User login
Official Newspaper of the American College of Surgeons
Surgery may benefit elderly women with endometrial cancer
NATIONAL HARBOR, MD. – Surgery is a safe option for elderly women who have endometrial cancer, significantly extending life with a low rate of surgical complications, findings from a small study showed.
A review of 68 women aged 75-94 years found that those who underwent surgery lived about 2 years longer than those who didn’t, Dr. Eloise Chapman-Davis reported at a meeting sponsored by the AAGL.
"Age, multiple comorbidities, high-risk endometrial histology, and stage alone should not exclude elderly patients from surgical treatment options," said Dr. Chapman-Davis, a gynecologic oncologist at Tufts Medical Center, Boston. "Survival may be improved in patients with endometrial cancer who undergo surgery as a part of their treatment."
The women in the current study were treated for endometrial cancer from 2005 to 2012. The first analysis broke the cohort down into those who had surgery (55) and those who did not. Significantly more women in the surgery group were younger than 80 years (85% vs. 45% of the nonsurgery group).
Stage 3 cancer was present in 16% of the surgical group and in 8% of the nonsurgical group. Stage 4 cancer was present in 3% of the surgical group and 31% of the nonsurgical group.
There were no significant differences in baseline comorbidities, including hypertension, diabetes, and pulmonary and coronary artery disease.
Every woman in the nonsurgical group underwent chemotherapy and 46% had radiation. In the surgical group, 20% had radiation and 20%, chemotherapy.
Surgical management changed over the course of the study. The facility implemented robotic surgery in 2009; after 2011, only one patient had laparotomy. The oldest patient who underwent open surgery was 87 years; the oldest patient who had robotic surgery was 94 years.
The surgical group was divided into those who had open (36) and robotic hysterectomies (19). Node sampling was significantly greater in the open group for both pelvic (83% vs. 53%) and aortic nodes (61% vs. 5%).
Robotic surgery took significantly longer than open surgery (mean, 196 vs. 137 minutes). However, blood loss was significantly less in the robotic surgery group (113 vs. 287 mL). Four patients in the open group needed more than 2 U of blood, and one patient lost more than 1,000 mL of blood.
In the robotic group, there was one conversion to open surgery, one cardiac event, and one ileus. In the open group, there were six cardiac events and six cases of prolonged ileus. The mean length of stay was 2 days in the robotic group and 6 days in the open group – a significant difference.
Age did not significantly affect survival. By 3.5 years, 60% of those up to age 79 years and 60% of those 80 and older were still living. Treatment, however, did exert a significant effect. The mean survival of patients who had no surgery was 3 years, compared with about 4 years for those who did have surgery.
The study did not address any survival differences between open and robotic procedures.
Dr. Chapman-Davis said she had no relevant financial disclosures.
NATIONAL HARBOR, MD. – Surgery is a safe option for elderly women who have endometrial cancer, significantly extending life with a low rate of surgical complications, findings from a small study showed.
A review of 68 women aged 75-94 years found that those who underwent surgery lived about 2 years longer than those who didn’t, Dr. Eloise Chapman-Davis reported at a meeting sponsored by the AAGL.
"Age, multiple comorbidities, high-risk endometrial histology, and stage alone should not exclude elderly patients from surgical treatment options," said Dr. Chapman-Davis, a gynecologic oncologist at Tufts Medical Center, Boston. "Survival may be improved in patients with endometrial cancer who undergo surgery as a part of their treatment."
The women in the current study were treated for endometrial cancer from 2005 to 2012. The first analysis broke the cohort down into those who had surgery (55) and those who did not. Significantly more women in the surgery group were younger than 80 years (85% vs. 45% of the nonsurgery group).
Stage 3 cancer was present in 16% of the surgical group and in 8% of the nonsurgical group. Stage 4 cancer was present in 3% of the surgical group and 31% of the nonsurgical group.
There were no significant differences in baseline comorbidities, including hypertension, diabetes, and pulmonary and coronary artery disease.
Every woman in the nonsurgical group underwent chemotherapy and 46% had radiation. In the surgical group, 20% had radiation and 20%, chemotherapy.
Surgical management changed over the course of the study. The facility implemented robotic surgery in 2009; after 2011, only one patient had laparotomy. The oldest patient who underwent open surgery was 87 years; the oldest patient who had robotic surgery was 94 years.
The surgical group was divided into those who had open (36) and robotic hysterectomies (19). Node sampling was significantly greater in the open group for both pelvic (83% vs. 53%) and aortic nodes (61% vs. 5%).
Robotic surgery took significantly longer than open surgery (mean, 196 vs. 137 minutes). However, blood loss was significantly less in the robotic surgery group (113 vs. 287 mL). Four patients in the open group needed more than 2 U of blood, and one patient lost more than 1,000 mL of blood.
In the robotic group, there was one conversion to open surgery, one cardiac event, and one ileus. In the open group, there were six cardiac events and six cases of prolonged ileus. The mean length of stay was 2 days in the robotic group and 6 days in the open group – a significant difference.
Age did not significantly affect survival. By 3.5 years, 60% of those up to age 79 years and 60% of those 80 and older were still living. Treatment, however, did exert a significant effect. The mean survival of patients who had no surgery was 3 years, compared with about 4 years for those who did have surgery.
The study did not address any survival differences between open and robotic procedures.
Dr. Chapman-Davis said she had no relevant financial disclosures.
NATIONAL HARBOR, MD. – Surgery is a safe option for elderly women who have endometrial cancer, significantly extending life with a low rate of surgical complications, findings from a small study showed.
A review of 68 women aged 75-94 years found that those who underwent surgery lived about 2 years longer than those who didn’t, Dr. Eloise Chapman-Davis reported at a meeting sponsored by the AAGL.
"Age, multiple comorbidities, high-risk endometrial histology, and stage alone should not exclude elderly patients from surgical treatment options," said Dr. Chapman-Davis, a gynecologic oncologist at Tufts Medical Center, Boston. "Survival may be improved in patients with endometrial cancer who undergo surgery as a part of their treatment."
The women in the current study were treated for endometrial cancer from 2005 to 2012. The first analysis broke the cohort down into those who had surgery (55) and those who did not. Significantly more women in the surgery group were younger than 80 years (85% vs. 45% of the nonsurgery group).
Stage 3 cancer was present in 16% of the surgical group and in 8% of the nonsurgical group. Stage 4 cancer was present in 3% of the surgical group and 31% of the nonsurgical group.
There were no significant differences in baseline comorbidities, including hypertension, diabetes, and pulmonary and coronary artery disease.
Every woman in the nonsurgical group underwent chemotherapy and 46% had radiation. In the surgical group, 20% had radiation and 20%, chemotherapy.
Surgical management changed over the course of the study. The facility implemented robotic surgery in 2009; after 2011, only one patient had laparotomy. The oldest patient who underwent open surgery was 87 years; the oldest patient who had robotic surgery was 94 years.
The surgical group was divided into those who had open (36) and robotic hysterectomies (19). Node sampling was significantly greater in the open group for both pelvic (83% vs. 53%) and aortic nodes (61% vs. 5%).
Robotic surgery took significantly longer than open surgery (mean, 196 vs. 137 minutes). However, blood loss was significantly less in the robotic surgery group (113 vs. 287 mL). Four patients in the open group needed more than 2 U of blood, and one patient lost more than 1,000 mL of blood.
In the robotic group, there was one conversion to open surgery, one cardiac event, and one ileus. In the open group, there were six cardiac events and six cases of prolonged ileus. The mean length of stay was 2 days in the robotic group and 6 days in the open group – a significant difference.
Age did not significantly affect survival. By 3.5 years, 60% of those up to age 79 years and 60% of those 80 and older were still living. Treatment, however, did exert a significant effect. The mean survival of patients who had no surgery was 3 years, compared with about 4 years for those who did have surgery.
The study did not address any survival differences between open and robotic procedures.
Dr. Chapman-Davis said she had no relevant financial disclosures.
AT THE AAGL GLOBAL CONGRESS
Major finding: Elderly women who had surgery for endometrial cancer lived about 1 year longer than those who did not have surgery.
Data source: A retrospective study of 68 women.
Disclosures: Dr. Chapman-Davis said she had no relevant financial disclosures.
Lower urinary tract symptoms bother obese women more than obese men
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: On the Overactive Bladder Questionnaire, more obese women than obese men had higher scores in symptom severity (P = .036), concern (P = 0.002), and health-related quality of life (P =.028).
Data source: A study of baseline data from134 men and women who were planning to undergo laparoscopic-assisted gastric banding.
Disclosures: The researchers said they had no relevant financial disclosures.
Laparoscopic radical trachelectomy preserves fertility potential
WASHINGTON – Laparoscopic radical trachelectomy can be performed safely in well-selected patients with early cervical cancer who wish to preserve their fertility.
In a small retrospective analysis of 10 women, potential fertility was preserved in 8 women, Dr. Rene Pareja said at the AAGL Global Congress.
By 12 months, no pregnancies had been achieved, reported Dr. Pareja of the Instituto de Cancerología–Clinica las Américas (IDC) in Medellin, Colombia. However, conception should be possible for those who desire to have a child, he said at the meeting sponsored by AAGL.
Patients in the series were treated from 2009 to 2013. All had stage IB1 disease. In nine women, the lesion was less than 2 cm; in one woman, it was 3 cm. Half of the cancers were squamous, and the other half were adenocarcinomas.
All 10 patients underwent a minimally invasive radical trachelectomy. The mean surgical time was 240 minutes, with an estimated blood loss of 100 cc. There were no transfusions and no conversions to open surgery. One cystotomy was repaired laparoscopically. The mean hospital stay was 2 days.
Surgeons recovered a mean of 16 nodes from each patient (range, 10-24); none of these were positive. Four women had no residual disease. One had a positive endocervical margin on pathology; she underwent a hysterectomy. None of the patients required either chemotherapy or radiation therapy.
In addition to the hysterectomy, there were four postoperative complications: one necrosis of the right uterine cornua, one ureterovaginal fistula, and two lymphocysts.
At a mean follow-up of 12 months, there have been no cancer recurrences. One patient is attempting to conceive, although she has not yet done so.
The extant literature supports Dr. Pareja’s experience of laparoscopic radical trachelectomy. Since 2003, the procedure has been reported in 150 patients. Among these, there have been 38 pregnancies, 13 miscarriages, and 20 live births. Dr. Pareja did not say what percentage of women in these studies were attempting to conceive, however.
Five patients reported in the literature have had recurrent cancer and three have died, although Dr. Pareja did not mention whether these deaths were related to the cancers.
So far, the safety and obstetrical outcomes of his patients compare well with those reported in other forms of cervical cancer surgery. Among the 150 reported cases of laparoscopic radical trachelectomy, the relapse rate was 3.3% and death rate 2.9%. The total pregnancy rate was 25% and the delivery rate 13%.
Among the 1,088 reported cases of vaginal radical trachelectomy, there was a 4% relapse rate and 2.9% death rate. The total pregnancy rate was 24% and the delivery rate 28%.
Among the 485 reported cases of abdominal radical trachelectomy, the relapse rate was 3.8% and the death rate 0.4%. The pregnancy rate was 16% and the delivery rate 11%.
Dr. Pareja had no financial disclosures.
WASHINGTON – Laparoscopic radical trachelectomy can be performed safely in well-selected patients with early cervical cancer who wish to preserve their fertility.
In a small retrospective analysis of 10 women, potential fertility was preserved in 8 women, Dr. Rene Pareja said at the AAGL Global Congress.
By 12 months, no pregnancies had been achieved, reported Dr. Pareja of the Instituto de Cancerología–Clinica las Américas (IDC) in Medellin, Colombia. However, conception should be possible for those who desire to have a child, he said at the meeting sponsored by AAGL.
Patients in the series were treated from 2009 to 2013. All had stage IB1 disease. In nine women, the lesion was less than 2 cm; in one woman, it was 3 cm. Half of the cancers were squamous, and the other half were adenocarcinomas.
All 10 patients underwent a minimally invasive radical trachelectomy. The mean surgical time was 240 minutes, with an estimated blood loss of 100 cc. There were no transfusions and no conversions to open surgery. One cystotomy was repaired laparoscopically. The mean hospital stay was 2 days.
Surgeons recovered a mean of 16 nodes from each patient (range, 10-24); none of these were positive. Four women had no residual disease. One had a positive endocervical margin on pathology; she underwent a hysterectomy. None of the patients required either chemotherapy or radiation therapy.
In addition to the hysterectomy, there were four postoperative complications: one necrosis of the right uterine cornua, one ureterovaginal fistula, and two lymphocysts.
At a mean follow-up of 12 months, there have been no cancer recurrences. One patient is attempting to conceive, although she has not yet done so.
The extant literature supports Dr. Pareja’s experience of laparoscopic radical trachelectomy. Since 2003, the procedure has been reported in 150 patients. Among these, there have been 38 pregnancies, 13 miscarriages, and 20 live births. Dr. Pareja did not say what percentage of women in these studies were attempting to conceive, however.
Five patients reported in the literature have had recurrent cancer and three have died, although Dr. Pareja did not mention whether these deaths were related to the cancers.
So far, the safety and obstetrical outcomes of his patients compare well with those reported in other forms of cervical cancer surgery. Among the 150 reported cases of laparoscopic radical trachelectomy, the relapse rate was 3.3% and death rate 2.9%. The total pregnancy rate was 25% and the delivery rate 13%.
Among the 1,088 reported cases of vaginal radical trachelectomy, there was a 4% relapse rate and 2.9% death rate. The total pregnancy rate was 24% and the delivery rate 28%.
Among the 485 reported cases of abdominal radical trachelectomy, the relapse rate was 3.8% and the death rate 0.4%. The pregnancy rate was 16% and the delivery rate 11%.
Dr. Pareja had no financial disclosures.
WASHINGTON – Laparoscopic radical trachelectomy can be performed safely in well-selected patients with early cervical cancer who wish to preserve their fertility.
In a small retrospective analysis of 10 women, potential fertility was preserved in 8 women, Dr. Rene Pareja said at the AAGL Global Congress.
By 12 months, no pregnancies had been achieved, reported Dr. Pareja of the Instituto de Cancerología–Clinica las Américas (IDC) in Medellin, Colombia. However, conception should be possible for those who desire to have a child, he said at the meeting sponsored by AAGL.
Patients in the series were treated from 2009 to 2013. All had stage IB1 disease. In nine women, the lesion was less than 2 cm; in one woman, it was 3 cm. Half of the cancers were squamous, and the other half were adenocarcinomas.
All 10 patients underwent a minimally invasive radical trachelectomy. The mean surgical time was 240 minutes, with an estimated blood loss of 100 cc. There were no transfusions and no conversions to open surgery. One cystotomy was repaired laparoscopically. The mean hospital stay was 2 days.
Surgeons recovered a mean of 16 nodes from each patient (range, 10-24); none of these were positive. Four women had no residual disease. One had a positive endocervical margin on pathology; she underwent a hysterectomy. None of the patients required either chemotherapy or radiation therapy.
In addition to the hysterectomy, there were four postoperative complications: one necrosis of the right uterine cornua, one ureterovaginal fistula, and two lymphocysts.
At a mean follow-up of 12 months, there have been no cancer recurrences. One patient is attempting to conceive, although she has not yet done so.
The extant literature supports Dr. Pareja’s experience of laparoscopic radical trachelectomy. Since 2003, the procedure has been reported in 150 patients. Among these, there have been 38 pregnancies, 13 miscarriages, and 20 live births. Dr. Pareja did not say what percentage of women in these studies were attempting to conceive, however.
Five patients reported in the literature have had recurrent cancer and three have died, although Dr. Pareja did not mention whether these deaths were related to the cancers.
So far, the safety and obstetrical outcomes of his patients compare well with those reported in other forms of cervical cancer surgery. Among the 150 reported cases of laparoscopic radical trachelectomy, the relapse rate was 3.3% and death rate 2.9%. The total pregnancy rate was 25% and the delivery rate 13%.
Among the 1,088 reported cases of vaginal radical trachelectomy, there was a 4% relapse rate and 2.9% death rate. The total pregnancy rate was 24% and the delivery rate 28%.
Among the 485 reported cases of abdominal radical trachelectomy, the relapse rate was 3.8% and the death rate 0.4%. The pregnancy rate was 16% and the delivery rate 11%.
Dr. Pareja had no financial disclosures.
AT THE AAGL GLOBAL CONGRESS
Major finding: A laparoscopic radical trachelectomy preserved fertility in 8 of 10 women with early cervical cancer, with no recurrences at a mean follow-up of 12 months.
Data source: A retrospective study involving 10 women.
Disclosures: Dr. Pareja had no financial disclosures.
Application of estrogen cream before hysterectomy thickened tissue
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
AT THE AUGS ANNUAL MEETING
Major finding: On histological assessment, mean epithelial thickness among women in the estrogen group was increased by 1.8-fold while the muscularis thickness was increased by 2.7-fold.
Data source: Results from a study of 30 postmenopausal women who, 6 weeks prior to undergoing hysterectomy, were randomized to estrogen cream or placebo in an effort to determine the vaginal effects of estrogen.
Disclosures: The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
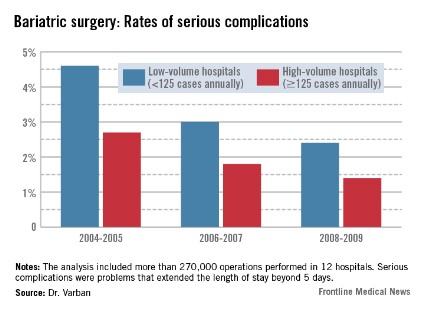
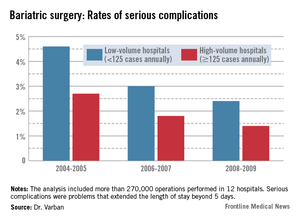
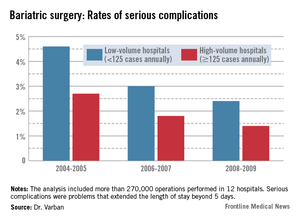
Complication gap narrows between low- and high-volume bariatric centers
WASHINGTON – Annual case volume appears to be falling out as a safety factor in bariatric surgery, Dr. Oliver Varban said at the annual clinical congress of the American College of Surgeons.
In the early days of the procedure, facilities that performed more than 125 operations each year had significantly better safety outcomes than did those performing fewer operations. But that difference is fading, particularly as laparoscopy continues to supplant open surgery, said Dr. Varban of the University of Michigan Health Systems, Ann Arbor.
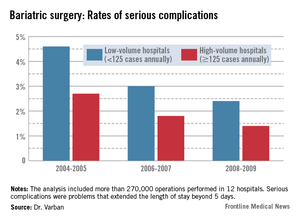
"Over time, safety is improving in both high- and low-volume centers, with lower rates of complications, morbidity, and mortality. The inverse relationship does still persist, but that effect is attenuating."
Dr. Varban conducted a review of more than 270,000 bariatric surgery procedures performed in 12 hospitals from 2004 to 2009. He separated the hospitals by annual case volume: 125 or more and less than 125 per year.
In each year, about two-thirds of the procedures were completed in high-volume hospitals. The type of surgery also varied over the study period. During 2004-2005, laparoscopic and open procedures were about equally common. By 2006-2007, laparoscopic operations made up 65% of all bariatric procedures, and that held steady through 2008-2009.
The type of procedure evolved as well, Dr. Varban noted. In 2004-2005, gastric banding comprised about 5% of the operations. By 2006-2007, that had risen to 20%, and by 2008-2009, the number was close to 30%.
In the first era, low-volume hospitals had significantly higher rates of any complication than did high-volume centers (9.3% vs. 6%). By 2006-2007, the difference had narrowed but was still statistically significant (7% vs. 4.8%). By 2008-2009, the difference was no longer significant (5.6% vs. 4.5%).
A multivariate analysis that controlled for type of surgery and patient demographics found a similar trend. The risk of any complication remained significantly elevated at low-volume centers during all three periods (odds ratio, 1.33 in 2004-2005; 1.35 in 2006-2007; and 1.21 in 2008-2009).
The pattern of serious complications (problems that extended the length of stay beyond 5 days) was similar, with a rate of 4.6% vs. 2.7% in the early era; 3% vs. 1.8% in the middle era; and 2.4% vs. 1.4% in the final era. The risk of serious complications was significantly higher in the low-volume group in every era (OR 1.35, 1.43, and 1.44, respectively).
The rates of reoperation were higher in low-volume centers in every era, and declined as time went on. However, the difference between low- and high-volume centers in terms of reoperation rates was nonsignificant at every time point (1.5% vs. 1.06%; 1% vs. 0.75%; 0.78% vs. 0.67%). Similarly, the adjusted odds ratios were nonsignificant (OR 1.22, 1.28, and 1.20).
Although overall the mortality rates were low and remained low, they declined significantly in both groups over the study period (from 0.22% vs. 0.1% and 0.09% vs. 0.04%). Only in the first era was the difference statistically significant, with an adjusted OR of 1.71.
Dr. Varban had no financial disclosures.
WASHINGTON – Annual case volume appears to be falling out as a safety factor in bariatric surgery, Dr. Oliver Varban said at the annual clinical congress of the American College of Surgeons.
In the early days of the procedure, facilities that performed more than 125 operations each year had significantly better safety outcomes than did those performing fewer operations. But that difference is fading, particularly as laparoscopy continues to supplant open surgery, said Dr. Varban of the University of Michigan Health Systems, Ann Arbor.
"Over time, safety is improving in both high- and low-volume centers, with lower rates of complications, morbidity, and mortality. The inverse relationship does still persist, but that effect is attenuating."
Dr. Varban conducted a review of more than 270,000 bariatric surgery procedures performed in 12 hospitals from 2004 to 2009. He separated the hospitals by annual case volume: 125 or more and less than 125 per year.
In each year, about two-thirds of the procedures were completed in high-volume hospitals. The type of surgery also varied over the study period. During 2004-2005, laparoscopic and open procedures were about equally common. By 2006-2007, laparoscopic operations made up 65% of all bariatric procedures, and that held steady through 2008-2009.
The type of procedure evolved as well, Dr. Varban noted. In 2004-2005, gastric banding comprised about 5% of the operations. By 2006-2007, that had risen to 20%, and by 2008-2009, the number was close to 30%.
In the first era, low-volume hospitals had significantly higher rates of any complication than did high-volume centers (9.3% vs. 6%). By 2006-2007, the difference had narrowed but was still statistically significant (7% vs. 4.8%). By 2008-2009, the difference was no longer significant (5.6% vs. 4.5%).
A multivariate analysis that controlled for type of surgery and patient demographics found a similar trend. The risk of any complication remained significantly elevated at low-volume centers during all three periods (odds ratio, 1.33 in 2004-2005; 1.35 in 2006-2007; and 1.21 in 2008-2009).
The pattern of serious complications (problems that extended the length of stay beyond 5 days) was similar, with a rate of 4.6% vs. 2.7% in the early era; 3% vs. 1.8% in the middle era; and 2.4% vs. 1.4% in the final era. The risk of serious complications was significantly higher in the low-volume group in every era (OR 1.35, 1.43, and 1.44, respectively).
The rates of reoperation were higher in low-volume centers in every era, and declined as time went on. However, the difference between low- and high-volume centers in terms of reoperation rates was nonsignificant at every time point (1.5% vs. 1.06%; 1% vs. 0.75%; 0.78% vs. 0.67%). Similarly, the adjusted odds ratios were nonsignificant (OR 1.22, 1.28, and 1.20).
Although overall the mortality rates were low and remained low, they declined significantly in both groups over the study period (from 0.22% vs. 0.1% and 0.09% vs. 0.04%). Only in the first era was the difference statistically significant, with an adjusted OR of 1.71.
Dr. Varban had no financial disclosures.
WASHINGTON – Annual case volume appears to be falling out as a safety factor in bariatric surgery, Dr. Oliver Varban said at the annual clinical congress of the American College of Surgeons.
In the early days of the procedure, facilities that performed more than 125 operations each year had significantly better safety outcomes than did those performing fewer operations. But that difference is fading, particularly as laparoscopy continues to supplant open surgery, said Dr. Varban of the University of Michigan Health Systems, Ann Arbor.
"Over time, safety is improving in both high- and low-volume centers, with lower rates of complications, morbidity, and mortality. The inverse relationship does still persist, but that effect is attenuating."
Dr. Varban conducted a review of more than 270,000 bariatric surgery procedures performed in 12 hospitals from 2004 to 2009. He separated the hospitals by annual case volume: 125 or more and less than 125 per year.
In each year, about two-thirds of the procedures were completed in high-volume hospitals. The type of surgery also varied over the study period. During 2004-2005, laparoscopic and open procedures were about equally common. By 2006-2007, laparoscopic operations made up 65% of all bariatric procedures, and that held steady through 2008-2009.
The type of procedure evolved as well, Dr. Varban noted. In 2004-2005, gastric banding comprised about 5% of the operations. By 2006-2007, that had risen to 20%, and by 2008-2009, the number was close to 30%.
In the first era, low-volume hospitals had significantly higher rates of any complication than did high-volume centers (9.3% vs. 6%). By 2006-2007, the difference had narrowed but was still statistically significant (7% vs. 4.8%). By 2008-2009, the difference was no longer significant (5.6% vs. 4.5%).
A multivariate analysis that controlled for type of surgery and patient demographics found a similar trend. The risk of any complication remained significantly elevated at low-volume centers during all three periods (odds ratio, 1.33 in 2004-2005; 1.35 in 2006-2007; and 1.21 in 2008-2009).
The pattern of serious complications (problems that extended the length of stay beyond 5 days) was similar, with a rate of 4.6% vs. 2.7% in the early era; 3% vs. 1.8% in the middle era; and 2.4% vs. 1.4% in the final era. The risk of serious complications was significantly higher in the low-volume group in every era (OR 1.35, 1.43, and 1.44, respectively).
The rates of reoperation were higher in low-volume centers in every era, and declined as time went on. However, the difference between low- and high-volume centers in terms of reoperation rates was nonsignificant at every time point (1.5% vs. 1.06%; 1% vs. 0.75%; 0.78% vs. 0.67%). Similarly, the adjusted odds ratios were nonsignificant (OR 1.22, 1.28, and 1.20).
Although overall the mortality rates were low and remained low, they declined significantly in both groups over the study period (from 0.22% vs. 0.1% and 0.09% vs. 0.04%). Only in the first era was the difference statistically significant, with an adjusted OR of 1.71.
Dr. Varban had no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: From 2004 to 2009, the rates of serious complications, reoperation, and mortality improved in low-volume hospitals, bringing their results closer to those seen in high-volume centers.
Data source: The study included data on more than 270,000 bariatric surgical procedures.
Disclosures: Dr. Varban had no financial disclosures.
Fistula risk quadrupled with hyperthermia during pancreaticoduodenectomy
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ASA ANNUAL MEETING
Major finding: The likelihood of postoperative pancreatic fistula quadrupled in patients with a body temperature higher than 99.5 degrees F at the end of pancreaticoduodenectomy.
Data source: Retrospective study of 123 patients undergoing elective pancreaticoduodenectomy at one hospital.
Disclosures: Dr. Tanioku reported having no financial disclosures.
Simulations may improve intraoperative handoffs
SAN FRANCISCO – A 1-day course with simulated intraoperative handoffs improved the rate of failed communications from 30% before the course to 17% immediately after the course, with a further improvement 1 year later to a 13% failure rate in a study of 10 anesthesiology residents.
The course combined simulation-based education, which has been used previously to train residents on postoperative handoffs, and deliberate practice, an educational strategy that has been used previously to teach technical skills to residents. Each resident in the study performed a simulated intraoperative handoff, followed by a debriefing with the whole group and individual feedback on the handoff performance. Participants together discussed barriers to effective communication and created an intraoperative handoff checklist. Each resident then repeated a simulated handoff to practice with the checklist.
One year later, 7 of the 10 residents did another simulated intraoperative handoff that was recorded on video and scored by trained raters using a handoff assessment tool to characterize the type and frequency of communication failures.
Before the course, none of the 10 residents knew the Joint Commission definition of a handoff, and none knew that patient handoff communication was a patient safety goal of the Joint Commission. A year later, all seven residents could accurately define the Joint Commission goal, Dr. Erin W. Pukenas reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
At the beginning of the course, residents had set individual communication goals for handoffs. Forty-six percent said they wanted to develop a more systematic approach to their handoffs, and 31% wanted to be more thorough in their handoffs. A year later, all residents said they had met or exceeded their goals, reported Dr. Pukenas of Rowan University, Camden, N.J.
The study was the first to assess retention of knowledge and skills 1 year after the course was added to the curriculum, she said.
Investigators may next study the effects of simulation-based handoff education and deliberate practice on handoff communications in clinical settings, she said.
The Accreditation Council for Graduate Medical Education requires handoff training for all medical residents.
Dr. Pukenas reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A 1-day course with simulated intraoperative handoffs improved the rate of failed communications from 30% before the course to 17% immediately after the course, with a further improvement 1 year later to a 13% failure rate in a study of 10 anesthesiology residents.
The course combined simulation-based education, which has been used previously to train residents on postoperative handoffs, and deliberate practice, an educational strategy that has been used previously to teach technical skills to residents. Each resident in the study performed a simulated intraoperative handoff, followed by a debriefing with the whole group and individual feedback on the handoff performance. Participants together discussed barriers to effective communication and created an intraoperative handoff checklist. Each resident then repeated a simulated handoff to practice with the checklist.
One year later, 7 of the 10 residents did another simulated intraoperative handoff that was recorded on video and scored by trained raters using a handoff assessment tool to characterize the type and frequency of communication failures.
Before the course, none of the 10 residents knew the Joint Commission definition of a handoff, and none knew that patient handoff communication was a patient safety goal of the Joint Commission. A year later, all seven residents could accurately define the Joint Commission goal, Dr. Erin W. Pukenas reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
At the beginning of the course, residents had set individual communication goals for handoffs. Forty-six percent said they wanted to develop a more systematic approach to their handoffs, and 31% wanted to be more thorough in their handoffs. A year later, all residents said they had met or exceeded their goals, reported Dr. Pukenas of Rowan University, Camden, N.J.
The study was the first to assess retention of knowledge and skills 1 year after the course was added to the curriculum, she said.
Investigators may next study the effects of simulation-based handoff education and deliberate practice on handoff communications in clinical settings, she said.
The Accreditation Council for Graduate Medical Education requires handoff training for all medical residents.
Dr. Pukenas reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A 1-day course with simulated intraoperative handoffs improved the rate of failed communications from 30% before the course to 17% immediately after the course, with a further improvement 1 year later to a 13% failure rate in a study of 10 anesthesiology residents.
The course combined simulation-based education, which has been used previously to train residents on postoperative handoffs, and deliberate practice, an educational strategy that has been used previously to teach technical skills to residents. Each resident in the study performed a simulated intraoperative handoff, followed by a debriefing with the whole group and individual feedback on the handoff performance. Participants together discussed barriers to effective communication and created an intraoperative handoff checklist. Each resident then repeated a simulated handoff to practice with the checklist.
One year later, 7 of the 10 residents did another simulated intraoperative handoff that was recorded on video and scored by trained raters using a handoff assessment tool to characterize the type and frequency of communication failures.
Before the course, none of the 10 residents knew the Joint Commission definition of a handoff, and none knew that patient handoff communication was a patient safety goal of the Joint Commission. A year later, all seven residents could accurately define the Joint Commission goal, Dr. Erin W. Pukenas reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
At the beginning of the course, residents had set individual communication goals for handoffs. Forty-six percent said they wanted to develop a more systematic approach to their handoffs, and 31% wanted to be more thorough in their handoffs. A year later, all residents said they had met or exceeded their goals, reported Dr. Pukenas of Rowan University, Camden, N.J.
The study was the first to assess retention of knowledge and skills 1 year after the course was added to the curriculum, she said.
Investigators may next study the effects of simulation-based handoff education and deliberate practice on handoff communications in clinical settings, she said.
The Accreditation Council for Graduate Medical Education requires handoff training for all medical residents.
Dr. Pukenas reported having no relevant financial disclosures.
On Twitter @sherryboschert
AT THE ASA ANNUAL MEETING
Major finding: The rate of communication failures during simulated intraoperative handoffs decreased from 30% before the course to 17% at course completion and to 13% a year later.
Data source: A prospective study of 10 residents who took a 1-day course on intraoperative handoffs that combined simulations and deliberate practice techniques, 7 of whom repeated a simulated handoff a year later.
Disclosures: Dr. Pukenas reported having no relevant financial disclosures.
Single-incision sling may help stress urinary incontinence
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
AT THE AAGL GLOBAL CONGRESS
Major finding: After receiving a single-incision incontinence sling, 90% of women had significant improvements in clinical and quality of life measures related to stress urinary incontinence.
Data source: A prospective study of 113 women.
Disclosures: Coloplast sponsored the study. Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
Bariatric surgery benefits in type 2 diabetes linked to disease duration
MELBOURNE – The benefits of bariatric surgery in people with type 2 diabetes are significantly reduced with longer disease duration at the time of surgery and with time since surgery, a long-running, prospective, controlled study has found.
The Swedish Obese Subjects study showed that 72% of surgery patients achieved remission at 2 years after treatment, compared with 16% of control patients.
Furthermore, 15 years after surgery, 31% of the surgery patients remained in remission, compared to 7% of control patients, according to data presented at the International Diabetes Federation world congress.
When stratified by disease duration at baseline, newly diagnosed patients maintained significantly higher remission rates at 2, 10 and 15 years’ follow-up (roughly 94%, 60%, and 47%, respectively) than did those who had had diabetes for more than 3 years at baseline (about 39%, 12%, and 9%).
These data came from the SOS (Swedish Obese Subjects) study, a nonrandomized, prospective, observational study involving 2,010 obese subjects who underwent bariatric surgery in 1987-2001, when they were 37-60 years old. A total of 68% of the bariatric surgery recipients had vertical band gastroplasty, 19% underwent gastric banding, and 13% had a Roux en-Y gastric bypass. They were extensively matched by 18 variables to 2,037 obese controls. The SOS study is being conducted at 25 surgical departments and 480 primary care clinics across Sweden. Follow-up is ongoing.
There were 343 individuals with type 2 diabetes in the surgical group and 260 in the control group, enabling a secondary analysis of the impact of bariatric surgery in type 2 diabetes.
Presenter Markku Peltonen said that although bariatric surgery achieves impressive results in the short-term, there is considerable relapse in the longer term.
"It’s typical of bariatric surgery that you achieve the greatest weight loss initially, after 2 years, then there is a slow regain again and this was observed in this study," said Dr. Peltonen, director of the department of chronic disease prevention at the National Institute for Health and Welfare, Helsinki.
"Even in the long term, they are doing much better than the controls who were treated with traditional weight management means," he said in an interview.
This also extended to the microvascular and macrovascular complications of diabetes, with the study showing a significant 47% lower incidence of complications in the surgery group, compared with the control group.
However, these benefits were also attenuated by disease duration. Patients who had had diabetes for more than 3 years and were treated with surgery showed no significant differences in diabetes complication rates, compared with the patients given medical care only.
Dr. Peltonen said he was surprised by the degree of impact that disease duration had on the outcomes of surgery.
"Somehow the expectation would be that we would see an effect even in those people with long diabetes duration, because they have a serious, advanced disease but it looks like, based on our results, that maybe it’s so that the disease has advanced for so long that bariatric surgery cannot reverse that development."
Session chair John Dixon said the SOS study represented the pinnacle of long-term data for bariatric surgery, and offered impressive insights.
"The fact that 31% of these patients are still in remission from diabetes some 15 years down the track is extraordinary, because we know the deterioration of beta cells is significant and this group has held it off for a long time," said Dr. Dixon, head of clinical obesity research at the Baker IDI Heart and Diabetes Institute in Melbourne.
Dr. Dixon said the finding that patients treated early fared better and had a reduction in long-term complications was also a very important clinical finding, suggesting that bariatric surgery should be considered earlier in obese patients not getting good control with conventional therapy.
SOS was supported by the Swedish Research Council, the Swedish Foundation for Strategic Research, and the Swedish government. Some study investigators authors had received paid lectureships, held stock in, or were on the advisory boards for pharmaceutical companies.
MELBOURNE – The benefits of bariatric surgery in people with type 2 diabetes are significantly reduced with longer disease duration at the time of surgery and with time since surgery, a long-running, prospective, controlled study has found.
The Swedish Obese Subjects study showed that 72% of surgery patients achieved remission at 2 years after treatment, compared with 16% of control patients.
Furthermore, 15 years after surgery, 31% of the surgery patients remained in remission, compared to 7% of control patients, according to data presented at the International Diabetes Federation world congress.
When stratified by disease duration at baseline, newly diagnosed patients maintained significantly higher remission rates at 2, 10 and 15 years’ follow-up (roughly 94%, 60%, and 47%, respectively) than did those who had had diabetes for more than 3 years at baseline (about 39%, 12%, and 9%).
These data came from the SOS (Swedish Obese Subjects) study, a nonrandomized, prospective, observational study involving 2,010 obese subjects who underwent bariatric surgery in 1987-2001, when they were 37-60 years old. A total of 68% of the bariatric surgery recipients had vertical band gastroplasty, 19% underwent gastric banding, and 13% had a Roux en-Y gastric bypass. They were extensively matched by 18 variables to 2,037 obese controls. The SOS study is being conducted at 25 surgical departments and 480 primary care clinics across Sweden. Follow-up is ongoing.
There were 343 individuals with type 2 diabetes in the surgical group and 260 in the control group, enabling a secondary analysis of the impact of bariatric surgery in type 2 diabetes.
Presenter Markku Peltonen said that although bariatric surgery achieves impressive results in the short-term, there is considerable relapse in the longer term.
"It’s typical of bariatric surgery that you achieve the greatest weight loss initially, after 2 years, then there is a slow regain again and this was observed in this study," said Dr. Peltonen, director of the department of chronic disease prevention at the National Institute for Health and Welfare, Helsinki.
"Even in the long term, they are doing much better than the controls who were treated with traditional weight management means," he said in an interview.
This also extended to the microvascular and macrovascular complications of diabetes, with the study showing a significant 47% lower incidence of complications in the surgery group, compared with the control group.
However, these benefits were also attenuated by disease duration. Patients who had had diabetes for more than 3 years and were treated with surgery showed no significant differences in diabetes complication rates, compared with the patients given medical care only.
Dr. Peltonen said he was surprised by the degree of impact that disease duration had on the outcomes of surgery.
"Somehow the expectation would be that we would see an effect even in those people with long diabetes duration, because they have a serious, advanced disease but it looks like, based on our results, that maybe it’s so that the disease has advanced for so long that bariatric surgery cannot reverse that development."
Session chair John Dixon said the SOS study represented the pinnacle of long-term data for bariatric surgery, and offered impressive insights.
"The fact that 31% of these patients are still in remission from diabetes some 15 years down the track is extraordinary, because we know the deterioration of beta cells is significant and this group has held it off for a long time," said Dr. Dixon, head of clinical obesity research at the Baker IDI Heart and Diabetes Institute in Melbourne.
Dr. Dixon said the finding that patients treated early fared better and had a reduction in long-term complications was also a very important clinical finding, suggesting that bariatric surgery should be considered earlier in obese patients not getting good control with conventional therapy.
SOS was supported by the Swedish Research Council, the Swedish Foundation for Strategic Research, and the Swedish government. Some study investigators authors had received paid lectureships, held stock in, or were on the advisory boards for pharmaceutical companies.
MELBOURNE – The benefits of bariatric surgery in people with type 2 diabetes are significantly reduced with longer disease duration at the time of surgery and with time since surgery, a long-running, prospective, controlled study has found.
The Swedish Obese Subjects study showed that 72% of surgery patients achieved remission at 2 years after treatment, compared with 16% of control patients.
Furthermore, 15 years after surgery, 31% of the surgery patients remained in remission, compared to 7% of control patients, according to data presented at the International Diabetes Federation world congress.
When stratified by disease duration at baseline, newly diagnosed patients maintained significantly higher remission rates at 2, 10 and 15 years’ follow-up (roughly 94%, 60%, and 47%, respectively) than did those who had had diabetes for more than 3 years at baseline (about 39%, 12%, and 9%).
These data came from the SOS (Swedish Obese Subjects) study, a nonrandomized, prospective, observational study involving 2,010 obese subjects who underwent bariatric surgery in 1987-2001, when they were 37-60 years old. A total of 68% of the bariatric surgery recipients had vertical band gastroplasty, 19% underwent gastric banding, and 13% had a Roux en-Y gastric bypass. They were extensively matched by 18 variables to 2,037 obese controls. The SOS study is being conducted at 25 surgical departments and 480 primary care clinics across Sweden. Follow-up is ongoing.
There were 343 individuals with type 2 diabetes in the surgical group and 260 in the control group, enabling a secondary analysis of the impact of bariatric surgery in type 2 diabetes.
Presenter Markku Peltonen said that although bariatric surgery achieves impressive results in the short-term, there is considerable relapse in the longer term.
"It’s typical of bariatric surgery that you achieve the greatest weight loss initially, after 2 years, then there is a slow regain again and this was observed in this study," said Dr. Peltonen, director of the department of chronic disease prevention at the National Institute for Health and Welfare, Helsinki.
"Even in the long term, they are doing much better than the controls who were treated with traditional weight management means," he said in an interview.
This also extended to the microvascular and macrovascular complications of diabetes, with the study showing a significant 47% lower incidence of complications in the surgery group, compared with the control group.
However, these benefits were also attenuated by disease duration. Patients who had had diabetes for more than 3 years and were treated with surgery showed no significant differences in diabetes complication rates, compared with the patients given medical care only.
Dr. Peltonen said he was surprised by the degree of impact that disease duration had on the outcomes of surgery.
"Somehow the expectation would be that we would see an effect even in those people with long diabetes duration, because they have a serious, advanced disease but it looks like, based on our results, that maybe it’s so that the disease has advanced for so long that bariatric surgery cannot reverse that development."
Session chair John Dixon said the SOS study represented the pinnacle of long-term data for bariatric surgery, and offered impressive insights.
"The fact that 31% of these patients are still in remission from diabetes some 15 years down the track is extraordinary, because we know the deterioration of beta cells is significant and this group has held it off for a long time," said Dr. Dixon, head of clinical obesity research at the Baker IDI Heart and Diabetes Institute in Melbourne.
Dr. Dixon said the finding that patients treated early fared better and had a reduction in long-term complications was also a very important clinical finding, suggesting that bariatric surgery should be considered earlier in obese patients not getting good control with conventional therapy.
SOS was supported by the Swedish Research Council, the Swedish Foundation for Strategic Research, and the Swedish government. Some study investigators authors had received paid lectureships, held stock in, or were on the advisory boards for pharmaceutical companies.
FROM THE WORLD DIABETES CONGRESS
Major finding: Type 2 diabetes remission persisted after 2 and 15 years in 72% and 31% of bariatric surgery patients, vs. 16% and 7% of matched control patients. Those with newly diagnosed disease at baseline maintained significantly higher remission rates at 2 and 15 years’ follow-up (94% and 47%) than did those who had had diabetes for more than 3 years (39% and 9%).
Data source: A subanalysis of the Swedish Obese Subjects study, which included 343 type 2 diabetes patients who underwent bariatric surgery in 1987-2001 and 260 matched control patients.
Disclosures: SOS was supported by the Swedish Research Council, the Swedish Foundation for Strategic Research, and the Swedish government. Some of the investigators declared paid lectureships, stock ownership, and board membership in pharmaceutical companies.
Point/Counterpoint – Are SCIP measures efficacious?
POINT: SCIP is both efficacious and effective.
The Surgical Care Improvement Project (SCIP) was a national campaign that set out to reduce surgical mortality and morbidity by 25% by 2010 through recommendations in targeted areas: wound infections, perioperative MIs, and venous thromboembolism. The recommendations have become pay-for-performance measures. There are seven in the area of infectious disease to reduce surgical site infections. There is one measure for reducing perioperative MI: Continue beta-blockers (for patients who are on them) in the perioperative period. For venous thromboembolism prevention, give prophylaxis within 24 hours before to 24 hours after surgery.
It’s key to understand the difference between efficacy and effectiveness. I think we would all agree that the SCIP measures have efficacy. Efficacy trials determine whether an intervention produces the expected result under ideal circumstances. Effectiveness trials measure the degree of beneficial effect under "real world" clinical conditions. The problem with effectiveness trials is that those real-world conditions may change the effect, or they might just change the ability to measure the effect.
I believe that the SCIP measures have proven efficacy because they all are based upon randomized controlled trials that were identified by systematic reviews amenable to meta-analysis. All of these measures are Level 1 recommendations, based on the highest forms of evidence. The studies that Dr. Barash uses to criticize SCIP measures are cohort studies. They do not randomize. There may be unknown confounding variables.
There have been effectiveness trials that show that the SCIP measures do work. One showed a 27% decrease in surgical site infections, another showed a 62% decrease in surgical site infections, and a third showed a 39% decrease in surgical site infections.
Perhaps the strongest endorsement of efficacy of the SCIP measures comes from Dr. Kaveh G. Shojania, who has written several reviews of the efficacy of medical interventions. This guy is like Mikey from the old Life cereal commercials ... he hates everything. He said there were 11 patient safety practices rated most highly in terms of strength of the evidence, and 3 are SCIP measures: appropriate use of prophylaxis to prevent venous thromboembolism in patients at risk, use of perioperative beta-blockers in appropriate patients, and appropriate use of antibiotic prophylaxis in surgical patients (AHRQ Publication No. 01-E058).
Several trials published by pretty good researchers in reputable journals show a lack of effectiveness of SCIP measures. Even those researchers admit to the efficacy of SCIP measures. The lead investigator of the best effectiveness trial, a retrospective cohort study, wrote, "There are several explanations as to why we did not observe an association between timely antibiotic administration and surgical site infection (SSI). The first is that timely antibiotic administration does not diminish SSI risk. This is an unlikely interpretation. There are numerous randomized controlled trials and observational studies that demonstrate the efficacy of prophylactic antibiotics in reducing SSI for various surgical procedures" (Ann. Surg. 2011;254:494-9).
A separate retrospective cohort study showed a decrease in surgical site infection only if two or more SCIP recommendations were followed (JAMA 2010;303:2479-85). Shocking – if you give the wrong antibiotic at the right time, it might not work.
Another retrospective cohort study found no association with adjusted complications and SCIP compliance. Hospitals in the lowest compliance group had patients in lower-income ZIP codes and lower unadjusted complication rates. So, poor people go home and don’t come back, perhaps because of payment considerations. The study didn’t have enough patients; it also used measures that don’t apply to SCIP (Arch. Surg. 2010;145:999-1004).
SCIP did not design these measures for pay-for-performance programs. The intent was to decrease perioperative complications by 25% by 2010. When you start changing the baseline with pay-for-performance, it doesn’t work. In a study by Hawkins et al., the authors tested the hypothesis that documented compliance with antibiotic prophylaxis guidelines on a pediatric surgery service does not reflect adherence to guidelines as intended. In a 7-week observational study of elective pediatric surgical cases, adherence was evaluated for appropriate administration, type, timing, weight-based dosing, and redosing of antibiotics. Prophylactic antibiotics were administered appropriately in 141 of 143 cases (99%). Of 100 cases in which antibiotic prophylaxis was indicated, compliance was documented in 100% of cases in the electronic medical record; but only 48% of cases adhered to all five guidelines. Lack of adherence was due primarily to dosing or timing errors.
The SCIP measures, however, are based on best evidence. They are tightly linked with the desired outcomes. They are measurable and effectible, as demonstrated in multiple randomized controlled trials. Studies of effectiveness have had variable results due to methodological flaws.
Dr. Lagasse is a professor of anesthesiology and director of quality management at the Yale School of Medicine, New Haven, Conn. He is on the steering committee for the Surgical Care Improvement Project. He reported having no financial disclosures.
COUNTERPOINT: Studies have not shown effectiveness.
When it was created, SCIP did not reflect reality. SCIP started at the U.S. Department of Veterans Affairs, which conducted a 10-year study. They found a 25% relative risk reduction, but that was only a 0.8% absolute risk reduction for the incidence of complications, a drop from about 3.1% to about 2.3% (Arch. Surg. 2002;137:20-27).
It would be great to have randomized controlled trials on the effectiveness of SCIP, but it’s not happening. We’re going to have to go by high-fidelity observational trials, which according to a number of researchers in the field have the same impact as randomized controlled trials.
One study of 35,543 patients in 44 hospitals found a whopping 27% reduction in surgical site infections, but that was only a 0.6% absolute reduction, from about 2.5% to about 1.9% (Am. J. Surg. 2005;190:9-15). There was no significant difference between groups.
Another study showed improved compliance with SCIP measures, but no change in surgical site infection rate (Dis. Colon Rectum 2010;53:24-30). This is the theme in study after study after study.
A 2008 study enrolled 9,195 patients undergoing colorectal, orthopedic, or vascular surgery and looked at SCIP compliance vs. surgical site infection. The SCIP rate correlated with the hospital case mix. If you look at the SCIP rate in terms of antibiotic timing, SCIP is not significant. The study basically showed that variables other than timely antibiotic administration are affecting surgical site infection rates (J. Am. Coll. Surg. 2008;206:814-19).
Hospital performance on process measures may not be a good marker of surgical site infection or the outcome we’re looking at, according to another study, which reported that unmeasured effects may have a larger impact than the measured effects (Health Serv. Res. 2008;43:1464-84).
There is a randomized controlled trial that randomized patients to strict control with the SCIP measures or routine treatment at the hospital. The SCIP-treated patients had nearly twice the incidence of surgical site infections as the patients receiving standard treatment. The authors concluded that combining each of the SCIP factors into one big category doesn’t necessarily work (Arch. Surg. 2011;146:263-9).
Should we be evaluating outcome measures with performance measures (e.g., percent timely antibiotic administration) to determine whether they work or not? One editorial evaluated eight articles with data on 31,448 patients, looking just at antibiotic administration within 1 hour of surgery, a SCIP measure. It found a higher infection rate if antibiotics were administered within 30 minutes of incision (JAMA 2010;303:2527-2528).
There was no significant difference in another study between standard of care and SCIP for venous thromboembolism (Am. J. Surg. 2012;204:591-97). The authors wrote that there is no convincing evidence that improvements in compliance are associated with better outcomes. We see this time and time again.
When people find that SCIP is not working, they turn to other measures to reduce surgical site infection. The Comprehensive Unit-based Safety Program (CUSP) is targeted at a specific problem that a specific hospital is having in managing infections. It’s not coming from Washington; it’s based at the hospital. One study showed that following CUSP, there was a significant reduction in surgical site infections despite the fact that previous to that there was 95% compliance with SCIP standards (J. Am. Coll. Surg. 2012;215:193-200). SCIP was working, but it wasn’t affecting outcome.
Dr. Lagasse and I interpret one key study very differently. He abstracts a sentence from a Limitations section of the study and makes a sweeping generalization out of context. But the study showed no relationship between facility adherence to SCIP and the surgical site infection rate. The authors concluded, "Policies regarding continued SCIP measurement and reporting should be reassessed" (Ann. Surg. 2011;254:494-99).
The largest SCIP study to date from a single entity involved 32,459 patients in the Veterans Affairs medical system. Overall, antibiotics were administered within 28 minutes of surgical incision. Once they adjusted for confounders, they found no significant relationship between surgical site infection and the SCIP measures (JAMA 2013;148:649-57). No one has proven that giving antibiotics within 60 minutes of surgical incision gives you a lower infection rate.
SCIP measures divert resources and divert clinical care. They obscure the nuances of care. They may harm the hospital and the provider, and they raise unnecessary legal risk if an antibiotic is not given within 60 minutes of incision.
Dr. Barash is a professor of anesthesiology at Yale University, New Haven, Conn. He reported having no financial disclosures.
These are excerpts from a debate at the annual meeting of the American Society of Anesthesiologists.
POINT: SCIP is both efficacious and effective.
The Surgical Care Improvement Project (SCIP) was a national campaign that set out to reduce surgical mortality and morbidity by 25% by 2010 through recommendations in targeted areas: wound infections, perioperative MIs, and venous thromboembolism. The recommendations have become pay-for-performance measures. There are seven in the area of infectious disease to reduce surgical site infections. There is one measure for reducing perioperative MI: Continue beta-blockers (for patients who are on them) in the perioperative period. For venous thromboembolism prevention, give prophylaxis within 24 hours before to 24 hours after surgery.
It’s key to understand the difference between efficacy and effectiveness. I think we would all agree that the SCIP measures have efficacy. Efficacy trials determine whether an intervention produces the expected result under ideal circumstances. Effectiveness trials measure the degree of beneficial effect under "real world" clinical conditions. The problem with effectiveness trials is that those real-world conditions may change the effect, or they might just change the ability to measure the effect.
I believe that the SCIP measures have proven efficacy because they all are based upon randomized controlled trials that were identified by systematic reviews amenable to meta-analysis. All of these measures are Level 1 recommendations, based on the highest forms of evidence. The studies that Dr. Barash uses to criticize SCIP measures are cohort studies. They do not randomize. There may be unknown confounding variables.
There have been effectiveness trials that show that the SCIP measures do work. One showed a 27% decrease in surgical site infections, another showed a 62% decrease in surgical site infections, and a third showed a 39% decrease in surgical site infections.
Perhaps the strongest endorsement of efficacy of the SCIP measures comes from Dr. Kaveh G. Shojania, who has written several reviews of the efficacy of medical interventions. This guy is like Mikey from the old Life cereal commercials ... he hates everything. He said there were 11 patient safety practices rated most highly in terms of strength of the evidence, and 3 are SCIP measures: appropriate use of prophylaxis to prevent venous thromboembolism in patients at risk, use of perioperative beta-blockers in appropriate patients, and appropriate use of antibiotic prophylaxis in surgical patients (AHRQ Publication No. 01-E058).
Several trials published by pretty good researchers in reputable journals show a lack of effectiveness of SCIP measures. Even those researchers admit to the efficacy of SCIP measures. The lead investigator of the best effectiveness trial, a retrospective cohort study, wrote, "There are several explanations as to why we did not observe an association between timely antibiotic administration and surgical site infection (SSI). The first is that timely antibiotic administration does not diminish SSI risk. This is an unlikely interpretation. There are numerous randomized controlled trials and observational studies that demonstrate the efficacy of prophylactic antibiotics in reducing SSI for various surgical procedures" (Ann. Surg. 2011;254:494-9).
A separate retrospective cohort study showed a decrease in surgical site infection only if two or more SCIP recommendations were followed (JAMA 2010;303:2479-85). Shocking – if you give the wrong antibiotic at the right time, it might not work.
Another retrospective cohort study found no association with adjusted complications and SCIP compliance. Hospitals in the lowest compliance group had patients in lower-income ZIP codes and lower unadjusted complication rates. So, poor people go home and don’t come back, perhaps because of payment considerations. The study didn’t have enough patients; it also used measures that don’t apply to SCIP (Arch. Surg. 2010;145:999-1004).
SCIP did not design these measures for pay-for-performance programs. The intent was to decrease perioperative complications by 25% by 2010. When you start changing the baseline with pay-for-performance, it doesn’t work. In a study by Hawkins et al., the authors tested the hypothesis that documented compliance with antibiotic prophylaxis guidelines on a pediatric surgery service does not reflect adherence to guidelines as intended. In a 7-week observational study of elective pediatric surgical cases, adherence was evaluated for appropriate administration, type, timing, weight-based dosing, and redosing of antibiotics. Prophylactic antibiotics were administered appropriately in 141 of 143 cases (99%). Of 100 cases in which antibiotic prophylaxis was indicated, compliance was documented in 100% of cases in the electronic medical record; but only 48% of cases adhered to all five guidelines. Lack of adherence was due primarily to dosing or timing errors.
The SCIP measures, however, are based on best evidence. They are tightly linked with the desired outcomes. They are measurable and effectible, as demonstrated in multiple randomized controlled trials. Studies of effectiveness have had variable results due to methodological flaws.
Dr. Lagasse is a professor of anesthesiology and director of quality management at the Yale School of Medicine, New Haven, Conn. He is on the steering committee for the Surgical Care Improvement Project. He reported having no financial disclosures.
COUNTERPOINT: Studies have not shown effectiveness.
When it was created, SCIP did not reflect reality. SCIP started at the U.S. Department of Veterans Affairs, which conducted a 10-year study. They found a 25% relative risk reduction, but that was only a 0.8% absolute risk reduction for the incidence of complications, a drop from about 3.1% to about 2.3% (Arch. Surg. 2002;137:20-27).
It would be great to have randomized controlled trials on the effectiveness of SCIP, but it’s not happening. We’re going to have to go by high-fidelity observational trials, which according to a number of researchers in the field have the same impact as randomized controlled trials.
One study of 35,543 patients in 44 hospitals found a whopping 27% reduction in surgical site infections, but that was only a 0.6% absolute reduction, from about 2.5% to about 1.9% (Am. J. Surg. 2005;190:9-15). There was no significant difference between groups.
Another study showed improved compliance with SCIP measures, but no change in surgical site infection rate (Dis. Colon Rectum 2010;53:24-30). This is the theme in study after study after study.
A 2008 study enrolled 9,195 patients undergoing colorectal, orthopedic, or vascular surgery and looked at SCIP compliance vs. surgical site infection. The SCIP rate correlated with the hospital case mix. If you look at the SCIP rate in terms of antibiotic timing, SCIP is not significant. The study basically showed that variables other than timely antibiotic administration are affecting surgical site infection rates (J. Am. Coll. Surg. 2008;206:814-19).
Hospital performance on process measures may not be a good marker of surgical site infection or the outcome we’re looking at, according to another study, which reported that unmeasured effects may have a larger impact than the measured effects (Health Serv. Res. 2008;43:1464-84).
There is a randomized controlled trial that randomized patients to strict control with the SCIP measures or routine treatment at the hospital. The SCIP-treated patients had nearly twice the incidence of surgical site infections as the patients receiving standard treatment. The authors concluded that combining each of the SCIP factors into one big category doesn’t necessarily work (Arch. Surg. 2011;146:263-9).
Should we be evaluating outcome measures with performance measures (e.g., percent timely antibiotic administration) to determine whether they work or not? One editorial evaluated eight articles with data on 31,448 patients, looking just at antibiotic administration within 1 hour of surgery, a SCIP measure. It found a higher infection rate if antibiotics were administered within 30 minutes of incision (JAMA 2010;303:2527-2528).
There was no significant difference in another study between standard of care and SCIP for venous thromboembolism (Am. J. Surg. 2012;204:591-97). The authors wrote that there is no convincing evidence that improvements in compliance are associated with better outcomes. We see this time and time again.
When people find that SCIP is not working, they turn to other measures to reduce surgical site infection. The Comprehensive Unit-based Safety Program (CUSP) is targeted at a specific problem that a specific hospital is having in managing infections. It’s not coming from Washington; it’s based at the hospital. One study showed that following CUSP, there was a significant reduction in surgical site infections despite the fact that previous to that there was 95% compliance with SCIP standards (J. Am. Coll. Surg. 2012;215:193-200). SCIP was working, but it wasn’t affecting outcome.
Dr. Lagasse and I interpret one key study very differently. He abstracts a sentence from a Limitations section of the study and makes a sweeping generalization out of context. But the study showed no relationship between facility adherence to SCIP and the surgical site infection rate. The authors concluded, "Policies regarding continued SCIP measurement and reporting should be reassessed" (Ann. Surg. 2011;254:494-99).
The largest SCIP study to date from a single entity involved 32,459 patients in the Veterans Affairs medical system. Overall, antibiotics were administered within 28 minutes of surgical incision. Once they adjusted for confounders, they found no significant relationship between surgical site infection and the SCIP measures (JAMA 2013;148:649-57). No one has proven that giving antibiotics within 60 minutes of surgical incision gives you a lower infection rate.
SCIP measures divert resources and divert clinical care. They obscure the nuances of care. They may harm the hospital and the provider, and they raise unnecessary legal risk if an antibiotic is not given within 60 minutes of incision.
Dr. Barash is a professor of anesthesiology at Yale University, New Haven, Conn. He reported having no financial disclosures.
These are excerpts from a debate at the annual meeting of the American Society of Anesthesiologists.
POINT: SCIP is both efficacious and effective.
The Surgical Care Improvement Project (SCIP) was a national campaign that set out to reduce surgical mortality and morbidity by 25% by 2010 through recommendations in targeted areas: wound infections, perioperative MIs, and venous thromboembolism. The recommendations have become pay-for-performance measures. There are seven in the area of infectious disease to reduce surgical site infections. There is one measure for reducing perioperative MI: Continue beta-blockers (for patients who are on them) in the perioperative period. For venous thromboembolism prevention, give prophylaxis within 24 hours before to 24 hours after surgery.
It’s key to understand the difference between efficacy and effectiveness. I think we would all agree that the SCIP measures have efficacy. Efficacy trials determine whether an intervention produces the expected result under ideal circumstances. Effectiveness trials measure the degree of beneficial effect under "real world" clinical conditions. The problem with effectiveness trials is that those real-world conditions may change the effect, or they might just change the ability to measure the effect.
I believe that the SCIP measures have proven efficacy because they all are based upon randomized controlled trials that were identified by systematic reviews amenable to meta-analysis. All of these measures are Level 1 recommendations, based on the highest forms of evidence. The studies that Dr. Barash uses to criticize SCIP measures are cohort studies. They do not randomize. There may be unknown confounding variables.
There have been effectiveness trials that show that the SCIP measures do work. One showed a 27% decrease in surgical site infections, another showed a 62% decrease in surgical site infections, and a third showed a 39% decrease in surgical site infections.
Perhaps the strongest endorsement of efficacy of the SCIP measures comes from Dr. Kaveh G. Shojania, who has written several reviews of the efficacy of medical interventions. This guy is like Mikey from the old Life cereal commercials ... he hates everything. He said there were 11 patient safety practices rated most highly in terms of strength of the evidence, and 3 are SCIP measures: appropriate use of prophylaxis to prevent venous thromboembolism in patients at risk, use of perioperative beta-blockers in appropriate patients, and appropriate use of antibiotic prophylaxis in surgical patients (AHRQ Publication No. 01-E058).
Several trials published by pretty good researchers in reputable journals show a lack of effectiveness of SCIP measures. Even those researchers admit to the efficacy of SCIP measures. The lead investigator of the best effectiveness trial, a retrospective cohort study, wrote, "There are several explanations as to why we did not observe an association between timely antibiotic administration and surgical site infection (SSI). The first is that timely antibiotic administration does not diminish SSI risk. This is an unlikely interpretation. There are numerous randomized controlled trials and observational studies that demonstrate the efficacy of prophylactic antibiotics in reducing SSI for various surgical procedures" (Ann. Surg. 2011;254:494-9).
A separate retrospective cohort study showed a decrease in surgical site infection only if two or more SCIP recommendations were followed (JAMA 2010;303:2479-85). Shocking – if you give the wrong antibiotic at the right time, it might not work.
Another retrospective cohort study found no association with adjusted complications and SCIP compliance. Hospitals in the lowest compliance group had patients in lower-income ZIP codes and lower unadjusted complication rates. So, poor people go home and don’t come back, perhaps because of payment considerations. The study didn’t have enough patients; it also used measures that don’t apply to SCIP (Arch. Surg. 2010;145:999-1004).
SCIP did not design these measures for pay-for-performance programs. The intent was to decrease perioperative complications by 25% by 2010. When you start changing the baseline with pay-for-performance, it doesn’t work. In a study by Hawkins et al., the authors tested the hypothesis that documented compliance with antibiotic prophylaxis guidelines on a pediatric surgery service does not reflect adherence to guidelines as intended. In a 7-week observational study of elective pediatric surgical cases, adherence was evaluated for appropriate administration, type, timing, weight-based dosing, and redosing of antibiotics. Prophylactic antibiotics were administered appropriately in 141 of 143 cases (99%). Of 100 cases in which antibiotic prophylaxis was indicated, compliance was documented in 100% of cases in the electronic medical record; but only 48% of cases adhered to all five guidelines. Lack of adherence was due primarily to dosing or timing errors.
The SCIP measures, however, are based on best evidence. They are tightly linked with the desired outcomes. They are measurable and effectible, as demonstrated in multiple randomized controlled trials. Studies of effectiveness have had variable results due to methodological flaws.
Dr. Lagasse is a professor of anesthesiology and director of quality management at the Yale School of Medicine, New Haven, Conn. He is on the steering committee for the Surgical Care Improvement Project. He reported having no financial disclosures.
COUNTERPOINT: Studies have not shown effectiveness.
When it was created, SCIP did not reflect reality. SCIP started at the U.S. Department of Veterans Affairs, which conducted a 10-year study. They found a 25% relative risk reduction, but that was only a 0.8% absolute risk reduction for the incidence of complications, a drop from about 3.1% to about 2.3% (Arch. Surg. 2002;137:20-27).
It would be great to have randomized controlled trials on the effectiveness of SCIP, but it’s not happening. We’re going to have to go by high-fidelity observational trials, which according to a number of researchers in the field have the same impact as randomized controlled trials.
One study of 35,543 patients in 44 hospitals found a whopping 27% reduction in surgical site infections, but that was only a 0.6% absolute reduction, from about 2.5% to about 1.9% (Am. J. Surg. 2005;190:9-15). There was no significant difference between groups.
Another study showed improved compliance with SCIP measures, but no change in surgical site infection rate (Dis. Colon Rectum 2010;53:24-30). This is the theme in study after study after study.
A 2008 study enrolled 9,195 patients undergoing colorectal, orthopedic, or vascular surgery and looked at SCIP compliance vs. surgical site infection. The SCIP rate correlated with the hospital case mix. If you look at the SCIP rate in terms of antibiotic timing, SCIP is not significant. The study basically showed that variables other than timely antibiotic administration are affecting surgical site infection rates (J. Am. Coll. Surg. 2008;206:814-19).
Hospital performance on process measures may not be a good marker of surgical site infection or the outcome we’re looking at, according to another study, which reported that unmeasured effects may have a larger impact than the measured effects (Health Serv. Res. 2008;43:1464-84).
There is a randomized controlled trial that randomized patients to strict control with the SCIP measures or routine treatment at the hospital. The SCIP-treated patients had nearly twice the incidence of surgical site infections as the patients receiving standard treatment. The authors concluded that combining each of the SCIP factors into one big category doesn’t necessarily work (Arch. Surg. 2011;146:263-9).
Should we be evaluating outcome measures with performance measures (e.g., percent timely antibiotic administration) to determine whether they work or not? One editorial evaluated eight articles with data on 31,448 patients, looking just at antibiotic administration within 1 hour of surgery, a SCIP measure. It found a higher infection rate if antibiotics were administered within 30 minutes of incision (JAMA 2010;303:2527-2528).
There was no significant difference in another study between standard of care and SCIP for venous thromboembolism (Am. J. Surg. 2012;204:591-97). The authors wrote that there is no convincing evidence that improvements in compliance are associated with better outcomes. We see this time and time again.
When people find that SCIP is not working, they turn to other measures to reduce surgical site infection. The Comprehensive Unit-based Safety Program (CUSP) is targeted at a specific problem that a specific hospital is having in managing infections. It’s not coming from Washington; it’s based at the hospital. One study showed that following CUSP, there was a significant reduction in surgical site infections despite the fact that previous to that there was 95% compliance with SCIP standards (J. Am. Coll. Surg. 2012;215:193-200). SCIP was working, but it wasn’t affecting outcome.
Dr. Lagasse and I interpret one key study very differently. He abstracts a sentence from a Limitations section of the study and makes a sweeping generalization out of context. But the study showed no relationship between facility adherence to SCIP and the surgical site infection rate. The authors concluded, "Policies regarding continued SCIP measurement and reporting should be reassessed" (Ann. Surg. 2011;254:494-99).
The largest SCIP study to date from a single entity involved 32,459 patients in the Veterans Affairs medical system. Overall, antibiotics were administered within 28 minutes of surgical incision. Once they adjusted for confounders, they found no significant relationship between surgical site infection and the SCIP measures (JAMA 2013;148:649-57). No one has proven that giving antibiotics within 60 minutes of surgical incision gives you a lower infection rate.
SCIP measures divert resources and divert clinical care. They obscure the nuances of care. They may harm the hospital and the provider, and they raise unnecessary legal risk if an antibiotic is not given within 60 minutes of incision.
Dr. Barash is a professor of anesthesiology at Yale University, New Haven, Conn. He reported having no financial disclosures.
These are excerpts from a debate at the annual meeting of the American Society of Anesthesiologists.