User login
BRCA2 mutations linked to childhood NHL
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
Pediatric non-Hodgkin lymphomas should be added to the list of cancers associated with BRCA2 mutations, and survivors of childhood NHL should be considered for genetic counseling, investigators suggest.
Among 1,380 survivors of childhood lymphomas, those who were retrospectively found to be carriers of BRCA2 mutations had a fivefold higher risk for non-Hodgkin lymphoma than controls without cancer, reported Zhaoming Wang, PhD, and colleagues from St. Jude Children’s Research Hospital in Memphis.
“Genetic counseling and the option of BRCA2 genetic testing should be offered to survivors of pediatric or adolescent non–Hodgkin lymphoma, particularly those with a family history of BRCA2-associated cancers,” they wrote in JAMA Oncology.
The investigators had previously reported that BRCA2 was the third-most frequently mutated gene among 3006 survivors of childhood cancers, with the highest number of mutations seen in lymphoma survivors. In that study, 7 of 586 survivors of Hodgkin and non-Hodgkin lymphoma (1.2%) were found to carry BRCA2 mutations.
In the current study, the investigators performed germline whole-genome sequencing on samples from 815 survivors of childhood Hodgkin lymphoma and 748 survivors of non-Hodgkin lymphoma from the St. Jude Lifetime Cohort and Childhood Cancer Survivor studies and compared the data with those of controls without cancer from the Genome Aggregation Database.
They identified mutations in five Hodgkin lymphoma survivors (0.6%) and eight non-Hodgkin lymphoma survivors.
A comparison of cancer risk among lymphoma survivors and controls found that non-Hodgkin lymphoma survivors and BRCA2 carriers had an odds ratio for cancer of 5.0, compared with controls who were not BRCA2 carriers (P less than .001). Among Hodgkin lymphoma survivors the OR for carriers vs. controls was 2.1, but was not statistically significant.
Available family histories for seven of the eight non-Hodgkin lymphoma BRCA2 mutation carriers showed histories of BRCA2-linked cancers, including breast, prostate, and pancreas tumors and malignant melanoma.
“Survivors whose test results are positive for mutation should be offered surveillance for BRCA2-associated cancers, such as breast and ovarian, and counseled about cancer risk–reducing strategies. Currently, it remains unclear whether surveillance for non–Hodgkin lymphoma is associated with early detection of lymphomas or with other medical advantages,” the investigators wrote.
“This study was funded by a grant to St Jude Children’s Research Hospital from the American Lebanese Syrian Associated Charities and by grants to St Jude Children’s Research Hospital from the National Institutes of Health. The authors reported having no conflicts of interest.
SOURCE: Wang Z et al. JAMA Oncology. 2019 Jul 25. doi: 10.1001/jamaoncol.2019.2203.
FROM JAMA ONCOLOGY
Hurricanes delay RT, worsening survival of NSCLC
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
FROM JAMA
Potential improvements in convenience, tolerability of hematologic treatment
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two recent presentations regarding potential improvements in the convenience and tolerability of treatment for two hematologic malignancies: multiple myeloma and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
SC-Dara in myeloma
At the 2019 annual meeting of the American Society of Clinical Oncology, Maria-Victoria Mateos, MD, PhD, and colleagues, reported the results of COLUMBA, a phase 3 evaluation in 522 patients with multiple myeloma who were randomized to subcutaneous daratumumab (SC-Dara) or standard intravenous infusions of daratumumab (IV-Dara). A previous phase 1b study (Blood. 2017;130:838) had suggested comparable efficacy from the more convenient SC regime. Whereas conventional infusions of IV-Dara (16 mg/kg) take several hours, the SC formulation (1,800 mg–flat dose) is delivered in minutes. In COLUMBA, patients were randomized between SC- and IV-Dara weekly (cycles 1-2), then every 2 weeks (cycles 3-6), then every 4 weeks until disease progression.
Among the IV-Dara patients, the median duration of the first infusion was 421 minutes in cycle 1, 255 minutes in cycle 2, and 205 minutes in subsequent cycles – compatible with standard practice in the United States. As reported, at a median follow-up of 7.46 months, the efficacy (overall response rate, complete response rate, stringent-complete response rate, very good-partial response rate, progression-free survival, and 6-month overall survival) and safety profile were non-inferior for SC-Dara. SC-Dara patients also reported higher satisfaction with therapy.
What this means in practice
It is always a good idea to await publication of the manuscript because there may be study details and statistical nuances that make SC-Dara appear better than it will prove to be. For example, patient characteristics were slightly different between the two arms. Peer review of the final manuscript could be important in placing these results in context.
However, for treatments that demand frequent office visits over many months, reducing treatment burden for patients has value. Based on COLUMBA, it appears likely that SC-Dara will be a major convenience for patients, without obvious drawbacks in efficacy or toxicity. Meanwhile, flat dosing will be a time-saver for physicians, nursing, and pharmacy staff. If the price of the SC formulation is not exorbitant, I would expect a “win-win” that will support converting from IV- to SC-Dara as standard practice.
Acalabrutinib in CLL/SLL
Preclinical studies have shown acalabrutinib (Acala) to be more selective for Bruton’s tyrosine kinase (BTK) than the first-in-class agent ibrutinib, with less off-target kinase inhibition. As reported at the 2019 annual congress of the European Hematology Association by Paolo Ghia, MD, PhD, and colleagues in the phase 3 ASCEND trial, 310 patients with previously treated CLL were randomized between oral Acala twice daily and treatment of physician’s choice (TPC) – either idelalisib plus rituximab (maximum of seven infusions) or bendamustine plus rituximab (maximum of six cycles).
Progression-free survival was the primary endpoint. At a median of 16.1 months, progression-free survival had not been reached for Acala, in comparison with 16.5 months for TPC. Significant benefit of Acala was observed in all prognostic subsets.
Although there was no difference in overall survival at a median follow-up of about 16 months, 85% of Acala patients had a response lasting at least 12 months, compared with 60% of TPC patients. Adverse events of any grade occurred in 94% of patients treated with Acala, with 45% being grade 3-4 toxicities and six treatment-related deaths.
What this means in practice
The vast majority of CLL/SLL patients will relapse after primary therapy and will require further treatment, so the progression-free survival improvement associated with Acala in ASCEND is eye-catching. However, there are important considerations that demand closer scrutiny.
With oral agents administered until progression or unacceptable toxicity, low-grade toxicities can influence patient adherence, quality of life, and potentially the need for dose reduction or treatment interruptions. Regimens of finite duration and easy adherence monitoring may be, on balance, preferred by patients and providers – especially if the oral agent can be given in later-line with comparable overall survival.
With ibrutinib (Blood. 2017;129:2612-5), Paul M. Barr, MD, and colleagues demonstrated that higher dose intensity was associated with improved progression-free survival and that holds were associated with worsened progression-free survival. Acala’s promise of high efficacy and lower off-target toxicity will be solidified if the large (more than 500 patients) phase 3 ACE-CL-006 study (Acala vs. ibrutinib) demonstrates its relative benefit from efficacy, toxicity, and adherence perspectives, in comparison with a standard therapy that similarly demands adherence until disease progression or unacceptable toxicity.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
Gaps in patient-provider survivorship communication persist
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Comorbidities drive excess mortality after breast cancer diagnosis in childhood cancer survivors
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Risk of atrial fibrillation 900% higher with cancer
MELBOURNE – The overall prevalence of atrial fibrillation in people who have or have had cancer is 10 times that of individuals without cancer, according to a study presented at the International Society on Thrombosis and Haemostasis congress.
Cihan Ay, MD, of the division of hematology and hemostaseology at the Medical University of Vienna reported on a nationwide cohort study using health insurance data from more than 8.3 million people in Austria, including roughly 159,000 with a diagnosis of cancer and 113,000 with a diagnosis of atrial fibrillation.
The analysis found that, in individuals whose records showed a diagnosis of cancer, there was a 950% higher relative risk of also having a diagnosis of atrial fibrillation, compared with those with no cancer diagnosis.
The overall prevalence of atrial fibrillation among individuals with a cancer diagnosis was 9.8%, compared with 1.2% in those without cancer.
There was significant variation in relative risk according to age. Although the prevalence of atrial fibrillation increased with age, the highest relative risks were seen in the youngest age groups.
In those aged 12 years or under with a cancer diagnosis, the relative risk of atrial fibrillation was 150 times greater than in those without cancer, and in those aged 13-18 years, it was 200 times higher. At the other end of the age spectrum, individuals aged 70-79 years with a recorded cancer diagnosis, the relative risk of atrial fibrillation was still 130% higher than the noncancer population, and in those aged 80-90 years it was a significant 54% higher.
However, the analysis did not find any effect of gender on the risk of atrial fibrillation associated with cancer, regardless of the age group.
Researchers also examined the influence of different cancer types. They found the highest relative risk of atrial fibrillation was in persons with hematologic malignancies – at nine times the risk in the noncancer population – and the lowest was in the endocrine cancer patients, who had three times the risk.
Dr. Ay told the conference that the association between cancer and atrial fibrillation had been suggested in the literature, but it was still an unexplored field. “The exact magnitude of this association between cancer and atrial fibrillation is still unclear.”
There was also the question of what mechanisms might underlie the association. Dr. Ay pointed out that the health insurance database did not allow researchers to explore the temporal relationship between the two diagnoses, and therefore could not tell which came first.
One audience member queried whether the fact that cancer patients were likely to be visiting a clinician more frequently might mean that the atrial fibrillation would be more likely to be diagnosed.
To that, Dr. Ay suggested the significantly higher relative risk in children was supportive of the notion that cancer itself, or treatment effects, were influencing atrial fibrillation risk.
“There is evidence suggesting that cancer treatments are triggering atrial fibrillation,” he said in an interview. “Also, patients with cancer have situations of in which they are sick – they have neutropenia or sepsis and so on – which can also trigger atrial fibrillation.”
Given the limitations of the retrospective cohort study, Dr. Ay said he was hoping to do a prospective study that would enable baseline measurements of cancer patients to determine how much of the atrial fibrillation was preexisting.
“We have also more and more cancer survivors, and over the years they’re living longer and the likelihood of getting atrial fibrillation increases,” he added.
Commenting on the data, Gerald Soff, MD, chief of hematology at the Memorial Sloan Kettering Cancer Center in New York, said it was very important to quantify the association between cancer and atrial fibrillation.
“What’s striking to me is how many people with cancer come in with preexisting atrial fibrillation,” he said. “It could be that they have cancer and they’re already messed up, but we have, on a given day, several people coming in with newly diagnosed cancers, already on warfarin or apixaban or rivaroxaban because they have atrial fibrillation.”
Dr. Ay reported advisory board positions and speaking engagements for the pharmaceutical sector.
MELBOURNE – The overall prevalence of atrial fibrillation in people who have or have had cancer is 10 times that of individuals without cancer, according to a study presented at the International Society on Thrombosis and Haemostasis congress.
Cihan Ay, MD, of the division of hematology and hemostaseology at the Medical University of Vienna reported on a nationwide cohort study using health insurance data from more than 8.3 million people in Austria, including roughly 159,000 with a diagnosis of cancer and 113,000 with a diagnosis of atrial fibrillation.
The analysis found that, in individuals whose records showed a diagnosis of cancer, there was a 950% higher relative risk of also having a diagnosis of atrial fibrillation, compared with those with no cancer diagnosis.
The overall prevalence of atrial fibrillation among individuals with a cancer diagnosis was 9.8%, compared with 1.2% in those without cancer.
There was significant variation in relative risk according to age. Although the prevalence of atrial fibrillation increased with age, the highest relative risks were seen in the youngest age groups.
In those aged 12 years or under with a cancer diagnosis, the relative risk of atrial fibrillation was 150 times greater than in those without cancer, and in those aged 13-18 years, it was 200 times higher. At the other end of the age spectrum, individuals aged 70-79 years with a recorded cancer diagnosis, the relative risk of atrial fibrillation was still 130% higher than the noncancer population, and in those aged 80-90 years it was a significant 54% higher.
However, the analysis did not find any effect of gender on the risk of atrial fibrillation associated with cancer, regardless of the age group.
Researchers also examined the influence of different cancer types. They found the highest relative risk of atrial fibrillation was in persons with hematologic malignancies – at nine times the risk in the noncancer population – and the lowest was in the endocrine cancer patients, who had three times the risk.
Dr. Ay told the conference that the association between cancer and atrial fibrillation had been suggested in the literature, but it was still an unexplored field. “The exact magnitude of this association between cancer and atrial fibrillation is still unclear.”
There was also the question of what mechanisms might underlie the association. Dr. Ay pointed out that the health insurance database did not allow researchers to explore the temporal relationship between the two diagnoses, and therefore could not tell which came first.
One audience member queried whether the fact that cancer patients were likely to be visiting a clinician more frequently might mean that the atrial fibrillation would be more likely to be diagnosed.
To that, Dr. Ay suggested the significantly higher relative risk in children was supportive of the notion that cancer itself, or treatment effects, were influencing atrial fibrillation risk.
“There is evidence suggesting that cancer treatments are triggering atrial fibrillation,” he said in an interview. “Also, patients with cancer have situations of in which they are sick – they have neutropenia or sepsis and so on – which can also trigger atrial fibrillation.”
Given the limitations of the retrospective cohort study, Dr. Ay said he was hoping to do a prospective study that would enable baseline measurements of cancer patients to determine how much of the atrial fibrillation was preexisting.
“We have also more and more cancer survivors, and over the years they’re living longer and the likelihood of getting atrial fibrillation increases,” he added.
Commenting on the data, Gerald Soff, MD, chief of hematology at the Memorial Sloan Kettering Cancer Center in New York, said it was very important to quantify the association between cancer and atrial fibrillation.
“What’s striking to me is how many people with cancer come in with preexisting atrial fibrillation,” he said. “It could be that they have cancer and they’re already messed up, but we have, on a given day, several people coming in with newly diagnosed cancers, already on warfarin or apixaban or rivaroxaban because they have atrial fibrillation.”
Dr. Ay reported advisory board positions and speaking engagements for the pharmaceutical sector.
MELBOURNE – The overall prevalence of atrial fibrillation in people who have or have had cancer is 10 times that of individuals without cancer, according to a study presented at the International Society on Thrombosis and Haemostasis congress.
Cihan Ay, MD, of the division of hematology and hemostaseology at the Medical University of Vienna reported on a nationwide cohort study using health insurance data from more than 8.3 million people in Austria, including roughly 159,000 with a diagnosis of cancer and 113,000 with a diagnosis of atrial fibrillation.
The analysis found that, in individuals whose records showed a diagnosis of cancer, there was a 950% higher relative risk of also having a diagnosis of atrial fibrillation, compared with those with no cancer diagnosis.
The overall prevalence of atrial fibrillation among individuals with a cancer diagnosis was 9.8%, compared with 1.2% in those without cancer.
There was significant variation in relative risk according to age. Although the prevalence of atrial fibrillation increased with age, the highest relative risks were seen in the youngest age groups.
In those aged 12 years or under with a cancer diagnosis, the relative risk of atrial fibrillation was 150 times greater than in those without cancer, and in those aged 13-18 years, it was 200 times higher. At the other end of the age spectrum, individuals aged 70-79 years with a recorded cancer diagnosis, the relative risk of atrial fibrillation was still 130% higher than the noncancer population, and in those aged 80-90 years it was a significant 54% higher.
However, the analysis did not find any effect of gender on the risk of atrial fibrillation associated with cancer, regardless of the age group.
Researchers also examined the influence of different cancer types. They found the highest relative risk of atrial fibrillation was in persons with hematologic malignancies – at nine times the risk in the noncancer population – and the lowest was in the endocrine cancer patients, who had three times the risk.
Dr. Ay told the conference that the association between cancer and atrial fibrillation had been suggested in the literature, but it was still an unexplored field. “The exact magnitude of this association between cancer and atrial fibrillation is still unclear.”
There was also the question of what mechanisms might underlie the association. Dr. Ay pointed out that the health insurance database did not allow researchers to explore the temporal relationship between the two diagnoses, and therefore could not tell which came first.
One audience member queried whether the fact that cancer patients were likely to be visiting a clinician more frequently might mean that the atrial fibrillation would be more likely to be diagnosed.
To that, Dr. Ay suggested the significantly higher relative risk in children was supportive of the notion that cancer itself, or treatment effects, were influencing atrial fibrillation risk.
“There is evidence suggesting that cancer treatments are triggering atrial fibrillation,” he said in an interview. “Also, patients with cancer have situations of in which they are sick – they have neutropenia or sepsis and so on – which can also trigger atrial fibrillation.”
Given the limitations of the retrospective cohort study, Dr. Ay said he was hoping to do a prospective study that would enable baseline measurements of cancer patients to determine how much of the atrial fibrillation was preexisting.
“We have also more and more cancer survivors, and over the years they’re living longer and the likelihood of getting atrial fibrillation increases,” he added.
Commenting on the data, Gerald Soff, MD, chief of hematology at the Memorial Sloan Kettering Cancer Center in New York, said it was very important to quantify the association between cancer and atrial fibrillation.
“What’s striking to me is how many people with cancer come in with preexisting atrial fibrillation,” he said. “It could be that they have cancer and they’re already messed up, but we have, on a given day, several people coming in with newly diagnosed cancers, already on warfarin or apixaban or rivaroxaban because they have atrial fibrillation.”
Dr. Ay reported advisory board positions and speaking engagements for the pharmaceutical sector.
REPORTING FROM 2019 ISTH CONGRESS
Recombinant vaccine cut herpes zoster rate in immunocompromised patients
Two doses of recombinant zoster vaccine significantly reduced incidence of herpes zoster in adults who had undergone autologous hematopoietic stem cell transplantation (HSCT), results of a randomized, placebo-controlled trial indicate.
The incidence of herpes zoster was 30 per 1,000 person-years for patients who received the adjuvanted recombinant zoster vaccine (Shingrix) versus 94 per 1,000 person-years for those who received placebo, according to study results.
Recombinant zoster vaccine induced humoral and cellular responses that were strong and occurring at a rate higher than what was seen in the placebo group, said senior author Keith M. Sullivan, MD, of Duke University Medical Center, Durham, N.C., and coauthors, who reported findings on behalf of the Zoster Efficacy Study in Patients Undergoing HSCT (ZOE-HSCT) Study Group.
“The vaccinations were generally well tolerated, and most symptoms were mild and transient and did not substantially deter participants from receiving their second dose,” Dr. Sullivan and colleagues wrote in JAMA.
The risk of herpes zoster is increased for 2-3 years after autologous HSCT because of diminished T-cell immunity, according to the authors.
“Antiviral prophylaxis is commonly administered to patients after HSCT to prevent such complications, but the efficacy depends on adherence to treatment,” they said.
While vaccines could provide long-term protection, immunocompromised individuals receiving live attenuated vaccine would be at increased risk of varicella caused by spread of the vaccine strain, they added.
There have been a few encouraging recent studies of non-live vaccines in this setting, including one large phase 3 trial of a heat-inactivated varicella-zoster virus vaccine that showed patients undergoing autologous HSCT had a 63.8% estimated efficacy in preventing herpes zoster, investigators from that study said in The Lancet (2018 May 26;391[10135]:2116-27).
A phase 1/2a study of the adjuvanted recombinant zoster vaccine in patients undergoing HSCT demonstrated strong humoral and cell-mediated immunity responses, which provided the rationale for studying the vaccine further in the randomized ZOE-HSCT study, according to Dr. Sullivan and coauthors.
Their study included a total of 1,846 adults who had undergone autologous HSCT. They were randomized to receive two doses of the recombinant zoster vaccine, the first at 50-70 days after the procedure and the second 1-2 months later.
Herpes zoster cases were seen in 49 and 136 individuals in the vaccine and placebo groups, respectively, which resulted in overall incidences of 30 and 94 per 1,000 person-years.
The incidence rate ratio of a first episode of herpes zoster was 0.36 for individuals receiving at least one dose, which authors said was equivalent to a vaccine efficacy of 63.7%.
That efficacy rate is “very similar” to the estimated efficacy reported for the heat-inactivated varicella-zoster virus vaccine reported in The Lancet, said Dr. Sullivan and coauthors.
However, the heat-inactivated vaccine achieved that level of protection with a four-dose schedule, including one dose given prior to autologous HSCT.
“An advantage of the short 2-dose posttransplantation schedule is that more patients might complete the vaccination program,” they said in a discussion of the results, noting that 94.7% of the recombinant zoster vaccine recipients completed two doses, compared with 81.9% of recipients who received the heat-inactivated herpes zoster vaccine in the previous report.
The study was funded and sponsored by GlaxoSmithKline Biologicals SA. Dr. Sullivan reported disclosures related to GlaxoSmithKline (GSK), Kiadis Pharmaceutical, Roche Genentech, and the National Institute of Allergy and Infectious Diseases. Coauthors provided disclosures related to GSK, AbbVie, Roche, Gilead, Janssen, Pharmacyclics, Morphosys, Helsinn, Celgene, and others.
SOURCE: Bastidas A et al. JAMA. 2019 July 9. doi: 10.1001/jama.2019.9053.
Two doses of recombinant zoster vaccine significantly reduced incidence of herpes zoster in adults who had undergone autologous hematopoietic stem cell transplantation (HSCT), results of a randomized, placebo-controlled trial indicate.
The incidence of herpes zoster was 30 per 1,000 person-years for patients who received the adjuvanted recombinant zoster vaccine (Shingrix) versus 94 per 1,000 person-years for those who received placebo, according to study results.
Recombinant zoster vaccine induced humoral and cellular responses that were strong and occurring at a rate higher than what was seen in the placebo group, said senior author Keith M. Sullivan, MD, of Duke University Medical Center, Durham, N.C., and coauthors, who reported findings on behalf of the Zoster Efficacy Study in Patients Undergoing HSCT (ZOE-HSCT) Study Group.
“The vaccinations were generally well tolerated, and most symptoms were mild and transient and did not substantially deter participants from receiving their second dose,” Dr. Sullivan and colleagues wrote in JAMA.
The risk of herpes zoster is increased for 2-3 years after autologous HSCT because of diminished T-cell immunity, according to the authors.
“Antiviral prophylaxis is commonly administered to patients after HSCT to prevent such complications, but the efficacy depends on adherence to treatment,” they said.
While vaccines could provide long-term protection, immunocompromised individuals receiving live attenuated vaccine would be at increased risk of varicella caused by spread of the vaccine strain, they added.
There have been a few encouraging recent studies of non-live vaccines in this setting, including one large phase 3 trial of a heat-inactivated varicella-zoster virus vaccine that showed patients undergoing autologous HSCT had a 63.8% estimated efficacy in preventing herpes zoster, investigators from that study said in The Lancet (2018 May 26;391[10135]:2116-27).
A phase 1/2a study of the adjuvanted recombinant zoster vaccine in patients undergoing HSCT demonstrated strong humoral and cell-mediated immunity responses, which provided the rationale for studying the vaccine further in the randomized ZOE-HSCT study, according to Dr. Sullivan and coauthors.
Their study included a total of 1,846 adults who had undergone autologous HSCT. They were randomized to receive two doses of the recombinant zoster vaccine, the first at 50-70 days after the procedure and the second 1-2 months later.
Herpes zoster cases were seen in 49 and 136 individuals in the vaccine and placebo groups, respectively, which resulted in overall incidences of 30 and 94 per 1,000 person-years.
The incidence rate ratio of a first episode of herpes zoster was 0.36 for individuals receiving at least one dose, which authors said was equivalent to a vaccine efficacy of 63.7%.
That efficacy rate is “very similar” to the estimated efficacy reported for the heat-inactivated varicella-zoster virus vaccine reported in The Lancet, said Dr. Sullivan and coauthors.
However, the heat-inactivated vaccine achieved that level of protection with a four-dose schedule, including one dose given prior to autologous HSCT.
“An advantage of the short 2-dose posttransplantation schedule is that more patients might complete the vaccination program,” they said in a discussion of the results, noting that 94.7% of the recombinant zoster vaccine recipients completed two doses, compared with 81.9% of recipients who received the heat-inactivated herpes zoster vaccine in the previous report.
The study was funded and sponsored by GlaxoSmithKline Biologicals SA. Dr. Sullivan reported disclosures related to GlaxoSmithKline (GSK), Kiadis Pharmaceutical, Roche Genentech, and the National Institute of Allergy and Infectious Diseases. Coauthors provided disclosures related to GSK, AbbVie, Roche, Gilead, Janssen, Pharmacyclics, Morphosys, Helsinn, Celgene, and others.
SOURCE: Bastidas A et al. JAMA. 2019 July 9. doi: 10.1001/jama.2019.9053.
Two doses of recombinant zoster vaccine significantly reduced incidence of herpes zoster in adults who had undergone autologous hematopoietic stem cell transplantation (HSCT), results of a randomized, placebo-controlled trial indicate.
The incidence of herpes zoster was 30 per 1,000 person-years for patients who received the adjuvanted recombinant zoster vaccine (Shingrix) versus 94 per 1,000 person-years for those who received placebo, according to study results.
Recombinant zoster vaccine induced humoral and cellular responses that were strong and occurring at a rate higher than what was seen in the placebo group, said senior author Keith M. Sullivan, MD, of Duke University Medical Center, Durham, N.C., and coauthors, who reported findings on behalf of the Zoster Efficacy Study in Patients Undergoing HSCT (ZOE-HSCT) Study Group.
“The vaccinations were generally well tolerated, and most symptoms were mild and transient and did not substantially deter participants from receiving their second dose,” Dr. Sullivan and colleagues wrote in JAMA.
The risk of herpes zoster is increased for 2-3 years after autologous HSCT because of diminished T-cell immunity, according to the authors.
“Antiviral prophylaxis is commonly administered to patients after HSCT to prevent such complications, but the efficacy depends on adherence to treatment,” they said.
While vaccines could provide long-term protection, immunocompromised individuals receiving live attenuated vaccine would be at increased risk of varicella caused by spread of the vaccine strain, they added.
There have been a few encouraging recent studies of non-live vaccines in this setting, including one large phase 3 trial of a heat-inactivated varicella-zoster virus vaccine that showed patients undergoing autologous HSCT had a 63.8% estimated efficacy in preventing herpes zoster, investigators from that study said in The Lancet (2018 May 26;391[10135]:2116-27).
A phase 1/2a study of the adjuvanted recombinant zoster vaccine in patients undergoing HSCT demonstrated strong humoral and cell-mediated immunity responses, which provided the rationale for studying the vaccine further in the randomized ZOE-HSCT study, according to Dr. Sullivan and coauthors.
Their study included a total of 1,846 adults who had undergone autologous HSCT. They were randomized to receive two doses of the recombinant zoster vaccine, the first at 50-70 days after the procedure and the second 1-2 months later.
Herpes zoster cases were seen in 49 and 136 individuals in the vaccine and placebo groups, respectively, which resulted in overall incidences of 30 and 94 per 1,000 person-years.
The incidence rate ratio of a first episode of herpes zoster was 0.36 for individuals receiving at least one dose, which authors said was equivalent to a vaccine efficacy of 63.7%.
That efficacy rate is “very similar” to the estimated efficacy reported for the heat-inactivated varicella-zoster virus vaccine reported in The Lancet, said Dr. Sullivan and coauthors.
However, the heat-inactivated vaccine achieved that level of protection with a four-dose schedule, including one dose given prior to autologous HSCT.
“An advantage of the short 2-dose posttransplantation schedule is that more patients might complete the vaccination program,” they said in a discussion of the results, noting that 94.7% of the recombinant zoster vaccine recipients completed two doses, compared with 81.9% of recipients who received the heat-inactivated herpes zoster vaccine in the previous report.
The study was funded and sponsored by GlaxoSmithKline Biologicals SA. Dr. Sullivan reported disclosures related to GlaxoSmithKline (GSK), Kiadis Pharmaceutical, Roche Genentech, and the National Institute of Allergy and Infectious Diseases. Coauthors provided disclosures related to GSK, AbbVie, Roche, Gilead, Janssen, Pharmacyclics, Morphosys, Helsinn, Celgene, and others.
SOURCE: Bastidas A et al. JAMA. 2019 July 9. doi: 10.1001/jama.2019.9053.
FROM JAMA
Key clinical point: Two doses of recombinant zoster vaccine significantly reduced incidence of herpes zoster versus placebo in adults who had undergone autologous hematopoietic stem cell transplantation (HSCT).
Major finding: Herpes zoster cases were seen in 49 and 136 individuals in the vaccine and placebo groups, respectively, resulting in overall incidences of 30 and 94 per 1,000 person-years.
Study details: A randomized clinical trial (ZOE-HSCT) including 1,846 adults who had undergone autologous HSCT.
Disclosures: The study was funded and sponsored by GlaxoSmithKline Biologicals SA. Study authors reported disclosures related to GlaxoSmithKline, Kiadis Pharmaceutical, Roche Genentech, AbbVie, Roche, Gilead, Janssen, Pharmacyclics, Morphosys, Helsinn, Celgene, and others.
Source: Bastidas A et al. JAMA. 2019 July 9. doi: 10.1001/jama.2019.9053.
Influenza vaccination status in DLBCL poorly documented
Annual influenza vaccination rates and documentation of vaccination status appear to be suboptimal among patients with newly diagnosed diffuse large B-cell lymphoma, based on a retrospective analysis of data in the state of Georgia.
The researchers reviewed medical records of patients with a new diagnosis of diffuse large B-cell lymphoma at three Georgia hospitals. Documentation related to vaccine administration, refusal, and patient counseling was collected between Feb. 1, 2015, and Oct. 31, 2017, Andres Chang, MD, PhD, of Emory University, Atlanta, and colleagues wrote. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
Vaccination status within 1 year of diagnosis was documented for 61 of 107 patients. Among the 61 patients with documentation of influenza vaccination status, 35 (57%) were vaccinated. No reason was documented for vaccine refusal, and there was no follow-up documentation on vaccine counseling by nursing staff, physicians, or advanced practice providers in any of these admitted patients.
Nearly all documentation of influenza vaccination status came from the nursing staff. Only 4 of the 61 patients had documentation provided by primary oncologists or advanced practice providers, and those patients also had documentation from the outpatient nursing staff who subsequently administered the influenza vaccine.
“Routine outpatient vaccination screening and strategies for sharing and linking patient vaccination status between providers in different health care systems at the state and national levels could improve vaccination documentation in patients with lymphoma and provide opportunities to improve compliance,” the researchers wrote.
A key limitation of the study was the lack of adequate documentation, they explained. As a result, the reported vaccination rates were not more rigorously evaluated.
The study was funded by the Winship Cancer Institute and the National Institutes of Health. The authors reported financial affiliations with AbbVie, Acerta Pharma, Celgene, Gilead, Janssen, Pharmacyclics, and others.
SOURCE: Chang A et al. Clin Lymphoma Myeloma Leuk. 2019 Jan 2. doi: 10.1016/j.clml.2018.12.018.
Annual influenza vaccination rates and documentation of vaccination status appear to be suboptimal among patients with newly diagnosed diffuse large B-cell lymphoma, based on a retrospective analysis of data in the state of Georgia.
The researchers reviewed medical records of patients with a new diagnosis of diffuse large B-cell lymphoma at three Georgia hospitals. Documentation related to vaccine administration, refusal, and patient counseling was collected between Feb. 1, 2015, and Oct. 31, 2017, Andres Chang, MD, PhD, of Emory University, Atlanta, and colleagues wrote. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
Vaccination status within 1 year of diagnosis was documented for 61 of 107 patients. Among the 61 patients with documentation of influenza vaccination status, 35 (57%) were vaccinated. No reason was documented for vaccine refusal, and there was no follow-up documentation on vaccine counseling by nursing staff, physicians, or advanced practice providers in any of these admitted patients.
Nearly all documentation of influenza vaccination status came from the nursing staff. Only 4 of the 61 patients had documentation provided by primary oncologists or advanced practice providers, and those patients also had documentation from the outpatient nursing staff who subsequently administered the influenza vaccine.
“Routine outpatient vaccination screening and strategies for sharing and linking patient vaccination status between providers in different health care systems at the state and national levels could improve vaccination documentation in patients with lymphoma and provide opportunities to improve compliance,” the researchers wrote.
A key limitation of the study was the lack of adequate documentation, they explained. As a result, the reported vaccination rates were not more rigorously evaluated.
The study was funded by the Winship Cancer Institute and the National Institutes of Health. The authors reported financial affiliations with AbbVie, Acerta Pharma, Celgene, Gilead, Janssen, Pharmacyclics, and others.
SOURCE: Chang A et al. Clin Lymphoma Myeloma Leuk. 2019 Jan 2. doi: 10.1016/j.clml.2018.12.018.
Annual influenza vaccination rates and documentation of vaccination status appear to be suboptimal among patients with newly diagnosed diffuse large B-cell lymphoma, based on a retrospective analysis of data in the state of Georgia.
The researchers reviewed medical records of patients with a new diagnosis of diffuse large B-cell lymphoma at three Georgia hospitals. Documentation related to vaccine administration, refusal, and patient counseling was collected between Feb. 1, 2015, and Oct. 31, 2017, Andres Chang, MD, PhD, of Emory University, Atlanta, and colleagues wrote. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
Vaccination status within 1 year of diagnosis was documented for 61 of 107 patients. Among the 61 patients with documentation of influenza vaccination status, 35 (57%) were vaccinated. No reason was documented for vaccine refusal, and there was no follow-up documentation on vaccine counseling by nursing staff, physicians, or advanced practice providers in any of these admitted patients.
Nearly all documentation of influenza vaccination status came from the nursing staff. Only 4 of the 61 patients had documentation provided by primary oncologists or advanced practice providers, and those patients also had documentation from the outpatient nursing staff who subsequently administered the influenza vaccine.
“Routine outpatient vaccination screening and strategies for sharing and linking patient vaccination status between providers in different health care systems at the state and national levels could improve vaccination documentation in patients with lymphoma and provide opportunities to improve compliance,” the researchers wrote.
A key limitation of the study was the lack of adequate documentation, they explained. As a result, the reported vaccination rates were not more rigorously evaluated.
The study was funded by the Winship Cancer Institute and the National Institutes of Health. The authors reported financial affiliations with AbbVie, Acerta Pharma, Celgene, Gilead, Janssen, Pharmacyclics, and others.
SOURCE: Chang A et al. Clin Lymphoma Myeloma Leuk. 2019 Jan 2. doi: 10.1016/j.clml.2018.12.018.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Cancer deaths cost over $94 billion in lost earnings in 2015
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
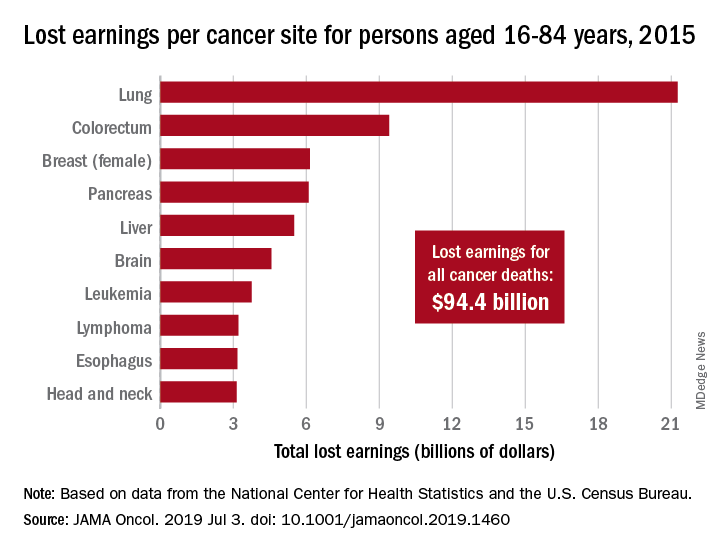
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
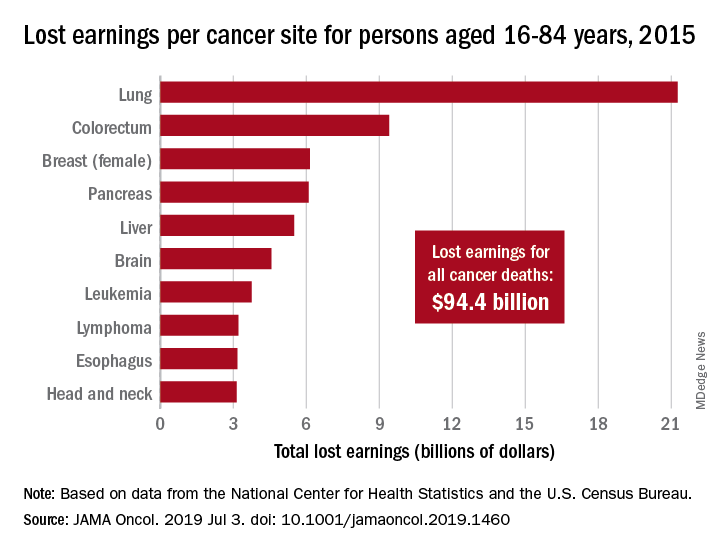
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
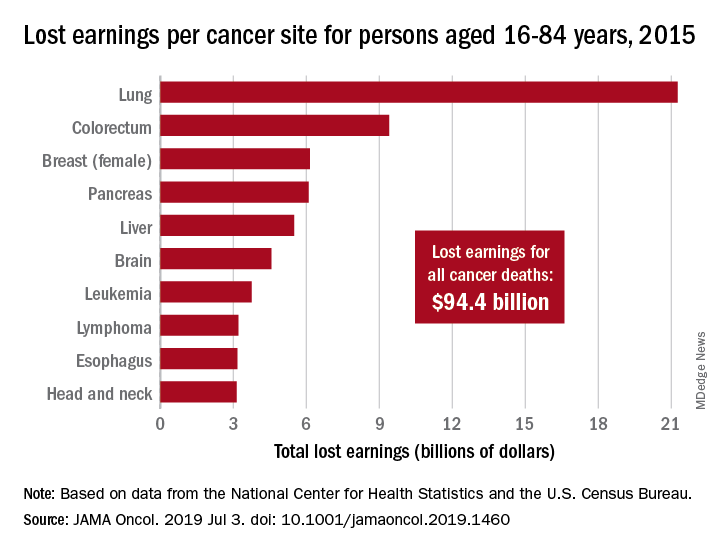
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
FROM JAMA ONCOLOGY
Whose needs come first – the patient’s or the trial’s?
Debra Banks (not her real name) had hope. There was a clinical trial open at an academic hospital 200 miles from where she lived. She would commute or find local housing. It would cost her, but this is what her savings were for, she reasoned. What expense could be more important than her life?
Next came the tests. Blood tests, an ultrasound of her heart, breathing tests. She gave vials of blood, lay in scanners, and eagerly jumped through every hoop placed before her. Then came the call from the trial coordinator. Her heart ultrasound showed a mild dysfunction in how it pumped. It excluded her from the trial.
“Not eligible.” The two words that took away everything reverberated in her mind. Her heart had never caused her any problems before. So after the shock wore off, she tried to bargain with the trial coordinator: Had the study drug been shown to cause or worsen heart damage? Could they repeat the ultrasound? Did this blip in her heart function really matter?
When the trial coordinator couldn’t answer all these questions, she encouraged Debra to come into the clinic and talk to the doctors directly. That’s where I met her.
Debra found herself in the middle of a painful crossroads she had no interest being in. What happens when the needs of an individual patient and the needs of medical research are at odds? From Debra’s perspective, she had one goal. She wanted the therapy that would give her the best chance of living.
But the aim of the trial was not to help Debra – not directly, at least. Clinical trials help patient populations. The goal is to add to a body of knowledge: To study new therapies, demonstrate safety and efficacy, and ultimately find better treatments. The bulk of benefit goes to future patients, not individual participants. If an individual participant does benefit, all the better. But this is a bonus, not a requirement.
In order to meet these goals, trials come with inclusion and exclusion criteria. These are often strict. Individuals with certain other medical conditions are frequently excluded, as the person needs to be able to tolerate the toxicities of the drug being tested.
This, of course, is very different from our usual approach to patient care. Outside of trials, the needs of the individual patient are our North Star. Instead of inclusion and exclusion criteria, we have guidelines: general goalposts that hint at the right answer, but are able to be bent based on individual circumstances. It’s something I love about medicine. Part science, part art. Part algorithmic, part creative.
I can give chemotherapy to a patient with a low platelet count, if I think it’s best. I can override an elevated bilirubin. I can simply not check a heart ultrasound in the first place, if I don’t believe it will change my management.
I understand why trial criteria exist. I fully support investing in novel therapies that will help future patients on a large scale. There will invariably be individuals for whom a clinical trial is unsafe or inappropriate for a multitude of reasons, and our job as oncologists is to make that call and convey that news.
Still, that can be hard to square with the human being sitting in front of you. Debra was only in her mid-50s. She was an artist, an educator, a parent. She was a person who was so, so not ready to die. That she would because of a glitch in her heart function – the significance of which nobody knew – was excruciating.
While we can’t enroll every patient in every trial, the least we can do is comb through trial criteria thoughtfully. With the role of clinical investigator comes great responsibility. Are we choosing a cutoff because it makes clinical sense – or because that’s how it was done before? Is there a medical justification behind each and every exclusion criterion? A careless cutoff is not just a line on a protocol. It can be the difference between someone’s last hope – and no more options.
Every time I saw Debra in clinic, she asked about the trial. Then one day she stopped asking. She was distracted by more pressing problems. Her breathing had worsened and her energy levels were so low she could hardly get out of bed. Debra became sicker and sicker until she could no longer request the last hope that might make her better.
A wonderful physician-scientist I worked with once said she split her time between patient care and medical research because they complement each other. Whenever she lost a patient, she turned that pain into motivation to delve deeper into her research. She coped with individual loss by helping to make small, incremental improvements for the needs of many.
I think about this, months later, as I look around the empty exam room where I first met Debra. I imagine a roomful of patients, alive and healthy, for whom the research she was excluded from has benefited.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
Debra Banks (not her real name) had hope. There was a clinical trial open at an academic hospital 200 miles from where she lived. She would commute or find local housing. It would cost her, but this is what her savings were for, she reasoned. What expense could be more important than her life?
Next came the tests. Blood tests, an ultrasound of her heart, breathing tests. She gave vials of blood, lay in scanners, and eagerly jumped through every hoop placed before her. Then came the call from the trial coordinator. Her heart ultrasound showed a mild dysfunction in how it pumped. It excluded her from the trial.
“Not eligible.” The two words that took away everything reverberated in her mind. Her heart had never caused her any problems before. So after the shock wore off, she tried to bargain with the trial coordinator: Had the study drug been shown to cause or worsen heart damage? Could they repeat the ultrasound? Did this blip in her heart function really matter?
When the trial coordinator couldn’t answer all these questions, she encouraged Debra to come into the clinic and talk to the doctors directly. That’s where I met her.
Debra found herself in the middle of a painful crossroads she had no interest being in. What happens when the needs of an individual patient and the needs of medical research are at odds? From Debra’s perspective, she had one goal. She wanted the therapy that would give her the best chance of living.
But the aim of the trial was not to help Debra – not directly, at least. Clinical trials help patient populations. The goal is to add to a body of knowledge: To study new therapies, demonstrate safety and efficacy, and ultimately find better treatments. The bulk of benefit goes to future patients, not individual participants. If an individual participant does benefit, all the better. But this is a bonus, not a requirement.
In order to meet these goals, trials come with inclusion and exclusion criteria. These are often strict. Individuals with certain other medical conditions are frequently excluded, as the person needs to be able to tolerate the toxicities of the drug being tested.
This, of course, is very different from our usual approach to patient care. Outside of trials, the needs of the individual patient are our North Star. Instead of inclusion and exclusion criteria, we have guidelines: general goalposts that hint at the right answer, but are able to be bent based on individual circumstances. It’s something I love about medicine. Part science, part art. Part algorithmic, part creative.
I can give chemotherapy to a patient with a low platelet count, if I think it’s best. I can override an elevated bilirubin. I can simply not check a heart ultrasound in the first place, if I don’t believe it will change my management.
I understand why trial criteria exist. I fully support investing in novel therapies that will help future patients on a large scale. There will invariably be individuals for whom a clinical trial is unsafe or inappropriate for a multitude of reasons, and our job as oncologists is to make that call and convey that news.
Still, that can be hard to square with the human being sitting in front of you. Debra was only in her mid-50s. She was an artist, an educator, a parent. She was a person who was so, so not ready to die. That she would because of a glitch in her heart function – the significance of which nobody knew – was excruciating.
While we can’t enroll every patient in every trial, the least we can do is comb through trial criteria thoughtfully. With the role of clinical investigator comes great responsibility. Are we choosing a cutoff because it makes clinical sense – or because that’s how it was done before? Is there a medical justification behind each and every exclusion criterion? A careless cutoff is not just a line on a protocol. It can be the difference between someone’s last hope – and no more options.
Every time I saw Debra in clinic, she asked about the trial. Then one day she stopped asking. She was distracted by more pressing problems. Her breathing had worsened and her energy levels were so low she could hardly get out of bed. Debra became sicker and sicker until she could no longer request the last hope that might make her better.
A wonderful physician-scientist I worked with once said she split her time between patient care and medical research because they complement each other. Whenever she lost a patient, she turned that pain into motivation to delve deeper into her research. She coped with individual loss by helping to make small, incremental improvements for the needs of many.
I think about this, months later, as I look around the empty exam room where I first met Debra. I imagine a roomful of patients, alive and healthy, for whom the research she was excluded from has benefited.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
Debra Banks (not her real name) had hope. There was a clinical trial open at an academic hospital 200 miles from where she lived. She would commute or find local housing. It would cost her, but this is what her savings were for, she reasoned. What expense could be more important than her life?
Next came the tests. Blood tests, an ultrasound of her heart, breathing tests. She gave vials of blood, lay in scanners, and eagerly jumped through every hoop placed before her. Then came the call from the trial coordinator. Her heart ultrasound showed a mild dysfunction in how it pumped. It excluded her from the trial.
“Not eligible.” The two words that took away everything reverberated in her mind. Her heart had never caused her any problems before. So after the shock wore off, she tried to bargain with the trial coordinator: Had the study drug been shown to cause or worsen heart damage? Could they repeat the ultrasound? Did this blip in her heart function really matter?
When the trial coordinator couldn’t answer all these questions, she encouraged Debra to come into the clinic and talk to the doctors directly. That’s where I met her.
Debra found herself in the middle of a painful crossroads she had no interest being in. What happens when the needs of an individual patient and the needs of medical research are at odds? From Debra’s perspective, she had one goal. She wanted the therapy that would give her the best chance of living.
But the aim of the trial was not to help Debra – not directly, at least. Clinical trials help patient populations. The goal is to add to a body of knowledge: To study new therapies, demonstrate safety and efficacy, and ultimately find better treatments. The bulk of benefit goes to future patients, not individual participants. If an individual participant does benefit, all the better. But this is a bonus, not a requirement.
In order to meet these goals, trials come with inclusion and exclusion criteria. These are often strict. Individuals with certain other medical conditions are frequently excluded, as the person needs to be able to tolerate the toxicities of the drug being tested.
This, of course, is very different from our usual approach to patient care. Outside of trials, the needs of the individual patient are our North Star. Instead of inclusion and exclusion criteria, we have guidelines: general goalposts that hint at the right answer, but are able to be bent based on individual circumstances. It’s something I love about medicine. Part science, part art. Part algorithmic, part creative.
I can give chemotherapy to a patient with a low platelet count, if I think it’s best. I can override an elevated bilirubin. I can simply not check a heart ultrasound in the first place, if I don’t believe it will change my management.
I understand why trial criteria exist. I fully support investing in novel therapies that will help future patients on a large scale. There will invariably be individuals for whom a clinical trial is unsafe or inappropriate for a multitude of reasons, and our job as oncologists is to make that call and convey that news.
Still, that can be hard to square with the human being sitting in front of you. Debra was only in her mid-50s. She was an artist, an educator, a parent. She was a person who was so, so not ready to die. That she would because of a glitch in her heart function – the significance of which nobody knew – was excruciating.
While we can’t enroll every patient in every trial, the least we can do is comb through trial criteria thoughtfully. With the role of clinical investigator comes great responsibility. Are we choosing a cutoff because it makes clinical sense – or because that’s how it was done before? Is there a medical justification behind each and every exclusion criterion? A careless cutoff is not just a line on a protocol. It can be the difference between someone’s last hope – and no more options.
Every time I saw Debra in clinic, she asked about the trial. Then one day she stopped asking. She was distracted by more pressing problems. Her breathing had worsened and her energy levels were so low she could hardly get out of bed. Debra became sicker and sicker until she could no longer request the last hope that might make her better.
A wonderful physician-scientist I worked with once said she split her time between patient care and medical research because they complement each other. Whenever she lost a patient, she turned that pain into motivation to delve deeper into her research. She coped with individual loss by helping to make small, incremental improvements for the needs of many.
I think about this, months later, as I look around the empty exam room where I first met Debra. I imagine a roomful of patients, alive and healthy, for whom the research she was excluded from has benefited.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.






