often, family members who bring their child to the BACPAC “feel that their child’s school is not helping them,” he said. “We should try to figure out why those schools are having such a hard time and see if we can help them.”
Dr. Raffalli reported having no financial disclosures.
NEW ORLEANS – After Massachusetts passed antibullying legislation in 2009, Peter C. Raffalli, MD, saw an opportunity to improve care for the increasing numbers of children presenting to his neurology practice at Boston Children’s Hospital who were victims of bullying – especially those with developmental disabilities.
“I had been thinking of a clinic to help kids with these issues, aside from just helping them deal with the fallout: the depression, anxiety, et cetera, that comes with being bullied,” Dr. Raffalli recalled at the annual meeting of the American Academy of Pediatrics. “I wanted to do something to help present to families the evidence-based strategies regarding bullying prevention, detection, and intervention that might help to stop the bullying.”
This led him to launch the Bullying and Cyberbullying Prevention and Advocacy Collaborative (BACPAC) at Boston Children’s Hospital, which began in 2009 as an educational resource for families, medical colleagues, and schools. Dr. Raffalli also formed an alliance with the Massachusetts Aggression Reduction Center at Bridgewater State University (Ann Neurol. 2016;79[2]:167-8).
Two years later in 2011, BACPAC became a formal clinic at Boston Children’s that serves as a subspecialty consult service for victims of bullying and their families. The clinic team consists of a child neurologist, a social worker, and an education resource specialist who meet with the bullying victim and his/her family in initial consultation for 90 minutes. The goal is to develop an evidence-based plan for bullying prevention, detection, and intervention that is individualized to the patient’s developmental and social needs.
“We tell families that bullying is recognized medically and legally as a form of abuse,” said Dr. Raffalli. “The medical and psychological consequences are similar to other forms of abuse. You’d be surprised how often patients do think the bullying is their fault.”
The extent of the problem
Researchers estimate that 25%-30% of children will experience some form of bullying between kindergarten and grade 12, and about 8% will engage in bullying themselves. When BACPAC began in 2009, Dr. Raffalli conducted an informal search of peer-reviewed literature on bullying in children with special needs; it yielded just four articles. “Since then, there’s been an exponential explosion of literature on various aspects of bullying,” he said. Now there is ample evidence in the peer-reviewed literature to show the increased risk for bullying/cyberbullying in children/teens, not just with neurodevelopmental disorders, but also for kids with other medical disorders such as obesity, asthma, and allergies.
“We’ve had a good number of kids over the years with peanut allergy who were literally threatened physically with peanut butter at school,” he said. “It’s incredible how callous some kids can be. Kids with oppositional defiant disorder, impulse control disorder, and callous/unemotional traits from a psychological standpoint are hardest to reach when it comes to getting them to stop bullying. You’d be surprised how frequently bullies use the phrase [to their victims], ‘You should kill yourself.’ They don’t realize the damage they’re doing to people. Bullying can lead to severe psychological but also long-term medical problems, including suicidal ideation.”
Published studies show that the highest incidences of bullying occur in children with neurodevelopmental conditions such as ADHD, autistic spectrum disorders, Tourette syndrome, and other learning disabilities (Eur J Spec Needs Ed. 2010;25[1]:77-91). This population of children is overrepresented in bullying “because the services they receive at school make their disabilities more visible,” explained Dr. Raffalli, who is also an assistant professor of neurology at Harvard Medical School, Boston. “They stand out, and they have social information–processing deficits or distortions that exacerbate bullying involvement. They also have difficulty interpreting social cues or attributing hostile characteristics to their peer’s behavior.”
The consequences of bullying
The psychological and educational consequences of bullying among children in general include being more likely to develop depression, loneliness, low self-esteem, alcohol and drug abuse, sleeping difficulties, self-harm, and suicidal ideation and attempts. “We’re social creatures, and when we don’t have those social connections, we get very depressed.”
Bullying victims also are more likely to develop school avoidance and absence, decreased school performance, poor concentration, high anxiety, and social withdrawal – all of which limit their opportunities to learn. “The No. 1 thing you can do to help these kids is to believe their story – to explain to them that it’s not their fault, and to explain that you are there for them and that you support them,” he said. “When a kid gets the feeling that someone is willing to listen to them and believe them, it does an enormous good for their emotional state.”
Dr. Raffalli added that a toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity – such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship – without adequate adult support. This kind of prolonged activation of the stress response systems can disrupt the development of brain architecture and other organ systems, and increase the risk for stress-related disease and cognitive impairment well into the adult years.
In the Harvard Review of Psychiatry, researchers set out to investigate what’s known about the long-term health effects of childhood bullying. They found that bullying can induce “aspects of the stress response, via epigenetic, inflammatory, and metabolic mediators [that] have the capacity to compromise mental and physical health, and to increase the risk of disease.” The researchers advised clinicians who care for children to assess the mental and physical health effects of bullying (Harv Rev Psychiatry. 2017;25[2]:89-95).
Additional vulnerabilities for bullying victims include parents and children whose primary language is not English, as well as parents with mental illness or substance abuse and families living in poverty. “We have to keep in mind how much additional stress they may be dealing with. This can make it harder for them to cope. Bullies also are shown to be at higher risk for psychological and legal trouble into adulthood, so we should be trying to help them too. We have to keep in mind that these are all developing kids.”
Cyberbullying
In Dr. Raffalli’s clinical experience, cyberbullying has become the bully’s weapon of choice. “I call it the stealth bomber of bullying,” he said. “Cyberbullying can start as early as the second or third grade. Most parents are not giving phones to second-graders. I’m worried that it’s going to get worse, though, with the excuse that ‘I feel safer if they have a cell phone so they can call me.’ I tell parents that they still make flip phones. You don’t have to get a smartphone for a second- or third-grader, or even for a sixth-grader.”
By the time kids reach fourth and fifth grade, he continued, they begin to form their opinion “about what they believe is cool and not cool, and they begin to get into cliques that have similar beliefs, and support each other, and may break off from old friends.” He added that, while adult predation “makes the news and is certainly something we should all be concerned about, the incidence of being harassed and bullied by someone in your own age group at school is actually much higher and still has serious outcomes, including the possibility of death.”
The Massachusetts antibullying law stipulates that all teachers and all school personnel have to participate in mandatory bullying training. Schools also are required to draft and follow a bullying investigative protocol.
“Apparently the schools have all done this, yet the number of times that schools use interventions that are not advisable, such as mediation, is incredible to me,” Dr. Raffalli said. “Bringing the bully and the victim together for a ‘cup of coffee and a handshake’ is not advisable. Mediation has been shown in a number of studies to be detrimental in bullying situations. Things can easily get worse.”
Often, family members who bring their child to the BACPAC “feel that their child’s school is not helping them,” he said. “We should try to figure out why those schools are having such a hard time and see if we can help them.”
Dr. Raffalli reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2019