User login
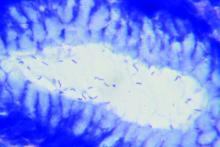
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
Compared with usual care, screening for and the eradication of Helicobacter pylori infection did not significantly improve the risk of dyspepsia or peptic ulcer disease, use of health care services, or quality of life in a large randomized, controlled trial reported in the November issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.06.006).
After 13 years of follow-up, the prevalence of dyspepsia was 19% in both arms (adjusted odds ratio, 0.93; 95% confidence interval, 0.82-1.04), reported Maria Bomme, MD, of University of Southern Denmark (Odense), and her associates. The cumulative risk of the coprimary endpoint, peptic ulcer disease, was 3% in both groups (risk ratio, 0.93; 95% confidence interval, 0.79-1.09). Screening and eradication also did not affect secondary endpoints such as rates of gastroesophageal reflux, endoscopy, antacid use, or health care utilization, or mental and physical quality of life.
The study “was designed to provide evidence on the effect of H. pylori screening at a population scale,” the researchers wrote. “It showed no significant long-term effect of population screening when compared with current clinical practice in a low-prevalence area.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Prior studies have suggested that eradicating H. pylori infection might help prevent peptic ulcers and dyspepsia and could reduce the risk of gastric cancer, the researchers noted. For this trial, they randomly assigned 20,011 adults aged 40-65 years from a single county in Denmark to receive H. pylori screening or usual care. Screening consisted of an outpatient blood test for H. pylori, which was confirmed by 13C-urea breath test (UBT) if positive. Individuals with confirmed infections were offered triple eradication therapy (20 mg omeprazole, 500 mg clarithromycin, and either 1 g amoxicillin or 500 mg metronidazole) twice daily for 1 week. This regimen eradicated 95% of infections, based on UBT results from a subset of 200 individuals.
Compared with nonparticipants, the 12,530 (63%) study enrollees were significantly more likely to be female, 50 years or older, married, and to have a history of peptic ulcer disease. Rates of follow-up were 92% at 1 year, 83% at 5 years, and 69% (8,658 individuals) at 13 years. Among 5,749 screened participants, 17.5% tested positive for H. pylori. Nearly all underwent eradication therapy. At 5 years, screening and eradication were associated with a significant reduction in the incidence of peptic ulcers and associated complications and with modest improvements in dyspepsia, health care visits for dyspepsia, and sick leave days, compared with usual care. But the prevalence of dyspepsia waned in both groups over time and did not significantly differ between groups at 13 years in either the intention-to-treat or per-protocol analysis. Likewise, annual rates of peptic ulcer disease were very similar (1.9 cases/1,000 screened individuals and 2.2 cases/1,000 controls; incidence rate ratio, 0.87; 95% CI, 0.69-1.10). Rates of gastroesophageal cancer also were similar among groups throughout the study.
Screening for and eradicating H. pylori also did not affect the likelihood of dyspepsia or peptic ulcer disease at 13 years among individuals who were dyspeptic at baseline, the researchers said. The relatively low prevalence of H. pylori infection in Denmark might have diluted the effects of screening and eradication, they added.
Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Screening for and eradicating H. pylori infections did not significantly improve long-term prevalence of dyspepsia, incidence of peptic ulcer disease, use of health care services, or quality of life.
Major finding: At 13-year follow-up, both arms had a 19% prevalence of dyspepsia (aOR, 0.93; 95% CI, 0.82-1.04) and a 3% cumulative incidence of peptic ulcer disease (RR, 0.93; 95% CI, 0.79-1.09).
Data source: A randomized controlled trial of 8,658 adults aged 40-65 years
Disclosures: Funders included the Region of Southern Denmark, the department of clinical research at the University of Southern Denmark, the Odense University Hospital research board, and the Aase and Ejnar Danielsens Foundation, Beckett- Fonden, and Helsefonden. The researchers reported having no conflicts of interest.