User login
Joint effort: CBD not just innocent bystander in weed
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.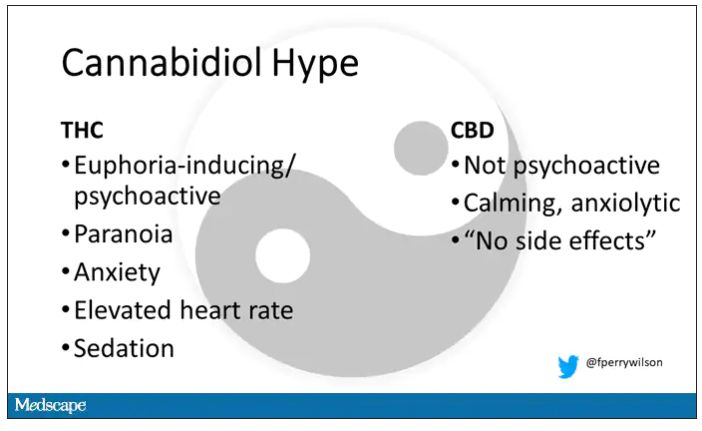
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.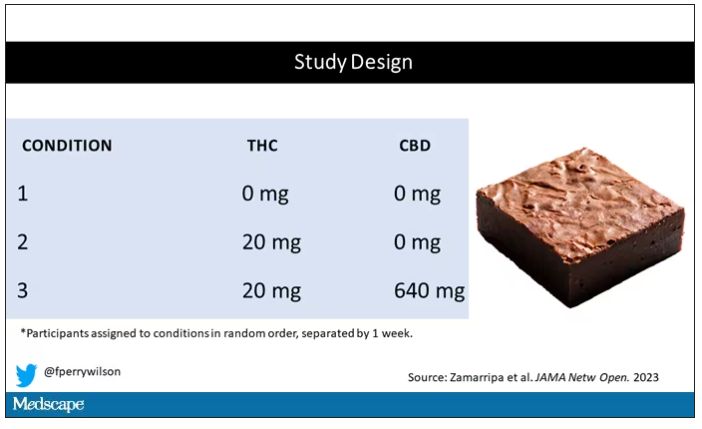
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.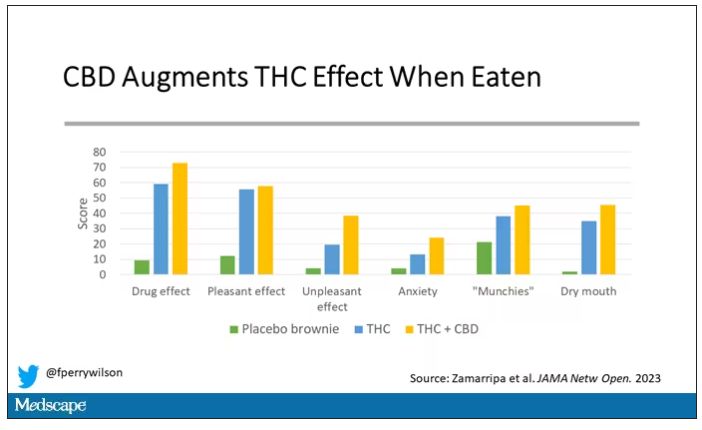
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.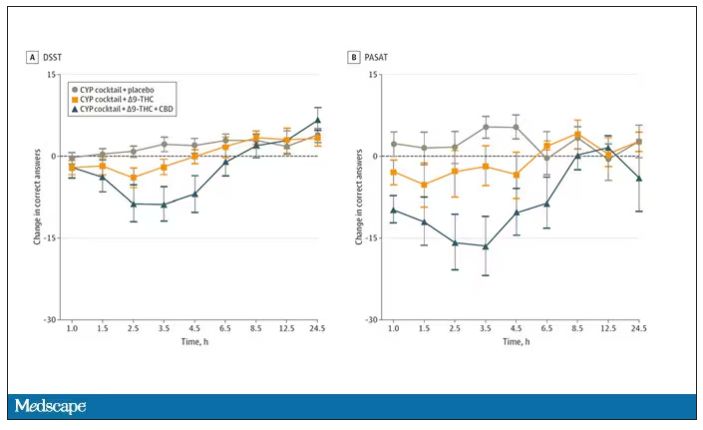
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.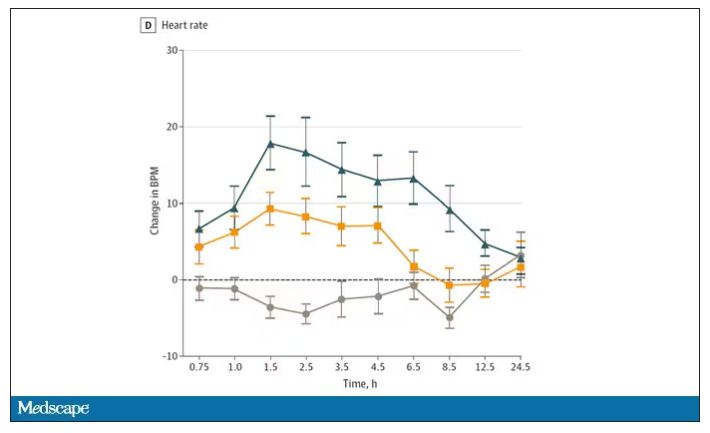
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.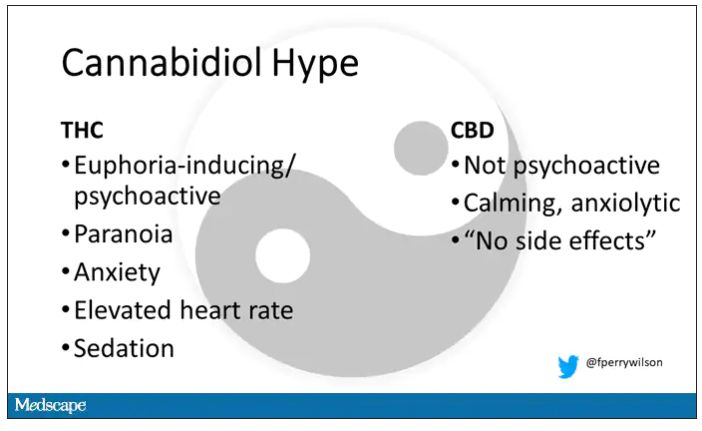
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.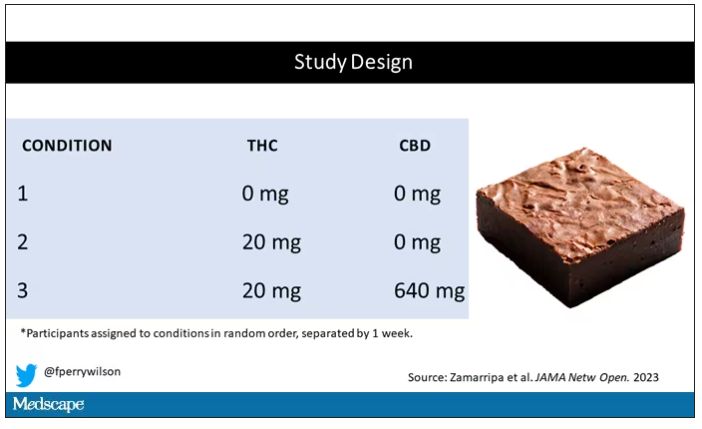
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.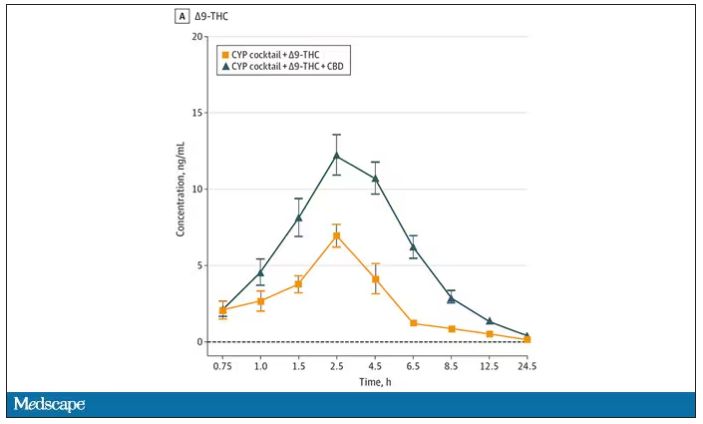
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.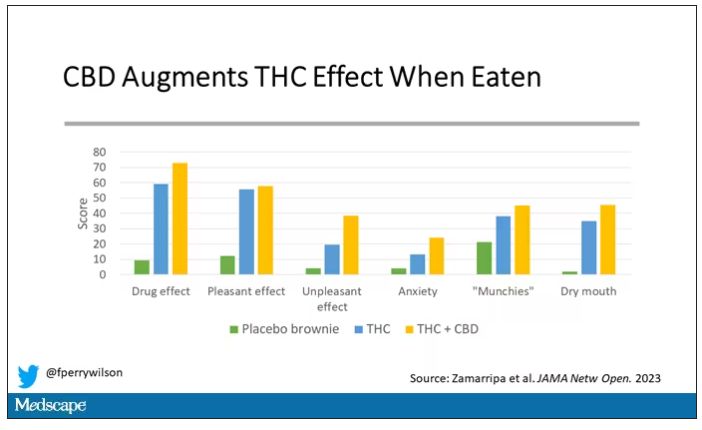
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.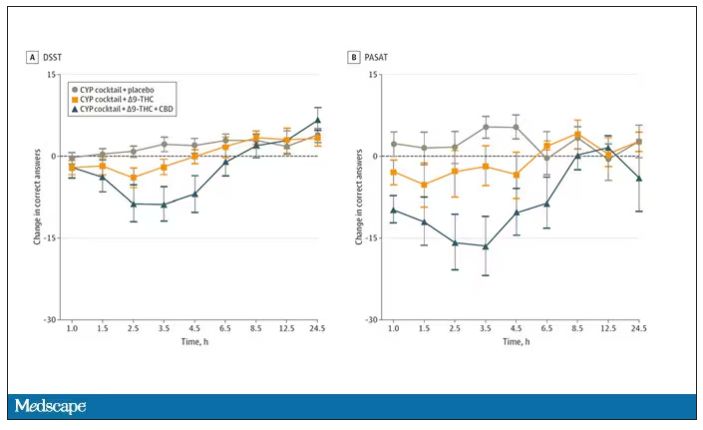
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.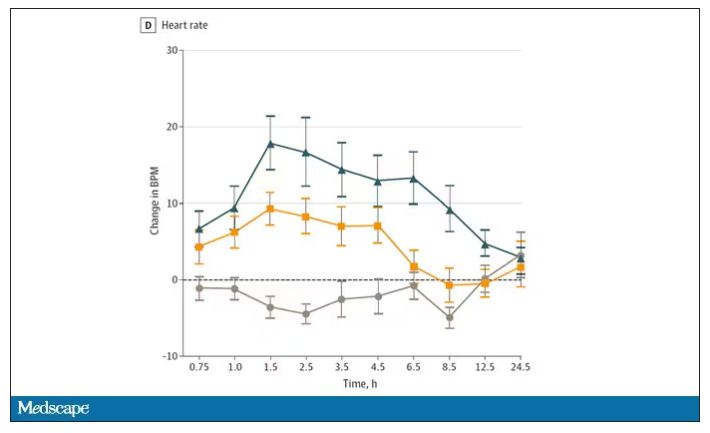
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.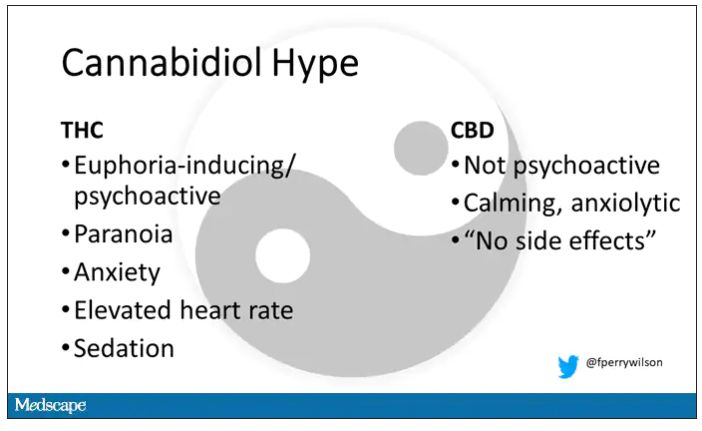
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.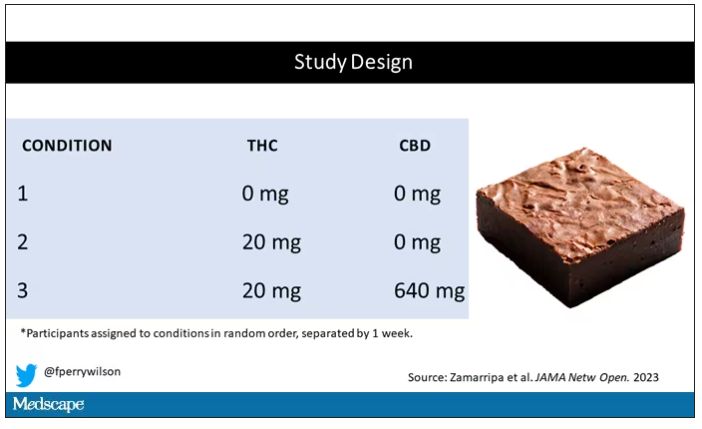
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.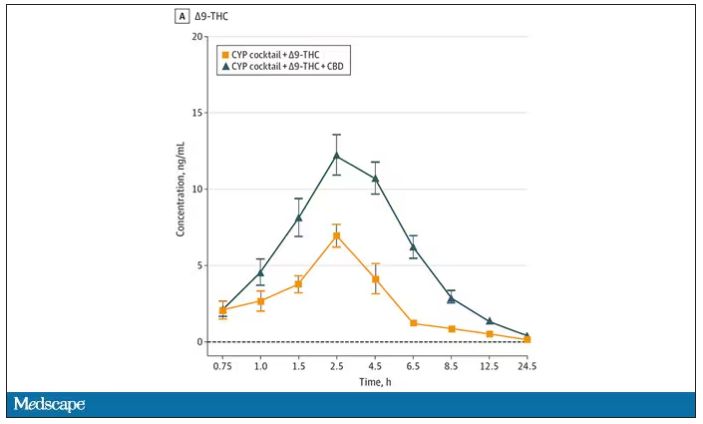
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.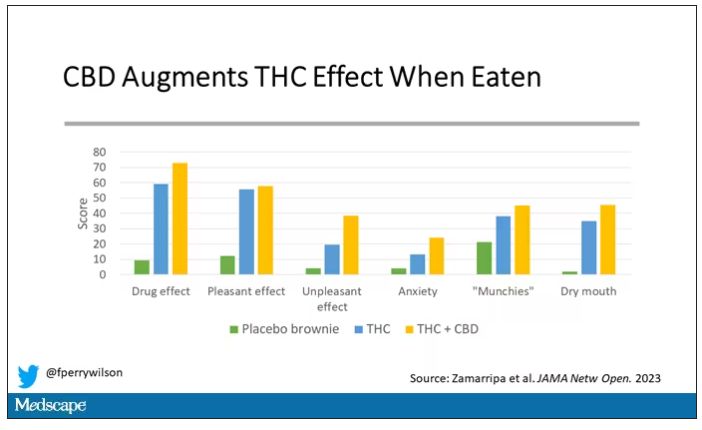
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.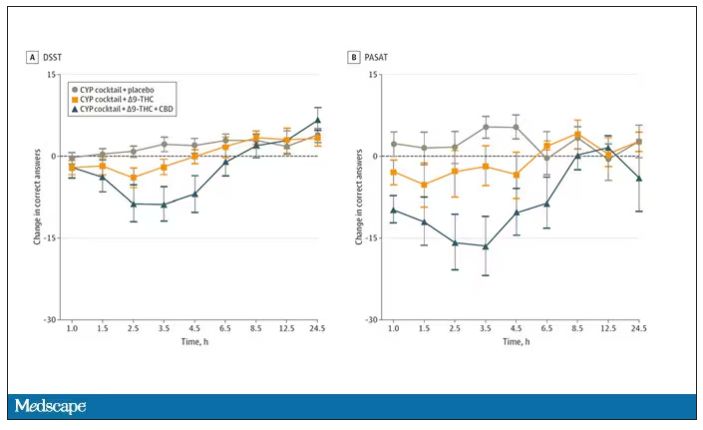
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.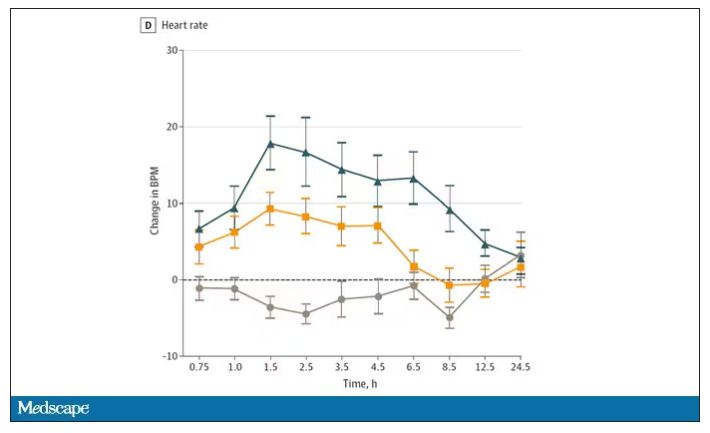
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
The 5-year survival rate for pancreatic cancer is increasing
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
Forced hospitalization for mental illness not a permanent solution
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
I met Eleanor when I was writing a book on involuntary psychiatric treatment. She was very ill when she presented to an emergency department in Northern California. She was looking for help and would have signed herself in, but after waiting 8 hours with no food or medical attention, she walked out and went to another hospital.
At this point, she was agitated and distressed and began screaming uncontrollably. The physician in the second ED did not offer her the option of signing in, and she was placed on a 72-hour hold and subsequently held in the hospital for 3 weeks after a judge committed her.
Like so many issues, involuntary psychiatric care is highly polarized. Some groups favor legislation to make involuntary treatment easier, while patient advocacy and civil rights groups vehemently oppose such legislation.
We don’t hear from these combatants as much as we hear from those who trumpet their views on abortion or gun control, yet this battlefield exists. It is not surprising that when New York City Mayor Eric Adams announced a plan to hospitalize homeless people with mental illnesses – involuntarily if necessary, and at the discretion of the police – people were outraged.
New York City is not the only place using this strategy to address the problem of mental illness and homelessness; California has enacted similar legislation, and every major city has homeless citizens.
Eleanor was not homeless, and fortunately, she recovered and returned to her family. However, she remained distressed and traumatized by her hospitalization for years. “It sticks with you,” she told me. “I would rather die than go in again.”
I wish I could tell you that Eleanor is unique in saying that she would rather die than go to a hospital unit for treatment, but it is not an uncommon sentiment for patients. Some people who are charged with crimes and end up in the judicial system will opt to go to jail rather than to a psychiatric hospital. It is also not easy to access outpatient psychiatric treatment.
Barriers to care
Many psychiatrists don’t participate with insurance networks, and publicly funded clinics may have long waiting lists, so illnesses escalate until there is a crisis and hospitalization is necessary. For many, stigma and fear of potential professional repercussions are significant barriers to care.
What are the issues that legislation attempts to address? The first is the standard for hospitalizing individuals against their will. In some states, the patient must be dangerous, while in others there is a lower standard of “gravely disabled,” and finally there are those that promote a standard of a “need for treatment.”
The second is related to medicating people against their will, a process that can be rightly perceived as an assault if the patient refuses to take oral medications and must be held down for injections. Next, the use of outpatient civil commitment – legally requiring people to get treatment if they are not in the hospital – has been increasingly invoked as a way to prevent mass murders and random violence against strangers.
All but four states have some legislation for outpatient commitment, euphemistically called Assisted Outpatient Treatment (AOT), yet these laws are difficult to enforce and expensive to enact. They are also not fully effective.
In New York City, Kendra’s Law has not eliminated subway violence by people with psychiatric disturbances, and the shooter who killed 32 people and wounded 17 others at Virginia Tech in 2007 had previously been ordered by a judge to go to outpatient treatment, but he simply never showed up for his appointment.
Finally, the battle includes the right of patients to refuse to have their psychiatric information released to their caretakers under the Health Insurance Portability and Accountability Act of 1996 – a measure that many families believe would help them to get loved ones to take medications and go to appointments.
The concern about how to negotiate the needs of society and the civil rights of people with psychiatric disorders has been with us for centuries. There is a strong antipsychiatry movement that asserts that psychotropic medications are ineffective or harmful and refers to patients as “psychiatric survivors.” We value the right to medical autonomy, and when there is controversy over the validity of a treatment, there is even more controversy over forcing it upon people.
Psychiatric medications are very effective and benefit many people, but they don’t help everyone, and some people experience side effects. Also, we can’t deny that involuntary care can go wrong; the conservatorship of Britney Spears for 13 years is a very public example.
Multiple stakeholders
Many have a stake in how this plays out. There are the patients, who may be suffering and unable to recognize that they are ill, who may have valid reasons for not wanting the treatments, and who ideally should have the right to refuse care.
There are the families who watch their loved ones suffer, deteriorate, and miss the opportunities that life has to offer; who do not want their children to be homeless or incarcerated; and who may be at risk from violent behavior.
There are the mental health professionals who want to do what’s in the best interest of their patients while following legal and ethical mandates, who worry about being sued for tragic outcomes, and who can’t meet the current demand for services.
There is the taxpayer who foots the bill for disability payments, lost productivity, and institutionalization. There is our society that worries that people with psychiatric disorders will commit random acts of violence.
Finally, there are the insurers, who want to pay for as little care as possible and throw up constant hurdles in the treatment process. We must acknowledge that resources used for involuntary treatment are diverted away from those who want care.
Eleanor had many advantages that unhoused people don’t have: a supportive family, health insurance, and the financial means to pay a psychiatrist who respected her wishes to wean off her medications. She returned to a comfortable home and to personal and occupational success.
It is tragic that we have people living on the streets because of a psychiatric disorder, addiction, poverty, or some combination of these. No one should be unhoused. If the rationale of hospitalization is to decrease violence, I am not hopeful. The Epidemiologic Catchment Area study shows that people with psychiatric disorders are responsible for only 4% of all violence.
The logistics of determining which people living on the streets have psychiatric disorders, transporting them safely to medical facilities, and then finding the resources to provide for compassionate and thoughtful care in meaningful and sustained ways are very challenging.
If we don’t want people living on the streets, we need to create supports, including infrastructure to facilitate housing, access to mental health care, and addiction treatment before we resort to involuntary hospitalization.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
An 11-year-old boy presents with small itchy bumps on the wrists, face, arms, and legs
The patient was diagnosed with lichen nitidus, given the characteristic clinical presentation.
Lichen nitidus is a rare chronic inflammatory condition of the skin that most commonly presents in children and young adults and does not seem to be restricted to any sex or race. The classic lesions are described as asymptomatic to slightly pruritic, small (1 mm), skin-colored to hypopigmented flat-topped papules.
Koebner phenomenon is usually seen in which the skin lesions appear in areas of traumatized healthy skin. The extremities, abdomen, chest, and penis are common locations for the lesions to occur. Rarely, the oral mucosa or nails can be involved. It has been described in patients with a diagnosis of Crohn’s disease, Niemann-Pick disease, Down syndrome, and HIV. The rare, generalized purpuric variant has been reported in a few cases associated with interferon and ribavirin treatment for hepatitis C infection and nivolumab treatment for cancer. The pathophysiology of lichen nitidus is unknown.
Lichen nitidus can occur in the presence of other skin conditions like lichen planus, atopic dermatitis, vitiligo, erythema nodosum, and lichen spinulosus. Histopathologic characteristics of lichen nitidus are described as a “ball and claw” of epidermal rete around a lymphohistiocytic infiltrate. Parakeratosis overlying epidermal atrophy and focal basal liquefaction degeneration is also seen.
The differential diagnosis of lichen nitidus includes flat warts, which can present as clusters of small flat-topped papules that can show a pseudo-Koebner phenomenon (where the virus is seeded in traumatized skin). The morphological difference between the condition is that lichen nitidus lesions are usually monomorphic, compared with flat warts, which usually present with different sizes and shapes.
Patients with a history of allergic contact dermatitis may present with a generalized monomorphic eruption of skin-colored papules (known as ID reaction) that can sometimes be very similar to lichen nitidus. Allergic contact dermatitis tends to respond fairly quickly to topical or systemic corticosteroids, unlike lichen nitidus. There are a few reports that consider lichen nitidus to be a variant of lichen planus, although they have different histopathologic findings. Lichen planus lesions are described as polygonal, pruritic, purple to pink papules most commonly seen on the wrists, lower back, and ankles. Lichen planus can be seen in patients with hepatitis C and may also occur secondary to medication.
Milia are small keratin cysts on the skin that are commonly seen in babies as primary milia and can be seen in older children secondary to trauma (commonly on the eyelids) or medications. Given their size and monomorphic appearance, they can sometimes be confused with lichen nitidus.
Lichen nitidus is often asymptomatic and the lesions resolve within a few months to years. Topical corticosteroids can be helpful to alleviate the symptoms in patients who present with pruritus. In more persistent and generalized cases, phototherapy, systemic corticosteroids, acitretin, isotretinoin, or cyclosporine can be considered.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Chu J and Lam JM. CMAJ. 2014 Dec 9;186(18):E688.
Lestringant G et al. Dermatology 1996;192:171-3.
Peterson JA et al. Proc (Bayl Univ Med Cent). 2021 Aug 25;35(1):70-2.
Schwartz C and Goodman MB. “Lichen nitidus,” in StatPearls. Treasure Island, Fla.: StatPearls Publishing, 2022.
The patient was diagnosed with lichen nitidus, given the characteristic clinical presentation.
Lichen nitidus is a rare chronic inflammatory condition of the skin that most commonly presents in children and young adults and does not seem to be restricted to any sex or race. The classic lesions are described as asymptomatic to slightly pruritic, small (1 mm), skin-colored to hypopigmented flat-topped papules.
Koebner phenomenon is usually seen in which the skin lesions appear in areas of traumatized healthy skin. The extremities, abdomen, chest, and penis are common locations for the lesions to occur. Rarely, the oral mucosa or nails can be involved. It has been described in patients with a diagnosis of Crohn’s disease, Niemann-Pick disease, Down syndrome, and HIV. The rare, generalized purpuric variant has been reported in a few cases associated with interferon and ribavirin treatment for hepatitis C infection and nivolumab treatment for cancer. The pathophysiology of lichen nitidus is unknown.
Lichen nitidus can occur in the presence of other skin conditions like lichen planus, atopic dermatitis, vitiligo, erythema nodosum, and lichen spinulosus. Histopathologic characteristics of lichen nitidus are described as a “ball and claw” of epidermal rete around a lymphohistiocytic infiltrate. Parakeratosis overlying epidermal atrophy and focal basal liquefaction degeneration is also seen.
The differential diagnosis of lichen nitidus includes flat warts, which can present as clusters of small flat-topped papules that can show a pseudo-Koebner phenomenon (where the virus is seeded in traumatized skin). The morphological difference between the condition is that lichen nitidus lesions are usually monomorphic, compared with flat warts, which usually present with different sizes and shapes.
Patients with a history of allergic contact dermatitis may present with a generalized monomorphic eruption of skin-colored papules (known as ID reaction) that can sometimes be very similar to lichen nitidus. Allergic contact dermatitis tends to respond fairly quickly to topical or systemic corticosteroids, unlike lichen nitidus. There are a few reports that consider lichen nitidus to be a variant of lichen planus, although they have different histopathologic findings. Lichen planus lesions are described as polygonal, pruritic, purple to pink papules most commonly seen on the wrists, lower back, and ankles. Lichen planus can be seen in patients with hepatitis C and may also occur secondary to medication.
Milia are small keratin cysts on the skin that are commonly seen in babies as primary milia and can be seen in older children secondary to trauma (commonly on the eyelids) or medications. Given their size and monomorphic appearance, they can sometimes be confused with lichen nitidus.
Lichen nitidus is often asymptomatic and the lesions resolve within a few months to years. Topical corticosteroids can be helpful to alleviate the symptoms in patients who present with pruritus. In more persistent and generalized cases, phototherapy, systemic corticosteroids, acitretin, isotretinoin, or cyclosporine can be considered.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Chu J and Lam JM. CMAJ. 2014 Dec 9;186(18):E688.
Lestringant G et al. Dermatology 1996;192:171-3.
Peterson JA et al. Proc (Bayl Univ Med Cent). 2021 Aug 25;35(1):70-2.
Schwartz C and Goodman MB. “Lichen nitidus,” in StatPearls. Treasure Island, Fla.: StatPearls Publishing, 2022.
The patient was diagnosed with lichen nitidus, given the characteristic clinical presentation.
Lichen nitidus is a rare chronic inflammatory condition of the skin that most commonly presents in children and young adults and does not seem to be restricted to any sex or race. The classic lesions are described as asymptomatic to slightly pruritic, small (1 mm), skin-colored to hypopigmented flat-topped papules.
Koebner phenomenon is usually seen in which the skin lesions appear in areas of traumatized healthy skin. The extremities, abdomen, chest, and penis are common locations for the lesions to occur. Rarely, the oral mucosa or nails can be involved. It has been described in patients with a diagnosis of Crohn’s disease, Niemann-Pick disease, Down syndrome, and HIV. The rare, generalized purpuric variant has been reported in a few cases associated with interferon and ribavirin treatment for hepatitis C infection and nivolumab treatment for cancer. The pathophysiology of lichen nitidus is unknown.
Lichen nitidus can occur in the presence of other skin conditions like lichen planus, atopic dermatitis, vitiligo, erythema nodosum, and lichen spinulosus. Histopathologic characteristics of lichen nitidus are described as a “ball and claw” of epidermal rete around a lymphohistiocytic infiltrate. Parakeratosis overlying epidermal atrophy and focal basal liquefaction degeneration is also seen.
The differential diagnosis of lichen nitidus includes flat warts, which can present as clusters of small flat-topped papules that can show a pseudo-Koebner phenomenon (where the virus is seeded in traumatized skin). The morphological difference between the condition is that lichen nitidus lesions are usually monomorphic, compared with flat warts, which usually present with different sizes and shapes.
Patients with a history of allergic contact dermatitis may present with a generalized monomorphic eruption of skin-colored papules (known as ID reaction) that can sometimes be very similar to lichen nitidus. Allergic contact dermatitis tends to respond fairly quickly to topical or systemic corticosteroids, unlike lichen nitidus. There are a few reports that consider lichen nitidus to be a variant of lichen planus, although they have different histopathologic findings. Lichen planus lesions are described as polygonal, pruritic, purple to pink papules most commonly seen on the wrists, lower back, and ankles. Lichen planus can be seen in patients with hepatitis C and may also occur secondary to medication.
Milia are small keratin cysts on the skin that are commonly seen in babies as primary milia and can be seen in older children secondary to trauma (commonly on the eyelids) or medications. Given their size and monomorphic appearance, they can sometimes be confused with lichen nitidus.
Lichen nitidus is often asymptomatic and the lesions resolve within a few months to years. Topical corticosteroids can be helpful to alleviate the symptoms in patients who present with pruritus. In more persistent and generalized cases, phototherapy, systemic corticosteroids, acitretin, isotretinoin, or cyclosporine can be considered.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Chu J and Lam JM. CMAJ. 2014 Dec 9;186(18):E688.
Lestringant G et al. Dermatology 1996;192:171-3.
Peterson JA et al. Proc (Bayl Univ Med Cent). 2021 Aug 25;35(1):70-2.
Schwartz C and Goodman MB. “Lichen nitidus,” in StatPearls. Treasure Island, Fla.: StatPearls Publishing, 2022.
An 11-year-old male with a prior history of atopic dermatitis as a young child, presents with 6 months of slightly itchy, small bumps on the wrists, face, arms, and legs. Has been treated with fluocinolone oil and hydrocortisone 2.5% for a month with no change in the lesions. Besides the use of topical corticosteroids, he has not been taking any other medications.
On physical examination he has multiple skin-colored, flat-topped papules that coalesce into plaques on the arms, legs, chest, and back (Photo 1). Koebner phenomenon was also seen on the knees and arms. There were no lesions in the mouth or on the nails.
Scams
It’s amazing how many phone calls I get from different agencies and groups:
The Drug Enforcement Administration – A car rented in your name was found with fentanyl in the trunk.
The Maricopa County Sheriff’s Department – There is a warrant for your arrest due to failure to show up for jury duty and/or as an expert witness.
Doctors Without Borders – We treated one of your patients while they were overseas and need payment for the supplies used.
The Arizona Medical Board – Your license has been suspended.
The Department of Health & Human Services – Your patient database has been posted on the dark web.
Of course, any of these problems can be fixed simply paying the caller a fee by credit card, Bitcoin, or purchasing gift cards and reading off the numbers to them.
Really.
As you’ve probably guessed, none of these calls are real, they’re just popular scams that have been circulating among doctors’ (and other) offices for the last several years. You may have gotten some of them yourself.
I’m sure the vast majority of us don’t fall for them, but the scammer on the other end doesn’t care.
And, realistically, that sucker could be any of us on a bad day. Timing is everything. If we’re frazzled by office events, or aware that the local medical board is looking into something, or have just been up all night at the hospital and are exhausted ... that’s when we’re most vulnerable, our razor’s edge is dull, our thought process slowed, and maybe at that moment we are just not as able to think clearly.
If I were younger I’d probably be more inclined to waste time messing around with them for the entertainment, trying to get them to give up on me after a while. But nowadays I have neither the time nor interest for that. In the rare cases that they make it past my secretary (which is pretty hard) I just hang up.
I’m not sure if it says more about us or them that this happens. I suppose doctors’ offices are the low-hanging fruit where they assume there’s money and (hopefully) someone who’s either gullible, not paying attention, or just not on top of things. As with any other business, if it weren’t profitable they wouldn’t do it. The best we can do is to make it as unprofitable as possible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s amazing how many phone calls I get from different agencies and groups:
The Drug Enforcement Administration – A car rented in your name was found with fentanyl in the trunk.
The Maricopa County Sheriff’s Department – There is a warrant for your arrest due to failure to show up for jury duty and/or as an expert witness.
Doctors Without Borders – We treated one of your patients while they were overseas and need payment for the supplies used.
The Arizona Medical Board – Your license has been suspended.
The Department of Health & Human Services – Your patient database has been posted on the dark web.
Of course, any of these problems can be fixed simply paying the caller a fee by credit card, Bitcoin, or purchasing gift cards and reading off the numbers to them.
Really.
As you’ve probably guessed, none of these calls are real, they’re just popular scams that have been circulating among doctors’ (and other) offices for the last several years. You may have gotten some of them yourself.
I’m sure the vast majority of us don’t fall for them, but the scammer on the other end doesn’t care.
And, realistically, that sucker could be any of us on a bad day. Timing is everything. If we’re frazzled by office events, or aware that the local medical board is looking into something, or have just been up all night at the hospital and are exhausted ... that’s when we’re most vulnerable, our razor’s edge is dull, our thought process slowed, and maybe at that moment we are just not as able to think clearly.
If I were younger I’d probably be more inclined to waste time messing around with them for the entertainment, trying to get them to give up on me after a while. But nowadays I have neither the time nor interest for that. In the rare cases that they make it past my secretary (which is pretty hard) I just hang up.
I’m not sure if it says more about us or them that this happens. I suppose doctors’ offices are the low-hanging fruit where they assume there’s money and (hopefully) someone who’s either gullible, not paying attention, or just not on top of things. As with any other business, if it weren’t profitable they wouldn’t do it. The best we can do is to make it as unprofitable as possible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s amazing how many phone calls I get from different agencies and groups:
The Drug Enforcement Administration – A car rented in your name was found with fentanyl in the trunk.
The Maricopa County Sheriff’s Department – There is a warrant for your arrest due to failure to show up for jury duty and/or as an expert witness.
Doctors Without Borders – We treated one of your patients while they were overseas and need payment for the supplies used.
The Arizona Medical Board – Your license has been suspended.
The Department of Health & Human Services – Your patient database has been posted on the dark web.
Of course, any of these problems can be fixed simply paying the caller a fee by credit card, Bitcoin, or purchasing gift cards and reading off the numbers to them.
Really.
As you’ve probably guessed, none of these calls are real, they’re just popular scams that have been circulating among doctors’ (and other) offices for the last several years. You may have gotten some of them yourself.
I’m sure the vast majority of us don’t fall for them, but the scammer on the other end doesn’t care.
And, realistically, that sucker could be any of us on a bad day. Timing is everything. If we’re frazzled by office events, or aware that the local medical board is looking into something, or have just been up all night at the hospital and are exhausted ... that’s when we’re most vulnerable, our razor’s edge is dull, our thought process slowed, and maybe at that moment we are just not as able to think clearly.
If I were younger I’d probably be more inclined to waste time messing around with them for the entertainment, trying to get them to give up on me after a while. But nowadays I have neither the time nor interest for that. In the rare cases that they make it past my secretary (which is pretty hard) I just hang up.
I’m not sure if it says more about us or them that this happens. I suppose doctors’ offices are the low-hanging fruit where they assume there’s money and (hopefully) someone who’s either gullible, not paying attention, or just not on top of things. As with any other business, if it weren’t profitable they wouldn’t do it. The best we can do is to make it as unprofitable as possible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Facial lipoatrophy with semaglutide-related weight loss
Ozempic and Wegovy are two prescription drugs that have transformed the management of type 2 diabetes and obesity. Both are a form of semaglutide; the Food and Drug Administration approved Ozempic for treating type 2 diabetes in 2017, followed by Wegovy in 2021 for weight loss in adults with obesity or those who are overweight and have least one weight-related health condition, such as hypertension or hypercholesterolemia. Ozempic is not approved for weight loss, but it has been prescribed off label for that purpose.
An effective treatment, participants with overweight or obesity in one study experienced almost a mean 15% drop in body weight with subcutaneous semaglutide administered once a week versus about 2% with placebo after 68 weeks.
In 2022, high demand and global supply constraints gave rise to shortages of both medications. The FDA reported a Wegovy shortage in March 2022, followed by an Ozempic shortage in August. Social media attention and increased off-label prescribing, with some patients purporting to have had significant improvements with weight loss and their quality of life, including having their clothing fit better and being able to bend over and tie their shoes, increased attention on these medications to the point that off-label prescribing of both drugs for weight loss resulted in some patients with type 2 diabetes unable to receive their medication on time. In late January 2023, NBC reported that Ozempic prescriptions had “tripled from 2021 to 2022,” based on data from the prescription drug discount company SingleCare.
Semaglutide is designed to mimic a hormone that signals to the brain when a person is full and promotes the release of insulin. In turn, the medications can result in lower blood glucose levels, appetite suppression, and reduced caloric intake. Injected once weekly, the medication, a glucagonlike peptide–1 receptor agonist, specifically, activates GLP-1 receptors in the brain, increasing insulin secretion, decreasing glucagon secretion, and delaying gastric emptying (acting as an incretin mimetic).
‘Ozempic face’
Common adverse events with semaglutide can include nausea, vomiting, diarrhea, abdominal pain, constipation, and injection-site reactions. Rare, but more severe adverse events may include thyroid C-cell tumor (in animal studies), medullary thyroid cancer risk, hypersensitivity reaction, anaphylaxis, acute renal injury, chronic renal failure exacerbation, pancreatitis, and cholelithiasis.
A less severe but noticeable side effect that has gained attention is facial wasting and aging, reportedly coined “Ozempic face” by a dermatologist interviewed for an article published in January in The New York Times.
As of Feb. 9, TikTok videos from individuals describing their personal experiences, health care professionals, and others with the tag #ozempicface had 4.8 million views.
Theories as to why noticeable facial changes occur with these medications include: accelerated loss of facial pads that already tend to diminish or shift with normal aging, as well as the inability of skin elasticity to keep up with the loss of volume (fat), resulting in more prominent hanging skin and the appearance of “jowls.” Wan and colleagues have described the fat pad distribution in the face and the facial aging that occurs as a result of the loss and shifting of these fat pads over time.
In the same way that we use facial fillers to help treat and correct volume/fat loss associated with photoaging, facial fillers may be used to help restore volume where it’s been lost after weight loss. The sagging skin or loss of elasticity often associated with Ozempic-related weight loss or with rapid or noticeable weight loss in general, may or may not also require other interventions that include treatment with tissue tightening devices – such as radiofrequency energy, high-focused ultrasound energy, threads, and/or surgery – such as a face lift. The potential high cost of both off-label prescribing of these medications (especially without use of prescription health insurance) as well as treatment to correct any facial wasting has also received attention in news media and social media discussions of this topic.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She has no relevant disclosures.
*Correction 1/28/23: An earlier version of this story misstated the approval date of Wegovy. It was in 2021.
Ozempic and Wegovy are two prescription drugs that have transformed the management of type 2 diabetes and obesity. Both are a form of semaglutide; the Food and Drug Administration approved Ozempic for treating type 2 diabetes in 2017, followed by Wegovy in 2021 for weight loss in adults with obesity or those who are overweight and have least one weight-related health condition, such as hypertension or hypercholesterolemia. Ozempic is not approved for weight loss, but it has been prescribed off label for that purpose.
An effective treatment, participants with overweight or obesity in one study experienced almost a mean 15% drop in body weight with subcutaneous semaglutide administered once a week versus about 2% with placebo after 68 weeks.
In 2022, high demand and global supply constraints gave rise to shortages of both medications. The FDA reported a Wegovy shortage in March 2022, followed by an Ozempic shortage in August. Social media attention and increased off-label prescribing, with some patients purporting to have had significant improvements with weight loss and their quality of life, including having their clothing fit better and being able to bend over and tie their shoes, increased attention on these medications to the point that off-label prescribing of both drugs for weight loss resulted in some patients with type 2 diabetes unable to receive their medication on time. In late January 2023, NBC reported that Ozempic prescriptions had “tripled from 2021 to 2022,” based on data from the prescription drug discount company SingleCare.
Semaglutide is designed to mimic a hormone that signals to the brain when a person is full and promotes the release of insulin. In turn, the medications can result in lower blood glucose levels, appetite suppression, and reduced caloric intake. Injected once weekly, the medication, a glucagonlike peptide–1 receptor agonist, specifically, activates GLP-1 receptors in the brain, increasing insulin secretion, decreasing glucagon secretion, and delaying gastric emptying (acting as an incretin mimetic).
‘Ozempic face’
Common adverse events with semaglutide can include nausea, vomiting, diarrhea, abdominal pain, constipation, and injection-site reactions. Rare, but more severe adverse events may include thyroid C-cell tumor (in animal studies), medullary thyroid cancer risk, hypersensitivity reaction, anaphylaxis, acute renal injury, chronic renal failure exacerbation, pancreatitis, and cholelithiasis.
A less severe but noticeable side effect that has gained attention is facial wasting and aging, reportedly coined “Ozempic face” by a dermatologist interviewed for an article published in January in The New York Times.
As of Feb. 9, TikTok videos from individuals describing their personal experiences, health care professionals, and others with the tag #ozempicface had 4.8 million views.
Theories as to why noticeable facial changes occur with these medications include: accelerated loss of facial pads that already tend to diminish or shift with normal aging, as well as the inability of skin elasticity to keep up with the loss of volume (fat), resulting in more prominent hanging skin and the appearance of “jowls.” Wan and colleagues have described the fat pad distribution in the face and the facial aging that occurs as a result of the loss and shifting of these fat pads over time.
In the same way that we use facial fillers to help treat and correct volume/fat loss associated with photoaging, facial fillers may be used to help restore volume where it’s been lost after weight loss. The sagging skin or loss of elasticity often associated with Ozempic-related weight loss or with rapid or noticeable weight loss in general, may or may not also require other interventions that include treatment with tissue tightening devices – such as radiofrequency energy, high-focused ultrasound energy, threads, and/or surgery – such as a face lift. The potential high cost of both off-label prescribing of these medications (especially without use of prescription health insurance) as well as treatment to correct any facial wasting has also received attention in news media and social media discussions of this topic.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She has no relevant disclosures.
*Correction 1/28/23: An earlier version of this story misstated the approval date of Wegovy. It was in 2021.
Ozempic and Wegovy are two prescription drugs that have transformed the management of type 2 diabetes and obesity. Both are a form of semaglutide; the Food and Drug Administration approved Ozempic for treating type 2 diabetes in 2017, followed by Wegovy in 2021 for weight loss in adults with obesity or those who are overweight and have least one weight-related health condition, such as hypertension or hypercholesterolemia. Ozempic is not approved for weight loss, but it has been prescribed off label for that purpose.
An effective treatment, participants with overweight or obesity in one study experienced almost a mean 15% drop in body weight with subcutaneous semaglutide administered once a week versus about 2% with placebo after 68 weeks.
In 2022, high demand and global supply constraints gave rise to shortages of both medications. The FDA reported a Wegovy shortage in March 2022, followed by an Ozempic shortage in August. Social media attention and increased off-label prescribing, with some patients purporting to have had significant improvements with weight loss and their quality of life, including having their clothing fit better and being able to bend over and tie their shoes, increased attention on these medications to the point that off-label prescribing of both drugs for weight loss resulted in some patients with type 2 diabetes unable to receive their medication on time. In late January 2023, NBC reported that Ozempic prescriptions had “tripled from 2021 to 2022,” based on data from the prescription drug discount company SingleCare.
Semaglutide is designed to mimic a hormone that signals to the brain when a person is full and promotes the release of insulin. In turn, the medications can result in lower blood glucose levels, appetite suppression, and reduced caloric intake. Injected once weekly, the medication, a glucagonlike peptide–1 receptor agonist, specifically, activates GLP-1 receptors in the brain, increasing insulin secretion, decreasing glucagon secretion, and delaying gastric emptying (acting as an incretin mimetic).
‘Ozempic face’
Common adverse events with semaglutide can include nausea, vomiting, diarrhea, abdominal pain, constipation, and injection-site reactions. Rare, but more severe adverse events may include thyroid C-cell tumor (in animal studies), medullary thyroid cancer risk, hypersensitivity reaction, anaphylaxis, acute renal injury, chronic renal failure exacerbation, pancreatitis, and cholelithiasis.
A less severe but noticeable side effect that has gained attention is facial wasting and aging, reportedly coined “Ozempic face” by a dermatologist interviewed for an article published in January in The New York Times.
As of Feb. 9, TikTok videos from individuals describing their personal experiences, health care professionals, and others with the tag #ozempicface had 4.8 million views.
Theories as to why noticeable facial changes occur with these medications include: accelerated loss of facial pads that already tend to diminish or shift with normal aging, as well as the inability of skin elasticity to keep up with the loss of volume (fat), resulting in more prominent hanging skin and the appearance of “jowls.” Wan and colleagues have described the fat pad distribution in the face and the facial aging that occurs as a result of the loss and shifting of these fat pads over time.
In the same way that we use facial fillers to help treat and correct volume/fat loss associated with photoaging, facial fillers may be used to help restore volume where it’s been lost after weight loss. The sagging skin or loss of elasticity often associated with Ozempic-related weight loss or with rapid or noticeable weight loss in general, may or may not also require other interventions that include treatment with tissue tightening devices – such as radiofrequency energy, high-focused ultrasound energy, threads, and/or surgery – such as a face lift. The potential high cost of both off-label prescribing of these medications (especially without use of prescription health insurance) as well as treatment to correct any facial wasting has also received attention in news media and social media discussions of this topic.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She has no relevant disclosures.
*Correction 1/28/23: An earlier version of this story misstated the approval date of Wegovy. It was in 2021.
Must-read acute care medicine articles from 2022
When 2022 began, we started seeing some light at the end of the COVID-19 tunnel. Vaccines were widely available, and even with new variants of the virus still occasionally emerging, the rates of severe morbidity and mortality appeared to be decreasing.
Expectedly, journals appeared to start moving more toward mainstream topics and publications rather than what seemed like a major focus on COVID-19 publications. The resulting literature was fantastic.
Several of those topics were discussed in a prior Emergency Medicine Viewpoint from this news organization, and many more of the research advances of 2022 will be discussed in the near future. However, in this Viewpoint, I would like to present my annual review of my three “must-read” articles of the past year.
As in past years, I am choosing reviews of the literature rather than original research articles (which, all too often, become outdated or debunked within a few years). I choose these articles in the hopes that readers will not simply settle for my brief reviews of the key points but instead will feel compelled to download and read the entire articles. These publications address common conditions and quandaries we face in the daily practice of emergency medicine and are practice-changing.
Myocardial dysfunction after cardiac arrest: Tips and pitfalls
The management of post–cardiac arrest patients remains a hot topic in the resuscitation literature as we continue to understand that the immediate post-arrest period is critical to patient outcome.
Ortuno and colleagues reviewed the current literature on post-arrest care and wrote an outstanding summary of how to optimally care for these patients. More specifically, they focused on post-arrest patients who demonstrate continued shock, or “post–cardiac arrest myocardial dysfunction” (PCAMD).
They propose three mechanisms for the pathogenesis of PCAMD: ischemia reperfusion phenomenon, systemic inflammatory response, and increased catecholamine release
I will skip through the details of the pathophysiology that they describe in the article, but I certainly do recommend that everyone review their descriptions.
Management of these patients begins with a good hemodynamic assessment, which includes clinical markers of perfusion (blood pressure, capillary refill), ECG, and point-of-care ultrasound (POCUS). If the initial assessment reveals an obvious cause of the cardiac arrest (e.g., massive pulmonary embolism, myocardial infarction, pericardial tamponade), then the underlying cause should be treated expeditiously.
In the absence of an obvious treatable cause of the shock, the fluid status and cardiac function should be addressed with POCUS. If the patient is hypovolemic, intravenous fluids should be administered. If the fluid status is adequate, POCUS should be used to estimate the patient’s ventricular function. If the ventricle appears to be hyperdynamic with good contractility, shock should be treated with norepinephrine. On the other hand, if the ventricle is hypodynamic, dobutamine should be substituted for norepinephrine or, more often, added to norepinephrine.
The above represents a simplified summary of the critical points, but the authors do delve into further detail and also discuss some other options for therapies, including steroids, coronary revascularization, extracorporeal membrane oxygenation, and so on. The review is very thoughtful, thorough, and definitely worth a full read.
Top myths of diagnosis and management of infectious diseases in hospital medicine
Most, if not all of us in medicine, have heard the saying that 50% of what we learn in medical school (or residency) will turn out to be wrong. I certainly believe in this concept and consequently, like many of you, I enjoy reading about myths and misconceptions that we have been taught. With that in mind, I have to say that I love this article because it seems to have been written specifically to address what I was taught!
This author group, consisting mostly of clinical PharmDs who are experts in antibiotic use, provide us with an evidence-based discussion of myths and pitfalls in how antibiotics are often used in current clinical practice. The authors review their top 10 myths involving the use of antibiotics in treating infections in the hospital setting. A few of these relate more to the inpatient setting, but here are my favorite emergency department (ED)–related myths that they address:
- “Antibiotics do no harm.” The authors address the risk-benefit of antibiotics based on assumed vs. confirmed infections, including a brief discussion of adverse drug effects.
- “Antibiotic durations of 7, 14, or 21 days are typically necessary.” The authors address appropriate duration of antibiotic use and the fact that unnecessarily long durations of use can lead to resistance. They also provide reassurance that some infections can be treated with quite short durations of antibiotics.
- “If one drug is good, two (or more!) is better.” The use of multiple antibiotics, often with overlapping bacterial coverage, is rampant in medicine and further increases the risk for adverse drug effects and resistance.
- “Oral antibiotics are not as good as intravenous antibiotics for hospitalized patients.” This is definitely a myth that I learned. I recall being taught by many senior physicians that anyone sick enough for admission should be treated with intravenous antibiotics. As it turns out, absorption and effectiveness of most oral antibiotics is just as good as intravenous antibiotics, and the oral formulations are often safer.
- “A history of a penicillin allergy means the patient can never receive a beta-lactam antibiotic.” This is a myth that was debunked quite a few years ago, but it seems that many clinicians still need a reminder.
The authors included five more myths that are worth the read. This is an article that needs to be disseminated among all hospital clinicians.
Guidelines for low-risk, recurrent abdominal pain in the emergency department
The Society for Academic Emergency Medicine (SAEM) recently initiated a program focused on creating evidence-based approaches to challenging chief complaints and presentations in the emergency department (ED). In 2021, they published an approach to managing patients with recurrent, low-risk chest pain in the ED. This past year, they published their second guideline, focused on the management of patients with low-risk, recurrent abdominal pain in the ED.
Recurrent low-risk abdominal pain is a common and vexing presentation to EDs around the world, and there is little prior published guidance. Do all of these patients need repeat imaging? How do we manage their pain? Are there nonabdominal conditions that should be considered?
Broder and colleagues did a fantastic review of the current literature and, on behalf of SAEM, have provided a rational approach to optimal management of these patients. The four major questions they addressed, with brief summaries of their recommendations, are:
- Should adult ED patients with low-risk, recurrent and previously undifferentiated abdominal pain receive a repeat CT abdomen-pelvis (CTAP) after a negative CTAP within the past 12 months? This is a typical question that we all ponder when managing these patients. Unfortunately, the writing group found insufficient evidence to definitively identify populations in whom CTAP was recommended vs could be safely withheld. It is a bit disappointing that there is no definite answer to the question. On the other hand, it is reassuring to know that the world’s best evidence essentially says that it is perfectly appropriate to use your own good clinical judgment.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain with a negative CTAP receive additional imaging with abdominal ultrasound? In this case, the writing group found enough evidence, though low-level, to suggest against routine ultrasound in the absence of concern specifically for pelvic or hepatobiliary pathology. Like most tests, ultrasound is best used when there are specific concerns rather than being used in an undifferentiated fashion.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive screening for depression/anxiety? The writing group found enough evidence, though low-level again, to suggest that screening for depression and/or anxiety be performed during the ED evaluation. This could lead to successful therapy for the abdominal pain.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive nonopioid and/or nonpharmacologic analgesics? The writing group found little evidence to suggest for or against these analgesics, but they made a consensus recommendation suggesting an opioid-minimizing strategy for pain control.
Although the final recommendations of the writing group were not definitive or based on the strongest level of evidence, I find it helpful to have this guidance, nevertheless, on behalf of a major national organization. I also find it helpful to know that even with the best evidence available, optimal patient care will often boil down to physician experience and gestalt. I should also add that the overall article is chock-full of pearls and helpful information that will further inform the readers’ decisions, and so the full version is definitely worth the read.
In summary
There you have it – my three favorite practice-changing articles of 2022. Although I have tried to provide key points here, the full discussions of those key points in the published articles will provide a great deal more education than I can offer in this brief write-up, and so I strongly encourage everyone to read the full versions. Please be sure to include in the comments section your own pick for favorite or must-read articles from the past year.
Amal Mattu, MD, is a professor, vice chair of education, and codirector of the emergency cardiology fellowship in the department of emergency medicine at the University of Maryland, Baltimore. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
When 2022 began, we started seeing some light at the end of the COVID-19 tunnel. Vaccines were widely available, and even with new variants of the virus still occasionally emerging, the rates of severe morbidity and mortality appeared to be decreasing.
Expectedly, journals appeared to start moving more toward mainstream topics and publications rather than what seemed like a major focus on COVID-19 publications. The resulting literature was fantastic.
Several of those topics were discussed in a prior Emergency Medicine Viewpoint from this news organization, and many more of the research advances of 2022 will be discussed in the near future. However, in this Viewpoint, I would like to present my annual review of my three “must-read” articles of the past year.
As in past years, I am choosing reviews of the literature rather than original research articles (which, all too often, become outdated or debunked within a few years). I choose these articles in the hopes that readers will not simply settle for my brief reviews of the key points but instead will feel compelled to download and read the entire articles. These publications address common conditions and quandaries we face in the daily practice of emergency medicine and are practice-changing.
Myocardial dysfunction after cardiac arrest: Tips and pitfalls
The management of post–cardiac arrest patients remains a hot topic in the resuscitation literature as we continue to understand that the immediate post-arrest period is critical to patient outcome.
Ortuno and colleagues reviewed the current literature on post-arrest care and wrote an outstanding summary of how to optimally care for these patients. More specifically, they focused on post-arrest patients who demonstrate continued shock, or “post–cardiac arrest myocardial dysfunction” (PCAMD).
They propose three mechanisms for the pathogenesis of PCAMD: ischemia reperfusion phenomenon, systemic inflammatory response, and increased catecholamine release
I will skip through the details of the pathophysiology that they describe in the article, but I certainly do recommend that everyone review their descriptions.
Management of these patients begins with a good hemodynamic assessment, which includes clinical markers of perfusion (blood pressure, capillary refill), ECG, and point-of-care ultrasound (POCUS). If the initial assessment reveals an obvious cause of the cardiac arrest (e.g., massive pulmonary embolism, myocardial infarction, pericardial tamponade), then the underlying cause should be treated expeditiously.
In the absence of an obvious treatable cause of the shock, the fluid status and cardiac function should be addressed with POCUS. If the patient is hypovolemic, intravenous fluids should be administered. If the fluid status is adequate, POCUS should be used to estimate the patient’s ventricular function. If the ventricle appears to be hyperdynamic with good contractility, shock should be treated with norepinephrine. On the other hand, if the ventricle is hypodynamic, dobutamine should be substituted for norepinephrine or, more often, added to norepinephrine.
The above represents a simplified summary of the critical points, but the authors do delve into further detail and also discuss some other options for therapies, including steroids, coronary revascularization, extracorporeal membrane oxygenation, and so on. The review is very thoughtful, thorough, and definitely worth a full read.
Top myths of diagnosis and management of infectious diseases in hospital medicine
Most, if not all of us in medicine, have heard the saying that 50% of what we learn in medical school (or residency) will turn out to be wrong. I certainly believe in this concept and consequently, like many of you, I enjoy reading about myths and misconceptions that we have been taught. With that in mind, I have to say that I love this article because it seems to have been written specifically to address what I was taught!
This author group, consisting mostly of clinical PharmDs who are experts in antibiotic use, provide us with an evidence-based discussion of myths and pitfalls in how antibiotics are often used in current clinical practice. The authors review their top 10 myths involving the use of antibiotics in treating infections in the hospital setting. A few of these relate more to the inpatient setting, but here are my favorite emergency department (ED)–related myths that they address:
- “Antibiotics do no harm.” The authors address the risk-benefit of antibiotics based on assumed vs. confirmed infections, including a brief discussion of adverse drug effects.
- “Antibiotic durations of 7, 14, or 21 days are typically necessary.” The authors address appropriate duration of antibiotic use and the fact that unnecessarily long durations of use can lead to resistance. They also provide reassurance that some infections can be treated with quite short durations of antibiotics.
- “If one drug is good, two (or more!) is better.” The use of multiple antibiotics, often with overlapping bacterial coverage, is rampant in medicine and further increases the risk for adverse drug effects and resistance.
- “Oral antibiotics are not as good as intravenous antibiotics for hospitalized patients.” This is definitely a myth that I learned. I recall being taught by many senior physicians that anyone sick enough for admission should be treated with intravenous antibiotics. As it turns out, absorption and effectiveness of most oral antibiotics is just as good as intravenous antibiotics, and the oral formulations are often safer.
- “A history of a penicillin allergy means the patient can never receive a beta-lactam antibiotic.” This is a myth that was debunked quite a few years ago, but it seems that many clinicians still need a reminder.
The authors included five more myths that are worth the read. This is an article that needs to be disseminated among all hospital clinicians.
Guidelines for low-risk, recurrent abdominal pain in the emergency department
The Society for Academic Emergency Medicine (SAEM) recently initiated a program focused on creating evidence-based approaches to challenging chief complaints and presentations in the emergency department (ED). In 2021, they published an approach to managing patients with recurrent, low-risk chest pain in the ED. This past year, they published their second guideline, focused on the management of patients with low-risk, recurrent abdominal pain in the ED.
Recurrent low-risk abdominal pain is a common and vexing presentation to EDs around the world, and there is little prior published guidance. Do all of these patients need repeat imaging? How do we manage their pain? Are there nonabdominal conditions that should be considered?
Broder and colleagues did a fantastic review of the current literature and, on behalf of SAEM, have provided a rational approach to optimal management of these patients. The four major questions they addressed, with brief summaries of their recommendations, are:
- Should adult ED patients with low-risk, recurrent and previously undifferentiated abdominal pain receive a repeat CT abdomen-pelvis (CTAP) after a negative CTAP within the past 12 months? This is a typical question that we all ponder when managing these patients. Unfortunately, the writing group found insufficient evidence to definitively identify populations in whom CTAP was recommended vs could be safely withheld. It is a bit disappointing that there is no definite answer to the question. On the other hand, it is reassuring to know that the world’s best evidence essentially says that it is perfectly appropriate to use your own good clinical judgment.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain with a negative CTAP receive additional imaging with abdominal ultrasound? In this case, the writing group found enough evidence, though low-level, to suggest against routine ultrasound in the absence of concern specifically for pelvic or hepatobiliary pathology. Like most tests, ultrasound is best used when there are specific concerns rather than being used in an undifferentiated fashion.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive screening for depression/anxiety? The writing group found enough evidence, though low-level again, to suggest that screening for depression and/or anxiety be performed during the ED evaluation. This could lead to successful therapy for the abdominal pain.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive nonopioid and/or nonpharmacologic analgesics? The writing group found little evidence to suggest for or against these analgesics, but they made a consensus recommendation suggesting an opioid-minimizing strategy for pain control.
Although the final recommendations of the writing group were not definitive or based on the strongest level of evidence, I find it helpful to have this guidance, nevertheless, on behalf of a major national organization. I also find it helpful to know that even with the best evidence available, optimal patient care will often boil down to physician experience and gestalt. I should also add that the overall article is chock-full of pearls and helpful information that will further inform the readers’ decisions, and so the full version is definitely worth the read.
In summary
There you have it – my three favorite practice-changing articles of 2022. Although I have tried to provide key points here, the full discussions of those key points in the published articles will provide a great deal more education than I can offer in this brief write-up, and so I strongly encourage everyone to read the full versions. Please be sure to include in the comments section your own pick for favorite or must-read articles from the past year.
Amal Mattu, MD, is a professor, vice chair of education, and codirector of the emergency cardiology fellowship in the department of emergency medicine at the University of Maryland, Baltimore. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
When 2022 began, we started seeing some light at the end of the COVID-19 tunnel. Vaccines were widely available, and even with new variants of the virus still occasionally emerging, the rates of severe morbidity and mortality appeared to be decreasing.
Expectedly, journals appeared to start moving more toward mainstream topics and publications rather than what seemed like a major focus on COVID-19 publications. The resulting literature was fantastic.
Several of those topics were discussed in a prior Emergency Medicine Viewpoint from this news organization, and many more of the research advances of 2022 will be discussed in the near future. However, in this Viewpoint, I would like to present my annual review of my three “must-read” articles of the past year.
As in past years, I am choosing reviews of the literature rather than original research articles (which, all too often, become outdated or debunked within a few years). I choose these articles in the hopes that readers will not simply settle for my brief reviews of the key points but instead will feel compelled to download and read the entire articles. These publications address common conditions and quandaries we face in the daily practice of emergency medicine and are practice-changing.
Myocardial dysfunction after cardiac arrest: Tips and pitfalls
The management of post–cardiac arrest patients remains a hot topic in the resuscitation literature as we continue to understand that the immediate post-arrest period is critical to patient outcome.
Ortuno and colleagues reviewed the current literature on post-arrest care and wrote an outstanding summary of how to optimally care for these patients. More specifically, they focused on post-arrest patients who demonstrate continued shock, or “post–cardiac arrest myocardial dysfunction” (PCAMD).
They propose three mechanisms for the pathogenesis of PCAMD: ischemia reperfusion phenomenon, systemic inflammatory response, and increased catecholamine release
I will skip through the details of the pathophysiology that they describe in the article, but I certainly do recommend that everyone review their descriptions.
Management of these patients begins with a good hemodynamic assessment, which includes clinical markers of perfusion (blood pressure, capillary refill), ECG, and point-of-care ultrasound (POCUS). If the initial assessment reveals an obvious cause of the cardiac arrest (e.g., massive pulmonary embolism, myocardial infarction, pericardial tamponade), then the underlying cause should be treated expeditiously.
In the absence of an obvious treatable cause of the shock, the fluid status and cardiac function should be addressed with POCUS. If the patient is hypovolemic, intravenous fluids should be administered. If the fluid status is adequate, POCUS should be used to estimate the patient’s ventricular function. If the ventricle appears to be hyperdynamic with good contractility, shock should be treated with norepinephrine. On the other hand, if the ventricle is hypodynamic, dobutamine should be substituted for norepinephrine or, more often, added to norepinephrine.
The above represents a simplified summary of the critical points, but the authors do delve into further detail and also discuss some other options for therapies, including steroids, coronary revascularization, extracorporeal membrane oxygenation, and so on. The review is very thoughtful, thorough, and definitely worth a full read.
Top myths of diagnosis and management of infectious diseases in hospital medicine
Most, if not all of us in medicine, have heard the saying that 50% of what we learn in medical school (or residency) will turn out to be wrong. I certainly believe in this concept and consequently, like many of you, I enjoy reading about myths and misconceptions that we have been taught. With that in mind, I have to say that I love this article because it seems to have been written specifically to address what I was taught!
This author group, consisting mostly of clinical PharmDs who are experts in antibiotic use, provide us with an evidence-based discussion of myths and pitfalls in how antibiotics are often used in current clinical practice. The authors review their top 10 myths involving the use of antibiotics in treating infections in the hospital setting. A few of these relate more to the inpatient setting, but here are my favorite emergency department (ED)–related myths that they address:
- “Antibiotics do no harm.” The authors address the risk-benefit of antibiotics based on assumed vs. confirmed infections, including a brief discussion of adverse drug effects.
- “Antibiotic durations of 7, 14, or 21 days are typically necessary.” The authors address appropriate duration of antibiotic use and the fact that unnecessarily long durations of use can lead to resistance. They also provide reassurance that some infections can be treated with quite short durations of antibiotics.
- “If one drug is good, two (or more!) is better.” The use of multiple antibiotics, often with overlapping bacterial coverage, is rampant in medicine and further increases the risk for adverse drug effects and resistance.
- “Oral antibiotics are not as good as intravenous antibiotics for hospitalized patients.” This is definitely a myth that I learned. I recall being taught by many senior physicians that anyone sick enough for admission should be treated with intravenous antibiotics. As it turns out, absorption and effectiveness of most oral antibiotics is just as good as intravenous antibiotics, and the oral formulations are often safer.
- “A history of a penicillin allergy means the patient can never receive a beta-lactam antibiotic.” This is a myth that was debunked quite a few years ago, but it seems that many clinicians still need a reminder.
The authors included five more myths that are worth the read. This is an article that needs to be disseminated among all hospital clinicians.
Guidelines for low-risk, recurrent abdominal pain in the emergency department
The Society for Academic Emergency Medicine (SAEM) recently initiated a program focused on creating evidence-based approaches to challenging chief complaints and presentations in the emergency department (ED). In 2021, they published an approach to managing patients with recurrent, low-risk chest pain in the ED. This past year, they published their second guideline, focused on the management of patients with low-risk, recurrent abdominal pain in the ED.
Recurrent low-risk abdominal pain is a common and vexing presentation to EDs around the world, and there is little prior published guidance. Do all of these patients need repeat imaging? How do we manage their pain? Are there nonabdominal conditions that should be considered?
Broder and colleagues did a fantastic review of the current literature and, on behalf of SAEM, have provided a rational approach to optimal management of these patients. The four major questions they addressed, with brief summaries of their recommendations, are:
- Should adult ED patients with low-risk, recurrent and previously undifferentiated abdominal pain receive a repeat CT abdomen-pelvis (CTAP) after a negative CTAP within the past 12 months? This is a typical question that we all ponder when managing these patients. Unfortunately, the writing group found insufficient evidence to definitively identify populations in whom CTAP was recommended vs could be safely withheld. It is a bit disappointing that there is no definite answer to the question. On the other hand, it is reassuring to know that the world’s best evidence essentially says that it is perfectly appropriate to use your own good clinical judgment.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain with a negative CTAP receive additional imaging with abdominal ultrasound? In this case, the writing group found enough evidence, though low-level, to suggest against routine ultrasound in the absence of concern specifically for pelvic or hepatobiliary pathology. Like most tests, ultrasound is best used when there are specific concerns rather than being used in an undifferentiated fashion.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive screening for depression/anxiety? The writing group found enough evidence, though low-level again, to suggest that screening for depression and/or anxiety be performed during the ED evaluation. This could lead to successful therapy for the abdominal pain.
- Should adult ED patients with low-risk, recurrent, and previously undifferentiated abdominal pain receive nonopioid and/or nonpharmacologic analgesics? The writing group found little evidence to suggest for or against these analgesics, but they made a consensus recommendation suggesting an opioid-minimizing strategy for pain control.
Although the final recommendations of the writing group were not definitive or based on the strongest level of evidence, I find it helpful to have this guidance, nevertheless, on behalf of a major national organization. I also find it helpful to know that even with the best evidence available, optimal patient care will often boil down to physician experience and gestalt. I should also add that the overall article is chock-full of pearls and helpful information that will further inform the readers’ decisions, and so the full version is definitely worth the read.
In summary
There you have it – my three favorite practice-changing articles of 2022. Although I have tried to provide key points here, the full discussions of those key points in the published articles will provide a great deal more education than I can offer in this brief write-up, and so I strongly encourage everyone to read the full versions. Please be sure to include in the comments section your own pick for favorite or must-read articles from the past year.
Amal Mattu, MD, is a professor, vice chair of education, and codirector of the emergency cardiology fellowship in the department of emergency medicine at the University of Maryland, Baltimore. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The X-waiver is dead
In 2016, when Erin Schanning lost her brother Ethan to an overdose, she wanted to know what could have been done to have helped him. Ethan, who had struggled with opioids since getting a prescription for the drugs after a dental procedure in middle school, had tried dozens of treatments. But at the age of 30, he was gone.
“After my brother died, I started researching and was surprised to learn that there were many evidence-based ways to treat substance use disorder that he hadn’t had access to, even though he had doggedly pursued treatment,” Ms. Schanning told me in an interview. One of those treatments, buprenorphine, is one of the most effective tools that health care providers have to treat opioid use disorder. A partial opioid agonist, it reduces cravings and prevents overdose, decreasing mortality more effectively than almost any medication for any disease. Yet most providers have never prescribed it.
That may be about to change. The special license to prescribe the medication, commonly known as the “X-waiver,” was officially eliminated as part of the passage of the Mainstreaming Addiction Treatment (MAT) Act. Immediately, following the passage of the Act, any provider with a DEA license became eligible to prescribe buprenorphine to treat opioid use disorder, and limits on the number of patients they could treat were eliminated.
Previously, buprenorphine, which has a better safety profile than almost any other prescription opioid because of its ceiling effect on respiratory depression, nonetheless required providers to obtain a special license to prescribe it, and – prior to an executive order from the Biden administration – 8 to 24 hours of training to do so. This led to a misconception that buprenorphine was dangerous, and created barriers for treatment during the worst overdose crisis in our country’s history. More than 110,00 overdose deaths occurred in 2021, representing a 468% increase in the last 2 decades.
Along with the MAT Act, the Medication Access and Training Expansion Act was passed in the same spending bill, requiring all prescribers who obtain a DEA license to do 8 hours of training on the treatment of substance use disorders. According to the Act, addiction specialty societies will have a role in creating trainings. Medical schools and residencies will also be able to fulfill this requirement with a “comprehensive” curriculum that covers all approved medications for the treatment of substance use disorders.
The DEA has not yet confirmed what training will be accepted, according to the Chief Medical Officer of the Substance Abuse and Mental Health Services Administration, Neeraj Gandotra, MD, who spoke to me in an interview. However, it is required to do so by April 5, 2023. Dr. Gandotra also emphasized that state and local laws, as well as insurance requirements, remain in place, and may place other constraints on prescribing. According to the Act, this new rule will be in effect by June 2023.
As an addiction medicine specialist and longtime buprenorphine prescriber, I am excited about these changes but wary of lingering resistance among health care providers. Will providers who have chosen not to get an X-waiver now look for another reason to not treat patients with substance use disorders?
Ms. Schanning remains hopeful. “I’m incredibly optimistic that health care providers are going to learn about buprenorphine and prescribe it to patients, and that patients are going to start asking about this medication,” she told me. “Seven in 10 providers say that they do feel an obligation to treat their patients with [opioid use disorder], but the federal government has made it very difficult to do so.”
Now with the X-waiver gone, providers and patients may be able to push for a long overdue shift in how we treat and conceptualize substance use disorders, she noted.
“Health care providers need to recognize substance use disorder as a medical condition that deserves treatment, and to speak about it like a medical condition,” Ms. Schanning said, by, for instance, moving away from using words such as “abuse” and “clean” and, instead, talking about treatable substance use disorders that can improve with evidence-based care, such as buprenorphine and methadone. “We also need to share stories of success and hope with people,” she added. “Once you’ve seen how someone can be transformed by treatment, it’s really difficult to say that substance use disorder is a character flaw, or their fault.”
A patient-centered approach
Over the past decade of practicing medicine, I have experienced this transformation personally. In residency, I believed that people had to be ready for help, to stop using, to change. I failed to recognize that many of those same people were asking me for help, and I wasn’t offering what they needed. The person who had to change was me.
As I moved toward a patient-centered approach, lowering barriers to starting and remaining in treatment, and collaborating with teams that could meet people wherever they might be, addictions became the most rewarding part of my practice.
I have never had more people thank me spontaneously and deeply for the care I provide. Plus, I have never seen a more profound change in the students I work with than when they witness someone with a substance use disorder offered treatment that works.
The X-waiver was not the only barrier to care, and the overdose crisis is not slowing down. But maybe with a new tool widely accessible, more of us will be ready to help.
Dr. Poorman is board certified in internal medicine and addiction medicine, assistant professor of medicine, University of Illinois at Chicago, and provides primary care and addiction services in Chicago. Her views do not necessarily reflect the views of her employer. She has reported no relevant disclosures, and she serves on the editorial advisory board of Internal Medicine News.
In 2016, when Erin Schanning lost her brother Ethan to an overdose, she wanted to know what could have been done to have helped him. Ethan, who had struggled with opioids since getting a prescription for the drugs after a dental procedure in middle school, had tried dozens of treatments. But at the age of 30, he was gone.
“After my brother died, I started researching and was surprised to learn that there were many evidence-based ways to treat substance use disorder that he hadn’t had access to, even though he had doggedly pursued treatment,” Ms. Schanning told me in an interview. One of those treatments, buprenorphine, is one of the most effective tools that health care providers have to treat opioid use disorder. A partial opioid agonist, it reduces cravings and prevents overdose, decreasing mortality more effectively than almost any medication for any disease. Yet most providers have never prescribed it.
That may be about to change. The special license to prescribe the medication, commonly known as the “X-waiver,” was officially eliminated as part of the passage of the Mainstreaming Addiction Treatment (MAT) Act. Immediately, following the passage of the Act, any provider with a DEA license became eligible to prescribe buprenorphine to treat opioid use disorder, and limits on the number of patients they could treat were eliminated.
Previously, buprenorphine, which has a better safety profile than almost any other prescription opioid because of its ceiling effect on respiratory depression, nonetheless required providers to obtain a special license to prescribe it, and – prior to an executive order from the Biden administration – 8 to 24 hours of training to do so. This led to a misconception that buprenorphine was dangerous, and created barriers for treatment during the worst overdose crisis in our country’s history. More than 110,00 overdose deaths occurred in 2021, representing a 468% increase in the last 2 decades.
Along with the MAT Act, the Medication Access and Training Expansion Act was passed in the same spending bill, requiring all prescribers who obtain a DEA license to do 8 hours of training on the treatment of substance use disorders. According to the Act, addiction specialty societies will have a role in creating trainings. Medical schools and residencies will also be able to fulfill this requirement with a “comprehensive” curriculum that covers all approved medications for the treatment of substance use disorders.
The DEA has not yet confirmed what training will be accepted, according to the Chief Medical Officer of the Substance Abuse and Mental Health Services Administration, Neeraj Gandotra, MD, who spoke to me in an interview. However, it is required to do so by April 5, 2023. Dr. Gandotra also emphasized that state and local laws, as well as insurance requirements, remain in place, and may place other constraints on prescribing. According to the Act, this new rule will be in effect by June 2023.
As an addiction medicine specialist and longtime buprenorphine prescriber, I am excited about these changes but wary of lingering resistance among health care providers. Will providers who have chosen not to get an X-waiver now look for another reason to not treat patients with substance use disorders?
Ms. Schanning remains hopeful. “I’m incredibly optimistic that health care providers are going to learn about buprenorphine and prescribe it to patients, and that patients are going to start asking about this medication,” she told me. “Seven in 10 providers say that they do feel an obligation to treat their patients with [opioid use disorder], but the federal government has made it very difficult to do so.”
Now with the X-waiver gone, providers and patients may be able to push for a long overdue shift in how we treat and conceptualize substance use disorders, she noted.
“Health care providers need to recognize substance use disorder as a medical condition that deserves treatment, and to speak about it like a medical condition,” Ms. Schanning said, by, for instance, moving away from using words such as “abuse” and “clean” and, instead, talking about treatable substance use disorders that can improve with evidence-based care, such as buprenorphine and methadone. “We also need to share stories of success and hope with people,” she added. “Once you’ve seen how someone can be transformed by treatment, it’s really difficult to say that substance use disorder is a character flaw, or their fault.”
A patient-centered approach
Over the past decade of practicing medicine, I have experienced this transformation personally. In residency, I believed that people had to be ready for help, to stop using, to change. I failed to recognize that many of those same people were asking me for help, and I wasn’t offering what they needed. The person who had to change was me.
As I moved toward a patient-centered approach, lowering barriers to starting and remaining in treatment, and collaborating with teams that could meet people wherever they might be, addictions became the most rewarding part of my practice.
I have never had more people thank me spontaneously and deeply for the care I provide. Plus, I have never seen a more profound change in the students I work with than when they witness someone with a substance use disorder offered treatment that works.
The X-waiver was not the only barrier to care, and the overdose crisis is not slowing down. But maybe with a new tool widely accessible, more of us will be ready to help.
Dr. Poorman is board certified in internal medicine and addiction medicine, assistant professor of medicine, University of Illinois at Chicago, and provides primary care and addiction services in Chicago. Her views do not necessarily reflect the views of her employer. She has reported no relevant disclosures, and she serves on the editorial advisory board of Internal Medicine News.
In 2016, when Erin Schanning lost her brother Ethan to an overdose, she wanted to know what could have been done to have helped him. Ethan, who had struggled with opioids since getting a prescription for the drugs after a dental procedure in middle school, had tried dozens of treatments. But at the age of 30, he was gone.
“After my brother died, I started researching and was surprised to learn that there were many evidence-based ways to treat substance use disorder that he hadn’t had access to, even though he had doggedly pursued treatment,” Ms. Schanning told me in an interview. One of those treatments, buprenorphine, is one of the most effective tools that health care providers have to treat opioid use disorder. A partial opioid agonist, it reduces cravings and prevents overdose, decreasing mortality more effectively than almost any medication for any disease. Yet most providers have never prescribed it.
That may be about to change. The special license to prescribe the medication, commonly known as the “X-waiver,” was officially eliminated as part of the passage of the Mainstreaming Addiction Treatment (MAT) Act. Immediately, following the passage of the Act, any provider with a DEA license became eligible to prescribe buprenorphine to treat opioid use disorder, and limits on the number of patients they could treat were eliminated.
Previously, buprenorphine, which has a better safety profile than almost any other prescription opioid because of its ceiling effect on respiratory depression, nonetheless required providers to obtain a special license to prescribe it, and – prior to an executive order from the Biden administration – 8 to 24 hours of training to do so. This led to a misconception that buprenorphine was dangerous, and created barriers for treatment during the worst overdose crisis in our country’s history. More than 110,00 overdose deaths occurred in 2021, representing a 468% increase in the last 2 decades.
Along with the MAT Act, the Medication Access and Training Expansion Act was passed in the same spending bill, requiring all prescribers who obtain a DEA license to do 8 hours of training on the treatment of substance use disorders. According to the Act, addiction specialty societies will have a role in creating trainings. Medical schools and residencies will also be able to fulfill this requirement with a “comprehensive” curriculum that covers all approved medications for the treatment of substance use disorders.
The DEA has not yet confirmed what training will be accepted, according to the Chief Medical Officer of the Substance Abuse and Mental Health Services Administration, Neeraj Gandotra, MD, who spoke to me in an interview. However, it is required to do so by April 5, 2023. Dr. Gandotra also emphasized that state and local laws, as well as insurance requirements, remain in place, and may place other constraints on prescribing. According to the Act, this new rule will be in effect by June 2023.
As an addiction medicine specialist and longtime buprenorphine prescriber, I am excited about these changes but wary of lingering resistance among health care providers. Will providers who have chosen not to get an X-waiver now look for another reason to not treat patients with substance use disorders?
Ms. Schanning remains hopeful. “I’m incredibly optimistic that health care providers are going to learn about buprenorphine and prescribe it to patients, and that patients are going to start asking about this medication,” she told me. “Seven in 10 providers say that they do feel an obligation to treat their patients with [opioid use disorder], but the federal government has made it very difficult to do so.”
Now with the X-waiver gone, providers and patients may be able to push for a long overdue shift in how we treat and conceptualize substance use disorders, she noted.
“Health care providers need to recognize substance use disorder as a medical condition that deserves treatment, and to speak about it like a medical condition,” Ms. Schanning said, by, for instance, moving away from using words such as “abuse” and “clean” and, instead, talking about treatable substance use disorders that can improve with evidence-based care, such as buprenorphine and methadone. “We also need to share stories of success and hope with people,” she added. “Once you’ve seen how someone can be transformed by treatment, it’s really difficult to say that substance use disorder is a character flaw, or their fault.”
A patient-centered approach
Over the past decade of practicing medicine, I have experienced this transformation personally. In residency, I believed that people had to be ready for help, to stop using, to change. I failed to recognize that many of those same people were asking me for help, and I wasn’t offering what they needed. The person who had to change was me.
As I moved toward a patient-centered approach, lowering barriers to starting and remaining in treatment, and collaborating with teams that could meet people wherever they might be, addictions became the most rewarding part of my practice.
I have never had more people thank me spontaneously and deeply for the care I provide. Plus, I have never seen a more profound change in the students I work with than when they witness someone with a substance use disorder offered treatment that works.
The X-waiver was not the only barrier to care, and the overdose crisis is not slowing down. But maybe with a new tool widely accessible, more of us will be ready to help.
Dr. Poorman is board certified in internal medicine and addiction medicine, assistant professor of medicine, University of Illinois at Chicago, and provides primary care and addiction services in Chicago. Her views do not necessarily reflect the views of her employer. She has reported no relevant disclosures, and she serves on the editorial advisory board of Internal Medicine News.
The five biggest changes in the 2023 adult vaccine schedules
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
Finding catatonia requires knowing what to look for
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).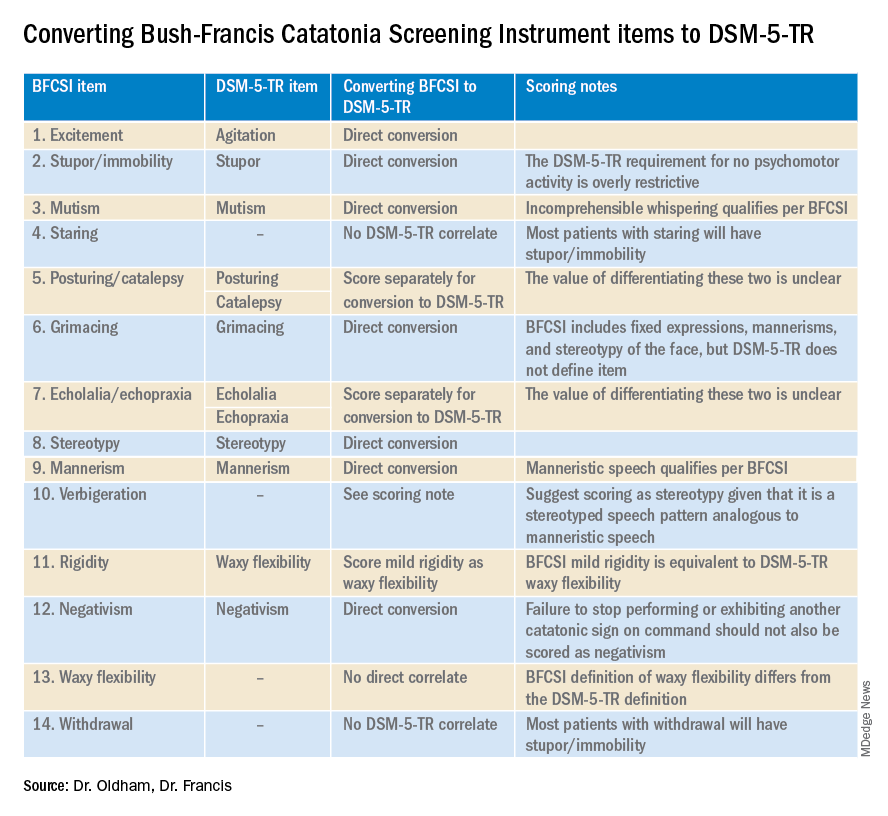
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).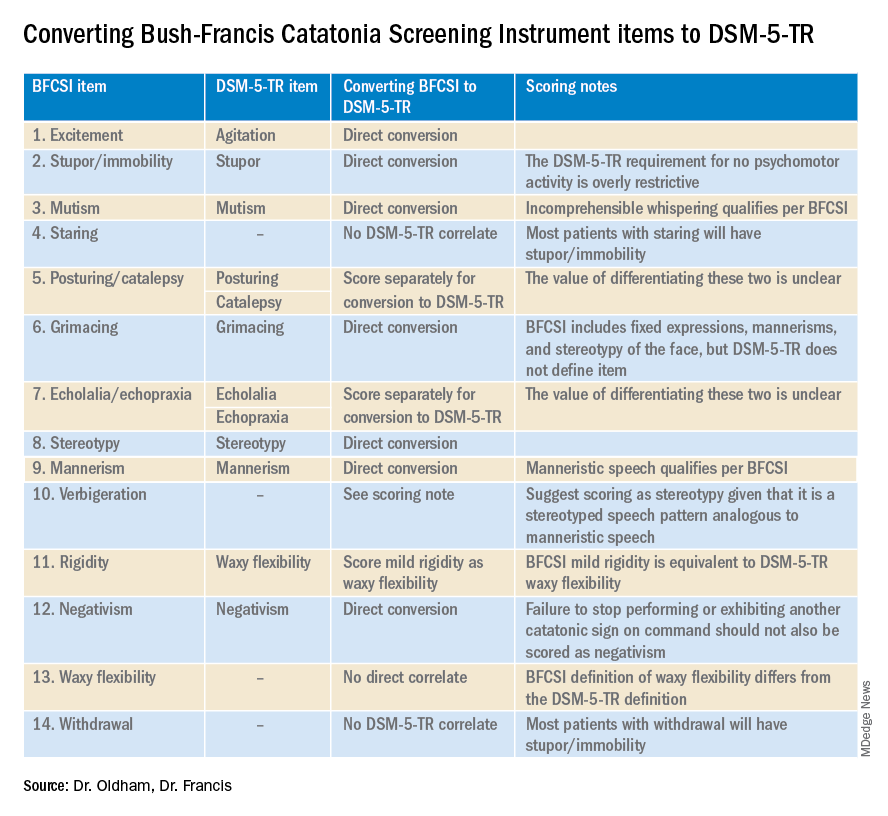
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).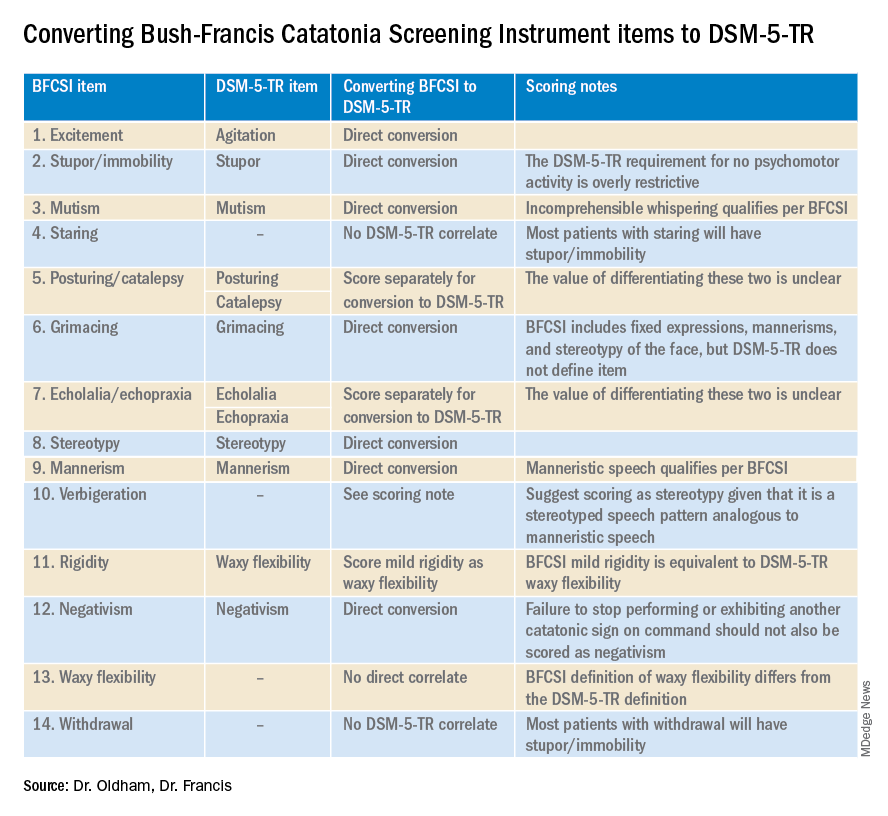
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.