User login
Shingles Vaccine Protection Lasted 5-6 Years in Autoimmune Disease Patients
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
FROM THE ACR ANNUAL MEETING
Stroke risk rose in autoimmune disease patients after herpes zoster
Stroke risk was 50% higher in the month after patients with autoimmune diseases developed herpes zoster, compared with the next 2-6 years, according to Dr. Leonard H. Calabrese.
“These data provide urgency for developing strategies to reduce the risk of varicella zoster virus in vulnerable immunosuppressed patients,” said Dr. Calabrese of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
Immunosuppressive therapies increase the frequency and complexity of herpes zoster, which is a known risk factor for stroke. To examine the temporal relationship between herpes zoster and stroke among immunosuppressed patients, Dr. Calabrese and his associates studied Medicare data for almost 51,000 patients with new-onset herpes zoster who also had physician-diagnosed ankylosing spondylitis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis. The researchers excluded patients with a history of stroke.
In the multivariable analysis, stroke was 1.5 times more likely during the 6 months immediately after herpes zoster than in the 2-6 years after herpes zoster (95% confidence interval, 1.06-2.12). During this 6-month window, there were 9.8 strokes per 1,000 person-years, compared with 8.7 per 1,000 person-years in the 2-6 years after herpes zoster. Stroke risk also remained somewhat elevated during the entire year after herpes zoster (incidence rate ratio, 1.3; 95% CI, 1.05-1.61).
In general, stroke was more likely to occur among patients who were older, were receiving high-dose glucocorticoids, or had diabetes, hypertension, atrial fibrillation, or a history of transient ischemic attack, he said at the annual meeting of the American College of Rheumatology in San Francisco.
Dr. Calabrese disclosed relationships with Bristol-Myers Squibb, Crescendo, AbbVie, Genentech, Biogen, Pfizer, Sanofi-Aventis Pharmaceutical, and Johnson & Johnson. Two coauthors also disclosed relationships with several pharmaceutical companies. The other four coinvestigators had no disclosures.
Stroke risk was 50% higher in the month after patients with autoimmune diseases developed herpes zoster, compared with the next 2-6 years, according to Dr. Leonard H. Calabrese.
“These data provide urgency for developing strategies to reduce the risk of varicella zoster virus in vulnerable immunosuppressed patients,” said Dr. Calabrese of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
Immunosuppressive therapies increase the frequency and complexity of herpes zoster, which is a known risk factor for stroke. To examine the temporal relationship between herpes zoster and stroke among immunosuppressed patients, Dr. Calabrese and his associates studied Medicare data for almost 51,000 patients with new-onset herpes zoster who also had physician-diagnosed ankylosing spondylitis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis. The researchers excluded patients with a history of stroke.
In the multivariable analysis, stroke was 1.5 times more likely during the 6 months immediately after herpes zoster than in the 2-6 years after herpes zoster (95% confidence interval, 1.06-2.12). During this 6-month window, there were 9.8 strokes per 1,000 person-years, compared with 8.7 per 1,000 person-years in the 2-6 years after herpes zoster. Stroke risk also remained somewhat elevated during the entire year after herpes zoster (incidence rate ratio, 1.3; 95% CI, 1.05-1.61).
In general, stroke was more likely to occur among patients who were older, were receiving high-dose glucocorticoids, or had diabetes, hypertension, atrial fibrillation, or a history of transient ischemic attack, he said at the annual meeting of the American College of Rheumatology in San Francisco.
Dr. Calabrese disclosed relationships with Bristol-Myers Squibb, Crescendo, AbbVie, Genentech, Biogen, Pfizer, Sanofi-Aventis Pharmaceutical, and Johnson & Johnson. Two coauthors also disclosed relationships with several pharmaceutical companies. The other four coinvestigators had no disclosures.
Stroke risk was 50% higher in the month after patients with autoimmune diseases developed herpes zoster, compared with the next 2-6 years, according to Dr. Leonard H. Calabrese.
“These data provide urgency for developing strategies to reduce the risk of varicella zoster virus in vulnerable immunosuppressed patients,” said Dr. Calabrese of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
Immunosuppressive therapies increase the frequency and complexity of herpes zoster, which is a known risk factor for stroke. To examine the temporal relationship between herpes zoster and stroke among immunosuppressed patients, Dr. Calabrese and his associates studied Medicare data for almost 51,000 patients with new-onset herpes zoster who also had physician-diagnosed ankylosing spondylitis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis. The researchers excluded patients with a history of stroke.
In the multivariable analysis, stroke was 1.5 times more likely during the 6 months immediately after herpes zoster than in the 2-6 years after herpes zoster (95% confidence interval, 1.06-2.12). During this 6-month window, there were 9.8 strokes per 1,000 person-years, compared with 8.7 per 1,000 person-years in the 2-6 years after herpes zoster. Stroke risk also remained somewhat elevated during the entire year after herpes zoster (incidence rate ratio, 1.3; 95% CI, 1.05-1.61).
In general, stroke was more likely to occur among patients who were older, were receiving high-dose glucocorticoids, or had diabetes, hypertension, atrial fibrillation, or a history of transient ischemic attack, he said at the annual meeting of the American College of Rheumatology in San Francisco.
Dr. Calabrese disclosed relationships with Bristol-Myers Squibb, Crescendo, AbbVie, Genentech, Biogen, Pfizer, Sanofi-Aventis Pharmaceutical, and Johnson & Johnson. Two coauthors also disclosed relationships with several pharmaceutical companies. The other four coinvestigators had no disclosures.
FROM THE ACR ANNUAL MEETING
Key clinical point: Stroke risk increased by 50% in the month after patients with autoimmune diseases had an episode of herpes zoster.
Major finding: The risk of stroke was 50% higher in the 6 months immediately after incident herpes zoster than 2-6 years after herpes zoster (95% CI, 1.06- 2.12).
Data source: An analysis of Medicare data for 50,929 patients with autoimmune disease and incident herpes zoster between 2006 and 2012.
Disclosures: Dr. Calabrese disclosed relationships with Bristol-Myers Squibb, Crescendo, AbbVie, Genentech, Biogen, Pfizer, Sanofi-Aventis Pharmaceutical, and Johnson & Johnson. Two coauthors also disclosed relationships with several pharmaceutical companies. The other four coinvestigators had no disclosures.
Shingles vaccine protection lasted 5-6 years in autoimmune disease patients
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.*
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
* Correction, 11/13/2015: The article previously misstated Dr. Yun's gender.
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.*
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
* Correction, 11/13/2015: The article previously misstated Dr. Yun's gender.
Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients, reported Dr. Huifeng Yun, assistant professor of epidemiology at the University of Alabama, Birmingham. Based on the findings, clinicians could consider revaccinating patients with autoimmune diseases about 5 years after their first live herpes zoster vaccine, she said.*
The long-term Shingles Prevention Study recently showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals, but the duration of protection for patients with autoimmune diseases was unclear, the investigators said. Therefore, they retrospectively studied Medicare data for more than 130,000 such patients between 2006 and 2012. About one-third of patients were vaccinated against herpes zoster, and 47% had rheumatoid arthritis, 32% had psoriasis, 21% had inflammatory bowel disease, 5% had psoriatic arthritis, and 1% had ankylosing spondylitis.
Rates of herpes zoster among vaccinated patients rose from 0.75 per 100 person-years during the first year after vaccination to 1.36 during the sixth year. In the adjusted analysis, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52; 95% confidence interval, 0.45-0.61) and remained substantially less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92; 95% CI, 0.45-1.86). There was no overall change in risk among unvaccinated patients during the study period, the investigators noted.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
* Correction, 11/13/2015: The article previously misstated Dr. Yun's gender.
FROM THE ACR ANNUAL MEETING
Key clinical point: Protection against shingles appeared to wane between the fifth and sixth years after patients with autoimmune diseases received the live herpes zoster vaccine.
Major finding: The rate of herpes zoster rose from 0.75 per 100 person-years in the first year after vaccination to 1.36 in the sixth year, when it approached the rate among unvaccinated patients.
Data source: Retrospective analysis of 130,107 Medicare patients with autoimmune diseases between 2006 and 2012.
Disclosures: Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
Survivors of out-of-hospital cardiac arrest usually had intact brain function
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr. Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, N.C., and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Dr. Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation.
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr. Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, N.C., and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Dr. Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation.
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr. Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, N.C., and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Dr. Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation.
FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, regardless of duration of CPR in the field.
Major finding: Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Data source: A retrospective observational study of 3,814 adults who had an out-of-hospital cardiac arrest between 2005 and 2014.
Disclosures: Dr. Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation.
Long working hours raised stroke risk
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
FROM THE LANCET
Key clinical point: Long work weeks were tied to increased stroke risk in a large meta-analysis.
Major finding: Individuals worked an average of at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours (P = .002).
Data source: Meta-analysis of 25 prospective cohort studies from Europe, the United States, and Australia.
Disclosures: The study was funded by a variety of governmental research councils, programs, funds, foundations, ministries, and academies in various countries. The investigators reported having no conflicts of interest.
Modified Valsalva More Than Doubled Conversion Rate in Supraventricular Tachycardia
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
FROM THE LANCET
Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published Oct. 31 in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with only 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% confidence interval, 2.3-5.8; P less than .0001), reported Dr. Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5%-20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted (Lancet 2015;386:1747-53). For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semirecumbent, but then immediately laid flat while a staff member raised their legs to a 45 ° angle for 15 seconds. They returned to the semirecumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the investigators. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
FROM THE LANCET
Key clinical point: A modified version of the Valsalva maneuver, in which patients were immediately laid flat afterward with their legs passively raised, more than doubled the rate of conversion from acute supraventricular tachycardia normal sinus rhythm as compared with the standard Valsalva maneuver.
Major finding: The conversion rate was 43% for the modified Valsalva group and 17% for patients undergoing the standard maneuver (adjusted OR, 3.7; P less than .0001).
Data source: Multicenter, randomized, controlled, parallel-group trial of 428 patients presenting to emergency departments with acute SVT.
Disclosures: The National Institute for Health Research funded the study. The investigators declared no competing interests.
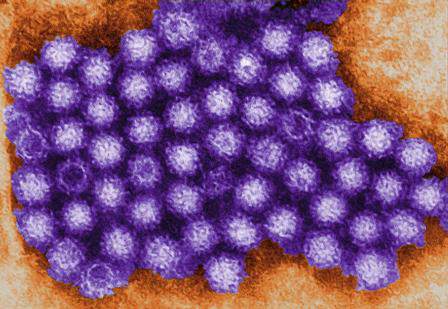
Norovirus sends 1.6 million to doctors every year
SAN DIEGO – Norovirus infections send about 1.6 million people to the doctor every year in the United States, according to the first active surveillance study to cover all age groups here.
“This provides a baseline burden of norovirus disease to assess the potential impact of future vaccines,” said Dr. Aron Hall of the Centers for Disease Control and Prevention in Atlanta. Estimated infection rates generally resembled those from past studies, but were more robust and granular, Dr. Hall said at an annual scientific meeting on infectious diseases.
About 19-21 million Americans suffer acute gastroenteritis because of norovirus infection every year, Dr. Hall noted. About 400,000 of these patients seek urgent care, at least 56,000 are hospitalized, and 570-800 ultimately die from associated complications. However, several factors have impeded large epidemiologic studies of norovirus disease, he added. Most infected patients do not seek care, those who do often do not undergo stool testing, there is no national norovirus case reporting system, turnaround times and the sensitivity of clinical assays remain suboptimal, and there are no specific ICD codes for norovirus gastroenteritis, he said.
To overcome these obstacles, Dr. Hall and his associates spent a year studying 480,000 Kaiser Permanente Northwest enrollees in the Portland, Ore. area. Enrollees seek care almost entirely in-network and demographically resemble other residents in the region, Dr. Hall said. The researchers used automated software to identify about 19,000 patients with ICD-9 codes for acute gastroenteritis. They called about half of these patients to request stool samples within 3 days of their appointments, while they were likely to still be shedding pathogens. They aimed to test all patients who were younger than 5 years or older than 65 years, and called a random sample of 35% of the other patients.
In all, the researchers tested stool specimens for 84% (1,467) of patients whom they reached within the 3-day window, said Dr. Hall. About 13% of these patients tested positive for norovirus, of which 85% were genotype II, while the rest were genotype I. The overall incidence of medically attended acute gastroenteritis due to norovirus was 5 cases per 100,00 person-years, but rates were four to five times higher among infants and children under the age of 2 years (22.7 and 29.1 cases per 100,000 person-years, respectively), and about 50% higher among adults aged 85 years and older (7.4 cases per 100,000 person-years).
“Extrapolation to the U.S. population would yield 1.6 million norovirus-associated MAAGE [medically attended acute gastroenteritis] encounters per year,” Dr. Hall concluded. The research team is now sequencing norovirus genotypes, testing stool samples for other enteric pathogens, and studying high-risk subgroups, clinical severity, and cases of potential household transmission, he added.
Dr. Hall spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. He had no disclosures. One of his coauthors reported receiving research support from GlaxoSmithKline.
SAN DIEGO – Norovirus infections send about 1.6 million people to the doctor every year in the United States, according to the first active surveillance study to cover all age groups here.
“This provides a baseline burden of norovirus disease to assess the potential impact of future vaccines,” said Dr. Aron Hall of the Centers for Disease Control and Prevention in Atlanta. Estimated infection rates generally resembled those from past studies, but were more robust and granular, Dr. Hall said at an annual scientific meeting on infectious diseases.
About 19-21 million Americans suffer acute gastroenteritis because of norovirus infection every year, Dr. Hall noted. About 400,000 of these patients seek urgent care, at least 56,000 are hospitalized, and 570-800 ultimately die from associated complications. However, several factors have impeded large epidemiologic studies of norovirus disease, he added. Most infected patients do not seek care, those who do often do not undergo stool testing, there is no national norovirus case reporting system, turnaround times and the sensitivity of clinical assays remain suboptimal, and there are no specific ICD codes for norovirus gastroenteritis, he said.
To overcome these obstacles, Dr. Hall and his associates spent a year studying 480,000 Kaiser Permanente Northwest enrollees in the Portland, Ore. area. Enrollees seek care almost entirely in-network and demographically resemble other residents in the region, Dr. Hall said. The researchers used automated software to identify about 19,000 patients with ICD-9 codes for acute gastroenteritis. They called about half of these patients to request stool samples within 3 days of their appointments, while they were likely to still be shedding pathogens. They aimed to test all patients who were younger than 5 years or older than 65 years, and called a random sample of 35% of the other patients.
In all, the researchers tested stool specimens for 84% (1,467) of patients whom they reached within the 3-day window, said Dr. Hall. About 13% of these patients tested positive for norovirus, of which 85% were genotype II, while the rest were genotype I. The overall incidence of medically attended acute gastroenteritis due to norovirus was 5 cases per 100,00 person-years, but rates were four to five times higher among infants and children under the age of 2 years (22.7 and 29.1 cases per 100,000 person-years, respectively), and about 50% higher among adults aged 85 years and older (7.4 cases per 100,000 person-years).
“Extrapolation to the U.S. population would yield 1.6 million norovirus-associated MAAGE [medically attended acute gastroenteritis] encounters per year,” Dr. Hall concluded. The research team is now sequencing norovirus genotypes, testing stool samples for other enteric pathogens, and studying high-risk subgroups, clinical severity, and cases of potential household transmission, he added.
Dr. Hall spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. He had no disclosures. One of his coauthors reported receiving research support from GlaxoSmithKline.
SAN DIEGO – Norovirus infections send about 1.6 million people to the doctor every year in the United States, according to the first active surveillance study to cover all age groups here.
“This provides a baseline burden of norovirus disease to assess the potential impact of future vaccines,” said Dr. Aron Hall of the Centers for Disease Control and Prevention in Atlanta. Estimated infection rates generally resembled those from past studies, but were more robust and granular, Dr. Hall said at an annual scientific meeting on infectious diseases.
About 19-21 million Americans suffer acute gastroenteritis because of norovirus infection every year, Dr. Hall noted. About 400,000 of these patients seek urgent care, at least 56,000 are hospitalized, and 570-800 ultimately die from associated complications. However, several factors have impeded large epidemiologic studies of norovirus disease, he added. Most infected patients do not seek care, those who do often do not undergo stool testing, there is no national norovirus case reporting system, turnaround times and the sensitivity of clinical assays remain suboptimal, and there are no specific ICD codes for norovirus gastroenteritis, he said.
To overcome these obstacles, Dr. Hall and his associates spent a year studying 480,000 Kaiser Permanente Northwest enrollees in the Portland, Ore. area. Enrollees seek care almost entirely in-network and demographically resemble other residents in the region, Dr. Hall said. The researchers used automated software to identify about 19,000 patients with ICD-9 codes for acute gastroenteritis. They called about half of these patients to request stool samples within 3 days of their appointments, while they were likely to still be shedding pathogens. They aimed to test all patients who were younger than 5 years or older than 65 years, and called a random sample of 35% of the other patients.
In all, the researchers tested stool specimens for 84% (1,467) of patients whom they reached within the 3-day window, said Dr. Hall. About 13% of these patients tested positive for norovirus, of which 85% were genotype II, while the rest were genotype I. The overall incidence of medically attended acute gastroenteritis due to norovirus was 5 cases per 100,00 person-years, but rates were four to five times higher among infants and children under the age of 2 years (22.7 and 29.1 cases per 100,000 person-years, respectively), and about 50% higher among adults aged 85 years and older (7.4 cases per 100,000 person-years).
“Extrapolation to the U.S. population would yield 1.6 million norovirus-associated MAAGE [medically attended acute gastroenteritis] encounters per year,” Dr. Hall concluded. The research team is now sequencing norovirus genotypes, testing stool samples for other enteric pathogens, and studying high-risk subgroups, clinical severity, and cases of potential household transmission, he added.
Dr. Hall spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. He had no disclosures. One of his coauthors reported receiving research support from GlaxoSmithKline.
AT IDWEEK 2015
Key clinical point: Norovirus infection is a common cause of medically attended acute gastroenteritis.
Major finding: Every year, about 1.6 million patients in the United States seek medical care for norovirus-associated MAAGE.
Data source: Active surveillance of 480,000 health maintenance organization enrollees in the urban Pacific Northwest between March 2014 and April 2015.
Disclosures: Dr. Hall had no disclosures. A coauthor reported receiving research support from GlaxoSmithKline.
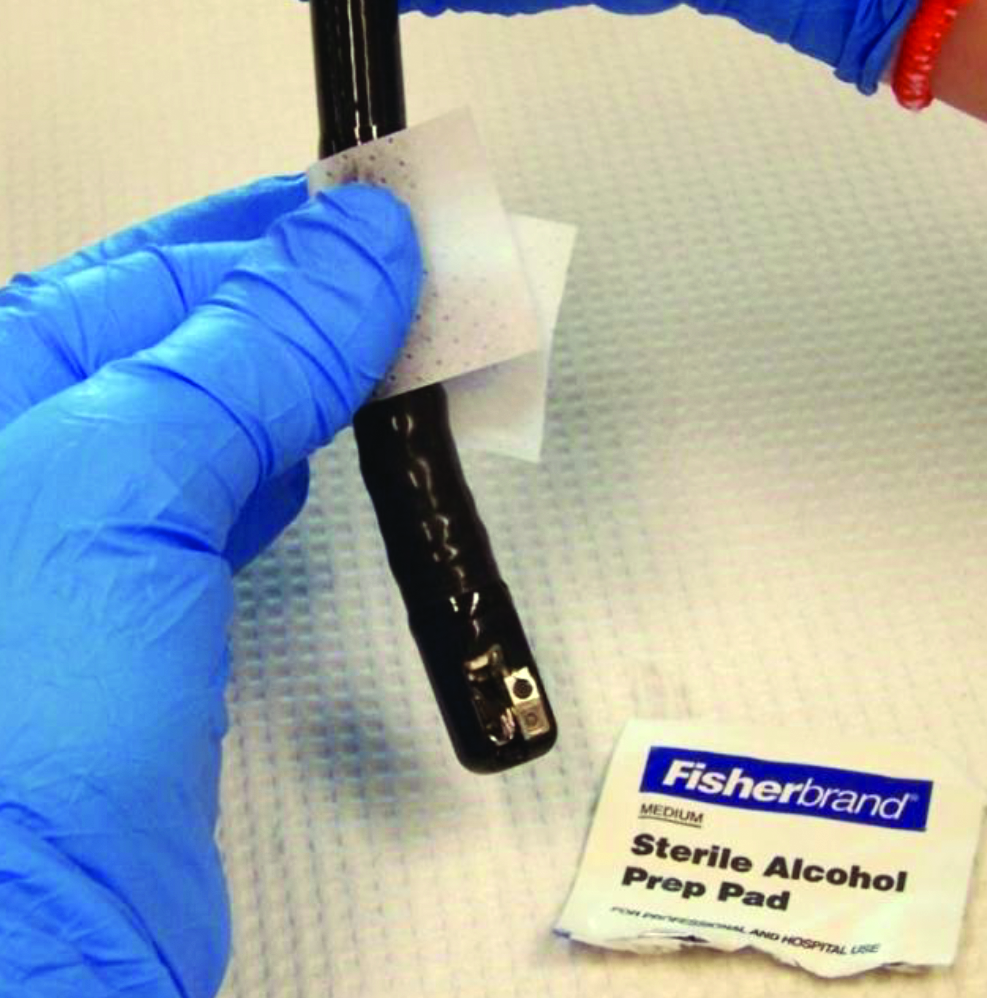
Duodenoscopes often cultured high-concern organisms
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
AT IDWEEK 2015
Key clinical point: High-concern organisms often contaminated duodenoscopes after ERCP.
Major finding: Investigators cultured these bacteria from 92% of duodenoscopes immediately after ERCP, and from 17% of scopes after reprocessing.
Data source: Cultures of 12 duodenoscopes immediately after ERCP and again after reprocessing, and surveillance cultures of 11 stored duodenoscopes.
Disclosures: Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
Gastrointestinal and liver diseases remain substantial public health burden
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Gastrointestinal and liver diseases remain a major cause of health care utilization and associated costs in the United States.
Major finding: Hospital admissions and associated costs for Clostridium difficile infection, inflammatory bowel disease, and liver disease all rose substantially between 1993 and 2012.
Data source: Analysis of surveillance data from the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, and National Cancer Institute.
Disclosures: The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.