User login
Tocilizumab markedly increases rate of lower gastrointestinal perforation
SAN FRANCISCO – Patients with rheumatoid arthritis were five to nine times more likely to develop lower intestinal perforation on tocilizumab, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), tumor necrosis factor inhibitors, abatacept, or rituximab, according to a large observational registry study.
“The increased risk could not be explained by glucocorticoid use or the age of the patients, which was similar to other patients treated with biologics,” said Dr. Anja Strangfeld of the German Rheumatism Research Center in Berlin. The findings reinforce previous smaller analyses of clinical trial data, and also localize the risk of perforation exclusively to the lower gastrointestinal tract, she added. “Overall, the mortality with lower intestinal perforation was high, and even higher with tocilizumab,” she said. “Tocilizumab patients with lower intestinal perforation present atypically, and patients starting treatment should be advised that symptoms might be mild, but the event is severe.”
Lower intestinal perforation is fairly rare, with a population-level incidence of about .04 cases for every 1,000 person-years. The risk in patients with rheumatoid arthritis (RA) is higher – anywhere from 0.15 to 1.3 cases per 1,000 person-years, Dr. Strangfeld noted. And the reported risk for tocilizumab is higher still, approaching two cases per 1,000 person-years, according to an analysis of 18 cases reported from clinical trials.
To better evaluate that risk, Dr. Strangfeld and her colleagues analyzed observational data collected between 2001 and 2015 for 15,000 patients with RA who were included in the German biologics registry, RABBIT. Patients were followed for 5-10 years, with Disease Activity Score in 28 joints (DAS28), treatment, and adverse events tracked every 6 months. Patients had been on RA therapies for about 7-14 years; tocilizumab patients had received the monoclonal antibody for an average of 10.6 years.
Medical record reviews confirmed 36 cases of lower intestinal perforation, 11 each on tocilizumab and csDMARDs, 12 on tumor necrosis factor (TNF) inhibitors, and one each on abatacept and rituximab. Notably, the incidence rate for lower intestinal perforation on tocilizumab was three cases per 1,000 person-years, compared with 0.5-0.6 cases per 1,000 person-years for csDMARDs, abatacept, and TNF inhibitors; and 0.2 cases per 1,000 person-years for rituximab, Dr. Strangfeld said at the annual meeting of the American College of Rheumatology.
Furthermore, four of the 11 patients who developed a perforation on tocilizumab only had late-onset abdominal pain, whereas more than 90% of those on csDMARDs had early, acute abdominal pain, Dr. Strangfeld said. That might have explained why 66% of the tocilizumab patients died, compared with 18%-25% of patients who perforated while on csDMARDs or TNF inhibitors. The tocilizumab patients also tended to report diffuse rather than localized pain and nausea or lack of appetite, but were rarely febrile. Their C-reactive protein levels were not elevated, in contrast to levels of 200-380 mg/L for cases involving csDMARDs or TNF inhibitors.
Patients who had a perforation while on tocilizumab or TNF inhibitors were receiving about two-thirds more prednisolone a day, compared with the average dose of about 5-6 mg for the entire cohort, Dr. Strangfeld reported. The risk of lower intestinal perforation rose by 130% with every 5-mg increase in prednisolone per day, and by 150% with every 10-year increase in age, she said. There was no difference in risk by sex, DAS28 score, body mass index, or number of previous biologics. Lower intestinal perforations occurred most often among patients with diverticulitis, as has been previously reported (Clin Rheumatol. 2011;30:1471-4). But “none of the patients with lower intestinal perforation had a history of diverticulitis known to the treating rheumatologist,” Dr. Strangfeld emphasized. “Most often, diverticulitis was diagnosed simultaneously with lower intestinal perforation.”
Dr. Strangfeld reported receiving unconditional research grants from AbbVie, Celltrion, Hospira, Bristol-Myers Squibb, Merck, Pfizer, Roche, and UCB Pharma.
SAN FRANCISCO – Patients with rheumatoid arthritis were five to nine times more likely to develop lower intestinal perforation on tocilizumab, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), tumor necrosis factor inhibitors, abatacept, or rituximab, according to a large observational registry study.
“The increased risk could not be explained by glucocorticoid use or the age of the patients, which was similar to other patients treated with biologics,” said Dr. Anja Strangfeld of the German Rheumatism Research Center in Berlin. The findings reinforce previous smaller analyses of clinical trial data, and also localize the risk of perforation exclusively to the lower gastrointestinal tract, she added. “Overall, the mortality with lower intestinal perforation was high, and even higher with tocilizumab,” she said. “Tocilizumab patients with lower intestinal perforation present atypically, and patients starting treatment should be advised that symptoms might be mild, but the event is severe.”
Lower intestinal perforation is fairly rare, with a population-level incidence of about .04 cases for every 1,000 person-years. The risk in patients with rheumatoid arthritis (RA) is higher – anywhere from 0.15 to 1.3 cases per 1,000 person-years, Dr. Strangfeld noted. And the reported risk for tocilizumab is higher still, approaching two cases per 1,000 person-years, according to an analysis of 18 cases reported from clinical trials.
To better evaluate that risk, Dr. Strangfeld and her colleagues analyzed observational data collected between 2001 and 2015 for 15,000 patients with RA who were included in the German biologics registry, RABBIT. Patients were followed for 5-10 years, with Disease Activity Score in 28 joints (DAS28), treatment, and adverse events tracked every 6 months. Patients had been on RA therapies for about 7-14 years; tocilizumab patients had received the monoclonal antibody for an average of 10.6 years.
Medical record reviews confirmed 36 cases of lower intestinal perforation, 11 each on tocilizumab and csDMARDs, 12 on tumor necrosis factor (TNF) inhibitors, and one each on abatacept and rituximab. Notably, the incidence rate for lower intestinal perforation on tocilizumab was three cases per 1,000 person-years, compared with 0.5-0.6 cases per 1,000 person-years for csDMARDs, abatacept, and TNF inhibitors; and 0.2 cases per 1,000 person-years for rituximab, Dr. Strangfeld said at the annual meeting of the American College of Rheumatology.
Furthermore, four of the 11 patients who developed a perforation on tocilizumab only had late-onset abdominal pain, whereas more than 90% of those on csDMARDs had early, acute abdominal pain, Dr. Strangfeld said. That might have explained why 66% of the tocilizumab patients died, compared with 18%-25% of patients who perforated while on csDMARDs or TNF inhibitors. The tocilizumab patients also tended to report diffuse rather than localized pain and nausea or lack of appetite, but were rarely febrile. Their C-reactive protein levels were not elevated, in contrast to levels of 200-380 mg/L for cases involving csDMARDs or TNF inhibitors.
Patients who had a perforation while on tocilizumab or TNF inhibitors were receiving about two-thirds more prednisolone a day, compared with the average dose of about 5-6 mg for the entire cohort, Dr. Strangfeld reported. The risk of lower intestinal perforation rose by 130% with every 5-mg increase in prednisolone per day, and by 150% with every 10-year increase in age, she said. There was no difference in risk by sex, DAS28 score, body mass index, or number of previous biologics. Lower intestinal perforations occurred most often among patients with diverticulitis, as has been previously reported (Clin Rheumatol. 2011;30:1471-4). But “none of the patients with lower intestinal perforation had a history of diverticulitis known to the treating rheumatologist,” Dr. Strangfeld emphasized. “Most often, diverticulitis was diagnosed simultaneously with lower intestinal perforation.”
Dr. Strangfeld reported receiving unconditional research grants from AbbVie, Celltrion, Hospira, Bristol-Myers Squibb, Merck, Pfizer, Roche, and UCB Pharma.
SAN FRANCISCO – Patients with rheumatoid arthritis were five to nine times more likely to develop lower intestinal perforation on tocilizumab, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), tumor necrosis factor inhibitors, abatacept, or rituximab, according to a large observational registry study.
“The increased risk could not be explained by glucocorticoid use or the age of the patients, which was similar to other patients treated with biologics,” said Dr. Anja Strangfeld of the German Rheumatism Research Center in Berlin. The findings reinforce previous smaller analyses of clinical trial data, and also localize the risk of perforation exclusively to the lower gastrointestinal tract, she added. “Overall, the mortality with lower intestinal perforation was high, and even higher with tocilizumab,” she said. “Tocilizumab patients with lower intestinal perforation present atypically, and patients starting treatment should be advised that symptoms might be mild, but the event is severe.”
Lower intestinal perforation is fairly rare, with a population-level incidence of about .04 cases for every 1,000 person-years. The risk in patients with rheumatoid arthritis (RA) is higher – anywhere from 0.15 to 1.3 cases per 1,000 person-years, Dr. Strangfeld noted. And the reported risk for tocilizumab is higher still, approaching two cases per 1,000 person-years, according to an analysis of 18 cases reported from clinical trials.
To better evaluate that risk, Dr. Strangfeld and her colleagues analyzed observational data collected between 2001 and 2015 for 15,000 patients with RA who were included in the German biologics registry, RABBIT. Patients were followed for 5-10 years, with Disease Activity Score in 28 joints (DAS28), treatment, and adverse events tracked every 6 months. Patients had been on RA therapies for about 7-14 years; tocilizumab patients had received the monoclonal antibody for an average of 10.6 years.
Medical record reviews confirmed 36 cases of lower intestinal perforation, 11 each on tocilizumab and csDMARDs, 12 on tumor necrosis factor (TNF) inhibitors, and one each on abatacept and rituximab. Notably, the incidence rate for lower intestinal perforation on tocilizumab was three cases per 1,000 person-years, compared with 0.5-0.6 cases per 1,000 person-years for csDMARDs, abatacept, and TNF inhibitors; and 0.2 cases per 1,000 person-years for rituximab, Dr. Strangfeld said at the annual meeting of the American College of Rheumatology.
Furthermore, four of the 11 patients who developed a perforation on tocilizumab only had late-onset abdominal pain, whereas more than 90% of those on csDMARDs had early, acute abdominal pain, Dr. Strangfeld said. That might have explained why 66% of the tocilizumab patients died, compared with 18%-25% of patients who perforated while on csDMARDs or TNF inhibitors. The tocilizumab patients also tended to report diffuse rather than localized pain and nausea or lack of appetite, but were rarely febrile. Their C-reactive protein levels were not elevated, in contrast to levels of 200-380 mg/L for cases involving csDMARDs or TNF inhibitors.
Patients who had a perforation while on tocilizumab or TNF inhibitors were receiving about two-thirds more prednisolone a day, compared with the average dose of about 5-6 mg for the entire cohort, Dr. Strangfeld reported. The risk of lower intestinal perforation rose by 130% with every 5-mg increase in prednisolone per day, and by 150% with every 10-year increase in age, she said. There was no difference in risk by sex, DAS28 score, body mass index, or number of previous biologics. Lower intestinal perforations occurred most often among patients with diverticulitis, as has been previously reported (Clin Rheumatol. 2011;30:1471-4). But “none of the patients with lower intestinal perforation had a history of diverticulitis known to the treating rheumatologist,” Dr. Strangfeld emphasized. “Most often, diverticulitis was diagnosed simultaneously with lower intestinal perforation.”
Dr. Strangfeld reported receiving unconditional research grants from AbbVie, Celltrion, Hospira, Bristol-Myers Squibb, Merck, Pfizer, Roche, and UCB Pharma.
AT THE ACR ANNUAL MEETING
Key clinical point: Tocilizumab was associated with a markedly increased rate of lower gastrointestinal perforation among patients with rheumatoid arthritis.
Major finding: Patients with rheumatoid arthritis were five to nine times more likely to develop lower intestinal perforation on tocilizumab, compared with csDMARDs, TNF inhibitors, abatacept, or rituximab.
Data source: Analysis of 15,000 patients with rheumatoid arthritis from the German observational registry, RABBIT.
Disclosures: Dr. Strangfeld reported receiving unconditional research grants from AbbVie, Celltrion, Hospira, Bristol-Myers Squibb, Merck, Pfizer, Roche, and UCB Pharma.
ACR: Cryoglobulinemic vasculitis in Sjögren’s linked to lymphoma, mortality
San Francisco – Patients with primary Sjögren’s syndrome who met criteria for cryoglobulinemic vasculitis were significantly more likely to develop B-cell lymphoma and to die during follow-up, compared with patients who did not have cryoglobulins, in a large multicenter study.
The study’s findings reveal one subset of Sjögren’s patients who need more frequent and intensive follow-up, said Dr. Soledad Retamozo, who led the study while she was at the rheumatology unit at Hospital Privado Centro Médico de Córdoba in Córdoba, Argentina. She is now with the department of autoimmune diseases at CELLEX Biomedical Research Center, part of the University of Barcelona’s Institut d’Investigacions Biomèdiques August Pi i Sunyer.
Patients with primary Sjögren’s syndrome can have cryoglobulins and several other kinds of autoantibodies, including anti-SSA/Ro, anti-SSB/La, rheumatoid factor, and antinuclear antibodies (Clin Epidemiol. 2014;6:247-55). That diversity helps explain why patients have such varying clinical presentations and long-term outcomes, as researchers have noted. Cryoglobulinemic vasculitis is known to precede lymphoma in primary Sjögren’s syndrome, but few studies have examined the association or effects on mortality.
To explore those questions, Dr. Retamozo and her colleagues at rheumatology centers in Spain and Italy performed cryocrit testing in 515 consecutive patients with primary Sjögren’s syndrome. A total of 94% of patients were female, and they averaged 54 years of age at diagnosis. In all, 65 (12%) of the patients tested positive for cryoglobulins, resembling the prevalence in a prior report (Semin Arthritis Rheum. 1998 Dec;28[3]:200-5).
About one in every three patients with cryoglobulinemia also fulfilled the classification criteria for cryoglobulinemic vasculitis that were published in 2011 (Ann Rheum Dis. 2011;70:1183-90) and validated last year (Rheumatology [Oxford]. 2014;53[12]:2209-13). Patients who met the vasculitis criteria were “sicker” than other cryoglobulinemic patients by many measures, according to Dr. Retamozo. They had about twice the rate of type II cryoglobulinemia (86% vs. 43%), a fivefold higher average cryocrit level (6.6% vs. 1.25%), a more than twofold higher cumulative mean ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score (35.3 vs. 16.2), and significantly higher rates of hypocomplementemia, monoclonality, lymphadenopathy, peripheral neuropathy, and renal, skin, and joint disease.
Over an average follow-up period of 9.1 years, 9% of the entire cohort developed B-cell lymphoma, and 6% of the cohort died, Dr. Retamozo and her associates found. Cryoglobulinemic patients with primary Sjögren’s syndrome were more likely than test-negative patients to develop B-cell lymphoma (hazard ratio, 2.56; 95% confidence interval, 1.03-6.35), and the association was even stronger for patients with cryoglobulinemic vasculitis (HR, 7.47; 95% CI, 3.38-16.53). Patients with vasculitis also were significantly more likely to die during follow-up in a Kaplan-Meier survival analysis (HR, 4.36; 95% CI, 1.32-14.47), Dr. Retamozo reported.
The findings reflect a recent systemic review and meta-analysis by researchers from the Mayo Clinic (Rheumatology [Oxford]. 2015 Sep 27. doi: 10.1093/rheumatology/kev354) that separately linked vasculitis and cryoglobulinemia to mortality in primary Sjögren’s syndrome. “We measure cryocrit every 3-6 months in our Sjögren’s patients, and it helps us catch patients at greater risk of developing B-cell lymphoma,” Dr. Retamozo said. “For us it has been very helpful, in addition to tests for hypocomplementemia and monoclonality.”
The findings have been accepted for publication in the journal Rheumatology, she added.
Dr. Retamozo had no disclosures. One coauthor reported receiving research funding from Bristol-Myers Squibb.
San Francisco – Patients with primary Sjögren’s syndrome who met criteria for cryoglobulinemic vasculitis were significantly more likely to develop B-cell lymphoma and to die during follow-up, compared with patients who did not have cryoglobulins, in a large multicenter study.
The study’s findings reveal one subset of Sjögren’s patients who need more frequent and intensive follow-up, said Dr. Soledad Retamozo, who led the study while she was at the rheumatology unit at Hospital Privado Centro Médico de Córdoba in Córdoba, Argentina. She is now with the department of autoimmune diseases at CELLEX Biomedical Research Center, part of the University of Barcelona’s Institut d’Investigacions Biomèdiques August Pi i Sunyer.
Patients with primary Sjögren’s syndrome can have cryoglobulins and several other kinds of autoantibodies, including anti-SSA/Ro, anti-SSB/La, rheumatoid factor, and antinuclear antibodies (Clin Epidemiol. 2014;6:247-55). That diversity helps explain why patients have such varying clinical presentations and long-term outcomes, as researchers have noted. Cryoglobulinemic vasculitis is known to precede lymphoma in primary Sjögren’s syndrome, but few studies have examined the association or effects on mortality.
To explore those questions, Dr. Retamozo and her colleagues at rheumatology centers in Spain and Italy performed cryocrit testing in 515 consecutive patients with primary Sjögren’s syndrome. A total of 94% of patients were female, and they averaged 54 years of age at diagnosis. In all, 65 (12%) of the patients tested positive for cryoglobulins, resembling the prevalence in a prior report (Semin Arthritis Rheum. 1998 Dec;28[3]:200-5).
About one in every three patients with cryoglobulinemia also fulfilled the classification criteria for cryoglobulinemic vasculitis that were published in 2011 (Ann Rheum Dis. 2011;70:1183-90) and validated last year (Rheumatology [Oxford]. 2014;53[12]:2209-13). Patients who met the vasculitis criteria were “sicker” than other cryoglobulinemic patients by many measures, according to Dr. Retamozo. They had about twice the rate of type II cryoglobulinemia (86% vs. 43%), a fivefold higher average cryocrit level (6.6% vs. 1.25%), a more than twofold higher cumulative mean ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score (35.3 vs. 16.2), and significantly higher rates of hypocomplementemia, monoclonality, lymphadenopathy, peripheral neuropathy, and renal, skin, and joint disease.
Over an average follow-up period of 9.1 years, 9% of the entire cohort developed B-cell lymphoma, and 6% of the cohort died, Dr. Retamozo and her associates found. Cryoglobulinemic patients with primary Sjögren’s syndrome were more likely than test-negative patients to develop B-cell lymphoma (hazard ratio, 2.56; 95% confidence interval, 1.03-6.35), and the association was even stronger for patients with cryoglobulinemic vasculitis (HR, 7.47; 95% CI, 3.38-16.53). Patients with vasculitis also were significantly more likely to die during follow-up in a Kaplan-Meier survival analysis (HR, 4.36; 95% CI, 1.32-14.47), Dr. Retamozo reported.
The findings reflect a recent systemic review and meta-analysis by researchers from the Mayo Clinic (Rheumatology [Oxford]. 2015 Sep 27. doi: 10.1093/rheumatology/kev354) that separately linked vasculitis and cryoglobulinemia to mortality in primary Sjögren’s syndrome. “We measure cryocrit every 3-6 months in our Sjögren’s patients, and it helps us catch patients at greater risk of developing B-cell lymphoma,” Dr. Retamozo said. “For us it has been very helpful, in addition to tests for hypocomplementemia and monoclonality.”
The findings have been accepted for publication in the journal Rheumatology, she added.
Dr. Retamozo had no disclosures. One coauthor reported receiving research funding from Bristol-Myers Squibb.
San Francisco – Patients with primary Sjögren’s syndrome who met criteria for cryoglobulinemic vasculitis were significantly more likely to develop B-cell lymphoma and to die during follow-up, compared with patients who did not have cryoglobulins, in a large multicenter study.
The study’s findings reveal one subset of Sjögren’s patients who need more frequent and intensive follow-up, said Dr. Soledad Retamozo, who led the study while she was at the rheumatology unit at Hospital Privado Centro Médico de Córdoba in Córdoba, Argentina. She is now with the department of autoimmune diseases at CELLEX Biomedical Research Center, part of the University of Barcelona’s Institut d’Investigacions Biomèdiques August Pi i Sunyer.
Patients with primary Sjögren’s syndrome can have cryoglobulins and several other kinds of autoantibodies, including anti-SSA/Ro, anti-SSB/La, rheumatoid factor, and antinuclear antibodies (Clin Epidemiol. 2014;6:247-55). That diversity helps explain why patients have such varying clinical presentations and long-term outcomes, as researchers have noted. Cryoglobulinemic vasculitis is known to precede lymphoma in primary Sjögren’s syndrome, but few studies have examined the association or effects on mortality.
To explore those questions, Dr. Retamozo and her colleagues at rheumatology centers in Spain and Italy performed cryocrit testing in 515 consecutive patients with primary Sjögren’s syndrome. A total of 94% of patients were female, and they averaged 54 years of age at diagnosis. In all, 65 (12%) of the patients tested positive for cryoglobulins, resembling the prevalence in a prior report (Semin Arthritis Rheum. 1998 Dec;28[3]:200-5).
About one in every three patients with cryoglobulinemia also fulfilled the classification criteria for cryoglobulinemic vasculitis that were published in 2011 (Ann Rheum Dis. 2011;70:1183-90) and validated last year (Rheumatology [Oxford]. 2014;53[12]:2209-13). Patients who met the vasculitis criteria were “sicker” than other cryoglobulinemic patients by many measures, according to Dr. Retamozo. They had about twice the rate of type II cryoglobulinemia (86% vs. 43%), a fivefold higher average cryocrit level (6.6% vs. 1.25%), a more than twofold higher cumulative mean ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index) score (35.3 vs. 16.2), and significantly higher rates of hypocomplementemia, monoclonality, lymphadenopathy, peripheral neuropathy, and renal, skin, and joint disease.
Over an average follow-up period of 9.1 years, 9% of the entire cohort developed B-cell lymphoma, and 6% of the cohort died, Dr. Retamozo and her associates found. Cryoglobulinemic patients with primary Sjögren’s syndrome were more likely than test-negative patients to develop B-cell lymphoma (hazard ratio, 2.56; 95% confidence interval, 1.03-6.35), and the association was even stronger for patients with cryoglobulinemic vasculitis (HR, 7.47; 95% CI, 3.38-16.53). Patients with vasculitis also were significantly more likely to die during follow-up in a Kaplan-Meier survival analysis (HR, 4.36; 95% CI, 1.32-14.47), Dr. Retamozo reported.
The findings reflect a recent systemic review and meta-analysis by researchers from the Mayo Clinic (Rheumatology [Oxford]. 2015 Sep 27. doi: 10.1093/rheumatology/kev354) that separately linked vasculitis and cryoglobulinemia to mortality in primary Sjögren’s syndrome. “We measure cryocrit every 3-6 months in our Sjögren’s patients, and it helps us catch patients at greater risk of developing B-cell lymphoma,” Dr. Retamozo said. “For us it has been very helpful, in addition to tests for hypocomplementemia and monoclonality.”
The findings have been accepted for publication in the journal Rheumatology, she added.
Dr. Retamozo had no disclosures. One coauthor reported receiving research funding from Bristol-Myers Squibb.
AT THE ACR ANNUAL MEETING
Key clinical point: Cryoglobulinemic vasculitis increases the risk of B-cell lymphoma and death in patients with primary Sjögren’s syndrome.
Major finding: Both associations were statistically significant, using noncryoglobulinemic patients as the comparison group.
Data source: Multicenter study of 515 patients who were tested for serum cryoglobulins and fulfilled the 2011 classification criteria for primary Sjögren’s syndrome.
Disclosures: Dr. Retamozo had no disclosures. One coauthor reported receiving research funding from Bristol-Myers Squibb.
ACR: Study challenges protein citrullination as a central cause of RA
SAN FRANCISCO – Autoantibodies in patients with rheumatoid arthritis target both the native and citrullinated forms of the RA33 autoantigen, challenging the idea that protein citrullination underlies loss of tolerance in this disease, Dr. Maximilian Konig said at the annual meeting of the American College of Rheumatology.
“I think the important thing is that this makes us rethink how RA actually starts,” Dr. Konig said in an interview. “We identified three different antibody groups that clinically behave very differently. We identified a group of patients that has cross-reactive antibodies against RA33, and they seem to be the ones with the highest and the most rapid disease progression. Maybe identifying these patients early and targeting them more would help bring a subset of patients with the most advanced and aggressive disease under better control.”
Signs and symptoms are often inconclusive early in the course of RA, leading to the search for reliable biomarkers that can hasten diagnosis and treatment. Anti-citrullinated protein antibodies (ACPAs) are one hallmark of RA, and protein citrullination has been seen as central to autoimmunity in its pathogenesis, said Dr. Konig, a postdoctoral fellow in rheumatology at Johns Hopkins University, Baltimore. But patients also have autoantibodies against native or unmodified proteins, including calpastatin, Fc-gamma, peptidylarginine deiminase type 4, and heterogeneous nuclear ribonucleoprotein A2/B1 (also known as RA33), which has been correlated with clinical disease activity, radiographic evidence of bone resorption, C-reactive protein levels, and erythrocyte sedimentation rate in a few previous studies (Pediatr Int. 2009 Apr;51[2]:188-92 and J Immunol Res. 2014;2014:516593).
Dr. Konig and his coinvestigators contended that current models of RA do not adequately account for autoimmunity against native proteins. To explore that idea, they tested sera from 196 patients from the ESCAPE RA (Evaluation of Subclinical Cardiovascular Disease and Predictors of Events in Rheumatoid Arthritis) cohort study and from 56 healthy controls. They used quantitative ELISA to identify autoantibodies, and performed immunoblotting and immunoprecipitation to test antibody specificity. They also used immunoblotting and mass spectrometry to study synovial fluid from the patients.
The assays identified citrullinated RA33 in the joints of RA patients, and revealed distinct autoantibodies that targeted native and citrullinated RA33. Furthermore, this single antibody system seemed to change with disease duration, Dr. Konig said. Autoantibody against native RA33 was almost exclusively found in samples from patients in early-stage disease, whereas patients with long-established RA had much higher levels of anti-citrullinated RA33 antibodies. The switch from a predominance of anti-RA33 to anti-citrullinated RA33 autoantibodies seemed to happen about a decade into the disease course, Dr. Konig added. “These data suggest that citrullination may not be required to break tolerance to RA33, and support a model in which RA autoantigens are initially targeted as a native protein, and only later become targets of a citrulline-specific response,” he said.
Notably, immunoprecipitation, immunoblotting, and competitive assays all confirmed a third type of autoantibody that cross-reacted against both RA33 and citrullinated RA33. The “RA33 [protein] is targeted by patient sera in three ways: only as a native protein, both as a native and as a citrullinated protein, and only as a citrullinated protein,” Dr. Konig concluded. He and his associates are exploring the clinical implications of the finding, particularly because patients with the cross-reactive anti-RA33 autoantibodies seem to have the most rapidly progressive and severe disease, he added. The presence of these antibodies might one day help identify a patient who needs especially aggressive monitoring and treatment, he concluded.
Dr. Konig had no disclosures.*
*This story was updated 12/3/2015.
SAN FRANCISCO – Autoantibodies in patients with rheumatoid arthritis target both the native and citrullinated forms of the RA33 autoantigen, challenging the idea that protein citrullination underlies loss of tolerance in this disease, Dr. Maximilian Konig said at the annual meeting of the American College of Rheumatology.
“I think the important thing is that this makes us rethink how RA actually starts,” Dr. Konig said in an interview. “We identified three different antibody groups that clinically behave very differently. We identified a group of patients that has cross-reactive antibodies against RA33, and they seem to be the ones with the highest and the most rapid disease progression. Maybe identifying these patients early and targeting them more would help bring a subset of patients with the most advanced and aggressive disease under better control.”
Signs and symptoms are often inconclusive early in the course of RA, leading to the search for reliable biomarkers that can hasten diagnosis and treatment. Anti-citrullinated protein antibodies (ACPAs) are one hallmark of RA, and protein citrullination has been seen as central to autoimmunity in its pathogenesis, said Dr. Konig, a postdoctoral fellow in rheumatology at Johns Hopkins University, Baltimore. But patients also have autoantibodies against native or unmodified proteins, including calpastatin, Fc-gamma, peptidylarginine deiminase type 4, and heterogeneous nuclear ribonucleoprotein A2/B1 (also known as RA33), which has been correlated with clinical disease activity, radiographic evidence of bone resorption, C-reactive protein levels, and erythrocyte sedimentation rate in a few previous studies (Pediatr Int. 2009 Apr;51[2]:188-92 and J Immunol Res. 2014;2014:516593).
Dr. Konig and his coinvestigators contended that current models of RA do not adequately account for autoimmunity against native proteins. To explore that idea, they tested sera from 196 patients from the ESCAPE RA (Evaluation of Subclinical Cardiovascular Disease and Predictors of Events in Rheumatoid Arthritis) cohort study and from 56 healthy controls. They used quantitative ELISA to identify autoantibodies, and performed immunoblotting and immunoprecipitation to test antibody specificity. They also used immunoblotting and mass spectrometry to study synovial fluid from the patients.
The assays identified citrullinated RA33 in the joints of RA patients, and revealed distinct autoantibodies that targeted native and citrullinated RA33. Furthermore, this single antibody system seemed to change with disease duration, Dr. Konig said. Autoantibody against native RA33 was almost exclusively found in samples from patients in early-stage disease, whereas patients with long-established RA had much higher levels of anti-citrullinated RA33 antibodies. The switch from a predominance of anti-RA33 to anti-citrullinated RA33 autoantibodies seemed to happen about a decade into the disease course, Dr. Konig added. “These data suggest that citrullination may not be required to break tolerance to RA33, and support a model in which RA autoantigens are initially targeted as a native protein, and only later become targets of a citrulline-specific response,” he said.
Notably, immunoprecipitation, immunoblotting, and competitive assays all confirmed a third type of autoantibody that cross-reacted against both RA33 and citrullinated RA33. The “RA33 [protein] is targeted by patient sera in three ways: only as a native protein, both as a native and as a citrullinated protein, and only as a citrullinated protein,” Dr. Konig concluded. He and his associates are exploring the clinical implications of the finding, particularly because patients with the cross-reactive anti-RA33 autoantibodies seem to have the most rapidly progressive and severe disease, he added. The presence of these antibodies might one day help identify a patient who needs especially aggressive monitoring and treatment, he concluded.
Dr. Konig had no disclosures.*
*This story was updated 12/3/2015.
SAN FRANCISCO – Autoantibodies in patients with rheumatoid arthritis target both the native and citrullinated forms of the RA33 autoantigen, challenging the idea that protein citrullination underlies loss of tolerance in this disease, Dr. Maximilian Konig said at the annual meeting of the American College of Rheumatology.
“I think the important thing is that this makes us rethink how RA actually starts,” Dr. Konig said in an interview. “We identified three different antibody groups that clinically behave very differently. We identified a group of patients that has cross-reactive antibodies against RA33, and they seem to be the ones with the highest and the most rapid disease progression. Maybe identifying these patients early and targeting them more would help bring a subset of patients with the most advanced and aggressive disease under better control.”
Signs and symptoms are often inconclusive early in the course of RA, leading to the search for reliable biomarkers that can hasten diagnosis and treatment. Anti-citrullinated protein antibodies (ACPAs) are one hallmark of RA, and protein citrullination has been seen as central to autoimmunity in its pathogenesis, said Dr. Konig, a postdoctoral fellow in rheumatology at Johns Hopkins University, Baltimore. But patients also have autoantibodies against native or unmodified proteins, including calpastatin, Fc-gamma, peptidylarginine deiminase type 4, and heterogeneous nuclear ribonucleoprotein A2/B1 (also known as RA33), which has been correlated with clinical disease activity, radiographic evidence of bone resorption, C-reactive protein levels, and erythrocyte sedimentation rate in a few previous studies (Pediatr Int. 2009 Apr;51[2]:188-92 and J Immunol Res. 2014;2014:516593).
Dr. Konig and his coinvestigators contended that current models of RA do not adequately account for autoimmunity against native proteins. To explore that idea, they tested sera from 196 patients from the ESCAPE RA (Evaluation of Subclinical Cardiovascular Disease and Predictors of Events in Rheumatoid Arthritis) cohort study and from 56 healthy controls. They used quantitative ELISA to identify autoantibodies, and performed immunoblotting and immunoprecipitation to test antibody specificity. They also used immunoblotting and mass spectrometry to study synovial fluid from the patients.
The assays identified citrullinated RA33 in the joints of RA patients, and revealed distinct autoantibodies that targeted native and citrullinated RA33. Furthermore, this single antibody system seemed to change with disease duration, Dr. Konig said. Autoantibody against native RA33 was almost exclusively found in samples from patients in early-stage disease, whereas patients with long-established RA had much higher levels of anti-citrullinated RA33 antibodies. The switch from a predominance of anti-RA33 to anti-citrullinated RA33 autoantibodies seemed to happen about a decade into the disease course, Dr. Konig added. “These data suggest that citrullination may not be required to break tolerance to RA33, and support a model in which RA autoantigens are initially targeted as a native protein, and only later become targets of a citrulline-specific response,” he said.
Notably, immunoprecipitation, immunoblotting, and competitive assays all confirmed a third type of autoantibody that cross-reacted against both RA33 and citrullinated RA33. The “RA33 [protein] is targeted by patient sera in three ways: only as a native protein, both as a native and as a citrullinated protein, and only as a citrullinated protein,” Dr. Konig concluded. He and his associates are exploring the clinical implications of the finding, particularly because patients with the cross-reactive anti-RA33 autoantibodies seem to have the most rapidly progressive and severe disease, he added. The presence of these antibodies might one day help identify a patient who needs especially aggressive monitoring and treatment, he concluded.
Dr. Konig had no disclosures.*
*This story was updated 12/3/2015.
AT THE ACR ANNUAL MEETING
Key clinical point: Patterns of antibody activity against the RA33 autoantigen challenge the idea that citrullination is central to the pathology of rheumatoid arthritis.
Major finding: Laboratory analyses revealed three distinct groups of autoantibodies targeting native RA33, citrullinated RA33, or both forms of the autoantigen.
Data source: Assays of serum and synovial fluid samples from 56 controls and 196 participants from the ESCAPE RA (Evaluation of Subclinical Cardiovascular Disease and Predictors of Events in Rheumatoid Arthritis) cohort study.
Disclosures: Dr. Konig had no disclosures.*
ACR: Cardiovascular risk factors in psoriatic diseases are common, often go untreated
SAN FRANCISCO – Despite their frequent contact with the health care system, patients with psoriasis and psoriatic arthritis often receive no treatment for major cardiovascular risk factors, according to two large multicenter studies.
“We identified a gap in quality of care in terms of the primary prevention of cardiovascular risk factors in psoriatic arthritis and psoriasis. The next step will be to develop strategies to increase awareness and implement treatment recommendations among primary care physicians, dermatologists, and rheumatologists,” Dr. Lihi Eder of the University of Toronto said in an interview at the annual meeting of the American College of Rheumatology.
Psoriatic and cardiovascular diseases share an inflammatory etiology and often co-occur. In past studies, patients with psoriasis and psoriatic arthritis were about 50% more likely than average to have dyslipidemia and ischemic heart disease, and about 80%-90% more likely than usual to have hypertension and diabetes, Dr. Eder said.
She and her associates studied dyslipidemia and hypertension among 1,327 patients with psoriatic arthritis and 927 patients with psoriasis at eight sites in Canada, the United States, and Israel as part of the International Psoriasis & Arthritis Research Team (IPART). Based on medical and laboratory reports and self-reported data, the investigators assessed these comorbidities and whether treatment adhered to cholesterol and hypertension guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2014 Jul 1;129:S1-45), and the Eighth Joint National Committee (JAMA. 2014 Feb 5;311[5]:507-20), respectively.
More than 80% of patients in the cohort had at least one modifiable cardiovascular risk factor, Dr. Eder said. While 6% had ischemic heart disease, 45% had hypertension, 71% had dyslipidemia, 13% had diabetes, 54% had central obesity, and 17% were current smokers. Furthermore, close to half of patients who had been diagnosed with hypertension had uncontrolled high blood pressure, and 57% were not receiving antihypertensive medications. Likewise, 58% of patients with dyslipidemia met criteria for statins, but only a third of these patients were receiving them.
Undertreatment was associated with having psoriatic arthritis or severe psoriasis and with having a high school or lower level of education, Dr. Eder added. “You have to remember that this study was conducted among specialists – these are supposed to be experts in the field,” she said. “If the treatment adherence is relatively low in these centers, then I would expect that for patients who are being followed in centers that do not specialize in psoriatic disease, adherence would be even lower.”
The second study detected significantly higher rates of cardiovascular risk factors among patients with psoriatic diseases, compared with controls from the Health Improvement Network, a medical records database that covers more than 9 million individuals in the United Kingdom. Patients with psoriatic arthritis or severe psoriasis were significantly more likely than were controls to develop hypertension, hyperlipidemia, obesity, or diabetes, with odds ratios ranging from 1.22 to 1.78, reported Dr. Kashif A. Jafri, who led the study while he was an internal medicine resident at the University of Pennsylvania in Philadelphia.
But despite their disproportionate risk, patients were treated at about the same rate as controls, Dr. Jafri said. About 15% of individuals with hypertension received no treatment, 30%-40% with hyperlipidemia went untreated, and nearly 60% with diabetes received no documented therapy. “The absence of a significant difference in receipt of appropriate therapy among the groups reflects a need for more careful attention to the management of cardiovascular risk factors in patients with inflammatory diseases,” Dr. Jafri emphasized. Because these risk factors can be successfully treated, it is “critical” to educate primary care providers about the need to do so, he said.
Rheumatologists also should periodically discuss cardiovascular risk factors with their patients as part of routine care, Dr. Jafri advised. “Although there are obviously time constraints during each office visit, this is a topic that dramatically influences the morbidity and mortality of our patient population, and rheumatologists have the unique ability to address this issue in the context of their long-term relationships with their patients,” he said.
Dr. Jafri is now a fellow in rheumatology at the University of California, San Francisco. His was supported by an Ephraim P. Engleman Endowed Resident Research Preceptorship Award from the Rheumatology Research Foundation. IPART is sponsored by the Krembil Foundation and the Canadian Institutes of Health Research. Dr. Jafri and Dr. Eder had no disclosures.
SAN FRANCISCO – Despite their frequent contact with the health care system, patients with psoriasis and psoriatic arthritis often receive no treatment for major cardiovascular risk factors, according to two large multicenter studies.
“We identified a gap in quality of care in terms of the primary prevention of cardiovascular risk factors in psoriatic arthritis and psoriasis. The next step will be to develop strategies to increase awareness and implement treatment recommendations among primary care physicians, dermatologists, and rheumatologists,” Dr. Lihi Eder of the University of Toronto said in an interview at the annual meeting of the American College of Rheumatology.
Psoriatic and cardiovascular diseases share an inflammatory etiology and often co-occur. In past studies, patients with psoriasis and psoriatic arthritis were about 50% more likely than average to have dyslipidemia and ischemic heart disease, and about 80%-90% more likely than usual to have hypertension and diabetes, Dr. Eder said.
She and her associates studied dyslipidemia and hypertension among 1,327 patients with psoriatic arthritis and 927 patients with psoriasis at eight sites in Canada, the United States, and Israel as part of the International Psoriasis & Arthritis Research Team (IPART). Based on medical and laboratory reports and self-reported data, the investigators assessed these comorbidities and whether treatment adhered to cholesterol and hypertension guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2014 Jul 1;129:S1-45), and the Eighth Joint National Committee (JAMA. 2014 Feb 5;311[5]:507-20), respectively.
More than 80% of patients in the cohort had at least one modifiable cardiovascular risk factor, Dr. Eder said. While 6% had ischemic heart disease, 45% had hypertension, 71% had dyslipidemia, 13% had diabetes, 54% had central obesity, and 17% were current smokers. Furthermore, close to half of patients who had been diagnosed with hypertension had uncontrolled high blood pressure, and 57% were not receiving antihypertensive medications. Likewise, 58% of patients with dyslipidemia met criteria for statins, but only a third of these patients were receiving them.
Undertreatment was associated with having psoriatic arthritis or severe psoriasis and with having a high school or lower level of education, Dr. Eder added. “You have to remember that this study was conducted among specialists – these are supposed to be experts in the field,” she said. “If the treatment adherence is relatively low in these centers, then I would expect that for patients who are being followed in centers that do not specialize in psoriatic disease, adherence would be even lower.”
The second study detected significantly higher rates of cardiovascular risk factors among patients with psoriatic diseases, compared with controls from the Health Improvement Network, a medical records database that covers more than 9 million individuals in the United Kingdom. Patients with psoriatic arthritis or severe psoriasis were significantly more likely than were controls to develop hypertension, hyperlipidemia, obesity, or diabetes, with odds ratios ranging from 1.22 to 1.78, reported Dr. Kashif A. Jafri, who led the study while he was an internal medicine resident at the University of Pennsylvania in Philadelphia.
But despite their disproportionate risk, patients were treated at about the same rate as controls, Dr. Jafri said. About 15% of individuals with hypertension received no treatment, 30%-40% with hyperlipidemia went untreated, and nearly 60% with diabetes received no documented therapy. “The absence of a significant difference in receipt of appropriate therapy among the groups reflects a need for more careful attention to the management of cardiovascular risk factors in patients with inflammatory diseases,” Dr. Jafri emphasized. Because these risk factors can be successfully treated, it is “critical” to educate primary care providers about the need to do so, he said.
Rheumatologists also should periodically discuss cardiovascular risk factors with their patients as part of routine care, Dr. Jafri advised. “Although there are obviously time constraints during each office visit, this is a topic that dramatically influences the morbidity and mortality of our patient population, and rheumatologists have the unique ability to address this issue in the context of their long-term relationships with their patients,” he said.
Dr. Jafri is now a fellow in rheumatology at the University of California, San Francisco. His was supported by an Ephraim P. Engleman Endowed Resident Research Preceptorship Award from the Rheumatology Research Foundation. IPART is sponsored by the Krembil Foundation and the Canadian Institutes of Health Research. Dr. Jafri and Dr. Eder had no disclosures.
SAN FRANCISCO – Despite their frequent contact with the health care system, patients with psoriasis and psoriatic arthritis often receive no treatment for major cardiovascular risk factors, according to two large multicenter studies.
“We identified a gap in quality of care in terms of the primary prevention of cardiovascular risk factors in psoriatic arthritis and psoriasis. The next step will be to develop strategies to increase awareness and implement treatment recommendations among primary care physicians, dermatologists, and rheumatologists,” Dr. Lihi Eder of the University of Toronto said in an interview at the annual meeting of the American College of Rheumatology.
Psoriatic and cardiovascular diseases share an inflammatory etiology and often co-occur. In past studies, patients with psoriasis and psoriatic arthritis were about 50% more likely than average to have dyslipidemia and ischemic heart disease, and about 80%-90% more likely than usual to have hypertension and diabetes, Dr. Eder said.
She and her associates studied dyslipidemia and hypertension among 1,327 patients with psoriatic arthritis and 927 patients with psoriasis at eight sites in Canada, the United States, and Israel as part of the International Psoriasis & Arthritis Research Team (IPART). Based on medical and laboratory reports and self-reported data, the investigators assessed these comorbidities and whether treatment adhered to cholesterol and hypertension guidelines from the American College of Cardiology and the American Heart Association (Circulation. 2014 Jul 1;129:S1-45), and the Eighth Joint National Committee (JAMA. 2014 Feb 5;311[5]:507-20), respectively.
More than 80% of patients in the cohort had at least one modifiable cardiovascular risk factor, Dr. Eder said. While 6% had ischemic heart disease, 45% had hypertension, 71% had dyslipidemia, 13% had diabetes, 54% had central obesity, and 17% were current smokers. Furthermore, close to half of patients who had been diagnosed with hypertension had uncontrolled high blood pressure, and 57% were not receiving antihypertensive medications. Likewise, 58% of patients with dyslipidemia met criteria for statins, but only a third of these patients were receiving them.
Undertreatment was associated with having psoriatic arthritis or severe psoriasis and with having a high school or lower level of education, Dr. Eder added. “You have to remember that this study was conducted among specialists – these are supposed to be experts in the field,” she said. “If the treatment adherence is relatively low in these centers, then I would expect that for patients who are being followed in centers that do not specialize in psoriatic disease, adherence would be even lower.”
The second study detected significantly higher rates of cardiovascular risk factors among patients with psoriatic diseases, compared with controls from the Health Improvement Network, a medical records database that covers more than 9 million individuals in the United Kingdom. Patients with psoriatic arthritis or severe psoriasis were significantly more likely than were controls to develop hypertension, hyperlipidemia, obesity, or diabetes, with odds ratios ranging from 1.22 to 1.78, reported Dr. Kashif A. Jafri, who led the study while he was an internal medicine resident at the University of Pennsylvania in Philadelphia.
But despite their disproportionate risk, patients were treated at about the same rate as controls, Dr. Jafri said. About 15% of individuals with hypertension received no treatment, 30%-40% with hyperlipidemia went untreated, and nearly 60% with diabetes received no documented therapy. “The absence of a significant difference in receipt of appropriate therapy among the groups reflects a need for more careful attention to the management of cardiovascular risk factors in patients with inflammatory diseases,” Dr. Jafri emphasized. Because these risk factors can be successfully treated, it is “critical” to educate primary care providers about the need to do so, he said.
Rheumatologists also should periodically discuss cardiovascular risk factors with their patients as part of routine care, Dr. Jafri advised. “Although there are obviously time constraints during each office visit, this is a topic that dramatically influences the morbidity and mortality of our patient population, and rheumatologists have the unique ability to address this issue in the context of their long-term relationships with their patients,” he said.
Dr. Jafri is now a fellow in rheumatology at the University of California, San Francisco. His was supported by an Ephraim P. Engleman Endowed Resident Research Preceptorship Award from the Rheumatology Research Foundation. IPART is sponsored by the Krembil Foundation and the Canadian Institutes of Health Research. Dr. Jafri and Dr. Eder had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Patients with psoriatic diseases have high rates of modifiable cardiovascular risk factors that often go untreated, based on two large studies.
Major finding: These risk factors were untreated about one-third to one-half of the time.
Data source: The first study included 1,327 patients with psoriatic arthritis and 927 patients with psoriasis identified through the International Psoriasis & Arthritis Research Team (IPART). The second study analyzed data from The Health Improvement Network, including 211,832 patients with psoriatic disease and more than 1.3 million controls.
Disclosures: The IPART is sponsored by the Krembil Foundation and the Canadian Institutes of Health Research. The second study was supported by an Ephraim P. Engleman Endowed Resident Research Preceptorship Award from the Rheumatology Research Foundation. Dr. Eder and Dr. Jafri had no disclosures.
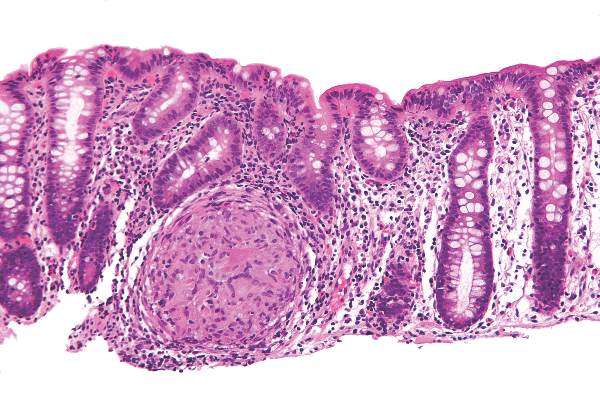
Crohn’s study found no reason to continue immunomodulators after starting anti-TNFs
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Continuing an immunomodulator was no more effective than switching to anti-TNF monotherapy in a meta-analysis of patients with Crohn’s disease.
Major finding: Combination therapy was no more effective than anti-TNF monotherapy in terms of clinical response, remission induction, or fistula closure.
Data source: Meta-analysis of 11 randomized, controlled trials of 1,601 patients with luminal or fistulizing CD.
Disclosures: The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and serving on advisory boards for Janssen, Abbott, and Takeda. Nine coauthors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
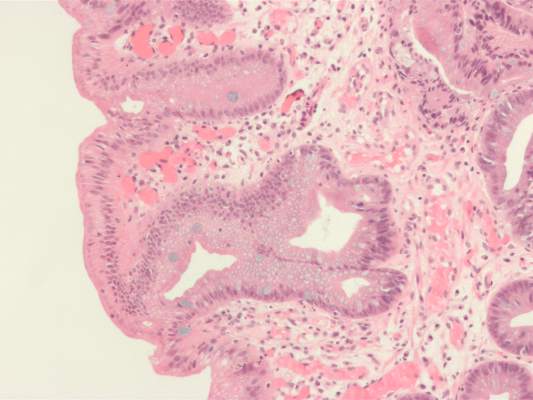
Portal venous blood yielded higher levels of circulating tumor cells
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Circulating pancreaticobiliary tumor cells were much more common in portal venous blood than in peripheral blood, and were molecularly similar to tumor tissue.
Major finding: Magnetic cell sorting revealed CTCs in the portal venous blood of all patients, but in the peripheral blood of only 22% of patients.
Data source: Prospective cohort study of 18 patients with pancreaticobiliary cancers, with portal venous blood collected under endoscopic guidance.
Disclosures: The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The investigators reported having no conflicts of interest.
High serum leptin, insulin levels linked to Barrett’s esophagus risk
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High serum levels of leptin and insulin were associated with Barrett’s esophagus in a meta-analysis.
Major finding: Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia.
Data source: Meta-analysis of nine observational studies that included 1,432 Barrett’s esophagus patients and 3,550 controls.
Disclosures: The National Cancer Institute funded the study. The investigators had no conflicts of interest.
ACR: Filgotinib cleared phase IIb trials for rheumatoid arthritis
SAN FRANCISCO – Filgotinib monotherapy yielded a 72% week 12 ACR 20 response for patients with rheumatoid arthritis and a 79% response when combined with methotrexate, according to two phase IIb dose-finding studies reported at the annual meeting of the American College of Rheumatology.
The Janus 1 kinase (JAK1) inhibitor caused dose-dependent increases in hemoglobin levels in both trials, and a few patients also had “substantial increases in creatinine, with some indication of a dose response,” said Dr. Arthur Kavanaugh, professor of clinical medicine and director of the Center for Innovative Therapy at the University of California, San Diego. But the overall safety profile for filgotinib was “attractive. We can see that this is an effective therapy,” he added.
Filgotinib, the first selective JAK1 inhibitor in development for rheumatoid arthritis, entered double-blind phase IIb trials in 2013. The DARWIN 1 trial compared filgotinib and a stable methotrexate dose with methotrexate and placebo in 594 patients with rheumatoid arthritis. The DARWIN 2 study compared filgotinib monotherapy with placebo in 283 patients who had not responded adequately to methotrexate. Patients in both trials were usually in their mid-fifties, had been diagnosed 7-10 years earlier, and had baseline 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) scores ranging from 6.0 to 6.2. The primary endpoint in both studies was the proportion of patients who achieved an ACR 20 response by week 12, said Dr. Rene R. Westhovens of KU Leuven (Belgium). He reported the results of DARWIN 1.
The combination regimen statistically outperformed methotrexate plus placebo at filgotinib doses of 100 mg once per day (week 12 ACR 20, 64% vs. 44%; P =.044), 200 mg once per day (69%; P less than .01), and 100 mg twice per day (79%; P less than .0001), Dr. Westhovens said. Filgotinib monotherapy also significantly outperformed placebo in terms of week 12 ACR 20, at all three doses tested – 50 mg once a day (67% vs. 29% for placebo), 100 mg once a day (66%), and 200 mg once a day (72%; all P less than .0001), according to Dr. Kavanaugh. “You might take away that perhaps the higher dose group got there faster. That should be the focus of future studies,” he said.
All three doses of filgotinib, given alone, also significantly outperformed placebo on several other endpoints, including ACR 50, ACR-N, DAS28-CRP, the Clinical Disease Activity Index, and the Simple Disease Activity Index, Dr. Kavanaugh added. By week 12, 24%-45% of patients who received filgotinib achieved low disease activity (DAS28-CRP of 3.2 or less), compared with 14% of the placebo group. Furthermore, after just 1 week of 100 mg or 200 mg of filgotinib per day, patients significantly improved on the ACR-N and the DAS28-CRP, compared with the placebo group.
Rates of serious adverse events were similar for the filgotinib and comparison groups in both trials, Dr. Kavanaugh and Dr. Westhovens reported. Notably, filgotinib was not associated with declines in natural killer cells or other forms of lymphopenia. Neutrophil counts declined slightly, compared with placebo, through 24 weeks, but did not seem to increase the risk of serious infections, although there was one case of cutaneous herpes zoster, Dr. Kavanaugh said. Likewise, rises in creatinine were usually mild and clinically insignificant, he added. “The reason for the rise in creatinine is unclear. It might be mechanistic, but whether we will see differences among the different [JAK] compounds remains to be elucidated,” he said.
Both DARWIN 1 and DARWIN 2 also reported dose-dependent rises in hemoglobin levels. Patients tended to have “small” increases in blood lipid levels, but the effects on HDL cholesterol were greater than for LDL cholesterol, Dr. Westhovens said.
For DARWIN 1, Dr. Westhovens reported financial support from Galapagos, the maker of filgotinib, and from Roche, Bristol-Myers Squibb, and Janssen. His senior author and three coauthors also reported financial relationships with Galapagos, and the other five coauthors had no disclosures. For DARWIN 2, Dr. Kavanaugh, his senior author, and three coauthors reported financial support from Galapagos, and five coauthors had no disclosures.
SAN FRANCISCO – Filgotinib monotherapy yielded a 72% week 12 ACR 20 response for patients with rheumatoid arthritis and a 79% response when combined with methotrexate, according to two phase IIb dose-finding studies reported at the annual meeting of the American College of Rheumatology.
The Janus 1 kinase (JAK1) inhibitor caused dose-dependent increases in hemoglobin levels in both trials, and a few patients also had “substantial increases in creatinine, with some indication of a dose response,” said Dr. Arthur Kavanaugh, professor of clinical medicine and director of the Center for Innovative Therapy at the University of California, San Diego. But the overall safety profile for filgotinib was “attractive. We can see that this is an effective therapy,” he added.
Filgotinib, the first selective JAK1 inhibitor in development for rheumatoid arthritis, entered double-blind phase IIb trials in 2013. The DARWIN 1 trial compared filgotinib and a stable methotrexate dose with methotrexate and placebo in 594 patients with rheumatoid arthritis. The DARWIN 2 study compared filgotinib monotherapy with placebo in 283 patients who had not responded adequately to methotrexate. Patients in both trials were usually in their mid-fifties, had been diagnosed 7-10 years earlier, and had baseline 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) scores ranging from 6.0 to 6.2. The primary endpoint in both studies was the proportion of patients who achieved an ACR 20 response by week 12, said Dr. Rene R. Westhovens of KU Leuven (Belgium). He reported the results of DARWIN 1.
The combination regimen statistically outperformed methotrexate plus placebo at filgotinib doses of 100 mg once per day (week 12 ACR 20, 64% vs. 44%; P =.044), 200 mg once per day (69%; P less than .01), and 100 mg twice per day (79%; P less than .0001), Dr. Westhovens said. Filgotinib monotherapy also significantly outperformed placebo in terms of week 12 ACR 20, at all three doses tested – 50 mg once a day (67% vs. 29% for placebo), 100 mg once a day (66%), and 200 mg once a day (72%; all P less than .0001), according to Dr. Kavanaugh. “You might take away that perhaps the higher dose group got there faster. That should be the focus of future studies,” he said.
All three doses of filgotinib, given alone, also significantly outperformed placebo on several other endpoints, including ACR 50, ACR-N, DAS28-CRP, the Clinical Disease Activity Index, and the Simple Disease Activity Index, Dr. Kavanaugh added. By week 12, 24%-45% of patients who received filgotinib achieved low disease activity (DAS28-CRP of 3.2 or less), compared with 14% of the placebo group. Furthermore, after just 1 week of 100 mg or 200 mg of filgotinib per day, patients significantly improved on the ACR-N and the DAS28-CRP, compared with the placebo group.
Rates of serious adverse events were similar for the filgotinib and comparison groups in both trials, Dr. Kavanaugh and Dr. Westhovens reported. Notably, filgotinib was not associated with declines in natural killer cells or other forms of lymphopenia. Neutrophil counts declined slightly, compared with placebo, through 24 weeks, but did not seem to increase the risk of serious infections, although there was one case of cutaneous herpes zoster, Dr. Kavanaugh said. Likewise, rises in creatinine were usually mild and clinically insignificant, he added. “The reason for the rise in creatinine is unclear. It might be mechanistic, but whether we will see differences among the different [JAK] compounds remains to be elucidated,” he said.
Both DARWIN 1 and DARWIN 2 also reported dose-dependent rises in hemoglobin levels. Patients tended to have “small” increases in blood lipid levels, but the effects on HDL cholesterol were greater than for LDL cholesterol, Dr. Westhovens said.
For DARWIN 1, Dr. Westhovens reported financial support from Galapagos, the maker of filgotinib, and from Roche, Bristol-Myers Squibb, and Janssen. His senior author and three coauthors also reported financial relationships with Galapagos, and the other five coauthors had no disclosures. For DARWIN 2, Dr. Kavanaugh, his senior author, and three coauthors reported financial support from Galapagos, and five coauthors had no disclosures.
SAN FRANCISCO – Filgotinib monotherapy yielded a 72% week 12 ACR 20 response for patients with rheumatoid arthritis and a 79% response when combined with methotrexate, according to two phase IIb dose-finding studies reported at the annual meeting of the American College of Rheumatology.
The Janus 1 kinase (JAK1) inhibitor caused dose-dependent increases in hemoglobin levels in both trials, and a few patients also had “substantial increases in creatinine, with some indication of a dose response,” said Dr. Arthur Kavanaugh, professor of clinical medicine and director of the Center for Innovative Therapy at the University of California, San Diego. But the overall safety profile for filgotinib was “attractive. We can see that this is an effective therapy,” he added.
Filgotinib, the first selective JAK1 inhibitor in development for rheumatoid arthritis, entered double-blind phase IIb trials in 2013. The DARWIN 1 trial compared filgotinib and a stable methotrexate dose with methotrexate and placebo in 594 patients with rheumatoid arthritis. The DARWIN 2 study compared filgotinib monotherapy with placebo in 283 patients who had not responded adequately to methotrexate. Patients in both trials were usually in their mid-fifties, had been diagnosed 7-10 years earlier, and had baseline 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) scores ranging from 6.0 to 6.2. The primary endpoint in both studies was the proportion of patients who achieved an ACR 20 response by week 12, said Dr. Rene R. Westhovens of KU Leuven (Belgium). He reported the results of DARWIN 1.
The combination regimen statistically outperformed methotrexate plus placebo at filgotinib doses of 100 mg once per day (week 12 ACR 20, 64% vs. 44%; P =.044), 200 mg once per day (69%; P less than .01), and 100 mg twice per day (79%; P less than .0001), Dr. Westhovens said. Filgotinib monotherapy also significantly outperformed placebo in terms of week 12 ACR 20, at all three doses tested – 50 mg once a day (67% vs. 29% for placebo), 100 mg once a day (66%), and 200 mg once a day (72%; all P less than .0001), according to Dr. Kavanaugh. “You might take away that perhaps the higher dose group got there faster. That should be the focus of future studies,” he said.
All three doses of filgotinib, given alone, also significantly outperformed placebo on several other endpoints, including ACR 50, ACR-N, DAS28-CRP, the Clinical Disease Activity Index, and the Simple Disease Activity Index, Dr. Kavanaugh added. By week 12, 24%-45% of patients who received filgotinib achieved low disease activity (DAS28-CRP of 3.2 or less), compared with 14% of the placebo group. Furthermore, after just 1 week of 100 mg or 200 mg of filgotinib per day, patients significantly improved on the ACR-N and the DAS28-CRP, compared with the placebo group.
Rates of serious adverse events were similar for the filgotinib and comparison groups in both trials, Dr. Kavanaugh and Dr. Westhovens reported. Notably, filgotinib was not associated with declines in natural killer cells or other forms of lymphopenia. Neutrophil counts declined slightly, compared with placebo, through 24 weeks, but did not seem to increase the risk of serious infections, although there was one case of cutaneous herpes zoster, Dr. Kavanaugh said. Likewise, rises in creatinine were usually mild and clinically insignificant, he added. “The reason for the rise in creatinine is unclear. It might be mechanistic, but whether we will see differences among the different [JAK] compounds remains to be elucidated,” he said.
Both DARWIN 1 and DARWIN 2 also reported dose-dependent rises in hemoglobin levels. Patients tended to have “small” increases in blood lipid levels, but the effects on HDL cholesterol were greater than for LDL cholesterol, Dr. Westhovens said.
For DARWIN 1, Dr. Westhovens reported financial support from Galapagos, the maker of filgotinib, and from Roche, Bristol-Myers Squibb, and Janssen. His senior author and three coauthors also reported financial relationships with Galapagos, and the other five coauthors had no disclosures. For DARWIN 2, Dr. Kavanaugh, his senior author, and three coauthors reported financial support from Galapagos, and five coauthors had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Filgotinib appeared effective and safe as monotherapy or in combination with methotrexate in two phase IIb trials of patients with rheumatoid arthritis.
Major finding: The highest week 12 ACR 20 response for filgotinib with methotrexate was 79% at 100 mg twice daily versus 44% for methotrexate with placebo (P less than .0001). For filgotinib monotherapy, week 12 ACR 20 responses were 67% at 50 mg once daily, 66% at 100 mg once daily, and 72% at 200 mg once daily, versus 29% for placebo (all P values less than .0001).
Data source: The DARWIN 1 trial compared filgotinib plus methotrexate and methotrexate plus placebo in 594 patients. DARWIN 2 compared filgotinib monotherapy with placebo in 283 patients who had responded inadequately to methotrexate.
Disclosures: For DARWIN 1, Dr. Westhovens reported financial support from Galapagos, the maker of filgotinib, and from Roche, Bristol-Myers Squibb, and Janssen. His senior author and three coauthors also reported financial relationships with Galapagos, and the other five coauthors had no disclosures. For DARWIN 2, Dr. Kavanaugh, his senior author, and three coauthors reported financial support from Galapagos, and five coauthors had no disclosures.
Schizophrenia risk, loss of white matter integrity share genes, twin study shows
Many genes that confer an increased risk for schizophrenia also underlie decreases in the integrity of white matter, according to a study of twins reported online Nov. 25 in JAMA Psychiatry.
“Global white matter integrity had a significant genetic association with schizophrenia liability, with 83.4% of the association explained by common genes,” said Marc M. Bohlken of the department of psychiatry at the University Medical Center Utrecht (The Netherlands), and his associates. “Therefore, the often reported reductions in white matter integrity [among patients with schizophrenia] can largely be explained as a genetic liability.”
The study also found that separate genetic pathways underlie white and gray matter abnormalities in patients with schizophrenia, the researchers said (JAMA Psychiatry. 2015 Nov 25. [doi: 10.1001/jamapsychiatry.2015.1925]).Patients with schizophrenia were known to have fewer of the white matter connections that efficiently transfer information among regions of the normal brain, but it was unclear whether this loss related to genetic predisposition for the disease. Therefore, the researchers used diffusion-weighted and T1-weighted imaging to study 70 individual twins whose cotwin was discordant for schizophrenia and 130 healthy individual matched control twins.
Decreased global white matter integrity, as measured by fractional anisotropy (FA), correlated phenotypically with increased risk for schizophrenia (phenotypic correlation = –0.25; 95% confidence interval, –0.38 to –0.10; P = .001), and common genes explained 83% of that link, the researchers said. “Furthermore, 8.1% of the total genetic variance in global FA was shared with genetic variance for schizophrenia liability,” they reported. Compared with controls, global FA was about 3% lower in patients with schizophrenia, and 2% lower in their monozygotic cotwins, but 0.4% higher in dizygotic cotwins, perhaps because they often were under the “liability threshold,” the investigators added. “Still, it is unlikely that this genetic correlation is entirely explained by nonadditive factors,” they added.
Half of all genetically affected brain regions involved the frontal cortex, while the rest were subcortical structures, such as the striatum and thalamus. “Decreases in white matter integrity connecting the frontal cortex with other brain regions have been suggested as a genetic marker for schizophrenia, which is consistent with our findings,” the researchers said. “Although the high connection density in frontal and subcortical regions may have influenced these findings, they are consistent with the hypothesis that impairments in frontostriatal connections are critical to the pathogenesis of schizophrenia.”
A Vidi grant from the Netherlands Organisation for Scientific Research helped fund the work. The researchers had no disclosures.
The investigators found that white matter integrity (as indexed by fractional anisotropy) and cortical gray matter thickness were “heritable traits that were significantly reduced in people with schizophrenia,” wrote Tyrone D. Cannon, Ph.D., in an accompanying editorial. “In both cases, genetic influences shared with schizophrenia were found to account for a high proportion of these phenotypic correlations.”
But the genetic factors influencing the correlation between schizophrenia and reduced fractional anisotropy (FA) proved “independent of the genetic factors that influenced the correlation between schizophrenia and reduced cortical gray matter thickness. Thus, their phenotypic correlation in schizophrenia may reflect an additional degree of effect over and above that associated with their respective inherited substrates, as in a secondary effect,” he wrote.
“In this case, it remains ambiguous whether reduced dendritic spine density is primary, driving some further degree of reduction in FA in tracts that link the affected pyramidal cells (i.e., beyond the reduced FA associated with schizophrenia-related susceptibility genes) or, conversely, whether disrupted white matter development leads to an additional degree of spine and synapse elimination (i.e., beyond the reductions in cortical thickness associated with schizophrenia susceptibility genes). To parse these alternatives, we need multimodal imaging data from the same high-risk individuals who are undergoing imaging on multiple occasions before the onset of illness.”
Dr. Cannon is with the departments of psychiatry and psychology at Yale University, New Haven, Conn. He reported consulting relationships with the Los Angeles County Department of Mental Health and Boehringer Ingelheim, and is listed as a coinventor on a pending patent for a biomarker for psychosis.
The investigators found that white matter integrity (as indexed by fractional anisotropy) and cortical gray matter thickness were “heritable traits that were significantly reduced in people with schizophrenia,” wrote Tyrone D. Cannon, Ph.D., in an accompanying editorial. “In both cases, genetic influences shared with schizophrenia were found to account for a high proportion of these phenotypic correlations.”
But the genetic factors influencing the correlation between schizophrenia and reduced fractional anisotropy (FA) proved “independent of the genetic factors that influenced the correlation between schizophrenia and reduced cortical gray matter thickness. Thus, their phenotypic correlation in schizophrenia may reflect an additional degree of effect over and above that associated with their respective inherited substrates, as in a secondary effect,” he wrote.
“In this case, it remains ambiguous whether reduced dendritic spine density is primary, driving some further degree of reduction in FA in tracts that link the affected pyramidal cells (i.e., beyond the reduced FA associated with schizophrenia-related susceptibility genes) or, conversely, whether disrupted white matter development leads to an additional degree of spine and synapse elimination (i.e., beyond the reductions in cortical thickness associated with schizophrenia susceptibility genes). To parse these alternatives, we need multimodal imaging data from the same high-risk individuals who are undergoing imaging on multiple occasions before the onset of illness.”
Dr. Cannon is with the departments of psychiatry and psychology at Yale University, New Haven, Conn. He reported consulting relationships with the Los Angeles County Department of Mental Health and Boehringer Ingelheim, and is listed as a coinventor on a pending patent for a biomarker for psychosis.
The investigators found that white matter integrity (as indexed by fractional anisotropy) and cortical gray matter thickness were “heritable traits that were significantly reduced in people with schizophrenia,” wrote Tyrone D. Cannon, Ph.D., in an accompanying editorial. “In both cases, genetic influences shared with schizophrenia were found to account for a high proportion of these phenotypic correlations.”
But the genetic factors influencing the correlation between schizophrenia and reduced fractional anisotropy (FA) proved “independent of the genetic factors that influenced the correlation between schizophrenia and reduced cortical gray matter thickness. Thus, their phenotypic correlation in schizophrenia may reflect an additional degree of effect over and above that associated with their respective inherited substrates, as in a secondary effect,” he wrote.
“In this case, it remains ambiguous whether reduced dendritic spine density is primary, driving some further degree of reduction in FA in tracts that link the affected pyramidal cells (i.e., beyond the reduced FA associated with schizophrenia-related susceptibility genes) or, conversely, whether disrupted white matter development leads to an additional degree of spine and synapse elimination (i.e., beyond the reductions in cortical thickness associated with schizophrenia susceptibility genes). To parse these alternatives, we need multimodal imaging data from the same high-risk individuals who are undergoing imaging on multiple occasions before the onset of illness.”
Dr. Cannon is with the departments of psychiatry and psychology at Yale University, New Haven, Conn. He reported consulting relationships with the Los Angeles County Department of Mental Health and Boehringer Ingelheim, and is listed as a coinventor on a pending patent for a biomarker for psychosis.
Many genes that confer an increased risk for schizophrenia also underlie decreases in the integrity of white matter, according to a study of twins reported online Nov. 25 in JAMA Psychiatry.
“Global white matter integrity had a significant genetic association with schizophrenia liability, with 83.4% of the association explained by common genes,” said Marc M. Bohlken of the department of psychiatry at the University Medical Center Utrecht (The Netherlands), and his associates. “Therefore, the often reported reductions in white matter integrity [among patients with schizophrenia] can largely be explained as a genetic liability.”
The study also found that separate genetic pathways underlie white and gray matter abnormalities in patients with schizophrenia, the researchers said (JAMA Psychiatry. 2015 Nov 25. [doi: 10.1001/jamapsychiatry.2015.1925]).Patients with schizophrenia were known to have fewer of the white matter connections that efficiently transfer information among regions of the normal brain, but it was unclear whether this loss related to genetic predisposition for the disease. Therefore, the researchers used diffusion-weighted and T1-weighted imaging to study 70 individual twins whose cotwin was discordant for schizophrenia and 130 healthy individual matched control twins.
Decreased global white matter integrity, as measured by fractional anisotropy (FA), correlated phenotypically with increased risk for schizophrenia (phenotypic correlation = –0.25; 95% confidence interval, –0.38 to –0.10; P = .001), and common genes explained 83% of that link, the researchers said. “Furthermore, 8.1% of the total genetic variance in global FA was shared with genetic variance for schizophrenia liability,” they reported. Compared with controls, global FA was about 3% lower in patients with schizophrenia, and 2% lower in their monozygotic cotwins, but 0.4% higher in dizygotic cotwins, perhaps because they often were under the “liability threshold,” the investigators added. “Still, it is unlikely that this genetic correlation is entirely explained by nonadditive factors,” they added.
Half of all genetically affected brain regions involved the frontal cortex, while the rest were subcortical structures, such as the striatum and thalamus. “Decreases in white matter integrity connecting the frontal cortex with other brain regions have been suggested as a genetic marker for schizophrenia, which is consistent with our findings,” the researchers said. “Although the high connection density in frontal and subcortical regions may have influenced these findings, they are consistent with the hypothesis that impairments in frontostriatal connections are critical to the pathogenesis of schizophrenia.”
A Vidi grant from the Netherlands Organisation for Scientific Research helped fund the work. The researchers had no disclosures.
Many genes that confer an increased risk for schizophrenia also underlie decreases in the integrity of white matter, according to a study of twins reported online Nov. 25 in JAMA Psychiatry.
“Global white matter integrity had a significant genetic association with schizophrenia liability, with 83.4% of the association explained by common genes,” said Marc M. Bohlken of the department of psychiatry at the University Medical Center Utrecht (The Netherlands), and his associates. “Therefore, the often reported reductions in white matter integrity [among patients with schizophrenia] can largely be explained as a genetic liability.”
The study also found that separate genetic pathways underlie white and gray matter abnormalities in patients with schizophrenia, the researchers said (JAMA Psychiatry. 2015 Nov 25. [doi: 10.1001/jamapsychiatry.2015.1925]).Patients with schizophrenia were known to have fewer of the white matter connections that efficiently transfer information among regions of the normal brain, but it was unclear whether this loss related to genetic predisposition for the disease. Therefore, the researchers used diffusion-weighted and T1-weighted imaging to study 70 individual twins whose cotwin was discordant for schizophrenia and 130 healthy individual matched control twins.
Decreased global white matter integrity, as measured by fractional anisotropy (FA), correlated phenotypically with increased risk for schizophrenia (phenotypic correlation = –0.25; 95% confidence interval, –0.38 to –0.10; P = .001), and common genes explained 83% of that link, the researchers said. “Furthermore, 8.1% of the total genetic variance in global FA was shared with genetic variance for schizophrenia liability,” they reported. Compared with controls, global FA was about 3% lower in patients with schizophrenia, and 2% lower in their monozygotic cotwins, but 0.4% higher in dizygotic cotwins, perhaps because they often were under the “liability threshold,” the investigators added. “Still, it is unlikely that this genetic correlation is entirely explained by nonadditive factors,” they added.
Half of all genetically affected brain regions involved the frontal cortex, while the rest were subcortical structures, such as the striatum and thalamus. “Decreases in white matter integrity connecting the frontal cortex with other brain regions have been suggested as a genetic marker for schizophrenia, which is consistent with our findings,” the researchers said. “Although the high connection density in frontal and subcortical regions may have influenced these findings, they are consistent with the hypothesis that impairments in frontostriatal connections are critical to the pathogenesis of schizophrenia.”
A Vidi grant from the Netherlands Organisation for Scientific Research helped fund the work. The researchers had no disclosures.
FROM JAMA PSYCHIATRY
Key clinical point: Common genes seem to underlie the genetic risk for schizophrenia and decreases in white matter integrity, especially in the frontal cortex.
Major finding: Fully 83% of lower global fractional anisotropy and increased risk for schizophrenia could be explained by common genes.
Data source: An analysis of T1-weighted and diffusion-weighted scans of 70 twins with discordance for schizophrenia and 130 control twins.
Disclosures: A Vidi grant from the Netherlands Organisation for Scientific Research helped fund the work. The researchers had no disclosures.
ACR: Years of TNF blockers did not increase risk of lymphoma in RA
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
AT THE ACR ANNUAL MEETING
Key clinical point: Exposure to biological disease-modifying antirheumatic drugs did not increase the overall risk of lymphoma among patients with rheumatoid arthritis.
Major finding: Patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), but there was no significant difference in risk compared with bDMARD-naive patients. However, patients on bDMARDs had about a fourfold greater risk of NK/T-cell lymphoma compared with bDMARD-naive patients.
Data source: A matched registry analysis of 13,240 patients from the Swedish Biologics (ARTIS), Patient, and Cancer Registers; 46,568 bio-naive patients; and 458,846 members of the general population.
Disclosures: The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.