User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Shift in approach is encouraged in assessing chronic pain
In many cases, dietary interventions can lead to less inflammation
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
In many cases, dietary interventions can lead to less inflammation
In many cases, dietary interventions can lead to less inflammation
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
REPORTING FROM A NATURAL SUPPLEMENTS UPDATE
Data emerging to support personalized nutrition in oncology
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
REPORTING FROM A NATURAL SUPPLEMENTS UPDATE
Remdesivir under study as treatment for novel coronavirus
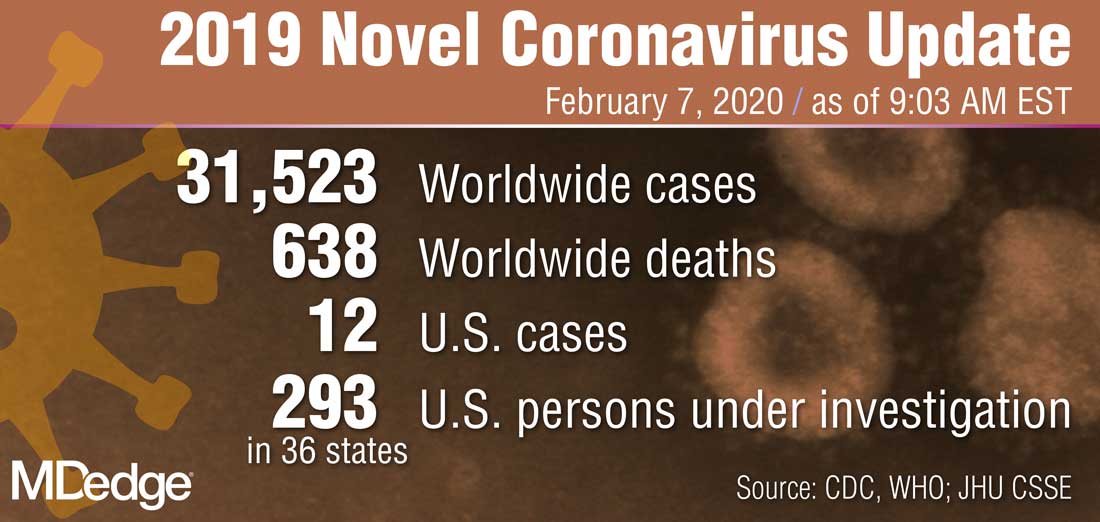
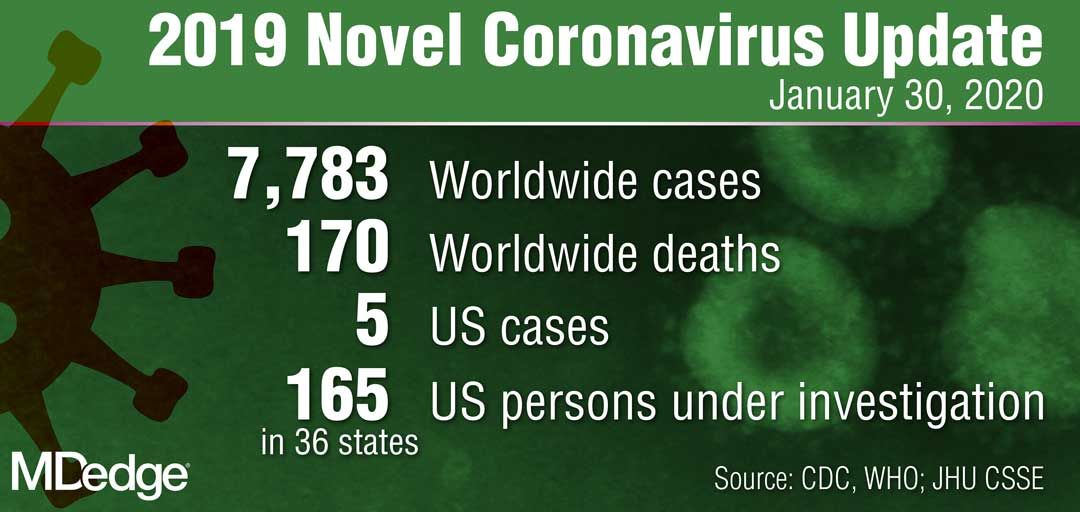
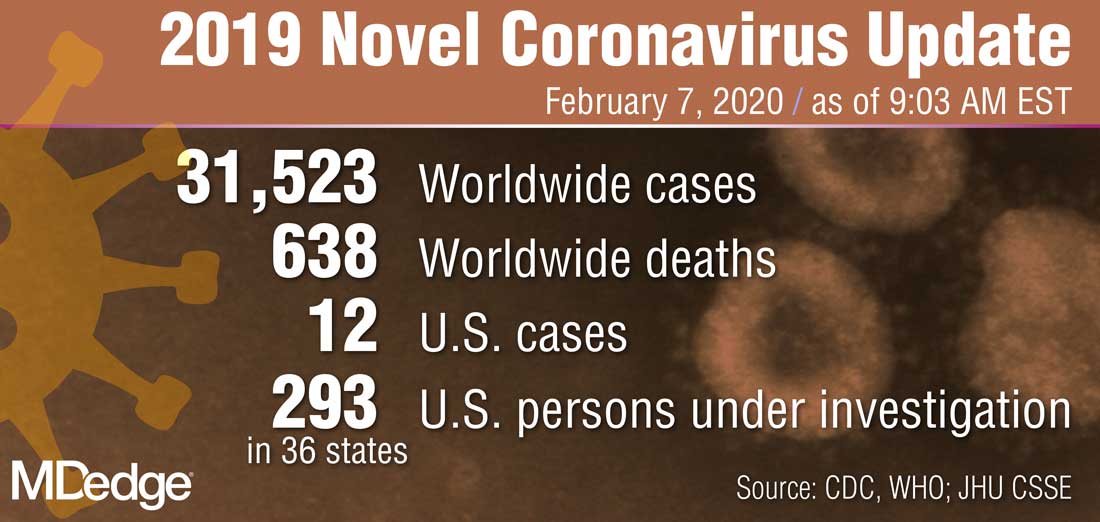
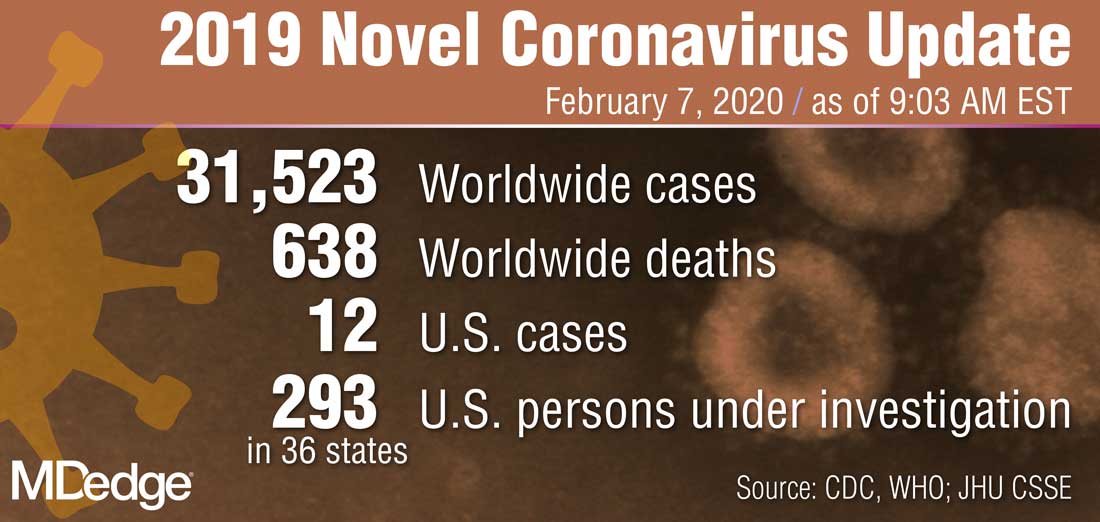
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
“What they’re looking at is the effect of this drug -- either the drug plus standard of care versus standard of care alone,” Anthony S. Fauci, MD, reported Feb. 7 during a press briefing held by members of President Trump’s Coronavirus Task Force. “I think pretty soon we are going to get a definitive answer, whether one of these among several drugs works.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases, added that several organizations and individual investigators are developing vaccines for 2019-nCoV. In one such effort, the National Institutes of Health is working with Moderna Inc. to develop a vaccine built on a messenger RNA platform. “One of the first steps is to successfully get that [novel coronavirus] gene and insert it into the messenger RNA platform successfully and allow it to express proteins,” Dr. Fauci explained. “We’ve succeeded in that. The next [step] is to put it in a mouse animal model to induce immunogenicity, and to get the company to make [gold nanoparticle] products. All of those have been successfully implemented. There have been no glitches so far. If that continues, we will be in Phase 1 trials in people within the next two-and-a-half months.”
In another development on the same day, Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, announced that Heath & Human Services issued an interim final rule to amend foreign quarantine regulations in the wake of the public health threat posed by the 2019-nCoV. “This will enable CDC to collect certain contact information data regarding airline passengers and crew when they arrive from other countries. . .and may be exposed to communicable disease,” Dr. Redfield said. “This action is part of our multi-layered approach to the U.S. response and demonstrates our commitment to take all necessary actions to protect the American people.”
According to Alex Azar, secretary of Health and Human Services, and chair of President Trump’s Coronavirus Task Force, there are 12 confirmed cases of the novel coronavirus in the United States, including two cases of transmission to people who had not recently been in China. “Although the virus represents a potentially very serious public health threat, and we expect to continue seeing more cases here, the immediate risk to the American public is low at this time,” Mr. Azar said. “We are working as quickly as possible on the many unanswered questions about this virus. That includes exactly how it spreads, how deadly it is, whether it’s commonly transmitted by patients who are not yet displaying symptoms, and other issues.”
NASH ‘an epidemic of the 21st century’
LOS ANGELES – The way Christos S. Mantzoros, MD, DSc, PhD, sees it, nonalcoholic steatohepatitis (NASH) is an epidemic of the 21st century that can trigger a cascade of reactions.
“If more than 5.8% of fat is in the liver, we call it nonalcoholic fatty liver disease [NAFLD],” Dr. Mantzoros, professor of medicine at Harvard Medical School, Boston, and Boston University, explained at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “If inflammation develops to remove the fat, we call it NASH. If this progresses to decompensated reaction and fibrosis and cirrhosis, then we call it nonalcoholic steatohepatitis with fibrosis. That can lead to liver cirrhosis, hepatocellular carcinoma, and liver failure.”
The underlying problem stems from the rise in obesity prevalence, according to Dr. Mantzoros, who is also chief of endocrinology at the Boston Veterans Affairs Healthcare System. For 75%-80% of individuals with metabolically unhealthy obesity, the storage space in their adipose tissue is exceeded. “Fat is deposited into muscle, causing insulin resistance, and into the liver,” he explained. “If it’s more than 5.8%, it causes NAFLD. Most of us don’t realize that most of the patients with diabetes we have in our clinics also have nonalcoholic fatty liver disease. That’s because we don’t have an easy diagnostic tool or an easy treatment. It’s an unmet clinical need.” (There are currently no drugs approved for the treatment of NASH or NAFLD. Current recommended first-line treatment is weight loss through diet and exercise and control of diabetes, if it is present.)
“Assuming the rate of increase in cost due to NAFLD parallels the growth in obesity, the 10-year projection for direct cost is $1.005 trillion,” said Dr. Mantzoros, who is also editor in chief of the journal Metabolism. “Obesity, NAFLD, and insulin resistance are each independently associated with a twofold risk for diabetes. If all three are present, there is a 14-fold risk for diabetes. Insulin resistance promotes an increase in free fatty acid traffic to the liver, which can trigger hepatic lipotoxicity. Hyperinsulinemia enhances free fatty acid uptake and activates de novo lipogenesis. Hyperglycemia can also activate de novo lipogenesis.”
About 85 million Americans have NAFLD, he continued. Most (80%) are cases of steatosis, but 20% have NASH. Of those, 20% develop advanced fibrosis, which leads to liver failure and transplantation or death. A study of data from the National Health and Nutrition Examination Survey found that (odds ratio, 18.20), followed by a body mass index of 30 kg/m2 or greater (OR, 9.10), hypertension (OR, 1.20), and age (OR, 1.08; Ailment Pharmacol Ther. 2017;46:974-80). “Most of the patients who come to our clinics with diabetes have nonalcoholic fatty liver disease – 75%-80% in our clinics, and about 10% have advanced fibrosis,” Dr. Mantzoros said. “Most of them go undiagnosed.”
Patients with type 2 diabetes and NAFLD progress faster to fibrosis and end-stage liver disease, compared with those who do not have diabetes. One study of 108 patients with biopsy-proven NALFD showed that 84% of those with fibrosis progression had type 2 diabetes (J Hepatol. 2015;62:1148-55). Other findings have shown that patients with type 2 diabetes are at increased risk of chronic NAFLD and hepatocellular carcinoma (Gastroenterol. 2001;126:460-8). “We are doing more liver transplantations because of NAFLD and NASH than because of hepatitis C,” Dr. Mantzoros said. “What we need to keep in mind is that, although liver morbidity and mortality is important, this is a component of the cardiometabolic syndrome. So, people have all the risk factors for cardiovascular disease. Because CVD is much more common, people with NAFLD suffer from and die from CVD. The more advanced the NAFLD, the higher the risk of death from cardiovascular disease.”
Multiple risk factors can help identify patients with advanced fibrosis because of NASH, he continued, including having features of the metabolic syndrome, being over 50 years of age, being Hispanic, having high levels of ALT/AST, low platelets, and having low albumin. “These are frequent tests that we can find in the EMR,” Dr. Mantzoros said. “The problem with ALT is that, in many stages of the disease, ALT goes up. But after a certain stage of the disease, when most of the liver is controlled by fibrosis and cirrhosis, most of the hepatocytes are dead and don’t secrete ALT, so ALT in end-stage renal disease goes up.”
Recent guidelines recognize the association between diabetes, NAFLD, and NASH, and call for increased vigilance and screening tests. According to guidelines from the American Association for the Study of Liver Diseases, the Fibrosis-4 Index or the NAFLD Fibrosis Score are clinically useful tools for identifying NAFLD in patients with higher likelihood of having bridging fibrosis or cirrhosis (Hepatology. 2018;67[1]:328-57). Vibration-controlled transient elastography or MRI are clinically useful tools for identifying advanced fibrosis in patients with NAFLD, whereas clinical decision aids, such as Fibrosis-4, NAFLD Fibrosis Score, or vibration-controlled transient elastography, can be used to identify patients at low or high risk for advanced fibrosis.
“If we have a patient with suspected NAFLD, we need to rule out alcohol use, we need to confirm NAFLD, and we need to risk stratify, and classify as low, intermediate, or high risk,” Dr. Mantzoros said. Most of his patients who meet criteria for high-risk NASH do not elect to undergo a liver biopsy. “I don’t blame them for that,” he said. “There is a 0.1 per 1,000 mortality risk, even in the best hands. If 80 million people who have fatty liver were to undergo a liver biopsy, we would have 16,000 deaths every year just because of that. We would not tolerate that.”
Recently, Dr. Mantzoros and colleagues published a proof-of-concept study that proposes novel models using lipids, hormones, and glycans that can diagnose the presence of NASH, NAFLD, or healthy status with high accuracy (Metabolism. 2019 Nov 8. doi: 10.1016/j.metabol.2019.154005). “We are now working with companies to validate it and expand it, not only as a diagnostic marker, but as a prognostic marker, and to try to commercialize it in the future,” he said.
Current pharmacotherapies are limited to patients with biopsy-confirmed NASH and fibrosis. Pioglitazone is a first-line, off-label pharmacologic treatment, while vitamin E may be used in patients with biopsy-confirmed NASH without diabetes. Metformin, glucagonlike peptide–1 receptor agonists, and sodium-glucose transporter 2 inhibitors are either not recommended or have insufficient evidence to recommend their use. More than 60 phase 2 trials are planned or ongoing, Dr. Mantzoros added, with phase trials underway for cenicriviroc, elafibranor, obeticholic acid, and selonsertib.
The role of lifestyle management is also important. “The Mediterranean diet has the best evidence, along with exercise, to improve early stages of NAFLD,” he said. “Weight loss is very important. If the patient loses 10% of their weight or more, there is NASH resolution 90% of the time. With less weight loss, we have less resolution. The problem is that only 10% of patients or less can sustain a more than 90% weight loss over a year.”
Dr. Mantzoros reported being a shareholder of Coherus BioSciences and Pangea Therapeutics, having served as an adviser to Coherus, Novo Nordisk, and Genfit and having received research grants through his institution from Coherus, Eisai, and Novo Nordisk.
LOS ANGELES – The way Christos S. Mantzoros, MD, DSc, PhD, sees it, nonalcoholic steatohepatitis (NASH) is an epidemic of the 21st century that can trigger a cascade of reactions.
“If more than 5.8% of fat is in the liver, we call it nonalcoholic fatty liver disease [NAFLD],” Dr. Mantzoros, professor of medicine at Harvard Medical School, Boston, and Boston University, explained at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “If inflammation develops to remove the fat, we call it NASH. If this progresses to decompensated reaction and fibrosis and cirrhosis, then we call it nonalcoholic steatohepatitis with fibrosis. That can lead to liver cirrhosis, hepatocellular carcinoma, and liver failure.”
The underlying problem stems from the rise in obesity prevalence, according to Dr. Mantzoros, who is also chief of endocrinology at the Boston Veterans Affairs Healthcare System. For 75%-80% of individuals with metabolically unhealthy obesity, the storage space in their adipose tissue is exceeded. “Fat is deposited into muscle, causing insulin resistance, and into the liver,” he explained. “If it’s more than 5.8%, it causes NAFLD. Most of us don’t realize that most of the patients with diabetes we have in our clinics also have nonalcoholic fatty liver disease. That’s because we don’t have an easy diagnostic tool or an easy treatment. It’s an unmet clinical need.” (There are currently no drugs approved for the treatment of NASH or NAFLD. Current recommended first-line treatment is weight loss through diet and exercise and control of diabetes, if it is present.)
“Assuming the rate of increase in cost due to NAFLD parallels the growth in obesity, the 10-year projection for direct cost is $1.005 trillion,” said Dr. Mantzoros, who is also editor in chief of the journal Metabolism. “Obesity, NAFLD, and insulin resistance are each independently associated with a twofold risk for diabetes. If all three are present, there is a 14-fold risk for diabetes. Insulin resistance promotes an increase in free fatty acid traffic to the liver, which can trigger hepatic lipotoxicity. Hyperinsulinemia enhances free fatty acid uptake and activates de novo lipogenesis. Hyperglycemia can also activate de novo lipogenesis.”
About 85 million Americans have NAFLD, he continued. Most (80%) are cases of steatosis, but 20% have NASH. Of those, 20% develop advanced fibrosis, which leads to liver failure and transplantation or death. A study of data from the National Health and Nutrition Examination Survey found that (odds ratio, 18.20), followed by a body mass index of 30 kg/m2 or greater (OR, 9.10), hypertension (OR, 1.20), and age (OR, 1.08; Ailment Pharmacol Ther. 2017;46:974-80). “Most of the patients who come to our clinics with diabetes have nonalcoholic fatty liver disease – 75%-80% in our clinics, and about 10% have advanced fibrosis,” Dr. Mantzoros said. “Most of them go undiagnosed.”
Patients with type 2 diabetes and NAFLD progress faster to fibrosis and end-stage liver disease, compared with those who do not have diabetes. One study of 108 patients with biopsy-proven NALFD showed that 84% of those with fibrosis progression had type 2 diabetes (J Hepatol. 2015;62:1148-55). Other findings have shown that patients with type 2 diabetes are at increased risk of chronic NAFLD and hepatocellular carcinoma (Gastroenterol. 2001;126:460-8). “We are doing more liver transplantations because of NAFLD and NASH than because of hepatitis C,” Dr. Mantzoros said. “What we need to keep in mind is that, although liver morbidity and mortality is important, this is a component of the cardiometabolic syndrome. So, people have all the risk factors for cardiovascular disease. Because CVD is much more common, people with NAFLD suffer from and die from CVD. The more advanced the NAFLD, the higher the risk of death from cardiovascular disease.”
Multiple risk factors can help identify patients with advanced fibrosis because of NASH, he continued, including having features of the metabolic syndrome, being over 50 years of age, being Hispanic, having high levels of ALT/AST, low platelets, and having low albumin. “These are frequent tests that we can find in the EMR,” Dr. Mantzoros said. “The problem with ALT is that, in many stages of the disease, ALT goes up. But after a certain stage of the disease, when most of the liver is controlled by fibrosis and cirrhosis, most of the hepatocytes are dead and don’t secrete ALT, so ALT in end-stage renal disease goes up.”
Recent guidelines recognize the association between diabetes, NAFLD, and NASH, and call for increased vigilance and screening tests. According to guidelines from the American Association for the Study of Liver Diseases, the Fibrosis-4 Index or the NAFLD Fibrosis Score are clinically useful tools for identifying NAFLD in patients with higher likelihood of having bridging fibrosis or cirrhosis (Hepatology. 2018;67[1]:328-57). Vibration-controlled transient elastography or MRI are clinically useful tools for identifying advanced fibrosis in patients with NAFLD, whereas clinical decision aids, such as Fibrosis-4, NAFLD Fibrosis Score, or vibration-controlled transient elastography, can be used to identify patients at low or high risk for advanced fibrosis.
“If we have a patient with suspected NAFLD, we need to rule out alcohol use, we need to confirm NAFLD, and we need to risk stratify, and classify as low, intermediate, or high risk,” Dr. Mantzoros said. Most of his patients who meet criteria for high-risk NASH do not elect to undergo a liver biopsy. “I don’t blame them for that,” he said. “There is a 0.1 per 1,000 mortality risk, even in the best hands. If 80 million people who have fatty liver were to undergo a liver biopsy, we would have 16,000 deaths every year just because of that. We would not tolerate that.”
Recently, Dr. Mantzoros and colleagues published a proof-of-concept study that proposes novel models using lipids, hormones, and glycans that can diagnose the presence of NASH, NAFLD, or healthy status with high accuracy (Metabolism. 2019 Nov 8. doi: 10.1016/j.metabol.2019.154005). “We are now working with companies to validate it and expand it, not only as a diagnostic marker, but as a prognostic marker, and to try to commercialize it in the future,” he said.
Current pharmacotherapies are limited to patients with biopsy-confirmed NASH and fibrosis. Pioglitazone is a first-line, off-label pharmacologic treatment, while vitamin E may be used in patients with biopsy-confirmed NASH without diabetes. Metformin, glucagonlike peptide–1 receptor agonists, and sodium-glucose transporter 2 inhibitors are either not recommended or have insufficient evidence to recommend their use. More than 60 phase 2 trials are planned or ongoing, Dr. Mantzoros added, with phase trials underway for cenicriviroc, elafibranor, obeticholic acid, and selonsertib.
The role of lifestyle management is also important. “The Mediterranean diet has the best evidence, along with exercise, to improve early stages of NAFLD,” he said. “Weight loss is very important. If the patient loses 10% of their weight or more, there is NASH resolution 90% of the time. With less weight loss, we have less resolution. The problem is that only 10% of patients or less can sustain a more than 90% weight loss over a year.”
Dr. Mantzoros reported being a shareholder of Coherus BioSciences and Pangea Therapeutics, having served as an adviser to Coherus, Novo Nordisk, and Genfit and having received research grants through his institution from Coherus, Eisai, and Novo Nordisk.
LOS ANGELES – The way Christos S. Mantzoros, MD, DSc, PhD, sees it, nonalcoholic steatohepatitis (NASH) is an epidemic of the 21st century that can trigger a cascade of reactions.
“If more than 5.8% of fat is in the liver, we call it nonalcoholic fatty liver disease [NAFLD],” Dr. Mantzoros, professor of medicine at Harvard Medical School, Boston, and Boston University, explained at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “If inflammation develops to remove the fat, we call it NASH. If this progresses to decompensated reaction and fibrosis and cirrhosis, then we call it nonalcoholic steatohepatitis with fibrosis. That can lead to liver cirrhosis, hepatocellular carcinoma, and liver failure.”
The underlying problem stems from the rise in obesity prevalence, according to Dr. Mantzoros, who is also chief of endocrinology at the Boston Veterans Affairs Healthcare System. For 75%-80% of individuals with metabolically unhealthy obesity, the storage space in their adipose tissue is exceeded. “Fat is deposited into muscle, causing insulin resistance, and into the liver,” he explained. “If it’s more than 5.8%, it causes NAFLD. Most of us don’t realize that most of the patients with diabetes we have in our clinics also have nonalcoholic fatty liver disease. That’s because we don’t have an easy diagnostic tool or an easy treatment. It’s an unmet clinical need.” (There are currently no drugs approved for the treatment of NASH or NAFLD. Current recommended first-line treatment is weight loss through diet and exercise and control of diabetes, if it is present.)
“Assuming the rate of increase in cost due to NAFLD parallels the growth in obesity, the 10-year projection for direct cost is $1.005 trillion,” said Dr. Mantzoros, who is also editor in chief of the journal Metabolism. “Obesity, NAFLD, and insulin resistance are each independently associated with a twofold risk for diabetes. If all three are present, there is a 14-fold risk for diabetes. Insulin resistance promotes an increase in free fatty acid traffic to the liver, which can trigger hepatic lipotoxicity. Hyperinsulinemia enhances free fatty acid uptake and activates de novo lipogenesis. Hyperglycemia can also activate de novo lipogenesis.”
About 85 million Americans have NAFLD, he continued. Most (80%) are cases of steatosis, but 20% have NASH. Of those, 20% develop advanced fibrosis, which leads to liver failure and transplantation or death. A study of data from the National Health and Nutrition Examination Survey found that (odds ratio, 18.20), followed by a body mass index of 30 kg/m2 or greater (OR, 9.10), hypertension (OR, 1.20), and age (OR, 1.08; Ailment Pharmacol Ther. 2017;46:974-80). “Most of the patients who come to our clinics with diabetes have nonalcoholic fatty liver disease – 75%-80% in our clinics, and about 10% have advanced fibrosis,” Dr. Mantzoros said. “Most of them go undiagnosed.”
Patients with type 2 diabetes and NAFLD progress faster to fibrosis and end-stage liver disease, compared with those who do not have diabetes. One study of 108 patients with biopsy-proven NALFD showed that 84% of those with fibrosis progression had type 2 diabetes (J Hepatol. 2015;62:1148-55). Other findings have shown that patients with type 2 diabetes are at increased risk of chronic NAFLD and hepatocellular carcinoma (Gastroenterol. 2001;126:460-8). “We are doing more liver transplantations because of NAFLD and NASH than because of hepatitis C,” Dr. Mantzoros said. “What we need to keep in mind is that, although liver morbidity and mortality is important, this is a component of the cardiometabolic syndrome. So, people have all the risk factors for cardiovascular disease. Because CVD is much more common, people with NAFLD suffer from and die from CVD. The more advanced the NAFLD, the higher the risk of death from cardiovascular disease.”
Multiple risk factors can help identify patients with advanced fibrosis because of NASH, he continued, including having features of the metabolic syndrome, being over 50 years of age, being Hispanic, having high levels of ALT/AST, low platelets, and having low albumin. “These are frequent tests that we can find in the EMR,” Dr. Mantzoros said. “The problem with ALT is that, in many stages of the disease, ALT goes up. But after a certain stage of the disease, when most of the liver is controlled by fibrosis and cirrhosis, most of the hepatocytes are dead and don’t secrete ALT, so ALT in end-stage renal disease goes up.”
Recent guidelines recognize the association between diabetes, NAFLD, and NASH, and call for increased vigilance and screening tests. According to guidelines from the American Association for the Study of Liver Diseases, the Fibrosis-4 Index or the NAFLD Fibrosis Score are clinically useful tools for identifying NAFLD in patients with higher likelihood of having bridging fibrosis or cirrhosis (Hepatology. 2018;67[1]:328-57). Vibration-controlled transient elastography or MRI are clinically useful tools for identifying advanced fibrosis in patients with NAFLD, whereas clinical decision aids, such as Fibrosis-4, NAFLD Fibrosis Score, or vibration-controlled transient elastography, can be used to identify patients at low or high risk for advanced fibrosis.
“If we have a patient with suspected NAFLD, we need to rule out alcohol use, we need to confirm NAFLD, and we need to risk stratify, and classify as low, intermediate, or high risk,” Dr. Mantzoros said. Most of his patients who meet criteria for high-risk NASH do not elect to undergo a liver biopsy. “I don’t blame them for that,” he said. “There is a 0.1 per 1,000 mortality risk, even in the best hands. If 80 million people who have fatty liver were to undergo a liver biopsy, we would have 16,000 deaths every year just because of that. We would not tolerate that.”
Recently, Dr. Mantzoros and colleagues published a proof-of-concept study that proposes novel models using lipids, hormones, and glycans that can diagnose the presence of NASH, NAFLD, or healthy status with high accuracy (Metabolism. 2019 Nov 8. doi: 10.1016/j.metabol.2019.154005). “We are now working with companies to validate it and expand it, not only as a diagnostic marker, but as a prognostic marker, and to try to commercialize it in the future,” he said.
Current pharmacotherapies are limited to patients with biopsy-confirmed NASH and fibrosis. Pioglitazone is a first-line, off-label pharmacologic treatment, while vitamin E may be used in patients with biopsy-confirmed NASH without diabetes. Metformin, glucagonlike peptide–1 receptor agonists, and sodium-glucose transporter 2 inhibitors are either not recommended or have insufficient evidence to recommend their use. More than 60 phase 2 trials are planned or ongoing, Dr. Mantzoros added, with phase trials underway for cenicriviroc, elafibranor, obeticholic acid, and selonsertib.
The role of lifestyle management is also important. “The Mediterranean diet has the best evidence, along with exercise, to improve early stages of NAFLD,” he said. “Weight loss is very important. If the patient loses 10% of their weight or more, there is NASH resolution 90% of the time. With less weight loss, we have less resolution. The problem is that only 10% of patients or less can sustain a more than 90% weight loss over a year.”
Dr. Mantzoros reported being a shareholder of Coherus BioSciences and Pangea Therapeutics, having served as an adviser to Coherus, Novo Nordisk, and Genfit and having received research grants through his institution from Coherus, Eisai, and Novo Nordisk.
EXPERT ANALYSIS FROM WCIRDC 2019
New Barbie lineup includes a doll with vitiligo
A new line of Barbie dolls unveiled by Mattel earlier this month includes one with vitiligo, much to the delight of clinicians who treat children and adolescents with the condition.
“When I see young children and adolescents with vitiligo, it is very common for me to feel their emotional suffering from their skin condition,” Seemal R. Desai, MD, a dermatologist at the University of Texas Southwestern Medical Center in Dallas said in an interview. “Kids can be cruel. Name calling, social ostracizing, [and] effects on self-esteem are all things I have seen amongst my patients and their families in their own struggles with vitiligo.”
According to a brand communications representative from toymaker Mattel, which began manufacturing Barbie dolls in 1959, the company worked with a board-certified dermatologist to include a doll with vitiligo in its 2020 “Fashionistas” line. “As we continue to redefine what it means to be a ‘Barbie’ or look like Barbie, offering a doll with vitiligo in our main doll line allows kids to play out even more stories they see in the world around them,” the representative wrote in an email message. Other dolls debuting as part of the lineup include one with no hair, one with a darker skin tone that uses a gold prosthetic limb, and a Ken doll with long rooted hair (think Jeff Spicoli in “Fast Times at Ridgemont High,” but about six inches longer).
Such efforts to celebrate diversity and inclusiveness go far in helping children and young adults to embrace their skin and their own identities, said Dr. Desai, the immediate past president of the Skin of Color Society and a member of the American Academy of Dermatology board of directors. “One nuance, perhaps even more important, is that the Barbie can help to break down barriers, create awareness, and potentially even reduce bullying, stigma, and lack of knowledge about vitiligo amongst the general public who don’t understand vitiligo,” he said. “I hope the public and social media will embrace this new Barbie. Who knows? Pretty soon, vitiligo may no longer be a ‘thing’ that causes ‘stares’ and ‘glares.’ ”
Referring to the Barbie with no hair in the new line of dolls, the Mattel statement said, “ if a girl is experiencing hair loss for any reason, she can see herself reflected in the line.”
In 2019, Mattel introduced a lineup of Barbie dolls reflecting permanent disabilities, including one with a prosthetic limb. For that effort, the company collaborated with then-12-year-old Jordan Reeves, the “Born Just Right” coauthor “who is on a mission to build creative solutions that help kids with disabilities, to create a play experience that is as representative as possible,” the Mattel representative wrote.
A new line of Barbie dolls unveiled by Mattel earlier this month includes one with vitiligo, much to the delight of clinicians who treat children and adolescents with the condition.
“When I see young children and adolescents with vitiligo, it is very common for me to feel their emotional suffering from their skin condition,” Seemal R. Desai, MD, a dermatologist at the University of Texas Southwestern Medical Center in Dallas said in an interview. “Kids can be cruel. Name calling, social ostracizing, [and] effects on self-esteem are all things I have seen amongst my patients and their families in their own struggles with vitiligo.”
According to a brand communications representative from toymaker Mattel, which began manufacturing Barbie dolls in 1959, the company worked with a board-certified dermatologist to include a doll with vitiligo in its 2020 “Fashionistas” line. “As we continue to redefine what it means to be a ‘Barbie’ or look like Barbie, offering a doll with vitiligo in our main doll line allows kids to play out even more stories they see in the world around them,” the representative wrote in an email message. Other dolls debuting as part of the lineup include one with no hair, one with a darker skin tone that uses a gold prosthetic limb, and a Ken doll with long rooted hair (think Jeff Spicoli in “Fast Times at Ridgemont High,” but about six inches longer).
Such efforts to celebrate diversity and inclusiveness go far in helping children and young adults to embrace their skin and their own identities, said Dr. Desai, the immediate past president of the Skin of Color Society and a member of the American Academy of Dermatology board of directors. “One nuance, perhaps even more important, is that the Barbie can help to break down barriers, create awareness, and potentially even reduce bullying, stigma, and lack of knowledge about vitiligo amongst the general public who don’t understand vitiligo,” he said. “I hope the public and social media will embrace this new Barbie. Who knows? Pretty soon, vitiligo may no longer be a ‘thing’ that causes ‘stares’ and ‘glares.’ ”
Referring to the Barbie with no hair in the new line of dolls, the Mattel statement said, “ if a girl is experiencing hair loss for any reason, she can see herself reflected in the line.”
In 2019, Mattel introduced a lineup of Barbie dolls reflecting permanent disabilities, including one with a prosthetic limb. For that effort, the company collaborated with then-12-year-old Jordan Reeves, the “Born Just Right” coauthor “who is on a mission to build creative solutions that help kids with disabilities, to create a play experience that is as representative as possible,” the Mattel representative wrote.
A new line of Barbie dolls unveiled by Mattel earlier this month includes one with vitiligo, much to the delight of clinicians who treat children and adolescents with the condition.
“When I see young children and adolescents with vitiligo, it is very common for me to feel their emotional suffering from their skin condition,” Seemal R. Desai, MD, a dermatologist at the University of Texas Southwestern Medical Center in Dallas said in an interview. “Kids can be cruel. Name calling, social ostracizing, [and] effects on self-esteem are all things I have seen amongst my patients and their families in their own struggles with vitiligo.”
According to a brand communications representative from toymaker Mattel, which began manufacturing Barbie dolls in 1959, the company worked with a board-certified dermatologist to include a doll with vitiligo in its 2020 “Fashionistas” line. “As we continue to redefine what it means to be a ‘Barbie’ or look like Barbie, offering a doll with vitiligo in our main doll line allows kids to play out even more stories they see in the world around them,” the representative wrote in an email message. Other dolls debuting as part of the lineup include one with no hair, one with a darker skin tone that uses a gold prosthetic limb, and a Ken doll with long rooted hair (think Jeff Spicoli in “Fast Times at Ridgemont High,” but about six inches longer).
Such efforts to celebrate diversity and inclusiveness go far in helping children and young adults to embrace their skin and their own identities, said Dr. Desai, the immediate past president of the Skin of Color Society and a member of the American Academy of Dermatology board of directors. “One nuance, perhaps even more important, is that the Barbie can help to break down barriers, create awareness, and potentially even reduce bullying, stigma, and lack of knowledge about vitiligo amongst the general public who don’t understand vitiligo,” he said. “I hope the public and social media will embrace this new Barbie. Who knows? Pretty soon, vitiligo may no longer be a ‘thing’ that causes ‘stares’ and ‘glares.’ ”
Referring to the Barbie with no hair in the new line of dolls, the Mattel statement said, “ if a girl is experiencing hair loss for any reason, she can see herself reflected in the line.”
In 2019, Mattel introduced a lineup of Barbie dolls reflecting permanent disabilities, including one with a prosthetic limb. For that effort, the company collaborated with then-12-year-old Jordan Reeves, the “Born Just Right” coauthor “who is on a mission to build creative solutions that help kids with disabilities, to create a play experience that is as representative as possible,” the Mattel representative wrote.
Noninjectable modes of insulin delivery coming of age
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
EXPERT ANALYSIS FROM WCIRDC 2019
HHS declares coronavirus emergency, orders quarantine
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
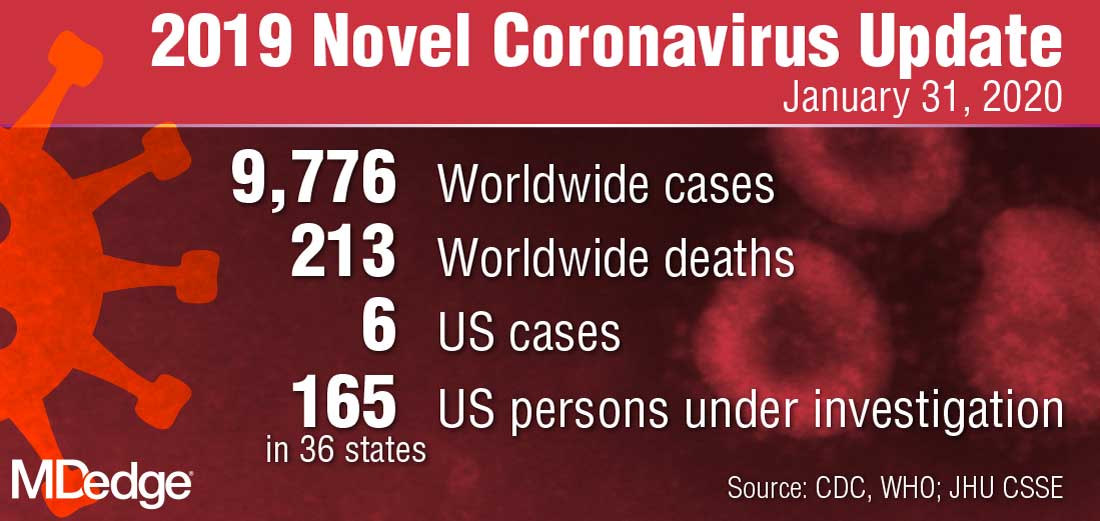
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
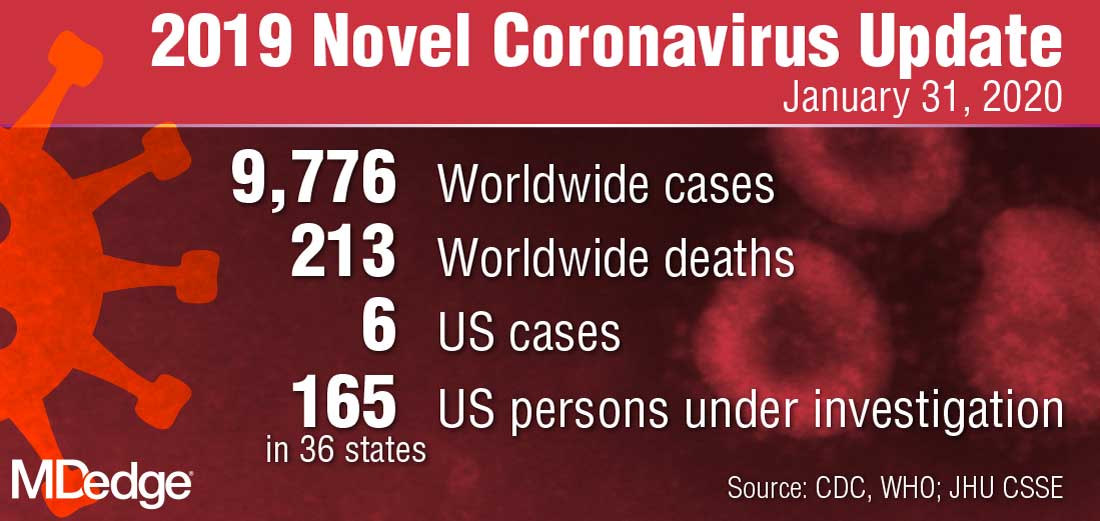
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
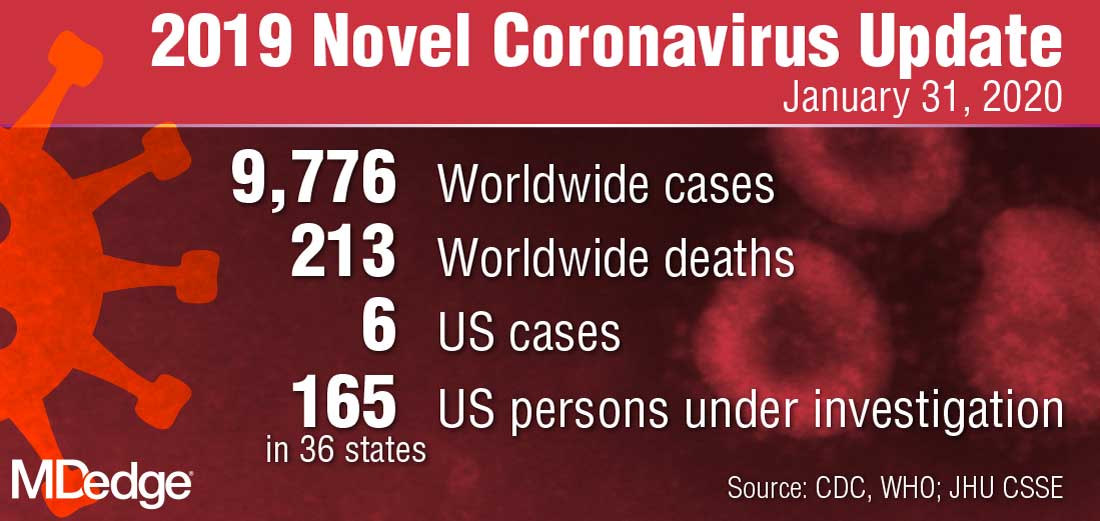
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
Menopause hormone therapy found to delay type 2 diabetes
LOS ANGELES – Although menopausal hormone therapy is not approved for the prevention of type 2 diabetes because of its complex balance of risks and benefits, it should not be withheld from women with increased risk of type 2 diabetes who seek treatment for menopausal symptoms, according to Franck Mauvais-Jarvis, MD.
“During the menopause transition, women accumulate metabolic disturbances, including visceral obesity, systemic inflammation, insulin resistance, dyslipidemia, and hypertension,” Dr. Mauvais-Jarvis, director of the Tulane Diabetes Research Program at Tulane University Health Sciences Center, New Orleans, said at the Annual World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “They also lose muscle mass. Some of these abnormalities are partially explained by chronological aging, but they are also caused by estrogen deficiency. There’s a synergism between aging and estrogen deficiency.”
The best evidence of this synergy comes from older trials. Nearly 30 years ago, researchers examined the association between postmenopausal hormone use and the subsequent incidence of non–insulin dependent diabetes in a prospective cohort of 21,028 postmenopausal U.S. women aged 30-55 years, who were enrolled in the Nurse’s Health Study and followed for 12 years (Ann Epidemiol. 1992;2[5]:665-73). They found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes. In a more recent trial, researchers examined the association between use of hormone therapy and new-onset diabetes in 63,624 postmenopausal women who were enrolled in the prospective French cohort of the Etude Epidemiologique de Femmes de la Mutuelle Générale de l’Education Nationale (E3N) and followed for 15 years (Diabetologia. 2009;52[10]:2092-100). It found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes.
In the Heart and Estrogen/Progestin Replacement Study, researchers evaluated the effect of hormone therapy on fasting glucose level and incident diabetes in 2,763 postmenopausal women with coronary heart disease (Ann Intern Med. 2003;138[1]:1-9). At 20 U.S. centers, the study participants received 0.625 mg of conjugated estrogen plus 2.5 mg of medroxyprogesterone, or placebo, and were followed for 4 years. The researchers found that the use of hormone therapy reduced the incidence of diabetes by 35%.
According to Dr. Mauvais-Jarvis, the strongest data come from the Women’s Health Initiative (WHI), a randomized, double-blind trial that compared the effect of daily 0.625 mg conjugated estrogen plus 2.5 mg medroxyprogesterone acetate with that of placebo during 5.6 years of follow-up (Diabetologia. 2004; 47[7]:1175-87). It showed a 20% decrease in the incidence of diabetes at 5 years. More recently, researchers found that, whether WHI participants took estrogen plus medroxyprogesterone or estrogen alone, the protection from diabetes was present (N Engl J Med. 2016;374:803-6).
In 2006, researchers published results from a meta-analysis of 107 trials in an effort to quantify the effects of hormone therapy on components of metabolic syndrome in postmenopausal women (Diabetes Obes Metab. 2006;8[5]:538-54). In women without diabetes, hormone therapy reduced the HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) score by 13% and incidence of type 2 diabetes by 30%. In women with diabetes, hormone therapy reduced fasting glucose by 11% and HOMA-IR by 36%.
The mechanisms by which estrogens improve glucose homeostasis are yet to be fully understood. “One of the most important [mechanisms] is a decrease in abdominal fat, which improves insulin resistance and systemic inflammation,” Dr. Mauvais-Jarvis said. “However, in the WHI, it was clear that the improvement in HOMA-IR was independent from the body weight and fat. Estrogen has also been found to increase insulin clearance and sensitivity, increase glucose disposal and effectiveness and decrease sarcopenia. There are fewer than 20 studies looking at beta-cell function. Half of them have shown that estrogen improves insulin secretion.”
Route of estrogen administration also comes into play. For example, oral estrogens increase liver exposure to estrogen, increase triglycerides, and increase clotting factors. “That is why oral estrogens are not indicated in women with risk of deep venous thrombosis,” Dr. Mauvais-Jarvis said. “They also increase inflammatory factors like C-reactive protein. Advantages are that they decrease LDL cholesterol levels and increase HDL cholesterol levels more than transdermal estrogen does.”
The main advantage with transdermal delivery of estrogen, he continued, is that it does not raise triglycerides, clotting factors, or inflammatory factors, and it confers less exposure to the liver. “That’s why it’s the preferred way of administration in women who are obese, who have a risk of DVT, or who have cardiovascular risk factors,” he said. “It has a lower suppression of hepatic glucose production, it increases circulating estradiol, and the delivery to nonhepatic tissue is increased. The oral form of estrogen is cheaper, compared with the transdermal form, though. This is a factor that is always taken into account.”
Dr. Mauvais-Jarvis and colleagues were first to evaluate the effect of conjugated estrogens plus bazedoxifene in mice (Mol Metab. 2014;3[2]:177-90). “The idea was that by combining estrogen and bazedoxifene, you have the beneficial effect of estrogen in the tissues but you block estrogen in the breast and in the uterus, and therefore, you prevent the risk of cancer,” he said. “We found that tissue-selective estrogen complexes with bazedoxifene prevent metabolic dysfunction in female mice. It increased energy expenditure and decreased fatty liver.”
In a subsequent pilot study, he and his colleagues assessed the effect of 12 weeks’ treatment with bazedoxifene/conjugated estrogens, compared with placebo, on glucose homeostasis and body composition in 12 postmenopausal women (NCT02237079). “We did not find any significant alterations in the IVGTT [Intravenous Glucose Tolerance Test] but we observed improved fasting beta-cell function and serum glucose in menopausal women with obesity,” Dr. Mauvais-Jarvis said (J Endocr Soc. 2019;3[8]:1583-94).
In a separate, randomized, double-blind, placebo-controlled, crossover trial that he and his colleagues performed in eight postmenopausal women with obesity, the primary endpoint was insulin action as measured by a two-step hyperinsulinemic-euglycemic clamp. Secondary endpoints were body composition, basal metabolic rate, ectopic fat, and metabolome. “We did not find any difference in systemic insulin action, ectopic fat, or energy expenditure,” he said. “But we found something very interesting. We did a metabolic analysis and found that oral estrogens increase hepatic de novo lipogenesis and liver triacylglycerol production. In other words, the oral estrogens were increasing [triacylglycerol] synthesis from glucose, but it does not accumulate in the liver.”
Dr. Mauvais-Jarvis disclosed that he has received research support from the National Institutes of Health, the American Diabetes Association, the Department of Veterans Affairs, and Pfizer.
LOS ANGELES – Although menopausal hormone therapy is not approved for the prevention of type 2 diabetes because of its complex balance of risks and benefits, it should not be withheld from women with increased risk of type 2 diabetes who seek treatment for menopausal symptoms, according to Franck Mauvais-Jarvis, MD.
“During the menopause transition, women accumulate metabolic disturbances, including visceral obesity, systemic inflammation, insulin resistance, dyslipidemia, and hypertension,” Dr. Mauvais-Jarvis, director of the Tulane Diabetes Research Program at Tulane University Health Sciences Center, New Orleans, said at the Annual World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “They also lose muscle mass. Some of these abnormalities are partially explained by chronological aging, but they are also caused by estrogen deficiency. There’s a synergism between aging and estrogen deficiency.”
The best evidence of this synergy comes from older trials. Nearly 30 years ago, researchers examined the association between postmenopausal hormone use and the subsequent incidence of non–insulin dependent diabetes in a prospective cohort of 21,028 postmenopausal U.S. women aged 30-55 years, who were enrolled in the Nurse’s Health Study and followed for 12 years (Ann Epidemiol. 1992;2[5]:665-73). They found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes. In a more recent trial, researchers examined the association between use of hormone therapy and new-onset diabetes in 63,624 postmenopausal women who were enrolled in the prospective French cohort of the Etude Epidemiologique de Femmes de la Mutuelle Générale de l’Education Nationale (E3N) and followed for 15 years (Diabetologia. 2009;52[10]:2092-100). It found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes.
In the Heart and Estrogen/Progestin Replacement Study, researchers evaluated the effect of hormone therapy on fasting glucose level and incident diabetes in 2,763 postmenopausal women with coronary heart disease (Ann Intern Med. 2003;138[1]:1-9). At 20 U.S. centers, the study participants received 0.625 mg of conjugated estrogen plus 2.5 mg of medroxyprogesterone, or placebo, and were followed for 4 years. The researchers found that the use of hormone therapy reduced the incidence of diabetes by 35%.
According to Dr. Mauvais-Jarvis, the strongest data come from the Women’s Health Initiative (WHI), a randomized, double-blind trial that compared the effect of daily 0.625 mg conjugated estrogen plus 2.5 mg medroxyprogesterone acetate with that of placebo during 5.6 years of follow-up (Diabetologia. 2004; 47[7]:1175-87). It showed a 20% decrease in the incidence of diabetes at 5 years. More recently, researchers found that, whether WHI participants took estrogen plus medroxyprogesterone or estrogen alone, the protection from diabetes was present (N Engl J Med. 2016;374:803-6).
In 2006, researchers published results from a meta-analysis of 107 trials in an effort to quantify the effects of hormone therapy on components of metabolic syndrome in postmenopausal women (Diabetes Obes Metab. 2006;8[5]:538-54). In women without diabetes, hormone therapy reduced the HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) score by 13% and incidence of type 2 diabetes by 30%. In women with diabetes, hormone therapy reduced fasting glucose by 11% and HOMA-IR by 36%.
The mechanisms by which estrogens improve glucose homeostasis are yet to be fully understood. “One of the most important [mechanisms] is a decrease in abdominal fat, which improves insulin resistance and systemic inflammation,” Dr. Mauvais-Jarvis said. “However, in the WHI, it was clear that the improvement in HOMA-IR was independent from the body weight and fat. Estrogen has also been found to increase insulin clearance and sensitivity, increase glucose disposal and effectiveness and decrease sarcopenia. There are fewer than 20 studies looking at beta-cell function. Half of them have shown that estrogen improves insulin secretion.”
Route of estrogen administration also comes into play. For example, oral estrogens increase liver exposure to estrogen, increase triglycerides, and increase clotting factors. “That is why oral estrogens are not indicated in women with risk of deep venous thrombosis,” Dr. Mauvais-Jarvis said. “They also increase inflammatory factors like C-reactive protein. Advantages are that they decrease LDL cholesterol levels and increase HDL cholesterol levels more than transdermal estrogen does.”
The main advantage with transdermal delivery of estrogen, he continued, is that it does not raise triglycerides, clotting factors, or inflammatory factors, and it confers less exposure to the liver. “That’s why it’s the preferred way of administration in women who are obese, who have a risk of DVT, or who have cardiovascular risk factors,” he said. “It has a lower suppression of hepatic glucose production, it increases circulating estradiol, and the delivery to nonhepatic tissue is increased. The oral form of estrogen is cheaper, compared with the transdermal form, though. This is a factor that is always taken into account.”
Dr. Mauvais-Jarvis and colleagues were first to evaluate the effect of conjugated estrogens plus bazedoxifene in mice (Mol Metab. 2014;3[2]:177-90). “The idea was that by combining estrogen and bazedoxifene, you have the beneficial effect of estrogen in the tissues but you block estrogen in the breast and in the uterus, and therefore, you prevent the risk of cancer,” he said. “We found that tissue-selective estrogen complexes with bazedoxifene prevent metabolic dysfunction in female mice. It increased energy expenditure and decreased fatty liver.”
In a subsequent pilot study, he and his colleagues assessed the effect of 12 weeks’ treatment with bazedoxifene/conjugated estrogens, compared with placebo, on glucose homeostasis and body composition in 12 postmenopausal women (NCT02237079). “We did not find any significant alterations in the IVGTT [Intravenous Glucose Tolerance Test] but we observed improved fasting beta-cell function and serum glucose in menopausal women with obesity,” Dr. Mauvais-Jarvis said (J Endocr Soc. 2019;3[8]:1583-94).
In a separate, randomized, double-blind, placebo-controlled, crossover trial that he and his colleagues performed in eight postmenopausal women with obesity, the primary endpoint was insulin action as measured by a two-step hyperinsulinemic-euglycemic clamp. Secondary endpoints were body composition, basal metabolic rate, ectopic fat, and metabolome. “We did not find any difference in systemic insulin action, ectopic fat, or energy expenditure,” he said. “But we found something very interesting. We did a metabolic analysis and found that oral estrogens increase hepatic de novo lipogenesis and liver triacylglycerol production. In other words, the oral estrogens were increasing [triacylglycerol] synthesis from glucose, but it does not accumulate in the liver.”
Dr. Mauvais-Jarvis disclosed that he has received research support from the National Institutes of Health, the American Diabetes Association, the Department of Veterans Affairs, and Pfizer.
LOS ANGELES – Although menopausal hormone therapy is not approved for the prevention of type 2 diabetes because of its complex balance of risks and benefits, it should not be withheld from women with increased risk of type 2 diabetes who seek treatment for menopausal symptoms, according to Franck Mauvais-Jarvis, MD.
“During the menopause transition, women accumulate metabolic disturbances, including visceral obesity, systemic inflammation, insulin resistance, dyslipidemia, and hypertension,” Dr. Mauvais-Jarvis, director of the Tulane Diabetes Research Program at Tulane University Health Sciences Center, New Orleans, said at the Annual World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “They also lose muscle mass. Some of these abnormalities are partially explained by chronological aging, but they are also caused by estrogen deficiency. There’s a synergism between aging and estrogen deficiency.”
The best evidence of this synergy comes from older trials. Nearly 30 years ago, researchers examined the association between postmenopausal hormone use and the subsequent incidence of non–insulin dependent diabetes in a prospective cohort of 21,028 postmenopausal U.S. women aged 30-55 years, who were enrolled in the Nurse’s Health Study and followed for 12 years (Ann Epidemiol. 1992;2[5]:665-73). They found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes. In a more recent trial, researchers examined the association between use of hormone therapy and new-onset diabetes in 63,624 postmenopausal women who were enrolled in the prospective French cohort of the Etude Epidemiologique de Femmes de la Mutuelle Générale de l’Education Nationale (E3N) and followed for 15 years (Diabetologia. 2009;52[10]:2092-100). It found that study participants on hormone therapy experienced a 20% reduction in the incidence of type 2 diabetes.
In the Heart and Estrogen/Progestin Replacement Study, researchers evaluated the effect of hormone therapy on fasting glucose level and incident diabetes in 2,763 postmenopausal women with coronary heart disease (Ann Intern Med. 2003;138[1]:1-9). At 20 U.S. centers, the study participants received 0.625 mg of conjugated estrogen plus 2.5 mg of medroxyprogesterone, or placebo, and were followed for 4 years. The researchers found that the use of hormone therapy reduced the incidence of diabetes by 35%.
According to Dr. Mauvais-Jarvis, the strongest data come from the Women’s Health Initiative (WHI), a randomized, double-blind trial that compared the effect of daily 0.625 mg conjugated estrogen plus 2.5 mg medroxyprogesterone acetate with that of placebo during 5.6 years of follow-up (Diabetologia. 2004; 47[7]:1175-87). It showed a 20% decrease in the incidence of diabetes at 5 years. More recently, researchers found that, whether WHI participants took estrogen plus medroxyprogesterone or estrogen alone, the protection from diabetes was present (N Engl J Med. 2016;374:803-6).
In 2006, researchers published results from a meta-analysis of 107 trials in an effort to quantify the effects of hormone therapy on components of metabolic syndrome in postmenopausal women (Diabetes Obes Metab. 2006;8[5]:538-54). In women without diabetes, hormone therapy reduced the HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) score by 13% and incidence of type 2 diabetes by 30%. In women with diabetes, hormone therapy reduced fasting glucose by 11% and HOMA-IR by 36%.
The mechanisms by which estrogens improve glucose homeostasis are yet to be fully understood. “One of the most important [mechanisms] is a decrease in abdominal fat, which improves insulin resistance and systemic inflammation,” Dr. Mauvais-Jarvis said. “However, in the WHI, it was clear that the improvement in HOMA-IR was independent from the body weight and fat. Estrogen has also been found to increase insulin clearance and sensitivity, increase glucose disposal and effectiveness and decrease sarcopenia. There are fewer than 20 studies looking at beta-cell function. Half of them have shown that estrogen improves insulin secretion.”
Route of estrogen administration also comes into play. For example, oral estrogens increase liver exposure to estrogen, increase triglycerides, and increase clotting factors. “That is why oral estrogens are not indicated in women with risk of deep venous thrombosis,” Dr. Mauvais-Jarvis said. “They also increase inflammatory factors like C-reactive protein. Advantages are that they decrease LDL cholesterol levels and increase HDL cholesterol levels more than transdermal estrogen does.”
The main advantage with transdermal delivery of estrogen, he continued, is that it does not raise triglycerides, clotting factors, or inflammatory factors, and it confers less exposure to the liver. “That’s why it’s the preferred way of administration in women who are obese, who have a risk of DVT, or who have cardiovascular risk factors,” he said. “It has a lower suppression of hepatic glucose production, it increases circulating estradiol, and the delivery to nonhepatic tissue is increased. The oral form of estrogen is cheaper, compared with the transdermal form, though. This is a factor that is always taken into account.”
Dr. Mauvais-Jarvis and colleagues were first to evaluate the effect of conjugated estrogens plus bazedoxifene in mice (Mol Metab. 2014;3[2]:177-90). “The idea was that by combining estrogen and bazedoxifene, you have the beneficial effect of estrogen in the tissues but you block estrogen in the breast and in the uterus, and therefore, you prevent the risk of cancer,” he said. “We found that tissue-selective estrogen complexes with bazedoxifene prevent metabolic dysfunction in female mice. It increased energy expenditure and decreased fatty liver.”
In a subsequent pilot study, he and his colleagues assessed the effect of 12 weeks’ treatment with bazedoxifene/conjugated estrogens, compared with placebo, on glucose homeostasis and body composition in 12 postmenopausal women (NCT02237079). “We did not find any significant alterations in the IVGTT [Intravenous Glucose Tolerance Test] but we observed improved fasting beta-cell function and serum glucose in menopausal women with obesity,” Dr. Mauvais-Jarvis said (J Endocr Soc. 2019;3[8]:1583-94).
In a separate, randomized, double-blind, placebo-controlled, crossover trial that he and his colleagues performed in eight postmenopausal women with obesity, the primary endpoint was insulin action as measured by a two-step hyperinsulinemic-euglycemic clamp. Secondary endpoints were body composition, basal metabolic rate, ectopic fat, and metabolome. “We did not find any difference in systemic insulin action, ectopic fat, or energy expenditure,” he said. “But we found something very interesting. We did a metabolic analysis and found that oral estrogens increase hepatic de novo lipogenesis and liver triacylglycerol production. In other words, the oral estrogens were increasing [triacylglycerol] synthesis from glucose, but it does not accumulate in the liver.”
Dr. Mauvais-Jarvis disclosed that he has received research support from the National Institutes of Health, the American Diabetes Association, the Department of Veterans Affairs, and Pfizer.
EXPERT ANALYSIS FROM THE WCIRDC 2019
CDC: First person-to-person spread of novel coronavirus in U.S.
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
CDC: Risk in U.S. from 2019-nCoV remains low
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
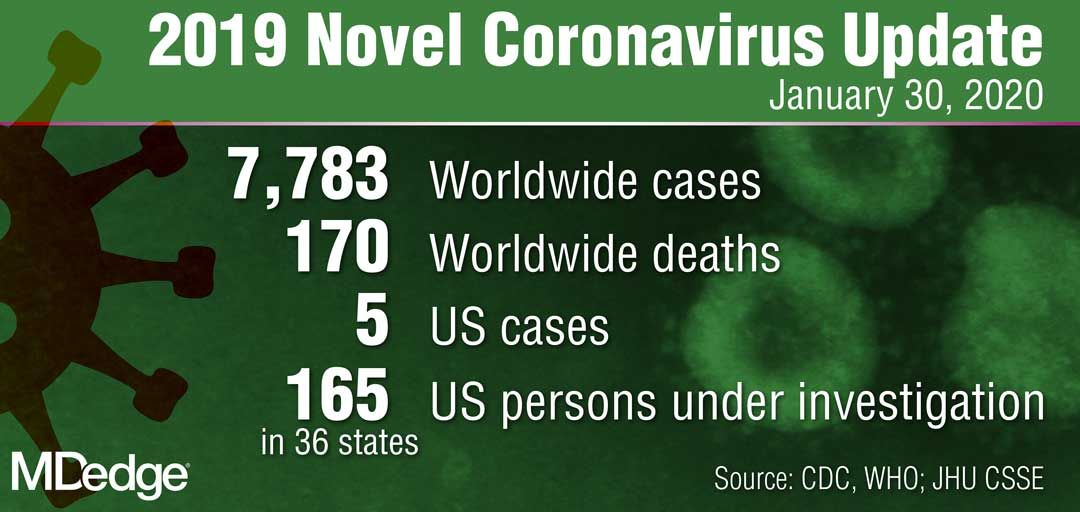
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”