User login
Official Newspaper of the American College of Surgeons
Obama 2015 budget would extend Medicaid pay bump
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
CDC sounds alarm on hospital antibiotic use
A scathing new report by the Centers for Disease Control and Prevention found ample room for improvement in inpatient antibiotic prescribing.
Findings include continued overuse of antibiotics in hospitals, errors in prescribing, and the lifesaving potential of efforts to reduce antibiotic use:
• Physicians in some hospitals prescribed three times as many antibiotics as doctors in other hospitals, even though patients were being cared for in similar areas of each hospital.
• Antibiotic prescriptions contained an error in 37% of cases involving treatment for urinary tract infections or use of the common and critical drug, vancomycin (Vancocin).
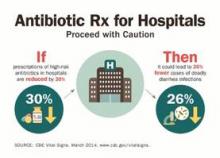
• Models predicted that a 30% decrease in the use of broad-spectrum antibiotics would lead to a 26% reduction in Clostridium difficile infections, which kill roughly 14,000 hospitalized patients each year.
"Antibiotics are often lifesaving, and we have to protect them before our medicine chests run empty," CDC director Tom Frieden said during a press conference highlighting the report, released in the CDC’s March 4 Morbidity and Mortality Weekly Report (MMWR 2014 March 4;63:1-7).
Dr. Frieden announced that the CDC’s fiscal 2015 budget, part of President Obama’s budget initiative rolled out today, contains a $30 million increase in funds to establish a robust infrastructure in the United States to detect antibiotic threats and protect patients and communities.
The new monies would allow the CDC to extend the "detect and protect" strategy to combat antibiotic resistance outlined last year, help support state and hospital efforts to implement antibiotic stewardship programs, and improve rapid detection of antimicrobial threats and outbreaks.
"One of the things that makes us so focused on antimicrobial resistance is that not only is it a really serious problem, but [also] it’s not too late," Dr. Frieden said.
If funded, he anticipates the CDC and other stakeholders will be able to reverse drug resistance and cut in half the rate of C. difficile and the "nightmare" carbapenem-resistant Enterobacteriaceae infections.
It was noted that robust efforts to improve the use of antibiotics associated with C. difficile in the United Kingdom have resulted in more than a 50% reduction in use of those targeted agents and a roughly 70% reduction in C. difficile infections over the past 6 to 7 years.
The CDC is strongly recommending that every hospital in the United States have an antibiotic stewardship program and is providing a new checklist to help facilities with the task. The checklist contains seven core elements of an effective program: leadership commitment; accountability for outcomes under a single leader; drug expertise under a single pharmacist leader; taking action on at least one prescribing improvement practice; tracking antibiotic prescribing and resistance patterns; reporting regularly to staff about these patterns; and educating staff on antibiotic resistance and improving prescribing practices.
Specific advice was also given to clinicians to order recommended cultures before antibiotics are given and to start drugs promptly; make sure the indication, dose, and expected duration are specified in the patient record; and reassess patients within 48 hours and adjust treatment, if necessary, or stop treatment, if indicated.
Concerns were raised during the briefing over whether voluntary strategies will curb interfacility transmission caused by transfers of patients with multidrug-resistant infections and the failure to report outbreaks between facilities. Dr. John R. Combes, the American Hospital Association’s senior vice president said several groups are working to smooth out these transfers and that the AHA’s "Hospitals in Pursuit of Excellence" program provides best practices to facilitate transfers and foster cooperation with surrounding facilities to prevent infections.
The new CDC report is based on a review of data from all 323 hospitals in the MarketScan Hospital Drug Database and from hospitals in the CDC’s Emerging Infections Program.
Antibiotics were prescribed for 55.7% of patients hospitalized in 2010 in the MarketScan Hospital Drug Database, with 30% receiving at least one dose of broad-spectrum antibiotics.
One or more antibiotics were used to treat active infections in 37% of 11,282 patients treated in 2011 at 183 acute care hospitals evaluated by the Emerging Infections Program. Half of the antibiotics were prescribed for one of three scenarios: lower respiratory tract infections (22.2%), urinary tract infections (14%), and suspected drug-resistant Gram-positive infections such as methicillin-resistant Staphylococcus aureus (17.6%).
The CDC previously called on physicians to address antibiotic resistance in its Antibiotic Threats in the United States, 2013 report and the 2013 Get Smart About Antibiotics Week. The issue also will be tackled in the CDC’s forthcoming Transatlantic Taskforce on Antimicrobial Resistance 2013 report, with additional research expected to focus on contributing factors that led to such wide variances in antibiotic use between hospitals.
Dr. Frieden and Dr. Combes reported having no financial disclosures.

|
| Dr. Franklin A. Michota |
Dr. Franklin A. Michota is director of academic affairs, department of hospital medicine, Cleveland Clinic. He reports having no disclosures.

|
| Dr. Franklin A. Michota |
Dr. Franklin A. Michota is director of academic affairs, department of hospital medicine, Cleveland Clinic. He reports having no disclosures.

|
| Dr. Franklin A. Michota |
Dr. Franklin A. Michota is director of academic affairs, department of hospital medicine, Cleveland Clinic. He reports having no disclosures.
A scathing new report by the Centers for Disease Control and Prevention found ample room for improvement in inpatient antibiotic prescribing.
Findings include continued overuse of antibiotics in hospitals, errors in prescribing, and the lifesaving potential of efforts to reduce antibiotic use:
• Physicians in some hospitals prescribed three times as many antibiotics as doctors in other hospitals, even though patients were being cared for in similar areas of each hospital.
• Antibiotic prescriptions contained an error in 37% of cases involving treatment for urinary tract infections or use of the common and critical drug, vancomycin (Vancocin).
• Models predicted that a 30% decrease in the use of broad-spectrum antibiotics would lead to a 26% reduction in Clostridium difficile infections, which kill roughly 14,000 hospitalized patients each year.
"Antibiotics are often lifesaving, and we have to protect them before our medicine chests run empty," CDC director Tom Frieden said during a press conference highlighting the report, released in the CDC’s March 4 Morbidity and Mortality Weekly Report (MMWR 2014 March 4;63:1-7).
Dr. Frieden announced that the CDC’s fiscal 2015 budget, part of President Obama’s budget initiative rolled out today, contains a $30 million increase in funds to establish a robust infrastructure in the United States to detect antibiotic threats and protect patients and communities.
The new monies would allow the CDC to extend the "detect and protect" strategy to combat antibiotic resistance outlined last year, help support state and hospital efforts to implement antibiotic stewardship programs, and improve rapid detection of antimicrobial threats and outbreaks.
"One of the things that makes us so focused on antimicrobial resistance is that not only is it a really serious problem, but [also] it’s not too late," Dr. Frieden said.
If funded, he anticipates the CDC and other stakeholders will be able to reverse drug resistance and cut in half the rate of C. difficile and the "nightmare" carbapenem-resistant Enterobacteriaceae infections.
It was noted that robust efforts to improve the use of antibiotics associated with C. difficile in the United Kingdom have resulted in more than a 50% reduction in use of those targeted agents and a roughly 70% reduction in C. difficile infections over the past 6 to 7 years.
The CDC is strongly recommending that every hospital in the United States have an antibiotic stewardship program and is providing a new checklist to help facilities with the task. The checklist contains seven core elements of an effective program: leadership commitment; accountability for outcomes under a single leader; drug expertise under a single pharmacist leader; taking action on at least one prescribing improvement practice; tracking antibiotic prescribing and resistance patterns; reporting regularly to staff about these patterns; and educating staff on antibiotic resistance and improving prescribing practices.
Specific advice was also given to clinicians to order recommended cultures before antibiotics are given and to start drugs promptly; make sure the indication, dose, and expected duration are specified in the patient record; and reassess patients within 48 hours and adjust treatment, if necessary, or stop treatment, if indicated.
Concerns were raised during the briefing over whether voluntary strategies will curb interfacility transmission caused by transfers of patients with multidrug-resistant infections and the failure to report outbreaks between facilities. Dr. John R. Combes, the American Hospital Association’s senior vice president said several groups are working to smooth out these transfers and that the AHA’s "Hospitals in Pursuit of Excellence" program provides best practices to facilitate transfers and foster cooperation with surrounding facilities to prevent infections.
The new CDC report is based on a review of data from all 323 hospitals in the MarketScan Hospital Drug Database and from hospitals in the CDC’s Emerging Infections Program.
Antibiotics were prescribed for 55.7% of patients hospitalized in 2010 in the MarketScan Hospital Drug Database, with 30% receiving at least one dose of broad-spectrum antibiotics.
One or more antibiotics were used to treat active infections in 37% of 11,282 patients treated in 2011 at 183 acute care hospitals evaluated by the Emerging Infections Program. Half of the antibiotics were prescribed for one of three scenarios: lower respiratory tract infections (22.2%), urinary tract infections (14%), and suspected drug-resistant Gram-positive infections such as methicillin-resistant Staphylococcus aureus (17.6%).
The CDC previously called on physicians to address antibiotic resistance in its Antibiotic Threats in the United States, 2013 report and the 2013 Get Smart About Antibiotics Week. The issue also will be tackled in the CDC’s forthcoming Transatlantic Taskforce on Antimicrobial Resistance 2013 report, with additional research expected to focus on contributing factors that led to such wide variances in antibiotic use between hospitals.
Dr. Frieden and Dr. Combes reported having no financial disclosures.
A scathing new report by the Centers for Disease Control and Prevention found ample room for improvement in inpatient antibiotic prescribing.
Findings include continued overuse of antibiotics in hospitals, errors in prescribing, and the lifesaving potential of efforts to reduce antibiotic use:
• Physicians in some hospitals prescribed three times as many antibiotics as doctors in other hospitals, even though patients were being cared for in similar areas of each hospital.
• Antibiotic prescriptions contained an error in 37% of cases involving treatment for urinary tract infections or use of the common and critical drug, vancomycin (Vancocin).
• Models predicted that a 30% decrease in the use of broad-spectrum antibiotics would lead to a 26% reduction in Clostridium difficile infections, which kill roughly 14,000 hospitalized patients each year.
"Antibiotics are often lifesaving, and we have to protect them before our medicine chests run empty," CDC director Tom Frieden said during a press conference highlighting the report, released in the CDC’s March 4 Morbidity and Mortality Weekly Report (MMWR 2014 March 4;63:1-7).
Dr. Frieden announced that the CDC’s fiscal 2015 budget, part of President Obama’s budget initiative rolled out today, contains a $30 million increase in funds to establish a robust infrastructure in the United States to detect antibiotic threats and protect patients and communities.
The new monies would allow the CDC to extend the "detect and protect" strategy to combat antibiotic resistance outlined last year, help support state and hospital efforts to implement antibiotic stewardship programs, and improve rapid detection of antimicrobial threats and outbreaks.
"One of the things that makes us so focused on antimicrobial resistance is that not only is it a really serious problem, but [also] it’s not too late," Dr. Frieden said.
If funded, he anticipates the CDC and other stakeholders will be able to reverse drug resistance and cut in half the rate of C. difficile and the "nightmare" carbapenem-resistant Enterobacteriaceae infections.
It was noted that robust efforts to improve the use of antibiotics associated with C. difficile in the United Kingdom have resulted in more than a 50% reduction in use of those targeted agents and a roughly 70% reduction in C. difficile infections over the past 6 to 7 years.
The CDC is strongly recommending that every hospital in the United States have an antibiotic stewardship program and is providing a new checklist to help facilities with the task. The checklist contains seven core elements of an effective program: leadership commitment; accountability for outcomes under a single leader; drug expertise under a single pharmacist leader; taking action on at least one prescribing improvement practice; tracking antibiotic prescribing and resistance patterns; reporting regularly to staff about these patterns; and educating staff on antibiotic resistance and improving prescribing practices.
Specific advice was also given to clinicians to order recommended cultures before antibiotics are given and to start drugs promptly; make sure the indication, dose, and expected duration are specified in the patient record; and reassess patients within 48 hours and adjust treatment, if necessary, or stop treatment, if indicated.
Concerns were raised during the briefing over whether voluntary strategies will curb interfacility transmission caused by transfers of patients with multidrug-resistant infections and the failure to report outbreaks between facilities. Dr. John R. Combes, the American Hospital Association’s senior vice president said several groups are working to smooth out these transfers and that the AHA’s "Hospitals in Pursuit of Excellence" program provides best practices to facilitate transfers and foster cooperation with surrounding facilities to prevent infections.
The new CDC report is based on a review of data from all 323 hospitals in the MarketScan Hospital Drug Database and from hospitals in the CDC’s Emerging Infections Program.
Antibiotics were prescribed for 55.7% of patients hospitalized in 2010 in the MarketScan Hospital Drug Database, with 30% receiving at least one dose of broad-spectrum antibiotics.
One or more antibiotics were used to treat active infections in 37% of 11,282 patients treated in 2011 at 183 acute care hospitals evaluated by the Emerging Infections Program. Half of the antibiotics were prescribed for one of three scenarios: lower respiratory tract infections (22.2%), urinary tract infections (14%), and suspected drug-resistant Gram-positive infections such as methicillin-resistant Staphylococcus aureus (17.6%).
The CDC previously called on physicians to address antibiotic resistance in its Antibiotic Threats in the United States, 2013 report and the 2013 Get Smart About Antibiotics Week. The issue also will be tackled in the CDC’s forthcoming Transatlantic Taskforce on Antimicrobial Resistance 2013 report, with additional research expected to focus on contributing factors that led to such wide variances in antibiotic use between hospitals.
Dr. Frieden and Dr. Combes reported having no financial disclosures.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Disclosure programs reduce lawsuits, but bring challenges
Disclosure and apology programs may be one answer to reducing malpractice litigation against physicians, hospitals, and other health care providers.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million dollars since 2010.
"Through effectively communicating, you can eliminate a whole lot of lawsuits [in which] the patients and families are suing you just because they want answers," said Dr. Tim McDonald, chief safety and risk officer for health affairs for the system. "We think that’s one of the big keys to substantially reducing malpractice costs."
So-called communication and resolution programs (CRPs) involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if deemed necessary.
Under such programs, physicians or administrators immediately communicate with patients after a poor medical outcome or questionable circumstance and explain that the event is being rapidly investigated.
Once investigation is complete, risk managers or administrators discuss the findings with the patient and the clinician. The team admits any errors and provides an apology to the patient or family if harm was caused. If care was deemed substandard, administrators offer the patient or family appropriate compensation. In the event the care was deemed reasonable, the involved physician and risk manager explain their conclusions and seek understanding, but commit to defending the clinician in court, if necessary.
The CRP program at Illinois was modeled after a similar program at the University of Michigan Health System, Ann Arbor, which started in late 2001. Since the program began, the average legal expenses per case has been cut at least in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100/year.
Contributing factors to the success of six early adopters – including the Michigan and Illinois programs – included sufficient resources to fund the ventures, a passionate program advocate, and strong marketing, according to an analysis in the journal Health Affairs.
"The things that really distinguished [the successful early adopters] from the later adopters were they had an incredibly strong champion of the program who made it his job to build the program full time," said Michelle Mello, J.D., Ph.D., director of the law and public health program at Harvard School of Public Health, Boston (Health Aff. 2014;33:120-9).
Ascension Health, a large system of more than 1,900 hospitals in 23 states and the District of Columbia, saw a 52% decrease in the total number of actual and potential liability cases in a demonstration project of an obstetrical CRP (Health Aff. 2014;33:139-45).
The program included the immediate reporting of unexpected events, investigation, documentation and causal analysis, as well as having staff fully disclose unexpected events to patients and families. To do so, each of five hospitals in the pilot created an Obstetrics Event Response Team that consisted of an obstetrician, a neonatologist, an obstetrics nurse manager, a risk manager, and a medical coder.
Following training, the teams became accountable for immediate identification and reporting of any event that resulted in patient harm, expedited investigation of the event, prompt and ongoing disclosure, early resolution of events involving probable liability, and accessing lessons learned from each event to improve patient care.
In just over 3 years after implementation of the demonstration project, the rate of full disclosures more than doubled (221% increase in full disclosures).
"Based on the success of the ... demonstration project, Ascension Health has begun to spread the care model – including electronic fetal monitoring (EFM) and shoulder dystocia e-learning stimulation, TeamSTEPPS training, disclosure and root cause analysis training, and implementation of the Ascension Health shoulder dystocia bundle – as a standard for all obstetrics units throughout the health system," said Ann Hendrich, RN, Ph.D., senior vice president for quality and safety at Ascension Health.
Adoption of CRPs is not without challenges. Participants at five of the six early adoption sites reported practical challenges in educating physicians about the program. Program founders initially struggled to soothe physicians’ skepticism and discomfort with making disclosures to patients. Strong communication by administrators and trust building with physicians was key in overcoming these obstacles, Dr. Mello and her colleagues found.
CRPs would be easier to implement if the current legal and governmental environment supported them, health care experts said (Health Aff. 2014 33:111-19). State laws that prohibit using health care providers’ apologies against them in court would go far to support CRPs. Currently, more than 30 states have some form of apology statute aimed at physicians and other health care providers, but the extent of legal protection differs.
Pennsylvania was the latest state to enact an apology protection law. The statute, which became effective in December 2013, shields any physician action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses."
So far, "there have not been any reports or complaints about the new law coming into the medical society," said Chuck Moran, director of media relations and public affairs at the Pennsylvania Medical Society. "That could be a good sign, or it could mean it’s too early to tell."
Disclosure and apology programs may be one answer to reducing malpractice litigation against physicians, hospitals, and other health care providers.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million dollars since 2010.
"Through effectively communicating, you can eliminate a whole lot of lawsuits [in which] the patients and families are suing you just because they want answers," said Dr. Tim McDonald, chief safety and risk officer for health affairs for the system. "We think that’s one of the big keys to substantially reducing malpractice costs."
So-called communication and resolution programs (CRPs) involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if deemed necessary.
Under such programs, physicians or administrators immediately communicate with patients after a poor medical outcome or questionable circumstance and explain that the event is being rapidly investigated.
Once investigation is complete, risk managers or administrators discuss the findings with the patient and the clinician. The team admits any errors and provides an apology to the patient or family if harm was caused. If care was deemed substandard, administrators offer the patient or family appropriate compensation. In the event the care was deemed reasonable, the involved physician and risk manager explain their conclusions and seek understanding, but commit to defending the clinician in court, if necessary.
The CRP program at Illinois was modeled after a similar program at the University of Michigan Health System, Ann Arbor, which started in late 2001. Since the program began, the average legal expenses per case has been cut at least in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100/year.
Contributing factors to the success of six early adopters – including the Michigan and Illinois programs – included sufficient resources to fund the ventures, a passionate program advocate, and strong marketing, according to an analysis in the journal Health Affairs.
"The things that really distinguished [the successful early adopters] from the later adopters were they had an incredibly strong champion of the program who made it his job to build the program full time," said Michelle Mello, J.D., Ph.D., director of the law and public health program at Harvard School of Public Health, Boston (Health Aff. 2014;33:120-9).
Ascension Health, a large system of more than 1,900 hospitals in 23 states and the District of Columbia, saw a 52% decrease in the total number of actual and potential liability cases in a demonstration project of an obstetrical CRP (Health Aff. 2014;33:139-45).
The program included the immediate reporting of unexpected events, investigation, documentation and causal analysis, as well as having staff fully disclose unexpected events to patients and families. To do so, each of five hospitals in the pilot created an Obstetrics Event Response Team that consisted of an obstetrician, a neonatologist, an obstetrics nurse manager, a risk manager, and a medical coder.
Following training, the teams became accountable for immediate identification and reporting of any event that resulted in patient harm, expedited investigation of the event, prompt and ongoing disclosure, early resolution of events involving probable liability, and accessing lessons learned from each event to improve patient care.
In just over 3 years after implementation of the demonstration project, the rate of full disclosures more than doubled (221% increase in full disclosures).
"Based on the success of the ... demonstration project, Ascension Health has begun to spread the care model – including electronic fetal monitoring (EFM) and shoulder dystocia e-learning stimulation, TeamSTEPPS training, disclosure and root cause analysis training, and implementation of the Ascension Health shoulder dystocia bundle – as a standard for all obstetrics units throughout the health system," said Ann Hendrich, RN, Ph.D., senior vice president for quality and safety at Ascension Health.
Adoption of CRPs is not without challenges. Participants at five of the six early adoption sites reported practical challenges in educating physicians about the program. Program founders initially struggled to soothe physicians’ skepticism and discomfort with making disclosures to patients. Strong communication by administrators and trust building with physicians was key in overcoming these obstacles, Dr. Mello and her colleagues found.
CRPs would be easier to implement if the current legal and governmental environment supported them, health care experts said (Health Aff. 2014 33:111-19). State laws that prohibit using health care providers’ apologies against them in court would go far to support CRPs. Currently, more than 30 states have some form of apology statute aimed at physicians and other health care providers, but the extent of legal protection differs.
Pennsylvania was the latest state to enact an apology protection law. The statute, which became effective in December 2013, shields any physician action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses."
So far, "there have not been any reports or complaints about the new law coming into the medical society," said Chuck Moran, director of media relations and public affairs at the Pennsylvania Medical Society. "That could be a good sign, or it could mean it’s too early to tell."
Disclosure and apology programs may be one answer to reducing malpractice litigation against physicians, hospitals, and other health care providers.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million dollars since 2010.
"Through effectively communicating, you can eliminate a whole lot of lawsuits [in which] the patients and families are suing you just because they want answers," said Dr. Tim McDonald, chief safety and risk officer for health affairs for the system. "We think that’s one of the big keys to substantially reducing malpractice costs."
So-called communication and resolution programs (CRPs) involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if deemed necessary.
Under such programs, physicians or administrators immediately communicate with patients after a poor medical outcome or questionable circumstance and explain that the event is being rapidly investigated.
Once investigation is complete, risk managers or administrators discuss the findings with the patient and the clinician. The team admits any errors and provides an apology to the patient or family if harm was caused. If care was deemed substandard, administrators offer the patient or family appropriate compensation. In the event the care was deemed reasonable, the involved physician and risk manager explain their conclusions and seek understanding, but commit to defending the clinician in court, if necessary.
The CRP program at Illinois was modeled after a similar program at the University of Michigan Health System, Ann Arbor, which started in late 2001. Since the program began, the average legal expenses per case has been cut at least in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100/year.
Contributing factors to the success of six early adopters – including the Michigan and Illinois programs – included sufficient resources to fund the ventures, a passionate program advocate, and strong marketing, according to an analysis in the journal Health Affairs.
"The things that really distinguished [the successful early adopters] from the later adopters were they had an incredibly strong champion of the program who made it his job to build the program full time," said Michelle Mello, J.D., Ph.D., director of the law and public health program at Harvard School of Public Health, Boston (Health Aff. 2014;33:120-9).
Ascension Health, a large system of more than 1,900 hospitals in 23 states and the District of Columbia, saw a 52% decrease in the total number of actual and potential liability cases in a demonstration project of an obstetrical CRP (Health Aff. 2014;33:139-45).
The program included the immediate reporting of unexpected events, investigation, documentation and causal analysis, as well as having staff fully disclose unexpected events to patients and families. To do so, each of five hospitals in the pilot created an Obstetrics Event Response Team that consisted of an obstetrician, a neonatologist, an obstetrics nurse manager, a risk manager, and a medical coder.
Following training, the teams became accountable for immediate identification and reporting of any event that resulted in patient harm, expedited investigation of the event, prompt and ongoing disclosure, early resolution of events involving probable liability, and accessing lessons learned from each event to improve patient care.
In just over 3 years after implementation of the demonstration project, the rate of full disclosures more than doubled (221% increase in full disclosures).
"Based on the success of the ... demonstration project, Ascension Health has begun to spread the care model – including electronic fetal monitoring (EFM) and shoulder dystocia e-learning stimulation, TeamSTEPPS training, disclosure and root cause analysis training, and implementation of the Ascension Health shoulder dystocia bundle – as a standard for all obstetrics units throughout the health system," said Ann Hendrich, RN, Ph.D., senior vice president for quality and safety at Ascension Health.
Adoption of CRPs is not without challenges. Participants at five of the six early adoption sites reported practical challenges in educating physicians about the program. Program founders initially struggled to soothe physicians’ skepticism and discomfort with making disclosures to patients. Strong communication by administrators and trust building with physicians was key in overcoming these obstacles, Dr. Mello and her colleagues found.
CRPs would be easier to implement if the current legal and governmental environment supported them, health care experts said (Health Aff. 2014 33:111-19). State laws that prohibit using health care providers’ apologies against them in court would go far to support CRPs. Currently, more than 30 states have some form of apology statute aimed at physicians and other health care providers, but the extent of legal protection differs.
Pennsylvania was the latest state to enact an apology protection law. The statute, which became effective in December 2013, shields any physician action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses."
So far, "there have not been any reports or complaints about the new law coming into the medical society," said Chuck Moran, director of media relations and public affairs at the Pennsylvania Medical Society. "That could be a good sign, or it could mean it’s too early to tell."
New takeaways from the Boston Marathon bombings
NAPLES, FLA. – Without a single life lost at area hospitals, the medical response to the Boston Marathon bombings was by all accounts remarkable. But what if police and other first-responders had tourniquets and were trained in their use?
As it was, advanced topical hemostatic agents and tourniquets were MIA in the field, forcing all but one prehospital tourniquet to be improvised, according to Massachusetts General Hospital trauma surgeon Lt. Col. David King, U. S. Army Reserve.
"It’s abundantly clear from the literature that improvised tourniquets almost never work," he said. "The fact that every soldier down range has one in his pocket and we couldn’t muster up more than one in the city of Boston is a shame and we need to rectify that."
In all, there were 66 limb injuries, with 29 patients having recognized limb exsanguination at the scene. Of the 27 tourniquets applied, 26 were improvised.
Failure to translate this important lesson from military experience meant that these homemade devices were most likely wildly ineffective and, in some cases, may have even exacerbated blood loss, he said. Surprisingly, there’s no formal protocol for tourniquet application or training paradigm in Massachusetts, such that exists in the Army’s prehospital Tactical Combat Casualty Care handbook.
"If you look across the paramedic medical guidelines, there is no protocol on the right, evidence-based way to put on a tourniquet or what the indications are for a tourniquet," Dr. King said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). "We don’t have it, and we need to" have it nationwide.
EAST is hoping to provide some guidance in this area with the development of practice management guidelines (PMG) for tourniquet use in extremity trauma. Dr. King, who heads this PMG committee, reported at the meeting that the guidelines, due out later this year, will emphasize that commercially made tourniquets should be available in the prehospital setting, improvised tourniquets rarely work and cannot be recommended; essentially all commercially made tourniquets are equieffective; and that nonmedical personnel can be trained to correctly apply a proper tourniquet.
The need for bleeding control equipment and training for the public has not gone unnoticed by other stakeholders and is the central focus of the newest statement from the Hartford Consensus, a collaborative group of trauma surgeons, law enforcement officers, and emergency responders led by the American College of Surgeons (J. Am. Coll. Surg. 2014;218:467-75).
In dissecting the medical response to the Boston bombings, much has been made of the fact that Boston is home to six Level 1 trauma centers, and that it was race day, a city holiday, 3 p.m., and low-yield devices were used. Dr. King, however, gave high praise to an unsung hero, the Boston EMS loading officer who managed most of the transport destination decisions and smartly distributed critical cases throughout the area’s hospitals.
All critical patients were evacuated within 1 hour, but some have argued this could have been accomplished more quickly were it not for a "stay-and-play" mentality in the medical tent. The after-action review suggests there probably were enough ambulances to do the job in 30 minutes, said Dr. King, who remarked that the only thing that matters in critical trauma cases is time to surgical hemorrhage control.
"This will remain a controversial issue for Boston, whether staying and playing in the medical tent was a good idea," he said. "I don’t know what the right answer is."
Credit was also given to Massachusetts General, and many of the other city hospitals, for their insistence on regular full-scale drills that allowed quick lock-down of the facility to control access and manage the surge capacity in the emergency department.
"It’s more than just a tabletop exercise," Dr. King said. "When we test the surge capacity, we actually empty the emergency room for real. Usually, it occurs between 5:00 and 7:00 or 4:30 and 7:30 in the morning, but actually doing these things was useful, because when it came time to do it for real, no one was tripping over their own feet."
ED volume on that April afternoon was reduced from 97 patients to just 39 within 1.5 hours. Nontrauma physicians, including psychiatrists, did their part by writing "barebones orders" to get patients transferred to the wards.
Staff at Massachusetts General treated 43 patients, performing nine emergent operations, six amputations, two laparotomies, and one thoracotomy, with two traumatic arrests within the first 72 hours. As with other Boston hospitals, there were no in-hospital deaths, he said.
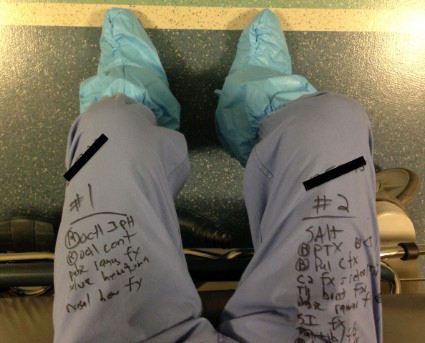
Patients arrived in such rapid succession, however, that it slowed the electronic medical record system and forced staff to use sequential record numbers, which can be dangerous. Registration couldn’t keep up and orders couldn’t be put in fast enough with 43 patients arriving in roughly 35 minutes, Dr. King explained. Workarounds were often old-school, and reminiscent of his days as a green trauma surgeon serving at Ibn Sina Hospital, Baghdad, Iraq.
"In the midst of this entire event, I turned to my nurse practitioner and asked for x, y, z information on a particular patient," he said. "She didn’t turn to her tablet or desktop computer in the operating room. She pulled out a piece of paper where she’d written all the relevant information. At the end of the event, I looked down and realized I’d done the same thing. I was keeping track of my patients on my pants with a Sharpie."
King describes this as a failure of technology and translation from the battlefield, but noted that the hospital did use the military’s practice of reviewing a critical event. Once they’d finished in the operating room and achieved hemorrhage and contamination control, the entire trauma team was reassembled. They did detailed tertiary trauma surveys and went back through every single patient to determine what additional studies they needed, what injuries had been missed.
"It was remarkable the number of things that were missed," Dr. King said. "No one was bleeding to death, but tons and tons of [small, non–life threatening] missed injuries [like ruptured ear drums], and to me this was one of the more important events that surrounded our response to the entire bombing – sitting down after the dust had settled and carefully going over every patient’s medical record."
Dr. King reported having no financial disclosures.
Lt. Col. King makes some excellent points. However, despite Dr. King's combat medicine experience, his contribution to this article reveals a gap that still exists between field medicine and hospital medicine.
The case against improvised tourniquets
There is no consensus on the definition of an "improvised" tourniquet. Homemade applications such as neckties and sticks are defined as improvised, but the Boston EMS kits (surgical tubing and Kelly clamps) also could be considered improvised. All of these methods may sound primitive since the advent of Combat-Application Tourniquets; however CATS are relatively new to the scene. Should we consider every tourniquet applied prior to their introduction to have been improvised? For the price of one CAT, we can assemble 10 tourniquet kits. And if Dr. King's initial contention was that tourniquets were in short supply, then it is a better system to deploy as many as possible. This point may be moot, however, because since the Boston bombing incident, federal grant money has allowed the purchase of CAT units in great numbers within the Metro-Boston area.
Tourniquet efficacy
"It is abundantly clear from the literature that improvised tourniquets almost never work." I feel this study had the wrong focus. Rather than ask which tourniquets have a better success rate, the study should have asked whose tourniquets have a better success rate.
Study after study has shown that successful intubation rates have little to do with the level of training of the practitioner, and everything to do with the frequency of intubation. More tubes equal more successful passes. I propose that this applies to tourniquet application as well. Field personnel who do not practice or have the opportunity to apply tourniquets frequently (which is the great majority of us) may not be applying tourniquets properly. This is why we instituted a massive tourniquet training and review program almost immediately following the 2013 bombing at the Boston Marathon.
Another point not addressed in studies is the effectiveness of nonresponder tourniquets. I would contend that an experienced practitioner with a necktie and a stick would be more successful in hemorrhage control that a civilian with a CAT, but those data have not been explored yet either.
The Loading Officer as unsung hero
All our Action Area Officers performed brilliantly (full disclosure, I was the Loading Officer). However the term Loading Officer is a misnomer. Yes, there is a Loading Officer, but there is actually a Loading Team. It consists of staff at the scene who liaise with the treatment areas and the true unsung heroes, the staff in the Operations Division or Dispatch Center. Dispatchers are in constant contact with the hospitals, scene operations, as well as continuing city service. They perform the hospital destination designations because they have a global sense of traffic, while at the scene we have only a worm's-eye view.
The stay-and-play critique
"All critical patients were evacuated within 1 hour, but some argued this could have been accomplished more quickly were it not for a 'stay-and-play' mentality." I take exception to this assertion. First, the point is contradictory. All critical patients were evacuated within 1 hour, but there was a stay-and-play mentality? Every EMT and paramedic knows that transport times translate into positive results with trauma.
Emergency personnel are taught that what matters most in trauma survival is not basic life support, advance life support, or wheelbarrow, but getting them to the ED fast. Yes, there were slowdowns in the medical tents, but most of delays came from non-EMS personnel who were not well versed in field medicine. We questioned, pleaded, and ultimately ordered some practitioners away from patients as they were attempting to perform procedures that we would never attempt on a trauma patient in the field. This is by no means a condemnation on my part. The staff we worked with was exceptional, and I witnessed true skill, heroism, and compassion. But it also demonstrated to me that a disconnect exists between field medicine and hospital medicine.
I see an opportunity here for training to better acclimate responders to working together with our hospital counterparts. We also need hospital personnel to be oriented to realities and limitations of field medicine.
Lt. Brian Pomodoro is a member of the Boston EMS.
Lt. Col. King makes some excellent points. However, despite Dr. King's combat medicine experience, his contribution to this article reveals a gap that still exists between field medicine and hospital medicine.
The case against improvised tourniquets
There is no consensus on the definition of an "improvised" tourniquet. Homemade applications such as neckties and sticks are defined as improvised, but the Boston EMS kits (surgical tubing and Kelly clamps) also could be considered improvised. All of these methods may sound primitive since the advent of Combat-Application Tourniquets; however CATS are relatively new to the scene. Should we consider every tourniquet applied prior to their introduction to have been improvised? For the price of one CAT, we can assemble 10 tourniquet kits. And if Dr. King's initial contention was that tourniquets were in short supply, then it is a better system to deploy as many as possible. This point may be moot, however, because since the Boston bombing incident, federal grant money has allowed the purchase of CAT units in great numbers within the Metro-Boston area.
Tourniquet efficacy
"It is abundantly clear from the literature that improvised tourniquets almost never work." I feel this study had the wrong focus. Rather than ask which tourniquets have a better success rate, the study should have asked whose tourniquets have a better success rate.
Study after study has shown that successful intubation rates have little to do with the level of training of the practitioner, and everything to do with the frequency of intubation. More tubes equal more successful passes. I propose that this applies to tourniquet application as well. Field personnel who do not practice or have the opportunity to apply tourniquets frequently (which is the great majority of us) may not be applying tourniquets properly. This is why we instituted a massive tourniquet training and review program almost immediately following the 2013 bombing at the Boston Marathon.
Another point not addressed in studies is the effectiveness of nonresponder tourniquets. I would contend that an experienced practitioner with a necktie and a stick would be more successful in hemorrhage control that a civilian with a CAT, but those data have not been explored yet either.
The Loading Officer as unsung hero
All our Action Area Officers performed brilliantly (full disclosure, I was the Loading Officer). However the term Loading Officer is a misnomer. Yes, there is a Loading Officer, but there is actually a Loading Team. It consists of staff at the scene who liaise with the treatment areas and the true unsung heroes, the staff in the Operations Division or Dispatch Center. Dispatchers are in constant contact with the hospitals, scene operations, as well as continuing city service. They perform the hospital destination designations because they have a global sense of traffic, while at the scene we have only a worm's-eye view.
The stay-and-play critique
"All critical patients were evacuated within 1 hour, but some argued this could have been accomplished more quickly were it not for a 'stay-and-play' mentality." I take exception to this assertion. First, the point is contradictory. All critical patients were evacuated within 1 hour, but there was a stay-and-play mentality? Every EMT and paramedic knows that transport times translate into positive results with trauma.
Emergency personnel are taught that what matters most in trauma survival is not basic life support, advance life support, or wheelbarrow, but getting them to the ED fast. Yes, there were slowdowns in the medical tents, but most of delays came from non-EMS personnel who were not well versed in field medicine. We questioned, pleaded, and ultimately ordered some practitioners away from patients as they were attempting to perform procedures that we would never attempt on a trauma patient in the field. This is by no means a condemnation on my part. The staff we worked with was exceptional, and I witnessed true skill, heroism, and compassion. But it also demonstrated to me that a disconnect exists between field medicine and hospital medicine.
I see an opportunity here for training to better acclimate responders to working together with our hospital counterparts. We also need hospital personnel to be oriented to realities and limitations of field medicine.
Lt. Brian Pomodoro is a member of the Boston EMS.
Lt. Col. King makes some excellent points. However, despite Dr. King's combat medicine experience, his contribution to this article reveals a gap that still exists between field medicine and hospital medicine.
The case against improvised tourniquets
There is no consensus on the definition of an "improvised" tourniquet. Homemade applications such as neckties and sticks are defined as improvised, but the Boston EMS kits (surgical tubing and Kelly clamps) also could be considered improvised. All of these methods may sound primitive since the advent of Combat-Application Tourniquets; however CATS are relatively new to the scene. Should we consider every tourniquet applied prior to their introduction to have been improvised? For the price of one CAT, we can assemble 10 tourniquet kits. And if Dr. King's initial contention was that tourniquets were in short supply, then it is a better system to deploy as many as possible. This point may be moot, however, because since the Boston bombing incident, federal grant money has allowed the purchase of CAT units in great numbers within the Metro-Boston area.
Tourniquet efficacy
"It is abundantly clear from the literature that improvised tourniquets almost never work." I feel this study had the wrong focus. Rather than ask which tourniquets have a better success rate, the study should have asked whose tourniquets have a better success rate.
Study after study has shown that successful intubation rates have little to do with the level of training of the practitioner, and everything to do with the frequency of intubation. More tubes equal more successful passes. I propose that this applies to tourniquet application as well. Field personnel who do not practice or have the opportunity to apply tourniquets frequently (which is the great majority of us) may not be applying tourniquets properly. This is why we instituted a massive tourniquet training and review program almost immediately following the 2013 bombing at the Boston Marathon.
Another point not addressed in studies is the effectiveness of nonresponder tourniquets. I would contend that an experienced practitioner with a necktie and a stick would be more successful in hemorrhage control that a civilian with a CAT, but those data have not been explored yet either.
The Loading Officer as unsung hero
All our Action Area Officers performed brilliantly (full disclosure, I was the Loading Officer). However the term Loading Officer is a misnomer. Yes, there is a Loading Officer, but there is actually a Loading Team. It consists of staff at the scene who liaise with the treatment areas and the true unsung heroes, the staff in the Operations Division or Dispatch Center. Dispatchers are in constant contact with the hospitals, scene operations, as well as continuing city service. They perform the hospital destination designations because they have a global sense of traffic, while at the scene we have only a worm's-eye view.
The stay-and-play critique
"All critical patients were evacuated within 1 hour, but some argued this could have been accomplished more quickly were it not for a 'stay-and-play' mentality." I take exception to this assertion. First, the point is contradictory. All critical patients were evacuated within 1 hour, but there was a stay-and-play mentality? Every EMT and paramedic knows that transport times translate into positive results with trauma.
Emergency personnel are taught that what matters most in trauma survival is not basic life support, advance life support, or wheelbarrow, but getting them to the ED fast. Yes, there were slowdowns in the medical tents, but most of delays came from non-EMS personnel who were not well versed in field medicine. We questioned, pleaded, and ultimately ordered some practitioners away from patients as they were attempting to perform procedures that we would never attempt on a trauma patient in the field. This is by no means a condemnation on my part. The staff we worked with was exceptional, and I witnessed true skill, heroism, and compassion. But it also demonstrated to me that a disconnect exists between field medicine and hospital medicine.
I see an opportunity here for training to better acclimate responders to working together with our hospital counterparts. We also need hospital personnel to be oriented to realities and limitations of field medicine.
Lt. Brian Pomodoro is a member of the Boston EMS.
NAPLES, FLA. – Without a single life lost at area hospitals, the medical response to the Boston Marathon bombings was by all accounts remarkable. But what if police and other first-responders had tourniquets and were trained in their use?
As it was, advanced topical hemostatic agents and tourniquets were MIA in the field, forcing all but one prehospital tourniquet to be improvised, according to Massachusetts General Hospital trauma surgeon Lt. Col. David King, U. S. Army Reserve.
"It’s abundantly clear from the literature that improvised tourniquets almost never work," he said. "The fact that every soldier down range has one in his pocket and we couldn’t muster up more than one in the city of Boston is a shame and we need to rectify that."
In all, there were 66 limb injuries, with 29 patients having recognized limb exsanguination at the scene. Of the 27 tourniquets applied, 26 were improvised.
Failure to translate this important lesson from military experience meant that these homemade devices were most likely wildly ineffective and, in some cases, may have even exacerbated blood loss, he said. Surprisingly, there’s no formal protocol for tourniquet application or training paradigm in Massachusetts, such that exists in the Army’s prehospital Tactical Combat Casualty Care handbook.
"If you look across the paramedic medical guidelines, there is no protocol on the right, evidence-based way to put on a tourniquet or what the indications are for a tourniquet," Dr. King said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). "We don’t have it, and we need to" have it nationwide.
EAST is hoping to provide some guidance in this area with the development of practice management guidelines (PMG) for tourniquet use in extremity trauma. Dr. King, who heads this PMG committee, reported at the meeting that the guidelines, due out later this year, will emphasize that commercially made tourniquets should be available in the prehospital setting, improvised tourniquets rarely work and cannot be recommended; essentially all commercially made tourniquets are equieffective; and that nonmedical personnel can be trained to correctly apply a proper tourniquet.
The need for bleeding control equipment and training for the public has not gone unnoticed by other stakeholders and is the central focus of the newest statement from the Hartford Consensus, a collaborative group of trauma surgeons, law enforcement officers, and emergency responders led by the American College of Surgeons (J. Am. Coll. Surg. 2014;218:467-75).
In dissecting the medical response to the Boston bombings, much has been made of the fact that Boston is home to six Level 1 trauma centers, and that it was race day, a city holiday, 3 p.m., and low-yield devices were used. Dr. King, however, gave high praise to an unsung hero, the Boston EMS loading officer who managed most of the transport destination decisions and smartly distributed critical cases throughout the area’s hospitals.
All critical patients were evacuated within 1 hour, but some have argued this could have been accomplished more quickly were it not for a "stay-and-play" mentality in the medical tent. The after-action review suggests there probably were enough ambulances to do the job in 30 minutes, said Dr. King, who remarked that the only thing that matters in critical trauma cases is time to surgical hemorrhage control.
"This will remain a controversial issue for Boston, whether staying and playing in the medical tent was a good idea," he said. "I don’t know what the right answer is."
Credit was also given to Massachusetts General, and many of the other city hospitals, for their insistence on regular full-scale drills that allowed quick lock-down of the facility to control access and manage the surge capacity in the emergency department.
"It’s more than just a tabletop exercise," Dr. King said. "When we test the surge capacity, we actually empty the emergency room for real. Usually, it occurs between 5:00 and 7:00 or 4:30 and 7:30 in the morning, but actually doing these things was useful, because when it came time to do it for real, no one was tripping over their own feet."
ED volume on that April afternoon was reduced from 97 patients to just 39 within 1.5 hours. Nontrauma physicians, including psychiatrists, did their part by writing "barebones orders" to get patients transferred to the wards.
Staff at Massachusetts General treated 43 patients, performing nine emergent operations, six amputations, two laparotomies, and one thoracotomy, with two traumatic arrests within the first 72 hours. As with other Boston hospitals, there were no in-hospital deaths, he said.
Patients arrived in such rapid succession, however, that it slowed the electronic medical record system and forced staff to use sequential record numbers, which can be dangerous. Registration couldn’t keep up and orders couldn’t be put in fast enough with 43 patients arriving in roughly 35 minutes, Dr. King explained. Workarounds were often old-school, and reminiscent of his days as a green trauma surgeon serving at Ibn Sina Hospital, Baghdad, Iraq.
"In the midst of this entire event, I turned to my nurse practitioner and asked for x, y, z information on a particular patient," he said. "She didn’t turn to her tablet or desktop computer in the operating room. She pulled out a piece of paper where she’d written all the relevant information. At the end of the event, I looked down and realized I’d done the same thing. I was keeping track of my patients on my pants with a Sharpie."
King describes this as a failure of technology and translation from the battlefield, but noted that the hospital did use the military’s practice of reviewing a critical event. Once they’d finished in the operating room and achieved hemorrhage and contamination control, the entire trauma team was reassembled. They did detailed tertiary trauma surveys and went back through every single patient to determine what additional studies they needed, what injuries had been missed.
"It was remarkable the number of things that were missed," Dr. King said. "No one was bleeding to death, but tons and tons of [small, non–life threatening] missed injuries [like ruptured ear drums], and to me this was one of the more important events that surrounded our response to the entire bombing – sitting down after the dust had settled and carefully going over every patient’s medical record."
Dr. King reported having no financial disclosures.
NAPLES, FLA. – Without a single life lost at area hospitals, the medical response to the Boston Marathon bombings was by all accounts remarkable. But what if police and other first-responders had tourniquets and were trained in their use?
As it was, advanced topical hemostatic agents and tourniquets were MIA in the field, forcing all but one prehospital tourniquet to be improvised, according to Massachusetts General Hospital trauma surgeon Lt. Col. David King, U. S. Army Reserve.
"It’s abundantly clear from the literature that improvised tourniquets almost never work," he said. "The fact that every soldier down range has one in his pocket and we couldn’t muster up more than one in the city of Boston is a shame and we need to rectify that."
In all, there were 66 limb injuries, with 29 patients having recognized limb exsanguination at the scene. Of the 27 tourniquets applied, 26 were improvised.
Failure to translate this important lesson from military experience meant that these homemade devices were most likely wildly ineffective and, in some cases, may have even exacerbated blood loss, he said. Surprisingly, there’s no formal protocol for tourniquet application or training paradigm in Massachusetts, such that exists in the Army’s prehospital Tactical Combat Casualty Care handbook.
"If you look across the paramedic medical guidelines, there is no protocol on the right, evidence-based way to put on a tourniquet or what the indications are for a tourniquet," Dr. King said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). "We don’t have it, and we need to" have it nationwide.
EAST is hoping to provide some guidance in this area with the development of practice management guidelines (PMG) for tourniquet use in extremity trauma. Dr. King, who heads this PMG committee, reported at the meeting that the guidelines, due out later this year, will emphasize that commercially made tourniquets should be available in the prehospital setting, improvised tourniquets rarely work and cannot be recommended; essentially all commercially made tourniquets are equieffective; and that nonmedical personnel can be trained to correctly apply a proper tourniquet.
The need for bleeding control equipment and training for the public has not gone unnoticed by other stakeholders and is the central focus of the newest statement from the Hartford Consensus, a collaborative group of trauma surgeons, law enforcement officers, and emergency responders led by the American College of Surgeons (J. Am. Coll. Surg. 2014;218:467-75).
In dissecting the medical response to the Boston bombings, much has been made of the fact that Boston is home to six Level 1 trauma centers, and that it was race day, a city holiday, 3 p.m., and low-yield devices were used. Dr. King, however, gave high praise to an unsung hero, the Boston EMS loading officer who managed most of the transport destination decisions and smartly distributed critical cases throughout the area’s hospitals.
All critical patients were evacuated within 1 hour, but some have argued this could have been accomplished more quickly were it not for a "stay-and-play" mentality in the medical tent. The after-action review suggests there probably were enough ambulances to do the job in 30 minutes, said Dr. King, who remarked that the only thing that matters in critical trauma cases is time to surgical hemorrhage control.
"This will remain a controversial issue for Boston, whether staying and playing in the medical tent was a good idea," he said. "I don’t know what the right answer is."
Credit was also given to Massachusetts General, and many of the other city hospitals, for their insistence on regular full-scale drills that allowed quick lock-down of the facility to control access and manage the surge capacity in the emergency department.
"It’s more than just a tabletop exercise," Dr. King said. "When we test the surge capacity, we actually empty the emergency room for real. Usually, it occurs between 5:00 and 7:00 or 4:30 and 7:30 in the morning, but actually doing these things was useful, because when it came time to do it for real, no one was tripping over their own feet."
ED volume on that April afternoon was reduced from 97 patients to just 39 within 1.5 hours. Nontrauma physicians, including psychiatrists, did their part by writing "barebones orders" to get patients transferred to the wards.
Staff at Massachusetts General treated 43 patients, performing nine emergent operations, six amputations, two laparotomies, and one thoracotomy, with two traumatic arrests within the first 72 hours. As with other Boston hospitals, there were no in-hospital deaths, he said.
Patients arrived in such rapid succession, however, that it slowed the electronic medical record system and forced staff to use sequential record numbers, which can be dangerous. Registration couldn’t keep up and orders couldn’t be put in fast enough with 43 patients arriving in roughly 35 minutes, Dr. King explained. Workarounds were often old-school, and reminiscent of his days as a green trauma surgeon serving at Ibn Sina Hospital, Baghdad, Iraq.
"In the midst of this entire event, I turned to my nurse practitioner and asked for x, y, z information on a particular patient," he said. "She didn’t turn to her tablet or desktop computer in the operating room. She pulled out a piece of paper where she’d written all the relevant information. At the end of the event, I looked down and realized I’d done the same thing. I was keeping track of my patients on my pants with a Sharpie."
King describes this as a failure of technology and translation from the battlefield, but noted that the hospital did use the military’s practice of reviewing a critical event. Once they’d finished in the operating room and achieved hemorrhage and contamination control, the entire trauma team was reassembled. They did detailed tertiary trauma surveys and went back through every single patient to determine what additional studies they needed, what injuries had been missed.
"It was remarkable the number of things that were missed," Dr. King said. "No one was bleeding to death, but tons and tons of [small, non–life threatening] missed injuries [like ruptured ear drums], and to me this was one of the more important events that surrounded our response to the entire bombing – sitting down after the dust had settled and carefully going over every patient’s medical record."
Dr. King reported having no financial disclosures.
EXPERT ANALYSIS FROM EAST SCIENTIFIC ASSEMBLY 2014
IT survey underlines move to mobile health
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
AT HIMSS14
Physicians are major source for frequent opioid misusers
Most people who misuse opioid pain relievers cite friends and relatives as their sources for the drugs, but more of the people who misuse these agents most often – those who take them from 200 to 365 days of the year – obtain their opioids from physicians’ prescriptions than from any other single source, according to a report published online March 3 in JAMA Internal Medicine.
"These results underscore the need for interventions targeting prescribing behaviors, in addition to those targeting medication sharing, selling, and diversion," the report’s authors warned.
It is a commonly cited statistic that most people who misuse opioid pain relievers obtain the drugs from family and friends for free, so many interventions to stop such misuse focus on patients. But few studies have examined whether the source of these drugs, and thus an appropriate target for interventions, might differ according to the frequency of misuse.
To study this issue, researchers analyzed data from the National Survey on Drug Use and Health, an annual survey that provides information on drug use among U.S. residents aged 12 years and older.
Survey data from 2008 through 2011 identified 11,018,735 respondents who said they misused an opioid pain reliever either by obtaining the drug without a prescription or by getting a prescription but taking the drug strictly because of the feeling or experience it provided. The source of the drug differed according to the frequency of use: As the days of use increased, the likelihood that the user obtained the drug from a friend or family member decreased, and the likelihood that he or she obtained the drug from a physician rose, said Christopher M. Jones, Pharm.D., and his associates at the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta.
Among people who misused opioids only 1-29 days of the year, 54.4% said they got them from a friend or relative for free – the most popular source. In contrast, only 18% of this patient group said the opioids were prescribed by one or more physicians.
But the percentage of patients who obtained misused opioids through physician prescriptions steadily rose with increasing use.
Among those who misused the drugs 200-365 days a year, the top source was physician prescriptions, 27.3% of users, followed by opioids obtained for free from friends or relatives, 26.4%. A total of 23.2% of users said they bought their opioids from friends or relatives, while another 15% of frequent users bought their drugs from dealers or strangers.
"This pattern is similar to that of patients in opioid treatment programs, who cite dealers and physicians as frequent sources," Dr. Jones and his associates said in a Research Letter to the Editor (JAMA Intern. Med. 2014 March 3 [doi:10.1001/jamainternmed.2013.12809]).
"Many abusers of opioid pain relievers are going directly to doctors for their drugs," CDC Director Tom Frieden commented in a statement. "Health care providers need to screen for abuse risk and prescribe judiciously by checking past records in state prescription drug monitoring programs. It’s time we stop the source and treat the troubled."
"The essential steps health care providers can take to curb this serious health problem include more judicious prescribing, use of prescription-drug–monitoring programs, and screening patients for abuse before prescribing opioids," the study authors noted.
The federal government is encouraging the development of abuse-deterrent opioid formulations, the CDC noted, and requiring companies that make extended-release and long-acting opioids to offer prescribers educational programs about the understanding the risks of opioid therapy; choosing, managing, and monitoring patients; and counseling patients on safe use of opioids.
The Centers for Disease Control and Prevention supported the study. No financial conflicts of interest were reported.
Most people who misuse opioid pain relievers cite friends and relatives as their sources for the drugs, but more of the people who misuse these agents most often – those who take them from 200 to 365 days of the year – obtain their opioids from physicians’ prescriptions than from any other single source, according to a report published online March 3 in JAMA Internal Medicine.
"These results underscore the need for interventions targeting prescribing behaviors, in addition to those targeting medication sharing, selling, and diversion," the report’s authors warned.
It is a commonly cited statistic that most people who misuse opioid pain relievers obtain the drugs from family and friends for free, so many interventions to stop such misuse focus on patients. But few studies have examined whether the source of these drugs, and thus an appropriate target for interventions, might differ according to the frequency of misuse.
To study this issue, researchers analyzed data from the National Survey on Drug Use and Health, an annual survey that provides information on drug use among U.S. residents aged 12 years and older.
Survey data from 2008 through 2011 identified 11,018,735 respondents who said they misused an opioid pain reliever either by obtaining the drug without a prescription or by getting a prescription but taking the drug strictly because of the feeling or experience it provided. The source of the drug differed according to the frequency of use: As the days of use increased, the likelihood that the user obtained the drug from a friend or family member decreased, and the likelihood that he or she obtained the drug from a physician rose, said Christopher M. Jones, Pharm.D., and his associates at the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta.
Among people who misused opioids only 1-29 days of the year, 54.4% said they got them from a friend or relative for free – the most popular source. In contrast, only 18% of this patient group said the opioids were prescribed by one or more physicians.
But the percentage of patients who obtained misused opioids through physician prescriptions steadily rose with increasing use.
Among those who misused the drugs 200-365 days a year, the top source was physician prescriptions, 27.3% of users, followed by opioids obtained for free from friends or relatives, 26.4%. A total of 23.2% of users said they bought their opioids from friends or relatives, while another 15% of frequent users bought their drugs from dealers or strangers.
"This pattern is similar to that of patients in opioid treatment programs, who cite dealers and physicians as frequent sources," Dr. Jones and his associates said in a Research Letter to the Editor (JAMA Intern. Med. 2014 March 3 [doi:10.1001/jamainternmed.2013.12809]).
"Many abusers of opioid pain relievers are going directly to doctors for their drugs," CDC Director Tom Frieden commented in a statement. "Health care providers need to screen for abuse risk and prescribe judiciously by checking past records in state prescription drug monitoring programs. It’s time we stop the source and treat the troubled."
"The essential steps health care providers can take to curb this serious health problem include more judicious prescribing, use of prescription-drug–monitoring programs, and screening patients for abuse before prescribing opioids," the study authors noted.
The federal government is encouraging the development of abuse-deterrent opioid formulations, the CDC noted, and requiring companies that make extended-release and long-acting opioids to offer prescribers educational programs about the understanding the risks of opioid therapy; choosing, managing, and monitoring patients; and counseling patients on safe use of opioids.
The Centers for Disease Control and Prevention supported the study. No financial conflicts of interest were reported.
Most people who misuse opioid pain relievers cite friends and relatives as their sources for the drugs, but more of the people who misuse these agents most often – those who take them from 200 to 365 days of the year – obtain their opioids from physicians’ prescriptions than from any other single source, according to a report published online March 3 in JAMA Internal Medicine.
"These results underscore the need for interventions targeting prescribing behaviors, in addition to those targeting medication sharing, selling, and diversion," the report’s authors warned.
It is a commonly cited statistic that most people who misuse opioid pain relievers obtain the drugs from family and friends for free, so many interventions to stop such misuse focus on patients. But few studies have examined whether the source of these drugs, and thus an appropriate target for interventions, might differ according to the frequency of misuse.
To study this issue, researchers analyzed data from the National Survey on Drug Use and Health, an annual survey that provides information on drug use among U.S. residents aged 12 years and older.
Survey data from 2008 through 2011 identified 11,018,735 respondents who said they misused an opioid pain reliever either by obtaining the drug without a prescription or by getting a prescription but taking the drug strictly because of the feeling or experience it provided. The source of the drug differed according to the frequency of use: As the days of use increased, the likelihood that the user obtained the drug from a friend or family member decreased, and the likelihood that he or she obtained the drug from a physician rose, said Christopher M. Jones, Pharm.D., and his associates at the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta.
Among people who misused opioids only 1-29 days of the year, 54.4% said they got them from a friend or relative for free – the most popular source. In contrast, only 18% of this patient group said the opioids were prescribed by one or more physicians.
But the percentage of patients who obtained misused opioids through physician prescriptions steadily rose with increasing use.
Among those who misused the drugs 200-365 days a year, the top source was physician prescriptions, 27.3% of users, followed by opioids obtained for free from friends or relatives, 26.4%. A total of 23.2% of users said they bought their opioids from friends or relatives, while another 15% of frequent users bought their drugs from dealers or strangers.
"This pattern is similar to that of patients in opioid treatment programs, who cite dealers and physicians as frequent sources," Dr. Jones and his associates said in a Research Letter to the Editor (JAMA Intern. Med. 2014 March 3 [doi:10.1001/jamainternmed.2013.12809]).
"Many abusers of opioid pain relievers are going directly to doctors for their drugs," CDC Director Tom Frieden commented in a statement. "Health care providers need to screen for abuse risk and prescribe judiciously by checking past records in state prescription drug monitoring programs. It’s time we stop the source and treat the troubled."
"The essential steps health care providers can take to curb this serious health problem include more judicious prescribing, use of prescription-drug–monitoring programs, and screening patients for abuse before prescribing opioids," the study authors noted.
The federal government is encouraging the development of abuse-deterrent opioid formulations, the CDC noted, and requiring companies that make extended-release and long-acting opioids to offer prescribers educational programs about the understanding the risks of opioid therapy; choosing, managing, and monitoring patients; and counseling patients on safe use of opioids.
The Centers for Disease Control and Prevention supported the study. No financial conflicts of interest were reported.
FROM JAMA INTERNAL MEDICINE
Major Finding: Opioid pain relievers were prescribed by a physician for 18% of people who used them only 1-29 days of the year, but that percentage steadily rose with increasing use, so that 27.3% of people who used the drugs 200-365 days/year obtained them via physician prescription, more than any other single source.
Data Source: An analysis of data on 11,018,735 survey respondents aged 12 years and older who reported misusing opioid pain relievers during a 4-year period.
Disclosures: The Centers for Disease Control and Prevention supported the study. No financial conflicts of interest were reported.
Point/Counterpoint – Another surgeon’s error – Must you tell the patient?
POINT: Surgeons have a duty to tell patients when a medical error has been made by a physician colleague.
Surgeons have a moral and ethical obligation to inform a patient when a medical error has occurred, including cases when the error was made by another surgeon.
Principles that support complete and honest disclosure to the patient and/or the patient’s family in such cases include professional obligation on the part of both the surgeon who made the error and the surgeon who discovered the error, the integrity of both surgeons, the patient’s right to informed care throughout the continuum of care, and the patient’s right to informed consent.
With respect to the first, the American Medical Association’s code of ethics provides a framework for disclosure; it clearly states that situations occur in which a patient experiences significant complications that may have resulted from a physician’s mistake or judgment and that the physician is ethically required to inform the patient of all facts necessary to ensure understanding of the error that occurred.
The American College of Physicians’ ethics manual also states that physicians should disclose to patients information about procedural or judgment errors made during the course of care, as long as that information is pertinent and material to the patient’s well-being.
Errors do not necessarily imply negligence or unethical behavior, but failure to disclose may.
As for patients’ rights, I think that patients are entitled to honest information. They shouldn’t bear the burden of determining how they came to be in another surgeon’s care.
Patients with complications may have impactful financial burdens that result from the additional treatment that is needed, and without all pertinent information, they may have difficulty understanding the benefits, such as deferment of payments, to which they are entitled.
The patient must also be kept informed as to the long-term care plan, and honest and timely disclosure will facilitate moving beyond blame and toward patient advocacy.
The patient is entitled to informed consent, and this requires an understanding of the conditions under which they arrived in another surgeon’s care. If a second procedure is required, the patient must be made aware of potential complications – including how the effects of the initial error might impact outcomes.
Although surgeons have an ethical obligation to disclose errors made by another surgeon, this is admittedly a difficult task. Pressures from society and medical professionals can make disclosure difficult, but the benefits of disclosure are very real; studies show that open, honest communication improves patient satisfaction, strengthens the physician-patient relationship, and can ultimately improve outcomes.
Disclosure also has the potential to improve the well-being of the surgeons involved, through relieving feelings of guilt, and satisfying the need to fulfill one’s obligations. Furthermore, data suggest that error disclosure reduces long-term litigation and costs. Admittedly, however, there are little data on how disclosure of another surgeon’s errors ultimately reduces litigation and costs.
Ultimately, supporting a just culture allows us to emphasize the importance of disclosing errors and to be accountable in setting a standard that involves exploring errors rather than ignoring them; it must be remembered, though, that this process of disclosure involves obtaining facts to help both surgeons and patients understand what truly happened.
Surgeon-to-surgeon discussions can be productive and can facilitate disclosure. However, if the doctor who made the error declines to be part of the disclosure process, one still has an obligation to disclose the error and to answer the patient’s questions honestly.
This approach requires a commitment to support surgeons in their efforts to promote transparency, and it requires a clear understanding of our obligations and the role of disclosure during training; we need to engage medical students and residents in the very important role of health care advocacy.
Dr. Bruce is an associate professor at the Ohio State University, Columbus.
COUNTERPOINT: Surgeons are not required to inform a patient of another physician’s possible error.
Surgeons do not have an obligation to disclose to a patient another surgeon’s possible medical error.
A consensus has been reached in medicine about our ethical duty to inform patients about our own medical errors. Although nondisclosure has previously been rationalized by concerns about invoking anxiety or confusion in the patient, this approach has largely been discredited; disclosure preserves patient trust and bolsters the physician-patient relationship.
However, it is an entirely different story when it comes to disclosing another surgeon’s mistake – a situation that is quite common. A recent survey showed that two-thirds of respondents had encountered a similar dilemma in the past 6 months (Qual. Saf. Health Care 2009;18:209-12).
The approach that physicians have previously taken when faced with this dilemma is an important measure of what they believe represents an ethical or just response. A poll of many of my colleagues across the country and at my own institution suggests that the preferred approach is to provide appropriate care for the patient and to answer their questions honestly, but to not proactively disclose the perceived medical error.
In fact, this was the preferred approach of every surgeon who responded.
A recent article in the New England Journal of Medicine addressed this very topic. The authors noted that there is little guidance available regarding the reporting of another physician’s error (2013;369:1752-7).
Among the challenges inherent in disclosing another’s mistake is the difficulty in determining exactly what happened. Uncertainty inevitably exists regarding the conversations that took place between the patient and the surgeon, and also about what actually defines a medical error. Incidents regarded as medical errors may comprise a large spectrum, ranging from "not what I would have done – but within the standard of care," to "blatant negligence."
Several studies suggest that highly trained physicians and surgeons routinely disagree about whether negligence has occurred in a given case. In one study, two reviewers disagreed 38% of the time as to whether appropriate care was provided.
Physicians have difficulty judging if the standard of care has been met. Therefore, it is not acceptable for each of us to assume we are the medical expert capable of rendering an opinion of whether previous care was appropriate and informing patients of our opinion.
Physicians overwhelmingly report that in the event they are responsible for a medical error discovered by another physician, they would prefer that the physician come to them first to discuss the matter. In fact, 93% of 400 respondents in one survey reported this preference.
The most acceptable approach when dealing with a peer’s medical error is to discuss the error with the responsible physician and to encourage the physician to disclose any error with the patient.
If there is disagreement as to whether an error occurred, institutional guidance should be applied. Only a collaborative approach can appropriately meet the needs of the patient and family after harmful medical errors.
Dr. Chadrick E. Denlinger is an associate professor at the Medical University of South Carolina, Charleston.
POINT: Surgeons have a duty to tell patients when a medical error has been made by a physician colleague.
Surgeons have a moral and ethical obligation to inform a patient when a medical error has occurred, including cases when the error was made by another surgeon.
Principles that support complete and honest disclosure to the patient and/or the patient’s family in such cases include professional obligation on the part of both the surgeon who made the error and the surgeon who discovered the error, the integrity of both surgeons, the patient’s right to informed care throughout the continuum of care, and the patient’s right to informed consent.
With respect to the first, the American Medical Association’s code of ethics provides a framework for disclosure; it clearly states that situations occur in which a patient experiences significant complications that may have resulted from a physician’s mistake or judgment and that the physician is ethically required to inform the patient of all facts necessary to ensure understanding of the error that occurred.
The American College of Physicians’ ethics manual also states that physicians should disclose to patients information about procedural or judgment errors made during the course of care, as long as that information is pertinent and material to the patient’s well-being.
Errors do not necessarily imply negligence or unethical behavior, but failure to disclose may.
As for patients’ rights, I think that patients are entitled to honest information. They shouldn’t bear the burden of determining how they came to be in another surgeon’s care.
Patients with complications may have impactful financial burdens that result from the additional treatment that is needed, and without all pertinent information, they may have difficulty understanding the benefits, such as deferment of payments, to which they are entitled.
The patient must also be kept informed as to the long-term care plan, and honest and timely disclosure will facilitate moving beyond blame and toward patient advocacy.
The patient is entitled to informed consent, and this requires an understanding of the conditions under which they arrived in another surgeon’s care. If a second procedure is required, the patient must be made aware of potential complications – including how the effects of the initial error might impact outcomes.
Although surgeons have an ethical obligation to disclose errors made by another surgeon, this is admittedly a difficult task. Pressures from society and medical professionals can make disclosure difficult, but the benefits of disclosure are very real; studies show that open, honest communication improves patient satisfaction, strengthens the physician-patient relationship, and can ultimately improve outcomes.
Disclosure also has the potential to improve the well-being of the surgeons involved, through relieving feelings of guilt, and satisfying the need to fulfill one’s obligations. Furthermore, data suggest that error disclosure reduces long-term litigation and costs. Admittedly, however, there are little data on how disclosure of another surgeon’s errors ultimately reduces litigation and costs.
Ultimately, supporting a just culture allows us to emphasize the importance of disclosing errors and to be accountable in setting a standard that involves exploring errors rather than ignoring them; it must be remembered, though, that this process of disclosure involves obtaining facts to help both surgeons and patients understand what truly happened.
Surgeon-to-surgeon discussions can be productive and can facilitate disclosure. However, if the doctor who made the error declines to be part of the disclosure process, one still has an obligation to disclose the error and to answer the patient’s questions honestly.
This approach requires a commitment to support surgeons in their efforts to promote transparency, and it requires a clear understanding of our obligations and the role of disclosure during training; we need to engage medical students and residents in the very important role of health care advocacy.
Dr. Bruce is an associate professor at the Ohio State University, Columbus.
COUNTERPOINT: Surgeons are not required to inform a patient of another physician’s possible error.
Surgeons do not have an obligation to disclose to a patient another surgeon’s possible medical error.
A consensus has been reached in medicine about our ethical duty to inform patients about our own medical errors. Although nondisclosure has previously been rationalized by concerns about invoking anxiety or confusion in the patient, this approach has largely been discredited; disclosure preserves patient trust and bolsters the physician-patient relationship.
However, it is an entirely different story when it comes to disclosing another surgeon’s mistake – a situation that is quite common. A recent survey showed that two-thirds of respondents had encountered a similar dilemma in the past 6 months (Qual. Saf. Health Care 2009;18:209-12).
The approach that physicians have previously taken when faced with this dilemma is an important measure of what they believe represents an ethical or just response. A poll of many of my colleagues across the country and at my own institution suggests that the preferred approach is to provide appropriate care for the patient and to answer their questions honestly, but to not proactively disclose the perceived medical error.
In fact, this was the preferred approach of every surgeon who responded.
A recent article in the New England Journal of Medicine addressed this very topic. The authors noted that there is little guidance available regarding the reporting of another physician’s error (2013;369:1752-7).
Among the challenges inherent in disclosing another’s mistake is the difficulty in determining exactly what happened. Uncertainty inevitably exists regarding the conversations that took place between the patient and the surgeon, and also about what actually defines a medical error. Incidents regarded as medical errors may comprise a large spectrum, ranging from "not what I would have done – but within the standard of care," to "blatant negligence."
Several studies suggest that highly trained physicians and surgeons routinely disagree about whether negligence has occurred in a given case. In one study, two reviewers disagreed 38% of the time as to whether appropriate care was provided.
Physicians have difficulty judging if the standard of care has been met. Therefore, it is not acceptable for each of us to assume we are the medical expert capable of rendering an opinion of whether previous care was appropriate and informing patients of our opinion.
Physicians overwhelmingly report that in the event they are responsible for a medical error discovered by another physician, they would prefer that the physician come to them first to discuss the matter. In fact, 93% of 400 respondents in one survey reported this preference.
The most acceptable approach when dealing with a peer’s medical error is to discuss the error with the responsible physician and to encourage the physician to disclose any error with the patient.
If there is disagreement as to whether an error occurred, institutional guidance should be applied. Only a collaborative approach can appropriately meet the needs of the patient and family after harmful medical errors.
Dr. Chadrick E. Denlinger is an associate professor at the Medical University of South Carolina, Charleston.
POINT: Surgeons have a duty to tell patients when a medical error has been made by a physician colleague.
Surgeons have a moral and ethical obligation to inform a patient when a medical error has occurred, including cases when the error was made by another surgeon.
Principles that support complete and honest disclosure to the patient and/or the patient’s family in such cases include professional obligation on the part of both the surgeon who made the error and the surgeon who discovered the error, the integrity of both surgeons, the patient’s right to informed care throughout the continuum of care, and the patient’s right to informed consent.
With respect to the first, the American Medical Association’s code of ethics provides a framework for disclosure; it clearly states that situations occur in which a patient experiences significant complications that may have resulted from a physician’s mistake or judgment and that the physician is ethically required to inform the patient of all facts necessary to ensure understanding of the error that occurred.
The American College of Physicians’ ethics manual also states that physicians should disclose to patients information about procedural or judgment errors made during the course of care, as long as that information is pertinent and material to the patient’s well-being.
Errors do not necessarily imply negligence or unethical behavior, but failure to disclose may.
As for patients’ rights, I think that patients are entitled to honest information. They shouldn’t bear the burden of determining how they came to be in another surgeon’s care.
Patients with complications may have impactful financial burdens that result from the additional treatment that is needed, and without all pertinent information, they may have difficulty understanding the benefits, such as deferment of payments, to which they are entitled.
The patient must also be kept informed as to the long-term care plan, and honest and timely disclosure will facilitate moving beyond blame and toward patient advocacy.
The patient is entitled to informed consent, and this requires an understanding of the conditions under which they arrived in another surgeon’s care. If a second procedure is required, the patient must be made aware of potential complications – including how the effects of the initial error might impact outcomes.
Although surgeons have an ethical obligation to disclose errors made by another surgeon, this is admittedly a difficult task. Pressures from society and medical professionals can make disclosure difficult, but the benefits of disclosure are very real; studies show that open, honest communication improves patient satisfaction, strengthens the physician-patient relationship, and can ultimately improve outcomes.
Disclosure also has the potential to improve the well-being of the surgeons involved, through relieving feelings of guilt, and satisfying the need to fulfill one’s obligations. Furthermore, data suggest that error disclosure reduces long-term litigation and costs. Admittedly, however, there are little data on how disclosure of another surgeon’s errors ultimately reduces litigation and costs.
Ultimately, supporting a just culture allows us to emphasize the importance of disclosing errors and to be accountable in setting a standard that involves exploring errors rather than ignoring them; it must be remembered, though, that this process of disclosure involves obtaining facts to help both surgeons and patients understand what truly happened.
Surgeon-to-surgeon discussions can be productive and can facilitate disclosure. However, if the doctor who made the error declines to be part of the disclosure process, one still has an obligation to disclose the error and to answer the patient’s questions honestly.
This approach requires a commitment to support surgeons in their efforts to promote transparency, and it requires a clear understanding of our obligations and the role of disclosure during training; we need to engage medical students and residents in the very important role of health care advocacy.
Dr. Bruce is an associate professor at the Ohio State University, Columbus.
COUNTERPOINT: Surgeons are not required to inform a patient of another physician’s possible error.
Surgeons do not have an obligation to disclose to a patient another surgeon’s possible medical error.
A consensus has been reached in medicine about our ethical duty to inform patients about our own medical errors. Although nondisclosure has previously been rationalized by concerns about invoking anxiety or confusion in the patient, this approach has largely been discredited; disclosure preserves patient trust and bolsters the physician-patient relationship.
However, it is an entirely different story when it comes to disclosing another surgeon’s mistake – a situation that is quite common. A recent survey showed that two-thirds of respondents had encountered a similar dilemma in the past 6 months (Qual. Saf. Health Care 2009;18:209-12).
The approach that physicians have previously taken when faced with this dilemma is an important measure of what they believe represents an ethical or just response. A poll of many of my colleagues across the country and at my own institution suggests that the preferred approach is to provide appropriate care for the patient and to answer their questions honestly, but to not proactively disclose the perceived medical error.
In fact, this was the preferred approach of every surgeon who responded.
A recent article in the New England Journal of Medicine addressed this very topic. The authors noted that there is little guidance available regarding the reporting of another physician’s error (2013;369:1752-7).
Among the challenges inherent in disclosing another’s mistake is the difficulty in determining exactly what happened. Uncertainty inevitably exists regarding the conversations that took place between the patient and the surgeon, and also about what actually defines a medical error. Incidents regarded as medical errors may comprise a large spectrum, ranging from "not what I would have done – but within the standard of care," to "blatant negligence."
Several studies suggest that highly trained physicians and surgeons routinely disagree about whether negligence has occurred in a given case. In one study, two reviewers disagreed 38% of the time as to whether appropriate care was provided.
Physicians have difficulty judging if the standard of care has been met. Therefore, it is not acceptable for each of us to assume we are the medical expert capable of rendering an opinion of whether previous care was appropriate and informing patients of our opinion.
Physicians overwhelmingly report that in the event they are responsible for a medical error discovered by another physician, they would prefer that the physician come to them first to discuss the matter. In fact, 93% of 400 respondents in one survey reported this preference.
The most acceptable approach when dealing with a peer’s medical error is to discuss the error with the responsible physician and to encourage the physician to disclose any error with the patient.
If there is disagreement as to whether an error occurred, institutional guidance should be applied. Only a collaborative approach can appropriately meet the needs of the patient and family after harmful medical errors.
Dr. Chadrick E. Denlinger is an associate professor at the Medical University of South Carolina, Charleston.
Volume matters: Whipple success hinges on surgeon experience
MIAMI BEACH – Studies continue to confirm it: When it comes to complex surgical procedures, higher volume equals better outcomes. But like the chicken-or-egg conundrum, researchers are asking which factor comes first – surgeon or facility.
Data presented at the annual meeting of the Americas Hepato-Pancreato-Biliary Association suggest that personal experience makes the biggest difference, at least for the difficult Whipple procedure. Surgeons who performed the highest number of pancreaticoduodenectomies each year had the best outcomes; when they transferred to low-volume hospitals with historically poor results, these surgeons improved perioperative complications, mortality, and readmissions, and lowered costs.
"The salutary effects of being a high-volume hospital for pancreaticoduodenectomy are transferred when high-volume surgeons relocate," said Dr. Paul Toomey. "It seems that the benefits of a high-volume hospital are more due to who does the surgery rather than where it’s undertaken."
Dr. Toomey, a surgical fellow at the Florida Hospital, Tampa, had a unique opportunity to study what happens when two surgeons highly experienced in the Whipple procedure transferred from a busy hospital to low-volume facilities. The surgeons, who together performed more than 100 of the procedures each year, moved for personal reasons, Dr. Toomey said in an interview.
The study focused on perioperative outcomes, mortality, and readmissions in two groups of Whipple patients: the last 50 undertaken at the high-volume hospital (more than 12 pancreaticoduodenectomies per year), and the first 50 at the low-volume hospital where they worked afterward.
The patient groups were similar. Their mean age was 78 years, a little more than half were men, and the average American Society of Anesthesiologists class was 3. The rates of malignancy were similar in the high- and low-volume centers (88% vs. 82%, respectively).
Overall, the average operative time was 252 minutes, with an estimated blood loss of 300 mL. Patients were in intensive care for 2 days, with an average hospital stay of 9 days. The readmission rate was 19% and 30-day mortality, 5%.
But when Dr. Toomey compared the two time periods, he found significant differences in outcomes, which appeared to be associated with the transfer of the highly experienced surgeons. In fact, he said, outcomes were actually much better at the low- than the high-volume centers after the transfer.
The mean operative time at the low-volume centers was 205 minutes, compared with 305 minutes at the high-volume centers. Estimated blood loss was also less at the low-volume centers (350 vs. 255 mL). ICU stays were significantly shorter (1 vs. 3 days), as was total length of stay (7 vs. 12 days). Readmission rates over 30 days were similar (20% vs. 18%), as was 30-day mortality (4% vs. 6%).
"The salutary benefits of being a high-volume hospital for pancreaticoduodenectomy seem to be transferred when high-volume surgeons relocate," Dr. Toomey said. "The benefits of a high-volume hospital may be more due to who does the pancreaticoduodenectomy rather than where the pancreaticoduodenectomy is undertaken."
Dr. Thomas Wood, also of the Florida Hospital, found a similar trend in his study, which examined Whipple outcomes statewide over 20 years. He related the outcomes to concentration, rather decentralization, of care.
For his study, Dr. Wood examined data from the Florida Agency for Health Care Administration, collected over three 3-year epochs: 1992-1994, 2001-2003, and 2010-2012. The data were sorted by surgeon volume of pancreaticoduodenectomy during these periods and correlated to length of stay, in-hospital mortality, and hospital charges, which were adjusted to 2012 dollars.
Over the 9 years, 893 surgeons performed 3,531 pancreaticoduodenectomies. During each epoch, the number of surgeons went down as the number of operations increased.
In the first epoch, 363 surgeons performed 729 operations. In the second, 334 surgeons performed 1,233 surgeries, and in the third, 196 performed 1,569 operations.
"By 2010-2012, 46% fewer surgeons undertook 115% more surgeries compared to the first period," Dr. Wood said. "In 1992-1994, 62% of pancreaticoduodenectomies were undertaken by surgeons who performed one or fewer per year. This fell to 13% by 2010-2012."
At the same time, the number of surgeons who performed more than 36 procedures in each 3-year period (12 per year) grew significantly. In the first epoch, one surgeon alone performed 45 procedures. In the second, six surgeons performed a total of 361. And in the third epoch, 11 surgeons performed 806 Whipples.
"From [the first through third periods,] there was an 11-fold increase in the number of high-volume surgeons and a corresponding 18-fold increase in the number of pancreaticoduodenectomies by surgeons who were performing at least 12 each year. They were performing more than 50% of these operations."
A separate analysis of just the 2010-2012 data evaluated outcomes by surgeons’ operation volume.
In the first epoch, in-hospital mortality was about 12%. In the second, it fell to 8%, and by the third, to 4%. Patients whose surgeons performed one to nine procedures (up to three per year) were hospitalized an average of about 14 days. Those whose surgeons performed 19 to 36 procedures (up to 12 per year) stayed an average of 8 days – a significant difference.
Mortality followed the same pattern. About 9% of patients whose surgeons performed one to three procedures per year died after surgery, compared with 2% of those whose doctors performed 12 procedures per year.
These more experienced surgeons also discharged more patients to home rather than nursing facilities (88% vs. 82%, a significant difference).
Both hospital and surgeon volume also affected costs. Overall, hospital costs increased significantly, even after adjustment for inflation, jumping from $93,000 to $133,000. But surgeons who performed at least 12 Whipples per year did so at a half the cost of those who performed 1-3 per year ($100,000 vs. $200,000).
"Suffice it to say, the busiest surgeons got the best results," Dr. Wood said.
Despite advances in centralizing this kind of specialized care, though, many low-volume centers are still performing the operations, said Dr. Jeffrey Sutton of the University of Cincinnati. "Research continues to show that high-volume centers have better outcomes," he said. "And yet a significant number of cases are still being done at hospitals that do less than one per year."
If research data aren’t enough to persuade hospitals to send patients to regional centers, Dr. Sutton wondered, could money be a motivating factor? He examined the records of almost 10,000 Whipple operations performed at 419 centers that are part of the University Health Systems Consortium clinical database. Of these, 120 were academic centers and 299 were affiliated hospitals. The procedures were performed from 2009 to 2011. Clinical outcomes included length of stay, mortality, and readmissions. He also assessed the cost of both the index admission and readmissions.
Hospitals were divided into volume quintiles of lowest, low, middle, high, and highest. The lowest-volume centers performed up to 21 cases/year in 2009 to up to 23 in 2011. The highest-volume centers performed up to 180 cases/year in 2009 and up to 216 in 2011.
Intraoperative mortality hovered around 2% at the middle-, high-, and highest-volume centers. At the low-volume centers, it reached 2.5% – not significantly different. But at the lowest-volume centers, 30-day mortality was significantly higher – nearly 4%.
Length of stay was similarly associated with volume. In low-, middle-, and high-volume centers, it was about 9 days. But in the lowest-volume centers, the average length of stay was 11 days – significantly longer than any of the others.
Readmission rates over the first postoperative month were also lowest in the highest-volume centers (16.5%). In the low-volume centers, 30-day readmission was just under 19%. But in the middle-, low-, and lowest-volume centers, it was significantly greater, hovering at nearly 20%.
"It’s not only that lower-volume centers are holding on to patients longer, they also are readmitting those same patients significantly more often," Dr. Sutton noted.
The cost analysis looked at Medicare charge data. "When both index and readmission costs were considered, the median per-patient cost at the lowest-volume centers was $23,005 – 11% more than at the highest-volume center."
But there was no significant difference in the cost of readmissions. "That means that the difference of about $2,263 extra per case was based solely on the index admission," Dr. Sutton said. "Essentially what we saw was that the more cases that are performed, the cheaper each individual case becomes."
"To put it bluntly, some low-volume centers are currently reimbursed higher sums of money for delivering suboptimal care to patients," Dr. Sutton said in an interview. In our current health care climate, which emphasizes improved outcomes at lower costs, this is a travesty. As health service researchers, it is our obligation to our patients to analyze and disseminate these data in an effort to urge policymakers to limit the financial reimbursements for poorer-performing providers."
None of the researchers quoted in this article reported any financial disclosures.
MIAMI BEACH – Studies continue to confirm it: When it comes to complex surgical procedures, higher volume equals better outcomes. But like the chicken-or-egg conundrum, researchers are asking which factor comes first – surgeon or facility.
Data presented at the annual meeting of the Americas Hepato-Pancreato-Biliary Association suggest that personal experience makes the biggest difference, at least for the difficult Whipple procedure. Surgeons who performed the highest number of pancreaticoduodenectomies each year had the best outcomes; when they transferred to low-volume hospitals with historically poor results, these surgeons improved perioperative complications, mortality, and readmissions, and lowered costs.
"The salutary effects of being a high-volume hospital for pancreaticoduodenectomy are transferred when high-volume surgeons relocate," said Dr. Paul Toomey. "It seems that the benefits of a high-volume hospital are more due to who does the surgery rather than where it’s undertaken."
Dr. Toomey, a surgical fellow at the Florida Hospital, Tampa, had a unique opportunity to study what happens when two surgeons highly experienced in the Whipple procedure transferred from a busy hospital to low-volume facilities. The surgeons, who together performed more than 100 of the procedures each year, moved for personal reasons, Dr. Toomey said in an interview.
The study focused on perioperative outcomes, mortality, and readmissions in two groups of Whipple patients: the last 50 undertaken at the high-volume hospital (more than 12 pancreaticoduodenectomies per year), and the first 50 at the low-volume hospital where they worked afterward.
The patient groups were similar. Their mean age was 78 years, a little more than half were men, and the average American Society of Anesthesiologists class was 3. The rates of malignancy were similar in the high- and low-volume centers (88% vs. 82%, respectively).
Overall, the average operative time was 252 minutes, with an estimated blood loss of 300 mL. Patients were in intensive care for 2 days, with an average hospital stay of 9 days. The readmission rate was 19% and 30-day mortality, 5%.
But when Dr. Toomey compared the two time periods, he found significant differences in outcomes, which appeared to be associated with the transfer of the highly experienced surgeons. In fact, he said, outcomes were actually much better at the low- than the high-volume centers after the transfer.
The mean operative time at the low-volume centers was 205 minutes, compared with 305 minutes at the high-volume centers. Estimated blood loss was also less at the low-volume centers (350 vs. 255 mL). ICU stays were significantly shorter (1 vs. 3 days), as was total length of stay (7 vs. 12 days). Readmission rates over 30 days were similar (20% vs. 18%), as was 30-day mortality (4% vs. 6%).
"The salutary benefits of being a high-volume hospital for pancreaticoduodenectomy seem to be transferred when high-volume surgeons relocate," Dr. Toomey said. "The benefits of a high-volume hospital may be more due to who does the pancreaticoduodenectomy rather than where the pancreaticoduodenectomy is undertaken."
Dr. Thomas Wood, also of the Florida Hospital, found a similar trend in his study, which examined Whipple outcomes statewide over 20 years. He related the outcomes to concentration, rather decentralization, of care.
For his study, Dr. Wood examined data from the Florida Agency for Health Care Administration, collected over three 3-year epochs: 1992-1994, 2001-2003, and 2010-2012. The data were sorted by surgeon volume of pancreaticoduodenectomy during these periods and correlated to length of stay, in-hospital mortality, and hospital charges, which were adjusted to 2012 dollars.
Over the 9 years, 893 surgeons performed 3,531 pancreaticoduodenectomies. During each epoch, the number of surgeons went down as the number of operations increased.
In the first epoch, 363 surgeons performed 729 operations. In the second, 334 surgeons performed 1,233 surgeries, and in the third, 196 performed 1,569 operations.
"By 2010-2012, 46% fewer surgeons undertook 115% more surgeries compared to the first period," Dr. Wood said. "In 1992-1994, 62% of pancreaticoduodenectomies were undertaken by surgeons who performed one or fewer per year. This fell to 13% by 2010-2012."
At the same time, the number of surgeons who performed more than 36 procedures in each 3-year period (12 per year) grew significantly. In the first epoch, one surgeon alone performed 45 procedures. In the second, six surgeons performed a total of 361. And in the third epoch, 11 surgeons performed 806 Whipples.
"From [the first through third periods,] there was an 11-fold increase in the number of high-volume surgeons and a corresponding 18-fold increase in the number of pancreaticoduodenectomies by surgeons who were performing at least 12 each year. They were performing more than 50% of these operations."
A separate analysis of just the 2010-2012 data evaluated outcomes by surgeons’ operation volume.
In the first epoch, in-hospital mortality was about 12%. In the second, it fell to 8%, and by the third, to 4%. Patients whose surgeons performed one to nine procedures (up to three per year) were hospitalized an average of about 14 days. Those whose surgeons performed 19 to 36 procedures (up to 12 per year) stayed an average of 8 days – a significant difference.
Mortality followed the same pattern. About 9% of patients whose surgeons performed one to three procedures per year died after surgery, compared with 2% of those whose doctors performed 12 procedures per year.
These more experienced surgeons also discharged more patients to home rather than nursing facilities (88% vs. 82%, a significant difference).
Both hospital and surgeon volume also affected costs. Overall, hospital costs increased significantly, even after adjustment for inflation, jumping from $93,000 to $133,000. But surgeons who performed at least 12 Whipples per year did so at a half the cost of those who performed 1-3 per year ($100,000 vs. $200,000).
"Suffice it to say, the busiest surgeons got the best results," Dr. Wood said.
Despite advances in centralizing this kind of specialized care, though, many low-volume centers are still performing the operations, said Dr. Jeffrey Sutton of the University of Cincinnati. "Research continues to show that high-volume centers have better outcomes," he said. "And yet a significant number of cases are still being done at hospitals that do less than one per year."
If research data aren’t enough to persuade hospitals to send patients to regional centers, Dr. Sutton wondered, could money be a motivating factor? He examined the records of almost 10,000 Whipple operations performed at 419 centers that are part of the University Health Systems Consortium clinical database. Of these, 120 were academic centers and 299 were affiliated hospitals. The procedures were performed from 2009 to 2011. Clinical outcomes included length of stay, mortality, and readmissions. He also assessed the cost of both the index admission and readmissions.
Hospitals were divided into volume quintiles of lowest, low, middle, high, and highest. The lowest-volume centers performed up to 21 cases/year in 2009 to up to 23 in 2011. The highest-volume centers performed up to 180 cases/year in 2009 and up to 216 in 2011.
Intraoperative mortality hovered around 2% at the middle-, high-, and highest-volume centers. At the low-volume centers, it reached 2.5% – not significantly different. But at the lowest-volume centers, 30-day mortality was significantly higher – nearly 4%.
Length of stay was similarly associated with volume. In low-, middle-, and high-volume centers, it was about 9 days. But in the lowest-volume centers, the average length of stay was 11 days – significantly longer than any of the others.
Readmission rates over the first postoperative month were also lowest in the highest-volume centers (16.5%). In the low-volume centers, 30-day readmission was just under 19%. But in the middle-, low-, and lowest-volume centers, it was significantly greater, hovering at nearly 20%.
"It’s not only that lower-volume centers are holding on to patients longer, they also are readmitting those same patients significantly more often," Dr. Sutton noted.
The cost analysis looked at Medicare charge data. "When both index and readmission costs were considered, the median per-patient cost at the lowest-volume centers was $23,005 – 11% more than at the highest-volume center."
But there was no significant difference in the cost of readmissions. "That means that the difference of about $2,263 extra per case was based solely on the index admission," Dr. Sutton said. "Essentially what we saw was that the more cases that are performed, the cheaper each individual case becomes."
"To put it bluntly, some low-volume centers are currently reimbursed higher sums of money for delivering suboptimal care to patients," Dr. Sutton said in an interview. In our current health care climate, which emphasizes improved outcomes at lower costs, this is a travesty. As health service researchers, it is our obligation to our patients to analyze and disseminate these data in an effort to urge policymakers to limit the financial reimbursements for poorer-performing providers."
None of the researchers quoted in this article reported any financial disclosures.
MIAMI BEACH – Studies continue to confirm it: When it comes to complex surgical procedures, higher volume equals better outcomes. But like the chicken-or-egg conundrum, researchers are asking which factor comes first – surgeon or facility.
Data presented at the annual meeting of the Americas Hepato-Pancreato-Biliary Association suggest that personal experience makes the biggest difference, at least for the difficult Whipple procedure. Surgeons who performed the highest number of pancreaticoduodenectomies each year had the best outcomes; when they transferred to low-volume hospitals with historically poor results, these surgeons improved perioperative complications, mortality, and readmissions, and lowered costs.
"The salutary effects of being a high-volume hospital for pancreaticoduodenectomy are transferred when high-volume surgeons relocate," said Dr. Paul Toomey. "It seems that the benefits of a high-volume hospital are more due to who does the surgery rather than where it’s undertaken."
Dr. Toomey, a surgical fellow at the Florida Hospital, Tampa, had a unique opportunity to study what happens when two surgeons highly experienced in the Whipple procedure transferred from a busy hospital to low-volume facilities. The surgeons, who together performed more than 100 of the procedures each year, moved for personal reasons, Dr. Toomey said in an interview.
The study focused on perioperative outcomes, mortality, and readmissions in two groups of Whipple patients: the last 50 undertaken at the high-volume hospital (more than 12 pancreaticoduodenectomies per year), and the first 50 at the low-volume hospital where they worked afterward.
The patient groups were similar. Their mean age was 78 years, a little more than half were men, and the average American Society of Anesthesiologists class was 3. The rates of malignancy were similar in the high- and low-volume centers (88% vs. 82%, respectively).
Overall, the average operative time was 252 minutes, with an estimated blood loss of 300 mL. Patients were in intensive care for 2 days, with an average hospital stay of 9 days. The readmission rate was 19% and 30-day mortality, 5%.
But when Dr. Toomey compared the two time periods, he found significant differences in outcomes, which appeared to be associated with the transfer of the highly experienced surgeons. In fact, he said, outcomes were actually much better at the low- than the high-volume centers after the transfer.
The mean operative time at the low-volume centers was 205 minutes, compared with 305 minutes at the high-volume centers. Estimated blood loss was also less at the low-volume centers (350 vs. 255 mL). ICU stays were significantly shorter (1 vs. 3 days), as was total length of stay (7 vs. 12 days). Readmission rates over 30 days were similar (20% vs. 18%), as was 30-day mortality (4% vs. 6%).
"The salutary benefits of being a high-volume hospital for pancreaticoduodenectomy seem to be transferred when high-volume surgeons relocate," Dr. Toomey said. "The benefits of a high-volume hospital may be more due to who does the pancreaticoduodenectomy rather than where the pancreaticoduodenectomy is undertaken."
Dr. Thomas Wood, also of the Florida Hospital, found a similar trend in his study, which examined Whipple outcomes statewide over 20 years. He related the outcomes to concentration, rather decentralization, of care.
For his study, Dr. Wood examined data from the Florida Agency for Health Care Administration, collected over three 3-year epochs: 1992-1994, 2001-2003, and 2010-2012. The data were sorted by surgeon volume of pancreaticoduodenectomy during these periods and correlated to length of stay, in-hospital mortality, and hospital charges, which were adjusted to 2012 dollars.
Over the 9 years, 893 surgeons performed 3,531 pancreaticoduodenectomies. During each epoch, the number of surgeons went down as the number of operations increased.
In the first epoch, 363 surgeons performed 729 operations. In the second, 334 surgeons performed 1,233 surgeries, and in the third, 196 performed 1,569 operations.
"By 2010-2012, 46% fewer surgeons undertook 115% more surgeries compared to the first period," Dr. Wood said. "In 1992-1994, 62% of pancreaticoduodenectomies were undertaken by surgeons who performed one or fewer per year. This fell to 13% by 2010-2012."
At the same time, the number of surgeons who performed more than 36 procedures in each 3-year period (12 per year) grew significantly. In the first epoch, one surgeon alone performed 45 procedures. In the second, six surgeons performed a total of 361. And in the third epoch, 11 surgeons performed 806 Whipples.
"From [the first through third periods,] there was an 11-fold increase in the number of high-volume surgeons and a corresponding 18-fold increase in the number of pancreaticoduodenectomies by surgeons who were performing at least 12 each year. They were performing more than 50% of these operations."
A separate analysis of just the 2010-2012 data evaluated outcomes by surgeons’ operation volume.
In the first epoch, in-hospital mortality was about 12%. In the second, it fell to 8%, and by the third, to 4%. Patients whose surgeons performed one to nine procedures (up to three per year) were hospitalized an average of about 14 days. Those whose surgeons performed 19 to 36 procedures (up to 12 per year) stayed an average of 8 days – a significant difference.
Mortality followed the same pattern. About 9% of patients whose surgeons performed one to three procedures per year died after surgery, compared with 2% of those whose doctors performed 12 procedures per year.
These more experienced surgeons also discharged more patients to home rather than nursing facilities (88% vs. 82%, a significant difference).
Both hospital and surgeon volume also affected costs. Overall, hospital costs increased significantly, even after adjustment for inflation, jumping from $93,000 to $133,000. But surgeons who performed at least 12 Whipples per year did so at a half the cost of those who performed 1-3 per year ($100,000 vs. $200,000).
"Suffice it to say, the busiest surgeons got the best results," Dr. Wood said.
Despite advances in centralizing this kind of specialized care, though, many low-volume centers are still performing the operations, said Dr. Jeffrey Sutton of the University of Cincinnati. "Research continues to show that high-volume centers have better outcomes," he said. "And yet a significant number of cases are still being done at hospitals that do less than one per year."
If research data aren’t enough to persuade hospitals to send patients to regional centers, Dr. Sutton wondered, could money be a motivating factor? He examined the records of almost 10,000 Whipple operations performed at 419 centers that are part of the University Health Systems Consortium clinical database. Of these, 120 were academic centers and 299 were affiliated hospitals. The procedures were performed from 2009 to 2011. Clinical outcomes included length of stay, mortality, and readmissions. He also assessed the cost of both the index admission and readmissions.
Hospitals were divided into volume quintiles of lowest, low, middle, high, and highest. The lowest-volume centers performed up to 21 cases/year in 2009 to up to 23 in 2011. The highest-volume centers performed up to 180 cases/year in 2009 and up to 216 in 2011.
Intraoperative mortality hovered around 2% at the middle-, high-, and highest-volume centers. At the low-volume centers, it reached 2.5% – not significantly different. But at the lowest-volume centers, 30-day mortality was significantly higher – nearly 4%.
Length of stay was similarly associated with volume. In low-, middle-, and high-volume centers, it was about 9 days. But in the lowest-volume centers, the average length of stay was 11 days – significantly longer than any of the others.
Readmission rates over the first postoperative month were also lowest in the highest-volume centers (16.5%). In the low-volume centers, 30-day readmission was just under 19%. But in the middle-, low-, and lowest-volume centers, it was significantly greater, hovering at nearly 20%.
"It’s not only that lower-volume centers are holding on to patients longer, they also are readmitting those same patients significantly more often," Dr. Sutton noted.
The cost analysis looked at Medicare charge data. "When both index and readmission costs were considered, the median per-patient cost at the lowest-volume centers was $23,005 – 11% more than at the highest-volume center."
But there was no significant difference in the cost of readmissions. "That means that the difference of about $2,263 extra per case was based solely on the index admission," Dr. Sutton said. "Essentially what we saw was that the more cases that are performed, the cheaper each individual case becomes."
"To put it bluntly, some low-volume centers are currently reimbursed higher sums of money for delivering suboptimal care to patients," Dr. Sutton said in an interview. In our current health care climate, which emphasizes improved outcomes at lower costs, this is a travesty. As health service researchers, it is our obligation to our patients to analyze and disseminate these data in an effort to urge policymakers to limit the financial reimbursements for poorer-performing providers."
None of the researchers quoted in this article reported any financial disclosures.
AT AHPBA 2014
Major finding: When high-volume surgeons transferred to low-volume institutions, these surgeons improved perioperative complications, mortality, and readmissions, and lowered costs in the low-volume institutions. The mean operative time at the low-volume centers was 205 minutes, compared with 305 minutes at the high-volume centers. Estimated blood loss was also less at the low-volume centers (350 vs. 255 mL), as was total length of stay (7 vs. 12 days).
Data source: Data from more than 100 Whipple procedures performed by two experienced surgeons who transferred to low-volume institutions.
Disclosures: None of the researchers quoted in this article reported any financial disclosures.
Outcomes similar for two reconstruction techniques, except for risk of severe complications
MIAMI BEACH* – There appears to be no difference in the rate of anastomotic leak in pancreaticogastrostomy compared with pancreaticojejunostomy reconstruction after a Whipple procedure, but pancreaticogastrostomy does appear to increase the risk of some serious postoperative complications, a study found.
"We didn’t show any significant differences in terms of leaks, severity of leaks, or even overall complications," Dr. Jan Grendar said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association. "But we did show a significant difference in complications of Clavien grades III-V severity. This anastomosis just did a little bit worse in terms of severe complications."
Grade III Clavien complications are those that require a second invasive procedure, like reoperation or drainage, with local or general anesthesia. Grade IV complications are more serious – they include organ failures such as renal failure requiring hemodialysis, heart failure, and liver failure, and intubation. The Grade V complication is patient death.
Dr. Grendar, a surgical resident at the University of Calgary (Alta.), and his colleagues randomized 98 patients with benign or malignant pancreatic disease to either of the two reconstruction techniques after a Whipple procedure. Pancreaticojejunostomy (PJ) is the procedure typically performed in North America. Pancreaticogastrostomy (PG) is typically performed in Europe. The hepatobiliary pancreatic surgeons and residents at the university, however, have become adept at this second procedure and employ it as an alternative reconstruction, depending on the characteristics of the pancreas discovered during surgery. They most often use it on patients who have a soft pancreas or small pancreatic duct.
All of the patients in the study had a pancreatic or periampullary neoplasm that appeared resectable on preoperative imaging. There were no differences in baseline patient characteristics. The mean age was 64 in the PG group and 68 in the PJ group. The median Charlson comorbidity index score was 2.
The intraoperative outcomes were mostly similar. Gland mobilization occurred significantly more often in the PG group (31 vs. 18 mm). Significantly fewer PG patients had a two-layer anastomosis (77% vs. 94%). The mean pancreatic duct size was smaller in the PG patients (3.8 vs. 4.3 mm), but this wasn’t statistically significant. Significantly fewer PG patients had a pancreatic duct stent placed (22% vs. 83%).
Postoperative outcomes included pancreatic fistula, any postoperative complications, severe complications, and length of stay.
There was no difference between the groups in Clavien grade complications separately, but significantly more PG patients had severe, Clavien grade III-V complications (31% vs. 12%). But these didn’t affect the mean length of stay, which was similar between the groups (17 vs. 14 days).
In a multivariate analysis, only having a soft pancreas significantly increased the risk of developing a pancreatic fistula (odds ratio, 5.87). Female gender significantly decreased the risk (OR, 0.31). This most likely represents a correlation between pancreatic texture and patient sex rather than a true protective property of being female. Having a soft pancreas also significantly increased the risk of any postoperative complications (OR, 3.08).
Several factors significantly increased the risk of a severe complication. These included a baseline American Society of Anesthesiologists grade of 2 or 3 (OR, 12.75 and 29.56, respectively). Being randomized to the PJ procedure significantly decreased the risk of a severe complication (OR, 0.11).
"Unlike the European centers that report different outcomes, these results are coming from a center that wasn’t very enthusiastic about this type of reconstruction prior to this study," Dr. Grendar said in an interview. "Despite the initial preference, high-risk patients in Calgary, those with soft pancreatic glands and small pancreatic ducts, are now likely to be offered a pancreaticogastrostomy"
Dr. Grendar said he had no relevant financial disclosures.
*Correction, 3/11/2014: An earlier version of the article misstated the name of the city where the AHPBA meeting took place.
MIAMI BEACH* – There appears to be no difference in the rate of anastomotic leak in pancreaticogastrostomy compared with pancreaticojejunostomy reconstruction after a Whipple procedure, but pancreaticogastrostomy does appear to increase the risk of some serious postoperative complications, a study found.
"We didn’t show any significant differences in terms of leaks, severity of leaks, or even overall complications," Dr. Jan Grendar said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association. "But we did show a significant difference in complications of Clavien grades III-V severity. This anastomosis just did a little bit worse in terms of severe complications."
Grade III Clavien complications are those that require a second invasive procedure, like reoperation or drainage, with local or general anesthesia. Grade IV complications are more serious – they include organ failures such as renal failure requiring hemodialysis, heart failure, and liver failure, and intubation. The Grade V complication is patient death.
Dr. Grendar, a surgical resident at the University of Calgary (Alta.), and his colleagues randomized 98 patients with benign or malignant pancreatic disease to either of the two reconstruction techniques after a Whipple procedure. Pancreaticojejunostomy (PJ) is the procedure typically performed in North America. Pancreaticogastrostomy (PG) is typically performed in Europe. The hepatobiliary pancreatic surgeons and residents at the university, however, have become adept at this second procedure and employ it as an alternative reconstruction, depending on the characteristics of the pancreas discovered during surgery. They most often use it on patients who have a soft pancreas or small pancreatic duct.
All of the patients in the study had a pancreatic or periampullary neoplasm that appeared resectable on preoperative imaging. There were no differences in baseline patient characteristics. The mean age was 64 in the PG group and 68 in the PJ group. The median Charlson comorbidity index score was 2.
The intraoperative outcomes were mostly similar. Gland mobilization occurred significantly more often in the PG group (31 vs. 18 mm). Significantly fewer PG patients had a two-layer anastomosis (77% vs. 94%). The mean pancreatic duct size was smaller in the PG patients (3.8 vs. 4.3 mm), but this wasn’t statistically significant. Significantly fewer PG patients had a pancreatic duct stent placed (22% vs. 83%).
Postoperative outcomes included pancreatic fistula, any postoperative complications, severe complications, and length of stay.
There was no difference between the groups in Clavien grade complications separately, but significantly more PG patients had severe, Clavien grade III-V complications (31% vs. 12%). But these didn’t affect the mean length of stay, which was similar between the groups (17 vs. 14 days).
In a multivariate analysis, only having a soft pancreas significantly increased the risk of developing a pancreatic fistula (odds ratio, 5.87). Female gender significantly decreased the risk (OR, 0.31). This most likely represents a correlation between pancreatic texture and patient sex rather than a true protective property of being female. Having a soft pancreas also significantly increased the risk of any postoperative complications (OR, 3.08).
Several factors significantly increased the risk of a severe complication. These included a baseline American Society of Anesthesiologists grade of 2 or 3 (OR, 12.75 and 29.56, respectively). Being randomized to the PJ procedure significantly decreased the risk of a severe complication (OR, 0.11).
"Unlike the European centers that report different outcomes, these results are coming from a center that wasn’t very enthusiastic about this type of reconstruction prior to this study," Dr. Grendar said in an interview. "Despite the initial preference, high-risk patients in Calgary, those with soft pancreatic glands and small pancreatic ducts, are now likely to be offered a pancreaticogastrostomy"
Dr. Grendar said he had no relevant financial disclosures.
*Correction, 3/11/2014: An earlier version of the article misstated the name of the city where the AHPBA meeting took place.
MIAMI BEACH* – There appears to be no difference in the rate of anastomotic leak in pancreaticogastrostomy compared with pancreaticojejunostomy reconstruction after a Whipple procedure, but pancreaticogastrostomy does appear to increase the risk of some serious postoperative complications, a study found.
"We didn’t show any significant differences in terms of leaks, severity of leaks, or even overall complications," Dr. Jan Grendar said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association. "But we did show a significant difference in complications of Clavien grades III-V severity. This anastomosis just did a little bit worse in terms of severe complications."
Grade III Clavien complications are those that require a second invasive procedure, like reoperation or drainage, with local or general anesthesia. Grade IV complications are more serious – they include organ failures such as renal failure requiring hemodialysis, heart failure, and liver failure, and intubation. The Grade V complication is patient death.
Dr. Grendar, a surgical resident at the University of Calgary (Alta.), and his colleagues randomized 98 patients with benign or malignant pancreatic disease to either of the two reconstruction techniques after a Whipple procedure. Pancreaticojejunostomy (PJ) is the procedure typically performed in North America. Pancreaticogastrostomy (PG) is typically performed in Europe. The hepatobiliary pancreatic surgeons and residents at the university, however, have become adept at this second procedure and employ it as an alternative reconstruction, depending on the characteristics of the pancreas discovered during surgery. They most often use it on patients who have a soft pancreas or small pancreatic duct.
All of the patients in the study had a pancreatic or periampullary neoplasm that appeared resectable on preoperative imaging. There were no differences in baseline patient characteristics. The mean age was 64 in the PG group and 68 in the PJ group. The median Charlson comorbidity index score was 2.
The intraoperative outcomes were mostly similar. Gland mobilization occurred significantly more often in the PG group (31 vs. 18 mm). Significantly fewer PG patients had a two-layer anastomosis (77% vs. 94%). The mean pancreatic duct size was smaller in the PG patients (3.8 vs. 4.3 mm), but this wasn’t statistically significant. Significantly fewer PG patients had a pancreatic duct stent placed (22% vs. 83%).
Postoperative outcomes included pancreatic fistula, any postoperative complications, severe complications, and length of stay.
There was no difference between the groups in Clavien grade complications separately, but significantly more PG patients had severe, Clavien grade III-V complications (31% vs. 12%). But these didn’t affect the mean length of stay, which was similar between the groups (17 vs. 14 days).
In a multivariate analysis, only having a soft pancreas significantly increased the risk of developing a pancreatic fistula (odds ratio, 5.87). Female gender significantly decreased the risk (OR, 0.31). This most likely represents a correlation between pancreatic texture and patient sex rather than a true protective property of being female. Having a soft pancreas also significantly increased the risk of any postoperative complications (OR, 3.08).
Several factors significantly increased the risk of a severe complication. These included a baseline American Society of Anesthesiologists grade of 2 or 3 (OR, 12.75 and 29.56, respectively). Being randomized to the PJ procedure significantly decreased the risk of a severe complication (OR, 0.11).
"Unlike the European centers that report different outcomes, these results are coming from a center that wasn’t very enthusiastic about this type of reconstruction prior to this study," Dr. Grendar said in an interview. "Despite the initial preference, high-risk patients in Calgary, those with soft pancreatic glands and small pancreatic ducts, are now likely to be offered a pancreaticogastrostomy"
Dr. Grendar said he had no relevant financial disclosures.
*Correction, 3/11/2014: An earlier version of the article misstated the name of the city where the AHPBA meeting took place.
AT AHPBA 2014
Major finding: Severe complications occurred in significantly more Whipple patients who had a pancreaticogastrostomy reconstruction than a pancreaticojejunostomy (31% vs. 12%).
Data source: A randomized study involving 98 patients.
Disclosures: Dr. Grendar said he had no relevant financial disclosures.
No propofol reactions seen in egg, soy allergic patients
SAN DIEGO – Patients with food allergies – including those with a history of anaphylaxis – had no adverse reactions to propofol administered for anesthesia during endoscopy, based on a study that included 160 patients with food allergies.
Intravenous propofol (2,6-diisopropylphenol) includes lipid suspensions that contain egg lecithin/phosphatide and soy oil, ingredients that have raised "concern regarding administration of propofol in patients with egg and soy allergy," explained Dr. Harshna Mehta, a pediatric allergist-immunologist at the Icahn School of Medicine at Mount Sinai, New York. "Additionally, since the peanut is a legume similar to soy, there is also potential concern for peanut allergic patients."
Case reports of propofol-associated allergic reactions – presumably related to cross-reactivity to foods – have appeared in the medical literature. "However, most of these cases lacked confirmatory testing for actual food allergy vs. mere sensitization," Dr. Mehta said in an interview before the annual meeting of the American Academy of Allergy, Asthma, and Immunology, where the study results were presented.
Prior to this study, the largest study included 28 egg allergic patients, with two having a history of anaphylaxis (Anesth. Analg. 2011;113: 140-4).
Dr. Mehta and her associates reviewed the records of 563 patients who had endoscopies performed at the Mount Sinai Center for Eosinophilic Disorders from November 2004 to January 2014.
The researchers identified 160 patients with a median age of 14 years who had one or more food allergies, including 31 with a history of anaphylaxis. Egg, peanut, and soy allergies were confirmed based on finding elevated food specific serum IgE levels, positive skin prick tests and/or convincing allergic reaction history. Patients were included in the study if anesthesia records indicated propofol as the chief anesthetic administered.
Of the 160 patients, 95 had evidence of egg allergy (median egg-IgE = 9.57 kIU/L); 15 of these patients had a history of an anaphylactic reaction to egg. Of the 28 patients with confirmed soy allergy (median soy-IgE = 6.63 kU/L), 2 had a history of anaphylaxis. Dr. Mehta also reported that 117 patients had peanut allergy (median peanut-IgE =38.8 kIU/L); 11 o these patients had a history of anaphylaxis to peanuts.
There were no reported reactions to propofol in any of the patients.
"The most surprising finding was the number of egg/peanut/soy patients who have significant allergic comorbidities – such as history of anaphylaxis, allergic rhinitis, asthma, and atopic disease – that have safely received this medication," Dr. Mehta noted. "We are still in the process of determining the statistical confidence with which we can say how safe propofol is for administration to egg/soy/peanut allergic patients. We are also planning to test the product in the laboratory for the presence of egg protein."
Dr. Mehta said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients with food allergies – including those with a history of anaphylaxis – had no adverse reactions to propofol administered for anesthesia during endoscopy, based on a study that included 160 patients with food allergies.
Intravenous propofol (2,6-diisopropylphenol) includes lipid suspensions that contain egg lecithin/phosphatide and soy oil, ingredients that have raised "concern regarding administration of propofol in patients with egg and soy allergy," explained Dr. Harshna Mehta, a pediatric allergist-immunologist at the Icahn School of Medicine at Mount Sinai, New York. "Additionally, since the peanut is a legume similar to soy, there is also potential concern for peanut allergic patients."
Case reports of propofol-associated allergic reactions – presumably related to cross-reactivity to foods – have appeared in the medical literature. "However, most of these cases lacked confirmatory testing for actual food allergy vs. mere sensitization," Dr. Mehta said in an interview before the annual meeting of the American Academy of Allergy, Asthma, and Immunology, where the study results were presented.
Prior to this study, the largest study included 28 egg allergic patients, with two having a history of anaphylaxis (Anesth. Analg. 2011;113: 140-4).
Dr. Mehta and her associates reviewed the records of 563 patients who had endoscopies performed at the Mount Sinai Center for Eosinophilic Disorders from November 2004 to January 2014.
The researchers identified 160 patients with a median age of 14 years who had one or more food allergies, including 31 with a history of anaphylaxis. Egg, peanut, and soy allergies were confirmed based on finding elevated food specific serum IgE levels, positive skin prick tests and/or convincing allergic reaction history. Patients were included in the study if anesthesia records indicated propofol as the chief anesthetic administered.
Of the 160 patients, 95 had evidence of egg allergy (median egg-IgE = 9.57 kIU/L); 15 of these patients had a history of an anaphylactic reaction to egg. Of the 28 patients with confirmed soy allergy (median soy-IgE = 6.63 kU/L), 2 had a history of anaphylaxis. Dr. Mehta also reported that 117 patients had peanut allergy (median peanut-IgE =38.8 kIU/L); 11 o these patients had a history of anaphylaxis to peanuts.
There were no reported reactions to propofol in any of the patients.
"The most surprising finding was the number of egg/peanut/soy patients who have significant allergic comorbidities – such as history of anaphylaxis, allergic rhinitis, asthma, and atopic disease – that have safely received this medication," Dr. Mehta noted. "We are still in the process of determining the statistical confidence with which we can say how safe propofol is for administration to egg/soy/peanut allergic patients. We are also planning to test the product in the laboratory for the presence of egg protein."
Dr. Mehta said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients with food allergies – including those with a history of anaphylaxis – had no adverse reactions to propofol administered for anesthesia during endoscopy, based on a study that included 160 patients with food allergies.
Intravenous propofol (2,6-diisopropylphenol) includes lipid suspensions that contain egg lecithin/phosphatide and soy oil, ingredients that have raised "concern regarding administration of propofol in patients with egg and soy allergy," explained Dr. Harshna Mehta, a pediatric allergist-immunologist at the Icahn School of Medicine at Mount Sinai, New York. "Additionally, since the peanut is a legume similar to soy, there is also potential concern for peanut allergic patients."
Case reports of propofol-associated allergic reactions – presumably related to cross-reactivity to foods – have appeared in the medical literature. "However, most of these cases lacked confirmatory testing for actual food allergy vs. mere sensitization," Dr. Mehta said in an interview before the annual meeting of the American Academy of Allergy, Asthma, and Immunology, where the study results were presented.
Prior to this study, the largest study included 28 egg allergic patients, with two having a history of anaphylaxis (Anesth. Analg. 2011;113: 140-4).
Dr. Mehta and her associates reviewed the records of 563 patients who had endoscopies performed at the Mount Sinai Center for Eosinophilic Disorders from November 2004 to January 2014.
The researchers identified 160 patients with a median age of 14 years who had one or more food allergies, including 31 with a history of anaphylaxis. Egg, peanut, and soy allergies were confirmed based on finding elevated food specific serum IgE levels, positive skin prick tests and/or convincing allergic reaction history. Patients were included in the study if anesthesia records indicated propofol as the chief anesthetic administered.
Of the 160 patients, 95 had evidence of egg allergy (median egg-IgE = 9.57 kIU/L); 15 of these patients had a history of an anaphylactic reaction to egg. Of the 28 patients with confirmed soy allergy (median soy-IgE = 6.63 kU/L), 2 had a history of anaphylaxis. Dr. Mehta also reported that 117 patients had peanut allergy (median peanut-IgE =38.8 kIU/L); 11 o these patients had a history of anaphylaxis to peanuts.
There were no reported reactions to propofol in any of the patients.
"The most surprising finding was the number of egg/peanut/soy patients who have significant allergic comorbidities – such as history of anaphylaxis, allergic rhinitis, asthma, and atopic disease – that have safely received this medication," Dr. Mehta noted. "We are still in the process of determining the statistical confidence with which we can say how safe propofol is for administration to egg/soy/peanut allergic patients. We are also planning to test the product in the laboratory for the presence of egg protein."
Dr. Mehta said that she had no relevant financial conflicts to disclose.
AT THE 2014 AAAAI ANNUAL MEETING
Major finding: No allergic reactions were reported in patients with known food allergies who received propofol prior to undergoing endoscopy.
Data source: A review of records from 160 food allergy patients who had endoscopies performed at the Mount Sinai Center for Eosinophilic Disorders from November 2004 to January 2014.
Disclosures: Dr. Mehta said that she had no relevant financial conflicts to disclose.