User login
Official Newspaper of the American College of Surgeons
Guidelines update best practices for hemorrhoid treatment
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
Each year, more than 2.2 million patients in the United States undergo evaluations for symptoms of hemorrhoids, according to updated guidelines on the management of hemorrhoids issued by the American Society of Colon and Rectal Surgeons.
“As a result, it is important to identify symptomatic hemorrhoids as the underlying source of the anorectal symptom and to have a clear understanding of the evaluation and management of this disease process,” wrote Bradley R. Davis, MD, FACS, chief of colon and rectal surgery at the Carolinas Medical Center, Charlotte, N.C., and the fellow members of the Clinical Practice Guidelines Committee of the ASCRS.
The guidelines recommend evaluation of hemorrhoids based on a disease-specific history, and a physical that emphasizes the degree and duration of symptoms and identifies risk factors. But the guideline writers note that the recommendation is a grade 1C because the supporting data mainly come from observational or case studies.
“The cardinal signs of internal hemorrhoids are painless bleeding with bowel movements with intermittent protrusion,” the committee said, also emphasizing that patients should be evaluated for fecal incontinence, which could inform surgical decision making.
In addition, the guidelines call for a complete endoscopic evaluation of the colon for patients who present with symptomatic hemorrhoids and rectal bleeding; this recommendation is based on moderately strong evidence, and presented with a grade of 1B.
Medical management of hemorrhoids may include office-based procedures or surgery, according to the guidelines.
“Most patients with grade I and II and select patients with grade III internal hemorrhoidal disease who fail medical treatment can be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation,” the committee wrote, and medical office treatment received a strong grade 1A recommendation based on high-quality evidence. Although office procedures are generally well tolerated, the condition can recur. Bleeding is the most common complication, and it is more likely after rubber-band ligation than other office-based options, the guidelines state.
The guidelines offer a weak recommendation of 2C, based on the lack of quality evidence, for the use of early surgical excision to treat patients with thrombosed external hemorrhoids. “Although most patients treated nonoperatively will experience eventual resolution of their symptoms, excision of thrombosed external hemorrhoids may result in more rapid symptom resolution, lower incidence of recurrence, and longer remission intervals,” the committee noted.
Surgical hemorrhoidectomy received the strongest possible recommendation (1A, based on high-quality evidence) for the treatment of patients with external hemorrhoids or a combination of internal and external hemorrhoids with prolapse.
Surgical options described in the recommendations include surgical excision (hemorrhoidectomy), hemorrhoidopexy, and Doppler-guided hemorrhoidectomy, with citations of studies on each procedure. Data from a meta-analysis of 18 randomized prospective studies comparing hemorrhoidectomy with office-based procedures showed that hemorrhoidectomy was “the most effective treatment for patients with grade III hemorrhoids,” but it was associated with greater pain and complication rates, according to the guidelines.
However, complications in general are low after surgical hemorrhoidectomy, with reported complication rates of 1%-2% for the most common complication of postprocedure hemorrhage, the guidelines state. After surgery, the guidelines recommend with a 1B grade (moderate quality evidence) that patients use “a multimodality pain regimen to reduce narcotic usage and promote a faster recovery.”
The committee members had no financial conflicts to disclose.
SOURCE: Davis BR et al. Dis Colon Rectum. 2018; 61:284-92.
FROM DISEASES OF THE COLON & RECTUM
Defining incisional hernia risk in IBD surgery
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Open surgery for inflammatory bowel disease (IBD) has been known to carry a high risk of incisional hernia, but the risk factors have not been well understood.
A review of 1,000 operations performed over nearly 40 years at a high-volume, nationally recognized center has identified five patient factors that can raise the risk of incisional hernia in these operations by 50% or more, according to a study published in the Annals of Surgery.
The study followed the patients for an average of 8 years after their operations, which were performed between January 1976 and December 2014 at Mount Sinai Medical Center in New York. The overall incidence of incisional hernia was 20%-21% for patients with ulcerative colitis and 20% for those with Crohn’s disease.
Half of these patients developed an incisional hernia less than 2 years after the index surgery and 75% in less than 4 years.
The researchers identified the following statistically significant risk factors for incisional hernia: wound infection (hazard ratio, 3.66; P less than .001); hypoalbuminemia (HR, 2.02; P = .002); previous bowel resection (HR, 1.6; P = .003); ileostomy created at time of procedure (HR, 1.53; P = .01); and a history of smoking (HR, 1.52; P less than .013). Other risk factors to lesser degrees are body mass index at time of surgery (HR, 1.036; P = .009); age at time of surgery (HR, 1.021; P less than .001), and age at disease onset (HR, 1.018; P less than .001).
Lead author Tomas Heimann, MD, and his coauthors pointed out that this study population had severe levels of disease. Almost half of the patients had severe intractable disease that had resisted medical treatment. More than a quarter of these patients had received preoperative steroid therapy within 6 weeks, and 15% had received recent immunosuppressive therapy. Almost 80% were either anemic or had hypoalbuminemia or both. The average duration of disease was 12 years. More than half had undergone previous bowel surgery – “often lengthy and difficult” – with many patients suffering from fistulae, abscesses, and dense adhesions. “These factors were more likely to predispose patients to develop wound infections and delayed healing resulting in incisional hernia in one-fifth of our patients,” Dr. Heimann and his coauthors noted.
A somewhat unexpected finding was that immunosuppressive therapy and steroids were not linked to incisional hernia in these patients.
Prophylactic mesh placement in patients with IBD is impractical because of the risk of infection it carries, Dr. Heimann and his coauthors said.
Dr. Heimann and his coauthors reported having no financial disclosures.
SOURCE: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
FROM ANNALS OF SURGERY
Key clinical point: Patients with IBD have a high incidence of incisional hernia after open bowel resection.
Major finding: The overall incidence of incisional hernia after open bowel resection was 20%.
Data source: One thousand patients who had undergone open bowel surgery for IBD at Mount Sinai Medical Center, New York, between January 1976 and December 2014.
Disclosures: Dr. Heimann and his coauthors reported having no financial disclosures.
Source: Heimann T et al. Ann Surg. 2018 Mar;267(3):532-6.
Cyberliability insurance: Should you purchase a policy?
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
Pre–bariatric surgery weight loss improves outcomes
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Preoperative weight loss improves bariatric surgery outcomes, according to findings from a single-institution retrospective analysis. The weight loss came from following a 4-week low-calorie diet (LCD) and was of greatest benefit to patients who lost 8% or more of their excess weight. These patients had a greater loss of excess weight in the 12 months following surgery, as well as shorter average hospital length of stay.
Preliminary studies indicated that short-term weight loss before surgery might reduce surgical complexity by reducing the size of the liver and intra-abdominal fat mass, but it remained uncertain what effect weight loss might have on long-term outcomes.
The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. Liquids included at least 80 ounces of calorie-free, caffeine-free, carbonation-free beverages per day. Patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
Deborah A. Hutcheon, DCN, and her fellow researchers analyzed data from their own institution, where a presurgical 4-week LCD with a target loss of 8% or more of excess weight had been standard policy already. The population included 355 patients who underwent sleeve gastrectomy (n = 167) or Roux-en-Y gastric bypass (n = 188) between January 2014 and January 2016.
Almost two-thirds (63.3%) of patients achieved the target weight loss before surgery. There were some differences between the two groups. The group that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively; P = .013), a higher proportion of white patients (84.8% vs. 74.1%; P = .011), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%; P = .048). The two groups had similar rates of preoperative comorbidities and surgery types.
Those who achieved the target weight loss had a shorter hospital length of stay (1.8 days vs. 2.1 days; P = .006). They also had a higher percentage loss of excess weight at 3 months (42.3% vs. 36.1%; P less than .001), 6 months (56.0% vs. 47.5%; P less than .001), and at 12 months (65.1% vs. 55.7%; P = .003).
After controlling for patient characteristics, insurance status, 12-month diet compliance, and surgery type, successful presurgery weight loss was associated with greater weight loss at 12 months.
SOURCE: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Weight loss before bariatric surgery boosts results.
Major finding: Patients who lost at least 8% of excess body weight had an average of 65.1% loss of excess weight at 12 months, compared with the 55.7% seen in those who did not.
Data source: Retrospective, single-center analysis (n = 355).
Disclosures: No source of funding was disclosed.
Source: Hutcheon DA et al. J Am Coll Surgeons. 2018 Jan 31. doi: 10.1016/j.jamcollsurg.2017.12.032.
Trump administration proposes rule to loosen curbs on short-term health plans
Insurers will again be able to sell short-term health insurance good for up to 12 months under a proposed rule released Feb. 20 by the Trump administration that could further roil the marketplace.
“We want to open up affordable alternatives to unaffordable Affordable Care Act policies,” said Health and Human Services Secretary Alex Azar. “This is one step in the direction of providing Americans health insurance options that are more affordable and more suitable to individual and family circumstances.”
The proposed rule said short-term plans could add more choices to the market at lower cost and may offer broader provider networks than Affordable Care Act plans in rural areas.
But most short-term coverage requires answering a string of medical questions, and insurers can reject applicants with preexisting medical problems, which ACA plans cannot do. As a result, the proposed rule also noted that some people who switch to them from ACA coverage may see “reduced access to some services,” and “increased out of pocket costs, possibly leading to financial hardship.”
The directive follows an executive order issued in October to roll back restrictions put in place during the Obama administration that limited these plans to 3 months. The rule comes on the heels of Congress’ approval of tax legislation that in 2019 will end the penalty for people who opt not to carry insurance coverage.
The administration also issued separate regulations Jan. 4 that would make it easier to form “association health plans,” which are offered to small businesses through membership organizations.
Together, the proposed regulations and the elimination of the so-called individual mandate by Congress could further undermine the Affordable Care Act marketplace, critics say.
Seema Verma, who now heads the Centers for Medicare & Medicaid Services, which oversees the marketplaces, told reporters Feb. 20 that federal officials believe that between 100,000 and 200,000 “healthy people” now buying insurance through those federal exchanges would switch to the short-term plans, as well as others who are now uninsured.
The new rule is expected to entice younger and healthier people from the general insurance pool by allowing a range of lower-cost options that don’t include all the benefits required by the federal law – including plans that can reject people with preexisting medical conditions. Most short-term coverage excludes benefits for maternity care, preventive care, mental health services, or substance abuse treatment.
“It’s deeply concerning to me, considering the tragedy in Florida and national opioid crisis, that the administration would be encouraging the sale of policies that don’t have to cover mental health and substance abuse,” said Kevin Lucia, a research professor and project director at Georgetown University’s Health Policy Institute.
Over time, those remaining in ACA plans will increasingly be those who qualify for premium tax credit subsidies and the sick, who can’t get an alternative like a short-term plan, predict Mr. Lucia and other experts. That, in turn, would drive up ACA premiums further.
“If consumers think Obamacare premiums are high today, wait until people flood into these short-term and association health plans,” said industry consultant Robert Laszewski. “The Trump administration will bring rates down substantially for healthy people, but woe unto those who get a condition and have to go back into Obamacare.”
If 100,000-200,000 people shift from ACA-compliant plans in 2019, this would cause “average monthly individual market premiums … to increase,” the proposed rule states. That, in turn, would cause subsidies for eligible policyholders in the ACA market to rise, costing the government $96 million–$168 million.
Supporters said the rules are needed because the ACA plans have already become too costly for people who don’t receive a government subsidy to help them purchase the coverage. “The current system is failing too many,” said Ms. Verma.
And, many supporters don’t think the change is as significant as skeptics fear.
“It simply reverts back to where the short-term plan rules were prior to Obama limiting those plans,” said Christopher Condeluci, a benefits attorney who also served as tax counsel to the U.S. Senate Finance Committee. “While these plans might not be the best answer, people do need a choice, and this new proposal provides needed choice to a certain subsection of the population.”
But, in their call with reporters, CMS officials said the proposed rule seeks comment on whether there are ways to guarantee renewability of the plans, which currently cannot be renewed. Instead, policyholders must reapply and answer medical questions again. The proposal also seeks comments on whether the plans should be allowed for longer than 12-month periods.
The comment period for the proposed rule runs for 60 days. Ms. Verma said CMS hopes to get final rules out “as quickly as possible,” so insurers could start offering the longer duration plans.
Short-term plans had been designed as temporary coverage, lasting for a few months while, for instance, a worker is between jobs and employer-sponsored insurances. They provide some protection to those who enroll, generally paying a percentage of hospital and doctor bills after the policyholder meets a deductible.
They are generally less expensive than ACA plans, because they cover less. For example, they set annual and lifetime caps on benefits, and few cover prescription drugs.
Most require applicants to pass a medical questionnaire – and they can also exclude coverage for preexisting medical conditions.
The plans are appealing to consumers because they are cheaper than Obamacare plans. They are also attractive to brokers, because they often pay higher commissions than ACA plans. Insurers like them because their profit margins are relatively high – and are not held to the ACA requirement that they spend at least 80 percent of premium revenue on plan members’ medical care.
Extending short-term plans to a full year could be a benefit to consumers because they must pass the health questionnaire only once. Still, if a consumer develops a health condition during the contract’s term, that person would likely be rejected if he or she tried to renew.
Both supporters and critics of short-term plans say consumers who do develop health problems could then sign up for an ACA plan during the next open enrollment because the ACA bars insurers from rejecting people with preexisting conditions.
“We’re going to have two different markets, a Wild West frontier called short-term medical … and a high-risk pool called Obamacare,” said Laszewski.
KHN senior correspondent Phil Galewitz contributed to this article. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Insurers will again be able to sell short-term health insurance good for up to 12 months under a proposed rule released Feb. 20 by the Trump administration that could further roil the marketplace.
“We want to open up affordable alternatives to unaffordable Affordable Care Act policies,” said Health and Human Services Secretary Alex Azar. “This is one step in the direction of providing Americans health insurance options that are more affordable and more suitable to individual and family circumstances.”
The proposed rule said short-term plans could add more choices to the market at lower cost and may offer broader provider networks than Affordable Care Act plans in rural areas.
But most short-term coverage requires answering a string of medical questions, and insurers can reject applicants with preexisting medical problems, which ACA plans cannot do. As a result, the proposed rule also noted that some people who switch to them from ACA coverage may see “reduced access to some services,” and “increased out of pocket costs, possibly leading to financial hardship.”
The directive follows an executive order issued in October to roll back restrictions put in place during the Obama administration that limited these plans to 3 months. The rule comes on the heels of Congress’ approval of tax legislation that in 2019 will end the penalty for people who opt not to carry insurance coverage.
The administration also issued separate regulations Jan. 4 that would make it easier to form “association health plans,” which are offered to small businesses through membership organizations.
Together, the proposed regulations and the elimination of the so-called individual mandate by Congress could further undermine the Affordable Care Act marketplace, critics say.
Seema Verma, who now heads the Centers for Medicare & Medicaid Services, which oversees the marketplaces, told reporters Feb. 20 that federal officials believe that between 100,000 and 200,000 “healthy people” now buying insurance through those federal exchanges would switch to the short-term plans, as well as others who are now uninsured.
The new rule is expected to entice younger and healthier people from the general insurance pool by allowing a range of lower-cost options that don’t include all the benefits required by the federal law – including plans that can reject people with preexisting medical conditions. Most short-term coverage excludes benefits for maternity care, preventive care, mental health services, or substance abuse treatment.
“It’s deeply concerning to me, considering the tragedy in Florida and national opioid crisis, that the administration would be encouraging the sale of policies that don’t have to cover mental health and substance abuse,” said Kevin Lucia, a research professor and project director at Georgetown University’s Health Policy Institute.
Over time, those remaining in ACA plans will increasingly be those who qualify for premium tax credit subsidies and the sick, who can’t get an alternative like a short-term plan, predict Mr. Lucia and other experts. That, in turn, would drive up ACA premiums further.
“If consumers think Obamacare premiums are high today, wait until people flood into these short-term and association health plans,” said industry consultant Robert Laszewski. “The Trump administration will bring rates down substantially for healthy people, but woe unto those who get a condition and have to go back into Obamacare.”
If 100,000-200,000 people shift from ACA-compliant plans in 2019, this would cause “average monthly individual market premiums … to increase,” the proposed rule states. That, in turn, would cause subsidies for eligible policyholders in the ACA market to rise, costing the government $96 million–$168 million.
Supporters said the rules are needed because the ACA plans have already become too costly for people who don’t receive a government subsidy to help them purchase the coverage. “The current system is failing too many,” said Ms. Verma.
And, many supporters don’t think the change is as significant as skeptics fear.
“It simply reverts back to where the short-term plan rules were prior to Obama limiting those plans,” said Christopher Condeluci, a benefits attorney who also served as tax counsel to the U.S. Senate Finance Committee. “While these plans might not be the best answer, people do need a choice, and this new proposal provides needed choice to a certain subsection of the population.”
But, in their call with reporters, CMS officials said the proposed rule seeks comment on whether there are ways to guarantee renewability of the plans, which currently cannot be renewed. Instead, policyholders must reapply and answer medical questions again. The proposal also seeks comments on whether the plans should be allowed for longer than 12-month periods.
The comment period for the proposed rule runs for 60 days. Ms. Verma said CMS hopes to get final rules out “as quickly as possible,” so insurers could start offering the longer duration plans.
Short-term plans had been designed as temporary coverage, lasting for a few months while, for instance, a worker is between jobs and employer-sponsored insurances. They provide some protection to those who enroll, generally paying a percentage of hospital and doctor bills after the policyholder meets a deductible.
They are generally less expensive than ACA plans, because they cover less. For example, they set annual and lifetime caps on benefits, and few cover prescription drugs.
Most require applicants to pass a medical questionnaire – and they can also exclude coverage for preexisting medical conditions.
The plans are appealing to consumers because they are cheaper than Obamacare plans. They are also attractive to brokers, because they often pay higher commissions than ACA plans. Insurers like them because their profit margins are relatively high – and are not held to the ACA requirement that they spend at least 80 percent of premium revenue on plan members’ medical care.
Extending short-term plans to a full year could be a benefit to consumers because they must pass the health questionnaire only once. Still, if a consumer develops a health condition during the contract’s term, that person would likely be rejected if he or she tried to renew.
Both supporters and critics of short-term plans say consumers who do develop health problems could then sign up for an ACA plan during the next open enrollment because the ACA bars insurers from rejecting people with preexisting conditions.
“We’re going to have two different markets, a Wild West frontier called short-term medical … and a high-risk pool called Obamacare,” said Laszewski.
KHN senior correspondent Phil Galewitz contributed to this article. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Insurers will again be able to sell short-term health insurance good for up to 12 months under a proposed rule released Feb. 20 by the Trump administration that could further roil the marketplace.
“We want to open up affordable alternatives to unaffordable Affordable Care Act policies,” said Health and Human Services Secretary Alex Azar. “This is one step in the direction of providing Americans health insurance options that are more affordable and more suitable to individual and family circumstances.”
The proposed rule said short-term plans could add more choices to the market at lower cost and may offer broader provider networks than Affordable Care Act plans in rural areas.
But most short-term coverage requires answering a string of medical questions, and insurers can reject applicants with preexisting medical problems, which ACA plans cannot do. As a result, the proposed rule also noted that some people who switch to them from ACA coverage may see “reduced access to some services,” and “increased out of pocket costs, possibly leading to financial hardship.”
The directive follows an executive order issued in October to roll back restrictions put in place during the Obama administration that limited these plans to 3 months. The rule comes on the heels of Congress’ approval of tax legislation that in 2019 will end the penalty for people who opt not to carry insurance coverage.
The administration also issued separate regulations Jan. 4 that would make it easier to form “association health plans,” which are offered to small businesses through membership organizations.
Together, the proposed regulations and the elimination of the so-called individual mandate by Congress could further undermine the Affordable Care Act marketplace, critics say.
Seema Verma, who now heads the Centers for Medicare & Medicaid Services, which oversees the marketplaces, told reporters Feb. 20 that federal officials believe that between 100,000 and 200,000 “healthy people” now buying insurance through those federal exchanges would switch to the short-term plans, as well as others who are now uninsured.
The new rule is expected to entice younger and healthier people from the general insurance pool by allowing a range of lower-cost options that don’t include all the benefits required by the federal law – including plans that can reject people with preexisting medical conditions. Most short-term coverage excludes benefits for maternity care, preventive care, mental health services, or substance abuse treatment.
“It’s deeply concerning to me, considering the tragedy in Florida and national opioid crisis, that the administration would be encouraging the sale of policies that don’t have to cover mental health and substance abuse,” said Kevin Lucia, a research professor and project director at Georgetown University’s Health Policy Institute.
Over time, those remaining in ACA plans will increasingly be those who qualify for premium tax credit subsidies and the sick, who can’t get an alternative like a short-term plan, predict Mr. Lucia and other experts. That, in turn, would drive up ACA premiums further.
“If consumers think Obamacare premiums are high today, wait until people flood into these short-term and association health plans,” said industry consultant Robert Laszewski. “The Trump administration will bring rates down substantially for healthy people, but woe unto those who get a condition and have to go back into Obamacare.”
If 100,000-200,000 people shift from ACA-compliant plans in 2019, this would cause “average monthly individual market premiums … to increase,” the proposed rule states. That, in turn, would cause subsidies for eligible policyholders in the ACA market to rise, costing the government $96 million–$168 million.
Supporters said the rules are needed because the ACA plans have already become too costly for people who don’t receive a government subsidy to help them purchase the coverage. “The current system is failing too many,” said Ms. Verma.
And, many supporters don’t think the change is as significant as skeptics fear.
“It simply reverts back to where the short-term plan rules were prior to Obama limiting those plans,” said Christopher Condeluci, a benefits attorney who also served as tax counsel to the U.S. Senate Finance Committee. “While these plans might not be the best answer, people do need a choice, and this new proposal provides needed choice to a certain subsection of the population.”
But, in their call with reporters, CMS officials said the proposed rule seeks comment on whether there are ways to guarantee renewability of the plans, which currently cannot be renewed. Instead, policyholders must reapply and answer medical questions again. The proposal also seeks comments on whether the plans should be allowed for longer than 12-month periods.
The comment period for the proposed rule runs for 60 days. Ms. Verma said CMS hopes to get final rules out “as quickly as possible,” so insurers could start offering the longer duration plans.
Short-term plans had been designed as temporary coverage, lasting for a few months while, for instance, a worker is between jobs and employer-sponsored insurances. They provide some protection to those who enroll, generally paying a percentage of hospital and doctor bills after the policyholder meets a deductible.
They are generally less expensive than ACA plans, because they cover less. For example, they set annual and lifetime caps on benefits, and few cover prescription drugs.
Most require applicants to pass a medical questionnaire – and they can also exclude coverage for preexisting medical conditions.
The plans are appealing to consumers because they are cheaper than Obamacare plans. They are also attractive to brokers, because they often pay higher commissions than ACA plans. Insurers like them because their profit margins are relatively high – and are not held to the ACA requirement that they spend at least 80 percent of premium revenue on plan members’ medical care.
Extending short-term plans to a full year could be a benefit to consumers because they must pass the health questionnaire only once. Still, if a consumer develops a health condition during the contract’s term, that person would likely be rejected if he or she tried to renew.
Both supporters and critics of short-term plans say consumers who do develop health problems could then sign up for an ACA plan during the next open enrollment because the ACA bars insurers from rejecting people with preexisting conditions.
“We’re going to have two different markets, a Wild West frontier called short-term medical … and a high-risk pool called Obamacare,” said Laszewski.
KHN senior correspondent Phil Galewitz contributed to this article. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Parental leave not available to all academic surgeons
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.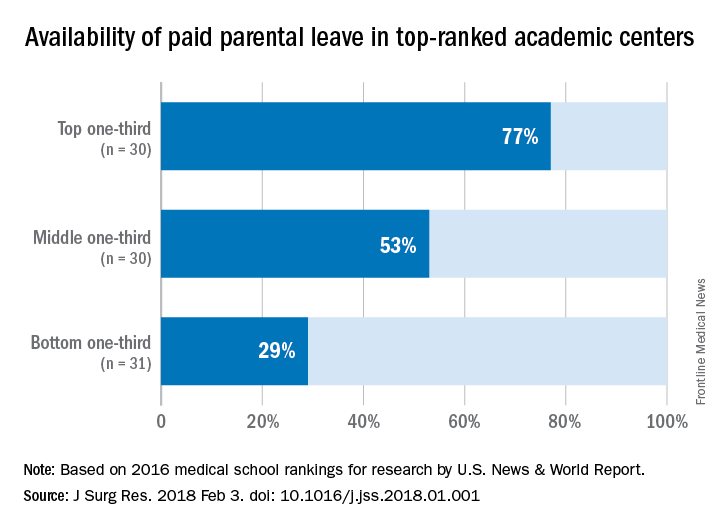
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.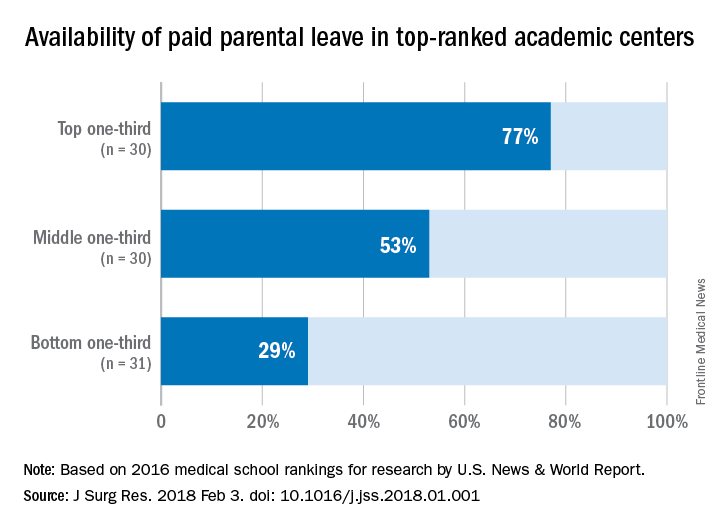
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.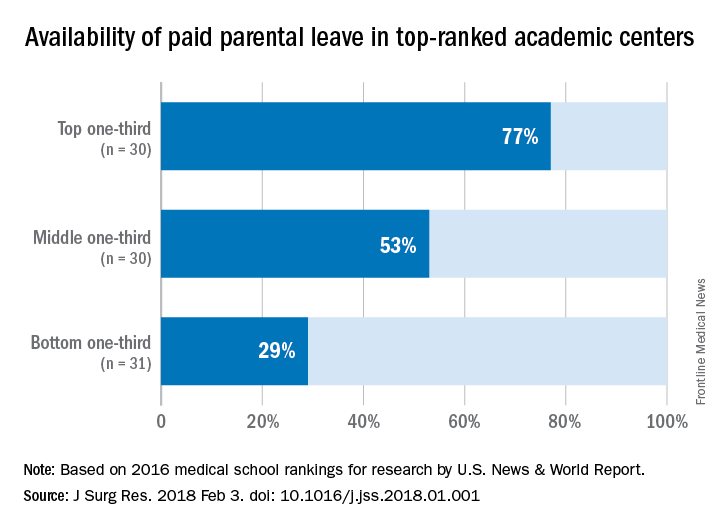
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Parental leave policies have been unevenly adopted by U.S. medical schools.
Major finding: Among the top 91 ranked medical schools, 53% offer paid parental leave.
Data source: Survey of 91 top academic medical centers identified in U.S. News & World Report 2016 listing.
Disclosures: The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
How real is resident burnout?
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
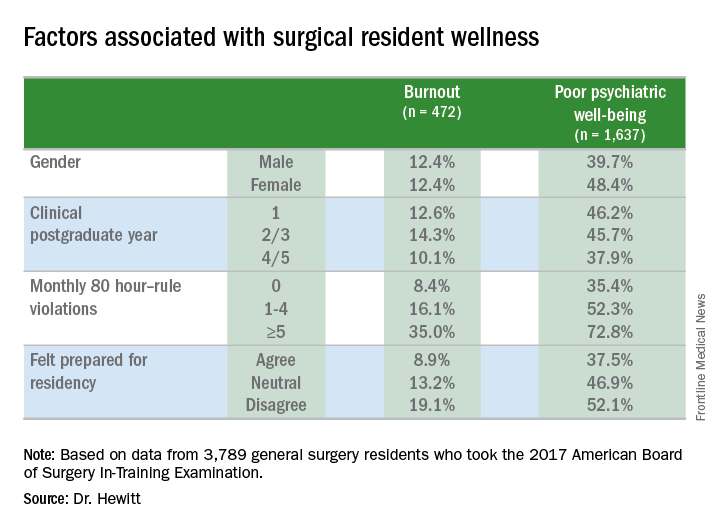
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
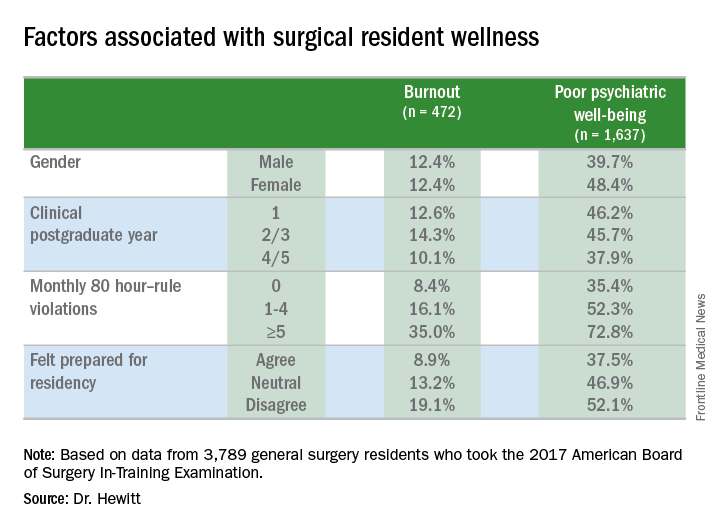
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
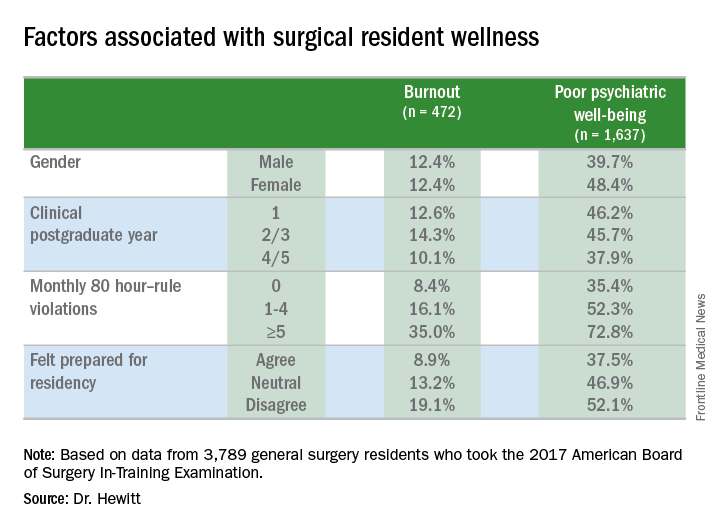
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Almost one in four surgical residents manifest a daily symptom of burnout.
Major finding: Overall 22.8% of daily and 44.3% had poor psychiatric well-being scores.
Study details: Surveys completed by 3,789 general surgery residents during the American Board of Surgery In-Training Examination in January 2017.
Disclosures: The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
Source: Hewitt B et al. abstract 21.01
Salpingectomy at cesarean feasible, but adds to operative time
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Salpingectomy was successful in two-thirds of patients but added 15 minutes to operative time.
Major finding: The intended procedure was successful in 27 of 40 salpingectomy patients (67.5%) and 38 of 40 tubal ligation patients (95%; P = .02).
Study details: Randomized controlled trial of 80 women receiving bilateral salpingectomy or tubal ligation at cesarean delivery.
Disclosures: Study funding was received from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
Source: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
Postcesarean SSI rate declines with care bundle*
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: The postcesarean surgical site infection rate dropped by more than half after a multicomponent care bundle was put in place.*
Major finding: SSIs patients went from 2.44 to 1.10/1,000 after the bundle was implemented (P = .013).
Study details: Case-control study of 1,085 women pre– and 1,261 women post–care bundle implementation.
Disclosures: The authors reported no conflicts of interest.
Source: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Liver cancer deaths expected to increase again in 2018
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.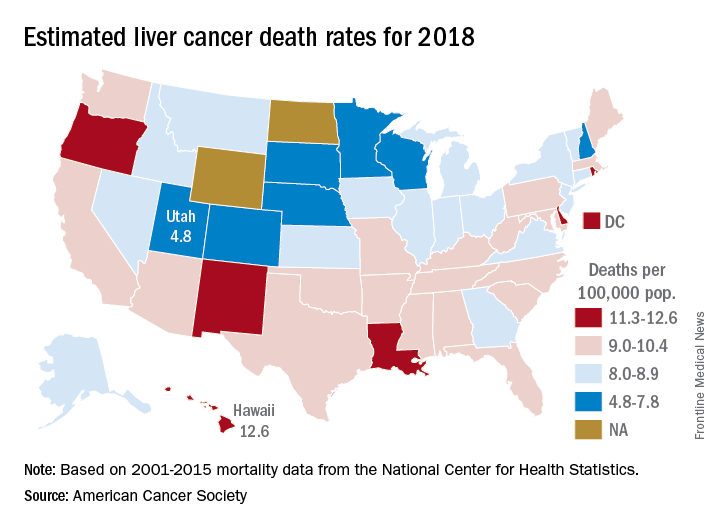
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.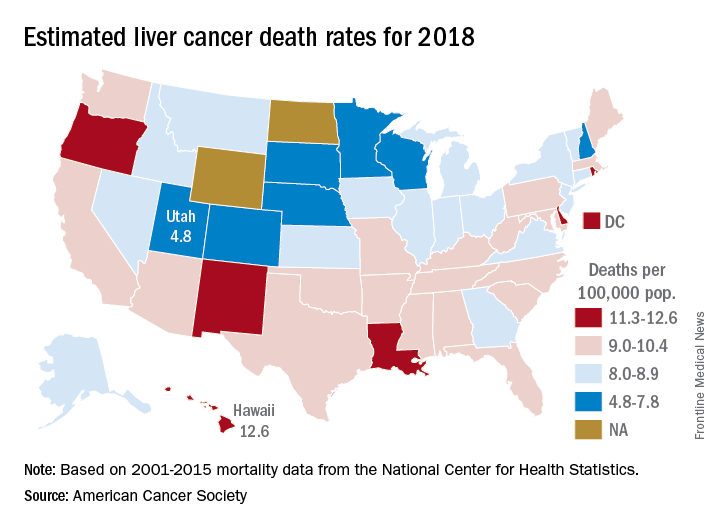
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.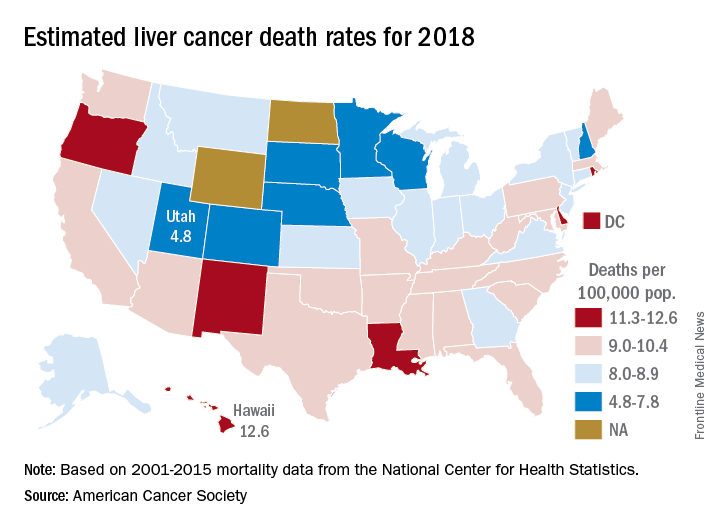
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.














