User login
Pre-exposure prophylaxis could cut HIV incidence by 44%
Rates of HIV infection in the United Kingdom could drop by 44% this decade if just a quarter of high-risk men who have sex with men receive pre-exposure prophylaxis, regular HIV testing, and early treatment, according to investigators.
“Our findings show that PrEP can be highly effective against HIV transmission at the population level, and could outperform other interventions at the same level of program coverage,” reported Dr. Narat Punyacharoensin of the London School of Hygiene and Tropical Medicine and his associates. The study was published online Jan. 13 in The Lancet HIV.
The incidence of HIV infection in the United Kingdom rose slightly in 2014, and shows no signs of reversing course. Among 104,000 UK residents living with HIV, about 43% are MSM, the researchers noted. After fitting a mathematical model with surveillance and behavioral data, they estimated the effects of seven HIV interventions targeting MSM, including expanded testing, test-and-treat programs, antiretroviral PrEP, and measures to reduce sexual partners and unprotected anal intercourse (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00056-9).
If nothing is done, the UK can expect about 17,000 new HIV infections by 2020, the model showed. But offering just 25% of high-risk MSM PrEP along with regular HIV testing and early treatment would prevent 7,399 HIV infections by 2020 (interquartile range, 5,587-9,813), or about 44% of the total incidence (IQR, 33-58).
“An increase in unsafe sex or sexual partners to 50% or more could substantially reduce the effect of interventions, but is unlikely to negate the prevention benefit completely,” the investigators added. “Pre-exposure prophylaxis could prevent a large number of new HIV infections if other key strategies, including HIV testing and treatment, are simultaneously expanded and improved. Without PrEP, HIV incidence in MSM in the UK is unlikely to decrease substantially by the end of this decade.”
The Health Protection Agency (now Public Health England), the Medical Research Council, and the Bill and Melinda Gates Foundation funded the work. The investigators had no disclosures.
Punyacharoensin and colleagues estimated that the greatest number of infections would be prevented in a practical combination prevention program that included pre-exposure prophylaxis alongside annual HIV testing for HIV-negative men and immediate treatment for HIV-positive men. In addition to promising findings from the PROUD study (Lancet. 2015 Sep 9. doi:10.1016/S0140-6736(15)00056-2), in which PrEP reduced the risk of HIV infection in MSM by 86%, the evidence is mounting for national policies in the UK and elsewhere that incorporate PrEP as a viable and accessible prevention strategy for MSM.
To maximize success, PrEP implementation needs to include the ability to engage with MSM communities and reach high-risk individuals, and should provide a point of access that is convenient and does not elicit fears of stigma, adherence counseling and monitoring for drug side-effects to ensure that individuals use PrEP effectively, and support for the uptake of complementary behavioral prevention strategies (e.g., reduced number of partners and condom use).
In addition, medical providers need guidance about how to manage patients receiving PrEP, and how drug and ancillary care costs should be covered. Finally, gay communities should be mobilized and educated about PrEP use and its use not only in prevention of HIV transmission but also in promotion of sexual health and well-being.
Dr. Emily A. Arnold and Dr. Wayne T. Steward are at the Center for AIDS Prevention Studies, University of California, San Francisco. They had no disclosures. These comments are based on their editorial (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00060-0).
Punyacharoensin and colleagues estimated that the greatest number of infections would be prevented in a practical combination prevention program that included pre-exposure prophylaxis alongside annual HIV testing for HIV-negative men and immediate treatment for HIV-positive men. In addition to promising findings from the PROUD study (Lancet. 2015 Sep 9. doi:10.1016/S0140-6736(15)00056-2), in which PrEP reduced the risk of HIV infection in MSM by 86%, the evidence is mounting for national policies in the UK and elsewhere that incorporate PrEP as a viable and accessible prevention strategy for MSM.
To maximize success, PrEP implementation needs to include the ability to engage with MSM communities and reach high-risk individuals, and should provide a point of access that is convenient and does not elicit fears of stigma, adherence counseling and monitoring for drug side-effects to ensure that individuals use PrEP effectively, and support for the uptake of complementary behavioral prevention strategies (e.g., reduced number of partners and condom use).
In addition, medical providers need guidance about how to manage patients receiving PrEP, and how drug and ancillary care costs should be covered. Finally, gay communities should be mobilized and educated about PrEP use and its use not only in prevention of HIV transmission but also in promotion of sexual health and well-being.
Dr. Emily A. Arnold and Dr. Wayne T. Steward are at the Center for AIDS Prevention Studies, University of California, San Francisco. They had no disclosures. These comments are based on their editorial (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00060-0).
Punyacharoensin and colleagues estimated that the greatest number of infections would be prevented in a practical combination prevention program that included pre-exposure prophylaxis alongside annual HIV testing for HIV-negative men and immediate treatment for HIV-positive men. In addition to promising findings from the PROUD study (Lancet. 2015 Sep 9. doi:10.1016/S0140-6736(15)00056-2), in which PrEP reduced the risk of HIV infection in MSM by 86%, the evidence is mounting for national policies in the UK and elsewhere that incorporate PrEP as a viable and accessible prevention strategy for MSM.
To maximize success, PrEP implementation needs to include the ability to engage with MSM communities and reach high-risk individuals, and should provide a point of access that is convenient and does not elicit fears of stigma, adherence counseling and monitoring for drug side-effects to ensure that individuals use PrEP effectively, and support for the uptake of complementary behavioral prevention strategies (e.g., reduced number of partners and condom use).
In addition, medical providers need guidance about how to manage patients receiving PrEP, and how drug and ancillary care costs should be covered. Finally, gay communities should be mobilized and educated about PrEP use and its use not only in prevention of HIV transmission but also in promotion of sexual health and well-being.
Dr. Emily A. Arnold and Dr. Wayne T. Steward are at the Center for AIDS Prevention Studies, University of California, San Francisco. They had no disclosures. These comments are based on their editorial (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00060-0).
Rates of HIV infection in the United Kingdom could drop by 44% this decade if just a quarter of high-risk men who have sex with men receive pre-exposure prophylaxis, regular HIV testing, and early treatment, according to investigators.
“Our findings show that PrEP can be highly effective against HIV transmission at the population level, and could outperform other interventions at the same level of program coverage,” reported Dr. Narat Punyacharoensin of the London School of Hygiene and Tropical Medicine and his associates. The study was published online Jan. 13 in The Lancet HIV.
The incidence of HIV infection in the United Kingdom rose slightly in 2014, and shows no signs of reversing course. Among 104,000 UK residents living with HIV, about 43% are MSM, the researchers noted. After fitting a mathematical model with surveillance and behavioral data, they estimated the effects of seven HIV interventions targeting MSM, including expanded testing, test-and-treat programs, antiretroviral PrEP, and measures to reduce sexual partners and unprotected anal intercourse (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00056-9).
If nothing is done, the UK can expect about 17,000 new HIV infections by 2020, the model showed. But offering just 25% of high-risk MSM PrEP along with regular HIV testing and early treatment would prevent 7,399 HIV infections by 2020 (interquartile range, 5,587-9,813), or about 44% of the total incidence (IQR, 33-58).
“An increase in unsafe sex or sexual partners to 50% or more could substantially reduce the effect of interventions, but is unlikely to negate the prevention benefit completely,” the investigators added. “Pre-exposure prophylaxis could prevent a large number of new HIV infections if other key strategies, including HIV testing and treatment, are simultaneously expanded and improved. Without PrEP, HIV incidence in MSM in the UK is unlikely to decrease substantially by the end of this decade.”
The Health Protection Agency (now Public Health England), the Medical Research Council, and the Bill and Melinda Gates Foundation funded the work. The investigators had no disclosures.
Rates of HIV infection in the United Kingdom could drop by 44% this decade if just a quarter of high-risk men who have sex with men receive pre-exposure prophylaxis, regular HIV testing, and early treatment, according to investigators.
“Our findings show that PrEP can be highly effective against HIV transmission at the population level, and could outperform other interventions at the same level of program coverage,” reported Dr. Narat Punyacharoensin of the London School of Hygiene and Tropical Medicine and his associates. The study was published online Jan. 13 in The Lancet HIV.
The incidence of HIV infection in the United Kingdom rose slightly in 2014, and shows no signs of reversing course. Among 104,000 UK residents living with HIV, about 43% are MSM, the researchers noted. After fitting a mathematical model with surveillance and behavioral data, they estimated the effects of seven HIV interventions targeting MSM, including expanded testing, test-and-treat programs, antiretroviral PrEP, and measures to reduce sexual partners and unprotected anal intercourse (Lancet HIV. 2016 Jan 13. doi:10.1016/S2352-3018[15]00056-9).
If nothing is done, the UK can expect about 17,000 new HIV infections by 2020, the model showed. But offering just 25% of high-risk MSM PrEP along with regular HIV testing and early treatment would prevent 7,399 HIV infections by 2020 (interquartile range, 5,587-9,813), or about 44% of the total incidence (IQR, 33-58).
“An increase in unsafe sex or sexual partners to 50% or more could substantially reduce the effect of interventions, but is unlikely to negate the prevention benefit completely,” the investigators added. “Pre-exposure prophylaxis could prevent a large number of new HIV infections if other key strategies, including HIV testing and treatment, are simultaneously expanded and improved. Without PrEP, HIV incidence in MSM in the UK is unlikely to decrease substantially by the end of this decade.”
The Health Protection Agency (now Public Health England), the Medical Research Council, and the Bill and Melinda Gates Foundation funded the work. The investigators had no disclosures.
Key clinical point: Pre-exposure prophylaxis with antiretroviral therapy could markedly reduce the incidence of HIV infection among men who have sex with men.
Major finding: Offering just 25% of high-risk MSM PrEP along with regular testing and early treatment would prevent about 7,400 HIV infections by 2020.
Data source: A mathematical model of seven HIV interventions implemented separately and together among MSM in the United Kingdom.
Disclosures: The Health Protection Agency (now Public Health England), the Medical Research Council, and the Bill and Melinda Gates Foundation funded the research. The investigators had no disclosures.
Proton Pump Inhibitors Linked to Chronic Kidney Disease
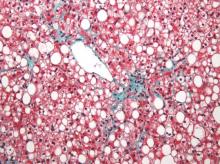
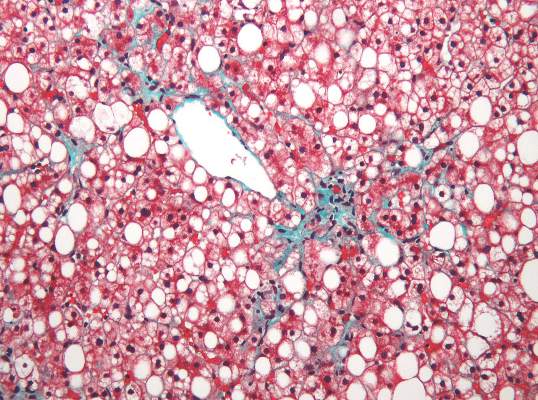
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
See below for "Views on the News," a pro/con discussion on PPIs.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
Pro: When used as indicated, PPIs are good medicine
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
See below for "Views on the News," a pro/con discussion on PPIs.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
Pro: When used as indicated, PPIs are good medicine
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
See below for "Views on the News," a pro/con discussion on PPIs.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
Pro: When used as indicated, PPIs are good medicine
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
FROM JAMA INTERNAL MEDICINE
Proton pump inhibitors linked to chronic kidney disease
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
Available evidence suggests that proton pump inhibitor use is associated with an increased risk of both acute and chronic kidney disease, hypomagnesemia, Clostridium difficile infection, and osteoporotic fractures. Caution in prescribing PPIs should be used in patients at high risk for any of these conditions. Given the association with kidney disease and low magnesium levels, serum creatinine and magnesium levels probably should be monitored in patients using PPIs, especially those using high doses.
Given the evidence that PPI use is linked with a number of adverse outcomes, we recommend that patients and clinicians discuss the potential benefits and risks of PPI treatment, as well as potential alternative regimens such as histamine H2 receptor antagonists or lifestyle changes, before PPIs are prescribed. In patients with symptomatic gastrointestinal reflux, ulcer disease, and severe dyspepsia, the benefits of PPI use likely outweigh its potential harms. For less serious symptoms, however, and for prevention of bleeding in low-risk patients, potential harms may outweigh the benefits. A large number of patients are taking PPIs for no clear reason – often remote symptoms of dyspepsia or heartburn that have since resolved. In these patients, PPIs should be stopped to determine if symptomatic treatment is needed.
Dr. Adam J. Schoenfeld and Dr. Deborah Grady are with the University of California, San Francisco. They had no disclosures. These comments were taken from their editorial (JAMA Intern Med. 2016 Jan 11. doi: 10.1001/jamainternmed.2015.7927).
The bottom line is that PPIs should be used continually for the three specific conditions for which they are known to be beneficial – hypersecretory states, gastroesophageal reflux disease (in all its manifestations), and NSAID/aspirin prophylaxis. As with all drugs, treatment always should be at the lowest effective dose. Although it is quite appropriate to limit chronic PPI use to these groups, given the potential association (no causality identified) with various putative side effects including renal disease, in my opinion, the risks of denying PPIs when indicated are higher than the low risks of renal or other possible side effects.
Dr. David C. Metz is associate chief for clinical affairs, GI division; codirector, esophagology and swallowing program; director, acid-peptic program; codirector, neuroendocrine tumor center; and professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia.
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
The use of proton pump inhibitors increased the risk of chronic kidney disease by 20%-50%, said the authors of two large population-based cohort analyses published online Jan. 11 in JAMA Internal Medicine.
These are the first such studies to link PPI use to chronic kidney disease (CKD), and the association held up after controlling for multiple potential confounders, said Dr. Benjamin Lazarus of Johns Hopkins University, Baltimore, and his associates. “Further research is required to investigate whether PPI use itself causes kidney damage and, if so, the underlying mechanisms of this association,” they wrote.
Proton pump inhibitors have been linked to other adverse health effects but remain among the most frequently prescribed medications in the United States. To further explore the risk of PPI use, the researchers analyzed data for 10,482 adults from the Atherosclerosis Risk in Communities (ARIC) study who were followed for a median of 13.9 years, and a replication cohort of 248,751 patients from a large rural health care system who were followed for a median of 6.2 years.
Incident CKD was defined based on hospital discharge diagnosis codes, reports of end-stage renal disease from the United States Renal Data System Registry, or a glomerular filtration rate of less than 60 mL/min per 1.73 m2 that persisted at follow-up visits (JAMA Intern Med. 2016 Jan 11. doi: 0.1001/jamainternmed.2015.7193).
In the ARIC study, there were 56 cases of CKD among 322 self-reported baseline PPI users, for an incidence of 14.2 cases per 1,000 person-years – significantly higher than the rate of 10.7 cases per 1,000 person-years among self-reported baseline nonusers. The 10-year estimated absolute risk of CKD among baseline users was 11.8% – 3.3% higher than the expected risk had they not used PPIs. Furthermore, PPI users were at significantly higher risk of CKD after demographic, socioeconomic, and clinical variables were accounted for (hazard ratio, 1.50; 95% confidence interval, 1.1-2.0), after modeling varying use of PPIs over time (adjusted HR, 1.3; 95% CI, 1.2-1.5), after directly comparing PPI users with H2 receptor antagonist users (adjusted HR, 1.4; 95% CI, 1.01-1.9), and after comparing baseline PPI users with propensity score–matched nonusers (HR, 1.8; 95% CI, 1.1-2.7).
In the replication cohort, there were 1,921 new cases of CKD among 16,900 patients with an outpatient PPI prescription (incidence of 20.1 cases per 1,000 person-years). The incidence of CKD among the other patients was lower: 18.3 cases per 1,000 person-years. The use of PPIs was significantly associated with incident CKD in all analyses, and the 10-year absolute risk of CKD among baseline PPI users was 15.6% – 1.7% higher than the expected risk had they not used PPIs.
These observational analyses cannot show causality, but a causal relationship between PPIs and CKD “could have a considerable public health impact, give the widespread extent of use,” the researchers emphasized. “More than 15 million Americans used prescription PPIs in 2013, costing more than $10 billion. Study findings suggest that up to 70% of these prescriptions are without indication and that 25% of long-term PPI users could discontinue therapy without developing symptoms. Indeed, there are already calls for the reduction of unnecessary use of PPIs (BMJ. 2008;336:2-3).”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: The use of proton pump inhibitors was significantly associated with incident chronic kidney disease (CKD) in two large population-based studies.
Major finding: Baseline PPI use was associated with a 20%-50% increase in the risk of CKD, and the association held up in all sensitivity analyses.
Data source: A prospective, population-based cohort study of 10,482 adults from the Atherosclerosis Risk in Communities study and a separate replication analysis of 248,751 patients from a large health care system.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute, both of which are part of the National Institutes of Health. The researchers had no disclosures.
Statins might prevent vascular inflammation in sleep apnea
Statins reduced complement-related vascular inflammation in patients with obstructive sleep apnea, according to research published online Jan. 6 in Science Translational Medicine.
The “unexpected” finding suggests that statins might offer a targeted therapy for the significant vascular manifestations of OSA, wrote Dr. Memet Emin and Dr. Gang Wang of Columbia University College of Physicians and Surgeons, New York, together with their associates. “Statins also have antioxidant effects, which may be particularly beneficial in conditions associated with oxidative stress, such as OSA,” the investigators added.
Obstructive sleep apnea affects one in four Western adults and triples the risk of cardiovascular diseases. The disorder is uniquely characterized by intermittent hypoxia, which the researchers hypothesized might lead to a distinct pattern of endothelial cell (EC) activation. To test this theory, they used a phage display peptide library to analyze protein expression in vascular ECs from 76 patients with OSA and 52 OSA-free controls. They also modeled intermittent hypoxia by exposing cultured ECs to alternating periods of normal and low (2%) oxygen levels (Sci Transl Med. 2016 Jan 6. doi: 10.1126/scitranslmed.aad0634).
Patients with OSA who were receiving statins had EC surface levels of the CD59 complement inhibitor similar to those of controls, and significantly greater levels compared with patients with OSA who were not receiving statins (P = .05). The CD59 protein is a major complement regulator that inhibits the formation of the terminal membrane attack complex, and thereby protects cells from complement-mediated injury, the researchers noted. In addition, intermittent hypoxia induced the internalization of CD59 in cultured ECs, leading to MAC deposition and endothelial inflammation, they said.
Most notably, patients with OSA who were taking statins had normal EC surface levels of CD59, and cultured ECs that were treated with atorvastatin were better protected from complement activity in a cholesterol-dependent manner, the investigators reported. By reducing cholesterol biosynthesis, statins might decrease the formation of cholesterol-enriched plasma membrane and CD59 endocytosis, which would reduce its internalization and preserve its ability to protect cells against complement activity, they said.
The National Heart, Lung, and Blood Institute of the National Institutes of Health funded the study. The investigators had no disclosures.
Statins reduced complement-related vascular inflammation in patients with obstructive sleep apnea, according to research published online Jan. 6 in Science Translational Medicine.
The “unexpected” finding suggests that statins might offer a targeted therapy for the significant vascular manifestations of OSA, wrote Dr. Memet Emin and Dr. Gang Wang of Columbia University College of Physicians and Surgeons, New York, together with their associates. “Statins also have antioxidant effects, which may be particularly beneficial in conditions associated with oxidative stress, such as OSA,” the investigators added.
Obstructive sleep apnea affects one in four Western adults and triples the risk of cardiovascular diseases. The disorder is uniquely characterized by intermittent hypoxia, which the researchers hypothesized might lead to a distinct pattern of endothelial cell (EC) activation. To test this theory, they used a phage display peptide library to analyze protein expression in vascular ECs from 76 patients with OSA and 52 OSA-free controls. They also modeled intermittent hypoxia by exposing cultured ECs to alternating periods of normal and low (2%) oxygen levels (Sci Transl Med. 2016 Jan 6. doi: 10.1126/scitranslmed.aad0634).
Patients with OSA who were receiving statins had EC surface levels of the CD59 complement inhibitor similar to those of controls, and significantly greater levels compared with patients with OSA who were not receiving statins (P = .05). The CD59 protein is a major complement regulator that inhibits the formation of the terminal membrane attack complex, and thereby protects cells from complement-mediated injury, the researchers noted. In addition, intermittent hypoxia induced the internalization of CD59 in cultured ECs, leading to MAC deposition and endothelial inflammation, they said.
Most notably, patients with OSA who were taking statins had normal EC surface levels of CD59, and cultured ECs that were treated with atorvastatin were better protected from complement activity in a cholesterol-dependent manner, the investigators reported. By reducing cholesterol biosynthesis, statins might decrease the formation of cholesterol-enriched plasma membrane and CD59 endocytosis, which would reduce its internalization and preserve its ability to protect cells against complement activity, they said.
The National Heart, Lung, and Blood Institute of the National Institutes of Health funded the study. The investigators had no disclosures.
Statins reduced complement-related vascular inflammation in patients with obstructive sleep apnea, according to research published online Jan. 6 in Science Translational Medicine.
The “unexpected” finding suggests that statins might offer a targeted therapy for the significant vascular manifestations of OSA, wrote Dr. Memet Emin and Dr. Gang Wang of Columbia University College of Physicians and Surgeons, New York, together with their associates. “Statins also have antioxidant effects, which may be particularly beneficial in conditions associated with oxidative stress, such as OSA,” the investigators added.
Obstructive sleep apnea affects one in four Western adults and triples the risk of cardiovascular diseases. The disorder is uniquely characterized by intermittent hypoxia, which the researchers hypothesized might lead to a distinct pattern of endothelial cell (EC) activation. To test this theory, they used a phage display peptide library to analyze protein expression in vascular ECs from 76 patients with OSA and 52 OSA-free controls. They also modeled intermittent hypoxia by exposing cultured ECs to alternating periods of normal and low (2%) oxygen levels (Sci Transl Med. 2016 Jan 6. doi: 10.1126/scitranslmed.aad0634).
Patients with OSA who were receiving statins had EC surface levels of the CD59 complement inhibitor similar to those of controls, and significantly greater levels compared with patients with OSA who were not receiving statins (P = .05). The CD59 protein is a major complement regulator that inhibits the formation of the terminal membrane attack complex, and thereby protects cells from complement-mediated injury, the researchers noted. In addition, intermittent hypoxia induced the internalization of CD59 in cultured ECs, leading to MAC deposition and endothelial inflammation, they said.
Most notably, patients with OSA who were taking statins had normal EC surface levels of CD59, and cultured ECs that were treated with atorvastatin were better protected from complement activity in a cholesterol-dependent manner, the investigators reported. By reducing cholesterol biosynthesis, statins might decrease the formation of cholesterol-enriched plasma membrane and CD59 endocytosis, which would reduce its internalization and preserve its ability to protect cells against complement activity, they said.
The National Heart, Lung, and Blood Institute of the National Institutes of Health funded the study. The investigators had no disclosures.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Statin therapy might help prevent endothelial inflammation in patients with obstructive sleep apnea.
Major finding: Patients with OSA who were receiving statins had vascular endothelial cell surface levels of the CD59 complement inhibitor similar to those of controls, and greater cell surface levels compared with patients with OSA who were not receiving statins (P = .05).
Data source: A peptide library study of vascular endothelial cells from 76 patients with OSA and 52 OSA-free controls, plus an in vitro study of cultured endothelial cells.
Disclosures: The National Heart, Lung, and Blood Institute of the National Institutes of Health funded the study. The investigators had no disclosures.
3D imaging tracks causes of post-TAVR aortic regurgitation
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
FROM JACC CARDIOVASCULAR IMAGING
Key clinical point: Three-dimensional transesophageal echocardiography identified significant predictors of aortic regurgitation after transcatheter aortic valve replacement.
Major finding: Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape (P less than .01), and malpositioning of the prosthetic commissures (P less than .001) compared with patients without transvalvular AR.
Data source: A 3D TEE study of 201 patients with severe aortic stenosis who underwent TAVR with the Edwards SAPIEN device.
Disclosures: The investigators reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
Nonalcoholic fatty liver disease will keep rising ‘in near term’
Nonalcoholic fatty liver disease (NAFLD) almost tripled among United States veterans in a recent 9-year period, investigators reported in the February issue of Clinical Gastroenterology and Hepatology.
The trend “was evident in all racial groups, across all age groups, and in both genders,” said Dr. Fasiha Kanwal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, both in Houston, and her associates. The increasing prevalence of NAFLD “is likely generalizable to nonveterans,” and will probably persist because of a “fairly steady” 2%-3% overall annual incidence and a steeper rise among younger individuals, they added. “Nonalcoholic fatty liver disease will continue to remain a major public health problem in the United States, at least in the near and intermediate future.”
Although NAFLD is the leading cause of chronic liver failure in the United States, few studies have examined its incidence or prevalence over time, which are key to predicting future disease burden. Therefore, the investigators analyzed data for more than 9.78 million patients who visited the VA at least once between 2003 and 2011. They defined NAFLD as at least two elevated alanine aminotransferase (ALT) values (greater than 40 IU/mL) separated by at least 6 months, with no history of positive serology for hepatitis B surface antigen or hepatitis C virus RNA, and no alcohol-related ICD-9 codes or positive AUDIT-C scores within a year of elevated ALT levels (Clin Gastroenterol Hepatol. 2015 Aug 7. doi: 10.1016/j.cgh.2015.08.010).
During the study period, more than 1.3 million patients, or 13.6%, met the definition of NAFLD, said the researchers. Age-adjusted incidence rates dropped slightly from 3.16% in 2003 to 2.5% in 2011, ranging between 2.3% and 2.7% in most years. Prevalence, however, rose from 6.3% in 2003 (95% confidence interval, 6.26%-6.3%) to 17.6% in 2011 (95% CI, 17.58%-17.65%), a 2.8-fold increase. Moreover, about one in five patients with NAFLD who visited the VA in 2011 was at risk for advanced fibrosis.
Among individuals who were younger than 45 years, the incidence of NAFLD rose from 2.3 to 4.3 cases per 100 persons (annual percentage change, 7.4%; 95% CI, 5.7% to 9.2%), the researchers also found. “Although recent studies show that the rate of increase in both obesity and diabetes, which are both major risk factors for NAFLD, may be slowing down in the U.S., this may not be the case in the VA, where the prevalence of obesity and diabetes is in fact higher than in the U.S. population,” they said.
In general, the findings mirror a recent analysis of the National Health and Nutrition Examination Survey (Aliment Pharmacol Ther. 2015 Jan;41[1]:65-76), according to the investigators. “The VA is the largest integrated health care system in the United States,” they added. “We believe that the sheer size of the veteran cohort, combined with a complete dearth of information regarding the burden of NAFLD in the VA, renders our findings highly significant. Furthermore, the VA is in a unique position to test and implement systemic changes in medical care delivery to improve the health care of NAFLD patients.”
The study was partially supported by the Michael E. DeBakey Veterans Affairs Medical Center. The researchers had no disclosures.
Kanwal and colleagues present an interesting study assessing the trends in the incidence and prevalence of NAFLD in the United States. Findings suggest that the annual incidence of NAFLD has generally been stable (2.2%-3.2%), while the prevalence of NAFLD has increased by 2.8-fold (6.3%-17.6%). These findings are consistent with the literature and provide additional evidence supporting the increasing burden of NAFLD. Although an important study, there are some limitations to the study design. First, the diagnosis of NAFLD was solely based on elevated liver enzymes, which can underestimate the true incidence and prevalence of NAFLD. In fact, in a recent meta-analysis, NAFLD prevalence based on liver enzymes was 13%, while NAFLD prevalence based on radiologic diagnosis was 25% (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Second, the study subjects came from the VA system, which may not be representative of the U.S. population (Patrick AFB, FL: Defense Equal Opportunity Management Institute, 2010). This is important because sex-specific differences in the prevalence of NAFLD have been reported (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Nevertheless, these limitations do not minimize the important contribution of this study. There appears to be an alarming increase in the burden of NAFLD within all the racial and age groups in the U.S. Further, this increase in the incidence and prevalence of NAFLD is especially significant among the younger age groups (less than 45 years). This finding is in contrast to others who have reported a higher prevalence in older subjects (Presented at AASLD 2015. San Francisco. Abstract #534). If confirmed, this younger cohort of patients with NAFLD can fuel the future burden of liver disease for the next few decades (JAMA. 2012;307:491-7). Given the current lack of an effective treatment for NAFLD, a national strategy to deal with this important and rising cause of chronic liver disease is urgently needed.
Dr. Zobair M. Younossi, MPH, FACG, AGAF, FAASLD, is chairman, department of medicine, Inova Fairfax Hospital; vice president for research, Inova Health System; professor of medicine, VCU-Inova Campus and Beatty Center for Integrated Research, Falls Church, Va. He has consulted for Gilead, AbbVie, Intercept, BMS, and GSK.
Kanwal and colleagues present an interesting study assessing the trends in the incidence and prevalence of NAFLD in the United States. Findings suggest that the annual incidence of NAFLD has generally been stable (2.2%-3.2%), while the prevalence of NAFLD has increased by 2.8-fold (6.3%-17.6%). These findings are consistent with the literature and provide additional evidence supporting the increasing burden of NAFLD. Although an important study, there are some limitations to the study design. First, the diagnosis of NAFLD was solely based on elevated liver enzymes, which can underestimate the true incidence and prevalence of NAFLD. In fact, in a recent meta-analysis, NAFLD prevalence based on liver enzymes was 13%, while NAFLD prevalence based on radiologic diagnosis was 25% (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Second, the study subjects came from the VA system, which may not be representative of the U.S. population (Patrick AFB, FL: Defense Equal Opportunity Management Institute, 2010). This is important because sex-specific differences in the prevalence of NAFLD have been reported (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Nevertheless, these limitations do not minimize the important contribution of this study. There appears to be an alarming increase in the burden of NAFLD within all the racial and age groups in the U.S. Further, this increase in the incidence and prevalence of NAFLD is especially significant among the younger age groups (less than 45 years). This finding is in contrast to others who have reported a higher prevalence in older subjects (Presented at AASLD 2015. San Francisco. Abstract #534). If confirmed, this younger cohort of patients with NAFLD can fuel the future burden of liver disease for the next few decades (JAMA. 2012;307:491-7). Given the current lack of an effective treatment for NAFLD, a national strategy to deal with this important and rising cause of chronic liver disease is urgently needed.
Dr. Zobair M. Younossi, MPH, FACG, AGAF, FAASLD, is chairman, department of medicine, Inova Fairfax Hospital; vice president for research, Inova Health System; professor of medicine, VCU-Inova Campus and Beatty Center for Integrated Research, Falls Church, Va. He has consulted for Gilead, AbbVie, Intercept, BMS, and GSK.
Kanwal and colleagues present an interesting study assessing the trends in the incidence and prevalence of NAFLD in the United States. Findings suggest that the annual incidence of NAFLD has generally been stable (2.2%-3.2%), while the prevalence of NAFLD has increased by 2.8-fold (6.3%-17.6%). These findings are consistent with the literature and provide additional evidence supporting the increasing burden of NAFLD. Although an important study, there are some limitations to the study design. First, the diagnosis of NAFLD was solely based on elevated liver enzymes, which can underestimate the true incidence and prevalence of NAFLD. In fact, in a recent meta-analysis, NAFLD prevalence based on liver enzymes was 13%, while NAFLD prevalence based on radiologic diagnosis was 25% (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Second, the study subjects came from the VA system, which may not be representative of the U.S. population (Patrick AFB, FL: Defense Equal Opportunity Management Institute, 2010). This is important because sex-specific differences in the prevalence of NAFLD have been reported (Hepatology. 2015 Dec 28. doi: 10.1002/hep.28431. [Epub ahead of print]). Nevertheless, these limitations do not minimize the important contribution of this study. There appears to be an alarming increase in the burden of NAFLD within all the racial and age groups in the U.S. Further, this increase in the incidence and prevalence of NAFLD is especially significant among the younger age groups (less than 45 years). This finding is in contrast to others who have reported a higher prevalence in older subjects (Presented at AASLD 2015. San Francisco. Abstract #534). If confirmed, this younger cohort of patients with NAFLD can fuel the future burden of liver disease for the next few decades (JAMA. 2012;307:491-7). Given the current lack of an effective treatment for NAFLD, a national strategy to deal with this important and rising cause of chronic liver disease is urgently needed.
Dr. Zobair M. Younossi, MPH, FACG, AGAF, FAASLD, is chairman, department of medicine, Inova Fairfax Hospital; vice president for research, Inova Health System; professor of medicine, VCU-Inova Campus and Beatty Center for Integrated Research, Falls Church, Va. He has consulted for Gilead, AbbVie, Intercept, BMS, and GSK.
Nonalcoholic fatty liver disease (NAFLD) almost tripled among United States veterans in a recent 9-year period, investigators reported in the February issue of Clinical Gastroenterology and Hepatology.
The trend “was evident in all racial groups, across all age groups, and in both genders,” said Dr. Fasiha Kanwal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, both in Houston, and her associates. The increasing prevalence of NAFLD “is likely generalizable to nonveterans,” and will probably persist because of a “fairly steady” 2%-3% overall annual incidence and a steeper rise among younger individuals, they added. “Nonalcoholic fatty liver disease will continue to remain a major public health problem in the United States, at least in the near and intermediate future.”
Although NAFLD is the leading cause of chronic liver failure in the United States, few studies have examined its incidence or prevalence over time, which are key to predicting future disease burden. Therefore, the investigators analyzed data for more than 9.78 million patients who visited the VA at least once between 2003 and 2011. They defined NAFLD as at least two elevated alanine aminotransferase (ALT) values (greater than 40 IU/mL) separated by at least 6 months, with no history of positive serology for hepatitis B surface antigen or hepatitis C virus RNA, and no alcohol-related ICD-9 codes or positive AUDIT-C scores within a year of elevated ALT levels (Clin Gastroenterol Hepatol. 2015 Aug 7. doi: 10.1016/j.cgh.2015.08.010).
During the study period, more than 1.3 million patients, or 13.6%, met the definition of NAFLD, said the researchers. Age-adjusted incidence rates dropped slightly from 3.16% in 2003 to 2.5% in 2011, ranging between 2.3% and 2.7% in most years. Prevalence, however, rose from 6.3% in 2003 (95% confidence interval, 6.26%-6.3%) to 17.6% in 2011 (95% CI, 17.58%-17.65%), a 2.8-fold increase. Moreover, about one in five patients with NAFLD who visited the VA in 2011 was at risk for advanced fibrosis.
Among individuals who were younger than 45 years, the incidence of NAFLD rose from 2.3 to 4.3 cases per 100 persons (annual percentage change, 7.4%; 95% CI, 5.7% to 9.2%), the researchers also found. “Although recent studies show that the rate of increase in both obesity and diabetes, which are both major risk factors for NAFLD, may be slowing down in the U.S., this may not be the case in the VA, where the prevalence of obesity and diabetes is in fact higher than in the U.S. population,” they said.
In general, the findings mirror a recent analysis of the National Health and Nutrition Examination Survey (Aliment Pharmacol Ther. 2015 Jan;41[1]:65-76), according to the investigators. “The VA is the largest integrated health care system in the United States,” they added. “We believe that the sheer size of the veteran cohort, combined with a complete dearth of information regarding the burden of NAFLD in the VA, renders our findings highly significant. Furthermore, the VA is in a unique position to test and implement systemic changes in medical care delivery to improve the health care of NAFLD patients.”
The study was partially supported by the Michael E. DeBakey Veterans Affairs Medical Center. The researchers had no disclosures.
Nonalcoholic fatty liver disease (NAFLD) almost tripled among United States veterans in a recent 9-year period, investigators reported in the February issue of Clinical Gastroenterology and Hepatology.
The trend “was evident in all racial groups, across all age groups, and in both genders,” said Dr. Fasiha Kanwal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, both in Houston, and her associates. The increasing prevalence of NAFLD “is likely generalizable to nonveterans,” and will probably persist because of a “fairly steady” 2%-3% overall annual incidence and a steeper rise among younger individuals, they added. “Nonalcoholic fatty liver disease will continue to remain a major public health problem in the United States, at least in the near and intermediate future.”
Although NAFLD is the leading cause of chronic liver failure in the United States, few studies have examined its incidence or prevalence over time, which are key to predicting future disease burden. Therefore, the investigators analyzed data for more than 9.78 million patients who visited the VA at least once between 2003 and 2011. They defined NAFLD as at least two elevated alanine aminotransferase (ALT) values (greater than 40 IU/mL) separated by at least 6 months, with no history of positive serology for hepatitis B surface antigen or hepatitis C virus RNA, and no alcohol-related ICD-9 codes or positive AUDIT-C scores within a year of elevated ALT levels (Clin Gastroenterol Hepatol. 2015 Aug 7. doi: 10.1016/j.cgh.2015.08.010).
During the study period, more than 1.3 million patients, or 13.6%, met the definition of NAFLD, said the researchers. Age-adjusted incidence rates dropped slightly from 3.16% in 2003 to 2.5% in 2011, ranging between 2.3% and 2.7% in most years. Prevalence, however, rose from 6.3% in 2003 (95% confidence interval, 6.26%-6.3%) to 17.6% in 2011 (95% CI, 17.58%-17.65%), a 2.8-fold increase. Moreover, about one in five patients with NAFLD who visited the VA in 2011 was at risk for advanced fibrosis.
Among individuals who were younger than 45 years, the incidence of NAFLD rose from 2.3 to 4.3 cases per 100 persons (annual percentage change, 7.4%; 95% CI, 5.7% to 9.2%), the researchers also found. “Although recent studies show that the rate of increase in both obesity and diabetes, which are both major risk factors for NAFLD, may be slowing down in the U.S., this may not be the case in the VA, where the prevalence of obesity and diabetes is in fact higher than in the U.S. population,” they said.
In general, the findings mirror a recent analysis of the National Health and Nutrition Examination Survey (Aliment Pharmacol Ther. 2015 Jan;41[1]:65-76), according to the investigators. “The VA is the largest integrated health care system in the United States,” they added. “We believe that the sheer size of the veteran cohort, combined with a complete dearth of information regarding the burden of NAFLD in the VA, renders our findings highly significant. Furthermore, the VA is in a unique position to test and implement systemic changes in medical care delivery to improve the health care of NAFLD patients.”
The study was partially supported by the Michael E. DeBakey Veterans Affairs Medical Center. The researchers had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The prevalence of nonalcoholic fatty liver disease has risen substantially since 2003, and will probably keep increasing in the near term.
Major finding: Prevalence among veterans rose about 2.8 times between 2003 and 2011, mirroring trends reported in the general population.
Data source: An analysis of data from 9.78 million Veterans Affairs patients.
Disclosures: The study was partially supported by the Michael E. DeBakey Veterans Affairs Medical Center. The researchers had no disclosures.
Hepatitis C virus infection linked to cardiovascular death, disease, and stroke
Patients with hepatitis C virus (HCV) infection face a significantly increased risk of cardiovascular death, subclinical carotid thickening and atherosclerosis, and cerebrocardiovascular events, especially when they also have diabetes and hypertension, according to a systematic review and meta-analysis of 22 studies published in the January issue of Gastroenterology.
“To our knowledge, our meta-analysis clearly highlights, for the first time, that HCV infection increases the risk of cardiovascular disease-related mortality,” wrote Dr. Salvatore Petta and his associates at the University of Palermo, Italy. “We [also] found a twofold higher risk of subclinical carotid plaques among HCV-infected individuals compared to uninfected controls, without significant heterogeneity among studies, as well as an increased risk of carotid thickening. We observed a slightly significant increase in cerebrocardiovascular events among HCV-infected patients, despite the high heterogeneity among studies that was mostly related to the prevalence of diabetes mellitus and hypertension.”
A number of observational studies have reported cardiovascular outcomes in HCV-infected patients, but results have been “ambiguous,” Dr. Petta and his colleagues said. For their meta-analysis, they searched PubMed, Medline, EMBASE, the Cochrane Library, and reference lists of articles to identify studies published through July 2015 that either compared cardiovascular disease between HCV-infected and uninfected patients, or evaluated the prevalence of HCV infection among patients with cardiovascular disease. This literature search identified 12 case-control studies and 10 cohort studies. Outcome measures included carotid atherosclerosis (nine studies), intima media thickness (eight studies), coronary artery disease (seven studies), stroke (six studies), and cardiovascular mortality (three studies) (Gastroenterology. 2015 Sep 18. doi: 10.1053/j.gastro.2015.09.00).In the pooled analysis, the odds of cardiovascular death were 65% higher in HCV-infected patients, compared with uninfected individuals (95% confidence interval for this increase, 1.07%-2.56%). Compared with controls, HCV-infected patients also were at higher risk of carotid plaques (odds ratio, 2.27; 95% CI, 1.76-2.94), especially when they were smokers (P = .02). HCV infection also significantly increased the odds of carotid artery intima-media thickening (OR, 1.20; 95% CI, 1.03-1.40), and cerebrocardiovascular events (OR, 1.30; 95% CI, 1.10-1.55). However, subgroup analyses showed that HCV infection only increased the likelihood of cerebrocardiovascular events in populations with a more than 10% prevalence of diabetes or a more than 20% prevalence of hypertension (OR, 1.71; P less than .001 for both subgroup analyses).
Because the studies of cerebrocardiovascular events were heterogeneous, the researchers also stratified them by study design and by the average age of patients. Pooled odds ratios for the link between HCV infection and cerebrocardiovascular events remained significant at 1.21 for the cohort studies, 2.01 for the case-control studies, 2.46 among patients who averaged more than 50 years of age, and 1.35 among younger patients.
The Egger test for publication bias showed that the literature search was unlikely to have overlooked studies in terms of any of the outcome measures, the investigators noted. “From a clinical standpoint, the results of our meta-analysis suggest that HCV infection increases cardiovascular risk, particularly for individuals who already have cardiovascular risk factors, such as diabetes and hypertension,” they concluded. “Although effective and safe oral antiviral regimens are available, more information is needed to confirm whether anti-HCV medications will decrease cardiovascular risk, as suggested in some studies.”
The researchers reported having no funding sources or conflicts of interest.
Source: American Gastroenterological Association
Patients with hepatitis C virus (HCV) infection face a significantly increased risk of cardiovascular death, subclinical carotid thickening and atherosclerosis, and cerebrocardiovascular events, especially when they also have diabetes and hypertension, according to a systematic review and meta-analysis of 22 studies published in the January issue of Gastroenterology.
“To our knowledge, our meta-analysis clearly highlights, for the first time, that HCV infection increases the risk of cardiovascular disease-related mortality,” wrote Dr. Salvatore Petta and his associates at the University of Palermo, Italy. “We [also] found a twofold higher risk of subclinical carotid plaques among HCV-infected individuals compared to uninfected controls, without significant heterogeneity among studies, as well as an increased risk of carotid thickening. We observed a slightly significant increase in cerebrocardiovascular events among HCV-infected patients, despite the high heterogeneity among studies that was mostly related to the prevalence of diabetes mellitus and hypertension.”
A number of observational studies have reported cardiovascular outcomes in HCV-infected patients, but results have been “ambiguous,” Dr. Petta and his colleagues said. For their meta-analysis, they searched PubMed, Medline, EMBASE, the Cochrane Library, and reference lists of articles to identify studies published through July 2015 that either compared cardiovascular disease between HCV-infected and uninfected patients, or evaluated the prevalence of HCV infection among patients with cardiovascular disease. This literature search identified 12 case-control studies and 10 cohort studies. Outcome measures included carotid atherosclerosis (nine studies), intima media thickness (eight studies), coronary artery disease (seven studies), stroke (six studies), and cardiovascular mortality (three studies) (Gastroenterology. 2015 Sep 18. doi: 10.1053/j.gastro.2015.09.00).In the pooled analysis, the odds of cardiovascular death were 65% higher in HCV-infected patients, compared with uninfected individuals (95% confidence interval for this increase, 1.07%-2.56%). Compared with controls, HCV-infected patients also were at higher risk of carotid plaques (odds ratio, 2.27; 95% CI, 1.76-2.94), especially when they were smokers (P = .02). HCV infection also significantly increased the odds of carotid artery intima-media thickening (OR, 1.20; 95% CI, 1.03-1.40), and cerebrocardiovascular events (OR, 1.30; 95% CI, 1.10-1.55). However, subgroup analyses showed that HCV infection only increased the likelihood of cerebrocardiovascular events in populations with a more than 10% prevalence of diabetes or a more than 20% prevalence of hypertension (OR, 1.71; P less than .001 for both subgroup analyses).
Because the studies of cerebrocardiovascular events were heterogeneous, the researchers also stratified them by study design and by the average age of patients. Pooled odds ratios for the link between HCV infection and cerebrocardiovascular events remained significant at 1.21 for the cohort studies, 2.01 for the case-control studies, 2.46 among patients who averaged more than 50 years of age, and 1.35 among younger patients.
The Egger test for publication bias showed that the literature search was unlikely to have overlooked studies in terms of any of the outcome measures, the investigators noted. “From a clinical standpoint, the results of our meta-analysis suggest that HCV infection increases cardiovascular risk, particularly for individuals who already have cardiovascular risk factors, such as diabetes and hypertension,” they concluded. “Although effective and safe oral antiviral regimens are available, more information is needed to confirm whether anti-HCV medications will decrease cardiovascular risk, as suggested in some studies.”
The researchers reported having no funding sources or conflicts of interest.
Source: American Gastroenterological Association
Patients with hepatitis C virus (HCV) infection face a significantly increased risk of cardiovascular death, subclinical carotid thickening and atherosclerosis, and cerebrocardiovascular events, especially when they also have diabetes and hypertension, according to a systematic review and meta-analysis of 22 studies published in the January issue of Gastroenterology.
“To our knowledge, our meta-analysis clearly highlights, for the first time, that HCV infection increases the risk of cardiovascular disease-related mortality,” wrote Dr. Salvatore Petta and his associates at the University of Palermo, Italy. “We [also] found a twofold higher risk of subclinical carotid plaques among HCV-infected individuals compared to uninfected controls, without significant heterogeneity among studies, as well as an increased risk of carotid thickening. We observed a slightly significant increase in cerebrocardiovascular events among HCV-infected patients, despite the high heterogeneity among studies that was mostly related to the prevalence of diabetes mellitus and hypertension.”
A number of observational studies have reported cardiovascular outcomes in HCV-infected patients, but results have been “ambiguous,” Dr. Petta and his colleagues said. For their meta-analysis, they searched PubMed, Medline, EMBASE, the Cochrane Library, and reference lists of articles to identify studies published through July 2015 that either compared cardiovascular disease between HCV-infected and uninfected patients, or evaluated the prevalence of HCV infection among patients with cardiovascular disease. This literature search identified 12 case-control studies and 10 cohort studies. Outcome measures included carotid atherosclerosis (nine studies), intima media thickness (eight studies), coronary artery disease (seven studies), stroke (six studies), and cardiovascular mortality (three studies) (Gastroenterology. 2015 Sep 18. doi: 10.1053/j.gastro.2015.09.00).In the pooled analysis, the odds of cardiovascular death were 65% higher in HCV-infected patients, compared with uninfected individuals (95% confidence interval for this increase, 1.07%-2.56%). Compared with controls, HCV-infected patients also were at higher risk of carotid plaques (odds ratio, 2.27; 95% CI, 1.76-2.94), especially when they were smokers (P = .02). HCV infection also significantly increased the odds of carotid artery intima-media thickening (OR, 1.20; 95% CI, 1.03-1.40), and cerebrocardiovascular events (OR, 1.30; 95% CI, 1.10-1.55). However, subgroup analyses showed that HCV infection only increased the likelihood of cerebrocardiovascular events in populations with a more than 10% prevalence of diabetes or a more than 20% prevalence of hypertension (OR, 1.71; P less than .001 for both subgroup analyses).
Because the studies of cerebrocardiovascular events were heterogeneous, the researchers also stratified them by study design and by the average age of patients. Pooled odds ratios for the link between HCV infection and cerebrocardiovascular events remained significant at 1.21 for the cohort studies, 2.01 for the case-control studies, 2.46 among patients who averaged more than 50 years of age, and 1.35 among younger patients.
The Egger test for publication bias showed that the literature search was unlikely to have overlooked studies in terms of any of the outcome measures, the investigators noted. “From a clinical standpoint, the results of our meta-analysis suggest that HCV infection increases cardiovascular risk, particularly for individuals who already have cardiovascular risk factors, such as diabetes and hypertension,” they concluded. “Although effective and safe oral antiviral regimens are available, more information is needed to confirm whether anti-HCV medications will decrease cardiovascular risk, as suggested in some studies.”
The researchers reported having no funding sources or conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Patients with HCV infection are at increased risk of cardiovascular death, stroke, and subclinical carotid atherosclerosis and thickening.
Major finding: The pooled odds of cardiovascular death were 65% higher among infected, compared with uninfected individuals.
Data source: A systematic review and meta-analysis of 22 observational studies.
Disclosures: The researchers reported having no funding sources or conflicts of interest.
Nonalcoholic fatty liver disease linked to liver cancer without cirrhosis
About 13% of U.S. veterans with hepatocellular carcinoma had no evidence of preexisting cirrhosis, according to a report published in the January issue of Clinical Gastroenterology and Hepatology.
“The main risk factors for this entity were nonalcoholic fatty liver disease [NAFLD] or metabolic syndrome” – not hepatitis C virus infection [HCV], HBV [hepatitis B virus] infection, or alcohol abuse, said Dr. Sahil Mittal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine in Houston. Screening all patients with NAFLD for hepatocellular carcinoma [HCC] is impractical, so studies should seek “actionable risk factors” or biomarkers that reliably identify NAFLD patients who are at particular risk of HCC, wrote Dr. Mittal and his coinvestigators.
Researchers have debated whether chronic HCV infection or alcohol abuse can lead to HCC in the absence of cirrhosis, while at least one study has shown that NAFLD can predispose patients to this disease entity (Arch Pathol Lab Med. 2008;132:1761-6).
But few studies have systematically examined risk factors for HCC without cirrhosis in the general population, the investigators said. Therefore, they randomly selected 1,500 patients from the U.S. Veterans Affairs system who were diagnosed with HCC between 2005 and 2010 on the basis of histopathology or established imaging criteria (Hepatology 2005;42:1208-36).
They reviewed complete medical records for these patients, and classified those who did not have cirrhosis according to the quality of supporting histology, laboratory, and imaging data (Clin Gastroenterol Hepatol. 2015. doi: 0.1016/j.cgh.2015.07.019).
In all, 3% of the cohort had level 1 (“highest-quality”) evidence for not having cirrhosis, while another 10% had level 2 evidence for no cirrhosis, the investigators said. “Compared with HCC in the presence of cirrhosis, these patients were more likely to have metabolic syndrome or NAFLD or no identifiable risk factor, and less likely to have alcohol abuse or HCV infection,” they added. Only two-thirds of NAFLD patients with HCC had cirrhosis, compared with 91% of patients with chronic HCV infection, 92% of HCV-infected patients, and 88% of patients with an alcohol use disorder. Notably, the odds of HCC in the absence of cirrhosis were more than five times higher when patients had NAFLD (odds ratio [OR], 5.4; 95% confidence interval [CI], 3.4-8.5) or metabolic syndrome (OR, 5.0; 95% CI, 3.1-7.8) compared with HCV infection.
Patients with cirrhosis often go unscreened for HCC even though they are at greatest risk of this cancer. Therefore, trying to screen all patients with NAFLD for HCC would be “logistically impractical,” particularly when the absolute risk of HCC in noncirrhotic patients is unknown and no one has examined the best ways to screen this population, the investigators said. Instead, clinicians could prioritize screening and treating NAFLD patients for diabetes mellitus and obesity, both of which are associated with HCC. “There is evidence to suggest that metformin reduces the risk of HCC among diabetics,” they added. “Studies of these and other risk factors of HCC among NAFLD patients with and without cirrhosis are needed.”
Most patients in the study were male, potentially limiting the generalizability of the findings, the researchers noted.
The National Cancer Institute, the Houston Veterans Affairs Health Services Research and Development Center of Excellence, the Michael E. DeBakey Veterans Affairs Medical Center, and the Dan Duncan Cancer Center funded the study. The researchers had no disclosures.
Source: American Gastroenterological Association
About 13% of U.S. veterans with hepatocellular carcinoma had no evidence of preexisting cirrhosis, according to a report published in the January issue of Clinical Gastroenterology and Hepatology.
“The main risk factors for this entity were nonalcoholic fatty liver disease [NAFLD] or metabolic syndrome” – not hepatitis C virus infection [HCV], HBV [hepatitis B virus] infection, or alcohol abuse, said Dr. Sahil Mittal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine in Houston. Screening all patients with NAFLD for hepatocellular carcinoma [HCC] is impractical, so studies should seek “actionable risk factors” or biomarkers that reliably identify NAFLD patients who are at particular risk of HCC, wrote Dr. Mittal and his coinvestigators.
Researchers have debated whether chronic HCV infection or alcohol abuse can lead to HCC in the absence of cirrhosis, while at least one study has shown that NAFLD can predispose patients to this disease entity (Arch Pathol Lab Med. 2008;132:1761-6).
But few studies have systematically examined risk factors for HCC without cirrhosis in the general population, the investigators said. Therefore, they randomly selected 1,500 patients from the U.S. Veterans Affairs system who were diagnosed with HCC between 2005 and 2010 on the basis of histopathology or established imaging criteria (Hepatology 2005;42:1208-36).
They reviewed complete medical records for these patients, and classified those who did not have cirrhosis according to the quality of supporting histology, laboratory, and imaging data (Clin Gastroenterol Hepatol. 2015. doi: 0.1016/j.cgh.2015.07.019).
In all, 3% of the cohort had level 1 (“highest-quality”) evidence for not having cirrhosis, while another 10% had level 2 evidence for no cirrhosis, the investigators said. “Compared with HCC in the presence of cirrhosis, these patients were more likely to have metabolic syndrome or NAFLD or no identifiable risk factor, and less likely to have alcohol abuse or HCV infection,” they added. Only two-thirds of NAFLD patients with HCC had cirrhosis, compared with 91% of patients with chronic HCV infection, 92% of HCV-infected patients, and 88% of patients with an alcohol use disorder. Notably, the odds of HCC in the absence of cirrhosis were more than five times higher when patients had NAFLD (odds ratio [OR], 5.4; 95% confidence interval [CI], 3.4-8.5) or metabolic syndrome (OR, 5.0; 95% CI, 3.1-7.8) compared with HCV infection.
Patients with cirrhosis often go unscreened for HCC even though they are at greatest risk of this cancer. Therefore, trying to screen all patients with NAFLD for HCC would be “logistically impractical,” particularly when the absolute risk of HCC in noncirrhotic patients is unknown and no one has examined the best ways to screen this population, the investigators said. Instead, clinicians could prioritize screening and treating NAFLD patients for diabetes mellitus and obesity, both of which are associated with HCC. “There is evidence to suggest that metformin reduces the risk of HCC among diabetics,” they added. “Studies of these and other risk factors of HCC among NAFLD patients with and without cirrhosis are needed.”
Most patients in the study were male, potentially limiting the generalizability of the findings, the researchers noted.
The National Cancer Institute, the Houston Veterans Affairs Health Services Research and Development Center of Excellence, the Michael E. DeBakey Veterans Affairs Medical Center, and the Dan Duncan Cancer Center funded the study. The researchers had no disclosures.
Source: American Gastroenterological Association
About 13% of U.S. veterans with hepatocellular carcinoma had no evidence of preexisting cirrhosis, according to a report published in the January issue of Clinical Gastroenterology and Hepatology.
“The main risk factors for this entity were nonalcoholic fatty liver disease [NAFLD] or metabolic syndrome” – not hepatitis C virus infection [HCV], HBV [hepatitis B virus] infection, or alcohol abuse, said Dr. Sahil Mittal of the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine in Houston. Screening all patients with NAFLD for hepatocellular carcinoma [HCC] is impractical, so studies should seek “actionable risk factors” or biomarkers that reliably identify NAFLD patients who are at particular risk of HCC, wrote Dr. Mittal and his coinvestigators.
Researchers have debated whether chronic HCV infection or alcohol abuse can lead to HCC in the absence of cirrhosis, while at least one study has shown that NAFLD can predispose patients to this disease entity (Arch Pathol Lab Med. 2008;132:1761-6).
But few studies have systematically examined risk factors for HCC without cirrhosis in the general population, the investigators said. Therefore, they randomly selected 1,500 patients from the U.S. Veterans Affairs system who were diagnosed with HCC between 2005 and 2010 on the basis of histopathology or established imaging criteria (Hepatology 2005;42:1208-36).
They reviewed complete medical records for these patients, and classified those who did not have cirrhosis according to the quality of supporting histology, laboratory, and imaging data (Clin Gastroenterol Hepatol. 2015. doi: 0.1016/j.cgh.2015.07.019).
In all, 3% of the cohort had level 1 (“highest-quality”) evidence for not having cirrhosis, while another 10% had level 2 evidence for no cirrhosis, the investigators said. “Compared with HCC in the presence of cirrhosis, these patients were more likely to have metabolic syndrome or NAFLD or no identifiable risk factor, and less likely to have alcohol abuse or HCV infection,” they added. Only two-thirds of NAFLD patients with HCC had cirrhosis, compared with 91% of patients with chronic HCV infection, 92% of HCV-infected patients, and 88% of patients with an alcohol use disorder. Notably, the odds of HCC in the absence of cirrhosis were more than five times higher when patients had NAFLD (odds ratio [OR], 5.4; 95% confidence interval [CI], 3.4-8.5) or metabolic syndrome (OR, 5.0; 95% CI, 3.1-7.8) compared with HCV infection.
Patients with cirrhosis often go unscreened for HCC even though they are at greatest risk of this cancer. Therefore, trying to screen all patients with NAFLD for HCC would be “logistically impractical,” particularly when the absolute risk of HCC in noncirrhotic patients is unknown and no one has examined the best ways to screen this population, the investigators said. Instead, clinicians could prioritize screening and treating NAFLD patients for diabetes mellitus and obesity, both of which are associated with HCC. “There is evidence to suggest that metformin reduces the risk of HCC among diabetics,” they added. “Studies of these and other risk factors of HCC among NAFLD patients with and without cirrhosis are needed.”
Most patients in the study were male, potentially limiting the generalizability of the findings, the researchers noted.
The National Cancer Institute, the Houston Veterans Affairs Health Services Research and Development Center of Excellence, the Michael E. DeBakey Veterans Affairs Medical Center, and the Dan Duncan Cancer Center funded the study. The researchers had no disclosures.
Source: American Gastroenterological Association
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Nonalcoholic fatty liver disease and metabolic syndrome are risk factors for hepatocellular carcinoma in the absence of cirrhosis.
Major finding: Patients with these diseases were more than five times as likely to develop noncirrhotic HCC compared with patients with chronic hepatitis C virus infection.
Data source: A study of 1,500 randomly selected U.S. veterans diagnosed with HCC between 2005 and 2010.
Disclosures: The National Cancer Institute, the Houston Veterans Affairs Health Services Research and Development Center of Excellence, the Michael E. DeBakey Veterans Affairs Medical Center, and the Dan Duncan Cancer Center funded the study. The researchers had no disclosures.
Study lays groundwork for autologous nerve cell transplantation in Hirschsprung disease
Neural progenitor cells from the proximal colons of patients with Hirschsprung disease divided and formed neurons and glia in their own distal aganglionic colon tissue, according to a study published in the January issue of Cellular and Molecular Gastroenterology and Hepatology.
The approach could lead to “a promising therapeutic strategy” for Hirschsprung disease, because autologous transplantation of nerve progenitor cells would prevent immune rejection, said Dr. Benjamin Rollo of Murdoch Children’s Research Institute in Victoria, Australia, and his associates. But they cautioned against reading too much into their findings, “as there are distributional hurdles to surmount” before cell therapy can be used alone or in combination with surgery.
Hirschsprung disease is a congenital disorder in which embryonic neural crest cells fail to form the distal part of the enteric nervous system. The resulting lack of bowel motility leads to severe constipation and potentially fatal megacolon. Treatment involves surgically resecting the aganglionic distal bowel and anastomosing the normal proximal bowel to the anorectum, but this approach itself can cause constipation as well as fecal soiling, the investigators noted (Cell Molec Gastroenterol Hepatol. 2015 Oct. 22 [doi: 10.1016/j.jcmgh.2015.09.007]).
For the study, they harvested tissue from the proximal (neuronal) and distal (aneuronal) margins of resection of the colons of 31 infants and children with Hirschsprung disease. They cultured cells from the myenteric plexus of the proximal colon, and separated out nerve cells by using flow cytometry for the p75 neural crest marker. To test whether these nerve cells could colonize aganglionic colon, they co-cultured them with aneural avian embryo gut and with patients’ own aneuronal colon muscle. In addition, they co-cultured embryonic mouse enteric nernous system cells with human aneuronal colon muscle. They used quantitative reverse transcriptase PCR and several other standard laboratory techniques to detect cellular markers and mitosis.
Ganglia from the patients’ proximal colons expressed the neural crest markers p75, SOX10, and HNK1, as well as several neuronal, neurite, and glial markers, the researchers reported. The proximal colon specimens also contained ENS progenitor cells, which were SOX10-positive but lacked neuronal or glial markers. The progenitor cells comprised less than 5% of all cells from the proximal colon, but proliferated fourfold more after supplementation with CHIR-99021, a selective inhibitor of glycogen synthase kinase 3. They successfully colonized avian aneural embryonic gut and autologous postnatal aneuronal colon tissue, and the latter also was colonized successfully by mouse enteric neural crest cells.
The study “fulfilled three key requirements” for transplantation – harvesting enteric nervous system cells from the proximal colons of patients with Hirschsprung disease; confirming that postnatal aneuronal colon tissue could support an enteric nervous system; and showing that enteric nervous system–derived cells could colonize both embryonic gut and autologous postnatal colon tissue, said the researchers. More work is needed to sufficiently expand embryonic neural crest stem or progenitor cells and transplant them over a large area of colon, although supplementation with growth factors and use of elastic polymer substrates might help, they added.
The National Health and Medical Research Council, Murdoch Children’s Research Institute, Graham Burke and Yvonne Spencer, the Federation of Chinese Associations, Fonds du Service de chirurgie pédiatrique et de Perfectionnement du CHUV, Fondation SICPA, and Société Académique Vaudoise funded the study. The researchers disclosed no conflicts of interest.
Hirschsprung disease results from a failure of complete neural crest cell migration into the distal colon. Current therapy relies on surgical resection of the aganglionic distal colon. However, for many children, particularly those with large aganglionic segments, surgery often fails to completely normalize function.
One therapeutic approach might be to transplant new enteric neural cells into the aganglionic colon. This has been partially accomplished in rodent and avian models. However, it is not known if human smooth muscle can be colonized or if human postnatal enteric nervous system cells are capable of migration, expansion, and differentiation.
Rollo et al. show that human postnatal enteric nervous system cells isolated from the proximal, i.e., ganglionic, margin of Hirschsprung disease resection specimens can migrate and spread to colonize aganglionic smooth muscle from the distal margin of the same specimen. Remarkably, the transplanted cells differentiated into neurons and glia and formed normal-appearing neural structures.
Many questions remain. If neural cells isolated from the proximal margin can migrate ex vivo, why didn’t they migrate during in utero development? Do the transplanted cells restore normal motility, which requires a complex series of events that must be precisely orchestrated?
Nevertheless, the demonstration that human postnatal neural cells can be isolated from surgical specimens and used to colonize aganglionic smooth muscle suggests that it may be possible to conserve and restore motility and, potentially, to successfully treat Hirschprung disease patients without the need for surgery.
Marion France, Ph.D., is a postdoctoral research fellow at Brigham and Women’s Hospital and Harvard Medical School, Boston. She has no conflicts of interest.
Hirschsprung disease results from a failure of complete neural crest cell migration into the distal colon. Current therapy relies on surgical resection of the aganglionic distal colon. However, for many children, particularly those with large aganglionic segments, surgery often fails to completely normalize function.
One therapeutic approach might be to transplant new enteric neural cells into the aganglionic colon. This has been partially accomplished in rodent and avian models. However, it is not known if human smooth muscle can be colonized or if human postnatal enteric nervous system cells are capable of migration, expansion, and differentiation.
Rollo et al. show that human postnatal enteric nervous system cells isolated from the proximal, i.e., ganglionic, margin of Hirschsprung disease resection specimens can migrate and spread to colonize aganglionic smooth muscle from the distal margin of the same specimen. Remarkably, the transplanted cells differentiated into neurons and glia and formed normal-appearing neural structures.
Many questions remain. If neural cells isolated from the proximal margin can migrate ex vivo, why didn’t they migrate during in utero development? Do the transplanted cells restore normal motility, which requires a complex series of events that must be precisely orchestrated?
Nevertheless, the demonstration that human postnatal neural cells can be isolated from surgical specimens and used to colonize aganglionic smooth muscle suggests that it may be possible to conserve and restore motility and, potentially, to successfully treat Hirschprung disease patients without the need for surgery.
Marion France, Ph.D., is a postdoctoral research fellow at Brigham and Women’s Hospital and Harvard Medical School, Boston. She has no conflicts of interest.
Hirschsprung disease results from a failure of complete neural crest cell migration into the distal colon. Current therapy relies on surgical resection of the aganglionic distal colon. However, for many children, particularly those with large aganglionic segments, surgery often fails to completely normalize function.
One therapeutic approach might be to transplant new enteric neural cells into the aganglionic colon. This has been partially accomplished in rodent and avian models. However, it is not known if human smooth muscle can be colonized or if human postnatal enteric nervous system cells are capable of migration, expansion, and differentiation.
Rollo et al. show that human postnatal enteric nervous system cells isolated from the proximal, i.e., ganglionic, margin of Hirschsprung disease resection specimens can migrate and spread to colonize aganglionic smooth muscle from the distal margin of the same specimen. Remarkably, the transplanted cells differentiated into neurons and glia and formed normal-appearing neural structures.
Many questions remain. If neural cells isolated from the proximal margin can migrate ex vivo, why didn’t they migrate during in utero development? Do the transplanted cells restore normal motility, which requires a complex series of events that must be precisely orchestrated?
Nevertheless, the demonstration that human postnatal neural cells can be isolated from surgical specimens and used to colonize aganglionic smooth muscle suggests that it may be possible to conserve and restore motility and, potentially, to successfully treat Hirschprung disease patients without the need for surgery.
Marion France, Ph.D., is a postdoctoral research fellow at Brigham and Women’s Hospital and Harvard Medical School, Boston. She has no conflicts of interest.
Neural progenitor cells from the proximal colons of patients with Hirschsprung disease divided and formed neurons and glia in their own distal aganglionic colon tissue, according to a study published in the January issue of Cellular and Molecular Gastroenterology and Hepatology.
The approach could lead to “a promising therapeutic strategy” for Hirschsprung disease, because autologous transplantation of nerve progenitor cells would prevent immune rejection, said Dr. Benjamin Rollo of Murdoch Children’s Research Institute in Victoria, Australia, and his associates. But they cautioned against reading too much into their findings, “as there are distributional hurdles to surmount” before cell therapy can be used alone or in combination with surgery.
Hirschsprung disease is a congenital disorder in which embryonic neural crest cells fail to form the distal part of the enteric nervous system. The resulting lack of bowel motility leads to severe constipation and potentially fatal megacolon. Treatment involves surgically resecting the aganglionic distal bowel and anastomosing the normal proximal bowel to the anorectum, but this approach itself can cause constipation as well as fecal soiling, the investigators noted (Cell Molec Gastroenterol Hepatol. 2015 Oct. 22 [doi: 10.1016/j.jcmgh.2015.09.007]).
For the study, they harvested tissue from the proximal (neuronal) and distal (aneuronal) margins of resection of the colons of 31 infants and children with Hirschsprung disease. They cultured cells from the myenteric plexus of the proximal colon, and separated out nerve cells by using flow cytometry for the p75 neural crest marker. To test whether these nerve cells could colonize aganglionic colon, they co-cultured them with aneural avian embryo gut and with patients’ own aneuronal colon muscle. In addition, they co-cultured embryonic mouse enteric nernous system cells with human aneuronal colon muscle. They used quantitative reverse transcriptase PCR and several other standard laboratory techniques to detect cellular markers and mitosis.
Ganglia from the patients’ proximal colons expressed the neural crest markers p75, SOX10, and HNK1, as well as several neuronal, neurite, and glial markers, the researchers reported. The proximal colon specimens also contained ENS progenitor cells, which were SOX10-positive but lacked neuronal or glial markers. The progenitor cells comprised less than 5% of all cells from the proximal colon, but proliferated fourfold more after supplementation with CHIR-99021, a selective inhibitor of glycogen synthase kinase 3. They successfully colonized avian aneural embryonic gut and autologous postnatal aneuronal colon tissue, and the latter also was colonized successfully by mouse enteric neural crest cells.
The study “fulfilled three key requirements” for transplantation – harvesting enteric nervous system cells from the proximal colons of patients with Hirschsprung disease; confirming that postnatal aneuronal colon tissue could support an enteric nervous system; and showing that enteric nervous system–derived cells could colonize both embryonic gut and autologous postnatal colon tissue, said the researchers. More work is needed to sufficiently expand embryonic neural crest stem or progenitor cells and transplant them over a large area of colon, although supplementation with growth factors and use of elastic polymer substrates might help, they added.
The National Health and Medical Research Council, Murdoch Children’s Research Institute, Graham Burke and Yvonne Spencer, the Federation of Chinese Associations, Fonds du Service de chirurgie pédiatrique et de Perfectionnement du CHUV, Fondation SICPA, and Société Académique Vaudoise funded the study. The researchers disclosed no conflicts of interest.
Neural progenitor cells from the proximal colons of patients with Hirschsprung disease divided and formed neurons and glia in their own distal aganglionic colon tissue, according to a study published in the January issue of Cellular and Molecular Gastroenterology and Hepatology.
The approach could lead to “a promising therapeutic strategy” for Hirschsprung disease, because autologous transplantation of nerve progenitor cells would prevent immune rejection, said Dr. Benjamin Rollo of Murdoch Children’s Research Institute in Victoria, Australia, and his associates. But they cautioned against reading too much into their findings, “as there are distributional hurdles to surmount” before cell therapy can be used alone or in combination with surgery.
Hirschsprung disease is a congenital disorder in which embryonic neural crest cells fail to form the distal part of the enteric nervous system. The resulting lack of bowel motility leads to severe constipation and potentially fatal megacolon. Treatment involves surgically resecting the aganglionic distal bowel and anastomosing the normal proximal bowel to the anorectum, but this approach itself can cause constipation as well as fecal soiling, the investigators noted (Cell Molec Gastroenterol Hepatol. 2015 Oct. 22 [doi: 10.1016/j.jcmgh.2015.09.007]).
For the study, they harvested tissue from the proximal (neuronal) and distal (aneuronal) margins of resection of the colons of 31 infants and children with Hirschsprung disease. They cultured cells from the myenteric plexus of the proximal colon, and separated out nerve cells by using flow cytometry for the p75 neural crest marker. To test whether these nerve cells could colonize aganglionic colon, they co-cultured them with aneural avian embryo gut and with patients’ own aneuronal colon muscle. In addition, they co-cultured embryonic mouse enteric nernous system cells with human aneuronal colon muscle. They used quantitative reverse transcriptase PCR and several other standard laboratory techniques to detect cellular markers and mitosis.
Ganglia from the patients’ proximal colons expressed the neural crest markers p75, SOX10, and HNK1, as well as several neuronal, neurite, and glial markers, the researchers reported. The proximal colon specimens also contained ENS progenitor cells, which were SOX10-positive but lacked neuronal or glial markers. The progenitor cells comprised less than 5% of all cells from the proximal colon, but proliferated fourfold more after supplementation with CHIR-99021, a selective inhibitor of glycogen synthase kinase 3. They successfully colonized avian aneural embryonic gut and autologous postnatal aneuronal colon tissue, and the latter also was colonized successfully by mouse enteric neural crest cells.
The study “fulfilled three key requirements” for transplantation – harvesting enteric nervous system cells from the proximal colons of patients with Hirschsprung disease; confirming that postnatal aneuronal colon tissue could support an enteric nervous system; and showing that enteric nervous system–derived cells could colonize both embryonic gut and autologous postnatal colon tissue, said the researchers. More work is needed to sufficiently expand embryonic neural crest stem or progenitor cells and transplant them over a large area of colon, although supplementation with growth factors and use of elastic polymer substrates might help, they added.
The National Health and Medical Research Council, Murdoch Children’s Research Institute, Graham Burke and Yvonne Spencer, the Federation of Chinese Associations, Fonds du Service de chirurgie pédiatrique et de Perfectionnement du CHUV, Fondation SICPA, and Société Académique Vaudoise funded the study. The researchers disclosed no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A preclinical study took several key steps toward autologous transplantation of nerve progenitor cells to treat Hirschsprung disease.
Major finding: Neural progenitor cells from the proximal colons of patients with Hirschsprung disease divided and formed neurons and glia in their own distal aganglionic colon tissue.
Data source: Flow cytometry, reverse transcriptase-PCR, immunohistochemistry, and cell culture of proximal (neuronal) and distal (aneuronal) colon tissue from 31 affected patients, and co-culture with avian embryonic gut and mouse enteric nervous system cells.
Disclosures: The National Health and Medical Research Council, Murdoch Children’s Research Institute, Graham Burke and Yvonne Spencer, the Federation of Chinese Associations, Fonds du Service de chirurgie pédiatrique et de Perfectionnement du CHUV, Fondation SICPA, and Société Académique Vaudoise funded the study. The researchers disclosed no conflicts of interest.
PPIs caused remission in about half of esophageal eosinophilia cases
About half of patients with symptomatic esophageal eosinophilia achieved complete clinical and histologic remission on proton pump inhibitors (PPIs), according to a systematic review and meta-analysis of 33 studies.
“Our results support the concept of PPIs as first-line therapy in both children and adults,” Dr. Alfredo Lucendo of the Servicio de Salud de Castillo–La Mancha, Hospital General de Tomelloso, Albacete, Spain, and his associates wrote in the January issue of Clinical Gastroenterology and Hepatology. “Other effective alternatives, such as dietary or topical steroid therapy, likely might be set aside as second-line treatment, owing to long-term safety concerns (topical steroid therapy) and impairment of quality of life and nutritional inadequacy (dietary interventions).”
The study also confirmed that esophageal pH monitoring does not accurately predict therapeutic response to PPI therapy. “The performance of this test before histologic reevaluation on PPI therapy should be discouraged,” according to the researchers (Clin Gastroenterol Hepatol. 2015. [doi:10.1016/j.cgh.2015.07.041]). Eosinophilic esophagitis was first described as a distinct disorder about 20 years ago, but only recently was understood to be the most common cause of chronic esophageal symptoms among children and young adults. Some cases are now known to respond to PPI therapy, but reported remission rates have varied depending on study design and patient population, the investigators said. In addition, no one had systematically reviewed studies of PPI-responsive esophageal eosinophilia for quality or to determine the optimal type of PPI, dose, or treatment duration.
Therefore, the investigators searched MEDLINE, EMBASE, SCOPUS, and abstracts from the annual meetings of the American Gastroenterological Association, the American College of Gastroenterology, and United European Gastroenterology, identifying 33 studies of 619 patients with symptomatic esophageal eosinophilia. Eleven of the studies were prospective, of which only two were randomized controlled trials. The researchers defined a histologic response as less than 15 eosinophils per high-powered frame after PPI therapy. “Missing data regarding PPI therapy were common and prevented us from drawing conclusions on the most effective PPI drug and doses,” they said. In addition, most studies lacked structured or objective survey tools or other measures of clinical improvement, making it impossible to rule out self-adapted coping strategies as a main cause of improvement over time.
With those caveats in mind, about 61% of patients in the pooled analysis had a clinical response to PPI therapy (95% confidence interval, 48%-72%), and half achieved clinical and histologic remission (95% CI, 42%-59%), the investigators reported. Therapy was somewhat more effective when administered twice a day instead of once daily, when clinicians used esophageal pH monitoring, and when studies were prospective instead of retrospective, but the differences were not significant. Nor did therapeutic response significantly differ based on the age of patients, type of report, or quality of the study.
The overall findings “should be interpreted with caution because of poor-quality evidence, heterogeneity, and publication bias,” the researchers said. Prospective studies are needed to examine the best PPI, dose, and dosing interval to use in an initial trial in the clinic; to clarify long-term effects and dosing strategies; to assess the ability of PPIs to reverse fibrotic esophageal remodeling; and to examine the effects of the CYP2C19 genotype on clinical and histologic response, they added. “More quality evidence on pediatric PPI-responsive eosinophilic esophagitis is needed urgently,” they emphasized.
The authors reported no funding sources and had no disclosures.
Proton pump inhibitor–responsive esophageal eosinophilia (PPI-REE) is a condition in which patients have symptoms of esophageal dysfunction (often dysphagia or heartburn), biopsies with at least 15 eosinophils per high-power field (eos/hpf), and symptomatic and histologic resolution after a PPI trial, typically at twice-daily dosing. Currently, PPI-REE and eosinophilic esophagitis (EoE) overlap substantially, but in the most recent guidelines, they are still considered to be distinct entities. PPI-REE was first reported almost 10 years ago, and since then multiple prospective and retrospective studies in both children and adults have further characterized it. The study by Dr. Lucendo and colleagues, a comprehensive and rigorously conducted systematic review and meta-analysis of 33 studies accounting for 619 patients, found that just over 50% of patients with esophageal eosinophilia had histologic remission (less than 15 eos/hpf) and just over 60% had symptomatic improvement after PPI use. Moreover, similar responses were seen whether or not there was pathologic acid exposure on pH testing.

|
| Dr. Evan S. Dellon |
While there was heterogeneity between studies on meta-analysis, there are several important messages from this study. First, PPI-REE is commonly seen in patients with esophageal eosinophilia, and is not always simply due to reflux. Second, PPIs have a potent antieosinophil effect in these patients. Interestingly, novel acid-independent mechanisms for this anti-inflammatory action recently have been described in other studies. Third, a PPI trial remains important prior to confirming the diagnosis of EoE, and PPIs should be considered the first-line treatment when esophageal eosinophilia is identified. However, it bears emphasizing that all esophageal eosinophilia is not due to EoE. If a patient responds to the PPI trial, there is no clear need to move toward topical steroid or dietary elimination therapy specifically for EoE, and starting multiple antieosinophil treatments concomitantly precludes determining which is most effective. In the future, understanding which patients with esophageal eosinophilia will most benefit from a PPI trial will be important, as we are currently unable to predict this from clinical, endoscopic, and histologic factors. Future studies and guidelines will also need to address whether EoE and PPI-REE are distinct diseases or manifestations of the same underlying process.
Dr. Evan S. Dellon, MPH, is associate professor of medicine and epidemiology at the Center for Esophageal Diseases and Swallowing, division of gastroenterology and hepatology, University of North Carolina School of Medicine at Chapel Hill. He has received research funding from Meritage, Miraca, Receptos, and Regeneron and consulted for Aptalis, Banner, Novartis, Receptos, Regeneron, and Roche.
Proton pump inhibitor–responsive esophageal eosinophilia (PPI-REE) is a condition in which patients have symptoms of esophageal dysfunction (often dysphagia or heartburn), biopsies with at least 15 eosinophils per high-power field (eos/hpf), and symptomatic and histologic resolution after a PPI trial, typically at twice-daily dosing. Currently, PPI-REE and eosinophilic esophagitis (EoE) overlap substantially, but in the most recent guidelines, they are still considered to be distinct entities. PPI-REE was first reported almost 10 years ago, and since then multiple prospective and retrospective studies in both children and adults have further characterized it. The study by Dr. Lucendo and colleagues, a comprehensive and rigorously conducted systematic review and meta-analysis of 33 studies accounting for 619 patients, found that just over 50% of patients with esophageal eosinophilia had histologic remission (less than 15 eos/hpf) and just over 60% had symptomatic improvement after PPI use. Moreover, similar responses were seen whether or not there was pathologic acid exposure on pH testing.

|
| Dr. Evan S. Dellon |
While there was heterogeneity between studies on meta-analysis, there are several important messages from this study. First, PPI-REE is commonly seen in patients with esophageal eosinophilia, and is not always simply due to reflux. Second, PPIs have a potent antieosinophil effect in these patients. Interestingly, novel acid-independent mechanisms for this anti-inflammatory action recently have been described in other studies. Third, a PPI trial remains important prior to confirming the diagnosis of EoE, and PPIs should be considered the first-line treatment when esophageal eosinophilia is identified. However, it bears emphasizing that all esophageal eosinophilia is not due to EoE. If a patient responds to the PPI trial, there is no clear need to move toward topical steroid or dietary elimination therapy specifically for EoE, and starting multiple antieosinophil treatments concomitantly precludes determining which is most effective. In the future, understanding which patients with esophageal eosinophilia will most benefit from a PPI trial will be important, as we are currently unable to predict this from clinical, endoscopic, and histologic factors. Future studies and guidelines will also need to address whether EoE and PPI-REE are distinct diseases or manifestations of the same underlying process.
Dr. Evan S. Dellon, MPH, is associate professor of medicine and epidemiology at the Center for Esophageal Diseases and Swallowing, division of gastroenterology and hepatology, University of North Carolina School of Medicine at Chapel Hill. He has received research funding from Meritage, Miraca, Receptos, and Regeneron and consulted for Aptalis, Banner, Novartis, Receptos, Regeneron, and Roche.
Proton pump inhibitor–responsive esophageal eosinophilia (PPI-REE) is a condition in which patients have symptoms of esophageal dysfunction (often dysphagia or heartburn), biopsies with at least 15 eosinophils per high-power field (eos/hpf), and symptomatic and histologic resolution after a PPI trial, typically at twice-daily dosing. Currently, PPI-REE and eosinophilic esophagitis (EoE) overlap substantially, but in the most recent guidelines, they are still considered to be distinct entities. PPI-REE was first reported almost 10 years ago, and since then multiple prospective and retrospective studies in both children and adults have further characterized it. The study by Dr. Lucendo and colleagues, a comprehensive and rigorously conducted systematic review and meta-analysis of 33 studies accounting for 619 patients, found that just over 50% of patients with esophageal eosinophilia had histologic remission (less than 15 eos/hpf) and just over 60% had symptomatic improvement after PPI use. Moreover, similar responses were seen whether or not there was pathologic acid exposure on pH testing.

|
| Dr. Evan S. Dellon |
While there was heterogeneity between studies on meta-analysis, there are several important messages from this study. First, PPI-REE is commonly seen in patients with esophageal eosinophilia, and is not always simply due to reflux. Second, PPIs have a potent antieosinophil effect in these patients. Interestingly, novel acid-independent mechanisms for this anti-inflammatory action recently have been described in other studies. Third, a PPI trial remains important prior to confirming the diagnosis of EoE, and PPIs should be considered the first-line treatment when esophageal eosinophilia is identified. However, it bears emphasizing that all esophageal eosinophilia is not due to EoE. If a patient responds to the PPI trial, there is no clear need to move toward topical steroid or dietary elimination therapy specifically for EoE, and starting multiple antieosinophil treatments concomitantly precludes determining which is most effective. In the future, understanding which patients with esophageal eosinophilia will most benefit from a PPI trial will be important, as we are currently unable to predict this from clinical, endoscopic, and histologic factors. Future studies and guidelines will also need to address whether EoE and PPI-REE are distinct diseases or manifestations of the same underlying process.
Dr. Evan S. Dellon, MPH, is associate professor of medicine and epidemiology at the Center for Esophageal Diseases and Swallowing, division of gastroenterology and hepatology, University of North Carolina School of Medicine at Chapel Hill. He has received research funding from Meritage, Miraca, Receptos, and Regeneron and consulted for Aptalis, Banner, Novartis, Receptos, Regeneron, and Roche.
About half of patients with symptomatic esophageal eosinophilia achieved complete clinical and histologic remission on proton pump inhibitors (PPIs), according to a systematic review and meta-analysis of 33 studies.
“Our results support the concept of PPIs as first-line therapy in both children and adults,” Dr. Alfredo Lucendo of the Servicio de Salud de Castillo–La Mancha, Hospital General de Tomelloso, Albacete, Spain, and his associates wrote in the January issue of Clinical Gastroenterology and Hepatology. “Other effective alternatives, such as dietary or topical steroid therapy, likely might be set aside as second-line treatment, owing to long-term safety concerns (topical steroid therapy) and impairment of quality of life and nutritional inadequacy (dietary interventions).”
The study also confirmed that esophageal pH monitoring does not accurately predict therapeutic response to PPI therapy. “The performance of this test before histologic reevaluation on PPI therapy should be discouraged,” according to the researchers (Clin Gastroenterol Hepatol. 2015. [doi:10.1016/j.cgh.2015.07.041]). Eosinophilic esophagitis was first described as a distinct disorder about 20 years ago, but only recently was understood to be the most common cause of chronic esophageal symptoms among children and young adults. Some cases are now known to respond to PPI therapy, but reported remission rates have varied depending on study design and patient population, the investigators said. In addition, no one had systematically reviewed studies of PPI-responsive esophageal eosinophilia for quality or to determine the optimal type of PPI, dose, or treatment duration.
Therefore, the investigators searched MEDLINE, EMBASE, SCOPUS, and abstracts from the annual meetings of the American Gastroenterological Association, the American College of Gastroenterology, and United European Gastroenterology, identifying 33 studies of 619 patients with symptomatic esophageal eosinophilia. Eleven of the studies were prospective, of which only two were randomized controlled trials. The researchers defined a histologic response as less than 15 eosinophils per high-powered frame after PPI therapy. “Missing data regarding PPI therapy were common and prevented us from drawing conclusions on the most effective PPI drug and doses,” they said. In addition, most studies lacked structured or objective survey tools or other measures of clinical improvement, making it impossible to rule out self-adapted coping strategies as a main cause of improvement over time.
With those caveats in mind, about 61% of patients in the pooled analysis had a clinical response to PPI therapy (95% confidence interval, 48%-72%), and half achieved clinical and histologic remission (95% CI, 42%-59%), the investigators reported. Therapy was somewhat more effective when administered twice a day instead of once daily, when clinicians used esophageal pH monitoring, and when studies were prospective instead of retrospective, but the differences were not significant. Nor did therapeutic response significantly differ based on the age of patients, type of report, or quality of the study.
The overall findings “should be interpreted with caution because of poor-quality evidence, heterogeneity, and publication bias,” the researchers said. Prospective studies are needed to examine the best PPI, dose, and dosing interval to use in an initial trial in the clinic; to clarify long-term effects and dosing strategies; to assess the ability of PPIs to reverse fibrotic esophageal remodeling; and to examine the effects of the CYP2C19 genotype on clinical and histologic response, they added. “More quality evidence on pediatric PPI-responsive eosinophilic esophagitis is needed urgently,” they emphasized.
The authors reported no funding sources and had no disclosures.
About half of patients with symptomatic esophageal eosinophilia achieved complete clinical and histologic remission on proton pump inhibitors (PPIs), according to a systematic review and meta-analysis of 33 studies.
“Our results support the concept of PPIs as first-line therapy in both children and adults,” Dr. Alfredo Lucendo of the Servicio de Salud de Castillo–La Mancha, Hospital General de Tomelloso, Albacete, Spain, and his associates wrote in the January issue of Clinical Gastroenterology and Hepatology. “Other effective alternatives, such as dietary or topical steroid therapy, likely might be set aside as second-line treatment, owing to long-term safety concerns (topical steroid therapy) and impairment of quality of life and nutritional inadequacy (dietary interventions).”
The study also confirmed that esophageal pH monitoring does not accurately predict therapeutic response to PPI therapy. “The performance of this test before histologic reevaluation on PPI therapy should be discouraged,” according to the researchers (Clin Gastroenterol Hepatol. 2015. [doi:10.1016/j.cgh.2015.07.041]). Eosinophilic esophagitis was first described as a distinct disorder about 20 years ago, but only recently was understood to be the most common cause of chronic esophageal symptoms among children and young adults. Some cases are now known to respond to PPI therapy, but reported remission rates have varied depending on study design and patient population, the investigators said. In addition, no one had systematically reviewed studies of PPI-responsive esophageal eosinophilia for quality or to determine the optimal type of PPI, dose, or treatment duration.
Therefore, the investigators searched MEDLINE, EMBASE, SCOPUS, and abstracts from the annual meetings of the American Gastroenterological Association, the American College of Gastroenterology, and United European Gastroenterology, identifying 33 studies of 619 patients with symptomatic esophageal eosinophilia. Eleven of the studies were prospective, of which only two were randomized controlled trials. The researchers defined a histologic response as less than 15 eosinophils per high-powered frame after PPI therapy. “Missing data regarding PPI therapy were common and prevented us from drawing conclusions on the most effective PPI drug and doses,” they said. In addition, most studies lacked structured or objective survey tools or other measures of clinical improvement, making it impossible to rule out self-adapted coping strategies as a main cause of improvement over time.
With those caveats in mind, about 61% of patients in the pooled analysis had a clinical response to PPI therapy (95% confidence interval, 48%-72%), and half achieved clinical and histologic remission (95% CI, 42%-59%), the investigators reported. Therapy was somewhat more effective when administered twice a day instead of once daily, when clinicians used esophageal pH monitoring, and when studies were prospective instead of retrospective, but the differences were not significant. Nor did therapeutic response significantly differ based on the age of patients, type of report, or quality of the study.
The overall findings “should be interpreted with caution because of poor-quality evidence, heterogeneity, and publication bias,” the researchers said. Prospective studies are needed to examine the best PPI, dose, and dosing interval to use in an initial trial in the clinic; to clarify long-term effects and dosing strategies; to assess the ability of PPIs to reverse fibrotic esophageal remodeling; and to examine the effects of the CYP2C19 genotype on clinical and histologic response, they added. “More quality evidence on pediatric PPI-responsive eosinophilic esophagitis is needed urgently,” they emphasized.
The authors reported no funding sources and had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Proton pump inhibitors should be considered in the first-line treatment of esophageal eosinophilia.
Major finding: Half of patients achieved clinical and histologic remission after a trial of PPIs.
Data source: Meta-analysis of 33 studies of 619 patients with symptomatic esophageal eosinophilia indicative of eosinophilic esophagitis.
Disclosures: The authors reported no funding sources and had no disclosures.