User login
Adalimumab posts strong early results in refractory JIA-associated uveitis
SAN FRANCISCO – The monoclonal antibody adalimumab was more than twice as effective as was placebo for treating methotrexate-refractory uveitis in children with idiopathic arthritis, according to early results from the largest-ever double-blind, randomized, controlled trial of the disease.
Because the difference in time to treatment failure met the prespecified efficacy endpoint, investigators halted the trial after enrolling 90 patients, said Dr. Athimalaipet V. Ramanan, professor of pediatric rheumatology at the University of Bristol (England). But adalimumab also was associated with about three times more infections and other serious adverse events, compared with placebo, he reported in a late-breaker session at the annual meeting of the American College of Rheumatology. “We will, of course, be looking at the long-term data to evaluate cost-effectiveness, as well as safety,” he added.
About one in five children with juvenile idiopathic arthritis (JIA) develops uveitis, which threatens sight and is the most common type of pediatric intraocular inflammation. First-line methotrexate can substantially improve articular inflammation in JIA, but had not been studied in randomized, controlled trials of JIA-associated uveitis. Based on adalimumab’s success in treating the articular aspects of JIA, the investigators studied the biologic in patients aged 2-18 years who had active JIA-associated uveitis despite at least 12 weeks of stable methotrexate therapy. Most cases were mild to moderate, including mild flare and little vitreous haze. The average age of the patients was 9 years, about three-quarters were girls, and about half tested positive for antinuclear antibodies. All patients continued on methotrexate and were randomized 1:2 to subcutaneous, biweekly injections of placebo or weight-based adalimumab.
Patients in the adalimumab arm were about 75% less likely than were controls to fail treatment – that is, to meet Standardization of the Uveitis Nomenclature (SUN) criteria for progressive anterior segment inflammation (hazard ratio, 0.25; 95% confidence interval, 0.12-0.49; P less than .0001). The median time to treatment failure was about 20 weeks for the control arm, and nearly 60 weeks for the adalimumab arm. Specific definitions of treatment failure included a consecutive, two-step rise from baseline in the SUN cell activity score, sustained failure to improve from baseline grade 3 inflammation, persistent grade 1 or 2 inflammation after 6 months of treatment, and worsening ocular comorbidities, Dr. Ramanan said. Adalimumab also was associated with improved SUN scores, although the researchers are still analyzing those data, he added.
Serious adverse events occurred in 22% of patients who received adalimumab, Dr. Ramanan reported. These most often consisted of streptococcal disease, varicella, and other infections for which the immunomodulator has a black box warning. Although only 7% of the control group experienced serious adverse events, these included two flares of uveitis that caused patients to withdraw.
The National Institute for Health Research Health Technology Assessment Programme and Arthritis Research UK funded the study. Dr. Ramanan and one coauthor reported having received consulting fees from AbbVie, maker of Humira. AbbVie reviewed and commented on the abstract, but did not participate in trial design or data analysis.
SAN FRANCISCO – The monoclonal antibody adalimumab was more than twice as effective as was placebo for treating methotrexate-refractory uveitis in children with idiopathic arthritis, according to early results from the largest-ever double-blind, randomized, controlled trial of the disease.
Because the difference in time to treatment failure met the prespecified efficacy endpoint, investigators halted the trial after enrolling 90 patients, said Dr. Athimalaipet V. Ramanan, professor of pediatric rheumatology at the University of Bristol (England). But adalimumab also was associated with about three times more infections and other serious adverse events, compared with placebo, he reported in a late-breaker session at the annual meeting of the American College of Rheumatology. “We will, of course, be looking at the long-term data to evaluate cost-effectiveness, as well as safety,” he added.
About one in five children with juvenile idiopathic arthritis (JIA) develops uveitis, which threatens sight and is the most common type of pediatric intraocular inflammation. First-line methotrexate can substantially improve articular inflammation in JIA, but had not been studied in randomized, controlled trials of JIA-associated uveitis. Based on adalimumab’s success in treating the articular aspects of JIA, the investigators studied the biologic in patients aged 2-18 years who had active JIA-associated uveitis despite at least 12 weeks of stable methotrexate therapy. Most cases were mild to moderate, including mild flare and little vitreous haze. The average age of the patients was 9 years, about three-quarters were girls, and about half tested positive for antinuclear antibodies. All patients continued on methotrexate and were randomized 1:2 to subcutaneous, biweekly injections of placebo or weight-based adalimumab.
Patients in the adalimumab arm were about 75% less likely than were controls to fail treatment – that is, to meet Standardization of the Uveitis Nomenclature (SUN) criteria for progressive anterior segment inflammation (hazard ratio, 0.25; 95% confidence interval, 0.12-0.49; P less than .0001). The median time to treatment failure was about 20 weeks for the control arm, and nearly 60 weeks for the adalimumab arm. Specific definitions of treatment failure included a consecutive, two-step rise from baseline in the SUN cell activity score, sustained failure to improve from baseline grade 3 inflammation, persistent grade 1 or 2 inflammation after 6 months of treatment, and worsening ocular comorbidities, Dr. Ramanan said. Adalimumab also was associated with improved SUN scores, although the researchers are still analyzing those data, he added.
Serious adverse events occurred in 22% of patients who received adalimumab, Dr. Ramanan reported. These most often consisted of streptococcal disease, varicella, and other infections for which the immunomodulator has a black box warning. Although only 7% of the control group experienced serious adverse events, these included two flares of uveitis that caused patients to withdraw.
The National Institute for Health Research Health Technology Assessment Programme and Arthritis Research UK funded the study. Dr. Ramanan and one coauthor reported having received consulting fees from AbbVie, maker of Humira. AbbVie reviewed and commented on the abstract, but did not participate in trial design or data analysis.
SAN FRANCISCO – The monoclonal antibody adalimumab was more than twice as effective as was placebo for treating methotrexate-refractory uveitis in children with idiopathic arthritis, according to early results from the largest-ever double-blind, randomized, controlled trial of the disease.
Because the difference in time to treatment failure met the prespecified efficacy endpoint, investigators halted the trial after enrolling 90 patients, said Dr. Athimalaipet V. Ramanan, professor of pediatric rheumatology at the University of Bristol (England). But adalimumab also was associated with about three times more infections and other serious adverse events, compared with placebo, he reported in a late-breaker session at the annual meeting of the American College of Rheumatology. “We will, of course, be looking at the long-term data to evaluate cost-effectiveness, as well as safety,” he added.
About one in five children with juvenile idiopathic arthritis (JIA) develops uveitis, which threatens sight and is the most common type of pediatric intraocular inflammation. First-line methotrexate can substantially improve articular inflammation in JIA, but had not been studied in randomized, controlled trials of JIA-associated uveitis. Based on adalimumab’s success in treating the articular aspects of JIA, the investigators studied the biologic in patients aged 2-18 years who had active JIA-associated uveitis despite at least 12 weeks of stable methotrexate therapy. Most cases were mild to moderate, including mild flare and little vitreous haze. The average age of the patients was 9 years, about three-quarters were girls, and about half tested positive for antinuclear antibodies. All patients continued on methotrexate and were randomized 1:2 to subcutaneous, biweekly injections of placebo or weight-based adalimumab.
Patients in the adalimumab arm were about 75% less likely than were controls to fail treatment – that is, to meet Standardization of the Uveitis Nomenclature (SUN) criteria for progressive anterior segment inflammation (hazard ratio, 0.25; 95% confidence interval, 0.12-0.49; P less than .0001). The median time to treatment failure was about 20 weeks for the control arm, and nearly 60 weeks for the adalimumab arm. Specific definitions of treatment failure included a consecutive, two-step rise from baseline in the SUN cell activity score, sustained failure to improve from baseline grade 3 inflammation, persistent grade 1 or 2 inflammation after 6 months of treatment, and worsening ocular comorbidities, Dr. Ramanan said. Adalimumab also was associated with improved SUN scores, although the researchers are still analyzing those data, he added.
Serious adverse events occurred in 22% of patients who received adalimumab, Dr. Ramanan reported. These most often consisted of streptococcal disease, varicella, and other infections for which the immunomodulator has a black box warning. Although only 7% of the control group experienced serious adverse events, these included two flares of uveitis that caused patients to withdraw.
The National Institute for Health Research Health Technology Assessment Programme and Arthritis Research UK funded the study. Dr. Ramanan and one coauthor reported having received consulting fees from AbbVie, maker of Humira. AbbVie reviewed and commented on the abstract, but did not participate in trial design or data analysis.
AT THE ACR ANNUAL MEETING
Key clinical point: Adalimumab may effectively treat methotrexate-refractory JIA-associated uveitis.
Major finding: Patients in the adalimumab arm were about 75% less likely than were controls to meet SUN criteria for progressive anterior segment inflammation (HR, 0.25; P less than .0001). A total of 21.7% experienced a serious adverse event, compared with 6.7% of the control group.
Data source: A randomized, double-blinded trial of 90 patients who received optimized methotrexate plus either placebo or weight-based adalimumab.
Disclosures: The National Institute for Health Research Health Technology Assessment Programme and Arthritis Research UK funded the study. Dr. Ramanan and one coauthor reported having received consulting fees from AbbVie, maker of Humira. AbbVie reviewed and commented on the abstract, but did not participate in trial design or data analysis.
Gout hospitalizations, costs surpass those for rheumatoid arthritis
SAN FRANCISCO – Hospitalization rates for gout doubled between 1993 and 2011, while those for rheumatoid arthritis fell by 67%, Dr. Sian Yik Lim reported at the annual meeting of the American College of Rheumatology.
The trends reveal marked progress in the treatment of rheumatoid arthritis, but “also highlight a critical need to improve gout care” and to implement measures to combat its rising prevalence, said Dr. Lim, a research fellow in medicine at Massachusetts General Hospital, Boston.
The study is “a very nice piece of work,” added Dr. James Galloway, who helped moderate the session at the meeting and is a lecturer in rheumatology at King’s College Hospital in London. “It makes us wonder whether we should spend more time teaching our primary care physician colleagues more about gout than rheumatoid arthritis.”
Gout and rheumatoid arthritis are the two most common inflammatory joint diseases, but few longitudinal studies have examined trends in related hospital admissions or costs, Dr. Lim said. Therefore, he and his associates extracted primary hospital discharge ICD-9 diagnosis codes from the National Inpatient Sample and also studied primary procedure codes for total knee replacement, total hip replacement, and other major joint surgeries for 1993 through 2011. In addition, they merged these with cost data from the Healthcare Cost and Utilization Project for 2001 to 2011.
Hospitalizations for gout and rheumatoid arthritis “crisscrossed” during the study period, Dr. Lim said. While there were more than three times as many hospitalizations for rheumatoid arthritis (26,712) as for gout (8,485) in 1993, by 2011, there were nearly twice as many admissions for gout (20,949) as for rheumatoid arthritis (11,015). Likewise, hospitalization rates for gout rose from 4.5 to 9 per 100,000 adults, while rheumatoid arthritis admissions fell by about two-thirds, from 14 to 5 per 100,000 adults. For the entire study period, hospital admissions for gout totaled 254,982, compared with 323,649 for rheumatoid arthritis, Dr. Lim added.
The investigators also documented a steady drop in admissions for total knee replacement, total hip replacement, and other major joint surgeries among rheumatoid arthritis patients, mirroring the results of recent multicenter studies in California (Ann Rheum Dis. 2009 Jul 5. doi: 10.1136/ard.2009.112474), the United Kingdom (Rheumatology [Oxford]. 2015 Apr;54[4]:666-71), and Germany (Ann Rheum Dis. 2015;74:738-45), Dr. Lim said. “This finding contrasts with the overall dramatic increase in these surgeries in the general United States population in recent years,” he added.
Inflation-adjusted hospital costs for gout and rheumatoid arthritis also converged during the study period, and by 2011, costs for gout actually exceeded those for rheumatoid arthritis, Dr. Lim said.
Overall, the findings reflect stark differences in care for gout and rheumatoid arthritis in the United States, he added. “New and potent drugs, effective combination regimens, and management strategies are increasingly being adopted for rheumatoid arthritis, but care for gout remains suboptimal, even though its prevalence and incidence are increasing,” he said. “Although the vast majority of gout patients are indicated for urate-lowering therapy, only a small proportion retrieve treatment, and the level of uric acid is not even measured in the vast majority of patients.”
Surveys also indicate that patients with gout often do not receive clear explanations about their disease, which may explain why as few as 10% follow treatment recommendations, according to Dr. Lim. He pointed to a hospital-based, retrospective cohort study reported at last year’s ACR annual meeting in which 89% of hospitalizations for gout were considered preventable. “These data support the need to improve gout prevention and care,” he said.
Dr. Lim had no disclosures. Dr. Hyon Choi, the senior author, reported having served on advisory boards for Takeda and AstraZeneca.
SAN FRANCISCO – Hospitalization rates for gout doubled between 1993 and 2011, while those for rheumatoid arthritis fell by 67%, Dr. Sian Yik Lim reported at the annual meeting of the American College of Rheumatology.
The trends reveal marked progress in the treatment of rheumatoid arthritis, but “also highlight a critical need to improve gout care” and to implement measures to combat its rising prevalence, said Dr. Lim, a research fellow in medicine at Massachusetts General Hospital, Boston.
The study is “a very nice piece of work,” added Dr. James Galloway, who helped moderate the session at the meeting and is a lecturer in rheumatology at King’s College Hospital in London. “It makes us wonder whether we should spend more time teaching our primary care physician colleagues more about gout than rheumatoid arthritis.”
Gout and rheumatoid arthritis are the two most common inflammatory joint diseases, but few longitudinal studies have examined trends in related hospital admissions or costs, Dr. Lim said. Therefore, he and his associates extracted primary hospital discharge ICD-9 diagnosis codes from the National Inpatient Sample and also studied primary procedure codes for total knee replacement, total hip replacement, and other major joint surgeries for 1993 through 2011. In addition, they merged these with cost data from the Healthcare Cost and Utilization Project for 2001 to 2011.
Hospitalizations for gout and rheumatoid arthritis “crisscrossed” during the study period, Dr. Lim said. While there were more than three times as many hospitalizations for rheumatoid arthritis (26,712) as for gout (8,485) in 1993, by 2011, there were nearly twice as many admissions for gout (20,949) as for rheumatoid arthritis (11,015). Likewise, hospitalization rates for gout rose from 4.5 to 9 per 100,000 adults, while rheumatoid arthritis admissions fell by about two-thirds, from 14 to 5 per 100,000 adults. For the entire study period, hospital admissions for gout totaled 254,982, compared with 323,649 for rheumatoid arthritis, Dr. Lim added.
The investigators also documented a steady drop in admissions for total knee replacement, total hip replacement, and other major joint surgeries among rheumatoid arthritis patients, mirroring the results of recent multicenter studies in California (Ann Rheum Dis. 2009 Jul 5. doi: 10.1136/ard.2009.112474), the United Kingdom (Rheumatology [Oxford]. 2015 Apr;54[4]:666-71), and Germany (Ann Rheum Dis. 2015;74:738-45), Dr. Lim said. “This finding contrasts with the overall dramatic increase in these surgeries in the general United States population in recent years,” he added.
Inflation-adjusted hospital costs for gout and rheumatoid arthritis also converged during the study period, and by 2011, costs for gout actually exceeded those for rheumatoid arthritis, Dr. Lim said.
Overall, the findings reflect stark differences in care for gout and rheumatoid arthritis in the United States, he added. “New and potent drugs, effective combination regimens, and management strategies are increasingly being adopted for rheumatoid arthritis, but care for gout remains suboptimal, even though its prevalence and incidence are increasing,” he said. “Although the vast majority of gout patients are indicated for urate-lowering therapy, only a small proportion retrieve treatment, and the level of uric acid is not even measured in the vast majority of patients.”
Surveys also indicate that patients with gout often do not receive clear explanations about their disease, which may explain why as few as 10% follow treatment recommendations, according to Dr. Lim. He pointed to a hospital-based, retrospective cohort study reported at last year’s ACR annual meeting in which 89% of hospitalizations for gout were considered preventable. “These data support the need to improve gout prevention and care,” he said.
Dr. Lim had no disclosures. Dr. Hyon Choi, the senior author, reported having served on advisory boards for Takeda and AstraZeneca.
SAN FRANCISCO – Hospitalization rates for gout doubled between 1993 and 2011, while those for rheumatoid arthritis fell by 67%, Dr. Sian Yik Lim reported at the annual meeting of the American College of Rheumatology.
The trends reveal marked progress in the treatment of rheumatoid arthritis, but “also highlight a critical need to improve gout care” and to implement measures to combat its rising prevalence, said Dr. Lim, a research fellow in medicine at Massachusetts General Hospital, Boston.
The study is “a very nice piece of work,” added Dr. James Galloway, who helped moderate the session at the meeting and is a lecturer in rheumatology at King’s College Hospital in London. “It makes us wonder whether we should spend more time teaching our primary care physician colleagues more about gout than rheumatoid arthritis.”
Gout and rheumatoid arthritis are the two most common inflammatory joint diseases, but few longitudinal studies have examined trends in related hospital admissions or costs, Dr. Lim said. Therefore, he and his associates extracted primary hospital discharge ICD-9 diagnosis codes from the National Inpatient Sample and also studied primary procedure codes for total knee replacement, total hip replacement, and other major joint surgeries for 1993 through 2011. In addition, they merged these with cost data from the Healthcare Cost and Utilization Project for 2001 to 2011.
Hospitalizations for gout and rheumatoid arthritis “crisscrossed” during the study period, Dr. Lim said. While there were more than three times as many hospitalizations for rheumatoid arthritis (26,712) as for gout (8,485) in 1993, by 2011, there were nearly twice as many admissions for gout (20,949) as for rheumatoid arthritis (11,015). Likewise, hospitalization rates for gout rose from 4.5 to 9 per 100,000 adults, while rheumatoid arthritis admissions fell by about two-thirds, from 14 to 5 per 100,000 adults. For the entire study period, hospital admissions for gout totaled 254,982, compared with 323,649 for rheumatoid arthritis, Dr. Lim added.
The investigators also documented a steady drop in admissions for total knee replacement, total hip replacement, and other major joint surgeries among rheumatoid arthritis patients, mirroring the results of recent multicenter studies in California (Ann Rheum Dis. 2009 Jul 5. doi: 10.1136/ard.2009.112474), the United Kingdom (Rheumatology [Oxford]. 2015 Apr;54[4]:666-71), and Germany (Ann Rheum Dis. 2015;74:738-45), Dr. Lim said. “This finding contrasts with the overall dramatic increase in these surgeries in the general United States population in recent years,” he added.
Inflation-adjusted hospital costs for gout and rheumatoid arthritis also converged during the study period, and by 2011, costs for gout actually exceeded those for rheumatoid arthritis, Dr. Lim said.
Overall, the findings reflect stark differences in care for gout and rheumatoid arthritis in the United States, he added. “New and potent drugs, effective combination regimens, and management strategies are increasingly being adopted for rheumatoid arthritis, but care for gout remains suboptimal, even though its prevalence and incidence are increasing,” he said. “Although the vast majority of gout patients are indicated for urate-lowering therapy, only a small proportion retrieve treatment, and the level of uric acid is not even measured in the vast majority of patients.”
Surveys also indicate that patients with gout often do not receive clear explanations about their disease, which may explain why as few as 10% follow treatment recommendations, according to Dr. Lim. He pointed to a hospital-based, retrospective cohort study reported at last year’s ACR annual meeting in which 89% of hospitalizations for gout were considered preventable. “These data support the need to improve gout prevention and care,” he said.
Dr. Lim had no disclosures. Dr. Hyon Choi, the senior author, reported having served on advisory boards for Takeda and AstraZeneca.
AT THE ACR ANNUAL MEETING
Key clinical point: Hospitalizations and costs for gout in the United States have surpassed those for rheumatoid arthritis, reflecting stark differences in the state of care for these diseases.
Major finding: Between 1993 and 2011, hospitalizations for gout rose from 4.5 to 9 per 100,000 adults, while rheumatoid arthritis admissions fell from 14 to 5 per 100,000 adults.
Data source: Analysis of primary discharge diagnoses from the National Inpatient Sample and cost data from the Healthcare Cost and Utilization Project.
Disclosures: Dr. Lim had no disclosures. Dr. Hyon Choi, the senior author, reported having served on advisory boards for Takeda and AstraZeneca.
Shingles vaccine protection lasted about 5 years in autoimmune disease patients
SAN FRANCISCO – Protection against shingles appeared to wane about 5 years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients during 7 years of follow-up, reported Dr. Huifeng Yun of the department of epidemiology at the University of Alabama at Birmingham. “Our findings suggest that patients might benefit from a booster vaccine at some point after initial vaccination, but further research is needed to determine when and if such a strategy is effective at preventing herpes zoster,” she said.
The long-term Shingles Prevention Study showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals. But about 90% of zoster cases occur in patients with autoimmune and inflammatory diseases, for whom the duration of vaccine protection has been unclear, Dr. Yun said. “Antiviral medication approved for herpes zoster reduces the severity and duration of symptoms, but may not prevent postherpetic neuralgia,” making vaccine protection a priority, she added.
Dr. Yun and her associates retrospectively analyzed Medicare data for nearly 179,000 patients with autoimmune and inflammatory conditions between 2006 and 2013. About one-third of patients were vaccinated against herpes zoster, and more than 40% had rheumatoid arthritis, nearly one-third had psoriasis, about 20% had inflammatory bowel disease, about 5% had psoriatic arthritis, and about 1% had ankylosing spondylitis. The researchers matched unvaccinated and vaccinated patients in a 2:1 ratio based on calendar year, age, sex, race, disease type, and use of disease-modifying antirheumatic drugs, biologics, and glucocorticoids. They followed patients from 30 days after vaccination – or the corresponding date in the unvaccinated cohort – until death, first episode of herpes zoster, or the end of 2013, whichever came first.
The rates of herpes zoster among vaccinated patients rose from 0.75/100 person-years during the first year after vaccination to 1.25/100 person-years during the seventh year of follow-up, Dr. Yun said. In contrast, zoster rates among unvaccinated patients remained steady, ranging between 1.32 and 1.35 cases per 100 person-years. In an adjusted analysis of data from 2006 through 2012, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52) and remained significantly less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92).
“The herpes zoster vaccine was effective for about 5 years, and results of subgroup analyses were consistent with the main analysis,” Dr. Yun concluded. But the Medicare database lacked details on disease severity or lifestyle factors, both of which might have affected the results, she cautioned.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
SAN FRANCISCO – Protection against shingles appeared to wane about 5 years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients during 7 years of follow-up, reported Dr. Huifeng Yun of the department of epidemiology at the University of Alabama at Birmingham. “Our findings suggest that patients might benefit from a booster vaccine at some point after initial vaccination, but further research is needed to determine when and if such a strategy is effective at preventing herpes zoster,” she said.
The long-term Shingles Prevention Study showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals. But about 90% of zoster cases occur in patients with autoimmune and inflammatory diseases, for whom the duration of vaccine protection has been unclear, Dr. Yun said. “Antiviral medication approved for herpes zoster reduces the severity and duration of symptoms, but may not prevent postherpetic neuralgia,” making vaccine protection a priority, she added.
Dr. Yun and her associates retrospectively analyzed Medicare data for nearly 179,000 patients with autoimmune and inflammatory conditions between 2006 and 2013. About one-third of patients were vaccinated against herpes zoster, and more than 40% had rheumatoid arthritis, nearly one-third had psoriasis, about 20% had inflammatory bowel disease, about 5% had psoriatic arthritis, and about 1% had ankylosing spondylitis. The researchers matched unvaccinated and vaccinated patients in a 2:1 ratio based on calendar year, age, sex, race, disease type, and use of disease-modifying antirheumatic drugs, biologics, and glucocorticoids. They followed patients from 30 days after vaccination – or the corresponding date in the unvaccinated cohort – until death, first episode of herpes zoster, or the end of 2013, whichever came first.
The rates of herpes zoster among vaccinated patients rose from 0.75/100 person-years during the first year after vaccination to 1.25/100 person-years during the seventh year of follow-up, Dr. Yun said. In contrast, zoster rates among unvaccinated patients remained steady, ranging between 1.32 and 1.35 cases per 100 person-years. In an adjusted analysis of data from 2006 through 2012, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52) and remained significantly less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92).
“The herpes zoster vaccine was effective for about 5 years, and results of subgroup analyses were consistent with the main analysis,” Dr. Yun concluded. But the Medicare database lacked details on disease severity or lifestyle factors, both of which might have affected the results, she cautioned.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
SAN FRANCISCO – Protection against shingles appeared to wane about 5 years after patients with autoimmune diseases received the live herpes zoster vaccine, according to a large retrospective cohort study presented at the annual meeting of the American College of Rheumatology.
In contrast, shingles risk remained fairly constant among unvaccinated patients during 7 years of follow-up, reported Dr. Huifeng Yun of the department of epidemiology at the University of Alabama at Birmingham. “Our findings suggest that patients might benefit from a booster vaccine at some point after initial vaccination, but further research is needed to determine when and if such a strategy is effective at preventing herpes zoster,” she said.
The long-term Shingles Prevention Study showed that the live herpes zoster vaccine is effective for about a decade among healthy older individuals. But about 90% of zoster cases occur in patients with autoimmune and inflammatory diseases, for whom the duration of vaccine protection has been unclear, Dr. Yun said. “Antiviral medication approved for herpes zoster reduces the severity and duration of symptoms, but may not prevent postherpetic neuralgia,” making vaccine protection a priority, she added.
Dr. Yun and her associates retrospectively analyzed Medicare data for nearly 179,000 patients with autoimmune and inflammatory conditions between 2006 and 2013. About one-third of patients were vaccinated against herpes zoster, and more than 40% had rheumatoid arthritis, nearly one-third had psoriasis, about 20% had inflammatory bowel disease, about 5% had psoriatic arthritis, and about 1% had ankylosing spondylitis. The researchers matched unvaccinated and vaccinated patients in a 2:1 ratio based on calendar year, age, sex, race, disease type, and use of disease-modifying antirheumatic drugs, biologics, and glucocorticoids. They followed patients from 30 days after vaccination – or the corresponding date in the unvaccinated cohort – until death, first episode of herpes zoster, or the end of 2013, whichever came first.
The rates of herpes zoster among vaccinated patients rose from 0.75/100 person-years during the first year after vaccination to 1.25/100 person-years during the seventh year of follow-up, Dr. Yun said. In contrast, zoster rates among unvaccinated patients remained steady, ranging between 1.32 and 1.35 cases per 100 person-years. In an adjusted analysis of data from 2006 through 2012, vaccinated patients had about half the risk of herpes zoster, compared with unvaccinated patients, during year 1 (relative risk, 0.52) and remained significantly less likely to develop shingles until year 6, when the gap in risk between vaccinated and unvaccinated patients essentially closed (RR, 0.92).
“The herpes zoster vaccine was effective for about 5 years, and results of subgroup analyses were consistent with the main analysis,” Dr. Yun concluded. But the Medicare database lacked details on disease severity or lifestyle factors, both of which might have affected the results, she cautioned.
Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Protection against shingles appeared to wane 5 years after patients with autoimmune diseases received the live herpes zoster vaccine.
Major finding: The risk of herpes zoster was significantly lower among vaccinated, compared with unvaccinated, patients during each of the first 5 years after vaccination.
Data source: A retrospective analysis of 178,881 Medicare patients with autoimmune diseases between 2006 and 2013.
Disclosures: Dr. Yun disclosed a financial relationship with Amgen. The senior author and two coauthors also disclosed relationships with several pharmaceutical companies. Two investigators had no disclosures.
ACR: Epratuzumab falls flat in phase III lupus trials
SAN FRANCISCO – The anti-CD22 monoclonal antibody epratuzumab missed its primary and secondary endpoints in two phase III trials involving adults with moderate to severe systemic lupus erythematosus.
At week 48, patients who received epratuzumab and standard therapy fared no better than those who received standard care and placebo, said Dr. Megan E.B. Clowse, who is a rheumatologist and clinical researcher at Duke University in Durham, N.C. “Many additional exploratory analyses were performed, and we really did not find any difference among the groups that would reveal a set of patients that would benefit from this treatment,” she said in her presentation of the two trials at the annual meeting of the American College of Rheumatology.
The failed EMBODY 1 and EMBODY 2 trials were identically designed phase III, multicenter, double-blind, randomized, placebo-controlled studies of adults with moderate to severe systemic lupus erythematosus (SLE), based on at least four ACR criteria, who also tested positive for anti–double stranded DNA or antinuclear antibodies. Participants were required to have received corticosteroids for at least 5 days before enrollment at a stable dose equivalent to 5-60 mg/day of prednisone. Doses of immunosuppressants and antimalarials also had to be stable, and patients could not have antiphospholipid syndrome or a British Isles Lupus Activity Group (BILAG) A score involving the kidneys or central nervous system. Most patients had musculoskeletal or musculocutaneous disease activity at baseline, Dr. Clowse said.
The treatment groups received standard-of-care therapies plus intravenous epratuzumab at doses of 1,200 mg every other week or 600 mg every week for a cumulative dose of 2,400 mg per 12-week treatment cycle, followed by 8 weeks without infusion. The primary endpoint was the percentage of responders by 48 weeks, as assessed by the composite BILAG-based Combined Lupus Assessment (BICLA). The BICLA measures improvement in BILAG disease activity across all eight body systems, with no worsening in BILAG or other disease activity indexes at the same time point and no treatment failure at any time point. There were a total of 1,579 patients in both studies combined.
About two-thirds of patients completed each study, and lack of efficacy was the main reason for dropping out, Dr. Clowse said. The primary endpoint was about 40% for all groups in both trials. Secondary endpoints, including changes in corticosteroid use, physician’s global assessment of disease activity, patient’s global assessment of disease activity, and other physician-reported and patient-reported outcomes, also were similar among the groups, she said. About 40% of patients remained on their baseline dose of corticosteroids, while less than 20% were able to cut their dose by at least half.
Epratuzumab was associated with improved SLE disease activity in phase IIb trials, Dr. Clowse noted. The biologic’s phase III safety profile resembled that of phase IIb trials and other prior studies, with no new safety signals, she added. The most common adverse events were upper respiratory tract infection, urinary tract infection, headache, and nausea.
UCB Pharma funded the study. Dr. Clowse reported having received consulting fees from UCB Pharma. Twelve of 15 coinvestigators also reported financial relationships with UCB Pharma and a number of other pharmaceutical companies.
SAN FRANCISCO – The anti-CD22 monoclonal antibody epratuzumab missed its primary and secondary endpoints in two phase III trials involving adults with moderate to severe systemic lupus erythematosus.
At week 48, patients who received epratuzumab and standard therapy fared no better than those who received standard care and placebo, said Dr. Megan E.B. Clowse, who is a rheumatologist and clinical researcher at Duke University in Durham, N.C. “Many additional exploratory analyses were performed, and we really did not find any difference among the groups that would reveal a set of patients that would benefit from this treatment,” she said in her presentation of the two trials at the annual meeting of the American College of Rheumatology.
The failed EMBODY 1 and EMBODY 2 trials were identically designed phase III, multicenter, double-blind, randomized, placebo-controlled studies of adults with moderate to severe systemic lupus erythematosus (SLE), based on at least four ACR criteria, who also tested positive for anti–double stranded DNA or antinuclear antibodies. Participants were required to have received corticosteroids for at least 5 days before enrollment at a stable dose equivalent to 5-60 mg/day of prednisone. Doses of immunosuppressants and antimalarials also had to be stable, and patients could not have antiphospholipid syndrome or a British Isles Lupus Activity Group (BILAG) A score involving the kidneys or central nervous system. Most patients had musculoskeletal or musculocutaneous disease activity at baseline, Dr. Clowse said.
The treatment groups received standard-of-care therapies plus intravenous epratuzumab at doses of 1,200 mg every other week or 600 mg every week for a cumulative dose of 2,400 mg per 12-week treatment cycle, followed by 8 weeks without infusion. The primary endpoint was the percentage of responders by 48 weeks, as assessed by the composite BILAG-based Combined Lupus Assessment (BICLA). The BICLA measures improvement in BILAG disease activity across all eight body systems, with no worsening in BILAG or other disease activity indexes at the same time point and no treatment failure at any time point. There were a total of 1,579 patients in both studies combined.
About two-thirds of patients completed each study, and lack of efficacy was the main reason for dropping out, Dr. Clowse said. The primary endpoint was about 40% for all groups in both trials. Secondary endpoints, including changes in corticosteroid use, physician’s global assessment of disease activity, patient’s global assessment of disease activity, and other physician-reported and patient-reported outcomes, also were similar among the groups, she said. About 40% of patients remained on their baseline dose of corticosteroids, while less than 20% were able to cut their dose by at least half.
Epratuzumab was associated with improved SLE disease activity in phase IIb trials, Dr. Clowse noted. The biologic’s phase III safety profile resembled that of phase IIb trials and other prior studies, with no new safety signals, she added. The most common adverse events were upper respiratory tract infection, urinary tract infection, headache, and nausea.
UCB Pharma funded the study. Dr. Clowse reported having received consulting fees from UCB Pharma. Twelve of 15 coinvestigators also reported financial relationships with UCB Pharma and a number of other pharmaceutical companies.
SAN FRANCISCO – The anti-CD22 monoclonal antibody epratuzumab missed its primary and secondary endpoints in two phase III trials involving adults with moderate to severe systemic lupus erythematosus.
At week 48, patients who received epratuzumab and standard therapy fared no better than those who received standard care and placebo, said Dr. Megan E.B. Clowse, who is a rheumatologist and clinical researcher at Duke University in Durham, N.C. “Many additional exploratory analyses were performed, and we really did not find any difference among the groups that would reveal a set of patients that would benefit from this treatment,” she said in her presentation of the two trials at the annual meeting of the American College of Rheumatology.
The failed EMBODY 1 and EMBODY 2 trials were identically designed phase III, multicenter, double-blind, randomized, placebo-controlled studies of adults with moderate to severe systemic lupus erythematosus (SLE), based on at least four ACR criteria, who also tested positive for anti–double stranded DNA or antinuclear antibodies. Participants were required to have received corticosteroids for at least 5 days before enrollment at a stable dose equivalent to 5-60 mg/day of prednisone. Doses of immunosuppressants and antimalarials also had to be stable, and patients could not have antiphospholipid syndrome or a British Isles Lupus Activity Group (BILAG) A score involving the kidneys or central nervous system. Most patients had musculoskeletal or musculocutaneous disease activity at baseline, Dr. Clowse said.
The treatment groups received standard-of-care therapies plus intravenous epratuzumab at doses of 1,200 mg every other week or 600 mg every week for a cumulative dose of 2,400 mg per 12-week treatment cycle, followed by 8 weeks without infusion. The primary endpoint was the percentage of responders by 48 weeks, as assessed by the composite BILAG-based Combined Lupus Assessment (BICLA). The BICLA measures improvement in BILAG disease activity across all eight body systems, with no worsening in BILAG or other disease activity indexes at the same time point and no treatment failure at any time point. There were a total of 1,579 patients in both studies combined.
About two-thirds of patients completed each study, and lack of efficacy was the main reason for dropping out, Dr. Clowse said. The primary endpoint was about 40% for all groups in both trials. Secondary endpoints, including changes in corticosteroid use, physician’s global assessment of disease activity, patient’s global assessment of disease activity, and other physician-reported and patient-reported outcomes, also were similar among the groups, she said. About 40% of patients remained on their baseline dose of corticosteroids, while less than 20% were able to cut their dose by at least half.
Epratuzumab was associated with improved SLE disease activity in phase IIb trials, Dr. Clowse noted. The biologic’s phase III safety profile resembled that of phase IIb trials and other prior studies, with no new safety signals, she added. The most common adverse events were upper respiratory tract infection, urinary tract infection, headache, and nausea.
UCB Pharma funded the study. Dr. Clowse reported having received consulting fees from UCB Pharma. Twelve of 15 coinvestigators also reported financial relationships with UCB Pharma and a number of other pharmaceutical companies.
AT THE ACR ANNUAL MEETING
Key clinical point: Epratuzumab was no more effective than placebo in two phase III trials of adults with moderate to severe systemic lupus erythematosus.
Major finding: Rates of BICLA response at 48 weeks were similar for the epratuzumab and placebo groups, as were all secondary and exploratory endpoints.
Data source: EMBODY 1 and 2 were phase III, multicenter, randomized, double-blind, placebo-controlled studies involving 1,579 adults.
Disclosures: UCB Pharma funded the study. Dr. Clowse reported having received consulting fees from UCB Pharma. Twelve of 15 coinvestigators also reported financial relationships with UCB Pharma and a number of other pharmaceutical companies.
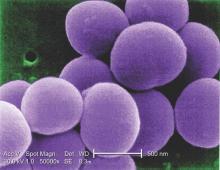
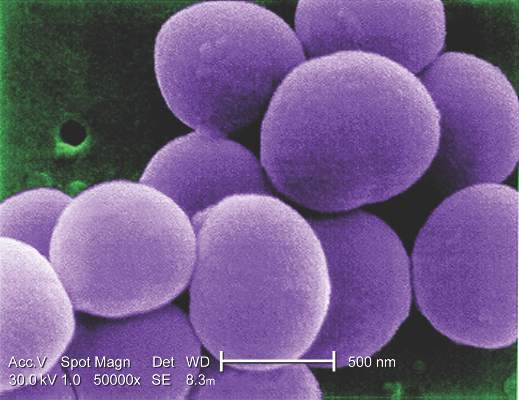
Staphylococcus aureus vaccine tolerable, immunogenic in preliminary study
SAN DIEGO – A vaccine designed to lower the risk of postoperative Staphylococcus aureus infections is being tested in a phase IIb study of adults who are preparing to undergo elective spinal fusion surgery.
In phase I-II trial results, reported at an annual scientific meeting on infectious diseases, the vaccine proved to be well tolerated, and it induced durable functional antibody responses.
The phase IIb trial aims to enroll 2,600 patients undergoing elective spinal fusion surgery, and is scheduled to end in 2017, said Dr. Buddy Creech of Vanderbilt University in Nashville, Tenn.
“We’re at a point where the disease frequency of Staphylococcus aureus is high enough that we could make the case for universal vaccination,” said Dr. Creech. “If we can prove it in high-risk hosts, I think that’s a win.”
Invasive staphylococcal disease causes more deaths in the United States than AIDS, viral hepatitis, and tuberculosis combined, but the complex virulence factors of S. aureus have eluded vaccine researchers for years. Other investigational vaccines failed in previous large phase III trials. The tetravalent vaccine now being tested targets type 5 and 8 capsular polysaccharides (CP5 and CP8), which are expressed by 95% of hospital-associated S. aureus strains; an adhesion molecule; and an essential recombinant manganese transport protein C.
The vaccine was well tolerated in a phase I study of healthy adults earlier this year. Single doses of vaccine or placebo were administered to 285 healthy adults aged 65-84 years in a randomized, multicenter double-blind trial. Patients averaged 71 years in age, and half were women, Dr. Creech said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Similar rates of mild to moderate adverse events occurred in both groups, and no participants died or had serious vaccine-related side effects, Dr. Creech said.
At 1 month after vaccination, all tetravalent vaccine recipients and 5% of placebo recipients had achieved a predetermined threshold for CP5 opsonophagocytic activity. Likewise, about 92% of vaccinated recipients and 19% of placebo recipients achieved the CP8 opsonophagocytic activity threshold. Further, 84% of vaccinated recipients and none of the placebo recipients had at least a fourfold rise in antibody titers against the adhesion molecule.
In vaccine recipients, an immunoassay found substantial rises in antibodies against all four antigens by day 8; levels peaked around day 15, Dr. Creech said. “There was a decline of antibody titers over the course of the next year, as one would expect with a single-dose vaccine, but they remained over prespecified thresholds,” he added.
“Durability of response is especially important for patients who are scheduling surgeries and others who have a definitive risk period” for infection, he said.
Pfizer is funding the research, and Dr. Creech is a grant investigator for the company. One coauthor is also a grant investigator for Pfizer, nine coauthors are Pfizer employees and shareholders, and three declared no relevant conflicts of interest.
SAN DIEGO – A vaccine designed to lower the risk of postoperative Staphylococcus aureus infections is being tested in a phase IIb study of adults who are preparing to undergo elective spinal fusion surgery.
In phase I-II trial results, reported at an annual scientific meeting on infectious diseases, the vaccine proved to be well tolerated, and it induced durable functional antibody responses.
The phase IIb trial aims to enroll 2,600 patients undergoing elective spinal fusion surgery, and is scheduled to end in 2017, said Dr. Buddy Creech of Vanderbilt University in Nashville, Tenn.
“We’re at a point where the disease frequency of Staphylococcus aureus is high enough that we could make the case for universal vaccination,” said Dr. Creech. “If we can prove it in high-risk hosts, I think that’s a win.”
Invasive staphylococcal disease causes more deaths in the United States than AIDS, viral hepatitis, and tuberculosis combined, but the complex virulence factors of S. aureus have eluded vaccine researchers for years. Other investigational vaccines failed in previous large phase III trials. The tetravalent vaccine now being tested targets type 5 and 8 capsular polysaccharides (CP5 and CP8), which are expressed by 95% of hospital-associated S. aureus strains; an adhesion molecule; and an essential recombinant manganese transport protein C.
The vaccine was well tolerated in a phase I study of healthy adults earlier this year. Single doses of vaccine or placebo were administered to 285 healthy adults aged 65-84 years in a randomized, multicenter double-blind trial. Patients averaged 71 years in age, and half were women, Dr. Creech said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Similar rates of mild to moderate adverse events occurred in both groups, and no participants died or had serious vaccine-related side effects, Dr. Creech said.
At 1 month after vaccination, all tetravalent vaccine recipients and 5% of placebo recipients had achieved a predetermined threshold for CP5 opsonophagocytic activity. Likewise, about 92% of vaccinated recipients and 19% of placebo recipients achieved the CP8 opsonophagocytic activity threshold. Further, 84% of vaccinated recipients and none of the placebo recipients had at least a fourfold rise in antibody titers against the adhesion molecule.
In vaccine recipients, an immunoassay found substantial rises in antibodies against all four antigens by day 8; levels peaked around day 15, Dr. Creech said. “There was a decline of antibody titers over the course of the next year, as one would expect with a single-dose vaccine, but they remained over prespecified thresholds,” he added.
“Durability of response is especially important for patients who are scheduling surgeries and others who have a definitive risk period” for infection, he said.
Pfizer is funding the research, and Dr. Creech is a grant investigator for the company. One coauthor is also a grant investigator for Pfizer, nine coauthors are Pfizer employees and shareholders, and three declared no relevant conflicts of interest.
SAN DIEGO – A vaccine designed to lower the risk of postoperative Staphylococcus aureus infections is being tested in a phase IIb study of adults who are preparing to undergo elective spinal fusion surgery.
In phase I-II trial results, reported at an annual scientific meeting on infectious diseases, the vaccine proved to be well tolerated, and it induced durable functional antibody responses.
The phase IIb trial aims to enroll 2,600 patients undergoing elective spinal fusion surgery, and is scheduled to end in 2017, said Dr. Buddy Creech of Vanderbilt University in Nashville, Tenn.
“We’re at a point where the disease frequency of Staphylococcus aureus is high enough that we could make the case for universal vaccination,” said Dr. Creech. “If we can prove it in high-risk hosts, I think that’s a win.”
Invasive staphylococcal disease causes more deaths in the United States than AIDS, viral hepatitis, and tuberculosis combined, but the complex virulence factors of S. aureus have eluded vaccine researchers for years. Other investigational vaccines failed in previous large phase III trials. The tetravalent vaccine now being tested targets type 5 and 8 capsular polysaccharides (CP5 and CP8), which are expressed by 95% of hospital-associated S. aureus strains; an adhesion molecule; and an essential recombinant manganese transport protein C.
The vaccine was well tolerated in a phase I study of healthy adults earlier this year. Single doses of vaccine or placebo were administered to 285 healthy adults aged 65-84 years in a randomized, multicenter double-blind trial. Patients averaged 71 years in age, and half were women, Dr. Creech said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Similar rates of mild to moderate adverse events occurred in both groups, and no participants died or had serious vaccine-related side effects, Dr. Creech said.
At 1 month after vaccination, all tetravalent vaccine recipients and 5% of placebo recipients had achieved a predetermined threshold for CP5 opsonophagocytic activity. Likewise, about 92% of vaccinated recipients and 19% of placebo recipients achieved the CP8 opsonophagocytic activity threshold. Further, 84% of vaccinated recipients and none of the placebo recipients had at least a fourfold rise in antibody titers against the adhesion molecule.
In vaccine recipients, an immunoassay found substantial rises in antibodies against all four antigens by day 8; levels peaked around day 15, Dr. Creech said. “There was a decline of antibody titers over the course of the next year, as one would expect with a single-dose vaccine, but they remained over prespecified thresholds,” he added.
“Durability of response is especially important for patients who are scheduling surgeries and others who have a definitive risk period” for infection, he said.
Pfizer is funding the research, and Dr. Creech is a grant investigator for the company. One coauthor is also a grant investigator for Pfizer, nine coauthors are Pfizer employees and shareholders, and three declared no relevant conflicts of interest.
AT IDWEEK 2015
Key clinical point: A four-antigen vaccine against Staphylococcus aureus yielded durable functional antibody responses and no major safety signals in a phase I-II trial.
Major finding: There were no vaccine-related serious adverse effects and no signs of dose-related reactogenicity, and researchers observed sustained bacterial killing at month 12.
Data source: A multicenter, randomized, double-blind placebo-controlled trial of 285 healthy adults aged 65-84 years.
Disclosures: Pfizer is funding the research. Dr. Creech is a grant investigator for the company. One coauthor is also a grant investigator for Pfizer, nine coauthors are Pfizer employees and shareholders, and three declared no relevant conflicts of interest.
ACR: New Sjögren’s classification criteria on the way
SAN FRANCISCO – New classification criteria for Sjögren’s syndrome are ready for sign-off by the American College of Rheumatology and the European League Against Rheumatism, Dr. Caroline Shiboski said.
“We hope this will be the last iteration of the international classification criteria that we have proposed to ACR and EULAR,” said Dr. Shiboski, professor of orofacial sciences at the University of California San Francisco School of Dentistry.
The criteria will give researchers a single set of consensus diagnostic measures for Sjögren’s syndrome, replacing both the provisional 2012 ACR criteria (Arthritis Care Res (Hoboken). 2012 Apr;64[4]:475-87) and criteria from the American-European Consensus Group, added Dr. Shiboski, who led the led the ACR steering committee that helped to create the criteria. “These criteria aim to classify clinical trial participants,” she added. “That doesn’t mean we can’t use them for diagnostic purposes, but that was not the primary purpose.”
Sjögren’s syndrome is complex, with differential diagnoses ranging from non-autoimmune sicca syndrome and IgG4-related disease to sarcoidosis, hematologic cancers, and amyloidosis, said Dr. Alan Baer, one of the clinician-experts who participated in the working group that led to the new criteria. Moreover, patients need care from rheumatologists, ophthalmologists, and oral medicine specialists to manage systemic symptoms and sequelae of sicca and xerostomia. The lack of consensus criteria has made it hard even to estimate the incidence and prevalence of the disease, researchers have noted (Clin Epidemiol. 2014;6:247-55). Furthermore, some rheumatologists criticized the provisional ACR criteria for requiring a salivary gland biopsy and ophthalmologic testing, both of which are time consuming and unavailable in many practices.
The new criteria help to solve some of those problems, Dr. Shiboski and her fellow experts said at the annual meeting of the American College of Rheumatology.* They add two simpler diagnostic options: the Schirmer tear test and the 5-minute salivary flow test. They also weight the various diagnostic tests, assigning 2 points each to the focus score for focal lymphocytic sialadenitis and the presence of anti–Sjögren’s syndrome antibody A; and 1 point each for a Schirmer test of 5 mm in less than 5 min, an ocular staining score of greater than 5, and salivary flow rate of less than 0.1 mL/min.
Patients need a total of 4 points for a confirmed diagnosis of Sjögren’s syndrome. Because diagnosis no longer requires mucosal dryness, the new criteria “are more flexible, and allow us to select patients in the earlier stages of Sjögren’s syndrome who are more likely to show improvement with treatment,” said Dr. Raphaèle Seror, a clinical rheumatologist at Hôpitaux universitaires Paris-Sud in France and a member of the EULAR Steering Committee for the criteria.
Nonetheless, the new criteria have “some recognizable limitations,” said Dr. Baer, director of the Johns Hopkins Jerome L. Greene Sjögren’s Syndrome Center in Baltimore. They are not validated for secondary or juvenile forms of Sjögren’s or for the subset of cases associated with anticentromere antibodies, he noted. They also exclude several established diagnostic tools, including CT, MRI, and sialography or scintigraphy, as well as several “emerging” tools such as parotid gland biopsy, ultrasonography, and tests for novel autoantibodies, he added.
Criteria aside, “when you go into the clinic, it’s important that you do a complete evaluation of the patient who comes to you complaining of dry eyes and a dry mouth,” Dr. Baer emphasized. “The way you ask these questions is really important. Look for daily, persistent, dry eyes and dry mouth.”
Diagnostic tests for Sjögren’s syndrome are imperfect, so clinicians should interpret them carefully. The Schirmer tear test is relatively unreliable and insensitive, and its values normally decline in older patients. Ocular surface staining results also are nonspecific and prone to inconsistent interpretation, according to Dr. Baer. The single most reliable test is a labial gland biopsy with a focus score of 1 or higher, meaning that a 4 mm2 area has at least one cluster of at least 50 lymphocytes adjacent to salivary gland acini, he said.
To draft the criteria, Dr. Shiboski and her colleagues used 1000Minds decision-making software to show 55 experts dozens of fictive clinical vignettes. For each vignette, the experts were asked to use the existing ACR criteria to determine whether or not the patient had Sjögren’s syndrome; they also could say that they were unsure. Analyzing the vignettes on which experts’ agreed approach yielded a set of draft diagnostic criteria, which were then tested among 1,200 real-life patients with Sjögren’s from the real-life Sjögren’s International Collaborative Clinical Alliance (SICCA), Paris-Sud, and Oklahoma Medical Research Foundation (OMRF) cohorts, Dr. Shiboski said. Specificity received double the weight of sensitivity, because “in clinical trials, you want specificity to be as high as possible,” she added.
The National Institutes of Health, the National Institute of Dental and Craniofacial Research, the Phileona Foundation, and the Sjögren’s Syndrome Foundation helped fund the SICCA and OMRF cohort studies on which the criteria were based. Dr. Shiboski and Dr. Seror had no disclosures. Dr. Baer reported having been a consultant for Bristol-Myers Squibb and Glenmark Pharmaceuticals.
* Correction, 11/17/15: Dr. Shiboski's gender was previously misstated.
SAN FRANCISCO – New classification criteria for Sjögren’s syndrome are ready for sign-off by the American College of Rheumatology and the European League Against Rheumatism, Dr. Caroline Shiboski said.
“We hope this will be the last iteration of the international classification criteria that we have proposed to ACR and EULAR,” said Dr. Shiboski, professor of orofacial sciences at the University of California San Francisco School of Dentistry.
The criteria will give researchers a single set of consensus diagnostic measures for Sjögren’s syndrome, replacing both the provisional 2012 ACR criteria (Arthritis Care Res (Hoboken). 2012 Apr;64[4]:475-87) and criteria from the American-European Consensus Group, added Dr. Shiboski, who led the led the ACR steering committee that helped to create the criteria. “These criteria aim to classify clinical trial participants,” she added. “That doesn’t mean we can’t use them for diagnostic purposes, but that was not the primary purpose.”
Sjögren’s syndrome is complex, with differential diagnoses ranging from non-autoimmune sicca syndrome and IgG4-related disease to sarcoidosis, hematologic cancers, and amyloidosis, said Dr. Alan Baer, one of the clinician-experts who participated in the working group that led to the new criteria. Moreover, patients need care from rheumatologists, ophthalmologists, and oral medicine specialists to manage systemic symptoms and sequelae of sicca and xerostomia. The lack of consensus criteria has made it hard even to estimate the incidence and prevalence of the disease, researchers have noted (Clin Epidemiol. 2014;6:247-55). Furthermore, some rheumatologists criticized the provisional ACR criteria for requiring a salivary gland biopsy and ophthalmologic testing, both of which are time consuming and unavailable in many practices.
The new criteria help to solve some of those problems, Dr. Shiboski and her fellow experts said at the annual meeting of the American College of Rheumatology.* They add two simpler diagnostic options: the Schirmer tear test and the 5-minute salivary flow test. They also weight the various diagnostic tests, assigning 2 points each to the focus score for focal lymphocytic sialadenitis and the presence of anti–Sjögren’s syndrome antibody A; and 1 point each for a Schirmer test of 5 mm in less than 5 min, an ocular staining score of greater than 5, and salivary flow rate of less than 0.1 mL/min.
Patients need a total of 4 points for a confirmed diagnosis of Sjögren’s syndrome. Because diagnosis no longer requires mucosal dryness, the new criteria “are more flexible, and allow us to select patients in the earlier stages of Sjögren’s syndrome who are more likely to show improvement with treatment,” said Dr. Raphaèle Seror, a clinical rheumatologist at Hôpitaux universitaires Paris-Sud in France and a member of the EULAR Steering Committee for the criteria.
Nonetheless, the new criteria have “some recognizable limitations,” said Dr. Baer, director of the Johns Hopkins Jerome L. Greene Sjögren’s Syndrome Center in Baltimore. They are not validated for secondary or juvenile forms of Sjögren’s or for the subset of cases associated with anticentromere antibodies, he noted. They also exclude several established diagnostic tools, including CT, MRI, and sialography or scintigraphy, as well as several “emerging” tools such as parotid gland biopsy, ultrasonography, and tests for novel autoantibodies, he added.
Criteria aside, “when you go into the clinic, it’s important that you do a complete evaluation of the patient who comes to you complaining of dry eyes and a dry mouth,” Dr. Baer emphasized. “The way you ask these questions is really important. Look for daily, persistent, dry eyes and dry mouth.”
Diagnostic tests for Sjögren’s syndrome are imperfect, so clinicians should interpret them carefully. The Schirmer tear test is relatively unreliable and insensitive, and its values normally decline in older patients. Ocular surface staining results also are nonspecific and prone to inconsistent interpretation, according to Dr. Baer. The single most reliable test is a labial gland biopsy with a focus score of 1 or higher, meaning that a 4 mm2 area has at least one cluster of at least 50 lymphocytes adjacent to salivary gland acini, he said.
To draft the criteria, Dr. Shiboski and her colleagues used 1000Minds decision-making software to show 55 experts dozens of fictive clinical vignettes. For each vignette, the experts were asked to use the existing ACR criteria to determine whether or not the patient had Sjögren’s syndrome; they also could say that they were unsure. Analyzing the vignettes on which experts’ agreed approach yielded a set of draft diagnostic criteria, which were then tested among 1,200 real-life patients with Sjögren’s from the real-life Sjögren’s International Collaborative Clinical Alliance (SICCA), Paris-Sud, and Oklahoma Medical Research Foundation (OMRF) cohorts, Dr. Shiboski said. Specificity received double the weight of sensitivity, because “in clinical trials, you want specificity to be as high as possible,” she added.
The National Institutes of Health, the National Institute of Dental and Craniofacial Research, the Phileona Foundation, and the Sjögren’s Syndrome Foundation helped fund the SICCA and OMRF cohort studies on which the criteria were based. Dr. Shiboski and Dr. Seror had no disclosures. Dr. Baer reported having been a consultant for Bristol-Myers Squibb and Glenmark Pharmaceuticals.
* Correction, 11/17/15: Dr. Shiboski's gender was previously misstated.
SAN FRANCISCO – New classification criteria for Sjögren’s syndrome are ready for sign-off by the American College of Rheumatology and the European League Against Rheumatism, Dr. Caroline Shiboski said.
“We hope this will be the last iteration of the international classification criteria that we have proposed to ACR and EULAR,” said Dr. Shiboski, professor of orofacial sciences at the University of California San Francisco School of Dentistry.
The criteria will give researchers a single set of consensus diagnostic measures for Sjögren’s syndrome, replacing both the provisional 2012 ACR criteria (Arthritis Care Res (Hoboken). 2012 Apr;64[4]:475-87) and criteria from the American-European Consensus Group, added Dr. Shiboski, who led the led the ACR steering committee that helped to create the criteria. “These criteria aim to classify clinical trial participants,” she added. “That doesn’t mean we can’t use them for diagnostic purposes, but that was not the primary purpose.”
Sjögren’s syndrome is complex, with differential diagnoses ranging from non-autoimmune sicca syndrome and IgG4-related disease to sarcoidosis, hematologic cancers, and amyloidosis, said Dr. Alan Baer, one of the clinician-experts who participated in the working group that led to the new criteria. Moreover, patients need care from rheumatologists, ophthalmologists, and oral medicine specialists to manage systemic symptoms and sequelae of sicca and xerostomia. The lack of consensus criteria has made it hard even to estimate the incidence and prevalence of the disease, researchers have noted (Clin Epidemiol. 2014;6:247-55). Furthermore, some rheumatologists criticized the provisional ACR criteria for requiring a salivary gland biopsy and ophthalmologic testing, both of which are time consuming and unavailable in many practices.
The new criteria help to solve some of those problems, Dr. Shiboski and her fellow experts said at the annual meeting of the American College of Rheumatology.* They add two simpler diagnostic options: the Schirmer tear test and the 5-minute salivary flow test. They also weight the various diagnostic tests, assigning 2 points each to the focus score for focal lymphocytic sialadenitis and the presence of anti–Sjögren’s syndrome antibody A; and 1 point each for a Schirmer test of 5 mm in less than 5 min, an ocular staining score of greater than 5, and salivary flow rate of less than 0.1 mL/min.
Patients need a total of 4 points for a confirmed diagnosis of Sjögren’s syndrome. Because diagnosis no longer requires mucosal dryness, the new criteria “are more flexible, and allow us to select patients in the earlier stages of Sjögren’s syndrome who are more likely to show improvement with treatment,” said Dr. Raphaèle Seror, a clinical rheumatologist at Hôpitaux universitaires Paris-Sud in France and a member of the EULAR Steering Committee for the criteria.
Nonetheless, the new criteria have “some recognizable limitations,” said Dr. Baer, director of the Johns Hopkins Jerome L. Greene Sjögren’s Syndrome Center in Baltimore. They are not validated for secondary or juvenile forms of Sjögren’s or for the subset of cases associated with anticentromere antibodies, he noted. They also exclude several established diagnostic tools, including CT, MRI, and sialography or scintigraphy, as well as several “emerging” tools such as parotid gland biopsy, ultrasonography, and tests for novel autoantibodies, he added.
Criteria aside, “when you go into the clinic, it’s important that you do a complete evaluation of the patient who comes to you complaining of dry eyes and a dry mouth,” Dr. Baer emphasized. “The way you ask these questions is really important. Look for daily, persistent, dry eyes and dry mouth.”
Diagnostic tests for Sjögren’s syndrome are imperfect, so clinicians should interpret them carefully. The Schirmer tear test is relatively unreliable and insensitive, and its values normally decline in older patients. Ocular surface staining results also are nonspecific and prone to inconsistent interpretation, according to Dr. Baer. The single most reliable test is a labial gland biopsy with a focus score of 1 or higher, meaning that a 4 mm2 area has at least one cluster of at least 50 lymphocytes adjacent to salivary gland acini, he said.
To draft the criteria, Dr. Shiboski and her colleagues used 1000Minds decision-making software to show 55 experts dozens of fictive clinical vignettes. For each vignette, the experts were asked to use the existing ACR criteria to determine whether or not the patient had Sjögren’s syndrome; they also could say that they were unsure. Analyzing the vignettes on which experts’ agreed approach yielded a set of draft diagnostic criteria, which were then tested among 1,200 real-life patients with Sjögren’s from the real-life Sjögren’s International Collaborative Clinical Alliance (SICCA), Paris-Sud, and Oklahoma Medical Research Foundation (OMRF) cohorts, Dr. Shiboski said. Specificity received double the weight of sensitivity, because “in clinical trials, you want specificity to be as high as possible,” she added.
The National Institutes of Health, the National Institute of Dental and Craniofacial Research, the Phileona Foundation, and the Sjögren’s Syndrome Foundation helped fund the SICCA and OMRF cohort studies on which the criteria were based. Dr. Shiboski and Dr. Seror had no disclosures. Dr. Baer reported having been a consultant for Bristol-Myers Squibb and Glenmark Pharmaceuticals.
* Correction, 11/17/15: Dr. Shiboski's gender was previously misstated.
AT THE ACR ANNUAL MEETING
VIDEO: Chondroitin tops celecoxib in reducing knee OA structural progression
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
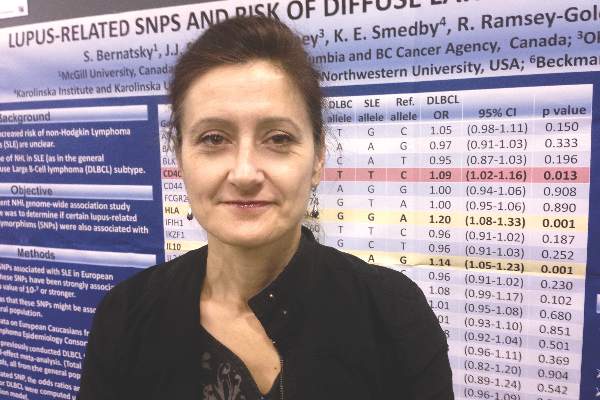
Lupus and diffuse large B-cell lymphoma share genetic risk
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Two genetic risk variants for systemic lupus erythematosus also were clearly linked to risk of diffuse large B-cell lymphoma.
Major finding: The single-nucleotide polymorphisms were rs3024505 on chromosome 1 (OR, 1.14; P = .001), and rs1270942 on chromosome 6 (OR, 1.2; P = .0007).
Data source: A fixed-effect meta-analysis of 28 SLE-related SNPs from 3,857 patients with diffuse large B-cell lymphoma and 7,666 controls.
Disclosures: The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
VIDEO: Obesity decreased chances of sustained RA remission
SAN FRANCISCO – Obese patients with rheumatoid arthritis are significantly less likely to achieve sustained disease remission than are their peers who are normal weight or overweight, based on data reported at the annual meeting of the American College of Rheumatology.
In an analysis of more than 1,000 patients with RA from the multicenter, prospective CATCH (Canadian Early Arthritis Cohort) study, about 28% of obese (body mass index of 30 kg/m2 or greater) patients achieved sustained remission, defined as a 28-joint Disease Activity Score of 2.6 or less at two consecutive clinical visits.
In contrast, 38% of overweight (BMI 25-29.9) and 48% of normal-weight (BMI 18.5-24.9) patients reached that goal, said Dr. Vivian P. Bykerk, director of the Inflammatory Arthritis Center of Excellence at the Hospital for Special Surgery, New York, and a clinical researcher at Weill Cornell Medical College, New York. In an exclusive video interview, Dr. Bykerk discusses the findings and their implications.
Dr. Bykerk is the founder and principal investigator for the CATCH study, which is sponsored by Amgen, Pfizer, Hoffmann-La Roche, UCB Canada, Bristol-Myers Squibb, AbbVie, and Janssen Biotech.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Obese patients with rheumatoid arthritis are significantly less likely to achieve sustained disease remission than are their peers who are normal weight or overweight, based on data reported at the annual meeting of the American College of Rheumatology.
In an analysis of more than 1,000 patients with RA from the multicenter, prospective CATCH (Canadian Early Arthritis Cohort) study, about 28% of obese (body mass index of 30 kg/m2 or greater) patients achieved sustained remission, defined as a 28-joint Disease Activity Score of 2.6 or less at two consecutive clinical visits.
In contrast, 38% of overweight (BMI 25-29.9) and 48% of normal-weight (BMI 18.5-24.9) patients reached that goal, said Dr. Vivian P. Bykerk, director of the Inflammatory Arthritis Center of Excellence at the Hospital for Special Surgery, New York, and a clinical researcher at Weill Cornell Medical College, New York. In an exclusive video interview, Dr. Bykerk discusses the findings and their implications.
Dr. Bykerk is the founder and principal investigator for the CATCH study, which is sponsored by Amgen, Pfizer, Hoffmann-La Roche, UCB Canada, Bristol-Myers Squibb, AbbVie, and Janssen Biotech.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Obese patients with rheumatoid arthritis are significantly less likely to achieve sustained disease remission than are their peers who are normal weight or overweight, based on data reported at the annual meeting of the American College of Rheumatology.
In an analysis of more than 1,000 patients with RA from the multicenter, prospective CATCH (Canadian Early Arthritis Cohort) study, about 28% of obese (body mass index of 30 kg/m2 or greater) patients achieved sustained remission, defined as a 28-joint Disease Activity Score of 2.6 or less at two consecutive clinical visits.
In contrast, 38% of overweight (BMI 25-29.9) and 48% of normal-weight (BMI 18.5-24.9) patients reached that goal, said Dr. Vivian P. Bykerk, director of the Inflammatory Arthritis Center of Excellence at the Hospital for Special Surgery, New York, and a clinical researcher at Weill Cornell Medical College, New York. In an exclusive video interview, Dr. Bykerk discusses the findings and their implications.
Dr. Bykerk is the founder and principal investigator for the CATCH study, which is sponsored by Amgen, Pfizer, Hoffmann-La Roche, UCB Canada, Bristol-Myers Squibb, AbbVie, and Janssen Biotech.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
Peer support program improved cardiovascular health, tobacco cessation
A monthly peer-led support program for adults with risk factors for heart disease achieved small but significant gains in overall cardiovascular health and smoking cessation, according to a multicenter, randomized, controlled trial.
After 12 months, participants scored an average of 0.75 points higher than baseline on a novel composite measure of cardiovascular health – the Fuster-BEWAT Score (FBS) – compared with controls, reported Emilia Gómez, Ph.D., at SHE Foundation, Barcelona, Dr. Juan Miguel Fernández-Alvira of Fundación Centro Nacional de Investigaciones Cardiovasculares, Madrid, and their associates.
“Even though the magnitude of the impact of our intervention was modest, epidemiological data suggest that even very small changes in health behaviors and risk factors can significantly decrease the long-term risk of cardiovascular disease,” the investigators wrote. They presented the findings at the American Heart Association scientific sessions and simultaneously in the Journal of the American College of Cardiology.
Peer support has been used for managing various chronic diseases, but the Fifty-Fifty Program is the first multicenter, randomized trial to assess its efficacy while also accounting for baseline health education, said the investigators.
To do so, they designed a run-in of six workshops for 543 adults aged 25-50 years who had hypertension, were overweight or obese, smoked, or exercised 150 minutes or less a week. The participants, 71% of whom were female, were then randomized to receive no further support or to attend monthly, 60- to 90-minute sessions that included role playing, brainstorming, and activities focused on managing emotions, diet, and exercise. The 10 members of each group elected their own leaders, who then completed 3 hours of training in health promotion and leadership.
After 12 months, the intervention group scored an average of 8.84 (95% confidence interval, 8.37-9.32) on the FBS’ composite measure of blood pressure, exercise, weight, diet, and tobacco use, compared with 8.17 for controls (95% CI, 7.55-8.79; P = .016). The intervention group also improved 0.75 points more from baseline, compared with controls (95% CI, 0.32-1.18).
In addition, support group members scored 0.24 points higher on the 1-year measure of tobacco cessation (95% CI, 0.09-0.38; P = .003). The groups did not otherwise significantly differ in terms of individual risk factors, but the intervention group outscored the control group on measures of blood pressure, exercise, and diet.
“The results of the Fifty-Fifty study show that promoting healthier lifestyles focusing on self control of unhealthy behaviors through peer group support can be beneficial to heterogeneous groups, without a single condition or specific CV risk factors,” the researchers concluded. “Although this is a relatively short-term intervention study, follow-up results will provide insight into long-term sustainability of peer group support and long-term effect on cardiovascular health.”
The SHE Foundation and the Spanish Ministry of Health, Social Services and Equality jointly funded the research. The investigators did not report conflicts of interest.
The Fifty-Fifty Program offers several innovations to the field of cardiovascular prevention. First, the program did not just address one risk factor, but instead emphasized multiple aspects of cardiovascular health, including health behaviors (healthy diet and increasing physical activity) and health metrics (blood pressure and body mass index) as measured by the novel risk score, the FBS. The ability of the FBS to predict clinical outcomes has not been fully validated; but all of the included measures are intimately linked to cardiovascular health and easily reproducible in other settings, since they consist of only health behaviors and non-laboratory–based health factors.

|
Dr. Fatima Rodriguez |
Second, the Fifty-Fifty Program employed the widely used psychological interventions of peer support and group dynamics to yield modest yet positive results in CVH improvement at 1 year follow-up. Importantly, participants in the study selected the peer leaders. When interventions have this type of community buy-in, they are more likely to be successful. Finally, peer-based interventions are more likely to be self sustainable and scalable in the long term, and have wide applicability in diverse and resource-limited settings.
An important limitation of the Fifty-Fifty program was its attrition rate of 16%. Those who dropped out of the study tended to be younger and to have less favorable CVH profiles, which may have created selection bias and impacted the generalizability of the results.
Dr. Fatima Rodriguez is with the division of cardiovascular medicine, Stanford (Calif.) University. Dr. Robert Harrington is with the department of medicine, Stanford University. They reported no conflicts of interest.
The Fifty-Fifty Program offers several innovations to the field of cardiovascular prevention. First, the program did not just address one risk factor, but instead emphasized multiple aspects of cardiovascular health, including health behaviors (healthy diet and increasing physical activity) and health metrics (blood pressure and body mass index) as measured by the novel risk score, the FBS. The ability of the FBS to predict clinical outcomes has not been fully validated; but all of the included measures are intimately linked to cardiovascular health and easily reproducible in other settings, since they consist of only health behaviors and non-laboratory–based health factors.

|
Dr. Fatima Rodriguez |
Second, the Fifty-Fifty Program employed the widely used psychological interventions of peer support and group dynamics to yield modest yet positive results in CVH improvement at 1 year follow-up. Importantly, participants in the study selected the peer leaders. When interventions have this type of community buy-in, they are more likely to be successful. Finally, peer-based interventions are more likely to be self sustainable and scalable in the long term, and have wide applicability in diverse and resource-limited settings.
An important limitation of the Fifty-Fifty program was its attrition rate of 16%. Those who dropped out of the study tended to be younger and to have less favorable CVH profiles, which may have created selection bias and impacted the generalizability of the results.
Dr. Fatima Rodriguez is with the division of cardiovascular medicine, Stanford (Calif.) University. Dr. Robert Harrington is with the department of medicine, Stanford University. They reported no conflicts of interest.
The Fifty-Fifty Program offers several innovations to the field of cardiovascular prevention. First, the program did not just address one risk factor, but instead emphasized multiple aspects of cardiovascular health, including health behaviors (healthy diet and increasing physical activity) and health metrics (blood pressure and body mass index) as measured by the novel risk score, the FBS. The ability of the FBS to predict clinical outcomes has not been fully validated; but all of the included measures are intimately linked to cardiovascular health and easily reproducible in other settings, since they consist of only health behaviors and non-laboratory–based health factors.

|
Dr. Fatima Rodriguez |
Second, the Fifty-Fifty Program employed the widely used psychological interventions of peer support and group dynamics to yield modest yet positive results in CVH improvement at 1 year follow-up. Importantly, participants in the study selected the peer leaders. When interventions have this type of community buy-in, they are more likely to be successful. Finally, peer-based interventions are more likely to be self sustainable and scalable in the long term, and have wide applicability in diverse and resource-limited settings.
An important limitation of the Fifty-Fifty program was its attrition rate of 16%. Those who dropped out of the study tended to be younger and to have less favorable CVH profiles, which may have created selection bias and impacted the generalizability of the results.
Dr. Fatima Rodriguez is with the division of cardiovascular medicine, Stanford (Calif.) University. Dr. Robert Harrington is with the department of medicine, Stanford University. They reported no conflicts of interest.
A monthly peer-led support program for adults with risk factors for heart disease achieved small but significant gains in overall cardiovascular health and smoking cessation, according to a multicenter, randomized, controlled trial.
After 12 months, participants scored an average of 0.75 points higher than baseline on a novel composite measure of cardiovascular health – the Fuster-BEWAT Score (FBS) – compared with controls, reported Emilia Gómez, Ph.D., at SHE Foundation, Barcelona, Dr. Juan Miguel Fernández-Alvira of Fundación Centro Nacional de Investigaciones Cardiovasculares, Madrid, and their associates.
“Even though the magnitude of the impact of our intervention was modest, epidemiological data suggest that even very small changes in health behaviors and risk factors can significantly decrease the long-term risk of cardiovascular disease,” the investigators wrote. They presented the findings at the American Heart Association scientific sessions and simultaneously in the Journal of the American College of Cardiology.
Peer support has been used for managing various chronic diseases, but the Fifty-Fifty Program is the first multicenter, randomized trial to assess its efficacy while also accounting for baseline health education, said the investigators.
To do so, they designed a run-in of six workshops for 543 adults aged 25-50 years who had hypertension, were overweight or obese, smoked, or exercised 150 minutes or less a week. The participants, 71% of whom were female, were then randomized to receive no further support or to attend monthly, 60- to 90-minute sessions that included role playing, brainstorming, and activities focused on managing emotions, diet, and exercise. The 10 members of each group elected their own leaders, who then completed 3 hours of training in health promotion and leadership.
After 12 months, the intervention group scored an average of 8.84 (95% confidence interval, 8.37-9.32) on the FBS’ composite measure of blood pressure, exercise, weight, diet, and tobacco use, compared with 8.17 for controls (95% CI, 7.55-8.79; P = .016). The intervention group also improved 0.75 points more from baseline, compared with controls (95% CI, 0.32-1.18).
In addition, support group members scored 0.24 points higher on the 1-year measure of tobacco cessation (95% CI, 0.09-0.38; P = .003). The groups did not otherwise significantly differ in terms of individual risk factors, but the intervention group outscored the control group on measures of blood pressure, exercise, and diet.
“The results of the Fifty-Fifty study show that promoting healthier lifestyles focusing on self control of unhealthy behaviors through peer group support can be beneficial to heterogeneous groups, without a single condition or specific CV risk factors,” the researchers concluded. “Although this is a relatively short-term intervention study, follow-up results will provide insight into long-term sustainability of peer group support and long-term effect on cardiovascular health.”
The SHE Foundation and the Spanish Ministry of Health, Social Services and Equality jointly funded the research. The investigators did not report conflicts of interest.
A monthly peer-led support program for adults with risk factors for heart disease achieved small but significant gains in overall cardiovascular health and smoking cessation, according to a multicenter, randomized, controlled trial.
After 12 months, participants scored an average of 0.75 points higher than baseline on a novel composite measure of cardiovascular health – the Fuster-BEWAT Score (FBS) – compared with controls, reported Emilia Gómez, Ph.D., at SHE Foundation, Barcelona, Dr. Juan Miguel Fernández-Alvira of Fundación Centro Nacional de Investigaciones Cardiovasculares, Madrid, and their associates.
“Even though the magnitude of the impact of our intervention was modest, epidemiological data suggest that even very small changes in health behaviors and risk factors can significantly decrease the long-term risk of cardiovascular disease,” the investigators wrote. They presented the findings at the American Heart Association scientific sessions and simultaneously in the Journal of the American College of Cardiology.
Peer support has been used for managing various chronic diseases, but the Fifty-Fifty Program is the first multicenter, randomized trial to assess its efficacy while also accounting for baseline health education, said the investigators.
To do so, they designed a run-in of six workshops for 543 adults aged 25-50 years who had hypertension, were overweight or obese, smoked, or exercised 150 minutes or less a week. The participants, 71% of whom were female, were then randomized to receive no further support or to attend monthly, 60- to 90-minute sessions that included role playing, brainstorming, and activities focused on managing emotions, diet, and exercise. The 10 members of each group elected their own leaders, who then completed 3 hours of training in health promotion and leadership.
After 12 months, the intervention group scored an average of 8.84 (95% confidence interval, 8.37-9.32) on the FBS’ composite measure of blood pressure, exercise, weight, diet, and tobacco use, compared with 8.17 for controls (95% CI, 7.55-8.79; P = .016). The intervention group also improved 0.75 points more from baseline, compared with controls (95% CI, 0.32-1.18).
In addition, support group members scored 0.24 points higher on the 1-year measure of tobacco cessation (95% CI, 0.09-0.38; P = .003). The groups did not otherwise significantly differ in terms of individual risk factors, but the intervention group outscored the control group on measures of blood pressure, exercise, and diet.
“The results of the Fifty-Fifty study show that promoting healthier lifestyles focusing on self control of unhealthy behaviors through peer group support can be beneficial to heterogeneous groups, without a single condition or specific CV risk factors,” the researchers concluded. “Although this is a relatively short-term intervention study, follow-up results will provide insight into long-term sustainability of peer group support and long-term effect on cardiovascular health.”
The SHE Foundation and the Spanish Ministry of Health, Social Services and Equality jointly funded the research. The investigators did not report conflicts of interest.
From the AHA Scientific Sessions
Key clinical point: A peer support program was linked to significantly improved cardiovascular health, and to tobacco cessation.
Major finding: At 12 months, the mean composite cardiovascular health score was 8.84 for the intervention group, and 8.17 for controls (P = .016).
Data source: Multicenter, randomized, controlled trial of 543 adults with at least one risk factor for cardiovascular disease.
Disclosures: The SHE Foundation and the Spanish Ministry of Health, Social Services and Equality jointly funded the research. The investigators did not report conflicts of interest.