User login
Navigating the Search for a Financial Adviser
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?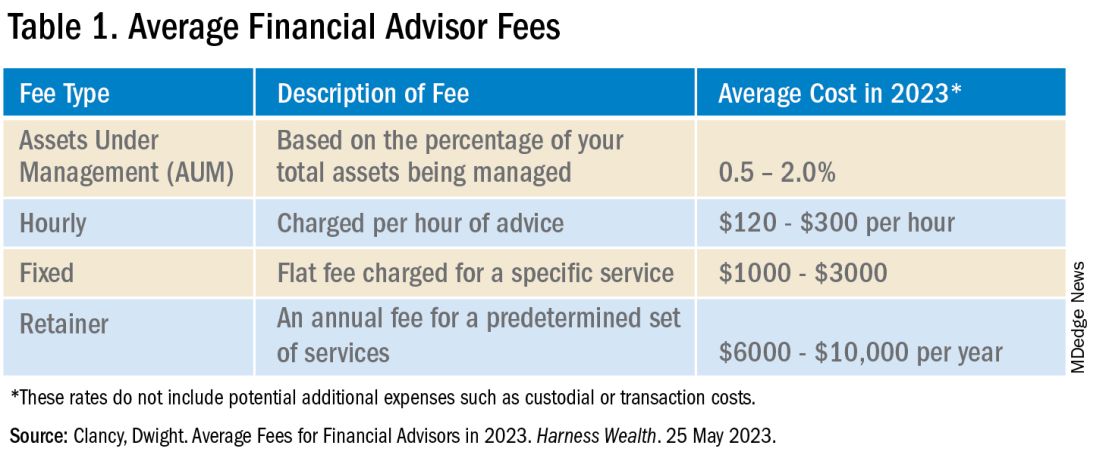
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?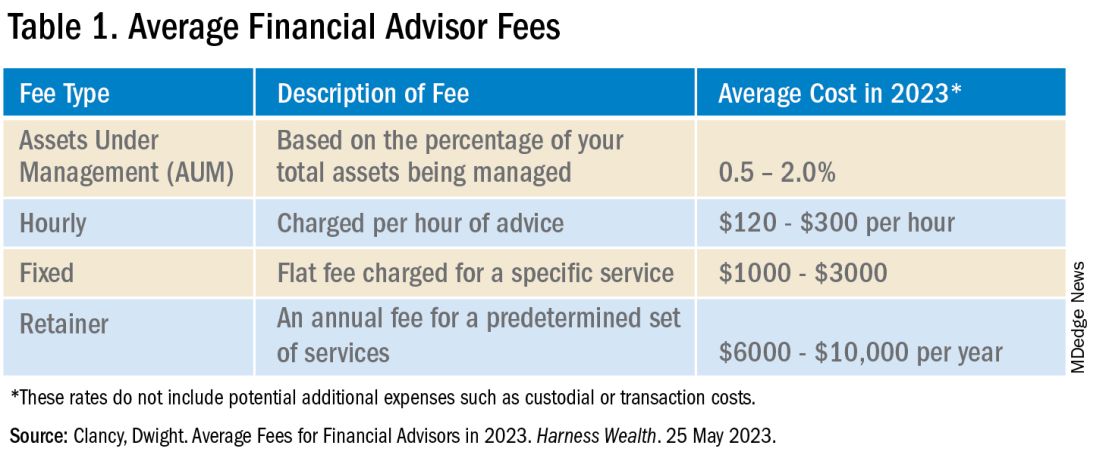
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
As gastroenterologists, we spend innumerable years in medical training with an abrupt and significant increase in our earning potential upon beginning practice. The majority of us also carry a sizeable amount of student loan debt. This combination results in a unique situation that can make us hesitant about how best to set ourselves up financially while also making us vulnerable to potentially predatory financial practices.
Although your initial steps to achieve financial wellness and build wealth can be obtained on your own with some education, a financial adviser becomes indispensable when you have significant assets, a high income, complex finances, and/or are experiencing a major life change. Additionally, as there are so many avenues to invest and grow your capital, a financial adviser can assist in designing a portfolio to best accomplish specific monetary goals. Studies have demonstrated that those working with a financial adviser reduce their single-stock risk and have more significant increase in portfolio value, reducing the total cost associated with their investments’ management.1 Those working with a financial adviser will also net up to a 3% larger annual return, compared with a standard baseline investment plan.2,3
Based on this information, it may appear that working with a personal financial adviser would be a no-brainer. Unfortunately, there is a caveat: There is no legal regulation regarding who can use the title “financial adviser.” It is therefore crucial to be aware of common practices and terminology to best help you identify a reputable financial adviser and reduce your risk of excessive fees or financial loss. This is also a highly personal decision and your search should first begin with understanding why you are looking for an adviser, as this will determine the appropriate type of service to look for.
Types of Advisers
A certified financial planner (CFP) is an expert in estate planning, taxes, retirement saving, and financial planning who has a formal designation by the Certified Financial Planner Board of Standards Inc.4 They must undergo stringent licensing examinations following a 3-year course with required continuing education to maintain their credentials. CFPs are fiduciaries, meaning they must make financial decisions in your best interest, even if they may make less money with that product or investment strategy. In other words, they are beholden to give honest, impartial recommendations to their clients, and may face sanctions by the CFP Board if found to violate its Code of Ethics and Standards of Conduct, which includes failure to act in a fiduciary duty.5
CFPs evaluate your total financial picture, such as investments, insurance policies, and overall current financial position, to develop a comprehensive strategy that will successfully guide you to your financial goal. There are many individuals who may refer to themselves as financial planners without having the CFP designation; while they may offer similar services as above, they will not be required to act as a fiduciary. Hence, it is important to do your due diligence and verify they hold this certification via the CFP Board website: www.cfp.net/verify-a-cfp-professional.
An investment adviser is a legal term from the U.S. Securities and Exchange Commission (SEC) and the Financial Industry Regulatory Authority (FINRA) referring to an individual who provides recommendations and analyses for financial securities such as stock. Both of these agencies ensure investment advisers adhere to regulatory requirements designed to protect client investers. Similar to CFPs, they are held to a fiduciary standard, and their firm is required to register with the SEC or the state of practice based on the amount of assets under management.6
An individual investment adviser must also register with their state as an Investment Adviser Representative (IAR), the distinctive term referring to an individual as opposed to an investment advising firm. Investment advisers are required to pass the extensive Series 65, Uniform Investment Advisor Law Exam, or equivalent, by states requiring licensure.7 They can guide you on the selection of particular investments and portfolio management based on a discussion with you regarding your current financial standing and what fiscal ambitions you wish to achieve.
A financial adviser provides direction on a multitude of financially related topics such as investing, tax laws, and life insurance with the goal to help you reach specific financial objectives. However, this term is often used quite ubiquitously given the lack of formal regulation of the title. Essentially, those with varying types of educational background can give themselves the title of financial adviser.
If a financial adviser buys or sells financial securities such as stocks or bonds, then they must be registered as a licensed broker with the SEC and IAR and pass the Series 6 or Series 7 exam. Unlike CFPs and investment advisers, a financial adviser (if also a licensed broker) is not required to be a fiduciary, and instead works under the suitability standard.8 Suitability requires that financial recommendations made by the adviser are appropriate but not necessarily the best for the client. In fact, these recommendations do not even have to be the most suitable. This is where conflicts of interest can arise with the adviser recommending products and securities that best compensate them while not serving the best return on investment for you.
Making the search for a financial adviser more complex, an individual can be a combination of any of the above, pending the appropriate licensing. For example, a CFP can also be an asset manager and thus hold the title of a financial adviser and/or IAR. A financial adviser may also not directly manage your assets if they have a partnership with a third party or another licensed individual. Questions to ask of your potential financial adviser should therefore include the following:
- What licensure and related education do you have?
- What is your particular area of expertise?
- How long have you been in practice?
- How will you be managing my assets?
Financial Adviser Fee Schedules
Prior to working with a financial adviser, you must also inquire about their fee structure. There are two kinds of fee schedules used by financial advisers: fee-only and fee-based.
Fee-only advisers receive payment solely for the services they provide. They do not collect commissions from third parties providing the recommended products. There is variability in how this type of payment schedule is structured, encompassing flat fees, hourly rates, or the adviser charging a retainer. The Table below compares the types of fee-only structures and range of charges based on 2023 rates.9 Of note, fee-only advisers serve as fiduciaries.10
Fee-based financial advisers receive payment for services but may also receive commission on specific products they sell to you.9 Most, if not all, financial experts recommend avoiding advisers using commission-based charges given the potential conflict of interest: How can one be absolutely sure this recommended financial product is best for you, knowing your adviser has a financial stake in said item?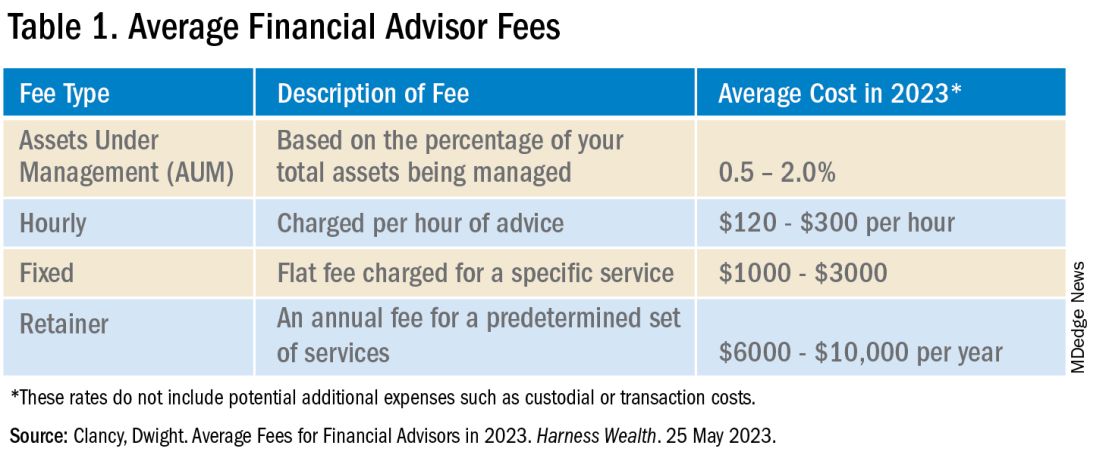
In addition to charging the fees above, your financial adviser, if they are actively managing your investment portfolio, will also charge an assets under management (AUM) fee. This is a percentage of the dollar amount within your portfolio. For example, if your adviser charges a 1% AUM rate for your account totaling $100,000, this equates to a $1,000 fee in that calendar year. AUM fees typically decrease as the size of your portfolio increases. As seen in the Table, there is a wide range of the average AUM rate (0.5%–2%); however, an AUM fee approaching 2% is unnecessarily high and consumes a significant portion of your portfolio. Thus, it is recommended to look for a money manager with an approximate 1% AUM fee.
Many of us delay or avoid working with a financial adviser due to the potential perceived risks of having poor portfolio management from an adviser not working in our best interest, along with the concern for excessive fees. In many ways, it is how we counsel our patients. While they can seek medical information on their own, their best care is under the guidance of an expert: a healthcare professional. That being said, personal finance is indeed personal, so I hope this guide helps facilitate your search and increase your financial wellness.
Dr. Luthra is a therapeutic endoscopist at Moffitt Cancer Center, Tampa, Florida, and the founder of The Scope of Finance, a financial wellness education and coaching company focused on physicians. Her interest in financial well-being is thanks to the teachings of her father, an entrepreneur and former Certified Financial Planner (CFP). She can be found on Instagram (thescopeoffinance) and X (@ScopeofFinance). She reports no financial disclosures relevant to this article.
References
1. Pagliaro CA and Utkus SP. Assessing the value of advice. Vanguard. 2019 Sept.
2. Kinniry Jr. FM et al. Putting a value on your value: Quantifying Vanguard Advisor’s Alpha. Vanguard. 2022 July.
3. Horan S. What Are the Benefits of Working with a Financial Advisor? – 2021 Study. Smart Asset. 2023 July 27.
4. Kagan J. Certified Financial PlannerTM(CFP): What It Is and How to Become One. Investopedia. 2023 Aug 3.
5. CFP Board. Our Commitment to Ethical Standards. CFP Board. 2024.
6. Staff of the Investment Adviser Regulation Office Division of Investment Management, U.S. Securities and Exchange Commission. Regulation of Investment Advisers by the U.S. Securities and Exchange Commission. 2013 Mar.
7. Hicks C. Investment Advisor vs. Financial Advisor: There is a Difference. US News & World Report. 2019 June 13.
8. Roberts K. Financial advisor vs. financial planner: What is the difference? Bankrate. 2023 Nov 21.
9. Clancy D. Average Fees for Financial Advisors in 2023. Harness Wealth. 2023 May 25.
10. Palmer B. Fee- vs. Commission-Based Advisor: What’s the Difference? Investopedia. 2023 June 20.
Achieving Promotion for Junior Faculty in Academic Medicine: An Interview With Experts
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Defining Your ‘Success’
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Danielle Kiefer ([email protected]), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Danielle Kiefer ([email protected]), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Dear Friends,
The prevailing theme of this issue is “Success.” I have learned that “success” is personal and personalized. What “success” looked like 10, or even 5, years ago to me is very different from how I perceive it now; and I know it may be different 5 years from now. My definition of success should not look like another’s — that was the best advice I have gotten over the years and it has kept me constantly redefining what is important to me and placing value on where I want to allocate my time and efforts, at work and at home.
This issue of The New Gastroenterologist highlights topics from successful GIs within their own realms of expertise, offering insights on advancing in academic medicine, navigating financial wellness with a financial adviser, and becoming a future leader in GI.
In this issue’s clinically-focused articles, we spotlight two very nuanced and challenging topics. Dr. Sachin Srinivasan and Dr. Prateek Sharma review Barrett’s esophagus management for our “In Focus” section, with a particular emphasis on Barrett’s endoscopic therapy modalities for dysplasia and early neoplasia. Dr. Brooke Corning and team simplify their approach to pelvic floor dysfunction (PFD) in our “Short Clinical Reviews.” They suggest validated ways to assess patient history, pros and cons of various diagnostic tests, and stepwise management of PFD.
Navigating academic promotion can be overwhelming and may not be at the forefront with our early career GIs’ priorities. In our “Early Career” section, Dr. Vineet Rolston interviews two highly accomplished professors in academic medicine, Dr. Sophie Balzora and Dr. Mark Schattner, for their insights into the promotion process and recommendations for junior faculty.
Dr. Anjuli K. Luthra, a therapeutic endoscopist and founder of The Scope of Finance, emphasizes financial wellness for physicians. She breaks down the search for a financial adviser, including the different types, what to ask when searching for the right fit, and what to expect.
Lastly, this issue highlights an AGA program that invests in the development of leaders for the field — the Future Leaders Program (FLP). Dr. Parakkal Deepak and Dr. Edward L. Barnes, along with their mentor, Dr. Aasma Shaukat, describe their experience as a mentee-mentor triad of FLP and how this program has impacted their careers.
If you are interested in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Danielle Kiefer ([email protected]), managing editor of TNG.
Until next time, I leave you with a historical fun fact because we would not be where we are now without appreciating where we were: Dr. C.G. Stockton was the first AGA president in 1897, a Professor of the Principles and Practice of Medicine and Clinical Medicine at the University of Buffalo in New York, and published on the relationship between GI/Hepatology and gout in the Journal of the American Medical Association the same year of his presidency.
Yours truly,
Judy A. Trieu, MD, MPH
Editor-in-Chief
Interventional Endoscopy, Division of Gastroenterology
Washington University in St. Louis
Converging on Our Nation’s Capital
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Release of our May issue coincides with our annual pilgrimage to Digestive Disease Week® (DDW), this year held in our nation’s capital of Washington, D.C.
As we peruse the preliminary program in planning our meeting coverage, I am always amazed at the breadth and depth of programming offered as part of a relatively brief, 4-day meeting — this is a testament to the hard work of the AGA Council and DDW organizing committees, who have the gargantuan task of ensuring an engaging, seamless meeting each year.
This year’s conference features over 400 original scientific sessions and 4,300 oral abstract and poster presentations, in addition to the always well-attended AGA Postgraduate Course. This year’s AGA Presidential Plenary, which will feature a series of thought-provoking panel discussions on the future of GI healthcare and innovations in how we treat, disseminate, and teach, also is not to be missed. Beyond DDW, I hope you will join me in taking advantage of some of D.C.’s amazing cultural offerings, including the Smithsonian museums, National Gallery, Kennedy Center for the Performing Arts, and many others.
In this month’s issue of GIHN, we highlight an important AGA expert consensus commentary published in Clinical Gastroenterology and Hepatology examining the role of blood-based tests (“liquid biopsy”) in colorectal cancer screening. This guidance, which recognizes the promise of such tests but also urges caution in their adoption, is particularly important considering recently published data from the ECLIPSE study (also covered in this issue) evaluating the performance of Guardant’s ctDNA liquid biopsy compared to a screening colonoscopy. Also relevant to CRC screening, we highlight data on the performance of the “next gen” Cologuard test compared with FIT, which was recently published in NEJM. In our May Member Spotlight, we feature gastroenterologist Adjoa Anyane-Yeboa, MD, MPH, who shares her passion for addressing barriers to CRC screening for Black patients. Finally, GIHN Associate Editor Dr. Avi Ketwaroo introduces our quarterly Perspectives column highlighting emerging applications of AI in GI endoscopy and hepatology. We hope you enjoy all the exciting content featured in this issue and look forward to seeing you in Washington, D.C. (or virtually) for DDW.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Do No Harm: What Smoldering Myeloma Teaches Us
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
My approach to treating SMM takes into account what its history can teach us about 1) how advancements in imaging and diagnostic reclassifications can revise the entire natural history of a disease, and 2) how evidence generated by even the best of studies may have an expiration date.
Much of what we know about SMM today dates to a pivotal study by Robert A. Kyle, MD, and colleagues, published in 2007. That inspirational team of investigators followed people diagnosed with SMM from 1970 to 1995 and established the first natural history of the condition. Their monumental effort and the data and conclusions it generated (eg,10% risk annually of SMM becoming MM for the first 5 years) are still cited today in references, papers, and slide sets.
Despite the seminal importance of this work, from today’s perspective the 2007 study might just as well have been describing a different disease. Back then people were diagnosed with SMM if their blood work detected a monoclonal protein and a follow-up bone marrow biopsy found at least 10% plasma cells (or a monoclonal protein exceeding 3g/dL). If there were no signs of end-organ damage (ie, no anemia or kidney problems) and an x-ray showed no fractures or lesions in the bones, the diagnosis was determined to be SMM.
What’s different in 2024? First and foremost: advanced, highly sensitive imaging techniques. MRIs can pick up small lytic lesions (and even the precursor to lytic lesions) that would not appear on an x-ray. In fact, relying solely on x-rays risks missing half of the lytic lesions.
Therefore, using the same criteria, many people who in the past were diagnosed with SMM would today be diagnosed with MM. Furthermore, in 2014 a diagnostic change reclassified people’s diagnosis from the highest risk category of SMM to the category of active MM.
Due to these scientific advances and classification changes, I believe that the natural history of SMM is unknown. Risk stratification models for SMM derived from data sets of people who had not undergone rigorous advanced imaging likely are skewed by data from people who had MM. In addition, current risk stratification models have very poor concordance with each other. I routinely see people whose 2-year risk according to different models varies by more than 30%-40%.
All this information tells us that SMM today is more indolent than the SMM of the past. Paradoxically, however, our therapies keep getting more and more aggressive, exposing this vulnerable group of people to intense treatment regimens that they may not require. Therapies tested on people diagnosed with SMM include an aggressive three-drug regimen, autologous stem cell transplant, and 2 years of additional therapy, as well as, more recently CAR T-cell therapy which so far has at least a 4%-5% treatment-related mortality risk in people with myeloma and a strong signal for secondary cancer risk. Other trials are testing bispecific therapies such as talquetamab, a drug which in my experience causes horrendous skin toxicity, profound weight loss, and one’s nails to fall off.
Doctors routinely keep showing slides from Kyle’s pivotal work to describe the natural history of SMM and to justify the need for treatment, and trials continue to use outdated progression prediction models. In my opinion, as people with MM keep living longer and treatments for MM keep getting better, the threshold for intervening with asymptomatic, healthy people with SMM should be getting higher, not lower.
I strongly believe that the current landscape of SMM treatment exemplifies good intentions leading to bad outcomes. A routine blood test in a completely healthy person that finds elevated total protein in the blood could culminate in well-intentioned but aggressive therapies that can lead to many serious side effects. (I repeat: Secondary cancers and deaths from infections have all occurred in SMM trials.)
With no control arm, we simply don’t know how well these people might have fared without any therapy. For all we know, treatment may have shortened their lives due to complications up to and including death — all because of a blood test often conducted for reasons that have no evidentiary basis.
For example, plasma cell diseases are not linked to low bone density or auto-immune diseases, yet these labs are sent routinely as part of a workup for those conditions, leading to increasing anxiety and costs.
So, what is my approach? When treating people with SMM, I hold nuanced discussions of this data to help prioritize and reach informed decisions. After our honest conversation about the limitations of SMM models, older data, and the limitations of prospective data studying pharmacological treatment, almost no one signs up for treatment.
I want these people to stay safe, and I’m proud to be a part of a trial (SPOTLIGHT, NCT06212323) that aims to show prospectively that these people can be watched off treatment with monitoring via advanced imaging modalities.
In conclusion: SMM teaches us how, even in the absence of pharmacological interventions, the natural history of a disease can change over time, simply via better imaging techniques and changes in diagnostic classifications. Unfortunately, SMM also illustrates how good intentions can lead to harm.
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
PCP Compensation, Part 1
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I recently read an op-ed piece in which the author wondered if any young people entering the practice of medicine felt that they were answering a “calling.” I suspect that there will continue to be, and will always be, idealists whose primary motivation for choosing medicine is that they will be healing the sick or at least providing comfort to the suffering. I occasionally hear that about a former patient who has been inspired by a personal or familial experience with a serious illness.
Unfortunately, I suspect those who feel called are the providers most likely to feel discouraged and frustrated by the current state of primary care. Luckily, I never felt a calling. For me, primary care pediatrics was a job. One that l felt obligated to perform to the best of my ability. Mine was not a calling but an inherited philosophy that work in itself was virtuous. A work ethic, if you will. Pediatrics offered the additional reward that, if well done, it might help some parents and their children feel a little better.
Fifty years ago I was not alone in treating medicine as a job. Most physicians were self-employed. Although there were exceptions like Albert Schweitzer, even those of us with a calling had to obey the basic rules of business as it applied to medicine. We were employer and employee and had to understand the critical factors of overhead, profit, and loss.
I have burdened you with this little history recitation not to suggest that things were better in the good old days, but to provide a stepping stone into the murky and uncomfortable topic of primary care physician (PCP) compensation. Because almost three quarters of you work for a hospital, health system, or corporate entity, I am going to illuminate our journey by leaning on the advice of an international company with 7000 employees and revenue of 2.5 billion dollars that considers itself a “global leader” in management consulting. Your employer is listening to some management consultant and it may help us to view your compensation from someone on their side of the table.
First, you should be aware that “most health systems lose money on their primary care operations — up to $200,000 or more per primary care physician.” This may help explain why despite being in short supply, you and most PCPs feel undervalued. However, if we are such losers, we must provide something(s) that the systems are seeking. It is likely that the system is looking to tout its ability to provide comprehensive care and demonstrate that it has a patient base broad enough to warrant attention and provide bargaining leverage on volume discounts.
The system also may want to minimize competition by absorbing the remaining PCPs in the community into their system. With you outside of the system, it had less control over your compensation than it does when you are under its umbrella.
Your employer may want to grow and feed its specialty care network, and it sees PCPs as having the fuel stored in their patient volume to do just that. In simplest and most cynical terms, the systems are willing to take a loss on us less profitable high-volume grunts in order to reap the profits of the lower-volume high-profitability specialties and subspecialties.
So that’s why you as a PCP have any value at all to a large healthcare system. But, it means that to maintain your value to the system you must continue to provide the volume it anticipates and needs. While the system may have been willing to accept some degrees of unprofitability when it hired you, there are limits. And, we shouldn’t be surprised if they continue to urge or demand that we narrow the gap between the revenue we generate and the costs that we incur, ie, our overhead.
In Part 2 of this series, I’m going to discuss the collateral damage that occurs when volume and overhead collide in an environment that claims to be committed to patient care.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
‘We Need to Rethink Our Options’: Lung Cancer Recurrence
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris reporting back after attending the New York Lung Cancer Foundation Summit here in New York. A large amount of discussion went on, but as usual, I was most interested in the perioperative space.
In previous videos, I’ve talked about this ongoing discussion of whether you should operate and give adjuvant therapy or give neoadjuvant therapy, and I’ve addressed that already. One thing I want to bring up – and as we move off of that argument, which frankly doesn’t have an answer today, with neoadjuvant therapy, having all the data to support it – is
I was taught early on by my surgical mentors that the issue here was systemic control. While they could do very successful surgery to get high levels of local control, they could not control systemic disease. Sadly, the tools we had early on with chemotherapy were just not good enough. Suddenly, we have better tools to control systemic spread. In the past, the vast majority of occurrences were systemic; they’re now local.
What I think we need to do as a group of practitioners trying to deal with the problems getting in the way of curing our patients is look at what the issue is now. Frankly, the big issue now, as systemic therapy has controlled metastatic disease, is recurrence in the chest.
We give adjuvant osimertinib. Please remember what the numbers are. In the osimertinib arm, of the 11 recurrences reported in the European Society for Medical Oncology presentation a few years back, nine of them were in the chest or mediastinal nodes. In the arm that got no osimertinib afterward, there were 46 recurrences, and 32 of those 46 recurrences were in the chest, either the lung or mediastinal nodes. Therefore, 74% of the recurrences are suddenly in the chest. What’s the issue here?
The issue is we need to find strategies to give better disease control in the chest, as we have made inroads in controlling systemic disease with the targeted therapies in the endothelial growth factor receptor space, and very likely the checkpoint inhibitors, too, as that data kind of filters out. We need to think about how better to get local control.
I think rather than continue to get into this argument of neoadjuvant vs adjuvant, we should move to what’s really hurting our patients. Again, the data I quoted you was from the ADAURA trial, which was adjuvant therapy, and I’m sure the neoadjuvant is going to show the same thing. It’s better systemic therapy but now, more trouble in the chest.
How are we going to deal with that? I’d like to throw out one strategy, and that is to rethink the role of radiation in these patients. Again, if the problem is local in the chest, lung, and lymph nodes, we have to think about local therapy. Yes, we’re not recommending it routinely for everybody, but now that we have better systemic control, we need to rethink our options. The obvious one to rethink is about giving radiotherapy.
We should also use what we learned in the earlier trials, which is that there is harm in giving excessive radiation to the heart. If you avoid the heart, you avoid the harm. We have better planning strategies for stereotactic body radiotherapy and more traditional radiation, and of course, we have proton therapy as well.
As we continue to struggle with the idea of that patient with stage II or III disease, whether to give adjuvant vs neoadjuvant therapy, please remember to consider their risk in 2024. Their risk for first recurrence is in the chest.
What are we going to do to better control disease in the chest? We have a challenge. I’m sure we can meet it if we put our heads together.
Dr. Kris is professor of medicine at Weill Cornell Medical College, and attending physician, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center, New York. He disclosed ties with AstraZeneca, Roche/Genentech, Ariad Pharmaceuticals, Pfizer, and PUMA.
A version of this article appeared on Medscape.com.
A Welcome Trade-off
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
At the end of March, in an anniversary no one but I noticed, I passed 4 years since I’d last rounded at the hospital.
It’s hard to comprehend that. I was at the hospital regularly for the first 22 years of my career, though admittedly it had dwindled from daily (1998-2011) to 1-2 weekends a month at the end.
Looking back, I still don’t miss it, and have no desire to go back. That’s not to say I don’t keep up on inpatient neurology, in case circumstances change, but at this point, honestly, I don’t want to. I’ve become accustomed to my non-hospital world, no late-night consults, no weekends spent rounding, no taking separate cars to restaurants or family events in case I get called in.
There are certainly things I miss about it. As odd as it may seem (and as much as I’d complain about it) I liked the wee hours of the really late night and early morning. It was quieter. Less chasing patients to tests or therapy. Pleasant idle chatter with staff and the few others docs around. Sitting at the computer and trying to think out a case on the fly. There was always junk food lying around.
But at this point in my life I’ll take the quiet of being home and my routine office hours. I know when my office day starts and ends. Aside from the occasional stop at Costco, I won’t be going anywhere else on my way home. I still get the occasional after-hours call, but none that require me to run to the ER.
On Fridays I’m glad the week is over, and don’t dread the 5:00 answering service switchover, or my call partner giving me the patient list.
There’s some revenue lost in the deal, but I’ll still take the trade-off.
It’s not like I ever had some grand plan to leave the hospital — I actually had thought I’d be there, at least occasionally, until retirement. But here I am.
Not to say there aren’t docs my age (and older) who still do it. Certainly our experience makes us good at it. But younger docs are closer to residency, which is primarily inpatient, so it’s an easier transition for many.
They probably have more energy, too.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
GLP-1 Receptor Agonists: Which Drug for Which Patient?
With all the excitement about GLP-1 agonists,
Of course, we want to make sure that we’re treating the right condition. If the patient has type 2 diabetes, we tend to give them medication that is indicated for type 2 diabetes. Many GLP-1 agonists are available in a diabetes version and a chronic weight management or obesity version. If a patient has diabetes and obesity, they can receive either one. If a patient has only diabetes but not obesity, they should be prescribed the diabetes version. For obesity without diabetes, we tend to stick with the drugs that are indicated for chronic weight management.
Let’s go through them.
Exenatide. In chronological order of approval, the first GLP-1 drug that was used for diabetes dates back to exenatide (Bydureon). Bydureon had a partner called Byetta (also exenatide), both of which are still on the market but infrequently used. Some patients reported that these medications were inconvenient because they required twice-daily injections and caused painful injection-site nodules.
Diabetes drugs in more common use include liraglutide (Victoza) for type 2 diabetes. It is a daily injection and has various doses. We always start low and increase with tolerance and desired effect for A1c.
Liraglutide. Victoza has an antiobesity counterpart called Saxenda. The Saxenda pen looks very similar to the Victoza pen. It is a daily GLP-1 agonist for chronic weight management. The SCALE trial demonstrated 8%-12% weight loss with Saxenda.
Those are the daily injections: Victoza for diabetes and Saxenda for weight loss.
Our patients are very excited about the advent of weekly injections for diabetes and weight management. Ozempic is very popular. It is a weekly GLP-1 agonist for type 2 diabetes. Many patients come in asking for Ozempic, and we must make sure that we’re moving them in the right direction depending on their condition.
Semaglutide. Ozempic has a few different doses. It is a weekly injection and has been found to be quite efficacious for treating diabetes. The drug’s weight loss counterpart is called Wegovy, which comes in a different pen. Both forms contain the compound semaglutide. While all of these GLP-1 agonists are indicated to treat type 2 diabetes or for weight management, Wegovy has a special indication that none of the others have. In March 2024, Wegovy acquired an indication to decrease cardiac risk in those with a BMI ≥ 27 and a previous cardiac history. This will really change the accessibility of this medication because patients with heart conditions who are on Medicare are expected to have access to Wegovy.
Tirzepatide. Another weekly injection for treatment of type 2 diabetes is called Mounjaro. Its counterpart for weight management is called Zepbound, which was found to have about 20.9% weight loss over 72 weeks. These medications have similar side effects in differing degrees, but the most-often reported are nausea, stool changes, abdominal pain, and reflux. There are some other potential side effects; I recommend that you read the individual prescribing information available for each drug to have more clarity about that.
It is important that we stay on label for using the GLP-1 receptor agonists, for many reasons. One, it increases our patients’ accessibility to the right medication for them, and we can also make sure that we’re treating the patient with the right drug according to the clinical trials. When the clinical trials are done, the study populations demonstrate safety and efficacy for that population. But if we’re prescribing a GLP-1 for a different population, it is considered off-label use.
Dr. Lofton, an obesity medicine specialist, is clinical associate professor of surgery and medicine at NYU Grossman School of Medicine, and director of the medical weight management program at NYU Langone Weight Management Center, New York. She disclosed ties to Novo Nordisk and Eli Lilly. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
With all the excitement about GLP-1 agonists,
Of course, we want to make sure that we’re treating the right condition. If the patient has type 2 diabetes, we tend to give them medication that is indicated for type 2 diabetes. Many GLP-1 agonists are available in a diabetes version and a chronic weight management or obesity version. If a patient has diabetes and obesity, they can receive either one. If a patient has only diabetes but not obesity, they should be prescribed the diabetes version. For obesity without diabetes, we tend to stick with the drugs that are indicated for chronic weight management.
Let’s go through them.
Exenatide. In chronological order of approval, the first GLP-1 drug that was used for diabetes dates back to exenatide (Bydureon). Bydureon had a partner called Byetta (also exenatide), both of which are still on the market but infrequently used. Some patients reported that these medications were inconvenient because they required twice-daily injections and caused painful injection-site nodules.
Diabetes drugs in more common use include liraglutide (Victoza) for type 2 diabetes. It is a daily injection and has various doses. We always start low and increase with tolerance and desired effect for A1c.
Liraglutide. Victoza has an antiobesity counterpart called Saxenda. The Saxenda pen looks very similar to the Victoza pen. It is a daily GLP-1 agonist for chronic weight management. The SCALE trial demonstrated 8%-12% weight loss with Saxenda.
Those are the daily injections: Victoza for diabetes and Saxenda for weight loss.
Our patients are very excited about the advent of weekly injections for diabetes and weight management. Ozempic is very popular. It is a weekly GLP-1 agonist for type 2 diabetes. Many patients come in asking for Ozempic, and we must make sure that we’re moving them in the right direction depending on their condition.
Semaglutide. Ozempic has a few different doses. It is a weekly injection and has been found to be quite efficacious for treating diabetes. The drug’s weight loss counterpart is called Wegovy, which comes in a different pen. Both forms contain the compound semaglutide. While all of these GLP-1 agonists are indicated to treat type 2 diabetes or for weight management, Wegovy has a special indication that none of the others have. In March 2024, Wegovy acquired an indication to decrease cardiac risk in those with a BMI ≥ 27 and a previous cardiac history. This will really change the accessibility of this medication because patients with heart conditions who are on Medicare are expected to have access to Wegovy.
Tirzepatide. Another weekly injection for treatment of type 2 diabetes is called Mounjaro. Its counterpart for weight management is called Zepbound, which was found to have about 20.9% weight loss over 72 weeks. These medications have similar side effects in differing degrees, but the most-often reported are nausea, stool changes, abdominal pain, and reflux. There are some other potential side effects; I recommend that you read the individual prescribing information available for each drug to have more clarity about that.
It is important that we stay on label for using the GLP-1 receptor agonists, for many reasons. One, it increases our patients’ accessibility to the right medication for them, and we can also make sure that we’re treating the patient with the right drug according to the clinical trials. When the clinical trials are done, the study populations demonstrate safety and efficacy for that population. But if we’re prescribing a GLP-1 for a different population, it is considered off-label use.
Dr. Lofton, an obesity medicine specialist, is clinical associate professor of surgery and medicine at NYU Grossman School of Medicine, and director of the medical weight management program at NYU Langone Weight Management Center, New York. She disclosed ties to Novo Nordisk and Eli Lilly. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
With all the excitement about GLP-1 agonists,
Of course, we want to make sure that we’re treating the right condition. If the patient has type 2 diabetes, we tend to give them medication that is indicated for type 2 diabetes. Many GLP-1 agonists are available in a diabetes version and a chronic weight management or obesity version. If a patient has diabetes and obesity, they can receive either one. If a patient has only diabetes but not obesity, they should be prescribed the diabetes version. For obesity without diabetes, we tend to stick with the drugs that are indicated for chronic weight management.
Let’s go through them.
Exenatide. In chronological order of approval, the first GLP-1 drug that was used for diabetes dates back to exenatide (Bydureon). Bydureon had a partner called Byetta (also exenatide), both of which are still on the market but infrequently used. Some patients reported that these medications were inconvenient because they required twice-daily injections and caused painful injection-site nodules.
Diabetes drugs in more common use include liraglutide (Victoza) for type 2 diabetes. It is a daily injection and has various doses. We always start low and increase with tolerance and desired effect for A1c.
Liraglutide. Victoza has an antiobesity counterpart called Saxenda. The Saxenda pen looks very similar to the Victoza pen. It is a daily GLP-1 agonist for chronic weight management. The SCALE trial demonstrated 8%-12% weight loss with Saxenda.
Those are the daily injections: Victoza for diabetes and Saxenda for weight loss.
Our patients are very excited about the advent of weekly injections for diabetes and weight management. Ozempic is very popular. It is a weekly GLP-1 agonist for type 2 diabetes. Many patients come in asking for Ozempic, and we must make sure that we’re moving them in the right direction depending on their condition.
Semaglutide. Ozempic has a few different doses. It is a weekly injection and has been found to be quite efficacious for treating diabetes. The drug’s weight loss counterpart is called Wegovy, which comes in a different pen. Both forms contain the compound semaglutide. While all of these GLP-1 agonists are indicated to treat type 2 diabetes or for weight management, Wegovy has a special indication that none of the others have. In March 2024, Wegovy acquired an indication to decrease cardiac risk in those with a BMI ≥ 27 and a previous cardiac history. This will really change the accessibility of this medication because patients with heart conditions who are on Medicare are expected to have access to Wegovy.
Tirzepatide. Another weekly injection for treatment of type 2 diabetes is called Mounjaro. Its counterpart for weight management is called Zepbound, which was found to have about 20.9% weight loss over 72 weeks. These medications have similar side effects in differing degrees, but the most-often reported are nausea, stool changes, abdominal pain, and reflux. There are some other potential side effects; I recommend that you read the individual prescribing information available for each drug to have more clarity about that.
It is important that we stay on label for using the GLP-1 receptor agonists, for many reasons. One, it increases our patients’ accessibility to the right medication for them, and we can also make sure that we’re treating the patient with the right drug according to the clinical trials. When the clinical trials are done, the study populations demonstrate safety and efficacy for that population. But if we’re prescribing a GLP-1 for a different population, it is considered off-label use.
Dr. Lofton, an obesity medicine specialist, is clinical associate professor of surgery and medicine at NYU Grossman School of Medicine, and director of the medical weight management program at NYU Langone Weight Management Center, New York. She disclosed ties to Novo Nordisk and Eli Lilly. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
The Obesogenic Environment of Preschool and Day Care
Thirty years ago I had an experience in the office that influenced my approach to obesity for the rest of my career. The patient was a 4-year-old whom I had been seeing since her birth. At her annual well-child visit her weight had jumped up significantly from the previous year’s visit. She appeared well, but the change in her growth trajectory prompted a bit more in-depth history taking.
It turned out that finances had forced the family to employ one of the child’s grandmothers as the day care provider. Unfortunately, this grandmother’s passion was cooking and she was particularly adept at baking. She had no other hobbies and a sore hip limited her mobility, so she seldom went outside. When I eventually met her she was a cheerful, overweight, and delightful woman.
Deconstructing this obesogenic environment without disrupting this otherwise healthy family was an exercise that required tact, patience, and creativity. Fortunately, the young girl’s mother had already harbored some concerns about her child’s weight and was more than willing to participate in this environmental re-engineering project. It’s a long story, but she and I achieved our goals and the child eventually coasted back toward her previous growth curve.
I have always suspected that this scenario is being replayed hundreds of thousands of time across this country. But, sadly most don’t share this one’s happy ending. Parents don’t alway perceive the seriousness of the problem. The economic hurdles are often too steep to overcome, even when the most creative minds are involved.
How prevalent are obesogenic day care environments? We certainly know childhood obesity is a problem and the statistics in the preschool age group are particularly concerning. More than 14 million children are in non-parental early care and education programs; these environments would seem to be a logical place to target our prevention strategies. Understandably, there seems to be a hesitancy to point fingers, but how many day care providers are similar to the well-intentioned grandmother in the scenario I described? We must at least suspect that the example set by the adults in the preschool and day care environment might be having some influence on the children under their care.
There has been some research that sheds some light on this question. A paper from the University of Oklahoma has looked at the predictors of overweight and obesity in early care and education (ECE) teachers in hopes of “finding modifiable opportunities to enhance the health of this critical workforce.” In their paper, the investigators refer to other research that has found the prevalence of overweight and obesity among ECE teachers is higher than our national average and their waist circumference is significantly greater than the standard recommendation for women.
A study from Norway has looked at the association between preschool staff’s activity level and that of the children under their care using accelerometers. This particular investigation couldn’t determine whether it was the staff’s activity level that influenced the children or vice versa because it wasn’t an observational study. Common sense would lead one to believe it was the staff’s relative inactivity that was being reflected in the children’s.
It is interesting that in this Norwegian study when the teachers were asked about their attitudes toward activity and their self-perception of their own activity, there was no relationship between the staff’s and the children’s level of activity. In other words, the educators and caregivers bought into the importance of activity but had difficulty translating this philosophy into own behavior.
So where does this leave us? It turns out my experience decades ago was not a one-off event, but instead represents the tip of very large iceberg. Should we immediately create a system of day care provider boot camps? Let’s remember that each educator and caregiver is one of us. They may be slight outliers but not a group of individuals deserving of forced marches and half-rations to get them in shape.
ECEs have listened to the same message we have all heard about diet and activity and their importance for a child’s health. It’s for their own health and that of their charges. This could be as simple as providing accelerometers or step-counting smartwatches. Or, by having physical educators perform on-site audits that could then be used to create site-specific plans for increasing both teacher and student activity.
Modifying the educators’ diet is a more complex procedure and can quickly become entangled in the socio-economic background of each individual teacher. A healthy diet is not always equally available to everyone. The solution may involve providing the teachers with food to be eaten at work and to be prepared at home. But, creative answers can be found if we look for them.
Before we get too far down the obesity-is-a-disease pathway, we must take a closer look at the role the early care and early school milieu are playing in the obesity problem. A little common sense behavior modification when children are in the controlled environment of school/day care may allow us to be less reliant on the those new wonder drugs in the long run.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Thirty years ago I had an experience in the office that influenced my approach to obesity for the rest of my career. The patient was a 4-year-old whom I had been seeing since her birth. At her annual well-child visit her weight had jumped up significantly from the previous year’s visit. She appeared well, but the change in her growth trajectory prompted a bit more in-depth history taking.
It turned out that finances had forced the family to employ one of the child’s grandmothers as the day care provider. Unfortunately, this grandmother’s passion was cooking and she was particularly adept at baking. She had no other hobbies and a sore hip limited her mobility, so she seldom went outside. When I eventually met her she was a cheerful, overweight, and delightful woman.
Deconstructing this obesogenic environment without disrupting this otherwise healthy family was an exercise that required tact, patience, and creativity. Fortunately, the young girl’s mother had already harbored some concerns about her child’s weight and was more than willing to participate in this environmental re-engineering project. It’s a long story, but she and I achieved our goals and the child eventually coasted back toward her previous growth curve.
I have always suspected that this scenario is being replayed hundreds of thousands of time across this country. But, sadly most don’t share this one’s happy ending. Parents don’t alway perceive the seriousness of the problem. The economic hurdles are often too steep to overcome, even when the most creative minds are involved.
How prevalent are obesogenic day care environments? We certainly know childhood obesity is a problem and the statistics in the preschool age group are particularly concerning. More than 14 million children are in non-parental early care and education programs; these environments would seem to be a logical place to target our prevention strategies. Understandably, there seems to be a hesitancy to point fingers, but how many day care providers are similar to the well-intentioned grandmother in the scenario I described? We must at least suspect that the example set by the adults in the preschool and day care environment might be having some influence on the children under their care.
There has been some research that sheds some light on this question. A paper from the University of Oklahoma has looked at the predictors of overweight and obesity in early care and education (ECE) teachers in hopes of “finding modifiable opportunities to enhance the health of this critical workforce.” In their paper, the investigators refer to other research that has found the prevalence of overweight and obesity among ECE teachers is higher than our national average and their waist circumference is significantly greater than the standard recommendation for women.
A study from Norway has looked at the association between preschool staff’s activity level and that of the children under their care using accelerometers. This particular investigation couldn’t determine whether it was the staff’s activity level that influenced the children or vice versa because it wasn’t an observational study. Common sense would lead one to believe it was the staff’s relative inactivity that was being reflected in the children’s.
It is interesting that in this Norwegian study when the teachers were asked about their attitudes toward activity and their self-perception of their own activity, there was no relationship between the staff’s and the children’s level of activity. In other words, the educators and caregivers bought into the importance of activity but had difficulty translating this philosophy into own behavior.
So where does this leave us? It turns out my experience decades ago was not a one-off event, but instead represents the tip of very large iceberg. Should we immediately create a system of day care provider boot camps? Let’s remember that each educator and caregiver is one of us. They may be slight outliers but not a group of individuals deserving of forced marches and half-rations to get them in shape.
ECEs have listened to the same message we have all heard about diet and activity and their importance for a child’s health. It’s for their own health and that of their charges. This could be as simple as providing accelerometers or step-counting smartwatches. Or, by having physical educators perform on-site audits that could then be used to create site-specific plans for increasing both teacher and student activity.
Modifying the educators’ diet is a more complex procedure and can quickly become entangled in the socio-economic background of each individual teacher. A healthy diet is not always equally available to everyone. The solution may involve providing the teachers with food to be eaten at work and to be prepared at home. But, creative answers can be found if we look for them.
Before we get too far down the obesity-is-a-disease pathway, we must take a closer look at the role the early care and early school milieu are playing in the obesity problem. A little common sense behavior modification when children are in the controlled environment of school/day care may allow us to be less reliant on the those new wonder drugs in the long run.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Thirty years ago I had an experience in the office that influenced my approach to obesity for the rest of my career. The patient was a 4-year-old whom I had been seeing since her birth. At her annual well-child visit her weight had jumped up significantly from the previous year’s visit. She appeared well, but the change in her growth trajectory prompted a bit more in-depth history taking.
It turned out that finances had forced the family to employ one of the child’s grandmothers as the day care provider. Unfortunately, this grandmother’s passion was cooking and she was particularly adept at baking. She had no other hobbies and a sore hip limited her mobility, so she seldom went outside. When I eventually met her she was a cheerful, overweight, and delightful woman.
Deconstructing this obesogenic environment without disrupting this otherwise healthy family was an exercise that required tact, patience, and creativity. Fortunately, the young girl’s mother had already harbored some concerns about her child’s weight and was more than willing to participate in this environmental re-engineering project. It’s a long story, but she and I achieved our goals and the child eventually coasted back toward her previous growth curve.
I have always suspected that this scenario is being replayed hundreds of thousands of time across this country. But, sadly most don’t share this one’s happy ending. Parents don’t alway perceive the seriousness of the problem. The economic hurdles are often too steep to overcome, even when the most creative minds are involved.
How prevalent are obesogenic day care environments? We certainly know childhood obesity is a problem and the statistics in the preschool age group are particularly concerning. More than 14 million children are in non-parental early care and education programs; these environments would seem to be a logical place to target our prevention strategies. Understandably, there seems to be a hesitancy to point fingers, but how many day care providers are similar to the well-intentioned grandmother in the scenario I described? We must at least suspect that the example set by the adults in the preschool and day care environment might be having some influence on the children under their care.
There has been some research that sheds some light on this question. A paper from the University of Oklahoma has looked at the predictors of overweight and obesity in early care and education (ECE) teachers in hopes of “finding modifiable opportunities to enhance the health of this critical workforce.” In their paper, the investigators refer to other research that has found the prevalence of overweight and obesity among ECE teachers is higher than our national average and their waist circumference is significantly greater than the standard recommendation for women.
A study from Norway has looked at the association between preschool staff’s activity level and that of the children under their care using accelerometers. This particular investigation couldn’t determine whether it was the staff’s activity level that influenced the children or vice versa because it wasn’t an observational study. Common sense would lead one to believe it was the staff’s relative inactivity that was being reflected in the children’s.
It is interesting that in this Norwegian study when the teachers were asked about their attitudes toward activity and their self-perception of their own activity, there was no relationship between the staff’s and the children’s level of activity. In other words, the educators and caregivers bought into the importance of activity but had difficulty translating this philosophy into own behavior.
So where does this leave us? It turns out my experience decades ago was not a one-off event, but instead represents the tip of very large iceberg. Should we immediately create a system of day care provider boot camps? Let’s remember that each educator and caregiver is one of us. They may be slight outliers but not a group of individuals deserving of forced marches and half-rations to get them in shape.
ECEs have listened to the same message we have all heard about diet and activity and their importance for a child’s health. It’s for their own health and that of their charges. This could be as simple as providing accelerometers or step-counting smartwatches. Or, by having physical educators perform on-site audits that could then be used to create site-specific plans for increasing both teacher and student activity.
Modifying the educators’ diet is a more complex procedure and can quickly become entangled in the socio-economic background of each individual teacher. A healthy diet is not always equally available to everyone. The solution may involve providing the teachers with food to be eaten at work and to be prepared at home. But, creative answers can be found if we look for them.
Before we get too far down the obesity-is-a-disease pathway, we must take a closer look at the role the early care and early school milieu are playing in the obesity problem. A little common sense behavior modification when children are in the controlled environment of school/day care may allow us to be less reliant on the those new wonder drugs in the long run.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].