User login
Commentary: Meningococcal vaccine shows moderate protective effect against gonorrhea
The data on cross-protection against gonorrhea by outer membrane vesicle (OMV)–based meningococcal B vaccine continue to look encouraging from a recent study in Clinical Infectious Diseases (2022; doi: 10.1093/cid/ciac436). The authors report matched-cohort study data involving over 33,000 teens/young adults followed at Kaiser Permanente Southern California during 2016-2020. Like the studies above, chlamydia-infected patients (n = 26,471) served as negative controls for the 6,641 gonorrhea patients. The researchers compared chances of getting gonorrhea vs. getting chlamydia in light of having previously gotten C4MenB vaccine (OMV-based) or MenACWY vaccine (not OMV-based). The authors reported gonorrhea incidence rates of 2.0/1,000 person-years (95% CI, 1.3–2.8) in 4CMenB vaccinees vs. 5.2 (4.6–5.8) for MenACWY recipients. An adjusted analysis revealed 46% lower gonorrhea rates in 4CMenB vs. MenACWY vaccinees. There was no difference in chlamydia rates.
We await prospective controlled data to validate these observational studies. However, it is intriguing that OMV-based meningococcal vaccine may be a two-fer vaccine with partial cross protection against gonorrhea because of outer membrane protein similarities between the two pathogens. These data seem worth sharing with families who are making decisions about whether to vaccinate their children against B strains of meningococcus whether or not the child has already had conjugate MenACWY.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The data on cross-protection against gonorrhea by outer membrane vesicle (OMV)–based meningococcal B vaccine continue to look encouraging from a recent study in Clinical Infectious Diseases (2022; doi: 10.1093/cid/ciac436). The authors report matched-cohort study data involving over 33,000 teens/young adults followed at Kaiser Permanente Southern California during 2016-2020. Like the studies above, chlamydia-infected patients (n = 26,471) served as negative controls for the 6,641 gonorrhea patients. The researchers compared chances of getting gonorrhea vs. getting chlamydia in light of having previously gotten C4MenB vaccine (OMV-based) or MenACWY vaccine (not OMV-based). The authors reported gonorrhea incidence rates of 2.0/1,000 person-years (95% CI, 1.3–2.8) in 4CMenB vaccinees vs. 5.2 (4.6–5.8) for MenACWY recipients. An adjusted analysis revealed 46% lower gonorrhea rates in 4CMenB vs. MenACWY vaccinees. There was no difference in chlamydia rates.
We await prospective controlled data to validate these observational studies. However, it is intriguing that OMV-based meningococcal vaccine may be a two-fer vaccine with partial cross protection against gonorrhea because of outer membrane protein similarities between the two pathogens. These data seem worth sharing with families who are making decisions about whether to vaccinate their children against B strains of meningococcus whether or not the child has already had conjugate MenACWY.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The data on cross-protection against gonorrhea by outer membrane vesicle (OMV)–based meningococcal B vaccine continue to look encouraging from a recent study in Clinical Infectious Diseases (2022; doi: 10.1093/cid/ciac436). The authors report matched-cohort study data involving over 33,000 teens/young adults followed at Kaiser Permanente Southern California during 2016-2020. Like the studies above, chlamydia-infected patients (n = 26,471) served as negative controls for the 6,641 gonorrhea patients. The researchers compared chances of getting gonorrhea vs. getting chlamydia in light of having previously gotten C4MenB vaccine (OMV-based) or MenACWY vaccine (not OMV-based). The authors reported gonorrhea incidence rates of 2.0/1,000 person-years (95% CI, 1.3–2.8) in 4CMenB vaccinees vs. 5.2 (4.6–5.8) for MenACWY recipients. An adjusted analysis revealed 46% lower gonorrhea rates in 4CMenB vs. MenACWY vaccinees. There was no difference in chlamydia rates.
We await prospective controlled data to validate these observational studies. However, it is intriguing that OMV-based meningococcal vaccine may be a two-fer vaccine with partial cross protection against gonorrhea because of outer membrane protein similarities between the two pathogens. These data seem worth sharing with families who are making decisions about whether to vaccinate their children against B strains of meningococcus whether or not the child has already had conjugate MenACWY.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Has the anti-benzodiazepine backlash gone too far?
When benzodiazepines were first introduced, they were greeted with enthusiasm. Librium came first, in 1960, followed by Valium in 1962, and they were seen as an improvement over barbiturates for the treatment of anxiety, insomnia, and seizures. From 1968 to 1982, Valium (diazepam) was the No. 1–selling U.S. pharmaceutical: 2.3 billion tablets of Valium were sold in 1978 alone. Valium was even the subject of a 1966 Rolling Stones hit, “Mother’s Little Helper.”
By the 1980s, it became apparent that there was a downside to these medications: patients became tolerant, dependent, and some became addicted to the medications. In older patients an association was noted with falls and cognitive impairment. And while safe in overdoses when they are the only agent, combined with alcohol or opioids, benzodiazepines can be lethal and have played a significant role in the current overdose crisis.
Because of the problems that are associated with their use, benzodiazepines and their relatives, the Z-drugs used for sleep, have become stigmatized, as have the patients who use them and perhaps even the doctors who prescribe them. Still, there are circumstances where patients find these medications to be helpful, where other medications don’t work, or don’t work quickly enough. They provide fast relief in conditions where there are not always good alternatives.
In the Facebook group, “Psychiatry for All Physicians,” it’s not uncommon for physicians to ask what to do with older patients who are transferred to them on therapeutic doses of benzodiazepines or zolpidem. These are outpatients coming for routine care, and they find the medications helpful and don’t want to discontinue them. They have tried other medications that were not helpful. I’ve been surprised at how often the respondents insist the patient should be told he must taper off the medication. “Just say no,” is often the advice, and perhaps it’s more about the doctor’s discomfort than it is about the individual patient. For sleep issues, cognitive-behavioral therapy is given as the gold-standard treatment, while in my practice I have found it difficult to motivate patients to engage in it, and of those who do, it is sometimes helpful, but not a panacea. Severe anxiety and sleepless nights, however, are not benign conditions.
This “just say no, hold the line” sentiment has me wondering if our pendulum has swung too far with respect to prescribing benzodiazepines. Is this just one more issue that has become strongly polarized? Certainly the literature would support that idea, with some physicians writing about how benzodiazepines are underused, and others urging avoidance.
I posted a poll on Twitter: Has the anti-benzo movement gone too far? In addition, I started a Twitter thread of my own thoughts about prescribing and deprescribing these medications and will give a synopsis of those ideas here.
Clearly, benzodiazepines are harmful to some patients, they have side effects, can be difficult to stop because of withdrawal symptoms, and they carry the risk of addiction. That’s not in question. Many medications, however, have the potential to do more harm than good, for example ibuprofen can cause bleeding or renal problems, and Fosamax, used to treat osteoporosis, can cause osteonecrosis of the jaw and femur, to name just two.
It would be so much easier if we could know in advance who benzodiazepines will harm, just as it would be good if we could know in advance who will get tardive dyskinesia or dyslipidemia from antipsychotic medications, or who will have life-threatening adverse reactions from cancer chemotherapy with no tumor response. There are risks to both starting and stopping sedatives, and if we insist a patient stop a medication because of potential risk, then we are cutting them off from being a partner in their own care. It also creates an adversarial relationship that can be draining for the doctor and upsetting for the patient.
By definition, if someone needs hospitalization for a psychiatric condition, their outpatient benzodiazepine is not keeping them stable and stopping it may be a good idea. If someone is seen in an ED for a fall, it’s common to blame the benzodiazepine, but older people who are not on these medications also fall and have memory problems. In his book, “Being Mortal: Illness, Medicine, and What Matters Most in the End” (New York: Picador, 2014), Atul Gawande, MD, makes the point that taking more than four prescriptions medications increases the risk for falls in the elderly. Still, no one is suggesting patients be taken off their antidepressants, antihypertensives, or blood thinners.
Finally, the question is not should we be giving benzodiazepines out without careful consideration – the answer is clearly no. Physicians don’t pass out benzodiazepines “like candy” for all the above reasons. They are initiated because the patient is suffering and sometimes desperate. Anxiety, panic, intractable insomnia, and severe agitation are all miserable, and alternative treatments may take weeks to work, or not work at all. Yet these subjective symptoms may be dismissed by physicians.
So what do I do in my own practice? I don’t encourage patients to take potentially addictive medications, but I do sometimes use them. I give ‘as needed’ benzodiazepines to people in distress who don’t have a history of misusing them. I never plan to start them as a permanent standing medication, though once in a while that ends up happening. As with other medications, it is best to use the minimally effective dose.
There is some controversy as to whether it is best to use anxiety medications on an “as-needed” basis or as a standing dosage. Psychiatrists who prescribe benzodiazepines more liberally often feel it’s better to give standing doses and prevent breakthrough anxiety. Patients may appear to be ‘medication seeking’ not because they are addicted, but because the doses used are too low to adequately treat their anxiety.
My hope is that there is less risk of tolerance, dependence, or addiction with less-frequent dosing, and I prescribe as-needed benzodiazepines for panic attacks, agitated major depression while we wait for the antidepressant to “kick in,” insomnia during manic episodes, and to people who get very anxious in specific situations such as flying or for medical procedures. I sometimes prescribe them for people with insomnia that does not respond to other treatments, or for disabling generalized anxiety.
For patients who have taken benzodiazepines for many years, I continue to discuss the risks, but often they are not looking to fix something that isn’t broken, or to live a risk-free life. A few of the patients who have come to me on low standing doses of sedatives are now in their 80’s, yet they remain active, live independently, drive, travel, and have busy social lives. One could argue either that the medications are working, or that the patient has become dependent on them and needs them to prevent withdrawal.
These medications present a quandary: by denying patients treatment with benzodiazepines, we are sparing some people addictions (this is good, we should be careful), but we are leaving some people to suffer. There is no perfect answer.
What I do know is that doctors should think carefully and consider the patient in front of them. “No Benzos Ever For Anyone” or “you must come off because there is risk and people will think I am a bad doctor for prescribing them to you” can be done by a robot.
So, yes, I think the pendulum has swung a bit too far; there is a place for these medications in acute treatment for those at low risk of addiction, and there are people who benefit from them over the long run. At times, they provide immense relief to someone who is really struggling.
So what was the result of my Twitter poll? Of the 219 voters, 34.2% voted: “No, the pendulum has not swung too far, and these medications are harmful”; 65.8% voted: “Yes, these medications are helpful.” There were many comments expressing a wide variety of sentiments. Of those who had taken prescription benzodiazepines, some felt they had been harmed and wished they had never been started on them, and others continue to find them helpful. Psychiatrists, it seems, see them from the vantage point of the populations they treat.
People who are uncomfortable search for answers, and those answers may come in the form of meditation or exercise, medicines, or illicit drugs. It’s interesting that these same patients can now easily obtain “medical” marijuana, and the Rolling Stones’ “Mother’s Little Helper” is often replaced by a gin and tonic.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
When benzodiazepines were first introduced, they were greeted with enthusiasm. Librium came first, in 1960, followed by Valium in 1962, and they were seen as an improvement over barbiturates for the treatment of anxiety, insomnia, and seizures. From 1968 to 1982, Valium (diazepam) was the No. 1–selling U.S. pharmaceutical: 2.3 billion tablets of Valium were sold in 1978 alone. Valium was even the subject of a 1966 Rolling Stones hit, “Mother’s Little Helper.”
By the 1980s, it became apparent that there was a downside to these medications: patients became tolerant, dependent, and some became addicted to the medications. In older patients an association was noted with falls and cognitive impairment. And while safe in overdoses when they are the only agent, combined with alcohol or opioids, benzodiazepines can be lethal and have played a significant role in the current overdose crisis.
Because of the problems that are associated with their use, benzodiazepines and their relatives, the Z-drugs used for sleep, have become stigmatized, as have the patients who use them and perhaps even the doctors who prescribe them. Still, there are circumstances where patients find these medications to be helpful, where other medications don’t work, or don’t work quickly enough. They provide fast relief in conditions where there are not always good alternatives.
In the Facebook group, “Psychiatry for All Physicians,” it’s not uncommon for physicians to ask what to do with older patients who are transferred to them on therapeutic doses of benzodiazepines or zolpidem. These are outpatients coming for routine care, and they find the medications helpful and don’t want to discontinue them. They have tried other medications that were not helpful. I’ve been surprised at how often the respondents insist the patient should be told he must taper off the medication. “Just say no,” is often the advice, and perhaps it’s more about the doctor’s discomfort than it is about the individual patient. For sleep issues, cognitive-behavioral therapy is given as the gold-standard treatment, while in my practice I have found it difficult to motivate patients to engage in it, and of those who do, it is sometimes helpful, but not a panacea. Severe anxiety and sleepless nights, however, are not benign conditions.
This “just say no, hold the line” sentiment has me wondering if our pendulum has swung too far with respect to prescribing benzodiazepines. Is this just one more issue that has become strongly polarized? Certainly the literature would support that idea, with some physicians writing about how benzodiazepines are underused, and others urging avoidance.
I posted a poll on Twitter: Has the anti-benzo movement gone too far? In addition, I started a Twitter thread of my own thoughts about prescribing and deprescribing these medications and will give a synopsis of those ideas here.
Clearly, benzodiazepines are harmful to some patients, they have side effects, can be difficult to stop because of withdrawal symptoms, and they carry the risk of addiction. That’s not in question. Many medications, however, have the potential to do more harm than good, for example ibuprofen can cause bleeding or renal problems, and Fosamax, used to treat osteoporosis, can cause osteonecrosis of the jaw and femur, to name just two.
It would be so much easier if we could know in advance who benzodiazepines will harm, just as it would be good if we could know in advance who will get tardive dyskinesia or dyslipidemia from antipsychotic medications, or who will have life-threatening adverse reactions from cancer chemotherapy with no tumor response. There are risks to both starting and stopping sedatives, and if we insist a patient stop a medication because of potential risk, then we are cutting them off from being a partner in their own care. It also creates an adversarial relationship that can be draining for the doctor and upsetting for the patient.
By definition, if someone needs hospitalization for a psychiatric condition, their outpatient benzodiazepine is not keeping them stable and stopping it may be a good idea. If someone is seen in an ED for a fall, it’s common to blame the benzodiazepine, but older people who are not on these medications also fall and have memory problems. In his book, “Being Mortal: Illness, Medicine, and What Matters Most in the End” (New York: Picador, 2014), Atul Gawande, MD, makes the point that taking more than four prescriptions medications increases the risk for falls in the elderly. Still, no one is suggesting patients be taken off their antidepressants, antihypertensives, or blood thinners.
Finally, the question is not should we be giving benzodiazepines out without careful consideration – the answer is clearly no. Physicians don’t pass out benzodiazepines “like candy” for all the above reasons. They are initiated because the patient is suffering and sometimes desperate. Anxiety, panic, intractable insomnia, and severe agitation are all miserable, and alternative treatments may take weeks to work, or not work at all. Yet these subjective symptoms may be dismissed by physicians.
So what do I do in my own practice? I don’t encourage patients to take potentially addictive medications, but I do sometimes use them. I give ‘as needed’ benzodiazepines to people in distress who don’t have a history of misusing them. I never plan to start them as a permanent standing medication, though once in a while that ends up happening. As with other medications, it is best to use the minimally effective dose.
There is some controversy as to whether it is best to use anxiety medications on an “as-needed” basis or as a standing dosage. Psychiatrists who prescribe benzodiazepines more liberally often feel it’s better to give standing doses and prevent breakthrough anxiety. Patients may appear to be ‘medication seeking’ not because they are addicted, but because the doses used are too low to adequately treat their anxiety.
My hope is that there is less risk of tolerance, dependence, or addiction with less-frequent dosing, and I prescribe as-needed benzodiazepines for panic attacks, agitated major depression while we wait for the antidepressant to “kick in,” insomnia during manic episodes, and to people who get very anxious in specific situations such as flying or for medical procedures. I sometimes prescribe them for people with insomnia that does not respond to other treatments, or for disabling generalized anxiety.
For patients who have taken benzodiazepines for many years, I continue to discuss the risks, but often they are not looking to fix something that isn’t broken, or to live a risk-free life. A few of the patients who have come to me on low standing doses of sedatives are now in their 80’s, yet they remain active, live independently, drive, travel, and have busy social lives. One could argue either that the medications are working, or that the patient has become dependent on them and needs them to prevent withdrawal.
These medications present a quandary: by denying patients treatment with benzodiazepines, we are sparing some people addictions (this is good, we should be careful), but we are leaving some people to suffer. There is no perfect answer.
What I do know is that doctors should think carefully and consider the patient in front of them. “No Benzos Ever For Anyone” or “you must come off because there is risk and people will think I am a bad doctor for prescribing them to you” can be done by a robot.
So, yes, I think the pendulum has swung a bit too far; there is a place for these medications in acute treatment for those at low risk of addiction, and there are people who benefit from them over the long run. At times, they provide immense relief to someone who is really struggling.
So what was the result of my Twitter poll? Of the 219 voters, 34.2% voted: “No, the pendulum has not swung too far, and these medications are harmful”; 65.8% voted: “Yes, these medications are helpful.” There were many comments expressing a wide variety of sentiments. Of those who had taken prescription benzodiazepines, some felt they had been harmed and wished they had never been started on them, and others continue to find them helpful. Psychiatrists, it seems, see them from the vantage point of the populations they treat.
People who are uncomfortable search for answers, and those answers may come in the form of meditation or exercise, medicines, or illicit drugs. It’s interesting that these same patients can now easily obtain “medical” marijuana, and the Rolling Stones’ “Mother’s Little Helper” is often replaced by a gin and tonic.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
When benzodiazepines were first introduced, they were greeted with enthusiasm. Librium came first, in 1960, followed by Valium in 1962, and they were seen as an improvement over barbiturates for the treatment of anxiety, insomnia, and seizures. From 1968 to 1982, Valium (diazepam) was the No. 1–selling U.S. pharmaceutical: 2.3 billion tablets of Valium were sold in 1978 alone. Valium was even the subject of a 1966 Rolling Stones hit, “Mother’s Little Helper.”
By the 1980s, it became apparent that there was a downside to these medications: patients became tolerant, dependent, and some became addicted to the medications. In older patients an association was noted with falls and cognitive impairment. And while safe in overdoses when they are the only agent, combined with alcohol or opioids, benzodiazepines can be lethal and have played a significant role in the current overdose crisis.
Because of the problems that are associated with their use, benzodiazepines and their relatives, the Z-drugs used for sleep, have become stigmatized, as have the patients who use them and perhaps even the doctors who prescribe them. Still, there are circumstances where patients find these medications to be helpful, where other medications don’t work, or don’t work quickly enough. They provide fast relief in conditions where there are not always good alternatives.
In the Facebook group, “Psychiatry for All Physicians,” it’s not uncommon for physicians to ask what to do with older patients who are transferred to them on therapeutic doses of benzodiazepines or zolpidem. These are outpatients coming for routine care, and they find the medications helpful and don’t want to discontinue them. They have tried other medications that were not helpful. I’ve been surprised at how often the respondents insist the patient should be told he must taper off the medication. “Just say no,” is often the advice, and perhaps it’s more about the doctor’s discomfort than it is about the individual patient. For sleep issues, cognitive-behavioral therapy is given as the gold-standard treatment, while in my practice I have found it difficult to motivate patients to engage in it, and of those who do, it is sometimes helpful, but not a panacea. Severe anxiety and sleepless nights, however, are not benign conditions.
This “just say no, hold the line” sentiment has me wondering if our pendulum has swung too far with respect to prescribing benzodiazepines. Is this just one more issue that has become strongly polarized? Certainly the literature would support that idea, with some physicians writing about how benzodiazepines are underused, and others urging avoidance.
I posted a poll on Twitter: Has the anti-benzo movement gone too far? In addition, I started a Twitter thread of my own thoughts about prescribing and deprescribing these medications and will give a synopsis of those ideas here.
Clearly, benzodiazepines are harmful to some patients, they have side effects, can be difficult to stop because of withdrawal symptoms, and they carry the risk of addiction. That’s not in question. Many medications, however, have the potential to do more harm than good, for example ibuprofen can cause bleeding or renal problems, and Fosamax, used to treat osteoporosis, can cause osteonecrosis of the jaw and femur, to name just two.
It would be so much easier if we could know in advance who benzodiazepines will harm, just as it would be good if we could know in advance who will get tardive dyskinesia or dyslipidemia from antipsychotic medications, or who will have life-threatening adverse reactions from cancer chemotherapy with no tumor response. There are risks to both starting and stopping sedatives, and if we insist a patient stop a medication because of potential risk, then we are cutting them off from being a partner in their own care. It also creates an adversarial relationship that can be draining for the doctor and upsetting for the patient.
By definition, if someone needs hospitalization for a psychiatric condition, their outpatient benzodiazepine is not keeping them stable and stopping it may be a good idea. If someone is seen in an ED for a fall, it’s common to blame the benzodiazepine, but older people who are not on these medications also fall and have memory problems. In his book, “Being Mortal: Illness, Medicine, and What Matters Most in the End” (New York: Picador, 2014), Atul Gawande, MD, makes the point that taking more than four prescriptions medications increases the risk for falls in the elderly. Still, no one is suggesting patients be taken off their antidepressants, antihypertensives, or blood thinners.
Finally, the question is not should we be giving benzodiazepines out without careful consideration – the answer is clearly no. Physicians don’t pass out benzodiazepines “like candy” for all the above reasons. They are initiated because the patient is suffering and sometimes desperate. Anxiety, panic, intractable insomnia, and severe agitation are all miserable, and alternative treatments may take weeks to work, or not work at all. Yet these subjective symptoms may be dismissed by physicians.
So what do I do in my own practice? I don’t encourage patients to take potentially addictive medications, but I do sometimes use them. I give ‘as needed’ benzodiazepines to people in distress who don’t have a history of misusing them. I never plan to start them as a permanent standing medication, though once in a while that ends up happening. As with other medications, it is best to use the minimally effective dose.
There is some controversy as to whether it is best to use anxiety medications on an “as-needed” basis or as a standing dosage. Psychiatrists who prescribe benzodiazepines more liberally often feel it’s better to give standing doses and prevent breakthrough anxiety. Patients may appear to be ‘medication seeking’ not because they are addicted, but because the doses used are too low to adequately treat their anxiety.
My hope is that there is less risk of tolerance, dependence, or addiction with less-frequent dosing, and I prescribe as-needed benzodiazepines for panic attacks, agitated major depression while we wait for the antidepressant to “kick in,” insomnia during manic episodes, and to people who get very anxious in specific situations such as flying or for medical procedures. I sometimes prescribe them for people with insomnia that does not respond to other treatments, or for disabling generalized anxiety.
For patients who have taken benzodiazepines for many years, I continue to discuss the risks, but often they are not looking to fix something that isn’t broken, or to live a risk-free life. A few of the patients who have come to me on low standing doses of sedatives are now in their 80’s, yet they remain active, live independently, drive, travel, and have busy social lives. One could argue either that the medications are working, or that the patient has become dependent on them and needs them to prevent withdrawal.
These medications present a quandary: by denying patients treatment with benzodiazepines, we are sparing some people addictions (this is good, we should be careful), but we are leaving some people to suffer. There is no perfect answer.
What I do know is that doctors should think carefully and consider the patient in front of them. “No Benzos Ever For Anyone” or “you must come off because there is risk and people will think I am a bad doctor for prescribing them to you” can be done by a robot.
So, yes, I think the pendulum has swung a bit too far; there is a place for these medications in acute treatment for those at low risk of addiction, and there are people who benefit from them over the long run. At times, they provide immense relief to someone who is really struggling.
So what was the result of my Twitter poll? Of the 219 voters, 34.2% voted: “No, the pendulum has not swung too far, and these medications are harmful”; 65.8% voted: “Yes, these medications are helpful.” There were many comments expressing a wide variety of sentiments. Of those who had taken prescription benzodiazepines, some felt they had been harmed and wished they had never been started on them, and others continue to find them helpful. Psychiatrists, it seems, see them from the vantage point of the populations they treat.
People who are uncomfortable search for answers, and those answers may come in the form of meditation or exercise, medicines, or illicit drugs. It’s interesting that these same patients can now easily obtain “medical” marijuana, and the Rolling Stones’ “Mother’s Little Helper” is often replaced by a gin and tonic.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. Dr. Miller has no conflicts of interest.
Contraception for women taking enzyme-inducing antiepileptics
Topiramate, introduced as an antiepileptic drug (AED), is currently most widely used for prevention of migraine headaches.
Because reproductive-aged women represent a population in which migraines are prevalent, clinicians need guidance to help women taking topiramate make sound contraceptive choices.
Several issues are relevant here. First, women who have migraines with aura should avoid estrogen-containing contraceptive pills, patches, and rings. Instead, progestin-only methods, including the contraceptive implant, may be recommended to patients with migraines.
Second, because topiramate, as with a number of other AEDs, is a teratogen, women using this medication need highly effective contraception. This consideration may also lead clinicians to recommend use of the implant in women with migraines.
Finally, topiramate, along with other AEDs (phenytoin, carbamazepine, barbiturates, primidone, and oxcarbazepine) induces hepatic enzymes, which results in reduced serum contraceptive steroid levels.
Because there is uncertainty regarding the degree to which the use of topiramate reduces serum levels of etonogestrel (the progestin released by the implant), investigators performed a prospective study to assess the pharmacokinetic impact of topiramate in women with the implant.
Ongoing users of contraceptive implants who agreed to use additional nonhormonal contraception were recruited to a 6-week study, during which they took topiramate and periodically had blood drawn.
Overall, use of topiramate was found to lower serum etonogestrel levels from baseline on a dose-related basis. At study completion, almost one-third of study participants were found to have serum progestin levels lower than the threshold associated with predictable ovulation suppression.
The results of this carefully conducted study support guidance from the Centers for Disease Control and Prevention that women seeking contraception and using topiramate or other enzyme-inducing AEDs should be encouraged to use intrauterine devices or injectable contraception. The contraceptive efficacy of these latter methods is not diminished by concomitant use of enzyme inducers.
I am Andrew Kaunitz. Please take care of yourself and each other.
Any views expressed above are the author’s own and do not necessarily reflect the views of WebMD or Medscape.
Andrew M. Kaunitz is a professor and Associate Chairman, department of obstetrics and gynecology, University of Florida, Jacksonville.
A version of this article first appeared on Medscape.com.
Topiramate, introduced as an antiepileptic drug (AED), is currently most widely used for prevention of migraine headaches.
Because reproductive-aged women represent a population in which migraines are prevalent, clinicians need guidance to help women taking topiramate make sound contraceptive choices.
Several issues are relevant here. First, women who have migraines with aura should avoid estrogen-containing contraceptive pills, patches, and rings. Instead, progestin-only methods, including the contraceptive implant, may be recommended to patients with migraines.
Second, because topiramate, as with a number of other AEDs, is a teratogen, women using this medication need highly effective contraception. This consideration may also lead clinicians to recommend use of the implant in women with migraines.
Finally, topiramate, along with other AEDs (phenytoin, carbamazepine, barbiturates, primidone, and oxcarbazepine) induces hepatic enzymes, which results in reduced serum contraceptive steroid levels.
Because there is uncertainty regarding the degree to which the use of topiramate reduces serum levels of etonogestrel (the progestin released by the implant), investigators performed a prospective study to assess the pharmacokinetic impact of topiramate in women with the implant.
Ongoing users of contraceptive implants who agreed to use additional nonhormonal contraception were recruited to a 6-week study, during which they took topiramate and periodically had blood drawn.
Overall, use of topiramate was found to lower serum etonogestrel levels from baseline on a dose-related basis. At study completion, almost one-third of study participants were found to have serum progestin levels lower than the threshold associated with predictable ovulation suppression.
The results of this carefully conducted study support guidance from the Centers for Disease Control and Prevention that women seeking contraception and using topiramate or other enzyme-inducing AEDs should be encouraged to use intrauterine devices or injectable contraception. The contraceptive efficacy of these latter methods is not diminished by concomitant use of enzyme inducers.
I am Andrew Kaunitz. Please take care of yourself and each other.
Any views expressed above are the author’s own and do not necessarily reflect the views of WebMD or Medscape.
Andrew M. Kaunitz is a professor and Associate Chairman, department of obstetrics and gynecology, University of Florida, Jacksonville.
A version of this article first appeared on Medscape.com.
Topiramate, introduced as an antiepileptic drug (AED), is currently most widely used for prevention of migraine headaches.
Because reproductive-aged women represent a population in which migraines are prevalent, clinicians need guidance to help women taking topiramate make sound contraceptive choices.
Several issues are relevant here. First, women who have migraines with aura should avoid estrogen-containing contraceptive pills, patches, and rings. Instead, progestin-only methods, including the contraceptive implant, may be recommended to patients with migraines.
Second, because topiramate, as with a number of other AEDs, is a teratogen, women using this medication need highly effective contraception. This consideration may also lead clinicians to recommend use of the implant in women with migraines.
Finally, topiramate, along with other AEDs (phenytoin, carbamazepine, barbiturates, primidone, and oxcarbazepine) induces hepatic enzymes, which results in reduced serum contraceptive steroid levels.
Because there is uncertainty regarding the degree to which the use of topiramate reduces serum levels of etonogestrel (the progestin released by the implant), investigators performed a prospective study to assess the pharmacokinetic impact of topiramate in women with the implant.
Ongoing users of contraceptive implants who agreed to use additional nonhormonal contraception were recruited to a 6-week study, during which they took topiramate and periodically had blood drawn.
Overall, use of topiramate was found to lower serum etonogestrel levels from baseline on a dose-related basis. At study completion, almost one-third of study participants were found to have serum progestin levels lower than the threshold associated with predictable ovulation suppression.
The results of this carefully conducted study support guidance from the Centers for Disease Control and Prevention that women seeking contraception and using topiramate or other enzyme-inducing AEDs should be encouraged to use intrauterine devices or injectable contraception. The contraceptive efficacy of these latter methods is not diminished by concomitant use of enzyme inducers.
I am Andrew Kaunitz. Please take care of yourself and each other.
Any views expressed above are the author’s own and do not necessarily reflect the views of WebMD or Medscape.
Andrew M. Kaunitz is a professor and Associate Chairman, department of obstetrics and gynecology, University of Florida, Jacksonville.
A version of this article first appeared on Medscape.com.
What COVID-19 taught us: The challenge of maintaining contingency level care to proactively forestall crisis care
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
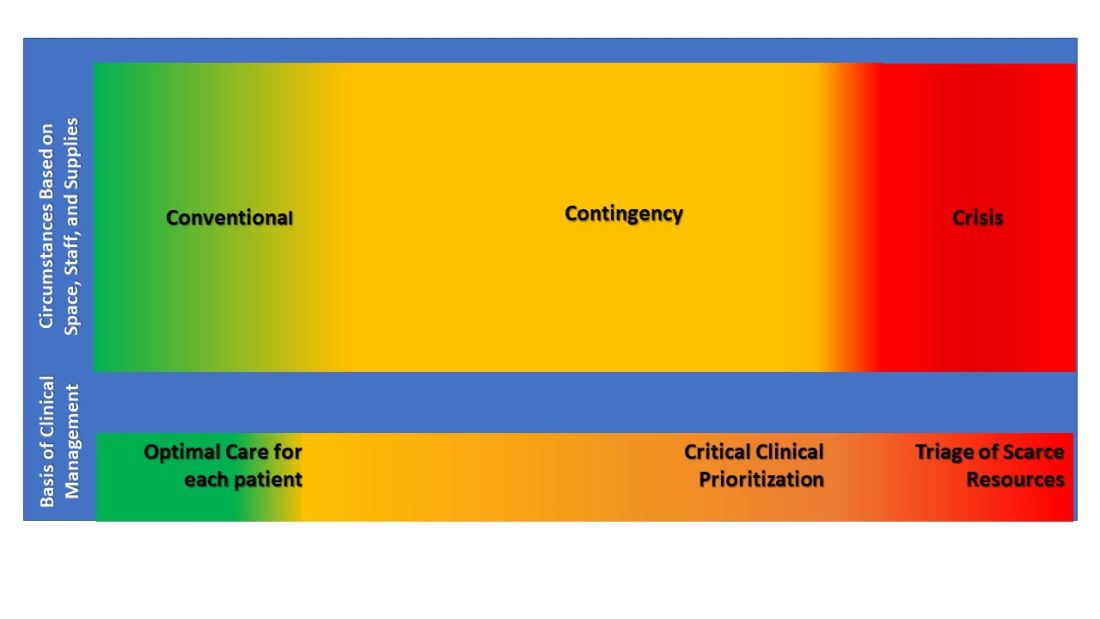
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure).
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
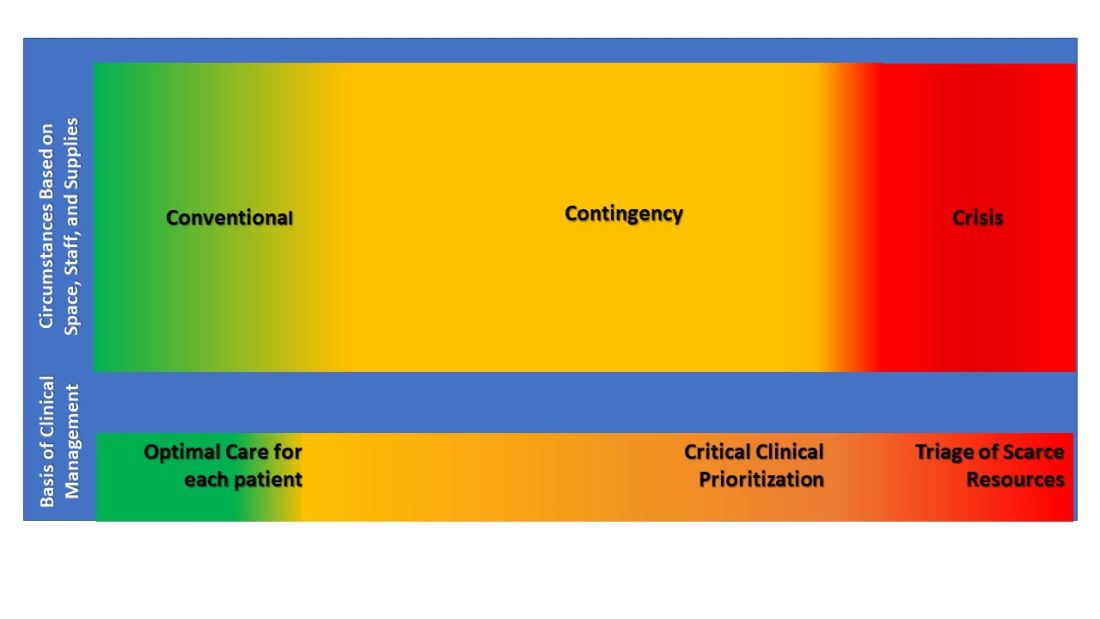
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure).
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
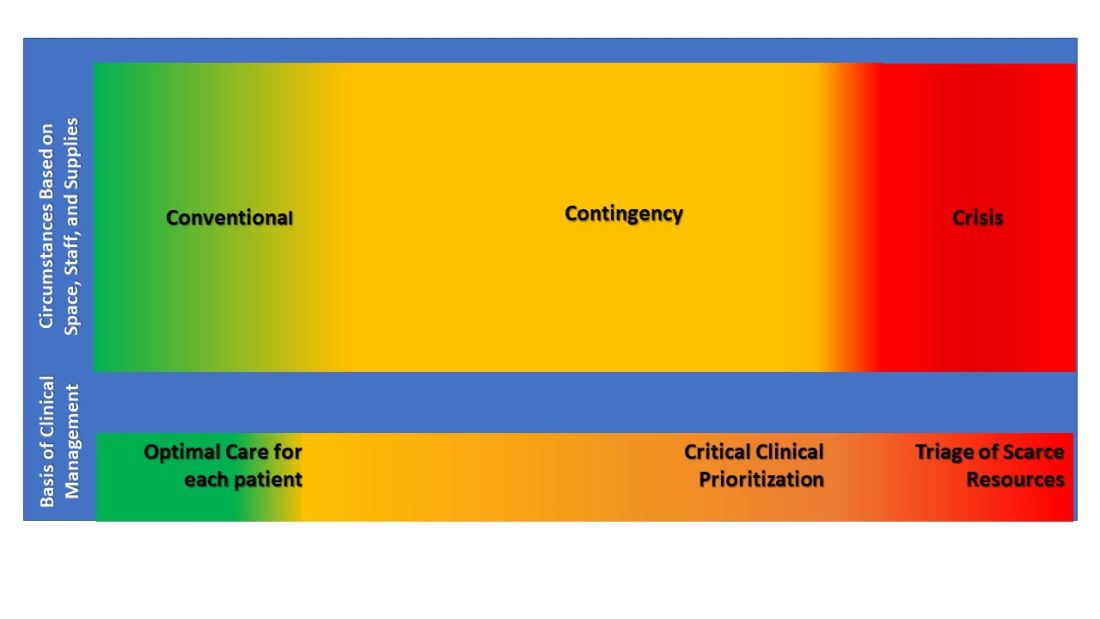
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure).
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
Patients need Sep-1: Why don’t some doctors like it?
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
Since its inception, the CMS Sep-1 Core Quality Measure has been unpopular in some circles. It is now under official attack by the American College of Emergency Physicians (ACEP) and the Infectious Diseases Society of America (IDSA), along with a handful of smaller professional societies. These societies appealed the National Quality Forum’s (NQF) 2021 recommendation that the measure be renewed. The NQF is the multidisciplinary and broadly representative group of evaluators who evaluate proposals for CMS-sponsored quality improvement on behalf of the American people and of the Centers for Medicare & Medicaid Services (CMS). Readers of CHEST Physician are likely familiar with core measures, in general, and with Sep-1, in particular. CMS requires hospitals to publicly report their compliance with several Core Quality Measures, and the failure to do so results in across the board reductions in Medicare payments. As of now, no penalties are levied for the degree of compliance but only for failure to report the degree of compliance.
The measure asks, in the main, for hospitals to perform what most physicians can agree should be standard care for patients with sepsis. Depending on whether shock is present, the measure requires:
1. Blood cultures before antibiotics
2. Antibiotics within 3 hours of recognition of sepsis
3. Serum lactate measurement in the first 3 hours and, if increased, a repeat measurement by 6 hours
4. If the patient is hypotensive, 30 mL/kg IV crystalloid within 3 hours, or documentation of why that is not appropriate for the patient
5. If hypotension persists, vasopressors within 6 hours
6. Repeat cardiovascular assessment within 6 hours for patients with shock
If I evaluate these criteria as a patient who has been hospitalized for a serious infection, which I am, they do not seem particularly stringent. In fact, as a patient, I would want my doctors and nurses to act substantially faster than this if I had sepsis or septic shock. If my doctor did not come back in less than 6 hours to check on my shock status, I would be disappointed, to say the least. Nevertheless, some physicians and professional societies see no reason why these should be standards and state that the data underlying them are of low quality. Meanwhile, according to CMS’ own careful evaluation, national compliance with the measures is less than 50%, while being compliant with the measures reduces absolute overall mortality by approximately 4%, from 26.3% to 22.2% (Townsend SR et al. Chest. 2022;161[2]:392-406). This would translate to between 14,000 and 15,000 fewer patients dying from sepsis per year, if all patients received bundled, measure-compliant care. These are patients I don’t care to ignore.
ACEP and IDSA point specifically to the new Surviving Sepsis Campaign Guidelines (SSC) recommendations as evidence that the antibiotic measure is based on low quality evidence (Evans L et al. Crit Care Med. 2021;49[11]:1974-82). In this regard, they are technically correct; the system of evidence review that the SSC panel uses, Grading of Assessment, Recommendations, and Evaluation (GRADE), considers that retrospective analyses, which nearly all of these studies are, can be graded no higher than low quality. Clearly, retrospective studies will never achieve the level of certainty that we achieve with randomized controlled trials, but the NQF, itself, typically views that when a number of well-performed retrospective studies point in the same direction, the level of evidence is at least moderate. After all, just as it would be inappropriate to randomize participants to decades of smoking vs nonsmoking in order prove that smoking causes lung cancer, it is not appropriate to randomize patients with sepsis to receive delayed antibiotics before we accept that such delays are harmful to them.
ACEP and IDSA also assert that the association of early antibiotics with survival is “stronger” for septic shock than for sepsis. In fact, the association is quite strong for both severities of illness. Until it progresses to septic shock, the expected mortality of sepsis is lower, and the percent reduction in mortality is less than for septic shock. However, the opportunity for lives preserved is quite large, because the number of patients with sepsis at presentation is approximately 10 times higher than the number with septic shock at presentation. Antibiotic delays are also associated with progression from infection or sepsis to septic shock (Whiles BB et al. Crit Care Med. 2017;45[4]:623-29; Bisarya R et al. Chest. 2022;161[1]:112-20). Importantly, SSC gave a strong recommendation for all patients with suspected sepsis to receive antibiotics within 3 hours of suspecting sepsis and within 1 hour of suspecting septic shock, a recommendation even stronger than that of Sep-1.
Critics opine that CMS should stop looking at the process measures and focus only on the outcomes of sepsis care. There is a certain attractiveness to this proposition. One could say that it does not matter so much how a hospital achieves lower mortality as long as they do achieve it. However, the question would then become – how low should the mortality rate be? I have a notion that whatever the number, the Sep-1 critics would find it unbearable.
There is a core principle embedded in the Sep-1 process measures, in SSC guidelines, and in the concept of early goal-directed therapy that preceded them: success is not dependent only on what we do but on when we do it. All of you have experienced this. Each of you has attended a professional school, whether medical, nursing, respiratory therapy, etc. None of you showed up unannounced on opening day of the semester and was admitted to that school. All of you garnered the grades, solicited the letters of recommendation, took the entrance exams, and submitted an application. Some of you went to an interview. All of these things were done in a timely fashion; professional schools do not accept incomplete applications or late applications. Doing the right things at the wrong time would have left us all pursuing different careers.
Very early in my career as an attending physician in the ICU, I found myself exasperated by the circumstances of many patients who we received in the ICU with sepsis. I would peruse their medical records and find that they had been septic, ie, had met criteria for severe sepsis, 1 to 2 days before their deterioration to septic shock, yet they had not been diagnosed with sepsis until shock developed. In the ICU, we began resuscitative fluids, ensured appropriate antibiotics, and started vasopressors, but it was often to no avail. The treatments we gave made no difference for many patients, because they were given too late. For me, this was career altering; much of my career since that time has focused on teaching medical personnel how to recognize sepsis, how to give timely and appropriate treatments, and how to keep the data to show when they have done that and when they have not.
Before Sep-1 many, if not most, of the hospitals in the United States had no particular strategy in place to recognize and treat patients with sepsis, even though it was and is the most common cause of death and the costliest condition in American hospitals. Now, most hospitals do have such strategies. Assertions by professional societies that it is difficult to collect the data for Sep-1 reporting are likely true. However, keeping patients safe and alive is a hospital’s primary reason for existing. As long as hospitals are tracking each antibiotic and every liter of fluid so that they can bill for them, my own ears are deaf to hearing that it is too difficult to make sure that we are doing our job. Modifying or eliminating Sep-1 for any reason except data that show we can clearly further improve the outcome for all patients with sepsis is the wrong move to make. So far, other professional societies want to remove elements of Sep-1 without evidence that it would improve our care for patients with sepsis or their outcomes. Thankfully, from the time we proposed the first criteria for diagnosing sepsis, CHEST has promoted what is best for patients, whether it is difficult or not.
Dr. Simpson is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement, including by serving as a senior adviser to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the U.S. Department of Health and Human Services and an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. Dr. Simpson is the senior medical adviser for Sepsis Alliance, a nationwide patient information and advocacy organization. He is the immediate past president of CHEST.
Commentary: Adolescents are undertested for STIs
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Despite current guidelines permitting opt-out STI screening and the ability in most states to treat adolescents 13 years old and older for STIs without parental notification, STI testing rates remain low. The articles about the 2019 survey raise several concerns.
Screening was more common with certain known risky behaviors, so risk-based screening seems prevalent. Of note, one recently reported factor increasing risky behaviors, but not noted above, is homelessness, suggesting it also be a trigger for STI screening (Child Youth Services Rev. 2022;139. doi: 10.1016/j.childyouth.2022.106538). But won’t risk-based screening inevitably lead to undertesting/treating? Are adolescents comfortable/willing to answer even the most carefully crafted, gentle, and simple questions about risky behaviors?
Because STIs are so frequent in adolescents (many asymptomatic), is risk-based screening/testing adequate for common STIs? Could urine-based screening for gonorrhea and chlamydia be useful in any adolescent who has been sexually active or uses the ED for routine care? Syphilis seems different. Screening requires a blood draw and is more difficult to implement, so risk-based testing seems okay. Also, the CDC recommends risk-based screening for syphilis.
Chief complaints at adolescent visits are usually not STI-related, unless symptomatic or visible, e.g., genital warts or herpes. So STI screening (even opt-out) will lengthen visits, perhaps a lot, over what was scheduled – even if only to explain negative results. Multiple visits with screening in the same morning could wreck patient flow. Maybe this doesn’t influence decisions to screen/test, but reexamining our approach can maximize appropriate STI screening/testing.
STIs run in packs, so if you detect one, expand testing to include the others.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
What can be new about developmental milestones?
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
The American Academy of Pediatrics, with funding from the Centers for Disease Control and Prevention, studied the CDC’s “Learn the Signs. Act Early” developmental surveillance milestones for children 0-5 years to update the milestones based on published studies. The goal was to improve this tool for developmental surveillance and use by the public. Developmental surveillance is not just observing a child at a check-up but rather “is a longitudinal process that involves eliciting concerns, taking a developmental history based on milestone attainment, observing milestones and other behaviors, examining the child, and applying clinical judgment during health supervision visits (HSVs).”1
While the milestones we were trained on were a good start and highlighted the developmental progression central to pediatrics, they were not based on norms or cut scores indicating significant developmental risk unless taught from a validated tool. The CDC was concerned that their public handouts and apps were based on median ages (middle number of the entire range) of attainment not the mode (most common) or even average ages. That means that about half of all typically developing children would “not have attained” that skill at the age noted, potentially evoking unnecessary concern for parents and a “wait-and-see” message from a knowledgeable provider who realized the statistical meaning and the broad range of normal. Another potential problem with using milestones set at the median age is that parents, especially those with several children or experienced friends, may see the provider as an alarmist when they have seen great variation in children who later were normal. This reaction can dampen provider willingness to discuss development or even to screen with validated tools. We have learned the hard way from COVID-19 that it is difficult to convey concepts of risk effectively both balancing fear and stimulating action.
The AAP experts reviewed the English literature for data-based milestones, finding 34 articles, 10 of which had an opinion for at least one milestone. If this sounds like a very small number, you are correct. You may not realize that almost all screening and diagnostic tools have been based on data collected by Gesell in 1928!2 While most of health care has changed since then, which milestones are measured in infants has not.
The biggest change from this review was deciding to use as milestones skills reported for 75% of children at each age of typical HSVs, adding ones for 15 and 30 months. The implication is that children not attaining these milestones are all at risk and deserving of more careful history, examination, and administration of a validated screening tool; not true when based on median data. Of the 94 existing CDC milestones retained after the review, one-third were moved to a different age with 21 of 31 assigned to an older age. Domains of functioning for the milestones were consolidated into social emotional, cognitive, language/communication, and motor, to help parents learn to distinguish these areas, and, although many milestones reflect several domains, each was included only once to reduce confusion.
Psychosocial assessment is recommended by the AAP and Bright Futures at every HSV but the fewest milestones with normative data were identified for this domain, often self-help rather than social engagement or emotion regulation skills. The cross-cultural study cited for many of the new milestones was reassuring overall in that the median ages for 67%-88% of milestones in most domains were equivalent across the four countries sampled, but only 22% of self-help skills were equivalent.3 This should remind us that parenting has more influence over psychosocial skills than other domains. Psychosocial and behavioral functioning, especially emotional regulation, also deserve “surveillance” as they have enormous impact on life outcomes but need to be measured and supported differently. Routine use of validated tools such as the Early Childhood Screening Assessment or the Ages & Stages Questionnaires: Social-Emotional for these domains are also needed.
Normal variations in temperament and patterns of attachment can affect many milestones including courage for walking, exploration, social engagement, and prosocial behaviors or self-control for social situations, attention, range of affect, and cooperation. All of these skills are among the 42 total (14 new) social-emotional milestones for 0- to 5-year-olds. Variations in these functions are at the root of the most common “challenging behaviors” in our studies in primary care. They are also the most vulnerable to suboptimal parent-child relationships, adverse childhood experiences, and social determinants of health.
As primary care providers, we not only need to detect children at risk for developmental problems but also promote and celebrate developmental progress. I hope that changing the threshold for concern to 75% will allow for a more positive review with the family (as fewer will be flagged as at risk) and chance to congratulate parents on all that is going well. But I also hope the change will not make us overlook parenting challenges, often from the psychosocial milestones most amenable to our guidance and support.
Early identification is mainly important to obtain the early intervention shown to improve outcomes. However, less than 25% of children with delays or disabilities receive early intervention before age 3 and most with emotional, behavioral, and developmental conditions, other than autism spectrum disorder, not before age 5. Since early intervention services are freely available in all states, we also need to do better at getting children to this care.
Let’s reconsider the process of developmental surveillance in this light of delayed referral: “Eliciting concerns” is key as parents have been shown to be usually correct in their worries. Listening to how they express the concerns can help you connect their specific issues when discussing reasons for referral. While most parent “recall of past milestones” is not accurate, current milestones reported are; thus, the need to have the new more accurate norms for all ages for comparison. When we make observations of a child’s abilities and behaviors ourselves we may not only pick up on issues missed by the parent, but will be more convincing in conveying the need for referral when indicated. When we “examine” the child we can use our professional skills to determine the very important risk factor of the quality of how a skill is performed, not just that it is. The recommended “use of validated screening tools” when the new milestones are not met give us an objective tool to share with parents, more confidence in when referral is warranted, which we will convey to parents (and perhaps skeptical relatives), and baseline documentation from which we can “track” referrals, progress, and, hopefully, better outcomes.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
References
1. Zubler JM et al. Pediatrics. 2022;149(3):e2021052138.
2. Gessell A et al. Macmillan: New York, 1928.
3. Ertem IO et al. Lancet Glob Health. 2018 Mar;6(3):e279-91.
The EMR gets it wrong: SNAFU
The medical news is full of articles about the coming epidemic of dementia. How many people will have it in 10 years, 20 years, etc. It’s a very legitimate concern, and I am not going to make light of it, or disagree with the predictions.
In my everyday practice, though, I find there’s an epidemic of overdiagnosed dementia, in those who aren’t even close.
This occurs in a few ways:
Aricept is pretty inexpensive these days. Long off patent, insurance companies don’t bother to question its use anymore. So anyone older than 60 who complains of losing their car keys gets put on it. Why? Because patients want their doctors to DO SOMETHING. Even if the doctor knows that there’s really nothing of alarm going on, sometimes it’s easier to go with the placebo effect than argue. I think we’ve all done that before.
There are also a lot of nonneurologists in practice who still, after almost 30 years on the market, think Aricept improves memory, when in fact that’s far from the truth. The best it can claim to do is slow down the rate at which patients get worse, but nobody wants to hear that.
I’ve also seen Aricept used for pseudodementia due to depression. Actually, I’ve seen it used for depression, too. Sometimes it’s used to counteract the side effects dof drugs that can impair cognition, such as Topamax, even in patients who aren’t even remotely demented.
None of the above are a major issue on their own. Where the trouble really happens, as with so many other things, is when they collide with an EMR, or someone too rushed to take a history, or both.
Let’s say Mrs. Jones is on Aricept because she went into a room, then forgot why she did.
Then she gets admitted to the hospital for pneumonia. Or she changes doctors and, like many practices these days, her medications are put in the computer by an MA or secretary.
A lot of times , so that gets punched in as a diagnosis and the patient is now believed to be unable to provide a reliable history. Or the person entering the info looks up its indication and enters “Alzheimer’s disease.”
Even worse is that I’ve seen EMRs where, in an effort to save time, the computer automatically enters diagnoses as you type medications in, and it’s up to the doctor to review them for accuracy. How that saves time I have no idea. But, as above, in these cases it’s going to lead to an entry of dementia where there isn’t any.
That, in particular, is pretty scary. As I wrote here in January of this year, what happens in the EMR stays in the EMR (kind of like Las Vegas).
I’m not knocking off-label use of medications. I don’t know a doctor who doesn’t use some that way, including myself.
But when doing so leads to the wrong assumptions and diagnoses it creates a lot of problems.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The medical news is full of articles about the coming epidemic of dementia. How many people will have it in 10 years, 20 years, etc. It’s a very legitimate concern, and I am not going to make light of it, or disagree with the predictions.
In my everyday practice, though, I find there’s an epidemic of overdiagnosed dementia, in those who aren’t even close.
This occurs in a few ways:
Aricept is pretty inexpensive these days. Long off patent, insurance companies don’t bother to question its use anymore. So anyone older than 60 who complains of losing their car keys gets put on it. Why? Because patients want their doctors to DO SOMETHING. Even if the doctor knows that there’s really nothing of alarm going on, sometimes it’s easier to go with the placebo effect than argue. I think we’ve all done that before.
There are also a lot of nonneurologists in practice who still, after almost 30 years on the market, think Aricept improves memory, when in fact that’s far from the truth. The best it can claim to do is slow down the rate at which patients get worse, but nobody wants to hear that.
I’ve also seen Aricept used for pseudodementia due to depression. Actually, I’ve seen it used for depression, too. Sometimes it’s used to counteract the side effects dof drugs that can impair cognition, such as Topamax, even in patients who aren’t even remotely demented.
None of the above are a major issue on their own. Where the trouble really happens, as with so many other things, is when they collide with an EMR, or someone too rushed to take a history, or both.
Let’s say Mrs. Jones is on Aricept because she went into a room, then forgot why she did.
Then she gets admitted to the hospital for pneumonia. Or she changes doctors and, like many practices these days, her medications are put in the computer by an MA or secretary.
A lot of times , so that gets punched in as a diagnosis and the patient is now believed to be unable to provide a reliable history. Or the person entering the info looks up its indication and enters “Alzheimer’s disease.”
Even worse is that I’ve seen EMRs where, in an effort to save time, the computer automatically enters diagnoses as you type medications in, and it’s up to the doctor to review them for accuracy. How that saves time I have no idea. But, as above, in these cases it’s going to lead to an entry of dementia where there isn’t any.
That, in particular, is pretty scary. As I wrote here in January of this year, what happens in the EMR stays in the EMR (kind of like Las Vegas).
I’m not knocking off-label use of medications. I don’t know a doctor who doesn’t use some that way, including myself.
But when doing so leads to the wrong assumptions and diagnoses it creates a lot of problems.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The medical news is full of articles about the coming epidemic of dementia. How many people will have it in 10 years, 20 years, etc. It’s a very legitimate concern, and I am not going to make light of it, or disagree with the predictions.
In my everyday practice, though, I find there’s an epidemic of overdiagnosed dementia, in those who aren’t even close.
This occurs in a few ways:
Aricept is pretty inexpensive these days. Long off patent, insurance companies don’t bother to question its use anymore. So anyone older than 60 who complains of losing their car keys gets put on it. Why? Because patients want their doctors to DO SOMETHING. Even if the doctor knows that there’s really nothing of alarm going on, sometimes it’s easier to go with the placebo effect than argue. I think we’ve all done that before.
There are also a lot of nonneurologists in practice who still, after almost 30 years on the market, think Aricept improves memory, when in fact that’s far from the truth. The best it can claim to do is slow down the rate at which patients get worse, but nobody wants to hear that.
I’ve also seen Aricept used for pseudodementia due to depression. Actually, I’ve seen it used for depression, too. Sometimes it’s used to counteract the side effects dof drugs that can impair cognition, such as Topamax, even in patients who aren’t even remotely demented.
None of the above are a major issue on their own. Where the trouble really happens, as with so many other things, is when they collide with an EMR, or someone too rushed to take a history, or both.
Let’s say Mrs. Jones is on Aricept because she went into a room, then forgot why she did.
Then she gets admitted to the hospital for pneumonia. Or she changes doctors and, like many practices these days, her medications are put in the computer by an MA or secretary.
A lot of times , so that gets punched in as a diagnosis and the patient is now believed to be unable to provide a reliable history. Or the person entering the info looks up its indication and enters “Alzheimer’s disease.”
Even worse is that I’ve seen EMRs where, in an effort to save time, the computer automatically enters diagnoses as you type medications in, and it’s up to the doctor to review them for accuracy. How that saves time I have no idea. But, as above, in these cases it’s going to lead to an entry of dementia where there isn’t any.
That, in particular, is pretty scary. As I wrote here in January of this year, what happens in the EMR stays in the EMR (kind of like Las Vegas).
I’m not knocking off-label use of medications. I don’t know a doctor who doesn’t use some that way, including myself.
But when doing so leads to the wrong assumptions and diagnoses it creates a lot of problems.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Transgender youth: Bringing evidence to the political debates
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
On the receiving end of care
It’s tough being on the receiving end of care. I’ve tried to avoid it as much as possible, being ever mindful of the law from Samuel Shem’s The House of God: “They can always hurt you more.”
Fortunately, each procedure went more smoothly than the prior one.
The first was not so elective. I had some uncomfortable symptoms while exercising and, not wanting to totally be in denial, contacted my doctor to ensure that it was not cardiac in origin since symptoms are often atypical in women.
My physician promptly saw me, then scheduled a nuclear stress test. There was a series of needless glitches. Registration at the diagnostic center had me on their schedule but did not have an order. They would have canceled the procedure had I not been able to get hold of the doctor’s office. Why isn’t an order automatically entered when the physician schedules the test?
While I was given the euphemistic “Patient Rights” brochure, asking to have reports sent to a physician outside of the University of Pittsburgh Medical Center empire is apparently not included.
The staff canceled the stress test because I was not fasting. I had received no instructions from diagnostic cardiology. They suggested it was my internist’s responsibility.
I deliberately ate (2 hours earlier) because my trainer always wants me to eat a light meal so I don’t get hypoglycemic during our workouts, and an exercise stress test, is, of course, a workout. The nurse practitioner said that they were concerned I would vomit. I offered to sign a waiver. She parried, saying they would not be able to get adequate images, so I was out of luck.
When I expressed concern about getting hypoglycemic and having difficulty with the test if fasting, the tech said I should bring a soda and snack. Who tells a “borderline” diabetic to bring a soda?
The tech also said she had called our home to give instructions but encountered a busy signal and had not had time to call back. I had not left the house during the prior week (or most of the past 2 years), so this was a pretty lame excuse.
I suggested to the administration that the hospital offer to email the patient instructions well ahead of time (and perhaps ask for confirmation of receipt). If calling, they should try more than once. They should also have patient instruction sheets at the physician’s office and perhaps have them on their website.
It turns out that the hospital mailed me instructions, not on the date it was ordered, but with the postmark being the day of the procedure itself. With Trump donor Louis DeJoy in charge of the U.S. Postal Service, mail across town now has to travel to Baltimore, 3 hours away, be sorted, and returned.
I did finally have the stress test, which was reassuringly normal. I was not surprised, given that the fury I felt on the first attempt had not precipitated symptoms. The hospital sent a patient ombudsman to meet me there to discuss my previous complaints. I have no idea if they implemented any of the changes I had suggested. In 2021, when I urgently had to take my husband to the ED, I couldn’t see the sign pointing toward the ED and had to ask for directions at the main entrance. They said they would fix that promptly but still have not improved the signage. How I miss the friendly community hospital we had before!
Next was trigger-finger surgery. I had developed that in 1978 from using crutches after a fall. I figured that the relative lull in COVID and my activities made it as good a time as any to finally have it fixed. The surgicenter was great; the surgeon was someone I had worked with and respected for decades. The only glitch was not really knowing how long I was going to be out of commission.
The third encounter (at yet another institution) went really well, despite some early administrative glitches. My major complaint was with the lack of communication between preoperative anesthesia and the operating room and the lack of personalization of preoperative instructions. Despite EPIC, medicines were not correctly reconciled between the different encounters, even on the same day!
After about 15 years of diplopia, which has been gradually worsening, my eye doc had suggested that I consider strabismus surgery as a sort of last-ditch effort to improve my quality of life.
Anesthesiology has stock instructions, which they made no effort to individualize. For example, there is no reason to stop NSAIDs a week before such minor surgery. That’s a problem if you depend on NSAIDs for pain control. Similarly, nothing by mouth after midnight is passé and could be tailored for the patient. I felt particularly inconvenienced that I had to go out of town for the preoperative visit and then have a redundant preoperative clearance by my physician.
The nurses in the preoperative area made me feel quite comfortable and as relaxed as I could be under the circumstances. They had a good sense of humor, which helped too. And from the time I met him a few weeks earlier, I instantly liked my surgeon and felt very comfortable with him and had complete trust.
I was pleased that the chief anesthesiologist responded promptly and undefensively to my letter expressing concerns. I do believe that he will try to improve the systemic problems.
The best part: The surgery appears to have been successful and I should have a significantly improved quality of life.
Hospitals could do so much better by improving communications with patients and by viewing them as customers whose loyalty they must earn and will value. With monopolies growing, memories of such care are quickly fading, soon to be as extinct as the family doc who made house calls.
Dr. Stone is an infectious disease specialist and author of Resilience: One Family’s Story of Hope and Triumph over Evil and Conducting Clinical Research: A Practical Guide. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
It’s tough being on the receiving end of care. I’ve tried to avoid it as much as possible, being ever mindful of the law from Samuel Shem’s The House of God: “They can always hurt you more.”
Fortunately, each procedure went more smoothly than the prior one.
The first was not so elective. I had some uncomfortable symptoms while exercising and, not wanting to totally be in denial, contacted my doctor to ensure that it was not cardiac in origin since symptoms are often atypical in women.
My physician promptly saw me, then scheduled a nuclear stress test. There was a series of needless glitches. Registration at the diagnostic center had me on their schedule but did not have an order. They would have canceled the procedure had I not been able to get hold of the doctor’s office. Why isn’t an order automatically entered when the physician schedules the test?
While I was given the euphemistic “Patient Rights” brochure, asking to have reports sent to a physician outside of the University of Pittsburgh Medical Center empire is apparently not included.
The staff canceled the stress test because I was not fasting. I had received no instructions from diagnostic cardiology. They suggested it was my internist’s responsibility.
I deliberately ate (2 hours earlier) because my trainer always wants me to eat a light meal so I don’t get hypoglycemic during our workouts, and an exercise stress test, is, of course, a workout. The nurse practitioner said that they were concerned I would vomit. I offered to sign a waiver. She parried, saying they would not be able to get adequate images, so I was out of luck.
When I expressed concern about getting hypoglycemic and having difficulty with the test if fasting, the tech said I should bring a soda and snack. Who tells a “borderline” diabetic to bring a soda?
The tech also said she had called our home to give instructions but encountered a busy signal and had not had time to call back. I had not left the house during the prior week (or most of the past 2 years), so this was a pretty lame excuse.
I suggested to the administration that the hospital offer to email the patient instructions well ahead of time (and perhaps ask for confirmation of receipt). If calling, they should try more than once. They should also have patient instruction sheets at the physician’s office and perhaps have them on their website.
It turns out that the hospital mailed me instructions, not on the date it was ordered, but with the postmark being the day of the procedure itself. With Trump donor Louis DeJoy in charge of the U.S. Postal Service, mail across town now has to travel to Baltimore, 3 hours away, be sorted, and returned.
I did finally have the stress test, which was reassuringly normal. I was not surprised, given that the fury I felt on the first attempt had not precipitated symptoms. The hospital sent a patient ombudsman to meet me there to discuss my previous complaints. I have no idea if they implemented any of the changes I had suggested. In 2021, when I urgently had to take my husband to the ED, I couldn’t see the sign pointing toward the ED and had to ask for directions at the main entrance. They said they would fix that promptly but still have not improved the signage. How I miss the friendly community hospital we had before!
Next was trigger-finger surgery. I had developed that in 1978 from using crutches after a fall. I figured that the relative lull in COVID and my activities made it as good a time as any to finally have it fixed. The surgicenter was great; the surgeon was someone I had worked with and respected for decades. The only glitch was not really knowing how long I was going to be out of commission.
The third encounter (at yet another institution) went really well, despite some early administrative glitches. My major complaint was with the lack of communication between preoperative anesthesia and the operating room and the lack of personalization of preoperative instructions. Despite EPIC, medicines were not correctly reconciled between the different encounters, even on the same day!
After about 15 years of diplopia, which has been gradually worsening, my eye doc had suggested that I consider strabismus surgery as a sort of last-ditch effort to improve my quality of life.
Anesthesiology has stock instructions, which they made no effort to individualize. For example, there is no reason to stop NSAIDs a week before such minor surgery. That’s a problem if you depend on NSAIDs for pain control. Similarly, nothing by mouth after midnight is passé and could be tailored for the patient. I felt particularly inconvenienced that I had to go out of town for the preoperative visit and then have a redundant preoperative clearance by my physician.
The nurses in the preoperative area made me feel quite comfortable and as relaxed as I could be under the circumstances. They had a good sense of humor, which helped too. And from the time I met him a few weeks earlier, I instantly liked my surgeon and felt very comfortable with him and had complete trust.
I was pleased that the chief anesthesiologist responded promptly and undefensively to my letter expressing concerns. I do believe that he will try to improve the systemic problems.
The best part: The surgery appears to have been successful and I should have a significantly improved quality of life.
Hospitals could do so much better by improving communications with patients and by viewing them as customers whose loyalty they must earn and will value. With monopolies growing, memories of such care are quickly fading, soon to be as extinct as the family doc who made house calls.
Dr. Stone is an infectious disease specialist and author of Resilience: One Family’s Story of Hope and Triumph over Evil and Conducting Clinical Research: A Practical Guide. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
It’s tough being on the receiving end of care. I’ve tried to avoid it as much as possible, being ever mindful of the law from Samuel Shem’s The House of God: “They can always hurt you more.”
Fortunately, each procedure went more smoothly than the prior one.
The first was not so elective. I had some uncomfortable symptoms while exercising and, not wanting to totally be in denial, contacted my doctor to ensure that it was not cardiac in origin since symptoms are often atypical in women.
My physician promptly saw me, then scheduled a nuclear stress test. There was a series of needless glitches. Registration at the diagnostic center had me on their schedule but did not have an order. They would have canceled the procedure had I not been able to get hold of the doctor’s office. Why isn’t an order automatically entered when the physician schedules the test?
While I was given the euphemistic “Patient Rights” brochure, asking to have reports sent to a physician outside of the University of Pittsburgh Medical Center empire is apparently not included.
The staff canceled the stress test because I was not fasting. I had received no instructions from diagnostic cardiology. They suggested it was my internist’s responsibility.
I deliberately ate (2 hours earlier) because my trainer always wants me to eat a light meal so I don’t get hypoglycemic during our workouts, and an exercise stress test, is, of course, a workout. The nurse practitioner said that they were concerned I would vomit. I offered to sign a waiver. She parried, saying they would not be able to get adequate images, so I was out of luck.
When I expressed concern about getting hypoglycemic and having difficulty with the test if fasting, the tech said I should bring a soda and snack. Who tells a “borderline” diabetic to bring a soda?
The tech also said she had called our home to give instructions but encountered a busy signal and had not had time to call back. I had not left the house during the prior week (or most of the past 2 years), so this was a pretty lame excuse.
I suggested to the administration that the hospital offer to email the patient instructions well ahead of time (and perhaps ask for confirmation of receipt). If calling, they should try more than once. They should also have patient instruction sheets at the physician’s office and perhaps have them on their website.
It turns out that the hospital mailed me instructions, not on the date it was ordered, but with the postmark being the day of the procedure itself. With Trump donor Louis DeJoy in charge of the U.S. Postal Service, mail across town now has to travel to Baltimore, 3 hours away, be sorted, and returned.
I did finally have the stress test, which was reassuringly normal. I was not surprised, given that the fury I felt on the first attempt had not precipitated symptoms. The hospital sent a patient ombudsman to meet me there to discuss my previous complaints. I have no idea if they implemented any of the changes I had suggested. In 2021, when I urgently had to take my husband to the ED, I couldn’t see the sign pointing toward the ED and had to ask for directions at the main entrance. They said they would fix that promptly but still have not improved the signage. How I miss the friendly community hospital we had before!
Next was trigger-finger surgery. I had developed that in 1978 from using crutches after a fall. I figured that the relative lull in COVID and my activities made it as good a time as any to finally have it fixed. The surgicenter was great; the surgeon was someone I had worked with and respected for decades. The only glitch was not really knowing how long I was going to be out of commission.
The third encounter (at yet another institution) went really well, despite some early administrative glitches. My major complaint was with the lack of communication between preoperative anesthesia and the operating room and the lack of personalization of preoperative instructions. Despite EPIC, medicines were not correctly reconciled between the different encounters, even on the same day!
After about 15 years of diplopia, which has been gradually worsening, my eye doc had suggested that I consider strabismus surgery as a sort of last-ditch effort to improve my quality of life.
Anesthesiology has stock instructions, which they made no effort to individualize. For example, there is no reason to stop NSAIDs a week before such minor surgery. That’s a problem if you depend on NSAIDs for pain control. Similarly, nothing by mouth after midnight is passé and could be tailored for the patient. I felt particularly inconvenienced that I had to go out of town for the preoperative visit and then have a redundant preoperative clearance by my physician.
The nurses in the preoperative area made me feel quite comfortable and as relaxed as I could be under the circumstances. They had a good sense of humor, which helped too. And from the time I met him a few weeks earlier, I instantly liked my surgeon and felt very comfortable with him and had complete trust.
I was pleased that the chief anesthesiologist responded promptly and undefensively to my letter expressing concerns. I do believe that he will try to improve the systemic problems.
The best part: The surgery appears to have been successful and I should have a significantly improved quality of life.
Hospitals could do so much better by improving communications with patients and by viewing them as customers whose loyalty they must earn and will value. With monopolies growing, memories of such care are quickly fading, soon to be as extinct as the family doc who made house calls.
Dr. Stone is an infectious disease specialist and author of Resilience: One Family’s Story of Hope and Triumph over Evil and Conducting Clinical Research: A Practical Guide. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.












