User login
Assessing progression, impact of radiofrequency ablation in Barrett’s esophagus
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
FROM GASTROENTEROLOGY
Key clinical point: Barrett’s esophagus with low-grade dysplasia had a lower rate of progression to cancer than that suggested by prospective surveillance studies, but radiofrequency ablation might further cut the risk.
Major finding: About 0.2% of cases progress during the 5 years after diagnosis, and RFA might significantly decrease risk of progression (adjusted hazard ratio, 0.06).
Data source: A model of rates of progression based on population-level studies, and a multicenter retrospective study of 170 patients with Barrett’s esophagus and low-grade dysplasia.
Disclosures: The study by Dr. Small and associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest; seven coauthors reported ties with a number of pharmaceutical companies. The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest.
Gluten exposure tied to worsened GI and extraintestinal symptoms in gluten sensitivity
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Patients with self-diagnosed gluten sensitivity reported significantly worse intestinal and extraintestinal symptoms when ingesting small amounts of gluten, compared with placebo.
Major finding: Gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034).
Data source: Double-blind, placebo-controlled, crossover trial of 61 patients with self-diagnosed gluten sensitivity.
Disclosures: St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
Circulating tumor DNA marked progressive liver cancer
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The presence of circulating tumor (ct) DNA indicated progression of hepatocellular carcinoma.
Major finding: Among seven patients who tested positive for ctDNA before undergoing surgical resection, six developed recurrent HCC and four developed extrahepatic metastases.
Data source: Real-time quantitative PCR analysis of serum samples from 46 patients with HCC who underwent hepatectomy or liver transplantation.
Disclosures: The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
AAP: Give peanut products to high-risk infants to cut allergy risk
Infants at high risk for peanut allergy should start a peanut-based diet by age 4-11 months, experts from the American Academy of Pediatrics and nine other medical groups advised in the September issue of Pediatrics.*
The consensus communication upends traditional views about preventing childhood peanut allergy and highlights the landmark LEAP study in which high-risk infants fed peanut-based foods had about an 80% lower risk of developing peanut allergy, compared with those fed a peanut-free diet.
“Early intervention will prevent peanut allergy, and the pediatrician’s involvement is absolutely essential to the success of this approach,” said Dr. Hugh Sampson, who contributed to the guidance and is at the Icahn School of Medicine at Mount Sinai, New York. “Without very early evaluation and implementation, we won’t change anything.”
LEAP investigators defined “high risk” for peanut allergy as severe eczema with or without egg allergy, “but many other infants are likely at risk, and thus would benefit from early peanut introduction,” added Dr. David Fleischer, who also contributed to the guidance and is at the University of Colorado at Denver, Aurora. “Many feel that given the potential benefit, all infants, regardless of risk level, should have peanut introduced early into the diet,” he said.
Peanut allergy affects more than 2% of American children and is about twice as prevalent in Western countries as it was a decade ago. It’s not clear why rates have increased, but pediatricians can help stem the rising tide, Dr. Sampson said. “When a pediatrician suspects a ‘high-risk’ baby, he or she needs to explain to parents the risks involved in their baby developing peanut allergy, and the benefits of early evaluation and introduction. Once peanut allergy is established, the vast majority of young children will retain the allergy for life.”
Because “high-risk” children might already be allergic to peanuts, they could benefit from evaluation by an allergist, according to the consensus communication (Pediatrics 2015;136[3]:601-4). Expert consultation might also benefit those who feel reluctant to introduce peanuts for other reasons, Dr. Fleischer said.
Dr. Sampson recommends peanut-based skin prick testing for high-risk infants aged 4-8 months. Patients with a negative result should receive 2 grams of peanut protein three times a week for the next 3 years. Those who are mildly sensitive (wheal diameter less than 4 mm) should undergo a peanut challenge observed by an experienced physician. Infants who do not react can start the peanut-based diet.
The LEAP study randomized 640 high-risk infants to either avoid peanuts or consume at least 6 grams per week of the allergen in foods such as smooth peanut butter mixed with mashed fruit, peanut soup, and ground peanuts in other foods. Five-year-olds in the peanut group had significantly lower rates of peanut allergy, regardless of whether their skin prick test had been positive at baseline (N. Engl. J. Med. 2015;372[9]:803-13). While the consensus communication provides interim guidance, a panel sponsored by the National Institute of Allergy and Infectious Diseases is reviewing food allergy data in preparation for updating its guidelines, Dr. Sampson noted. “Several major questions remain,” he said. “Do we need to give such large amounts of peanut to induce tolerance? Is it necessary to give this amount of peanut for such an extended period? What happens if parents don’t give peanut to their infants on a regular basis, as done in the LEAP trial? Could this put them at higher risk? And will this approach apply to other foods?”
Another key knowledge gap is whether the results from one single-center study can be applied elsewhere, said Dr. Fleischer. “We do not know the effects of early peanut introduction in other risk populations.”
Authors of the consensus communication reported no funding sources or conflicts of interest.
*Correction, 8/31/2015: An earlier version of this article misstated the journal in which the study was published.
Infants at high risk for peanut allergy should start a peanut-based diet by age 4-11 months, experts from the American Academy of Pediatrics and nine other medical groups advised in the September issue of Pediatrics.*
The consensus communication upends traditional views about preventing childhood peanut allergy and highlights the landmark LEAP study in which high-risk infants fed peanut-based foods had about an 80% lower risk of developing peanut allergy, compared with those fed a peanut-free diet.
“Early intervention will prevent peanut allergy, and the pediatrician’s involvement is absolutely essential to the success of this approach,” said Dr. Hugh Sampson, who contributed to the guidance and is at the Icahn School of Medicine at Mount Sinai, New York. “Without very early evaluation and implementation, we won’t change anything.”
LEAP investigators defined “high risk” for peanut allergy as severe eczema with or without egg allergy, “but many other infants are likely at risk, and thus would benefit from early peanut introduction,” added Dr. David Fleischer, who also contributed to the guidance and is at the University of Colorado at Denver, Aurora. “Many feel that given the potential benefit, all infants, regardless of risk level, should have peanut introduced early into the diet,” he said.
Peanut allergy affects more than 2% of American children and is about twice as prevalent in Western countries as it was a decade ago. It’s not clear why rates have increased, but pediatricians can help stem the rising tide, Dr. Sampson said. “When a pediatrician suspects a ‘high-risk’ baby, he or she needs to explain to parents the risks involved in their baby developing peanut allergy, and the benefits of early evaluation and introduction. Once peanut allergy is established, the vast majority of young children will retain the allergy for life.”
Because “high-risk” children might already be allergic to peanuts, they could benefit from evaluation by an allergist, according to the consensus communication (Pediatrics 2015;136[3]:601-4). Expert consultation might also benefit those who feel reluctant to introduce peanuts for other reasons, Dr. Fleischer said.
Dr. Sampson recommends peanut-based skin prick testing for high-risk infants aged 4-8 months. Patients with a negative result should receive 2 grams of peanut protein three times a week for the next 3 years. Those who are mildly sensitive (wheal diameter less than 4 mm) should undergo a peanut challenge observed by an experienced physician. Infants who do not react can start the peanut-based diet.
The LEAP study randomized 640 high-risk infants to either avoid peanuts or consume at least 6 grams per week of the allergen in foods such as smooth peanut butter mixed with mashed fruit, peanut soup, and ground peanuts in other foods. Five-year-olds in the peanut group had significantly lower rates of peanut allergy, regardless of whether their skin prick test had been positive at baseline (N. Engl. J. Med. 2015;372[9]:803-13). While the consensus communication provides interim guidance, a panel sponsored by the National Institute of Allergy and Infectious Diseases is reviewing food allergy data in preparation for updating its guidelines, Dr. Sampson noted. “Several major questions remain,” he said. “Do we need to give such large amounts of peanut to induce tolerance? Is it necessary to give this amount of peanut for such an extended period? What happens if parents don’t give peanut to their infants on a regular basis, as done in the LEAP trial? Could this put them at higher risk? And will this approach apply to other foods?”
Another key knowledge gap is whether the results from one single-center study can be applied elsewhere, said Dr. Fleischer. “We do not know the effects of early peanut introduction in other risk populations.”
Authors of the consensus communication reported no funding sources or conflicts of interest.
*Correction, 8/31/2015: An earlier version of this article misstated the journal in which the study was published.
Infants at high risk for peanut allergy should start a peanut-based diet by age 4-11 months, experts from the American Academy of Pediatrics and nine other medical groups advised in the September issue of Pediatrics.*
The consensus communication upends traditional views about preventing childhood peanut allergy and highlights the landmark LEAP study in which high-risk infants fed peanut-based foods had about an 80% lower risk of developing peanut allergy, compared with those fed a peanut-free diet.
“Early intervention will prevent peanut allergy, and the pediatrician’s involvement is absolutely essential to the success of this approach,” said Dr. Hugh Sampson, who contributed to the guidance and is at the Icahn School of Medicine at Mount Sinai, New York. “Without very early evaluation and implementation, we won’t change anything.”
LEAP investigators defined “high risk” for peanut allergy as severe eczema with or without egg allergy, “but many other infants are likely at risk, and thus would benefit from early peanut introduction,” added Dr. David Fleischer, who also contributed to the guidance and is at the University of Colorado at Denver, Aurora. “Many feel that given the potential benefit, all infants, regardless of risk level, should have peanut introduced early into the diet,” he said.
Peanut allergy affects more than 2% of American children and is about twice as prevalent in Western countries as it was a decade ago. It’s not clear why rates have increased, but pediatricians can help stem the rising tide, Dr. Sampson said. “When a pediatrician suspects a ‘high-risk’ baby, he or she needs to explain to parents the risks involved in their baby developing peanut allergy, and the benefits of early evaluation and introduction. Once peanut allergy is established, the vast majority of young children will retain the allergy for life.”
Because “high-risk” children might already be allergic to peanuts, they could benefit from evaluation by an allergist, according to the consensus communication (Pediatrics 2015;136[3]:601-4). Expert consultation might also benefit those who feel reluctant to introduce peanuts for other reasons, Dr. Fleischer said.
Dr. Sampson recommends peanut-based skin prick testing for high-risk infants aged 4-8 months. Patients with a negative result should receive 2 grams of peanut protein three times a week for the next 3 years. Those who are mildly sensitive (wheal diameter less than 4 mm) should undergo a peanut challenge observed by an experienced physician. Infants who do not react can start the peanut-based diet.
The LEAP study randomized 640 high-risk infants to either avoid peanuts or consume at least 6 grams per week of the allergen in foods such as smooth peanut butter mixed with mashed fruit, peanut soup, and ground peanuts in other foods. Five-year-olds in the peanut group had significantly lower rates of peanut allergy, regardless of whether their skin prick test had been positive at baseline (N. Engl. J. Med. 2015;372[9]:803-13). While the consensus communication provides interim guidance, a panel sponsored by the National Institute of Allergy and Infectious Diseases is reviewing food allergy data in preparation for updating its guidelines, Dr. Sampson noted. “Several major questions remain,” he said. “Do we need to give such large amounts of peanut to induce tolerance? Is it necessary to give this amount of peanut for such an extended period? What happens if parents don’t give peanut to their infants on a regular basis, as done in the LEAP trial? Could this put them at higher risk? And will this approach apply to other foods?”
Another key knowledge gap is whether the results from one single-center study can be applied elsewhere, said Dr. Fleischer. “We do not know the effects of early peanut introduction in other risk populations.”
Authors of the consensus communication reported no funding sources or conflicts of interest.
*Correction, 8/31/2015: An earlier version of this article misstated the journal in which the study was published.
FROM PEDIATRICS
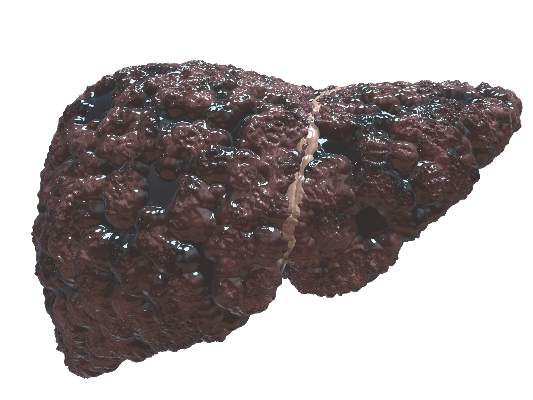
Less posttransplant primary biliary cirrhosis with preventive UDCA
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
Only 21% of liver transplantation patients who received ursodeoxycholic acid (UDCA) after surgery developed recurrent primary biliary cirrhosis, compared with 62% of patients who did not receive the bile acid, researchers reported in the Journal of Hepatology.
The results provide strong evidence that routinely giving liver transplant patients UDCA can prevent or delay recurrent primary biliary cirrhosis, said Alexie Bosch at Hôpital Edouard Herriot in Lyon, France, and his associates.
Primary biliary cirrhosis can recur after liver transplantation and increases the chances of graft dysfunction, the researchers noted. UDCA is the only approved medical treatment for primary biliary cirrhosis in the United States or Europe, but no research team has studied its potential to prevent recurrent primary biliary cirrhosis after liver transplantation, they added. Therefore, they retrospectively studied 90 patients with primary biliary cirrhosis who underwent liver transplantation at five centers in France and Switzerland between 1988 and 2010. In all, 21% of patients received oral UDCA (10-15 mg/kg per day in two divided doses) within 2 weeks after their operation, while the rest received it only if they developed biopsy-confirmed recurrent primary biliary cirrhosis. Biopsies were taken at posttransplant year 1 and every 5 years after that, or when clinically indicated, the investigators noted (J Hepatol. 2015 Aug. 14. doi: 10.1016/j.jhep.2015.07.038).
Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of postsurgical follow-up (P = .014), the researchers reported. The chances of recurrent primary biliary cirrhosis at 5, 10, and 15 years after transplantation were 11%, 21%, and 40% in the UDCA group, compared with 32%, 53%, and 70% for patients who did not receive prophylactic UDCA, they added. A multivariable analysis showed that recurrent primary biliary cirrhosis was associated with not receiving prophylactic UDCA (hazard ratio, 0.32; 95% confidence interval, 0.11, 0.91), but was not linked to donor age, Model For End-Stage Liver Disease (MELD) score, or sex mismatch between donor and recipient, the investigators said. Preventive UDCA also was tied to a 1.6-year longer median time to recurrence, although the trend did not reach statistical significance.
Although the study was retrospective and most patients who received UDCA were treated at one transplant center, all centers had similar histologic findings for recurrent primary biliary cirrhosis, said the researchers. Biopsies also were histologically similar regardless of whether they were event driven or obtained based on the study protocol, and time to recurrence did not vary based on biopsy type, they added. “In our multivariate analysis, we took care to account for all risk factors and confounders, as well as to test multilevel models in order to exclude potential misleading results and center effects,” they emphasized. “Given the extremely limited feasibility of prospective studies and the good tolerance and acceptability of long-term UDCA therapy, these results support the extended use of UDCA as prophylaxis for primary biliary cirrhosis recurrence after liver transplantation.”
The researchers declared no funding sources and reported having no conflicts of interest.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: Treatment with prophylactic ursodeoxycholic acid might help prevent recurrent primary biliary cirrhosis after liver transplantation.
Major finding: Patients who received preventive UDCA had a lower cumulative rate of recurrence throughout 15 years of follow-up (P = .014).
Data source: Multicenter retrospective study of 90 patients who underwent liver transplantation for primary biliary cirrhosis.
Disclosures: The researchers declared no funding sources and reported having no conflicts of interest.
Cirrhosis in HCV often goes unreported
More than 28% of patients with chronic hepatitis C (CHC) virus infection met at least one criterion for cirrhosis, while only 7% had biopsy confirmation of the condition, investigators reported in the August issue of the American Journal of Gastroenterology.
Furthermore, only half of the patients with a positive biopsy had been given an associated ICD-9-CM code, said Dr. Stuart Gordon at Henry Ford Health System in Detroit and his associates. Cirrhosis in CHC therefore might often go unreported, leading to “overly conservative” estimates of its prevalence, associated health care costs, and the cost-effectiveness of the newer HCV treatments, they said.
The researchers analyzed data for 9,783 patients with CHC from the Chronic Hepatitis Cohort Study who were treated between 2006 and 2010. They compared the prevalence of biopsy-confirmed cirrhosis (Metavir stage 4 or pathologist’s report) with the proportion of patients who met at least one of four criteria: positive biopsy; Fibrosis-4 score of at least 5.88, or the presence of a diagnosis or procedural code for cirrhosis or hepatic decompensation. Patients averaged 55 years of age, and most were white males with health insurance, the researchers said (Am. J. Gastroenterol. 2015;110:1169-77).
In all, 28.5% of CHC patients met at least one of the four criteria, including 22% who met the Fibrosis-4 threshold, 6.8% who were biopsy positive, and 5.7% and 4.9% who had a diagnostic or procedural code for cirrhosis or hepatic decompensation, respectively, said the investigators. Patients had significantly greater odds of cirrhosis (P less than .05) if they were older, male, Asian, Hispanic, had genotype 3 HCV infection, HIV coinfection, or a history of antiviral treatment, alcohol abuse, or diabetes, they added. “Our findings are the first in the United States to attempt an accurate estimate of the prevalence of cirrhosis in the CHC patient population at large,” the researchers concluded. “Use of additional parameters suggests a fourfold higher prevalence of cirrhosis than is revealed by biopsy alone. These findings suggest that cirrhosis in CHC patients may be significantly underdocumented and underdiagnosed.”
The CDC Foundation funds the Chronic Hepatitis Cohort Study. Dr. Gordon reported financial relationships with numerous makers of anti-HCV therapies. The other investigators reported having no conflicts of interest.
More than 28% of patients with chronic hepatitis C (CHC) virus infection met at least one criterion for cirrhosis, while only 7% had biopsy confirmation of the condition, investigators reported in the August issue of the American Journal of Gastroenterology.
Furthermore, only half of the patients with a positive biopsy had been given an associated ICD-9-CM code, said Dr. Stuart Gordon at Henry Ford Health System in Detroit and his associates. Cirrhosis in CHC therefore might often go unreported, leading to “overly conservative” estimates of its prevalence, associated health care costs, and the cost-effectiveness of the newer HCV treatments, they said.
The researchers analyzed data for 9,783 patients with CHC from the Chronic Hepatitis Cohort Study who were treated between 2006 and 2010. They compared the prevalence of biopsy-confirmed cirrhosis (Metavir stage 4 or pathologist’s report) with the proportion of patients who met at least one of four criteria: positive biopsy; Fibrosis-4 score of at least 5.88, or the presence of a diagnosis or procedural code for cirrhosis or hepatic decompensation. Patients averaged 55 years of age, and most were white males with health insurance, the researchers said (Am. J. Gastroenterol. 2015;110:1169-77).
In all, 28.5% of CHC patients met at least one of the four criteria, including 22% who met the Fibrosis-4 threshold, 6.8% who were biopsy positive, and 5.7% and 4.9% who had a diagnostic or procedural code for cirrhosis or hepatic decompensation, respectively, said the investigators. Patients had significantly greater odds of cirrhosis (P less than .05) if they were older, male, Asian, Hispanic, had genotype 3 HCV infection, HIV coinfection, or a history of antiviral treatment, alcohol abuse, or diabetes, they added. “Our findings are the first in the United States to attempt an accurate estimate of the prevalence of cirrhosis in the CHC patient population at large,” the researchers concluded. “Use of additional parameters suggests a fourfold higher prevalence of cirrhosis than is revealed by biopsy alone. These findings suggest that cirrhosis in CHC patients may be significantly underdocumented and underdiagnosed.”
The CDC Foundation funds the Chronic Hepatitis Cohort Study. Dr. Gordon reported financial relationships with numerous makers of anti-HCV therapies. The other investigators reported having no conflicts of interest.
More than 28% of patients with chronic hepatitis C (CHC) virus infection met at least one criterion for cirrhosis, while only 7% had biopsy confirmation of the condition, investigators reported in the August issue of the American Journal of Gastroenterology.
Furthermore, only half of the patients with a positive biopsy had been given an associated ICD-9-CM code, said Dr. Stuart Gordon at Henry Ford Health System in Detroit and his associates. Cirrhosis in CHC therefore might often go unreported, leading to “overly conservative” estimates of its prevalence, associated health care costs, and the cost-effectiveness of the newer HCV treatments, they said.
The researchers analyzed data for 9,783 patients with CHC from the Chronic Hepatitis Cohort Study who were treated between 2006 and 2010. They compared the prevalence of biopsy-confirmed cirrhosis (Metavir stage 4 or pathologist’s report) with the proportion of patients who met at least one of four criteria: positive biopsy; Fibrosis-4 score of at least 5.88, or the presence of a diagnosis or procedural code for cirrhosis or hepatic decompensation. Patients averaged 55 years of age, and most were white males with health insurance, the researchers said (Am. J. Gastroenterol. 2015;110:1169-77).
In all, 28.5% of CHC patients met at least one of the four criteria, including 22% who met the Fibrosis-4 threshold, 6.8% who were biopsy positive, and 5.7% and 4.9% who had a diagnostic or procedural code for cirrhosis or hepatic decompensation, respectively, said the investigators. Patients had significantly greater odds of cirrhosis (P less than .05) if they were older, male, Asian, Hispanic, had genotype 3 HCV infection, HIV coinfection, or a history of antiviral treatment, alcohol abuse, or diabetes, they added. “Our findings are the first in the United States to attempt an accurate estimate of the prevalence of cirrhosis in the CHC patient population at large,” the researchers concluded. “Use of additional parameters suggests a fourfold higher prevalence of cirrhosis than is revealed by biopsy alone. These findings suggest that cirrhosis in CHC patients may be significantly underdocumented and underdiagnosed.”
The CDC Foundation funds the Chronic Hepatitis Cohort Study. Dr. Gordon reported financial relationships with numerous makers of anti-HCV therapies. The other investigators reported having no conflicts of interest.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Key clinical point: Cirrhosis might be more common among patients with HCV virus infection than studies based on ICD-9 codes would suggest.
Major finding: 28.5% of patients met more than one of four criteria for cirrhosis, but only 7% had a positive biopsy.
Data source: Observational study of 9,783 patients with chronic HCV infection from the Chronic Hepatitis Cohort Study.
Disclosures: The CDC Foundation funds the Chronic Hepatitis Cohort Study. Dr. Gordon reported financial relationships with numerous makers of therapies for chronic HCV infection. The other investigators reported having no conflicts of interest.
Alzheimer’s patients often had low cerebral amyloid
One in four patients with mild to moderate Alzheimer’s disease dementia had only scant evidence of neuritic amyloid plaques, and the finding was almost three times more common among apolipoprotein E epsilon-4 noncarriers than in carriers, researchers reported online in JAMA Neurology.
“These findings suggest that a nonamyloidogenic variant resembling the clinical phenotype of Alzheimer disease may be more common than previously expected … particularly in APOE4 [apolipoprotein E epsilon-4] noncarriers,” said Sarah Monsell of the University of Washington’s National Alzheimer’s Coordinating Center, Seattle, and her associates. Such patients might not respond to treatments targeting fibrillar or soluble amyloid-beta, the researchers said.
Their study explored clinical and neuropathologic data from 100 APOE4 noncarriers and 100 APOE4 carriers who were diagnosed with mild to moderate Alzheimer’s disease (AD) at their last visit to an AD center. All patients had a Mini-Mental State Examination score of 16-26 and died within 24 months of their last evaluation (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1721).
Fully 37% of APOE4 noncarriers had scant postmortem evidence of amyloid-beta peptide plaques, compared with only 13% of carriers, the investigators reported. Also, 45% of patients with sparse neuritic plaques had extensive (Braak stages III or IV) neurofibrillary degeneration, and most others met neuropathologic criteria for diseases related to dementia, including vascular disease, Lewy body disease, hippocampal sclerosis, frontotemporal lobar degeneration, and tangle-only dementia. “These findings support the results of recent PET imaging studies suggesting that many participants who meet clinical criteria for mild to moderate Alzheimer dementia do not appear to have high levels of amyloid-beta accumulation in the cerebral cortex,” the researchers wrote.
The National Institute on Aging and the Arizona Alzheimer’s Consortium funded the study. Two coauthors reported financial relationships with GE Healthcare, Avid Radiopharmaceuticals, Navidea Biopharmaceuticals, and Merck.
“Thoughtful use of biomarkers will help improve diagnostic accuracy of Alzheimer’s disease (AD), and advances in tau PET imaging will help investigate the role of tau pathology in cognitively normal and impaired elderly individuals. Distinguishing between AD and non-AD pathologies will become increasingly important as more targeted treatments become available for intervention in the preclinical and early clinical stages of AD,” wrote Dr. Stephen Salloway and Dr. Reisa Sperling.
“The collective findings cited herein provide a strong rationale for using amyloid biomarkers (PET and cerebrospinal fluid) in AD clinical trials to recruit more homogeneous populations most likely to respond to amyloid-based treatments. The question we will ultimately face is when should APOE genotyping and amyloid PET be performed in the clinic. A consensus panel of the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging has developed recommendations (Alzheimers Dement. 2013;9[1]:e1-16) to guide the appropriate use of amyloid PET in clinical practice. Testing for APOE is not included in the appropriate use criteria recommendations. Given that APOE4 carrier status is a strong predictor of amyloid and AD pathology, it may be prudent to consider a hierarchical approach to amyloid biomarkers based on APOE genotyping,” they said.
Dr. Salloway is a neurologist at Brown University in Providence, R.I. Dr. Sperling is a neurologist at Harvard University in Boston. Both reported financial relationships with a number of pharmaceutical companies. These comments were taken from their accompanying editorial (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1804).
“Thoughtful use of biomarkers will help improve diagnostic accuracy of Alzheimer’s disease (AD), and advances in tau PET imaging will help investigate the role of tau pathology in cognitively normal and impaired elderly individuals. Distinguishing between AD and non-AD pathologies will become increasingly important as more targeted treatments become available for intervention in the preclinical and early clinical stages of AD,” wrote Dr. Stephen Salloway and Dr. Reisa Sperling.
“The collective findings cited herein provide a strong rationale for using amyloid biomarkers (PET and cerebrospinal fluid) in AD clinical trials to recruit more homogeneous populations most likely to respond to amyloid-based treatments. The question we will ultimately face is when should APOE genotyping and amyloid PET be performed in the clinic. A consensus panel of the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging has developed recommendations (Alzheimers Dement. 2013;9[1]:e1-16) to guide the appropriate use of amyloid PET in clinical practice. Testing for APOE is not included in the appropriate use criteria recommendations. Given that APOE4 carrier status is a strong predictor of amyloid and AD pathology, it may be prudent to consider a hierarchical approach to amyloid biomarkers based on APOE genotyping,” they said.
Dr. Salloway is a neurologist at Brown University in Providence, R.I. Dr. Sperling is a neurologist at Harvard University in Boston. Both reported financial relationships with a number of pharmaceutical companies. These comments were taken from their accompanying editorial (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1804).
“Thoughtful use of biomarkers will help improve diagnostic accuracy of Alzheimer’s disease (AD), and advances in tau PET imaging will help investigate the role of tau pathology in cognitively normal and impaired elderly individuals. Distinguishing between AD and non-AD pathologies will become increasingly important as more targeted treatments become available for intervention in the preclinical and early clinical stages of AD,” wrote Dr. Stephen Salloway and Dr. Reisa Sperling.
“The collective findings cited herein provide a strong rationale for using amyloid biomarkers (PET and cerebrospinal fluid) in AD clinical trials to recruit more homogeneous populations most likely to respond to amyloid-based treatments. The question we will ultimately face is when should APOE genotyping and amyloid PET be performed in the clinic. A consensus panel of the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging has developed recommendations (Alzheimers Dement. 2013;9[1]:e1-16) to guide the appropriate use of amyloid PET in clinical practice. Testing for APOE is not included in the appropriate use criteria recommendations. Given that APOE4 carrier status is a strong predictor of amyloid and AD pathology, it may be prudent to consider a hierarchical approach to amyloid biomarkers based on APOE genotyping,” they said.
Dr. Salloway is a neurologist at Brown University in Providence, R.I. Dr. Sperling is a neurologist at Harvard University in Boston. Both reported financial relationships with a number of pharmaceutical companies. These comments were taken from their accompanying editorial (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1804).
One in four patients with mild to moderate Alzheimer’s disease dementia had only scant evidence of neuritic amyloid plaques, and the finding was almost three times more common among apolipoprotein E epsilon-4 noncarriers than in carriers, researchers reported online in JAMA Neurology.
“These findings suggest that a nonamyloidogenic variant resembling the clinical phenotype of Alzheimer disease may be more common than previously expected … particularly in APOE4 [apolipoprotein E epsilon-4] noncarriers,” said Sarah Monsell of the University of Washington’s National Alzheimer’s Coordinating Center, Seattle, and her associates. Such patients might not respond to treatments targeting fibrillar or soluble amyloid-beta, the researchers said.
Their study explored clinical and neuropathologic data from 100 APOE4 noncarriers and 100 APOE4 carriers who were diagnosed with mild to moderate Alzheimer’s disease (AD) at their last visit to an AD center. All patients had a Mini-Mental State Examination score of 16-26 and died within 24 months of their last evaluation (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1721).
Fully 37% of APOE4 noncarriers had scant postmortem evidence of amyloid-beta peptide plaques, compared with only 13% of carriers, the investigators reported. Also, 45% of patients with sparse neuritic plaques had extensive (Braak stages III or IV) neurofibrillary degeneration, and most others met neuropathologic criteria for diseases related to dementia, including vascular disease, Lewy body disease, hippocampal sclerosis, frontotemporal lobar degeneration, and tangle-only dementia. “These findings support the results of recent PET imaging studies suggesting that many participants who meet clinical criteria for mild to moderate Alzheimer dementia do not appear to have high levels of amyloid-beta accumulation in the cerebral cortex,” the researchers wrote.
The National Institute on Aging and the Arizona Alzheimer’s Consortium funded the study. Two coauthors reported financial relationships with GE Healthcare, Avid Radiopharmaceuticals, Navidea Biopharmaceuticals, and Merck.
One in four patients with mild to moderate Alzheimer’s disease dementia had only scant evidence of neuritic amyloid plaques, and the finding was almost three times more common among apolipoprotein E epsilon-4 noncarriers than in carriers, researchers reported online in JAMA Neurology.
“These findings suggest that a nonamyloidogenic variant resembling the clinical phenotype of Alzheimer disease may be more common than previously expected … particularly in APOE4 [apolipoprotein E epsilon-4] noncarriers,” said Sarah Monsell of the University of Washington’s National Alzheimer’s Coordinating Center, Seattle, and her associates. Such patients might not respond to treatments targeting fibrillar or soluble amyloid-beta, the researchers said.
Their study explored clinical and neuropathologic data from 100 APOE4 noncarriers and 100 APOE4 carriers who were diagnosed with mild to moderate Alzheimer’s disease (AD) at their last visit to an AD center. All patients had a Mini-Mental State Examination score of 16-26 and died within 24 months of their last evaluation (JAMA Neurol. 2015 Aug 24. doi: 10.1001/jamaneurol.2015.1721).
Fully 37% of APOE4 noncarriers had scant postmortem evidence of amyloid-beta peptide plaques, compared with only 13% of carriers, the investigators reported. Also, 45% of patients with sparse neuritic plaques had extensive (Braak stages III or IV) neurofibrillary degeneration, and most others met neuropathologic criteria for diseases related to dementia, including vascular disease, Lewy body disease, hippocampal sclerosis, frontotemporal lobar degeneration, and tangle-only dementia. “These findings support the results of recent PET imaging studies suggesting that many participants who meet clinical criteria for mild to moderate Alzheimer dementia do not appear to have high levels of amyloid-beta accumulation in the cerebral cortex,” the researchers wrote.
The National Institute on Aging and the Arizona Alzheimer’s Consortium funded the study. Two coauthors reported financial relationships with GE Healthcare, Avid Radiopharmaceuticals, Navidea Biopharmaceuticals, and Merck.
FROM JAMA NEUROLOGY
Key clinical point:Patients diagnosed with mild to moderate Alzheimer’s disease, especially apolipoprotein E epsilon-4 noncarriers, may have low cerebral amyloid levels.
Major finding: Fully 37% of APOE4 noncarriers had low amyloid levels, compared with 13% of carriers.
Data source: Neuropathologic and clinical study of 200 patients with a diagnosis of mild to moderate AD, half of whom were APOE4 carriers.
Disclosures: The National Institute on Aging and the Arizona Alzheimer’s Consortium funded the study. Two coauthors reported financial relationships with GE Healthcare, Avid Radiopharmaceuticals, Navidea Biopharmaceuticals, and Merck.
Longer hospitalization after bariatric surgery ups readmission risk
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
FROM SURGERY
Key clinical point: Short length of hospital stay after bariatric surgery was not a risk factor for readmission.
Major finding: Patients who were hospitalized for 3 days and longer were two to four times as likely to be readmitted than were patients with 1-day stays (P less than .001 for both).
Data source: Multicenter database analysis of postoperative outcomes for 95,294 bariatric surgery patients.
Disclosures: The Medical College of Wisconsin and the National Institutes of Health supported the research. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Ingenol mebutate helped clear actinic keratoses
Cryosurgery followed by topical ingenol mebutate cleared extensive regions of actinic keratosis, which helped reveal residual squamous cell carcinomas, according to a report in the August issue of the Journal of Drugs in Dermatology.
The findings show that ingenol mebutate can clear multiple AKs and reduce the number of scarring biopsies required to identify SCCs, said Dr. Miriam S. Bettencourt, a dermatologist in group practice in Henderson, Nev. “In our dermatology clinic, many of the patients with a long history of AK who were treated with ingenol mebutate used sequentially after cryosurgery have achieved complete or partial clearance of AKs.”
Ingenol mebutate gel after cryosurgery cleared AKs more effectively than cryosurgery alone in a recent phase III trial (J Drugs Dermatol. 2014 Jun;13[6]741-7), Dr. Bettencourt noted. She described six men and one woman who each had at least 10 recurrent or hyperkeratotic AKs and previously had undergone cryosurgery. She treated all patients with cryosurgery, followed 2 weeks later by two or three once-daily applications of ingenol mebutate gel at strengths of 0.05% or 0.015%, respectively (J Drugs Dermatol. 2015 Aug;14[8];813-8). One course of ingenol mebutate gel cleared 50%-100% of AKs, Dr. Bettencourt said. She treated residual AKs with cryosurgery, and five patients also received at least one more course of ingenol mebutate to re-treat a partially cleared area or to treat a separate area. Shave biopsies of 10 residual suspicious lesions taken 3-8 months later all revealed invasive SCCs, which were treated with Mohs micrographic surgery (MMS). “These lesions may have been preexisting at the time of topical treatment but not readily recognized as suspicious in the heavily actinically damaged skin, in which suspected or small SCCs may be adjacent to or obscured by AKs,” she said. “Alternatively, these tumors may have been spontaneous new SCCs. In either case, we suggest that effective clearance of AKs from the palette of sun-damaged skin with ingenol mebutate permitted prompt recognition of these lesions as suspicious, and led to further diagnosis and treatment with MMS.”
All patients developed mild to moderate localized redness, flaking, and crusting starting on the second day of ingenol mebutate treatment and resolving within a week of finishing the course, Dr. Bettencourt said.
She reported that she had no relevant financial conflicts.
Cryosurgery followed by topical ingenol mebutate cleared extensive regions of actinic keratosis, which helped reveal residual squamous cell carcinomas, according to a report in the August issue of the Journal of Drugs in Dermatology.
The findings show that ingenol mebutate can clear multiple AKs and reduce the number of scarring biopsies required to identify SCCs, said Dr. Miriam S. Bettencourt, a dermatologist in group practice in Henderson, Nev. “In our dermatology clinic, many of the patients with a long history of AK who were treated with ingenol mebutate used sequentially after cryosurgery have achieved complete or partial clearance of AKs.”
Ingenol mebutate gel after cryosurgery cleared AKs more effectively than cryosurgery alone in a recent phase III trial (J Drugs Dermatol. 2014 Jun;13[6]741-7), Dr. Bettencourt noted. She described six men and one woman who each had at least 10 recurrent or hyperkeratotic AKs and previously had undergone cryosurgery. She treated all patients with cryosurgery, followed 2 weeks later by two or three once-daily applications of ingenol mebutate gel at strengths of 0.05% or 0.015%, respectively (J Drugs Dermatol. 2015 Aug;14[8];813-8). One course of ingenol mebutate gel cleared 50%-100% of AKs, Dr. Bettencourt said. She treated residual AKs with cryosurgery, and five patients also received at least one more course of ingenol mebutate to re-treat a partially cleared area or to treat a separate area. Shave biopsies of 10 residual suspicious lesions taken 3-8 months later all revealed invasive SCCs, which were treated with Mohs micrographic surgery (MMS). “These lesions may have been preexisting at the time of topical treatment but not readily recognized as suspicious in the heavily actinically damaged skin, in which suspected or small SCCs may be adjacent to or obscured by AKs,” she said. “Alternatively, these tumors may have been spontaneous new SCCs. In either case, we suggest that effective clearance of AKs from the palette of sun-damaged skin with ingenol mebutate permitted prompt recognition of these lesions as suspicious, and led to further diagnosis and treatment with MMS.”
All patients developed mild to moderate localized redness, flaking, and crusting starting on the second day of ingenol mebutate treatment and resolving within a week of finishing the course, Dr. Bettencourt said.
She reported that she had no relevant financial conflicts.
Cryosurgery followed by topical ingenol mebutate cleared extensive regions of actinic keratosis, which helped reveal residual squamous cell carcinomas, according to a report in the August issue of the Journal of Drugs in Dermatology.
The findings show that ingenol mebutate can clear multiple AKs and reduce the number of scarring biopsies required to identify SCCs, said Dr. Miriam S. Bettencourt, a dermatologist in group practice in Henderson, Nev. “In our dermatology clinic, many of the patients with a long history of AK who were treated with ingenol mebutate used sequentially after cryosurgery have achieved complete or partial clearance of AKs.”
Ingenol mebutate gel after cryosurgery cleared AKs more effectively than cryosurgery alone in a recent phase III trial (J Drugs Dermatol. 2014 Jun;13[6]741-7), Dr. Bettencourt noted. She described six men and one woman who each had at least 10 recurrent or hyperkeratotic AKs and previously had undergone cryosurgery. She treated all patients with cryosurgery, followed 2 weeks later by two or three once-daily applications of ingenol mebutate gel at strengths of 0.05% or 0.015%, respectively (J Drugs Dermatol. 2015 Aug;14[8];813-8). One course of ingenol mebutate gel cleared 50%-100% of AKs, Dr. Bettencourt said. She treated residual AKs with cryosurgery, and five patients also received at least one more course of ingenol mebutate to re-treat a partially cleared area or to treat a separate area. Shave biopsies of 10 residual suspicious lesions taken 3-8 months later all revealed invasive SCCs, which were treated with Mohs micrographic surgery (MMS). “These lesions may have been preexisting at the time of topical treatment but not readily recognized as suspicious in the heavily actinically damaged skin, in which suspected or small SCCs may be adjacent to or obscured by AKs,” she said. “Alternatively, these tumors may have been spontaneous new SCCs. In either case, we suggest that effective clearance of AKs from the palette of sun-damaged skin with ingenol mebutate permitted prompt recognition of these lesions as suspicious, and led to further diagnosis and treatment with MMS.”
All patients developed mild to moderate localized redness, flaking, and crusting starting on the second day of ingenol mebutate treatment and resolving within a week of finishing the course, Dr. Bettencourt said.
She reported that she had no relevant financial conflicts.
FROM THE JOURNAL OF DRUGS IN DERMATOLOGY
Key clinical point: Several courses of cryosurgery and ingenol mebutate helped clear actinic keratoses, helping a clinician identify residual squamous cell carcinomas.
Major finding: Lesion counts dropped by 50%-100% after cryosurgery followed by one to three courses of ingenol mebutate gel.
Data source: A case series of seven patients who had multiple AKs and 10 SCCs.
Disclosures: Dr. Bettencourt reported that she had no relevant financial conflicts.
Long-term RA remission can restore physical function
Long-term remission of rheumatoid arthritis for 24 weeks allowed 58%-73% of patients to regain full physical function, depending on which disease activity index is used, researchers reported online in Arthritis Research & Therapy.
“Physical function continues to improve over time when remission is maintained,” wrote Dr. Helga Radner and her associates at the Medical University of Vienna. Patients with DAS28 (Disease Activity Score using 28-joint counts including C-reactive protein) remission of at least 24 weeks improved by an average of 0.08 on the Health Assessment Questionnaire (HAQ), while those with sustained SDAI (Simplified Disease Activity Index) remissions improved by an average of 0.04, the investigators said.
The changes might seem small, but reflected the “very good” functional status of rheumatoid arthritis (RA) patients who achieve long-term remission, they noted, adding that, “on the group level in this population, the relative further improvement was between a quarter and a third of the initial HAQ assessment.”
Remission is a common treatment goal in RA, but maintaining it is the best way to slow or stop further joint damage. To better understand physical function within the context of sustained remission, the investigators analyzed HAQ disability index functional scores for 4,364 patients with active baseline disease who participated in the ASPIRE, ATTRACT, PREMIER, DE019, ERA, TEMPO, and leflunomide trials (Arthritis Res Ther. 2015;17:203).
In all, 14% of patients remained in DAS28 remission (scoring 2.6 or less) for at least 24 consecutive weeks and 5.8% achieved sustained SDAI remission (3.3 or less), Dr. Radner and her associates reported. Lower baseline disease activity, rheumatoid factor levels, and disease duration all predicted sustained remission (P less than .05 for all associations).
Full physical function, defined as a score of zero on the HAQ, occurred in 58% of patients in DAS28 remission for 24 weeks and in 73% of patients in SDAI remission for 24 weeks. Among patients in sustained DAS28 remission, women were significantly more likely than men to regain full physical function (hazard ratio, 1.41; 95% confidence interval, 1.13-1.76), as were patients with early (less than 2 years), compared with longer-term, disease (HR, 1.29; 95% CI, 1.01-1.65). Seropositivity and treatment regimen did not significantly affect the chances of regaining full function.
The researchers may not have captured some disease fluctuations because of the study design, they said. They also did not account for factors such as psychological status and comorbidities, which can affect physical disability.
The Medical University of Vienna funded the study. The investigators declared no competing interests.
Long-term remission of rheumatoid arthritis for 24 weeks allowed 58%-73% of patients to regain full physical function, depending on which disease activity index is used, researchers reported online in Arthritis Research & Therapy.
“Physical function continues to improve over time when remission is maintained,” wrote Dr. Helga Radner and her associates at the Medical University of Vienna. Patients with DAS28 (Disease Activity Score using 28-joint counts including C-reactive protein) remission of at least 24 weeks improved by an average of 0.08 on the Health Assessment Questionnaire (HAQ), while those with sustained SDAI (Simplified Disease Activity Index) remissions improved by an average of 0.04, the investigators said.
The changes might seem small, but reflected the “very good” functional status of rheumatoid arthritis (RA) patients who achieve long-term remission, they noted, adding that, “on the group level in this population, the relative further improvement was between a quarter and a third of the initial HAQ assessment.”
Remission is a common treatment goal in RA, but maintaining it is the best way to slow or stop further joint damage. To better understand physical function within the context of sustained remission, the investigators analyzed HAQ disability index functional scores for 4,364 patients with active baseline disease who participated in the ASPIRE, ATTRACT, PREMIER, DE019, ERA, TEMPO, and leflunomide trials (Arthritis Res Ther. 2015;17:203).
In all, 14% of patients remained in DAS28 remission (scoring 2.6 or less) for at least 24 consecutive weeks and 5.8% achieved sustained SDAI remission (3.3 or less), Dr. Radner and her associates reported. Lower baseline disease activity, rheumatoid factor levels, and disease duration all predicted sustained remission (P less than .05 for all associations).
Full physical function, defined as a score of zero on the HAQ, occurred in 58% of patients in DAS28 remission for 24 weeks and in 73% of patients in SDAI remission for 24 weeks. Among patients in sustained DAS28 remission, women were significantly more likely than men to regain full physical function (hazard ratio, 1.41; 95% confidence interval, 1.13-1.76), as were patients with early (less than 2 years), compared with longer-term, disease (HR, 1.29; 95% CI, 1.01-1.65). Seropositivity and treatment regimen did not significantly affect the chances of regaining full function.
The researchers may not have captured some disease fluctuations because of the study design, they said. They also did not account for factors such as psychological status and comorbidities, which can affect physical disability.
The Medical University of Vienna funded the study. The investigators declared no competing interests.
Long-term remission of rheumatoid arthritis for 24 weeks allowed 58%-73% of patients to regain full physical function, depending on which disease activity index is used, researchers reported online in Arthritis Research & Therapy.
“Physical function continues to improve over time when remission is maintained,” wrote Dr. Helga Radner and her associates at the Medical University of Vienna. Patients with DAS28 (Disease Activity Score using 28-joint counts including C-reactive protein) remission of at least 24 weeks improved by an average of 0.08 on the Health Assessment Questionnaire (HAQ), while those with sustained SDAI (Simplified Disease Activity Index) remissions improved by an average of 0.04, the investigators said.
The changes might seem small, but reflected the “very good” functional status of rheumatoid arthritis (RA) patients who achieve long-term remission, they noted, adding that, “on the group level in this population, the relative further improvement was between a quarter and a third of the initial HAQ assessment.”
Remission is a common treatment goal in RA, but maintaining it is the best way to slow or stop further joint damage. To better understand physical function within the context of sustained remission, the investigators analyzed HAQ disability index functional scores for 4,364 patients with active baseline disease who participated in the ASPIRE, ATTRACT, PREMIER, DE019, ERA, TEMPO, and leflunomide trials (Arthritis Res Ther. 2015;17:203).
In all, 14% of patients remained in DAS28 remission (scoring 2.6 or less) for at least 24 consecutive weeks and 5.8% achieved sustained SDAI remission (3.3 or less), Dr. Radner and her associates reported. Lower baseline disease activity, rheumatoid factor levels, and disease duration all predicted sustained remission (P less than .05 for all associations).
Full physical function, defined as a score of zero on the HAQ, occurred in 58% of patients in DAS28 remission for 24 weeks and in 73% of patients in SDAI remission for 24 weeks. Among patients in sustained DAS28 remission, women were significantly more likely than men to regain full physical function (hazard ratio, 1.41; 95% confidence interval, 1.13-1.76), as were patients with early (less than 2 years), compared with longer-term, disease (HR, 1.29; 95% CI, 1.01-1.65). Seropositivity and treatment regimen did not significantly affect the chances of regaining full function.
The researchers may not have captured some disease fluctuations because of the study design, they said. They also did not account for factors such as psychological status and comorbidities, which can affect physical disability.
The Medical University of Vienna funded the study. The investigators declared no competing interests.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point: Patients with rheumatoid arthritis can regain full physical functioning after achieving sustained clinical remission.
Major finding: Full physical function, defined as a score of zero on the HAQ, occurred in 58% of patients in DAS28 remission for 24 weeks and in 73% of patients in SDAI remission for 24 weeks.
Data source: Combined analysis of data for 4,364 patients from the ASPIRE, ATTRACT, PREMIER, DE019, ERA, TEMPO, and leflunomide trials.
Disclosures: The Medical University of Vienna funded the study. The investigators declared no competing interests.