User login
Postmenopausal stress linked to mood, cognitive symptoms
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
PHILADELPHIA – , according to research presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
“This work suggests that markers of hypothalamic-pituitary-axis activation that capture total cortisol secretion over multiple months, [such as] hair cortisol, strongly correlate with cognitive performance on attention and working memory tasks, whereas measures of more acute cortisol, [such as] salivary cortisol, may be more strongly associated with depression symptom severity and verbal learning,” Christina Metcalf, PhD, an assistant professor of psychiatry in the Colorado Center for Women’s Behavioral Health and Wellness at the University of Colorado at Denver, Aurora, told attendees. “Given the associations with chronic stress, there’s a lot of potential here to increase our knowledge about how women are doing and managing stress and life stressors during this life transition,” she said.
The study involved collecting hair and saliva samples from 43 healthy women in late perimenopause or early postmenopause with an average age of 51. The participants were predominantly white and college educated. The hair sample was taken within 2 cm of the scalp, and the saliva samples were collected the day after the hair sample collection, at the start and end of a 30-minute rest period that took place between 2:00 and 3:00 p.m. local time.
All the participants had an intact uterus and at least one ovary. None of the participants were current smokers or had recent alcohol or drug dependence, and none had used hormones within the previous 6 months. The study also excluded women who were pregnant or breastfeeding, who had bleached hair or no hair, who were taking steroids, beta blockers or opioid medication, and who had recently taken NSAIDS.
Measuring hair cortisol more feasible
The study was conducted remotely, with participants using video conferencing to communicate with the study personnel and then completing study procedures at home, including 2 days of cognitive testing with the California Verbal Learning Test – Third Edition and the n-back and continuous performance tasks. The participants also completed the Center for Epidemiologic Studies Depression Scale (CES-D).
Participants with higher levels of hair cortisol and salivary cortisol also had more severe depression symptoms (P < .001). Hair cortisol was also significantly associated with attention and working memory: Women with higher levels had fewer correct answers on the 0-back and 1-back trials (P < .01) and made more mistakes on the 2-back trial (P < .001). They also scored with less specificity on the continuous performance tasks (P = .022).
Although no association existed between hair cortisol levels and verbal learning or verbal memory (P > .05), participants with higher hair cortisol did score worse on the immediate recall trials (P = .034). Salivary cortisol levels, on the other hand, showed no association with memory recall trials, attention or working memory (P > .05).
Measuring cortisol from hair samples is more feasible than using saliva samples and may offer valuable insights regarding hypothalamic-pituitary-axis activity “to consider alongside the cognitive and mental health of late peri-/early postmenopausal women,” Dr. Metcalf told attendees. The next step is to find out whether the hypothalamic-pituitary-axis axis is a modifiable biomarker that can be used to improve executive function.
The study was limited by its small population, its cross-sectional design, and the lack of covariates in the current analyses.
Monitor symptoms in midlife
Hadine Joffe, MD, MSc, a professor of psychiatry and executive director of the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, said the study findings were not surprising given how common the complaints of stress and depressive symptoms are.
“Mood changes are linked with acute, immediate cortisol levels at the same point in time, and cognitive symptoms were linked to more chronically elevated cortisol levels,” Dr. Joffe said in an interview. “Women and their providers should monitor for these challenging brain symptoms in midlife as they affect performance and quality of life and are linked with changes in the HPA axis as stress biomarkers.”
Because the study is small and has a cross-sectional design, it’s not possible to determine the direction of the associations or to make any inferences about causation, Dr. Joffe said.
“We cannot make the conclusion that stress is adversely affecting mood and cognitive performance given the design limitations. It is possible that mood and cognitive issues contributed to these stress markers,” Dr. Joffe said.“However, it is known that the experience of stress is linked with vulnerability to mood and cognitive symptoms, and also that mood and cognitive symptoms induce significant stress.”
The research was funded by the Menopause Society, Colorado University, the Ludeman Family Center for Women’s Health Research, the National Institute of Mental Health, and the National Institute of Aging. Dr. Metcalf had no disclosures. Dr. Joffe has received grant support from Merck, Pfizer and Sage, and has been a consultant or advisor for Bayer, Merck and Hello Therapeutics.
AT NAMS 2023
A dozen genes emerge as dangerous during pregnancy
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
FROM OBSTETRICS & GYNECOLOGY
Three-quarters of menopausal women report unexpected symptoms
GLASGOW – Three-quarters of women going through perimenopause and menopause experience unexpected distressing, debilitating, and embarrassing symptoms but often fail to receive appropriate treatment, a large U.K.-based survey found.
“For too long, many people have thought of menopause as just hot flashes and vaginal dryness. But we know hormones work all over our body, so there are many symptoms beyond that,” said Daniel Reisel, MBBS, PhD, a gynecologist at University College London, who presented the survey findings at the 2023 annual meeting of the Royal College of General Practitioners.
Primary care physicians in the United Kingdom have seen an increase in cases of women presenting with symptoms associated with menopause at a time when the country’s Parliament is debating whether all women should have a menopause check-up in their early 40s, he said.
Still, only around 14% of menopausal women in the United Kingdom are prescribed hormone replacement therapy (HRT), despite national and international guidelines clearly stating the benefits of the treatment generally outweigh the risks.
Louise Newson, MBChB, who runs the U.K.’s largest menopause clinic, said many women with symptoms of menopause feel the medical system “gaslights” them – dismissing their concerns as trivial or even fabricated.
In her clinic, she typically sees many women with poor sleep, as well as muscle and joint pains. “Yet [when they visit their GPs], they are incorrectly told that it can’t be hormones because they’re still having periods,” she said.
Prescribed antidepressants often precede HRT
The new study sought to learn what women knew and experienced with respect to menopause symptoms and what they thought was important.
Of the 5,744 women who responded to the survey, 79.4% were aged 40-60 years and 84.6% were White. “The survey respondents were not different from the distribution of ethnicities we see in NHS menopause care,” said Dr. Reisel, adding that “the barriers are greater for women in poorer areas and for those who are non-White.”
A total of 30.4% had two to five hospital consultations before the health care professional considered that symptoms were related to changing hormone levels; 38.5% were offered antidepressants before HRT. Nearly all (94.6%) said they had experienced negative mood changes and emotions since becoming perimenopausal or menopausal; of these, 19.1% were formally diagnosed with depression or a mood disorder.
“This all just highlights the frustrations I feel around menopause care,” Dr. Newson said. “Women are often not given the tools to properly understand what’s going on and then they don’t ask for the right treatment, and many are given antidepressants. It’s still medicalizing the menopause but in a different way.”
Education gap
The researchers also asked women if they had experienced any surprising or unexpected symptoms since becoming perimenopausal or menopausal. To this question, 74.2% said they had. Joint pain was the most common unexpected issue (34%), followed by dry eyes (26%), heart palpitations (25%), and hair issues such as dryness, thinning, and loss (20%).
Dr. Reisel said words used to describe these symptoms in free text responses included “distressing,” “debilitating,” “depressing,” and “embarrassing.”
“When an early-50s woman comes to the GP with dry eyes, joint pain, or recurrent urinary tract infections, for example, before prescribing ibuprofen, or antibiotics, GPs should consider replacing a woman’s hormones and then see what is left in terms of symptoms,” he said.
Cognitive problems and negative mood changes also are common and often overlooked, Dr. Reisel noted. “We often see striking improvements in mood and cognition in women who are prescribed testosterone for low libido, yet symptoms in these areas are not currently an indication to start treatment,” he said. “Data from Newson Health show that 18% have suicidal thoughts in the past 2 weeks, and not many people think about this.”
Much of this lack of understanding around unexpected symptoms relates to a lack of awareness and education. “It goes back to primary and secondary school, and more broadly, these issues are not often talked about in society,” he said.
Dr. Reisel also noted that language and cultural barriers often stand in the way. “Many cultures don’t discuss menopause and hormone health in general at all. For example, in Bengali, spoken by 300 million people, there is no word in for menopause. So many women are gaslighted when they try and describe their symptoms, or they’re simply just unaware.”
Dr. Reisel and Dr. Newson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
GLASGOW – Three-quarters of women going through perimenopause and menopause experience unexpected distressing, debilitating, and embarrassing symptoms but often fail to receive appropriate treatment, a large U.K.-based survey found.
“For too long, many people have thought of menopause as just hot flashes and vaginal dryness. But we know hormones work all over our body, so there are many symptoms beyond that,” said Daniel Reisel, MBBS, PhD, a gynecologist at University College London, who presented the survey findings at the 2023 annual meeting of the Royal College of General Practitioners.
Primary care physicians in the United Kingdom have seen an increase in cases of women presenting with symptoms associated with menopause at a time when the country’s Parliament is debating whether all women should have a menopause check-up in their early 40s, he said.
Still, only around 14% of menopausal women in the United Kingdom are prescribed hormone replacement therapy (HRT), despite national and international guidelines clearly stating the benefits of the treatment generally outweigh the risks.
Louise Newson, MBChB, who runs the U.K.’s largest menopause clinic, said many women with symptoms of menopause feel the medical system “gaslights” them – dismissing their concerns as trivial or even fabricated.
In her clinic, she typically sees many women with poor sleep, as well as muscle and joint pains. “Yet [when they visit their GPs], they are incorrectly told that it can’t be hormones because they’re still having periods,” she said.
Prescribed antidepressants often precede HRT
The new study sought to learn what women knew and experienced with respect to menopause symptoms and what they thought was important.
Of the 5,744 women who responded to the survey, 79.4% were aged 40-60 years and 84.6% were White. “The survey respondents were not different from the distribution of ethnicities we see in NHS menopause care,” said Dr. Reisel, adding that “the barriers are greater for women in poorer areas and for those who are non-White.”
A total of 30.4% had two to five hospital consultations before the health care professional considered that symptoms were related to changing hormone levels; 38.5% were offered antidepressants before HRT. Nearly all (94.6%) said they had experienced negative mood changes and emotions since becoming perimenopausal or menopausal; of these, 19.1% were formally diagnosed with depression or a mood disorder.
“This all just highlights the frustrations I feel around menopause care,” Dr. Newson said. “Women are often not given the tools to properly understand what’s going on and then they don’t ask for the right treatment, and many are given antidepressants. It’s still medicalizing the menopause but in a different way.”
Education gap
The researchers also asked women if they had experienced any surprising or unexpected symptoms since becoming perimenopausal or menopausal. To this question, 74.2% said they had. Joint pain was the most common unexpected issue (34%), followed by dry eyes (26%), heart palpitations (25%), and hair issues such as dryness, thinning, and loss (20%).
Dr. Reisel said words used to describe these symptoms in free text responses included “distressing,” “debilitating,” “depressing,” and “embarrassing.”
“When an early-50s woman comes to the GP with dry eyes, joint pain, or recurrent urinary tract infections, for example, before prescribing ibuprofen, or antibiotics, GPs should consider replacing a woman’s hormones and then see what is left in terms of symptoms,” he said.
Cognitive problems and negative mood changes also are common and often overlooked, Dr. Reisel noted. “We often see striking improvements in mood and cognition in women who are prescribed testosterone for low libido, yet symptoms in these areas are not currently an indication to start treatment,” he said. “Data from Newson Health show that 18% have suicidal thoughts in the past 2 weeks, and not many people think about this.”
Much of this lack of understanding around unexpected symptoms relates to a lack of awareness and education. “It goes back to primary and secondary school, and more broadly, these issues are not often talked about in society,” he said.
Dr. Reisel also noted that language and cultural barriers often stand in the way. “Many cultures don’t discuss menopause and hormone health in general at all. For example, in Bengali, spoken by 300 million people, there is no word in for menopause. So many women are gaslighted when they try and describe their symptoms, or they’re simply just unaware.”
Dr. Reisel and Dr. Newson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
GLASGOW – Three-quarters of women going through perimenopause and menopause experience unexpected distressing, debilitating, and embarrassing symptoms but often fail to receive appropriate treatment, a large U.K.-based survey found.
“For too long, many people have thought of menopause as just hot flashes and vaginal dryness. But we know hormones work all over our body, so there are many symptoms beyond that,” said Daniel Reisel, MBBS, PhD, a gynecologist at University College London, who presented the survey findings at the 2023 annual meeting of the Royal College of General Practitioners.
Primary care physicians in the United Kingdom have seen an increase in cases of women presenting with symptoms associated with menopause at a time when the country’s Parliament is debating whether all women should have a menopause check-up in their early 40s, he said.
Still, only around 14% of menopausal women in the United Kingdom are prescribed hormone replacement therapy (HRT), despite national and international guidelines clearly stating the benefits of the treatment generally outweigh the risks.
Louise Newson, MBChB, who runs the U.K.’s largest menopause clinic, said many women with symptoms of menopause feel the medical system “gaslights” them – dismissing their concerns as trivial or even fabricated.
In her clinic, she typically sees many women with poor sleep, as well as muscle and joint pains. “Yet [when they visit their GPs], they are incorrectly told that it can’t be hormones because they’re still having periods,” she said.
Prescribed antidepressants often precede HRT
The new study sought to learn what women knew and experienced with respect to menopause symptoms and what they thought was important.
Of the 5,744 women who responded to the survey, 79.4% were aged 40-60 years and 84.6% were White. “The survey respondents were not different from the distribution of ethnicities we see in NHS menopause care,” said Dr. Reisel, adding that “the barriers are greater for women in poorer areas and for those who are non-White.”
A total of 30.4% had two to five hospital consultations before the health care professional considered that symptoms were related to changing hormone levels; 38.5% were offered antidepressants before HRT. Nearly all (94.6%) said they had experienced negative mood changes and emotions since becoming perimenopausal or menopausal; of these, 19.1% were formally diagnosed with depression or a mood disorder.
“This all just highlights the frustrations I feel around menopause care,” Dr. Newson said. “Women are often not given the tools to properly understand what’s going on and then they don’t ask for the right treatment, and many are given antidepressants. It’s still medicalizing the menopause but in a different way.”
Education gap
The researchers also asked women if they had experienced any surprising or unexpected symptoms since becoming perimenopausal or menopausal. To this question, 74.2% said they had. Joint pain was the most common unexpected issue (34%), followed by dry eyes (26%), heart palpitations (25%), and hair issues such as dryness, thinning, and loss (20%).
Dr. Reisel said words used to describe these symptoms in free text responses included “distressing,” “debilitating,” “depressing,” and “embarrassing.”
“When an early-50s woman comes to the GP with dry eyes, joint pain, or recurrent urinary tract infections, for example, before prescribing ibuprofen, or antibiotics, GPs should consider replacing a woman’s hormones and then see what is left in terms of symptoms,” he said.
Cognitive problems and negative mood changes also are common and often overlooked, Dr. Reisel noted. “We often see striking improvements in mood and cognition in women who are prescribed testosterone for low libido, yet symptoms in these areas are not currently an indication to start treatment,” he said. “Data from Newson Health show that 18% have suicidal thoughts in the past 2 weeks, and not many people think about this.”
Much of this lack of understanding around unexpected symptoms relates to a lack of awareness and education. “It goes back to primary and secondary school, and more broadly, these issues are not often talked about in society,” he said.
Dr. Reisel also noted that language and cultural barriers often stand in the way. “Many cultures don’t discuss menopause and hormone health in general at all. For example, in Bengali, spoken by 300 million people, there is no word in for menopause. So many women are gaslighted when they try and describe their symptoms, or they’re simply just unaware.”
Dr. Reisel and Dr. Newson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment order evidence comes to light for premenopausal idiopathic osteoporosis: What to do after denosumab
VANCOUVER – With treatment with a bisphosphonate following sequential use of teriparatide (Forteo) and denosumab (Prolia) for premenopausal women with idiopathic osteoporosis, bone mineral density (BMD) was maintained over the first year following denosumab cessation, according to results from a small, nonrandomized extension of a phase 2 study.
Bisphosphonates are recommended for patients after they have completed a course of denosumab because cessation of the bone resorption blocker is known to increase bone turnover markers, decrease BMD, and raise the risk of vertebral fractures. Although there is evidence to support this treatment sequence for postmenopausal women, there was no evidence regarding premenopausal women with idiopathic osteoporosis, said Adi Cohen, MD, who presented the results of the study at the annual meeting of the American Society for Bone and Mineral Research.
In the extension study, neither length of treatment with denosumab nor transition to menopause affected BMD results. Weekly doses of alendronate (ALN) better suppressed C-terminal telopeptide (CTX) than did zoledronic acid (ZOL) and led to better maintenance of BMD than did a single dose of ZOL. The researchers suggested that single-dose ZOL may not prevent bone loss for an entire year.
It is too early to call the results practice changing, said Dr. Cohen, professor of medicine and endocrinology at Columbia University Irving Medical Center, New York, but she noted, “It’s important just to provide information about how sequences of osteoporosis medications might be used in a rare but certainly understudied group of premenopausal women with osteoporosis who need treatment, and these data hopefully will help make some treatment decisions.”
In the early 2000s, researchers initially believed that premenopausal women with low BMD had experienced some kind of temporary event and that they would likely improve on their own over time. “I think we now recognize that whatever it is that causes this is an ongoing issue and that this is a problem they’re going to have to deal with for the rest of their lives. This is something that they have to stay on top of,” said coauthor Elizabeth Shane, MD, who is a professor of medicine at CUIMC.
However, there are no practice guidelines for the management of osteoporosis in premenopausal women, according to Dr. Shane. She noted that there is controversy as to whether to treat women with low bone density who do not have a history of fractures. “I think that there’s pretty much agreement that anybody who has a lot of fractures has an early-onset form of osteoporosis. The controversy is what to do about the person who just has a low bone density and hasn’t yet fractured and what is the utility of trying to treat them at that point and perhaps prevent a fracture. I don’t think we have enough data to address that,” Dr. Shane said.
Still, the research has provided some clarity in her own practice. “I think if somebody would come to my office who had very low bone density, I would probably treat them. If they have fractures, I would definitely treat them. I think that our work has provided a framework for people to approach that,” she said.
The study was an extension of a sequential treatment approach that began with 2 years of teriparatide (20 mcg daily) followed by an extension study of 2–3 years of treatment with denosumab (60 mg every 6 months). Seven months after the last dose of denosumab, patients underwent 1 year of treatment with ALN (70 mg weekly; n = 18) or a single dose of ZOL (5 mg IV; n = 6), according to patient choice.
The original phase 2 study started with 41 women. At 24 months, teriparatide treatment led to BMD increases of 13% in the lumbar spine (LS), 5% in the total hip (TH), and 5% in the femoral neck (FN). There was a 2% decline in BMD in the forearm (distal radius [DR]). A group of 32 of the women participated in an extension study and took denosumab for 12 months. Of those patients, 29 continued to take it for another 12 months. At 12 months, BMD increased 5% in the LS, 3% in the TH, 3% in the FN, and 1% in the DR (P < .05 for all). At 24 months, BMD rose by 22%, 10%, and 10% at the first three of those locations. BMD in the DR remained stable, compared with the baseline after taking teriparatide.
The bisphosphonate phase of the extension study included 24 women (mean age, 43 years). The mean body mass index of the patients was 23.0 kg/m2. The patients had experienced a mean of 3.0 fractures in adulthood, and 38% of patients had a history of vertebral fracture.
Over 12 months of follow-up, the researchers found no statistically significant difference in BMD in the LS, TH, or FN, compared with bisphosphonate extension baseline. There was also no statistically significant change in serum CTX. There was evidence that, among patients with higher rates of bone turnover, there were higher rates of LS and FN bone loss during bisphosphonate treatment.
Among patients taking ZOL, at 12 months there was a statistically significant rise in CTX levels, but not among patients taking ALN. There were no new vertebral fractures among any participants during the bisphosphonate extension period.
The results represent critical data for an understudied population, according to Yumie Rhee, MD, PhD, who was comoderator of the session in which the study was presented. “They are showing that by using a bisphosphonate [patients] have this just slight decrease, but within error, so it’s maintaining the BMD, at least. I think it’s very important. It will be fascinating to see next year’s follow-up,” said Dr. Rhee, a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea. “The problem with premenopausal osteoporosis is that we don’t have good evidence. Even though this study is very small, we’re just following that data, all of us.”
Comoderator Maria Zanchetta, MD, a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires, agreed. “We know what to do when we stop denosumab in postmenopausal women. We didn’t have any work about what to do when we stopped in premenopausal women. You can think that probably it’s going to be the same, but this is the first time you have the evidence that if you give bisphosphonate, you will maintain BMD.”
Limitations to the study include its small size and the lack of a placebo-treated control group. In addition, the bisphosphonate extension was not randomized.
The studies were funded by the U.S. Food and Drug Administration and Amgen. Dr. Cohen and Dr. Shane received research funding from Amgen. Dr. Rhee and Dr. Zanchetta have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
VANCOUVER – With treatment with a bisphosphonate following sequential use of teriparatide (Forteo) and denosumab (Prolia) for premenopausal women with idiopathic osteoporosis, bone mineral density (BMD) was maintained over the first year following denosumab cessation, according to results from a small, nonrandomized extension of a phase 2 study.
Bisphosphonates are recommended for patients after they have completed a course of denosumab because cessation of the bone resorption blocker is known to increase bone turnover markers, decrease BMD, and raise the risk of vertebral fractures. Although there is evidence to support this treatment sequence for postmenopausal women, there was no evidence regarding premenopausal women with idiopathic osteoporosis, said Adi Cohen, MD, who presented the results of the study at the annual meeting of the American Society for Bone and Mineral Research.
In the extension study, neither length of treatment with denosumab nor transition to menopause affected BMD results. Weekly doses of alendronate (ALN) better suppressed C-terminal telopeptide (CTX) than did zoledronic acid (ZOL) and led to better maintenance of BMD than did a single dose of ZOL. The researchers suggested that single-dose ZOL may not prevent bone loss for an entire year.
It is too early to call the results practice changing, said Dr. Cohen, professor of medicine and endocrinology at Columbia University Irving Medical Center, New York, but she noted, “It’s important just to provide information about how sequences of osteoporosis medications might be used in a rare but certainly understudied group of premenopausal women with osteoporosis who need treatment, and these data hopefully will help make some treatment decisions.”
In the early 2000s, researchers initially believed that premenopausal women with low BMD had experienced some kind of temporary event and that they would likely improve on their own over time. “I think we now recognize that whatever it is that causes this is an ongoing issue and that this is a problem they’re going to have to deal with for the rest of their lives. This is something that they have to stay on top of,” said coauthor Elizabeth Shane, MD, who is a professor of medicine at CUIMC.
However, there are no practice guidelines for the management of osteoporosis in premenopausal women, according to Dr. Shane. She noted that there is controversy as to whether to treat women with low bone density who do not have a history of fractures. “I think that there’s pretty much agreement that anybody who has a lot of fractures has an early-onset form of osteoporosis. The controversy is what to do about the person who just has a low bone density and hasn’t yet fractured and what is the utility of trying to treat them at that point and perhaps prevent a fracture. I don’t think we have enough data to address that,” Dr. Shane said.
Still, the research has provided some clarity in her own practice. “I think if somebody would come to my office who had very low bone density, I would probably treat them. If they have fractures, I would definitely treat them. I think that our work has provided a framework for people to approach that,” she said.
The study was an extension of a sequential treatment approach that began with 2 years of teriparatide (20 mcg daily) followed by an extension study of 2–3 years of treatment with denosumab (60 mg every 6 months). Seven months after the last dose of denosumab, patients underwent 1 year of treatment with ALN (70 mg weekly; n = 18) or a single dose of ZOL (5 mg IV; n = 6), according to patient choice.
The original phase 2 study started with 41 women. At 24 months, teriparatide treatment led to BMD increases of 13% in the lumbar spine (LS), 5% in the total hip (TH), and 5% in the femoral neck (FN). There was a 2% decline in BMD in the forearm (distal radius [DR]). A group of 32 of the women participated in an extension study and took denosumab for 12 months. Of those patients, 29 continued to take it for another 12 months. At 12 months, BMD increased 5% in the LS, 3% in the TH, 3% in the FN, and 1% in the DR (P < .05 for all). At 24 months, BMD rose by 22%, 10%, and 10% at the first three of those locations. BMD in the DR remained stable, compared with the baseline after taking teriparatide.
The bisphosphonate phase of the extension study included 24 women (mean age, 43 years). The mean body mass index of the patients was 23.0 kg/m2. The patients had experienced a mean of 3.0 fractures in adulthood, and 38% of patients had a history of vertebral fracture.
Over 12 months of follow-up, the researchers found no statistically significant difference in BMD in the LS, TH, or FN, compared with bisphosphonate extension baseline. There was also no statistically significant change in serum CTX. There was evidence that, among patients with higher rates of bone turnover, there were higher rates of LS and FN bone loss during bisphosphonate treatment.
Among patients taking ZOL, at 12 months there was a statistically significant rise in CTX levels, but not among patients taking ALN. There were no new vertebral fractures among any participants during the bisphosphonate extension period.
The results represent critical data for an understudied population, according to Yumie Rhee, MD, PhD, who was comoderator of the session in which the study was presented. “They are showing that by using a bisphosphonate [patients] have this just slight decrease, but within error, so it’s maintaining the BMD, at least. I think it’s very important. It will be fascinating to see next year’s follow-up,” said Dr. Rhee, a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea. “The problem with premenopausal osteoporosis is that we don’t have good evidence. Even though this study is very small, we’re just following that data, all of us.”
Comoderator Maria Zanchetta, MD, a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires, agreed. “We know what to do when we stop denosumab in postmenopausal women. We didn’t have any work about what to do when we stopped in premenopausal women. You can think that probably it’s going to be the same, but this is the first time you have the evidence that if you give bisphosphonate, you will maintain BMD.”
Limitations to the study include its small size and the lack of a placebo-treated control group. In addition, the bisphosphonate extension was not randomized.
The studies were funded by the U.S. Food and Drug Administration and Amgen. Dr. Cohen and Dr. Shane received research funding from Amgen. Dr. Rhee and Dr. Zanchetta have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
VANCOUVER – With treatment with a bisphosphonate following sequential use of teriparatide (Forteo) and denosumab (Prolia) for premenopausal women with idiopathic osteoporosis, bone mineral density (BMD) was maintained over the first year following denosumab cessation, according to results from a small, nonrandomized extension of a phase 2 study.
Bisphosphonates are recommended for patients after they have completed a course of denosumab because cessation of the bone resorption blocker is known to increase bone turnover markers, decrease BMD, and raise the risk of vertebral fractures. Although there is evidence to support this treatment sequence for postmenopausal women, there was no evidence regarding premenopausal women with idiopathic osteoporosis, said Adi Cohen, MD, who presented the results of the study at the annual meeting of the American Society for Bone and Mineral Research.
In the extension study, neither length of treatment with denosumab nor transition to menopause affected BMD results. Weekly doses of alendronate (ALN) better suppressed C-terminal telopeptide (CTX) than did zoledronic acid (ZOL) and led to better maintenance of BMD than did a single dose of ZOL. The researchers suggested that single-dose ZOL may not prevent bone loss for an entire year.
It is too early to call the results practice changing, said Dr. Cohen, professor of medicine and endocrinology at Columbia University Irving Medical Center, New York, but she noted, “It’s important just to provide information about how sequences of osteoporosis medications might be used in a rare but certainly understudied group of premenopausal women with osteoporosis who need treatment, and these data hopefully will help make some treatment decisions.”
In the early 2000s, researchers initially believed that premenopausal women with low BMD had experienced some kind of temporary event and that they would likely improve on their own over time. “I think we now recognize that whatever it is that causes this is an ongoing issue and that this is a problem they’re going to have to deal with for the rest of their lives. This is something that they have to stay on top of,” said coauthor Elizabeth Shane, MD, who is a professor of medicine at CUIMC.
However, there are no practice guidelines for the management of osteoporosis in premenopausal women, according to Dr. Shane. She noted that there is controversy as to whether to treat women with low bone density who do not have a history of fractures. “I think that there’s pretty much agreement that anybody who has a lot of fractures has an early-onset form of osteoporosis. The controversy is what to do about the person who just has a low bone density and hasn’t yet fractured and what is the utility of trying to treat them at that point and perhaps prevent a fracture. I don’t think we have enough data to address that,” Dr. Shane said.
Still, the research has provided some clarity in her own practice. “I think if somebody would come to my office who had very low bone density, I would probably treat them. If they have fractures, I would definitely treat them. I think that our work has provided a framework for people to approach that,” she said.
The study was an extension of a sequential treatment approach that began with 2 years of teriparatide (20 mcg daily) followed by an extension study of 2–3 years of treatment with denosumab (60 mg every 6 months). Seven months after the last dose of denosumab, patients underwent 1 year of treatment with ALN (70 mg weekly; n = 18) or a single dose of ZOL (5 mg IV; n = 6), according to patient choice.
The original phase 2 study started with 41 women. At 24 months, teriparatide treatment led to BMD increases of 13% in the lumbar spine (LS), 5% in the total hip (TH), and 5% in the femoral neck (FN). There was a 2% decline in BMD in the forearm (distal radius [DR]). A group of 32 of the women participated in an extension study and took denosumab for 12 months. Of those patients, 29 continued to take it for another 12 months. At 12 months, BMD increased 5% in the LS, 3% in the TH, 3% in the FN, and 1% in the DR (P < .05 for all). At 24 months, BMD rose by 22%, 10%, and 10% at the first three of those locations. BMD in the DR remained stable, compared with the baseline after taking teriparatide.
The bisphosphonate phase of the extension study included 24 women (mean age, 43 years). The mean body mass index of the patients was 23.0 kg/m2. The patients had experienced a mean of 3.0 fractures in adulthood, and 38% of patients had a history of vertebral fracture.
Over 12 months of follow-up, the researchers found no statistically significant difference in BMD in the LS, TH, or FN, compared with bisphosphonate extension baseline. There was also no statistically significant change in serum CTX. There was evidence that, among patients with higher rates of bone turnover, there were higher rates of LS and FN bone loss during bisphosphonate treatment.
Among patients taking ZOL, at 12 months there was a statistically significant rise in CTX levels, but not among patients taking ALN. There were no new vertebral fractures among any participants during the bisphosphonate extension period.
The results represent critical data for an understudied population, according to Yumie Rhee, MD, PhD, who was comoderator of the session in which the study was presented. “They are showing that by using a bisphosphonate [patients] have this just slight decrease, but within error, so it’s maintaining the BMD, at least. I think it’s very important. It will be fascinating to see next year’s follow-up,” said Dr. Rhee, a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea. “The problem with premenopausal osteoporosis is that we don’t have good evidence. Even though this study is very small, we’re just following that data, all of us.”
Comoderator Maria Zanchetta, MD, a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires, agreed. “We know what to do when we stop denosumab in postmenopausal women. We didn’t have any work about what to do when we stopped in premenopausal women. You can think that probably it’s going to be the same, but this is the first time you have the evidence that if you give bisphosphonate, you will maintain BMD.”
Limitations to the study include its small size and the lack of a placebo-treated control group. In addition, the bisphosphonate extension was not randomized.
The studies were funded by the U.S. Food and Drug Administration and Amgen. Dr. Cohen and Dr. Shane received research funding from Amgen. Dr. Rhee and Dr. Zanchetta have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
AT ASBMR 2023
A focus on women with diabetes and their offspring
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 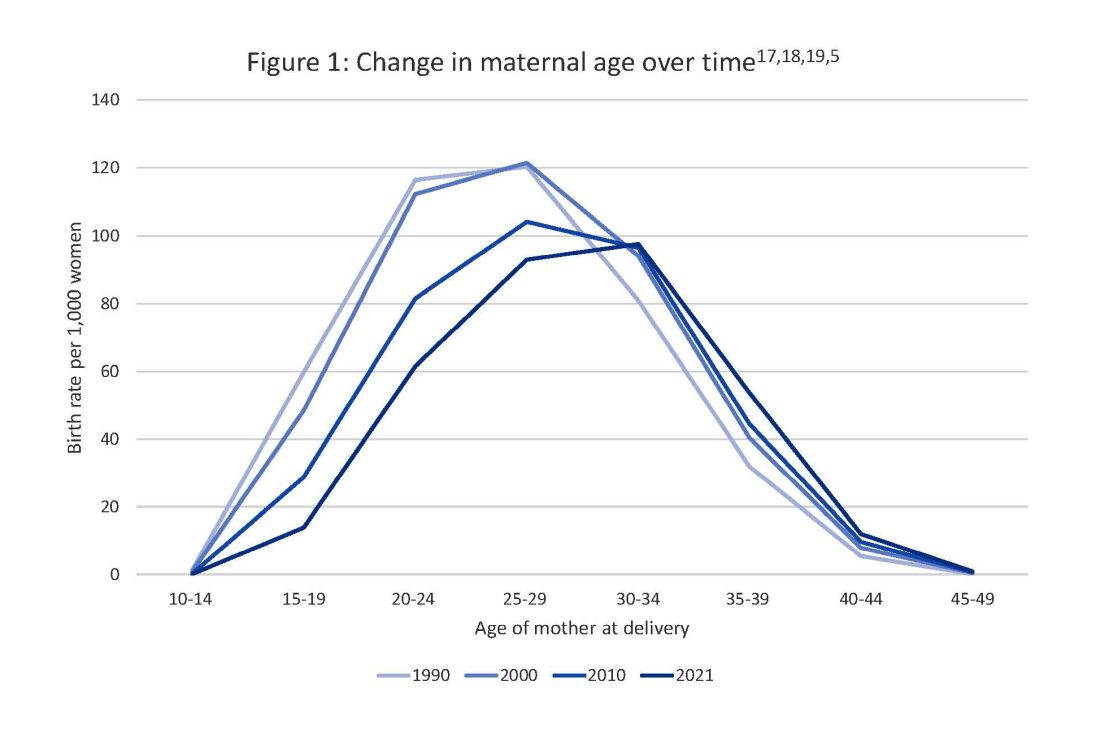
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 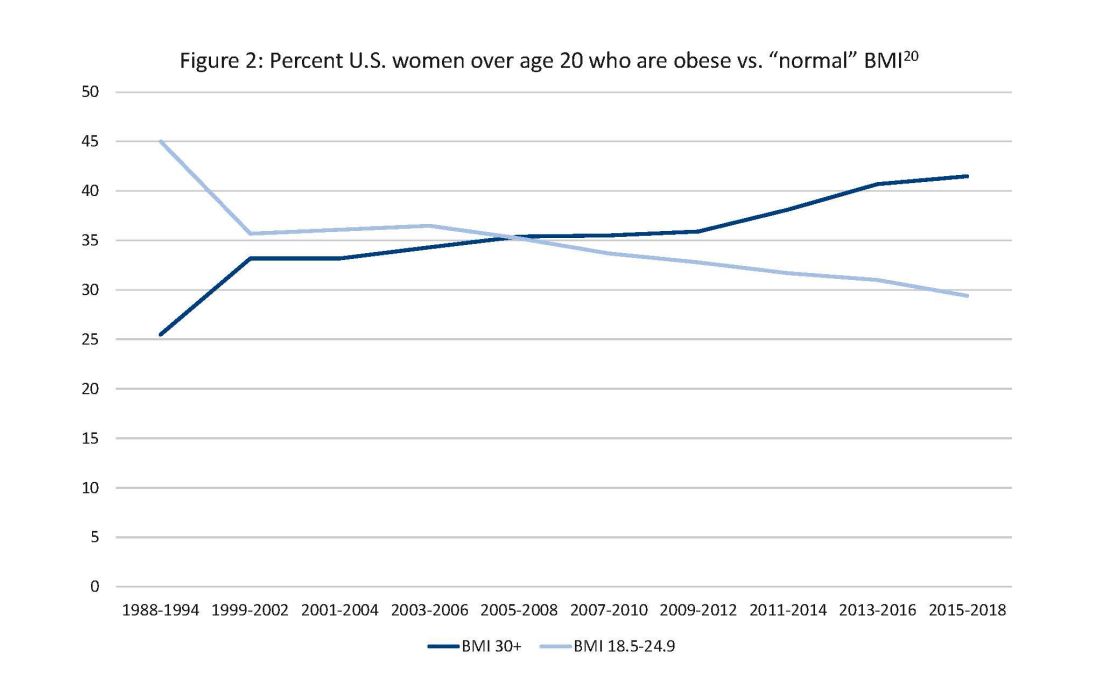
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 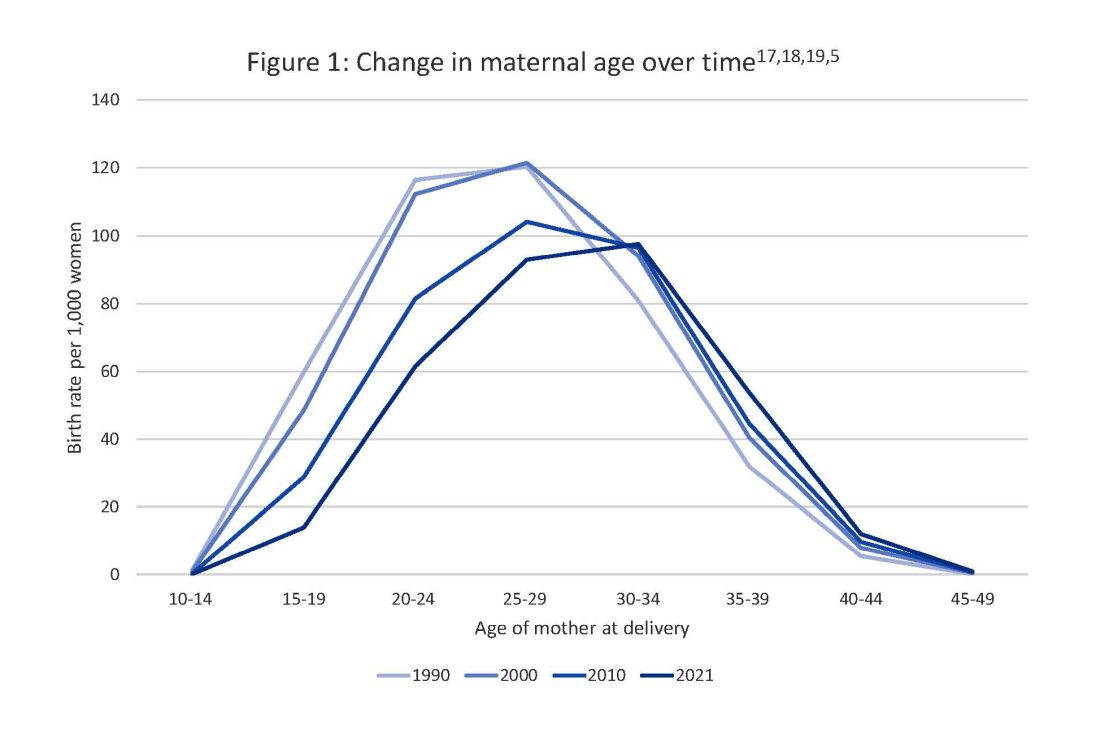
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 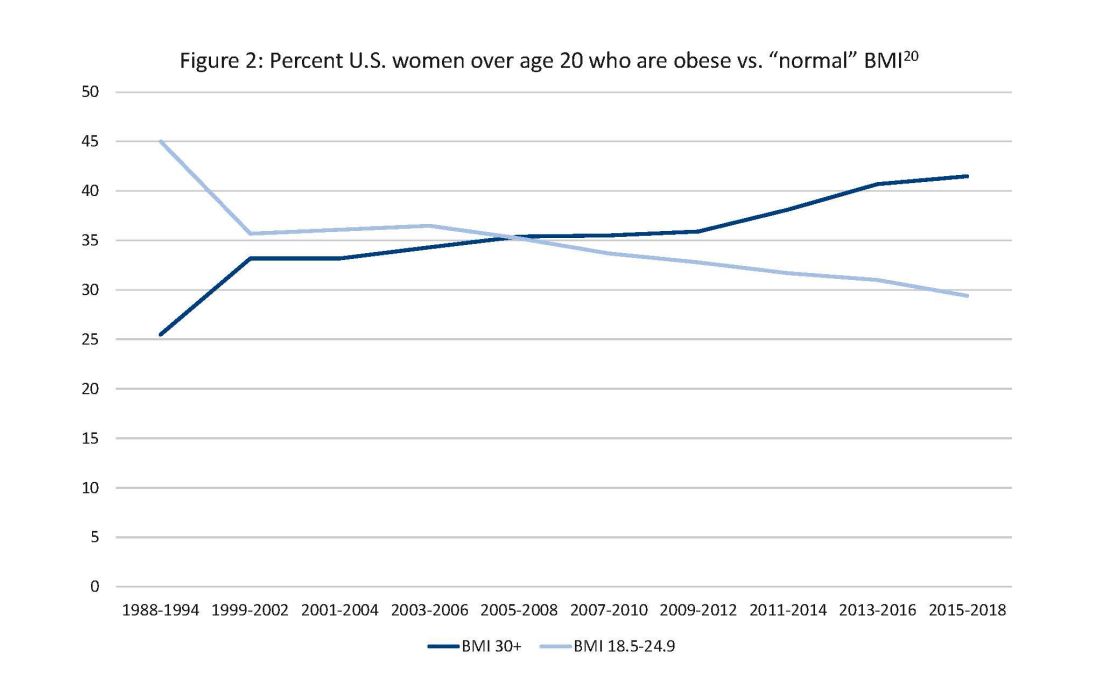
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 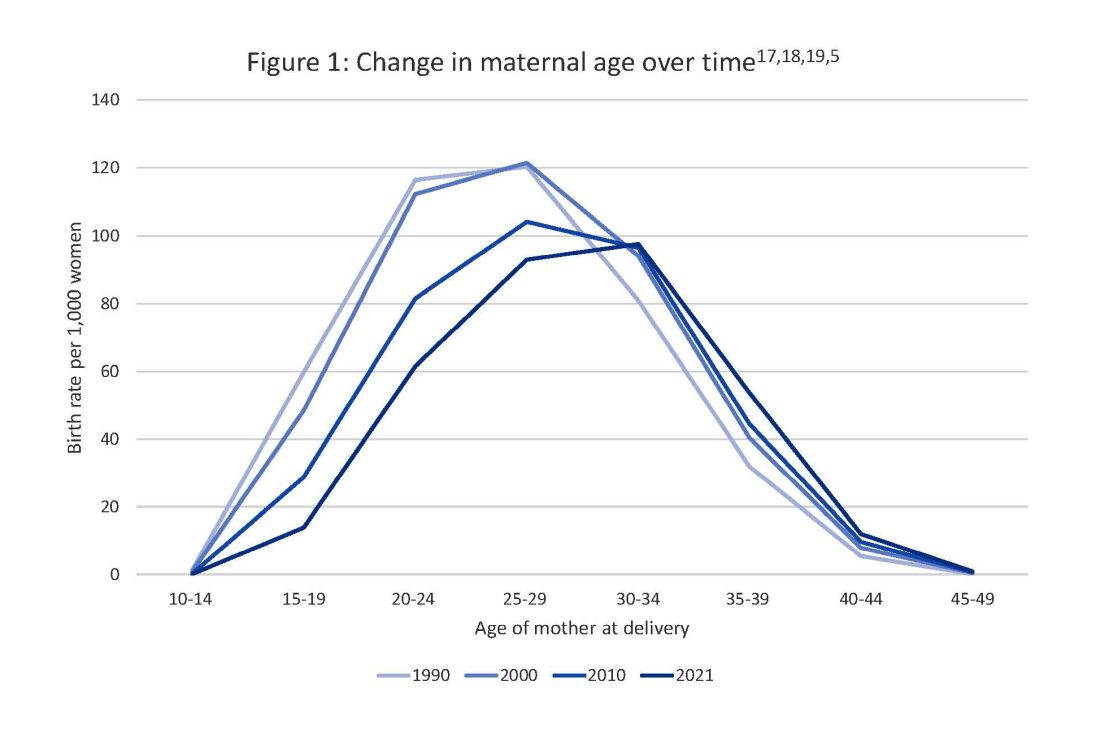
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 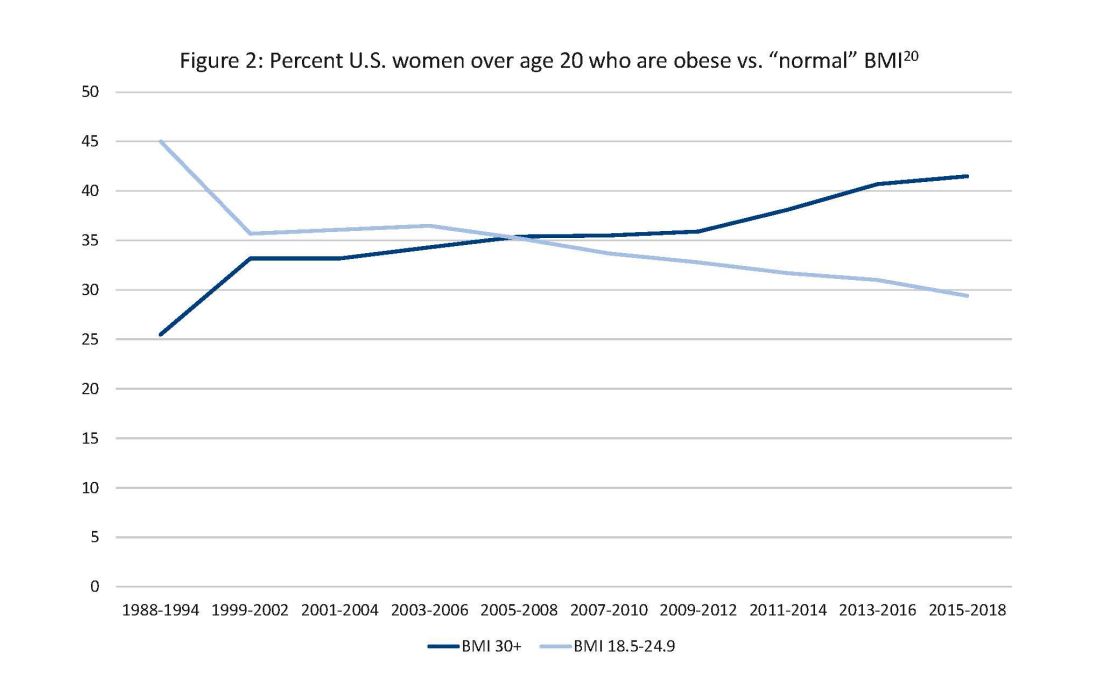
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
Taking a new obesity drug and birth control pills? Be careful
For women who are obese, daily life is wrought with landmines. Whether it’s the challenges of air travel because plane seats are too small, the need to shield themselves from the world’s discriminating eyes, or the great lengths many will go to achieve better health and the promise of longevity, navigating life as an obese person requires a thick skin.
So, it’s no wonder so many are willing to pay more than $1,000 a month out of pocket to get their hands on drugs like semaglutide (Ozempic and Wegovy) or tirzepatide (Mounjaro). The benefits of these drugs, which are part of a new class called glucagonlike peptide–1 (GLP-1) receptor agonists, include significant and rapid weight loss, blood sugar control, and improved life quality; they are unprecedented in a setting where surgery has long been considered the most effective long-term option.
On the flip side, the desire for rapid weight loss and better blood sugar control also comes with an unexpected cost. , making an unintended pregnancy more likely.
Neel Shah, MD, an endocrinologist and associate professor at the University of Texas Health Science Center at Houston, said he has had several patients become pregnant without intending to.
“It was when Mounjaro came out on the market when we started using it,” he said of the drug the Food and Drug Administration approved for type 2 diabetes in 2022. “It [the warning] was in the product insert, but clinically speaking, I don’t know if it was at the top of providers’ minds when they were prescribing Mounjaro.”
When asked if he believed that we were going to be seeing a significant increase in so-called Mounjaro babies, Dr. Shah was sure in his response.
“Absolutely. We will because the sheer volume [of patients] will increase,” he said.
It’s all in the gut
One of the ways that drugs like Mounjaro work is by delaying the time that it takes for food to move from the stomach to the small intestine. Although data are still evolving, it is believed that this process – delayed gastric emptying – may affect the absorption of birth control pills.
Dr. Shah said another theory is that vomiting, which is a common side effect of these types of drugs, also affects the pills’ ability to prevent pregnancy.
And “there’s a prolonged period of ramping up the dose because of the GI side effects,” said Pinar Kodaman, MD, PhD, a reproductive endocrinologist and assistant professor of gynecology at Yale University in New Haven, Conn.
“Initially, at the lowest dose, there may not be a lot of potential effect on absorption and gastric emptying. But as the dose goes up, it becomes more common, and it can cause diarrhea, which is another condition that can affect the absorption of any medication,” she said.
Unanticipated outcomes, extra prevention
Roughly 42% of women in the United States are obese, 40% of whom are between the ages of 20 and 39. Although these new drugs can improve fertility outcomes for women who are obese (especially those with polycystic ovary syndrome, or PCOS), only one – Mounjaro – currently carries a warning about birth control pill effectiveness on its label. Unfortunately, it appears that some doctors are unaware or not counseling patients about this risk, and the data are unclear about whether other drugs in this class, like Ozempic and Wegovy, have the same risks.
“To date, it hasn’t been a typical thing that we counsel about,” said Dr. Kodaman. “It’s all fairly new, but when we have patients on birth control pills, we do review other medications that they are on because some can affect efficacy, and it’s something to keep in mind.”
It’s also unclear if other forms of birth control – for example, birth control patches that deliver through the skin – might carry similar pregnancy risks. Dr. Shah said some of his patients who became pregnant without intending to were using these patches. This raises even more questions, since they deliver drugs through the skin directly into the bloodstream and not through the GI system.
What can women do to help ensure that they don’t become pregnant while using these drugs?
“I really think that if patients want to protect themselves from an unplanned pregnancy, that as soon as they start the GLP receptor agonists, it wouldn’t be a bad idea to use condoms, because the onset of action is pretty quick,” said Dr. Kodaman, noting also that “at the lowest dose there may not be a lot of potential effect on gastric emptying. But as the dose goes up, it becomes much more common or can cause diarrhea.”
Dr. Shah said that in his practice he’s “been telling patients to add barrier contraception” 4 weeks before they start their first dose “and at any dose adjustment.”
Zoobia Chaudhry, an obesity medicine doctor and assistant professor of medicine at Johns Hopkins University in Baltimore, recommends that “patients just make sure that the injection and medication that they take are at least 1 hour apart.”
“Most of the time, patients do take birth control before bedtime, so if the two are spaced, it should be OK,” she said.
Another option is for women to speak to their doctors about other contraceptive options like IUDs or implantable rods, where gastric absorption is not going to be an issue.
“There’s very little research on this class of drugs,” said Emily Goodstein, a 40-year-old small-business owner in Washington, who recently switched from Ozempic to Mounjaro. “Being a person who lives in a larger body is such a horrifying experience because of the way that the world discriminates against you.”
She appreciates the feeling of being proactive that these new drugs grant. It has “opened up a bunch of opportunities for me to be seen as a full individual by the medical establishment,” she said. “I was willing to take the risk, knowing that I would be on these drugs for the rest of my life.”
In addition to being what Dr. Goodstein refers to as a guinea pig, she said she made sure that her primary care doctor was aware that she was not trying or planning to become pregnant again. (She has a 3-year-old child.) Still, her doctor mentioned only the most common side effects linked to these drugs, like nausea, vomiting, and diarrhea, and did not mention the risk of pregnancy.
“Folks are really not talking about the reproductive implications,” she said, referring to members of a Facebook group on these drugs that she belongs to.
Like patients themselves, many doctors are just beginning to get their arms around these agents. “Awareness, education, provider involvement, and having a multidisciplinary team could help patients achieve the goals that they set out for themselves,” said Dr. Shah.
Clear conversations are key.
A version of this article first appeared on WebMD.com.
For women who are obese, daily life is wrought with landmines. Whether it’s the challenges of air travel because plane seats are too small, the need to shield themselves from the world’s discriminating eyes, or the great lengths many will go to achieve better health and the promise of longevity, navigating life as an obese person requires a thick skin.
So, it’s no wonder so many are willing to pay more than $1,000 a month out of pocket to get their hands on drugs like semaglutide (Ozempic and Wegovy) or tirzepatide (Mounjaro). The benefits of these drugs, which are part of a new class called glucagonlike peptide–1 (GLP-1) receptor agonists, include significant and rapid weight loss, blood sugar control, and improved life quality; they are unprecedented in a setting where surgery has long been considered the most effective long-term option.
On the flip side, the desire for rapid weight loss and better blood sugar control also comes with an unexpected cost. , making an unintended pregnancy more likely.
Neel Shah, MD, an endocrinologist and associate professor at the University of Texas Health Science Center at Houston, said he has had several patients become pregnant without intending to.
“It was when Mounjaro came out on the market when we started using it,” he said of the drug the Food and Drug Administration approved for type 2 diabetes in 2022. “It [the warning] was in the product insert, but clinically speaking, I don’t know if it was at the top of providers’ minds when they were prescribing Mounjaro.”
When asked if he believed that we were going to be seeing a significant increase in so-called Mounjaro babies, Dr. Shah was sure in his response.
“Absolutely. We will because the sheer volume [of patients] will increase,” he said.
It’s all in the gut
One of the ways that drugs like Mounjaro work is by delaying the time that it takes for food to move from the stomach to the small intestine. Although data are still evolving, it is believed that this process – delayed gastric emptying – may affect the absorption of birth control pills.
Dr. Shah said another theory is that vomiting, which is a common side effect of these types of drugs, also affects the pills’ ability to prevent pregnancy.
And “there’s a prolonged period of ramping up the dose because of the GI side effects,” said Pinar Kodaman, MD, PhD, a reproductive endocrinologist and assistant professor of gynecology at Yale University in New Haven, Conn.
“Initially, at the lowest dose, there may not be a lot of potential effect on absorption and gastric emptying. But as the dose goes up, it becomes more common, and it can cause diarrhea, which is another condition that can affect the absorption of any medication,” she said.
Unanticipated outcomes, extra prevention
Roughly 42% of women in the United States are obese, 40% of whom are between the ages of 20 and 39. Although these new drugs can improve fertility outcomes for women who are obese (especially those with polycystic ovary syndrome, or PCOS), only one – Mounjaro – currently carries a warning about birth control pill effectiveness on its label. Unfortunately, it appears that some doctors are unaware or not counseling patients about this risk, and the data are unclear about whether other drugs in this class, like Ozempic and Wegovy, have the same risks.
“To date, it hasn’t been a typical thing that we counsel about,” said Dr. Kodaman. “It’s all fairly new, but when we have patients on birth control pills, we do review other medications that they are on because some can affect efficacy, and it’s something to keep in mind.”
It’s also unclear if other forms of birth control – for example, birth control patches that deliver through the skin – might carry similar pregnancy risks. Dr. Shah said some of his patients who became pregnant without intending to were using these patches. This raises even more questions, since they deliver drugs through the skin directly into the bloodstream and not through the GI system.
What can women do to help ensure that they don’t become pregnant while using these drugs?
“I really think that if patients want to protect themselves from an unplanned pregnancy, that as soon as they start the GLP receptor agonists, it wouldn’t be a bad idea to use condoms, because the onset of action is pretty quick,” said Dr. Kodaman, noting also that “at the lowest dose there may not be a lot of potential effect on gastric emptying. But as the dose goes up, it becomes much more common or can cause diarrhea.”
Dr. Shah said that in his practice he’s “been telling patients to add barrier contraception” 4 weeks before they start their first dose “and at any dose adjustment.”
Zoobia Chaudhry, an obesity medicine doctor and assistant professor of medicine at Johns Hopkins University in Baltimore, recommends that “patients just make sure that the injection and medication that they take are at least 1 hour apart.”
“Most of the time, patients do take birth control before bedtime, so if the two are spaced, it should be OK,” she said.
Another option is for women to speak to their doctors about other contraceptive options like IUDs or implantable rods, where gastric absorption is not going to be an issue.
“There’s very little research on this class of drugs,” said Emily Goodstein, a 40-year-old small-business owner in Washington, who recently switched from Ozempic to Mounjaro. “Being a person who lives in a larger body is such a horrifying experience because of the way that the world discriminates against you.”
She appreciates the feeling of being proactive that these new drugs grant. It has “opened up a bunch of opportunities for me to be seen as a full individual by the medical establishment,” she said. “I was willing to take the risk, knowing that I would be on these drugs for the rest of my life.”
In addition to being what Dr. Goodstein refers to as a guinea pig, she said she made sure that her primary care doctor was aware that she was not trying or planning to become pregnant again. (She has a 3-year-old child.) Still, her doctor mentioned only the most common side effects linked to these drugs, like nausea, vomiting, and diarrhea, and did not mention the risk of pregnancy.
“Folks are really not talking about the reproductive implications,” she said, referring to members of a Facebook group on these drugs that she belongs to.
Like patients themselves, many doctors are just beginning to get their arms around these agents. “Awareness, education, provider involvement, and having a multidisciplinary team could help patients achieve the goals that they set out for themselves,” said Dr. Shah.
Clear conversations are key.
A version of this article first appeared on WebMD.com.
For women who are obese, daily life is wrought with landmines. Whether it’s the challenges of air travel because plane seats are too small, the need to shield themselves from the world’s discriminating eyes, or the great lengths many will go to achieve better health and the promise of longevity, navigating life as an obese person requires a thick skin.
So, it’s no wonder so many are willing to pay more than $1,000 a month out of pocket to get their hands on drugs like semaglutide (Ozempic and Wegovy) or tirzepatide (Mounjaro). The benefits of these drugs, which are part of a new class called glucagonlike peptide–1 (GLP-1) receptor agonists, include significant and rapid weight loss, blood sugar control, and improved life quality; they are unprecedented in a setting where surgery has long been considered the most effective long-term option.
On the flip side, the desire for rapid weight loss and better blood sugar control also comes with an unexpected cost. , making an unintended pregnancy more likely.
Neel Shah, MD, an endocrinologist and associate professor at the University of Texas Health Science Center at Houston, said he has had several patients become pregnant without intending to.
“It was when Mounjaro came out on the market when we started using it,” he said of the drug the Food and Drug Administration approved for type 2 diabetes in 2022. “It [the warning] was in the product insert, but clinically speaking, I don’t know if it was at the top of providers’ minds when they were prescribing Mounjaro.”
When asked if he believed that we were going to be seeing a significant increase in so-called Mounjaro babies, Dr. Shah was sure in his response.
“Absolutely. We will because the sheer volume [of patients] will increase,” he said.
It’s all in the gut
One of the ways that drugs like Mounjaro work is by delaying the time that it takes for food to move from the stomach to the small intestine. Although data are still evolving, it is believed that this process – delayed gastric emptying – may affect the absorption of birth control pills.
Dr. Shah said another theory is that vomiting, which is a common side effect of these types of drugs, also affects the pills’ ability to prevent pregnancy.
And “there’s a prolonged period of ramping up the dose because of the GI side effects,” said Pinar Kodaman, MD, PhD, a reproductive endocrinologist and assistant professor of gynecology at Yale University in New Haven, Conn.
“Initially, at the lowest dose, there may not be a lot of potential effect on absorption and gastric emptying. But as the dose goes up, it becomes more common, and it can cause diarrhea, which is another condition that can affect the absorption of any medication,” she said.
Unanticipated outcomes, extra prevention
Roughly 42% of women in the United States are obese, 40% of whom are between the ages of 20 and 39. Although these new drugs can improve fertility outcomes for women who are obese (especially those with polycystic ovary syndrome, or PCOS), only one – Mounjaro – currently carries a warning about birth control pill effectiveness on its label. Unfortunately, it appears that some doctors are unaware or not counseling patients about this risk, and the data are unclear about whether other drugs in this class, like Ozempic and Wegovy, have the same risks.
“To date, it hasn’t been a typical thing that we counsel about,” said Dr. Kodaman. “It’s all fairly new, but when we have patients on birth control pills, we do review other medications that they are on because some can affect efficacy, and it’s something to keep in mind.”
It’s also unclear if other forms of birth control – for example, birth control patches that deliver through the skin – might carry similar pregnancy risks. Dr. Shah said some of his patients who became pregnant without intending to were using these patches. This raises even more questions, since they deliver drugs through the skin directly into the bloodstream and not through the GI system.
What can women do to help ensure that they don’t become pregnant while using these drugs?
“I really think that if patients want to protect themselves from an unplanned pregnancy, that as soon as they start the GLP receptor agonists, it wouldn’t be a bad idea to use condoms, because the onset of action is pretty quick,” said Dr. Kodaman, noting also that “at the lowest dose there may not be a lot of potential effect on gastric emptying. But as the dose goes up, it becomes much more common or can cause diarrhea.”
Dr. Shah said that in his practice he’s “been telling patients to add barrier contraception” 4 weeks before they start their first dose “and at any dose adjustment.”
Zoobia Chaudhry, an obesity medicine doctor and assistant professor of medicine at Johns Hopkins University in Baltimore, recommends that “patients just make sure that the injection and medication that they take are at least 1 hour apart.”
“Most of the time, patients do take birth control before bedtime, so if the two are spaced, it should be OK,” she said.
Another option is for women to speak to their doctors about other contraceptive options like IUDs or implantable rods, where gastric absorption is not going to be an issue.
“There’s very little research on this class of drugs,” said Emily Goodstein, a 40-year-old small-business owner in Washington, who recently switched from Ozempic to Mounjaro. “Being a person who lives in a larger body is such a horrifying experience because of the way that the world discriminates against you.”
She appreciates the feeling of being proactive that these new drugs grant. It has “opened up a bunch of opportunities for me to be seen as a full individual by the medical establishment,” she said. “I was willing to take the risk, knowing that I would be on these drugs for the rest of my life.”
In addition to being what Dr. Goodstein refers to as a guinea pig, she said she made sure that her primary care doctor was aware that she was not trying or planning to become pregnant again. (She has a 3-year-old child.) Still, her doctor mentioned only the most common side effects linked to these drugs, like nausea, vomiting, and diarrhea, and did not mention the risk of pregnancy.
“Folks are really not talking about the reproductive implications,” she said, referring to members of a Facebook group on these drugs that she belongs to.
Like patients themselves, many doctors are just beginning to get their arms around these agents. “Awareness, education, provider involvement, and having a multidisciplinary team could help patients achieve the goals that they set out for themselves,” said Dr. Shah.
Clear conversations are key.
A version of this article first appeared on WebMD.com.
Greater fracture risk reduction seen with denosumab vs. zoledronic acid in postmenopausal women
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VANCOUVER –
A previous head-to-head comparison showed that denosumab increased bone mineral density at key skeletal sites compared with zoledronic acid, but only a single, small observational study has examined fracture risk, and it found no difference.
The new study, presented at the annual meeting of the American Society for Bone and Mineral Research, used a relatively new method of real-world comparative effectiveness analysis called negative control outcome (NCO) to analyze Medicare fee-for-service data.
NCO analysis takes extra pains to remove bias through data that might be linked to potential confounders but could not reasonably be attributed to a drug. For example, people who have greater contact with the health care system may be more likely to get one drug or another. The researchers used the frequency of receiving a flu or pneumonia vaccine as a proxy for this. If the two comparison groups had a significant difference in a proxy, it suggested a hidden bias and forced the researchers to abandon those groupings. Another example used car accidents as a proxy for cognitive impairment.
“If you find meaningful differences between the two groups, and you can say there’s no way a bone drug could account for these differences, then we shouldn’t do this analysis because these groups just aren’t comparable. They probably differ by that confounding factor we couldn’t measure,” said Jeffrey Curtis, MD, who presented the study. He is a professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
The study strongly suggests superiority for denosumab. “There was a significant difference in multiple different groupings of fractures – beginning at year 2, extending to year 3 and even out to year 5 – that showed that there is a significant reduction in fracture risk if you get treated with denosumab [that was greater] than if you get treated with zoledronic acid,” Dr. Curtis said.
The researchers weighed 118 covariates and ultimately identified a population of 90,805 women taking denosumab and 37,328 taking zoledronic acid that was equally balanced in all patient characteristics. The mean age was about 75 years in the denosumab group and 74 in the zoledronic acid group.
The researchers found a 34% lower risk for hip fracture in the denosumab group by 5 years (relative risk, 0.66; 95% confidence interval, 0.43-0.90).
Similar patterns in fracture risk reduction were observed at 5 years for nonvertebral fracture (RR, 0.67; 95% CI, 0.52-0.82), nonhip nonvertebral fracture (RR, 0.69; 95% CI, 0.50-0.88), and major osteoporotic fracture (RR, 0.74; 95% CI, 0.59-0.89).
During the Q&A session after the talk, one audience member commented that the study was limited because the researchers only followed patients who received zoledronic acid for 60 days, which could have missed potential long-term benefits of the drug, especially since bisphosphonates have a lengthy skeletal retention time. Dr. Curtis acknowledged the point but said, “Usually, that’s not something we do, but these are different enough mechanisms of action that it may be warranted at least as a sensitivity analysis,” he said.
The study and its methodology were impressive, according to Yumie Rhee, MD, who comoderated the session where the study was presented. “I think they did a really good job by doing the negative control analysis. We’re not going to have a head-to-head clinical trial, so we don’t know the real fracture reduction differences [between denosumab and zoledronic acid]. [The NCO analysis] is more than the propensity matching score that we do usually,” said Dr. Rhee, who is a professor of endocrinology at Yonsei University College of Medicine in Seoul, South Korea.
In particular, the study showed a significantly greater reduction in hip fractures with denosumab. “Even in the RCTs, it was really hard to see the reduction in hip fracture, so I think this is showing much stronger data for denosumab. Especially in patients who have more [general fracture] risk and patients with higher hip fracture risk, I would go with denosumab,” Dr. Rhee said.
Her comoderator, Maria Zanchetta, MD, agreed. “It can have clinical implication, because we think denosumab is better than [zoledronic acid] for higher-risk patients, but we didn’t have the evidence. So at least we have a new [study] to look at, and I think it’s very important for our practice,” said Dr. Zanchetta, who is a professor of osteology at the Institute of Diagnostics and Metabolic Research, Universidad del Salvador, Buenos Aires.
The study was funded by Amgen, which markets denosumab. Dr. Curtis has consulted for Amgen. Dr. Rhee and Dr. Zanchetta report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ASBMR 2023
Lack of time is damaging women’s health
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Various speakers at the VII National Conference of the Onda Foundation, Italy’s National Observatory for Women and Gender’s Health, focused on this topic. The conference was dedicated to the social factors that determine health within the context of gender medicine.
In our society, housework and raising a family are responsibilities placed predominantly on the shoulders of women. These responsibilities contribute significantly to women’s daily workload. The most overburdened women are working mothers (according to ISTAT, Italy’s Office for National Statistics, 2019), who are forced to combine their professional responsibilities with family life, dedicating 8 hours and 20 minutes per day to paid and unpaid work overall, compared with the 7 hours and 29 minutes spent by working fathers. Working mothers between ages 25 and 44 years have on average 2 hours and 35 minutes of free time per day.
Stress and sleep deprivation
“Under these conditions, the risk of chronic stress is raised, and stress leads to depression. The rate of depression in the female population is double that of the male population,” said Claudio Mencacci, MD, chair of the Italian Society of Neuropsychopharmacology and the Onda Foundation. “What’s more, stress increases the risk of cardiovascular and metabolic diseases, asthma, arthritis, and autoimmune diseases.”
The one thing that is especially damaging to physical and mental health is sleep deprivation, and working mothers get less sleep than do working fathers. “This is partially due to biological factors: hormonal changes that take place toward the end of adolescence in women during the premenstrual period are responsible for an increased rate of sleep disturbance and insomnia,” said Dr. Mencacci. “During pregnancy and the postpartum period, female sex hormones make sleep lighter, reducing time spent in the REM sleep stage. Then there’s the social aspect that plays a decisive role: by and large, it’s mothers who take care of the youngest children at night.”
According to a 2019 German study, during the first 6 years of life of the first child, a mother loses on average 44 minutes sleep per night, compared with the average time spent sleeping before pregnancy; a father loses 14 minutes.
“Another aspect to bear in mind is that, for cultural reasons, women tend to overlook the issue and not seek help, deeming sleep deprivation normal,” said Dr. Mencacci.
Caregivers at greatest risk
The negative effects of stress are evident in people continuously caring for a dependent older or disabled family member, so-called caregivers. This is, “A group predominantly made up of women aged between 45 and 55 years,” said Marina Petrini, PhD, of the Italian Health Institute’s Gender Medicine Center of Excellence. Dr. Petrini coordinated a study on stress and health in family caregivers.
“The results obtained reveal a high level of stress, especially among female caregivers, who are more exposed to the risk of severe symptoms of depression, physical disorders, especially those affecting the nervous and immune systems, and who tend to adopt irregular eating patterns and sedentary habits,” said Dr. Petrini.
Limited treatment access
Another study presented at the Onda Foundation’s conference, which shows just how much a lack of “me time” can damage your health, is the Access to Diagnostic Medicine and Treatment by Region: the Patient’s Perspective Survey, conducted by market research agency Elma Research on a sample of cancer patients requiring specialist treatment.
“Forty percent of them had to move to a different region from the one they live in to get the care they needed,” said Massimo Massagrande, CEO of Elma Research. “Of that group, 40% had to move to an area not neighboring their own. The impact of area of residence is heavy, in terms of money and logistics – so much so that a large proportion of patients interviewed were forced to turn their back on the best available treatments. For women responding to our survey, the biggest obstacle is the impossibility of reconciling the effects of a move or the prospective of a temporary transfer to another region with their responsibilities for looking after their family.”
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Metabolic effects of estetrol are promising in postmenopausal women
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
PHILADELPHIA – presented at the annual meeting of the Menopause Society (formerly The North American Menopause Society).
Participants taking estetrol experienced a decrease in hemoglobin A1c, fasting plasma glucose, total cholesterol, LDL and lipoprotein as well as an increase in HDL cholesterol, according to the findings presented by Wolf Utian, MD, PhD, DSC, a professor emeritus of reproductive biology at Case Western Reserve University, Cleveland, and medical director emeritus of the Menopause Society.
A separate poster at the conference from the same trial also reported significant improvements from estetrol in quality of life, including that related to vasomotor symptoms, and several psychosocial and sexual functioning areas.
E4 is already available as combination oral contraception and is now being considered for treating vasomotor symptoms, explained Chrisandra Shufelt, MD, professor and chair of general internal of medicine and associate director of the Women’s Health Research Center at Mayo Clinic Florida, who was not involved in the study.
Background on estetrol
E4 is a human fetal liver estrogen produced during pregnancy that’s synthesized from plants for pharmaceutical use, including as the oral contraceptive drospirenone, Dr. Utian told attendees. It’s classified as a native estrogen with selective tissue activity (NEST), he said.
“E4 is a completely different native estrogen with oral administration mimicking the benefits of transdermals and hence safe and effective,” Dr. Utian said in an interview. “It would be a significant new addition to the pharmaceutical armamentarium.”
Two phase 3 trials presented by Dr. Utian at the same conference last year found estetrol reduced the frequency and severity of moderate to severe vasomotor symptoms, and a previous phase 2 trial finding vasomotor and genitourinary symptom benefits suggested it had potential benefits for lipids, carbohydrate metabolism, and bone turnover.
“In summary, E4 at a daily dose of 15 mg exhibited estrogenic effects in the vagina, leading to improved vaginal health and reduced signs of atrophy, emerging as a promising treatment option not only for vasomotor symptoms but also for other significant menopausal symptoms,” Dr. Utian said. “E4 could offer comprehensive relief for women experiencing a range of menopause-related discomforts.”
Dr. Utian also referenced a 2017 trial in which estetrol positively impacted lipid profiles, “lowering low-density lipoprotein cholesterol, increasing high-density lipoprotein cholesterol, and showing minimal influence on triglycerides,” he said. “Importantly, estetrol was associated with a significant decrease in osteocalcin levels in the higher dose groups, suggesting a potential preventive effect on bone loss,” he added. A recent review of the overall evidence on estetrol suggests its use is “promising,” Dr. Utian noted.
Current trial
His current randomized controlled phase 3 trial included postmenopausal women ages 40-65 from 151 sites in 14 countries in Europe, Latin America, and North America, and Russia. Among the 640 participants in the trial, 213 women randomly received 15 mg of estetrol, 213 women received 20 mg of estetrol, and 214 women received a placebo every day for 3 months. All women without hysterectomies also received 200 mg of progesterone once daily for two weeks after completing the estetrol treatment to protect the endometrium.
Researchers took blood samples from the participants at baseline and week 12 to assess total cholesterol, LDL, HDL, the total cholesterol/HDL ratio, triglycerides, lipoprotein A, fasting plasma glucose, insulin, and A1c.
Compared with women in the placebo group, women in both the 15 mg and 20 mg groups saw a statistically significant decrease in lipoprotein A and in the ratio of total cholesterol to HDL, and a statistically significant increase in HDL. Only the women in the 15 mg group saw a statistically significant decrease in LDL and increase in triglycerides; an increase in triglycerides in the 20 mg group did not reach statistical significance.
Statistically significant decreases in fasting plasma glucose and A1c also occurred in both treatment groups, but a decrease in insulin levels and in the homeostasis model-assessment-estimated insulin resistance (HOMA-IR) seen in both treatment arms did not reach significance.
“While the mean changes after 12 weeks from baseline overall were small changes to the cholesterol and blood sugar profiles, they are clinically meaningful because it suggests that E4 does not have any adverse effects to these measures,” Dr. Shufelt said in an interview. “An advantage is that this gives us another hormone option for vasomotor symptoms since it is a native estrogen with selective tissue.”
It’s too early, however, to determine whether estetrol offers benefits in terms of its safety profile, compared with currently available therapies, Dr. Shufelt said.
”These findings of E4 are similar to how oral estradiol changes lipids, which finds an increase in high-density lipoprotein cholesterol, and decreases plasma concentrations of total and low-density lipoprotein cholesterol. an increase in HDL-C and triglycerides and decrease in LDL-C,” she said.
Poster findings also promising
For the findings reported in the poster, researchers assessed quality of life and the clinical meaningfulness of vasomotor symptoms’ reduction at baseline and 12 weeks using the Menopause-Specific Quality of Life (MENQOL) questionnaire and the Clinical Global Impression questionnaire, respectively. They also assessed women’s self-reported genitourinary symptoms, including vaginal dryness, pain during urination, vaginal pain and bleeding related to sex, and vaginal or vulvar irritation or itching. Most of these findings primarily confirmed previous positive effects from E4 in other trials.
Women in both the 15 mg and 20 mg estetrol groups reported a statistically significant improvement at 12 weeks, compared with placebo, in their total MENQOL score and in the vasomotor, psychosocial, and sexual functioning domain scores (P < .05). Those in the 20 mg group also had a statistically significant improvement in their physical domain score (P < .05).
Although numerical improvements in genitourinary symptoms occurred at 12 weeks across all three groups, the only statistically significant difference from baseline occurred in patients taking 15 mg of estetrol, who experienced a decrease in vaginal dryness and vaginal pain during sex (P = .0142 and P = .003, respectively).
The Clinical Global Impression questionnaire asked women at 4 and 12 weeks to rate on a seven-item Likert scale their response to this question: “Rate the total improvement, whether or not in your judgment it is due entirely to drug treatment. Compared to your condition at admission to the study, how much has it changed?” Responses of “very much improved” and “much improved” counted as a clinically meaningful difference.
Compared with 27.9% of patients in the placebo group, 52.9% of patients in the 15 mg group and 59.8% of patients in the 20 mg group rated the weekly frequency of moderate to severe vasomotor symptoms as “much improved” or “very much improved” at 4 weeks (P < .0001). At 12 weeks, those numbers rose to 47% in the placebo group, 73.3% in the 15 mg group and 77.8% in the 20 mg group (P < .0001).
The trial’s primary limitation at this point is having only a 12-week follow-up, Dr. Shufelt said, though a few other questions remain.
“Because the two phase 3 RCTs included hysterectomized and nonhysterectomized women, it was unclear how many women in the study had E4 alone versus E4 with progesterone, as that might play a role in both cholesterol and carbohydrate metabolism,” Dr. Shufelt said. “While baseline data was not presented, it would also be important to know baseline values for the women and confirm that none were on lipid-lowering medications.”
The research was funded by Estetra SRL, an affiliate of Mithra Pharmaceuticals. Dr. Utian is a member of the Mithra and Elektra Scientific Advisory Boards. Dr. Shufelt has no disclosures.
AT NAMS 2023
Biomarkers may help women with RA to decide on medications in pregnancy
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
FROM ARTHRITIS RESEARCH & THERAPY