User login
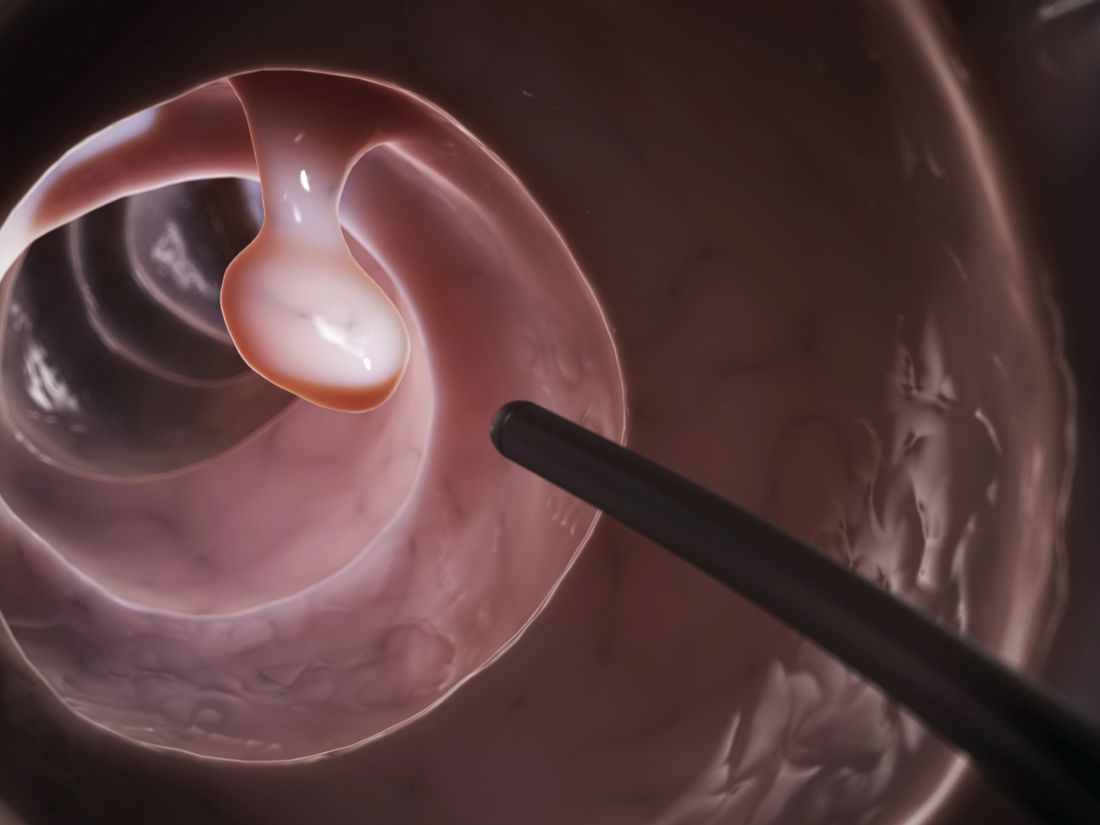
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
Gastroenterologists, female physicians, and physicians who were less than a decade out of residency had significantly higher adenoma detection rates (ADRs) than their counterparts in a retrospective cohort study of colonoscopists.
“Efforts to target physicians with lower-quality performance are needed,” wrote Ateev Mehrotra, MD, MPH, of Harvard Medical School in Boston, with his associates. The study, one of the first to use natural language processing to compare electronic health data from geographically diverse health care systems, was published online 30 in Gastrointestinal Endoscopy (2017 Aug 30. doi: 10.1016/j.gie.2017.08.023).
These associations persisted among patients who received only screening colonoscopies, who had complete colonoscopies with adequate bowel preparation, or who were younger than 80 years, the researchers said. The findings on sex reflect recent studies in which treatment by female hospitalists slightly decreased the risk of 30-day mortality when compared with treatment by a male hospitalist, they added. “A deliberate and meticulous approach to colonoscopy may facilitate achievement of a high ADR, and this method may be more common among female physicians,” they wrote. “This is supported by research showing that female physicians are more likely to adhere to clinical guidelines and to provide preventive care.” Studies of men in other fields have found them more likely to take risks, which contradicts the methodical approach needed for a high ADR, they emphasized. “Sex differences in color perception [also] may make it easier for female physicians to identify adenomas.”
Likewise, research outside gastroenterology has linked fewer years in practice with better quality of care. Improvements in fellowship training, better access to new equipment, “or simply decay of performance with age” all could explain the findings, the researchers wrote. They also cited five prior studies in which nongastroenterologists had lower ADRs. They called for studies that would further explore the reasons why specific physician traits affect performance.
Physicians in the study tended to have practiced fewer years than gastroenterologists in general in the United States, the investigators noted. “We also could not measure some other physician factors that might explain some of the variation we observed, such as type of endoscopes used.”
The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: Adenoma detection rates were highest among gastroenterologists, female physicians, and physicians less than a decade out of residency.
Major finding: On average, their ADRs were 9.4, 6.0, and 4.2 percentage points higher than those of their respective comparison groups, and each difference was statistically significant (all P values less than .03).
Data source: A retrospective cohort study of four diverse health systems.
Disclosures: The National Cancer Institute provided funding. The researchers did not report having conflicts of interest.