User login
Researchers examine learning curve for gender-affirming vaginoplasty
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
FROM SGS 2020
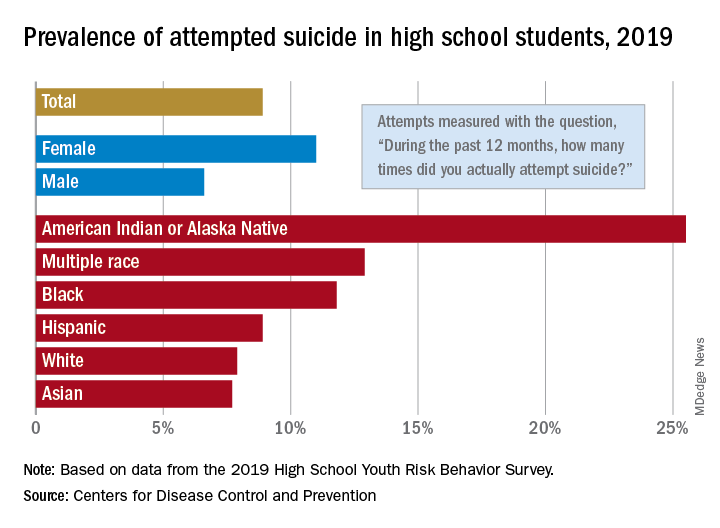
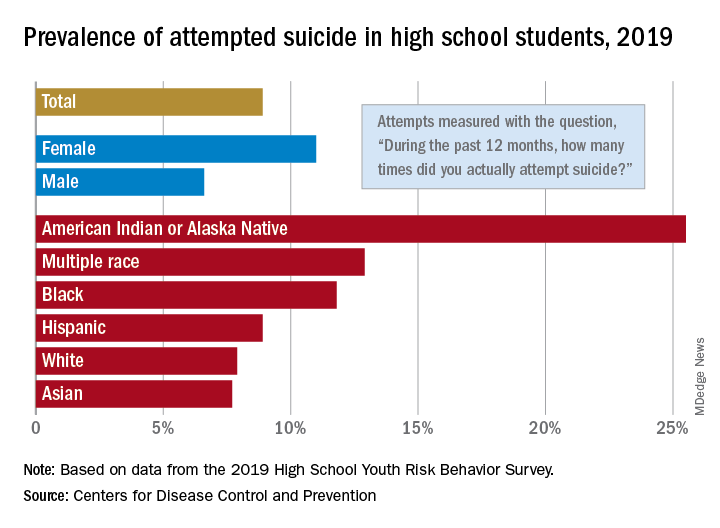
Attempted suicide in high school America, 2019
according to newly released data from the 2019 Youth Risk Behavior Survey.
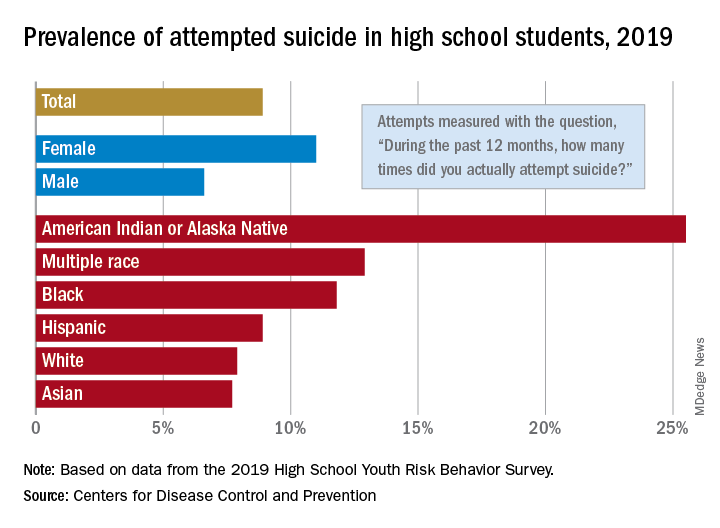
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
Back to school: How pediatricians can help LGBTQ youth
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at [email protected].
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at [email protected].
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at [email protected].
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
AAP releases new policy statement on barrier protection for teens
For adolescent patients, routinely take a sexual history, discuss the use of barrier methods, and perform relevant examinations, screenings, and vaccinations, according to a new policy statement on barrier protection use from the American Academy of Pediatrics’ Committee on Adolescence.
The policy statement has been expanded to cover multiple types of sexual activity and methods of barrier protection. These include not only traditional condoms, but also internal condoms (available in the United States only by prescription) and dental dams (for use during oral sex) or a latex sheet. “Pediatricians and other clinicians are encouraged to provide barrier methods within their offices and support availability within their communities,” said Laura K. Grubb, MD, MPH, of Tufts Medical Center in Boston, who authored both the policy statement and the technical report.
Counsel adolescents that abstaining from sexual intercourse is the best way to prevent genital sexually transmitted infections (STIs), HIV infection, and unplanned pregnancy. Also encourage and support consistent, correct barrier method use – in addition to other reliable contraception, if patients are sexually active or are thinking about becoming sexually active – the policy statement notes. Emphasize that all partners share responsibility to prevent STIs and unplanned pregnancies. “Adolescents with intellectual and physical disabilities are an overlooked group when it comes to sexual behavior, but they have similar rates of sexual behaviors when compared with their peers without disabilities,” Dr. Grubb and colleagues emphasized in the policy statement.
This is key because Centers for Disease Control and Prevention 2017 data showed that in the United States, “456,000 adolescent and young women younger than 20 years became pregnant; 448,000 of those pregnancies were among 15- to 19-year-olds, and 7,400 were among those 14 years of age and younger,” according to the technical report accompanying the policy statement. Also, “new cases of STIs increased 31% in the United States from 2013 to 2017, with half of the 2.3 million new STIs reported each year among young people 15 to 24 years of age.”
Parents may need support and encouragement to talk with their children about sex, sexuality, and the use of barrier methods to prevent STIs. Dr. Grubb and colleagues recommend via the policy statement: “Actively communicate to parents and communities that making barrier methods available to adolescents does not increase the onset or frequency of adolescent sexual activity, and that use of barrier methods can help decrease rates of unintended pregnancy and acquisition of STIs.”
Use Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Fourth Edition, for guidance on supporting parents and adolescents in promoting healthy sexual development and sexuality, including discussions of barrier methods.
Some groups of adolescents may use barrier methods less consistently because they perceive themselves to be lower risk. These include adolescents who use preexposure prophylaxis or nonbarrier contraception, who identify as bisexual or lesbian, or who are in established relationships. Monitor these patients to assess their risk and need for additional counseling. In the technical report, studies are cited finding that barrier methods are used less consistently during oral sex and that condom use is lower among cisgender and transgender females, and among adolescents who self-identify as gay, lesbian, or bisexual, compared with other groups.
In the policy statement, Dr. Grubb and colleagues call on pediatricians to advocate for more research and better access to barrier methods, especially for higher-risk adolescents and those living in underserved areas. In particular, school education programs on barrier methods can reach large adolescent groups and provide a “comprehensive array of educational and health care resources.”
Katie Brigham, MD, a pediatrician at MassGeneral Hospital for Children in Boston, affirmed the recommendations in the new policy statement (which she did not help write or research). “Even though the pregnancy rate is dropping in the United States, STI rates are increasing, so it is vital that pediatricians and other providers of adolescents and young adults counsel all their patients, regardless of gender and sexual orientation, of the importance of barrier methods when having oral, vaginal, or anal sex,” she said in an interview.
Dr. Brigham praised the technical report, adding that she found no major weaknesses in its methodology. “For future research, it would be interesting to see if there are different rates of pregnancy and STIs in pediatric practices that provide condoms and other barrier methods free to their patients, compared to those that do not.”
No external funding sources were reported. Dr. Grubb and Dr. Brigham reported having no relevant financial disclosures.
SOURCE: Grubb LK et al. Pediatrics. 2020 Jul 20. doi: 10.1542/peds.2020-007237.
For adolescent patients, routinely take a sexual history, discuss the use of barrier methods, and perform relevant examinations, screenings, and vaccinations, according to a new policy statement on barrier protection use from the American Academy of Pediatrics’ Committee on Adolescence.
The policy statement has been expanded to cover multiple types of sexual activity and methods of barrier protection. These include not only traditional condoms, but also internal condoms (available in the United States only by prescription) and dental dams (for use during oral sex) or a latex sheet. “Pediatricians and other clinicians are encouraged to provide barrier methods within their offices and support availability within their communities,” said Laura K. Grubb, MD, MPH, of Tufts Medical Center in Boston, who authored both the policy statement and the technical report.
Counsel adolescents that abstaining from sexual intercourse is the best way to prevent genital sexually transmitted infections (STIs), HIV infection, and unplanned pregnancy. Also encourage and support consistent, correct barrier method use – in addition to other reliable contraception, if patients are sexually active or are thinking about becoming sexually active – the policy statement notes. Emphasize that all partners share responsibility to prevent STIs and unplanned pregnancies. “Adolescents with intellectual and physical disabilities are an overlooked group when it comes to sexual behavior, but they have similar rates of sexual behaviors when compared with their peers without disabilities,” Dr. Grubb and colleagues emphasized in the policy statement.
This is key because Centers for Disease Control and Prevention 2017 data showed that in the United States, “456,000 adolescent and young women younger than 20 years became pregnant; 448,000 of those pregnancies were among 15- to 19-year-olds, and 7,400 were among those 14 years of age and younger,” according to the technical report accompanying the policy statement. Also, “new cases of STIs increased 31% in the United States from 2013 to 2017, with half of the 2.3 million new STIs reported each year among young people 15 to 24 years of age.”
Parents may need support and encouragement to talk with their children about sex, sexuality, and the use of barrier methods to prevent STIs. Dr. Grubb and colleagues recommend via the policy statement: “Actively communicate to parents and communities that making barrier methods available to adolescents does not increase the onset or frequency of adolescent sexual activity, and that use of barrier methods can help decrease rates of unintended pregnancy and acquisition of STIs.”
Use Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Fourth Edition, for guidance on supporting parents and adolescents in promoting healthy sexual development and sexuality, including discussions of barrier methods.
Some groups of adolescents may use barrier methods less consistently because they perceive themselves to be lower risk. These include adolescents who use preexposure prophylaxis or nonbarrier contraception, who identify as bisexual or lesbian, or who are in established relationships. Monitor these patients to assess their risk and need for additional counseling. In the technical report, studies are cited finding that barrier methods are used less consistently during oral sex and that condom use is lower among cisgender and transgender females, and among adolescents who self-identify as gay, lesbian, or bisexual, compared with other groups.
In the policy statement, Dr. Grubb and colleagues call on pediatricians to advocate for more research and better access to barrier methods, especially for higher-risk adolescents and those living in underserved areas. In particular, school education programs on barrier methods can reach large adolescent groups and provide a “comprehensive array of educational and health care resources.”
Katie Brigham, MD, a pediatrician at MassGeneral Hospital for Children in Boston, affirmed the recommendations in the new policy statement (which she did not help write or research). “Even though the pregnancy rate is dropping in the United States, STI rates are increasing, so it is vital that pediatricians and other providers of adolescents and young adults counsel all their patients, regardless of gender and sexual orientation, of the importance of barrier methods when having oral, vaginal, or anal sex,” she said in an interview.
Dr. Brigham praised the technical report, adding that she found no major weaknesses in its methodology. “For future research, it would be interesting to see if there are different rates of pregnancy and STIs in pediatric practices that provide condoms and other barrier methods free to their patients, compared to those that do not.”
No external funding sources were reported. Dr. Grubb and Dr. Brigham reported having no relevant financial disclosures.
SOURCE: Grubb LK et al. Pediatrics. 2020 Jul 20. doi: 10.1542/peds.2020-007237.
For adolescent patients, routinely take a sexual history, discuss the use of barrier methods, and perform relevant examinations, screenings, and vaccinations, according to a new policy statement on barrier protection use from the American Academy of Pediatrics’ Committee on Adolescence.
The policy statement has been expanded to cover multiple types of sexual activity and methods of barrier protection. These include not only traditional condoms, but also internal condoms (available in the United States only by prescription) and dental dams (for use during oral sex) or a latex sheet. “Pediatricians and other clinicians are encouraged to provide barrier methods within their offices and support availability within their communities,” said Laura K. Grubb, MD, MPH, of Tufts Medical Center in Boston, who authored both the policy statement and the technical report.
Counsel adolescents that abstaining from sexual intercourse is the best way to prevent genital sexually transmitted infections (STIs), HIV infection, and unplanned pregnancy. Also encourage and support consistent, correct barrier method use – in addition to other reliable contraception, if patients are sexually active or are thinking about becoming sexually active – the policy statement notes. Emphasize that all partners share responsibility to prevent STIs and unplanned pregnancies. “Adolescents with intellectual and physical disabilities are an overlooked group when it comes to sexual behavior, but they have similar rates of sexual behaviors when compared with their peers without disabilities,” Dr. Grubb and colleagues emphasized in the policy statement.
This is key because Centers for Disease Control and Prevention 2017 data showed that in the United States, “456,000 adolescent and young women younger than 20 years became pregnant; 448,000 of those pregnancies were among 15- to 19-year-olds, and 7,400 were among those 14 years of age and younger,” according to the technical report accompanying the policy statement. Also, “new cases of STIs increased 31% in the United States from 2013 to 2017, with half of the 2.3 million new STIs reported each year among young people 15 to 24 years of age.”
Parents may need support and encouragement to talk with their children about sex, sexuality, and the use of barrier methods to prevent STIs. Dr. Grubb and colleagues recommend via the policy statement: “Actively communicate to parents and communities that making barrier methods available to adolescents does not increase the onset or frequency of adolescent sexual activity, and that use of barrier methods can help decrease rates of unintended pregnancy and acquisition of STIs.”
Use Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Fourth Edition, for guidance on supporting parents and adolescents in promoting healthy sexual development and sexuality, including discussions of barrier methods.
Some groups of adolescents may use barrier methods less consistently because they perceive themselves to be lower risk. These include adolescents who use preexposure prophylaxis or nonbarrier contraception, who identify as bisexual or lesbian, or who are in established relationships. Monitor these patients to assess their risk and need for additional counseling. In the technical report, studies are cited finding that barrier methods are used less consistently during oral sex and that condom use is lower among cisgender and transgender females, and among adolescents who self-identify as gay, lesbian, or bisexual, compared with other groups.
In the policy statement, Dr. Grubb and colleagues call on pediatricians to advocate for more research and better access to barrier methods, especially for higher-risk adolescents and those living in underserved areas. In particular, school education programs on barrier methods can reach large adolescent groups and provide a “comprehensive array of educational and health care resources.”
Katie Brigham, MD, a pediatrician at MassGeneral Hospital for Children in Boston, affirmed the recommendations in the new policy statement (which she did not help write or research). “Even though the pregnancy rate is dropping in the United States, STI rates are increasing, so it is vital that pediatricians and other providers of adolescents and young adults counsel all their patients, regardless of gender and sexual orientation, of the importance of barrier methods when having oral, vaginal, or anal sex,” she said in an interview.
Dr. Brigham praised the technical report, adding that she found no major weaknesses in its methodology. “For future research, it would be interesting to see if there are different rates of pregnancy and STIs in pediatric practices that provide condoms and other barrier methods free to their patients, compared to those that do not.”
No external funding sources were reported. Dr. Grubb and Dr. Brigham reported having no relevant financial disclosures.
SOURCE: Grubb LK et al. Pediatrics. 2020 Jul 20. doi: 10.1542/peds.2020-007237.
FROM PEDIATRICS
Ignored by doctors, transgender people turn to DIY treatments
For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

Suicide often associated with bullying in LGBTQ youth
based on analysis of a national database.
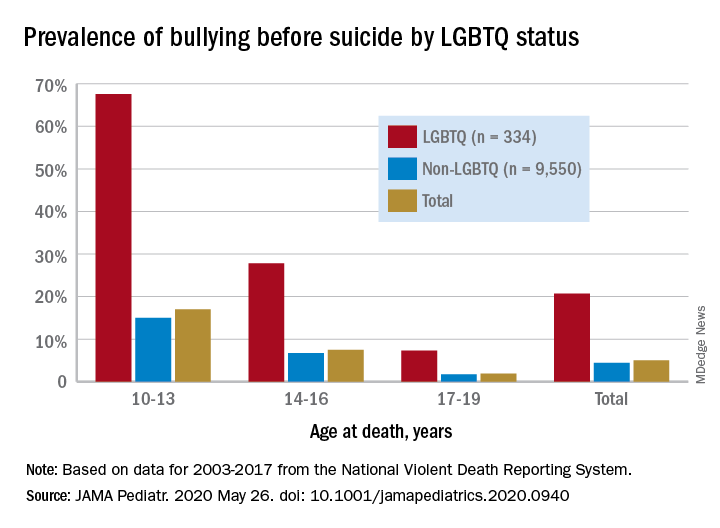
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.
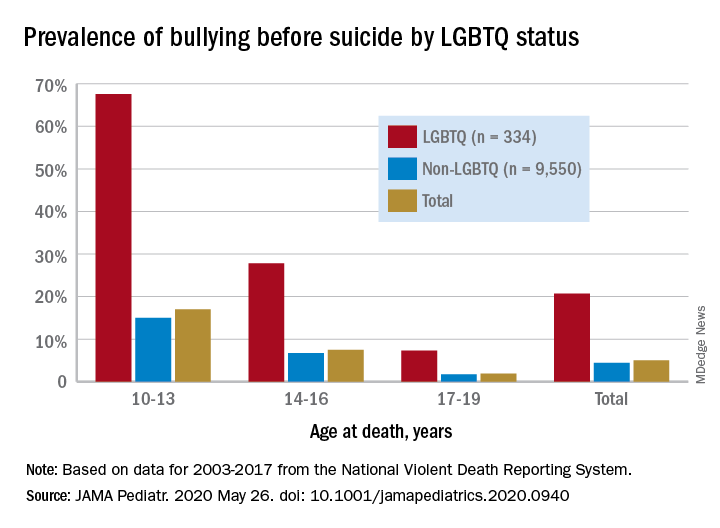
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.
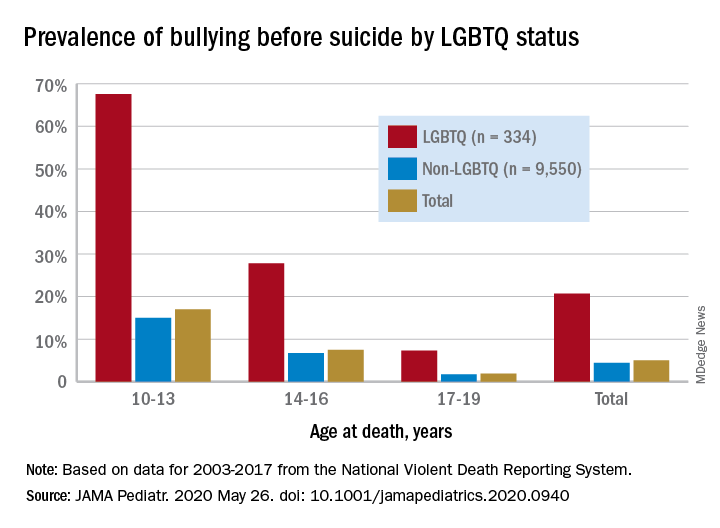
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
FROM JAMA PEDIATRICS
Hormone therapy boosts body image in transgender youth
based on data from 148 individuals.
“Understanding the impact of gender-affirming hormone therapy on the mental health of transgender youth is critical given the health disparities documented in this population,” wrote Laura E. Kuper, PhD, of Children’s Health Systems of Texas, Dallas, and colleagues.
In a study published in Pediatrics, the researchers reviewed data from 148 youth aged 9-18 years who underwent gender-affirming hormone therapy in a multidisciplinary program. The average age of the patients was 15 years; 25 were receiving puberty suppression hormones only, 93 were receiving just feminizing or masculinizing hormones, and 30 were receiving both treatments.
At baseline and at approximately 1 year follow-up, all patients completed the Body Image Scale, Quick Inventory of Depressive Symptoms, and Screen for Child Anxiety Related Emotional Disorders. In addition, clinicians collected information on patients’ suicidal ideation, suicide attempts, and nonsuicidal self-injury.
Overall, the average scores on the Body Image Scale on body dissatisfaction decreased from 70 to 52, and average scores on the Quick Inventory of Depressive Symptoms decreased from 9 to 7; both were statistically significant (P less than .001), as were changes from baseline on the anxiety subscale of the Screen for Child Anxiety Related Emotional Disorders, which decreased from 32 to 29 (P less than .01). No change occurred in the average overall clinician-reported depressive symptoms.
During the follow-up period, the rates of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 38%, 5%, and 17%, respectively. Of patients who reported these experiences, the lifetime histories of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 81%, 15%, and 52%, respectively.
The findings were limited by several factors including some missing data and the relatively small sample size, the researchers noted.
Nonetheless, the results suggest “that youth receiving gender-affirming hormone therapy experience meaningful short-term improvements in body dissatisfaction, and no participants discontinued feminizing or masculinizing hormone therapy.” These results support the use of such therapy, Dr. Kuper and associates wrote.
The study is important because of the need for evidence that hormones actually improve patient outcomes, said Shauna M. Lawlis, MD, of the University of Oklahoma Medical Center, Oklahoma City.
“Especially given the rash of legislation across the country aimed at blocking care for transgender youth, it is helpful to show that these treatments really do decrease patients’ anxiety and depressive symptoms,” she said in an interview. “In addition, previous research has been focused on those who have undergone puberty suppression followed by gender-affirming hormone therapy, but many patients are too far along in puberty for puberty suppression to be effective and providers often go straight to gender-affirming hormones in those cases.”
Dr. Lawlis said she was not at all surprised by the study findings. “In my own practice, I have seen patients improve greatly on gender-affirming hormones with overall improvement in anxiety and depression. As a patient’s outward appearance more closely matches their gender identity, they feel more comfortable in their own bodies and their interactions with the world around them, thus improving these symptoms.”
Dr. Lawlis added that the message for pediatricians who treat transgender youth is simple: Gender-affirming hormones improve patient outcomes. “They are essential for the mental health of this vulnerable population.”
She noted that long-term follow-up studies would be useful. “There is still a lot of concern about regret and detransitioning among health care providers and the general population – showing that patients maintain satisfaction in the long-term would be helpful.
“In addition, long-term studies about other health outcomes (cardiovascular disease, cancer risk, etc.) would also be helpful,” said Dr. Lawlis, who was asked to comment on this study, with which she had no involvement.
The study was supported in part by Children’s Health. The researchers had no financial conflicts to disclose. Dr. Lawlis had no relevant financial disclosures.
SOURCE: Kuper LE et al. Pediatrics. 2020 Mar 27. doi: 10.1542/peds.2019-3006.
based on data from 148 individuals.
“Understanding the impact of gender-affirming hormone therapy on the mental health of transgender youth is critical given the health disparities documented in this population,” wrote Laura E. Kuper, PhD, of Children’s Health Systems of Texas, Dallas, and colleagues.
In a study published in Pediatrics, the researchers reviewed data from 148 youth aged 9-18 years who underwent gender-affirming hormone therapy in a multidisciplinary program. The average age of the patients was 15 years; 25 were receiving puberty suppression hormones only, 93 were receiving just feminizing or masculinizing hormones, and 30 were receiving both treatments.
At baseline and at approximately 1 year follow-up, all patients completed the Body Image Scale, Quick Inventory of Depressive Symptoms, and Screen for Child Anxiety Related Emotional Disorders. In addition, clinicians collected information on patients’ suicidal ideation, suicide attempts, and nonsuicidal self-injury.
Overall, the average scores on the Body Image Scale on body dissatisfaction decreased from 70 to 52, and average scores on the Quick Inventory of Depressive Symptoms decreased from 9 to 7; both were statistically significant (P less than .001), as were changes from baseline on the anxiety subscale of the Screen for Child Anxiety Related Emotional Disorders, which decreased from 32 to 29 (P less than .01). No change occurred in the average overall clinician-reported depressive symptoms.
During the follow-up period, the rates of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 38%, 5%, and 17%, respectively. Of patients who reported these experiences, the lifetime histories of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 81%, 15%, and 52%, respectively.
The findings were limited by several factors including some missing data and the relatively small sample size, the researchers noted.
Nonetheless, the results suggest “that youth receiving gender-affirming hormone therapy experience meaningful short-term improvements in body dissatisfaction, and no participants discontinued feminizing or masculinizing hormone therapy.” These results support the use of such therapy, Dr. Kuper and associates wrote.
The study is important because of the need for evidence that hormones actually improve patient outcomes, said Shauna M. Lawlis, MD, of the University of Oklahoma Medical Center, Oklahoma City.
“Especially given the rash of legislation across the country aimed at blocking care for transgender youth, it is helpful to show that these treatments really do decrease patients’ anxiety and depressive symptoms,” she said in an interview. “In addition, previous research has been focused on those who have undergone puberty suppression followed by gender-affirming hormone therapy, but many patients are too far along in puberty for puberty suppression to be effective and providers often go straight to gender-affirming hormones in those cases.”
Dr. Lawlis said she was not at all surprised by the study findings. “In my own practice, I have seen patients improve greatly on gender-affirming hormones with overall improvement in anxiety and depression. As a patient’s outward appearance more closely matches their gender identity, they feel more comfortable in their own bodies and their interactions with the world around them, thus improving these symptoms.”
Dr. Lawlis added that the message for pediatricians who treat transgender youth is simple: Gender-affirming hormones improve patient outcomes. “They are essential for the mental health of this vulnerable population.”
She noted that long-term follow-up studies would be useful. “There is still a lot of concern about regret and detransitioning among health care providers and the general population – showing that patients maintain satisfaction in the long-term would be helpful.
“In addition, long-term studies about other health outcomes (cardiovascular disease, cancer risk, etc.) would also be helpful,” said Dr. Lawlis, who was asked to comment on this study, with which she had no involvement.
The study was supported in part by Children’s Health. The researchers had no financial conflicts to disclose. Dr. Lawlis had no relevant financial disclosures.
SOURCE: Kuper LE et al. Pediatrics. 2020 Mar 27. doi: 10.1542/peds.2019-3006.
based on data from 148 individuals.
“Understanding the impact of gender-affirming hormone therapy on the mental health of transgender youth is critical given the health disparities documented in this population,” wrote Laura E. Kuper, PhD, of Children’s Health Systems of Texas, Dallas, and colleagues.
In a study published in Pediatrics, the researchers reviewed data from 148 youth aged 9-18 years who underwent gender-affirming hormone therapy in a multidisciplinary program. The average age of the patients was 15 years; 25 were receiving puberty suppression hormones only, 93 were receiving just feminizing or masculinizing hormones, and 30 were receiving both treatments.
At baseline and at approximately 1 year follow-up, all patients completed the Body Image Scale, Quick Inventory of Depressive Symptoms, and Screen for Child Anxiety Related Emotional Disorders. In addition, clinicians collected information on patients’ suicidal ideation, suicide attempts, and nonsuicidal self-injury.
Overall, the average scores on the Body Image Scale on body dissatisfaction decreased from 70 to 52, and average scores on the Quick Inventory of Depressive Symptoms decreased from 9 to 7; both were statistically significant (P less than .001), as were changes from baseline on the anxiety subscale of the Screen for Child Anxiety Related Emotional Disorders, which decreased from 32 to 29 (P less than .01). No change occurred in the average overall clinician-reported depressive symptoms.
During the follow-up period, the rates of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 38%, 5%, and 17%, respectively. Of patients who reported these experiences, the lifetime histories of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 81%, 15%, and 52%, respectively.
The findings were limited by several factors including some missing data and the relatively small sample size, the researchers noted.
Nonetheless, the results suggest “that youth receiving gender-affirming hormone therapy experience meaningful short-term improvements in body dissatisfaction, and no participants discontinued feminizing or masculinizing hormone therapy.” These results support the use of such therapy, Dr. Kuper and associates wrote.
The study is important because of the need for evidence that hormones actually improve patient outcomes, said Shauna M. Lawlis, MD, of the University of Oklahoma Medical Center, Oklahoma City.
“Especially given the rash of legislation across the country aimed at blocking care for transgender youth, it is helpful to show that these treatments really do decrease patients’ anxiety and depressive symptoms,” she said in an interview. “In addition, previous research has been focused on those who have undergone puberty suppression followed by gender-affirming hormone therapy, but many patients are too far along in puberty for puberty suppression to be effective and providers often go straight to gender-affirming hormones in those cases.”
Dr. Lawlis said she was not at all surprised by the study findings. “In my own practice, I have seen patients improve greatly on gender-affirming hormones with overall improvement in anxiety and depression. As a patient’s outward appearance more closely matches their gender identity, they feel more comfortable in their own bodies and their interactions with the world around them, thus improving these symptoms.”
Dr. Lawlis added that the message for pediatricians who treat transgender youth is simple: Gender-affirming hormones improve patient outcomes. “They are essential for the mental health of this vulnerable population.”
She noted that long-term follow-up studies would be useful. “There is still a lot of concern about regret and detransitioning among health care providers and the general population – showing that patients maintain satisfaction in the long-term would be helpful.
“In addition, long-term studies about other health outcomes (cardiovascular disease, cancer risk, etc.) would also be helpful,” said Dr. Lawlis, who was asked to comment on this study, with which she had no involvement.
The study was supported in part by Children’s Health. The researchers had no financial conflicts to disclose. Dr. Lawlis had no relevant financial disclosures.
SOURCE: Kuper LE et al. Pediatrics. 2020 Mar 27. doi: 10.1542/peds.2019-3006.
FROM PEDIATRICS
Focus groups seek transgender experience with HIV prevention
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
FROM PEDIATRICS
Gender pronouns in EMR preferred by many gender nonconforming teens
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
FROM JAMA PEDIATRICS
Docs spurn state attempts to criminalize treatment of transgender kids
Many US endocrinologists are crying foul as a growing number of state lawmakers are attempting to enact legislation that would prohibit, and in some cases criminalize, medical treatment for minors with gender dysphoria.
As of press time, 13 states had introduced such bills, and legislators in two additional states said they were drafting bills. So far, one — in South Dakota — was defeated in a Senate committee, and another, in Florida, was essentially tabled without being enacted.
They all have a common goal of preventing minors from receiving puberty blockers, cross-sex hormones, or gender-affirmation surgery.
“These things are being proposed based on a lot of misinformation,” said Stephen Rosenthal, MD, professor of pediatrics at the University of California, San Francisco (UCSF), and a past president of the Pediatric Endocrine Society.
Lawmakers “are not looking at the scientific evidence that supports current clinical practice guidelines,” Rosenthal, who treats transgender children, told Medscape Medical News.
And “People just aren’t really understanding the harm that regulating this kind of medicine would do,” stressed Cassandra Brady, MD, assistant professor of pediatric endocrinology at Vanderbilt University School of Medicine, Memphis, Tennessee.
The bills come at a time when gender identity clinics for minors around the world have seen a significant uptick in cases. And, as widely reported by Medscape Medical News, some clinicians have begun to question whether treatment decisions are outpacing science.
Queries about use of puberty blockers and cross-sex hormones have embroiled the United Kingdom’s only publicly funded Gender Identity Development Service (GIDS) in controversy, for example, with five clinicians resigning last year over concerns about overuse of the treatments.
And earlier this month, the UK National Health Service (NHS) announced an independent review of services including the use of puberty blockers and cross-sex hormones in youth with gender dysphoria.
Meanwhile, the topic has ignited debate in Sweden, where a report from the Board of Health and Welfare confirmed a 1,500% rise between 2008 and 2018 in gender dysphoria diagnoses among 13- to 17-year-olds born as girls, as detailed by The Guardian.
Indeed, there is some indication of a so-called “rapid-onset gender dysphoria” in born females who say they wish to become males and some clinicians have said this represents a “social” phenomenon.
But guidelines from US clinical organizations – including the American Academy of Pediatrics issued in 2018, the Endocrine Society as reported by Medscape Medical News in 2017, and the US Professional Association for Transgender Health (USPATH) – all support the use of medical treatment in adolescents with gender dysphoria who have received mental health evaluations from appropriately trained professionals.
More data needed but evidence to intervene is compelling
Joshua Safer, MD, FACP, FACE, executive director of the Mount Sinai Center for Transgender Medicine and Surgery, New York City, says the data “even if it’s rudimentary, are convincing that there is a biological component to gender identity.”
Attempts to manipulate gender identity in people who are born intersex, for example, have uniformly failed, he noted.
Yet it’s still not known what causes gender identity – whether it might be a result of a cluster of genes or a bundle in the brain, or some other biological process – said Safer, who treats transgender adults, but not children, and is also a coauthor of the aforementioned Endocrine Society Clinical Practice Guideline on Endocrine Treatment of Gender Dysphoric/Gender Incongruent Persons.
This is an area for future research, he noted.
Nevertheless, “The data for interventions for transgender people ... is compelling,” he added, noting evidence for improved mental health morbidity among those gender-questioning people who have medical interventions.
“Those data are modest at this point and we need better data, but they do all move in the same direction,” he asserted.
Meanwhile, a large group of around 1,800 parents of transgender and nonbinary children have called on legislators to withdraw the proposals in an open letter organized by the Human Rights Campaign.
“We know better than anyone what our children need in order to thrive: access to best practice, evidence-based gender-affirming healthcare,” the parents write.
“These healthcare decisions must be made on a case-by-case basis, in careful consultation with a medical team, and with the goal of reducing the physical and emotional distress experienced by many transgender children,” they continue.
“They should not be made by politicians who think they know better than medical professionals,” they add.
The American Academy of Child and Adolescent Psychiatry has also condemned state efforts “to block access to these recognized interventions,” it said in a statement.
Proponents of laws speak of harms
Most of the state proposals portray medical interventions as harmful to minors.
Missouri’s proposed legislation labels surgical or hormonal treatment for a child under age 18 “abuse or neglect”; a physician or anyone who assists or provides for the child would be charged with a felony.
One of the first bills was introduced in South Dakota in January. House bill 1057 would have charged clinicians providing gender-affirming care in anyone under age 16 with a misdemeanor punishable by up to a year in prison and a $2,000 fine.
The bill was defeated in the Senate after the South Dakota State Medical Association and several other physicians, families, and adolescents testified against the proposal, according to the Argus Leader.
The Endocrine Society applauded the failure and noted in a statement that it “supports physicians’ ability to provide the best evidence-based treatment to their patients,” and that “these decisions should be made by the family and physician, and not dictated by policymakers.”
Jack Turban, MD, a resident physician in child and adolescent psychiatry at Massachusetts General Hospital, Boston, who conducted a pivotal study of some 26,000 transgender adults showing that early administration of puberty blockers led to lower odds of lifetime suicidal ideation, also expressed dismay over the bills in an opinion piece for the New York Times.
“The potential benefits of providing gender-affirmative care typically outweigh the minor risks associated with treatment,” wrote Turban.
“State legislators need to educate themselves about these young people and their medical care before introducing legislation that will hurt them,” he added.
Few states seem to have approached clinicians for feedback
In Tennessee, lawmakers have approached some clinicians at Vanderbilt and have appreciated the feedback they’ve received so far, said Brady.
But that may be an exception. It seems that few medical organizations have been consulted in the crafting of bills in the other states: Colorado, Florida, Idaho, Illinois, Kentucky, Mississippi, Missouri, New Hampshire, Oklahoma, South Carolina, South Dakota, and West Virginia. Lawmakers in Ohio and Utah also are drafting proposals.
Physicians could be charged with a felony in Florida, Idaho, Kentucky, Missouri, and reportedly, in the Ohio proposal under development.
The bills have been introduced at the behest of some conservative groups that doubt the existence of gender dysphoria or who have questions about treatment: the Eagle Forum, the Alliance Defending Freedom, and the Kelsey Coalition.
In a recent tweet clarifying its position on state efforts, the Kelsey Coalition said it “supports all bills that protect children, even those that may provide criminal penalties, because we believe these medical interventions should never be performed on children.”
“However, we do not support state bills that are not victim-led or used for political gain,” they added.
Existing knowledge imperfect but treatment indicated for some
The bills have also garnered support from some endocrinologists who have raised concerns about puberty blockers and other medical treatments for gender dysphoria.
One is Michael K. Laidlaw, MD, a Rocklin, California–based endocrinologist who has not treated transgender people but frequently writes about the subject, most recently calling the use of puberty blockers “a public health emergency.”
Laidlaw joined several other clinicians who do not treat transgender people in testifying in favor of the South Dakota bill.
Last year, as previously reported by Medscape Medical News, Laidlaw, along with others, criticized the Endocrine Society’s 2017 Clinical Practice Guideline on Treating Dysphoric/Gender-Incongruent Persons in a letter to the Journal of Clinical Endocrinology & Metabolism.
They stated that there is no lab, imaging, or other objective test to diagnose someone as transgender and that “the consequences of this gender-affirmative therapy are not trivial and include potential sterility, sexual dysfunction, thromboembolic and cardiovascular disease, and malignancy.”
Laidlaw told Medscape Medical News at the time that “If we’re talking about [transgender] adults [who have gone through puberty of their biological sex] and who can make a decision, if they have been truly notified of the risks and benefits [of cross-sex hormones] and have also had psychological evaluation, and they decide, ‘This is still the right course for me,’ then I don’t have any objection.”
But considering the use of cross-sex hormones in children and adolescents is “quite a different story,” he contended.
In May 2019, Rosenthal, Safer and colleagues responded to Laidlaw’s letter in the same journal, stating that for the right person, puberty blockers and cross-sex hormones are appropriate, and that medications can improve mental health outcomes.
“We agree that research to validate the safety and efficacy of all forms of treatment is desirable,” they wrote, noting some of that research is underway.
“However, we believe physicians would fall short in their duty of care if they withheld hormonal treatment of gender dysphoria/incongruence in pubertal youth, when indicated, given the existing state of knowledge, imperfect though it is.”
Research to validate safety and efficacy of transgender TX underway
Rosenthal’s center at UCSF is one of four in the United States that has been carrying out a National Institutes of Health-funded long-term observational study of the impact of early medical intervention on transgender adolescents.
It will take time to get those results, but in the meantime, clinicians should act on what is known now, said Rosenthal.
“We already have very compelling data to suggest that the benefits [of treatment] outweigh the potential harms,” he said.
Rosenthal told Medscape Medical News that Laidlaw has advanced the notion that clinicians who prescribe puberty blockers are forcing those individuals into a transgender outcome.
“We don’t push anybody down any path,” he said. “The guidelines make these treatments available in a very specific subset of people who are evaluated by skilled mental health professionals,” said Rosenthal.
Both he and Safer acknowledge that puberty blockers do have the potential for some harm. For instance, a frank discussion needs to happen about the likely lack of future fertility, said Rosenthal.
“Everything we do in medicine has a theoretical risk of harm,” noted Safer.
However, he said, to deny a puberty blocker to an individual approaching puberty who is distraught about growing breasts — but then to possibly have to surgically remove them later — is in itself doing harm.
“Puberty blockers are exactly the epitome of ‘do no harm’ in this case,” argued Safer.
The medications are reversible, he said, adding that they also give an individual and the family time to think through whether the adolescent is transgender, and, if yes, what they want to do in terms of taking cross-sex hormones in the future or getting other interventions.
Safer acknowledged that this doesn’t mean there aren’t still some concerns, however.
For instance, once puberty blockers — which have the potential to interfere with bone development — are started, “How much harm are you willing to risk? Maybe a couple of years is okay, but maybe 6 years is not,” he said.
“So, we do discuss how quickly...you have to get to your next decision point, whether it be to actually introduce hormones or not to introduce hormones,” he explained.
State proposals will have chilling effect on gender-questioning kids
Clinicians say that even if the proposals do not become law, just the fact of their existence could have a chilling effect on gender-questioning children, their families, and doctors considering whether to provide treatment.
“They’re already in a hard position,” Brady said of her patients.
“They’re coming here to seek something for a life that they’ve already not wanted to live and then we have people who are trying to put a real big block on that – I see that obviously affecting their mental health,” she observed.
“I can’t imagine how their lives would be without this care,” Brady said.
With the bills being out there, “two things can happen – one is, it can be very depressing and limiting, but it can also embolden people,” Rosenthal told Medscape Medical News.
“The people behind these things are the same people that have tried to stop our research at the National Institutes of Health (NIH),” he explained.
“These people are going to do everything they can, whether it’s to go state by state to try and exhaust us, or go to the NIH and try to get them to pull the plug on our research,” said Rosenthal.
Safer believes it’s ill-considered to try to legislate any aspect of medicine.
“The pitfalls of trying to legislate these things are myriad,” he said.
“Across all of medicine, interventions are very customized. Can you imagine a state legislature trying to legislate the optimal approach in medicines that can and cannot be given to people with diabetes? How crazy that would be,” he noted.
Rosenthal has served on an advisory panel for Endo Pharmaceuticals and is a grantee of the NIH. Safer has also served on an advisory panel for Endo Pharmaceuticals. Brady has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Many US endocrinologists are crying foul as a growing number of state lawmakers are attempting to enact legislation that would prohibit, and in some cases criminalize, medical treatment for minors with gender dysphoria.
As of press time, 13 states had introduced such bills, and legislators in two additional states said they were drafting bills. So far, one — in South Dakota — was defeated in a Senate committee, and another, in Florida, was essentially tabled without being enacted.
They all have a common goal of preventing minors from receiving puberty blockers, cross-sex hormones, or gender-affirmation surgery.
“These things are being proposed based on a lot of misinformation,” said Stephen Rosenthal, MD, professor of pediatrics at the University of California, San Francisco (UCSF), and a past president of the Pediatric Endocrine Society.
Lawmakers “are not looking at the scientific evidence that supports current clinical practice guidelines,” Rosenthal, who treats transgender children, told Medscape Medical News.
And “People just aren’t really understanding the harm that regulating this kind of medicine would do,” stressed Cassandra Brady, MD, assistant professor of pediatric endocrinology at Vanderbilt University School of Medicine, Memphis, Tennessee.
The bills come at a time when gender identity clinics for minors around the world have seen a significant uptick in cases. And, as widely reported by Medscape Medical News, some clinicians have begun to question whether treatment decisions are outpacing science.
Queries about use of puberty blockers and cross-sex hormones have embroiled the United Kingdom’s only publicly funded Gender Identity Development Service (GIDS) in controversy, for example, with five clinicians resigning last year over concerns about overuse of the treatments.
And earlier this month, the UK National Health Service (NHS) announced an independent review of services including the use of puberty blockers and cross-sex hormones in youth with gender dysphoria.
Meanwhile, the topic has ignited debate in Sweden, where a report from the Board of Health and Welfare confirmed a 1,500% rise between 2008 and 2018 in gender dysphoria diagnoses among 13- to 17-year-olds born as girls, as detailed by The Guardian.
Indeed, there is some indication of a so-called “rapid-onset gender dysphoria” in born females who say they wish to become males and some clinicians have said this represents a “social” phenomenon.
But guidelines from US clinical organizations – including the American Academy of Pediatrics issued in 2018, the Endocrine Society as reported by Medscape Medical News in 2017, and the US Professional Association for Transgender Health (USPATH) – all support the use of medical treatment in adolescents with gender dysphoria who have received mental health evaluations from appropriately trained professionals.
More data needed but evidence to intervene is compelling
Joshua Safer, MD, FACP, FACE, executive director of the Mount Sinai Center for Transgender Medicine and Surgery, New York City, says the data “even if it’s rudimentary, are convincing that there is a biological component to gender identity.”
Attempts to manipulate gender identity in people who are born intersex, for example, have uniformly failed, he noted.
Yet it’s still not known what causes gender identity – whether it might be a result of a cluster of genes or a bundle in the brain, or some other biological process – said Safer, who treats transgender adults, but not children, and is also a coauthor of the aforementioned Endocrine Society Clinical Practice Guideline on Endocrine Treatment of Gender Dysphoric/Gender Incongruent Persons.
This is an area for future research, he noted.
Nevertheless, “The data for interventions for transgender people ... is compelling,” he added, noting evidence for improved mental health morbidity among those gender-questioning people who have medical interventions.
“Those data are modest at this point and we need better data, but they do all move in the same direction,” he asserted.
Meanwhile, a large group of around 1,800 parents of transgender and nonbinary children have called on legislators to withdraw the proposals in an open letter organized by the Human Rights Campaign.
“We know better than anyone what our children need in order to thrive: access to best practice, evidence-based gender-affirming healthcare,” the parents write.
“These healthcare decisions must be made on a case-by-case basis, in careful consultation with a medical team, and with the goal of reducing the physical and emotional distress experienced by many transgender children,” they continue.
“They should not be made by politicians who think they know better than medical professionals,” they add.
The American Academy of Child and Adolescent Psychiatry has also condemned state efforts “to block access to these recognized interventions,” it said in a statement.
Proponents of laws speak of harms
Most of the state proposals portray medical interventions as harmful to minors.
Missouri’s proposed legislation labels surgical or hormonal treatment for a child under age 18 “abuse or neglect”; a physician or anyone who assists or provides for the child would be charged with a felony.
One of the first bills was introduced in South Dakota in January. House bill 1057 would have charged clinicians providing gender-affirming care in anyone under age 16 with a misdemeanor punishable by up to a year in prison and a $2,000 fine.
The bill was defeated in the Senate after the South Dakota State Medical Association and several other physicians, families, and adolescents testified against the proposal, according to the Argus Leader.
The Endocrine Society applauded the failure and noted in a statement that it “supports physicians’ ability to provide the best evidence-based treatment to their patients,” and that “these decisions should be made by the family and physician, and not dictated by policymakers.”
Jack Turban, MD, a resident physician in child and adolescent psychiatry at Massachusetts General Hospital, Boston, who conducted a pivotal study of some 26,000 transgender adults showing that early administration of puberty blockers led to lower odds of lifetime suicidal ideation, also expressed dismay over the bills in an opinion piece for the New York Times.
“The potential benefits of providing gender-affirmative care typically outweigh the minor risks associated with treatment,” wrote Turban.
“State legislators need to educate themselves about these young people and their medical care before introducing legislation that will hurt them,” he added.
Few states seem to have approached clinicians for feedback
In Tennessee, lawmakers have approached some clinicians at Vanderbilt and have appreciated the feedback they’ve received so far, said Brady.
But that may be an exception. It seems that few medical organizations have been consulted in the crafting of bills in the other states: Colorado, Florida, Idaho, Illinois, Kentucky, Mississippi, Missouri, New Hampshire, Oklahoma, South Carolina, South Dakota, and West Virginia. Lawmakers in Ohio and Utah also are drafting proposals.
Physicians could be charged with a felony in Florida, Idaho, Kentucky, Missouri, and reportedly, in the Ohio proposal under development.
The bills have been introduced at the behest of some conservative groups that doubt the existence of gender dysphoria or who have questions about treatment: the Eagle Forum, the Alliance Defending Freedom, and the Kelsey Coalition.
In a recent tweet clarifying its position on state efforts, the Kelsey Coalition said it “supports all bills that protect children, even those that may provide criminal penalties, because we believe these medical interventions should never be performed on children.”
“However, we do not support state bills that are not victim-led or used for political gain,” they added.
Existing knowledge imperfect but treatment indicated for some
The bills have also garnered support from some endocrinologists who have raised concerns about puberty blockers and other medical treatments for gender dysphoria.
One is Michael K. Laidlaw, MD, a Rocklin, California–based endocrinologist who has not treated transgender people but frequently writes about the subject, most recently calling the use of puberty blockers “a public health emergency.”
Laidlaw joined several other clinicians who do not treat transgender people in testifying in favor of the South Dakota bill.
Last year, as previously reported by Medscape Medical News, Laidlaw, along with others, criticized the Endocrine Society’s 2017 Clinical Practice Guideline on Treating Dysphoric/Gender-Incongruent Persons in a letter to the Journal of Clinical Endocrinology & Metabolism.
They stated that there is no lab, imaging, or other objective test to diagnose someone as transgender and that “the consequences of this gender-affirmative therapy are not trivial and include potential sterility, sexual dysfunction, thromboembolic and cardiovascular disease, and malignancy.”
Laidlaw told Medscape Medical News at the time that “If we’re talking about [transgender] adults [who have gone through puberty of their biological sex] and who can make a decision, if they have been truly notified of the risks and benefits [of cross-sex hormones] and have also had psychological evaluation, and they decide, ‘This is still the right course for me,’ then I don’t have any objection.”
But considering the use of cross-sex hormones in children and adolescents is “quite a different story,” he contended.
In May 2019, Rosenthal, Safer and colleagues responded to Laidlaw’s letter in the same journal, stating that for the right person, puberty blockers and cross-sex hormones are appropriate, and that medications can improve mental health outcomes.
“We agree that research to validate the safety and efficacy of all forms of treatment is desirable,” they wrote, noting some of that research is underway.
“However, we believe physicians would fall short in their duty of care if they withheld hormonal treatment of gender dysphoria/incongruence in pubertal youth, when indicated, given the existing state of knowledge, imperfect though it is.”
Research to validate safety and efficacy of transgender TX underway
Rosenthal’s center at UCSF is one of four in the United States that has been carrying out a National Institutes of Health-funded long-term observational study of the impact of early medical intervention on transgender adolescents.
It will take time to get those results, but in the meantime, clinicians should act on what is known now, said Rosenthal.
“We already have very compelling data to suggest that the benefits [of treatment] outweigh the potential harms,” he said.
Rosenthal told Medscape Medical News that Laidlaw has advanced the notion that clinicians who prescribe puberty blockers are forcing those individuals into a transgender outcome.
“We don’t push anybody down any path,” he said. “The guidelines make these treatments available in a very specific subset of people who are evaluated by skilled mental health professionals,” said Rosenthal.
Both he and Safer acknowledge that puberty blockers do have the potential for some harm. For instance, a frank discussion needs to happen about the likely lack of future fertility, said Rosenthal.
“Everything we do in medicine has a theoretical risk of harm,” noted Safer.
However, he said, to deny a puberty blocker to an individual approaching puberty who is distraught about growing breasts — but then to possibly have to surgically remove them later — is in itself doing harm.
“Puberty blockers are exactly the epitome of ‘do no harm’ in this case,” argued Safer.
The medications are reversible, he said, adding that they also give an individual and the family time to think through whether the adolescent is transgender, and, if yes, what they want to do in terms of taking cross-sex hormones in the future or getting other interventions.
Safer acknowledged that this doesn’t mean there aren’t still some concerns, however.
For instance, once puberty blockers — which have the potential to interfere with bone development — are started, “How much harm are you willing to risk? Maybe a couple of years is okay, but maybe 6 years is not,” he said.
“So, we do discuss how quickly...you have to get to your next decision point, whether it be to actually introduce hormones or not to introduce hormones,” he explained.
State proposals will have chilling effect on gender-questioning kids
Clinicians say that even if the proposals do not become law, just the fact of their existence could have a chilling effect on gender-questioning children, their families, and doctors considering whether to provide treatment.
“They’re already in a hard position,” Brady said of her patients.
“They’re coming here to seek something for a life that they’ve already not wanted to live and then we have people who are trying to put a real big block on that – I see that obviously affecting their mental health,” she observed.
“I can’t imagine how their lives would be without this care,” Brady said.
With the bills being out there, “two things can happen – one is, it can be very depressing and limiting, but it can also embolden people,” Rosenthal told Medscape Medical News.
“The people behind these things are the same people that have tried to stop our research at the National Institutes of Health (NIH),” he explained.
“These people are going to do everything they can, whether it’s to go state by state to try and exhaust us, or go to the NIH and try to get them to pull the plug on our research,” said Rosenthal.
Safer believes it’s ill-considered to try to legislate any aspect of medicine.
“The pitfalls of trying to legislate these things are myriad,” he said.
“Across all of medicine, interventions are very customized. Can you imagine a state legislature trying to legislate the optimal approach in medicines that can and cannot be given to people with diabetes? How crazy that would be,” he noted.
Rosenthal has served on an advisory panel for Endo Pharmaceuticals and is a grantee of the NIH. Safer has also served on an advisory panel for Endo Pharmaceuticals. Brady has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Many US endocrinologists are crying foul as a growing number of state lawmakers are attempting to enact legislation that would prohibit, and in some cases criminalize, medical treatment for minors with gender dysphoria.
As of press time, 13 states had introduced such bills, and legislators in two additional states said they were drafting bills. So far, one — in South Dakota — was defeated in a Senate committee, and another, in Florida, was essentially tabled without being enacted.
They all have a common goal of preventing minors from receiving puberty blockers, cross-sex hormones, or gender-affirmation surgery.
“These things are being proposed based on a lot of misinformation,” said Stephen Rosenthal, MD, professor of pediatrics at the University of California, San Francisco (UCSF), and a past president of the Pediatric Endocrine Society.
Lawmakers “are not looking at the scientific evidence that supports current clinical practice guidelines,” Rosenthal, who treats transgender children, told Medscape Medical News.
And “People just aren’t really understanding the harm that regulating this kind of medicine would do,” stressed Cassandra Brady, MD, assistant professor of pediatric endocrinology at Vanderbilt University School of Medicine, Memphis, Tennessee.
The bills come at a time when gender identity clinics for minors around the world have seen a significant uptick in cases. And, as widely reported by Medscape Medical News, some clinicians have begun to question whether treatment decisions are outpacing science.
Queries about use of puberty blockers and cross-sex hormones have embroiled the United Kingdom’s only publicly funded Gender Identity Development Service (GIDS) in controversy, for example, with five clinicians resigning last year over concerns about overuse of the treatments.
And earlier this month, the UK National Health Service (NHS) announced an independent review of services including the use of puberty blockers and cross-sex hormones in youth with gender dysphoria.
Meanwhile, the topic has ignited debate in Sweden, where a report from the Board of Health and Welfare confirmed a 1,500% rise between 2008 and 2018 in gender dysphoria diagnoses among 13- to 17-year-olds born as girls, as detailed by The Guardian.
Indeed, there is some indication of a so-called “rapid-onset gender dysphoria” in born females who say they wish to become males and some clinicians have said this represents a “social” phenomenon.
But guidelines from US clinical organizations – including the American Academy of Pediatrics issued in 2018, the Endocrine Society as reported by Medscape Medical News in 2017, and the US Professional Association for Transgender Health (USPATH) – all support the use of medical treatment in adolescents with gender dysphoria who have received mental health evaluations from appropriately trained professionals.
More data needed but evidence to intervene is compelling
Joshua Safer, MD, FACP, FACE, executive director of the Mount Sinai Center for Transgender Medicine and Surgery, New York City, says the data “even if it’s rudimentary, are convincing that there is a biological component to gender identity.”
Attempts to manipulate gender identity in people who are born intersex, for example, have uniformly failed, he noted.
Yet it’s still not known what causes gender identity – whether it might be a result of a cluster of genes or a bundle in the brain, or some other biological process – said Safer, who treats transgender adults, but not children, and is also a coauthor of the aforementioned Endocrine Society Clinical Practice Guideline on Endocrine Treatment of Gender Dysphoric/Gender Incongruent Persons.
This is an area for future research, he noted.
Nevertheless, “The data for interventions for transgender people ... is compelling,” he added, noting evidence for improved mental health morbidity among those gender-questioning people who have medical interventions.
“Those data are modest at this point and we need better data, but they do all move in the same direction,” he asserted.
Meanwhile, a large group of around 1,800 parents of transgender and nonbinary children have called on legislators to withdraw the proposals in an open letter organized by the Human Rights Campaign.
“We know better than anyone what our children need in order to thrive: access to best practice, evidence-based gender-affirming healthcare,” the parents write.
“These healthcare decisions must be made on a case-by-case basis, in careful consultation with a medical team, and with the goal of reducing the physical and emotional distress experienced by many transgender children,” they continue.
“They should not be made by politicians who think they know better than medical professionals,” they add.
The American Academy of Child and Adolescent Psychiatry has also condemned state efforts “to block access to these recognized interventions,” it said in a statement.
Proponents of laws speak of harms
Most of the state proposals portray medical interventions as harmful to minors.
Missouri’s proposed legislation labels surgical or hormonal treatment for a child under age 18 “abuse or neglect”; a physician or anyone who assists or provides for the child would be charged with a felony.
One of the first bills was introduced in South Dakota in January. House bill 1057 would have charged clinicians providing gender-affirming care in anyone under age 16 with a misdemeanor punishable by up to a year in prison and a $2,000 fine.
The bill was defeated in the Senate after the South Dakota State Medical Association and several other physicians, families, and adolescents testified against the proposal, according to the Argus Leader.
The Endocrine Society applauded the failure and noted in a statement that it “supports physicians’ ability to provide the best evidence-based treatment to their patients,” and that “these decisions should be made by the family and physician, and not dictated by policymakers.”
Jack Turban, MD, a resident physician in child and adolescent psychiatry at Massachusetts General Hospital, Boston, who conducted a pivotal study of some 26,000 transgender adults showing that early administration of puberty blockers led to lower odds of lifetime suicidal ideation, also expressed dismay over the bills in an opinion piece for the New York Times.
“The potential benefits of providing gender-affirmative care typically outweigh the minor risks associated with treatment,” wrote Turban.
“State legislators need to educate themselves about these young people and their medical care before introducing legislation that will hurt them,” he added.
Few states seem to have approached clinicians for feedback
In Tennessee, lawmakers have approached some clinicians at Vanderbilt and have appreciated the feedback they’ve received so far, said Brady.
But that may be an exception. It seems that few medical organizations have been consulted in the crafting of bills in the other states: Colorado, Florida, Idaho, Illinois, Kentucky, Mississippi, Missouri, New Hampshire, Oklahoma, South Carolina, South Dakota, and West Virginia. Lawmakers in Ohio and Utah also are drafting proposals.
Physicians could be charged with a felony in Florida, Idaho, Kentucky, Missouri, and reportedly, in the Ohio proposal under development.
The bills have been introduced at the behest of some conservative groups that doubt the existence of gender dysphoria or who have questions about treatment: the Eagle Forum, the Alliance Defending Freedom, and the Kelsey Coalition.
In a recent tweet clarifying its position on state efforts, the Kelsey Coalition said it “supports all bills that protect children, even those that may provide criminal penalties, because we believe these medical interventions should never be performed on children.”
“However, we do not support state bills that are not victim-led or used for political gain,” they added.
Existing knowledge imperfect but treatment indicated for some
The bills have also garnered support from some endocrinologists who have raised concerns about puberty blockers and other medical treatments for gender dysphoria.
One is Michael K. Laidlaw, MD, a Rocklin, California–based endocrinologist who has not treated transgender people but frequently writes about the subject, most recently calling the use of puberty blockers “a public health emergency.”
Laidlaw joined several other clinicians who do not treat transgender people in testifying in favor of the South Dakota bill.
Last year, as previously reported by Medscape Medical News, Laidlaw, along with others, criticized the Endocrine Society’s 2017 Clinical Practice Guideline on Treating Dysphoric/Gender-Incongruent Persons in a letter to the Journal of Clinical Endocrinology & Metabolism.
They stated that there is no lab, imaging, or other objective test to diagnose someone as transgender and that “the consequences of this gender-affirmative therapy are not trivial and include potential sterility, sexual dysfunction, thromboembolic and cardiovascular disease, and malignancy.”
Laidlaw told Medscape Medical News at the time that “If we’re talking about [transgender] adults [who have gone through puberty of their biological sex] and who can make a decision, if they have been truly notified of the risks and benefits [of cross-sex hormones] and have also had psychological evaluation, and they decide, ‘This is still the right course for me,’ then I don’t have any objection.”
But considering the use of cross-sex hormones in children and adolescents is “quite a different story,” he contended.
In May 2019, Rosenthal, Safer and colleagues responded to Laidlaw’s letter in the same journal, stating that for the right person, puberty blockers and cross-sex hormones are appropriate, and that medications can improve mental health outcomes.
“We agree that research to validate the safety and efficacy of all forms of treatment is desirable,” they wrote, noting some of that research is underway.
“However, we believe physicians would fall short in their duty of care if they withheld hormonal treatment of gender dysphoria/incongruence in pubertal youth, when indicated, given the existing state of knowledge, imperfect though it is.”
Research to validate safety and efficacy of transgender TX underway
Rosenthal’s center at UCSF is one of four in the United States that has been carrying out a National Institutes of Health-funded long-term observational study of the impact of early medical intervention on transgender adolescents.
It will take time to get those results, but in the meantime, clinicians should act on what is known now, said Rosenthal.
“We already have very compelling data to suggest that the benefits [of treatment] outweigh the potential harms,” he said.
Rosenthal told Medscape Medical News that Laidlaw has advanced the notion that clinicians who prescribe puberty blockers are forcing those individuals into a transgender outcome.
“We don’t push anybody down any path,” he said. “The guidelines make these treatments available in a very specific subset of people who are evaluated by skilled mental health professionals,” said Rosenthal.
Both he and Safer acknowledge that puberty blockers do have the potential for some harm. For instance, a frank discussion needs to happen about the likely lack of future fertility, said Rosenthal.
“Everything we do in medicine has a theoretical risk of harm,” noted Safer.
However, he said, to deny a puberty blocker to an individual approaching puberty who is distraught about growing breasts — but then to possibly have to surgically remove them later — is in itself doing harm.
“Puberty blockers are exactly the epitome of ‘do no harm’ in this case,” argued Safer.
The medications are reversible, he said, adding that they also give an individual and the family time to think through whether the adolescent is transgender, and, if yes, what they want to do in terms of taking cross-sex hormones in the future or getting other interventions.
Safer acknowledged that this doesn’t mean there aren’t still some concerns, however.
For instance, once puberty blockers — which have the potential to interfere with bone development — are started, “How much harm are you willing to risk? Maybe a couple of years is okay, but maybe 6 years is not,” he said.
“So, we do discuss how quickly...you have to get to your next decision point, whether it be to actually introduce hormones or not to introduce hormones,” he explained.
State proposals will have chilling effect on gender-questioning kids
Clinicians say that even if the proposals do not become law, just the fact of their existence could have a chilling effect on gender-questioning children, their families, and doctors considering whether to provide treatment.
“They’re already in a hard position,” Brady said of her patients.
“They’re coming here to seek something for a life that they’ve already not wanted to live and then we have people who are trying to put a real big block on that – I see that obviously affecting their mental health,” she observed.
“I can’t imagine how their lives would be without this care,” Brady said.
With the bills being out there, “two things can happen – one is, it can be very depressing and limiting, but it can also embolden people,” Rosenthal told Medscape Medical News.
“The people behind these things are the same people that have tried to stop our research at the National Institutes of Health (NIH),” he explained.
“These people are going to do everything they can, whether it’s to go state by state to try and exhaust us, or go to the NIH and try to get them to pull the plug on our research,” said Rosenthal.
Safer believes it’s ill-considered to try to legislate any aspect of medicine.
“The pitfalls of trying to legislate these things are myriad,” he said.
“Across all of medicine, interventions are very customized. Can you imagine a state legislature trying to legislate the optimal approach in medicines that can and cannot be given to people with diabetes? How crazy that would be,” he noted.
Rosenthal has served on an advisory panel for Endo Pharmaceuticals and is a grantee of the NIH. Safer has also served on an advisory panel for Endo Pharmaceuticals. Brady has reported no relevant financial relationships.
This article first appeared on Medscape.com.






