User login
Measure found significant variations in outpatient colonoscopy quality
Facilities that performed outpatient colonoscopies varied significantly in terms of subsequent unplanned hospital visits, even after patient-level risk factors were adjusted for, according to a Medicare claims analysis reported in the January issue of Gastroenterology.
This first-in-kind quality measure will help “make transparent the full range of adverse events requiring hospital care that patients experience post-[colonoscopy], inform patient choice, create incentives for improved care, and assist providers’ quality improvement efforts, wrote Dr. Isuru Ranasinghe of Yale–New Haven (Conn.) Hospital and his associates. Preventing unplanned hospitals visits after colonoscopy could also help improve patient outcomes and cut health care costs, they added.
More than 90% of colonoscopies occur in outpatient settings, where it is difficult to follow-up and track serious adverse events such as colonic perforation or gastrointestinal bleeding. Furthermore, there are no publicly available quality reports of providers or facilities that perform outpatient colonoscopies. To help fill that gap, the researchers tracked unplanned hospital visits within 7 days after colonoscopy as part of an outpatient quality initiative by the Centers for Medicare & Medicaid Services. The analysis included 20% of Medicare outpatient colonoscopy claims in 2010, which amounted to 331,880 colonoscopies performed at 8,140 facilities (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.09.009]).
In 2010, there were 16.3 unplanned hospital visits for every 1,000 Medicare claims for outpatient colonoscopies, which equated to 27,000 such visits nationwide, the investigators said. Patients who were older than 85 years were significantly more likely to have an unplanned hospital visit than were patients aged 65-69 years (odds ratio, 1.87; 95% confidence interval, 1.54-2.28). The other most significant predictors included having an electrolyte or acid/base imbalance (OR, 1.43) or a psychiatric disorder (OR, 1.34). After adjusting for these factors, unplanned admission rates varied significantly among facilities in all four states with available data, including New York, California, Florida, and Nebraska, the researchers said.
These findings might not apply to patients who are too young to be enrolled in Medicare, which “is important, as most colonoscopies are performed among patients aged less than 65 years, although older patients are more likely to suffer adverse events,” Dr. Ranasinghe and his associates noted. The study also did not assess deaths, the one-third of GI bleeding events that occur more than a week after colonoscopy, or the various factors that might affect quality of care, such as type of anesthesia, polypectomy technique, and access to follow-up care. “The goal of the measure is to reveal the opportunity for improvement, and to prompt facilities to examine their practices in depth to identify ways to lower hospital visit rates to the level achieved by the best providers,” the researchers emphasized.
The work was supported by the Centers for Medicare & Medicaid Services, the National Health and Medical Research Council, the National Heart Foundation of Australia, the National Institute on Aging, the American Federation for Aging Research. Dr. Ranasinghe and nine coinvestigators reported working under contract with CMS to develop and maintain performance measures. Three coinvestigators reported financial relationships with AbbVie, qMed, Pentax, Olympus, Myriad Genetics, UnitedHealth, Medtronic, and Johnson & Johnson.
Source: American Gastroenterological Association
As part of the Centers for Medicare & Medicaid Services initiative to develop outpatient quality measures, Dr. Ranasinghe and his colleagues designed a risk-adjusted measure to capture serious adverse events characterized by unplanned hospitalization within 7 days after colonoscopy.
While no measure is perfect, this measure captures many important adverse outcomes after colonoscopy. Their methods carefully excluded hospitalizations that were elective or could be attributable to other conditions. This is an important quality measure because the endoscopist is often unaware of hospitalizations that occur post colonoscopy (Arch Intern Med. 2010;170:1752-7), and therefore cannot target quality improvement (QI) efforts at preventing such unplanned outcomes.

|
| Dr. Jeremy Adler |
This measure can be calculated from available data without chart audit and will fulfill CMS reporting requirements. However, it will be important to keep in mind that it was developed for patients 65 years and older, and may not be applicable to younger patients. Furthermore, to make this measure meaningful, it should be used to improve quality, not just assess quality.
The authors demonstrated that they were able to identify practices that were outliers, even when risk adjusted and adjusted for practice volume. This could allow practices to become self-aware and provide benchmarks against which to compare and improve their performance.
However, one major limitation to using this measure for QI is that the Healthcare Cost and Utilization Project only provides updated data yearly, after a substantial time lag, making it unsuitable for short-term or rapid-cycle QI efforts. In order for individual practices to target their improvement efforts, they would need to review their own local postcolonoscopy hospitalization data as an outcome measure more frequently. They could then review each case in depth to learn details that could further help target improvement efforts.
Dr. Jeremy Adler, M.Sc. is assistant professor, division of pediatric gastroenterology and Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor. He has no conflicts of interest.
As part of the Centers for Medicare & Medicaid Services initiative to develop outpatient quality measures, Dr. Ranasinghe and his colleagues designed a risk-adjusted measure to capture serious adverse events characterized by unplanned hospitalization within 7 days after colonoscopy.
While no measure is perfect, this measure captures many important adverse outcomes after colonoscopy. Their methods carefully excluded hospitalizations that were elective or could be attributable to other conditions. This is an important quality measure because the endoscopist is often unaware of hospitalizations that occur post colonoscopy (Arch Intern Med. 2010;170:1752-7), and therefore cannot target quality improvement (QI) efforts at preventing such unplanned outcomes.

|
| Dr. Jeremy Adler |
This measure can be calculated from available data without chart audit and will fulfill CMS reporting requirements. However, it will be important to keep in mind that it was developed for patients 65 years and older, and may not be applicable to younger patients. Furthermore, to make this measure meaningful, it should be used to improve quality, not just assess quality.
The authors demonstrated that they were able to identify practices that were outliers, even when risk adjusted and adjusted for practice volume. This could allow practices to become self-aware and provide benchmarks against which to compare and improve their performance.
However, one major limitation to using this measure for QI is that the Healthcare Cost and Utilization Project only provides updated data yearly, after a substantial time lag, making it unsuitable for short-term or rapid-cycle QI efforts. In order for individual practices to target their improvement efforts, they would need to review their own local postcolonoscopy hospitalization data as an outcome measure more frequently. They could then review each case in depth to learn details that could further help target improvement efforts.
Dr. Jeremy Adler, M.Sc. is assistant professor, division of pediatric gastroenterology and Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor. He has no conflicts of interest.
As part of the Centers for Medicare & Medicaid Services initiative to develop outpatient quality measures, Dr. Ranasinghe and his colleagues designed a risk-adjusted measure to capture serious adverse events characterized by unplanned hospitalization within 7 days after colonoscopy.
While no measure is perfect, this measure captures many important adverse outcomes after colonoscopy. Their methods carefully excluded hospitalizations that were elective or could be attributable to other conditions. This is an important quality measure because the endoscopist is often unaware of hospitalizations that occur post colonoscopy (Arch Intern Med. 2010;170:1752-7), and therefore cannot target quality improvement (QI) efforts at preventing such unplanned outcomes.

|
| Dr. Jeremy Adler |
This measure can be calculated from available data without chart audit and will fulfill CMS reporting requirements. However, it will be important to keep in mind that it was developed for patients 65 years and older, and may not be applicable to younger patients. Furthermore, to make this measure meaningful, it should be used to improve quality, not just assess quality.
The authors demonstrated that they were able to identify practices that were outliers, even when risk adjusted and adjusted for practice volume. This could allow practices to become self-aware and provide benchmarks against which to compare and improve their performance.
However, one major limitation to using this measure for QI is that the Healthcare Cost and Utilization Project only provides updated data yearly, after a substantial time lag, making it unsuitable for short-term or rapid-cycle QI efforts. In order for individual practices to target their improvement efforts, they would need to review their own local postcolonoscopy hospitalization data as an outcome measure more frequently. They could then review each case in depth to learn details that could further help target improvement efforts.
Dr. Jeremy Adler, M.Sc. is assistant professor, division of pediatric gastroenterology and Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor. He has no conflicts of interest.
Facilities that performed outpatient colonoscopies varied significantly in terms of subsequent unplanned hospital visits, even after patient-level risk factors were adjusted for, according to a Medicare claims analysis reported in the January issue of Gastroenterology.
This first-in-kind quality measure will help “make transparent the full range of adverse events requiring hospital care that patients experience post-[colonoscopy], inform patient choice, create incentives for improved care, and assist providers’ quality improvement efforts, wrote Dr. Isuru Ranasinghe of Yale–New Haven (Conn.) Hospital and his associates. Preventing unplanned hospitals visits after colonoscopy could also help improve patient outcomes and cut health care costs, they added.
More than 90% of colonoscopies occur in outpatient settings, where it is difficult to follow-up and track serious adverse events such as colonic perforation or gastrointestinal bleeding. Furthermore, there are no publicly available quality reports of providers or facilities that perform outpatient colonoscopies. To help fill that gap, the researchers tracked unplanned hospital visits within 7 days after colonoscopy as part of an outpatient quality initiative by the Centers for Medicare & Medicaid Services. The analysis included 20% of Medicare outpatient colonoscopy claims in 2010, which amounted to 331,880 colonoscopies performed at 8,140 facilities (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.09.009]).
In 2010, there were 16.3 unplanned hospital visits for every 1,000 Medicare claims for outpatient colonoscopies, which equated to 27,000 such visits nationwide, the investigators said. Patients who were older than 85 years were significantly more likely to have an unplanned hospital visit than were patients aged 65-69 years (odds ratio, 1.87; 95% confidence interval, 1.54-2.28). The other most significant predictors included having an electrolyte or acid/base imbalance (OR, 1.43) or a psychiatric disorder (OR, 1.34). After adjusting for these factors, unplanned admission rates varied significantly among facilities in all four states with available data, including New York, California, Florida, and Nebraska, the researchers said.
These findings might not apply to patients who are too young to be enrolled in Medicare, which “is important, as most colonoscopies are performed among patients aged less than 65 years, although older patients are more likely to suffer adverse events,” Dr. Ranasinghe and his associates noted. The study also did not assess deaths, the one-third of GI bleeding events that occur more than a week after colonoscopy, or the various factors that might affect quality of care, such as type of anesthesia, polypectomy technique, and access to follow-up care. “The goal of the measure is to reveal the opportunity for improvement, and to prompt facilities to examine their practices in depth to identify ways to lower hospital visit rates to the level achieved by the best providers,” the researchers emphasized.
The work was supported by the Centers for Medicare & Medicaid Services, the National Health and Medical Research Council, the National Heart Foundation of Australia, the National Institute on Aging, the American Federation for Aging Research. Dr. Ranasinghe and nine coinvestigators reported working under contract with CMS to develop and maintain performance measures. Three coinvestigators reported financial relationships with AbbVie, qMed, Pentax, Olympus, Myriad Genetics, UnitedHealth, Medtronic, and Johnson & Johnson.
Source: American Gastroenterological Association
Facilities that performed outpatient colonoscopies varied significantly in terms of subsequent unplanned hospital visits, even after patient-level risk factors were adjusted for, according to a Medicare claims analysis reported in the January issue of Gastroenterology.
This first-in-kind quality measure will help “make transparent the full range of adverse events requiring hospital care that patients experience post-[colonoscopy], inform patient choice, create incentives for improved care, and assist providers’ quality improvement efforts, wrote Dr. Isuru Ranasinghe of Yale–New Haven (Conn.) Hospital and his associates. Preventing unplanned hospitals visits after colonoscopy could also help improve patient outcomes and cut health care costs, they added.
More than 90% of colonoscopies occur in outpatient settings, where it is difficult to follow-up and track serious adverse events such as colonic perforation or gastrointestinal bleeding. Furthermore, there are no publicly available quality reports of providers or facilities that perform outpatient colonoscopies. To help fill that gap, the researchers tracked unplanned hospital visits within 7 days after colonoscopy as part of an outpatient quality initiative by the Centers for Medicare & Medicaid Services. The analysis included 20% of Medicare outpatient colonoscopy claims in 2010, which amounted to 331,880 colonoscopies performed at 8,140 facilities (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.09.009]).
In 2010, there were 16.3 unplanned hospital visits for every 1,000 Medicare claims for outpatient colonoscopies, which equated to 27,000 such visits nationwide, the investigators said. Patients who were older than 85 years were significantly more likely to have an unplanned hospital visit than were patients aged 65-69 years (odds ratio, 1.87; 95% confidence interval, 1.54-2.28). The other most significant predictors included having an electrolyte or acid/base imbalance (OR, 1.43) or a psychiatric disorder (OR, 1.34). After adjusting for these factors, unplanned admission rates varied significantly among facilities in all four states with available data, including New York, California, Florida, and Nebraska, the researchers said.
These findings might not apply to patients who are too young to be enrolled in Medicare, which “is important, as most colonoscopies are performed among patients aged less than 65 years, although older patients are more likely to suffer adverse events,” Dr. Ranasinghe and his associates noted. The study also did not assess deaths, the one-third of GI bleeding events that occur more than a week after colonoscopy, or the various factors that might affect quality of care, such as type of anesthesia, polypectomy technique, and access to follow-up care. “The goal of the measure is to reveal the opportunity for improvement, and to prompt facilities to examine their practices in depth to identify ways to lower hospital visit rates to the level achieved by the best providers,” the researchers emphasized.
The work was supported by the Centers for Medicare & Medicaid Services, the National Health and Medical Research Council, the National Heart Foundation of Australia, the National Institute on Aging, the American Federation for Aging Research. Dr. Ranasinghe and nine coinvestigators reported working under contract with CMS to develop and maintain performance measures. Three coinvestigators reported financial relationships with AbbVie, qMed, Pentax, Olympus, Myriad Genetics, UnitedHealth, Medtronic, and Johnson & Johnson.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Researchers validated a new measure to evaluate the quality of outpatient colonoscopies.
Major finding: Risk-adjusted rates of these visits varied significantly among health care facilities in all four states with available data.
Data source: An analysis of 20% of Medicare outpatient colonoscopy claims in 2010, which included 331,880 procedures performed at 8,140 facilities.
Disclosures: The work was supported by the Centers for Medicare & Medicaid Services, the National Health and Medical Research Council, the National Heart Foundation of Australia, the National Institute on Aging, and the American Federation for Aging Research. Dr. Ranasinghe and nine coinvestigators reported working under contract with CMS to develop and maintain performance measures. Three coinvestigators reported financial relationships with AbbVie, gMed, Pentax, Olympus, Myriad Genetics, UnitedHealth, Medtronic, and Johnson & Johnson.
Acute care surgeons should watch for bariatric surgery complications
Acute care surgeons are likely to encounter problems related to bariatric surgery because patients have a lifelong risk of complications, said authors of a single-center retrospective study.
“Internal hernias or obstructive etiologies are the most common presentations, and often require emergent or urgent surgery,” added Dr. Joel F. Bradley of Premier Surgical Associates, Knoxville, Tenn., and his associates at Carolinas Medical Center, a quaternary care hospital in Charlotte, N.C. “We recommend that when diagnosis is unclear for former bariatric surgery patients, diagnostic laparoscopy be performed to answer definitively if a surgical complication is present.”
Bariatric surgeries in the United States have leveled off at about 100,000 per year, but postsurgical complications are rising along with the total patient population. The researchers reviewed all 33 such cases at their acute care surgical service between 2007 and 2013 (Am. J. Surg. 2015;210:456-61).
Most patients were middle-age women with a history of laparoscopic Roux-en-y gastric bypass (RYGB) surgery. Other common index procedures included open RYGB and laparoscopic gastric banding, the researchers said. The most frequent complication was internal hernia, which affected a third of patients, and in two cases involved ischemic bowel. Other complications included adhesive small bowel obstruction, laparoscopic band restriction, and biliary disease. “Of note, all three patients with biliary disease also had internal hernias at Peterson’s defect that were closed at the time of cholecystectomy,” the investigators said. Less-common complications included upper gastrointestinal bleeding or ulcer, perforated ulcer, gastric outlet obstruction, intussusception, and ventral incisional hernia.
About 91% of patients with complications needed surgery, and 43% were open rather than minimally invasive. Laparoscopic and open surgery cases had similar baseline characteristics and outcomes, but open surgery patients averaged 11 days in the hospital, compared with 5 days for laparoscopic cases (P less than .05).
Cases were often emergent (43%) or urgent (20%), the investigators emphasized. All three patients with a previous vertical banded gastroplasty were obstructed at the gastroplasty site and were converted to RYGB. Surgeons managed the single case of intussusception with laparoscopic reduction and colopexy of the proximal and distal bowel to the abdominal wall. All three patients with symptomatic cholelithiasis underwent laparoscopic cholecystectomy. Two patients underwent upper endoscopies for bleeding or ulcer, and one underwent gastric band deflation for obstruction. No patients died.
Patients who have undergone RYGB are at particular risk of obstructive internal hernias, which can be mesenteric, mesojejunal, jejunojejunal, or at the Petersen’s space, the researchers noted. Some bariatric surgeons do not routinely close mesenteric defects, and, even when closed at the index surgery, as many as 83% of patients spontaneously open their jejunojejunostomy mesenteric defect after losing weight, they added (JSLS. 2010 Apr-Jun;14[2]:213-6).
Surgeons should also watch for obstructions secondary to adhesive disease and lap band restriction, they said. “Importantly, patients presenting with bowel obstruction from adhesive disease after RYGB are indiscernible from those with internal herniation, and surgeons must have a low threshold to evaluate these patients with diagnostic laparoscopy,” they added.
Band slippage, the most common complication of gastric banding, can cause dysphagia and gastric outlet obstruction, the investigators noted. Port site infection and band erosion are thought to be rare and can be managed laparoscopically if caught early, they said. “Many general and acute care surgeons may think that these complications are rare, and do not pertain to their practice; however, as bariatric procedures have regionalized, patients’ emergent complications are often seen by the local surgeon, not at the regional center,” they added.
The researchers reported no funding sources and no disclosures.
Acute care surgeons are likely to encounter problems related to bariatric surgery because patients have a lifelong risk of complications, said authors of a single-center retrospective study.
“Internal hernias or obstructive etiologies are the most common presentations, and often require emergent or urgent surgery,” added Dr. Joel F. Bradley of Premier Surgical Associates, Knoxville, Tenn., and his associates at Carolinas Medical Center, a quaternary care hospital in Charlotte, N.C. “We recommend that when diagnosis is unclear for former bariatric surgery patients, diagnostic laparoscopy be performed to answer definitively if a surgical complication is present.”
Bariatric surgeries in the United States have leveled off at about 100,000 per year, but postsurgical complications are rising along with the total patient population. The researchers reviewed all 33 such cases at their acute care surgical service between 2007 and 2013 (Am. J. Surg. 2015;210:456-61).
Most patients were middle-age women with a history of laparoscopic Roux-en-y gastric bypass (RYGB) surgery. Other common index procedures included open RYGB and laparoscopic gastric banding, the researchers said. The most frequent complication was internal hernia, which affected a third of patients, and in two cases involved ischemic bowel. Other complications included adhesive small bowel obstruction, laparoscopic band restriction, and biliary disease. “Of note, all three patients with biliary disease also had internal hernias at Peterson’s defect that were closed at the time of cholecystectomy,” the investigators said. Less-common complications included upper gastrointestinal bleeding or ulcer, perforated ulcer, gastric outlet obstruction, intussusception, and ventral incisional hernia.
About 91% of patients with complications needed surgery, and 43% were open rather than minimally invasive. Laparoscopic and open surgery cases had similar baseline characteristics and outcomes, but open surgery patients averaged 11 days in the hospital, compared with 5 days for laparoscopic cases (P less than .05).
Cases were often emergent (43%) or urgent (20%), the investigators emphasized. All three patients with a previous vertical banded gastroplasty were obstructed at the gastroplasty site and were converted to RYGB. Surgeons managed the single case of intussusception with laparoscopic reduction and colopexy of the proximal and distal bowel to the abdominal wall. All three patients with symptomatic cholelithiasis underwent laparoscopic cholecystectomy. Two patients underwent upper endoscopies for bleeding or ulcer, and one underwent gastric band deflation for obstruction. No patients died.
Patients who have undergone RYGB are at particular risk of obstructive internal hernias, which can be mesenteric, mesojejunal, jejunojejunal, or at the Petersen’s space, the researchers noted. Some bariatric surgeons do not routinely close mesenteric defects, and, even when closed at the index surgery, as many as 83% of patients spontaneously open their jejunojejunostomy mesenteric defect after losing weight, they added (JSLS. 2010 Apr-Jun;14[2]:213-6).
Surgeons should also watch for obstructions secondary to adhesive disease and lap band restriction, they said. “Importantly, patients presenting with bowel obstruction from adhesive disease after RYGB are indiscernible from those with internal herniation, and surgeons must have a low threshold to evaluate these patients with diagnostic laparoscopy,” they added.
Band slippage, the most common complication of gastric banding, can cause dysphagia and gastric outlet obstruction, the investigators noted. Port site infection and band erosion are thought to be rare and can be managed laparoscopically if caught early, they said. “Many general and acute care surgeons may think that these complications are rare, and do not pertain to their practice; however, as bariatric procedures have regionalized, patients’ emergent complications are often seen by the local surgeon, not at the regional center,” they added.
The researchers reported no funding sources and no disclosures.
Acute care surgeons are likely to encounter problems related to bariatric surgery because patients have a lifelong risk of complications, said authors of a single-center retrospective study.
“Internal hernias or obstructive etiologies are the most common presentations, and often require emergent or urgent surgery,” added Dr. Joel F. Bradley of Premier Surgical Associates, Knoxville, Tenn., and his associates at Carolinas Medical Center, a quaternary care hospital in Charlotte, N.C. “We recommend that when diagnosis is unclear for former bariatric surgery patients, diagnostic laparoscopy be performed to answer definitively if a surgical complication is present.”
Bariatric surgeries in the United States have leveled off at about 100,000 per year, but postsurgical complications are rising along with the total patient population. The researchers reviewed all 33 such cases at their acute care surgical service between 2007 and 2013 (Am. J. Surg. 2015;210:456-61).
Most patients were middle-age women with a history of laparoscopic Roux-en-y gastric bypass (RYGB) surgery. Other common index procedures included open RYGB and laparoscopic gastric banding, the researchers said. The most frequent complication was internal hernia, which affected a third of patients, and in two cases involved ischemic bowel. Other complications included adhesive small bowel obstruction, laparoscopic band restriction, and biliary disease. “Of note, all three patients with biliary disease also had internal hernias at Peterson’s defect that were closed at the time of cholecystectomy,” the investigators said. Less-common complications included upper gastrointestinal bleeding or ulcer, perforated ulcer, gastric outlet obstruction, intussusception, and ventral incisional hernia.
About 91% of patients with complications needed surgery, and 43% were open rather than minimally invasive. Laparoscopic and open surgery cases had similar baseline characteristics and outcomes, but open surgery patients averaged 11 days in the hospital, compared with 5 days for laparoscopic cases (P less than .05).
Cases were often emergent (43%) or urgent (20%), the investigators emphasized. All three patients with a previous vertical banded gastroplasty were obstructed at the gastroplasty site and were converted to RYGB. Surgeons managed the single case of intussusception with laparoscopic reduction and colopexy of the proximal and distal bowel to the abdominal wall. All three patients with symptomatic cholelithiasis underwent laparoscopic cholecystectomy. Two patients underwent upper endoscopies for bleeding or ulcer, and one underwent gastric band deflation for obstruction. No patients died.
Patients who have undergone RYGB are at particular risk of obstructive internal hernias, which can be mesenteric, mesojejunal, jejunojejunal, or at the Petersen’s space, the researchers noted. Some bariatric surgeons do not routinely close mesenteric defects, and, even when closed at the index surgery, as many as 83% of patients spontaneously open their jejunojejunostomy mesenteric defect after losing weight, they added (JSLS. 2010 Apr-Jun;14[2]:213-6).
Surgeons should also watch for obstructions secondary to adhesive disease and lap band restriction, they said. “Importantly, patients presenting with bowel obstruction from adhesive disease after RYGB are indiscernible from those with internal herniation, and surgeons must have a low threshold to evaluate these patients with diagnostic laparoscopy,” they added.
Band slippage, the most common complication of gastric banding, can cause dysphagia and gastric outlet obstruction, the investigators noted. Port site infection and band erosion are thought to be rare and can be managed laparoscopically if caught early, they said. “Many general and acute care surgeons may think that these complications are rare, and do not pertain to their practice; however, as bariatric procedures have regionalized, patients’ emergent complications are often seen by the local surgeon, not at the regional center,” they added.
The researchers reported no funding sources and no disclosures.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Postsurgical complications from bariatric surgery are on the rise, and acute care surgeons should be familiar with them.
Major finding: The most common complication in the case series was internal hernia, followed by adhesive small bowel obstruction.
Data source: A single-center retrospective review of 33 bariatric complications treated at an acute case surgery service between 2007 and 2013.
Disclosures: The researchers reported no funding sources and had no disclosures.
Ivabradine again missed a primary endpoint in SIGNIFY
Adding ivabradine to standard therapy for stable angina pectoris did not improve self-reported physical limitations, compared with placebo, at 12 months, but seemed to decrease the frequency of angina and help patients feel better about their disease, according to a subgroup analysis of SIGNIFY data.
“The robustness of our results is demonstrated by the low rate of missing data and the good internal consistency and validity of the scales used,” Dr. Michal Tendera of the Medical University of Silesia in Katowice, Poland, and his associates wrote in Circulation: Cardiovascular Quality and Outcomes. “The main limitation is the generalizability of the study findings, because the study enrolled patients in sinus rhythm with a heart rate of at least 70 beats per minute.”
SIGNIFY (Study Assessing the Morbidity-Mortality Benefits of the If Inhibitor Ivabradine in Patients with Coronary Artery Disease) had compared ivabradine or placebo plus standard therapy in more than 19,000 patients who had stable coronary artery disease without clinical heart failure. Ivabradine missed its primary endpoint, a composite of cardiovascular deaths and nonfatal myocardial infarctions (N Engl J Med. 2014;371:1091-9).
Dr. Tendera and his associates subsequently performed a subgroup analysis of 4,187 SIGNIFY patients who had responded to the Seattle Angina Questionnaire. Ivabradine again missed its prespecified primary outcome, the mean change in physical limitation score at 12 months (4.56 points vs. 3.40 points, respectively), the investigators reported (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.00209).
However, ivabradine was associated with significant 12-month improvements in other quality of life measures, most notably the frequency of angina (P less than .001), said the investigators. The difference persisted but was somewhat attenuated at 24 and 36 months (P = .01 and .045, respectively). Ivabradine also beat placebo in terms of mean changes in disease perception at 12 months (10.6 vs. 8.6 points for placebo; P = .006).
In general, patients who scored in the lowest tertile for quality of life at baseline improved the most on ivabradine, indicating that the antianginal drug “has a positive effect on a range of quality of life indices in patients with angina, despite the lack of the long-term effect on physical limitation,” the researchers concluded.
Servier makes ivabradine and funded the study. Dr. Tendera and all six coauthors reported receiving financial compensation, including personal fees, from Servier.
The results of this study suggest that routine self-reported health status measurement would clearly improve our ability to provide patients with optimal therapy, given their own preferences. It is time that patient-reported outcomes, particularly those measured in randomized controlled trials, receive the prominence and recognition they deserve. And while Tendera et al. conducted a subgroup analysis, the significance of these results is no less important. Better familiarity with health-related quality of life measurement tools in clinical practice will also add toward greater understanding and appreciation of health status outcomes as those presented by Tendera et al.
Colleen M. Norris, Ph.D., and Dr. Kevin R. Bainey are at the Mazankowski Alberta Heart Institute at the University of Alberta in Edmonton. They had no disclosures. These comments are taken from their accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.002412).
The results of this study suggest that routine self-reported health status measurement would clearly improve our ability to provide patients with optimal therapy, given their own preferences. It is time that patient-reported outcomes, particularly those measured in randomized controlled trials, receive the prominence and recognition they deserve. And while Tendera et al. conducted a subgroup analysis, the significance of these results is no less important. Better familiarity with health-related quality of life measurement tools in clinical practice will also add toward greater understanding and appreciation of health status outcomes as those presented by Tendera et al.
Colleen M. Norris, Ph.D., and Dr. Kevin R. Bainey are at the Mazankowski Alberta Heart Institute at the University of Alberta in Edmonton. They had no disclosures. These comments are taken from their accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.002412).
The results of this study suggest that routine self-reported health status measurement would clearly improve our ability to provide patients with optimal therapy, given their own preferences. It is time that patient-reported outcomes, particularly those measured in randomized controlled trials, receive the prominence and recognition they deserve. And while Tendera et al. conducted a subgroup analysis, the significance of these results is no less important. Better familiarity with health-related quality of life measurement tools in clinical practice will also add toward greater understanding and appreciation of health status outcomes as those presented by Tendera et al.
Colleen M. Norris, Ph.D., and Dr. Kevin R. Bainey are at the Mazankowski Alberta Heart Institute at the University of Alberta in Edmonton. They had no disclosures. These comments are taken from their accompanying editorial (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.002412).
Adding ivabradine to standard therapy for stable angina pectoris did not improve self-reported physical limitations, compared with placebo, at 12 months, but seemed to decrease the frequency of angina and help patients feel better about their disease, according to a subgroup analysis of SIGNIFY data.
“The robustness of our results is demonstrated by the low rate of missing data and the good internal consistency and validity of the scales used,” Dr. Michal Tendera of the Medical University of Silesia in Katowice, Poland, and his associates wrote in Circulation: Cardiovascular Quality and Outcomes. “The main limitation is the generalizability of the study findings, because the study enrolled patients in sinus rhythm with a heart rate of at least 70 beats per minute.”
SIGNIFY (Study Assessing the Morbidity-Mortality Benefits of the If Inhibitor Ivabradine in Patients with Coronary Artery Disease) had compared ivabradine or placebo plus standard therapy in more than 19,000 patients who had stable coronary artery disease without clinical heart failure. Ivabradine missed its primary endpoint, a composite of cardiovascular deaths and nonfatal myocardial infarctions (N Engl J Med. 2014;371:1091-9).
Dr. Tendera and his associates subsequently performed a subgroup analysis of 4,187 SIGNIFY patients who had responded to the Seattle Angina Questionnaire. Ivabradine again missed its prespecified primary outcome, the mean change in physical limitation score at 12 months (4.56 points vs. 3.40 points, respectively), the investigators reported (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.00209).
However, ivabradine was associated with significant 12-month improvements in other quality of life measures, most notably the frequency of angina (P less than .001), said the investigators. The difference persisted but was somewhat attenuated at 24 and 36 months (P = .01 and .045, respectively). Ivabradine also beat placebo in terms of mean changes in disease perception at 12 months (10.6 vs. 8.6 points for placebo; P = .006).
In general, patients who scored in the lowest tertile for quality of life at baseline improved the most on ivabradine, indicating that the antianginal drug “has a positive effect on a range of quality of life indices in patients with angina, despite the lack of the long-term effect on physical limitation,” the researchers concluded.
Servier makes ivabradine and funded the study. Dr. Tendera and all six coauthors reported receiving financial compensation, including personal fees, from Servier.
Adding ivabradine to standard therapy for stable angina pectoris did not improve self-reported physical limitations, compared with placebo, at 12 months, but seemed to decrease the frequency of angina and help patients feel better about their disease, according to a subgroup analysis of SIGNIFY data.
“The robustness of our results is demonstrated by the low rate of missing data and the good internal consistency and validity of the scales used,” Dr. Michal Tendera of the Medical University of Silesia in Katowice, Poland, and his associates wrote in Circulation: Cardiovascular Quality and Outcomes. “The main limitation is the generalizability of the study findings, because the study enrolled patients in sinus rhythm with a heart rate of at least 70 beats per minute.”
SIGNIFY (Study Assessing the Morbidity-Mortality Benefits of the If Inhibitor Ivabradine in Patients with Coronary Artery Disease) had compared ivabradine or placebo plus standard therapy in more than 19,000 patients who had stable coronary artery disease without clinical heart failure. Ivabradine missed its primary endpoint, a composite of cardiovascular deaths and nonfatal myocardial infarctions (N Engl J Med. 2014;371:1091-9).
Dr. Tendera and his associates subsequently performed a subgroup analysis of 4,187 SIGNIFY patients who had responded to the Seattle Angina Questionnaire. Ivabradine again missed its prespecified primary outcome, the mean change in physical limitation score at 12 months (4.56 points vs. 3.40 points, respectively), the investigators reported (Circ Cardiovasc Qual Outcomes. 2015 Dec 22. doi: 10.1161/circoutcomes.115.00209).
However, ivabradine was associated with significant 12-month improvements in other quality of life measures, most notably the frequency of angina (P less than .001), said the investigators. The difference persisted but was somewhat attenuated at 24 and 36 months (P = .01 and .045, respectively). Ivabradine also beat placebo in terms of mean changes in disease perception at 12 months (10.6 vs. 8.6 points for placebo; P = .006).
In general, patients who scored in the lowest tertile for quality of life at baseline improved the most on ivabradine, indicating that the antianginal drug “has a positive effect on a range of quality of life indices in patients with angina, despite the lack of the long-term effect on physical limitation,” the researchers concluded.
Servier makes ivabradine and funded the study. Dr. Tendera and all six coauthors reported receiving financial compensation, including personal fees, from Servier.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Ivabradine missed its primary endpoint in a prespecified subgroup analysis of data from the SIGNIFY trial. The antiangina agent did perform on several secondary quality of life measures.
Major finding: At 12 months, the change in physical limitation score was 4.56 points for ivabradine versus 3.40 points for placebo (P = .085).
Data source: A prespecified subgroup analysis of data for 4,187 patients with stable angina pectoris from the double-blind, randomized, placebo-controlled SIGNIFY trial.
Disclosures: Servier makes ivabradine and funded the study. Dr. Tendera and all six coauthors reported receiving financial compensation, including personal fees, from Servier.
Ovarian suppression during breast cancer chemotherapy helped preserve long-term function
Ovarian suppression with triptorelin during chemotherapy for early-stage breast cancer significantly increased the chances that women would recover their long-term ovarian function, according to a multicenter phase III open-label study published online Dec. 22 in JAMA.
The treatment and control groups had similarly low pregnancy rates at 5 years, with no significant overall difference in disease-free survival, reported Dr. Matteo Lambertini of Istituto Nazionale per la Ricerca sul Cancro, Genova, Italy, and his associates.
Cryopreserving embryos or oocytes remains the main way to protect fertility in young women with breast cancer. Clinicians have debated whether to use luteinizing hormone–releasing hormone analogues because of scarce data showing efficacy and concerns about compromising disease-free survival, the investigators noted. They randomized 281 premenopausal women with stage I-III hormone receptor–positive or hormone receptor–negative breast cancer to receive chemotherapy alone or with 3.75 mg triptorelin, given intramuscularly at least 1 week before and every 4 weeks during cancer treatment. The median age of patients was 39 years, the range was 24-45 years (JAMA 2015 Dec. 22;314:2632-40).
Nearly 73% of the triptorelin group and 64% of controls resumed menstruating within 5 years of completing chemotherapy, for an age-adjusted hazard ratio of 1.48 (95% CI, 1.12 to 1.95; P = .006). Cumulative 5-year pregnancy rates were 2.1% for the triptorelin group and 1.6% for controls (aHR, 2.4; 95% CI, 0.62 to 9.22; P = .2). About 81% of triptorelin patients and 84% of controls remained disease free at 5 years (HR, 1.17; 95% CI, 0.72 to 1.92; P = .52). The increase in risk among triptorelin patients was generally limited to those with hormone receptor–negative disease (5-year DFS, 62% and 76%), the investigators said.
When combined with recent findings from the POEMS study, the results show that temporary ovarian suppression before and during chemotherapy is an option for preserving ovarian function in premenopausal women with early-stage breast cancer, they concluded.
Istituto Nazionale per la Ricerca sul Cancro and the Associazione Italiana per la Ricerca sul Cancro funded the study. Dr. Lambertini reported no relevant disclosures. Two coauthors reported receiving research funding and honoraria from Amgen, GlaxoSmithKline, and Eisai. The senior author reported financial relationships with Takeda and with Ipsen, which supplied the triptorelin used in the study
The report by Lambertini et al. adds long-term follow-up information to the growing literature regarding the use of LHRHa through chemotherapy for the prevention of premature menopause, a desired outcome for some patients for prevention of associated menopausal symptoms and adverse health effects. Although the findings suggest modest benefits regarding the potential prevention of treatment-associated infertility, these studies collectively reflect the emerging importance of understanding and improving such critical quality of life issues, offering patients new treatment and supportive care options, and ultimately providing hope regarding an issue that is highly valued by many young patients diagnosed with cancer.
Dr. Ann H. Partridge is at the Dana-Farber Cancer Institute in Boston. She reported serving on an advisory board for Pfizer in 2014. These comments are taken from her editorial (JAMA 2015;314:2625-7[doi: 10.1001/jama.2015.17299]).
The report by Lambertini et al. adds long-term follow-up information to the growing literature regarding the use of LHRHa through chemotherapy for the prevention of premature menopause, a desired outcome for some patients for prevention of associated menopausal symptoms and adverse health effects. Although the findings suggest modest benefits regarding the potential prevention of treatment-associated infertility, these studies collectively reflect the emerging importance of understanding and improving such critical quality of life issues, offering patients new treatment and supportive care options, and ultimately providing hope regarding an issue that is highly valued by many young patients diagnosed with cancer.
Dr. Ann H. Partridge is at the Dana-Farber Cancer Institute in Boston. She reported serving on an advisory board for Pfizer in 2014. These comments are taken from her editorial (JAMA 2015;314:2625-7[doi: 10.1001/jama.2015.17299]).
The report by Lambertini et al. adds long-term follow-up information to the growing literature regarding the use of LHRHa through chemotherapy for the prevention of premature menopause, a desired outcome for some patients for prevention of associated menopausal symptoms and adverse health effects. Although the findings suggest modest benefits regarding the potential prevention of treatment-associated infertility, these studies collectively reflect the emerging importance of understanding and improving such critical quality of life issues, offering patients new treatment and supportive care options, and ultimately providing hope regarding an issue that is highly valued by many young patients diagnosed with cancer.
Dr. Ann H. Partridge is at the Dana-Farber Cancer Institute in Boston. She reported serving on an advisory board for Pfizer in 2014. These comments are taken from her editorial (JAMA 2015;314:2625-7[doi: 10.1001/jama.2015.17299]).
Ovarian suppression with triptorelin during chemotherapy for early-stage breast cancer significantly increased the chances that women would recover their long-term ovarian function, according to a multicenter phase III open-label study published online Dec. 22 in JAMA.
The treatment and control groups had similarly low pregnancy rates at 5 years, with no significant overall difference in disease-free survival, reported Dr. Matteo Lambertini of Istituto Nazionale per la Ricerca sul Cancro, Genova, Italy, and his associates.
Cryopreserving embryos or oocytes remains the main way to protect fertility in young women with breast cancer. Clinicians have debated whether to use luteinizing hormone–releasing hormone analogues because of scarce data showing efficacy and concerns about compromising disease-free survival, the investigators noted. They randomized 281 premenopausal women with stage I-III hormone receptor–positive or hormone receptor–negative breast cancer to receive chemotherapy alone or with 3.75 mg triptorelin, given intramuscularly at least 1 week before and every 4 weeks during cancer treatment. The median age of patients was 39 years, the range was 24-45 years (JAMA 2015 Dec. 22;314:2632-40).
Nearly 73% of the triptorelin group and 64% of controls resumed menstruating within 5 years of completing chemotherapy, for an age-adjusted hazard ratio of 1.48 (95% CI, 1.12 to 1.95; P = .006). Cumulative 5-year pregnancy rates were 2.1% for the triptorelin group and 1.6% for controls (aHR, 2.4; 95% CI, 0.62 to 9.22; P = .2). About 81% of triptorelin patients and 84% of controls remained disease free at 5 years (HR, 1.17; 95% CI, 0.72 to 1.92; P = .52). The increase in risk among triptorelin patients was generally limited to those with hormone receptor–negative disease (5-year DFS, 62% and 76%), the investigators said.
When combined with recent findings from the POEMS study, the results show that temporary ovarian suppression before and during chemotherapy is an option for preserving ovarian function in premenopausal women with early-stage breast cancer, they concluded.
Istituto Nazionale per la Ricerca sul Cancro and the Associazione Italiana per la Ricerca sul Cancro funded the study. Dr. Lambertini reported no relevant disclosures. Two coauthors reported receiving research funding and honoraria from Amgen, GlaxoSmithKline, and Eisai. The senior author reported financial relationships with Takeda and with Ipsen, which supplied the triptorelin used in the study
Ovarian suppression with triptorelin during chemotherapy for early-stage breast cancer significantly increased the chances that women would recover their long-term ovarian function, according to a multicenter phase III open-label study published online Dec. 22 in JAMA.
The treatment and control groups had similarly low pregnancy rates at 5 years, with no significant overall difference in disease-free survival, reported Dr. Matteo Lambertini of Istituto Nazionale per la Ricerca sul Cancro, Genova, Italy, and his associates.
Cryopreserving embryos or oocytes remains the main way to protect fertility in young women with breast cancer. Clinicians have debated whether to use luteinizing hormone–releasing hormone analogues because of scarce data showing efficacy and concerns about compromising disease-free survival, the investigators noted. They randomized 281 premenopausal women with stage I-III hormone receptor–positive or hormone receptor–negative breast cancer to receive chemotherapy alone or with 3.75 mg triptorelin, given intramuscularly at least 1 week before and every 4 weeks during cancer treatment. The median age of patients was 39 years, the range was 24-45 years (JAMA 2015 Dec. 22;314:2632-40).
Nearly 73% of the triptorelin group and 64% of controls resumed menstruating within 5 years of completing chemotherapy, for an age-adjusted hazard ratio of 1.48 (95% CI, 1.12 to 1.95; P = .006). Cumulative 5-year pregnancy rates were 2.1% for the triptorelin group and 1.6% for controls (aHR, 2.4; 95% CI, 0.62 to 9.22; P = .2). About 81% of triptorelin patients and 84% of controls remained disease free at 5 years (HR, 1.17; 95% CI, 0.72 to 1.92; P = .52). The increase in risk among triptorelin patients was generally limited to those with hormone receptor–negative disease (5-year DFS, 62% and 76%), the investigators said.
When combined with recent findings from the POEMS study, the results show that temporary ovarian suppression before and during chemotherapy is an option for preserving ovarian function in premenopausal women with early-stage breast cancer, they concluded.
Istituto Nazionale per la Ricerca sul Cancro and the Associazione Italiana per la Ricerca sul Cancro funded the study. Dr. Lambertini reported no relevant disclosures. Two coauthors reported receiving research funding and honoraria from Amgen, GlaxoSmithKline, and Eisai. The senior author reported financial relationships with Takeda and with Ipsen, which supplied the triptorelin used in the study
FROM JAMA
Key clinical point: Ovarian suppression with triptorelin, a luteinizing hormone-releasing hormone analogue, helped stop chemotherapy from inducing early menopause among women with breast cancer.
Major finding: The 5-year cumulative incidence estimate of menstrual resumption was about 73% in the LHRHa group and 64% in the control group (age-adjusted HR, 1.48; P = .006).
Data source: A randomized, multicenter, phase III parallel-group trial of 281 patients with stage I-III hormone receptor–positive or hormone receptor–negative breast cancer.
Disclosures: Istituto Nazionale per la Ricerca sul Cancro and the Associazione Italiana per la Ricerca sul Cancro funded the study. Dr. Lambertini reported no relevant disclosures. Two coauthors reported receiving research funding and honoraria from Amgen, GlaxoSmithKline, and Eisai. The senior author reported financial relationships with Takeda and with Ipsen, which supplied the triptorelin used in the study.
More IVF cycles increase chances of a live birth
Among women undergoing in vitro fertilization, adjusted rates of live birth rose modestly but continuously through up to nine IVF cycles, according to a study published online Dec. 22 in JAMA.
After the researchers accounted for women who stopped trying to conceive by IVF, the estimated cumulative live birth rate was 65% after six cycles, compared with 54% after three cycles and 29% after one cycle, reported Andrew D.A.C. Smith, Ph.D., of the University of Bristol, England, and his associates.
“These findings support the efficacy of extending the number of IVF cycles beyond three or four,” they wrote.
Three unsuccessful embryo transfers, referred to as “repeat implantation failure,” is often seen as a sign to stop IVF, but that opinion is based on a study that did not use intracytoplasmic sperm injection, the researchers noted.
They studied nearly 157,000 women who underwent more than 257,000 IVF ovarian stimulation cycles in the United Kingdom between 2003 and 2010, following them until June 2012. Most women were 35 years old when they began treatment (JAMA 2015;314[24]:2654-62. doi:10.1001/jama.2015.17296).
Women who were younger than 40 years and used their own oocytes had slightly higher adjusted rates of live birth compared with the overall cohort, according to the researchers. The prognosis-adjusted live-birth rate was 32% in the first cycle and 68% at six cycles. In contrast, the live birth rate among women aged 40-42 years was 12% after the first cycle and 31% after six cycles. For women older than 42 years, live birth rates within each cycle were usually less than 4%.
“No age differential was observed among women using donor oocytes,” the researchers wrote. “Rates were lower for women with untreated male partner–related infertility compared with those with any other cause, but treatment with either intracytoplasmic sperm injection or sperm donation removed this difference.”
The researchers were able to assess only live birth as an outcome. But they noted that future studies should consider potential adverse effects of additional cycles of treatment, including ovarian hyperstimulation syndrome and a potential increased risk of preterm birth or congenital anomalies.
“For some couples, the emotional stress of repeat treatments may be undesirable, and the cost of a prolonged treatment course, with several repeat oocyte stimulation cycles, may be unsustainable for health services, insurers, or couples,” the researchers wrote. “However, we think the potential for success with further cycles should be discussed with couples.”
The UK Medical Research Council, the National Institute for Health Research, and the Wellcome Trust funded the study. One coauthor reported financial relationships with Beckman Coulter, Besins, Ferring, Merck Serono, Merck Sharp & Dohme, and Roche Diagnostic. The other researchers reported having no financial disclosures.
For some couples, especially those with a female partner younger than 40 years, those for whom male-factor infertility is treated with intracytoplasmic sperm injection, or those for whom oocyte or semen donation is used, the incremental increase in cumulative pregnancy probability after three or four assisted reproductive technology cycles may be worthwhile, especially if financial resources are available. For insurers who cover a specific number of cycles, the incremental cost-effectiveness of each additional cycle is unclear, at least in part because of the methodological complexities involved in economic assessments of fertility treatments, but there is clearly some benefit for the couple.
For clinicians, it is important that these data be shared with couples so that they can make a truly informed decision. This will require time and expertise in communication. For policy makers, revising the National ART Surveillance System to allow reporting of outcomes on a per-couple basis (including oocyte donors) would provide significantly more useful information for decision-making purposes.
Dr. Evan R. Myers is at Duke University Medical Center in Durham, N.C. He reported having no financial disclosures. These comments were adapted from his editorial (JAMA 2015;314[24]:2627-9. doi: 10.1001/jama.2015.17297).
For some couples, especially those with a female partner younger than 40 years, those for whom male-factor infertility is treated with intracytoplasmic sperm injection, or those for whom oocyte or semen donation is used, the incremental increase in cumulative pregnancy probability after three or four assisted reproductive technology cycles may be worthwhile, especially if financial resources are available. For insurers who cover a specific number of cycles, the incremental cost-effectiveness of each additional cycle is unclear, at least in part because of the methodological complexities involved in economic assessments of fertility treatments, but there is clearly some benefit for the couple.
For clinicians, it is important that these data be shared with couples so that they can make a truly informed decision. This will require time and expertise in communication. For policy makers, revising the National ART Surveillance System to allow reporting of outcomes on a per-couple basis (including oocyte donors) would provide significantly more useful information for decision-making purposes.
Dr. Evan R. Myers is at Duke University Medical Center in Durham, N.C. He reported having no financial disclosures. These comments were adapted from his editorial (JAMA 2015;314[24]:2627-9. doi: 10.1001/jama.2015.17297).
For some couples, especially those with a female partner younger than 40 years, those for whom male-factor infertility is treated with intracytoplasmic sperm injection, or those for whom oocyte or semen donation is used, the incremental increase in cumulative pregnancy probability after three or four assisted reproductive technology cycles may be worthwhile, especially if financial resources are available. For insurers who cover a specific number of cycles, the incremental cost-effectiveness of each additional cycle is unclear, at least in part because of the methodological complexities involved in economic assessments of fertility treatments, but there is clearly some benefit for the couple.
For clinicians, it is important that these data be shared with couples so that they can make a truly informed decision. This will require time and expertise in communication. For policy makers, revising the National ART Surveillance System to allow reporting of outcomes on a per-couple basis (including oocyte donors) would provide significantly more useful information for decision-making purposes.
Dr. Evan R. Myers is at Duke University Medical Center in Durham, N.C. He reported having no financial disclosures. These comments were adapted from his editorial (JAMA 2015;314[24]:2627-9. doi: 10.1001/jama.2015.17297).
Among women undergoing in vitro fertilization, adjusted rates of live birth rose modestly but continuously through up to nine IVF cycles, according to a study published online Dec. 22 in JAMA.
After the researchers accounted for women who stopped trying to conceive by IVF, the estimated cumulative live birth rate was 65% after six cycles, compared with 54% after three cycles and 29% after one cycle, reported Andrew D.A.C. Smith, Ph.D., of the University of Bristol, England, and his associates.
“These findings support the efficacy of extending the number of IVF cycles beyond three or four,” they wrote.
Three unsuccessful embryo transfers, referred to as “repeat implantation failure,” is often seen as a sign to stop IVF, but that opinion is based on a study that did not use intracytoplasmic sperm injection, the researchers noted.
They studied nearly 157,000 women who underwent more than 257,000 IVF ovarian stimulation cycles in the United Kingdom between 2003 and 2010, following them until June 2012. Most women were 35 years old when they began treatment (JAMA 2015;314[24]:2654-62. doi:10.1001/jama.2015.17296).
Women who were younger than 40 years and used their own oocytes had slightly higher adjusted rates of live birth compared with the overall cohort, according to the researchers. The prognosis-adjusted live-birth rate was 32% in the first cycle and 68% at six cycles. In contrast, the live birth rate among women aged 40-42 years was 12% after the first cycle and 31% after six cycles. For women older than 42 years, live birth rates within each cycle were usually less than 4%.
“No age differential was observed among women using donor oocytes,” the researchers wrote. “Rates were lower for women with untreated male partner–related infertility compared with those with any other cause, but treatment with either intracytoplasmic sperm injection or sperm donation removed this difference.”
The researchers were able to assess only live birth as an outcome. But they noted that future studies should consider potential adverse effects of additional cycles of treatment, including ovarian hyperstimulation syndrome and a potential increased risk of preterm birth or congenital anomalies.
“For some couples, the emotional stress of repeat treatments may be undesirable, and the cost of a prolonged treatment course, with several repeat oocyte stimulation cycles, may be unsustainable for health services, insurers, or couples,” the researchers wrote. “However, we think the potential for success with further cycles should be discussed with couples.”
The UK Medical Research Council, the National Institute for Health Research, and the Wellcome Trust funded the study. One coauthor reported financial relationships with Beckman Coulter, Besins, Ferring, Merck Serono, Merck Sharp & Dohme, and Roche Diagnostic. The other researchers reported having no financial disclosures.
Among women undergoing in vitro fertilization, adjusted rates of live birth rose modestly but continuously through up to nine IVF cycles, according to a study published online Dec. 22 in JAMA.
After the researchers accounted for women who stopped trying to conceive by IVF, the estimated cumulative live birth rate was 65% after six cycles, compared with 54% after three cycles and 29% after one cycle, reported Andrew D.A.C. Smith, Ph.D., of the University of Bristol, England, and his associates.
“These findings support the efficacy of extending the number of IVF cycles beyond three or four,” they wrote.
Three unsuccessful embryo transfers, referred to as “repeat implantation failure,” is often seen as a sign to stop IVF, but that opinion is based on a study that did not use intracytoplasmic sperm injection, the researchers noted.
They studied nearly 157,000 women who underwent more than 257,000 IVF ovarian stimulation cycles in the United Kingdom between 2003 and 2010, following them until June 2012. Most women were 35 years old when they began treatment (JAMA 2015;314[24]:2654-62. doi:10.1001/jama.2015.17296).
Women who were younger than 40 years and used their own oocytes had slightly higher adjusted rates of live birth compared with the overall cohort, according to the researchers. The prognosis-adjusted live-birth rate was 32% in the first cycle and 68% at six cycles. In contrast, the live birth rate among women aged 40-42 years was 12% after the first cycle and 31% after six cycles. For women older than 42 years, live birth rates within each cycle were usually less than 4%.
“No age differential was observed among women using donor oocytes,” the researchers wrote. “Rates were lower for women with untreated male partner–related infertility compared with those with any other cause, but treatment with either intracytoplasmic sperm injection or sperm donation removed this difference.”
The researchers were able to assess only live birth as an outcome. But they noted that future studies should consider potential adverse effects of additional cycles of treatment, including ovarian hyperstimulation syndrome and a potential increased risk of preterm birth or congenital anomalies.
“For some couples, the emotional stress of repeat treatments may be undesirable, and the cost of a prolonged treatment course, with several repeat oocyte stimulation cycles, may be unsustainable for health services, insurers, or couples,” the researchers wrote. “However, we think the potential for success with further cycles should be discussed with couples.”
The UK Medical Research Council, the National Institute for Health Research, and the Wellcome Trust funded the study. One coauthor reported financial relationships with Beckman Coulter, Besins, Ferring, Merck Serono, Merck Sharp & Dohme, and Roche Diagnostic. The other researchers reported having no financial disclosures.
FROM JAMA
Key clinical point: Extending in vitro fertilization beyond three to four cycles increased the likelihood of achieving a live birth.
Major finding: The estimated cumulative live birth rate was 65% after six cycles, compared with 54% after three cycles and 29% after one cycle.
Data source: A prospective study of 156,947 women who underwent 257,398 IVF cycles between 2003 and 2010.
Disclosures: The UK Medical Research Council, the National Institute for Health Research, and the Wellcome Trust funded the study. One coauthor reported financial relationships with Beckman Coulter, Besins, Ferring, Merck Serono, Merck Sharp & Dohme, and Roche Diagnostic. The other researchers reported having no financial disclosures.
Study suggests surgeons have heeded FDA warning about vaginal mesh
Surgeons seem to have heeded a beefed-up warning from the U.S. Food and Drug Administration about using transvaginal surgical mesh when repairing pelvic organ prolapse, investigators reported online Dec. 21 in JAMA Internal Medicine.
In New York state, the use of mesh fell by almost 25% just 2 years after the FDA intensified its original warning, said Dr. Art Sedrakyan of Cornell University in Ithaca, N.Y., and his associates. “Although other explanations are possible, we believe that the stronger language in the 2011 FDA warning is at least partly related to the decline in mesh use,” they said.
A prior study by the investigators found that use of mesh actually rose by almost 50% during the 3 years after the original FDA warning, issued in 2008 (BMJ. 2015 Jun 3;350:h2685 doi: 10.1136/bmj.h2685). During that time, FDA received about 1,500 reports of subsequent adverse events, such as erosion through the vagina, pain, infection, organ perforation, bleeding, dyspareunia, vaginal scarring or shrinkage, and urinary problems, the investigators noted (JAMA Intern Med. 2015 Dec 21. doi: 10.1001/jamainternmed.2015.6595).
In 2011, the FDA responded by strengthening its original warning. Instead of urging physicians to be aware of risks and training in each technique in which they used mesh, the agency noted that mesh-related complications are “not rare” and emphasized that pelvic organ prolapse (POP) can be repaired without mesh. To examine the effects of that warning, the investigators analyzed a database of all surgical procedures performed in New York state during 2011-2013. They excluded patients who had undergone previous POP repairs and broke down trends by hospital type and size.
Total annual POP repairs dropped from 6,960 in 2011 to 5,757 in 2013, they found. After the new FDA warning, the use of mesh also fell – from 30% (95% confidence interval, 29%-31%) in 2011 to 23% (95% CI, 22%-24%) in 2013. The drop was significantly less dramatic in academic and high-volume hospitals, perhaps because surgeons there were more comfortable using mesh or were treating worse disease, the researchers said. “The higher rate of decline in the use of mesh by low-volume and nonacademic providers may be related to a lower tolerance for litigation related to sizable awards and growing numbers of lawsuits in outpatient settings,” they added.
The National Institutes of Health and the FDA partially funded the study. The investigators had no disclosures.
Surgeons seem to have heeded a beefed-up warning from the U.S. Food and Drug Administration about using transvaginal surgical mesh when repairing pelvic organ prolapse, investigators reported online Dec. 21 in JAMA Internal Medicine.
In New York state, the use of mesh fell by almost 25% just 2 years after the FDA intensified its original warning, said Dr. Art Sedrakyan of Cornell University in Ithaca, N.Y., and his associates. “Although other explanations are possible, we believe that the stronger language in the 2011 FDA warning is at least partly related to the decline in mesh use,” they said.
A prior study by the investigators found that use of mesh actually rose by almost 50% during the 3 years after the original FDA warning, issued in 2008 (BMJ. 2015 Jun 3;350:h2685 doi: 10.1136/bmj.h2685). During that time, FDA received about 1,500 reports of subsequent adverse events, such as erosion through the vagina, pain, infection, organ perforation, bleeding, dyspareunia, vaginal scarring or shrinkage, and urinary problems, the investigators noted (JAMA Intern Med. 2015 Dec 21. doi: 10.1001/jamainternmed.2015.6595).
In 2011, the FDA responded by strengthening its original warning. Instead of urging physicians to be aware of risks and training in each technique in which they used mesh, the agency noted that mesh-related complications are “not rare” and emphasized that pelvic organ prolapse (POP) can be repaired without mesh. To examine the effects of that warning, the investigators analyzed a database of all surgical procedures performed in New York state during 2011-2013. They excluded patients who had undergone previous POP repairs and broke down trends by hospital type and size.
Total annual POP repairs dropped from 6,960 in 2011 to 5,757 in 2013, they found. After the new FDA warning, the use of mesh also fell – from 30% (95% confidence interval, 29%-31%) in 2011 to 23% (95% CI, 22%-24%) in 2013. The drop was significantly less dramatic in academic and high-volume hospitals, perhaps because surgeons there were more comfortable using mesh or were treating worse disease, the researchers said. “The higher rate of decline in the use of mesh by low-volume and nonacademic providers may be related to a lower tolerance for litigation related to sizable awards and growing numbers of lawsuits in outpatient settings,” they added.
The National Institutes of Health and the FDA partially funded the study. The investigators had no disclosures.
Surgeons seem to have heeded a beefed-up warning from the U.S. Food and Drug Administration about using transvaginal surgical mesh when repairing pelvic organ prolapse, investigators reported online Dec. 21 in JAMA Internal Medicine.
In New York state, the use of mesh fell by almost 25% just 2 years after the FDA intensified its original warning, said Dr. Art Sedrakyan of Cornell University in Ithaca, N.Y., and his associates. “Although other explanations are possible, we believe that the stronger language in the 2011 FDA warning is at least partly related to the decline in mesh use,” they said.
A prior study by the investigators found that use of mesh actually rose by almost 50% during the 3 years after the original FDA warning, issued in 2008 (BMJ. 2015 Jun 3;350:h2685 doi: 10.1136/bmj.h2685). During that time, FDA received about 1,500 reports of subsequent adverse events, such as erosion through the vagina, pain, infection, organ perforation, bleeding, dyspareunia, vaginal scarring or shrinkage, and urinary problems, the investigators noted (JAMA Intern Med. 2015 Dec 21. doi: 10.1001/jamainternmed.2015.6595).
In 2011, the FDA responded by strengthening its original warning. Instead of urging physicians to be aware of risks and training in each technique in which they used mesh, the agency noted that mesh-related complications are “not rare” and emphasized that pelvic organ prolapse (POP) can be repaired without mesh. To examine the effects of that warning, the investigators analyzed a database of all surgical procedures performed in New York state during 2011-2013. They excluded patients who had undergone previous POP repairs and broke down trends by hospital type and size.
Total annual POP repairs dropped from 6,960 in 2011 to 5,757 in 2013, they found. After the new FDA warning, the use of mesh also fell – from 30% (95% confidence interval, 29%-31%) in 2011 to 23% (95% CI, 22%-24%) in 2013. The drop was significantly less dramatic in academic and high-volume hospitals, perhaps because surgeons there were more comfortable using mesh or were treating worse disease, the researchers said. “The higher rate of decline in the use of mesh by low-volume and nonacademic providers may be related to a lower tolerance for litigation related to sizable awards and growing numbers of lawsuits in outpatient settings,” they added.
The National Institutes of Health and the FDA partially funded the study. The investigators had no disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Surgeons seem to have heeded stronger language from FDA about the risks of using transvaginal surgical mesh.
Major finding: The use of mesh to repair pelvic organ prolapse fell from 30% to 23% within 2 years after the FDA beefed up its original warning.
Data source: A retrospective analysis of data from the New York Statewide Planning and Research Cooperative System, which has records of all surgical procedures in the state.
Disclosures: The National Institutes of Health and the U.S. FDA partially funded the study. The investigators had no disclosures.
Six factors predicted poor surgical outcomes in toxic colitis
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Older age, female sex, preoperative azotemia, chronic steroid use, preoperative respiratory failure, and coagulopathy predicted adverse surgical outcomes in patients with toxic colitis.
Major finding: Odds ratios for these factors in the multivariate model ranged from 2.7 (preoperative respiratory failure) to 22.2 (age older than 80 years).
Data source: A multicenter prospective analysis of data from the National Surgical Quality Improvement Project.
Disclosures: The investigators reported no funding sources and had no disclosures.
Measures that don’t account for DNR status could unfairly penalize hospitals
Mortality-based quality measures that do not account for do-not-resuscitate orders paint a skewed picture of hospital performance, said authors of a multicenter retrospective cohort study.
“Our findings suggest that current methods of comparing hospitals, which do not account for patient DNR status, penalize potentially high-quality hospitals [that admit] a larger proportion of patients who had chosen to forgo resuscitation,” Dr. Allan J. Walkey of Boston University, and his associates wrote online Dec. 14 in JAMA Internal Medicine. Accounting for DNR status when evaluating mortality outcomes “may substantially affect publicly reportable hospital rankings and hospital reimbursements,” the researchers added.
Early DNR orders typically reflect patient-specific variables, such as baseline comorbidities and attitudes about end-of-life care, the researchers noted. “Despite the potential for hospital variation in DNR orders to influence patients’ end-of-life experiences and outcomes, DNR status is generally unreported by hospitals and unaccounted for in hospital outcome measures,” they added. Their population-based cohort study assessed DNR status and mortality for more than 90,000 pneumonia cases at 303 hospitals in California during 2011 (JAMA Intern Med. 2015 Dec. 14. doi: 10.1001/jamainternmed.2015.6324).
The lower and upper quartiles for DNR rates were about 9% and 22%, said the researchers. Without accounting for these differences, hospitals in the highest quartile had significantly greater patient mortality than did those in the lowest quartile (adjusted odds ratio, 1.17; 95% confidence interval, 1.04-1.32), corresponding to worse mortality rankings. But this trend actually reversed after the investigators accounted for DNR rates (adjusted OR, 0.79; 95% CI, 0.70-0.89), as did the link between hospital mortality rankings and DNR rates.
Only about half of hospitals that were low-performing outliers without accounting for DNR status remained outliers after adjustment, the researchers noted. And although DNR rates did not significantly correlate with composite quality measures of pneumonia care, they were positively linked to patient satisfaction scores (P less than .001). Based on the findings, “stakeholders should seek to improve methods to standardize and report DNR status in hospital discharge records,” they concluded.
The study was funded by the National Institutes of Health, the National Heart, Lung, and Blood Institute of the NIH, the Agency for Healthcare Research and Quality, the Edith Nourse Rogers Memorial Veterans Affairs Hospital, and Boston University. The researchers had no disclosures.
Mortality-based quality measures that do not account for do-not-resuscitate orders paint a skewed picture of hospital performance, said authors of a multicenter retrospective cohort study.
“Our findings suggest that current methods of comparing hospitals, which do not account for patient DNR status, penalize potentially high-quality hospitals [that admit] a larger proportion of patients who had chosen to forgo resuscitation,” Dr. Allan J. Walkey of Boston University, and his associates wrote online Dec. 14 in JAMA Internal Medicine. Accounting for DNR status when evaluating mortality outcomes “may substantially affect publicly reportable hospital rankings and hospital reimbursements,” the researchers added.
Early DNR orders typically reflect patient-specific variables, such as baseline comorbidities and attitudes about end-of-life care, the researchers noted. “Despite the potential for hospital variation in DNR orders to influence patients’ end-of-life experiences and outcomes, DNR status is generally unreported by hospitals and unaccounted for in hospital outcome measures,” they added. Their population-based cohort study assessed DNR status and mortality for more than 90,000 pneumonia cases at 303 hospitals in California during 2011 (JAMA Intern Med. 2015 Dec. 14. doi: 10.1001/jamainternmed.2015.6324).
The lower and upper quartiles for DNR rates were about 9% and 22%, said the researchers. Without accounting for these differences, hospitals in the highest quartile had significantly greater patient mortality than did those in the lowest quartile (adjusted odds ratio, 1.17; 95% confidence interval, 1.04-1.32), corresponding to worse mortality rankings. But this trend actually reversed after the investigators accounted for DNR rates (adjusted OR, 0.79; 95% CI, 0.70-0.89), as did the link between hospital mortality rankings and DNR rates.
Only about half of hospitals that were low-performing outliers without accounting for DNR status remained outliers after adjustment, the researchers noted. And although DNR rates did not significantly correlate with composite quality measures of pneumonia care, they were positively linked to patient satisfaction scores (P less than .001). Based on the findings, “stakeholders should seek to improve methods to standardize and report DNR status in hospital discharge records,” they concluded.
The study was funded by the National Institutes of Health, the National Heart, Lung, and Blood Institute of the NIH, the Agency for Healthcare Research and Quality, the Edith Nourse Rogers Memorial Veterans Affairs Hospital, and Boston University. The researchers had no disclosures.
Mortality-based quality measures that do not account for do-not-resuscitate orders paint a skewed picture of hospital performance, said authors of a multicenter retrospective cohort study.
“Our findings suggest that current methods of comparing hospitals, which do not account for patient DNR status, penalize potentially high-quality hospitals [that admit] a larger proportion of patients who had chosen to forgo resuscitation,” Dr. Allan J. Walkey of Boston University, and his associates wrote online Dec. 14 in JAMA Internal Medicine. Accounting for DNR status when evaluating mortality outcomes “may substantially affect publicly reportable hospital rankings and hospital reimbursements,” the researchers added.
Early DNR orders typically reflect patient-specific variables, such as baseline comorbidities and attitudes about end-of-life care, the researchers noted. “Despite the potential for hospital variation in DNR orders to influence patients’ end-of-life experiences and outcomes, DNR status is generally unreported by hospitals and unaccounted for in hospital outcome measures,” they added. Their population-based cohort study assessed DNR status and mortality for more than 90,000 pneumonia cases at 303 hospitals in California during 2011 (JAMA Intern Med. 2015 Dec. 14. doi: 10.1001/jamainternmed.2015.6324).
The lower and upper quartiles for DNR rates were about 9% and 22%, said the researchers. Without accounting for these differences, hospitals in the highest quartile had significantly greater patient mortality than did those in the lowest quartile (adjusted odds ratio, 1.17; 95% confidence interval, 1.04-1.32), corresponding to worse mortality rankings. But this trend actually reversed after the investigators accounted for DNR rates (adjusted OR, 0.79; 95% CI, 0.70-0.89), as did the link between hospital mortality rankings and DNR rates.
Only about half of hospitals that were low-performing outliers without accounting for DNR status remained outliers after adjustment, the researchers noted. And although DNR rates did not significantly correlate with composite quality measures of pneumonia care, they were positively linked to patient satisfaction scores (P less than .001). Based on the findings, “stakeholders should seek to improve methods to standardize and report DNR status in hospital discharge records,” they concluded.
The study was funded by the National Institutes of Health, the National Heart, Lung, and Blood Institute of the NIH, the Agency for Healthcare Research and Quality, the Edith Nourse Rogers Memorial Veterans Affairs Hospital, and Boston University. The researchers had no disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Quality measures that fail to account for DNR orders could lead to unfair hospital penalties.
Major finding: Without accounting for DNR status, hospitals whose rates were in the highest quartile had significantly greater mortality rates (adjusted odds ratio, 1.17) than did those in the lowest quartile, corresponding with worse mortality rankings.
Data source: A retrospective, population-based cohort study of 90,644 cases of pneumonia at 303 hospitals in California.
Disclosures: The study was funded by the National Institutes of Health, the National Heart, Lung, and Blood Institute of the NIH, the Agency for Healthcare Research and Quality, the Edith Nourse Rogers Memorial Veterans Affairs Hospital, and Boston University. The researchers had no disclosures.
Review: Opioid prescriptions are the work of many physicians
A “broad swath” of Medicare providers wrote scripts for opioids in 2013, contradicting the idea that the overdose epidemic is mainly the work of “small groups of prolific prescribers and corrupt pill mills,” investigators wrote online in JAMA Internal Medicine.
“Contrary to the California workers’ compensation data showing a small subset of prescribers accounting for a disproportionately large percentage of opioid prescribing, Medicare opioid prescribing is distributed across many prescribers and is, if anything, less skewed than all drug prescribing,” said Dr. Jonathan H. Chen of the Veterans Affairs Palo Alto (Calif.) Health Care System, and his associates.
Their study included 808,020 prescribers and almost 1.2 billion Medicare Part D claims worth nearly $81 billion dollars. They focused on schedule II opioid prescriptions containing oxycodone, fentanyl, hydrocodone, morphine, methadone, hydromorphone, oxymorphone, meperidine, codeine, opium, or levorphanol (JAMA Intern Med. 2015 Dec 14. doi: 10.1001/jamainternmed.2015.6662).
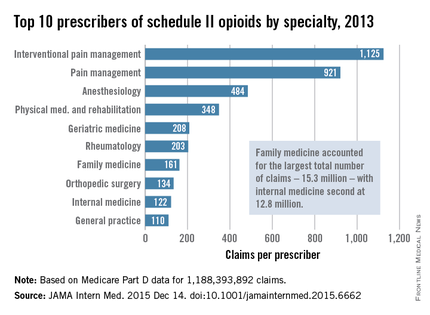
Not surprisingly, specialists in pain management, anesthesia, and physical medicine wrote the most prescriptions per provider. But family practitioners, internists, nurse practitioners, and physician assistants wrote 35,268,234 prescriptions – more than all other specialties combined. “The trends hold up across state lines, with negligible geographic variability,” the researchers said.
The findings contradict an analysis of California workers’ compensation data, in which 1% of prescribers accounted for a third of schedule II opioid prescriptions, and 10% of prescribers accounted for 80% of prescriptions, the investigators noted. Nonetheless, 10% of Medicare prescribers in Dr. Chen’s study accounted for 78% of the total cost of opioids, possibly because they were prescribing pricier formulations or higher doses.
Overall, the findings suggest that opioid prescribing is “widespread” and “relatively indifferent to individual physicians, specialty, or region” – and that efforts to stem the tide must be equally broad, the researchers concluded.
Their study was supported by the VA Office of Academic Affiliations, the VA Health Services Research and Development Service, the National Institute of General Medical Sciences, and the Peter F. McManus Charitable Trust. The researchers had no disclosures.
A “broad swath” of Medicare providers wrote scripts for opioids in 2013, contradicting the idea that the overdose epidemic is mainly the work of “small groups of prolific prescribers and corrupt pill mills,” investigators wrote online in JAMA Internal Medicine.
“Contrary to the California workers’ compensation data showing a small subset of prescribers accounting for a disproportionately large percentage of opioid prescribing, Medicare opioid prescribing is distributed across many prescribers and is, if anything, less skewed than all drug prescribing,” said Dr. Jonathan H. Chen of the Veterans Affairs Palo Alto (Calif.) Health Care System, and his associates.
Their study included 808,020 prescribers and almost 1.2 billion Medicare Part D claims worth nearly $81 billion dollars. They focused on schedule II opioid prescriptions containing oxycodone, fentanyl, hydrocodone, morphine, methadone, hydromorphone, oxymorphone, meperidine, codeine, opium, or levorphanol (JAMA Intern Med. 2015 Dec 14. doi: 10.1001/jamainternmed.2015.6662).
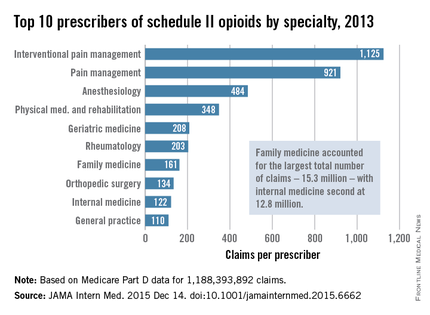
Not surprisingly, specialists in pain management, anesthesia, and physical medicine wrote the most prescriptions per provider. But family practitioners, internists, nurse practitioners, and physician assistants wrote 35,268,234 prescriptions – more than all other specialties combined. “The trends hold up across state lines, with negligible geographic variability,” the researchers said.
The findings contradict an analysis of California workers’ compensation data, in which 1% of prescribers accounted for a third of schedule II opioid prescriptions, and 10% of prescribers accounted for 80% of prescriptions, the investigators noted. Nonetheless, 10% of Medicare prescribers in Dr. Chen’s study accounted for 78% of the total cost of opioids, possibly because they were prescribing pricier formulations or higher doses.
Overall, the findings suggest that opioid prescribing is “widespread” and “relatively indifferent to individual physicians, specialty, or region” – and that efforts to stem the tide must be equally broad, the researchers concluded.
Their study was supported by the VA Office of Academic Affiliations, the VA Health Services Research and Development Service, the National Institute of General Medical Sciences, and the Peter F. McManus Charitable Trust. The researchers had no disclosures.
A “broad swath” of Medicare providers wrote scripts for opioids in 2013, contradicting the idea that the overdose epidemic is mainly the work of “small groups of prolific prescribers and corrupt pill mills,” investigators wrote online in JAMA Internal Medicine.
“Contrary to the California workers’ compensation data showing a small subset of prescribers accounting for a disproportionately large percentage of opioid prescribing, Medicare opioid prescribing is distributed across many prescribers and is, if anything, less skewed than all drug prescribing,” said Dr. Jonathan H. Chen of the Veterans Affairs Palo Alto (Calif.) Health Care System, and his associates.
Their study included 808,020 prescribers and almost 1.2 billion Medicare Part D claims worth nearly $81 billion dollars. They focused on schedule II opioid prescriptions containing oxycodone, fentanyl, hydrocodone, morphine, methadone, hydromorphone, oxymorphone, meperidine, codeine, opium, or levorphanol (JAMA Intern Med. 2015 Dec 14. doi: 10.1001/jamainternmed.2015.6662).
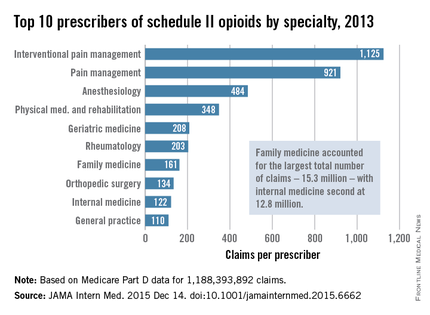
Not surprisingly, specialists in pain management, anesthesia, and physical medicine wrote the most prescriptions per provider. But family practitioners, internists, nurse practitioners, and physician assistants wrote 35,268,234 prescriptions – more than all other specialties combined. “The trends hold up across state lines, with negligible geographic variability,” the researchers said.
The findings contradict an analysis of California workers’ compensation data, in which 1% of prescribers accounted for a third of schedule II opioid prescriptions, and 10% of prescribers accounted for 80% of prescriptions, the investigators noted. Nonetheless, 10% of Medicare prescribers in Dr. Chen’s study accounted for 78% of the total cost of opioids, possibly because they were prescribing pricier formulations or higher doses.
Overall, the findings suggest that opioid prescribing is “widespread” and “relatively indifferent to individual physicians, specialty, or region” – and that efforts to stem the tide must be equally broad, the researchers concluded.
Their study was supported by the VA Office of Academic Affiliations, the VA Health Services Research and Development Service, the National Institute of General Medical Sciences, and the Peter F. McManus Charitable Trust. The researchers had no disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Many different types of general practitioners and specialists often prescribe opioids to Medicare beneficiaries.
Major finding: Family practitioners, internists, nurse practitioners, and physician assistants wrote 35,268,234 prescriptions – more than all other specialties combined.
Data source: An analysis of nearly 1.2 billion Medicare part D claims from 2013.
Disclosures: The study was supported by the VA Office of Academic Affiliations, the VA Health Services Research and Development Service, the National Institute of General Medical Sciences, and the Peter F. McManus Charitable Trust. The researchers had no disclosures.
Radiography missed most clinical cases of hip osteoarthritis
Radiography detected up to 16% of cases of hip osteoarthritis among older patients with frequent hip pain in an analysis of participants in the Framingham Osteoarthritis Study and the Osteoarthritis Initiative.
“In older patients, inadequate recognition of osteoarthritis has consequences. Decreased functional status from osteoarthritis significantly increases morbidity from coronary heart disease, lung disease, diabetes, obesity, falls, frailty, and various other ailments,” said Dr. Chan Kim of Boston University and his associates. “Because many patients with hip pain do not have radiographic hip osteoarthritis, a health professional should continue with the evaluation and treatment of osteoarthritis, despite negative radiographic findings.”
Radiographic pathology often is detected late in the course of knee OA and correlates poorly with knee pain, but few studies have examined these trends for the hip. The researchers analyzed pelvic radiographs and hip pain among 946 participants in the Framingham Osteoarthritis Study and 4,366 participants in the Osteoarthritis Initiative. They defined radiographic hip OA as a Kellgren-Lawrence grade of 2 or more – that is, definite superolateral or superomedial joint space narrowing and a definite osteophyte. They used various clinical symptoms of hip OA for comparison. Participants in both studies were older than 45 years, and tended to be in their early 60s (BMJ 2015 Dec 2. doi: 10.1136/bmj.h5983).
The most sensitive criterion in the study was groin pain, for which radiography was positive in 37% of hips in the Framingham Study and 17% of hips in the Osteoarthritis Initiative, the researchers said. Other clinical criteria were less sensitive, including anterior thigh pain, frequent hip pain, and painful internal rotation. Moreover, about 21%-24% of hips with radiographic OA were frequently painful.
The study did not evaluate MRI findings, the investigators noted. They suggested that such results would resemble those for the knee, in which MRI is “more sensitive than radiography, [but] it is far less specific for abnormalities suggestive of osteoarthritis in most middle-aged and older people.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases funded the study. The Osteoarthritis Initiative is funded by the National Institutes of Health, Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. The researchers had no disclosures.
Radiography detected up to 16% of cases of hip osteoarthritis among older patients with frequent hip pain in an analysis of participants in the Framingham Osteoarthritis Study and the Osteoarthritis Initiative.
“In older patients, inadequate recognition of osteoarthritis has consequences. Decreased functional status from osteoarthritis significantly increases morbidity from coronary heart disease, lung disease, diabetes, obesity, falls, frailty, and various other ailments,” said Dr. Chan Kim of Boston University and his associates. “Because many patients with hip pain do not have radiographic hip osteoarthritis, a health professional should continue with the evaluation and treatment of osteoarthritis, despite negative radiographic findings.”
Radiographic pathology often is detected late in the course of knee OA and correlates poorly with knee pain, but few studies have examined these trends for the hip. The researchers analyzed pelvic radiographs and hip pain among 946 participants in the Framingham Osteoarthritis Study and 4,366 participants in the Osteoarthritis Initiative. They defined radiographic hip OA as a Kellgren-Lawrence grade of 2 or more – that is, definite superolateral or superomedial joint space narrowing and a definite osteophyte. They used various clinical symptoms of hip OA for comparison. Participants in both studies were older than 45 years, and tended to be in their early 60s (BMJ 2015 Dec 2. doi: 10.1136/bmj.h5983).
The most sensitive criterion in the study was groin pain, for which radiography was positive in 37% of hips in the Framingham Study and 17% of hips in the Osteoarthritis Initiative, the researchers said. Other clinical criteria were less sensitive, including anterior thigh pain, frequent hip pain, and painful internal rotation. Moreover, about 21%-24% of hips with radiographic OA were frequently painful.
The study did not evaluate MRI findings, the investigators noted. They suggested that such results would resemble those for the knee, in which MRI is “more sensitive than radiography, [but] it is far less specific for abnormalities suggestive of osteoarthritis in most middle-aged and older people.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases funded the study. The Osteoarthritis Initiative is funded by the National Institutes of Health, Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. The researchers had no disclosures.
Radiography detected up to 16% of cases of hip osteoarthritis among older patients with frequent hip pain in an analysis of participants in the Framingham Osteoarthritis Study and the Osteoarthritis Initiative.
“In older patients, inadequate recognition of osteoarthritis has consequences. Decreased functional status from osteoarthritis significantly increases morbidity from coronary heart disease, lung disease, diabetes, obesity, falls, frailty, and various other ailments,” said Dr. Chan Kim of Boston University and his associates. “Because many patients with hip pain do not have radiographic hip osteoarthritis, a health professional should continue with the evaluation and treatment of osteoarthritis, despite negative radiographic findings.”
Radiographic pathology often is detected late in the course of knee OA and correlates poorly with knee pain, but few studies have examined these trends for the hip. The researchers analyzed pelvic radiographs and hip pain among 946 participants in the Framingham Osteoarthritis Study and 4,366 participants in the Osteoarthritis Initiative. They defined radiographic hip OA as a Kellgren-Lawrence grade of 2 or more – that is, definite superolateral or superomedial joint space narrowing and a definite osteophyte. They used various clinical symptoms of hip OA for comparison. Participants in both studies were older than 45 years, and tended to be in their early 60s (BMJ 2015 Dec 2. doi: 10.1136/bmj.h5983).
The most sensitive criterion in the study was groin pain, for which radiography was positive in 37% of hips in the Framingham Study and 17% of hips in the Osteoarthritis Initiative, the researchers said. Other clinical criteria were less sensitive, including anterior thigh pain, frequent hip pain, and painful internal rotation. Moreover, about 21%-24% of hips with radiographic OA were frequently painful.
The study did not evaluate MRI findings, the investigators noted. They suggested that such results would resemble those for the knee, in which MRI is “more sensitive than radiography, [but] it is far less specific for abnormalities suggestive of osteoarthritis in most middle-aged and older people.”
The National Institute of Arthritis and Musculoskeletal and Skin Diseases funded the study. The Osteoarthritis Initiative is funded by the National Institutes of Health, Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. The researchers had no disclosures.
FROM BMJ
Key clinical point: Radiographic hip osteoarthritis correlates poorly with hip pain, even among older patients with a high index of suspicion for hip OA.
Major finding: Radiography detected up to 16% of cases of hip OA among older patients with frequent hip pain.
Data source: An analysis of pelvic radiographs and hip pain reported by 946 participants in the Framingham Osteoarthritis Study and 4,366 participants in the Osteoarthritis Initiative.
Disclosures: The National Institute of Arthritis and Musculoskeletal and Skin Diseases funded the study. The Osteoarthritis Initiative is funded by the National Institutes of Health, Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. The researchers had no disclosures.