User login
November 2015: Click for Credit
Here are 8 articles in the November issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. Low-risk Prostate Cancer: Immediate Contemplation, Not Immediate Intervention
To take the posttest, go to http://bit.ly/1Vz6Cok
VITALS
Key clinical point: Men with favorable-risk prostate cancer have a low risk for progression to a lethal phenotype and should consider active surveillance.
Major finding: Of 1,298 men with favorable-risk prostate cancer who were enrolled in an active surveillance program, overall, cancer-specific, and metastasis-free survival rates were 69%, 99.9%, and 99.4%, respectively, at 15 years.
Data source: A follow-up of a cohort of men with favorable-risk prostate cancer receiving active surveillance at a single institution that used a clearly defined protocol for enrollment, monitoring, and intervention.
Disclosures: There were no outside funding sources reported. Some coauthors reported consulting or advisory roles with Metamark Genetics, MDxHealth, Dianon Systems, DAKO, Trock, SonaCare Medical, Myriad Genetics, Rochon Genova, Rothwell Figg, and Roche.
2. Diabetes in Seniors Increases Dementia Risk
To take the posttest, go to http://bit.ly/1Q1bITm
VITALS
Key clinical point: Even short-term hyperglycemia in late life can trigger or accelerate cognitive decline, and incident diabetes is a risk factor for dementia after adjustment for differences in cardiovascular disease and other common risk factors.
Major finding: Individuals diagnosed with diabetes later in life have a 16% higher risk for dementia than do those without diabetes.
Data source: A population-based matched cohort study in 225,045 seniors newly diagnosed with diabetes and 668,070 nondiabetic controls.
Disclosures: The Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario, the Canadian Institutes of Health Research, the University of Toronto, and the Ontario Ministry of Health and Long-Term Care supported the study. One author reported an unrestricted grant from Amgen, but there were no other conflicts of interest declared.
3. Extremes of Sleep Linked With Early Signs of CVD
To take the posttest, go to http://bit.ly/1FSvLmw
VITALS
Key clinical point: Individuals with very long or short sleep, or poor sleep quality, showed signs of early cardiovascular disease.
Major finding: Extremely short and extremely long sleep duration were associated with significantly increased levels of coronary artery calcification (CAC) and increased brachial-ankle pulse wave velocity (baPWV).
Data source: Cross-sectional study of more than 47,000 healthy adult men and women who reported sleep duration and quality and underwent either measurement of CAC.
Disclosures: The funding source was not reported. The authors reported no disclosures.
4. Sunscreens With DNA Repair Enzymes Might Lessen AK Progression
To take the posttest, go to http://bit.ly/1LdZWFf
VITALS
Key clinical point: Sunscreen containing DNA repair enzymes might prevent malignant progression of actinic keratosis better than sunscreen alone.
Major finding: Field cancerization and cyclobutane pyrimidine dimer levels improved significantly more with sunscreen plus enzymes than with sunscreen only (P < .0001 for each).
Data source: Six-month randomized trial of 28 patients with actinic keratosis.
Disclosures: Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
5. Breastfeeding Protects Against Postpartum MS Relapse
To take the posttest, go to http://bit.ly/1OSYU49
VITALS
Key clinical point: Don’t discourage new mothers with multiple sclerosis from breastfeeding.
Major finding: Among 81 women who did not breastfeed or who supplemented breastfeeding early on, 31 (38.3%) had an MS relapse within the first six postpartum months, compared with 29 women (24.2%) among the 120 who intended to breastfeed their children exclusively for at least two months (adjusted HR, 1.70).
Data source: A prospective study of 201 pregnant women with relapsing-remitting MS who were followed for one year post partum.
Disclosures: The work was funded by the German Research Foundation. The German MS and pregnancy registry was partly supported by Bayer HealthCare, Biogen Idec, Merck Serono, Novartis Pharma, and Genzyme Pharmaceuticals. Five of the researchers reported receiving speaker honoraria or other financial support from pharmaceutical companies.
6. S aureus Seen in 1% of Pediatric CAP Cases
To take the posttest, go to http://bit.ly/1FPJnQ3
VITALS
Key clinical point: About 1% of children presenting to a hospital with community-acquired pneumonia had Staphylococcus aureus infections, which do not respond to recommended firstline narrow-spectrum antibiotics for CAP.
Major finding: In a cohort of 554 children admitted with CAP, seven had S aureus infections, six classified as complicated. All received vancomycin within 24 hours of admission; anemia incidence was significantly higher in S aureus patients than for the rest of the cohort.
Data source: Retrospective cohort study of more than 3,400 children.
Disclosures: The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
7. Higher Arrhythmia Risk for Psoriasis Patients
To take the posttest, go to http://bit.ly/1VBdbS6
VITALS
Key clinical point: Patients with psoriasis are at increased risk for arrhythmia compared to those without psoriasis.
Major finding: After researchers adjusted for history and medication use, patients with psoriasis were at increased risk for overall arrhythmia (adjusted hazard ratio, 1.34; 95% confidence interval, 1.29-1.39).
Data source: A retrospective cohort study using data from almost 41,000 psoriasis patients identified from the Taiwan National Health Insurance Research Database, and almost 163,000 age- and sex-matched cohorts from the same database.
Disclosures: The study was institutionally funded. Dr. Chiu, Ms. Chang, and three other authors had no disclosures; one author disclosed having conducted clinical trials or received honoraria from several companies, including Pfizer and Novartis, and having received speaking fees from AbbVie.
8. Hepatitis C Drove Steep Rises in Cirrhosis, HCC, and Related Deaths
To take the posttest, go to http://bit.ly/1jyNrdp
VITALS
Key clinical point: Cirrhosis, hepatocellular carcinoma (HCC), and liver-related mortality rose substantially among Veterans Affairs (VA) patients over the past 12 years, mainly driven by hepatitis C virus infection.
Major finding: The prevalence of cirrhosis nearly doubled between 2001 and 2013, while cirrhosis-related deaths rose by about 50% and the incidence of HCC almost tripled.
Data source: A retrospective cohort study of 129,998 VA patients with cirrhosis and 21,326 VA patients with HCC between 2001 and 2013.
Disclosures: The Department of VA and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Here are 8 articles in the November issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. Low-risk Prostate Cancer: Immediate Contemplation, Not Immediate Intervention
To take the posttest, go to http://bit.ly/1Vz6Cok
VITALS
Key clinical point: Men with favorable-risk prostate cancer have a low risk for progression to a lethal phenotype and should consider active surveillance.
Major finding: Of 1,298 men with favorable-risk prostate cancer who were enrolled in an active surveillance program, overall, cancer-specific, and metastasis-free survival rates were 69%, 99.9%, and 99.4%, respectively, at 15 years.
Data source: A follow-up of a cohort of men with favorable-risk prostate cancer receiving active surveillance at a single institution that used a clearly defined protocol for enrollment, monitoring, and intervention.
Disclosures: There were no outside funding sources reported. Some coauthors reported consulting or advisory roles with Metamark Genetics, MDxHealth, Dianon Systems, DAKO, Trock, SonaCare Medical, Myriad Genetics, Rochon Genova, Rothwell Figg, and Roche.
2. Diabetes in Seniors Increases Dementia Risk
To take the posttest, go to http://bit.ly/1Q1bITm
VITALS
Key clinical point: Even short-term hyperglycemia in late life can trigger or accelerate cognitive decline, and incident diabetes is a risk factor for dementia after adjustment for differences in cardiovascular disease and other common risk factors.
Major finding: Individuals diagnosed with diabetes later in life have a 16% higher risk for dementia than do those without diabetes.
Data source: A population-based matched cohort study in 225,045 seniors newly diagnosed with diabetes and 668,070 nondiabetic controls.
Disclosures: The Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario, the Canadian Institutes of Health Research, the University of Toronto, and the Ontario Ministry of Health and Long-Term Care supported the study. One author reported an unrestricted grant from Amgen, but there were no other conflicts of interest declared.
3. Extremes of Sleep Linked With Early Signs of CVD
To take the posttest, go to http://bit.ly/1FSvLmw
VITALS
Key clinical point: Individuals with very long or short sleep, or poor sleep quality, showed signs of early cardiovascular disease.
Major finding: Extremely short and extremely long sleep duration were associated with significantly increased levels of coronary artery calcification (CAC) and increased brachial-ankle pulse wave velocity (baPWV).
Data source: Cross-sectional study of more than 47,000 healthy adult men and women who reported sleep duration and quality and underwent either measurement of CAC.
Disclosures: The funding source was not reported. The authors reported no disclosures.
4. Sunscreens With DNA Repair Enzymes Might Lessen AK Progression
To take the posttest, go to http://bit.ly/1LdZWFf
VITALS
Key clinical point: Sunscreen containing DNA repair enzymes might prevent malignant progression of actinic keratosis better than sunscreen alone.
Major finding: Field cancerization and cyclobutane pyrimidine dimer levels improved significantly more with sunscreen plus enzymes than with sunscreen only (P < .0001 for each).
Data source: Six-month randomized trial of 28 patients with actinic keratosis.
Disclosures: Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
5. Breastfeeding Protects Against Postpartum MS Relapse
To take the posttest, go to http://bit.ly/1OSYU49
VITALS
Key clinical point: Don’t discourage new mothers with multiple sclerosis from breastfeeding.
Major finding: Among 81 women who did not breastfeed or who supplemented breastfeeding early on, 31 (38.3%) had an MS relapse within the first six postpartum months, compared with 29 women (24.2%) among the 120 who intended to breastfeed their children exclusively for at least two months (adjusted HR, 1.70).
Data source: A prospective study of 201 pregnant women with relapsing-remitting MS who were followed for one year post partum.
Disclosures: The work was funded by the German Research Foundation. The German MS and pregnancy registry was partly supported by Bayer HealthCare, Biogen Idec, Merck Serono, Novartis Pharma, and Genzyme Pharmaceuticals. Five of the researchers reported receiving speaker honoraria or other financial support from pharmaceutical companies.
6. S aureus Seen in 1% of Pediatric CAP Cases
To take the posttest, go to http://bit.ly/1FPJnQ3
VITALS
Key clinical point: About 1% of children presenting to a hospital with community-acquired pneumonia had Staphylococcus aureus infections, which do not respond to recommended firstline narrow-spectrum antibiotics for CAP.
Major finding: In a cohort of 554 children admitted with CAP, seven had S aureus infections, six classified as complicated. All received vancomycin within 24 hours of admission; anemia incidence was significantly higher in S aureus patients than for the rest of the cohort.
Data source: Retrospective cohort study of more than 3,400 children.
Disclosures: The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
7. Higher Arrhythmia Risk for Psoriasis Patients
To take the posttest, go to http://bit.ly/1VBdbS6
VITALS
Key clinical point: Patients with psoriasis are at increased risk for arrhythmia compared to those without psoriasis.
Major finding: After researchers adjusted for history and medication use, patients with psoriasis were at increased risk for overall arrhythmia (adjusted hazard ratio, 1.34; 95% confidence interval, 1.29-1.39).
Data source: A retrospective cohort study using data from almost 41,000 psoriasis patients identified from the Taiwan National Health Insurance Research Database, and almost 163,000 age- and sex-matched cohorts from the same database.
Disclosures: The study was institutionally funded. Dr. Chiu, Ms. Chang, and three other authors had no disclosures; one author disclosed having conducted clinical trials or received honoraria from several companies, including Pfizer and Novartis, and having received speaking fees from AbbVie.
8. Hepatitis C Drove Steep Rises in Cirrhosis, HCC, and Related Deaths
To take the posttest, go to http://bit.ly/1jyNrdp
VITALS
Key clinical point: Cirrhosis, hepatocellular carcinoma (HCC), and liver-related mortality rose substantially among Veterans Affairs (VA) patients over the past 12 years, mainly driven by hepatitis C virus infection.
Major finding: The prevalence of cirrhosis nearly doubled between 2001 and 2013, while cirrhosis-related deaths rose by about 50% and the incidence of HCC almost tripled.
Data source: A retrospective cohort study of 129,998 VA patients with cirrhosis and 21,326 VA patients with HCC between 2001 and 2013.
Disclosures: The Department of VA and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Here are 8 articles in the November issue of Clinician Reviews (accreditation valid until January 1, 2016):
1. Low-risk Prostate Cancer: Immediate Contemplation, Not Immediate Intervention
To take the posttest, go to http://bit.ly/1Vz6Cok
VITALS
Key clinical point: Men with favorable-risk prostate cancer have a low risk for progression to a lethal phenotype and should consider active surveillance.
Major finding: Of 1,298 men with favorable-risk prostate cancer who were enrolled in an active surveillance program, overall, cancer-specific, and metastasis-free survival rates were 69%, 99.9%, and 99.4%, respectively, at 15 years.
Data source: A follow-up of a cohort of men with favorable-risk prostate cancer receiving active surveillance at a single institution that used a clearly defined protocol for enrollment, monitoring, and intervention.
Disclosures: There were no outside funding sources reported. Some coauthors reported consulting or advisory roles with Metamark Genetics, MDxHealth, Dianon Systems, DAKO, Trock, SonaCare Medical, Myriad Genetics, Rochon Genova, Rothwell Figg, and Roche.
2. Diabetes in Seniors Increases Dementia Risk
To take the posttest, go to http://bit.ly/1Q1bITm
VITALS
Key clinical point: Even short-term hyperglycemia in late life can trigger or accelerate cognitive decline, and incident diabetes is a risk factor for dementia after adjustment for differences in cardiovascular disease and other common risk factors.
Major finding: Individuals diagnosed with diabetes later in life have a 16% higher risk for dementia than do those without diabetes.
Data source: A population-based matched cohort study in 225,045 seniors newly diagnosed with diabetes and 668,070 nondiabetic controls.
Disclosures: The Canadian Institutes of Health Research, the Heart and Stroke Foundation of Ontario, the Canadian Institutes of Health Research, the University of Toronto, and the Ontario Ministry of Health and Long-Term Care supported the study. One author reported an unrestricted grant from Amgen, but there were no other conflicts of interest declared.
3. Extremes of Sleep Linked With Early Signs of CVD
To take the posttest, go to http://bit.ly/1FSvLmw
VITALS
Key clinical point: Individuals with very long or short sleep, or poor sleep quality, showed signs of early cardiovascular disease.
Major finding: Extremely short and extremely long sleep duration were associated with significantly increased levels of coronary artery calcification (CAC) and increased brachial-ankle pulse wave velocity (baPWV).
Data source: Cross-sectional study of more than 47,000 healthy adult men and women who reported sleep duration and quality and underwent either measurement of CAC.
Disclosures: The funding source was not reported. The authors reported no disclosures.
4. Sunscreens With DNA Repair Enzymes Might Lessen AK Progression
To take the posttest, go to http://bit.ly/1LdZWFf
VITALS
Key clinical point: Sunscreen containing DNA repair enzymes might prevent malignant progression of actinic keratosis better than sunscreen alone.
Major finding: Field cancerization and cyclobutane pyrimidine dimer levels improved significantly more with sunscreen plus enzymes than with sunscreen only (P < .0001 for each).
Data source: Six-month randomized trial of 28 patients with actinic keratosis.
Disclosures: Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
5. Breastfeeding Protects Against Postpartum MS Relapse
To take the posttest, go to http://bit.ly/1OSYU49
VITALS
Key clinical point: Don’t discourage new mothers with multiple sclerosis from breastfeeding.
Major finding: Among 81 women who did not breastfeed or who supplemented breastfeeding early on, 31 (38.3%) had an MS relapse within the first six postpartum months, compared with 29 women (24.2%) among the 120 who intended to breastfeed their children exclusively for at least two months (adjusted HR, 1.70).
Data source: A prospective study of 201 pregnant women with relapsing-remitting MS who were followed for one year post partum.
Disclosures: The work was funded by the German Research Foundation. The German MS and pregnancy registry was partly supported by Bayer HealthCare, Biogen Idec, Merck Serono, Novartis Pharma, and Genzyme Pharmaceuticals. Five of the researchers reported receiving speaker honoraria or other financial support from pharmaceutical companies.
6. S aureus Seen in 1% of Pediatric CAP Cases
To take the posttest, go to http://bit.ly/1FPJnQ3
VITALS
Key clinical point: About 1% of children presenting to a hospital with community-acquired pneumonia had Staphylococcus aureus infections, which do not respond to recommended firstline narrow-spectrum antibiotics for CAP.
Major finding: In a cohort of 554 children admitted with CAP, seven had S aureus infections, six classified as complicated. All received vancomycin within 24 hours of admission; anemia incidence was significantly higher in S aureus patients than for the rest of the cohort.
Data source: Retrospective cohort study of more than 3,400 children.
Disclosures: The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
7. Higher Arrhythmia Risk for Psoriasis Patients
To take the posttest, go to http://bit.ly/1VBdbS6
VITALS
Key clinical point: Patients with psoriasis are at increased risk for arrhythmia compared to those without psoriasis.
Major finding: After researchers adjusted for history and medication use, patients with psoriasis were at increased risk for overall arrhythmia (adjusted hazard ratio, 1.34; 95% confidence interval, 1.29-1.39).
Data source: A retrospective cohort study using data from almost 41,000 psoriasis patients identified from the Taiwan National Health Insurance Research Database, and almost 163,000 age- and sex-matched cohorts from the same database.
Disclosures: The study was institutionally funded. Dr. Chiu, Ms. Chang, and three other authors had no disclosures; one author disclosed having conducted clinical trials or received honoraria from several companies, including Pfizer and Novartis, and having received speaking fees from AbbVie.
8. Hepatitis C Drove Steep Rises in Cirrhosis, HCC, and Related Deaths
To take the posttest, go to http://bit.ly/1jyNrdp
VITALS
Key clinical point: Cirrhosis, hepatocellular carcinoma (HCC), and liver-related mortality rose substantially among Veterans Affairs (VA) patients over the past 12 years, mainly driven by hepatitis C virus infection.
Major finding: The prevalence of cirrhosis nearly doubled between 2001 and 2013, while cirrhosis-related deaths rose by about 50% and the incidence of HCC almost tripled.
Data source: A retrospective cohort study of 129,998 VA patients with cirrhosis and 21,326 VA patients with HCC between 2001 and 2013.
Disclosures: The Department of VA and the Veterans Health Administration funded the study. The investigators declared no competing interests.
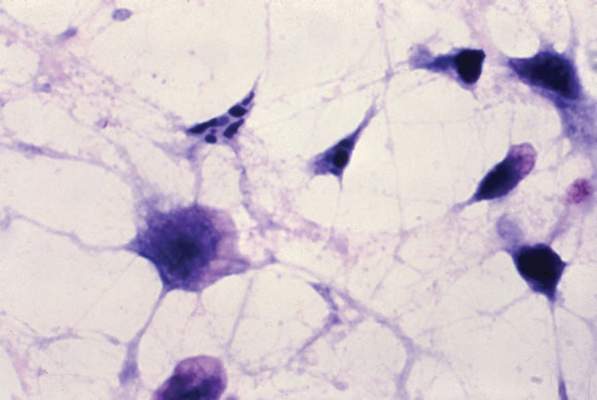
P2X7 receptor implicated in visceral pain caused by chronic pancreatitis
A subtype of purinergic receptor on spinal microglial cells mediated visceral pain hypersensitivity in rats with chronic pancreatitis, and pharmacologic or genetic inhibition of this receptor improved hyperalgesia, according to a report in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
“Our study may be the first to identify that P2X7 receptors in spinal microglia are upregulated in chronic pancreatitis, and that this upregulation is associated with the development of visceral hyperalgesia,” said Dr. Pei-Yi Liu at National Yang-Ming University in Taipei, Taiwan, and her associates. A common laboratory dye known as brilliant blue G, which is an antagonist of P2X7R, “not only attenuated but also prevented CP-related chronic visceral hyperalgesia,” the researchers reported.
Chronic pancreatitis causes intense, recurrent epigastric pain that is “difficult and frustrating” to control and can lead to malnutrition, narcotic analgesic addiction, and social and financial problems, said the researchers. Previously, they had linked visceral pain in murine CP to activation of spinal microglia, the main effector immune cells in the central nervous system. The molecular pathways remained unclear, but some research had implicated extracellular adenosine triphosphate (ATP) as well as purinergic receptors in the CNS. Because a purine receptor subtype known as P2X7 had been linked to neuropathic and inflammatory pain, the researchers wondered if it also facilitated visceral pain (Cell Mol Gastroenterol Hepatol. 2015 Jul 22. doi: 10.1016/j.jcmgh.2015.07.008). To explore that question, they created a CP model by injecting 2% trinitrobenzene sulfonic acid into the pancreatic ducts of male rats. They measured behavioral responses to mechanical and electrical stimulation and quantified spinal cord P2X7R levels with the help of standard laboratory assays. They also watched for changes in pain-related behaviors after blocking spinal cord P2X7R with brilliant blue G or knocking it down with short interfering RNA (siRNA).
Spinal P2X7R expression rose significantly after CP induction, as did levels of the OX-42 microglial marker in the dorsal horn of the spinal cord, said the investigators. Brilliant blue G and genetic knock down suppressed P2X7R expression, inhibited activation of spinal microglia, and “significantly attenuated” nociceptive behaviors, they added.
The researchers also pretreated some rats with brilliant blue G before inducing CP and saw that these rats exhibited significantly lower pain responses to mechanical and electrical stimuli compared with other CP rats. In fact, the nociceptive responses of the pretreated CP rats resembled those of non-CP control rats, the investigators said. Spinal tissue from pretreated rats also lacked signs of P2X7R upregulation, they noted.
Taken together, the data “indicate a critical role of P2X7R expressed in the spinal cord in the development of chronic visceral pain in CP,” concluded the researchers. Brilliant blue G inhibits voltage-gated sodium channels, which are known to contribute to chronic visceral pain, and “may represent an effective drug for the treatment of chronic pain in chronic pancreatitis patients,” they added.
The study was funded by Taipei Veterans General Hospital, National Science Council of Taiwan, and the Taiwan Ministry of Education Aim for Top University Grant. The investigators declared no competing interests.
The traditional approach to treating pain in chronic pancreatitis is as if it were a “plumbing” problem – problems with ductal drainage. More recently, the emphasis has been on sensitization of the sensorineural system (“wiring”), in which the pain responses are greatly exaggerated. An additional consideration is whether this sensitization occurs in peripheral nerves that directly innervate the pancreas, or in the central nervous system, or both. This is clinically important because treatments directed at the periphery, e.g., pancreatectomy, may not be effective in patients in whom central sensitization is dominant.

|
Dr. Pankaj Jay Pasricha |
The findings of Dr. Lui and colleagues show that spinal (hence central) sensitization is important in chronic pancreatitis pain, and that this may be mediated by nonneuronal cells (microglia) in the spinal cord via P2X7R, a nucleotide receptor. This is not surprising, given that this signaling system has shown to be important in other forms of chronic pain. However, some questions remain – is peripheral sensitization driving these changes?
Clearly the “drug” they have used (BBG) is relatively harmless, but it is not practical because it may not be safe in humans (apart from coloring them blue). BBG also affects other channels, notably neuronal voltage-dependent sodium channels. Nevertheless, this study does offer new insight into the pathogenesis of pain in chronic pancreatitis and by itself is an important cautionary message for the growing enthusiasm for total pancreatectomy. It also identifies potential new therapeutic targets for treatment of pain and will, it is hoped, stimulate engagement from the pharmaceutical industry that is developing drugs directed toward glial activation and in particular the P2X7 receptor.
Dr. Pankaj Jay Pasricha, AGAF, is professor of medicine, Johns Hopkins University School of Medicine, director of Johns Hopkins Center for Motility Disorders and Digestive Diseases, and professor of innovation management, The Carey Business School, Johns Hopkins University, Baltimore. He has no conflicts of interest.
The traditional approach to treating pain in chronic pancreatitis is as if it were a “plumbing” problem – problems with ductal drainage. More recently, the emphasis has been on sensitization of the sensorineural system (“wiring”), in which the pain responses are greatly exaggerated. An additional consideration is whether this sensitization occurs in peripheral nerves that directly innervate the pancreas, or in the central nervous system, or both. This is clinically important because treatments directed at the periphery, e.g., pancreatectomy, may not be effective in patients in whom central sensitization is dominant.

|
Dr. Pankaj Jay Pasricha |
The findings of Dr. Lui and colleagues show that spinal (hence central) sensitization is important in chronic pancreatitis pain, and that this may be mediated by nonneuronal cells (microglia) in the spinal cord via P2X7R, a nucleotide receptor. This is not surprising, given that this signaling system has shown to be important in other forms of chronic pain. However, some questions remain – is peripheral sensitization driving these changes?
Clearly the “drug” they have used (BBG) is relatively harmless, but it is not practical because it may not be safe in humans (apart from coloring them blue). BBG also affects other channels, notably neuronal voltage-dependent sodium channels. Nevertheless, this study does offer new insight into the pathogenesis of pain in chronic pancreatitis and by itself is an important cautionary message for the growing enthusiasm for total pancreatectomy. It also identifies potential new therapeutic targets for treatment of pain and will, it is hoped, stimulate engagement from the pharmaceutical industry that is developing drugs directed toward glial activation and in particular the P2X7 receptor.
Dr. Pankaj Jay Pasricha, AGAF, is professor of medicine, Johns Hopkins University School of Medicine, director of Johns Hopkins Center for Motility Disorders and Digestive Diseases, and professor of innovation management, The Carey Business School, Johns Hopkins University, Baltimore. He has no conflicts of interest.
The traditional approach to treating pain in chronic pancreatitis is as if it were a “plumbing” problem – problems with ductal drainage. More recently, the emphasis has been on sensitization of the sensorineural system (“wiring”), in which the pain responses are greatly exaggerated. An additional consideration is whether this sensitization occurs in peripheral nerves that directly innervate the pancreas, or in the central nervous system, or both. This is clinically important because treatments directed at the periphery, e.g., pancreatectomy, may not be effective in patients in whom central sensitization is dominant.

|
Dr. Pankaj Jay Pasricha |
The findings of Dr. Lui and colleagues show that spinal (hence central) sensitization is important in chronic pancreatitis pain, and that this may be mediated by nonneuronal cells (microglia) in the spinal cord via P2X7R, a nucleotide receptor. This is not surprising, given that this signaling system has shown to be important in other forms of chronic pain. However, some questions remain – is peripheral sensitization driving these changes?
Clearly the “drug” they have used (BBG) is relatively harmless, but it is not practical because it may not be safe in humans (apart from coloring them blue). BBG also affects other channels, notably neuronal voltage-dependent sodium channels. Nevertheless, this study does offer new insight into the pathogenesis of pain in chronic pancreatitis and by itself is an important cautionary message for the growing enthusiasm for total pancreatectomy. It also identifies potential new therapeutic targets for treatment of pain and will, it is hoped, stimulate engagement from the pharmaceutical industry that is developing drugs directed toward glial activation and in particular the P2X7 receptor.
Dr. Pankaj Jay Pasricha, AGAF, is professor of medicine, Johns Hopkins University School of Medicine, director of Johns Hopkins Center for Motility Disorders and Digestive Diseases, and professor of innovation management, The Carey Business School, Johns Hopkins University, Baltimore. He has no conflicts of interest.
A subtype of purinergic receptor on spinal microglial cells mediated visceral pain hypersensitivity in rats with chronic pancreatitis, and pharmacologic or genetic inhibition of this receptor improved hyperalgesia, according to a report in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
“Our study may be the first to identify that P2X7 receptors in spinal microglia are upregulated in chronic pancreatitis, and that this upregulation is associated with the development of visceral hyperalgesia,” said Dr. Pei-Yi Liu at National Yang-Ming University in Taipei, Taiwan, and her associates. A common laboratory dye known as brilliant blue G, which is an antagonist of P2X7R, “not only attenuated but also prevented CP-related chronic visceral hyperalgesia,” the researchers reported.
Chronic pancreatitis causes intense, recurrent epigastric pain that is “difficult and frustrating” to control and can lead to malnutrition, narcotic analgesic addiction, and social and financial problems, said the researchers. Previously, they had linked visceral pain in murine CP to activation of spinal microglia, the main effector immune cells in the central nervous system. The molecular pathways remained unclear, but some research had implicated extracellular adenosine triphosphate (ATP) as well as purinergic receptors in the CNS. Because a purine receptor subtype known as P2X7 had been linked to neuropathic and inflammatory pain, the researchers wondered if it also facilitated visceral pain (Cell Mol Gastroenterol Hepatol. 2015 Jul 22. doi: 10.1016/j.jcmgh.2015.07.008). To explore that question, they created a CP model by injecting 2% trinitrobenzene sulfonic acid into the pancreatic ducts of male rats. They measured behavioral responses to mechanical and electrical stimulation and quantified spinal cord P2X7R levels with the help of standard laboratory assays. They also watched for changes in pain-related behaviors after blocking spinal cord P2X7R with brilliant blue G or knocking it down with short interfering RNA (siRNA).
Spinal P2X7R expression rose significantly after CP induction, as did levels of the OX-42 microglial marker in the dorsal horn of the spinal cord, said the investigators. Brilliant blue G and genetic knock down suppressed P2X7R expression, inhibited activation of spinal microglia, and “significantly attenuated” nociceptive behaviors, they added.
The researchers also pretreated some rats with brilliant blue G before inducing CP and saw that these rats exhibited significantly lower pain responses to mechanical and electrical stimuli compared with other CP rats. In fact, the nociceptive responses of the pretreated CP rats resembled those of non-CP control rats, the investigators said. Spinal tissue from pretreated rats also lacked signs of P2X7R upregulation, they noted.
Taken together, the data “indicate a critical role of P2X7R expressed in the spinal cord in the development of chronic visceral pain in CP,” concluded the researchers. Brilliant blue G inhibits voltage-gated sodium channels, which are known to contribute to chronic visceral pain, and “may represent an effective drug for the treatment of chronic pain in chronic pancreatitis patients,” they added.
The study was funded by Taipei Veterans General Hospital, National Science Council of Taiwan, and the Taiwan Ministry of Education Aim for Top University Grant. The investigators declared no competing interests.
A subtype of purinergic receptor on spinal microglial cells mediated visceral pain hypersensitivity in rats with chronic pancreatitis, and pharmacologic or genetic inhibition of this receptor improved hyperalgesia, according to a report in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
“Our study may be the first to identify that P2X7 receptors in spinal microglia are upregulated in chronic pancreatitis, and that this upregulation is associated with the development of visceral hyperalgesia,” said Dr. Pei-Yi Liu at National Yang-Ming University in Taipei, Taiwan, and her associates. A common laboratory dye known as brilliant blue G, which is an antagonist of P2X7R, “not only attenuated but also prevented CP-related chronic visceral hyperalgesia,” the researchers reported.
Chronic pancreatitis causes intense, recurrent epigastric pain that is “difficult and frustrating” to control and can lead to malnutrition, narcotic analgesic addiction, and social and financial problems, said the researchers. Previously, they had linked visceral pain in murine CP to activation of spinal microglia, the main effector immune cells in the central nervous system. The molecular pathways remained unclear, but some research had implicated extracellular adenosine triphosphate (ATP) as well as purinergic receptors in the CNS. Because a purine receptor subtype known as P2X7 had been linked to neuropathic and inflammatory pain, the researchers wondered if it also facilitated visceral pain (Cell Mol Gastroenterol Hepatol. 2015 Jul 22. doi: 10.1016/j.jcmgh.2015.07.008). To explore that question, they created a CP model by injecting 2% trinitrobenzene sulfonic acid into the pancreatic ducts of male rats. They measured behavioral responses to mechanical and electrical stimulation and quantified spinal cord P2X7R levels with the help of standard laboratory assays. They also watched for changes in pain-related behaviors after blocking spinal cord P2X7R with brilliant blue G or knocking it down with short interfering RNA (siRNA).
Spinal P2X7R expression rose significantly after CP induction, as did levels of the OX-42 microglial marker in the dorsal horn of the spinal cord, said the investigators. Brilliant blue G and genetic knock down suppressed P2X7R expression, inhibited activation of spinal microglia, and “significantly attenuated” nociceptive behaviors, they added.
The researchers also pretreated some rats with brilliant blue G before inducing CP and saw that these rats exhibited significantly lower pain responses to mechanical and electrical stimuli compared with other CP rats. In fact, the nociceptive responses of the pretreated CP rats resembled those of non-CP control rats, the investigators said. Spinal tissue from pretreated rats also lacked signs of P2X7R upregulation, they noted.
Taken together, the data “indicate a critical role of P2X7R expressed in the spinal cord in the development of chronic visceral pain in CP,” concluded the researchers. Brilliant blue G inhibits voltage-gated sodium channels, which are known to contribute to chronic visceral pain, and “may represent an effective drug for the treatment of chronic pain in chronic pancreatitis patients,” they added.
The study was funded by Taipei Veterans General Hospital, National Science Council of Taiwan, and the Taiwan Ministry of Education Aim for Top University Grant. The investigators declared no competing interests.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A subtype of purinergic receptor on spinal microglial cells mediated visceral pain hypersensitivity in rats with chronic pancreatitis.
Major finding: Spinal P2X7R expression rose significantly after CP induction, and pharmacologic inhibition and genetic knock down inhibited activation of spinal microglia and “significantly attenuated” nociceptive behaviors.
Data source: Controlled, prospective, molecular and behavioral study of rats with chemically induced chronic pancreatitis.
Disclosures: The study was funded by Taipei Veterans General Hospital, National Science Council of Taiwan, and the Taiwan Ministry of Education Aim for Top University Grant. The investigators declared no competing interests.
No link found between IBS and serologic markers for celiac disease
Irritable bowel syndrome did not increase the likelihood of having serologic markers of celiac disease, according to a study of more than 3,000 residents of Southeastern Minnesota reported in the November issue of Clinical Gastroenterology and Hepatology.
Although several current guidelines list IBS as a risk factor for celiac disease, “our results suggest that testing for celiac disease [CD] in IBS will not have a significantly increased yield over population-based serologic screening,” said Dr. Rok Seon Choung of the Mayo Clinic, Rochester, Minn., and his associates. “In terms of IBS and other major GI syndromes, undetected CD does not appear to be positively associated with GI symptoms in the United States community.”
Despite widely available screening tests for CD, at least 80% of cases go undiagnosed. Testing based only on the presence of malabsorptive signs and symptoms misses many cases because of the trend toward “nonclassic” CD, said the researchers. “Physicians are especially likely to encounter patients with CD who have no classic symptoms while investigating other GI disorders,” they noted. “We aimed to determine whether positive results of serologic testing for CD by using a highly sensitive and specific assaywere associated with IBS and other functional gastrointestinal disorders in a large representative U.S. white population” (Clin Gastroenterol Hepatol. 2015 May doi: 10.1016/j.cgh.2015.05.014).
The investigators sent validated self-report bowel disease questionnaires to randomly chosen adults living in Olmsted County in Southeastern Minnesota. They also performed CD testing on serum from a convenience sample of 47,000 county residents with no prior diagnosis of CD. In all, 3,202 subjects completed questionnaires and had serum available for testing. About 55% of this group reported at least one GI symptom (95% confidence interval, 53%-57%), while 13.6% met criteria for IBS (95% CI, 12%-15%), the researchers said. A total of 1% of respondents had serologic markers for CD (95% CI, 0.7%-1.4%), in keeping with other epidemiologic studies in the United States, they added.
Notably, IBS affected only 3% of CD patients, compared with 14% of patients without CD, although the difference was not statistically significant (OR, 0.2; 95% CI, 0.03-1.5), the investigators said. Seropositive CD patients most often reported abdominal pain, constipation, weight loss, and dyspepsia, but none of these GI symptoms and no functional GI disorders were significantly more prevalent in CD patients than in non-CD patients. “These results may have important management and screening implications,” said the researchers. “Cost-effectiveness data suggest that testing for CD in patients with diarrhea-predominant IBS has an acceptable cost when the prevalence is above 1%, and becomes the dominant strategy when the prevalence exceeds 8%. However, we cannot confirm whether CD testing is a cost-effective approach in our population.”
The findings should be generalizable to white Americans, but not to the U.S. population as a whole because most participants were white, the researchers noted. “The prevalence of CD may vary by ethnic group, but the disease has been shown to be more common in whites than in other races,” they added. Responder bias was also possible, but past studies of the same bowel disease questionnaire uncovered no significant differences in rates of GI symptoms between responders and nonresponders, they noted.
The National Institutes of Health funded part of the work. Coauthor Dr. Nicholas Talley reported having colicensed the questionnaire used in the study. The remaining authors disclosed no financial conflicts.
In the well-designed and rigorous study by Choung et al., the authors conducted a community-based, cross-sectional survey among residents of Olmsted County, Minn., collecting data on symptoms compatible with functional GI disorders, including irritable bowel syndrome; the authors linked these data to prevalence surveys testing for undiagnosed celiac disease using serologic tests conducted among more than 47,000 individuals within the same regio

|
| Dr. Alexander Ford |
Patients with celiac disease may present with GI symptoms such as abdominal pain, bloating, and diarrhea, leading to confusion with IBS and diagnostic delay. Current guidelines, therefore, recommend screening patients consulting with IBS-type symptoms routinely for celiac disease. Despite this, in the study only 3% of individuals with positive celiac serology met the criteria for IBS, compared with 14% of those testing negative. Also of note is that subjects with positive serology were no more likely to report other GI symptoms felt to be typical presenting features of celiac disease, including abdominal pain, diarrhea, bloating, or abdominal distension. This suggests the yield of opportunistic screening of people reporting GI symptoms in the U.S. community is low.
However, current guidelines do not recommend screening people with IBS for celiac disease in the general population, and based their recommendations on studies conducted among patients consulting with GI symptoms. As a result, although the authors concluded, justifiably, that testing in the community is unlikely to have a significantly increased yield over population-based screening, it should not lead to a change in recommendations for practice in either primary or secondary care in other countries.
Dr. Alexander C. Ford is associate professor and honorary consultant gastroenterologist at Leeds Gastroenterology Institute, St. James’s University Hospital, and Leeds (England) Institute of Biomedical and Clinical Sciences, University of Leeds. He had no relevant financial conflicts of interest.
In the well-designed and rigorous study by Choung et al., the authors conducted a community-based, cross-sectional survey among residents of Olmsted County, Minn., collecting data on symptoms compatible with functional GI disorders, including irritable bowel syndrome; the authors linked these data to prevalence surveys testing for undiagnosed celiac disease using serologic tests conducted among more than 47,000 individuals within the same regio

|
| Dr. Alexander Ford |
Patients with celiac disease may present with GI symptoms such as abdominal pain, bloating, and diarrhea, leading to confusion with IBS and diagnostic delay. Current guidelines, therefore, recommend screening patients consulting with IBS-type symptoms routinely for celiac disease. Despite this, in the study only 3% of individuals with positive celiac serology met the criteria for IBS, compared with 14% of those testing negative. Also of note is that subjects with positive serology were no more likely to report other GI symptoms felt to be typical presenting features of celiac disease, including abdominal pain, diarrhea, bloating, or abdominal distension. This suggests the yield of opportunistic screening of people reporting GI symptoms in the U.S. community is low.
However, current guidelines do not recommend screening people with IBS for celiac disease in the general population, and based their recommendations on studies conducted among patients consulting with GI symptoms. As a result, although the authors concluded, justifiably, that testing in the community is unlikely to have a significantly increased yield over population-based screening, it should not lead to a change in recommendations for practice in either primary or secondary care in other countries.
Dr. Alexander C. Ford is associate professor and honorary consultant gastroenterologist at Leeds Gastroenterology Institute, St. James’s University Hospital, and Leeds (England) Institute of Biomedical and Clinical Sciences, University of Leeds. He had no relevant financial conflicts of interest.
In the well-designed and rigorous study by Choung et al., the authors conducted a community-based, cross-sectional survey among residents of Olmsted County, Minn., collecting data on symptoms compatible with functional GI disorders, including irritable bowel syndrome; the authors linked these data to prevalence surveys testing for undiagnosed celiac disease using serologic tests conducted among more than 47,000 individuals within the same regio

|
| Dr. Alexander Ford |
Patients with celiac disease may present with GI symptoms such as abdominal pain, bloating, and diarrhea, leading to confusion with IBS and diagnostic delay. Current guidelines, therefore, recommend screening patients consulting with IBS-type symptoms routinely for celiac disease. Despite this, in the study only 3% of individuals with positive celiac serology met the criteria for IBS, compared with 14% of those testing negative. Also of note is that subjects with positive serology were no more likely to report other GI symptoms felt to be typical presenting features of celiac disease, including abdominal pain, diarrhea, bloating, or abdominal distension. This suggests the yield of opportunistic screening of people reporting GI symptoms in the U.S. community is low.
However, current guidelines do not recommend screening people with IBS for celiac disease in the general population, and based their recommendations on studies conducted among patients consulting with GI symptoms. As a result, although the authors concluded, justifiably, that testing in the community is unlikely to have a significantly increased yield over population-based screening, it should not lead to a change in recommendations for practice in either primary or secondary care in other countries.
Dr. Alexander C. Ford is associate professor and honorary consultant gastroenterologist at Leeds Gastroenterology Institute, St. James’s University Hospital, and Leeds (England) Institute of Biomedical and Clinical Sciences, University of Leeds. He had no relevant financial conflicts of interest.
Irritable bowel syndrome did not increase the likelihood of having serologic markers of celiac disease, according to a study of more than 3,000 residents of Southeastern Minnesota reported in the November issue of Clinical Gastroenterology and Hepatology.
Although several current guidelines list IBS as a risk factor for celiac disease, “our results suggest that testing for celiac disease [CD] in IBS will not have a significantly increased yield over population-based serologic screening,” said Dr. Rok Seon Choung of the Mayo Clinic, Rochester, Minn., and his associates. “In terms of IBS and other major GI syndromes, undetected CD does not appear to be positively associated with GI symptoms in the United States community.”
Despite widely available screening tests for CD, at least 80% of cases go undiagnosed. Testing based only on the presence of malabsorptive signs and symptoms misses many cases because of the trend toward “nonclassic” CD, said the researchers. “Physicians are especially likely to encounter patients with CD who have no classic symptoms while investigating other GI disorders,” they noted. “We aimed to determine whether positive results of serologic testing for CD by using a highly sensitive and specific assaywere associated with IBS and other functional gastrointestinal disorders in a large representative U.S. white population” (Clin Gastroenterol Hepatol. 2015 May doi: 10.1016/j.cgh.2015.05.014).
The investigators sent validated self-report bowel disease questionnaires to randomly chosen adults living in Olmsted County in Southeastern Minnesota. They also performed CD testing on serum from a convenience sample of 47,000 county residents with no prior diagnosis of CD. In all, 3,202 subjects completed questionnaires and had serum available for testing. About 55% of this group reported at least one GI symptom (95% confidence interval, 53%-57%), while 13.6% met criteria for IBS (95% CI, 12%-15%), the researchers said. A total of 1% of respondents had serologic markers for CD (95% CI, 0.7%-1.4%), in keeping with other epidemiologic studies in the United States, they added.
Notably, IBS affected only 3% of CD patients, compared with 14% of patients without CD, although the difference was not statistically significant (OR, 0.2; 95% CI, 0.03-1.5), the investigators said. Seropositive CD patients most often reported abdominal pain, constipation, weight loss, and dyspepsia, but none of these GI symptoms and no functional GI disorders were significantly more prevalent in CD patients than in non-CD patients. “These results may have important management and screening implications,” said the researchers. “Cost-effectiveness data suggest that testing for CD in patients with diarrhea-predominant IBS has an acceptable cost when the prevalence is above 1%, and becomes the dominant strategy when the prevalence exceeds 8%. However, we cannot confirm whether CD testing is a cost-effective approach in our population.”
The findings should be generalizable to white Americans, but not to the U.S. population as a whole because most participants were white, the researchers noted. “The prevalence of CD may vary by ethnic group, but the disease has been shown to be more common in whites than in other races,” they added. Responder bias was also possible, but past studies of the same bowel disease questionnaire uncovered no significant differences in rates of GI symptoms between responders and nonresponders, they noted.
The National Institutes of Health funded part of the work. Coauthor Dr. Nicholas Talley reported having colicensed the questionnaire used in the study. The remaining authors disclosed no financial conflicts.
Irritable bowel syndrome did not increase the likelihood of having serologic markers of celiac disease, according to a study of more than 3,000 residents of Southeastern Minnesota reported in the November issue of Clinical Gastroenterology and Hepatology.
Although several current guidelines list IBS as a risk factor for celiac disease, “our results suggest that testing for celiac disease [CD] in IBS will not have a significantly increased yield over population-based serologic screening,” said Dr. Rok Seon Choung of the Mayo Clinic, Rochester, Minn., and his associates. “In terms of IBS and other major GI syndromes, undetected CD does not appear to be positively associated with GI symptoms in the United States community.”
Despite widely available screening tests for CD, at least 80% of cases go undiagnosed. Testing based only on the presence of malabsorptive signs and symptoms misses many cases because of the trend toward “nonclassic” CD, said the researchers. “Physicians are especially likely to encounter patients with CD who have no classic symptoms while investigating other GI disorders,” they noted. “We aimed to determine whether positive results of serologic testing for CD by using a highly sensitive and specific assaywere associated with IBS and other functional gastrointestinal disorders in a large representative U.S. white population” (Clin Gastroenterol Hepatol. 2015 May doi: 10.1016/j.cgh.2015.05.014).
The investigators sent validated self-report bowel disease questionnaires to randomly chosen adults living in Olmsted County in Southeastern Minnesota. They also performed CD testing on serum from a convenience sample of 47,000 county residents with no prior diagnosis of CD. In all, 3,202 subjects completed questionnaires and had serum available for testing. About 55% of this group reported at least one GI symptom (95% confidence interval, 53%-57%), while 13.6% met criteria for IBS (95% CI, 12%-15%), the researchers said. A total of 1% of respondents had serologic markers for CD (95% CI, 0.7%-1.4%), in keeping with other epidemiologic studies in the United States, they added.
Notably, IBS affected only 3% of CD patients, compared with 14% of patients without CD, although the difference was not statistically significant (OR, 0.2; 95% CI, 0.03-1.5), the investigators said. Seropositive CD patients most often reported abdominal pain, constipation, weight loss, and dyspepsia, but none of these GI symptoms and no functional GI disorders were significantly more prevalent in CD patients than in non-CD patients. “These results may have important management and screening implications,” said the researchers. “Cost-effectiveness data suggest that testing for CD in patients with diarrhea-predominant IBS has an acceptable cost when the prevalence is above 1%, and becomes the dominant strategy when the prevalence exceeds 8%. However, we cannot confirm whether CD testing is a cost-effective approach in our population.”
The findings should be generalizable to white Americans, but not to the U.S. population as a whole because most participants were white, the researchers noted. “The prevalence of CD may vary by ethnic group, but the disease has been shown to be more common in whites than in other races,” they added. Responder bias was also possible, but past studies of the same bowel disease questionnaire uncovered no significant differences in rates of GI symptoms between responders and nonresponders, they noted.
The National Institutes of Health funded part of the work. Coauthor Dr. Nicholas Talley reported having colicensed the questionnaire used in the study. The remaining authors disclosed no financial conflicts.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Irritable bowel syndrome did not increase the likelihood of seropositivity for celiac disease.
Major finding: Patients with IBS were no more likely than others to have serologic markers for celiac disease (odds ratio, 0.2; 95% confidence interval, 0.03-1.5).
Data source: An analysis of bowel symptom surveys and serum samples from 3,202 residents of one county.
Disclosures: The National Institutes of Health funded part of the work. Coauthor Dr. Nicholas Talley reported having colicensed the questionnaire used in the study. The remaining authors disclosed no conflicts.
Low-FODMAP and traditional IBS diets found equally effective for symptom reduction
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
FROM GASTROENTEROLOGY
Key clinical point: Diets low in fermentable short-chain carbohydrates cut irritable bowel disease symptoms as effectively as did “traditional” IBS diets.
Major finding: After 4 weeks, patients in both groups experienced similar and significant (P < .0001) decreases in IBS symptoms.
Data source: A randomized, multicenter, parallel-group, single-blinded study of 75 patients.
Disclosures: The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
Low-FODMAP and traditional IBS diets found equally effective for symptom reduction
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
Advising patients with irritable bowel syndrome to cut their intake of fermentable short-chain carbohydrates improved GI symptoms as much as “traditional” recommendations to reduce meal size, gas-producing foods, insoluble fiber, fat, and caffeine, investigators reported in a randomized, multicenter, single-blinded study that appears in the November issue of Gastroenterology.
“Combining elements from these two strategies might further reduce symptoms of IBS,” said Lena Böhn, a registered dietician at the University of Gothenburg (Sweden) and her associates. Clinicians, however, should be aware that patients may cut calories in response to dietary advice even if they do not need to do so, which could eventually lead to malnutrition. “Monitoring calorie and nutrient intake in patients who follow dietary advice seems important,” the investigators wrote.
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) such as apples, beans, white bread, and milk are poorly absorbed in the small intestine, which can trigger bouts of gas from colonic bacterial fermentation and diarrhea because of osmotic water transfer into the lumen of the colon. Several recent studies had linked FODMAPs to GI symptoms in IBS, but no prior randomized controlled trial had compared real-world recommendations to follow either a low-FODMAP or traditional IBS diet, the researchers noted (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
For the study, they randomized 75 patients who met Rome III IBS criteria to either the low-FODMAP or traditional IBS diet for 4 weeks. They used the IBS severity scoring system (Aliment Pharmacol Ther. 1997;11[2]:395-402) to assess symptomatic response and studied food diaries completed before and after the interventions to understand how closely patients followed the dietary advice.
A total of 67 patients completed the study, including 56 women and 14 men, Ms. Böhn and her associates reported. Both diets led to similarly significant (P < .0001) decreases in IBS symptoms, with no clear differences between them. Half the patients in the low-FODMAP group experienced at least a 50-point improvement in their IBS severity score, compared with 46% of patients in the traditional IBS diet cohort (P = .72).
Food diaries showed that patients adhered well to their diets, the investigators said, but “an unwanted and somewhat surprising finding” was that patients cut their caloric intake – by an average of 442 kcal/day on the low-FODMAP diet and almost 200 kcal/day on the traditional diet. “We hypothesize that even though patients were not advised to reduce calorie intake, receiving detailed dietary advice [to] limit intake of certain food constituents may result in this unwanted effect,” said the investigators. “In the short term, this should not be harmful, but a lesson from this trial is that calorie and nutrient intake needs to be supervised in order to avoid malnutrition if long-term dietary changes are initiated.”
The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
FROM GASTROENTEROLOGY
Key clinical point: Diets low in fermentable short-chain carbohydrates cut irritable bowel disease symptoms as effectively as did “traditional” IBS diets.
Major finding: After 4 weeks, patients in both groups experienced similar and significant (P < .0001) decreases in IBS symptoms.
Data source: A randomized, multicenter, parallel-group, single-blinded study of 75 patients.
Disclosures: The study was supported by the Swedish Medical Research Council and by the University of Gothenburg’s Marianne and Marcus Wallenberg Foundation, Centre for Person-Centered Care, and Faculty of Medicine. The investigators declared no competing interests.
No link found between immunosuppression and anal dysplasia in IBD
Immunosuppression did not affect the probability of abnormal anal cytology among patients with inflammatory bowel disease (IBD), according to a prospective, single-center, cross-sectional study of 270 adults published in the November issue of Clinical Gastroenterology and Hepatology.
“Although our study suggested that immunosuppression may not play a role in the risk of dysplasia, a question remains as to whether it contributes to malignant transformation in patients with dysplasia. More research needs to be performed to identify the utility of wider anal dysplasia screening programs in high-risk populations, and the role of HPV vaccine in prevention,” Dr. Shamita Shah of Stanford (Calif.) University and her associates wrote in Clinical Gastroenterology and Hepatology.
Immunosuppression is a cornerstone of IBD management. Because immunosuppressive medications inhibit cell-mediated immunity, patients are at increased risk of opportunistic infections and neoplasias, the researchers noted. One study reported a greater risk of cervical dysplasia among immunosuppressed women with IBD, but the risk of anal dysplasia and cancer in IBD has not been well studied, they said (Clinical Gasteroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.05.031).
To examine associations between anal dysplasia and IBD, human papillomavirus infection, and immunosuppression, the researchers analyzed anal Pap tests from 100 IBD patients who were immunosuppressed, 94 IBD patients who were not immunosuppressed, and 76 healthy controls. They identified 19 cases of atypical squamous cells of undetermined significance (ASCUS). The prevalence of ASCUS was somewhat higher among IBD patients (8.8%) than controls (2.6%; P = 0.1), but did not vary based on immunosuppression status or HPV infection. High-risk HPV occurred in 2% of the entire cohort, including 11% of patients with ASCUS and 1.5% of patients with normal Pap cytology (P = .01). High-resolution anoscopy of six patients with ASCUS revealed two cases of condylomatous disease, but no biopsy-positive dysplasia, the investigators reported.
Patients with Crohn’s disease had a significantly higher prevalence of ASCUS than other study participants (P = .02), but patients with ulcerative colitis or unspecified IBD did not, said the researchers. Having had Crohn’s disease for at least 10 years was associated with a fivefold increase in the odds of ASCUS in the multivariate analysis (95% confidence interval, 1.9-13.6), and female sex was also a risk factor (odds ratio, 3.3; P = .047). Notably, women with long-standing Crohn’s disease were almost five times more likely to have abnormal anal Pap cytology than other subjects (P = .0038), the investigators said. “One proposed mechanism for this was a reduction in human defensins in Crohn’s disease patients,” they added. Defensins – antiviral proteins that are found in immune cells – are known to inhibit cutaneous and mucosal HPV, and can be decreased in patients with Crohn’s disease for several reasons, they said. “Although more research is needed in this area, the hindered ability for an IBD patient to defend against viral illness may be responsible for their susceptibility to HPV-related cervical and anal neoplasias.”
Hologic donated the anal Pap tests used in the study. The researchers disclosed no conflicts of interest.
Immunosuppression did not affect the probability of abnormal anal cytology among patients with inflammatory bowel disease (IBD), according to a prospective, single-center, cross-sectional study of 270 adults published in the November issue of Clinical Gastroenterology and Hepatology.
“Although our study suggested that immunosuppression may not play a role in the risk of dysplasia, a question remains as to whether it contributes to malignant transformation in patients with dysplasia. More research needs to be performed to identify the utility of wider anal dysplasia screening programs in high-risk populations, and the role of HPV vaccine in prevention,” Dr. Shamita Shah of Stanford (Calif.) University and her associates wrote in Clinical Gastroenterology and Hepatology.
Immunosuppression is a cornerstone of IBD management. Because immunosuppressive medications inhibit cell-mediated immunity, patients are at increased risk of opportunistic infections and neoplasias, the researchers noted. One study reported a greater risk of cervical dysplasia among immunosuppressed women with IBD, but the risk of anal dysplasia and cancer in IBD has not been well studied, they said (Clinical Gasteroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.05.031).
To examine associations between anal dysplasia and IBD, human papillomavirus infection, and immunosuppression, the researchers analyzed anal Pap tests from 100 IBD patients who were immunosuppressed, 94 IBD patients who were not immunosuppressed, and 76 healthy controls. They identified 19 cases of atypical squamous cells of undetermined significance (ASCUS). The prevalence of ASCUS was somewhat higher among IBD patients (8.8%) than controls (2.6%; P = 0.1), but did not vary based on immunosuppression status or HPV infection. High-risk HPV occurred in 2% of the entire cohort, including 11% of patients with ASCUS and 1.5% of patients with normal Pap cytology (P = .01). High-resolution anoscopy of six patients with ASCUS revealed two cases of condylomatous disease, but no biopsy-positive dysplasia, the investigators reported.
Patients with Crohn’s disease had a significantly higher prevalence of ASCUS than other study participants (P = .02), but patients with ulcerative colitis or unspecified IBD did not, said the researchers. Having had Crohn’s disease for at least 10 years was associated with a fivefold increase in the odds of ASCUS in the multivariate analysis (95% confidence interval, 1.9-13.6), and female sex was also a risk factor (odds ratio, 3.3; P = .047). Notably, women with long-standing Crohn’s disease were almost five times more likely to have abnormal anal Pap cytology than other subjects (P = .0038), the investigators said. “One proposed mechanism for this was a reduction in human defensins in Crohn’s disease patients,” they added. Defensins – antiviral proteins that are found in immune cells – are known to inhibit cutaneous and mucosal HPV, and can be decreased in patients with Crohn’s disease for several reasons, they said. “Although more research is needed in this area, the hindered ability for an IBD patient to defend against viral illness may be responsible for their susceptibility to HPV-related cervical and anal neoplasias.”
Hologic donated the anal Pap tests used in the study. The researchers disclosed no conflicts of interest.
Immunosuppression did not affect the probability of abnormal anal cytology among patients with inflammatory bowel disease (IBD), according to a prospective, single-center, cross-sectional study of 270 adults published in the November issue of Clinical Gastroenterology and Hepatology.
“Although our study suggested that immunosuppression may not play a role in the risk of dysplasia, a question remains as to whether it contributes to malignant transformation in patients with dysplasia. More research needs to be performed to identify the utility of wider anal dysplasia screening programs in high-risk populations, and the role of HPV vaccine in prevention,” Dr. Shamita Shah of Stanford (Calif.) University and her associates wrote in Clinical Gastroenterology and Hepatology.
Immunosuppression is a cornerstone of IBD management. Because immunosuppressive medications inhibit cell-mediated immunity, patients are at increased risk of opportunistic infections and neoplasias, the researchers noted. One study reported a greater risk of cervical dysplasia among immunosuppressed women with IBD, but the risk of anal dysplasia and cancer in IBD has not been well studied, they said (Clinical Gasteroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.05.031).
To examine associations between anal dysplasia and IBD, human papillomavirus infection, and immunosuppression, the researchers analyzed anal Pap tests from 100 IBD patients who were immunosuppressed, 94 IBD patients who were not immunosuppressed, and 76 healthy controls. They identified 19 cases of atypical squamous cells of undetermined significance (ASCUS). The prevalence of ASCUS was somewhat higher among IBD patients (8.8%) than controls (2.6%; P = 0.1), but did not vary based on immunosuppression status or HPV infection. High-risk HPV occurred in 2% of the entire cohort, including 11% of patients with ASCUS and 1.5% of patients with normal Pap cytology (P = .01). High-resolution anoscopy of six patients with ASCUS revealed two cases of condylomatous disease, but no biopsy-positive dysplasia, the investigators reported.
Patients with Crohn’s disease had a significantly higher prevalence of ASCUS than other study participants (P = .02), but patients with ulcerative colitis or unspecified IBD did not, said the researchers. Having had Crohn’s disease for at least 10 years was associated with a fivefold increase in the odds of ASCUS in the multivariate analysis (95% confidence interval, 1.9-13.6), and female sex was also a risk factor (odds ratio, 3.3; P = .047). Notably, women with long-standing Crohn’s disease were almost five times more likely to have abnormal anal Pap cytology than other subjects (P = .0038), the investigators said. “One proposed mechanism for this was a reduction in human defensins in Crohn’s disease patients,” they added. Defensins – antiviral proteins that are found in immune cells – are known to inhibit cutaneous and mucosal HPV, and can be decreased in patients with Crohn’s disease for several reasons, they said. “Although more research is needed in this area, the hindered ability for an IBD patient to defend against viral illness may be responsible for their susceptibility to HPV-related cervical and anal neoplasias.”
Hologic donated the anal Pap tests used in the study. The researchers disclosed no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Immunosuppression did not affect the probability of abnormal anal cytology among patients with inflammatory bowel disease.
Major finding: Almost 9% of patients had atypical squamous cells on anal Pap testing, with no difference in prevalence based on immunosuppression.
Data source: A prospective, single-center, cross-sectional study of 270 subjects.
Disclosures: Hologic donated the anal Pap tests used in the study. The researchers disclosed no conflicts of interest.
Experts debate fecal transplants as first-line therapy for CDI
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.

|
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.

|
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.

|
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.
EXPERT ANALYSIS AT IDWEEK 2015
IDWeek: EV-D68 found more virulent but not more deadly in children
SAN DIEGO – Enterovirus D68 appeared more virulent – but not more lethal – than rhinovirus and other strains of enterovirus among children, said the authors of a single-center study.
The pulmonary pathogen was linked to higher rates of respiratory distress, hospital admission, and magnesium sulfate therapy, but patients were no more likely to die or require critical care unit admission than were those infected with other EV genotypes or rhinovirus, said Dr. Dominik Mertz of the division of infectious diseases at McMaster University, in Hamilton, Ont.
The study also uncovered no evidence of EV-68 transmission at the hospital, Dr. Mertz and his associates said at an annual scientific meeting on infectious diseases.
In 2014, an outbreak of EV-D68 in the United States included more than 1,000 confirmed cases, almost all among children, and many of whom had comorbid asthma or a history of wheezing. Fourteen patients died, and the Centers for Disease Control and Prevention noted that millions more individuals probably had milder EV-D68 infections for which they were never tested.
Dr. Mertz and his associates studied children who presented consecutively to the hospital during the 3 months between Aug. 1 and Oct. 31, 2014. During that time, nasopharyngeal swabs that were positive for EV or rhinovirus were automatically tested for EV-D68. The researchers matched EV-D68–positive patients with children who were positive for rhinovirus or other EVs on the basis of sex, age, and date of presentation to the hospital.
Almost a third (93 of 297; 31%) of rhinovirus or EV samples were positive for EV-D68. Among 87 matched pairs, EV-D68 infection was associated with a threefold greater odds of respiratory distress (95% confidence interval, 1.47-6.14), and a more than twofold rise in the odds of needing magnesium sulfate therapy (odds ratio, 2.62; 95% CI, 1.06-6.47). There was a trend toward greater risk of hospital admission with EV-D68, although it was not statistically significant (OR, 2.29; 95% CI, 0.96-5.46; P = .06).
Notably, EV-68 did not increase the likelihood of death or CCU admission, while, influenza causes dozens of deaths among children in the United States every year, Dr. Mertz and his coinvestigator Dr. Jeffrey Pernica noted in an interview (MMWR. 2014 Jun 6:63[22];483-90). Studies have yet to compare the morbidity and mortality burdens of influenza, respiratory syncytial virus, and EV-D68, and they would like to do so, they said.
“There was a lot of fuss made about EV-D68,” said Dr. Mertz. “But we have flu every year, and many more kids get the flu and die of flu than EV-D68.”
Patients with EV-D68 infection were more likely than others to have a family history of atopy (OR, 2.25) and a personal history of asthma or wheezing (OR, 1.77), hay fever (1.22), and eosinophilia (4.5), although none of these associations reached statistical significance, the investigators reported. “It seems reasonable to hypothesize that EV-D68 is a more virulent pulmonary pathogen to those with preexisting atopic disease than other rhinoviruses and enteroviruses,” Dr. Mertz and his associates wrote in an associated article (CMAJ. 2015 Oct. 13. doi: 10.1503/cmaj.150619). “We can hypothesize that these children are more likely to have respiratory distress because of the combination of allergy and EV-D68, but why the same doesn’t hold true for rhinovirus or other enterovirus strains, we don’t know,” Dr. Mertz said.
The investigators received no funding for the study and reported no conflicts of interest.
SAN DIEGO – Enterovirus D68 appeared more virulent – but not more lethal – than rhinovirus and other strains of enterovirus among children, said the authors of a single-center study.
The pulmonary pathogen was linked to higher rates of respiratory distress, hospital admission, and magnesium sulfate therapy, but patients were no more likely to die or require critical care unit admission than were those infected with other EV genotypes or rhinovirus, said Dr. Dominik Mertz of the division of infectious diseases at McMaster University, in Hamilton, Ont.
The study also uncovered no evidence of EV-68 transmission at the hospital, Dr. Mertz and his associates said at an annual scientific meeting on infectious diseases.
In 2014, an outbreak of EV-D68 in the United States included more than 1,000 confirmed cases, almost all among children, and many of whom had comorbid asthma or a history of wheezing. Fourteen patients died, and the Centers for Disease Control and Prevention noted that millions more individuals probably had milder EV-D68 infections for which they were never tested.
Dr. Mertz and his associates studied children who presented consecutively to the hospital during the 3 months between Aug. 1 and Oct. 31, 2014. During that time, nasopharyngeal swabs that were positive for EV or rhinovirus were automatically tested for EV-D68. The researchers matched EV-D68–positive patients with children who were positive for rhinovirus or other EVs on the basis of sex, age, and date of presentation to the hospital.
Almost a third (93 of 297; 31%) of rhinovirus or EV samples were positive for EV-D68. Among 87 matched pairs, EV-D68 infection was associated with a threefold greater odds of respiratory distress (95% confidence interval, 1.47-6.14), and a more than twofold rise in the odds of needing magnesium sulfate therapy (odds ratio, 2.62; 95% CI, 1.06-6.47). There was a trend toward greater risk of hospital admission with EV-D68, although it was not statistically significant (OR, 2.29; 95% CI, 0.96-5.46; P = .06).
Notably, EV-68 did not increase the likelihood of death or CCU admission, while, influenza causes dozens of deaths among children in the United States every year, Dr. Mertz and his coinvestigator Dr. Jeffrey Pernica noted in an interview (MMWR. 2014 Jun 6:63[22];483-90). Studies have yet to compare the morbidity and mortality burdens of influenza, respiratory syncytial virus, and EV-D68, and they would like to do so, they said.
“There was a lot of fuss made about EV-D68,” said Dr. Mertz. “But we have flu every year, and many more kids get the flu and die of flu than EV-D68.”
Patients with EV-D68 infection were more likely than others to have a family history of atopy (OR, 2.25) and a personal history of asthma or wheezing (OR, 1.77), hay fever (1.22), and eosinophilia (4.5), although none of these associations reached statistical significance, the investigators reported. “It seems reasonable to hypothesize that EV-D68 is a more virulent pulmonary pathogen to those with preexisting atopic disease than other rhinoviruses and enteroviruses,” Dr. Mertz and his associates wrote in an associated article (CMAJ. 2015 Oct. 13. doi: 10.1503/cmaj.150619). “We can hypothesize that these children are more likely to have respiratory distress because of the combination of allergy and EV-D68, but why the same doesn’t hold true for rhinovirus or other enterovirus strains, we don’t know,” Dr. Mertz said.
The investigators received no funding for the study and reported no conflicts of interest.
SAN DIEGO – Enterovirus D68 appeared more virulent – but not more lethal – than rhinovirus and other strains of enterovirus among children, said the authors of a single-center study.
The pulmonary pathogen was linked to higher rates of respiratory distress, hospital admission, and magnesium sulfate therapy, but patients were no more likely to die or require critical care unit admission than were those infected with other EV genotypes or rhinovirus, said Dr. Dominik Mertz of the division of infectious diseases at McMaster University, in Hamilton, Ont.
The study also uncovered no evidence of EV-68 transmission at the hospital, Dr. Mertz and his associates said at an annual scientific meeting on infectious diseases.
In 2014, an outbreak of EV-D68 in the United States included more than 1,000 confirmed cases, almost all among children, and many of whom had comorbid asthma or a history of wheezing. Fourteen patients died, and the Centers for Disease Control and Prevention noted that millions more individuals probably had milder EV-D68 infections for which they were never tested.
Dr. Mertz and his associates studied children who presented consecutively to the hospital during the 3 months between Aug. 1 and Oct. 31, 2014. During that time, nasopharyngeal swabs that were positive for EV or rhinovirus were automatically tested for EV-D68. The researchers matched EV-D68–positive patients with children who were positive for rhinovirus or other EVs on the basis of sex, age, and date of presentation to the hospital.
Almost a third (93 of 297; 31%) of rhinovirus or EV samples were positive for EV-D68. Among 87 matched pairs, EV-D68 infection was associated with a threefold greater odds of respiratory distress (95% confidence interval, 1.47-6.14), and a more than twofold rise in the odds of needing magnesium sulfate therapy (odds ratio, 2.62; 95% CI, 1.06-6.47). There was a trend toward greater risk of hospital admission with EV-D68, although it was not statistically significant (OR, 2.29; 95% CI, 0.96-5.46; P = .06).
Notably, EV-68 did not increase the likelihood of death or CCU admission, while, influenza causes dozens of deaths among children in the United States every year, Dr. Mertz and his coinvestigator Dr. Jeffrey Pernica noted in an interview (MMWR. 2014 Jun 6:63[22];483-90). Studies have yet to compare the morbidity and mortality burdens of influenza, respiratory syncytial virus, and EV-D68, and they would like to do so, they said.
“There was a lot of fuss made about EV-D68,” said Dr. Mertz. “But we have flu every year, and many more kids get the flu and die of flu than EV-D68.”
Patients with EV-D68 infection were more likely than others to have a family history of atopy (OR, 2.25) and a personal history of asthma or wheezing (OR, 1.77), hay fever (1.22), and eosinophilia (4.5), although none of these associations reached statistical significance, the investigators reported. “It seems reasonable to hypothesize that EV-D68 is a more virulent pulmonary pathogen to those with preexisting atopic disease than other rhinoviruses and enteroviruses,” Dr. Mertz and his associates wrote in an associated article (CMAJ. 2015 Oct. 13. doi: 10.1503/cmaj.150619). “We can hypothesize that these children are more likely to have respiratory distress because of the combination of allergy and EV-D68, but why the same doesn’t hold true for rhinovirus or other enterovirus strains, we don’t know,” Dr. Mertz said.
The investigators received no funding for the study and reported no conflicts of interest.
AT IDWEEK 2015
Key clinical point: Enterovirus D68 was more virulent – but not more lethal – than other strains of EV and rhinovirus.
Major finding: Among 87 matched pairs, EV-D68 infection was associated with a threefold greater odds of respiratory distress (95% CI, 1.47-6.14), and a more than twofold rise in the odds of needing magnesium sulfate therapy (OR, 2.62; 95% CI, 1.06-6.47).
Data source: Matched cohort study of 87 pairs of children seen at one hospital during August-October 2014.
Disclosures: The study received no funding. The investigators reported having no conflicts of interest.
Experts debate infection control merits of ‘bare beneath the elbows’
SAN DIEGO – Going tieless and “bare beneath the elbows” has been touted for infection control. But while some clinicians endorse the practice, others call it inconvenient, unprofessional, and distracting. At an annual conference on infectious diseases, two specialists in the field debated going “BBE” and its evidence base.
Widespread practice of BBE dates to at least 2008, when the National Health Service in the United Kingdom mandated it as part of a set of measures to decrease nosocomial transmission of methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile. Clinicians at NHS were directed to leave jewelry, neckties, and wrist watches at home, hang up their lab coats, and wear short sleeves. The policy aims not only to reduce points of physical contact between providers and patients, but also to improve hand and wrist washing, said Dr. Michael Edmond, who is at the University of Iowa Hospitals and Clinics in Iowa City.
Some evidence supports going BBE, said Dr. Edmond. Pathogenic gram-negative rods have been cultured from neckties, scrubs, uniforms, and white coats in multiple studies, he added. Inadequate laundering is part of the problem – clinical faculty in one study reported washing their coats about once every 2 weeks, even less often than medical students did.
“So when is biological plausibility enough to support a change in practice?” Dr. Edmond asked. “There is a potential for benefit in going BBE. There is no risk for harm. And there is minimal cost. On the basis of the same evidence and assumptions, we are willing to wrap ourselves in plastic and confine patients to their hospital rooms – that is, to use contact precautions. And yet, we are not willing to eliminate white coats and ties.”
Patient perception is not at issue, Dr. Edmond argued. Only about half of patients at one British hospital said they wanted physicians to wear traditional white coats, and that proportion dropped to 22% after patients received educational materials on clothing contamination, he noted. In another study, patients ranked their physician’s appearance behind knowledge, compassion, and politeness when asked which characteristics they valued most.
“Without strong evidence for benefit, we should recommend – not mandate – this new practice,” Dr. Edmond concluded.
But Dr. Neil O. Fishman disagreed, calling BBE “an evidence-free zone.” Dr. Fishman, who is at the University of Pennsylvania in Philadelphia, noted a total lack of randomized, controlled trials or well-performed observational studies supporting BBE. “No clinical studies have demonstrated cross-transmission of health care–associated pathogens from a health care provider to a patient,” he said.
Moreover, BBE does not prevent contamination, Dr. Fishman said. Bacterial cultures of the hands of BBE clinicians and controls revealed no differences in total bacteria counts or numbers of clinically significant pathogens, he said. Cultures of white coats and the undersides of wrists also were similar in terms of total bacteria and MRSA counts, he added.
Despite the lack of evidence, BBE has been implemented at NHS “mainly as a political gesture and has had unintended consequences,” Dr. Fishman said. Informal attire has promoted a less-robust view of infection control, junior doctors have adopted scruffy attire and “slovenly” personal hygiene, and all the focus on clothing has distracted from hand washing, he added.
Furthermore, less than 12% of clinicians have complied with BBE, according to Dr. Fishman. Abstainers report feeling cold and not knowing what time it is. Women, in particular, say they have no pockets to carry work essentials. “This is a gender equity issue,” Dr. Fishman said. “Can we afford to promote practices based on limited evidence, a theoretical rationale, or individual opinions? This is a lack of focus on what really matters.”
Dr. Edmond and Dr. Fishman reported no disclosures.
SAN DIEGO – Going tieless and “bare beneath the elbows” has been touted for infection control. But while some clinicians endorse the practice, others call it inconvenient, unprofessional, and distracting. At an annual conference on infectious diseases, two specialists in the field debated going “BBE” and its evidence base.
Widespread practice of BBE dates to at least 2008, when the National Health Service in the United Kingdom mandated it as part of a set of measures to decrease nosocomial transmission of methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile. Clinicians at NHS were directed to leave jewelry, neckties, and wrist watches at home, hang up their lab coats, and wear short sleeves. The policy aims not only to reduce points of physical contact between providers and patients, but also to improve hand and wrist washing, said Dr. Michael Edmond, who is at the University of Iowa Hospitals and Clinics in Iowa City.
Some evidence supports going BBE, said Dr. Edmond. Pathogenic gram-negative rods have been cultured from neckties, scrubs, uniforms, and white coats in multiple studies, he added. Inadequate laundering is part of the problem – clinical faculty in one study reported washing their coats about once every 2 weeks, even less often than medical students did.
“So when is biological plausibility enough to support a change in practice?” Dr. Edmond asked. “There is a potential for benefit in going BBE. There is no risk for harm. And there is minimal cost. On the basis of the same evidence and assumptions, we are willing to wrap ourselves in plastic and confine patients to their hospital rooms – that is, to use contact precautions. And yet, we are not willing to eliminate white coats and ties.”
Patient perception is not at issue, Dr. Edmond argued. Only about half of patients at one British hospital said they wanted physicians to wear traditional white coats, and that proportion dropped to 22% after patients received educational materials on clothing contamination, he noted. In another study, patients ranked their physician’s appearance behind knowledge, compassion, and politeness when asked which characteristics they valued most.
“Without strong evidence for benefit, we should recommend – not mandate – this new practice,” Dr. Edmond concluded.
But Dr. Neil O. Fishman disagreed, calling BBE “an evidence-free zone.” Dr. Fishman, who is at the University of Pennsylvania in Philadelphia, noted a total lack of randomized, controlled trials or well-performed observational studies supporting BBE. “No clinical studies have demonstrated cross-transmission of health care–associated pathogens from a health care provider to a patient,” he said.
Moreover, BBE does not prevent contamination, Dr. Fishman said. Bacterial cultures of the hands of BBE clinicians and controls revealed no differences in total bacteria counts or numbers of clinically significant pathogens, he said. Cultures of white coats and the undersides of wrists also were similar in terms of total bacteria and MRSA counts, he added.
Despite the lack of evidence, BBE has been implemented at NHS “mainly as a political gesture and has had unintended consequences,” Dr. Fishman said. Informal attire has promoted a less-robust view of infection control, junior doctors have adopted scruffy attire and “slovenly” personal hygiene, and all the focus on clothing has distracted from hand washing, he added.
Furthermore, less than 12% of clinicians have complied with BBE, according to Dr. Fishman. Abstainers report feeling cold and not knowing what time it is. Women, in particular, say they have no pockets to carry work essentials. “This is a gender equity issue,” Dr. Fishman said. “Can we afford to promote practices based on limited evidence, a theoretical rationale, or individual opinions? This is a lack of focus on what really matters.”
Dr. Edmond and Dr. Fishman reported no disclosures.
SAN DIEGO – Going tieless and “bare beneath the elbows” has been touted for infection control. But while some clinicians endorse the practice, others call it inconvenient, unprofessional, and distracting. At an annual conference on infectious diseases, two specialists in the field debated going “BBE” and its evidence base.
Widespread practice of BBE dates to at least 2008, when the National Health Service in the United Kingdom mandated it as part of a set of measures to decrease nosocomial transmission of methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile. Clinicians at NHS were directed to leave jewelry, neckties, and wrist watches at home, hang up their lab coats, and wear short sleeves. The policy aims not only to reduce points of physical contact between providers and patients, but also to improve hand and wrist washing, said Dr. Michael Edmond, who is at the University of Iowa Hospitals and Clinics in Iowa City.
Some evidence supports going BBE, said Dr. Edmond. Pathogenic gram-negative rods have been cultured from neckties, scrubs, uniforms, and white coats in multiple studies, he added. Inadequate laundering is part of the problem – clinical faculty in one study reported washing their coats about once every 2 weeks, even less often than medical students did.
“So when is biological plausibility enough to support a change in practice?” Dr. Edmond asked. “There is a potential for benefit in going BBE. There is no risk for harm. And there is minimal cost. On the basis of the same evidence and assumptions, we are willing to wrap ourselves in plastic and confine patients to their hospital rooms – that is, to use contact precautions. And yet, we are not willing to eliminate white coats and ties.”
Patient perception is not at issue, Dr. Edmond argued. Only about half of patients at one British hospital said they wanted physicians to wear traditional white coats, and that proportion dropped to 22% after patients received educational materials on clothing contamination, he noted. In another study, patients ranked their physician’s appearance behind knowledge, compassion, and politeness when asked which characteristics they valued most.
“Without strong evidence for benefit, we should recommend – not mandate – this new practice,” Dr. Edmond concluded.
But Dr. Neil O. Fishman disagreed, calling BBE “an evidence-free zone.” Dr. Fishman, who is at the University of Pennsylvania in Philadelphia, noted a total lack of randomized, controlled trials or well-performed observational studies supporting BBE. “No clinical studies have demonstrated cross-transmission of health care–associated pathogens from a health care provider to a patient,” he said.
Moreover, BBE does not prevent contamination, Dr. Fishman said. Bacterial cultures of the hands of BBE clinicians and controls revealed no differences in total bacteria counts or numbers of clinically significant pathogens, he said. Cultures of white coats and the undersides of wrists also were similar in terms of total bacteria and MRSA counts, he added.
Despite the lack of evidence, BBE has been implemented at NHS “mainly as a political gesture and has had unintended consequences,” Dr. Fishman said. Informal attire has promoted a less-robust view of infection control, junior doctors have adopted scruffy attire and “slovenly” personal hygiene, and all the focus on clothing has distracted from hand washing, he added.
Furthermore, less than 12% of clinicians have complied with BBE, according to Dr. Fishman. Abstainers report feeling cold and not knowing what time it is. Women, in particular, say they have no pockets to carry work essentials. “This is a gender equity issue,” Dr. Fishman said. “Can we afford to promote practices based on limited evidence, a theoretical rationale, or individual opinions? This is a lack of focus on what really matters.”
Dr. Edmond and Dr. Fishman reported no disclosures.
EXPERT ANALYSIS AT IDWEEK 2015
IDWEEK: Smother and pull, but don’t chop – how to identify and remove botfly larvae
SAN DIEGO – Identifying a botfly infestation can be the toughest part of treating it. It’s not uncommon for travelers to return from Costa Rica, Belize, and other Central and South American countries with Dermatobia hominis infestations, but clinicians in North America are not necessarily comfortable diagnosing them or removing the larvae,, said Dr. Susan McLellan, who explained how to do so at an annual scientific meeting on infectious diseases.
Clinicians here may confuse botfly infestations with infected sebaceous cysts, staphylococcal infections, cellulitis, or even cutaneous leismaniasis. To make the diagnosis, ask about travel history in patients who present with painful furuncular lesions, said Dr. McLellan, associate professor of clinical medicine at Tulane University, New Orleans.
Closer inspection of these lesions may reveal the two dark spiracles, or breathing holes, of the larvae, which are key to removing them, Dr. Mclellan added. “The larvae have to stick their little spiracles out to breathe,” she said. “You can get them to come further out by covering up these breathing holes with anything occlusive. It can be peanut butter. It can be petroleum jelly. Just cover them up until they stick themselves out more, and then you can grab them and pull them out.”
The “first smother, then pull” approach does not always work with botfly larvae because they have spines on their bodies that can hook into subepidermal tissue, Dr. McLellan noted. “Sometimes you have to make a very, very careful incision,” she said. “Do not incise the larva at all, though. Just pop it out. These lesions do not get superinfected unless you chop up the larva while they are still inside.”
Also do not bother asking patients if they were bitten by the black adult botfly, said Dr. McLellan. Adult D. hominis do not bite, but instead lay their eggs on mosquitos. “Any biting insect that flies could potentially be a carrier,” Dr. McLellan noted. “The mother botfly catches the other flying insect, dumps her eggs on it, and that other insect starts delivering them.” A single mosquito bite can transfer several botfly eggs to a human host. When the larvae hatch and burrow into the skin, they cause pain, redness, and swelling until removed.
Dr. McLellan spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no conflicts of interest.
SAN DIEGO – Identifying a botfly infestation can be the toughest part of treating it. It’s not uncommon for travelers to return from Costa Rica, Belize, and other Central and South American countries with Dermatobia hominis infestations, but clinicians in North America are not necessarily comfortable diagnosing them or removing the larvae,, said Dr. Susan McLellan, who explained how to do so at an annual scientific meeting on infectious diseases.
Clinicians here may confuse botfly infestations with infected sebaceous cysts, staphylococcal infections, cellulitis, or even cutaneous leismaniasis. To make the diagnosis, ask about travel history in patients who present with painful furuncular lesions, said Dr. McLellan, associate professor of clinical medicine at Tulane University, New Orleans.
Closer inspection of these lesions may reveal the two dark spiracles, or breathing holes, of the larvae, which are key to removing them, Dr. Mclellan added. “The larvae have to stick their little spiracles out to breathe,” she said. “You can get them to come further out by covering up these breathing holes with anything occlusive. It can be peanut butter. It can be petroleum jelly. Just cover them up until they stick themselves out more, and then you can grab them and pull them out.”
The “first smother, then pull” approach does not always work with botfly larvae because they have spines on their bodies that can hook into subepidermal tissue, Dr. McLellan noted. “Sometimes you have to make a very, very careful incision,” she said. “Do not incise the larva at all, though. Just pop it out. These lesions do not get superinfected unless you chop up the larva while they are still inside.”
Also do not bother asking patients if they were bitten by the black adult botfly, said Dr. McLellan. Adult D. hominis do not bite, but instead lay their eggs on mosquitos. “Any biting insect that flies could potentially be a carrier,” Dr. McLellan noted. “The mother botfly catches the other flying insect, dumps her eggs on it, and that other insect starts delivering them.” A single mosquito bite can transfer several botfly eggs to a human host. When the larvae hatch and burrow into the skin, they cause pain, redness, and swelling until removed.
Dr. McLellan spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no conflicts of interest.
SAN DIEGO – Identifying a botfly infestation can be the toughest part of treating it. It’s not uncommon for travelers to return from Costa Rica, Belize, and other Central and South American countries with Dermatobia hominis infestations, but clinicians in North America are not necessarily comfortable diagnosing them or removing the larvae,, said Dr. Susan McLellan, who explained how to do so at an annual scientific meeting on infectious diseases.
Clinicians here may confuse botfly infestations with infected sebaceous cysts, staphylococcal infections, cellulitis, or even cutaneous leismaniasis. To make the diagnosis, ask about travel history in patients who present with painful furuncular lesions, said Dr. McLellan, associate professor of clinical medicine at Tulane University, New Orleans.
Closer inspection of these lesions may reveal the two dark spiracles, or breathing holes, of the larvae, which are key to removing them, Dr. Mclellan added. “The larvae have to stick their little spiracles out to breathe,” she said. “You can get them to come further out by covering up these breathing holes with anything occlusive. It can be peanut butter. It can be petroleum jelly. Just cover them up until they stick themselves out more, and then you can grab them and pull them out.”
The “first smother, then pull” approach does not always work with botfly larvae because they have spines on their bodies that can hook into subepidermal tissue, Dr. McLellan noted. “Sometimes you have to make a very, very careful incision,” she said. “Do not incise the larva at all, though. Just pop it out. These lesions do not get superinfected unless you chop up the larva while they are still inside.”
Also do not bother asking patients if they were bitten by the black adult botfly, said Dr. McLellan. Adult D. hominis do not bite, but instead lay their eggs on mosquitos. “Any biting insect that flies could potentially be a carrier,” Dr. McLellan noted. “The mother botfly catches the other flying insect, dumps her eggs on it, and that other insect starts delivering them.” A single mosquito bite can transfer several botfly eggs to a human host. When the larvae hatch and burrow into the skin, they cause pain, redness, and swelling until removed.
Dr. McLellan spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. She reported having no conflicts of interest.
EXPERT ANALYSIS FROM IDWEEK 2015