User login
Monkeypox largely a mystery for pregnant people
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with high-risk pregnancies could die if Roe is overturned
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
High maternal, fetal morbidity rates in SLE pregnancies
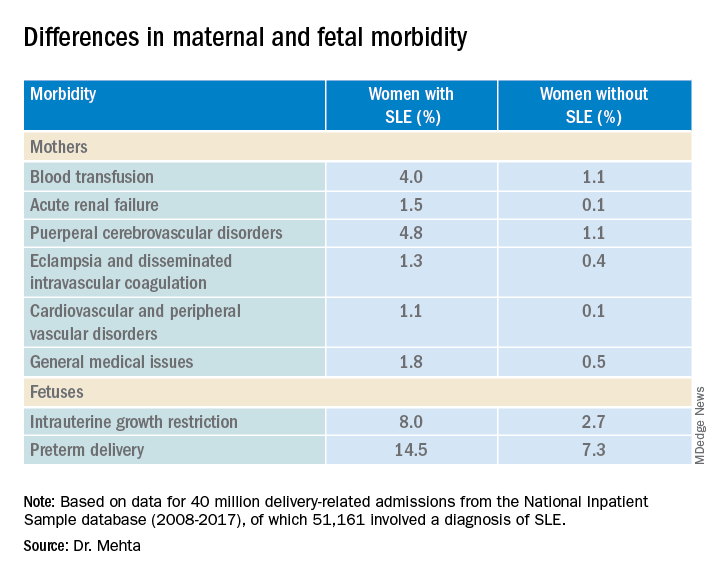
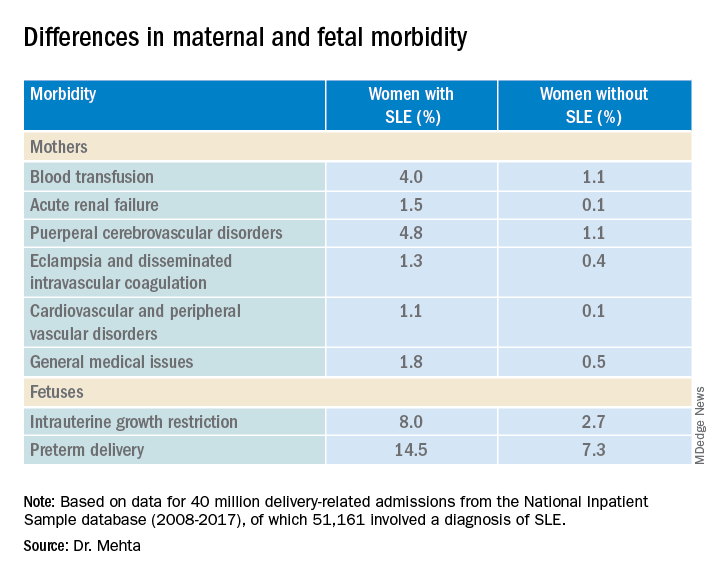
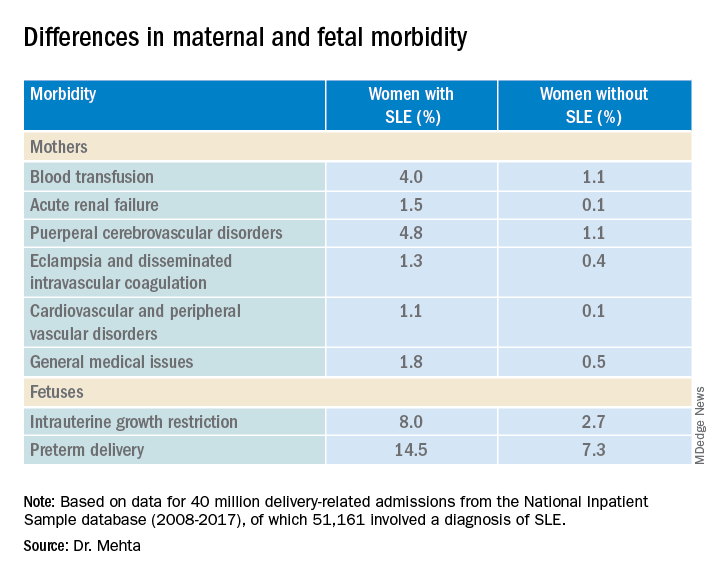
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
AT THE EULAR 2022 CONGRESS
At-home vagus nerve stimulation promising for postpartum depression
At-home, noninvasive auricular vagus nerve stimulation (aVNS) therapy is well-tolerated and associated with a significant reduction in postpartum depressive and anxiety symptoms, new research suggests.
In a small proof-of-concept pilot study of 25 women with postpartum depression receiving 6 weeks of daily aVNS treatment, results showed that 74% achieved response and 61% achieved remission, as shown in reduced scores on the Hamilton Rating Scale for Depression (HAM-D17).
Although invasive electrical stimulation of the vagus nerve was approved by the U.S. Food and Drug Administration for treatment-resistant depression in 2005, it involves risk for implantation, infection, and significant side effects, coinvestigator Kristina M. Deligiannidis, MD, director, Women’s Behavioral Health, Zucker Hillside Hospital, Northwell Health, Glen Oaks, New York, told this news organization.
“This newer approach, transcutaneous auricular VNS, is non-invasive, is well tolerated, and has shown initial efficacy in major depression in men and women,” she said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) Annual Meeting.
Potential alternative to meds
“Given that aVNS is a non-invasive treatment which can be administered at home, we wanted to test if this approach was safe, feasible, and could reduce depressive symptoms in women with postpartum depression, as many of these women have barriers to accessing current treatments,” Dr. Deligiannidis said.
Auricular VNS uses surface skin electrodes to stimulate nerve endings of a branch of the vagus nerve, located on the surface of the outer ear. Those nerve endings travel to the brain where they have been shown to modulate brain communication in areas important for mood and anxiety regulation, she said.
Dr. Deligiannidis noted that evidence-based treatments for postpartum depression include psychotherapies and antidepressants. However, some women have difficulty accessing weekly psychotherapy, and, when antidepressants are indicated, many are reluctant to take them if they are breastfeeding because of concerns about the medications getting into their breast milk, she said.
Although most antidepressants are safe in lactation, many women postpone antidepressant treatment until they have finished breastfeeding, which can postpone their postpartum depression treatment, Dr. Deligiannidis added.
“At home treatments reduce many barriers women have to current treatments, and this intervention [of aVNS] does not impact breastfeeding, as it is not a medication approach,” she said.
The researchers enrolled 25 women (mean age, 33.7 years) diagnosed with postpartum depression. Ten of the women (40%) were on a stable dose of antidepressant medication.
The participants self-administered 6 weeks of open-label aVNS for 15 minutes daily at home. They were then observed without intervention for an additional 2 weeks. The women also completed medical, psychiatric, and safety interviews throughout the study period.
Promising findings
At baseline, the mean HAM-D17 was 18.4 and was similar for those on (17.8) and off (18.9) antidepressants.
By week 6, the mean HAM-D17 total score decreased by 9.7 points overall, compared with baseline score. For participants on antidepressants, the HAM-D17 decreased by 8.7 points; for women off antidepressants, it decreased by 10.3 points.
In addition, 74% of the women achieved a response to the therapy, and 61% achieved remission of their depressive symptoms.
The most common adverse effects were discomfort (n = 5 patients), headache (n = 3), and dizziness (n = 2). All resolved without intervention.
Commenting on the findings, Anita Clayton, MD, professor and chair, department of psychiatry and neurobehavioral sciences, University of Virginia School of Medicine, Charlottesville, said the study was “quite interesting.”
Dr. Clayton, who was not involved with the research, also noted the “pretty high” response and remission rates.
“So, I think this does have promise, and it would be worth doing a study where you look at placebo versus this treatment,” she said.
“Many women are fearful of taking medicines postpartum, even peripartum, unless they have had pre-existing severe depression. This is not a medicine, and it sounds like it could be useful even in people who are pregnant, although it’s harder to do studies in pregnant women,” Dr. Clayton added.
The study was funded by Nesos Corporation. Dr. Deligiannidis received contracted research funds from Nesos Corporation to conduct this study. She also serves as a consultant to Sage Therapeutics, Brii Biosciences, and GH Research. Dr. Clayton reports financial relationships with Dare Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, AbbVie, Brii Biosciences, Fabre-Kramer, Field Trip Health, Mind Cure Health, Ovoca Bio, PureTech Health, S1 Biopharma, Takeda/Lundbeck, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Changes in Sexual Functioning Questionnaire, Guilford Publications, Euthymics Bioscience, and Mediflix.
A version of this article first appeared on Medscape.com.
At-home, noninvasive auricular vagus nerve stimulation (aVNS) therapy is well-tolerated and associated with a significant reduction in postpartum depressive and anxiety symptoms, new research suggests.
In a small proof-of-concept pilot study of 25 women with postpartum depression receiving 6 weeks of daily aVNS treatment, results showed that 74% achieved response and 61% achieved remission, as shown in reduced scores on the Hamilton Rating Scale for Depression (HAM-D17).
Although invasive electrical stimulation of the vagus nerve was approved by the U.S. Food and Drug Administration for treatment-resistant depression in 2005, it involves risk for implantation, infection, and significant side effects, coinvestigator Kristina M. Deligiannidis, MD, director, Women’s Behavioral Health, Zucker Hillside Hospital, Northwell Health, Glen Oaks, New York, told this news organization.
“This newer approach, transcutaneous auricular VNS, is non-invasive, is well tolerated, and has shown initial efficacy in major depression in men and women,” she said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) Annual Meeting.
Potential alternative to meds
“Given that aVNS is a non-invasive treatment which can be administered at home, we wanted to test if this approach was safe, feasible, and could reduce depressive symptoms in women with postpartum depression, as many of these women have barriers to accessing current treatments,” Dr. Deligiannidis said.
Auricular VNS uses surface skin electrodes to stimulate nerve endings of a branch of the vagus nerve, located on the surface of the outer ear. Those nerve endings travel to the brain where they have been shown to modulate brain communication in areas important for mood and anxiety regulation, she said.
Dr. Deligiannidis noted that evidence-based treatments for postpartum depression include psychotherapies and antidepressants. However, some women have difficulty accessing weekly psychotherapy, and, when antidepressants are indicated, many are reluctant to take them if they are breastfeeding because of concerns about the medications getting into their breast milk, she said.
Although most antidepressants are safe in lactation, many women postpone antidepressant treatment until they have finished breastfeeding, which can postpone their postpartum depression treatment, Dr. Deligiannidis added.
“At home treatments reduce many barriers women have to current treatments, and this intervention [of aVNS] does not impact breastfeeding, as it is not a medication approach,” she said.
The researchers enrolled 25 women (mean age, 33.7 years) diagnosed with postpartum depression. Ten of the women (40%) were on a stable dose of antidepressant medication.
The participants self-administered 6 weeks of open-label aVNS for 15 minutes daily at home. They were then observed without intervention for an additional 2 weeks. The women also completed medical, psychiatric, and safety interviews throughout the study period.
Promising findings
At baseline, the mean HAM-D17 was 18.4 and was similar for those on (17.8) and off (18.9) antidepressants.
By week 6, the mean HAM-D17 total score decreased by 9.7 points overall, compared with baseline score. For participants on antidepressants, the HAM-D17 decreased by 8.7 points; for women off antidepressants, it decreased by 10.3 points.
In addition, 74% of the women achieved a response to the therapy, and 61% achieved remission of their depressive symptoms.
The most common adverse effects were discomfort (n = 5 patients), headache (n = 3), and dizziness (n = 2). All resolved without intervention.
Commenting on the findings, Anita Clayton, MD, professor and chair, department of psychiatry and neurobehavioral sciences, University of Virginia School of Medicine, Charlottesville, said the study was “quite interesting.”
Dr. Clayton, who was not involved with the research, also noted the “pretty high” response and remission rates.
“So, I think this does have promise, and it would be worth doing a study where you look at placebo versus this treatment,” she said.
“Many women are fearful of taking medicines postpartum, even peripartum, unless they have had pre-existing severe depression. This is not a medicine, and it sounds like it could be useful even in people who are pregnant, although it’s harder to do studies in pregnant women,” Dr. Clayton added.
The study was funded by Nesos Corporation. Dr. Deligiannidis received contracted research funds from Nesos Corporation to conduct this study. She also serves as a consultant to Sage Therapeutics, Brii Biosciences, and GH Research. Dr. Clayton reports financial relationships with Dare Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, AbbVie, Brii Biosciences, Fabre-Kramer, Field Trip Health, Mind Cure Health, Ovoca Bio, PureTech Health, S1 Biopharma, Takeda/Lundbeck, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Changes in Sexual Functioning Questionnaire, Guilford Publications, Euthymics Bioscience, and Mediflix.
A version of this article first appeared on Medscape.com.
At-home, noninvasive auricular vagus nerve stimulation (aVNS) therapy is well-tolerated and associated with a significant reduction in postpartum depressive and anxiety symptoms, new research suggests.
In a small proof-of-concept pilot study of 25 women with postpartum depression receiving 6 weeks of daily aVNS treatment, results showed that 74% achieved response and 61% achieved remission, as shown in reduced scores on the Hamilton Rating Scale for Depression (HAM-D17).
Although invasive electrical stimulation of the vagus nerve was approved by the U.S. Food and Drug Administration for treatment-resistant depression in 2005, it involves risk for implantation, infection, and significant side effects, coinvestigator Kristina M. Deligiannidis, MD, director, Women’s Behavioral Health, Zucker Hillside Hospital, Northwell Health, Glen Oaks, New York, told this news organization.
“This newer approach, transcutaneous auricular VNS, is non-invasive, is well tolerated, and has shown initial efficacy in major depression in men and women,” she said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) Annual Meeting.
Potential alternative to meds
“Given that aVNS is a non-invasive treatment which can be administered at home, we wanted to test if this approach was safe, feasible, and could reduce depressive symptoms in women with postpartum depression, as many of these women have barriers to accessing current treatments,” Dr. Deligiannidis said.
Auricular VNS uses surface skin electrodes to stimulate nerve endings of a branch of the vagus nerve, located on the surface of the outer ear. Those nerve endings travel to the brain where they have been shown to modulate brain communication in areas important for mood and anxiety regulation, she said.
Dr. Deligiannidis noted that evidence-based treatments for postpartum depression include psychotherapies and antidepressants. However, some women have difficulty accessing weekly psychotherapy, and, when antidepressants are indicated, many are reluctant to take them if they are breastfeeding because of concerns about the medications getting into their breast milk, she said.
Although most antidepressants are safe in lactation, many women postpone antidepressant treatment until they have finished breastfeeding, which can postpone their postpartum depression treatment, Dr. Deligiannidis added.
“At home treatments reduce many barriers women have to current treatments, and this intervention [of aVNS] does not impact breastfeeding, as it is not a medication approach,” she said.
The researchers enrolled 25 women (mean age, 33.7 years) diagnosed with postpartum depression. Ten of the women (40%) were on a stable dose of antidepressant medication.
The participants self-administered 6 weeks of open-label aVNS for 15 minutes daily at home. They were then observed without intervention for an additional 2 weeks. The women also completed medical, psychiatric, and safety interviews throughout the study period.
Promising findings
At baseline, the mean HAM-D17 was 18.4 and was similar for those on (17.8) and off (18.9) antidepressants.
By week 6, the mean HAM-D17 total score decreased by 9.7 points overall, compared with baseline score. For participants on antidepressants, the HAM-D17 decreased by 8.7 points; for women off antidepressants, it decreased by 10.3 points.
In addition, 74% of the women achieved a response to the therapy, and 61% achieved remission of their depressive symptoms.
The most common adverse effects were discomfort (n = 5 patients), headache (n = 3), and dizziness (n = 2). All resolved without intervention.
Commenting on the findings, Anita Clayton, MD, professor and chair, department of psychiatry and neurobehavioral sciences, University of Virginia School of Medicine, Charlottesville, said the study was “quite interesting.”
Dr. Clayton, who was not involved with the research, also noted the “pretty high” response and remission rates.
“So, I think this does have promise, and it would be worth doing a study where you look at placebo versus this treatment,” she said.
“Many women are fearful of taking medicines postpartum, even peripartum, unless they have had pre-existing severe depression. This is not a medicine, and it sounds like it could be useful even in people who are pregnant, although it’s harder to do studies in pregnant women,” Dr. Clayton added.
The study was funded by Nesos Corporation. Dr. Deligiannidis received contracted research funds from Nesos Corporation to conduct this study. She also serves as a consultant to Sage Therapeutics, Brii Biosciences, and GH Research. Dr. Clayton reports financial relationships with Dare Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, AbbVie, Brii Biosciences, Fabre-Kramer, Field Trip Health, Mind Cure Health, Ovoca Bio, PureTech Health, S1 Biopharma, Takeda/Lundbeck, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Changes in Sexual Functioning Questionnaire, Guilford Publications, Euthymics Bioscience, and Mediflix.
A version of this article first appeared on Medscape.com.
Five-year cervical screening interval safe for HPV-negative women
A 5-year cervical screening interval is as safe and effective for women who test negative for human papillomavirus (HPV) as are 3-year intervals, according to a new ‘real life’ study led by King’s College London (KCL) with researchers from the University of Manchester, and the NHS, on behalf of the HPV pilot steering group.
The study, published in The BMJ, used data from the HPV screening pilot to assess rates of detection of high-grade cervical intraepithelial neoplasia (CIN3+) and of cervical cancer following a negative HPV test. It confirmed that 5-yearly screening prevents as many cancers as screening at 3-year intervals, even in women who are not vaccinated against HPV.
Change to primary HPV testing since 2019
Before 2019, the NHS cervical screening program conducted cytology testing first, testing for HPV only if abnormalities were found. In 2019, following reporting of early results of the HPV pilot by the same researchers, the program in England switched to testing for HPV first, on the grounds that since having HPV infection comes before having abnormal cells, HPV testing would detect more women at risk of cervical cancer.
Following the switch to primary HPV testing, the same screening intervals were retained, meaning 3-yearly screening for those aged 24-49 years and testing every 5 years for women aged 50-64 years, or 3 years if they tested positive. However, the National Screening Committee had recommended that invites should be changed from 3 to 5 years for those in the under-50 age group found not to have high-risk HPV at their routine screening test.
For the latest study, funded by Cancer Research UK, the steering group researchers analyzed details for more than 1.3 million women who had attended screening for two rounds of the HPV screening pilot, the first from 2013 to 2016, with a follow-up to the end of 2019. By this time, the data set had doubled in size from the pilot study, and results had been linked with the national cancer registry.
They confirmed that HPV testing was more accurate than a cytology test, irrespective of whether the HPV test assay was DNA- or mRNA-based. With HPV testing, the risk of subsequent cytological changes more than halved overall. Eligible women under 50 who had a negative HPV screen in the first round had a much lower risk of detection of CIN3+ in the second round, with a rate of 1.21 in 1,000, compared with 4.52 in 1,000 after a negative cytology test.
Data support extension of the testing interval
“The study confirms that women in this age group are much less likely to develop clinically relevant cervical lesions and cervical cancer, 3 years after a negative HPV screen, compared with a negative smear test,” the researchers said.
They suggested that most women do not need to be screened as frequently as the current program allows, and that the data support an extension of the screening intervals, regardless of the test assay used, to 5 years after a negative HPV test in women aged 25-49 years, and even longer for women aged 50 years and older.
However, the screening interval for HPV-positive women who have negative HPV tests at early recall should be kept at 3 years, they said.
“These results are very reassuring,” said lead author Matejka Rebolj, PhD, senior epidemiologist at KCL. “They build on previous research that shows that following the introduction of HPV testing for cervical screening, a 5-year interval is at least as safe as the previous 3-year interval. Changing to 5-yearly screening will mean we can prevent just as many cancers as before, while allowing for fewer screens.”
Michelle Mitchell, Cancer Research UK’s chief executive, said: “This large study shows that offering cervical screening using HPV testing effectively prevents cervical cancer, without having to be screened as often. This builds on findings from years of research showing HPV testing is more accurate at predicting who is at risk of developing cervical cancer compared to the previous way of testing. As changes to the screening [programs] are made, they will be monitored to help ensure that cervical screening is as effective as possible for all who take part.”
If HPV is present, testing interval should remain every 3 years
Responding to the study, Theresa Freeman-Wang, MBChB, consultant gynecologist, president of the British Society for Colposcopy and Cervical Pathology, and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “England, Scotland, and Wales and many other countries now use HPV primary screening, which is much better at assessing risk than previous methods. HPV testing is more sensitive and accurate, so changes are picked up earlier.
“Studies have confirmed that if someone is HPV negative (i.e., HPV is not present in the screen test), intervals between tests can very safely be increased from 3 to 5 years.
“If HPV is present, then the program will automatically look for any abnormal cells. If there are no abnormalities, the woman will be advised to have a repeat screen test in a year. If the HPV remains present over 3 successive years or if abnormal cells are detected at any stage, she will be referred for a more detailed screening examination called a colposcopy.
“It’s important that with any change like this, there is clear information available to explain what these changes mean.
“We have an effective cervical screening program in the UK that has significantly reduced the number of cases and deaths from this preventable cancer.
“HPV screening every 5 years is safe and to be fully effective it is vital that women take up the invitation for cervical screening when called.”
A version of this article first appeared on Medscape UK.
A 5-year cervical screening interval is as safe and effective for women who test negative for human papillomavirus (HPV) as are 3-year intervals, according to a new ‘real life’ study led by King’s College London (KCL) with researchers from the University of Manchester, and the NHS, on behalf of the HPV pilot steering group.
The study, published in The BMJ, used data from the HPV screening pilot to assess rates of detection of high-grade cervical intraepithelial neoplasia (CIN3+) and of cervical cancer following a negative HPV test. It confirmed that 5-yearly screening prevents as many cancers as screening at 3-year intervals, even in women who are not vaccinated against HPV.
Change to primary HPV testing since 2019
Before 2019, the NHS cervical screening program conducted cytology testing first, testing for HPV only if abnormalities were found. In 2019, following reporting of early results of the HPV pilot by the same researchers, the program in England switched to testing for HPV first, on the grounds that since having HPV infection comes before having abnormal cells, HPV testing would detect more women at risk of cervical cancer.
Following the switch to primary HPV testing, the same screening intervals were retained, meaning 3-yearly screening for those aged 24-49 years and testing every 5 years for women aged 50-64 years, or 3 years if they tested positive. However, the National Screening Committee had recommended that invites should be changed from 3 to 5 years for those in the under-50 age group found not to have high-risk HPV at their routine screening test.
For the latest study, funded by Cancer Research UK, the steering group researchers analyzed details for more than 1.3 million women who had attended screening for two rounds of the HPV screening pilot, the first from 2013 to 2016, with a follow-up to the end of 2019. By this time, the data set had doubled in size from the pilot study, and results had been linked with the national cancer registry.
They confirmed that HPV testing was more accurate than a cytology test, irrespective of whether the HPV test assay was DNA- or mRNA-based. With HPV testing, the risk of subsequent cytological changes more than halved overall. Eligible women under 50 who had a negative HPV screen in the first round had a much lower risk of detection of CIN3+ in the second round, with a rate of 1.21 in 1,000, compared with 4.52 in 1,000 after a negative cytology test.
Data support extension of the testing interval
“The study confirms that women in this age group are much less likely to develop clinically relevant cervical lesions and cervical cancer, 3 years after a negative HPV screen, compared with a negative smear test,” the researchers said.
They suggested that most women do not need to be screened as frequently as the current program allows, and that the data support an extension of the screening intervals, regardless of the test assay used, to 5 years after a negative HPV test in women aged 25-49 years, and even longer for women aged 50 years and older.
However, the screening interval for HPV-positive women who have negative HPV tests at early recall should be kept at 3 years, they said.
“These results are very reassuring,” said lead author Matejka Rebolj, PhD, senior epidemiologist at KCL. “They build on previous research that shows that following the introduction of HPV testing for cervical screening, a 5-year interval is at least as safe as the previous 3-year interval. Changing to 5-yearly screening will mean we can prevent just as many cancers as before, while allowing for fewer screens.”
Michelle Mitchell, Cancer Research UK’s chief executive, said: “This large study shows that offering cervical screening using HPV testing effectively prevents cervical cancer, without having to be screened as often. This builds on findings from years of research showing HPV testing is more accurate at predicting who is at risk of developing cervical cancer compared to the previous way of testing. As changes to the screening [programs] are made, they will be monitored to help ensure that cervical screening is as effective as possible for all who take part.”
If HPV is present, testing interval should remain every 3 years
Responding to the study, Theresa Freeman-Wang, MBChB, consultant gynecologist, president of the British Society for Colposcopy and Cervical Pathology, and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “England, Scotland, and Wales and many other countries now use HPV primary screening, which is much better at assessing risk than previous methods. HPV testing is more sensitive and accurate, so changes are picked up earlier.
“Studies have confirmed that if someone is HPV negative (i.e., HPV is not present in the screen test), intervals between tests can very safely be increased from 3 to 5 years.
“If HPV is present, then the program will automatically look for any abnormal cells. If there are no abnormalities, the woman will be advised to have a repeat screen test in a year. If the HPV remains present over 3 successive years or if abnormal cells are detected at any stage, she will be referred for a more detailed screening examination called a colposcopy.
“It’s important that with any change like this, there is clear information available to explain what these changes mean.
“We have an effective cervical screening program in the UK that has significantly reduced the number of cases and deaths from this preventable cancer.
“HPV screening every 5 years is safe and to be fully effective it is vital that women take up the invitation for cervical screening when called.”
A version of this article first appeared on Medscape UK.
A 5-year cervical screening interval is as safe and effective for women who test negative for human papillomavirus (HPV) as are 3-year intervals, according to a new ‘real life’ study led by King’s College London (KCL) with researchers from the University of Manchester, and the NHS, on behalf of the HPV pilot steering group.
The study, published in The BMJ, used data from the HPV screening pilot to assess rates of detection of high-grade cervical intraepithelial neoplasia (CIN3+) and of cervical cancer following a negative HPV test. It confirmed that 5-yearly screening prevents as many cancers as screening at 3-year intervals, even in women who are not vaccinated against HPV.
Change to primary HPV testing since 2019
Before 2019, the NHS cervical screening program conducted cytology testing first, testing for HPV only if abnormalities were found. In 2019, following reporting of early results of the HPV pilot by the same researchers, the program in England switched to testing for HPV first, on the grounds that since having HPV infection comes before having abnormal cells, HPV testing would detect more women at risk of cervical cancer.
Following the switch to primary HPV testing, the same screening intervals were retained, meaning 3-yearly screening for those aged 24-49 years and testing every 5 years for women aged 50-64 years, or 3 years if they tested positive. However, the National Screening Committee had recommended that invites should be changed from 3 to 5 years for those in the under-50 age group found not to have high-risk HPV at their routine screening test.
For the latest study, funded by Cancer Research UK, the steering group researchers analyzed details for more than 1.3 million women who had attended screening for two rounds of the HPV screening pilot, the first from 2013 to 2016, with a follow-up to the end of 2019. By this time, the data set had doubled in size from the pilot study, and results had been linked with the national cancer registry.
They confirmed that HPV testing was more accurate than a cytology test, irrespective of whether the HPV test assay was DNA- or mRNA-based. With HPV testing, the risk of subsequent cytological changes more than halved overall. Eligible women under 50 who had a negative HPV screen in the first round had a much lower risk of detection of CIN3+ in the second round, with a rate of 1.21 in 1,000, compared with 4.52 in 1,000 after a negative cytology test.
Data support extension of the testing interval
“The study confirms that women in this age group are much less likely to develop clinically relevant cervical lesions and cervical cancer, 3 years after a negative HPV screen, compared with a negative smear test,” the researchers said.
They suggested that most women do not need to be screened as frequently as the current program allows, and that the data support an extension of the screening intervals, regardless of the test assay used, to 5 years after a negative HPV test in women aged 25-49 years, and even longer for women aged 50 years and older.
However, the screening interval for HPV-positive women who have negative HPV tests at early recall should be kept at 3 years, they said.
“These results are very reassuring,” said lead author Matejka Rebolj, PhD, senior epidemiologist at KCL. “They build on previous research that shows that following the introduction of HPV testing for cervical screening, a 5-year interval is at least as safe as the previous 3-year interval. Changing to 5-yearly screening will mean we can prevent just as many cancers as before, while allowing for fewer screens.”
Michelle Mitchell, Cancer Research UK’s chief executive, said: “This large study shows that offering cervical screening using HPV testing effectively prevents cervical cancer, without having to be screened as often. This builds on findings from years of research showing HPV testing is more accurate at predicting who is at risk of developing cervical cancer compared to the previous way of testing. As changes to the screening [programs] are made, they will be monitored to help ensure that cervical screening is as effective as possible for all who take part.”
If HPV is present, testing interval should remain every 3 years
Responding to the study, Theresa Freeman-Wang, MBChB, consultant gynecologist, president of the British Society for Colposcopy and Cervical Pathology, and spokesperson for the Royal College of Obstetricians and Gynaecologists, told this news organization: “England, Scotland, and Wales and many other countries now use HPV primary screening, which is much better at assessing risk than previous methods. HPV testing is more sensitive and accurate, so changes are picked up earlier.
“Studies have confirmed that if someone is HPV negative (i.e., HPV is not present in the screen test), intervals between tests can very safely be increased from 3 to 5 years.
“If HPV is present, then the program will automatically look for any abnormal cells. If there are no abnormalities, the woman will be advised to have a repeat screen test in a year. If the HPV remains present over 3 successive years or if abnormal cells are detected at any stage, she will be referred for a more detailed screening examination called a colposcopy.
“It’s important that with any change like this, there is clear information available to explain what these changes mean.
“We have an effective cervical screening program in the UK that has significantly reduced the number of cases and deaths from this preventable cancer.
“HPV screening every 5 years is safe and to be fully effective it is vital that women take up the invitation for cervical screening when called.”
A version of this article first appeared on Medscape UK.
FROM THE BMJ
Tin in permanent contraception implants causes toxicity
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Mother’s distress disrupts fetal brain development
Babies of mothers who experience significant psychological distress during pregnancy showed evidence of altered brain development in utero and reduced cognitive outcomes at 18 months, based on data from a pair of studies including approximately 300 women.
In a longitudinal study published in JAMA Network Open, Yao Wu, PhD, of Children’s National Hospital, Washington, and colleagues recruited 97 healthy mother-infant dyads between January 2016 and October 2020 at a single center. Of these, 87 underwent two fetal brain imaging studies each, and 10 completed the first MRI visit, for a total of 184 fetal MRIs.
Neurodevelopment and social-emotional development for infants at 18 months of age was measured using the Bayley Scales of Infant and Toddler Development and Infant-Toddler Social and Emotional Assessment. The mean age of the mothers was 35 years; maternal distress was assessed between 24 and 40 weeks’ gestation using validated self-report questionnaires. Parenting stress was assessed at the 18-month infant testing using the Parenting Stress Index-Short Form.
Overall, prenatal maternal stress was negatively associated with infant cognitive performance (P = .01) at 18 months, mediated by fetal left hippocampal volume.
In addition, increased fetal cortical local gyrification index and sulcal depth measured during reported times of prenatal maternal distress were associated with significantly poorer social-emotional scores and competence scores at age 18 months. The beta coefficients for local gyrification index and sulcal depth were –54.62 and –14.22, respectively, for social-emotional and competence scores, –24.01 and –7.53, respectively; P values were P < .001, P < .002, P = .003, P < .001, respectively.
“Increased cortical gyrification has been suggested in children with dyslexia and autism, and sulcal depth has been associated with the severity of impaired performance on working memory and executive function in adults with schizophrenia,” the researchers wrote in their discussion of the findings.
The current study “extends our previous findings and suggests a critical role for disturbances in emerging fetal cerebral cortical folding development in mediating the association between prenatal maternal distress and neurodevelopmental problems that later manifest in infancy,” they explained.
The researchers also found that prenatal maternal anxiety, stress, and depression were positively associated with all measures of parenting stress at the 18-month testing visit.
The study findings were limited by several factors including the use of self-reports for both maternal distress and infant social-emotional assessment, despite the use of validated questionnaires, and the fact that assessment of maternal distress at specific times may not reflect the entire pregnancy, the researchers noted. Other potential limitations included the inability to use some MRI data because of fetal movement and the homogenous population of relatively highly educated women with access to health care that may not reflect other areas, they said.
“Identifying early brain developmental biomarkers may help improve the identification of infants at risk for later neurodevelopmental impairment who might benefit from early targeted interventions,” the researchers concluded.
Technology enhances health and disease models
The effect of the prenatal period on future well-being is recognized, but the current study makes “substantial contributions to prenatal programming science, with implications for ways to transform the prenatal care ecosystem for two-generation impact,” Catherine Monk, PhD, and Cristina R. Fernández, MD, both of Columbia University, New York, wrote in an accompanying editorial.
The developmental origins of health and disease (DOHaD) conceptual model introduced by Dr. David Barker in 1995 were later applied to show that maternal stress, depression, and anxiety affected child prenatal and future development, they said. However, the current study uses cutting-edge neuroscience to directly assess developing fetal brains. The finding of reduced cognitive functioning at 18 months associated with maternal stress is consistent with other findings, they noted.
“Finding an association between maternal prenatal stress and infant cognitive outcomes in the setting of what may be modest stress relative to that of a low-resourced or historically marginalized sample underscores the importance of this research; presumably, with higher stress, and greater social determinants of health burden, the effect sizes would be even greater and of greater concern,” they said.
However, studies such as the current one “have the potential to transform the prenatal and postpartum care ecosystems,” by encouraging a whole-person approach to the care of pregnant women, including attention to mental well-being and quality of life, they emphasized.
COVID-19 stress considerations
In a separate study published in Communications Medicine, Yuan-Chiao Lu, MD, also of Children’s National Hospital in Washington, and colleagues found a similar effect of maternal stress on fetal brain development.
The researchers imaged the brains of fetuses before and during the COVID-19 pandemic and interviewed mothers about any distress they experienced during pregnancy.
The study population included 65 women with known COVID-19 exposures who underwent 92 fetal MRIs and 137 prepandemic controls who underwent 182 fetal MRIs. Maternal distress was measured via the Spielberger State Anxiety Inventory, Spielberger Trait Anxiety Inventory, Perceived Stress Scale, and Edinburgh Postnatal Depression Scale.
Overall, scores on measures of stress and depression were significantly higher for women in the pandemic group compared with controls. Of the 173 women for whom maternal distress measures were available, 28% of the prepandemic group and 52% of the pandemic group met criteria for elevated maternal psychological distress, defined as above the threshold for distress on any one of the four measures.
After the researchers controlled for maternal distress, MRI data showed decreases in fetal white matter and in hippocampal and cerebellar volumes in fetuses in the pandemic group compared with controls.
Other signs of impaired brain development were similar to those seen in the JAMA Network Open study, including decreased cortical surface area and local gyrification index, as well as reduced sulcal depth in multiple brain lobes, indicating delayed cerebral cortical gyrification.
The second study was limited by a lack of data on other lifestyle changes during the pandemic that might influence maternal health and fetal development, the researchers noted. Other limitations were the possible lack of generalizability to a range of racial and ethnic populations and geographic areas outside of Washington, and the inability to control for unknown COVID-19 exposures or subclinical infections in controls, they said.
However, the results support findings from previous studies, and provide a unique opportunity to study the effect of prenatal stress on early development, as well as a chance to implement “novel and timely interventions,” the researchers wrote.
“Monitoring the COVID generation of infants for long-term cognitive and health outcomes after birth is warranted and currently underway,” and continued research may inform preventive strategies for pregnant women experiencing multiple stressors beyond the pandemic, they concluded.
Interpret pandemic effect with caution
“Research studies, as well as our own daily experiences, have made it abundantly clear that stress is on the rise as a consequence of the COVID-19 pandemic,” said editorial author Dr. Monk, who commented on the second study in an interview. “This is an important public health question: Early identification of pandemic effects on child development can help garner the necessary resources to intervene early, dramatically increasing the likelihood of improving that child’s developmental trajectory,” she said.
“The pandemic is an unprecedented experience that has widespread impact on people’s lives, how could it not also alter gestational biology and the developing brain? That being said, we need to be cautious in that we do not yet know the functional implications of these brain changes for longer-term development,” Dr. Monk said. “Also, we do not know what aspects of women’s pandemic-affected lives had an influence on fetal brain development. The authors found higher stress in pandemic versus nonpandemic women, but not evidence that distress was the mediating variable relating pregnancy during the pandemic to altered brain development,” she explained.
The take-home message for clinicians is to “provide your patients with realistic avenues for neurodevelopmental assessments of their children if they, or you, have concerns,” Dr. Monk said. “However, do not prejudge ‘pandemic babies,’ as not all children will be affected by these potential pandemic effects,” she emphasized. “It is possible to misjudge normal variation in children’s development and unnecessarily raise parents’ anxiety levels. Importantly, this period of brain plasticity means any needed intervention likely can have a big, ameliorating impact,” she added.
“We need follow-up studies looking at pandemic effects on prenatal and postnatal development and what factors protect the fetus and birthing person from the negative influences,” she said.
The JAMA study was supported by the National Institutes of Health and the A. James & Alice B. Clark Foundation. The study in Communications Medicine was supported by the National Institutes of Health, the Intellectual and Developmental Disabilities Research Center, and the A. James & Alice B. Clark Foundation. None of the researchers in either study disclosed conflicts of interest. Dr. Monk disclosed grants from the National Institutes of Health, the Bezos Family Foundation, and the Robin Hood Foundation outside the submitted work.
Babies of mothers who experience significant psychological distress during pregnancy showed evidence of altered brain development in utero and reduced cognitive outcomes at 18 months, based on data from a pair of studies including approximately 300 women.
In a longitudinal study published in JAMA Network Open, Yao Wu, PhD, of Children’s National Hospital, Washington, and colleagues recruited 97 healthy mother-infant dyads between January 2016 and October 2020 at a single center. Of these, 87 underwent two fetal brain imaging studies each, and 10 completed the first MRI visit, for a total of 184 fetal MRIs.
Neurodevelopment and social-emotional development for infants at 18 months of age was measured using the Bayley Scales of Infant and Toddler Development and Infant-Toddler Social and Emotional Assessment. The mean age of the mothers was 35 years; maternal distress was assessed between 24 and 40 weeks’ gestation using validated self-report questionnaires. Parenting stress was assessed at the 18-month infant testing using the Parenting Stress Index-Short Form.
Overall, prenatal maternal stress was negatively associated with infant cognitive performance (P = .01) at 18 months, mediated by fetal left hippocampal volume.
In addition, increased fetal cortical local gyrification index and sulcal depth measured during reported times of prenatal maternal distress were associated with significantly poorer social-emotional scores and competence scores at age 18 months. The beta coefficients for local gyrification index and sulcal depth were –54.62 and –14.22, respectively, for social-emotional and competence scores, –24.01 and –7.53, respectively; P values were P < .001, P < .002, P = .003, P < .001, respectively.
“Increased cortical gyrification has been suggested in children with dyslexia and autism, and sulcal depth has been associated with the severity of impaired performance on working memory and executive function in adults with schizophrenia,” the researchers wrote in their discussion of the findings.
The current study “extends our previous findings and suggests a critical role for disturbances in emerging fetal cerebral cortical folding development in mediating the association between prenatal maternal distress and neurodevelopmental problems that later manifest in infancy,” they explained.
The researchers also found that prenatal maternal anxiety, stress, and depression were positively associated with all measures of parenting stress at the 18-month testing visit.
The study findings were limited by several factors including the use of self-reports for both maternal distress and infant social-emotional assessment, despite the use of validated questionnaires, and the fact that assessment of maternal distress at specific times may not reflect the entire pregnancy, the researchers noted. Other potential limitations included the inability to use some MRI data because of fetal movement and the homogenous population of relatively highly educated women with access to health care that may not reflect other areas, they said.
“Identifying early brain developmental biomarkers may help improve the identification of infants at risk for later neurodevelopmental impairment who might benefit from early targeted interventions,” the researchers concluded.
Technology enhances health and disease models
The effect of the prenatal period on future well-being is recognized, but the current study makes “substantial contributions to prenatal programming science, with implications for ways to transform the prenatal care ecosystem for two-generation impact,” Catherine Monk, PhD, and Cristina R. Fernández, MD, both of Columbia University, New York, wrote in an accompanying editorial.
The developmental origins of health and disease (DOHaD) conceptual model introduced by Dr. David Barker in 1995 were later applied to show that maternal stress, depression, and anxiety affected child prenatal and future development, they said. However, the current study uses cutting-edge neuroscience to directly assess developing fetal brains. The finding of reduced cognitive functioning at 18 months associated with maternal stress is consistent with other findings, they noted.
“Finding an association between maternal prenatal stress and infant cognitive outcomes in the setting of what may be modest stress relative to that of a low-resourced or historically marginalized sample underscores the importance of this research; presumably, with higher stress, and greater social determinants of health burden, the effect sizes would be even greater and of greater concern,” they said.
However, studies such as the current one “have the potential to transform the prenatal and postpartum care ecosystems,” by encouraging a whole-person approach to the care of pregnant women, including attention to mental well-being and quality of life, they emphasized.
COVID-19 stress considerations
In a separate study published in Communications Medicine, Yuan-Chiao Lu, MD, also of Children’s National Hospital in Washington, and colleagues found a similar effect of maternal stress on fetal brain development.
The researchers imaged the brains of fetuses before and during the COVID-19 pandemic and interviewed mothers about any distress they experienced during pregnancy.
The study population included 65 women with known COVID-19 exposures who underwent 92 fetal MRIs and 137 prepandemic controls who underwent 182 fetal MRIs. Maternal distress was measured via the Spielberger State Anxiety Inventory, Spielberger Trait Anxiety Inventory, Perceived Stress Scale, and Edinburgh Postnatal Depression Scale.
Overall, scores on measures of stress and depression were significantly higher for women in the pandemic group compared with controls. Of the 173 women for whom maternal distress measures were available, 28% of the prepandemic group and 52% of the pandemic group met criteria for elevated maternal psychological distress, defined as above the threshold for distress on any one of the four measures.
After the researchers controlled for maternal distress, MRI data showed decreases in fetal white matter and in hippocampal and cerebellar volumes in fetuses in the pandemic group compared with controls.
Other signs of impaired brain development were similar to those seen in the JAMA Network Open study, including decreased cortical surface area and local gyrification index, as well as reduced sulcal depth in multiple brain lobes, indicating delayed cerebral cortical gyrification.
The second study was limited by a lack of data on other lifestyle changes during the pandemic that might influence maternal health and fetal development, the researchers noted. Other limitations were the possible lack of generalizability to a range of racial and ethnic populations and geographic areas outside of Washington, and the inability to control for unknown COVID-19 exposures or subclinical infections in controls, they said.
However, the results support findings from previous studies, and provide a unique opportunity to study the effect of prenatal stress on early development, as well as a chance to implement “novel and timely interventions,” the researchers wrote.
“Monitoring the COVID generation of infants for long-term cognitive and health outcomes after birth is warranted and currently underway,” and continued research may inform preventive strategies for pregnant women experiencing multiple stressors beyond the pandemic, they concluded.
Interpret pandemic effect with caution
“Research studies, as well as our own daily experiences, have made it abundantly clear that stress is on the rise as a consequence of the COVID-19 pandemic,” said editorial author Dr. Monk, who commented on the second study in an interview. “This is an important public health question: Early identification of pandemic effects on child development can help garner the necessary resources to intervene early, dramatically increasing the likelihood of improving that child’s developmental trajectory,” she said.
“The pandemic is an unprecedented experience that has widespread impact on people’s lives, how could it not also alter gestational biology and the developing brain? That being said, we need to be cautious in that we do not yet know the functional implications of these brain changes for longer-term development,” Dr. Monk said. “Also, we do not know what aspects of women’s pandemic-affected lives had an influence on fetal brain development. The authors found higher stress in pandemic versus nonpandemic women, but not evidence that distress was the mediating variable relating pregnancy during the pandemic to altered brain development,” she explained.
The take-home message for clinicians is to “provide your patients with realistic avenues for neurodevelopmental assessments of their children if they, or you, have concerns,” Dr. Monk said. “However, do not prejudge ‘pandemic babies,’ as not all children will be affected by these potential pandemic effects,” she emphasized. “It is possible to misjudge normal variation in children’s development and unnecessarily raise parents’ anxiety levels. Importantly, this period of brain plasticity means any needed intervention likely can have a big, ameliorating impact,” she added.
“We need follow-up studies looking at pandemic effects on prenatal and postnatal development and what factors protect the fetus and birthing person from the negative influences,” she said.
The JAMA study was supported by the National Institutes of Health and the A. James & Alice B. Clark Foundation. The study in Communications Medicine was supported by the National Institutes of Health, the Intellectual and Developmental Disabilities Research Center, and the A. James & Alice B. Clark Foundation. None of the researchers in either study disclosed conflicts of interest. Dr. Monk disclosed grants from the National Institutes of Health, the Bezos Family Foundation, and the Robin Hood Foundation outside the submitted work.
Babies of mothers who experience significant psychological distress during pregnancy showed evidence of altered brain development in utero and reduced cognitive outcomes at 18 months, based on data from a pair of studies including approximately 300 women.
In a longitudinal study published in JAMA Network Open, Yao Wu, PhD, of Children’s National Hospital, Washington, and colleagues recruited 97 healthy mother-infant dyads between January 2016 and October 2020 at a single center. Of these, 87 underwent two fetal brain imaging studies each, and 10 completed the first MRI visit, for a total of 184 fetal MRIs.
Neurodevelopment and social-emotional development for infants at 18 months of age was measured using the Bayley Scales of Infant and Toddler Development and Infant-Toddler Social and Emotional Assessment. The mean age of the mothers was 35 years; maternal distress was assessed between 24 and 40 weeks’ gestation using validated self-report questionnaires. Parenting stress was assessed at the 18-month infant testing using the Parenting Stress Index-Short Form.
Overall, prenatal maternal stress was negatively associated with infant cognitive performance (P = .01) at 18 months, mediated by fetal left hippocampal volume.
In addition, increased fetal cortical local gyrification index and sulcal depth measured during reported times of prenatal maternal distress were associated with significantly poorer social-emotional scores and competence scores at age 18 months. The beta coefficients for local gyrification index and sulcal depth were –54.62 and –14.22, respectively, for social-emotional and competence scores, –24.01 and –7.53, respectively; P values were P < .001, P < .002, P = .003, P < .001, respectively.
“Increased cortical gyrification has been suggested in children with dyslexia and autism, and sulcal depth has been associated with the severity of impaired performance on working memory and executive function in adults with schizophrenia,” the researchers wrote in their discussion of the findings.
The current study “extends our previous findings and suggests a critical role for disturbances in emerging fetal cerebral cortical folding development in mediating the association between prenatal maternal distress and neurodevelopmental problems that later manifest in infancy,” they explained.
The researchers also found that prenatal maternal anxiety, stress, and depression were positively associated with all measures of parenting stress at the 18-month testing visit.
The study findings were limited by several factors including the use of self-reports for both maternal distress and infant social-emotional assessment, despite the use of validated questionnaires, and the fact that assessment of maternal distress at specific times may not reflect the entire pregnancy, the researchers noted. Other potential limitations included the inability to use some MRI data because of fetal movement and the homogenous population of relatively highly educated women with access to health care that may not reflect other areas, they said.
“Identifying early brain developmental biomarkers may help improve the identification of infants at risk for later neurodevelopmental impairment who might benefit from early targeted interventions,” the researchers concluded.
Technology enhances health and disease models
The effect of the prenatal period on future well-being is recognized, but the current study makes “substantial contributions to prenatal programming science, with implications for ways to transform the prenatal care ecosystem for two-generation impact,” Catherine Monk, PhD, and Cristina R. Fernández, MD, both of Columbia University, New York, wrote in an accompanying editorial.
The developmental origins of health and disease (DOHaD) conceptual model introduced by Dr. David Barker in 1995 were later applied to show that maternal stress, depression, and anxiety affected child prenatal and future development, they said. However, the current study uses cutting-edge neuroscience to directly assess developing fetal brains. The finding of reduced cognitive functioning at 18 months associated with maternal stress is consistent with other findings, they noted.
“Finding an association between maternal prenatal stress and infant cognitive outcomes in the setting of what may be modest stress relative to that of a low-resourced or historically marginalized sample underscores the importance of this research; presumably, with higher stress, and greater social determinants of health burden, the effect sizes would be even greater and of greater concern,” they said.
However, studies such as the current one “have the potential to transform the prenatal and postpartum care ecosystems,” by encouraging a whole-person approach to the care of pregnant women, including attention to mental well-being and quality of life, they emphasized.
COVID-19 stress considerations
In a separate study published in Communications Medicine, Yuan-Chiao Lu, MD, also of Children’s National Hospital in Washington, and colleagues found a similar effect of maternal stress on fetal brain development.
The researchers imaged the brains of fetuses before and during the COVID-19 pandemic and interviewed mothers about any distress they experienced during pregnancy.
The study population included 65 women with known COVID-19 exposures who underwent 92 fetal MRIs and 137 prepandemic controls who underwent 182 fetal MRIs. Maternal distress was measured via the Spielberger State Anxiety Inventory, Spielberger Trait Anxiety Inventory, Perceived Stress Scale, and Edinburgh Postnatal Depression Scale.
Overall, scores on measures of stress and depression were significantly higher for women in the pandemic group compared with controls. Of the 173 women for whom maternal distress measures were available, 28% of the prepandemic group and 52% of the pandemic group met criteria for elevated maternal psychological distress, defined as above the threshold for distress on any one of the four measures.
After the researchers controlled for maternal distress, MRI data showed decreases in fetal white matter and in hippocampal and cerebellar volumes in fetuses in the pandemic group compared with controls.
Other signs of impaired brain development were similar to those seen in the JAMA Network Open study, including decreased cortical surface area and local gyrification index, as well as reduced sulcal depth in multiple brain lobes, indicating delayed cerebral cortical gyrification.
The second study was limited by a lack of data on other lifestyle changes during the pandemic that might influence maternal health and fetal development, the researchers noted. Other limitations were the possible lack of generalizability to a range of racial and ethnic populations and geographic areas outside of Washington, and the inability to control for unknown COVID-19 exposures or subclinical infections in controls, they said.
However, the results support findings from previous studies, and provide a unique opportunity to study the effect of prenatal stress on early development, as well as a chance to implement “novel and timely interventions,” the researchers wrote.
“Monitoring the COVID generation of infants for long-term cognitive and health outcomes after birth is warranted and currently underway,” and continued research may inform preventive strategies for pregnant women experiencing multiple stressors beyond the pandemic, they concluded.
Interpret pandemic effect with caution
“Research studies, as well as our own daily experiences, have made it abundantly clear that stress is on the rise as a consequence of the COVID-19 pandemic,” said editorial author Dr. Monk, who commented on the second study in an interview. “This is an important public health question: Early identification of pandemic effects on child development can help garner the necessary resources to intervene early, dramatically increasing the likelihood of improving that child’s developmental trajectory,” she said.
“The pandemic is an unprecedented experience that has widespread impact on people’s lives, how could it not also alter gestational biology and the developing brain? That being said, we need to be cautious in that we do not yet know the functional implications of these brain changes for longer-term development,” Dr. Monk said. “Also, we do not know what aspects of women’s pandemic-affected lives had an influence on fetal brain development. The authors found higher stress in pandemic versus nonpandemic women, but not evidence that distress was the mediating variable relating pregnancy during the pandemic to altered brain development,” she explained.
The take-home message for clinicians is to “provide your patients with realistic avenues for neurodevelopmental assessments of their children if they, or you, have concerns,” Dr. Monk said. “However, do not prejudge ‘pandemic babies,’ as not all children will be affected by these potential pandemic effects,” she emphasized. “It is possible to misjudge normal variation in children’s development and unnecessarily raise parents’ anxiety levels. Importantly, this period of brain plasticity means any needed intervention likely can have a big, ameliorating impact,” she added.
“We need follow-up studies looking at pandemic effects on prenatal and postnatal development and what factors protect the fetus and birthing person from the negative influences,” she said.
The JAMA study was supported by the National Institutes of Health and the A. James & Alice B. Clark Foundation. The study in Communications Medicine was supported by the National Institutes of Health, the Intellectual and Developmental Disabilities Research Center, and the A. James & Alice B. Clark Foundation. None of the researchers in either study disclosed conflicts of interest. Dr. Monk disclosed grants from the National Institutes of Health, the Bezos Family Foundation, and the Robin Hood Foundation outside the submitted work.
FROM JAMA NETWORK OPEN AND COMMUNICATIONS MEDICINE
Abortion debate may affect Rx decisions for pregnant women
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Duration of breastfeeding associated with cognition in children
Breastfeeding duration is associated with improved cognitive scores at ages 5-14, even after controlling for maternal socioeconomic position and cognitive ability, said the researchers behind a new study.
Despite previous studies demonstrating an association between breastfeeding and standardized intelligence test scores – with breastfed infants scoring higher on intelligence tests than non-breastfed infants – a causal relationship is still contested.
“There is some debate about whether breastfeeding a baby for a longer period of time improves their cognitive development,” the authors of the new study said. They went on to explain how improved cognitive outcomes in breastfed infants could potentially be explained by other characteristics of the women, such as “socioeconomics and maternal intelligence.”
Important at the population level
For the study, published in the open-access journal PLOS ONE, researchers from the University of Oxford (England) set out to investigate how much these confounders influenced the association between breastfeeding duration and cognitive development.
They analyzed data from the U.K. Millennium Cohort Study on 7,855 infants born in 2000 to 2002 and followed until age 14. They highlighted that although the cohort was not specifically designed to address the association between breastfeeding and cognition, it included information on duration of any breastfeeding, duration of exclusive breastfeeding, verbal cognitive scores at ages 5, 7, 11, and 14, spatial cognitive scores at ages 5, 7, and 11, as well as potential confounders, including socioeconomic characteristics and maternal cognition, based on a vocabulary test.
The researchers discovered that longer breastfeeding durations were associated with higher verbal and spatial cognitive scores at all ages up to 14 and 11, respectively.
After taking the differences in socioeconomic position and maternal cognitive ability into account, those children who were breastfed for longer scored higher in cognitive measures up to age 14, compared with children who were not breastfed. They also found that longer breastfeeding durations were associated with mean cognitive scores 0.08-0.26 standard deviations higher than the mean cognitive score of those who were never breastfed. “This difference may seem small for an individual child but could be important at the population level,” the authors commented.
Modest effect
In the United Kingdom, women who have more educational qualifications and are more economically advantaged tend to breastfeed for longer, said the authors. In addition, they added, this group tends to “score more highly on cognitive tests.”
These differences could explain why babies who breastfeed for longer do better in cognitive assessments. However, they said that in their study, “we found that even after taking these differences into account, children breastfed for longer scored higher in cognitive measures up to age 14, in comparison to children who were not breastfed.”
The authors explained that the association between breastfeeding duration and cognitive scores “persists after adjusting for socioeconomics and maternal intelligence.” However, they pointed out that “the effect was modest.”
A version of this article first appeared on Medscape UK.
Breastfeeding duration is associated with improved cognitive scores at ages 5-14, even after controlling for maternal socioeconomic position and cognitive ability, said the researchers behind a new study.
Despite previous studies demonstrating an association between breastfeeding and standardized intelligence test scores – with breastfed infants scoring higher on intelligence tests than non-breastfed infants – a causal relationship is still contested.
“There is some debate about whether breastfeeding a baby for a longer period of time improves their cognitive development,” the authors of the new study said. They went on to explain how improved cognitive outcomes in breastfed infants could potentially be explained by other characteristics of the women, such as “socioeconomics and maternal intelligence.”
Important at the population level
For the study, published in the open-access journal PLOS ONE, researchers from the University of Oxford (England) set out to investigate how much these confounders influenced the association between breastfeeding duration and cognitive development.
They analyzed data from the U.K. Millennium Cohort Study on 7,855 infants born in 2000 to 2002 and followed until age 14. They highlighted that although the cohort was not specifically designed to address the association between breastfeeding and cognition, it included information on duration of any breastfeeding, duration of exclusive breastfeeding, verbal cognitive scores at ages 5, 7, 11, and 14, spatial cognitive scores at ages 5, 7, and 11, as well as potential confounders, including socioeconomic characteristics and maternal cognition, based on a vocabulary test.
The researchers discovered that longer breastfeeding durations were associated with higher verbal and spatial cognitive scores at all ages up to 14 and 11, respectively.
After taking the differences in socioeconomic position and maternal cognitive ability into account, those children who were breastfed for longer scored higher in cognitive measures up to age 14, compared with children who were not breastfed. They also found that longer breastfeeding durations were associated with mean cognitive scores 0.08-0.26 standard deviations higher than the mean cognitive score of those who were never breastfed. “This difference may seem small for an individual child but could be important at the population level,” the authors commented.
Modest effect
In the United Kingdom, women who have more educational qualifications and are more economically advantaged tend to breastfeed for longer, said the authors. In addition, they added, this group tends to “score more highly on cognitive tests.”
These differences could explain why babies who breastfeed for longer do better in cognitive assessments. However, they said that in their study, “we found that even after taking these differences into account, children breastfed for longer scored higher in cognitive measures up to age 14, in comparison to children who were not breastfed.”
The authors explained that the association between breastfeeding duration and cognitive scores “persists after adjusting for socioeconomics and maternal intelligence.” However, they pointed out that “the effect was modest.”
A version of this article first appeared on Medscape UK.
Breastfeeding duration is associated with improved cognitive scores at ages 5-14, even after controlling for maternal socioeconomic position and cognitive ability, said the researchers behind a new study.
Despite previous studies demonstrating an association between breastfeeding and standardized intelligence test scores – with breastfed infants scoring higher on intelligence tests than non-breastfed infants – a causal relationship is still contested.
“There is some debate about whether breastfeeding a baby for a longer period of time improves their cognitive development,” the authors of the new study said. They went on to explain how improved cognitive outcomes in breastfed infants could potentially be explained by other characteristics of the women, such as “socioeconomics and maternal intelligence.”
Important at the population level
For the study, published in the open-access journal PLOS ONE, researchers from the University of Oxford (England) set out to investigate how much these confounders influenced the association between breastfeeding duration and cognitive development.
They analyzed data from the U.K. Millennium Cohort Study on 7,855 infants born in 2000 to 2002 and followed until age 14. They highlighted that although the cohort was not specifically designed to address the association between breastfeeding and cognition, it included information on duration of any breastfeeding, duration of exclusive breastfeeding, verbal cognitive scores at ages 5, 7, 11, and 14, spatial cognitive scores at ages 5, 7, and 11, as well as potential confounders, including socioeconomic characteristics and maternal cognition, based on a vocabulary test.
The researchers discovered that longer breastfeeding durations were associated with higher verbal and spatial cognitive scores at all ages up to 14 and 11, respectively.
After taking the differences in socioeconomic position and maternal cognitive ability into account, those children who were breastfed for longer scored higher in cognitive measures up to age 14, compared with children who were not breastfed. They also found that longer breastfeeding durations were associated with mean cognitive scores 0.08-0.26 standard deviations higher than the mean cognitive score of those who were never breastfed. “This difference may seem small for an individual child but could be important at the population level,” the authors commented.
Modest effect
In the United Kingdom, women who have more educational qualifications and are more economically advantaged tend to breastfeed for longer, said the authors. In addition, they added, this group tends to “score more highly on cognitive tests.”
These differences could explain why babies who breastfeed for longer do better in cognitive assessments. However, they said that in their study, “we found that even after taking these differences into account, children breastfed for longer scored higher in cognitive measures up to age 14, in comparison to children who were not breastfed.”
The authors explained that the association between breastfeeding duration and cognitive scores “persists after adjusting for socioeconomics and maternal intelligence.” However, they pointed out that “the effect was modest.”
A version of this article first appeared on Medscape UK.
FROM PLOS ONE
Takotsubo syndrome more deadly in men
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY