User login
The work schedule that prevents burnout
The schedule is easier to change than the work itself
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
The schedule is easier to change than the work itself
The schedule is easier to change than the work itself
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
Caring for the offensive patient
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Medication management
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
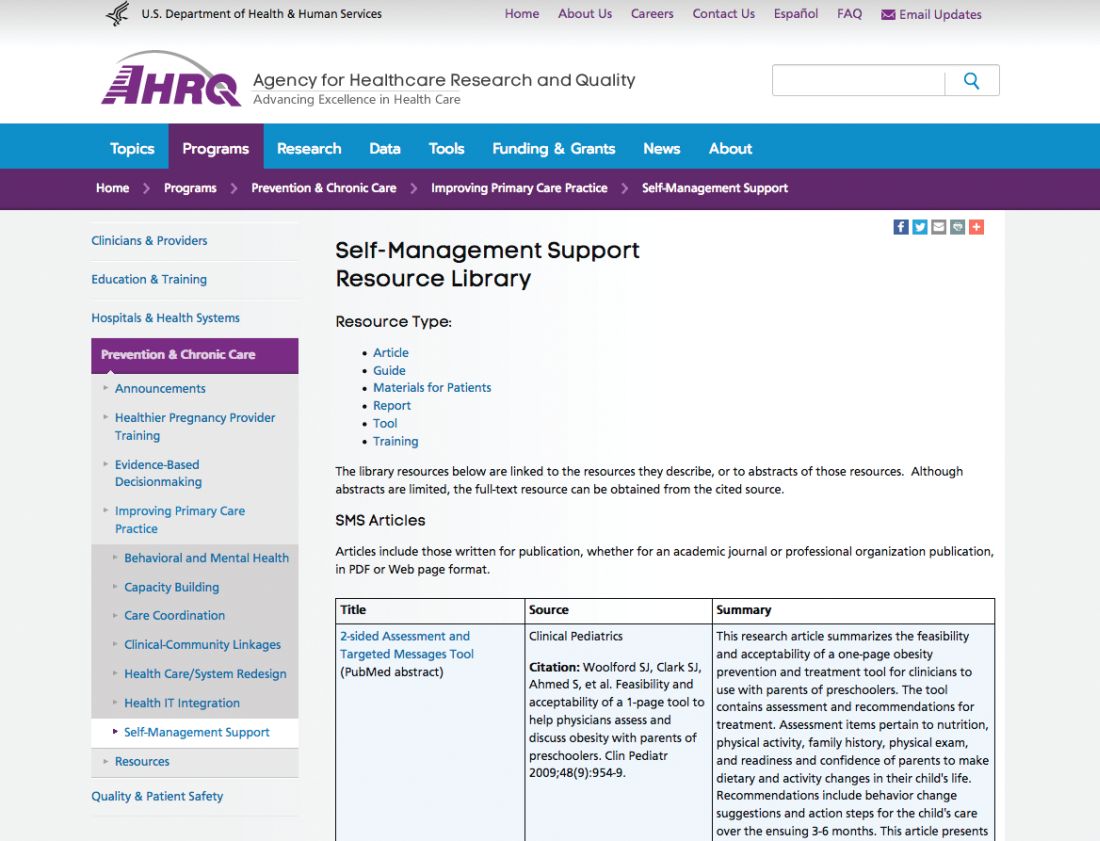
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
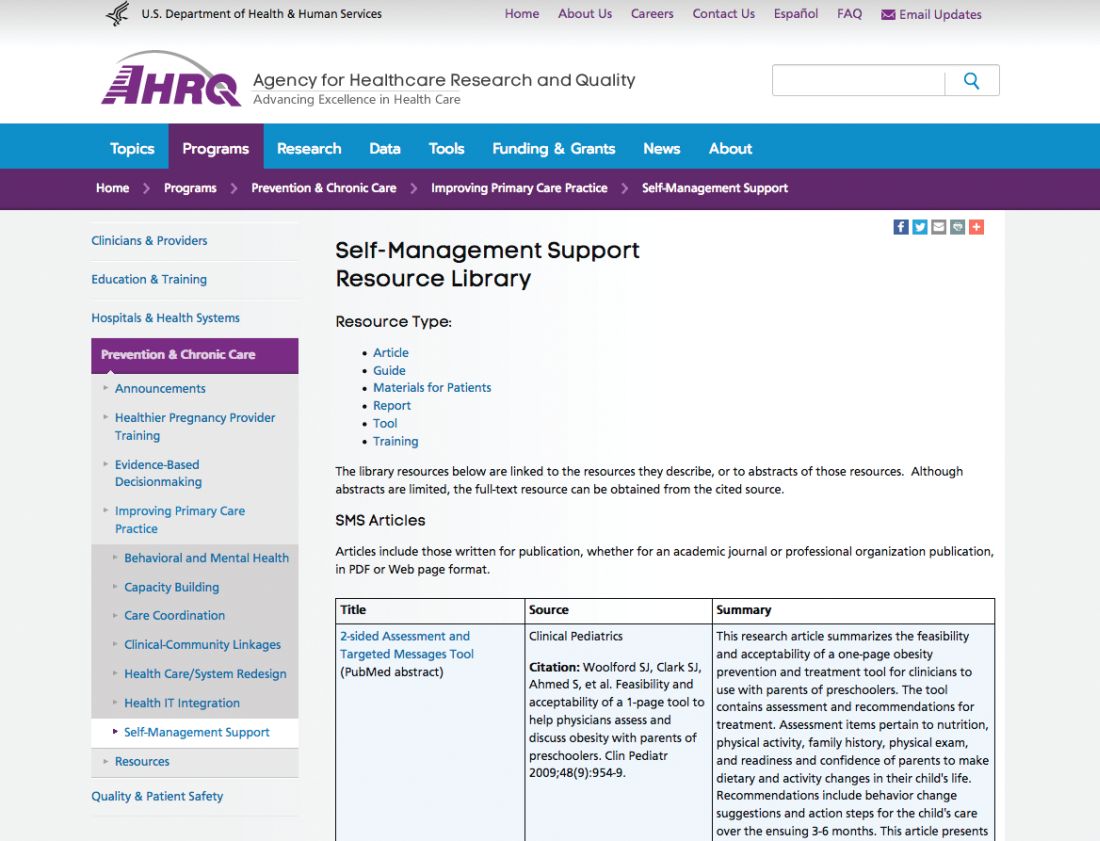
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
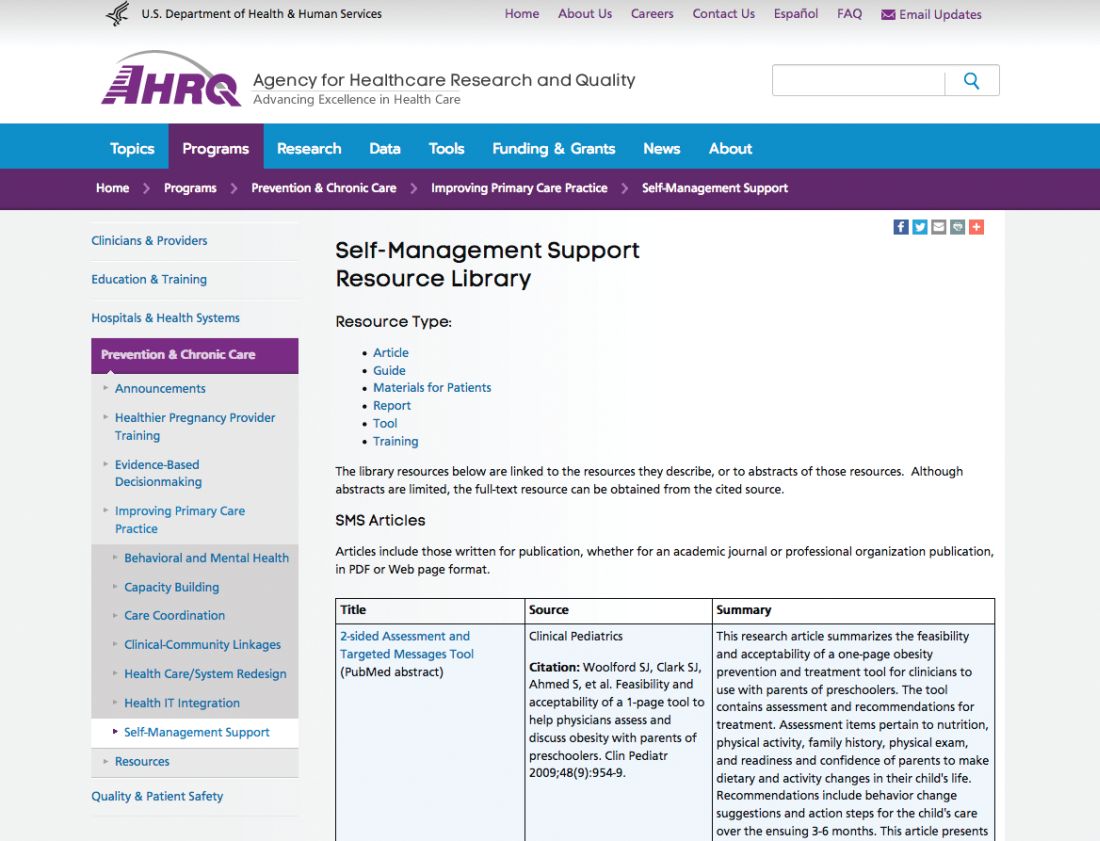
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
What is causing my patients’ macrocytosis?
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
New models of gastroenterology practice
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).
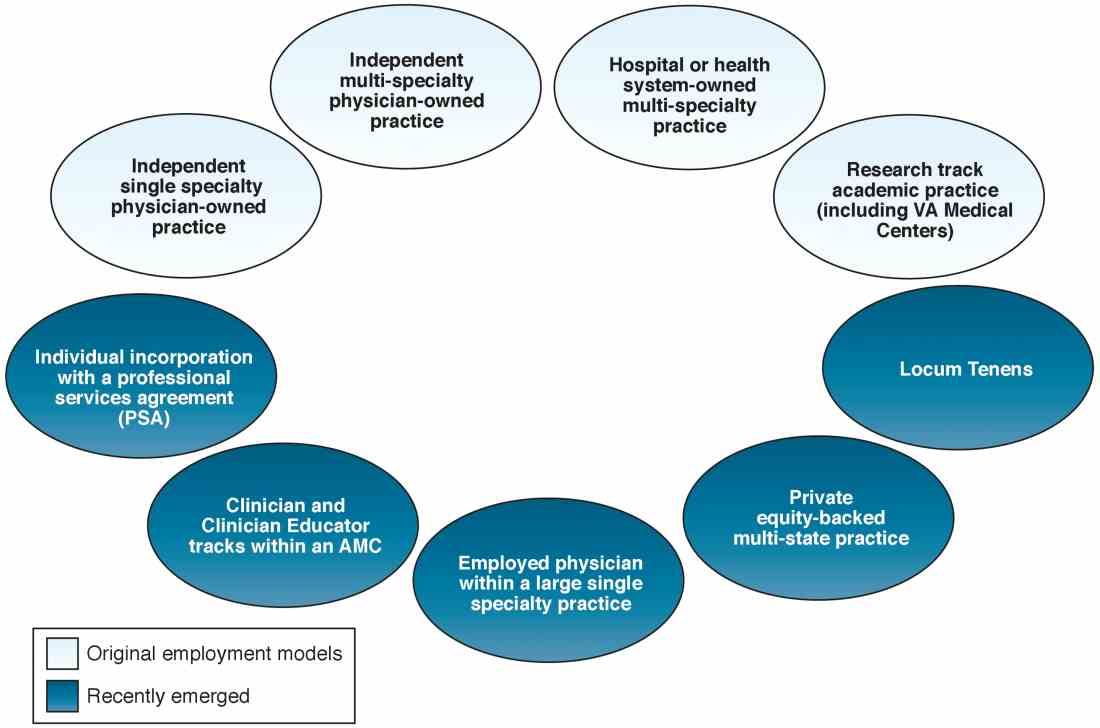
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).
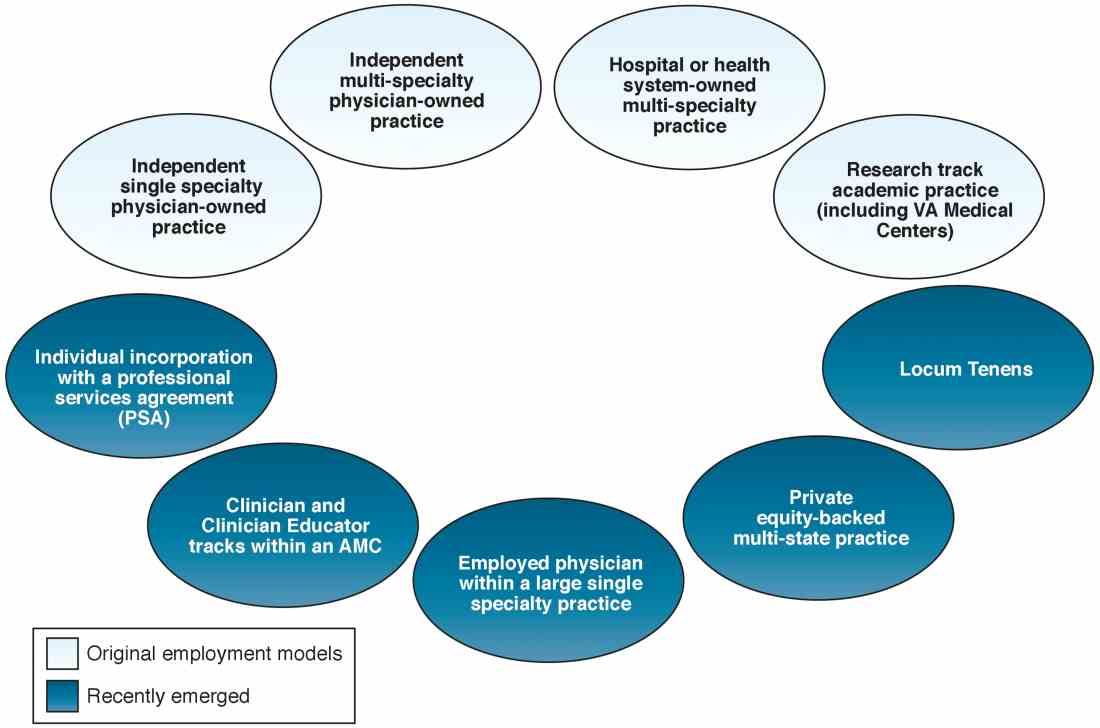
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).
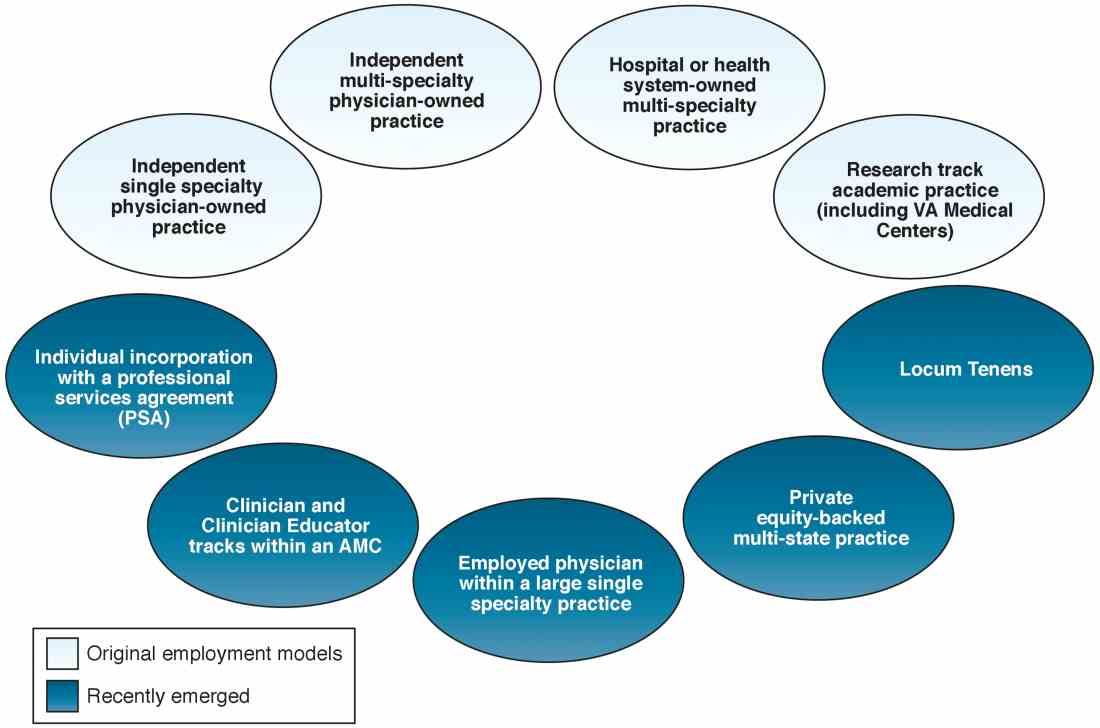
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
Opioids and us: Designed to fail
AIDS, the Vietnam War, whatever your preferred scale for measuring horrific events, the numbers from the opioid crisis are as grave or worse. And, once again, it is the young who are dying. How we got to this point is an unbelievable story of corporate greed, government incompetence, regulatory commission overreach, and, unfortunately, physician ignorance.
In 1995, as their patent on MS Contin was set to expire, Purdue Pharma gained Food and Drug Administration approval for OxyContin (“contin” is pharma talk for continuous). At this time, opioids generally were considered to be dangerous and mainly prescribed for cancer or end-of-life patients. Purdue representatives began an aggressive marketing campaign to break out of this niche. They were aided in this pursuit by the FDA, which wrote in the package insert that iatrogenic addiction was rare and the delayed absorption of OxyContin “is believed to reduce the abuse liability of a drug.” These statements were made without the backing of any clinical trials. But with an on-label statement of reduced addiction risk, representatives could sell OxyContin based on a diminished potential for abuse.
In addition to oncologists, the drug was now marketed to rheumatologists, primary care physicians, and surgeons. OxyContin, therefore, broke through the cancer barrier and became one of the most widely prescribed painkillers in the United States. While generating billions in profits, OxyContin also would become one of the most abused drugs in history.
There were several issues with OxyContin that led to its widespread misuse. The preparation contained up to 160 mg of oxycodone per pill, 16 times more than the strongest Percocet formulary. The tablet also could easily be crushed, overcoming the delayed-release formulation. Because of the FDA insert, sales representatives were free to report an addiction risk of less than 1%, which they did. Widely.
But what science backed this claim? The study referenced was not a study at all. The citation was a one-paragraph, five-sentence letter to the editor published by the New England Journal of Medicine in 1980. In it, the authors briefly described their experience with inpatient opioid therapy. No reference was made to outpatient opioid prescriptions. Still, this letter has been scientifically cited more than 600 times, with a spike starting in 1995, the year OxyContin was released. Even as thousands of Americans were dying each year from opioid use, the “study” continued to be offered as proof of a low risk of addiction. As recently as 2014, the letter was cited in the journal OncoTargets and Therapy to support the statement, “In reality, medical opioid addiction is very rare.”
Maybe if we knew our history we could avoid repeating it. Previously, the drug diacetylmorphine was introduced as a safe, nonaddictive substitute for morphine by Bayer Pharmaceutical in the late 1890s. Diacetylmorphine is better known by its trademarked name, Heroin.
In 1996, the American Pain Society and the American Academy of Pain Medicine formed a committee to issue a joint statement that advocated opioid use for chronic pain and again stating a low risk of addiction. The committee was chaired by J. David Haddox, DDS, MD, a paid speaker (and later executive) for Purdue Pharma. The American Pain Society also launched a campaign to treat pain more aggressively. “Pain is the fifth vital sign” became a far-reaching strategy, which was adopted by the Department of Veterans Affairs and, ultimately, nearly every hospital in the country. The campaign was so successful that, in 2001, the Joint Commission required hospitals to:
- Assess pain in every patient.
- Record the results.
- Provide treatment for the pain.
- Reassess the effectiveness of the treatment.
- Teach staff how to manage pain.
The Joint Commission is not alone in creating opioid-friendly regulations. The Hospital Consumer Assessment of Healthcare Providers and Systems surveys patients after hospital stays. Several of the questions include pain management. One asks the patient whether the hospital staff did “everything they could” to assist with the patient’s pain. The satisfaction scores from these surveys are directly tied to hospital payments.
In 1998, the Federation of State Medical Boards published a statement reassuring doctors that they would not be punished for prescribing even large amounts of opioids if it were in the course of medical treatment. In 2004, the FSMB went further, stating that medical boards should consider “undertreatment of pain” to be a “departure from an acceptable standard of practice,” suggesting that state medical boards should sanction doctors who undertreated pain. According to a report by Catan et al. in the Wall Street Journal, this policy was drawn up with help from Dr. Haddox, who is now a senior executive with Purdue. The FSMB also would later disclose nearly $2 million in funding from opioid manufacturers.
These regulatory groups created widespread legal and financial pressure for doctors to diagnose and quickly treat pain in every patient. But what resources did we have to do this swiftly and effectively? Opioid prescriptions soared. There were 116 million opioid prescriptions issued in 1999; by 2013, it was 207 million. Annually, there are now more opioid prescriptions filled in the United States than there are people. Overdose deaths rose 500% between 1999 and 2016. Last year, there were more than 42,000 opioid-related mortalities in the United States. Like an untended fire, the crisis now spreads unabated.
What about vascular surgeons? Few of us prescribe OxyContin. Surely the 30 Percocets we give out after surgery are safe? In reality, Percocet contains oxycodone, the same opioid found in OxyContin, and therefore, carries a high risk of addiction. Norco, Vicodin, and Lortab all contain the opioid hydrocodone. Some studies have shown a higher risk of addiction with oxycodone, but all opioids carry a significant danger of abuse and dependence. As surgeons, we came into to this crisis with little or no training. This made us susceptible to bad science, bad-faith marketing, and bad ideas from regulatory commissions. Most of us learned how to prescribe postop opioids during the “hidden curriculum” of our third and fourth years of medical school: In other words, the residents taught us. Much like learning sex education on the streets, your mileage may vary. It is no wonder that a 2016 JAMA Internal Medicine news release found that simply having surgery was a risk factor for developing an opioid addiction. Surgeons don’t have an evidence-based plan to treat postoperative pain with opioids. About 6.5% of patients are still taking “postop” opioids 3-6 months after minor surgery; the numbers are about the same for major surgery (5.9%). Therefore, it is unlikely that pain is driving this chronic use.
Richard J. Barth Jr., MD, of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., has studied opioid use following surgery extensively. He found there is a wide variety in surgeons’ opioid-prescribing habits and most of us overprescribe. In one study, 72% of the prescribed pills after surgery were not taken. He recommends the following guideline for opioid prescriptions after inpatient surgical procedures: If the patient took no opioids the day before discharge, no script is needed. For patients taking 1-3 pills the day before discharge, 15 pills are given; and for those taking 4 or more pills, a script for 30 is given.
As vascular surgeons, we must break out of our bubble and address our contributions to this crisis. It is past time to look at our own habits. Overprescribing is dangerous; the excess pills often are found by abusers, sold, or used recreationally by others in the household. Some patients take all of the pills simply because that is what the doctor prescribed; to the patient, he or she is merely following the doctor’s orders, and therefore not engaging in a risky behavior.
As vascular surgeons, there are several steps we can take immediately to reduce our contributions to the opioid epidemic and protect our patients:
- Always use the lowest effective dose of opioids and dramatically reduce the number of pills in your postop scripts. Fewer than 15 pills will cover most surgeries we perform.
- New data show that acetaminophen combined with ibuprofen works better for acute pain than acetaminophen combined with an opioid. Increase your use of nonnarcotic pain medications.
- Counsel your patients on the risk of addiction. If you plan to issue a script with only a few pills or nonnarcotics, let them know why in advance.
- Use caution when prescribing opioids to patients with anxiety or depression. The risk of addiction is much higher in these patients because of the anxiolytic and antidepressant qualities that opioids have.
- Avoid opioids in patients taking benzodiazepines, which can exacerbate the risk of respiratory depression and death.
- Help patients safely dispose of unused opioids.
- Use drug-monitoring programs whenever available.
- Use opioids for acute pain only. We do not have the training to manage long-term use.
Meanwhile, OxyContin still is available and sold exclusively by Purdue Pharma. Before its patent expired, Purdue altered the formulation to make it harder to abuse when crushing the tablets. They then lobbied the FDA to block generic production of the original formula because it was “unsafe.” Though Purdue (under Mundipharma) now markets this original version in South America, Europe, and Asia.
Many lawsuits have been brought against Purdue. Even with such high-profile lawyers as Rudy Giuliani and Eric Holder, Purdue has paid more than $600 million in fines and pleaded guilty to marketing OxyContin with “the intent to defraud or mislead.” Three Purdue executives have pleaded guilty to criminal misdemeanor charges.
In 2015, the FDA approved marketing OxyContin to children as young as age 11 years..
To address their role in the opioid crisis, the Joint Commission issued a statement on April 18, 2016. It was not a master class in self-awareness; the statement claimed that it is a “misconception” that Joint Commission standards pushed doctors to prescribe opioids. Yet, according to a Class Action complaint (Kenova v. JCAHO), in a 2001 monograph published by the Joint Commission (and funded by Purdue Pharma), they wrote “Some clinicians have inaccurate and exaggerated concerns about addiction, tolerance, and risk of death. This attitude prevails despite the fact that there is no evidence that addiction is a significant issue when persons are given opioids for pain control.”
In 2016, the AMA passed a resolution to drop pain as a vital sign. They also urged the Joint Commission to stop requiring hospitals to ask patients about the quality of their pain care. The American College of Surgeons has started an education initiative to help surgeons and patients learn about opioids and surgery (funded by Pacira Pharmaceuticals, makers of EXPAREL, an injectable long-lasting local anesthetic). In a March 2016 statement in the New England Journal of Medicine, Centers for Disease Control and Prevention representatives said of opioids “We know of no other medication routinely used for a nonfatal condition that kills patients so frequently.” As vascular surgeons, we are long overdue for a self-assessment. It is now time to change our practices and habits to help end this national addiction.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
Resources
1. Hill M et al. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. In Press.
2. Kenova v. JCAHO Class Action Complaint. United States District Court for the Southern District of West Virginia.
3. Mandell BF. The fifth vital sign: a complex story of politics and patient care. Cleveland Clinic Journal of Medicine 2016 Jun:83:400.
4. Leung PT et al. A 1980 letter on the risk of opioid addiction. New England Journal of Medicine 2017;376:2194-5.
5. www.jointcommission.org/joint_commission_statement_on_pain_management
6. www.cdc.gov/drugoverdose/epidemic/index.html
7. Catan T et al. A pain-drug champion has second thoughts. Wall Street Journal. Dec. 17, 2012 (updated online version).
8. Federation of State Medical Boards news release. www.fsmb.org/globalassets/advocacy/news-releases/2014/rems-grant-press-release-jan2014-final.pdf
9. Chou R et al. American Pain Society – American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009;10:113-130.
10. Van Zee A. The promotion and marketing of OxyContin: Commercial triumph, public health tragedy. Am J Public Health 2009;99:221-7.
11. Keefe, PR. The family that built an empire of pain. The New Yorker. October 30, 2017.
AIDS, the Vietnam War, whatever your preferred scale for measuring horrific events, the numbers from the opioid crisis are as grave or worse. And, once again, it is the young who are dying. How we got to this point is an unbelievable story of corporate greed, government incompetence, regulatory commission overreach, and, unfortunately, physician ignorance.
In 1995, as their patent on MS Contin was set to expire, Purdue Pharma gained Food and Drug Administration approval for OxyContin (“contin” is pharma talk for continuous). At this time, opioids generally were considered to be dangerous and mainly prescribed for cancer or end-of-life patients. Purdue representatives began an aggressive marketing campaign to break out of this niche. They were aided in this pursuit by the FDA, which wrote in the package insert that iatrogenic addiction was rare and the delayed absorption of OxyContin “is believed to reduce the abuse liability of a drug.” These statements were made without the backing of any clinical trials. But with an on-label statement of reduced addiction risk, representatives could sell OxyContin based on a diminished potential for abuse.
In addition to oncologists, the drug was now marketed to rheumatologists, primary care physicians, and surgeons. OxyContin, therefore, broke through the cancer barrier and became one of the most widely prescribed painkillers in the United States. While generating billions in profits, OxyContin also would become one of the most abused drugs in history.
There were several issues with OxyContin that led to its widespread misuse. The preparation contained up to 160 mg of oxycodone per pill, 16 times more than the strongest Percocet formulary. The tablet also could easily be crushed, overcoming the delayed-release formulation. Because of the FDA insert, sales representatives were free to report an addiction risk of less than 1%, which they did. Widely.
But what science backed this claim? The study referenced was not a study at all. The citation was a one-paragraph, five-sentence letter to the editor published by the New England Journal of Medicine in 1980. In it, the authors briefly described their experience with inpatient opioid therapy. No reference was made to outpatient opioid prescriptions. Still, this letter has been scientifically cited more than 600 times, with a spike starting in 1995, the year OxyContin was released. Even as thousands of Americans were dying each year from opioid use, the “study” continued to be offered as proof of a low risk of addiction. As recently as 2014, the letter was cited in the journal OncoTargets and Therapy to support the statement, “In reality, medical opioid addiction is very rare.”
Maybe if we knew our history we could avoid repeating it. Previously, the drug diacetylmorphine was introduced as a safe, nonaddictive substitute for morphine by Bayer Pharmaceutical in the late 1890s. Diacetylmorphine is better known by its trademarked name, Heroin.
In 1996, the American Pain Society and the American Academy of Pain Medicine formed a committee to issue a joint statement that advocated opioid use for chronic pain and again stating a low risk of addiction. The committee was chaired by J. David Haddox, DDS, MD, a paid speaker (and later executive) for Purdue Pharma. The American Pain Society also launched a campaign to treat pain more aggressively. “Pain is the fifth vital sign” became a far-reaching strategy, which was adopted by the Department of Veterans Affairs and, ultimately, nearly every hospital in the country. The campaign was so successful that, in 2001, the Joint Commission required hospitals to:
- Assess pain in every patient.
- Record the results.
- Provide treatment for the pain.
- Reassess the effectiveness of the treatment.
- Teach staff how to manage pain.
The Joint Commission is not alone in creating opioid-friendly regulations. The Hospital Consumer Assessment of Healthcare Providers and Systems surveys patients after hospital stays. Several of the questions include pain management. One asks the patient whether the hospital staff did “everything they could” to assist with the patient’s pain. The satisfaction scores from these surveys are directly tied to hospital payments.
In 1998, the Federation of State Medical Boards published a statement reassuring doctors that they would not be punished for prescribing even large amounts of opioids if it were in the course of medical treatment. In 2004, the FSMB went further, stating that medical boards should consider “undertreatment of pain” to be a “departure from an acceptable standard of practice,” suggesting that state medical boards should sanction doctors who undertreated pain. According to a report by Catan et al. in the Wall Street Journal, this policy was drawn up with help from Dr. Haddox, who is now a senior executive with Purdue. The FSMB also would later disclose nearly $2 million in funding from opioid manufacturers.
These regulatory groups created widespread legal and financial pressure for doctors to diagnose and quickly treat pain in every patient. But what resources did we have to do this swiftly and effectively? Opioid prescriptions soared. There were 116 million opioid prescriptions issued in 1999; by 2013, it was 207 million. Annually, there are now more opioid prescriptions filled in the United States than there are people. Overdose deaths rose 500% between 1999 and 2016. Last year, there were more than 42,000 opioid-related mortalities in the United States. Like an untended fire, the crisis now spreads unabated.
What about vascular surgeons? Few of us prescribe OxyContin. Surely the 30 Percocets we give out after surgery are safe? In reality, Percocet contains oxycodone, the same opioid found in OxyContin, and therefore, carries a high risk of addiction. Norco, Vicodin, and Lortab all contain the opioid hydrocodone. Some studies have shown a higher risk of addiction with oxycodone, but all opioids carry a significant danger of abuse and dependence. As surgeons, we came into to this crisis with little or no training. This made us susceptible to bad science, bad-faith marketing, and bad ideas from regulatory commissions. Most of us learned how to prescribe postop opioids during the “hidden curriculum” of our third and fourth years of medical school: In other words, the residents taught us. Much like learning sex education on the streets, your mileage may vary. It is no wonder that a 2016 JAMA Internal Medicine news release found that simply having surgery was a risk factor for developing an opioid addiction. Surgeons don’t have an evidence-based plan to treat postoperative pain with opioids. About 6.5% of patients are still taking “postop” opioids 3-6 months after minor surgery; the numbers are about the same for major surgery (5.9%). Therefore, it is unlikely that pain is driving this chronic use.
Richard J. Barth Jr., MD, of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., has studied opioid use following surgery extensively. He found there is a wide variety in surgeons’ opioid-prescribing habits and most of us overprescribe. In one study, 72% of the prescribed pills after surgery were not taken. He recommends the following guideline for opioid prescriptions after inpatient surgical procedures: If the patient took no opioids the day before discharge, no script is needed. For patients taking 1-3 pills the day before discharge, 15 pills are given; and for those taking 4 or more pills, a script for 30 is given.
As vascular surgeons, we must break out of our bubble and address our contributions to this crisis. It is past time to look at our own habits. Overprescribing is dangerous; the excess pills often are found by abusers, sold, or used recreationally by others in the household. Some patients take all of the pills simply because that is what the doctor prescribed; to the patient, he or she is merely following the doctor’s orders, and therefore not engaging in a risky behavior.
As vascular surgeons, there are several steps we can take immediately to reduce our contributions to the opioid epidemic and protect our patients:
- Always use the lowest effective dose of opioids and dramatically reduce the number of pills in your postop scripts. Fewer than 15 pills will cover most surgeries we perform.
- New data show that acetaminophen combined with ibuprofen works better for acute pain than acetaminophen combined with an opioid. Increase your use of nonnarcotic pain medications.
- Counsel your patients on the risk of addiction. If you plan to issue a script with only a few pills or nonnarcotics, let them know why in advance.
- Use caution when prescribing opioids to patients with anxiety or depression. The risk of addiction is much higher in these patients because of the anxiolytic and antidepressant qualities that opioids have.
- Avoid opioids in patients taking benzodiazepines, which can exacerbate the risk of respiratory depression and death.
- Help patients safely dispose of unused opioids.
- Use drug-monitoring programs whenever available.
- Use opioids for acute pain only. We do not have the training to manage long-term use.
Meanwhile, OxyContin still is available and sold exclusively by Purdue Pharma. Before its patent expired, Purdue altered the formulation to make it harder to abuse when crushing the tablets. They then lobbied the FDA to block generic production of the original formula because it was “unsafe.” Though Purdue (under Mundipharma) now markets this original version in South America, Europe, and Asia.
Many lawsuits have been brought against Purdue. Even with such high-profile lawyers as Rudy Giuliani and Eric Holder, Purdue has paid more than $600 million in fines and pleaded guilty to marketing OxyContin with “the intent to defraud or mislead.” Three Purdue executives have pleaded guilty to criminal misdemeanor charges.
In 2015, the FDA approved marketing OxyContin to children as young as age 11 years..
To address their role in the opioid crisis, the Joint Commission issued a statement on April 18, 2016. It was not a master class in self-awareness; the statement claimed that it is a “misconception” that Joint Commission standards pushed doctors to prescribe opioids. Yet, according to a Class Action complaint (Kenova v. JCAHO), in a 2001 monograph published by the Joint Commission (and funded by Purdue Pharma), they wrote “Some clinicians have inaccurate and exaggerated concerns about addiction, tolerance, and risk of death. This attitude prevails despite the fact that there is no evidence that addiction is a significant issue when persons are given opioids for pain control.”
In 2016, the AMA passed a resolution to drop pain as a vital sign. They also urged the Joint Commission to stop requiring hospitals to ask patients about the quality of their pain care. The American College of Surgeons has started an education initiative to help surgeons and patients learn about opioids and surgery (funded by Pacira Pharmaceuticals, makers of EXPAREL, an injectable long-lasting local anesthetic). In a March 2016 statement in the New England Journal of Medicine, Centers for Disease Control and Prevention representatives said of opioids “We know of no other medication routinely used for a nonfatal condition that kills patients so frequently.” As vascular surgeons, we are long overdue for a self-assessment. It is now time to change our practices and habits to help end this national addiction.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
Resources
1. Hill M et al. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. In Press.
2. Kenova v. JCAHO Class Action Complaint. United States District Court for the Southern District of West Virginia.
3. Mandell BF. The fifth vital sign: a complex story of politics and patient care. Cleveland Clinic Journal of Medicine 2016 Jun:83:400.
4. Leung PT et al. A 1980 letter on the risk of opioid addiction. New England Journal of Medicine 2017;376:2194-5.
5. www.jointcommission.org/joint_commission_statement_on_pain_management
6. www.cdc.gov/drugoverdose/epidemic/index.html
7. Catan T et al. A pain-drug champion has second thoughts. Wall Street Journal. Dec. 17, 2012 (updated online version).
8. Federation of State Medical Boards news release. www.fsmb.org/globalassets/advocacy/news-releases/2014/rems-grant-press-release-jan2014-final.pdf
9. Chou R et al. American Pain Society – American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009;10:113-130.
10. Van Zee A. The promotion and marketing of OxyContin: Commercial triumph, public health tragedy. Am J Public Health 2009;99:221-7.
11. Keefe, PR. The family that built an empire of pain. The New Yorker. October 30, 2017.
AIDS, the Vietnam War, whatever your preferred scale for measuring horrific events, the numbers from the opioid crisis are as grave or worse. And, once again, it is the young who are dying. How we got to this point is an unbelievable story of corporate greed, government incompetence, regulatory commission overreach, and, unfortunately, physician ignorance.
In 1995, as their patent on MS Contin was set to expire, Purdue Pharma gained Food and Drug Administration approval for OxyContin (“contin” is pharma talk for continuous). At this time, opioids generally were considered to be dangerous and mainly prescribed for cancer or end-of-life patients. Purdue representatives began an aggressive marketing campaign to break out of this niche. They were aided in this pursuit by the FDA, which wrote in the package insert that iatrogenic addiction was rare and the delayed absorption of OxyContin “is believed to reduce the abuse liability of a drug.” These statements were made without the backing of any clinical trials. But with an on-label statement of reduced addiction risk, representatives could sell OxyContin based on a diminished potential for abuse.
In addition to oncologists, the drug was now marketed to rheumatologists, primary care physicians, and surgeons. OxyContin, therefore, broke through the cancer barrier and became one of the most widely prescribed painkillers in the United States. While generating billions in profits, OxyContin also would become one of the most abused drugs in history.
There were several issues with OxyContin that led to its widespread misuse. The preparation contained up to 160 mg of oxycodone per pill, 16 times more than the strongest Percocet formulary. The tablet also could easily be crushed, overcoming the delayed-release formulation. Because of the FDA insert, sales representatives were free to report an addiction risk of less than 1%, which they did. Widely.
But what science backed this claim? The study referenced was not a study at all. The citation was a one-paragraph, five-sentence letter to the editor published by the New England Journal of Medicine in 1980. In it, the authors briefly described their experience with inpatient opioid therapy. No reference was made to outpatient opioid prescriptions. Still, this letter has been scientifically cited more than 600 times, with a spike starting in 1995, the year OxyContin was released. Even as thousands of Americans were dying each year from opioid use, the “study” continued to be offered as proof of a low risk of addiction. As recently as 2014, the letter was cited in the journal OncoTargets and Therapy to support the statement, “In reality, medical opioid addiction is very rare.”
Maybe if we knew our history we could avoid repeating it. Previously, the drug diacetylmorphine was introduced as a safe, nonaddictive substitute for morphine by Bayer Pharmaceutical in the late 1890s. Diacetylmorphine is better known by its trademarked name, Heroin.
In 1996, the American Pain Society and the American Academy of Pain Medicine formed a committee to issue a joint statement that advocated opioid use for chronic pain and again stating a low risk of addiction. The committee was chaired by J. David Haddox, DDS, MD, a paid speaker (and later executive) for Purdue Pharma. The American Pain Society also launched a campaign to treat pain more aggressively. “Pain is the fifth vital sign” became a far-reaching strategy, which was adopted by the Department of Veterans Affairs and, ultimately, nearly every hospital in the country. The campaign was so successful that, in 2001, the Joint Commission required hospitals to:
- Assess pain in every patient.
- Record the results.
- Provide treatment for the pain.
- Reassess the effectiveness of the treatment.
- Teach staff how to manage pain.
The Joint Commission is not alone in creating opioid-friendly regulations. The Hospital Consumer Assessment of Healthcare Providers and Systems surveys patients after hospital stays. Several of the questions include pain management. One asks the patient whether the hospital staff did “everything they could” to assist with the patient’s pain. The satisfaction scores from these surveys are directly tied to hospital payments.
In 1998, the Federation of State Medical Boards published a statement reassuring doctors that they would not be punished for prescribing even large amounts of opioids if it were in the course of medical treatment. In 2004, the FSMB went further, stating that medical boards should consider “undertreatment of pain” to be a “departure from an acceptable standard of practice,” suggesting that state medical boards should sanction doctors who undertreated pain. According to a report by Catan et al. in the Wall Street Journal, this policy was drawn up with help from Dr. Haddox, who is now a senior executive with Purdue. The FSMB also would later disclose nearly $2 million in funding from opioid manufacturers.
These regulatory groups created widespread legal and financial pressure for doctors to diagnose and quickly treat pain in every patient. But what resources did we have to do this swiftly and effectively? Opioid prescriptions soared. There were 116 million opioid prescriptions issued in 1999; by 2013, it was 207 million. Annually, there are now more opioid prescriptions filled in the United States than there are people. Overdose deaths rose 500% between 1999 and 2016. Last year, there were more than 42,000 opioid-related mortalities in the United States. Like an untended fire, the crisis now spreads unabated.
What about vascular surgeons? Few of us prescribe OxyContin. Surely the 30 Percocets we give out after surgery are safe? In reality, Percocet contains oxycodone, the same opioid found in OxyContin, and therefore, carries a high risk of addiction. Norco, Vicodin, and Lortab all contain the opioid hydrocodone. Some studies have shown a higher risk of addiction with oxycodone, but all opioids carry a significant danger of abuse and dependence. As surgeons, we came into to this crisis with little or no training. This made us susceptible to bad science, bad-faith marketing, and bad ideas from regulatory commissions. Most of us learned how to prescribe postop opioids during the “hidden curriculum” of our third and fourth years of medical school: In other words, the residents taught us. Much like learning sex education on the streets, your mileage may vary. It is no wonder that a 2016 JAMA Internal Medicine news release found that simply having surgery was a risk factor for developing an opioid addiction. Surgeons don’t have an evidence-based plan to treat postoperative pain with opioids. About 6.5% of patients are still taking “postop” opioids 3-6 months after minor surgery; the numbers are about the same for major surgery (5.9%). Therefore, it is unlikely that pain is driving this chronic use.
Richard J. Barth Jr., MD, of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., has studied opioid use following surgery extensively. He found there is a wide variety in surgeons’ opioid-prescribing habits and most of us overprescribe. In one study, 72% of the prescribed pills after surgery were not taken. He recommends the following guideline for opioid prescriptions after inpatient surgical procedures: If the patient took no opioids the day before discharge, no script is needed. For patients taking 1-3 pills the day before discharge, 15 pills are given; and for those taking 4 or more pills, a script for 30 is given.
As vascular surgeons, we must break out of our bubble and address our contributions to this crisis. It is past time to look at our own habits. Overprescribing is dangerous; the excess pills often are found by abusers, sold, or used recreationally by others in the household. Some patients take all of the pills simply because that is what the doctor prescribed; to the patient, he or she is merely following the doctor’s orders, and therefore not engaging in a risky behavior.
As vascular surgeons, there are several steps we can take immediately to reduce our contributions to the opioid epidemic and protect our patients:
- Always use the lowest effective dose of opioids and dramatically reduce the number of pills in your postop scripts. Fewer than 15 pills will cover most surgeries we perform.
- New data show that acetaminophen combined with ibuprofen works better for acute pain than acetaminophen combined with an opioid. Increase your use of nonnarcotic pain medications.
- Counsel your patients on the risk of addiction. If you plan to issue a script with only a few pills or nonnarcotics, let them know why in advance.
- Use caution when prescribing opioids to patients with anxiety or depression. The risk of addiction is much higher in these patients because of the anxiolytic and antidepressant qualities that opioids have.
- Avoid opioids in patients taking benzodiazepines, which can exacerbate the risk of respiratory depression and death.
- Help patients safely dispose of unused opioids.
- Use drug-monitoring programs whenever available.
- Use opioids for acute pain only. We do not have the training to manage long-term use.
Meanwhile, OxyContin still is available and sold exclusively by Purdue Pharma. Before its patent expired, Purdue altered the formulation to make it harder to abuse when crushing the tablets. They then lobbied the FDA to block generic production of the original formula because it was “unsafe.” Though Purdue (under Mundipharma) now markets this original version in South America, Europe, and Asia.
Many lawsuits have been brought against Purdue. Even with such high-profile lawyers as Rudy Giuliani and Eric Holder, Purdue has paid more than $600 million in fines and pleaded guilty to marketing OxyContin with “the intent to defraud or mislead.” Three Purdue executives have pleaded guilty to criminal misdemeanor charges.
In 2015, the FDA approved marketing OxyContin to children as young as age 11 years..
To address their role in the opioid crisis, the Joint Commission issued a statement on April 18, 2016. It was not a master class in self-awareness; the statement claimed that it is a “misconception” that Joint Commission standards pushed doctors to prescribe opioids. Yet, according to a Class Action complaint (Kenova v. JCAHO), in a 2001 monograph published by the Joint Commission (and funded by Purdue Pharma), they wrote “Some clinicians have inaccurate and exaggerated concerns about addiction, tolerance, and risk of death. This attitude prevails despite the fact that there is no evidence that addiction is a significant issue when persons are given opioids for pain control.”
In 2016, the AMA passed a resolution to drop pain as a vital sign. They also urged the Joint Commission to stop requiring hospitals to ask patients about the quality of their pain care. The American College of Surgeons has started an education initiative to help surgeons and patients learn about opioids and surgery (funded by Pacira Pharmaceuticals, makers of EXPAREL, an injectable long-lasting local anesthetic). In a March 2016 statement in the New England Journal of Medicine, Centers for Disease Control and Prevention representatives said of opioids “We know of no other medication routinely used for a nonfatal condition that kills patients so frequently.” As vascular surgeons, we are long overdue for a self-assessment. It is now time to change our practices and habits to help end this national addiction.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
Resources
1. Hill M et al. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. In Press.
2. Kenova v. JCAHO Class Action Complaint. United States District Court for the Southern District of West Virginia.
3. Mandell BF. The fifth vital sign: a complex story of politics and patient care. Cleveland Clinic Journal of Medicine 2016 Jun:83:400.
4. Leung PT et al. A 1980 letter on the risk of opioid addiction. New England Journal of Medicine 2017;376:2194-5.
5. www.jointcommission.org/joint_commission_statement_on_pain_management
6. www.cdc.gov/drugoverdose/epidemic/index.html
7. Catan T et al. A pain-drug champion has second thoughts. Wall Street Journal. Dec. 17, 2012 (updated online version).
8. Federation of State Medical Boards news release. www.fsmb.org/globalassets/advocacy/news-releases/2014/rems-grant-press-release-jan2014-final.pdf
9. Chou R et al. American Pain Society – American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009;10:113-130.
10. Van Zee A. The promotion and marketing of OxyContin: Commercial triumph, public health tragedy. Am J Public Health 2009;99:221-7.
11. Keefe, PR. The family that built an empire of pain. The New Yorker. October 30, 2017.
What to eat
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It’s not about time
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Pediatric Dermatology Consult - June 2018
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
A 9-year-old girl presented to the dermatology clinic, referred by her pediatrician, for evaluation of asymptomatic lesions on her shins and feet for 2 months. She started developing one lesion over her right shin with other lesions appearing on the opposite leg a few weeks after, and treated the areas initially with an over-the-counter antifungal cream without improvement. She has been healthy and denied any recent fevers or upper respiratory infections, and said she had not taken any medications or vitamin supplements. She reported camping with her father occasionally but denied any bug or tick bites. No other family members were affected. There was no personal or family history of diabetes mellitus or high cholesterol, and there are no pets at home.
Americans back from captivity need decompression period
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.