User login
Official Newspaper of the American College of Surgeons
Americans support the right to affordable health care
Despite the rhetorical winds blowing out of Washington, 92% of Americans believe that they have the right to affordable health care, according to a recent survey by the Commonwealth Fund.
Political affiliation, it turns out, does not appear to determine support for such a right. Democrats aged 19-64 years voiced their support to the tune of 99% in favor of a right to affordable care, compared with 82% of Republicans and 92% of independents, the Commonwealth Fund said in a survey brief released March 1.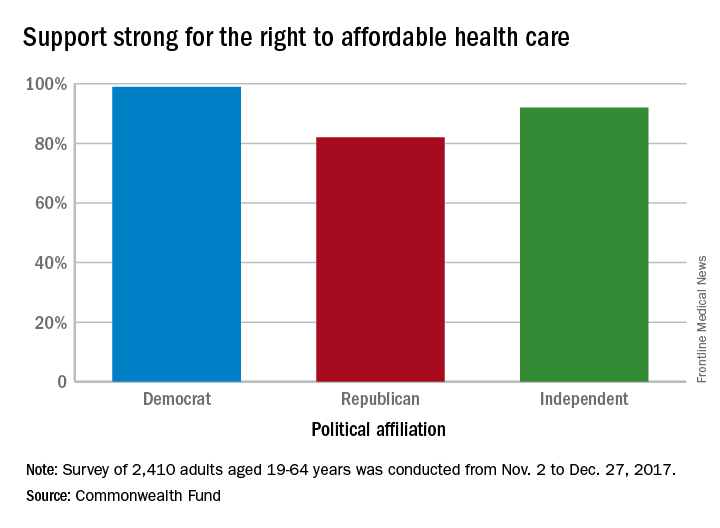
“This survey’s finding that strong majorities of U.S. adults, regardless of party affiliation, believe that all Americans should have a right to affordable health care suggests there may be popular support for a discussion over our preferred path,” the report’s authors wrote.
The survey showed that 36% of those who have health care insurance through the Affordable Care Act marketplaces are pessimistic about their chances of keeping that coverage, compared with 27% of those with Medicaid and 9% of adults with employer-sponsored health benefits.
Among those who lacked confidence about maintaining their coverage, the largest proportion (32%) of respondents believe that they will lose it because the “Trump administration will not carry out the law” and 19% think that they won’t be able to afford it in the future, they said.
“ Such a shift also would provide a more stable regulatory environment for insurers participating in both the marketplaces and Medicaid,” according to the report.
The Commonwealth Fund’s sixth Affordable Care Act Tracking Survey was conducted by the research firm SSRS between Nov. 2 and Dec. 27, 2017, with responses from 2,410 adults aged 19-64 years. The overall margin of error was ±2.7 percentage points at the 95% confidence level.
Despite the rhetorical winds blowing out of Washington, 92% of Americans believe that they have the right to affordable health care, according to a recent survey by the Commonwealth Fund.
Political affiliation, it turns out, does not appear to determine support for such a right. Democrats aged 19-64 years voiced their support to the tune of 99% in favor of a right to affordable care, compared with 82% of Republicans and 92% of independents, the Commonwealth Fund said in a survey brief released March 1.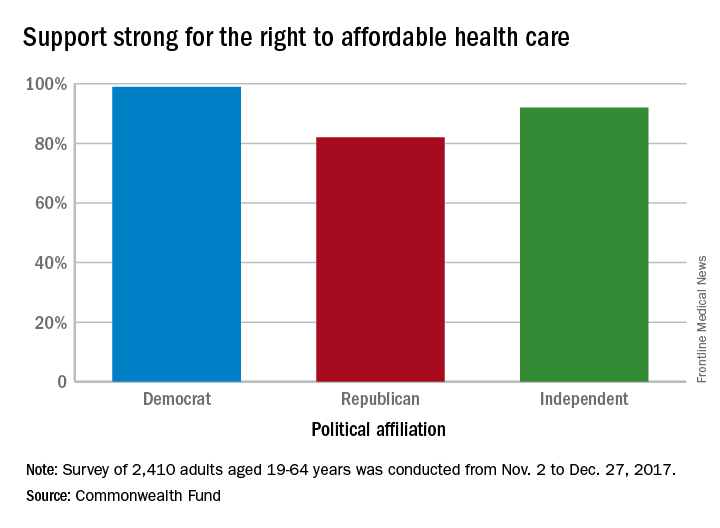
“This survey’s finding that strong majorities of U.S. adults, regardless of party affiliation, believe that all Americans should have a right to affordable health care suggests there may be popular support for a discussion over our preferred path,” the report’s authors wrote.
The survey showed that 36% of those who have health care insurance through the Affordable Care Act marketplaces are pessimistic about their chances of keeping that coverage, compared with 27% of those with Medicaid and 9% of adults with employer-sponsored health benefits.
Among those who lacked confidence about maintaining their coverage, the largest proportion (32%) of respondents believe that they will lose it because the “Trump administration will not carry out the law” and 19% think that they won’t be able to afford it in the future, they said.
“ Such a shift also would provide a more stable regulatory environment for insurers participating in both the marketplaces and Medicaid,” according to the report.
The Commonwealth Fund’s sixth Affordable Care Act Tracking Survey was conducted by the research firm SSRS between Nov. 2 and Dec. 27, 2017, with responses from 2,410 adults aged 19-64 years. The overall margin of error was ±2.7 percentage points at the 95% confidence level.
Despite the rhetorical winds blowing out of Washington, 92% of Americans believe that they have the right to affordable health care, according to a recent survey by the Commonwealth Fund.
Political affiliation, it turns out, does not appear to determine support for such a right. Democrats aged 19-64 years voiced their support to the tune of 99% in favor of a right to affordable care, compared with 82% of Republicans and 92% of independents, the Commonwealth Fund said in a survey brief released March 1.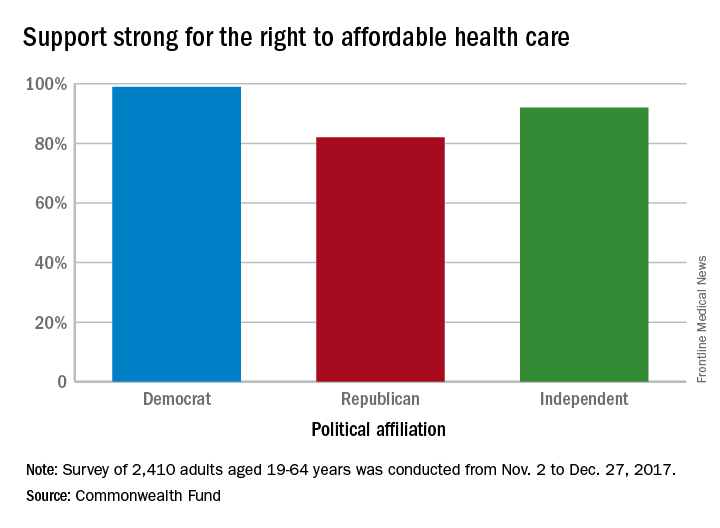
“This survey’s finding that strong majorities of U.S. adults, regardless of party affiliation, believe that all Americans should have a right to affordable health care suggests there may be popular support for a discussion over our preferred path,” the report’s authors wrote.
The survey showed that 36% of those who have health care insurance through the Affordable Care Act marketplaces are pessimistic about their chances of keeping that coverage, compared with 27% of those with Medicaid and 9% of adults with employer-sponsored health benefits.
Among those who lacked confidence about maintaining their coverage, the largest proportion (32%) of respondents believe that they will lose it because the “Trump administration will not carry out the law” and 19% think that they won’t be able to afford it in the future, they said.
“ Such a shift also would provide a more stable regulatory environment for insurers participating in both the marketplaces and Medicaid,” according to the report.
The Commonwealth Fund’s sixth Affordable Care Act Tracking Survey was conducted by the research firm SSRS between Nov. 2 and Dec. 27, 2017, with responses from 2,410 adults aged 19-64 years. The overall margin of error was ±2.7 percentage points at the 95% confidence level.
VIDEO: Model supports endoscopic resection for some T1b esophageal adenocarcinomas
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A Markov model supports endoscopic resection for some T1b esophageal adenocarcinomas.
Major finding: Endoscopic resection was preferred in T1b patients who were more than 80 years old or had a Charlson comorbidity index of 1or 2.
Data source: A Markov model with Surveillance, Epidemiology, and End Results (SEER) Medicare mortality data and published cost data converted to 2017 U.S. dollars based on the national Consumer Price Index.
Disclosures: The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
Source: Chu JN et al. Clin Gastroenterol Hepatol .2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Expert argues for improving MACRA, not scrapping it
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Gender affirmation surgery has become more common
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
The study is thought provoking and suggests many areas for future study.
Gender-affirming surgery is the final step in a spectrum of treatments for gender identity disorders or transsexualism, including psychological counseling, hormonal therapies, and pubertal hormone blockers. Referrals for these treatments are increasing, and likely the demand for surgical treatment will also continue to increase.
A comprehensive database or other prospective tool to assess the comparative efficacy of these treatments, create quality metrics, and address long-term health or psychiatric outcomes should be pursued.
Future research must address cost effectiveness and cost burdens, given increased public funding for gender affirmation surgeries. Most longitudinal studies of patients who have undergone gender affirmation procedures have found high satisfaction rates with low rates of regret (less than 5%). However, when regret occurs, it can be surgically challenging and costly to reverse these procedures.
Marie Crandall , MD, is a professor of surgery at the University of Florida, Jacksonville. She made her comments in an editorial and had no industry disclosures (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6232).
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
, and private insurers and Medicare and Medicaid are covering more of them, according to a review of the National Inpatient Sample from 2000 to 2014.
“As coverage for these procedures increases, likely so will demand for qualified surgeons to perform them,” said investigators led by Joseph Canner, MHS, of Johns Hopkins University, Baltimore (JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231).
The team sought to correct a glaring lack of demographic, hospital, and surgical data on transgender people, a problem due mainly to “the absence of routine, standardized collection and reporting of gender identity in health care settings,” the investigators said.
The Affordable Care Act banned gender identity discrimination, and state and federal governments – as well as private insurers – are expanding coverage of gender affirmation surgery and care. Given the trend, it’s essential that quality improvement agencies begin to “focus on adopting a new set of patient-centered measures to better monitor transgender care and identify opportunities for advancing transition-related services,” the researchers said.
The team identified 37,827 hospital encounters in the national database that had ICD-9 diagnosis codes of transsexualism or gender identity disorder that were listed in the National Inpatient Sample. The rate of those codes increased from 3.87/100,000 patients in 2000 to 14.22 /100,000 patients in 2014.
Mental health was the leading cause of hospitalization, accounting for 40.5% of admissions, a finding that “is consistent with the high prevalence of depression, anxiety, and suicidal ideation in this population,” the investigators said.
Patients were a median age of 38 years old; 57.1% identified as white; and 54.3% were categorized as male, 38.3% as female, and most of the rest as “inconsistent,” meaning their sex in the medical record did not match their procedures.
Almost 11% were hospitalized for gender affirmation surgery, including penile or vaginal construction. From 2000 to 2005, 72% of patients who underwent affirmation procedures had genital surgery; the number increased to 83.9% from 2006 to 2011. More than half of the patients weren’t covered by insurance, but the number covered by Medicare or Medicaid increased from 25 patients in 2012-2013 to 70 in 2014. Meanwhile, no one died in the hospital from gender reassignment surgery, and the median stay was 4 days.
“Our data suggest that genital surgery is the most common type of inpatient gender-affirming surgery; however, these data do not include gender-affirming surgical procedures performed in outpatient settings, which likely include most chest, breast, and facial surgery,” the investigators wrote.
Surgery patients in high-volume centers (performing more than 50 gender-affirming procedures per year) were mostly self-pay, while those admitted to low-volume centers were not. “It is possible that self-paying patients may be getting higher-quality care at high-volume centers, as has been observed in other types of surgery,” according to the investigators. There is a need for national clinical and patient-reported outcomes data to assess and improve the quality of gender-affirming surgery. Gender identity information should be a part of all electronic health records and reported back to national data repositories, they said.
The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
SOURCE: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
FROM JAMA SURGERY
Key clinical point: With gender affirmation surgeries on the rise in the United States, it’s time for a more rigorous system to track outcomes.
Major finding: The rate of transsexual and gender identity disorder codes in the National Inpatient Sample increased from 3.87/100,000 patients in 2000 to 14.22/100,000 patients in 2014.
Study details: A review of 37,827 hospital encounters reported in the National Inpatient Sample.
Disclosures: The investigators are supported by the Patient-Centered Outcomes Research Institute, the Agency for Healthcare Research and Quality, and the National Institutes of Health, among others. They had no industry disclosures.
Source: Canner JK et al. JAMA Surg. 2018 Feb 28. doi: 10.1001/jamasurg.2017.6231.
Supreme Court declines to hear DACA case
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
Preoperative penicillin allergy tests could decrease SSI
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Patients with reported penicillin allergies are at higher risk of developing a surgical site infection.
Major finding: Having a penicillin allergy was associated with a 50% increased risk of developing a surgical site infection, compared with those without the allergy (adjusted odds ratio, 1.5; P = .04).
Study details: Retrospective cohort study of 8,385 patients operated on at Massachusetts General Hospital, Boston, during 2010-2014.
Disclosures: The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
Source: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
Deeply entrenched gender bias in academic medicine is treatable
TAMPA, FLA. – Gender bias that disadvantages women from rising in academic medicine might require specific habit-changing strategies rather than efforts that draw on goodwill alone, according to new follow-up data from a randomized trial discussed and reevaluated at the annual meeting of the American College of Psychiatrists.
One premise of this trial, supported by other research, is that entrenched gender stereotypes drive both male and female behavior and must be addressed directly for change, said Molly Carnes, MD, professor of psychiatry at the University of Wisconsin, Madison.
The initial results of the trial, which randomized academic departments at the University of Wisconsin to participate in habit-changing workshops or to serve as controls, were published almost 3 years ago (Acad Med. 2015 Feb;90[2]:221-30). It is the most recent follow-up (Devine et al. J Exp Soc Psychol. 2017 Nov;73:211-5) that corroborates that long-term changes are possible with intervention.
The published findings showed that when 1,137 faculty members from 46 departments in the experimental arm were compared with 1,153 faculty members from 46 departments in the control arm, there were significant improvements in the experimental arm in surveyed attitudes reflecting personal bias awareness (P = .001) and willingness to support gender equity (P = .013).
These changes in attitude translated into concrete changes in new female faculty hires in the most recent analysis. From 32% in a 2-year period before the workshops, the new female hires climbed to 46% in the 2-year period after the workshops – a relative increase of 44% in the departments participating in the experimental arm. In the control departments, female new faculty hires remained at 32% in both time periods.
“Basically, there are 20 new women faculty members at the University of Wisconsin because of this study,” Dr. Carnes said.
. The result was a fundamental change in culture within departments randomized to the experimental arm, according to data generated by a variety of study analyses.
“When we looked at questions about department climate, we found that both male and female faculty members in the experimental groups were significantly more likely to say they fit in their department, they felt respected for their research and scholarship by their colleagues, and they felt comfortable raising personal and family issues even if they conflicted with departmental activities,” Dr. Carnes said.
This general attitude change is important, because Dr. Carnes emphasized that women share the cultural biases that can result in reduced female career opportunities in clinical and academic medicine. In addition, women generally are aware that stereotypical positive “agentic” adjectives for men, such as decisive, competitive, and ambitious, often are viewed negatively and generate backlash when applied to women. They therefore act on this awareness.
“Stereotype-based bias is a habit that can be broken, but it requires more than good intentions,” said Dr. Carnes, who emphasized that “gender-based assumptions and stereotypes are deeply embedded in the patterns of thinking of both men and women.”
As one example, Dr. Carnes cited her work evaluating female resident behavior when leading in-hospital code resuscitations. There are data to show that there is no difference in the effectiveness of male and female resident code leaders, but women typically feel that the assertive, aggressive behavior required for code leadership is “counternormative.” After the code, some women feel compelled to apologize to team members for being demanding or assertive, a step that Dr. Carnes attributed at least in part to fear of backlash from stepping out of gender-expected behavior.
The fix is not necessarily suppression of gender-related attributes. Dr. Carnes cited evidence that the stereotypical positive communal adjectives for women, such as nurturing, supportive, and sympathetic, might explain why studies suggest that women are more likely than men to be transformational leaders who inspire team members to contribute beyond their own self-interest in achieving goals.
Ultimately, the fix is replacement of stereotypes that impair men as well as women from defusing biases that “lead to subtle unintentional advantages in academic career advancement for Jack not afforded to Jill,” Dr. Carnes said. Based on the low numbers of female leaders in academic medicine decades after medical schools began enrolling women in substantial numbers, she concluded that meaningful change in gender bias is not likely to occur without implementation of specific proactive strategies aimed at challenging current perceptions. Her published study confirms that such strategies can help.
Dr. Carnes reported no conflicts of interest.
Patricia Devine et al. in a recent study published in the Journal of Experimental Social Psychology tested the effect of one 2.5-hour workshop that sought to positively influence the mental habit of gender bias, which exists in our academic world (and elsewhere) in both men and women.
Bevra H. Hahn, MD, is Distinguished Professor of Medicine (emeritus) at the University of California, Los Angeles.
Patricia Devine et al. in a recent study published in the Journal of Experimental Social Psychology tested the effect of one 2.5-hour workshop that sought to positively influence the mental habit of gender bias, which exists in our academic world (and elsewhere) in both men and women.
Bevra H. Hahn, MD, is Distinguished Professor of Medicine (emeritus) at the University of California, Los Angeles.
Patricia Devine et al. in a recent study published in the Journal of Experimental Social Psychology tested the effect of one 2.5-hour workshop that sought to positively influence the mental habit of gender bias, which exists in our academic world (and elsewhere) in both men and women.
Bevra H. Hahn, MD, is Distinguished Professor of Medicine (emeritus) at the University of California, Los Angeles.
TAMPA, FLA. – Gender bias that disadvantages women from rising in academic medicine might require specific habit-changing strategies rather than efforts that draw on goodwill alone, according to new follow-up data from a randomized trial discussed and reevaluated at the annual meeting of the American College of Psychiatrists.
One premise of this trial, supported by other research, is that entrenched gender stereotypes drive both male and female behavior and must be addressed directly for change, said Molly Carnes, MD, professor of psychiatry at the University of Wisconsin, Madison.
The initial results of the trial, which randomized academic departments at the University of Wisconsin to participate in habit-changing workshops or to serve as controls, were published almost 3 years ago (Acad Med. 2015 Feb;90[2]:221-30). It is the most recent follow-up (Devine et al. J Exp Soc Psychol. 2017 Nov;73:211-5) that corroborates that long-term changes are possible with intervention.
The published findings showed that when 1,137 faculty members from 46 departments in the experimental arm were compared with 1,153 faculty members from 46 departments in the control arm, there were significant improvements in the experimental arm in surveyed attitudes reflecting personal bias awareness (P = .001) and willingness to support gender equity (P = .013).
These changes in attitude translated into concrete changes in new female faculty hires in the most recent analysis. From 32% in a 2-year period before the workshops, the new female hires climbed to 46% in the 2-year period after the workshops – a relative increase of 44% in the departments participating in the experimental arm. In the control departments, female new faculty hires remained at 32% in both time periods.
“Basically, there are 20 new women faculty members at the University of Wisconsin because of this study,” Dr. Carnes said.
. The result was a fundamental change in culture within departments randomized to the experimental arm, according to data generated by a variety of study analyses.
“When we looked at questions about department climate, we found that both male and female faculty members in the experimental groups were significantly more likely to say they fit in their department, they felt respected for their research and scholarship by their colleagues, and they felt comfortable raising personal and family issues even if they conflicted with departmental activities,” Dr. Carnes said.
This general attitude change is important, because Dr. Carnes emphasized that women share the cultural biases that can result in reduced female career opportunities in clinical and academic medicine. In addition, women generally are aware that stereotypical positive “agentic” adjectives for men, such as decisive, competitive, and ambitious, often are viewed negatively and generate backlash when applied to women. They therefore act on this awareness.
“Stereotype-based bias is a habit that can be broken, but it requires more than good intentions,” said Dr. Carnes, who emphasized that “gender-based assumptions and stereotypes are deeply embedded in the patterns of thinking of both men and women.”
As one example, Dr. Carnes cited her work evaluating female resident behavior when leading in-hospital code resuscitations. There are data to show that there is no difference in the effectiveness of male and female resident code leaders, but women typically feel that the assertive, aggressive behavior required for code leadership is “counternormative.” After the code, some women feel compelled to apologize to team members for being demanding or assertive, a step that Dr. Carnes attributed at least in part to fear of backlash from stepping out of gender-expected behavior.
The fix is not necessarily suppression of gender-related attributes. Dr. Carnes cited evidence that the stereotypical positive communal adjectives for women, such as nurturing, supportive, and sympathetic, might explain why studies suggest that women are more likely than men to be transformational leaders who inspire team members to contribute beyond their own self-interest in achieving goals.
Ultimately, the fix is replacement of stereotypes that impair men as well as women from defusing biases that “lead to subtle unintentional advantages in academic career advancement for Jack not afforded to Jill,” Dr. Carnes said. Based on the low numbers of female leaders in academic medicine decades after medical schools began enrolling women in substantial numbers, she concluded that meaningful change in gender bias is not likely to occur without implementation of specific proactive strategies aimed at challenging current perceptions. Her published study confirms that such strategies can help.
Dr. Carnes reported no conflicts of interest.
TAMPA, FLA. – Gender bias that disadvantages women from rising in academic medicine might require specific habit-changing strategies rather than efforts that draw on goodwill alone, according to new follow-up data from a randomized trial discussed and reevaluated at the annual meeting of the American College of Psychiatrists.
One premise of this trial, supported by other research, is that entrenched gender stereotypes drive both male and female behavior and must be addressed directly for change, said Molly Carnes, MD, professor of psychiatry at the University of Wisconsin, Madison.
The initial results of the trial, which randomized academic departments at the University of Wisconsin to participate in habit-changing workshops or to serve as controls, were published almost 3 years ago (Acad Med. 2015 Feb;90[2]:221-30). It is the most recent follow-up (Devine et al. J Exp Soc Psychol. 2017 Nov;73:211-5) that corroborates that long-term changes are possible with intervention.
The published findings showed that when 1,137 faculty members from 46 departments in the experimental arm were compared with 1,153 faculty members from 46 departments in the control arm, there were significant improvements in the experimental arm in surveyed attitudes reflecting personal bias awareness (P = .001) and willingness to support gender equity (P = .013).
These changes in attitude translated into concrete changes in new female faculty hires in the most recent analysis. From 32% in a 2-year period before the workshops, the new female hires climbed to 46% in the 2-year period after the workshops – a relative increase of 44% in the departments participating in the experimental arm. In the control departments, female new faculty hires remained at 32% in both time periods.
“Basically, there are 20 new women faculty members at the University of Wisconsin because of this study,” Dr. Carnes said.
. The result was a fundamental change in culture within departments randomized to the experimental arm, according to data generated by a variety of study analyses.
“When we looked at questions about department climate, we found that both male and female faculty members in the experimental groups were significantly more likely to say they fit in their department, they felt respected for their research and scholarship by their colleagues, and they felt comfortable raising personal and family issues even if they conflicted with departmental activities,” Dr. Carnes said.
This general attitude change is important, because Dr. Carnes emphasized that women share the cultural biases that can result in reduced female career opportunities in clinical and academic medicine. In addition, women generally are aware that stereotypical positive “agentic” adjectives for men, such as decisive, competitive, and ambitious, often are viewed negatively and generate backlash when applied to women. They therefore act on this awareness.
“Stereotype-based bias is a habit that can be broken, but it requires more than good intentions,” said Dr. Carnes, who emphasized that “gender-based assumptions and stereotypes are deeply embedded in the patterns of thinking of both men and women.”
As one example, Dr. Carnes cited her work evaluating female resident behavior when leading in-hospital code resuscitations. There are data to show that there is no difference in the effectiveness of male and female resident code leaders, but women typically feel that the assertive, aggressive behavior required for code leadership is “counternormative.” After the code, some women feel compelled to apologize to team members for being demanding or assertive, a step that Dr. Carnes attributed at least in part to fear of backlash from stepping out of gender-expected behavior.
The fix is not necessarily suppression of gender-related attributes. Dr. Carnes cited evidence that the stereotypical positive communal adjectives for women, such as nurturing, supportive, and sympathetic, might explain why studies suggest that women are more likely than men to be transformational leaders who inspire team members to contribute beyond their own self-interest in achieving goals.
Ultimately, the fix is replacement of stereotypes that impair men as well as women from defusing biases that “lead to subtle unintentional advantages in academic career advancement for Jack not afforded to Jill,” Dr. Carnes said. Based on the low numbers of female leaders in academic medicine decades after medical schools began enrolling women in substantial numbers, she concluded that meaningful change in gender bias is not likely to occur without implementation of specific proactive strategies aimed at challenging current perceptions. Her published study confirms that such strategies can help.
Dr. Carnes reported no conflicts of interest.
REPORTING FROM THE COLLEGE 2018
New device cuts postoperative pulmonary complications
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
AT THE CRITICAL CARE CONGRESS
Key clinical point: A device that combines lung expansion, secretion clearance, and aerosol delivery (MetaNeb) appears to reduce postoperative pulmonary complications and resource use.Major finding: Pulmonary complications occurred in 36.7% of intubated patients, compared with 69.8% for a prospectively evaluated reference population (P less than 0.05).
Data source: A prospective, nonrandomized, two-stage study including 417 subjects who underwent thoracic, upper-abdominal, or aortic open surgical procedure at one of three centers.
Disclosures: The study was sponsored by Hill-Rom, which manufactures the MetaNeb device. Investigators had no financial conflicts related to the study.
Source: Huynh T et al. Critical Care Congress, Abstract 17.
Adenotonsillectomy reduced hypertension in OSA subgroup
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
FROM JAMA OTOLARYNGOLOGY-HEAD & NECK SURGERY
Key clinical point: Hypertensive children with obstructive sleep apnea (OSA) who had an adenotonsillectomy experienced significant improvements in their blood pressure after surgery.
Major finding: Sixty-six percent of hypertensive patients with OSA became nonhypertensive after adenotonsillectomy.
Study details: A retrospective analysis of 240 nonobese children with OSA who underwent adenotonsillectomy.
Disclosures: The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
Source: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
Will Indiana Medicaid work requirements pass legal muster?
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.