User login
Official Newspaper of the American College of Surgeons
Psychoeducation, compliance contracts curb postsurgery alcohol abuse
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
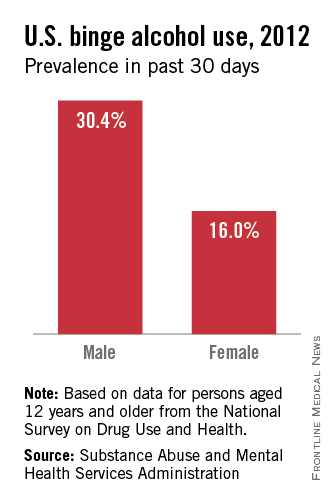
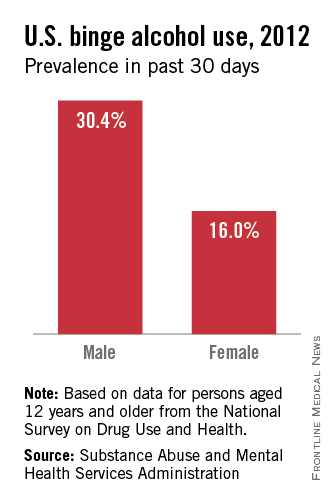
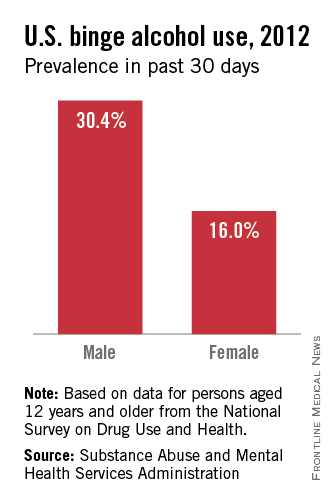
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
EXPERT ANALYSIS FROM OBESITY WEEK
Radiotherapy can be omitted for many older breast cancer patients
SAN ANTONIO – Avoiding whole-breast radiation therapy is a reasonable – and even attractive – option for many older women with early-stage breast cancer, according to the results of the Postoperative Radiotherapy in Minimum-Risk Elderly (PRIME II) trial.
The patient population identified in PRIME II as being suitable for omission of postoperative radiotherapy on the basis of a relatively benign natural history consists of women aged 65 or older who are on adjuvant hormone therapy after undergoing lumpectomy with clear margins for estrogen receptor–rich, axillary node–negative breast cancer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PRIME II was a six-country trial in which 1,326 patients 65 or older with hormone receptor–positive early breast cancer were randomized to radiotherapy or no radiotherapy following breast-conserving surgery and endocrine therapy. The 5-year actuarial rate of ipsilateral breast cancer recurrence – the primary study endpoint – was 1.3% in those who received radiotherapy and 4.1% in those who did not, Dr. Ian H. Kunkler reported at the San Antonio Breast Cancer Symposium.
The 5-year actuarial rate of overall survival was 94.2% in patients randomized to radiotherapy and closely similar at 93.8% in the no-radiotherapy group, added Dr. Kunkler, professor of clinical oncology at the University of Edinburgh.
The relative benefit of radiotherapy was even smaller in the 91% of subjects who had estrogen-rich tumors as defined by an ER score of at least 7. They had a local recurrence rate of 3.2% with radiotherapy and 0.8% without. While that absolute 2.4% difference was statistically significant, it is arguably not clinically meaningful. For every 100 women who fit the description carefully defined in PRIME II and who undergo radiotherapy, three will have a recurrence prevented, one will have a recurrence anyway, and 96 will have had treatment that was not beneficial, he said.
"I think we’re really at the cusp of overtreatment here. I think it’s a matter for discussion between the physician and patient as to whether that very modest benefit is worth the potential complications of radiotherapy and the burdens of ongoing treatment, as well as the costs to the health service. Older patients find radiotherapy very burdensome, the relative benefits are very small, and there is no compromise in terms of overall survival with its omission," Dr. Kunkler said.
An important caveat: Among the 9% of patients with low estrogen receptor status, the local recurrence rate was 11.1% with no radiotherapy compared to zero with radiation.
"This is a group for whom radiotherapy should not be omitted," Dr. Kunkler declared.
More than one-half of all early breast cancers present in women aged 65 or older. While postoperative radiotherapy after lumpectomy has been the standard of care regardless of age and other risk factors, there has been only sparse high-quality supporting evidence for this practice in older patients.
Dr. Kunkler estimated that the PRIME II findings are generalizable to 60%-70% of all breast cancer patients over age 65. He predicted that the PRIME II study will "very likely" alter practice in the United Kingdom, and symposium codirector Dr. C. Kent Osborne predicted that the study will be practice changing in the United States as well.
"When I was in training, everybody thought that more was better: more drug treatment, more radiation, more surgery, high-dose chemotherapy, and bone marrow transplant. As we’ve evolved over the last 3 decades, that’s turning out not to be the case. I think we’re gradually doing less and less treatment, either with radiotherapy or with surgery, to control the local disease in appropriate patients. And I think more and more people will begin to accept it," said Dr. Osborne, director of the Dan L. Duncan Cancer Center and the Lester and Sue Smith Breast Center at Baylor College of Medicine, Houston.
PRIME II was funded by the Chief Scientist Office for Scotland. Dr. Kunkler declared having no conflicts of interest.
SAN ANTONIO – Avoiding whole-breast radiation therapy is a reasonable – and even attractive – option for many older women with early-stage breast cancer, according to the results of the Postoperative Radiotherapy in Minimum-Risk Elderly (PRIME II) trial.
The patient population identified in PRIME II as being suitable for omission of postoperative radiotherapy on the basis of a relatively benign natural history consists of women aged 65 or older who are on adjuvant hormone therapy after undergoing lumpectomy with clear margins for estrogen receptor–rich, axillary node–negative breast cancer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PRIME II was a six-country trial in which 1,326 patients 65 or older with hormone receptor–positive early breast cancer were randomized to radiotherapy or no radiotherapy following breast-conserving surgery and endocrine therapy. The 5-year actuarial rate of ipsilateral breast cancer recurrence – the primary study endpoint – was 1.3% in those who received radiotherapy and 4.1% in those who did not, Dr. Ian H. Kunkler reported at the San Antonio Breast Cancer Symposium.
The 5-year actuarial rate of overall survival was 94.2% in patients randomized to radiotherapy and closely similar at 93.8% in the no-radiotherapy group, added Dr. Kunkler, professor of clinical oncology at the University of Edinburgh.
The relative benefit of radiotherapy was even smaller in the 91% of subjects who had estrogen-rich tumors as defined by an ER score of at least 7. They had a local recurrence rate of 3.2% with radiotherapy and 0.8% without. While that absolute 2.4% difference was statistically significant, it is arguably not clinically meaningful. For every 100 women who fit the description carefully defined in PRIME II and who undergo radiotherapy, three will have a recurrence prevented, one will have a recurrence anyway, and 96 will have had treatment that was not beneficial, he said.
"I think we’re really at the cusp of overtreatment here. I think it’s a matter for discussion between the physician and patient as to whether that very modest benefit is worth the potential complications of radiotherapy and the burdens of ongoing treatment, as well as the costs to the health service. Older patients find radiotherapy very burdensome, the relative benefits are very small, and there is no compromise in terms of overall survival with its omission," Dr. Kunkler said.
An important caveat: Among the 9% of patients with low estrogen receptor status, the local recurrence rate was 11.1% with no radiotherapy compared to zero with radiation.
"This is a group for whom radiotherapy should not be omitted," Dr. Kunkler declared.
More than one-half of all early breast cancers present in women aged 65 or older. While postoperative radiotherapy after lumpectomy has been the standard of care regardless of age and other risk factors, there has been only sparse high-quality supporting evidence for this practice in older patients.
Dr. Kunkler estimated that the PRIME II findings are generalizable to 60%-70% of all breast cancer patients over age 65. He predicted that the PRIME II study will "very likely" alter practice in the United Kingdom, and symposium codirector Dr. C. Kent Osborne predicted that the study will be practice changing in the United States as well.
"When I was in training, everybody thought that more was better: more drug treatment, more radiation, more surgery, high-dose chemotherapy, and bone marrow transplant. As we’ve evolved over the last 3 decades, that’s turning out not to be the case. I think we’re gradually doing less and less treatment, either with radiotherapy or with surgery, to control the local disease in appropriate patients. And I think more and more people will begin to accept it," said Dr. Osborne, director of the Dan L. Duncan Cancer Center and the Lester and Sue Smith Breast Center at Baylor College of Medicine, Houston.
PRIME II was funded by the Chief Scientist Office for Scotland. Dr. Kunkler declared having no conflicts of interest.
SAN ANTONIO – Avoiding whole-breast radiation therapy is a reasonable – and even attractive – option for many older women with early-stage breast cancer, according to the results of the Postoperative Radiotherapy in Minimum-Risk Elderly (PRIME II) trial.
The patient population identified in PRIME II as being suitable for omission of postoperative radiotherapy on the basis of a relatively benign natural history consists of women aged 65 or older who are on adjuvant hormone therapy after undergoing lumpectomy with clear margins for estrogen receptor–rich, axillary node–negative breast cancer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PRIME II was a six-country trial in which 1,326 patients 65 or older with hormone receptor–positive early breast cancer were randomized to radiotherapy or no radiotherapy following breast-conserving surgery and endocrine therapy. The 5-year actuarial rate of ipsilateral breast cancer recurrence – the primary study endpoint – was 1.3% in those who received radiotherapy and 4.1% in those who did not, Dr. Ian H. Kunkler reported at the San Antonio Breast Cancer Symposium.
The 5-year actuarial rate of overall survival was 94.2% in patients randomized to radiotherapy and closely similar at 93.8% in the no-radiotherapy group, added Dr. Kunkler, professor of clinical oncology at the University of Edinburgh.
The relative benefit of radiotherapy was even smaller in the 91% of subjects who had estrogen-rich tumors as defined by an ER score of at least 7. They had a local recurrence rate of 3.2% with radiotherapy and 0.8% without. While that absolute 2.4% difference was statistically significant, it is arguably not clinically meaningful. For every 100 women who fit the description carefully defined in PRIME II and who undergo radiotherapy, three will have a recurrence prevented, one will have a recurrence anyway, and 96 will have had treatment that was not beneficial, he said.
"I think we’re really at the cusp of overtreatment here. I think it’s a matter for discussion between the physician and patient as to whether that very modest benefit is worth the potential complications of radiotherapy and the burdens of ongoing treatment, as well as the costs to the health service. Older patients find radiotherapy very burdensome, the relative benefits are very small, and there is no compromise in terms of overall survival with its omission," Dr. Kunkler said.
An important caveat: Among the 9% of patients with low estrogen receptor status, the local recurrence rate was 11.1% with no radiotherapy compared to zero with radiation.
"This is a group for whom radiotherapy should not be omitted," Dr. Kunkler declared.
More than one-half of all early breast cancers present in women aged 65 or older. While postoperative radiotherapy after lumpectomy has been the standard of care regardless of age and other risk factors, there has been only sparse high-quality supporting evidence for this practice in older patients.
Dr. Kunkler estimated that the PRIME II findings are generalizable to 60%-70% of all breast cancer patients over age 65. He predicted that the PRIME II study will "very likely" alter practice in the United Kingdom, and symposium codirector Dr. C. Kent Osborne predicted that the study will be practice changing in the United States as well.
"When I was in training, everybody thought that more was better: more drug treatment, more radiation, more surgery, high-dose chemotherapy, and bone marrow transplant. As we’ve evolved over the last 3 decades, that’s turning out not to be the case. I think we’re gradually doing less and less treatment, either with radiotherapy or with surgery, to control the local disease in appropriate patients. And I think more and more people will begin to accept it," said Dr. Osborne, director of the Dan L. Duncan Cancer Center and the Lester and Sue Smith Breast Center at Baylor College of Medicine, Houston.
PRIME II was funded by the Chief Scientist Office for Scotland. Dr. Kunkler declared having no conflicts of interest.
AT SABCS 2013
Major finding: The 5-year ipsilateral breast cancer recurrence rate in a selected population of older women undergoing breast-conserving surgery and adjuvant hormone therapy was 1.3% with postoperative radiotherapy and 4.1% without it, a modest difference that did not impact overall survival.
Data source: A prospective randomized trial in six countries, involving 1,326 patients aged 65 or older who underwent lumpectomy with clear margins for hormone receptor–positive, axillary node–negative breast cancer and were on adjuvant endocrine therapy. They were randomized to postoperative radiotherapy or no radiotherapy.
Disclosures: The PRIME II study was funded by the Chief Scientist Office for Scotland. The presenter reported having no financial conflicts.
Congress poised to vote on 3-month SGR patch
WASHINGTON – Congress is preparing to vote on a proposal that would give physicians a temporary 3-month reprieve from the 20% Medicare pay cut that’s due to take effect on Jan. 1.
The proposal was quickly attached to legislation federal budget legislation that would also ameliorate some of the automatic, across-the-board spending cuts known as sequestration.
The House is scheduled to vote on the budget measure before it leaves for a month-long recess on Dec. 13. It is expected that the "doc fix" proposal could be voted on within the same time frame; however, it may not get support of the full House, even though there is bipartisan consensus to replace the Sustainable Growth Rate formula.
At a House Rules Committee hearing on Dec. 11, Democratic leaders said that they would not support the temporary SGR patch unless Republicans agreed to also vote on restoring unemployment compensation benefits for 3 months. Those benefits are due to expire at the end of December for 1.3 million Americans.
"I’m not sure that Democrats can vote for a package that adds SGR, which we support, but does not allow us to address long-term unemployment," said Rep. Nita Lowey (D-N.Y.).
The SGR amendment would increase physician fees by 0.5% for January-March 2014 and encourage Congress to keep working on a new, permanent Medicare fee system teamed with reduced administrative burdens and timely feedback on performance and to develop new payment models.
The temporary fix would be paid for by adjusting disproportionate share payments for hospitals, according to Rep. Michael Burgess (R-Tex.), an ob.gyn. who serves on the Rules Committee. The payment mechanism is noncontroversial, he said in an interview.
Physician groups have said that they would support a short-term fix, provided lawmakers continue working on a permanent repeal of the SGR.
"This is simply a pathway," Dr. Ardis Dee Hoven, president of the American Medical Association, said in an interview. "We want to keep up the momentum to get the SGR repealed. We recognize that it’s going to take a little more time."
Dr. Molly Cooke, president of the American College of Physicians, agreed. "This measure will allow Congress time to complete work early next year on comprehensive legislation to repeal the Medicare SGR formula," she said in a statement.
The Senate Finance Committee and the House Ways and Means Committee are both meeting to vote on proposals to permanently replace the SGR on Dec. 12.
On Twitter @aliciaault
WASHINGTON – Congress is preparing to vote on a proposal that would give physicians a temporary 3-month reprieve from the 20% Medicare pay cut that’s due to take effect on Jan. 1.
The proposal was quickly attached to legislation federal budget legislation that would also ameliorate some of the automatic, across-the-board spending cuts known as sequestration.
The House is scheduled to vote on the budget measure before it leaves for a month-long recess on Dec. 13. It is expected that the "doc fix" proposal could be voted on within the same time frame; however, it may not get support of the full House, even though there is bipartisan consensus to replace the Sustainable Growth Rate formula.
At a House Rules Committee hearing on Dec. 11, Democratic leaders said that they would not support the temporary SGR patch unless Republicans agreed to also vote on restoring unemployment compensation benefits for 3 months. Those benefits are due to expire at the end of December for 1.3 million Americans.
"I’m not sure that Democrats can vote for a package that adds SGR, which we support, but does not allow us to address long-term unemployment," said Rep. Nita Lowey (D-N.Y.).
The SGR amendment would increase physician fees by 0.5% for January-March 2014 and encourage Congress to keep working on a new, permanent Medicare fee system teamed with reduced administrative burdens and timely feedback on performance and to develop new payment models.
The temporary fix would be paid for by adjusting disproportionate share payments for hospitals, according to Rep. Michael Burgess (R-Tex.), an ob.gyn. who serves on the Rules Committee. The payment mechanism is noncontroversial, he said in an interview.
Physician groups have said that they would support a short-term fix, provided lawmakers continue working on a permanent repeal of the SGR.
"This is simply a pathway," Dr. Ardis Dee Hoven, president of the American Medical Association, said in an interview. "We want to keep up the momentum to get the SGR repealed. We recognize that it’s going to take a little more time."
Dr. Molly Cooke, president of the American College of Physicians, agreed. "This measure will allow Congress time to complete work early next year on comprehensive legislation to repeal the Medicare SGR formula," she said in a statement.
The Senate Finance Committee and the House Ways and Means Committee are both meeting to vote on proposals to permanently replace the SGR on Dec. 12.
On Twitter @aliciaault
WASHINGTON – Congress is preparing to vote on a proposal that would give physicians a temporary 3-month reprieve from the 20% Medicare pay cut that’s due to take effect on Jan. 1.
The proposal was quickly attached to legislation federal budget legislation that would also ameliorate some of the automatic, across-the-board spending cuts known as sequestration.
The House is scheduled to vote on the budget measure before it leaves for a month-long recess on Dec. 13. It is expected that the "doc fix" proposal could be voted on within the same time frame; however, it may not get support of the full House, even though there is bipartisan consensus to replace the Sustainable Growth Rate formula.
At a House Rules Committee hearing on Dec. 11, Democratic leaders said that they would not support the temporary SGR patch unless Republicans agreed to also vote on restoring unemployment compensation benefits for 3 months. Those benefits are due to expire at the end of December for 1.3 million Americans.
"I’m not sure that Democrats can vote for a package that adds SGR, which we support, but does not allow us to address long-term unemployment," said Rep. Nita Lowey (D-N.Y.).
The SGR amendment would increase physician fees by 0.5% for January-March 2014 and encourage Congress to keep working on a new, permanent Medicare fee system teamed with reduced administrative burdens and timely feedback on performance and to develop new payment models.
The temporary fix would be paid for by adjusting disproportionate share payments for hospitals, according to Rep. Michael Burgess (R-Tex.), an ob.gyn. who serves on the Rules Committee. The payment mechanism is noncontroversial, he said in an interview.
Physician groups have said that they would support a short-term fix, provided lawmakers continue working on a permanent repeal of the SGR.
"This is simply a pathway," Dr. Ardis Dee Hoven, president of the American Medical Association, said in an interview. "We want to keep up the momentum to get the SGR repealed. We recognize that it’s going to take a little more time."
Dr. Molly Cooke, president of the American College of Physicians, agreed. "This measure will allow Congress time to complete work early next year on comprehensive legislation to repeal the Medicare SGR formula," she said in a statement.
The Senate Finance Committee and the House Ways and Means Committee are both meeting to vote on proposals to permanently replace the SGR on Dec. 12.
On Twitter @aliciaault
AT A HOUSE RULES COMMITTEE HEARING
ACA enrollment grows, but still less than expected
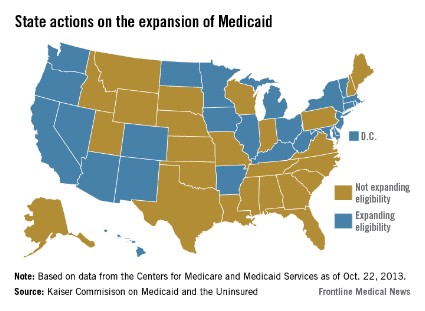
Even with a burst of activity on the state and federal health insurance exchanges during November, numbers released Dec. 11 by the Health and Human Services department indicate that the Obama administration may not be on track to meet the goal set by the Congressional Budget Office – insuring 7 million individuals by Mar. 31, 2014, the end of the current open enrollment for health insurance under the Affordable Care Act.
But Michael Hash, director of the HHS Office of Health Reform, said in a briefing with reporters, "We’re on track." Americans still have 6 months to enroll, he noted, and the expectation is that most people will sign up towards the end of that period.
According to HHS’s mid-December enrollment report, 364,682 individuals selected a health insurance plan from a state or federal exchange in October and November. The bulk of those (227,478) used a state-based exchange, while 137,204 signed up via the federal exchange, which operates in 36 states. The biggest proportion of overall sign-ups came in November, with 258,497 selecting a plan in the state or federal exchanges.
The numbers include consumers who have paid their first health insurance premium as well as those who have not.
About 2.3 million Americans have been determined to be eligible to enroll in a marketplace plan, but only 364,000 have actually selected a plan. Of the 2.3 million, 41% (944,531) are eligible for financial assistance. That number includes people who didn’t apply for financial assistance, who applied for financial assistance and were found ineligible, or those whose applications for financial assistance are pending, according to the HHS report.
Further, just over 803,000 consumers have been determined to be eligible for coverage from Medicaid or the Children’s Health Insurance Program (CHIP).
Enrollment has increased in part because of improvements to the federal exchange website, healthcare.gov. Mr. Hash said. "Healthcare.gov is night and day from where it was on October the first," he said in comments made in advance of testimony by HHS Secretary Kathleen Sebelius at a hearing called by the House Energy and Commerce Committee’s Health Subcommittee.
Overall, 83% of completed applications were done electronically, either through healthcare.gov or a state exchange website, or online when individuals applied at a community center or some other assistance location.
Mr. Hash also said that demand for exchange plans continues to grow, citing increasing visits to the federal and state websites and calls to the call centers.
Since Oct. 1, there have been 10.6 million visits to state exchanges and 1.7 million calls to state call centers. There have been 28.4 million visits to healthcare.gov and 3.4 million calls.
On Twitter @aliciaault
Even with a burst of activity on the state and federal health insurance exchanges during November, numbers released Dec. 11 by the Health and Human Services department indicate that the Obama administration may not be on track to meet the goal set by the Congressional Budget Office – insuring 7 million individuals by Mar. 31, 2014, the end of the current open enrollment for health insurance under the Affordable Care Act.
But Michael Hash, director of the HHS Office of Health Reform, said in a briefing with reporters, "We’re on track." Americans still have 6 months to enroll, he noted, and the expectation is that most people will sign up towards the end of that period.
According to HHS’s mid-December enrollment report, 364,682 individuals selected a health insurance plan from a state or federal exchange in October and November. The bulk of those (227,478) used a state-based exchange, while 137,204 signed up via the federal exchange, which operates in 36 states. The biggest proportion of overall sign-ups came in November, with 258,497 selecting a plan in the state or federal exchanges.
The numbers include consumers who have paid their first health insurance premium as well as those who have not.
About 2.3 million Americans have been determined to be eligible to enroll in a marketplace plan, but only 364,000 have actually selected a plan. Of the 2.3 million, 41% (944,531) are eligible for financial assistance. That number includes people who didn’t apply for financial assistance, who applied for financial assistance and were found ineligible, or those whose applications for financial assistance are pending, according to the HHS report.
Further, just over 803,000 consumers have been determined to be eligible for coverage from Medicaid or the Children’s Health Insurance Program (CHIP).
Enrollment has increased in part because of improvements to the federal exchange website, healthcare.gov. Mr. Hash said. "Healthcare.gov is night and day from where it was on October the first," he said in comments made in advance of testimony by HHS Secretary Kathleen Sebelius at a hearing called by the House Energy and Commerce Committee’s Health Subcommittee.
Overall, 83% of completed applications were done electronically, either through healthcare.gov or a state exchange website, or online when individuals applied at a community center or some other assistance location.
Mr. Hash also said that demand for exchange plans continues to grow, citing increasing visits to the federal and state websites and calls to the call centers.
Since Oct. 1, there have been 10.6 million visits to state exchanges and 1.7 million calls to state call centers. There have been 28.4 million visits to healthcare.gov and 3.4 million calls.
On Twitter @aliciaault
Even with a burst of activity on the state and federal health insurance exchanges during November, numbers released Dec. 11 by the Health and Human Services department indicate that the Obama administration may not be on track to meet the goal set by the Congressional Budget Office – insuring 7 million individuals by Mar. 31, 2014, the end of the current open enrollment for health insurance under the Affordable Care Act.
But Michael Hash, director of the HHS Office of Health Reform, said in a briefing with reporters, "We’re on track." Americans still have 6 months to enroll, he noted, and the expectation is that most people will sign up towards the end of that period.
According to HHS’s mid-December enrollment report, 364,682 individuals selected a health insurance plan from a state or federal exchange in October and November. The bulk of those (227,478) used a state-based exchange, while 137,204 signed up via the federal exchange, which operates in 36 states. The biggest proportion of overall sign-ups came in November, with 258,497 selecting a plan in the state or federal exchanges.
The numbers include consumers who have paid their first health insurance premium as well as those who have not.
About 2.3 million Americans have been determined to be eligible to enroll in a marketplace plan, but only 364,000 have actually selected a plan. Of the 2.3 million, 41% (944,531) are eligible for financial assistance. That number includes people who didn’t apply for financial assistance, who applied for financial assistance and were found ineligible, or those whose applications for financial assistance are pending, according to the HHS report.
Further, just over 803,000 consumers have been determined to be eligible for coverage from Medicaid or the Children’s Health Insurance Program (CHIP).
Enrollment has increased in part because of improvements to the federal exchange website, healthcare.gov. Mr. Hash said. "Healthcare.gov is night and day from where it was on October the first," he said in comments made in advance of testimony by HHS Secretary Kathleen Sebelius at a hearing called by the House Energy and Commerce Committee’s Health Subcommittee.
Overall, 83% of completed applications were done electronically, either through healthcare.gov or a state exchange website, or online when individuals applied at a community center or some other assistance location.
Mr. Hash also said that demand for exchange plans continues to grow, citing increasing visits to the federal and state websites and calls to the call centers.
Since Oct. 1, there have been 10.6 million visits to state exchanges and 1.7 million calls to state call centers. There have been 28.4 million visits to healthcare.gov and 3.4 million calls.
On Twitter @aliciaault
Review your insurance
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Skin & Allergy News.
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Skin & Allergy News.
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Skin & Allergy News.
Urinary tract injury incidence during laparoscopic hysterectomy pegged at 1.3%
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: Among 3,523 laparoscopic hysterectomies performed from 2001 to 2012, the incidence of urinary tract injury was 1.3%.
Data source: A review of patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center.
Disclosures: The researchers stated that they had no relevant financial disclosures.
18% of lung cancers caught by CT screening were indolent
An estimated 18% of the early lung cancers detected by low-dose CT screening in the National Lung Screening Trial were likely indolent and probably represent overdiagnosis, according to a report published online Dec. 9 in JAMA Internal Medicine.
The National Lung Screening Trial (NLST) found "an encouraging" 20% relative reduction in lung cancer–specific mortality among high-risk patients who were screened using low-dose CT, compared with chest radiography. "These findings were met with enthusiasm, but before a widespread public health screening program is implemented, risks of screening also need to be considered," said Dr. Edward F. Patz Jr. of the department of radiology, Duke University Medical Center, Durham, N.C., and his associates in the NLST.
The chief risk in this case is overdiagnosis: identifying an early-stage lesion in an asymptomatic patient that would not progress or affect that patient’s long-term health. It is likely that some of the tumors detected on low-dose CT were just such indolent cancers, and that those patients unnecessarily underwent invasive diagnostic procedures, surgical resection, and multiple follow-up studies.
To estimate how many of the detected cancers in the NLST were indolent – and thus overdiagnosed – Dr. Patz and his colleagues used statistical probability methods to analyze extended follow-up data from the study.
The NLST involved 53,452 men and women aged 55-74 years who were enrolled during 2002-2004 and who had at least a 30-pack-year history of cigarette smoking. The patients were randomly assigned to undergo lung cancer screening using either three annual low-dose CT exams or three annual single-view chest radiographs.
Mean follow-up was approximately 6 years. "At the end of the entire trial, there were 1,089 total lung cancer cases in the low-dose CT arm (649 detected by low-dose CT screening) and 969 cases in the [radiology] arm, for an excess of 120 cases. This gives [an] excess cancer rate of 18.5%," the investigators said (JAMA Intern. Med. 2013 Dec. 9 [doi:10.1001/jamainternmed.2013.12738]).
"The data from this study suggest that ... 18% of persons in the low-dose CT arm with screen-detected lung cancer and 22% of those in the low-dose CT arm with screen-detected NSCLC [non–small cell lung cancer] may be cases of overdiagnosis," Dr. Patz and his associates said. "In other words, if these individuals had not entered the NLST, they would not have received a lung cancer diagnosis or treatment, at least for the next 5 years."
In the future, the study authors noted, "once there are better biomarkers and imaging techniques to predict which individuals with a diagnosis of lung cancer will have more or less aggressive disease, treatment options can be optimized, and a mass screening program can become more valuable."
The National Institutes of Health supported the NSLT. No financial conflicts of interest were reported.
An estimated 18% of the early lung cancers detected by low-dose CT screening in the National Lung Screening Trial were likely indolent and probably represent overdiagnosis, according to a report published online Dec. 9 in JAMA Internal Medicine.
The National Lung Screening Trial (NLST) found "an encouraging" 20% relative reduction in lung cancer–specific mortality among high-risk patients who were screened using low-dose CT, compared with chest radiography. "These findings were met with enthusiasm, but before a widespread public health screening program is implemented, risks of screening also need to be considered," said Dr. Edward F. Patz Jr. of the department of radiology, Duke University Medical Center, Durham, N.C., and his associates in the NLST.
The chief risk in this case is overdiagnosis: identifying an early-stage lesion in an asymptomatic patient that would not progress or affect that patient’s long-term health. It is likely that some of the tumors detected on low-dose CT were just such indolent cancers, and that those patients unnecessarily underwent invasive diagnostic procedures, surgical resection, and multiple follow-up studies.
To estimate how many of the detected cancers in the NLST were indolent – and thus overdiagnosed – Dr. Patz and his colleagues used statistical probability methods to analyze extended follow-up data from the study.
The NLST involved 53,452 men and women aged 55-74 years who were enrolled during 2002-2004 and who had at least a 30-pack-year history of cigarette smoking. The patients were randomly assigned to undergo lung cancer screening using either three annual low-dose CT exams or three annual single-view chest radiographs.
Mean follow-up was approximately 6 years. "At the end of the entire trial, there were 1,089 total lung cancer cases in the low-dose CT arm (649 detected by low-dose CT screening) and 969 cases in the [radiology] arm, for an excess of 120 cases. This gives [an] excess cancer rate of 18.5%," the investigators said (JAMA Intern. Med. 2013 Dec. 9 [doi:10.1001/jamainternmed.2013.12738]).
"The data from this study suggest that ... 18% of persons in the low-dose CT arm with screen-detected lung cancer and 22% of those in the low-dose CT arm with screen-detected NSCLC [non–small cell lung cancer] may be cases of overdiagnosis," Dr. Patz and his associates said. "In other words, if these individuals had not entered the NLST, they would not have received a lung cancer diagnosis or treatment, at least for the next 5 years."
In the future, the study authors noted, "once there are better biomarkers and imaging techniques to predict which individuals with a diagnosis of lung cancer will have more or less aggressive disease, treatment options can be optimized, and a mass screening program can become more valuable."
The National Institutes of Health supported the NSLT. No financial conflicts of interest were reported.
An estimated 18% of the early lung cancers detected by low-dose CT screening in the National Lung Screening Trial were likely indolent and probably represent overdiagnosis, according to a report published online Dec. 9 in JAMA Internal Medicine.
The National Lung Screening Trial (NLST) found "an encouraging" 20% relative reduction in lung cancer–specific mortality among high-risk patients who were screened using low-dose CT, compared with chest radiography. "These findings were met with enthusiasm, but before a widespread public health screening program is implemented, risks of screening also need to be considered," said Dr. Edward F. Patz Jr. of the department of radiology, Duke University Medical Center, Durham, N.C., and his associates in the NLST.
The chief risk in this case is overdiagnosis: identifying an early-stage lesion in an asymptomatic patient that would not progress or affect that patient’s long-term health. It is likely that some of the tumors detected on low-dose CT were just such indolent cancers, and that those patients unnecessarily underwent invasive diagnostic procedures, surgical resection, and multiple follow-up studies.
To estimate how many of the detected cancers in the NLST were indolent – and thus overdiagnosed – Dr. Patz and his colleagues used statistical probability methods to analyze extended follow-up data from the study.
The NLST involved 53,452 men and women aged 55-74 years who were enrolled during 2002-2004 and who had at least a 30-pack-year history of cigarette smoking. The patients were randomly assigned to undergo lung cancer screening using either three annual low-dose CT exams or three annual single-view chest radiographs.
Mean follow-up was approximately 6 years. "At the end of the entire trial, there were 1,089 total lung cancer cases in the low-dose CT arm (649 detected by low-dose CT screening) and 969 cases in the [radiology] arm, for an excess of 120 cases. This gives [an] excess cancer rate of 18.5%," the investigators said (JAMA Intern. Med. 2013 Dec. 9 [doi:10.1001/jamainternmed.2013.12738]).
"The data from this study suggest that ... 18% of persons in the low-dose CT arm with screen-detected lung cancer and 22% of those in the low-dose CT arm with screen-detected NSCLC [non–small cell lung cancer] may be cases of overdiagnosis," Dr. Patz and his associates said. "In other words, if these individuals had not entered the NLST, they would not have received a lung cancer diagnosis or treatment, at least for the next 5 years."
In the future, the study authors noted, "once there are better biomarkers and imaging techniques to predict which individuals with a diagnosis of lung cancer will have more or less aggressive disease, treatment options can be optimized, and a mass screening program can become more valuable."
The National Institutes of Health supported the NSLT. No financial conflicts of interest were reported.
FROM JAMA INTERNAL MEDICINE
Major Finding: An estimated 18% of lung cancers detected by low-dose CT screening in the National Lung Screening Trial were likely indolent and may represent cases of overdiagnosis.
Data Source: A secondary analysis of data from the NLST which involved 53,452 patients aged 55-74 years who were at high risk for lung cancer because of their history of heavy smoking.
Disclosures: The National Institutes of Health supported the NSLT. No financial conflicts of interest were reported.
CMS extends Stage 2 ‘meaningful use’ reporting through 2016
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
States take different paths in Medicaid expansion
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
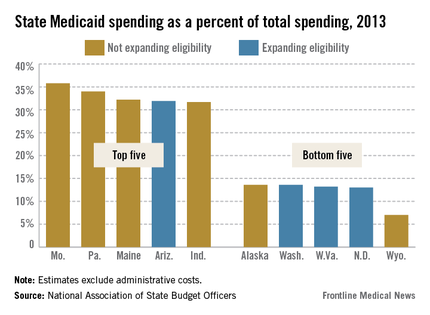
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
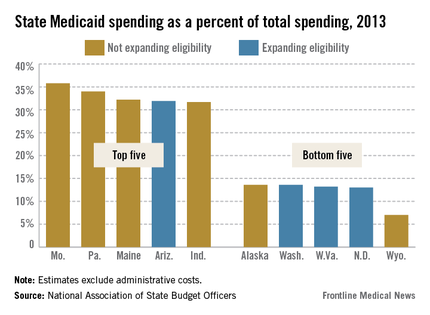
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
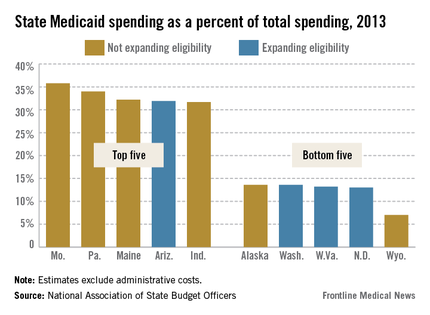
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
Laparoscopic hysterectomy appears less painful than robotic surgery
WASHINGTON – Patients who underwent a robotically assisted laparoscopic hysterectomy required significantly more postoperative analgesia than did those who had a conventional laparoscopic hysterectomy.
The findings of a retrospective review may help determine which procedure to go with, when postoperative pain is an important recovery factor, Dr. Megan Wasson said at a meeting sponsored by the AAGL.
Dr. Wasson, a fourth-year ob.gyn. resident at the Christiana Care Health System in Wilmington, Del., reviewed the postoperative analgesic requirements of 353 women who underwent minimally invasive hysterectomy for benign conditions at the facility from 2009 to 2012.
Among the group, 116 had a conventional procedure – 78 had a laparoscopic-assisted supracervical hysterectomy and 38 had a total laparoscopic hysterectomy. Robotically assisted hysterectomy was performed for 237 women – three of these were supracervical hysterectomies and 234 were total hysterectomies.
Because patients received different kinds of pain medication, Dr. Wasson and her colleagues converted all of the pain treatment to oxycodone equivalents.
While the oral oxycodone equivalent intake was not significantly different between the groups, the parenteral oxycodone equivalent was higher (14 mg vs. 26 mg). When both oral and parenteral were combined, the total oxycodone equivalent was 28 mg in the laparoscopic group and almost 38 mg in the robotically assisted group – a significant difference.
Women who had conventional laparoscopic surgery were significantly younger than those who had the robotically assisted surgery (42 vs. 46 years). Significantly more black than white women had laparoscopic surgery (51% vs.14%), while significantly more white women had robotically assisted surgery (83% vs. 41%). There were no differences in the rate of prior cesarean section, laparotomy, or laparoscopy.
The uterus was significantly larger in the laparoscopic group (281 g vs. 203 g). Significantly fewer of these women also had a concomitant salpingo-oophorectomy (25% vs. 29%). In the laparoscopic group, intraoperative blood loss was significantly less (131 mL vs. 170 mL), as was hemoglobin decrease (1.68 g/dL vs. 2.26 g/dL). The composite port size was significantly smaller (25.8 mm vs. 41.6 mm). Total procedure time was similar (176 vs. 170 minutes).
Dr. Wasson had no financial declarations.
WASHINGTON – Patients who underwent a robotically assisted laparoscopic hysterectomy required significantly more postoperative analgesia than did those who had a conventional laparoscopic hysterectomy.
The findings of a retrospective review may help determine which procedure to go with, when postoperative pain is an important recovery factor, Dr. Megan Wasson said at a meeting sponsored by the AAGL.
Dr. Wasson, a fourth-year ob.gyn. resident at the Christiana Care Health System in Wilmington, Del., reviewed the postoperative analgesic requirements of 353 women who underwent minimally invasive hysterectomy for benign conditions at the facility from 2009 to 2012.
Among the group, 116 had a conventional procedure – 78 had a laparoscopic-assisted supracervical hysterectomy and 38 had a total laparoscopic hysterectomy. Robotically assisted hysterectomy was performed for 237 women – three of these were supracervical hysterectomies and 234 were total hysterectomies.
Because patients received different kinds of pain medication, Dr. Wasson and her colleagues converted all of the pain treatment to oxycodone equivalents.
While the oral oxycodone equivalent intake was not significantly different between the groups, the parenteral oxycodone equivalent was higher (14 mg vs. 26 mg). When both oral and parenteral were combined, the total oxycodone equivalent was 28 mg in the laparoscopic group and almost 38 mg in the robotically assisted group – a significant difference.
Women who had conventional laparoscopic surgery were significantly younger than those who had the robotically assisted surgery (42 vs. 46 years). Significantly more black than white women had laparoscopic surgery (51% vs.14%), while significantly more white women had robotically assisted surgery (83% vs. 41%). There were no differences in the rate of prior cesarean section, laparotomy, or laparoscopy.
The uterus was significantly larger in the laparoscopic group (281 g vs. 203 g). Significantly fewer of these women also had a concomitant salpingo-oophorectomy (25% vs. 29%). In the laparoscopic group, intraoperative blood loss was significantly less (131 mL vs. 170 mL), as was hemoglobin decrease (1.68 g/dL vs. 2.26 g/dL). The composite port size was significantly smaller (25.8 mm vs. 41.6 mm). Total procedure time was similar (176 vs. 170 minutes).
Dr. Wasson had no financial declarations.
WASHINGTON – Patients who underwent a robotically assisted laparoscopic hysterectomy required significantly more postoperative analgesia than did those who had a conventional laparoscopic hysterectomy.
The findings of a retrospective review may help determine which procedure to go with, when postoperative pain is an important recovery factor, Dr. Megan Wasson said at a meeting sponsored by the AAGL.
Dr. Wasson, a fourth-year ob.gyn. resident at the Christiana Care Health System in Wilmington, Del., reviewed the postoperative analgesic requirements of 353 women who underwent minimally invasive hysterectomy for benign conditions at the facility from 2009 to 2012.
Among the group, 116 had a conventional procedure – 78 had a laparoscopic-assisted supracervical hysterectomy and 38 had a total laparoscopic hysterectomy. Robotically assisted hysterectomy was performed for 237 women – three of these were supracervical hysterectomies and 234 were total hysterectomies.
Because patients received different kinds of pain medication, Dr. Wasson and her colleagues converted all of the pain treatment to oxycodone equivalents.
While the oral oxycodone equivalent intake was not significantly different between the groups, the parenteral oxycodone equivalent was higher (14 mg vs. 26 mg). When both oral and parenteral were combined, the total oxycodone equivalent was 28 mg in the laparoscopic group and almost 38 mg in the robotically assisted group – a significant difference.
Women who had conventional laparoscopic surgery were significantly younger than those who had the robotically assisted surgery (42 vs. 46 years). Significantly more black than white women had laparoscopic surgery (51% vs.14%), while significantly more white women had robotically assisted surgery (83% vs. 41%). There were no differences in the rate of prior cesarean section, laparotomy, or laparoscopy.
The uterus was significantly larger in the laparoscopic group (281 g vs. 203 g). Significantly fewer of these women also had a concomitant salpingo-oophorectomy (25% vs. 29%). In the laparoscopic group, intraoperative blood loss was significantly less (131 mL vs. 170 mL), as was hemoglobin decrease (1.68 g/dL vs. 2.26 g/dL). The composite port size was significantly smaller (25.8 mm vs. 41.6 mm). Total procedure time was similar (176 vs. 170 minutes).
Dr. Wasson had no financial declarations.
AT THE AAGL GLOBAL CONGRESS
Major finding: Women who had a robotically assisted hysterectomy needed significantly more postoperative pain medication than did those who had a conventional laparoscopic hysterectomy.
Data source: The retrospective review included 353 women.
Disclosures: Dr. Wasson had no financial disclosures.