User login
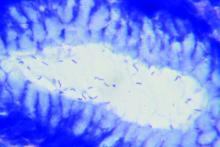
VIDEO: Trial posts null results for Helicobacter screening, eradication
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Screening for and eradicating H. pylori infections did not significantly improve long-term prevalence of dyspepsia, incidence of peptic ulcer disease, use of health care services, or quality of life.
Major finding: At 13-year follow-up, both arms had a 19% prevalence of dyspepsia (aOR, 0.93; 95% CI, 0.82-1.04) and a 3% cumulative incidence of peptic ulcer disease (RR, 0.93; 95% CI, 0.79-1.09).
Data source: A randomized controlled trial of 8,658 adults aged 40-65 years
Disclosures: Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
Alcohol showed no cardiovascular benefits in nonalcoholic fatty liver disease
Alcohol consumption produced no apparent cardiovascular benefits among individuals with nonalcoholic fatty liver disease, according to a study of 570 white and black adults from the Coronary Artery Risk Development in Young Adults (CARDIA) longitudinal cohort.
After researchers controlled for multiple demographic and clinical confounders, alcohol use was not associated with cardiovascular risk factors such as diabetes, hypertension, or hyperlipidemia, nor with homeostatic model assessment of insulin resistance, C-reactive protein level, total cholesterol, systolic or diastolic blood pressure, coronary artery calcification, E/A ratio, or global longitudinal strain among individuals with nonalcoholic fatty liver disease (NAFLD), reported Lisa B. VanWagner, MD, of Northwestern University, Chicago, and her associates. “[A] recommendation of cardiovascular disease risk benefit of alcohol use in persons with NAFLD cannot be made based on the current findings,” they wrote. They advocated for prospective, long-term studies to better understand how various types and doses of alcohol affect hard cardiovascular endpoints in patients with NAFLD. Their study was published in Gastroenterology.
CARDIA enrolled 5,115 black and white adults aged 18-30 years from four cities in the United States, and followed them long term. Participants were asked about alcohol consumption at study entry and again at 15, 20, and 25 years of follow-up. At year 25, participants underwent computed tomography (CT) examinations of the thorax and abdomen and tissue Doppler echocardiography with myocardial strain measured by speckle tracking (Gastroenterology. 2017 Aug 9. doi: 10.1053/j.gastro.2017.08.012).
The 570 participants with NAFLD averaged 50 years of age, 54% were black, 46% were female, and 58% consumed at least one alcoholic drink per week, said the researchers. Compared with nondrinkers, drinkers had attained significantly higher education levels, were significantly more likely to be white and male, and had a significantly lower average body mass index (34.4 kg/m2 vs. 37.3 kg/m2) and C-reactive protein level (4.2 vs. 6.1 mg per L), and a significantly lower prevalence of diabetes (23% vs. 37%), impaired glucose tolerance (42% vs. 49%), obesity (75% vs. 83%) and metabolic syndrome (55% vs. 66%) (P less than .05 for all comparisons). Drinkers and nondrinkers resembled each other in terms of lipid profiles, use of lipid-lowering medications, liver attenuation scores, and systolic and diastolic blood pressures, although significantly more nondrinkers used antihypertensive medications (46% vs.35%; P = .005).
Drinkers had a higher prevalence of coronary artery calcification, defined as Agatston score above 0 (42% vs. 34%), and the difference approached statistical significance (P = .05). However, after they adjusted for multiple potential confounders, the researchers found no link between alcohol consumption and risk factors for cardiovascular disease or between alcohol consumption and measures of subclinical cardiovascular disease. This finding persisted in sensitivity analyses that examined alcohol dose, binge drinking, history of cardiovascular events, and former heavy alcohol use.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Taken together, the findings “challenge the belief that alcohol use may reduce cardiovascular disease risk in persons with nonalcoholic fatty liver disease,” the investigators concluded. Clinical heart failure was too rare to reliably assess, but “we failed to observe an association between alcohol use and multiple markers of subclinical changes in cardiac structure and function that may be precursors of incident heart failure in NAFLD,” they wrote. More longitudinal studies would be needed to clarify how moderate alcohol use in NAFLD affects coronary artery calcification or changes in myocardial structure and function, they cautioned.
The National Institutes of Health supported the work. The investigators reported having no relevant conflicts of interest.
Alcohol consumption produced no apparent cardiovascular benefits among individuals with nonalcoholic fatty liver disease, according to a study of 570 white and black adults from the Coronary Artery Risk Development in Young Adults (CARDIA) longitudinal cohort.
After researchers controlled for multiple demographic and clinical confounders, alcohol use was not associated with cardiovascular risk factors such as diabetes, hypertension, or hyperlipidemia, nor with homeostatic model assessment of insulin resistance, C-reactive protein level, total cholesterol, systolic or diastolic blood pressure, coronary artery calcification, E/A ratio, or global longitudinal strain among individuals with nonalcoholic fatty liver disease (NAFLD), reported Lisa B. VanWagner, MD, of Northwestern University, Chicago, and her associates. “[A] recommendation of cardiovascular disease risk benefit of alcohol use in persons with NAFLD cannot be made based on the current findings,” they wrote. They advocated for prospective, long-term studies to better understand how various types and doses of alcohol affect hard cardiovascular endpoints in patients with NAFLD. Their study was published in Gastroenterology.
CARDIA enrolled 5,115 black and white adults aged 18-30 years from four cities in the United States, and followed them long term. Participants were asked about alcohol consumption at study entry and again at 15, 20, and 25 years of follow-up. At year 25, participants underwent computed tomography (CT) examinations of the thorax and abdomen and tissue Doppler echocardiography with myocardial strain measured by speckle tracking (Gastroenterology. 2017 Aug 9. doi: 10.1053/j.gastro.2017.08.012).
The 570 participants with NAFLD averaged 50 years of age, 54% were black, 46% were female, and 58% consumed at least one alcoholic drink per week, said the researchers. Compared with nondrinkers, drinkers had attained significantly higher education levels, were significantly more likely to be white and male, and had a significantly lower average body mass index (34.4 kg/m2 vs. 37.3 kg/m2) and C-reactive protein level (4.2 vs. 6.1 mg per L), and a significantly lower prevalence of diabetes (23% vs. 37%), impaired glucose tolerance (42% vs. 49%), obesity (75% vs. 83%) and metabolic syndrome (55% vs. 66%) (P less than .05 for all comparisons). Drinkers and nondrinkers resembled each other in terms of lipid profiles, use of lipid-lowering medications, liver attenuation scores, and systolic and diastolic blood pressures, although significantly more nondrinkers used antihypertensive medications (46% vs.35%; P = .005).
Drinkers had a higher prevalence of coronary artery calcification, defined as Agatston score above 0 (42% vs. 34%), and the difference approached statistical significance (P = .05). However, after they adjusted for multiple potential confounders, the researchers found no link between alcohol consumption and risk factors for cardiovascular disease or between alcohol consumption and measures of subclinical cardiovascular disease. This finding persisted in sensitivity analyses that examined alcohol dose, binge drinking, history of cardiovascular events, and former heavy alcohol use.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Taken together, the findings “challenge the belief that alcohol use may reduce cardiovascular disease risk in persons with nonalcoholic fatty liver disease,” the investigators concluded. Clinical heart failure was too rare to reliably assess, but “we failed to observe an association between alcohol use and multiple markers of subclinical changes in cardiac structure and function that may be precursors of incident heart failure in NAFLD,” they wrote. More longitudinal studies would be needed to clarify how moderate alcohol use in NAFLD affects coronary artery calcification or changes in myocardial structure and function, they cautioned.
The National Institutes of Health supported the work. The investigators reported having no relevant conflicts of interest.
Alcohol consumption produced no apparent cardiovascular benefits among individuals with nonalcoholic fatty liver disease, according to a study of 570 white and black adults from the Coronary Artery Risk Development in Young Adults (CARDIA) longitudinal cohort.
After researchers controlled for multiple demographic and clinical confounders, alcohol use was not associated with cardiovascular risk factors such as diabetes, hypertension, or hyperlipidemia, nor with homeostatic model assessment of insulin resistance, C-reactive protein level, total cholesterol, systolic or diastolic blood pressure, coronary artery calcification, E/A ratio, or global longitudinal strain among individuals with nonalcoholic fatty liver disease (NAFLD), reported Lisa B. VanWagner, MD, of Northwestern University, Chicago, and her associates. “[A] recommendation of cardiovascular disease risk benefit of alcohol use in persons with NAFLD cannot be made based on the current findings,” they wrote. They advocated for prospective, long-term studies to better understand how various types and doses of alcohol affect hard cardiovascular endpoints in patients with NAFLD. Their study was published in Gastroenterology.
CARDIA enrolled 5,115 black and white adults aged 18-30 years from four cities in the United States, and followed them long term. Participants were asked about alcohol consumption at study entry and again at 15, 20, and 25 years of follow-up. At year 25, participants underwent computed tomography (CT) examinations of the thorax and abdomen and tissue Doppler echocardiography with myocardial strain measured by speckle tracking (Gastroenterology. 2017 Aug 9. doi: 10.1053/j.gastro.2017.08.012).
The 570 participants with NAFLD averaged 50 years of age, 54% were black, 46% were female, and 58% consumed at least one alcoholic drink per week, said the researchers. Compared with nondrinkers, drinkers had attained significantly higher education levels, were significantly more likely to be white and male, and had a significantly lower average body mass index (34.4 kg/m2 vs. 37.3 kg/m2) and C-reactive protein level (4.2 vs. 6.1 mg per L), and a significantly lower prevalence of diabetes (23% vs. 37%), impaired glucose tolerance (42% vs. 49%), obesity (75% vs. 83%) and metabolic syndrome (55% vs. 66%) (P less than .05 for all comparisons). Drinkers and nondrinkers resembled each other in terms of lipid profiles, use of lipid-lowering medications, liver attenuation scores, and systolic and diastolic blood pressures, although significantly more nondrinkers used antihypertensive medications (46% vs.35%; P = .005).
Drinkers had a higher prevalence of coronary artery calcification, defined as Agatston score above 0 (42% vs. 34%), and the difference approached statistical significance (P = .05). However, after they adjusted for multiple potential confounders, the researchers found no link between alcohol consumption and risk factors for cardiovascular disease or between alcohol consumption and measures of subclinical cardiovascular disease. This finding persisted in sensitivity analyses that examined alcohol dose, binge drinking, history of cardiovascular events, and former heavy alcohol use.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Taken together, the findings “challenge the belief that alcohol use may reduce cardiovascular disease risk in persons with nonalcoholic fatty liver disease,” the investigators concluded. Clinical heart failure was too rare to reliably assess, but “we failed to observe an association between alcohol use and multiple markers of subclinical changes in cardiac structure and function that may be precursors of incident heart failure in NAFLD,” they wrote. More longitudinal studies would be needed to clarify how moderate alcohol use in NAFLD affects coronary artery calcification or changes in myocardial structure and function, they cautioned.
The National Institutes of Health supported the work. The investigators reported having no relevant conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: No cardioprotective effects were shown with alcohol consumption in adults with nonalcoholic fatty liver disease.
Major finding: After researchers adjusted for multiple confounders, alcohol use was not associated with risk factors for cardiovascular disease or with indicators of subclinical cardiovascular disease.
Data source: A longitudinal, population-based study of 570 individuals with nonalcoholic fatty liver disease.
Disclosures: The National Institutes of Health supported the work. The investigators reported having no relevant conflicts of interest.
Biophysical properties of HCV evolve over course of infection
Hepatitis C virus (HCV) particles are of lowest density and most infectious early in the course of infection, based on findings from a study of chimeric mice.
Over time, however, viral density became more heterogeneous and infectivity fell, reported Ursula Andreo, PhD, of Rockefeller University, New York, with her coinvestigators. A diet of 10% sucrose, which in rats induces hepatic secretion of very-low-density lipoprotein (VLDL), caused HCV particles to become slightly lower density and more infectious in the mice, the researchers reported. Although the shift was “minor,” it “correlated with a trend toward enhanced triglyceride and cholesterol levels in the same fractions,” they wrote. They recommended studying high-fat diets to determine whether altering the VLDL secretion pathway affects the biophysical properties of HCV. “A high-fat diet might have a more significant impact on the lipoprotein profile in this humanized mouse model,” they wrote in Cellular and Molecular Gastroenterology and Hepatology (2017 Jul;4[3]:405-17).
Because HCV tends to associate with lipoproteins, it shows a range of buoyant densities in the blood of infected patients. The “entry, replication, and assembly [of the virion] are linked closely to host lipid and lipoprotein metabolism,” wrote Dr. Andreo and her colleagues.
They created an in vivo model to study the buoyant density and infectivity of HCV particles, as well as their interaction with lipoproteins, by grafting human hepatocytes into the livers of immunodeficient mice that were homozygous recessive for fumarylacetoacetate hydrolase. Next, they infected 13 of these chimeric mice with J6-JFH1, an HCV strain that can establish long-term infections in mice that have human liver grafts (Proc Natl Acad Sci USA. 2006;103[10]:3805-9). The human liver xenograft reconstituted the FAH gene, restoring triglycerides to normal levels in the chimeric mice and creating a suitable “humanlike” model of lipoprotein metabolism, the investigators wrote.
Density fractionation of infectious mouse serum revealed higher infectivity in the low-density fractions soon after infection, which also has been observed in a human liver chimeric mouse model of severe combined immunodeficiency disease, they added. In the HCV model, the human liver grafts were conserved 5 weeks after infection, and the mice had a lower proportion of lighter, infectious HCV particles.
The researchers lacked sufficient material to directly study the composition of virions or detect viral proteins in the various density fractions. However, they determined that apolipoprotein C1 was the lightest fraction and that apolipoprotein E was mainly found in the five lightest fractions. Both these apolipoproteins are “essential factors of HCV infectivity,” and neither redistributed over time, they said. They suggested using immunoelectron microscopy or mass spectrometry to study the nature and infectivity of viral particles further.
In humans, ingesting a high-fat milkshake increases detectable HCV RNA in the VLDL fraction, the researchers noted. In rodents, a sucrose diet also has been found to increase VLDL lipidation and secretion, so they gave five of the infected chimeric mice drinking water containing 10% sucrose. After 5 weeks, these mice had increased infectivity and higher levels of triglycerides and cholesterol, but the effect was small and disappeared after the sucrose was withdrawn.
HCV “circulates as a population of particles of light, as well as dense, buoyant densities, and both are infectious,” the researchers concluded. “Changes in diet, as well as conditions such as fasting and feeding, affect the distribution of HCV buoyant density gradients.”
Funders included the National Institutes of Health and the American Association for the Study of Liver Diseases. The investigators disclosed no conflicts.
A hallmark of HCV infection is the association of virus particles with lipoproteins. The HCV virion (lipo-viro particle, LVP) is composed of nucleocapsid and envelope glycoproteins associated with very-low- and low-density lipoproteins, cholesterol, and apolipoproteins. The lipid components determine the size, density, hepatotropism, and infectivity of LVPs and play a role in cell entry, morphogenesis, release, and viral escape mechanisms. LVPs undergo dynamic changes during infection, and dietary triglycerides induce alterations in their biophysical properties and infectivity.
Dr. Andreo and colleagues used humanized Fah–/– mice to analyze the evolution of HCV particles during infection. As previously reported, two viral populations of different densities were detected in mice sera, with higher infectivity observed for the low-density population. The proportions and infectivity of these populations varied during infection, reflecting changes in biochemical features of the virus. Sucrose diet influenced the properties of virus particles; these properties’ changes correlated with a redistribution of triglycerides and cholesterol among lipoproteins.
Changes in biochemical features of the virus during infection represent a fascinating aspect of the structural heterogeneity, which influences HCV infectivity and evolution of the disease. Further studies in experimental models that reproduce the lipoprotein-dependent morphogenesis and release of virus particles, maturation, and intravascular remodeling of HCV-associated lipoproteins would help to develop novel lipid-targeting inhibitors to improve existing therapies.
Agata Budkowska, PhD, is scientific advisor for the department of international affairs at the Institut Pasteur, Paris. She has no conflicts of interest.
A hallmark of HCV infection is the association of virus particles with lipoproteins. The HCV virion (lipo-viro particle, LVP) is composed of nucleocapsid and envelope glycoproteins associated with very-low- and low-density lipoproteins, cholesterol, and apolipoproteins. The lipid components determine the size, density, hepatotropism, and infectivity of LVPs and play a role in cell entry, morphogenesis, release, and viral escape mechanisms. LVPs undergo dynamic changes during infection, and dietary triglycerides induce alterations in their biophysical properties and infectivity.
Dr. Andreo and colleagues used humanized Fah–/– mice to analyze the evolution of HCV particles during infection. As previously reported, two viral populations of different densities were detected in mice sera, with higher infectivity observed for the low-density population. The proportions and infectivity of these populations varied during infection, reflecting changes in biochemical features of the virus. Sucrose diet influenced the properties of virus particles; these properties’ changes correlated with a redistribution of triglycerides and cholesterol among lipoproteins.
Changes in biochemical features of the virus during infection represent a fascinating aspect of the structural heterogeneity, which influences HCV infectivity and evolution of the disease. Further studies in experimental models that reproduce the lipoprotein-dependent morphogenesis and release of virus particles, maturation, and intravascular remodeling of HCV-associated lipoproteins would help to develop novel lipid-targeting inhibitors to improve existing therapies.
Agata Budkowska, PhD, is scientific advisor for the department of international affairs at the Institut Pasteur, Paris. She has no conflicts of interest.
A hallmark of HCV infection is the association of virus particles with lipoproteins. The HCV virion (lipo-viro particle, LVP) is composed of nucleocapsid and envelope glycoproteins associated with very-low- and low-density lipoproteins, cholesterol, and apolipoproteins. The lipid components determine the size, density, hepatotropism, and infectivity of LVPs and play a role in cell entry, morphogenesis, release, and viral escape mechanisms. LVPs undergo dynamic changes during infection, and dietary triglycerides induce alterations in their biophysical properties and infectivity.
Dr. Andreo and colleagues used humanized Fah–/– mice to analyze the evolution of HCV particles during infection. As previously reported, two viral populations of different densities were detected in mice sera, with higher infectivity observed for the low-density population. The proportions and infectivity of these populations varied during infection, reflecting changes in biochemical features of the virus. Sucrose diet influenced the properties of virus particles; these properties’ changes correlated with a redistribution of triglycerides and cholesterol among lipoproteins.
Changes in biochemical features of the virus during infection represent a fascinating aspect of the structural heterogeneity, which influences HCV infectivity and evolution of the disease. Further studies in experimental models that reproduce the lipoprotein-dependent morphogenesis and release of virus particles, maturation, and intravascular remodeling of HCV-associated lipoproteins would help to develop novel lipid-targeting inhibitors to improve existing therapies.
Agata Budkowska, PhD, is scientific advisor for the department of international affairs at the Institut Pasteur, Paris. She has no conflicts of interest.
Hepatitis C virus (HCV) particles are of lowest density and most infectious early in the course of infection, based on findings from a study of chimeric mice.
Over time, however, viral density became more heterogeneous and infectivity fell, reported Ursula Andreo, PhD, of Rockefeller University, New York, with her coinvestigators. A diet of 10% sucrose, which in rats induces hepatic secretion of very-low-density lipoprotein (VLDL), caused HCV particles to become slightly lower density and more infectious in the mice, the researchers reported. Although the shift was “minor,” it “correlated with a trend toward enhanced triglyceride and cholesterol levels in the same fractions,” they wrote. They recommended studying high-fat diets to determine whether altering the VLDL secretion pathway affects the biophysical properties of HCV. “A high-fat diet might have a more significant impact on the lipoprotein profile in this humanized mouse model,” they wrote in Cellular and Molecular Gastroenterology and Hepatology (2017 Jul;4[3]:405-17).
Because HCV tends to associate with lipoproteins, it shows a range of buoyant densities in the blood of infected patients. The “entry, replication, and assembly [of the virion] are linked closely to host lipid and lipoprotein metabolism,” wrote Dr. Andreo and her colleagues.
They created an in vivo model to study the buoyant density and infectivity of HCV particles, as well as their interaction with lipoproteins, by grafting human hepatocytes into the livers of immunodeficient mice that were homozygous recessive for fumarylacetoacetate hydrolase. Next, they infected 13 of these chimeric mice with J6-JFH1, an HCV strain that can establish long-term infections in mice that have human liver grafts (Proc Natl Acad Sci USA. 2006;103[10]:3805-9). The human liver xenograft reconstituted the FAH gene, restoring triglycerides to normal levels in the chimeric mice and creating a suitable “humanlike” model of lipoprotein metabolism, the investigators wrote.
Density fractionation of infectious mouse serum revealed higher infectivity in the low-density fractions soon after infection, which also has been observed in a human liver chimeric mouse model of severe combined immunodeficiency disease, they added. In the HCV model, the human liver grafts were conserved 5 weeks after infection, and the mice had a lower proportion of lighter, infectious HCV particles.
The researchers lacked sufficient material to directly study the composition of virions or detect viral proteins in the various density fractions. However, they determined that apolipoprotein C1 was the lightest fraction and that apolipoprotein E was mainly found in the five lightest fractions. Both these apolipoproteins are “essential factors of HCV infectivity,” and neither redistributed over time, they said. They suggested using immunoelectron microscopy or mass spectrometry to study the nature and infectivity of viral particles further.
In humans, ingesting a high-fat milkshake increases detectable HCV RNA in the VLDL fraction, the researchers noted. In rodents, a sucrose diet also has been found to increase VLDL lipidation and secretion, so they gave five of the infected chimeric mice drinking water containing 10% sucrose. After 5 weeks, these mice had increased infectivity and higher levels of triglycerides and cholesterol, but the effect was small and disappeared after the sucrose was withdrawn.
HCV “circulates as a population of particles of light, as well as dense, buoyant densities, and both are infectious,” the researchers concluded. “Changes in diet, as well as conditions such as fasting and feeding, affect the distribution of HCV buoyant density gradients.”
Funders included the National Institutes of Health and the American Association for the Study of Liver Diseases. The investigators disclosed no conflicts.
Hepatitis C virus (HCV) particles are of lowest density and most infectious early in the course of infection, based on findings from a study of chimeric mice.
Over time, however, viral density became more heterogeneous and infectivity fell, reported Ursula Andreo, PhD, of Rockefeller University, New York, with her coinvestigators. A diet of 10% sucrose, which in rats induces hepatic secretion of very-low-density lipoprotein (VLDL), caused HCV particles to become slightly lower density and more infectious in the mice, the researchers reported. Although the shift was “minor,” it “correlated with a trend toward enhanced triglyceride and cholesterol levels in the same fractions,” they wrote. They recommended studying high-fat diets to determine whether altering the VLDL secretion pathway affects the biophysical properties of HCV. “A high-fat diet might have a more significant impact on the lipoprotein profile in this humanized mouse model,” they wrote in Cellular and Molecular Gastroenterology and Hepatology (2017 Jul;4[3]:405-17).
Because HCV tends to associate with lipoproteins, it shows a range of buoyant densities in the blood of infected patients. The “entry, replication, and assembly [of the virion] are linked closely to host lipid and lipoprotein metabolism,” wrote Dr. Andreo and her colleagues.
They created an in vivo model to study the buoyant density and infectivity of HCV particles, as well as their interaction with lipoproteins, by grafting human hepatocytes into the livers of immunodeficient mice that were homozygous recessive for fumarylacetoacetate hydrolase. Next, they infected 13 of these chimeric mice with J6-JFH1, an HCV strain that can establish long-term infections in mice that have human liver grafts (Proc Natl Acad Sci USA. 2006;103[10]:3805-9). The human liver xenograft reconstituted the FAH gene, restoring triglycerides to normal levels in the chimeric mice and creating a suitable “humanlike” model of lipoprotein metabolism, the investigators wrote.
Density fractionation of infectious mouse serum revealed higher infectivity in the low-density fractions soon after infection, which also has been observed in a human liver chimeric mouse model of severe combined immunodeficiency disease, they added. In the HCV model, the human liver grafts were conserved 5 weeks after infection, and the mice had a lower proportion of lighter, infectious HCV particles.
The researchers lacked sufficient material to directly study the composition of virions or detect viral proteins in the various density fractions. However, they determined that apolipoprotein C1 was the lightest fraction and that apolipoprotein E was mainly found in the five lightest fractions. Both these apolipoproteins are “essential factors of HCV infectivity,” and neither redistributed over time, they said. They suggested using immunoelectron microscopy or mass spectrometry to study the nature and infectivity of viral particles further.
In humans, ingesting a high-fat milkshake increases detectable HCV RNA in the VLDL fraction, the researchers noted. In rodents, a sucrose diet also has been found to increase VLDL lipidation and secretion, so they gave five of the infected chimeric mice drinking water containing 10% sucrose. After 5 weeks, these mice had increased infectivity and higher levels of triglycerides and cholesterol, but the effect was small and disappeared after the sucrose was withdrawn.
HCV “circulates as a population of particles of light, as well as dense, buoyant densities, and both are infectious,” the researchers concluded. “Changes in diet, as well as conditions such as fasting and feeding, affect the distribution of HCV buoyant density gradients.”
Funders included the National Institutes of Health and the American Association for the Study of Liver Diseases. The investigators disclosed no conflicts.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The biophysical properties of the hepatitis C virus evolve during the course of infection and shift with dietary changes.
Major finding: Density fractionation of infectious mouse serum showed higher infectivity in the low-density fractions soon after infection, but heterogeneity subsequently increased while infectivity decreased. A 5-week diet of 10% sucrose produced a minor shift toward infectivity that correlated with redistribution of triglycerides and cholesterol.
Data source: A study of 13 human liver chimeric mice.
Disclosures: Funders included the National Institutes of Health and the American Association for the Study of Liver Diseases. The investigators disclosed no conflicts.
Microbiome predicted response to high-fiber diet
Overweight individuals whose stool samples were abundant in Prevotella species lost about 2.3 kg more body fat on a 6-month high-fiber diet than individuals with a low ratio of Prevotella to Bacteroides, according to a randomized trial of 62 Danish adults.
The findings help explain why a high-fiber diet does not always produce meaningful weight loss, said Mads F. Hjorth, PhD, of the University of Copenhagen, and his associates. An “abundance of Prevotella” in the gut microbiome might underlie the “recent breakthrough in personalized nutrition,” they wrote in the International Journal of Obesity.
At the start of the study, 28 (45%) participants had a high (0.28; 95% confidence interval, 0.11-7.5) ratio of Prevotella to Bacteroides and 34 (55%) had a much lower ratio (0.00007) but did not otherwise differ significantly by age, sex, body weight, or fasting insulin levels. After 26 weeks, the high-Prevotella group lost an average of 3.2 kg more fat on the high-fiber diet than the control diet (P less than .001). In contrast, the low-Prevotella group lost only 0.9 kg more fat with the high-fiber diet, a statistically insignificant difference from the control diet. Changes in waistline circumference reflected the findings – the high-fiber diet produced a 4.8-cm average reduction in the high-Prevotella group, compared with a 0.8-cm reduction in the low-Prevotella group.
Next, the researchers asked all 62 participants to follow the high-fiber diet, but did not provide them with food. After 1 year, the high-Prevotella group had maintained a 1.2-kg weight loss, compared with baseline, while the low-Prevotella group had regained 2.8 kg of body weight (P less than .001). Thus, baseline Prevotella-to-Bacteroides ratio explained a 4-kg difference in responsiveness to the high-fiber diet, the researchers concluded. The difference was even more marked when they excluded eight participants with undetectable levels of Prevotella.
Only two individuals switched from a low to a high Prevotella-to-Bacteroides ratio during the 6-month intervention period, which reflects prior findings that the intestinal microbiome is difficult to shift without “extreme changes, such as complete removal of carbohydrates from the diet,” the researchers wrote. Individual gut microbiome might affect energy absorption from different types of foods, the ability to utilize fiber, gut-brain signaling, or the secretion of hormones affecting appetite, they hypothesized. Thus, Prevotella-to-Bacteroides ratio “may serve as a biomarker to predict future weight loss success on specific diets.”
Gelesis provided funding. Dr. Hjorth and two coinvestigators reported having applied for a patent on the use of biomarkers to predict response to weight loss efforts. The remaining five researchers had no conflicts.
Overweight individuals whose stool samples were abundant in Prevotella species lost about 2.3 kg more body fat on a 6-month high-fiber diet than individuals with a low ratio of Prevotella to Bacteroides, according to a randomized trial of 62 Danish adults.
The findings help explain why a high-fiber diet does not always produce meaningful weight loss, said Mads F. Hjorth, PhD, of the University of Copenhagen, and his associates. An “abundance of Prevotella” in the gut microbiome might underlie the “recent breakthrough in personalized nutrition,” they wrote in the International Journal of Obesity.
At the start of the study, 28 (45%) participants had a high (0.28; 95% confidence interval, 0.11-7.5) ratio of Prevotella to Bacteroides and 34 (55%) had a much lower ratio (0.00007) but did not otherwise differ significantly by age, sex, body weight, or fasting insulin levels. After 26 weeks, the high-Prevotella group lost an average of 3.2 kg more fat on the high-fiber diet than the control diet (P less than .001). In contrast, the low-Prevotella group lost only 0.9 kg more fat with the high-fiber diet, a statistically insignificant difference from the control diet. Changes in waistline circumference reflected the findings – the high-fiber diet produced a 4.8-cm average reduction in the high-Prevotella group, compared with a 0.8-cm reduction in the low-Prevotella group.
Next, the researchers asked all 62 participants to follow the high-fiber diet, but did not provide them with food. After 1 year, the high-Prevotella group had maintained a 1.2-kg weight loss, compared with baseline, while the low-Prevotella group had regained 2.8 kg of body weight (P less than .001). Thus, baseline Prevotella-to-Bacteroides ratio explained a 4-kg difference in responsiveness to the high-fiber diet, the researchers concluded. The difference was even more marked when they excluded eight participants with undetectable levels of Prevotella.
Only two individuals switched from a low to a high Prevotella-to-Bacteroides ratio during the 6-month intervention period, which reflects prior findings that the intestinal microbiome is difficult to shift without “extreme changes, such as complete removal of carbohydrates from the diet,” the researchers wrote. Individual gut microbiome might affect energy absorption from different types of foods, the ability to utilize fiber, gut-brain signaling, or the secretion of hormones affecting appetite, they hypothesized. Thus, Prevotella-to-Bacteroides ratio “may serve as a biomarker to predict future weight loss success on specific diets.”
Gelesis provided funding. Dr. Hjorth and two coinvestigators reported having applied for a patent on the use of biomarkers to predict response to weight loss efforts. The remaining five researchers had no conflicts.
Overweight individuals whose stool samples were abundant in Prevotella species lost about 2.3 kg more body fat on a 6-month high-fiber diet than individuals with a low ratio of Prevotella to Bacteroides, according to a randomized trial of 62 Danish adults.
The findings help explain why a high-fiber diet does not always produce meaningful weight loss, said Mads F. Hjorth, PhD, of the University of Copenhagen, and his associates. An “abundance of Prevotella” in the gut microbiome might underlie the “recent breakthrough in personalized nutrition,” they wrote in the International Journal of Obesity.
At the start of the study, 28 (45%) participants had a high (0.28; 95% confidence interval, 0.11-7.5) ratio of Prevotella to Bacteroides and 34 (55%) had a much lower ratio (0.00007) but did not otherwise differ significantly by age, sex, body weight, or fasting insulin levels. After 26 weeks, the high-Prevotella group lost an average of 3.2 kg more fat on the high-fiber diet than the control diet (P less than .001). In contrast, the low-Prevotella group lost only 0.9 kg more fat with the high-fiber diet, a statistically insignificant difference from the control diet. Changes in waistline circumference reflected the findings – the high-fiber diet produced a 4.8-cm average reduction in the high-Prevotella group, compared with a 0.8-cm reduction in the low-Prevotella group.
Next, the researchers asked all 62 participants to follow the high-fiber diet, but did not provide them with food. After 1 year, the high-Prevotella group had maintained a 1.2-kg weight loss, compared with baseline, while the low-Prevotella group had regained 2.8 kg of body weight (P less than .001). Thus, baseline Prevotella-to-Bacteroides ratio explained a 4-kg difference in responsiveness to the high-fiber diet, the researchers concluded. The difference was even more marked when they excluded eight participants with undetectable levels of Prevotella.
Only two individuals switched from a low to a high Prevotella-to-Bacteroides ratio during the 6-month intervention period, which reflects prior findings that the intestinal microbiome is difficult to shift without “extreme changes, such as complete removal of carbohydrates from the diet,” the researchers wrote. Individual gut microbiome might affect energy absorption from different types of foods, the ability to utilize fiber, gut-brain signaling, or the secretion of hormones affecting appetite, they hypothesized. Thus, Prevotella-to-Bacteroides ratio “may serve as a biomarker to predict future weight loss success on specific diets.”
Gelesis provided funding. Dr. Hjorth and two coinvestigators reported having applied for a patent on the use of biomarkers to predict response to weight loss efforts. The remaining five researchers had no conflicts.
FROM THE INTERNATIONAL JOURNAL OF OBESITY
Key clinical point: Fecal ratio of Prevotella to Bacteroides predicted amount of fat lost on a high-fiber diet.
Major finding: After 26 weeks, individuals with a high Prevotella-to-Bacteroides ratio lost an average of 2.3 kg more fat than individuals with a low ratio (P = .04).
Data source: A randomized prospective trial of 62 adults with increased waist circumference.
Disclosures: Gelesis provided funding. Dr. Hjorth and two coinvestigators reported that they have applied for a patent on the use of biomarkers to predict response to weight loss efforts. The remaining five researchers had no conflicts.
Motesanib flops again in lung cancer
Motesanib has flunked another phase III trial in advanced nonsquamous non–small-cell lung cancer, this time in East Asian patients.
Compared with placebo, the investigational oral vascular endothelial growth factor (VEGF) inhibitor did not significantly improve progression-free survival (PFS) or the secondary endpoint, overall survival (OS), when added to paclitaxel and carboplatin (P/C), reported Kaoru Kubota, MD, of Nippon Medical School, Tokyo, and his associates. “The findings are consistent with overall findings of the phase III MONET1 study but do not replicate those of the subgroup analysis of Asian patients,” they wrote in Journal of Clinical Oncology.
Motesanib is a small-molecular inhibitor of VEGF receptors 1, 2, and 3. In a phase II trial of patients with advanced nonsquamous non–small-cell lung cancer, motesanib resembled the anti-VEGF-A monoclonal antibody bevacizumab in terms of objective response rate, median PFS, and OS when added to paclitaxel and carboplatin. In the subsequent phase III MONET1 trial, however, motesanib plus P/C did not improve PFS over placebo plus P/C, except in a preplanned subgroup analysis of 227 East Asian patients, where it was associated with a 6.4-month greater median PFS (P = .02) and a 1.7-month greater OS (P = .001).
Based on those findings, Dr. Kubota and his associates randomly assigned 401 patients with advanced nonsquamous non–small-cell lung cancer to receive oral motesanib (125 mg) or placebo once daily plus paclitaxel (200 mg/m2 IV) and carboplatin (area under the concentration-time curve, 6 mg/mL per min IV) for up to six 3-week cycles. Patients were from Hong Kong, Korea, Japan, and Taiwan; averaged 65 years of age; and 72% were male (J Clin Oncol. 2017 Sep 13. doi: 10.1200/JCO.2017.72.7297).
After a median follow-up of 10 months, median PFS was 6.1 months in the motesanib plus P/C arm and 5.6 months in the placebo plus P/C arm (hazard ratio, 0.81; P = .08). Respective objective response rates were 60% and 42% (P less than .001), median times to tumor response were 1.4 and 1.6 months, and median durations of response were 5.3 and 4.1 months. Motesanib was associated with a higher rate of serious adverse events (87% versus 68%) and a higher rate of treatment discontinuation due to adverse events (33% versus 14%). Motesanib most often caused gastrointestinal disorders, hypertension, cholecystitis, gallbladder enlargement, and liver disorders.
Takeda Pharmaceuticals makes motesanib and sponsored the trial. Dr. Kubota disclosed honoraria and research funding from numerous pharmaceutical companies excluding Takeda. Four coinvestigators disclosed research funding from Takeda and two coinvestigators reported employment with the company. The remaining five researchers had no conflicts.
Motesanib has flunked another phase III trial in advanced nonsquamous non–small-cell lung cancer, this time in East Asian patients.
Compared with placebo, the investigational oral vascular endothelial growth factor (VEGF) inhibitor did not significantly improve progression-free survival (PFS) or the secondary endpoint, overall survival (OS), when added to paclitaxel and carboplatin (P/C), reported Kaoru Kubota, MD, of Nippon Medical School, Tokyo, and his associates. “The findings are consistent with overall findings of the phase III MONET1 study but do not replicate those of the subgroup analysis of Asian patients,” they wrote in Journal of Clinical Oncology.
Motesanib is a small-molecular inhibitor of VEGF receptors 1, 2, and 3. In a phase II trial of patients with advanced nonsquamous non–small-cell lung cancer, motesanib resembled the anti-VEGF-A monoclonal antibody bevacizumab in terms of objective response rate, median PFS, and OS when added to paclitaxel and carboplatin. In the subsequent phase III MONET1 trial, however, motesanib plus P/C did not improve PFS over placebo plus P/C, except in a preplanned subgroup analysis of 227 East Asian patients, where it was associated with a 6.4-month greater median PFS (P = .02) and a 1.7-month greater OS (P = .001).
Based on those findings, Dr. Kubota and his associates randomly assigned 401 patients with advanced nonsquamous non–small-cell lung cancer to receive oral motesanib (125 mg) or placebo once daily plus paclitaxel (200 mg/m2 IV) and carboplatin (area under the concentration-time curve, 6 mg/mL per min IV) for up to six 3-week cycles. Patients were from Hong Kong, Korea, Japan, and Taiwan; averaged 65 years of age; and 72% were male (J Clin Oncol. 2017 Sep 13. doi: 10.1200/JCO.2017.72.7297).
After a median follow-up of 10 months, median PFS was 6.1 months in the motesanib plus P/C arm and 5.6 months in the placebo plus P/C arm (hazard ratio, 0.81; P = .08). Respective objective response rates were 60% and 42% (P less than .001), median times to tumor response were 1.4 and 1.6 months, and median durations of response were 5.3 and 4.1 months. Motesanib was associated with a higher rate of serious adverse events (87% versus 68%) and a higher rate of treatment discontinuation due to adverse events (33% versus 14%). Motesanib most often caused gastrointestinal disorders, hypertension, cholecystitis, gallbladder enlargement, and liver disorders.
Takeda Pharmaceuticals makes motesanib and sponsored the trial. Dr. Kubota disclosed honoraria and research funding from numerous pharmaceutical companies excluding Takeda. Four coinvestigators disclosed research funding from Takeda and two coinvestigators reported employment with the company. The remaining five researchers had no conflicts.
Motesanib has flunked another phase III trial in advanced nonsquamous non–small-cell lung cancer, this time in East Asian patients.
Compared with placebo, the investigational oral vascular endothelial growth factor (VEGF) inhibitor did not significantly improve progression-free survival (PFS) or the secondary endpoint, overall survival (OS), when added to paclitaxel and carboplatin (P/C), reported Kaoru Kubota, MD, of Nippon Medical School, Tokyo, and his associates. “The findings are consistent with overall findings of the phase III MONET1 study but do not replicate those of the subgroup analysis of Asian patients,” they wrote in Journal of Clinical Oncology.
Motesanib is a small-molecular inhibitor of VEGF receptors 1, 2, and 3. In a phase II trial of patients with advanced nonsquamous non–small-cell lung cancer, motesanib resembled the anti-VEGF-A monoclonal antibody bevacizumab in terms of objective response rate, median PFS, and OS when added to paclitaxel and carboplatin. In the subsequent phase III MONET1 trial, however, motesanib plus P/C did not improve PFS over placebo plus P/C, except in a preplanned subgroup analysis of 227 East Asian patients, where it was associated with a 6.4-month greater median PFS (P = .02) and a 1.7-month greater OS (P = .001).
Based on those findings, Dr. Kubota and his associates randomly assigned 401 patients with advanced nonsquamous non–small-cell lung cancer to receive oral motesanib (125 mg) or placebo once daily plus paclitaxel (200 mg/m2 IV) and carboplatin (area under the concentration-time curve, 6 mg/mL per min IV) for up to six 3-week cycles. Patients were from Hong Kong, Korea, Japan, and Taiwan; averaged 65 years of age; and 72% were male (J Clin Oncol. 2017 Sep 13. doi: 10.1200/JCO.2017.72.7297).
After a median follow-up of 10 months, median PFS was 6.1 months in the motesanib plus P/C arm and 5.6 months in the placebo plus P/C arm (hazard ratio, 0.81; P = .08). Respective objective response rates were 60% and 42% (P less than .001), median times to tumor response were 1.4 and 1.6 months, and median durations of response were 5.3 and 4.1 months. Motesanib was associated with a higher rate of serious adverse events (87% versus 68%) and a higher rate of treatment discontinuation due to adverse events (33% versus 14%). Motesanib most often caused gastrointestinal disorders, hypertension, cholecystitis, gallbladder enlargement, and liver disorders.
Takeda Pharmaceuticals makes motesanib and sponsored the trial. Dr. Kubota disclosed honoraria and research funding from numerous pharmaceutical companies excluding Takeda. Four coinvestigators disclosed research funding from Takeda and two coinvestigators reported employment with the company. The remaining five researchers had no conflicts.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Belying a previous subgroup analysis, motesanib, an investigational oral vascular endothelial growth factor inhibitor, did not significantly improve progression-free survival when added to paclitaxel/carboplatin in East Asian patients with advanced nonsquamous non–small-cell lung cancer.
Major finding: After a median follow-up of 10 months, median PFS was 6.1 months among motesanib recipients and 5.6 months in the placebo group (hazard ratio, 0.81; P = .08).
Data source: A double-blind, phase III trial of 401 patients.
Disclosures: Takeda Pharmaceuticals makes motesanib and sponsored the trial. Dr. Kubota disclosed honoraria and research funding from numerous pharmaceutical companies excluding Takeda. Four coinvestigators disclosed research funding from Takeda and two coinvestigators reported employment with the company. The remaining five researchers had no conflicts.
Roux-en-Y gastric bypass produced durable clinical improvements at 12 years
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
Few prospective studies have tracked long-term outcomes after bariatric surgery. Among 1,156 participants in this study, 418 patients underwent RYGB, 417 individuals sought but did not undergo surgery – mainly for insurance reasons – and 321 individuals did not seek surgery. Participants were mostly females in their 40s or 50s at baseline, and typically weighed 120 kg-130 kg.
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
AGA Resource
Gastroenterologists are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide was created to provide a comprehensive, multi-disciplinary process to personalize innovative obesity care for safe and effective weight management. Learn more at www.gastro.org/obesity.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
Few prospective studies have tracked long-term outcomes after bariatric surgery. Among 1,156 participants in this study, 418 patients underwent RYGB, 417 individuals sought but did not undergo surgery – mainly for insurance reasons – and 321 individuals did not seek surgery. Participants were mostly females in their 40s or 50s at baseline, and typically weighed 120 kg-130 kg.
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
AGA Resource
Gastroenterologists are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide was created to provide a comprehensive, multi-disciplinary process to personalize innovative obesity care for safe and effective weight management. Learn more at www.gastro.org/obesity.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
Few prospective studies have tracked long-term outcomes after bariatric surgery. Among 1,156 participants in this study, 418 patients underwent RYGB, 417 individuals sought but did not undergo surgery – mainly for insurance reasons – and 321 individuals did not seek surgery. Participants were mostly females in their 40s or 50s at baseline, and typically weighed 120 kg-130 kg.
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
AGA Resource
Gastroenterologists are uniquely positioned to lead a care team to help patients with obesity achieve a healthy weight. The AGA Obesity Practice Guide was created to provide a comprehensive, multi-disciplinary process to personalize innovative obesity care for safe and effective weight management. Learn more at www.gastro.org/obesity.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Roux-en-Y gastric bypass produced durable results on numerous clinical outcome measures.
Major finding: Twelve years after surgery, RYGB patients averaged a 27% weight loss from baseline, with a 51% rate of diabetes remission and a 3% incidence of type 2 diabetes mellitus.
Data source: A prospective study of 1,156 severely obese individuals, of whom 418 underwent Roux-en-Y gastric bypass.
Disclosures: Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and the quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Roux-en-Y gastric bypass produced durable clinical improvements at 12 years
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Roux-en-Y gastric bypass produced durable results on numerous clinical outcome measures.
Major finding: Twelve years after surgery, RYGB patients averaged a 27% weight loss from baseline, with a 51% rate of remission and a 3% incidence of type 2 diabetes mellitus.
Data source: A prospective study of 1,156 severely obese individuals, of whom 418 underwent Roux-en-Y gastric bypass.
Disclosures: Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and the quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
ADRs highest among gastroenterologists, women, early-career physicians
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: Adenoma detection rates were highest among gastroenterologists, female physicians, and physicians less than a decade out of residency.
Major finding: On average, their ADRs were 9.4, 6.0, and 4.2 percentage points higher than those of their respective comparison groups, and each difference was statistically significant (all P values less than .03).
Data source: A retrospective cohort study of four diverse health systems.
Disclosures: The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
Statins linked to lower death rates in COPD
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
FROM CHEST
Key clinical point: Statins might reduce the risk of death among patients with chronic obstructive pulmonary disease.
Major finding: Statin use was associated with a 21% decrease in risk of all-cause mortality and a 45% decrease in risk of pulmonary mortality.
Data source: A retrospective cohort study of 39,678 patients with COPD, including 7,775 prescribed statins.
Disclosures: Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Adding T-vec might help surmount PD-1 resistance in melanoma
Almost two-thirds of patients with advanced melanoma responded to combination therapy with pembrolizumab and talimogene laherparepvec (T-vec) in a small phase 1b trial, investigators reported.
A third of patients achieved a complete response and median progression-free and overall survival were not reached after typically 18.6 (range, 17.7 to 20.8) months of follow-up, said Antoni Ribas, MD, of the University of California, Los Angeles, and his coinvestigators. In contrast to single-agent pembrolizumab therapy, responders to the combination regimen included patients with very low levels of CD8+ T cell infiltrates or negative interferon-gamma (IFN-gamma) gene signatures in baseline tumor biopsies, suggesting that oncolytic virotherapy might make anti-PD-1 therapy more effective by altering the tumor microenvironment, the researchers concluded. Serious adverse events were uncommon in this study, and there were no dose-limiting toxicities, they wrote (Cell. 2017 Sept. 7 doi: 10.1016/j.cell.2017.08.027).
To see if attracting CD8+ T cells into tumors helped surmount this obstacle, the researchers treated 21 patients with advanced melanoma with pembrolizumab and T-vec, an intratumorally administered, genetically modified clinical herpes simplex virus-1 strain approved for treating melanoma. Patients first received up to 4 mL T-vec (106 plaque-forming units [pfu] per mL) to induce a protective immune response. Three weeks later, they started receiving to 4 mL (108 pfu/mL) T-vec plus 200 mg intravenous pembrolizumab every 2 weeks.
Thirteen patients (62%) showed at least a partial response, and seven (33%) had a complete response based on immune criteria. Notably, 9 of 13 (69%) patients with baseline tumor CD8+ densities below 1,000 cells/mm2 responded to combination treatment, as did three of five patients with low baseline IFN-gamma signatures.
“There was only one baseline biopsy that was scored as PD-L1 negative, but that patient went on to have a complete response to the combined therapy,” the researchers wrote. “Patients who responded to combination therapy had increased CD8+ T cells, elevated PD-L1 protein expression, [and] IFN-gamma gene expression on several cell subsets in tumors after [T-vec] treatment. Response to combination therapy did not appear to be associated with baseline CD8+ T cell infiltration or baseline IFN-gamma signature.” Increased levels of circulating immune cells and shrinkage of untreated tumors both suggested that intratumoral T-vec injections led to systemic effects, they added.
Amgen and Merck provided funding. Dr. Ribas disclosed consulting fees from both companies.
Almost two-thirds of patients with advanced melanoma responded to combination therapy with pembrolizumab and talimogene laherparepvec (T-vec) in a small phase 1b trial, investigators reported.
A third of patients achieved a complete response and median progression-free and overall survival were not reached after typically 18.6 (range, 17.7 to 20.8) months of follow-up, said Antoni Ribas, MD, of the University of California, Los Angeles, and his coinvestigators. In contrast to single-agent pembrolizumab therapy, responders to the combination regimen included patients with very low levels of CD8+ T cell infiltrates or negative interferon-gamma (IFN-gamma) gene signatures in baseline tumor biopsies, suggesting that oncolytic virotherapy might make anti-PD-1 therapy more effective by altering the tumor microenvironment, the researchers concluded. Serious adverse events were uncommon in this study, and there were no dose-limiting toxicities, they wrote (Cell. 2017 Sept. 7 doi: 10.1016/j.cell.2017.08.027).
To see if attracting CD8+ T cells into tumors helped surmount this obstacle, the researchers treated 21 patients with advanced melanoma with pembrolizumab and T-vec, an intratumorally administered, genetically modified clinical herpes simplex virus-1 strain approved for treating melanoma. Patients first received up to 4 mL T-vec (106 plaque-forming units [pfu] per mL) to induce a protective immune response. Three weeks later, they started receiving to 4 mL (108 pfu/mL) T-vec plus 200 mg intravenous pembrolizumab every 2 weeks.
Thirteen patients (62%) showed at least a partial response, and seven (33%) had a complete response based on immune criteria. Notably, 9 of 13 (69%) patients with baseline tumor CD8+ densities below 1,000 cells/mm2 responded to combination treatment, as did three of five patients with low baseline IFN-gamma signatures.
“There was only one baseline biopsy that was scored as PD-L1 negative, but that patient went on to have a complete response to the combined therapy,” the researchers wrote. “Patients who responded to combination therapy had increased CD8+ T cells, elevated PD-L1 protein expression, [and] IFN-gamma gene expression on several cell subsets in tumors after [T-vec] treatment. Response to combination therapy did not appear to be associated with baseline CD8+ T cell infiltration or baseline IFN-gamma signature.” Increased levels of circulating immune cells and shrinkage of untreated tumors both suggested that intratumoral T-vec injections led to systemic effects, they added.
Amgen and Merck provided funding. Dr. Ribas disclosed consulting fees from both companies.
Almost two-thirds of patients with advanced melanoma responded to combination therapy with pembrolizumab and talimogene laherparepvec (T-vec) in a small phase 1b trial, investigators reported.
A third of patients achieved a complete response and median progression-free and overall survival were not reached after typically 18.6 (range, 17.7 to 20.8) months of follow-up, said Antoni Ribas, MD, of the University of California, Los Angeles, and his coinvestigators. In contrast to single-agent pembrolizumab therapy, responders to the combination regimen included patients with very low levels of CD8+ T cell infiltrates or negative interferon-gamma (IFN-gamma) gene signatures in baseline tumor biopsies, suggesting that oncolytic virotherapy might make anti-PD-1 therapy more effective by altering the tumor microenvironment, the researchers concluded. Serious adverse events were uncommon in this study, and there were no dose-limiting toxicities, they wrote (Cell. 2017 Sept. 7 doi: 10.1016/j.cell.2017.08.027).
To see if attracting CD8+ T cells into tumors helped surmount this obstacle, the researchers treated 21 patients with advanced melanoma with pembrolizumab and T-vec, an intratumorally administered, genetically modified clinical herpes simplex virus-1 strain approved for treating melanoma. Patients first received up to 4 mL T-vec (106 plaque-forming units [pfu] per mL) to induce a protective immune response. Three weeks later, they started receiving to 4 mL (108 pfu/mL) T-vec plus 200 mg intravenous pembrolizumab every 2 weeks.
Thirteen patients (62%) showed at least a partial response, and seven (33%) had a complete response based on immune criteria. Notably, 9 of 13 (69%) patients with baseline tumor CD8+ densities below 1,000 cells/mm2 responded to combination treatment, as did three of five patients with low baseline IFN-gamma signatures.
“There was only one baseline biopsy that was scored as PD-L1 negative, but that patient went on to have a complete response to the combined therapy,” the researchers wrote. “Patients who responded to combination therapy had increased CD8+ T cells, elevated PD-L1 protein expression, [and] IFN-gamma gene expression on several cell subsets in tumors after [T-vec] treatment. Response to combination therapy did not appear to be associated with baseline CD8+ T cell infiltration or baseline IFN-gamma signature.” Increased levels of circulating immune cells and shrinkage of untreated tumors both suggested that intratumoral T-vec injections led to systemic effects, they added.
Amgen and Merck provided funding. Dr. Ribas disclosed consulting fees from both companies.
FROM CELL
Key clinical point: Adding talimogene laherparepvec (T-vec) might help overcome resistance to anti-PD-1 antibodies in patients with advanced melanoma.
Major finding: In all, 62% of patients had at least a partial response and 33% had a complete response. Median progression-free and overall survival were not reached after a median of 18.6 weeks of follow-up.
Data source: A phase 1b clinical trial of 21 adults with advanced melanoma who received T-vec and pembrolizumab.
Disclosures: Amgen and Merck provided funding. Dr. Ribas disclosed consulting fees from both companies.