User login
AGA clinical practice update: Telemedicine in gastroenterology
moving forward, according to a new clinical practice update from the American Gastroenterological Association.
The postpandemic era must balance patient and provider preferences, medical needs, quality of care, regulatory requirements, and reimbursement rules, Ziad Gellad, MD, associate professor of medicine in the gastroenterology division at Duke University, Durham, N.C., and colleagues wrote.
“Spurred by the COVID-19 pandemic, telehealth, and specifically telemedicine, has become an integral part of outpatient gastrointestinal care in the United States,” the authors wrote.
Dr. Gellad and colleagues penned a clinical practice update based on recently published studies and the experiences of the authors, who are active gastroenterologists and hepatologists with extensive experience using telemedicine in clinical practice.
First, the group addressed patient preferences for telemedicine in gastroenterology based on emerging data. During the past 2 years, studies in both the United States and Australia found that most patients voiced ongoing interest and willingness to use video visits, as well as satisfaction with their medical concerns being addressed via telemedicine. They also reported significantly decreased absenteeism, as compared with face-to-face visits.
At the same time, patient preferences may vary based on age, race, and other factors. For instance, younger adults, those with higher incomes, and Hispanic and Latino patients appear to be more likely to prefer video visits than older adults, those with lower incomes, and White or Black patients. In gastroenterology, specific telemedicine studies, especially among patients with inflammatory bowel disease (IBD) or chronic liver disease, older patients, Black patients, and those with Medicaid or Medicare insurance were more likely to complete a phone-based visit rather than a video visit.
Even still, barriers exist for some patients, which should be recognized, the authors wrote. Studies have found racial and socioeconomic disparities in accessing telemedicine, including video visits. When possible, ambulatory practices, institutions, and health systems should provide technical solutions and individual support to help patients overcome these barriers.
So far, telemedicine appears to be better suited for stable chronic conditions rather than acute illnesses, which are more likely to require a follow-up in-person visit or ED care. At the gastrointestinal level, patients being evaluated for liver transplantation via telemedicine had a reduced time from referral to evaluation by a hepatologist and to transplant listing, and liver transplant recipients had lower readmission rates, improved physical function, and better general health. Among studies of IBD patients, telemedicine led to similar quality of care metrics and higher IBD-specific quality of life.
At this time, decisions about using telemedicine for patients with digestive diseases remain nuanced, the authors wrote. In general, those with stable conditions, such as gastroesophageal reflux, irritable bowel syndrome, IBD, chronic constipation, chronic liver disease, and chronic pancreatitis, appear to be good candidates for telemedicine. Patients who are considering a change in therapy and wish to schedule a visit for additional information may also use telemedicine.
In addition, those who live in remote areas could be appropriate candidates for telemedicine as long as they have access, particularly for video visits. Among these patients, studies have shown that telemedicine can be appropriate for patients with IBD and the transition of care from pediatric to adult gastroenterologists. Ultimately, the decision depends on several factors, including the practice setting, geography, and complexity of care.
Many times, the main barrier to virtual care is the regulatory requirement to be licensed in the state where the patient lives. Although these requirements were eased during the COVID-19 pandemic, many restrictions have now returned in most states. Some practices may now support their clinicians in obtaining licenses for surrounding states, but ultimately, some regulatory compromise will be needed to continue multistate telemedicine without additional licensure, the authors wrote.
Reimbursement rules have also remained a barrier. Despite some changes during the pandemic, reimbursement will likely shift in the future, and additional documentation requirements are suggested. For instance, it’s important to document patient consent to telemedicine, the method of telemedicine (whether a secure two-way interactive video or phone call), patient location, provider location, a listing of all clinical participants’ roles and actions, and other individuals (such as trainees) present at the visit.
Finally, the clinical workflow for telemedicine should include a few additional steps, the authors wrote. Office staff should connect with patients before the visit to address any technical issues and ensure a proper connection, set up any assistive services such as an interpreter, complete previsit questionnaires via secure messaging, and conduct standard practices such as medication review. Postvisit instructions should then be sent through a secure portal or mail.
Moving forward, additional studies are needed to verify long-term outcomes associated with telemedicine, as well as the optimal ratio of in-person versus telemedicine visits for various disease states, the authors wrote.
“Telemedicine is accepted by both patients and providers, and is associated with certain key advantages, including reducing patient travel time and cost and work absenteeism,” they wrote. However, “gastroenterology providers need to be cognizant of certain patient and illness barriers to telemedicine and adhere to best practices to ensure high-quality gastrointestinal virtual care.”
The clinical practice update received no funding support. Dr. Gellad disclosed financial relationships with Higgs Boson, Inc.; Merck & Co; and Novo Nordisk. Author Seth Crockett is a consultant for IngenioRx and has received research funding from Freenome, Guardant, and Exact Sciences. Raymond Cross disclosed financial relationships with AbbvVie, BMS, Fzata, Janssen, Magellan Health, Pfizer, and Takeda and has received support from the Crohn's and Colitis Foundation, IBD Education Group, and CorEvitas.
moving forward, according to a new clinical practice update from the American Gastroenterological Association.
The postpandemic era must balance patient and provider preferences, medical needs, quality of care, regulatory requirements, and reimbursement rules, Ziad Gellad, MD, associate professor of medicine in the gastroenterology division at Duke University, Durham, N.C., and colleagues wrote.
“Spurred by the COVID-19 pandemic, telehealth, and specifically telemedicine, has become an integral part of outpatient gastrointestinal care in the United States,” the authors wrote.
Dr. Gellad and colleagues penned a clinical practice update based on recently published studies and the experiences of the authors, who are active gastroenterologists and hepatologists with extensive experience using telemedicine in clinical practice.
First, the group addressed patient preferences for telemedicine in gastroenterology based on emerging data. During the past 2 years, studies in both the United States and Australia found that most patients voiced ongoing interest and willingness to use video visits, as well as satisfaction with their medical concerns being addressed via telemedicine. They also reported significantly decreased absenteeism, as compared with face-to-face visits.
At the same time, patient preferences may vary based on age, race, and other factors. For instance, younger adults, those with higher incomes, and Hispanic and Latino patients appear to be more likely to prefer video visits than older adults, those with lower incomes, and White or Black patients. In gastroenterology, specific telemedicine studies, especially among patients with inflammatory bowel disease (IBD) or chronic liver disease, older patients, Black patients, and those with Medicaid or Medicare insurance were more likely to complete a phone-based visit rather than a video visit.
Even still, barriers exist for some patients, which should be recognized, the authors wrote. Studies have found racial and socioeconomic disparities in accessing telemedicine, including video visits. When possible, ambulatory practices, institutions, and health systems should provide technical solutions and individual support to help patients overcome these barriers.
So far, telemedicine appears to be better suited for stable chronic conditions rather than acute illnesses, which are more likely to require a follow-up in-person visit or ED care. At the gastrointestinal level, patients being evaluated for liver transplantation via telemedicine had a reduced time from referral to evaluation by a hepatologist and to transplant listing, and liver transplant recipients had lower readmission rates, improved physical function, and better general health. Among studies of IBD patients, telemedicine led to similar quality of care metrics and higher IBD-specific quality of life.
At this time, decisions about using telemedicine for patients with digestive diseases remain nuanced, the authors wrote. In general, those with stable conditions, such as gastroesophageal reflux, irritable bowel syndrome, IBD, chronic constipation, chronic liver disease, and chronic pancreatitis, appear to be good candidates for telemedicine. Patients who are considering a change in therapy and wish to schedule a visit for additional information may also use telemedicine.
In addition, those who live in remote areas could be appropriate candidates for telemedicine as long as they have access, particularly for video visits. Among these patients, studies have shown that telemedicine can be appropriate for patients with IBD and the transition of care from pediatric to adult gastroenterologists. Ultimately, the decision depends on several factors, including the practice setting, geography, and complexity of care.
Many times, the main barrier to virtual care is the regulatory requirement to be licensed in the state where the patient lives. Although these requirements were eased during the COVID-19 pandemic, many restrictions have now returned in most states. Some practices may now support their clinicians in obtaining licenses for surrounding states, but ultimately, some regulatory compromise will be needed to continue multistate telemedicine without additional licensure, the authors wrote.
Reimbursement rules have also remained a barrier. Despite some changes during the pandemic, reimbursement will likely shift in the future, and additional documentation requirements are suggested. For instance, it’s important to document patient consent to telemedicine, the method of telemedicine (whether a secure two-way interactive video or phone call), patient location, provider location, a listing of all clinical participants’ roles and actions, and other individuals (such as trainees) present at the visit.
Finally, the clinical workflow for telemedicine should include a few additional steps, the authors wrote. Office staff should connect with patients before the visit to address any technical issues and ensure a proper connection, set up any assistive services such as an interpreter, complete previsit questionnaires via secure messaging, and conduct standard practices such as medication review. Postvisit instructions should then be sent through a secure portal or mail.
Moving forward, additional studies are needed to verify long-term outcomes associated with telemedicine, as well as the optimal ratio of in-person versus telemedicine visits for various disease states, the authors wrote.
“Telemedicine is accepted by both patients and providers, and is associated with certain key advantages, including reducing patient travel time and cost and work absenteeism,” they wrote. However, “gastroenterology providers need to be cognizant of certain patient and illness barriers to telemedicine and adhere to best practices to ensure high-quality gastrointestinal virtual care.”
The clinical practice update received no funding support. Dr. Gellad disclosed financial relationships with Higgs Boson, Inc.; Merck & Co; and Novo Nordisk. Author Seth Crockett is a consultant for IngenioRx and has received research funding from Freenome, Guardant, and Exact Sciences. Raymond Cross disclosed financial relationships with AbbvVie, BMS, Fzata, Janssen, Magellan Health, Pfizer, and Takeda and has received support from the Crohn's and Colitis Foundation, IBD Education Group, and CorEvitas.
moving forward, according to a new clinical practice update from the American Gastroenterological Association.
The postpandemic era must balance patient and provider preferences, medical needs, quality of care, regulatory requirements, and reimbursement rules, Ziad Gellad, MD, associate professor of medicine in the gastroenterology division at Duke University, Durham, N.C., and colleagues wrote.
“Spurred by the COVID-19 pandemic, telehealth, and specifically telemedicine, has become an integral part of outpatient gastrointestinal care in the United States,” the authors wrote.
Dr. Gellad and colleagues penned a clinical practice update based on recently published studies and the experiences of the authors, who are active gastroenterologists and hepatologists with extensive experience using telemedicine in clinical practice.
First, the group addressed patient preferences for telemedicine in gastroenterology based on emerging data. During the past 2 years, studies in both the United States and Australia found that most patients voiced ongoing interest and willingness to use video visits, as well as satisfaction with their medical concerns being addressed via telemedicine. They also reported significantly decreased absenteeism, as compared with face-to-face visits.
At the same time, patient preferences may vary based on age, race, and other factors. For instance, younger adults, those with higher incomes, and Hispanic and Latino patients appear to be more likely to prefer video visits than older adults, those with lower incomes, and White or Black patients. In gastroenterology, specific telemedicine studies, especially among patients with inflammatory bowel disease (IBD) or chronic liver disease, older patients, Black patients, and those with Medicaid or Medicare insurance were more likely to complete a phone-based visit rather than a video visit.
Even still, barriers exist for some patients, which should be recognized, the authors wrote. Studies have found racial and socioeconomic disparities in accessing telemedicine, including video visits. When possible, ambulatory practices, institutions, and health systems should provide technical solutions and individual support to help patients overcome these barriers.
So far, telemedicine appears to be better suited for stable chronic conditions rather than acute illnesses, which are more likely to require a follow-up in-person visit or ED care. At the gastrointestinal level, patients being evaluated for liver transplantation via telemedicine had a reduced time from referral to evaluation by a hepatologist and to transplant listing, and liver transplant recipients had lower readmission rates, improved physical function, and better general health. Among studies of IBD patients, telemedicine led to similar quality of care metrics and higher IBD-specific quality of life.
At this time, decisions about using telemedicine for patients with digestive diseases remain nuanced, the authors wrote. In general, those with stable conditions, such as gastroesophageal reflux, irritable bowel syndrome, IBD, chronic constipation, chronic liver disease, and chronic pancreatitis, appear to be good candidates for telemedicine. Patients who are considering a change in therapy and wish to schedule a visit for additional information may also use telemedicine.
In addition, those who live in remote areas could be appropriate candidates for telemedicine as long as they have access, particularly for video visits. Among these patients, studies have shown that telemedicine can be appropriate for patients with IBD and the transition of care from pediatric to adult gastroenterologists. Ultimately, the decision depends on several factors, including the practice setting, geography, and complexity of care.
Many times, the main barrier to virtual care is the regulatory requirement to be licensed in the state where the patient lives. Although these requirements were eased during the COVID-19 pandemic, many restrictions have now returned in most states. Some practices may now support their clinicians in obtaining licenses for surrounding states, but ultimately, some regulatory compromise will be needed to continue multistate telemedicine without additional licensure, the authors wrote.
Reimbursement rules have also remained a barrier. Despite some changes during the pandemic, reimbursement will likely shift in the future, and additional documentation requirements are suggested. For instance, it’s important to document patient consent to telemedicine, the method of telemedicine (whether a secure two-way interactive video or phone call), patient location, provider location, a listing of all clinical participants’ roles and actions, and other individuals (such as trainees) present at the visit.
Finally, the clinical workflow for telemedicine should include a few additional steps, the authors wrote. Office staff should connect with patients before the visit to address any technical issues and ensure a proper connection, set up any assistive services such as an interpreter, complete previsit questionnaires via secure messaging, and conduct standard practices such as medication review. Postvisit instructions should then be sent through a secure portal or mail.
Moving forward, additional studies are needed to verify long-term outcomes associated with telemedicine, as well as the optimal ratio of in-person versus telemedicine visits for various disease states, the authors wrote.
“Telemedicine is accepted by both patients and providers, and is associated with certain key advantages, including reducing patient travel time and cost and work absenteeism,” they wrote. However, “gastroenterology providers need to be cognizant of certain patient and illness barriers to telemedicine and adhere to best practices to ensure high-quality gastrointestinal virtual care.”
The clinical practice update received no funding support. Dr. Gellad disclosed financial relationships with Higgs Boson, Inc.; Merck & Co; and Novo Nordisk. Author Seth Crockett is a consultant for IngenioRx and has received research funding from Freenome, Guardant, and Exact Sciences. Raymond Cross disclosed financial relationships with AbbvVie, BMS, Fzata, Janssen, Magellan Health, Pfizer, and Takeda and has received support from the Crohn's and Colitis Foundation, IBD Education Group, and CorEvitas.
FROM GASTROENTEROLOGY
New coding policies to prevent surprise billing for CRC screening
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
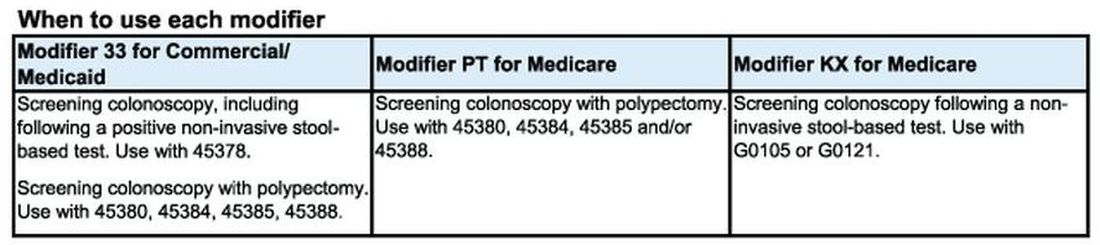
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
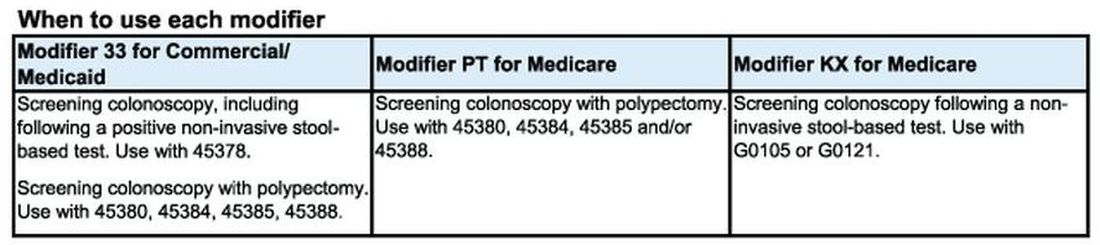
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
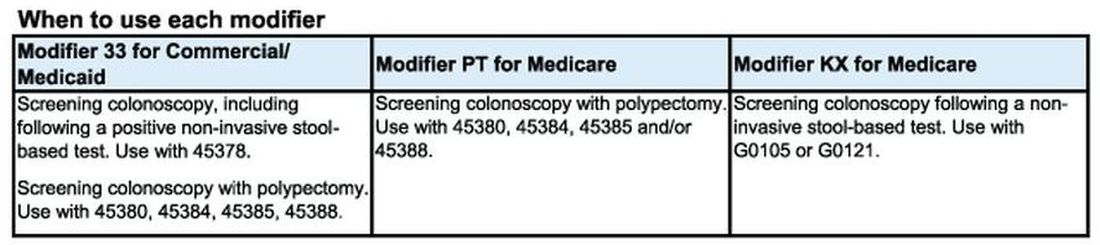
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.
Physician pleads guilty to 52 counts in opioid scheme
Jeffrey B. Sutton, DO, a neuromuscular medicine specialist, pled guilty on January 30 in federal court to 31 counts of illegally prescribing opioids and other controlled substances, 1 count of illegally distributing controlled substances, and 20 counts of health care fraud.
Prosecutors said Dr. Sutton admitted that he ignored warnings from prescription drug management organizations, insurers, and state authorities that he was prescribing excessively high dosages of opioids.
Dr. Sutton also admitted to ignoring patient requests to lower dosages and that he also ignored signs that patients were selling prescribed medications or otherwise engaging in illicit activity, including violations of a “pain management agreement” that he required them to sign.
The fraud counts pertained to Dr. Sutton billing Medicare, Medicaid, and other insurers for medically unnecessary visits that he required of patients so that he could prescribe inappropriate or unnecessary opioids.
In the charging document shared with this news organization, prosecutors said Dr. Sutton had sex with at least three patients, including during office visits and outside of the office. Occasionally, the physician would give opioids or other controlled substances – often benzodiazepines – to these patients, without a prescription or valid medical need.
Dr. Sutton escalated the dosage for one of those patients, even as the subjective pain score did not improve and when the patient’s urine tests showed the presence of THC and buprenorphine, but not any of the prescribed medications.
Another patient came to Dr. Sutton in 2007 with a warning that she had a history of “narcotic-seeking” behavior and diagnoses of depression, anxiety, paranoid schizophrenia, and obsessive-compulsive disorder.
The patient was hospitalized in 2018 for complications from benzodiazepine use (prescribed by Dr. Sutton). She weighed 80 pounds at the time. Dr. Sutton continued to prescribe benzodiazepines and extreme doses of opioids – in excess of 2,000 morphine equivalent dose – “despite recognizing and documenting repeated instances of noncompliance with treatment for psychiatric conditions, and despite the known contraindications of long-term opioid use for patients with these mental illnesses,” according to the charging document.
Dr. Sutton continued to prescribe opioids despite two hospitalizations for overdoses, more than 20 failed urine drug screens that showed presence of illicit drugs such as cocaine, and documented excessive use of alprazolam (Xanax) and methadone.
The physician surrendered his Drug Enforcement Administration Certificate of Registration of Controlled Substances Privileges in February 2022 “as an indication of your good faith in desiring to remedy any incorrect or unlawful practices on your part,” according to a letter to Dr. Sutton from the State Medical Board of Ohio. In that September 2022 letter, the Board notified Dr. Sutton of its intention to possibly suspend or revoke his license.
Dr. Sutton did not request a hearing, and the Board permanently revoked his medical license on January 16.
The court will sentence Dr. Sutton on May 23, according to a report by WFMJ.
A version of this article originally appeared on Medscape.com.
Jeffrey B. Sutton, DO, a neuromuscular medicine specialist, pled guilty on January 30 in federal court to 31 counts of illegally prescribing opioids and other controlled substances, 1 count of illegally distributing controlled substances, and 20 counts of health care fraud.
Prosecutors said Dr. Sutton admitted that he ignored warnings from prescription drug management organizations, insurers, and state authorities that he was prescribing excessively high dosages of opioids.
Dr. Sutton also admitted to ignoring patient requests to lower dosages and that he also ignored signs that patients were selling prescribed medications or otherwise engaging in illicit activity, including violations of a “pain management agreement” that he required them to sign.
The fraud counts pertained to Dr. Sutton billing Medicare, Medicaid, and other insurers for medically unnecessary visits that he required of patients so that he could prescribe inappropriate or unnecessary opioids.
In the charging document shared with this news organization, prosecutors said Dr. Sutton had sex with at least three patients, including during office visits and outside of the office. Occasionally, the physician would give opioids or other controlled substances – often benzodiazepines – to these patients, without a prescription or valid medical need.
Dr. Sutton escalated the dosage for one of those patients, even as the subjective pain score did not improve and when the patient’s urine tests showed the presence of THC and buprenorphine, but not any of the prescribed medications.
Another patient came to Dr. Sutton in 2007 with a warning that she had a history of “narcotic-seeking” behavior and diagnoses of depression, anxiety, paranoid schizophrenia, and obsessive-compulsive disorder.
The patient was hospitalized in 2018 for complications from benzodiazepine use (prescribed by Dr. Sutton). She weighed 80 pounds at the time. Dr. Sutton continued to prescribe benzodiazepines and extreme doses of opioids – in excess of 2,000 morphine equivalent dose – “despite recognizing and documenting repeated instances of noncompliance with treatment for psychiatric conditions, and despite the known contraindications of long-term opioid use for patients with these mental illnesses,” according to the charging document.
Dr. Sutton continued to prescribe opioids despite two hospitalizations for overdoses, more than 20 failed urine drug screens that showed presence of illicit drugs such as cocaine, and documented excessive use of alprazolam (Xanax) and methadone.
The physician surrendered his Drug Enforcement Administration Certificate of Registration of Controlled Substances Privileges in February 2022 “as an indication of your good faith in desiring to remedy any incorrect or unlawful practices on your part,” according to a letter to Dr. Sutton from the State Medical Board of Ohio. In that September 2022 letter, the Board notified Dr. Sutton of its intention to possibly suspend or revoke his license.
Dr. Sutton did not request a hearing, and the Board permanently revoked his medical license on January 16.
The court will sentence Dr. Sutton on May 23, according to a report by WFMJ.
A version of this article originally appeared on Medscape.com.
Jeffrey B. Sutton, DO, a neuromuscular medicine specialist, pled guilty on January 30 in federal court to 31 counts of illegally prescribing opioids and other controlled substances, 1 count of illegally distributing controlled substances, and 20 counts of health care fraud.
Prosecutors said Dr. Sutton admitted that he ignored warnings from prescription drug management organizations, insurers, and state authorities that he was prescribing excessively high dosages of opioids.
Dr. Sutton also admitted to ignoring patient requests to lower dosages and that he also ignored signs that patients were selling prescribed medications or otherwise engaging in illicit activity, including violations of a “pain management agreement” that he required them to sign.
The fraud counts pertained to Dr. Sutton billing Medicare, Medicaid, and other insurers for medically unnecessary visits that he required of patients so that he could prescribe inappropriate or unnecessary opioids.
In the charging document shared with this news organization, prosecutors said Dr. Sutton had sex with at least three patients, including during office visits and outside of the office. Occasionally, the physician would give opioids or other controlled substances – often benzodiazepines – to these patients, without a prescription or valid medical need.
Dr. Sutton escalated the dosage for one of those patients, even as the subjective pain score did not improve and when the patient’s urine tests showed the presence of THC and buprenorphine, but not any of the prescribed medications.
Another patient came to Dr. Sutton in 2007 with a warning that she had a history of “narcotic-seeking” behavior and diagnoses of depression, anxiety, paranoid schizophrenia, and obsessive-compulsive disorder.
The patient was hospitalized in 2018 for complications from benzodiazepine use (prescribed by Dr. Sutton). She weighed 80 pounds at the time. Dr. Sutton continued to prescribe benzodiazepines and extreme doses of opioids – in excess of 2,000 morphine equivalent dose – “despite recognizing and documenting repeated instances of noncompliance with treatment for psychiatric conditions, and despite the known contraindications of long-term opioid use for patients with these mental illnesses,” according to the charging document.
Dr. Sutton continued to prescribe opioids despite two hospitalizations for overdoses, more than 20 failed urine drug screens that showed presence of illicit drugs such as cocaine, and documented excessive use of alprazolam (Xanax) and methadone.
The physician surrendered his Drug Enforcement Administration Certificate of Registration of Controlled Substances Privileges in February 2022 “as an indication of your good faith in desiring to remedy any incorrect or unlawful practices on your part,” according to a letter to Dr. Sutton from the State Medical Board of Ohio. In that September 2022 letter, the Board notified Dr. Sutton of its intention to possibly suspend or revoke his license.
Dr. Sutton did not request a hearing, and the Board permanently revoked his medical license on January 16.
The court will sentence Dr. Sutton on May 23, according to a report by WFMJ.
A version of this article originally appeared on Medscape.com.
Physicians and clinicians should be required to get flu shots: Ethicist
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at New York University’s Grossman School of Medicine, where I’m the director.
I’ve long believed that every health care institution – nursing homes, hospitals, clinics, home care, hospice – should require flu shots for all doctors and all nurses because it is the easiest, cheapest, and most ethical way to protect the workforce, who you need to be in there when flu outbreaks take place, and to protect patients against getting the flu when they come into hospital settings and get exposed to health care workers who may have the flu already but don’t know it.
In a recent poll, I was happy to see that the majority of physicians surveyed agreed with me: 65% said they supported mandatory flu vaccination in hospitals and only 23% said they did not. I think flu vaccination is something that has already been shown to be useful and important, not only in stopping people from getting the flu but also in making sure that they don’t get as sick when they get the flu.
Just like COVID-19 vaccination, it doesn’t always prevent somebody from getting infected, but if you get it, it keeps you from winding up sick at home, or worse – from dying and winding up in the morgue. Flu kills many, many people every year. We don’t want that to happen. A flu vaccine will really help prevent deaths, help prevent the number of symptoms that somebody gets, and will get people back to work. The benefits are pretty clear.
Does the flu vaccine work equally well every year? It does not. Some years, the strains that are picked for the vaccine don’t match the ones that circulate, and we don’t get as much protection as we hoped for. I think the safety side is so strong that it’s worth making the investment and the effort to promote mandatory flu vaccination.
Can you opt out on religious grounds? Well, some hospitals permit that at New York University. You have to go before a committee and make a case that your exemption on religious grounds is based on an authentic set of beliefs that are deeply held, and not just something you thought up the day before flu vaccine requirements went into effect.
There may be room for some exemptions – obviously, for health reasons. If people think that the flu vaccine is dangerous to them and can get a physician to agree and sign off that they are not appropriate to vaccinate, okay.
On the other hand, if you’re working with an especially vulnerable population – newborns, people who are immunosuppressed – then I think you’ve got to be vaccinated and you shouldn’t be working around people who are at huge risk of getting the flu if you refuse to be vaccinated or, for that matter, can’t be vaccinated.
Would I extend these mandates? Yes, I would. I’d extend them to COVID-19 vaccination and to measles vaccination. I think physicians and nurses should be good role models. They should get vaccinated. We know that the best available evidence says that vaccination for infectious disease is safe. It is really the best thing we can do to combat a variety of diseases such as the flu and COVID-19.
It seems to me that, in addition, the data that are out there in terms of risks from flu and COVID-19 – deaths in places like nursing homes – are overwhelming about the importance of trying to get staff vaccinated so they don’t bring flu into an institutionalized population. This is similar for prison health and many other settings where people are kept close together and staff may move from place to place, rotating from institution to institution, spreading infectious disease.
I’m going to go with the poll. Let’s keep pushing for health care workers to do the right thing and to be good role models. Let’s get everybody a flu vaccination. Let’s extend it to a COVID-19 vaccination and its boosters.
Let’s try to show the nation that health care is going to be guided by good science, a duty to one’s own health, and a duty to one’s patients. It shouldn’t be political. It should be based on what works best for the interests of health care providers and those they care for.
I’m Art Caplan at the New York University Grossman School of Medicine. Thanks for watching.
Dr. Caplan has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position). Serves as a contributing author and advisor for Medscape. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at New York University’s Grossman School of Medicine, where I’m the director.
I’ve long believed that every health care institution – nursing homes, hospitals, clinics, home care, hospice – should require flu shots for all doctors and all nurses because it is the easiest, cheapest, and most ethical way to protect the workforce, who you need to be in there when flu outbreaks take place, and to protect patients against getting the flu when they come into hospital settings and get exposed to health care workers who may have the flu already but don’t know it.
In a recent poll, I was happy to see that the majority of physicians surveyed agreed with me: 65% said they supported mandatory flu vaccination in hospitals and only 23% said they did not. I think flu vaccination is something that has already been shown to be useful and important, not only in stopping people from getting the flu but also in making sure that they don’t get as sick when they get the flu.
Just like COVID-19 vaccination, it doesn’t always prevent somebody from getting infected, but if you get it, it keeps you from winding up sick at home, or worse – from dying and winding up in the morgue. Flu kills many, many people every year. We don’t want that to happen. A flu vaccine will really help prevent deaths, help prevent the number of symptoms that somebody gets, and will get people back to work. The benefits are pretty clear.
Does the flu vaccine work equally well every year? It does not. Some years, the strains that are picked for the vaccine don’t match the ones that circulate, and we don’t get as much protection as we hoped for. I think the safety side is so strong that it’s worth making the investment and the effort to promote mandatory flu vaccination.
Can you opt out on religious grounds? Well, some hospitals permit that at New York University. You have to go before a committee and make a case that your exemption on religious grounds is based on an authentic set of beliefs that are deeply held, and not just something you thought up the day before flu vaccine requirements went into effect.
There may be room for some exemptions – obviously, for health reasons. If people think that the flu vaccine is dangerous to them and can get a physician to agree and sign off that they are not appropriate to vaccinate, okay.
On the other hand, if you’re working with an especially vulnerable population – newborns, people who are immunosuppressed – then I think you’ve got to be vaccinated and you shouldn’t be working around people who are at huge risk of getting the flu if you refuse to be vaccinated or, for that matter, can’t be vaccinated.
Would I extend these mandates? Yes, I would. I’d extend them to COVID-19 vaccination and to measles vaccination. I think physicians and nurses should be good role models. They should get vaccinated. We know that the best available evidence says that vaccination for infectious disease is safe. It is really the best thing we can do to combat a variety of diseases such as the flu and COVID-19.
It seems to me that, in addition, the data that are out there in terms of risks from flu and COVID-19 – deaths in places like nursing homes – are overwhelming about the importance of trying to get staff vaccinated so they don’t bring flu into an institutionalized population. This is similar for prison health and many other settings where people are kept close together and staff may move from place to place, rotating from institution to institution, spreading infectious disease.
I’m going to go with the poll. Let’s keep pushing for health care workers to do the right thing and to be good role models. Let’s get everybody a flu vaccination. Let’s extend it to a COVID-19 vaccination and its boosters.
Let’s try to show the nation that health care is going to be guided by good science, a duty to one’s own health, and a duty to one’s patients. It shouldn’t be political. It should be based on what works best for the interests of health care providers and those they care for.
I’m Art Caplan at the New York University Grossman School of Medicine. Thanks for watching.
Dr. Caplan has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position). Serves as a contributing author and advisor for Medscape. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at New York University’s Grossman School of Medicine, where I’m the director.
I’ve long believed that every health care institution – nursing homes, hospitals, clinics, home care, hospice – should require flu shots for all doctors and all nurses because it is the easiest, cheapest, and most ethical way to protect the workforce, who you need to be in there when flu outbreaks take place, and to protect patients against getting the flu when they come into hospital settings and get exposed to health care workers who may have the flu already but don’t know it.
In a recent poll, I was happy to see that the majority of physicians surveyed agreed with me: 65% said they supported mandatory flu vaccination in hospitals and only 23% said they did not. I think flu vaccination is something that has already been shown to be useful and important, not only in stopping people from getting the flu but also in making sure that they don’t get as sick when they get the flu.
Just like COVID-19 vaccination, it doesn’t always prevent somebody from getting infected, but if you get it, it keeps you from winding up sick at home, or worse – from dying and winding up in the morgue. Flu kills many, many people every year. We don’t want that to happen. A flu vaccine will really help prevent deaths, help prevent the number of symptoms that somebody gets, and will get people back to work. The benefits are pretty clear.
Does the flu vaccine work equally well every year? It does not. Some years, the strains that are picked for the vaccine don’t match the ones that circulate, and we don’t get as much protection as we hoped for. I think the safety side is so strong that it’s worth making the investment and the effort to promote mandatory flu vaccination.
Can you opt out on religious grounds? Well, some hospitals permit that at New York University. You have to go before a committee and make a case that your exemption on religious grounds is based on an authentic set of beliefs that are deeply held, and not just something you thought up the day before flu vaccine requirements went into effect.
There may be room for some exemptions – obviously, for health reasons. If people think that the flu vaccine is dangerous to them and can get a physician to agree and sign off that they are not appropriate to vaccinate, okay.
On the other hand, if you’re working with an especially vulnerable population – newborns, people who are immunosuppressed – then I think you’ve got to be vaccinated and you shouldn’t be working around people who are at huge risk of getting the flu if you refuse to be vaccinated or, for that matter, can’t be vaccinated.
Would I extend these mandates? Yes, I would. I’d extend them to COVID-19 vaccination and to measles vaccination. I think physicians and nurses should be good role models. They should get vaccinated. We know that the best available evidence says that vaccination for infectious disease is safe. It is really the best thing we can do to combat a variety of diseases such as the flu and COVID-19.
It seems to me that, in addition, the data that are out there in terms of risks from flu and COVID-19 – deaths in places like nursing homes – are overwhelming about the importance of trying to get staff vaccinated so they don’t bring flu into an institutionalized population. This is similar for prison health and many other settings where people are kept close together and staff may move from place to place, rotating from institution to institution, spreading infectious disease.
I’m going to go with the poll. Let’s keep pushing for health care workers to do the right thing and to be good role models. Let’s get everybody a flu vaccination. Let’s extend it to a COVID-19 vaccination and its boosters.
Let’s try to show the nation that health care is going to be guided by good science, a duty to one’s own health, and a duty to one’s patients. It shouldn’t be political. It should be based on what works best for the interests of health care providers and those they care for.
I’m Art Caplan at the New York University Grossman School of Medicine. Thanks for watching.
Dr. Caplan has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position). Serves as a contributing author and advisor for Medscape. A version of this article originally appeared on Medscape.com.
How spirituality guides these three doctors
Whether you’re spiritual, religious – or neither – the Medscape Physician Lifestyle & Happiness Report 2023 asked if you have a religious or spiritual belief. Turns out 69% of physicians shared that they have a spiritual or religious practice.
Tapping into the universe
Nick Shamie, MD, an orthopedic surgeon specializing in spine surgery at University of California, Los Angeles, says the constant challenges of making life-and-death decisions offer an opportunity to check in with a higher power.
“Sometimes when I’m going into a tough surgery or have a tough situation, I pause and think about how this isn’t about me and the situation I’m in,” says Dr. Shamie, whose family is Muslim. “It’s about the whole universe. I feel like someone, or some being, is looking over my shoulders, and if my intentions are good, I’ll be fine. The person I’m going to take care of will be fine. That’s how I use my faith.”
Having a belief in something greater than herself also fuels Jill Carnahan, MD, a family medicine physician and functional medicine expert in Boulder, Colo.
“This is key for me as a physician,” says Dr. Carnahan, author of “Unexpected: Finding Resilience Through Functional Medicine, Science, and Faith.” “I urge physicians to think about their source of strength. That’s not necessarily even religious. It could be meditation or being in nature.”
Dr. Carnahan likes to share with patients that there are lessons that can come from being ill – whether treating ill patients or struggling with one’s own illness.
“I like to teach this idea of illness as a teacher,” says Dr. Carnahan, who has Crohn’s disease and is a cancer survivor. “This is tough, but what you’re saying here is that there is meaning or purpose to this experience. It brings awareness to your life that may not have been there before.”
Often illness is our body’s way of getting our attention that our life, relationships, or work needs adjustment. Illness can be a reminder to make changes. “For example, a diagnosis of autoimmunity may be a reminder to take better care of ourselves, or a diagnosis of cancer may cause us to get out of an unhealthy relationship or change jobs to do something more fulfilling, as we have increased awareness of the brevity of life.”
When patients are affected by illness, pain, reduced functionality, and even imminent death, understanding the experience is difficult, and finding any purpose in it may seem impossible. Still, studies show that those who find meaning in the experience cope better with their illness.
Finding that meaning may be a strong driver of survival and may be positively related to hope, belief, and happiness.
Spirituality supports patients
Even if you’re not religious yourself, it can be helpful to support a patient who opts to pray before an arduous procedure, says Sharyar Baradaran, DDS, a periodontist specializing in gum surgery in Beverly Hills, Calif.
“I’ve had patients who go into meditation mode, or they say a prayer before I start surgery,” he says. “I take that opportunity to connect. In that instance, we hold hands. I want them to know that I understand what they’re going through and how they’re trying to find the courage to undergo surgery.”
When Dr. Shamie was a child, his father described religion as embodying the basic tenet of being good to others. “I’ve taken that to heart,” he says. “All religions, all faiths have that as a central premise.”
These doctors agree that when you take the time to stop and hold a patient’s hand, bow your head during their prayer, or acknowledge or speak for a few moments about their faith, especially during a health crisis, surgery, or challenging diagnosis, patients appreciate it and develop an even deeper connection with you.
Dr. Baradaran believes spirituality can play an important role in how health care providers care for patients. Though it may not be widely discussed or reported, and physicians may find little time and space to address patients’ spiritual needs, there is growing sensitivity regarding spirituality in health care. One study found that while physicians understand its importance, nurses are more apt to integrate spirituality into practice.
“No matter the religion, if you’re spiritual, it means you’re listening and being respectful,” says Dr. Baradaran, who is Jewish. “There are times that I’m not familiar with the prayers my patients are saying, but I always take them in, absorb them, and respect them. This allows me to have a deeper connection with them, which is wonderful.”
Dr. Shamie says that he turns to his faith in good times as well as tough ones.
“I see a lot of people who are dealing with very difficult situations, and it’s not their choice to be in this position,” he says. “At those moments, I think to myself how fortunate I am that I’m not experiencing what this individual or family is going through. I do thank God at that time. I appreciate the life I have, and when I witness hardships, it resets my appreciation.”
For Dr. Carnahan, faith is about becoming comfortable with the inevitable uncertainty of life. It’s also about finding ways to tap into the day’s stresses.
“As physicians, we’re workaholics, and one in four of us are burnt out,” she says. “One solution that really works is to step back from the day-to-day grind and find time to pray or meditate or be in nature.”
There are times when a tragedy occurs, and despite your most intense efforts, a patient may die. Those experiences can be crushing to a physician. However, to guide you through the loss of a patient or the daily juggles of managing your practice, Dr. Carnahan suggests finding time every morning to focus on the day ahead and how you connect with the universe.
“I take 15 minutes in the morning and think about how I will bring love to the world,” she says. “If you look for the miracles and the good and the unexpected, that gratitude shift allows your mind to be transformed by what’s happening. It’s often in those moments that you’ll realize again why you went into medicine in the first place.”
Doctors without faith
So, what does this mean if you’re among the 25% of physicians in the Medscape report who do not have a religious or spiritual leaning and aren’t apt to be spiritually minded when it comes to your patients? An article on KevinMD.com points out that atheist physicians are often in the closet about their atheism because they usually bow their heads or keep a respectful silence when a patient or their family offers a prayer request before surgery or a prayer of thanks after a procedure.
The retired atheist physician who wrote the piece reminds us that nonreligious doctors are good people with a high moral compass who may not believe in an afterlife. However, that means they try to make their patients’ quality of life the best they can.
A version of this article first appeared on Medscape.com.
Whether you’re spiritual, religious – or neither – the Medscape Physician Lifestyle & Happiness Report 2023 asked if you have a religious or spiritual belief. Turns out 69% of physicians shared that they have a spiritual or religious practice.
Tapping into the universe
Nick Shamie, MD, an orthopedic surgeon specializing in spine surgery at University of California, Los Angeles, says the constant challenges of making life-and-death decisions offer an opportunity to check in with a higher power.
“Sometimes when I’m going into a tough surgery or have a tough situation, I pause and think about how this isn’t about me and the situation I’m in,” says Dr. Shamie, whose family is Muslim. “It’s about the whole universe. I feel like someone, or some being, is looking over my shoulders, and if my intentions are good, I’ll be fine. The person I’m going to take care of will be fine. That’s how I use my faith.”
Having a belief in something greater than herself also fuels Jill Carnahan, MD, a family medicine physician and functional medicine expert in Boulder, Colo.
“This is key for me as a physician,” says Dr. Carnahan, author of “Unexpected: Finding Resilience Through Functional Medicine, Science, and Faith.” “I urge physicians to think about their source of strength. That’s not necessarily even religious. It could be meditation or being in nature.”
Dr. Carnahan likes to share with patients that there are lessons that can come from being ill – whether treating ill patients or struggling with one’s own illness.
“I like to teach this idea of illness as a teacher,” says Dr. Carnahan, who has Crohn’s disease and is a cancer survivor. “This is tough, but what you’re saying here is that there is meaning or purpose to this experience. It brings awareness to your life that may not have been there before.”
Often illness is our body’s way of getting our attention that our life, relationships, or work needs adjustment. Illness can be a reminder to make changes. “For example, a diagnosis of autoimmunity may be a reminder to take better care of ourselves, or a diagnosis of cancer may cause us to get out of an unhealthy relationship or change jobs to do something more fulfilling, as we have increased awareness of the brevity of life.”
When patients are affected by illness, pain, reduced functionality, and even imminent death, understanding the experience is difficult, and finding any purpose in it may seem impossible. Still, studies show that those who find meaning in the experience cope better with their illness.
Finding that meaning may be a strong driver of survival and may be positively related to hope, belief, and happiness.
Spirituality supports patients
Even if you’re not religious yourself, it can be helpful to support a patient who opts to pray before an arduous procedure, says Sharyar Baradaran, DDS, a periodontist specializing in gum surgery in Beverly Hills, Calif.
“I’ve had patients who go into meditation mode, or they say a prayer before I start surgery,” he says. “I take that opportunity to connect. In that instance, we hold hands. I want them to know that I understand what they’re going through and how they’re trying to find the courage to undergo surgery.”
When Dr. Shamie was a child, his father described religion as embodying the basic tenet of being good to others. “I’ve taken that to heart,” he says. “All religions, all faiths have that as a central premise.”
These doctors agree that when you take the time to stop and hold a patient’s hand, bow your head during their prayer, or acknowledge or speak for a few moments about their faith, especially during a health crisis, surgery, or challenging diagnosis, patients appreciate it and develop an even deeper connection with you.
Dr. Baradaran believes spirituality can play an important role in how health care providers care for patients. Though it may not be widely discussed or reported, and physicians may find little time and space to address patients’ spiritual needs, there is growing sensitivity regarding spirituality in health care. One study found that while physicians understand its importance, nurses are more apt to integrate spirituality into practice.
“No matter the religion, if you’re spiritual, it means you’re listening and being respectful,” says Dr. Baradaran, who is Jewish. “There are times that I’m not familiar with the prayers my patients are saying, but I always take them in, absorb them, and respect them. This allows me to have a deeper connection with them, which is wonderful.”
Dr. Shamie says that he turns to his faith in good times as well as tough ones.
“I see a lot of people who are dealing with very difficult situations, and it’s not their choice to be in this position,” he says. “At those moments, I think to myself how fortunate I am that I’m not experiencing what this individual or family is going through. I do thank God at that time. I appreciate the life I have, and when I witness hardships, it resets my appreciation.”
For Dr. Carnahan, faith is about becoming comfortable with the inevitable uncertainty of life. It’s also about finding ways to tap into the day’s stresses.
“As physicians, we’re workaholics, and one in four of us are burnt out,” she says. “One solution that really works is to step back from the day-to-day grind and find time to pray or meditate or be in nature.”
There are times when a tragedy occurs, and despite your most intense efforts, a patient may die. Those experiences can be crushing to a physician. However, to guide you through the loss of a patient or the daily juggles of managing your practice, Dr. Carnahan suggests finding time every morning to focus on the day ahead and how you connect with the universe.
“I take 15 minutes in the morning and think about how I will bring love to the world,” she says. “If you look for the miracles and the good and the unexpected, that gratitude shift allows your mind to be transformed by what’s happening. It’s often in those moments that you’ll realize again why you went into medicine in the first place.”
Doctors without faith
So, what does this mean if you’re among the 25% of physicians in the Medscape report who do not have a religious or spiritual leaning and aren’t apt to be spiritually minded when it comes to your patients? An article on KevinMD.com points out that atheist physicians are often in the closet about their atheism because they usually bow their heads or keep a respectful silence when a patient or their family offers a prayer request before surgery or a prayer of thanks after a procedure.
The retired atheist physician who wrote the piece reminds us that nonreligious doctors are good people with a high moral compass who may not believe in an afterlife. However, that means they try to make their patients’ quality of life the best they can.
A version of this article first appeared on Medscape.com.
Whether you’re spiritual, religious – or neither – the Medscape Physician Lifestyle & Happiness Report 2023 asked if you have a religious or spiritual belief. Turns out 69% of physicians shared that they have a spiritual or religious practice.
Tapping into the universe
Nick Shamie, MD, an orthopedic surgeon specializing in spine surgery at University of California, Los Angeles, says the constant challenges of making life-and-death decisions offer an opportunity to check in with a higher power.
“Sometimes when I’m going into a tough surgery or have a tough situation, I pause and think about how this isn’t about me and the situation I’m in,” says Dr. Shamie, whose family is Muslim. “It’s about the whole universe. I feel like someone, or some being, is looking over my shoulders, and if my intentions are good, I’ll be fine. The person I’m going to take care of will be fine. That’s how I use my faith.”
Having a belief in something greater than herself also fuels Jill Carnahan, MD, a family medicine physician and functional medicine expert in Boulder, Colo.
“This is key for me as a physician,” says Dr. Carnahan, author of “Unexpected: Finding Resilience Through Functional Medicine, Science, and Faith.” “I urge physicians to think about their source of strength. That’s not necessarily even religious. It could be meditation or being in nature.”
Dr. Carnahan likes to share with patients that there are lessons that can come from being ill – whether treating ill patients or struggling with one’s own illness.
“I like to teach this idea of illness as a teacher,” says Dr. Carnahan, who has Crohn’s disease and is a cancer survivor. “This is tough, but what you’re saying here is that there is meaning or purpose to this experience. It brings awareness to your life that may not have been there before.”
Often illness is our body’s way of getting our attention that our life, relationships, or work needs adjustment. Illness can be a reminder to make changes. “For example, a diagnosis of autoimmunity may be a reminder to take better care of ourselves, or a diagnosis of cancer may cause us to get out of an unhealthy relationship or change jobs to do something more fulfilling, as we have increased awareness of the brevity of life.”
When patients are affected by illness, pain, reduced functionality, and even imminent death, understanding the experience is difficult, and finding any purpose in it may seem impossible. Still, studies show that those who find meaning in the experience cope better with their illness.
Finding that meaning may be a strong driver of survival and may be positively related to hope, belief, and happiness.
Spirituality supports patients
Even if you’re not religious yourself, it can be helpful to support a patient who opts to pray before an arduous procedure, says Sharyar Baradaran, DDS, a periodontist specializing in gum surgery in Beverly Hills, Calif.
“I’ve had patients who go into meditation mode, or they say a prayer before I start surgery,” he says. “I take that opportunity to connect. In that instance, we hold hands. I want them to know that I understand what they’re going through and how they’re trying to find the courage to undergo surgery.”
When Dr. Shamie was a child, his father described religion as embodying the basic tenet of being good to others. “I’ve taken that to heart,” he says. “All religions, all faiths have that as a central premise.”
These doctors agree that when you take the time to stop and hold a patient’s hand, bow your head during their prayer, or acknowledge or speak for a few moments about their faith, especially during a health crisis, surgery, or challenging diagnosis, patients appreciate it and develop an even deeper connection with you.
Dr. Baradaran believes spirituality can play an important role in how health care providers care for patients. Though it may not be widely discussed or reported, and physicians may find little time and space to address patients’ spiritual needs, there is growing sensitivity regarding spirituality in health care. One study found that while physicians understand its importance, nurses are more apt to integrate spirituality into practice.
“No matter the religion, if you’re spiritual, it means you’re listening and being respectful,” says Dr. Baradaran, who is Jewish. “There are times that I’m not familiar with the prayers my patients are saying, but I always take them in, absorb them, and respect them. This allows me to have a deeper connection with them, which is wonderful.”
Dr. Shamie says that he turns to his faith in good times as well as tough ones.
“I see a lot of people who are dealing with very difficult situations, and it’s not their choice to be in this position,” he says. “At those moments, I think to myself how fortunate I am that I’m not experiencing what this individual or family is going through. I do thank God at that time. I appreciate the life I have, and when I witness hardships, it resets my appreciation.”
For Dr. Carnahan, faith is about becoming comfortable with the inevitable uncertainty of life. It’s also about finding ways to tap into the day’s stresses.
“As physicians, we’re workaholics, and one in four of us are burnt out,” she says. “One solution that really works is to step back from the day-to-day grind and find time to pray or meditate or be in nature.”
There are times when a tragedy occurs, and despite your most intense efforts, a patient may die. Those experiences can be crushing to a physician. However, to guide you through the loss of a patient or the daily juggles of managing your practice, Dr. Carnahan suggests finding time every morning to focus on the day ahead and how you connect with the universe.
“I take 15 minutes in the morning and think about how I will bring love to the world,” she says. “If you look for the miracles and the good and the unexpected, that gratitude shift allows your mind to be transformed by what’s happening. It’s often in those moments that you’ll realize again why you went into medicine in the first place.”
Doctors without faith
So, what does this mean if you’re among the 25% of physicians in the Medscape report who do not have a religious or spiritual leaning and aren’t apt to be spiritually minded when it comes to your patients? An article on KevinMD.com points out that atheist physicians are often in the closet about their atheism because they usually bow their heads or keep a respectful silence when a patient or their family offers a prayer request before surgery or a prayer of thanks after a procedure.
The retired atheist physician who wrote the piece reminds us that nonreligious doctors are good people with a high moral compass who may not believe in an afterlife. However, that means they try to make their patients’ quality of life the best they can.
A version of this article first appeared on Medscape.com.
Physician group staffing down, expenses up, new reports show
Physician groups saw staff-to-physician ratios decline even as their workforce expenses rose between 2019 and 2021, according to recent reports from the American Medical Group Association (AMGA) and the Medical Group Management Association (MGMA).
As patients started to return to doctors’ offices as the pandemic eased in 2021, physician groups found it increasingly difficult to recruit and retain lower-level clinicians, including medical assistants and LPNs, officials from both associations told this news organization. Many clinics had to raise their pay scales to be competitive with employers in other fields, and some had to hire higher-priced RNs to keep their practices running.
The AMGA report was based largely on data from groups of over 500 physicians, mostly affiliated with health systems. According to a news release accompanying the report, the ratio between full-time equivalent (FTE) clinic staff and health care professionals in direct patient care dropped by 11.3% between 2019 and 2021. The ratio of medical assistants (MAs) to clinicians declined by a greater percentage.
In the MGMA report, which represented about 4,000 practices ranging from very small (two doctors) to very large groups, total support staff per FTE primary-care physician dropped by 18% from 2019 to 2021 in independent groups and by 13% in hospital-affiliated groups. The ratios decreased by smaller amounts in surgical practices.
In contrast, nonsurgical specialty groups under both types of ownership saw their staffing ratios rise slightly.
Although it’s unclear why medical specialties increased their staff while other types of specialties lost employees, Ron Holder, MHA, chief operating officer of MGMA, said that some specialists may have opened more ancillary facilities and hired new employees to recoup revenue lost during the pandemic.
Expenses rise sharply
The AMGA report found that staffing expenses for the surveyed groups increased by 15% between 2019 and 2021.
“We saw a decrease in staff and an increase in expenses during that time period, and there are a few reasons for that,” Rose Wagner, RN, chief operating officer of AMGA, said. “Groups increased salaries to maintain staff. We also saw lower-paid staff find other jobs outside of health care. For example, medical assistants and receptionists could find jobs outside of health care that paid more. [Open positions] got back-filled with other higher paid staff, such as RNs, doing lower skilled jobs.”
Mr. Holder added that rising wages in other sectors made leaving physician groups more attractive for employees.
“Three years ago, there weren’t many positions in a medical practice where you were competing with Chick-fil-A or Taco Bell,” he said. In Denver, where Mr. Holder is based, “every restaurant in town is now advertising $17-$19 [hourly] starting pay just to do fast food. That causes practices to either lose employees or pay more for the employees they have. So that raises per-employee expense significantly,” he said.
Mr. Holder noted that inflation also has driven up wages as employees demand higher pay to keep up with the cost of living.
Unusual exodus of employees
Fred Horton, MHA, president of AMGA Consulting, said he has never seen so many people leaving health care for other occupations.
Some exits resulted from practices laying people off early in the pandemic, but most staff members who left practices were seeking higher pay, he said. In addition, Ms. Wagner noted, some staff members didn’t want to be exposed to COVID at work.
“There was an exodus from health care that was different from what we’d experienced in the past,” Mr. Horton added. “It’s still extremely challenging to get up to the staffing levels that are appropriate.”
Mr. Holder, however, said that the situation is slowly improving. “Health care is fairly recession-proof, because people need it. So when you see companies in other industries closing shop or reducing their head count, that actually helps health care recruiting in some jobs. And people are coming back to the workplace who previously were worried about COVID or didn’t want to get the vaccine.”
Paying more for nurses
In 2021, groups adopted a variety of tactics to adapt to the pandemic and respond to patient demand, the AMGA survey shows. Forty percent of system-affiliated groups and 18% of independent practices changed registered nurses’ responsibilities, in many cases having them do the work of medical assistants who were in short supply.
Some practices hired RNs, who have historically been utilized less by primary care than by surgical specialties, Mr. Holder noted. Other clinics paid temp agencies to supply nurses at a steep cost.
“When you’re short staffed, you end up paying more overtime, you end up paying temporary agencies at higher dollars, and you hire higher skilled people to do lower-skilled work,” Ms. Wagner said.
Meanwhile, many physician groups tried to cope with the physician shortage by bringing on more advanced practice clinicians (APCs), including nurse practitioners (NPs) and physician assistants (PAs). Seventy percent of the AMGA groups used this strategy, the report revealed.
“The use of APCs has been steadily increasing as groups try to adopt a lower-cost care model in the midst of a nationwide physician shortage,” Ms. Wagner said in the press release.
Changes in patient care
About half of the groups in the AMGA survey said they changed their staff structure to allow APCs to carry their own patient panels. Although most of these clinicians were probably under physician supervision, nearly half of the states now allow NPs to practice autonomously.
Mr. Horton cautioned that APCs can’t fully substitute for physicians and require the same support staff that doctors do if they have their own panels. In primary care groups, Mr. Holder noted, the average salary of an APC “is continuing to rise, and there isn’t a huge difference between what they and doctors make.”
Nevertheless, he added, “there are more NPs and PAs being added to the marketplace all the time, whereas [physician] residency programs aren’t really growing. There are caps on the number of residency positions, and some physicians are retiring. So the clock is ticking to the point where someday doctors will be grossly outnumbered by NPs.”
A version of this article first appeared on Medscape.com.
Physician groups saw staff-to-physician ratios decline even as their workforce expenses rose between 2019 and 2021, according to recent reports from the American Medical Group Association (AMGA) and the Medical Group Management Association (MGMA).
As patients started to return to doctors’ offices as the pandemic eased in 2021, physician groups found it increasingly difficult to recruit and retain lower-level clinicians, including medical assistants and LPNs, officials from both associations told this news organization. Many clinics had to raise their pay scales to be competitive with employers in other fields, and some had to hire higher-priced RNs to keep their practices running.
The AMGA report was based largely on data from groups of over 500 physicians, mostly affiliated with health systems. According to a news release accompanying the report, the ratio between full-time equivalent (FTE) clinic staff and health care professionals in direct patient care dropped by 11.3% between 2019 and 2021. The ratio of medical assistants (MAs) to clinicians declined by a greater percentage.
In the MGMA report, which represented about 4,000 practices ranging from very small (two doctors) to very large groups, total support staff per FTE primary-care physician dropped by 18% from 2019 to 2021 in independent groups and by 13% in hospital-affiliated groups. The ratios decreased by smaller amounts in surgical practices.
In contrast, nonsurgical specialty groups under both types of ownership saw their staffing ratios rise slightly.
Although it’s unclear why medical specialties increased their staff while other types of specialties lost employees, Ron Holder, MHA, chief operating officer of MGMA, said that some specialists may have opened more ancillary facilities and hired new employees to recoup revenue lost during the pandemic.
Expenses rise sharply
The AMGA report found that staffing expenses for the surveyed groups increased by 15% between 2019 and 2021.
“We saw a decrease in staff and an increase in expenses during that time period, and there are a few reasons for that,” Rose Wagner, RN, chief operating officer of AMGA, said. “Groups increased salaries to maintain staff. We also saw lower-paid staff find other jobs outside of health care. For example, medical assistants and receptionists could find jobs outside of health care that paid more. [Open positions] got back-filled with other higher paid staff, such as RNs, doing lower skilled jobs.”
Mr. Holder added that rising wages in other sectors made leaving physician groups more attractive for employees.
“Three years ago, there weren’t many positions in a medical practice where you were competing with Chick-fil-A or Taco Bell,” he said. In Denver, where Mr. Holder is based, “every restaurant in town is now advertising $17-$19 [hourly] starting pay just to do fast food. That causes practices to either lose employees or pay more for the employees they have. So that raises per-employee expense significantly,” he said.
Mr. Holder noted that inflation also has driven up wages as employees demand higher pay to keep up with the cost of living.
Unusual exodus of employees
Fred Horton, MHA, president of AMGA Consulting, said he has never seen so many people leaving health care for other occupations.
Some exits resulted from practices laying people off early in the pandemic, but most staff members who left practices were seeking higher pay, he said. In addition, Ms. Wagner noted, some staff members didn’t want to be exposed to COVID at work.
“There was an exodus from health care that was different from what we’d experienced in the past,” Mr. Horton added. “It’s still extremely challenging to get up to the staffing levels that are appropriate.”
Mr. Holder, however, said that the situation is slowly improving. “Health care is fairly recession-proof, because people need it. So when you see companies in other industries closing shop or reducing their head count, that actually helps health care recruiting in some jobs. And people are coming back to the workplace who previously were worried about COVID or didn’t want to get the vaccine.”
Paying more for nurses
In 2021, groups adopted a variety of tactics to adapt to the pandemic and respond to patient demand, the AMGA survey shows. Forty percent of system-affiliated groups and 18% of independent practices changed registered nurses’ responsibilities, in many cases having them do the work of medical assistants who were in short supply.
Some practices hired RNs, who have historically been utilized less by primary care than by surgical specialties, Mr. Holder noted. Other clinics paid temp agencies to supply nurses at a steep cost.
“When you’re short staffed, you end up paying more overtime, you end up paying temporary agencies at higher dollars, and you hire higher skilled people to do lower-skilled work,” Ms. Wagner said.
Meanwhile, many physician groups tried to cope with the physician shortage by bringing on more advanced practice clinicians (APCs), including nurse practitioners (NPs) and physician assistants (PAs). Seventy percent of the AMGA groups used this strategy, the report revealed.
“The use of APCs has been steadily increasing as groups try to adopt a lower-cost care model in the midst of a nationwide physician shortage,” Ms. Wagner said in the press release.
Changes in patient care
About half of the groups in the AMGA survey said they changed their staff structure to allow APCs to carry their own patient panels. Although most of these clinicians were probably under physician supervision, nearly half of the states now allow NPs to practice autonomously.
Mr. Horton cautioned that APCs can’t fully substitute for physicians and require the same support staff that doctors do if they have their own panels. In primary care groups, Mr. Holder noted, the average salary of an APC “is continuing to rise, and there isn’t a huge difference between what they and doctors make.”
Nevertheless, he added, “there are more NPs and PAs being added to the marketplace all the time, whereas [physician] residency programs aren’t really growing. There are caps on the number of residency positions, and some physicians are retiring. So the clock is ticking to the point where someday doctors will be grossly outnumbered by NPs.”
A version of this article first appeared on Medscape.com.
Physician groups saw staff-to-physician ratios decline even as their workforce expenses rose between 2019 and 2021, according to recent reports from the American Medical Group Association (AMGA) and the Medical Group Management Association (MGMA).
As patients started to return to doctors’ offices as the pandemic eased in 2021, physician groups found it increasingly difficult to recruit and retain lower-level clinicians, including medical assistants and LPNs, officials from both associations told this news organization. Many clinics had to raise their pay scales to be competitive with employers in other fields, and some had to hire higher-priced RNs to keep their practices running.
The AMGA report was based largely on data from groups of over 500 physicians, mostly affiliated with health systems. According to a news release accompanying the report, the ratio between full-time equivalent (FTE) clinic staff and health care professionals in direct patient care dropped by 11.3% between 2019 and 2021. The ratio of medical assistants (MAs) to clinicians declined by a greater percentage.
In the MGMA report, which represented about 4,000 practices ranging from very small (two doctors) to very large groups, total support staff per FTE primary-care physician dropped by 18% from 2019 to 2021 in independent groups and by 13% in hospital-affiliated groups. The ratios decreased by smaller amounts in surgical practices.
In contrast, nonsurgical specialty groups under both types of ownership saw their staffing ratios rise slightly.
Although it’s unclear why medical specialties increased their staff while other types of specialties lost employees, Ron Holder, MHA, chief operating officer of MGMA, said that some specialists may have opened more ancillary facilities and hired new employees to recoup revenue lost during the pandemic.
Expenses rise sharply
The AMGA report found that staffing expenses for the surveyed groups increased by 15% between 2019 and 2021.
“We saw a decrease in staff and an increase in expenses during that time period, and there are a few reasons for that,” Rose Wagner, RN, chief operating officer of AMGA, said. “Groups increased salaries to maintain staff. We also saw lower-paid staff find other jobs outside of health care. For example, medical assistants and receptionists could find jobs outside of health care that paid more. [Open positions] got back-filled with other higher paid staff, such as RNs, doing lower skilled jobs.”
Mr. Holder added that rising wages in other sectors made leaving physician groups more attractive for employees.
“Three years ago, there weren’t many positions in a medical practice where you were competing with Chick-fil-A or Taco Bell,” he said. In Denver, where Mr. Holder is based, “every restaurant in town is now advertising $17-$19 [hourly] starting pay just to do fast food. That causes practices to either lose employees or pay more for the employees they have. So that raises per-employee expense significantly,” he said.
Mr. Holder noted that inflation also has driven up wages as employees demand higher pay to keep up with the cost of living.
Unusual exodus of employees
Fred Horton, MHA, president of AMGA Consulting, said he has never seen so many people leaving health care for other occupations.
Some exits resulted from practices laying people off early in the pandemic, but most staff members who left practices were seeking higher pay, he said. In addition, Ms. Wagner noted, some staff members didn’t want to be exposed to COVID at work.
“There was an exodus from health care that was different from what we’d experienced in the past,” Mr. Horton added. “It’s still extremely challenging to get up to the staffing levels that are appropriate.”
Mr. Holder, however, said that the situation is slowly improving. “Health care is fairly recession-proof, because people need it. So when you see companies in other industries closing shop or reducing their head count, that actually helps health care recruiting in some jobs. And people are coming back to the workplace who previously were worried about COVID or didn’t want to get the vaccine.”
Paying more for nurses
In 2021, groups adopted a variety of tactics to adapt to the pandemic and respond to patient demand, the AMGA survey shows. Forty percent of system-affiliated groups and 18% of independent practices changed registered nurses’ responsibilities, in many cases having them do the work of medical assistants who were in short supply.
Some practices hired RNs, who have historically been utilized less by primary care than by surgical specialties, Mr. Holder noted. Other clinics paid temp agencies to supply nurses at a steep cost.
“When you’re short staffed, you end up paying more overtime, you end up paying temporary agencies at higher dollars, and you hire higher skilled people to do lower-skilled work,” Ms. Wagner said.
Meanwhile, many physician groups tried to cope with the physician shortage by bringing on more advanced practice clinicians (APCs), including nurse practitioners (NPs) and physician assistants (PAs). Seventy percent of the AMGA groups used this strategy, the report revealed.
“The use of APCs has been steadily increasing as groups try to adopt a lower-cost care model in the midst of a nationwide physician shortage,” Ms. Wagner said in the press release.
Changes in patient care
About half of the groups in the AMGA survey said they changed their staff structure to allow APCs to carry their own patient panels. Although most of these clinicians were probably under physician supervision, nearly half of the states now allow NPs to practice autonomously.
Mr. Horton cautioned that APCs can’t fully substitute for physicians and require the same support staff that doctors do if they have their own panels. In primary care groups, Mr. Holder noted, the average salary of an APC “is continuing to rise, and there isn’t a huge difference between what they and doctors make.”
Nevertheless, he added, “there are more NPs and PAs being added to the marketplace all the time, whereas [physician] residency programs aren’t really growing. There are caps on the number of residency positions, and some physicians are retiring. So the clock is ticking to the point where someday doctors will be grossly outnumbered by NPs.”
A version of this article first appeared on Medscape.com.
Doctors and their families tend to ignore medical guidelines
according to a study by economic professors from the Massachusetts Institute of Technology, Cambridge; Stanford (Calif.) University; and the George Gund Professor of Economics and Business Administration at Harvard University, Boston.
What to know
- Doctors’ medical knowledge may influence them and their families to often ignore medical advice while the rest of the population adheres to general medication guidelines.
- Of the 63 guidelines used in the study, doctors and their families followed the standards less than a third of the time.
- The difference in adherence to guidelines between experts and nonexperts is largest with respect to antibiotics, in which doctors and their families are 5.2 percentage points less in compliance than everyone else.
- Doctors could be more likely to prescribe broader-spectrum antibiotics for themselves and their families, whereas most patients receive more narrow-spectrum antibiotics.
- Many members of the general public don’t understand medical guidelines, finding them too complex to follow, and many people don’t trust their doctors.
This is a summary of the article, “A Taste of Their Own Medicine: Guideline Adherence and Access to Expertise,” published in the American Economic Review: Insights on December 13, 2022. The full article can be found on aeaweb.org.
A version of this article first appeared on Medscape.com.
according to a study by economic professors from the Massachusetts Institute of Technology, Cambridge; Stanford (Calif.) University; and the George Gund Professor of Economics and Business Administration at Harvard University, Boston.
What to know
- Doctors’ medical knowledge may influence them and their families to often ignore medical advice while the rest of the population adheres to general medication guidelines.
- Of the 63 guidelines used in the study, doctors and their families followed the standards less than a third of the time.
- The difference in adherence to guidelines between experts and nonexperts is largest with respect to antibiotics, in which doctors and their families are 5.2 percentage points less in compliance than everyone else.
- Doctors could be more likely to prescribe broader-spectrum antibiotics for themselves and their families, whereas most patients receive more narrow-spectrum antibiotics.
- Many members of the general public don’t understand medical guidelines, finding them too complex to follow, and many people don’t trust their doctors.
This is a summary of the article, “A Taste of Their Own Medicine: Guideline Adherence and Access to Expertise,” published in the American Economic Review: Insights on December 13, 2022. The full article can be found on aeaweb.org.
A version of this article first appeared on Medscape.com.
according to a study by economic professors from the Massachusetts Institute of Technology, Cambridge; Stanford (Calif.) University; and the George Gund Professor of Economics and Business Administration at Harvard University, Boston.
What to know
- Doctors’ medical knowledge may influence them and their families to often ignore medical advice while the rest of the population adheres to general medication guidelines.
- Of the 63 guidelines used in the study, doctors and their families followed the standards less than a third of the time.
- The difference in adherence to guidelines between experts and nonexperts is largest with respect to antibiotics, in which doctors and their families are 5.2 percentage points less in compliance than everyone else.
- Doctors could be more likely to prescribe broader-spectrum antibiotics for themselves and their families, whereas most patients receive more narrow-spectrum antibiotics.
- Many members of the general public don’t understand medical guidelines, finding them too complex to follow, and many people don’t trust their doctors.
This is a summary of the article, “A Taste of Their Own Medicine: Guideline Adherence and Access to Expertise,” published in the American Economic Review: Insights on December 13, 2022. The full article can be found on aeaweb.org.
A version of this article first appeared on Medscape.com.
Docs with one paid malpractice claim are four times more likely to have another
In this retrospective case-control study, law and public health researchers from Georgetown University, the National Opinion Research Center, the University of Colorado, and Northwestern University analyzed paid malpractice claims for all licensed U.S. physicians.
The findings suggest that a single malpractice claim may not be a random stroke of bad luck but instead holds some predictive power into the risk for future paid claims.
“A four times increase in risk is huge, particularly since we observe a similar increase in both high-risk and lower-risk specialties,” David Hyman, JD, MD, professor of health law and policy at Georgetown University, Washington, and lead researcher on the study, told this news organization. “There are surely some false positives, but there must be lots of actual negligence too, or we would not see these results.”
For the 881,876 physicians analyzed, researchers looked at malpractice claims paid during two 5-year periods: 2009-2013 and 2014-2018. Nearly 96% of physicians had no paid malpractice claims between 2009 and 2013; 3% had one, and less than 1% had multiple claims. The proportion of physicians with paid claims between 2014 and 2018 was similar.
Compared with physicians with no 2009-2013 claims, a physician with just one paid claim in that time period had a 3.7 times higher risk for a future paid claim. Physicians with two paid claims were nearly 7 times more likely to have a future paid claim, and those with three or more paid claims were more than 11 times more likely to have one.
Approximately 3% of physicians with no paid claims between 2009 and 2013 had a future paid claim, growing to 12.4% of those with one paid claim during that time.
The study’s findings may have implications for medical licensing boards and hospitals granting staff privileges.
“After some number of paid claims, there should be an official response” from these entities, such as a hands-on assessment of technical skills or assignment of a peer mentor, said Dr. Hyman, who is also coauthor of a book titled “Medical Malpractice Litigation: How It Works, Why Tort Reform Hasn’t Helped.” A graduated set of interventions, whether voluntary or mandatory, can reduce future claim risk and patient harm, Dr. Hyman added.
Interventions may include error avoidance and post-error communication training, counseling to improve bedside skills, and encouragement to move into nonclinical practice. Either way, Dr. Hyman says a nuanced intervention strategy would be a welcome shift away from the current “all or nothing approach” that too often ends in the revocation of a physician’s medical license.
Although there are strategies to proactively identify physicians with excess risk for malpractice claims and implement preventive measures – like Vanderbilt University’s Patient Advocacy Reporting System, for example – most hospitals and physician groups fail to initiate even informal interventions after a malpractice settlement or verdict, which is a missed opportunity, Dr. Hyman said.
A version of this article first appeared on Medscape.com.
In this retrospective case-control study, law and public health researchers from Georgetown University, the National Opinion Research Center, the University of Colorado, and Northwestern University analyzed paid malpractice claims for all licensed U.S. physicians.
The findings suggest that a single malpractice claim may not be a random stroke of bad luck but instead holds some predictive power into the risk for future paid claims.
“A four times increase in risk is huge, particularly since we observe a similar increase in both high-risk and lower-risk specialties,” David Hyman, JD, MD, professor of health law and policy at Georgetown University, Washington, and lead researcher on the study, told this news organization. “There are surely some false positives, but there must be lots of actual negligence too, or we would not see these results.”
For the 881,876 physicians analyzed, researchers looked at malpractice claims paid during two 5-year periods: 2009-2013 and 2014-2018. Nearly 96% of physicians had no paid malpractice claims between 2009 and 2013; 3% had one, and less than 1% had multiple claims. The proportion of physicians with paid claims between 2014 and 2018 was similar.
Compared with physicians with no 2009-2013 claims, a physician with just one paid claim in that time period had a 3.7 times higher risk for a future paid claim. Physicians with two paid claims were nearly 7 times more likely to have a future paid claim, and those with three or more paid claims were more than 11 times more likely to have one.
Approximately 3% of physicians with no paid claims between 2009 and 2013 had a future paid claim, growing to 12.4% of those with one paid claim during that time.
The study’s findings may have implications for medical licensing boards and hospitals granting staff privileges.
“After some number of paid claims, there should be an official response” from these entities, such as a hands-on assessment of technical skills or assignment of a peer mentor, said Dr. Hyman, who is also coauthor of a book titled “Medical Malpractice Litigation: How It Works, Why Tort Reform Hasn’t Helped.” A graduated set of interventions, whether voluntary or mandatory, can reduce future claim risk and patient harm, Dr. Hyman added.
Interventions may include error avoidance and post-error communication training, counseling to improve bedside skills, and encouragement to move into nonclinical practice. Either way, Dr. Hyman says a nuanced intervention strategy would be a welcome shift away from the current “all or nothing approach” that too often ends in the revocation of a physician’s medical license.
Although there are strategies to proactively identify physicians with excess risk for malpractice claims and implement preventive measures – like Vanderbilt University’s Patient Advocacy Reporting System, for example – most hospitals and physician groups fail to initiate even informal interventions after a malpractice settlement or verdict, which is a missed opportunity, Dr. Hyman said.
A version of this article first appeared on Medscape.com.
In this retrospective case-control study, law and public health researchers from Georgetown University, the National Opinion Research Center, the University of Colorado, and Northwestern University analyzed paid malpractice claims for all licensed U.S. physicians.
The findings suggest that a single malpractice claim may not be a random stroke of bad luck but instead holds some predictive power into the risk for future paid claims.
“A four times increase in risk is huge, particularly since we observe a similar increase in both high-risk and lower-risk specialties,” David Hyman, JD, MD, professor of health law and policy at Georgetown University, Washington, and lead researcher on the study, told this news organization. “There are surely some false positives, but there must be lots of actual negligence too, or we would not see these results.”
For the 881,876 physicians analyzed, researchers looked at malpractice claims paid during two 5-year periods: 2009-2013 and 2014-2018. Nearly 96% of physicians had no paid malpractice claims between 2009 and 2013; 3% had one, and less than 1% had multiple claims. The proportion of physicians with paid claims between 2014 and 2018 was similar.
Compared with physicians with no 2009-2013 claims, a physician with just one paid claim in that time period had a 3.7 times higher risk for a future paid claim. Physicians with two paid claims were nearly 7 times more likely to have a future paid claim, and those with three or more paid claims were more than 11 times more likely to have one.
Approximately 3% of physicians with no paid claims between 2009 and 2013 had a future paid claim, growing to 12.4% of those with one paid claim during that time.
The study’s findings may have implications for medical licensing boards and hospitals granting staff privileges.
“After some number of paid claims, there should be an official response” from these entities, such as a hands-on assessment of technical skills or assignment of a peer mentor, said Dr. Hyman, who is also coauthor of a book titled “Medical Malpractice Litigation: How It Works, Why Tort Reform Hasn’t Helped.” A graduated set of interventions, whether voluntary or mandatory, can reduce future claim risk and patient harm, Dr. Hyman added.
Interventions may include error avoidance and post-error communication training, counseling to improve bedside skills, and encouragement to move into nonclinical practice. Either way, Dr. Hyman says a nuanced intervention strategy would be a welcome shift away from the current “all or nothing approach” that too often ends in the revocation of a physician’s medical license.
Although there are strategies to proactively identify physicians with excess risk for malpractice claims and implement preventive measures – like Vanderbilt University’s Patient Advocacy Reporting System, for example – most hospitals and physician groups fail to initiate even informal interventions after a malpractice settlement or verdict, which is a missed opportunity, Dr. Hyman said.
A version of this article first appeared on Medscape.com.
FROM JAMA
Oncologist stars in film and shares philosophy on death
When New York oncologist Gabriel Sara, MD, approached the French actress and film director Emmanuelle Bercot after a screening of one of her films in Manhattan, he was thinking big.
He never dreamed she would think bigger.
“I thought maybe she will do a movie about some of my beliefs,” he said.
“Ma’am, would you like to go in the trenches of cancer?” he asked her, inviting her to tour the oncology department at Mount Sinai West.
Whether it was the Lebanese-born doctor’s Parisian French, his gentle, double-handed handshake, or the perpetual twinkle in his eye, something convinced Ms. Bercot to go. After the visit, she decided to base an entire film on the doctor’s philosophy about death, and she even cast him as one of the leads.
With no formal training in acting, “it’s incredible and prodigious what he did,” Ms. Bercot said in an interview at the 2021 Cannes Film Festival, where the film, “Peaceful” (“De Son Vivant”) premiered.
she said.
Dr. Sara said that authenticity came easily, given that “a lot of my dialogue – maybe most – came from things I shared with Emmanuelle,” he said in an interview with this news organization. “She took the information from me, and she created the whole story. She studied my character and came up with really all the messages that I was hoping to share.”
He said that acting alongside professionals was not intimidating once he realized he was simply playing himself. “At some point ... it clicked in my head. Let me stop acting – I should just be me,” he recalled.
“Peaceful,” performed in French with English subtitles, was nominated for Best Film at the 2022 Lumières Awards.
It tells the story of a 39-year-old man (played by French actor Beno
It is also the story of an oncologist, played by Dr. Sara as himself, who takes his patient by the hand, and refuses to sugarcoat the truth, because he believes that it is only by facing the facts that patients can continue to live – and then die – in peace.
“You’ll never hear me say I’ll cure your cancer. I’d be a liar if I did,” he tells his patient in the film.
“Patients put their life in your hands, so if you don’t tell them the truth you are betraying them,” he explained in the interview. “I have refused to see patients whose family did not allow them to come to the consultation to hear the truth. ... Nobody hears the truth and feels great about it the next day, but the truth helps them focus on what they need to deal with. And once they focus, they’re in control ... a big part of what is terrible for patients is that loss of control.”
The approach may sound harsh, but it is conveyed tenderly in the film. “[Your mother] thinks that half-truths will hurt you half as much,” he tells his patient gently, but “the scariest thing is realizing someone is lying to you. ... We have a tough journey ahead, there’s no room for lies. ... For me, truth is nonnegotiable.”
Dr. Sara is brimming with stories of real-life patients whose lives were enriched and empowered by the clarity they gained in knowing the full truth.
However, not all oncologists agree with his style.
After screenings of the film in other parts of the world, and even in the United States, he has encountered some physicians who strongly disagree with his uncompromising honesty. “You always have somebody who says you know, in America, you will receive the truth but not in our culture – people are not used to it. I hear this all the time,” he said.
“And a long time ago, I decided I’m not going to accept that conversation. Truth works with all patients across all cultures,” Dr. Sara insisted.
“However, as caregivers, we have to be sensitive and present to the kind of culture we are dealing with. The content has to be always 100% honest but we adapt our language to the cultural and emotional state of the patient in order to successfully transmit the message,” he added.
Helping patients digest the news of their diagnosis and prognosis has been Dr. Sara’s recipe for his own survival at work. Now 68 and recently retired as medical director of the chemotherapy infusion suite and executive director of the patient services initiative at Mount Sinai West, he says he emerged from 40 years of practice without burning out by learning to step in time with each patient.
“My recipe for it is tango,” he said. Regular tango performances on his cancer ward were among his many real-life techniques that Ms. Bercot incorporated into the film. “I feel that we have to dance closely with our patients’ emotion,” he explained. “We have to feel our patients’ emotion and work with that. If you don’t move in harmony with your partner, you trip together and both of you will fall,” he told an audience after a screening of his film in New York City.
“I completely try to isolate my mind from anything else in order to be with the patient – this is what presence is about for me – to be right there for them, close to them. To spend that whole moment with them. That’s what will make the consultation really helpful, and will make me feel that I can move to the next page without feeling exhausted from the first one.”
A key scene in the film comes after the patient’s mother is stunned to discover a cheerful tango performance on her son’s ward, and confronts the doctor angrily.
“It’s like I’m abandoning him,” she says tearfully, when the doctor urges her to accept that her son’s chemotherapy is no longer working and let him live what life he has left.
“Give him permission to go,” he urges her. “It would be your greatest gift of love.”
Dr. Sara encourages a similar approach in his staff. He warns them about the “hero syndrome,” in which dying patients are made to feel they need to “hang on” and “fight” for the sake of their caregivers and families.
“The patient never asked to be the hero, but our attitude is telling him that he’s the hero,” he says in the film. “That puts him in an intolerable impasse because he figures that if he gives up, if he dies, he’s betraying his fans. He needs the exact opposite: to be set free. He needs the permission to die. That permission is given by two people: his doctor and his family.”
Of course, not all cancer patients have such a dim prognosis, and Dr. Sara is the first to forge ahead if he feels it’s appropriate. “If, if there is no option for them, I’m going to be aggressive to protect them. But when there is a curable disease, I will go broke to try to treat my patient. I’m willing to give them toxic drugs and hold their hand, get them through the storm if I believe it’s going to cure what they have, and I will coach them to accept being sick.”
He also believes in physical contact with the patient. “If we have some intimacy with the patient, we can at least palpate the kind of person they are,” he said. But his wife Nada pointed out that physical examinations can sometimes make patients nervous. “She told me, if you have a tie, they might have fun looking at it.” Thus began Dr. Sara’s collection of about 30 fun ties decorated with unicorns or jellyfish tailored to various patients’ preferences.
In the film, his patient teases him about this quirk, but Dr. Sara insists it is a small gesture that carries meaning. “One patient told me a story about lovebugs. She would see them in her kitchen when she was feeling well – so lovebugs became a sign of hope for her. I was telling the story to my wife ... so she got me a tie with lovebugs on it, and my patient was so happy when she saw me wearing that.”
In the film – and in real life – Dr. Sara often played guitar at breakfast music sessions with his staff in which he encouraged them to express their feelings about patients’ struggles. “If you cry, don’t be ashamed. Your patient will feel you’re with him,” he said in the film. In the final scenes, wearing a cloud-covered tie, he says goodbye to his patient with tears in his eyes. “They [the tears] are sincere,” he recalled. “Because I really felt I was looking at a dying patient. I really did.”
A version of this article first appeared on Medscape.com.
When New York oncologist Gabriel Sara, MD, approached the French actress and film director Emmanuelle Bercot after a screening of one of her films in Manhattan, he was thinking big.
He never dreamed she would think bigger.
“I thought maybe she will do a movie about some of my beliefs,” he said.
“Ma’am, would you like to go in the trenches of cancer?” he asked her, inviting her to tour the oncology department at Mount Sinai West.
Whether it was the Lebanese-born doctor’s Parisian French, his gentle, double-handed handshake, or the perpetual twinkle in his eye, something convinced Ms. Bercot to go. After the visit, she decided to base an entire film on the doctor’s philosophy about death, and she even cast him as one of the leads.
With no formal training in acting, “it’s incredible and prodigious what he did,” Ms. Bercot said in an interview at the 2021 Cannes Film Festival, where the film, “Peaceful” (“De Son Vivant”) premiered.
she said.
Dr. Sara said that authenticity came easily, given that “a lot of my dialogue – maybe most – came from things I shared with Emmanuelle,” he said in an interview with this news organization. “She took the information from me, and she created the whole story. She studied my character and came up with really all the messages that I was hoping to share.”
He said that acting alongside professionals was not intimidating once he realized he was simply playing himself. “At some point ... it clicked in my head. Let me stop acting – I should just be me,” he recalled.
“Peaceful,” performed in French with English subtitles, was nominated for Best Film at the 2022 Lumières Awards.
It tells the story of a 39-year-old man (played by French actor Beno
It is also the story of an oncologist, played by Dr. Sara as himself, who takes his patient by the hand, and refuses to sugarcoat the truth, because he believes that it is only by facing the facts that patients can continue to live – and then die – in peace.
“You’ll never hear me say I’ll cure your cancer. I’d be a liar if I did,” he tells his patient in the film.
“Patients put their life in your hands, so if you don’t tell them the truth you are betraying them,” he explained in the interview. “I have refused to see patients whose family did not allow them to come to the consultation to hear the truth. ... Nobody hears the truth and feels great about it the next day, but the truth helps them focus on what they need to deal with. And once they focus, they’re in control ... a big part of what is terrible for patients is that loss of control.”
The approach may sound harsh, but it is conveyed tenderly in the film. “[Your mother] thinks that half-truths will hurt you half as much,” he tells his patient gently, but “the scariest thing is realizing someone is lying to you. ... We have a tough journey ahead, there’s no room for lies. ... For me, truth is nonnegotiable.”
Dr. Sara is brimming with stories of real-life patients whose lives were enriched and empowered by the clarity they gained in knowing the full truth.
However, not all oncologists agree with his style.
After screenings of the film in other parts of the world, and even in the United States, he has encountered some physicians who strongly disagree with his uncompromising honesty. “You always have somebody who says you know, in America, you will receive the truth but not in our culture – people are not used to it. I hear this all the time,” he said.
“And a long time ago, I decided I’m not going to accept that conversation. Truth works with all patients across all cultures,” Dr. Sara insisted.
“However, as caregivers, we have to be sensitive and present to the kind of culture we are dealing with. The content has to be always 100% honest but we adapt our language to the cultural and emotional state of the patient in order to successfully transmit the message,” he added.
Helping patients digest the news of their diagnosis and prognosis has been Dr. Sara’s recipe for his own survival at work. Now 68 and recently retired as medical director of the chemotherapy infusion suite and executive director of the patient services initiative at Mount Sinai West, he says he emerged from 40 years of practice without burning out by learning to step in time with each patient.
“My recipe for it is tango,” he said. Regular tango performances on his cancer ward were among his many real-life techniques that Ms. Bercot incorporated into the film. “I feel that we have to dance closely with our patients’ emotion,” he explained. “We have to feel our patients’ emotion and work with that. If you don’t move in harmony with your partner, you trip together and both of you will fall,” he told an audience after a screening of his film in New York City.
“I completely try to isolate my mind from anything else in order to be with the patient – this is what presence is about for me – to be right there for them, close to them. To spend that whole moment with them. That’s what will make the consultation really helpful, and will make me feel that I can move to the next page without feeling exhausted from the first one.”
A key scene in the film comes after the patient’s mother is stunned to discover a cheerful tango performance on her son’s ward, and confronts the doctor angrily.
“It’s like I’m abandoning him,” she says tearfully, when the doctor urges her to accept that her son’s chemotherapy is no longer working and let him live what life he has left.
“Give him permission to go,” he urges her. “It would be your greatest gift of love.”
Dr. Sara encourages a similar approach in his staff. He warns them about the “hero syndrome,” in which dying patients are made to feel they need to “hang on” and “fight” for the sake of their caregivers and families.
“The patient never asked to be the hero, but our attitude is telling him that he’s the hero,” he says in the film. “That puts him in an intolerable impasse because he figures that if he gives up, if he dies, he’s betraying his fans. He needs the exact opposite: to be set free. He needs the permission to die. That permission is given by two people: his doctor and his family.”
Of course, not all cancer patients have such a dim prognosis, and Dr. Sara is the first to forge ahead if he feels it’s appropriate. “If, if there is no option for them, I’m going to be aggressive to protect them. But when there is a curable disease, I will go broke to try to treat my patient. I’m willing to give them toxic drugs and hold their hand, get them through the storm if I believe it’s going to cure what they have, and I will coach them to accept being sick.”
He also believes in physical contact with the patient. “If we have some intimacy with the patient, we can at least palpate the kind of person they are,” he said. But his wife Nada pointed out that physical examinations can sometimes make patients nervous. “She told me, if you have a tie, they might have fun looking at it.” Thus began Dr. Sara’s collection of about 30 fun ties decorated with unicorns or jellyfish tailored to various patients’ preferences.
In the film, his patient teases him about this quirk, but Dr. Sara insists it is a small gesture that carries meaning. “One patient told me a story about lovebugs. She would see them in her kitchen when she was feeling well – so lovebugs became a sign of hope for her. I was telling the story to my wife ... so she got me a tie with lovebugs on it, and my patient was so happy when she saw me wearing that.”
In the film – and in real life – Dr. Sara often played guitar at breakfast music sessions with his staff in which he encouraged them to express their feelings about patients’ struggles. “If you cry, don’t be ashamed. Your patient will feel you’re with him,” he said in the film. In the final scenes, wearing a cloud-covered tie, he says goodbye to his patient with tears in his eyes. “They [the tears] are sincere,” he recalled. “Because I really felt I was looking at a dying patient. I really did.”
A version of this article first appeared on Medscape.com.
When New York oncologist Gabriel Sara, MD, approached the French actress and film director Emmanuelle Bercot after a screening of one of her films in Manhattan, he was thinking big.
He never dreamed she would think bigger.
“I thought maybe she will do a movie about some of my beliefs,” he said.
“Ma’am, would you like to go in the trenches of cancer?” he asked her, inviting her to tour the oncology department at Mount Sinai West.
Whether it was the Lebanese-born doctor’s Parisian French, his gentle, double-handed handshake, or the perpetual twinkle in his eye, something convinced Ms. Bercot to go. After the visit, she decided to base an entire film on the doctor’s philosophy about death, and she even cast him as one of the leads.
With no formal training in acting, “it’s incredible and prodigious what he did,” Ms. Bercot said in an interview at the 2021 Cannes Film Festival, where the film, “Peaceful” (“De Son Vivant”) premiered.
she said.
Dr. Sara said that authenticity came easily, given that “a lot of my dialogue – maybe most – came from things I shared with Emmanuelle,” he said in an interview with this news organization. “She took the information from me, and she created the whole story. She studied my character and came up with really all the messages that I was hoping to share.”
He said that acting alongside professionals was not intimidating once he realized he was simply playing himself. “At some point ... it clicked in my head. Let me stop acting – I should just be me,” he recalled.
“Peaceful,” performed in French with English subtitles, was nominated for Best Film at the 2022 Lumières Awards.
It tells the story of a 39-year-old man (played by French actor Beno
It is also the story of an oncologist, played by Dr. Sara as himself, who takes his patient by the hand, and refuses to sugarcoat the truth, because he believes that it is only by facing the facts that patients can continue to live – and then die – in peace.
“You’ll never hear me say I’ll cure your cancer. I’d be a liar if I did,” he tells his patient in the film.
“Patients put their life in your hands, so if you don’t tell them the truth you are betraying them,” he explained in the interview. “I have refused to see patients whose family did not allow them to come to the consultation to hear the truth. ... Nobody hears the truth and feels great about it the next day, but the truth helps them focus on what they need to deal with. And once they focus, they’re in control ... a big part of what is terrible for patients is that loss of control.”
The approach may sound harsh, but it is conveyed tenderly in the film. “[Your mother] thinks that half-truths will hurt you half as much,” he tells his patient gently, but “the scariest thing is realizing someone is lying to you. ... We have a tough journey ahead, there’s no room for lies. ... For me, truth is nonnegotiable.”
Dr. Sara is brimming with stories of real-life patients whose lives were enriched and empowered by the clarity they gained in knowing the full truth.
However, not all oncologists agree with his style.
After screenings of the film in other parts of the world, and even in the United States, he has encountered some physicians who strongly disagree with his uncompromising honesty. “You always have somebody who says you know, in America, you will receive the truth but not in our culture – people are not used to it. I hear this all the time,” he said.
“And a long time ago, I decided I’m not going to accept that conversation. Truth works with all patients across all cultures,” Dr. Sara insisted.
“However, as caregivers, we have to be sensitive and present to the kind of culture we are dealing with. The content has to be always 100% honest but we adapt our language to the cultural and emotional state of the patient in order to successfully transmit the message,” he added.
Helping patients digest the news of their diagnosis and prognosis has been Dr. Sara’s recipe for his own survival at work. Now 68 and recently retired as medical director of the chemotherapy infusion suite and executive director of the patient services initiative at Mount Sinai West, he says he emerged from 40 years of practice without burning out by learning to step in time with each patient.
“My recipe for it is tango,” he said. Regular tango performances on his cancer ward were among his many real-life techniques that Ms. Bercot incorporated into the film. “I feel that we have to dance closely with our patients’ emotion,” he explained. “We have to feel our patients’ emotion and work with that. If you don’t move in harmony with your partner, you trip together and both of you will fall,” he told an audience after a screening of his film in New York City.
“I completely try to isolate my mind from anything else in order to be with the patient – this is what presence is about for me – to be right there for them, close to them. To spend that whole moment with them. That’s what will make the consultation really helpful, and will make me feel that I can move to the next page without feeling exhausted from the first one.”
A key scene in the film comes after the patient’s mother is stunned to discover a cheerful tango performance on her son’s ward, and confronts the doctor angrily.
“It’s like I’m abandoning him,” she says tearfully, when the doctor urges her to accept that her son’s chemotherapy is no longer working and let him live what life he has left.
“Give him permission to go,” he urges her. “It would be your greatest gift of love.”
Dr. Sara encourages a similar approach in his staff. He warns them about the “hero syndrome,” in which dying patients are made to feel they need to “hang on” and “fight” for the sake of their caregivers and families.
“The patient never asked to be the hero, but our attitude is telling him that he’s the hero,” he says in the film. “That puts him in an intolerable impasse because he figures that if he gives up, if he dies, he’s betraying his fans. He needs the exact opposite: to be set free. He needs the permission to die. That permission is given by two people: his doctor and his family.”
Of course, not all cancer patients have such a dim prognosis, and Dr. Sara is the first to forge ahead if he feels it’s appropriate. “If, if there is no option for them, I’m going to be aggressive to protect them. But when there is a curable disease, I will go broke to try to treat my patient. I’m willing to give them toxic drugs and hold their hand, get them through the storm if I believe it’s going to cure what they have, and I will coach them to accept being sick.”
He also believes in physical contact with the patient. “If we have some intimacy with the patient, we can at least palpate the kind of person they are,” he said. But his wife Nada pointed out that physical examinations can sometimes make patients nervous. “She told me, if you have a tie, they might have fun looking at it.” Thus began Dr. Sara’s collection of about 30 fun ties decorated with unicorns or jellyfish tailored to various patients’ preferences.
In the film, his patient teases him about this quirk, but Dr. Sara insists it is a small gesture that carries meaning. “One patient told me a story about lovebugs. She would see them in her kitchen when she was feeling well – so lovebugs became a sign of hope for her. I was telling the story to my wife ... so she got me a tie with lovebugs on it, and my patient was so happy when she saw me wearing that.”
In the film – and in real life – Dr. Sara often played guitar at breakfast music sessions with his staff in which he encouraged them to express their feelings about patients’ struggles. “If you cry, don’t be ashamed. Your patient will feel you’re with him,” he said in the film. In the final scenes, wearing a cloud-covered tie, he says goodbye to his patient with tears in his eyes. “They [the tears] are sincere,” he recalled. “Because I really felt I was looking at a dying patient. I really did.”
A version of this article first appeared on Medscape.com.
Factors linked to higher risk for death in young cancer survivors
according to new data from the St. Jude Lifetime Cohort.
Survivors with a greater number and severity of modifiable chronic health conditions as well as those living in the most versus least resource-deprived areas had a significantly higher risk of all-cause and health-related late death.
Finding ways to mitigate these factors “will be important to improving health outcomes and developing risk-stratification strategies to optimize care delivery to survivors at varying risk of adverse health events,” the researchers wrote.
The study indicates that treating chronic health conditions alone may not be enough to increase a cancer survivor’s lifespan; improving local environments matters too.
“It is important for clinicians to ask patients about their specific situation,” first author Matthew J. Ehrhardt, MD, department of oncology, St. Jude Children’s Research Hospital, Memphis, said in a news release. “It’s easy to prescribe medications or to tell people to exercise. It takes more time and more thoughtfulness to sit and understand environments in which they are residing.”
“As clinicians, we may have limited ability to modify some of those factors. But we can work closely with the rest of the health care team, such as social workers, for example, to help survivors to identify and access local resources,” Dr. Ehrhardt added.
The study was published online in JAMA Network Open.
A growing population of childhood cancer survivors faces an increased risk for premature death in the years following their diagnosis. However, associations between social determinants of health, modifiable health conditions, and late mortality in childhood cancer survivors remain unclear.
To assess late mortality, the study team analyzed data on 9,440 participants (median age at assessment, 27.5 years; range, 5.3-71.9 years) who lived at least 5 years after being diagnosed with a childhood cancer between 1962 and 2012.
During a median follow-up of about 18 years, childhood cancer survivors had an increased rate of both all-cause and health-related late mortality (standardized mortality rate, 7.6 for both). Among specific health-related causes of death, SMRs were 16.0 for subsequent neoplasms, 9.0 for pulmonary causes, 4.2 for cardiac causes, and 4.3 for other health-related causes.
To evaluate ties between modifiable chronic health conditions, social determinants, and late mortality, the researchers restricted their analysis to 3,407 adult study participants for whom relevant data were available. Modifiable chronic health conditions included dyslipidemia, hypertension, diabetes, underweight or obesity, bone mineral deficiency, and hypothyroidism.
After adjusting for individual factors, including age at diagnosis and treatment, as well as neighborhood-level factors, the researchers observed a significantly increased risk for death among survivors with one or more modifiable chronic health conditions of grade 2 or higher (relative risk, 2.2), two chronic health conditions of grade 2 or higher (RR, 2.6) or three chronic health conditions of grade 2 or higher (RR, 3.6).
These findings suggest that “increased late mortality experienced by childhood cancer survivors in adulthood may not be predetermined by treatment-related risk factors alone,” the researchers said.
In addition, survivors living in the most disadvantaged areas, as measured by the area deprivation index (ADI), had a five- to eightfold increased risk of late death from any cause compared with those living in the least disadvantaged areas, even after adjusting for modifiable chronic health conditions, cancer treatment, demographics, and individual socioeconomic factors.
The findings have important public health implications, Dr. Ehrhardt and colleagues said. The results can, for instance, help identify and stratify cancer survivors at higher lifetime risk for specific chronic conditions and late death.
This risk-stratified approach to care, however, is “relatively static” and does not account for risk factors acquired after cancer diagnosis and treatment, such as social determinants of health.
That is why also focusing on socioeconomic factors is important, and transitional care services following cancer treatment should consider that survivors in disadvantaged neighborhoods may lack supportive resources to address health issues, potentially leading to increased risk for death, the researchers said.
The knowledge that living in a resource-poor neighborhood may raise the risk for late death in childhood cancer survivors “strengthens support for public health policies that will direct resources to such regions and facilitate a multipronged approach to risk mitigation,” the authors concluded.
This study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new data from the St. Jude Lifetime Cohort.
Survivors with a greater number and severity of modifiable chronic health conditions as well as those living in the most versus least resource-deprived areas had a significantly higher risk of all-cause and health-related late death.
Finding ways to mitigate these factors “will be important to improving health outcomes and developing risk-stratification strategies to optimize care delivery to survivors at varying risk of adverse health events,” the researchers wrote.
The study indicates that treating chronic health conditions alone may not be enough to increase a cancer survivor’s lifespan; improving local environments matters too.
“It is important for clinicians to ask patients about their specific situation,” first author Matthew J. Ehrhardt, MD, department of oncology, St. Jude Children’s Research Hospital, Memphis, said in a news release. “It’s easy to prescribe medications or to tell people to exercise. It takes more time and more thoughtfulness to sit and understand environments in which they are residing.”
“As clinicians, we may have limited ability to modify some of those factors. But we can work closely with the rest of the health care team, such as social workers, for example, to help survivors to identify and access local resources,” Dr. Ehrhardt added.
The study was published online in JAMA Network Open.
A growing population of childhood cancer survivors faces an increased risk for premature death in the years following their diagnosis. However, associations between social determinants of health, modifiable health conditions, and late mortality in childhood cancer survivors remain unclear.
To assess late mortality, the study team analyzed data on 9,440 participants (median age at assessment, 27.5 years; range, 5.3-71.9 years) who lived at least 5 years after being diagnosed with a childhood cancer between 1962 and 2012.
During a median follow-up of about 18 years, childhood cancer survivors had an increased rate of both all-cause and health-related late mortality (standardized mortality rate, 7.6 for both). Among specific health-related causes of death, SMRs were 16.0 for subsequent neoplasms, 9.0 for pulmonary causes, 4.2 for cardiac causes, and 4.3 for other health-related causes.
To evaluate ties between modifiable chronic health conditions, social determinants, and late mortality, the researchers restricted their analysis to 3,407 adult study participants for whom relevant data were available. Modifiable chronic health conditions included dyslipidemia, hypertension, diabetes, underweight or obesity, bone mineral deficiency, and hypothyroidism.
After adjusting for individual factors, including age at diagnosis and treatment, as well as neighborhood-level factors, the researchers observed a significantly increased risk for death among survivors with one or more modifiable chronic health conditions of grade 2 or higher (relative risk, 2.2), two chronic health conditions of grade 2 or higher (RR, 2.6) or three chronic health conditions of grade 2 or higher (RR, 3.6).
These findings suggest that “increased late mortality experienced by childhood cancer survivors in adulthood may not be predetermined by treatment-related risk factors alone,” the researchers said.
In addition, survivors living in the most disadvantaged areas, as measured by the area deprivation index (ADI), had a five- to eightfold increased risk of late death from any cause compared with those living in the least disadvantaged areas, even after adjusting for modifiable chronic health conditions, cancer treatment, demographics, and individual socioeconomic factors.
The findings have important public health implications, Dr. Ehrhardt and colleagues said. The results can, for instance, help identify and stratify cancer survivors at higher lifetime risk for specific chronic conditions and late death.
This risk-stratified approach to care, however, is “relatively static” and does not account for risk factors acquired after cancer diagnosis and treatment, such as social determinants of health.
That is why also focusing on socioeconomic factors is important, and transitional care services following cancer treatment should consider that survivors in disadvantaged neighborhoods may lack supportive resources to address health issues, potentially leading to increased risk for death, the researchers said.
The knowledge that living in a resource-poor neighborhood may raise the risk for late death in childhood cancer survivors “strengthens support for public health policies that will direct resources to such regions and facilitate a multipronged approach to risk mitigation,” the authors concluded.
This study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new data from the St. Jude Lifetime Cohort.
Survivors with a greater number and severity of modifiable chronic health conditions as well as those living in the most versus least resource-deprived areas had a significantly higher risk of all-cause and health-related late death.
Finding ways to mitigate these factors “will be important to improving health outcomes and developing risk-stratification strategies to optimize care delivery to survivors at varying risk of adverse health events,” the researchers wrote.
The study indicates that treating chronic health conditions alone may not be enough to increase a cancer survivor’s lifespan; improving local environments matters too.
“It is important for clinicians to ask patients about their specific situation,” first author Matthew J. Ehrhardt, MD, department of oncology, St. Jude Children’s Research Hospital, Memphis, said in a news release. “It’s easy to prescribe medications or to tell people to exercise. It takes more time and more thoughtfulness to sit and understand environments in which they are residing.”
“As clinicians, we may have limited ability to modify some of those factors. But we can work closely with the rest of the health care team, such as social workers, for example, to help survivors to identify and access local resources,” Dr. Ehrhardt added.
The study was published online in JAMA Network Open.
A growing population of childhood cancer survivors faces an increased risk for premature death in the years following their diagnosis. However, associations between social determinants of health, modifiable health conditions, and late mortality in childhood cancer survivors remain unclear.
To assess late mortality, the study team analyzed data on 9,440 participants (median age at assessment, 27.5 years; range, 5.3-71.9 years) who lived at least 5 years after being diagnosed with a childhood cancer between 1962 and 2012.
During a median follow-up of about 18 years, childhood cancer survivors had an increased rate of both all-cause and health-related late mortality (standardized mortality rate, 7.6 for both). Among specific health-related causes of death, SMRs were 16.0 for subsequent neoplasms, 9.0 for pulmonary causes, 4.2 for cardiac causes, and 4.3 for other health-related causes.
To evaluate ties between modifiable chronic health conditions, social determinants, and late mortality, the researchers restricted their analysis to 3,407 adult study participants for whom relevant data were available. Modifiable chronic health conditions included dyslipidemia, hypertension, diabetes, underweight or obesity, bone mineral deficiency, and hypothyroidism.
After adjusting for individual factors, including age at diagnosis and treatment, as well as neighborhood-level factors, the researchers observed a significantly increased risk for death among survivors with one or more modifiable chronic health conditions of grade 2 or higher (relative risk, 2.2), two chronic health conditions of grade 2 or higher (RR, 2.6) or three chronic health conditions of grade 2 or higher (RR, 3.6).
These findings suggest that “increased late mortality experienced by childhood cancer survivors in adulthood may not be predetermined by treatment-related risk factors alone,” the researchers said.
In addition, survivors living in the most disadvantaged areas, as measured by the area deprivation index (ADI), had a five- to eightfold increased risk of late death from any cause compared with those living in the least disadvantaged areas, even after adjusting for modifiable chronic health conditions, cancer treatment, demographics, and individual socioeconomic factors.
The findings have important public health implications, Dr. Ehrhardt and colleagues said. The results can, for instance, help identify and stratify cancer survivors at higher lifetime risk for specific chronic conditions and late death.
This risk-stratified approach to care, however, is “relatively static” and does not account for risk factors acquired after cancer diagnosis and treatment, such as social determinants of health.
That is why also focusing on socioeconomic factors is important, and transitional care services following cancer treatment should consider that survivors in disadvantaged neighborhoods may lack supportive resources to address health issues, potentially leading to increased risk for death, the researchers said.
The knowledge that living in a resource-poor neighborhood may raise the risk for late death in childhood cancer survivors “strengthens support for public health policies that will direct resources to such regions and facilitate a multipronged approach to risk mitigation,” the authors concluded.
This study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN

