User login
AAD Updates Guidelines for Managing Acne
. The guidelines also conditionally recommend the use of topical clascoterone, salicylic acid, azelaic acid, oral minocycline, sarecycline, combined oral contraceptives, and spironolactone.
The development updates the AAD’s 2016 guidelines for managing acne. “Since there have been several important new treatments introduced since the prior guidelines, it was determined that there was a need to update these guidelines,” John S. Barbieri, MD, MBA, who cochaired a 16-member multidisciplinary work group that assembled the guidelines, told this news organization.
For the new guidelines, which were published online January 30, 2023, in the Journal of the American Academy of Dermatology, Dr. Barbieri, a dermatologist who directs the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, guidelines cochair Rachel V. Reynolds, MD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and colleagues conducted a systematic review of evidence regarding the management of acne. Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
In all, the work group made 18 recommendations and 5 good practice statements. They ranked 7 of the recommendations as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of benzoyl peroxide, the use of topical retinoids, the use of topical antibiotics, a fixed dose of a combination topical antibiotic with benzoyl peroxide, a fixed dose of a combination topical retinoid with topical antibiotic, a fixed dose combination of a topical retinoid with benzoyl peroxide, and the use of doxycycline.
“Conditional” recommendations include those for the use of clascoterone, salicylic acid, azelaic acid, minocycline, sarecycline, doxycycline over azithromycin; combined oral contraceptive pills, spironolactone, and, for patients with severe acne, traditional daily dosing of isotretinoin over intermittent dosing of isotretinoin.
Meanwhile, good clinical practice statements contained in the document include using topical therapies combining multiple mechanisms of action, limiting systemic antibiotic use, combining topical and systemic antibiotics with benzoyl peroxide and other topical therapies, and adjuvant intralesional corticosteroid injections.
In Dr. Barbieri’s opinion, the recommendations regarding clascoterone and sarecycline represent important developments. “Clascoterone is the first FDA-approved treatment that can address hormonal causes of acne in both men and women,” he told this news organization. “Sarecycline is a narrow-spectrum tetracycline that might have some advantages over other tetracyclines such as doxycycline and minocycline. It will be important to payers to provide coverage to ensure that patients have access to these valuable new treatments.”
Dr. Barbieri added that while no evidence exists to suggest that minocycline is more effective than doxycycline, minocycline can be associated with rare but serious side effects, such as vestibular dysfunction, autoimmune hepatitis, drug-induced lupus, and drug reaction with eosinophilia and systemic symptoms (DRESS). “We should consider whether reducing use of minocycline might be beneficial to our overall care of patients with acne,” he said. “In addition, we discuss that use of trimethoprim-sulfamethoxazole should be limited due to risk of severe adverse reactions such as Stevens-Johnson syndrome/toxic epidermal necrolysis, and acute respiratory failure.”
Another highlight of the guidelines, he continued, are specific recommendations for young, healthy patients on isotretinoin or spironolactone, which “can help clinicians and patients who are interested in less frequent monitoring feel more comfortable with these approaches,” he said.
Many discussions among work group members dealt with how to best implement the GRADE approach to the project “while ensuring the guidelines were as clinically relevant and actionable as possible,” according to Dr. Barbieri. “I think an important issue going forward will be to consider how to update and modify the GRADE approach to fit the unique needs of creating evidence-based guidelines for the management of skin disease.”
The work group acknowledged limitations of the guidelines, including identification of “important evidence gaps on the use of microbiology and endocrinology testing in acne, the use of systemic antibiotics beyond tetracycline-class antibiotics, physical modalities, complementary and alternative therapies, dietary interventions for the treatment of acne, and cost-effectiveness of acne treatments,” they wrote. “RCTs with long-term follow-up and comparative effectiveness research are necessary to examine and compare patient-centered acne treatment outcomes.”
The AAD funded the project. Dr. Barbieri disclosed that he serves as investigator for the National Institutes of Health and the National Psoriasis Foundation. Many coauthors reported being a speaker for and/or a consultant and advisory board member to many pharmaceutical companies.
. The guidelines also conditionally recommend the use of topical clascoterone, salicylic acid, azelaic acid, oral minocycline, sarecycline, combined oral contraceptives, and spironolactone.
The development updates the AAD’s 2016 guidelines for managing acne. “Since there have been several important new treatments introduced since the prior guidelines, it was determined that there was a need to update these guidelines,” John S. Barbieri, MD, MBA, who cochaired a 16-member multidisciplinary work group that assembled the guidelines, told this news organization.
For the new guidelines, which were published online January 30, 2023, in the Journal of the American Academy of Dermatology, Dr. Barbieri, a dermatologist who directs the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, guidelines cochair Rachel V. Reynolds, MD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and colleagues conducted a systematic review of evidence regarding the management of acne. Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
In all, the work group made 18 recommendations and 5 good practice statements. They ranked 7 of the recommendations as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of benzoyl peroxide, the use of topical retinoids, the use of topical antibiotics, a fixed dose of a combination topical antibiotic with benzoyl peroxide, a fixed dose of a combination topical retinoid with topical antibiotic, a fixed dose combination of a topical retinoid with benzoyl peroxide, and the use of doxycycline.
“Conditional” recommendations include those for the use of clascoterone, salicylic acid, azelaic acid, minocycline, sarecycline, doxycycline over azithromycin; combined oral contraceptive pills, spironolactone, and, for patients with severe acne, traditional daily dosing of isotretinoin over intermittent dosing of isotretinoin.
Meanwhile, good clinical practice statements contained in the document include using topical therapies combining multiple mechanisms of action, limiting systemic antibiotic use, combining topical and systemic antibiotics with benzoyl peroxide and other topical therapies, and adjuvant intralesional corticosteroid injections.
In Dr. Barbieri’s opinion, the recommendations regarding clascoterone and sarecycline represent important developments. “Clascoterone is the first FDA-approved treatment that can address hormonal causes of acne in both men and women,” he told this news organization. “Sarecycline is a narrow-spectrum tetracycline that might have some advantages over other tetracyclines such as doxycycline and minocycline. It will be important to payers to provide coverage to ensure that patients have access to these valuable new treatments.”
Dr. Barbieri added that while no evidence exists to suggest that minocycline is more effective than doxycycline, minocycline can be associated with rare but serious side effects, such as vestibular dysfunction, autoimmune hepatitis, drug-induced lupus, and drug reaction with eosinophilia and systemic symptoms (DRESS). “We should consider whether reducing use of minocycline might be beneficial to our overall care of patients with acne,” he said. “In addition, we discuss that use of trimethoprim-sulfamethoxazole should be limited due to risk of severe adverse reactions such as Stevens-Johnson syndrome/toxic epidermal necrolysis, and acute respiratory failure.”
Another highlight of the guidelines, he continued, are specific recommendations for young, healthy patients on isotretinoin or spironolactone, which “can help clinicians and patients who are interested in less frequent monitoring feel more comfortable with these approaches,” he said.
Many discussions among work group members dealt with how to best implement the GRADE approach to the project “while ensuring the guidelines were as clinically relevant and actionable as possible,” according to Dr. Barbieri. “I think an important issue going forward will be to consider how to update and modify the GRADE approach to fit the unique needs of creating evidence-based guidelines for the management of skin disease.”
The work group acknowledged limitations of the guidelines, including identification of “important evidence gaps on the use of microbiology and endocrinology testing in acne, the use of systemic antibiotics beyond tetracycline-class antibiotics, physical modalities, complementary and alternative therapies, dietary interventions for the treatment of acne, and cost-effectiveness of acne treatments,” they wrote. “RCTs with long-term follow-up and comparative effectiveness research are necessary to examine and compare patient-centered acne treatment outcomes.”
The AAD funded the project. Dr. Barbieri disclosed that he serves as investigator for the National Institutes of Health and the National Psoriasis Foundation. Many coauthors reported being a speaker for and/or a consultant and advisory board member to many pharmaceutical companies.
. The guidelines also conditionally recommend the use of topical clascoterone, salicylic acid, azelaic acid, oral minocycline, sarecycline, combined oral contraceptives, and spironolactone.
The development updates the AAD’s 2016 guidelines for managing acne. “Since there have been several important new treatments introduced since the prior guidelines, it was determined that there was a need to update these guidelines,” John S. Barbieri, MD, MBA, who cochaired a 16-member multidisciplinary work group that assembled the guidelines, told this news organization.
For the new guidelines, which were published online January 30, 2023, in the Journal of the American Academy of Dermatology, Dr. Barbieri, a dermatologist who directs the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, guidelines cochair Rachel V. Reynolds, MD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and colleagues conducted a systematic review of evidence regarding the management of acne. Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
In all, the work group made 18 recommendations and 5 good practice statements. They ranked 7 of the recommendations as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of benzoyl peroxide, the use of topical retinoids, the use of topical antibiotics, a fixed dose of a combination topical antibiotic with benzoyl peroxide, a fixed dose of a combination topical retinoid with topical antibiotic, a fixed dose combination of a topical retinoid with benzoyl peroxide, and the use of doxycycline.
“Conditional” recommendations include those for the use of clascoterone, salicylic acid, azelaic acid, minocycline, sarecycline, doxycycline over azithromycin; combined oral contraceptive pills, spironolactone, and, for patients with severe acne, traditional daily dosing of isotretinoin over intermittent dosing of isotretinoin.
Meanwhile, good clinical practice statements contained in the document include using topical therapies combining multiple mechanisms of action, limiting systemic antibiotic use, combining topical and systemic antibiotics with benzoyl peroxide and other topical therapies, and adjuvant intralesional corticosteroid injections.
In Dr. Barbieri’s opinion, the recommendations regarding clascoterone and sarecycline represent important developments. “Clascoterone is the first FDA-approved treatment that can address hormonal causes of acne in both men and women,” he told this news organization. “Sarecycline is a narrow-spectrum tetracycline that might have some advantages over other tetracyclines such as doxycycline and minocycline. It will be important to payers to provide coverage to ensure that patients have access to these valuable new treatments.”
Dr. Barbieri added that while no evidence exists to suggest that minocycline is more effective than doxycycline, minocycline can be associated with rare but serious side effects, such as vestibular dysfunction, autoimmune hepatitis, drug-induced lupus, and drug reaction with eosinophilia and systemic symptoms (DRESS). “We should consider whether reducing use of minocycline might be beneficial to our overall care of patients with acne,” he said. “In addition, we discuss that use of trimethoprim-sulfamethoxazole should be limited due to risk of severe adverse reactions such as Stevens-Johnson syndrome/toxic epidermal necrolysis, and acute respiratory failure.”
Another highlight of the guidelines, he continued, are specific recommendations for young, healthy patients on isotretinoin or spironolactone, which “can help clinicians and patients who are interested in less frequent monitoring feel more comfortable with these approaches,” he said.
Many discussions among work group members dealt with how to best implement the GRADE approach to the project “while ensuring the guidelines were as clinically relevant and actionable as possible,” according to Dr. Barbieri. “I think an important issue going forward will be to consider how to update and modify the GRADE approach to fit the unique needs of creating evidence-based guidelines for the management of skin disease.”
The work group acknowledged limitations of the guidelines, including identification of “important evidence gaps on the use of microbiology and endocrinology testing in acne, the use of systemic antibiotics beyond tetracycline-class antibiotics, physical modalities, complementary and alternative therapies, dietary interventions for the treatment of acne, and cost-effectiveness of acne treatments,” they wrote. “RCTs with long-term follow-up and comparative effectiveness research are necessary to examine and compare patient-centered acne treatment outcomes.”
The AAD funded the project. Dr. Barbieri disclosed that he serves as investigator for the National Institutes of Health and the National Psoriasis Foundation. Many coauthors reported being a speaker for and/or a consultant and advisory board member to many pharmaceutical companies.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Review Finds No Short-term MACE, VTE risk with JAK Inhibitors For Dermatoses
, at least in the short term, say the authors of a new meta-analysis published in JAMA Dermatology.
Considering data on over 17,000 patients with different dermatoses from 45 placebo-controlled randomized clinical trials with an average follow up of 16 weeks, they found there was no significant increase in the occurrence of major adverse cardiovascular events (MACE) or venous thromboembolism (VTE) in people with dermatoses treated with JAK-STAT inhibitors, compared with placebo.
The I² statistic was 0.00% for both MACE and VTE comparing the two arms, indicating that the results were unlikely to be due to chance. There was no increased risk in MACE between those on placebo and those on JAK-STAT inhibitors, with a risk ratio (RR) of 0.47; or for VTE risk, with an RR of 0.46.
Similar findings were obtained when data were analyzed according to the dermatological condition being treated, mechanism of action of the medication, or whether the medication carried a boxed warning.
These data “suggest inconsistency with established sentiments,” that JAK-STAT inhibitors increase the risk for cardiovascular events, Patrick Ireland, MD, of the University of New South Wales, Randwick, Australia, and coauthors wrote in the article. “This may be owing to the limited time frames in which these rare events could be adequately captured, or the ages of enrolled patients being too young to realize the well established heightened risks of developing MACE and VTE,” they suggested.
However, the findings challenge the notion that the cardiovascular complications of these drugs are the same in all patients; dermatological use may not be associated with the same risks as with use for rheumatologic indications.
Class-Wide Boxed Warning
“JAK-STAT [inhibitors] have had some pretty indemnifying data against their use, with the ORAL [Surveillance] study demonstrating increased all-cause mortality, cardiovascular events, venous thromboembolism, and malignancy,” Dr. Ireland said in an interview.
ORAL Surveillance was an open-label, postmarketing trial conducted in patients with rheumatoid arthritis treated with tofacitinib or a tumor necrosis factor (TNF) inhibitor. The results led the US Food and Drug Administration to require information about the risks of serious heart-related events, cancer, blood clots, and death in a boxed warning for JAK-STAT inhibitors in 2022.
“I think it’s important to recognize that these [ORAL Surveillance participants] are very different patients to the typical dermatological patient being treated with a JAK-STAT [inhibitors], with newer studies demonstrating a much safer profile than initially thought,” Dr. Ireland said.
Examining Risk in Dermatological Conditions
The meta-analysis performed by Dr. Ireland and associates focused specifically on the risk for MACE and VTE in patients being treated for dermatological conditions, and included trials published up until June 2023. Only trials that had included a placebo arm were considered; pooled analyses, long-term extension trial data, post hoc analyses, and pediatric-specific trials were excluded.
Most (25) of the trials were phase 2b or phase 3 trials, 18 were phase 2 to 2b, and two were phase 1 trials. The studies included 12,996 participants, mostly with atopic dermatitis or psoriasis, who were treated with JAK-STAT inhibitors, which included baricitinib (2846 patients), tofacitinib (2470), upadacitinib (2218), abrocitinib (1904), and deucravacitinib (1492), among others. There were 4925 patients on placebo.
Overall, MACE — defined as a combined endpoint of acute myocardial infarction, stroke, cardiovascular mortality, heart failure, and unstable angina, as well as arterial embolism — occurred in 13 of the JAK-STAT inhibitor-treated patients and in four of those on placebo. VTE — defined as deep vein thrombosis, pulmonary embolism, and any unusual site thrombosis — was reported in eight JAK-STAT inhibitor-treated patients and in one patient on placebo.
The pooled incidence ratios for MACE and VTE were calculated as 0.20 per 100 person exposure years (PEY) for JAK-STAT inhibitor treatment and 0.13 PEY for placebo. The pooled RRs comparing the two treatment groups were a respective 1.13 for MACE and 2.79 for VTE, but neither RR reached statistical significance.
No difference was seen between the treatment arms in terms of treatment emergent adverse events (RR, 1.05), serious adverse events (RR, 0.92), or study discontinuation because of adverse events (RR, 0.94).
Reassuring Results?
Dr. Ireland and coauthors said the finding should help to reassure clinicians that the short-term use of JAK-STAT inhibitors in patients with dermatological conditions with low cardiovascular risk profiles “appears to be both safe and well tolerated.” They cautioned, however, that “clinicians must remain judicious” when using these medications for longer periods and in high-risk patient populations.
This was a pragmatic meta-analysis that provides useful information for dermatologists, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, DC, said in an interview.
“When there are safety concerns, I think that’s where data like this are so important to not just allay the fears of practitioners, but also to arm the practitioner with information for when they discuss a possible treatment with a patient,” said Dr. Friedman, who was not involved in the study.
“What’s unique here is that they’re looking at any possible use of JAK inhibitors for dermatological disease,” so this represents patients that dermatologists would be seeing, he added.
“The limitation here is time, we only can say so much about the safety of the medication with the data that we have,” Dr. Friedman said. Almost 4 months is “a good amount of time” to know about the cardiovascular risks, he said, but added, what happens then? Will the risk increase and will patients need to be switched to another medication?
“There’s no line in the sand,” with regard to using a JAK-STAT inhibitor. “If you look at the label, they’re not meant to be used incrementally,” but as ongoing treatment, while considering the needs of the patient and the relative risks and benefits, he said.
With that in mind, “the open label extension studies for all these [JAK-STAT inhibitors] are really, really important to get a sense of ‘do new signals emerge down the road.’ ”
The meta-analysis received no commercial funding. One author of the work reported personal fees from several pharmaceutical companies which were done outside of analysis. Dr. Friedman has received research funding from or acted as a consultant for several pharmaceutical companies including, Incyte, Pfizer, Eli Lily, and AbbVie.
, at least in the short term, say the authors of a new meta-analysis published in JAMA Dermatology.
Considering data on over 17,000 patients with different dermatoses from 45 placebo-controlled randomized clinical trials with an average follow up of 16 weeks, they found there was no significant increase in the occurrence of major adverse cardiovascular events (MACE) or venous thromboembolism (VTE) in people with dermatoses treated with JAK-STAT inhibitors, compared with placebo.
The I² statistic was 0.00% for both MACE and VTE comparing the two arms, indicating that the results were unlikely to be due to chance. There was no increased risk in MACE between those on placebo and those on JAK-STAT inhibitors, with a risk ratio (RR) of 0.47; or for VTE risk, with an RR of 0.46.
Similar findings were obtained when data were analyzed according to the dermatological condition being treated, mechanism of action of the medication, or whether the medication carried a boxed warning.
These data “suggest inconsistency with established sentiments,” that JAK-STAT inhibitors increase the risk for cardiovascular events, Patrick Ireland, MD, of the University of New South Wales, Randwick, Australia, and coauthors wrote in the article. “This may be owing to the limited time frames in which these rare events could be adequately captured, or the ages of enrolled patients being too young to realize the well established heightened risks of developing MACE and VTE,” they suggested.
However, the findings challenge the notion that the cardiovascular complications of these drugs are the same in all patients; dermatological use may not be associated with the same risks as with use for rheumatologic indications.
Class-Wide Boxed Warning
“JAK-STAT [inhibitors] have had some pretty indemnifying data against their use, with the ORAL [Surveillance] study demonstrating increased all-cause mortality, cardiovascular events, venous thromboembolism, and malignancy,” Dr. Ireland said in an interview.
ORAL Surveillance was an open-label, postmarketing trial conducted in patients with rheumatoid arthritis treated with tofacitinib or a tumor necrosis factor (TNF) inhibitor. The results led the US Food and Drug Administration to require information about the risks of serious heart-related events, cancer, blood clots, and death in a boxed warning for JAK-STAT inhibitors in 2022.
“I think it’s important to recognize that these [ORAL Surveillance participants] are very different patients to the typical dermatological patient being treated with a JAK-STAT [inhibitors], with newer studies demonstrating a much safer profile than initially thought,” Dr. Ireland said.
Examining Risk in Dermatological Conditions
The meta-analysis performed by Dr. Ireland and associates focused specifically on the risk for MACE and VTE in patients being treated for dermatological conditions, and included trials published up until June 2023. Only trials that had included a placebo arm were considered; pooled analyses, long-term extension trial data, post hoc analyses, and pediatric-specific trials were excluded.
Most (25) of the trials were phase 2b or phase 3 trials, 18 were phase 2 to 2b, and two were phase 1 trials. The studies included 12,996 participants, mostly with atopic dermatitis or psoriasis, who were treated with JAK-STAT inhibitors, which included baricitinib (2846 patients), tofacitinib (2470), upadacitinib (2218), abrocitinib (1904), and deucravacitinib (1492), among others. There were 4925 patients on placebo.
Overall, MACE — defined as a combined endpoint of acute myocardial infarction, stroke, cardiovascular mortality, heart failure, and unstable angina, as well as arterial embolism — occurred in 13 of the JAK-STAT inhibitor-treated patients and in four of those on placebo. VTE — defined as deep vein thrombosis, pulmonary embolism, and any unusual site thrombosis — was reported in eight JAK-STAT inhibitor-treated patients and in one patient on placebo.
The pooled incidence ratios for MACE and VTE were calculated as 0.20 per 100 person exposure years (PEY) for JAK-STAT inhibitor treatment and 0.13 PEY for placebo. The pooled RRs comparing the two treatment groups were a respective 1.13 for MACE and 2.79 for VTE, but neither RR reached statistical significance.
No difference was seen between the treatment arms in terms of treatment emergent adverse events (RR, 1.05), serious adverse events (RR, 0.92), or study discontinuation because of adverse events (RR, 0.94).
Reassuring Results?
Dr. Ireland and coauthors said the finding should help to reassure clinicians that the short-term use of JAK-STAT inhibitors in patients with dermatological conditions with low cardiovascular risk profiles “appears to be both safe and well tolerated.” They cautioned, however, that “clinicians must remain judicious” when using these medications for longer periods and in high-risk patient populations.
This was a pragmatic meta-analysis that provides useful information for dermatologists, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, DC, said in an interview.
“When there are safety concerns, I think that’s where data like this are so important to not just allay the fears of practitioners, but also to arm the practitioner with information for when they discuss a possible treatment with a patient,” said Dr. Friedman, who was not involved in the study.
“What’s unique here is that they’re looking at any possible use of JAK inhibitors for dermatological disease,” so this represents patients that dermatologists would be seeing, he added.
“The limitation here is time, we only can say so much about the safety of the medication with the data that we have,” Dr. Friedman said. Almost 4 months is “a good amount of time” to know about the cardiovascular risks, he said, but added, what happens then? Will the risk increase and will patients need to be switched to another medication?
“There’s no line in the sand,” with regard to using a JAK-STAT inhibitor. “If you look at the label, they’re not meant to be used incrementally,” but as ongoing treatment, while considering the needs of the patient and the relative risks and benefits, he said.
With that in mind, “the open label extension studies for all these [JAK-STAT inhibitors] are really, really important to get a sense of ‘do new signals emerge down the road.’ ”
The meta-analysis received no commercial funding. One author of the work reported personal fees from several pharmaceutical companies which were done outside of analysis. Dr. Friedman has received research funding from or acted as a consultant for several pharmaceutical companies including, Incyte, Pfizer, Eli Lily, and AbbVie.
, at least in the short term, say the authors of a new meta-analysis published in JAMA Dermatology.
Considering data on over 17,000 patients with different dermatoses from 45 placebo-controlled randomized clinical trials with an average follow up of 16 weeks, they found there was no significant increase in the occurrence of major adverse cardiovascular events (MACE) or venous thromboembolism (VTE) in people with dermatoses treated with JAK-STAT inhibitors, compared with placebo.
The I² statistic was 0.00% for both MACE and VTE comparing the two arms, indicating that the results were unlikely to be due to chance. There was no increased risk in MACE between those on placebo and those on JAK-STAT inhibitors, with a risk ratio (RR) of 0.47; or for VTE risk, with an RR of 0.46.
Similar findings were obtained when data were analyzed according to the dermatological condition being treated, mechanism of action of the medication, or whether the medication carried a boxed warning.
These data “suggest inconsistency with established sentiments,” that JAK-STAT inhibitors increase the risk for cardiovascular events, Patrick Ireland, MD, of the University of New South Wales, Randwick, Australia, and coauthors wrote in the article. “This may be owing to the limited time frames in which these rare events could be adequately captured, or the ages of enrolled patients being too young to realize the well established heightened risks of developing MACE and VTE,” they suggested.
However, the findings challenge the notion that the cardiovascular complications of these drugs are the same in all patients; dermatological use may not be associated with the same risks as with use for rheumatologic indications.
Class-Wide Boxed Warning
“JAK-STAT [inhibitors] have had some pretty indemnifying data against their use, with the ORAL [Surveillance] study demonstrating increased all-cause mortality, cardiovascular events, venous thromboembolism, and malignancy,” Dr. Ireland said in an interview.
ORAL Surveillance was an open-label, postmarketing trial conducted in patients with rheumatoid arthritis treated with tofacitinib or a tumor necrosis factor (TNF) inhibitor. The results led the US Food and Drug Administration to require information about the risks of serious heart-related events, cancer, blood clots, and death in a boxed warning for JAK-STAT inhibitors in 2022.
“I think it’s important to recognize that these [ORAL Surveillance participants] are very different patients to the typical dermatological patient being treated with a JAK-STAT [inhibitors], with newer studies demonstrating a much safer profile than initially thought,” Dr. Ireland said.
Examining Risk in Dermatological Conditions
The meta-analysis performed by Dr. Ireland and associates focused specifically on the risk for MACE and VTE in patients being treated for dermatological conditions, and included trials published up until June 2023. Only trials that had included a placebo arm were considered; pooled analyses, long-term extension trial data, post hoc analyses, and pediatric-specific trials were excluded.
Most (25) of the trials were phase 2b or phase 3 trials, 18 were phase 2 to 2b, and two were phase 1 trials. The studies included 12,996 participants, mostly with atopic dermatitis or psoriasis, who were treated with JAK-STAT inhibitors, which included baricitinib (2846 patients), tofacitinib (2470), upadacitinib (2218), abrocitinib (1904), and deucravacitinib (1492), among others. There were 4925 patients on placebo.
Overall, MACE — defined as a combined endpoint of acute myocardial infarction, stroke, cardiovascular mortality, heart failure, and unstable angina, as well as arterial embolism — occurred in 13 of the JAK-STAT inhibitor-treated patients and in four of those on placebo. VTE — defined as deep vein thrombosis, pulmonary embolism, and any unusual site thrombosis — was reported in eight JAK-STAT inhibitor-treated patients and in one patient on placebo.
The pooled incidence ratios for MACE and VTE were calculated as 0.20 per 100 person exposure years (PEY) for JAK-STAT inhibitor treatment and 0.13 PEY for placebo. The pooled RRs comparing the two treatment groups were a respective 1.13 for MACE and 2.79 for VTE, but neither RR reached statistical significance.
No difference was seen between the treatment arms in terms of treatment emergent adverse events (RR, 1.05), serious adverse events (RR, 0.92), or study discontinuation because of adverse events (RR, 0.94).
Reassuring Results?
Dr. Ireland and coauthors said the finding should help to reassure clinicians that the short-term use of JAK-STAT inhibitors in patients with dermatological conditions with low cardiovascular risk profiles “appears to be both safe and well tolerated.” They cautioned, however, that “clinicians must remain judicious” when using these medications for longer periods and in high-risk patient populations.
This was a pragmatic meta-analysis that provides useful information for dermatologists, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, DC, said in an interview.
“When there are safety concerns, I think that’s where data like this are so important to not just allay the fears of practitioners, but also to arm the practitioner with information for when they discuss a possible treatment with a patient,” said Dr. Friedman, who was not involved in the study.
“What’s unique here is that they’re looking at any possible use of JAK inhibitors for dermatological disease,” so this represents patients that dermatologists would be seeing, he added.
“The limitation here is time, we only can say so much about the safety of the medication with the data that we have,” Dr. Friedman said. Almost 4 months is “a good amount of time” to know about the cardiovascular risks, he said, but added, what happens then? Will the risk increase and will patients need to be switched to another medication?
“There’s no line in the sand,” with regard to using a JAK-STAT inhibitor. “If you look at the label, they’re not meant to be used incrementally,” but as ongoing treatment, while considering the needs of the patient and the relative risks and benefits, he said.
With that in mind, “the open label extension studies for all these [JAK-STAT inhibitors] are really, really important to get a sense of ‘do new signals emerge down the road.’ ”
The meta-analysis received no commercial funding. One author of the work reported personal fees from several pharmaceutical companies which were done outside of analysis. Dr. Friedman has received research funding from or acted as a consultant for several pharmaceutical companies including, Incyte, Pfizer, Eli Lily, and AbbVie.
FROM JAMA DERMATOLOGY
Protein Before Exercise Curbs Hypoglycemia in Teens with T1D
TOPLINE:
Protein intake within 4 hours before exercise may shorten hypoglycemic episodes during moderate physical activity in teens with type 1 diabetes (T1D).
METHODOLOGY:
- For teenagers with T1D, regular physical activity improves blood sugar, insulin sensitivity, and other health measures, but the risk for hypoglycemia is a major barrier.
- In a secondary analysis of the FLEX study, researchers estimated the association between protein intake within 4 hours before moderate to vigorous physical activity bouts and glycemia during and following physical exercise.
- The final sample size included 447 bouts from 112 adolescents with T1D (median age, 14.5 years; 53.6% female) whose physical activity records and 24-hour dietary recall data were collected at baseline and 6 months.
- Data on continuous glucose monitoring (CGM) was a selection criterium and used to calculate the following measures of glycemia:
- Percentage of time above range (TAR; > 180 mg/dL)
- Percentage of time in range (TIR; 70-180 mg/dL)
- Percentage of time below range (TBR; < 70 mg/dL)
TAKEAWAY:
- There was a small reduction in TBR during physical activity in patients who consumed 10-19.9 g (−4.41%; P = .04) and more than 20 g (−4.83%; P = .02) of protein before moderate to vigorous exercise compared with those who consumed less than 10 g of protein.
- Similarly, protein intakes of 0.125-0.249 g/kg and ≥ 0.25 g/kg were associated with −5.38% (P = .01) and −4.32% (P = .03) reductions in TBR, respectively, compared with less than 0.125 g/kg of protein intake.
- However, the pre-exercise protein consumption was not associated with TAR or TIR during exercise or with any glycemic measurements (TAR, TIR, and TBR) after exercise.
- The benefits of protein intake on glycemia were observed only during moderate-intensity bouts of physical activity, which may reflect differing glycemic trajectories in more high-intensity activity.
IN PRACTICE:
“Consumption of at least 10 g or 0.125 g/kg bodyweight was associated with reduced TBR during moderate to vigorous physical activity, indicating improved safety for adolescents with T1D,” the authors wrote.
SOURCE:
This study, led by Franklin R. Muntis, PhD, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, North Carolina, was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
Self-reported measures of dietary intake were prone to underreporting, while moderate-to-vigorous physical activity was often overreported among adolescents. Approximately, 26% of identified bouts of moderate to vigorous physical activity were missing adequate CGM data, excluding participants from the analysis, which may have caused selection bias. There was no time-stamped insulin dosing data available.
DISCLOSURES:
The FLEX study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Protein intake within 4 hours before exercise may shorten hypoglycemic episodes during moderate physical activity in teens with type 1 diabetes (T1D).
METHODOLOGY:
- For teenagers with T1D, regular physical activity improves blood sugar, insulin sensitivity, and other health measures, but the risk for hypoglycemia is a major barrier.
- In a secondary analysis of the FLEX study, researchers estimated the association between protein intake within 4 hours before moderate to vigorous physical activity bouts and glycemia during and following physical exercise.
- The final sample size included 447 bouts from 112 adolescents with T1D (median age, 14.5 years; 53.6% female) whose physical activity records and 24-hour dietary recall data were collected at baseline and 6 months.
- Data on continuous glucose monitoring (CGM) was a selection criterium and used to calculate the following measures of glycemia:
- Percentage of time above range (TAR; > 180 mg/dL)
- Percentage of time in range (TIR; 70-180 mg/dL)
- Percentage of time below range (TBR; < 70 mg/dL)
TAKEAWAY:
- There was a small reduction in TBR during physical activity in patients who consumed 10-19.9 g (−4.41%; P = .04) and more than 20 g (−4.83%; P = .02) of protein before moderate to vigorous exercise compared with those who consumed less than 10 g of protein.
- Similarly, protein intakes of 0.125-0.249 g/kg and ≥ 0.25 g/kg were associated with −5.38% (P = .01) and −4.32% (P = .03) reductions in TBR, respectively, compared with less than 0.125 g/kg of protein intake.
- However, the pre-exercise protein consumption was not associated with TAR or TIR during exercise or with any glycemic measurements (TAR, TIR, and TBR) after exercise.
- The benefits of protein intake on glycemia were observed only during moderate-intensity bouts of physical activity, which may reflect differing glycemic trajectories in more high-intensity activity.
IN PRACTICE:
“Consumption of at least 10 g or 0.125 g/kg bodyweight was associated with reduced TBR during moderate to vigorous physical activity, indicating improved safety for adolescents with T1D,” the authors wrote.
SOURCE:
This study, led by Franklin R. Muntis, PhD, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, North Carolina, was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
Self-reported measures of dietary intake were prone to underreporting, while moderate-to-vigorous physical activity was often overreported among adolescents. Approximately, 26% of identified bouts of moderate to vigorous physical activity were missing adequate CGM data, excluding participants from the analysis, which may have caused selection bias. There was no time-stamped insulin dosing data available.
DISCLOSURES:
The FLEX study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Protein intake within 4 hours before exercise may shorten hypoglycemic episodes during moderate physical activity in teens with type 1 diabetes (T1D).
METHODOLOGY:
- For teenagers with T1D, regular physical activity improves blood sugar, insulin sensitivity, and other health measures, but the risk for hypoglycemia is a major barrier.
- In a secondary analysis of the FLEX study, researchers estimated the association between protein intake within 4 hours before moderate to vigorous physical activity bouts and glycemia during and following physical exercise.
- The final sample size included 447 bouts from 112 adolescents with T1D (median age, 14.5 years; 53.6% female) whose physical activity records and 24-hour dietary recall data were collected at baseline and 6 months.
- Data on continuous glucose monitoring (CGM) was a selection criterium and used to calculate the following measures of glycemia:
- Percentage of time above range (TAR; > 180 mg/dL)
- Percentage of time in range (TIR; 70-180 mg/dL)
- Percentage of time below range (TBR; < 70 mg/dL)
TAKEAWAY:
- There was a small reduction in TBR during physical activity in patients who consumed 10-19.9 g (−4.41%; P = .04) and more than 20 g (−4.83%; P = .02) of protein before moderate to vigorous exercise compared with those who consumed less than 10 g of protein.
- Similarly, protein intakes of 0.125-0.249 g/kg and ≥ 0.25 g/kg were associated with −5.38% (P = .01) and −4.32% (P = .03) reductions in TBR, respectively, compared with less than 0.125 g/kg of protein intake.
- However, the pre-exercise protein consumption was not associated with TAR or TIR during exercise or with any glycemic measurements (TAR, TIR, and TBR) after exercise.
- The benefits of protein intake on glycemia were observed only during moderate-intensity bouts of physical activity, which may reflect differing glycemic trajectories in more high-intensity activity.
IN PRACTICE:
“Consumption of at least 10 g or 0.125 g/kg bodyweight was associated with reduced TBR during moderate to vigorous physical activity, indicating improved safety for adolescents with T1D,” the authors wrote.
SOURCE:
This study, led by Franklin R. Muntis, PhD, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, North Carolina, was published online in Diabetes, Obesity and Metabolism.
LIMITATIONS:
Self-reported measures of dietary intake were prone to underreporting, while moderate-to-vigorous physical activity was often overreported among adolescents. Approximately, 26% of identified bouts of moderate to vigorous physical activity were missing adequate CGM data, excluding participants from the analysis, which may have caused selection bias. There was no time-stamped insulin dosing data available.
DISCLOSURES:
The FLEX study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Night Bracing: A Good Alternative for Adolescent Scoliosis
, new research suggests.
In the randomized Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS) trial, researchers, led by Anastasios Charalampidis, MD, PhD, with the Department of Clinical Science, Intervention and Technology at Karolinska Institutet in Stockholm, Sweden, tested whether a group using self-managed physical activity combined with either nighttime bracing for 8 hours or scoliosis-specific exercise achieved better results than a control group doing self-managed physical activity alone for 1 hour per day in preventing Cobb angle progression in moderate-grade AIS.
Findings of the trial, conducted in 6 public hospitals across Sweden, were published online in JAMA Network Open.
Night Bracing More Effective Than Comparison Arms
In the trial of 135 patients, aged 9-17 years, who were skeletally immature with moderate AIS, researchers found that night bracing plus self-managed physical activity prevented curve progression of more than 6 degrees (treatment success) to a significantly greater extent than did either self-managed physical activity alone or scoliosis-specific exercise.
A secondary outcome of curve progression was the number of patients who had surgery up until 2 years after the primary outcome.
The average age of patients was 12.7 years and most (82%) were female. Patients with treatment failure (curve progression of more than 6 degrees) had the option to transition to a full-time brace until skeletal maturity. That option resulted in similar frequency of surgery independent of initial treatment, according to the paper.
AIS is a structural deformity of the spinal column, affecting otherwise healthy children and adolescents during their growth spurt.
Previous studies have suggested that full-time bracing is effective in treating moderate-grade AIS. But the physical distress and psychological side effects that some experience can cause low adherence or rejection of the treatment.
The authors wrote that, “To our knowledge, there have been no randomized clinical trials investigating night bracing versus a control group.”
In this trial, treatment success was seen in 34 of 45 patients (76%) in the nighttime-bracing group and in 24 of 45 patients (53%) in the physical activity–alone group (odds ratio [OR], 2.7; 95% CI, 1.1-6.6). Success occurred in 26 of 45 patients (58%) in the scoliosis-specific exercise group (OR for scoliosis-specific exercise vs physical activity alone, 1.2; 95% CI, 0.5-2.8).
Adverse Events
Patients and clinicians could respond to an open-ended question regarding adverse events at each 6-month follow-up. Nineteen adverse events were reported in 15 patients between the start of the study up until the primary outcome was reached.
In the night-bracing group, there were 16 adverse events reported among 12 patients. They were: trunk pressure and skin problems (n = 10); sleeping problems (n = 2); emotional problems (n = 1); shoulder/neck pain (n = 2); and unspecified AEs (n = 1). In the scoliosis-specific exercise group, 3 adverse events were reported in 3 patients (pain during treatment (n = 1), muscle strain (n = 1), and low back pain (n = 1). No adverse events were reported in the physical activity alone group.
In an invited commentary, Kosei Nagata, MD, PhD, with the Department of Orthopaedic Surgery and Spinal Surgery at The University of Tokyo Hospital in Tokyo, Japan, said the study makes two important points.
“First, it was reaffirmed that the basis of scoliosis treatment is bracing and not a specific exercise therapy,” he wrote. “Second, nighttime bracing can be an effective alternative intervention for patients rejecting full-time bracing.”
He emphasized, however, that nighttime bracing alone is not enough to achieve success. In this study, bracing was combined with exercise. And the number of hours worn is important.
“Physicians should explain to patients with AIS and to their guardians the significant association between hours of brace wear and treatment success,” Dr. Nagata wrote. He pointed out that, in a previous randomized clinical trial in 2013 by Weinstein et al., patients were instructed to wear a brace for at least 18 hours a day. The treatment success rates of brace-wearing patients were 40% for less than 6 hours each day; 70% for 6-12 hours each day, and 90% for more than 13 hours each day, which suggests that full-time bracing is optimal.
However, he added that physicians should keep in mind the sensitivities of youth and effect on their self-esteem when prescribing bracing, as many adolescents will have a fear of ridicule.
“The goals of bracing treatment for AIS are manifold: avoiding surgical treatment, preventing future back pain, maintaining respiratory function, and reducing the psychological impact of the deformity,” Dr. Nagata wrote. “Physicians should understand these aspects and take a balanced view of patients who refuse full-time bracing.”
He added that future improvements in design of the braces and less rigid alternatives will be important.
The trial was funded by the Swedish Research Council and by the Stockholm County Council, the Swedish Society of Spinal Surgeons, the Karolinska Institutet and the Crown Princess Lovisas Foundation. Study coauthor Paul Gerdhem, MD, PhD, reports grants from the Karolinska Institutet beyond his usual salary during the study and personal fees for lectures from DePuy Synthes and grants from Philips Healthcare paid to the institution outside the submitted work. No other disclosures were reported. Dr. Nagata reported no relevant financial relationships.
, new research suggests.
In the randomized Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS) trial, researchers, led by Anastasios Charalampidis, MD, PhD, with the Department of Clinical Science, Intervention and Technology at Karolinska Institutet in Stockholm, Sweden, tested whether a group using self-managed physical activity combined with either nighttime bracing for 8 hours or scoliosis-specific exercise achieved better results than a control group doing self-managed physical activity alone for 1 hour per day in preventing Cobb angle progression in moderate-grade AIS.
Findings of the trial, conducted in 6 public hospitals across Sweden, were published online in JAMA Network Open.
Night Bracing More Effective Than Comparison Arms
In the trial of 135 patients, aged 9-17 years, who were skeletally immature with moderate AIS, researchers found that night bracing plus self-managed physical activity prevented curve progression of more than 6 degrees (treatment success) to a significantly greater extent than did either self-managed physical activity alone or scoliosis-specific exercise.
A secondary outcome of curve progression was the number of patients who had surgery up until 2 years after the primary outcome.
The average age of patients was 12.7 years and most (82%) were female. Patients with treatment failure (curve progression of more than 6 degrees) had the option to transition to a full-time brace until skeletal maturity. That option resulted in similar frequency of surgery independent of initial treatment, according to the paper.
AIS is a structural deformity of the spinal column, affecting otherwise healthy children and adolescents during their growth spurt.
Previous studies have suggested that full-time bracing is effective in treating moderate-grade AIS. But the physical distress and psychological side effects that some experience can cause low adherence or rejection of the treatment.
The authors wrote that, “To our knowledge, there have been no randomized clinical trials investigating night bracing versus a control group.”
In this trial, treatment success was seen in 34 of 45 patients (76%) in the nighttime-bracing group and in 24 of 45 patients (53%) in the physical activity–alone group (odds ratio [OR], 2.7; 95% CI, 1.1-6.6). Success occurred in 26 of 45 patients (58%) in the scoliosis-specific exercise group (OR for scoliosis-specific exercise vs physical activity alone, 1.2; 95% CI, 0.5-2.8).
Adverse Events
Patients and clinicians could respond to an open-ended question regarding adverse events at each 6-month follow-up. Nineteen adverse events were reported in 15 patients between the start of the study up until the primary outcome was reached.
In the night-bracing group, there were 16 adverse events reported among 12 patients. They were: trunk pressure and skin problems (n = 10); sleeping problems (n = 2); emotional problems (n = 1); shoulder/neck pain (n = 2); and unspecified AEs (n = 1). In the scoliosis-specific exercise group, 3 adverse events were reported in 3 patients (pain during treatment (n = 1), muscle strain (n = 1), and low back pain (n = 1). No adverse events were reported in the physical activity alone group.
In an invited commentary, Kosei Nagata, MD, PhD, with the Department of Orthopaedic Surgery and Spinal Surgery at The University of Tokyo Hospital in Tokyo, Japan, said the study makes two important points.
“First, it was reaffirmed that the basis of scoliosis treatment is bracing and not a specific exercise therapy,” he wrote. “Second, nighttime bracing can be an effective alternative intervention for patients rejecting full-time bracing.”
He emphasized, however, that nighttime bracing alone is not enough to achieve success. In this study, bracing was combined with exercise. And the number of hours worn is important.
“Physicians should explain to patients with AIS and to their guardians the significant association between hours of brace wear and treatment success,” Dr. Nagata wrote. He pointed out that, in a previous randomized clinical trial in 2013 by Weinstein et al., patients were instructed to wear a brace for at least 18 hours a day. The treatment success rates of brace-wearing patients were 40% for less than 6 hours each day; 70% for 6-12 hours each day, and 90% for more than 13 hours each day, which suggests that full-time bracing is optimal.
However, he added that physicians should keep in mind the sensitivities of youth and effect on their self-esteem when prescribing bracing, as many adolescents will have a fear of ridicule.
“The goals of bracing treatment for AIS are manifold: avoiding surgical treatment, preventing future back pain, maintaining respiratory function, and reducing the psychological impact of the deformity,” Dr. Nagata wrote. “Physicians should understand these aspects and take a balanced view of patients who refuse full-time bracing.”
He added that future improvements in design of the braces and less rigid alternatives will be important.
The trial was funded by the Swedish Research Council and by the Stockholm County Council, the Swedish Society of Spinal Surgeons, the Karolinska Institutet and the Crown Princess Lovisas Foundation. Study coauthor Paul Gerdhem, MD, PhD, reports grants from the Karolinska Institutet beyond his usual salary during the study and personal fees for lectures from DePuy Synthes and grants from Philips Healthcare paid to the institution outside the submitted work. No other disclosures were reported. Dr. Nagata reported no relevant financial relationships.
, new research suggests.
In the randomized Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS) trial, researchers, led by Anastasios Charalampidis, MD, PhD, with the Department of Clinical Science, Intervention and Technology at Karolinska Institutet in Stockholm, Sweden, tested whether a group using self-managed physical activity combined with either nighttime bracing for 8 hours or scoliosis-specific exercise achieved better results than a control group doing self-managed physical activity alone for 1 hour per day in preventing Cobb angle progression in moderate-grade AIS.
Findings of the trial, conducted in 6 public hospitals across Sweden, were published online in JAMA Network Open.
Night Bracing More Effective Than Comparison Arms
In the trial of 135 patients, aged 9-17 years, who were skeletally immature with moderate AIS, researchers found that night bracing plus self-managed physical activity prevented curve progression of more than 6 degrees (treatment success) to a significantly greater extent than did either self-managed physical activity alone or scoliosis-specific exercise.
A secondary outcome of curve progression was the number of patients who had surgery up until 2 years after the primary outcome.
The average age of patients was 12.7 years and most (82%) were female. Patients with treatment failure (curve progression of more than 6 degrees) had the option to transition to a full-time brace until skeletal maturity. That option resulted in similar frequency of surgery independent of initial treatment, according to the paper.
AIS is a structural deformity of the spinal column, affecting otherwise healthy children and adolescents during their growth spurt.
Previous studies have suggested that full-time bracing is effective in treating moderate-grade AIS. But the physical distress and psychological side effects that some experience can cause low adherence or rejection of the treatment.
The authors wrote that, “To our knowledge, there have been no randomized clinical trials investigating night bracing versus a control group.”
In this trial, treatment success was seen in 34 of 45 patients (76%) in the nighttime-bracing group and in 24 of 45 patients (53%) in the physical activity–alone group (odds ratio [OR], 2.7; 95% CI, 1.1-6.6). Success occurred in 26 of 45 patients (58%) in the scoliosis-specific exercise group (OR for scoliosis-specific exercise vs physical activity alone, 1.2; 95% CI, 0.5-2.8).
Adverse Events
Patients and clinicians could respond to an open-ended question regarding adverse events at each 6-month follow-up. Nineteen adverse events were reported in 15 patients between the start of the study up until the primary outcome was reached.
In the night-bracing group, there were 16 adverse events reported among 12 patients. They were: trunk pressure and skin problems (n = 10); sleeping problems (n = 2); emotional problems (n = 1); shoulder/neck pain (n = 2); and unspecified AEs (n = 1). In the scoliosis-specific exercise group, 3 adverse events were reported in 3 patients (pain during treatment (n = 1), muscle strain (n = 1), and low back pain (n = 1). No adverse events were reported in the physical activity alone group.
In an invited commentary, Kosei Nagata, MD, PhD, with the Department of Orthopaedic Surgery and Spinal Surgery at The University of Tokyo Hospital in Tokyo, Japan, said the study makes two important points.
“First, it was reaffirmed that the basis of scoliosis treatment is bracing and not a specific exercise therapy,” he wrote. “Second, nighttime bracing can be an effective alternative intervention for patients rejecting full-time bracing.”
He emphasized, however, that nighttime bracing alone is not enough to achieve success. In this study, bracing was combined with exercise. And the number of hours worn is important.
“Physicians should explain to patients with AIS and to their guardians the significant association between hours of brace wear and treatment success,” Dr. Nagata wrote. He pointed out that, in a previous randomized clinical trial in 2013 by Weinstein et al., patients were instructed to wear a brace for at least 18 hours a day. The treatment success rates of brace-wearing patients were 40% for less than 6 hours each day; 70% for 6-12 hours each day, and 90% for more than 13 hours each day, which suggests that full-time bracing is optimal.
However, he added that physicians should keep in mind the sensitivities of youth and effect on their self-esteem when prescribing bracing, as many adolescents will have a fear of ridicule.
“The goals of bracing treatment for AIS are manifold: avoiding surgical treatment, preventing future back pain, maintaining respiratory function, and reducing the psychological impact of the deformity,” Dr. Nagata wrote. “Physicians should understand these aspects and take a balanced view of patients who refuse full-time bracing.”
He added that future improvements in design of the braces and less rigid alternatives will be important.
The trial was funded by the Swedish Research Council and by the Stockholm County Council, the Swedish Society of Spinal Surgeons, the Karolinska Institutet and the Crown Princess Lovisas Foundation. Study coauthor Paul Gerdhem, MD, PhD, reports grants from the Karolinska Institutet beyond his usual salary during the study and personal fees for lectures from DePuy Synthes and grants from Philips Healthcare paid to the institution outside the submitted work. No other disclosures were reported. Dr. Nagata reported no relevant financial relationships.
FROM JAMA NETWORK OPEN
Treating Acne Scars Can Improve Aesthetics, Quality of Life
ORLANDO, FLORIDA — For some people, acne carries a one-two punch. First, they experience acne that is significant enough to decrease their quality of life, followed by scarring that can last a lifetime. For those patients, dermatologists have several options: Subcision to lift the depression of the scar, laser treatment to lower the height of scar tissue, and injections to fill scars.
“In my practice, I find that ,” Robyn Siperstein, MD, said at the annual ODAC Dermatology, Aesthetic & Surgical Conference.
Dr. Siperstein starts by identifying the type of acne scar — rolling scars, boxcar scars, or ice pick scars. Rolling scars tend to be shallower with no sharp edges; boxcar scars are deeper, more defined round or oval depressions; and ice pick scars, as the name suggests, look like someone stuck tiny ice picks into the skin, leaving a sunken or pitted appearance.
“It’s really important to categorize so that we know which ones are going to be effectively treated with different modalities and which ones aren’t, so that we can give our patients realistic expectations,” said Dr. Siperstein, a cosmetic dermatologist in private practice in Boca Raton, Florida, and a clinical affiliate associate professor of dermatology at Florida Atlantic University, Boca Raton.
“There’s not going to be one treatment that’s right for everything,” she said. Different approaches may be required even for the same patient because some people present with all three types of acne scars, she added.
Combining Treatments
When it comes to injecting dermal fillers into acne scars to lift the depressed areas, the US Food and Drug Administration approved a filler with polymethyl methacrylate filler and bovine collagen (Bellafill) for this indication (moderate to severe, atrophic, distensible facial acne scars on the cheek in patients over age 21) in 2015. “And off-label, I use hyaluronic acid in my practice,” Dr. Siperstein said. Each filler “probably works a little bit better or differently on different types of scars.”
For rolling scars, she recommends hyaluronic acid (HA) dermal filler for everyone. “Of course, this is my opinion.” She was also a lead investigator in a randomized, placebo-controlled split-face study comparing HA filler with saline for correcting atrophic facial scars in 15 patients. The HA filler emerged superior, although there were some improvements with saline.
In her clinical experience, patients are happy with the results and ask, “Why didn’t the last four doctors do this?”
Boxcar scars are more challenging to fill with HA. In some cases, Dr. Siperstein is able to raise the depressed portion of the scar, but some of the vertical edges remain. In this scenario, she might combine treatments. Laser resurfacing, for example, might help convert boxcar scars into rolling scars, which then can be filled more successfully.
“Ice pick scars are tough,” Dr. Siperstein said. A punch removal technique can work in some cases, or she might try the “cross technique.” This involves placing acetic acid inside the scar using a Q-tip. “You have to be really careful,” she added, “because if you get it around the edges, it’s actually going to make the scar bigger.”
Choosing the Right Candidates
Selecting the right candidate for HA treatment of acne scars is essential. Dr. Siperstein shared the example of a lifeguard who had prominent acne scarring down the center of his chest. “He was embarrassed to go to the beach and take off his shirt. He said he felt like he had bullet holes in his chest.”
One month following treatment, “he had a really nice improvement, and now he feels really comfortable,” she said.
Some dermatologists might be reluctant to consider HA fillers for acne scarring because there is a misconception that HA is short-acting, lasting 6 months to 1 year before the effect wears off. That impression can persist from company-sponsored studies that limit follow-up to 6 months or 1 year “to get their drug to market,” she noted.
Also adding to this impression is that HA fillers in wrinkles may not last as long. Dr. Siperstein explained that wrinkles on the face are dynamic and constantly moving. In contrast, acne scars experience less movement, which helps the HA last longer. There is MRI evidence that shows HA fillers last over 2 years in the face, she added.
One tip to predict how well an acne scar might respond to filler injections is to squeeze it and look for the “dimple sign.” If the floor of the scar lifts up when squeezed, “we know that they’ll be a good candidate for hyaluronic acid filler.” Another tip is to inject HA in a retrograde technique high up in the skin. Inject tiny amounts — microdroplets — of the HA filler high on the dermis, she advised.
Deeper injections run the risk of raising the entire scar instead of filling it, she added.
Like many dermatologic procedures, before and after photos are essential to demonstrate improvements, Dr. Siperstein pointed out. Patients are often skeptical. “This happens a lot with acne scar patients. They’ve been to a million places that have promised results, they have not gotten them, and they are frustrated.”
Acne scars can result from picking, inflammation, or treatment. “This is what we see all day in clinic,” Dr. Siperstein said. “Somebody who had to undergo Accutane treatment but unfortunately is left with holes. This is a huge psychological burden on our patients,” she said, describing a younger patient who had scarring, which “led to depression — it was ruining his life.”
“His mom was willing to do whatever it took. And I said, You know what, I think filler will be enough,” Dr. Siperstein said. She counseled them that treatment would not make the scars disappear completely. But patients used to 10% improvements are very happy when their acne scars look 80% or 90% better, she added.
Dr. Siperstein received grant or research support and is a member of the speakers bureau for Allergan and Galderma. She is also a consultant/advisory board member for Allergan.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — For some people, acne carries a one-two punch. First, they experience acne that is significant enough to decrease their quality of life, followed by scarring that can last a lifetime. For those patients, dermatologists have several options: Subcision to lift the depression of the scar, laser treatment to lower the height of scar tissue, and injections to fill scars.
“In my practice, I find that ,” Robyn Siperstein, MD, said at the annual ODAC Dermatology, Aesthetic & Surgical Conference.
Dr. Siperstein starts by identifying the type of acne scar — rolling scars, boxcar scars, or ice pick scars. Rolling scars tend to be shallower with no sharp edges; boxcar scars are deeper, more defined round or oval depressions; and ice pick scars, as the name suggests, look like someone stuck tiny ice picks into the skin, leaving a sunken or pitted appearance.
“It’s really important to categorize so that we know which ones are going to be effectively treated with different modalities and which ones aren’t, so that we can give our patients realistic expectations,” said Dr. Siperstein, a cosmetic dermatologist in private practice in Boca Raton, Florida, and a clinical affiliate associate professor of dermatology at Florida Atlantic University, Boca Raton.
“There’s not going to be one treatment that’s right for everything,” she said. Different approaches may be required even for the same patient because some people present with all three types of acne scars, she added.
Combining Treatments
When it comes to injecting dermal fillers into acne scars to lift the depressed areas, the US Food and Drug Administration approved a filler with polymethyl methacrylate filler and bovine collagen (Bellafill) for this indication (moderate to severe, atrophic, distensible facial acne scars on the cheek in patients over age 21) in 2015. “And off-label, I use hyaluronic acid in my practice,” Dr. Siperstein said. Each filler “probably works a little bit better or differently on different types of scars.”
For rolling scars, she recommends hyaluronic acid (HA) dermal filler for everyone. “Of course, this is my opinion.” She was also a lead investigator in a randomized, placebo-controlled split-face study comparing HA filler with saline for correcting atrophic facial scars in 15 patients. The HA filler emerged superior, although there were some improvements with saline.
In her clinical experience, patients are happy with the results and ask, “Why didn’t the last four doctors do this?”
Boxcar scars are more challenging to fill with HA. In some cases, Dr. Siperstein is able to raise the depressed portion of the scar, but some of the vertical edges remain. In this scenario, she might combine treatments. Laser resurfacing, for example, might help convert boxcar scars into rolling scars, which then can be filled more successfully.
“Ice pick scars are tough,” Dr. Siperstein said. A punch removal technique can work in some cases, or she might try the “cross technique.” This involves placing acetic acid inside the scar using a Q-tip. “You have to be really careful,” she added, “because if you get it around the edges, it’s actually going to make the scar bigger.”
Choosing the Right Candidates
Selecting the right candidate for HA treatment of acne scars is essential. Dr. Siperstein shared the example of a lifeguard who had prominent acne scarring down the center of his chest. “He was embarrassed to go to the beach and take off his shirt. He said he felt like he had bullet holes in his chest.”
One month following treatment, “he had a really nice improvement, and now he feels really comfortable,” she said.
Some dermatologists might be reluctant to consider HA fillers for acne scarring because there is a misconception that HA is short-acting, lasting 6 months to 1 year before the effect wears off. That impression can persist from company-sponsored studies that limit follow-up to 6 months or 1 year “to get their drug to market,” she noted.
Also adding to this impression is that HA fillers in wrinkles may not last as long. Dr. Siperstein explained that wrinkles on the face are dynamic and constantly moving. In contrast, acne scars experience less movement, which helps the HA last longer. There is MRI evidence that shows HA fillers last over 2 years in the face, she added.
One tip to predict how well an acne scar might respond to filler injections is to squeeze it and look for the “dimple sign.” If the floor of the scar lifts up when squeezed, “we know that they’ll be a good candidate for hyaluronic acid filler.” Another tip is to inject HA in a retrograde technique high up in the skin. Inject tiny amounts — microdroplets — of the HA filler high on the dermis, she advised.
Deeper injections run the risk of raising the entire scar instead of filling it, she added.
Like many dermatologic procedures, before and after photos are essential to demonstrate improvements, Dr. Siperstein pointed out. Patients are often skeptical. “This happens a lot with acne scar patients. They’ve been to a million places that have promised results, they have not gotten them, and they are frustrated.”
Acne scars can result from picking, inflammation, or treatment. “This is what we see all day in clinic,” Dr. Siperstein said. “Somebody who had to undergo Accutane treatment but unfortunately is left with holes. This is a huge psychological burden on our patients,” she said, describing a younger patient who had scarring, which “led to depression — it was ruining his life.”
“His mom was willing to do whatever it took. And I said, You know what, I think filler will be enough,” Dr. Siperstein said. She counseled them that treatment would not make the scars disappear completely. But patients used to 10% improvements are very happy when their acne scars look 80% or 90% better, she added.
Dr. Siperstein received grant or research support and is a member of the speakers bureau for Allergan and Galderma. She is also a consultant/advisory board member for Allergan.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — For some people, acne carries a one-two punch. First, they experience acne that is significant enough to decrease their quality of life, followed by scarring that can last a lifetime. For those patients, dermatologists have several options: Subcision to lift the depression of the scar, laser treatment to lower the height of scar tissue, and injections to fill scars.
“In my practice, I find that ,” Robyn Siperstein, MD, said at the annual ODAC Dermatology, Aesthetic & Surgical Conference.
Dr. Siperstein starts by identifying the type of acne scar — rolling scars, boxcar scars, or ice pick scars. Rolling scars tend to be shallower with no sharp edges; boxcar scars are deeper, more defined round or oval depressions; and ice pick scars, as the name suggests, look like someone stuck tiny ice picks into the skin, leaving a sunken or pitted appearance.
“It’s really important to categorize so that we know which ones are going to be effectively treated with different modalities and which ones aren’t, so that we can give our patients realistic expectations,” said Dr. Siperstein, a cosmetic dermatologist in private practice in Boca Raton, Florida, and a clinical affiliate associate professor of dermatology at Florida Atlantic University, Boca Raton.
“There’s not going to be one treatment that’s right for everything,” she said. Different approaches may be required even for the same patient because some people present with all three types of acne scars, she added.
Combining Treatments
When it comes to injecting dermal fillers into acne scars to lift the depressed areas, the US Food and Drug Administration approved a filler with polymethyl methacrylate filler and bovine collagen (Bellafill) for this indication (moderate to severe, atrophic, distensible facial acne scars on the cheek in patients over age 21) in 2015. “And off-label, I use hyaluronic acid in my practice,” Dr. Siperstein said. Each filler “probably works a little bit better or differently on different types of scars.”
For rolling scars, she recommends hyaluronic acid (HA) dermal filler for everyone. “Of course, this is my opinion.” She was also a lead investigator in a randomized, placebo-controlled split-face study comparing HA filler with saline for correcting atrophic facial scars in 15 patients. The HA filler emerged superior, although there were some improvements with saline.
In her clinical experience, patients are happy with the results and ask, “Why didn’t the last four doctors do this?”
Boxcar scars are more challenging to fill with HA. In some cases, Dr. Siperstein is able to raise the depressed portion of the scar, but some of the vertical edges remain. In this scenario, she might combine treatments. Laser resurfacing, for example, might help convert boxcar scars into rolling scars, which then can be filled more successfully.
“Ice pick scars are tough,” Dr. Siperstein said. A punch removal technique can work in some cases, or she might try the “cross technique.” This involves placing acetic acid inside the scar using a Q-tip. “You have to be really careful,” she added, “because if you get it around the edges, it’s actually going to make the scar bigger.”
Choosing the Right Candidates
Selecting the right candidate for HA treatment of acne scars is essential. Dr. Siperstein shared the example of a lifeguard who had prominent acne scarring down the center of his chest. “He was embarrassed to go to the beach and take off his shirt. He said he felt like he had bullet holes in his chest.”
One month following treatment, “he had a really nice improvement, and now he feels really comfortable,” she said.
Some dermatologists might be reluctant to consider HA fillers for acne scarring because there is a misconception that HA is short-acting, lasting 6 months to 1 year before the effect wears off. That impression can persist from company-sponsored studies that limit follow-up to 6 months or 1 year “to get their drug to market,” she noted.
Also adding to this impression is that HA fillers in wrinkles may not last as long. Dr. Siperstein explained that wrinkles on the face are dynamic and constantly moving. In contrast, acne scars experience less movement, which helps the HA last longer. There is MRI evidence that shows HA fillers last over 2 years in the face, she added.
One tip to predict how well an acne scar might respond to filler injections is to squeeze it and look for the “dimple sign.” If the floor of the scar lifts up when squeezed, “we know that they’ll be a good candidate for hyaluronic acid filler.” Another tip is to inject HA in a retrograde technique high up in the skin. Inject tiny amounts — microdroplets — of the HA filler high on the dermis, she advised.
Deeper injections run the risk of raising the entire scar instead of filling it, she added.
Like many dermatologic procedures, before and after photos are essential to demonstrate improvements, Dr. Siperstein pointed out. Patients are often skeptical. “This happens a lot with acne scar patients. They’ve been to a million places that have promised results, they have not gotten them, and they are frustrated.”
Acne scars can result from picking, inflammation, or treatment. “This is what we see all day in clinic,” Dr. Siperstein said. “Somebody who had to undergo Accutane treatment but unfortunately is left with holes. This is a huge psychological burden on our patients,” she said, describing a younger patient who had scarring, which “led to depression — it was ruining his life.”
“His mom was willing to do whatever it took. And I said, You know what, I think filler will be enough,” Dr. Siperstein said. She counseled them that treatment would not make the scars disappear completely. But patients used to 10% improvements are very happy when their acne scars look 80% or 90% better, she added.
Dr. Siperstein received grant or research support and is a member of the speakers bureau for Allergan and Galderma. She is also a consultant/advisory board member for Allergan.
A version of this article appeared on Medscape.com.
FROM ODAC 2024
New Criteria Identify Sepsis in Children With Infection
New criteria for pediatric sepsis, based on a novel score that predicts mortality in children with suspected or confirmed infection, perform better than existing organ dysfunction scores and criteria and have the potential to improve clinical care globally, researchers say.
Current pediatric-specific criteria for sepsis were published in 2005, based on expert opinion. In 2016, sepsis was redefined for adults as life-threatening organ dysfunction caused by a dysregulated host response to infection, as opposed to an earlier focus on systemic inflammation. But the paradigm-shifting changes were not extended to children (< 18 years, but not newborns), setting the stage for the new initiative.
The new criteria, and their development and validation, were published in JAMA and presented the same day at the Society of Critical Care Medicine’s 2024 Critical Care Congress in Phoenix, Arizona.
International Consensus
“The new criteria we derived are based on data from electronic health records and analysis of more than 3 million pediatric healthcare encounters from 10 hospitals around the world, including in low-resource settings,” L. Nelson Sanchez-Pinto, MD, MBI, a critical care physician at the Ann and Robert H. Lurie Children’s Hospital of Chicago, told this news organization.
Dr. Sanchez-Pinto co-led the data group of the international expert task force convened by the Society of Critical Care Medicine (SCCM) to develop and validate the criteria, which are based on evidence from an international survey, systematic review and meta-analysis, a newly created organ dysfunction score (Phoenix Sepsis Score), and sites on four continents.
Based on the findings, the task force now suggests that pediatric sepsis be defined by a Phoenix Sepsis Score of at least 2 points in children with suspected infection, which indicates potentially life-threatening dysfunction of the respiratory, cardiovascular, coagulation, and/or neurological systems. Septic shock is defined as sepsis with at least 1 cardiovascular point in the score.
Disparities Across Settings
To derive and validate the new criteria across differently resourced settings, the researchers conducted a multicenter, international, retrospective cohort study involving 10 health systems in the United States, Colombia, Bangladesh, China, and Kenya, 3 of which were used as external validation sites.
Data were collected from pediatric emergency and inpatient encounters from 2010 to 2019. The development set comprised 3,049,699 children, and the external validation set included 581,317.
Stacked regression models to predict mortality in children with suspected infection were derived and validated using the best-performing organ dysfunction subscores from eight existing scores.
The final model was then translated into the integer-based Phoenix Sepsis Score and used to establish binary criteria for sepsis and septic shock.
Among 172,984 children with suspected infection in the first 24 hours (development set; 1.2% mortality), a four-organ-system model performed best. The Phoenix Sepsis Score — the integer version of the model — had areas under the precision recall curve of 0.23 to 0.38, and areas under the receiver operating characteristic curve of 0.71 to 0.92 to predict mortality in the validation sets.
A Phoenix Sepsis Score of 2 points or higher in children with suspected infection as criteria for sepsis, plus 1 or more cardiovascular points as criteria for septic shock, resulted in a higher positive predictive value and higher or similar sensitivity compared with the 2005 International Pediatric Sepsis Consensus Conference criteria across differently resourced settings.
Specifically, children with a Phoenix Sepsis Score of at least 2 points had in-hospital mortality of 7.1% in higher-resource settings and 28.5% in lower-resource settings — more than 8 times that of children with suspected infection not meeting these criteria.
Mortality also was higher in children who had organ dysfunction in at least one of four organ systems — respiratory, cardiovascular, coagulation, and/or neurological — that was not the primary site of infection.
Children with septic shock, indicated by at least 1 cardiovascular point in the Phoenix Sepsis Score, had severe hypotension for age, blood lactate exceeding 5 mmol/L, or need for vasoactive medication. These children had an in-hospital mortality rate of 10.8% in higher-resource settings and 33.5% in lower-resource settings.
A Better Score
Given the findings, the task force recommends that “the former criteria based on systemic inflammatory response syndrome should not be used to diagnose sepsis in children [and] the former term severe sepsis should no longer be used because sepsis is life-threatening organ dysfunction associated with infection and is thus indicative of a severe disease state.”
The task force cautions that although the four organs in the Phoenix Sepsis Score are most commonly involved in sepsis, “this does not diminish the crucial importance of the assessment and management of other organ dysfunction.”
Furthermore, they emphasize that the Phoenix score was designed to identify sepsis in children, not to screen children at risk for developing sepsis or early identification of children with suspected sepsis.
Additional Considerations
In related editorials, commentators noted some caveats and concerns with regard to the study design and the new criteria.
Roberto Jabornisky, MD, PhD, of National University of the Northeast, Corrientes, Argentina, and colleagues pointed out that “all the low-resource validation sites were institutions with electronic health records and most had PICUs [pediatric intensive care units], which does not adequately reflect conditions in most low-resource settings. These factors introduce a distinct bias favoring a ‘PICU-based consensus,’ potentially limiting the generalizability and adoption of the new criteria by health care practitioners in non-PICU and nonhospital settings responsible for recognizing and managing children with sepsis.” The editorialists called for additional prospective validation in differently resourced settings, especially those with the highest disease burdens.
“Until then,” they wrote, “it is essential to refrain from considering these criteria as an inflexible directive governing medical interventions for pediatric sepsis. No definition can fully substitute for the clinical judgment of an experienced, vigilant clinician caring for an unwell child.”
Erin F. Carlton, MD, MSc of the University of Michigan, Ann Arbor, and colleagues added in a separate editorial, “The Phoenix criteria identify a sicker subset of patients than prior SIRS [systemic inflammatory response syndrome]-based criteria. Some may worry this higher threshold could delay management of patients not meeting sepsis criteria. Just as patients with chest pain and a troponin leak warrant monitoring and treatment (but are not prioritized for immediate heart catheterization), patients with infection need monitoring and treatment. Improvements in care should thus be judged not only by improved outcomes among patients with sepsis but also by decreased progression to sepsis among patients with infection.”
The International Consensus Criteria paper was supported by the Society of Critical Care Medicine and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to Tellen C. Bennett, MD, MS, and Nelson Sanchez-Pinto, MD. Data for the Kenya site were collected with support of the Wellcome Trust to the Kenya Major Overseas Programme. Dr. Jabornisky reported no conflicts of interest. Dr. Carlton reported serving on the Pediatric Surviving Sepsis Campaign Guideline committee and receiving grant support from the NIH.
New criteria for pediatric sepsis, based on a novel score that predicts mortality in children with suspected or confirmed infection, perform better than existing organ dysfunction scores and criteria and have the potential to improve clinical care globally, researchers say.
Current pediatric-specific criteria for sepsis were published in 2005, based on expert opinion. In 2016, sepsis was redefined for adults as life-threatening organ dysfunction caused by a dysregulated host response to infection, as opposed to an earlier focus on systemic inflammation. But the paradigm-shifting changes were not extended to children (< 18 years, but not newborns), setting the stage for the new initiative.
The new criteria, and their development and validation, were published in JAMA and presented the same day at the Society of Critical Care Medicine’s 2024 Critical Care Congress in Phoenix, Arizona.
International Consensus
“The new criteria we derived are based on data from electronic health records and analysis of more than 3 million pediatric healthcare encounters from 10 hospitals around the world, including in low-resource settings,” L. Nelson Sanchez-Pinto, MD, MBI, a critical care physician at the Ann and Robert H. Lurie Children’s Hospital of Chicago, told this news organization.
Dr. Sanchez-Pinto co-led the data group of the international expert task force convened by the Society of Critical Care Medicine (SCCM) to develop and validate the criteria, which are based on evidence from an international survey, systematic review and meta-analysis, a newly created organ dysfunction score (Phoenix Sepsis Score), and sites on four continents.
Based on the findings, the task force now suggests that pediatric sepsis be defined by a Phoenix Sepsis Score of at least 2 points in children with suspected infection, which indicates potentially life-threatening dysfunction of the respiratory, cardiovascular, coagulation, and/or neurological systems. Septic shock is defined as sepsis with at least 1 cardiovascular point in the score.
Disparities Across Settings
To derive and validate the new criteria across differently resourced settings, the researchers conducted a multicenter, international, retrospective cohort study involving 10 health systems in the United States, Colombia, Bangladesh, China, and Kenya, 3 of which were used as external validation sites.
Data were collected from pediatric emergency and inpatient encounters from 2010 to 2019. The development set comprised 3,049,699 children, and the external validation set included 581,317.
Stacked regression models to predict mortality in children with suspected infection were derived and validated using the best-performing organ dysfunction subscores from eight existing scores.
The final model was then translated into the integer-based Phoenix Sepsis Score and used to establish binary criteria for sepsis and septic shock.
Among 172,984 children with suspected infection in the first 24 hours (development set; 1.2% mortality), a four-organ-system model performed best. The Phoenix Sepsis Score — the integer version of the model — had areas under the precision recall curve of 0.23 to 0.38, and areas under the receiver operating characteristic curve of 0.71 to 0.92 to predict mortality in the validation sets.
A Phoenix Sepsis Score of 2 points or higher in children with suspected infection as criteria for sepsis, plus 1 or more cardiovascular points as criteria for septic shock, resulted in a higher positive predictive value and higher or similar sensitivity compared with the 2005 International Pediatric Sepsis Consensus Conference criteria across differently resourced settings.
Specifically, children with a Phoenix Sepsis Score of at least 2 points had in-hospital mortality of 7.1% in higher-resource settings and 28.5% in lower-resource settings — more than 8 times that of children with suspected infection not meeting these criteria.
Mortality also was higher in children who had organ dysfunction in at least one of four organ systems — respiratory, cardiovascular, coagulation, and/or neurological — that was not the primary site of infection.
Children with septic shock, indicated by at least 1 cardiovascular point in the Phoenix Sepsis Score, had severe hypotension for age, blood lactate exceeding 5 mmol/L, or need for vasoactive medication. These children had an in-hospital mortality rate of 10.8% in higher-resource settings and 33.5% in lower-resource settings.
A Better Score
Given the findings, the task force recommends that “the former criteria based on systemic inflammatory response syndrome should not be used to diagnose sepsis in children [and] the former term severe sepsis should no longer be used because sepsis is life-threatening organ dysfunction associated with infection and is thus indicative of a severe disease state.”
The task force cautions that although the four organs in the Phoenix Sepsis Score are most commonly involved in sepsis, “this does not diminish the crucial importance of the assessment and management of other organ dysfunction.”
Furthermore, they emphasize that the Phoenix score was designed to identify sepsis in children, not to screen children at risk for developing sepsis or early identification of children with suspected sepsis.
Additional Considerations
In related editorials, commentators noted some caveats and concerns with regard to the study design and the new criteria.
Roberto Jabornisky, MD, PhD, of National University of the Northeast, Corrientes, Argentina, and colleagues pointed out that “all the low-resource validation sites were institutions with electronic health records and most had PICUs [pediatric intensive care units], which does not adequately reflect conditions in most low-resource settings. These factors introduce a distinct bias favoring a ‘PICU-based consensus,’ potentially limiting the generalizability and adoption of the new criteria by health care practitioners in non-PICU and nonhospital settings responsible for recognizing and managing children with sepsis.” The editorialists called for additional prospective validation in differently resourced settings, especially those with the highest disease burdens.
“Until then,” they wrote, “it is essential to refrain from considering these criteria as an inflexible directive governing medical interventions for pediatric sepsis. No definition can fully substitute for the clinical judgment of an experienced, vigilant clinician caring for an unwell child.”
Erin F. Carlton, MD, MSc of the University of Michigan, Ann Arbor, and colleagues added in a separate editorial, “The Phoenix criteria identify a sicker subset of patients than prior SIRS [systemic inflammatory response syndrome]-based criteria. Some may worry this higher threshold could delay management of patients not meeting sepsis criteria. Just as patients with chest pain and a troponin leak warrant monitoring and treatment (but are not prioritized for immediate heart catheterization), patients with infection need monitoring and treatment. Improvements in care should thus be judged not only by improved outcomes among patients with sepsis but also by decreased progression to sepsis among patients with infection.”
The International Consensus Criteria paper was supported by the Society of Critical Care Medicine and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to Tellen C. Bennett, MD, MS, and Nelson Sanchez-Pinto, MD. Data for the Kenya site were collected with support of the Wellcome Trust to the Kenya Major Overseas Programme. Dr. Jabornisky reported no conflicts of interest. Dr. Carlton reported serving on the Pediatric Surviving Sepsis Campaign Guideline committee and receiving grant support from the NIH.
New criteria for pediatric sepsis, based on a novel score that predicts mortality in children with suspected or confirmed infection, perform better than existing organ dysfunction scores and criteria and have the potential to improve clinical care globally, researchers say.
Current pediatric-specific criteria for sepsis were published in 2005, based on expert opinion. In 2016, sepsis was redefined for adults as life-threatening organ dysfunction caused by a dysregulated host response to infection, as opposed to an earlier focus on systemic inflammation. But the paradigm-shifting changes were not extended to children (< 18 years, but not newborns), setting the stage for the new initiative.
The new criteria, and their development and validation, were published in JAMA and presented the same day at the Society of Critical Care Medicine’s 2024 Critical Care Congress in Phoenix, Arizona.
International Consensus
“The new criteria we derived are based on data from electronic health records and analysis of more than 3 million pediatric healthcare encounters from 10 hospitals around the world, including in low-resource settings,” L. Nelson Sanchez-Pinto, MD, MBI, a critical care physician at the Ann and Robert H. Lurie Children’s Hospital of Chicago, told this news organization.
Dr. Sanchez-Pinto co-led the data group of the international expert task force convened by the Society of Critical Care Medicine (SCCM) to develop and validate the criteria, which are based on evidence from an international survey, systematic review and meta-analysis, a newly created organ dysfunction score (Phoenix Sepsis Score), and sites on four continents.
Based on the findings, the task force now suggests that pediatric sepsis be defined by a Phoenix Sepsis Score of at least 2 points in children with suspected infection, which indicates potentially life-threatening dysfunction of the respiratory, cardiovascular, coagulation, and/or neurological systems. Septic shock is defined as sepsis with at least 1 cardiovascular point in the score.
Disparities Across Settings
To derive and validate the new criteria across differently resourced settings, the researchers conducted a multicenter, international, retrospective cohort study involving 10 health systems in the United States, Colombia, Bangladesh, China, and Kenya, 3 of which were used as external validation sites.
Data were collected from pediatric emergency and inpatient encounters from 2010 to 2019. The development set comprised 3,049,699 children, and the external validation set included 581,317.
Stacked regression models to predict mortality in children with suspected infection were derived and validated using the best-performing organ dysfunction subscores from eight existing scores.
The final model was then translated into the integer-based Phoenix Sepsis Score and used to establish binary criteria for sepsis and septic shock.
Among 172,984 children with suspected infection in the first 24 hours (development set; 1.2% mortality), a four-organ-system model performed best. The Phoenix Sepsis Score — the integer version of the model — had areas under the precision recall curve of 0.23 to 0.38, and areas under the receiver operating characteristic curve of 0.71 to 0.92 to predict mortality in the validation sets.
A Phoenix Sepsis Score of 2 points or higher in children with suspected infection as criteria for sepsis, plus 1 or more cardiovascular points as criteria for septic shock, resulted in a higher positive predictive value and higher or similar sensitivity compared with the 2005 International Pediatric Sepsis Consensus Conference criteria across differently resourced settings.
Specifically, children with a Phoenix Sepsis Score of at least 2 points had in-hospital mortality of 7.1% in higher-resource settings and 28.5% in lower-resource settings — more than 8 times that of children with suspected infection not meeting these criteria.
Mortality also was higher in children who had organ dysfunction in at least one of four organ systems — respiratory, cardiovascular, coagulation, and/or neurological — that was not the primary site of infection.
Children with septic shock, indicated by at least 1 cardiovascular point in the Phoenix Sepsis Score, had severe hypotension for age, blood lactate exceeding 5 mmol/L, or need for vasoactive medication. These children had an in-hospital mortality rate of 10.8% in higher-resource settings and 33.5% in lower-resource settings.
A Better Score
Given the findings, the task force recommends that “the former criteria based on systemic inflammatory response syndrome should not be used to diagnose sepsis in children [and] the former term severe sepsis should no longer be used because sepsis is life-threatening organ dysfunction associated with infection and is thus indicative of a severe disease state.”
The task force cautions that although the four organs in the Phoenix Sepsis Score are most commonly involved in sepsis, “this does not diminish the crucial importance of the assessment and management of other organ dysfunction.”
Furthermore, they emphasize that the Phoenix score was designed to identify sepsis in children, not to screen children at risk for developing sepsis or early identification of children with suspected sepsis.
Additional Considerations
In related editorials, commentators noted some caveats and concerns with regard to the study design and the new criteria.
Roberto Jabornisky, MD, PhD, of National University of the Northeast, Corrientes, Argentina, and colleagues pointed out that “all the low-resource validation sites were institutions with electronic health records and most had PICUs [pediatric intensive care units], which does not adequately reflect conditions in most low-resource settings. These factors introduce a distinct bias favoring a ‘PICU-based consensus,’ potentially limiting the generalizability and adoption of the new criteria by health care practitioners in non-PICU and nonhospital settings responsible for recognizing and managing children with sepsis.” The editorialists called for additional prospective validation in differently resourced settings, especially those with the highest disease burdens.
“Until then,” they wrote, “it is essential to refrain from considering these criteria as an inflexible directive governing medical interventions for pediatric sepsis. No definition can fully substitute for the clinical judgment of an experienced, vigilant clinician caring for an unwell child.”
Erin F. Carlton, MD, MSc of the University of Michigan, Ann Arbor, and colleagues added in a separate editorial, “The Phoenix criteria identify a sicker subset of patients than prior SIRS [systemic inflammatory response syndrome]-based criteria. Some may worry this higher threshold could delay management of patients not meeting sepsis criteria. Just as patients with chest pain and a troponin leak warrant monitoring and treatment (but are not prioritized for immediate heart catheterization), patients with infection need monitoring and treatment. Improvements in care should thus be judged not only by improved outcomes among patients with sepsis but also by decreased progression to sepsis among patients with infection.”
The International Consensus Criteria paper was supported by the Society of Critical Care Medicine and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to Tellen C. Bennett, MD, MS, and Nelson Sanchez-Pinto, MD. Data for the Kenya site were collected with support of the Wellcome Trust to the Kenya Major Overseas Programme. Dr. Jabornisky reported no conflicts of interest. Dr. Carlton reported serving on the Pediatric Surviving Sepsis Campaign Guideline committee and receiving grant support from the NIH.
FROM JAMA
CT Poses Risk for Malignant Hematopathies Among Children
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
Mental Health Screening May Benefit Youth With Obesity
TOPLINE:
Mental health comorbidities are prevalent among youth with overweight or obesity, with the strongest risk factors being male sex, older age, and extreme obesity.
METHODOLOGY:
- Researchers compared clinical characteristics and outcomes among children, adolescents, and young adults with overweight or obesity with or without a comorbid mental disorder who participated in a lifestyle intervention program.
- Overall, data from 114,248 individuals (age, 6-30 years; 53% females) from 226 centers in Germany and Austria participating in the Adiposity Patient Registry were evaluated.
- Individuals were excluded if they had bariatric surgery or used weight-modifying drugs (metformin, orlistat, or glucagon-like peptide-1 analogues).
- Body mass index (BMI) was calculated as a standard deviation score (SDS) from a German youth population reference and was used to define overweight (90th to < 97th percentile), obesity (97th percentile), and severe obesity (≥ 99.5th percentile), which at age 18 correspond to adult cutoffs for overweight and obesity (25 kg/m2 and 30 kg/m2, respectively).
- Regression analysis identified the factors associated with mental disorders in those with overweight or obesity.
TAKEAWAY:
- A comorbid mental disorder was reported in 3969 individuals, with attention-deficit disorder (ADHD, 42.5%), anxiety (31.3%), depression (24.3%), and eating disorders (12.9%) being the most common.
- The factors most strongly associated with mental health comorbidity were male sex (odds ratio [OR], 1.39; 95% CI, 1.27-1.52), older age (OR, 1.42; 95% CI, 1.25-1.62), and severe obesity (OR, 1.45; 95% CI, 1.30-1.63).
- Mean BMI-SDS was higher in individuals with depression and eating disorders and lower in individuals with ADHD (both P < .001) than in those without mental disorders.
- Individuals with and without mental disorders benefited from similar BMI changes from lifestyle intervention programs.
IN PRACTICE:
The authors wrote, “Healthcare professionals caring for youth with overweight or obesity should be aware of comorbid mental disorders, and regular mental health screening should be considered.”
SOURCE:
This study, led by Angela Galler from the Charité – Universitätsmedizin Berlin, Germany, was published online on January 9, 2024, in the International Journal of Obesity.
LIMITATIONS:
The study’s findings are based on data from a group of children, adolescents, and young adults with overweight or obesity treated in specialized obesity centers and may not be generalizable to all youth with obesity. Moreover, the study could not establish any conclusions regarding the cause or effect between obesity and mental disorders. Individuals were not tested psychologically for mental disorders and might have been underreported.
DISCLOSURES:
The manuscript is part of the Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy project, which was funded by the Innovative Medicines Initiative 2 Joint Undertaking. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Mental health comorbidities are prevalent among youth with overweight or obesity, with the strongest risk factors being male sex, older age, and extreme obesity.
METHODOLOGY:
- Researchers compared clinical characteristics and outcomes among children, adolescents, and young adults with overweight or obesity with or without a comorbid mental disorder who participated in a lifestyle intervention program.
- Overall, data from 114,248 individuals (age, 6-30 years; 53% females) from 226 centers in Germany and Austria participating in the Adiposity Patient Registry were evaluated.
- Individuals were excluded if they had bariatric surgery or used weight-modifying drugs (metformin, orlistat, or glucagon-like peptide-1 analogues).
- Body mass index (BMI) was calculated as a standard deviation score (SDS) from a German youth population reference and was used to define overweight (90th to < 97th percentile), obesity (97th percentile), and severe obesity (≥ 99.5th percentile), which at age 18 correspond to adult cutoffs for overweight and obesity (25 kg/m2 and 30 kg/m2, respectively).
- Regression analysis identified the factors associated with mental disorders in those with overweight or obesity.
TAKEAWAY:
- A comorbid mental disorder was reported in 3969 individuals, with attention-deficit disorder (ADHD, 42.5%), anxiety (31.3%), depression (24.3%), and eating disorders (12.9%) being the most common.
- The factors most strongly associated with mental health comorbidity were male sex (odds ratio [OR], 1.39; 95% CI, 1.27-1.52), older age (OR, 1.42; 95% CI, 1.25-1.62), and severe obesity (OR, 1.45; 95% CI, 1.30-1.63).
- Mean BMI-SDS was higher in individuals with depression and eating disorders and lower in individuals with ADHD (both P < .001) than in those without mental disorders.
- Individuals with and without mental disorders benefited from similar BMI changes from lifestyle intervention programs.
IN PRACTICE:
The authors wrote, “Healthcare professionals caring for youth with overweight or obesity should be aware of comorbid mental disorders, and regular mental health screening should be considered.”
SOURCE:
This study, led by Angela Galler from the Charité – Universitätsmedizin Berlin, Germany, was published online on January 9, 2024, in the International Journal of Obesity.
LIMITATIONS:
The study’s findings are based on data from a group of children, adolescents, and young adults with overweight or obesity treated in specialized obesity centers and may not be generalizable to all youth with obesity. Moreover, the study could not establish any conclusions regarding the cause or effect between obesity and mental disorders. Individuals were not tested psychologically for mental disorders and might have been underreported.
DISCLOSURES:
The manuscript is part of the Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy project, which was funded by the Innovative Medicines Initiative 2 Joint Undertaking. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Mental health comorbidities are prevalent among youth with overweight or obesity, with the strongest risk factors being male sex, older age, and extreme obesity.
METHODOLOGY:
- Researchers compared clinical characteristics and outcomes among children, adolescents, and young adults with overweight or obesity with or without a comorbid mental disorder who participated in a lifestyle intervention program.
- Overall, data from 114,248 individuals (age, 6-30 years; 53% females) from 226 centers in Germany and Austria participating in the Adiposity Patient Registry were evaluated.
- Individuals were excluded if they had bariatric surgery or used weight-modifying drugs (metformin, orlistat, or glucagon-like peptide-1 analogues).
- Body mass index (BMI) was calculated as a standard deviation score (SDS) from a German youth population reference and was used to define overweight (90th to < 97th percentile), obesity (97th percentile), and severe obesity (≥ 99.5th percentile), which at age 18 correspond to adult cutoffs for overweight and obesity (25 kg/m2 and 30 kg/m2, respectively).
- Regression analysis identified the factors associated with mental disorders in those with overweight or obesity.
TAKEAWAY:
- A comorbid mental disorder was reported in 3969 individuals, with attention-deficit disorder (ADHD, 42.5%), anxiety (31.3%), depression (24.3%), and eating disorders (12.9%) being the most common.
- The factors most strongly associated with mental health comorbidity were male sex (odds ratio [OR], 1.39; 95% CI, 1.27-1.52), older age (OR, 1.42; 95% CI, 1.25-1.62), and severe obesity (OR, 1.45; 95% CI, 1.30-1.63).
- Mean BMI-SDS was higher in individuals with depression and eating disorders and lower in individuals with ADHD (both P < .001) than in those without mental disorders.
- Individuals with and without mental disorders benefited from similar BMI changes from lifestyle intervention programs.
IN PRACTICE:
The authors wrote, “Healthcare professionals caring for youth with overweight or obesity should be aware of comorbid mental disorders, and regular mental health screening should be considered.”
SOURCE:
This study, led by Angela Galler from the Charité – Universitätsmedizin Berlin, Germany, was published online on January 9, 2024, in the International Journal of Obesity.
LIMITATIONS:
The study’s findings are based on data from a group of children, adolescents, and young adults with overweight or obesity treated in specialized obesity centers and may not be generalizable to all youth with obesity. Moreover, the study could not establish any conclusions regarding the cause or effect between obesity and mental disorders. Individuals were not tested psychologically for mental disorders and might have been underreported.
DISCLOSURES:
The manuscript is part of the Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy project, which was funded by the Innovative Medicines Initiative 2 Joint Undertaking. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Microbiome Impacts Vaccine Responses
When infants are born, they have nearly a clean slate with regard to their immune systems. Virtually all their immune cells are naive. They have no immunity memory. Vaccines at birth, and in the first 2 years of life, elicit variable antibody levels and cellular immune responses. Sometimes, this leaves fully vaccinated children unprotected against vaccine-preventable infectious diseases.
Newborns are bombarded at birth with microbes and other antigenic stimuli from the environment; food in the form of breast milk, formula, water; and vaccines, such as hepatitis B and, in other countries, with BCG. At birth, to avoid immunologically-induced injury, immune responses favor immunologic tolerance. However, adaptation must be rapid to avoid life-threatening infections. To navigate the gauntlet of microbe and environmental exposures and vaccines, the neonatal immune system moves through a gradual maturation process toward immune responsivity. The maturation occurs at different rates in different children.
Reassessing Vaccine Responsiveness
Vaccine responsiveness is usually assessed by measuring antibody levels in blood. Until recently, it was thought to be “bad luck” when a child failed to develop protective immunity following vaccination. The bad luck was suggested to involve illness at the time of vaccination, especially illness occurring with fever, and especially common viral infections. But studies proved that notion incorrect. About 10 years ago I became more interested in variability in vaccine responses in the first 2 years of life. In 2016, my laboratory described a specific population of children with specific cellular immune deficiencies that we classified as low vaccine responders (LVRs).1 To preclude the suggestion that low vaccine responses were to be considered normal biological variation, we chose an a priori definition of LVR as those with sub-protective IgG antibody levels to four (≥ 66 %) of six tested vaccines in DTaP-Hib (diphtheria toxoid, tetanus toxoid, pertussis toxoid, pertactin, and filamentous hemagglutinin [DTaP] and Haemophilus influenzae type b polysaccharide capsule [Hib]). Antibody levels were measured at 1 year of age following primary vaccinations at child age 2, 4, and 6 months old. The remaining 89% of children we termed normal vaccine responders (NVRs). We additionally tested antibody responses to viral protein and pneumococcal polysaccharide conjugated antigens (polio serotypes 1, 2, and 3, hepatitis B, and Streptococcus pneumoniae capsular polysaccharides serotypes 6B, 14, and 23F). Responses to these vaccine antigens were similar to the six vaccines (DTaP/Hib) used to define LVR. We and other groups have used alternative definitions of low vaccine responses that rely on statistics.
I recently reviewed the topic of the determinants of vaccine responses in early life, with a focus on the infant microbiome and metabolome: a.) cesarean section versus vaginal delivery, b.) breast versus formula feeding and c.) antibiotic exposure, that impact the immune response2 (Figure). In the review I also discussed how microbiome may serve as natural adjuvants for vaccine responses, how microbiota-derived metabolites influence vaccine responses, and how low vaccine responses in early life may be linked to increased infection susceptibility (Figure).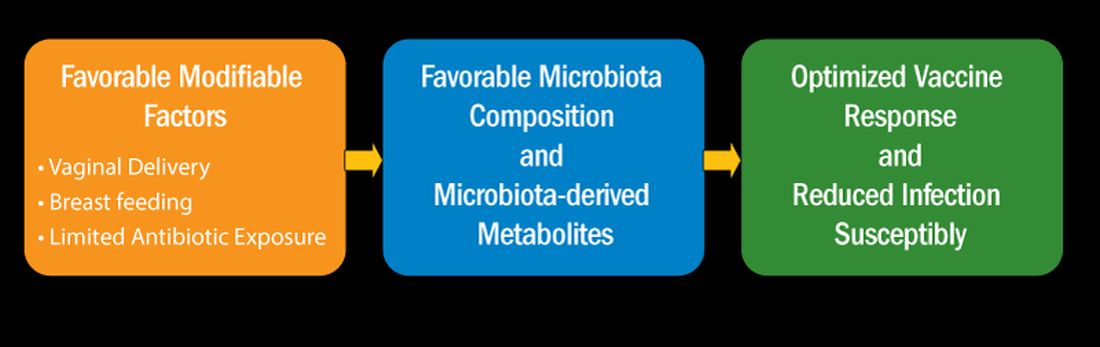
Cesarean section births occur in nearly 30% of newborns. Cesarean section birth has been associated with adverse effects on immune development, including predisposing to infections, allergies, and inflammatory disorders. The association of these adverse outcomes has been linked to lower total microbiome diversity. Fecal microbiome seeding from mother to infant in vaginal-delivered infants results in a more favorable and stable microbiome compared with cesarean-delivered infants. Nasopharyngeal microbiome may also be adversely affected by cesarean delivery. In turn, those microbiome differences can be linked to variation in vaccine responsiveness in infants.
Multiple studies strongly support the notion that breastfeeding has a favorable impact on immune development in early life associated with better vaccine responses, mediated by the microbiome. The mechanism of favorable immune responses to vaccines largely relates to the presence of a specific bacteria species, Bifidobacterium infantis. Breast milk contains human milk oligosaccharides that are not digestible by newborns. B. infantis is a strain of bacteria that utilizes these non-digestible oligosaccharides. Thereby, infants fed breast milk provides B. infantis the essential source of nutrition for its growth and predominance in the newborn gut. Studies have shown that Bifidobacterium spp. abundance in early life is correlated with better immune responses to multiple vaccines. Bifidobacterium spp. abundance has been positively correlated with antibody responses measured after 2 years, linking the microbiome composition to the durability of vaccine-induced immune responses.
Antibiotic exposure in early life may disproportionately damage the newborn and infant microbiome compared with later childhood. The average child receives about three antibiotic courses by the age of 2 years. My lab was among the first to describe the adverse effects of antibiotics on vaccine responses in early life.3 We found that broader spectrum antibiotics had a greater adverse effect on vaccine-induced antibody levels than narrower spectrum antibiotics. Ten-day versus five-day treatment courses had a greater negative effect. Multiple antibiotic courses over time (cumulative antibiotic exposure) was negatively associated with vaccine-induced antibody levels.
Over 11 % of live births worldwide occur preterm. Because bacterial infections are frequent complications of preterm birth, 79 % of very low birthweight and 87 % of extremely low birthweight infants in US NICUs receive antibiotics within 3 days of birth. Recently, my group studied full-term infants at birth and found that exposure to parenteral antibiotics at birth or during the first days of life had an adverse effect on vaccine responses.4
Microbiome Impacts Immunity
How does the microbiome affect immunity, and specifically vaccine responses? Microbial-derived metabolites affect host immunity. Gut bacteria produce short chain fatty acids (SCFAs: acetate, propionate, butyrate) [115]. SCFAs positively influence immunity cells. Vitamin D metabolites are generated by intestinal bacteria and those metabolites positively influence immunity. Secondary bile acids produced by Clostridium spp. are involved in favorable immune responses. Increased levels of phenylpyruvic acid produced by gut and/or nasopharyngeal microbiota correlate with reduced vaccine responses and upregulated metabolome genes that encode for oxidative phosphorylation correlate with increased vaccine responses.
In summary, immune development commences at birth. Impairment in responses to vaccination in children have been linked to disturbance in the microbiome. Cesarean section and absence of breastfeeding are associated with adverse microbiota composition. Antibiotics perturb healthy microbiota development. The microbiota affect immunity in several ways, among them are effects by metabolites generated by the commensals that inhabit the child host. A child who responds poorly to vaccines and has specific immune cell dysfunction caused by problems with the microbiome also displays increased infection proneness. But that is a story for another column, later.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Pichichero ME et al. J Infect Dis. 2016 Jun 15;213(12):2014-2019. doi: 10.1093/infdis/jiw053.
2. Pichichero ME. Cell Immunol. 2023 Nov-Dec:393-394:104777. doi: 10.1016/j.cellimm.2023.104777.
3. Chapman TJ et al. Pediatrics. 2022 May 1;149(5):e2021052061. doi: 10.1542/peds.2021-052061.
4. Shaffer M et al. mSystems. 2023 Oct 26;8(5):e0066123. doi: 10.1128/msystems.00661-23.
When infants are born, they have nearly a clean slate with regard to their immune systems. Virtually all their immune cells are naive. They have no immunity memory. Vaccines at birth, and in the first 2 years of life, elicit variable antibody levels and cellular immune responses. Sometimes, this leaves fully vaccinated children unprotected against vaccine-preventable infectious diseases.
Newborns are bombarded at birth with microbes and other antigenic stimuli from the environment; food in the form of breast milk, formula, water; and vaccines, such as hepatitis B and, in other countries, with BCG. At birth, to avoid immunologically-induced injury, immune responses favor immunologic tolerance. However, adaptation must be rapid to avoid life-threatening infections. To navigate the gauntlet of microbe and environmental exposures and vaccines, the neonatal immune system moves through a gradual maturation process toward immune responsivity. The maturation occurs at different rates in different children.
Reassessing Vaccine Responsiveness
Vaccine responsiveness is usually assessed by measuring antibody levels in blood. Until recently, it was thought to be “bad luck” when a child failed to develop protective immunity following vaccination. The bad luck was suggested to involve illness at the time of vaccination, especially illness occurring with fever, and especially common viral infections. But studies proved that notion incorrect. About 10 years ago I became more interested in variability in vaccine responses in the first 2 years of life. In 2016, my laboratory described a specific population of children with specific cellular immune deficiencies that we classified as low vaccine responders (LVRs).1 To preclude the suggestion that low vaccine responses were to be considered normal biological variation, we chose an a priori definition of LVR as those with sub-protective IgG antibody levels to four (≥ 66 %) of six tested vaccines in DTaP-Hib (diphtheria toxoid, tetanus toxoid, pertussis toxoid, pertactin, and filamentous hemagglutinin [DTaP] and Haemophilus influenzae type b polysaccharide capsule [Hib]). Antibody levels were measured at 1 year of age following primary vaccinations at child age 2, 4, and 6 months old. The remaining 89% of children we termed normal vaccine responders (NVRs). We additionally tested antibody responses to viral protein and pneumococcal polysaccharide conjugated antigens (polio serotypes 1, 2, and 3, hepatitis B, and Streptococcus pneumoniae capsular polysaccharides serotypes 6B, 14, and 23F). Responses to these vaccine antigens were similar to the six vaccines (DTaP/Hib) used to define LVR. We and other groups have used alternative definitions of low vaccine responses that rely on statistics.
I recently reviewed the topic of the determinants of vaccine responses in early life, with a focus on the infant microbiome and metabolome: a.) cesarean section versus vaginal delivery, b.) breast versus formula feeding and c.) antibiotic exposure, that impact the immune response2 (Figure). In the review I also discussed how microbiome may serve as natural adjuvants for vaccine responses, how microbiota-derived metabolites influence vaccine responses, and how low vaccine responses in early life may be linked to increased infection susceptibility (Figure).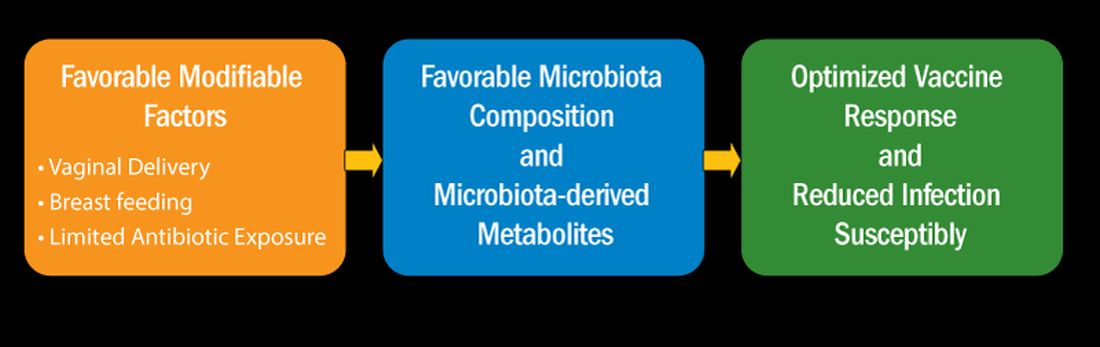
Cesarean section births occur in nearly 30% of newborns. Cesarean section birth has been associated with adverse effects on immune development, including predisposing to infections, allergies, and inflammatory disorders. The association of these adverse outcomes has been linked to lower total microbiome diversity. Fecal microbiome seeding from mother to infant in vaginal-delivered infants results in a more favorable and stable microbiome compared with cesarean-delivered infants. Nasopharyngeal microbiome may also be adversely affected by cesarean delivery. In turn, those microbiome differences can be linked to variation in vaccine responsiveness in infants.
Multiple studies strongly support the notion that breastfeeding has a favorable impact on immune development in early life associated with better vaccine responses, mediated by the microbiome. The mechanism of favorable immune responses to vaccines largely relates to the presence of a specific bacteria species, Bifidobacterium infantis. Breast milk contains human milk oligosaccharides that are not digestible by newborns. B. infantis is a strain of bacteria that utilizes these non-digestible oligosaccharides. Thereby, infants fed breast milk provides B. infantis the essential source of nutrition for its growth and predominance in the newborn gut. Studies have shown that Bifidobacterium spp. abundance in early life is correlated with better immune responses to multiple vaccines. Bifidobacterium spp. abundance has been positively correlated with antibody responses measured after 2 years, linking the microbiome composition to the durability of vaccine-induced immune responses.
Antibiotic exposure in early life may disproportionately damage the newborn and infant microbiome compared with later childhood. The average child receives about three antibiotic courses by the age of 2 years. My lab was among the first to describe the adverse effects of antibiotics on vaccine responses in early life.3 We found that broader spectrum antibiotics had a greater adverse effect on vaccine-induced antibody levels than narrower spectrum antibiotics. Ten-day versus five-day treatment courses had a greater negative effect. Multiple antibiotic courses over time (cumulative antibiotic exposure) was negatively associated with vaccine-induced antibody levels.
Over 11 % of live births worldwide occur preterm. Because bacterial infections are frequent complications of preterm birth, 79 % of very low birthweight and 87 % of extremely low birthweight infants in US NICUs receive antibiotics within 3 days of birth. Recently, my group studied full-term infants at birth and found that exposure to parenteral antibiotics at birth or during the first days of life had an adverse effect on vaccine responses.4
Microbiome Impacts Immunity
How does the microbiome affect immunity, and specifically vaccine responses? Microbial-derived metabolites affect host immunity. Gut bacteria produce short chain fatty acids (SCFAs: acetate, propionate, butyrate) [115]. SCFAs positively influence immunity cells. Vitamin D metabolites are generated by intestinal bacteria and those metabolites positively influence immunity. Secondary bile acids produced by Clostridium spp. are involved in favorable immune responses. Increased levels of phenylpyruvic acid produced by gut and/or nasopharyngeal microbiota correlate with reduced vaccine responses and upregulated metabolome genes that encode for oxidative phosphorylation correlate with increased vaccine responses.
In summary, immune development commences at birth. Impairment in responses to vaccination in children have been linked to disturbance in the microbiome. Cesarean section and absence of breastfeeding are associated with adverse microbiota composition. Antibiotics perturb healthy microbiota development. The microbiota affect immunity in several ways, among them are effects by metabolites generated by the commensals that inhabit the child host. A child who responds poorly to vaccines and has specific immune cell dysfunction caused by problems with the microbiome also displays increased infection proneness. But that is a story for another column, later.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Pichichero ME et al. J Infect Dis. 2016 Jun 15;213(12):2014-2019. doi: 10.1093/infdis/jiw053.
2. Pichichero ME. Cell Immunol. 2023 Nov-Dec:393-394:104777. doi: 10.1016/j.cellimm.2023.104777.
3. Chapman TJ et al. Pediatrics. 2022 May 1;149(5):e2021052061. doi: 10.1542/peds.2021-052061.
4. Shaffer M et al. mSystems. 2023 Oct 26;8(5):e0066123. doi: 10.1128/msystems.00661-23.
When infants are born, they have nearly a clean slate with regard to their immune systems. Virtually all their immune cells are naive. They have no immunity memory. Vaccines at birth, and in the first 2 years of life, elicit variable antibody levels and cellular immune responses. Sometimes, this leaves fully vaccinated children unprotected against vaccine-preventable infectious diseases.
Newborns are bombarded at birth with microbes and other antigenic stimuli from the environment; food in the form of breast milk, formula, water; and vaccines, such as hepatitis B and, in other countries, with BCG. At birth, to avoid immunologically-induced injury, immune responses favor immunologic tolerance. However, adaptation must be rapid to avoid life-threatening infections. To navigate the gauntlet of microbe and environmental exposures and vaccines, the neonatal immune system moves through a gradual maturation process toward immune responsivity. The maturation occurs at different rates in different children.
Reassessing Vaccine Responsiveness
Vaccine responsiveness is usually assessed by measuring antibody levels in blood. Until recently, it was thought to be “bad luck” when a child failed to develop protective immunity following vaccination. The bad luck was suggested to involve illness at the time of vaccination, especially illness occurring with fever, and especially common viral infections. But studies proved that notion incorrect. About 10 years ago I became more interested in variability in vaccine responses in the first 2 years of life. In 2016, my laboratory described a specific population of children with specific cellular immune deficiencies that we classified as low vaccine responders (LVRs).1 To preclude the suggestion that low vaccine responses were to be considered normal biological variation, we chose an a priori definition of LVR as those with sub-protective IgG antibody levels to four (≥ 66 %) of six tested vaccines in DTaP-Hib (diphtheria toxoid, tetanus toxoid, pertussis toxoid, pertactin, and filamentous hemagglutinin [DTaP] and Haemophilus influenzae type b polysaccharide capsule [Hib]). Antibody levels were measured at 1 year of age following primary vaccinations at child age 2, 4, and 6 months old. The remaining 89% of children we termed normal vaccine responders (NVRs). We additionally tested antibody responses to viral protein and pneumococcal polysaccharide conjugated antigens (polio serotypes 1, 2, and 3, hepatitis B, and Streptococcus pneumoniae capsular polysaccharides serotypes 6B, 14, and 23F). Responses to these vaccine antigens were similar to the six vaccines (DTaP/Hib) used to define LVR. We and other groups have used alternative definitions of low vaccine responses that rely on statistics.
I recently reviewed the topic of the determinants of vaccine responses in early life, with a focus on the infant microbiome and metabolome: a.) cesarean section versus vaginal delivery, b.) breast versus formula feeding and c.) antibiotic exposure, that impact the immune response2 (Figure). In the review I also discussed how microbiome may serve as natural adjuvants for vaccine responses, how microbiota-derived metabolites influence vaccine responses, and how low vaccine responses in early life may be linked to increased infection susceptibility (Figure).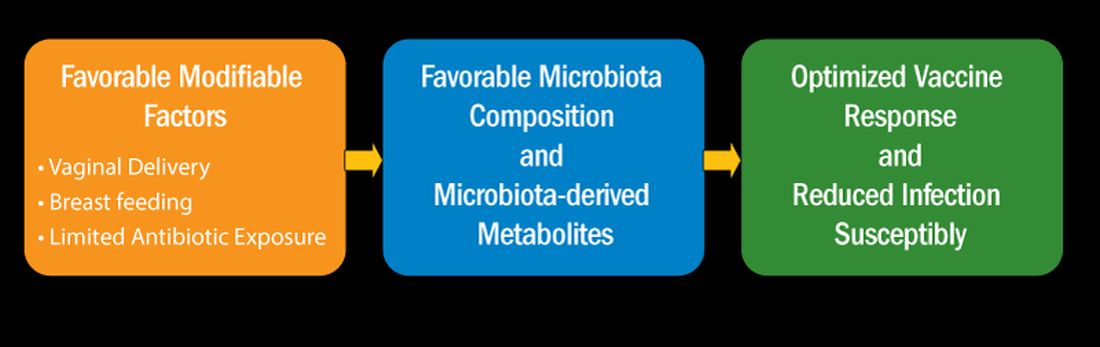
Cesarean section births occur in nearly 30% of newborns. Cesarean section birth has been associated with adverse effects on immune development, including predisposing to infections, allergies, and inflammatory disorders. The association of these adverse outcomes has been linked to lower total microbiome diversity. Fecal microbiome seeding from mother to infant in vaginal-delivered infants results in a more favorable and stable microbiome compared with cesarean-delivered infants. Nasopharyngeal microbiome may also be adversely affected by cesarean delivery. In turn, those microbiome differences can be linked to variation in vaccine responsiveness in infants.
Multiple studies strongly support the notion that breastfeeding has a favorable impact on immune development in early life associated with better vaccine responses, mediated by the microbiome. The mechanism of favorable immune responses to vaccines largely relates to the presence of a specific bacteria species, Bifidobacterium infantis. Breast milk contains human milk oligosaccharides that are not digestible by newborns. B. infantis is a strain of bacteria that utilizes these non-digestible oligosaccharides. Thereby, infants fed breast milk provides B. infantis the essential source of nutrition for its growth and predominance in the newborn gut. Studies have shown that Bifidobacterium spp. abundance in early life is correlated with better immune responses to multiple vaccines. Bifidobacterium spp. abundance has been positively correlated with antibody responses measured after 2 years, linking the microbiome composition to the durability of vaccine-induced immune responses.
Antibiotic exposure in early life may disproportionately damage the newborn and infant microbiome compared with later childhood. The average child receives about three antibiotic courses by the age of 2 years. My lab was among the first to describe the adverse effects of antibiotics on vaccine responses in early life.3 We found that broader spectrum antibiotics had a greater adverse effect on vaccine-induced antibody levels than narrower spectrum antibiotics. Ten-day versus five-day treatment courses had a greater negative effect. Multiple antibiotic courses over time (cumulative antibiotic exposure) was negatively associated with vaccine-induced antibody levels.
Over 11 % of live births worldwide occur preterm. Because bacterial infections are frequent complications of preterm birth, 79 % of very low birthweight and 87 % of extremely low birthweight infants in US NICUs receive antibiotics within 3 days of birth. Recently, my group studied full-term infants at birth and found that exposure to parenteral antibiotics at birth or during the first days of life had an adverse effect on vaccine responses.4
Microbiome Impacts Immunity
How does the microbiome affect immunity, and specifically vaccine responses? Microbial-derived metabolites affect host immunity. Gut bacteria produce short chain fatty acids (SCFAs: acetate, propionate, butyrate) [115]. SCFAs positively influence immunity cells. Vitamin D metabolites are generated by intestinal bacteria and those metabolites positively influence immunity. Secondary bile acids produced by Clostridium spp. are involved in favorable immune responses. Increased levels of phenylpyruvic acid produced by gut and/or nasopharyngeal microbiota correlate with reduced vaccine responses and upregulated metabolome genes that encode for oxidative phosphorylation correlate with increased vaccine responses.
In summary, immune development commences at birth. Impairment in responses to vaccination in children have been linked to disturbance in the microbiome. Cesarean section and absence of breastfeeding are associated with adverse microbiota composition. Antibiotics perturb healthy microbiota development. The microbiota affect immunity in several ways, among them are effects by metabolites generated by the commensals that inhabit the child host. A child who responds poorly to vaccines and has specific immune cell dysfunction caused by problems with the microbiome also displays increased infection proneness. But that is a story for another column, later.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Pichichero ME et al. J Infect Dis. 2016 Jun 15;213(12):2014-2019. doi: 10.1093/infdis/jiw053.
2. Pichichero ME. Cell Immunol. 2023 Nov-Dec:393-394:104777. doi: 10.1016/j.cellimm.2023.104777.
3. Chapman TJ et al. Pediatrics. 2022 May 1;149(5):e2021052061. doi: 10.1542/peds.2021-052061.
4. Shaffer M et al. mSystems. 2023 Oct 26;8(5):e0066123. doi: 10.1128/msystems.00661-23.
Ibuprofen Fails for Patent Ductus Arteriosus in Preterm Infants
The study population included infants born between 23 weeks 0 days’ and 28 weeks 6 days’ gestation. The researchers randomized 326 extremely preterm infants with patent ductus arteriosus (PDA) at 72 hours or less after birth to ibuprofen at a loading dose of 10 mg/kg followed by two doses of 5 mg/kg at least 24 hours apart, and 327 to placebo.
The PDAs in the infants had a diameter of at least 1.5 mm with pulsatile flow.
Severe dysplasia outcome
The study’s primary outcome was a composite of death or moderate to severe bronchopulmonary dysplasia at 36 weeks’ postmenstrual age. Overall, a primary outcome occurred in 69.2% of infants who received ibuprofen and 63.5% of those who received a placebo.
Risk of death or bronchopulmonary dysplasia at 36 weeks’ postmenstrual age was not reduced by early ibuprofen vs. placebo for preterm infants, the researchers concluded. Moderate or severe bronchopulmonary dysplasia occurred in 64.2% of the infants in the ibuprofen group and 59.3% of the placebo group who survived to 36 weeks’ postmenstrual age.
‘Unforeseeable’ serious adverse events
Forty-four deaths occurred in the ibuprofen group and 33 in the placebo group (adjusted risk ratio 1.09). Two “unforeseeable” serious adverse events occurred during the study that were potentially related to ibuprofen.
The lead author was Samir Gupta, MD, of Sidra Medicine, Doha, Qatar. The study was published online in the New England Journal of Medicine.
Study limitations include incomplete data for some patients.
The study was supported by the National Institute for Health Research Health Technology Assessment Programme. The researchers had no financial conflicts to disclose.
The study population included infants born between 23 weeks 0 days’ and 28 weeks 6 days’ gestation. The researchers randomized 326 extremely preterm infants with patent ductus arteriosus (PDA) at 72 hours or less after birth to ibuprofen at a loading dose of 10 mg/kg followed by two doses of 5 mg/kg at least 24 hours apart, and 327 to placebo.
The PDAs in the infants had a diameter of at least 1.5 mm with pulsatile flow.
Severe dysplasia outcome
The study’s primary outcome was a composite of death or moderate to severe bronchopulmonary dysplasia at 36 weeks’ postmenstrual age. Overall, a primary outcome occurred in 69.2% of infants who received ibuprofen and 63.5% of those who received a placebo.
Risk of death or bronchopulmonary dysplasia at 36 weeks’ postmenstrual age was not reduced by early ibuprofen vs. placebo for preterm infants, the researchers concluded. Moderate or severe bronchopulmonary dysplasia occurred in 64.2% of the infants in the ibuprofen group and 59.3% of the placebo group who survived to 36 weeks’ postmenstrual age.
‘Unforeseeable’ serious adverse events
Forty-four deaths occurred in the ibuprofen group and 33 in the placebo group (adjusted risk ratio 1.09). Two “unforeseeable” serious adverse events occurred during the study that were potentially related to ibuprofen.
The lead author was Samir Gupta, MD, of Sidra Medicine, Doha, Qatar. The study was published online in the New England Journal of Medicine.
Study limitations include incomplete data for some patients.
The study was supported by the National Institute for Health Research Health Technology Assessment Programme. The researchers had no financial conflicts to disclose.
The study population included infants born between 23 weeks 0 days’ and 28 weeks 6 days’ gestation. The researchers randomized 326 extremely preterm infants with patent ductus arteriosus (PDA) at 72 hours or less after birth to ibuprofen at a loading dose of 10 mg/kg followed by two doses of 5 mg/kg at least 24 hours apart, and 327 to placebo.
The PDAs in the infants had a diameter of at least 1.5 mm with pulsatile flow.
Severe dysplasia outcome
The study’s primary outcome was a composite of death or moderate to severe bronchopulmonary dysplasia at 36 weeks’ postmenstrual age. Overall, a primary outcome occurred in 69.2% of infants who received ibuprofen and 63.5% of those who received a placebo.
Risk of death or bronchopulmonary dysplasia at 36 weeks’ postmenstrual age was not reduced by early ibuprofen vs. placebo for preterm infants, the researchers concluded. Moderate or severe bronchopulmonary dysplasia occurred in 64.2% of the infants in the ibuprofen group and 59.3% of the placebo group who survived to 36 weeks’ postmenstrual age.
‘Unforeseeable’ serious adverse events
Forty-four deaths occurred in the ibuprofen group and 33 in the placebo group (adjusted risk ratio 1.09). Two “unforeseeable” serious adverse events occurred during the study that were potentially related to ibuprofen.
The lead author was Samir Gupta, MD, of Sidra Medicine, Doha, Qatar. The study was published online in the New England Journal of Medicine.
Study limitations include incomplete data for some patients.
The study was supported by the National Institute for Health Research Health Technology Assessment Programme. The researchers had no financial conflicts to disclose.


