User login
ASCO VTE guideline update: DOACs now an option for prevention, treatment
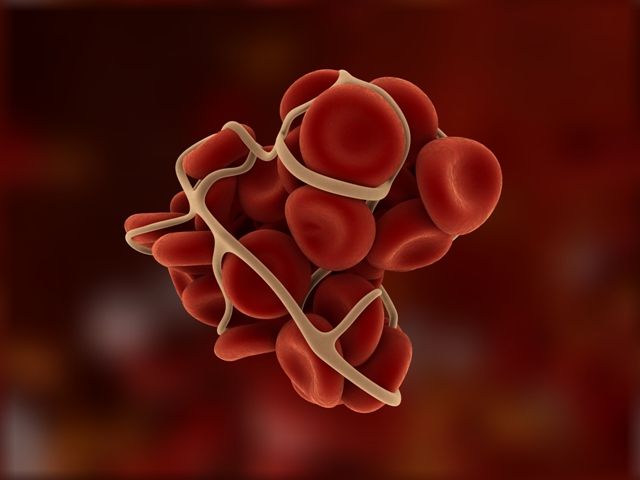
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
Low benefits spur alternative drug cost proposals
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
It’s no secret that cancer drugs are among the most expensive medical treatments in the United States, and now, new research reveals some high-priced cancer drugs may yield little benefit for patients.
A recent analysis of 71 oncology indications approved by the Food and Drug Administration between 2011 and 2017 found that overall survival gains were marginal for drugs approved by the FDA based on overall survival (OS) data. The majority of the 71 indications (75%) demonstrated no statistically significant improvement in patient-reported outcomes (PROs), according to the study (JAMA Oncol. 2019 Jul 3 doi: 10.1001/jamaoncol.2019.1760).
More than half of the indications evaluated demonstrated neither an OS benefit nor a PRO improvement post approval, the study found.
While the researchers did not analyze cost, a number of the cancer drugs that demonstrated little benefit come with a high price tag. Cabozantinib (Cabometyx) for example, approved for the treatment of medullary thyroid carcinoma and advanced renal cell carcinoma (RCC) during the study period, did not demonstrate an overall survival benefit post approval, findings showed. Cabometyx, approved based on survival data, had a 2016 wholesale acquisition cost of $13,750 for a 1-month supply. Olaparib (Lynparza) meanwhile, approved for the treatment of advanced ovarian cancer during the study period, also showed no overall survival benefit post approval. The 2017 wholesale acquisition cost for olaparib was $13,482 for a 30-day supply.
Investigators noted in the study that evaluation of OS can be challenging or unfeasible in some instances and is complicated by factors such as use of crossover trial design.
The findings emphasize the need for a sharper eye on how regulatory authorities approve drugs, said Chadi Nabhan, MD, senior author of the study and chief medical officer at Aptitude Health based in Chicago.
“We all want our patients to receive the best and the latest and the most important and innovative drug they can possible get, as long as these drugs show a benefit,” said Dr. Nabhan, a hematologist and medical oncologist. “We need to look critically at making sure drugs getting approved are truly helping patients by extending their lives or improving their quality of life.”
Growing questions about the benefits of some cancer drugs come as a push to reconsider the pricing of medications to better account for value gains momentum. A number of proposals have recently emerged that would revamp the current payment structure for prescription drugs with the aim of lowering costs and improving access. Value-based pricing proposals are not without challenges, namely defining what value truly means, said Leonard Saltz, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York.
“We’re all quite clear there is a huge absence of connection between cost and value,” Dr. Saltz said in an interview. “There is also a real absence of the definition of, ‘What is value?’ I think that ultimately we have to rely on defining value by its absence. By that I mean, where do we say, this is insufficient value?”
Many drugs show little benefit
The JAMA Oncology study builds on other data that raise doubts about how the FDA determines value when making approval decisions for cancer drugs.
Overall survival is the most direct measure of clinical benefit used to determine value. But OS as an endpoint in clinical trials generally requires larger patient numbers and increased time for follow-up, thereby delaying approvals. This is likely why the use of surrogate endpoints to approve drugs has increased. Dr. Nabhan’s study found the use of surrogate endpoints during trials grew from 67% during the period of 2008 through 2012 to 76% during the period of 2011 through 2017. Surrogate endpoints can include tumor shrinkage, time to progression, or time to reappearance of disease.
The use of surrogate endpoints to determine value however, has long come under scrutiny. A 2019 analysis published in JAMA Internal Medicine found that most cancer drugs approved by the FDA based on response rate (RR) – the percentage of patients who experience tumor shrinkage – have less than transformational response rates, and that such indications do not have confirmed clinical benefit.
Of 59 oncology drugs with 85 unique indications, most had a response rate ranging from 20% to 59%. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.) Investigators also reported that many of the drugs have remained on the market for years without subsequent confirmatory data.
In addition, a 2018 review of randomized clinical trials published in JAMA Internal Medicine that analyzed progression-free survival in cancer patients found the endpoint did not improve patients’ lives. A quantitative analysis of 52 articles that covered 38 randomized clinical trials involving 13,979 patients across 12 cancer types found no significant association between progression-free survival and health-related quality of life.
“These findings raise questions regarding the assumption that interventions prolonging [progression-free survival] also improve [health-related quality of life] in patients with cancer,” the study authors wrote. “Therefore, to ensure that patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure [health-related quality of life] directly and accurately, ensuring adequate duration and follow-up.
PROs, which can encompass health-related quality of life, is a measure the FDA has encouraged investigators to use during trials – when the benefit exists. In the analysis by Dr. Nabhan, trials evaluated PROs during pivotal studies supporting initial approval in 50 of the 71 indications. Before approval, 14 drugs demonstrated a statistically significant improvement in at least one PRO, but only 1 of the 14 – ruxolitinib – was granted a PRO labeling claim at the time of approval. Post approval, a statistically significant improvement in PROs was shown for only 18 of the 71 (25%) initial indications.
Meanwhile, although overall survival is considered the optimal yardstick with which to measure drug benefit, the value of longevity – and how it should be weighted – poses further questions. A number of new oncology drugs approved based on survival data lengthen lives by a very short time, Dr. Saltz noted. In the study of 71 indications for example, the median OS gain for drugs approved based on survival data was 1.7 months.
“We crossed the absurdity boundary a long time ago with drugs in the range of $10,000 to $20,000 a month with median survival benefits of less than 2 months,” Dr. Saltz said. “That’s not very much. Then we get into a rather circuitous argument that doesn’t settle anything as to whether it’s ‘worth it or not.’ The question becomes to whom is it worth what, and who’s paying for it?”
Proposals aim to lower cost
Recent cost ideas that center on value-pricing seek to answer some of those questions. Outcomes-based contracts is one such proposal. Under the approach, a drug manufacturer and a payer reach an agreement that ties reimbursement to observed outcomes in patients. Rather than a payer covering all prescriptions at a single price, the initial price remains in place if a certain volume of patients achieves the agreed-upon outcome. If the threshold is not met, the drugmaker refunds some of the original price to the payer.
Outcomes-based contracting sounds like a promising approach because various parties involved in the sale have a stake in the result, Dr. Nabhan said. “If you are a manufacturer, you want to make sure the outcomes are actually good,” he said. “If you’re a physician, you want to maximize monitoring your patient and managing adverse events. If you are the payer, you want to make sure your patient stays adherent to therapy, and you want to make sure you provide access to the doctor’s office, and to the hospital when needed. There’s more skin in the game when we look at outcomes-based contracting.”
Another idea gaining popularity is long-term financing for some drugs, particularly curative treatments. The idea has various models, but generally entails a financing arrangement, such as a loan mechanism for payers or a contractual annuitization that commits payers to pay costs over time. Such financing proposals are gaining speed in response to the high-cost of new gene therapies, according to a summary in Health Affairs. The payment agreements could be augmented by government funds such as government bonds or subsidies and/or efforts to promote risk-pooling across payers.
Peter B. Bach, MD, however, believes neither long-term financing nor outcomes-based contracting are good ideas. In January 2019 testimony to the U.S. Senate Committee on Finance, Dr. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center, New York, outlined why both value-based proposals are faulty. Outcomes-based contracting does not guarantee that prices are value based, he said, because it leaves untouched how much a drug costs when it does work. In addition, the long-term financing approach only pushes drug costs into future years, he testified.
“Financing does not reduce total spending, it just changes current obligations,” Dr. Bach said during testimony. “It is also relevant to appreciate that, whether for student loans or home mortgages, long-term payment arrangements are inflationary.”
Dr. Bach, a health policy expert whose work focuses on the cost and value of cancer drugs, and his colleagues at Memorial Sloan Kettering Cancer Center have spent the last few years fine-tuning an interactive drug-pricing tool that Dr. Bach says has distinct advantages over alternative drug-pricing proposals when it comes to considering value. The tool, called the DrugAbacus, integrates objective information about cancer drugs while empowering users to define what value means to them. For example, the DrugAbacus allows users to choose a dollar amount for each additional year of life the drug provides and lets them decide how much to discount the price for side effects, according to a summary of the tool by Dr. Bach published in the New England Journal of Medicine Catalyst. The price can be adjusted for factors such as treating a rare disease or having a novel action mechanism. The final result reveals the user’s self-valued DrugAbacus price and compares the cost with the drug’s initial market price.
“[DrugAbacus] provides a template for how we need to start thinking about value in drug pricing – by capturing some of the inherent complexity of value-based decisions without making the fundamentally flawed assumptions that are embedded in other drug-pricing proposals,” Dr. Bach wrote in the summary.
He declined to comment for this story.
A three-tiered approach
Another novel idea would link drug prices to value, but allow costs to change with new information. The proposal would create a three-part pricing model where prices vary over fixed time intervals, according to an article published in the New England Journal of Medicine Catalyst.
First, drugmakers would agree to launch a drug with a low price, with a potentially significant increase after a specified period to observe performance. During a second period, the price would be adjusted up or down based on newly emergent evidence. After a window of higher prices to reward innovation, the cost would then decline in a third period to ensure long-term access.
The advantage is access to truly miraculous therapies in a very short time – from 3 to 5 years earlier than the current system, said Luca Pani, MD, a coauthor of the paper and professor of psychiatry at the University of Miami.
“Another advantage emerges when it comes to drugs that treat patient populations with inaccurate epidemiology, in which we do not know exactly how many patients we have,” Dr. Pani said. “The model in this case allows to reduce the economic impact of this uncertainty.”
The main challenge would be finding a drug manufacturer that would agree to the arrangement, said Erik Snowberg, PhD, a coauthor of the study and a research associate for the National Bureau of Economic Research.
“There’s a lot of uncertainty right now,” Dr. Snowberg said. “The big challenge would be to find a drugmaker that would think about implementing this and finding the right payer for whom this would solve a pressing need.”
Despite the barriers to the idea, Dr. Pani said a more cost-effective drug cost structure is imperative, especially as the rapid rate of new therapies continues.
“We have a moral obligation to find alternative models that allow access and that are not only scientifically and economically sound and sustainable but also realistic and logical to implement,” he said.
Center’s experience casts doubt on clinical utility of NGS
Next-generation sequencing (NGS) of tumor samples seldom changes patient management, and even when it does prompt off-label therapy, outcomes are usually poor, one center’s experience suggests.
“NGS has allowed more personalized medicine in oncology. It is well established that treatment of certain actionable mutations improves outcomes in many cancer types,” wrote Gregory J. Kubicek, MD, of MD Anderson Cancer Center at Cooper in Camden, N.J., and colleagues.
However, evidence of its utility to date has been mixed, and key trials – NCI-MPACT (National Cancer Institute Molecular Profiling–Based Assignment of Cancer Therapy) and NCI-MATCH (National Cancer Institute Molecular Analysis for Therapy Choice)—are still ongoing. “In the interim, the oncologist must make clinical decisions with limited empiric data but an exponentially increasing number of options,” they noted.
The investigators studied outcomes of the first 305 consecutive patients at their institution for whom tissue samples were sent to FoundationOne for NGS testing between March 2014 and April 2017. On average, the patients had received two lines of therapy, and the test was ordered 1.1 years from diagnosis of metastatic disease.
Study findings reported in the Journal of Oncology Practice showed that 116 of the tests were unusable because they did not yield a report (most often as a result of insufficient tissue) or yielded a report that could not be acted on owing to follow-up issues (patient loss of contact, transfer to hospice, or death).
Of the 189 potentially usable tests, 40.2% and 66.7% showed an aberration targetable by on-label therapies and off-label therapies, respectively. And fully 89.9% had actionable aberrations via all potential avenues, including clinical trials.
However, only 11.1% of the 189 potentially usable tests (and merely 8.3% of 253 completed tests and 6.9% of all 305 ordered tests) yielded a change in management, including use of on-label or off-label therapies, enrollment in clinical trials, or discontinuation of medications with a predicted poor response.
Of the six patients who were started on an off-label therapy, the median duration of treatment was 46 days, with half of these patients each stopping therapy because of death or because of progression.
“A vast majority of NGS assay results were not actively incorporated into clinical decision making, despite many assays indicating potential on- or off-label therapies,” Dr. Kubicek and coinvestigators wrote. “Given the escalating cost of medical care and scrutiny thereof, it is important to analyze whether tests are changing management and order tests appropriately.”
Several factors may explain the observed low use of NGS test results, they noted. For example, many patients were heavily pretreated, so some NGS-detected mutations would have already been known. Also, clinicians at the center had little experience with NGS testing.
“A variety of factors make precisely defining the utility of these assays in clinical decision making difficult, but we can certainly conclude that we have observed substantial costs with few discernible benefits,” the investigators stated. “It is possible that there will be greater use in the future as familiarity with these assays increases. Similarly, although we found poor outcomes with NGS-directed off-label therapies, we will eagerly await the results of NCI-MPACT and NCI-MATCH.”
Dr. Kubicek disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Davis W et al. J Oncol Pract. 2019 Aug 2. doi: 10.1200/JOP.19.00269.
Next-generation sequencing (NGS) of tumor samples seldom changes patient management, and even when it does prompt off-label therapy, outcomes are usually poor, one center’s experience suggests.
“NGS has allowed more personalized medicine in oncology. It is well established that treatment of certain actionable mutations improves outcomes in many cancer types,” wrote Gregory J. Kubicek, MD, of MD Anderson Cancer Center at Cooper in Camden, N.J., and colleagues.
However, evidence of its utility to date has been mixed, and key trials – NCI-MPACT (National Cancer Institute Molecular Profiling–Based Assignment of Cancer Therapy) and NCI-MATCH (National Cancer Institute Molecular Analysis for Therapy Choice)—are still ongoing. “In the interim, the oncologist must make clinical decisions with limited empiric data but an exponentially increasing number of options,” they noted.
The investigators studied outcomes of the first 305 consecutive patients at their institution for whom tissue samples were sent to FoundationOne for NGS testing between March 2014 and April 2017. On average, the patients had received two lines of therapy, and the test was ordered 1.1 years from diagnosis of metastatic disease.
Study findings reported in the Journal of Oncology Practice showed that 116 of the tests were unusable because they did not yield a report (most often as a result of insufficient tissue) or yielded a report that could not be acted on owing to follow-up issues (patient loss of contact, transfer to hospice, or death).
Of the 189 potentially usable tests, 40.2% and 66.7% showed an aberration targetable by on-label therapies and off-label therapies, respectively. And fully 89.9% had actionable aberrations via all potential avenues, including clinical trials.
However, only 11.1% of the 189 potentially usable tests (and merely 8.3% of 253 completed tests and 6.9% of all 305 ordered tests) yielded a change in management, including use of on-label or off-label therapies, enrollment in clinical trials, or discontinuation of medications with a predicted poor response.
Of the six patients who were started on an off-label therapy, the median duration of treatment was 46 days, with half of these patients each stopping therapy because of death or because of progression.
“A vast majority of NGS assay results were not actively incorporated into clinical decision making, despite many assays indicating potential on- or off-label therapies,” Dr. Kubicek and coinvestigators wrote. “Given the escalating cost of medical care and scrutiny thereof, it is important to analyze whether tests are changing management and order tests appropriately.”
Several factors may explain the observed low use of NGS test results, they noted. For example, many patients were heavily pretreated, so some NGS-detected mutations would have already been known. Also, clinicians at the center had little experience with NGS testing.
“A variety of factors make precisely defining the utility of these assays in clinical decision making difficult, but we can certainly conclude that we have observed substantial costs with few discernible benefits,” the investigators stated. “It is possible that there will be greater use in the future as familiarity with these assays increases. Similarly, although we found poor outcomes with NGS-directed off-label therapies, we will eagerly await the results of NCI-MPACT and NCI-MATCH.”
Dr. Kubicek disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Davis W et al. J Oncol Pract. 2019 Aug 2. doi: 10.1200/JOP.19.00269.
Next-generation sequencing (NGS) of tumor samples seldom changes patient management, and even when it does prompt off-label therapy, outcomes are usually poor, one center’s experience suggests.
“NGS has allowed more personalized medicine in oncology. It is well established that treatment of certain actionable mutations improves outcomes in many cancer types,” wrote Gregory J. Kubicek, MD, of MD Anderson Cancer Center at Cooper in Camden, N.J., and colleagues.
However, evidence of its utility to date has been mixed, and key trials – NCI-MPACT (National Cancer Institute Molecular Profiling–Based Assignment of Cancer Therapy) and NCI-MATCH (National Cancer Institute Molecular Analysis for Therapy Choice)—are still ongoing. “In the interim, the oncologist must make clinical decisions with limited empiric data but an exponentially increasing number of options,” they noted.
The investigators studied outcomes of the first 305 consecutive patients at their institution for whom tissue samples were sent to FoundationOne for NGS testing between March 2014 and April 2017. On average, the patients had received two lines of therapy, and the test was ordered 1.1 years from diagnosis of metastatic disease.
Study findings reported in the Journal of Oncology Practice showed that 116 of the tests were unusable because they did not yield a report (most often as a result of insufficient tissue) or yielded a report that could not be acted on owing to follow-up issues (patient loss of contact, transfer to hospice, or death).
Of the 189 potentially usable tests, 40.2% and 66.7% showed an aberration targetable by on-label therapies and off-label therapies, respectively. And fully 89.9% had actionable aberrations via all potential avenues, including clinical trials.
However, only 11.1% of the 189 potentially usable tests (and merely 8.3% of 253 completed tests and 6.9% of all 305 ordered tests) yielded a change in management, including use of on-label or off-label therapies, enrollment in clinical trials, or discontinuation of medications with a predicted poor response.
Of the six patients who were started on an off-label therapy, the median duration of treatment was 46 days, with half of these patients each stopping therapy because of death or because of progression.
“A vast majority of NGS assay results were not actively incorporated into clinical decision making, despite many assays indicating potential on- or off-label therapies,” Dr. Kubicek and coinvestigators wrote. “Given the escalating cost of medical care and scrutiny thereof, it is important to analyze whether tests are changing management and order tests appropriately.”
Several factors may explain the observed low use of NGS test results, they noted. For example, many patients were heavily pretreated, so some NGS-detected mutations would have already been known. Also, clinicians at the center had little experience with NGS testing.
“A variety of factors make precisely defining the utility of these assays in clinical decision making difficult, but we can certainly conclude that we have observed substantial costs with few discernible benefits,” the investigators stated. “It is possible that there will be greater use in the future as familiarity with these assays increases. Similarly, although we found poor outcomes with NGS-directed off-label therapies, we will eagerly await the results of NCI-MPACT and NCI-MATCH.”
Dr. Kubicek disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Davis W et al. J Oncol Pract. 2019 Aug 2. doi: 10.1200/JOP.19.00269.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Aspirin interacts with epigenetics to influence breast cancer mortality
The impact of prediagnosis aspirin use on mortality in women with breast cancer is significantly tied to epigenetic changes in certain breast cancer-related genes, investigators reported.
While studies have shown aspirin reduces the risk of breast cancer development, there is limited and inconsistent data on the effect of aspirin on prognosis and mortality after a diagnosis of breast cancer, Tengteng Wang, PhD, from the department of epidemiology at the University of North Carolina at Chapel Hill and coauthors wrote in Cancer.
To address this, they analyzed data from 1,508 women who had a first diagnosis of primary breast cancer and were involved in the Long Island Breast Cancer Study Project; they then looked at the women’s methylation status, which is a mechanism of epigenetic change.
Around one in five participants reported ever using aspirin, and the analysis showed that ever use of aspirin was associated with an overall 13% decrease in breast cancer–specific mortality.
However researchers saw significant interactions between aspirin use and LINE-1 methylation status – which is a marker of methylation of genetic elements that play key roles in maintaining genomic stability – and breast cancer–specific genes.
They found that aspirin use in women with LINE-1 hypomethylation was associated with a risk of breast cancer–specific mortality that was 45% higher than that of nonusers (P = .05).
Compared with nonusers, aspirin users with methylated tumor BRCA1 promoter had significant 16% higher breast cancer mortality (P = .04) and 67% higher all-cause mortality (P = .02). However the study showed aspirin did not affect mortality in women with unmethylated BRCA1 promoter.
Among women with the PR breast cancer gene, aspirin use by those with methylation of the PR promoter was associated with a 63% higher breast cancer–specific mortality, but methylation showed no statistically significant effect on all-cause mortality, compared with nonusers.
The study found no significant change when they restricted the analysis to receptor-positive or invasive breast cancer, and the associations remained consistent even after adjusting for global methylation.
“Our findings suggest that the association between aspirin use and mortality after breast cancer may depend on methylation profiles and warrant further investigation,” the authors wrote. “These findings, if confirmed, may provide new biological insights into the association between aspirin use and breast cancer prognosis, may affect clinical decision making by identifying a subgroup of patients with breast cancer using epigenetic markers for whom prediagnosis aspirin use affects subsequent mortality, and may help refine risk-reduction strategies to improve survival among women with breast cancer.”
The study was partly supported by the National Institutes of Health. One author declared personal fees from the private sector outside the submitted work.
SOURCE: Wang T et al. Cancer. 2019 Aug 12. doi: 10.1002/cncr.32364.
This study offers new insights into the intersection of epigenetics, prediagnosis aspirin use, and breast cancer survival at a time when there is an urgent need to understand why some women respond differently to treatment and to find cost-effective therapies for the disease.
Epigenetics is a promising avenue of investigation because epigenetic shifts, such as DNA methylation, that impact the genes responsible for cell behavior and DNA damage and repair are known to contribute to and exacerbate cancer. These epigenetic signatures could act as biomarkers for risk in cancer and also aid with more effective treatment approaches. For example, aspirin is known to affect DNA methylation at certain sites in colon cancer, hence this study’s hypothesis that pre–cancer diagnosis aspirin use would interact with epigenetic signatures and influence breast cancer outcomes.
Kristen M. C. Malecki, PhD, is from the department of population health sciences in the School of Medicine and Public Health at the University of Wisconsin, Madison. The comments are adapted from an accompanying editorial (Cancer. 2019 Aug 12. doi: 10.1002/cncr.32365). Dr. Malecki declared support from the National Institutes of Health, National Institute for Environmental Health Sciences Breast Cancer, and the Environment Research Program.
This study offers new insights into the intersection of epigenetics, prediagnosis aspirin use, and breast cancer survival at a time when there is an urgent need to understand why some women respond differently to treatment and to find cost-effective therapies for the disease.
Epigenetics is a promising avenue of investigation because epigenetic shifts, such as DNA methylation, that impact the genes responsible for cell behavior and DNA damage and repair are known to contribute to and exacerbate cancer. These epigenetic signatures could act as biomarkers for risk in cancer and also aid with more effective treatment approaches. For example, aspirin is known to affect DNA methylation at certain sites in colon cancer, hence this study’s hypothesis that pre–cancer diagnosis aspirin use would interact with epigenetic signatures and influence breast cancer outcomes.
Kristen M. C. Malecki, PhD, is from the department of population health sciences in the School of Medicine and Public Health at the University of Wisconsin, Madison. The comments are adapted from an accompanying editorial (Cancer. 2019 Aug 12. doi: 10.1002/cncr.32365). Dr. Malecki declared support from the National Institutes of Health, National Institute for Environmental Health Sciences Breast Cancer, and the Environment Research Program.
This study offers new insights into the intersection of epigenetics, prediagnosis aspirin use, and breast cancer survival at a time when there is an urgent need to understand why some women respond differently to treatment and to find cost-effective therapies for the disease.
Epigenetics is a promising avenue of investigation because epigenetic shifts, such as DNA methylation, that impact the genes responsible for cell behavior and DNA damage and repair are known to contribute to and exacerbate cancer. These epigenetic signatures could act as biomarkers for risk in cancer and also aid with more effective treatment approaches. For example, aspirin is known to affect DNA methylation at certain sites in colon cancer, hence this study’s hypothesis that pre–cancer diagnosis aspirin use would interact with epigenetic signatures and influence breast cancer outcomes.
Kristen M. C. Malecki, PhD, is from the department of population health sciences in the School of Medicine and Public Health at the University of Wisconsin, Madison. The comments are adapted from an accompanying editorial (Cancer. 2019 Aug 12. doi: 10.1002/cncr.32365). Dr. Malecki declared support from the National Institutes of Health, National Institute for Environmental Health Sciences Breast Cancer, and the Environment Research Program.
The impact of prediagnosis aspirin use on mortality in women with breast cancer is significantly tied to epigenetic changes in certain breast cancer-related genes, investigators reported.
While studies have shown aspirin reduces the risk of breast cancer development, there is limited and inconsistent data on the effect of aspirin on prognosis and mortality after a diagnosis of breast cancer, Tengteng Wang, PhD, from the department of epidemiology at the University of North Carolina at Chapel Hill and coauthors wrote in Cancer.
To address this, they analyzed data from 1,508 women who had a first diagnosis of primary breast cancer and were involved in the Long Island Breast Cancer Study Project; they then looked at the women’s methylation status, which is a mechanism of epigenetic change.
Around one in five participants reported ever using aspirin, and the analysis showed that ever use of aspirin was associated with an overall 13% decrease in breast cancer–specific mortality.
However researchers saw significant interactions between aspirin use and LINE-1 methylation status – which is a marker of methylation of genetic elements that play key roles in maintaining genomic stability – and breast cancer–specific genes.
They found that aspirin use in women with LINE-1 hypomethylation was associated with a risk of breast cancer–specific mortality that was 45% higher than that of nonusers (P = .05).
Compared with nonusers, aspirin users with methylated tumor BRCA1 promoter had significant 16% higher breast cancer mortality (P = .04) and 67% higher all-cause mortality (P = .02). However the study showed aspirin did not affect mortality in women with unmethylated BRCA1 promoter.
Among women with the PR breast cancer gene, aspirin use by those with methylation of the PR promoter was associated with a 63% higher breast cancer–specific mortality, but methylation showed no statistically significant effect on all-cause mortality, compared with nonusers.
The study found no significant change when they restricted the analysis to receptor-positive or invasive breast cancer, and the associations remained consistent even after adjusting for global methylation.
“Our findings suggest that the association between aspirin use and mortality after breast cancer may depend on methylation profiles and warrant further investigation,” the authors wrote. “These findings, if confirmed, may provide new biological insights into the association between aspirin use and breast cancer prognosis, may affect clinical decision making by identifying a subgroup of patients with breast cancer using epigenetic markers for whom prediagnosis aspirin use affects subsequent mortality, and may help refine risk-reduction strategies to improve survival among women with breast cancer.”
The study was partly supported by the National Institutes of Health. One author declared personal fees from the private sector outside the submitted work.
SOURCE: Wang T et al. Cancer. 2019 Aug 12. doi: 10.1002/cncr.32364.
The impact of prediagnosis aspirin use on mortality in women with breast cancer is significantly tied to epigenetic changes in certain breast cancer-related genes, investigators reported.
While studies have shown aspirin reduces the risk of breast cancer development, there is limited and inconsistent data on the effect of aspirin on prognosis and mortality after a diagnosis of breast cancer, Tengteng Wang, PhD, from the department of epidemiology at the University of North Carolina at Chapel Hill and coauthors wrote in Cancer.
To address this, they analyzed data from 1,508 women who had a first diagnosis of primary breast cancer and were involved in the Long Island Breast Cancer Study Project; they then looked at the women’s methylation status, which is a mechanism of epigenetic change.
Around one in five participants reported ever using aspirin, and the analysis showed that ever use of aspirin was associated with an overall 13% decrease in breast cancer–specific mortality.
However researchers saw significant interactions between aspirin use and LINE-1 methylation status – which is a marker of methylation of genetic elements that play key roles in maintaining genomic stability – and breast cancer–specific genes.
They found that aspirin use in women with LINE-1 hypomethylation was associated with a risk of breast cancer–specific mortality that was 45% higher than that of nonusers (P = .05).
Compared with nonusers, aspirin users with methylated tumor BRCA1 promoter had significant 16% higher breast cancer mortality (P = .04) and 67% higher all-cause mortality (P = .02). However the study showed aspirin did not affect mortality in women with unmethylated BRCA1 promoter.
Among women with the PR breast cancer gene, aspirin use by those with methylation of the PR promoter was associated with a 63% higher breast cancer–specific mortality, but methylation showed no statistically significant effect on all-cause mortality, compared with nonusers.
The study found no significant change when they restricted the analysis to receptor-positive or invasive breast cancer, and the associations remained consistent even after adjusting for global methylation.
“Our findings suggest that the association between aspirin use and mortality after breast cancer may depend on methylation profiles and warrant further investigation,” the authors wrote. “These findings, if confirmed, may provide new biological insights into the association between aspirin use and breast cancer prognosis, may affect clinical decision making by identifying a subgroup of patients with breast cancer using epigenetic markers for whom prediagnosis aspirin use affects subsequent mortality, and may help refine risk-reduction strategies to improve survival among women with breast cancer.”
The study was partly supported by the National Institutes of Health. One author declared personal fees from the private sector outside the submitted work.
SOURCE: Wang T et al. Cancer. 2019 Aug 12. doi: 10.1002/cncr.32364.
FROM CANCER
Cardiovascular complications most common with carfilzomib in relapsed myeloma
Cardiovascular (CV) adverse events were common in patients receiving proteasome inhibitor therapy for relapsed multiple myeloma, especially with carfilzomib-based therapy, according to results from the PROTECT study.
While prior studies have shown an increased risk for CV toxicities with proteasome inhibitor therapy, detailed descriptions of the events and risk factors have been lacking. “Furthermore, there is no validated protocol to help determine which patients are at highest risk of CV toxicity during therapy, nor is there management guidance for patients who experience a [CV adverse event],” wrote Robert F. Cornell, MD, of Vanderbilt University, Nashville, Tenn., and colleagues in the Journal of Clinical Oncology.
The PROTECT (Prospective Observation of Cardiac Safety with Proteasome Inhibitor) study was conducted at Vanderbilt University Medical Center and the University of Pennsylvania Abramson Cancer Center, Philadelphia, between September 2015 and March 2018.
Researchers followed 95 patients with relapsed multiple myeloma who were treated with either bortezomib or carfilzomib for a total duration of 18 months. A total of 65 patients received a carfilzomib-based therapy and 30 patients received a bortezomib-based therapy.
Study patients received a CV assessment at baseline and at the beginning of each treatment cycle for the initial six cycles of proteasome inhibitor therapy. Subsequently, patients were monitored for the development of CV adverse events. CV assessments included ECG, echocardiography, and measurement of other cardiac biomarkers, such as NTproBNP and troponin I or T.
CV toxicities were reported among 5 patients (16.7%) of patients treated with bortezomib and 33 patients (50.7%) treated with carfilzomib (P = .005).
In total, there were 64 CV adverse events reported, most of which were grade 2 or 3, and 56 of which occurred while on carfilzomib-based therapy. For carfilzomib, the most common complications were heart failure (23 cases), followed by grade 3 or 4 hypertension (13 cases). Cardiac chest pain, atrial fibrillation, and acute coronary syndrome were reported in fewer cases.
The researchers also found that elevated natriuretic peptides that occurred before starting carfilzomib therapy or within the first 3 weeks of carfilzomib therapy were associated with a substantially higher risk of CV adverse events.
Patients who have multiple CV risk factors, and especially patients with a history of CV complications and elevated baseline natriuretic peptides, should be referred for a comprehensive cardiac evaluation, the researchers advised. “Such patients are at highest risk of CV [adverse events] with carfilzomib-based therapy, and optimization of CV therapy seems to improve overall care, allow continuation of potentially lifesaving cancer treatment, and affect severity or development of CV [adverse events],” they wrote.
A key limitation of the study was the lack of standardized treatment regimens. As a result, there was a broad dosing range for carfilzomib, in comparison to bortezomib.
Some authors reported financial relationships with carfilzomib maker Amgen and bortezomib maker Takeda, as well as with other companies.
SOURCE: Cornell RF et al. J Clin Oncol. 2019 Jun 12. doi: 10.1200/JCO.19.00231.
Cardiovascular (CV) adverse events were common in patients receiving proteasome inhibitor therapy for relapsed multiple myeloma, especially with carfilzomib-based therapy, according to results from the PROTECT study.
While prior studies have shown an increased risk for CV toxicities with proteasome inhibitor therapy, detailed descriptions of the events and risk factors have been lacking. “Furthermore, there is no validated protocol to help determine which patients are at highest risk of CV toxicity during therapy, nor is there management guidance for patients who experience a [CV adverse event],” wrote Robert F. Cornell, MD, of Vanderbilt University, Nashville, Tenn., and colleagues in the Journal of Clinical Oncology.
The PROTECT (Prospective Observation of Cardiac Safety with Proteasome Inhibitor) study was conducted at Vanderbilt University Medical Center and the University of Pennsylvania Abramson Cancer Center, Philadelphia, between September 2015 and March 2018.
Researchers followed 95 patients with relapsed multiple myeloma who were treated with either bortezomib or carfilzomib for a total duration of 18 months. A total of 65 patients received a carfilzomib-based therapy and 30 patients received a bortezomib-based therapy.
Study patients received a CV assessment at baseline and at the beginning of each treatment cycle for the initial six cycles of proteasome inhibitor therapy. Subsequently, patients were monitored for the development of CV adverse events. CV assessments included ECG, echocardiography, and measurement of other cardiac biomarkers, such as NTproBNP and troponin I or T.
CV toxicities were reported among 5 patients (16.7%) of patients treated with bortezomib and 33 patients (50.7%) treated with carfilzomib (P = .005).
In total, there were 64 CV adverse events reported, most of which were grade 2 or 3, and 56 of which occurred while on carfilzomib-based therapy. For carfilzomib, the most common complications were heart failure (23 cases), followed by grade 3 or 4 hypertension (13 cases). Cardiac chest pain, atrial fibrillation, and acute coronary syndrome were reported in fewer cases.
The researchers also found that elevated natriuretic peptides that occurred before starting carfilzomib therapy or within the first 3 weeks of carfilzomib therapy were associated with a substantially higher risk of CV adverse events.
Patients who have multiple CV risk factors, and especially patients with a history of CV complications and elevated baseline natriuretic peptides, should be referred for a comprehensive cardiac evaluation, the researchers advised. “Such patients are at highest risk of CV [adverse events] with carfilzomib-based therapy, and optimization of CV therapy seems to improve overall care, allow continuation of potentially lifesaving cancer treatment, and affect severity or development of CV [adverse events],” they wrote.
A key limitation of the study was the lack of standardized treatment regimens. As a result, there was a broad dosing range for carfilzomib, in comparison to bortezomib.
Some authors reported financial relationships with carfilzomib maker Amgen and bortezomib maker Takeda, as well as with other companies.
SOURCE: Cornell RF et al. J Clin Oncol. 2019 Jun 12. doi: 10.1200/JCO.19.00231.
Cardiovascular (CV) adverse events were common in patients receiving proteasome inhibitor therapy for relapsed multiple myeloma, especially with carfilzomib-based therapy, according to results from the PROTECT study.
While prior studies have shown an increased risk for CV toxicities with proteasome inhibitor therapy, detailed descriptions of the events and risk factors have been lacking. “Furthermore, there is no validated protocol to help determine which patients are at highest risk of CV toxicity during therapy, nor is there management guidance for patients who experience a [CV adverse event],” wrote Robert F. Cornell, MD, of Vanderbilt University, Nashville, Tenn., and colleagues in the Journal of Clinical Oncology.
The PROTECT (Prospective Observation of Cardiac Safety with Proteasome Inhibitor) study was conducted at Vanderbilt University Medical Center and the University of Pennsylvania Abramson Cancer Center, Philadelphia, between September 2015 and March 2018.
Researchers followed 95 patients with relapsed multiple myeloma who were treated with either bortezomib or carfilzomib for a total duration of 18 months. A total of 65 patients received a carfilzomib-based therapy and 30 patients received a bortezomib-based therapy.
Study patients received a CV assessment at baseline and at the beginning of each treatment cycle for the initial six cycles of proteasome inhibitor therapy. Subsequently, patients were monitored for the development of CV adverse events. CV assessments included ECG, echocardiography, and measurement of other cardiac biomarkers, such as NTproBNP and troponin I or T.
CV toxicities were reported among 5 patients (16.7%) of patients treated with bortezomib and 33 patients (50.7%) treated with carfilzomib (P = .005).
In total, there were 64 CV adverse events reported, most of which were grade 2 or 3, and 56 of which occurred while on carfilzomib-based therapy. For carfilzomib, the most common complications were heart failure (23 cases), followed by grade 3 or 4 hypertension (13 cases). Cardiac chest pain, atrial fibrillation, and acute coronary syndrome were reported in fewer cases.
The researchers also found that elevated natriuretic peptides that occurred before starting carfilzomib therapy or within the first 3 weeks of carfilzomib therapy were associated with a substantially higher risk of CV adverse events.
Patients who have multiple CV risk factors, and especially patients with a history of CV complications and elevated baseline natriuretic peptides, should be referred for a comprehensive cardiac evaluation, the researchers advised. “Such patients are at highest risk of CV [adverse events] with carfilzomib-based therapy, and optimization of CV therapy seems to improve overall care, allow continuation of potentially lifesaving cancer treatment, and affect severity or development of CV [adverse events],” they wrote.
A key limitation of the study was the lack of standardized treatment regimens. As a result, there was a broad dosing range for carfilzomib, in comparison to bortezomib.
Some authors reported financial relationships with carfilzomib maker Amgen and bortezomib maker Takeda, as well as with other companies.
SOURCE: Cornell RF et al. J Clin Oncol. 2019 Jun 12. doi: 10.1200/JCO.19.00231.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
CVD risk after breast cancer: Adipose distribution trumps BMI
When it comes to cardiovascular disease (CVD) risk after a breast cancer diagnosis, it’s not so much a matter of the amount of body fat carried but rather where it is located, results of a retrospective cohort study of nearly 3,000 survivors suggest.
“It is well known that higher body mass index (BMI) is associated with CVD mortality in the general population. However, BMI is not always an accurate proxy for individual-level adiposity and does not describe adipose tissue distribution,” note lead investigator Elizabeth M. Cespedes Feliciano, ScD, of Kaiser Permanente Northern California, Oakland, Calif., and coinvestigators.
The investigators studied 2,943 survivors of nonmetastatic breast cancer having a mean age of 56 years who were initially CVD free, using clinically acquired CT scans obtained near diagnosis to measure adiposity in three compartments: visceral, subcutaneous, and intramuscular.
The cohort experienced 328 CVD events (nonfatal stroke, myocardial infarction, heart failure, or CVD death) during a median follow-up of 6 years, the investigators reported in Journal of Clinical Oncology. The 10-year cumulative incidence was 15%.
In analyses that were adjusted for potential confounders and took into account competing risks, survivors’ CVD risk increased significantly with each standard deviation (SD) increase in visceral adiposity (hazard ratio, 1.15; 95% confidence interval, 1.03-1.29) and each SD increase in intramuscular adiposity (HR, 1.21; 95% CI, 1.06-1.37). The association for subcutaneous adiposity was not significant.
Findings were similar across all BMI categories. Of particular note, among survivors having a normal BMI, risk of CVD events increased by 70% with each SD greater visceral adiposity (HR, 1.70; 95% CI, 1.10-2.62).
Risk also rose with BMI exceeding the normal range, but the association became significant only in survivors with a BMI placing them in obesity class II (35 kg/m2 or greater) (HR, 1.70; 95% CI, 1.20-2.42).
“Although it has been assumed that excess adiposity increases the risk of CVD after breast cancer, this first-of-its-kind study demonstrates that adipose tissue distribution best identifies patients with breast cancer with higher CVD risk after diagnosis, including those with normal BMI,” Dr. Cespedes Feliciano and coinvestigators note.
“Software is now available that automatically measures body composition from clinically acquired CT scans, facilitating clinical integration,” they note. “Measures of adipose tissue distribution from CT or anthropometry (e.g., waist circumference) may help identify individuals with high CVD risk and tailor prevention efforts to patients’ body composition.”
Dr. Cespedes Feliciano disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Cespedes Feliciano EM et al. J Clin Oncol. 2019 Aug 1. doi: 10.1200/JCO.19.00286.
When it comes to cardiovascular disease (CVD) risk after a breast cancer diagnosis, it’s not so much a matter of the amount of body fat carried but rather where it is located, results of a retrospective cohort study of nearly 3,000 survivors suggest.
“It is well known that higher body mass index (BMI) is associated with CVD mortality in the general population. However, BMI is not always an accurate proxy for individual-level adiposity and does not describe adipose tissue distribution,” note lead investigator Elizabeth M. Cespedes Feliciano, ScD, of Kaiser Permanente Northern California, Oakland, Calif., and coinvestigators.
The investigators studied 2,943 survivors of nonmetastatic breast cancer having a mean age of 56 years who were initially CVD free, using clinically acquired CT scans obtained near diagnosis to measure adiposity in three compartments: visceral, subcutaneous, and intramuscular.
The cohort experienced 328 CVD events (nonfatal stroke, myocardial infarction, heart failure, or CVD death) during a median follow-up of 6 years, the investigators reported in Journal of Clinical Oncology. The 10-year cumulative incidence was 15%.
In analyses that were adjusted for potential confounders and took into account competing risks, survivors’ CVD risk increased significantly with each standard deviation (SD) increase in visceral adiposity (hazard ratio, 1.15; 95% confidence interval, 1.03-1.29) and each SD increase in intramuscular adiposity (HR, 1.21; 95% CI, 1.06-1.37). The association for subcutaneous adiposity was not significant.
Findings were similar across all BMI categories. Of particular note, among survivors having a normal BMI, risk of CVD events increased by 70% with each SD greater visceral adiposity (HR, 1.70; 95% CI, 1.10-2.62).
Risk also rose with BMI exceeding the normal range, but the association became significant only in survivors with a BMI placing them in obesity class II (35 kg/m2 or greater) (HR, 1.70; 95% CI, 1.20-2.42).
“Although it has been assumed that excess adiposity increases the risk of CVD after breast cancer, this first-of-its-kind study demonstrates that adipose tissue distribution best identifies patients with breast cancer with higher CVD risk after diagnosis, including those with normal BMI,” Dr. Cespedes Feliciano and coinvestigators note.
“Software is now available that automatically measures body composition from clinically acquired CT scans, facilitating clinical integration,” they note. “Measures of adipose tissue distribution from CT or anthropometry (e.g., waist circumference) may help identify individuals with high CVD risk and tailor prevention efforts to patients’ body composition.”
Dr. Cespedes Feliciano disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Cespedes Feliciano EM et al. J Clin Oncol. 2019 Aug 1. doi: 10.1200/JCO.19.00286.
When it comes to cardiovascular disease (CVD) risk after a breast cancer diagnosis, it’s not so much a matter of the amount of body fat carried but rather where it is located, results of a retrospective cohort study of nearly 3,000 survivors suggest.
“It is well known that higher body mass index (BMI) is associated with CVD mortality in the general population. However, BMI is not always an accurate proxy for individual-level adiposity and does not describe adipose tissue distribution,” note lead investigator Elizabeth M. Cespedes Feliciano, ScD, of Kaiser Permanente Northern California, Oakland, Calif., and coinvestigators.
The investigators studied 2,943 survivors of nonmetastatic breast cancer having a mean age of 56 years who were initially CVD free, using clinically acquired CT scans obtained near diagnosis to measure adiposity in three compartments: visceral, subcutaneous, and intramuscular.
The cohort experienced 328 CVD events (nonfatal stroke, myocardial infarction, heart failure, or CVD death) during a median follow-up of 6 years, the investigators reported in Journal of Clinical Oncology. The 10-year cumulative incidence was 15%.
In analyses that were adjusted for potential confounders and took into account competing risks, survivors’ CVD risk increased significantly with each standard deviation (SD) increase in visceral adiposity (hazard ratio, 1.15; 95% confidence interval, 1.03-1.29) and each SD increase in intramuscular adiposity (HR, 1.21; 95% CI, 1.06-1.37). The association for subcutaneous adiposity was not significant.
Findings were similar across all BMI categories. Of particular note, among survivors having a normal BMI, risk of CVD events increased by 70% with each SD greater visceral adiposity (HR, 1.70; 95% CI, 1.10-2.62).
Risk also rose with BMI exceeding the normal range, but the association became significant only in survivors with a BMI placing them in obesity class II (35 kg/m2 or greater) (HR, 1.70; 95% CI, 1.20-2.42).
“Although it has been assumed that excess adiposity increases the risk of CVD after breast cancer, this first-of-its-kind study demonstrates that adipose tissue distribution best identifies patients with breast cancer with higher CVD risk after diagnosis, including those with normal BMI,” Dr. Cespedes Feliciano and coinvestigators note.
“Software is now available that automatically measures body composition from clinically acquired CT scans, facilitating clinical integration,” they note. “Measures of adipose tissue distribution from CT or anthropometry (e.g., waist circumference) may help identify individuals with high CVD risk and tailor prevention efforts to patients’ body composition.”
Dr. Cespedes Feliciano disclosed no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Cespedes Feliciano EM et al. J Clin Oncol. 2019 Aug 1. doi: 10.1200/JCO.19.00286.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Cost a factor in breast cancer treatment decisions
Treatment costs are a significant factor in women’s decision making around breast cancer surgery, investigators reported.
With the health care costs of breast cancer estimated to reach $20 billion by 2020 in the United States, many of those costs are being shifted onto patients themselves, wrote Rachel A. Greenup, MD, from Duke University, Durham, N.C., and coauthors in the Journal of Oncology Practice.
“This financial hardship is now recognized as a major adverse effect of cancer care and has been associated with reduced quality of life, nonadherence, and an increased risk of early mortality,” they wrote.
Researchers surveyed 607 women with a history of breast cancer to examine the impact that cost had on their decisions about surgery and what financial harm they had experienced after breast cancer surgery.
Overall, 43% of women said they considered costs when making decisions about breast cancer treatment, 28% said cost influenced their decision making around breast cancer surgery, and 14% said costs were extremely important in that decision.
Women in the lowest income bracket – earning at or below $45,000 per year – identified cost as the most influential factor in their decision about breast cancer surgery, above loss of sensation, breast preservation or appearance, the need for long-term surveillance, or avoiding radiation.
However, more than three-quarters of women said they never discussed costs with their medical team.
Bilateral mastectomy, with and without reconstruction, was associated with higher patient-reported out-of-pocket costs, higher debt, higher rates of cancer-induced financial hardship, and higher rates of altered or reduced employment, compared with breast-conserving surgery.
More than one-third of participants reported significant to catastrophic financial burden because of their breast cancer care.
Even in the highest income brackets, two-thirds of women were financially unprepared for the cost of treatment, and 26% said their treatment costs were higher than expected.
The authors commented that “cost transparency” was uncommon between oncologically equivalent surgical treatments, “thus, patients with breast cancer may unknowingly be guiding therapeutic decisions that increase the risk of financial harm.”
“To date, patient out-of-pocket costs and subsequent risk of financial harm have not been routinely incorporated into shared decisions for breast cancer surgery, a process that has otherwise highly revered patient values,” they wrote.
The investigators suggested that revealing the greater risk for financial burden associated with treatments like bilateral mastectomy could help inform surgical treatment decisions.
The study was supported by the National Institutes of Health and the Duke Cancer Institute. Six authors reported honoraria, research funding, prior employment, and other support from the pharmaceutical sector.
SOURCE: Greenup RA et al. J Oncol Pract. 2019 Jul 29. doi: 10.1200/JOP.18.00796.
Treatment costs are a significant factor in women’s decision making around breast cancer surgery, investigators reported.
With the health care costs of breast cancer estimated to reach $20 billion by 2020 in the United States, many of those costs are being shifted onto patients themselves, wrote Rachel A. Greenup, MD, from Duke University, Durham, N.C., and coauthors in the Journal of Oncology Practice.
“This financial hardship is now recognized as a major adverse effect of cancer care and has been associated with reduced quality of life, nonadherence, and an increased risk of early mortality,” they wrote.
Researchers surveyed 607 women with a history of breast cancer to examine the impact that cost had on their decisions about surgery and what financial harm they had experienced after breast cancer surgery.
Overall, 43% of women said they considered costs when making decisions about breast cancer treatment, 28% said cost influenced their decision making around breast cancer surgery, and 14% said costs were extremely important in that decision.
Women in the lowest income bracket – earning at or below $45,000 per year – identified cost as the most influential factor in their decision about breast cancer surgery, above loss of sensation, breast preservation or appearance, the need for long-term surveillance, or avoiding radiation.
However, more than three-quarters of women said they never discussed costs with their medical team.
Bilateral mastectomy, with and without reconstruction, was associated with higher patient-reported out-of-pocket costs, higher debt, higher rates of cancer-induced financial hardship, and higher rates of altered or reduced employment, compared with breast-conserving surgery.
More than one-third of participants reported significant to catastrophic financial burden because of their breast cancer care.
Even in the highest income brackets, two-thirds of women were financially unprepared for the cost of treatment, and 26% said their treatment costs were higher than expected.
The authors commented that “cost transparency” was uncommon between oncologically equivalent surgical treatments, “thus, patients with breast cancer may unknowingly be guiding therapeutic decisions that increase the risk of financial harm.”
“To date, patient out-of-pocket costs and subsequent risk of financial harm have not been routinely incorporated into shared decisions for breast cancer surgery, a process that has otherwise highly revered patient values,” they wrote.
The investigators suggested that revealing the greater risk for financial burden associated with treatments like bilateral mastectomy could help inform surgical treatment decisions.
The study was supported by the National Institutes of Health and the Duke Cancer Institute. Six authors reported honoraria, research funding, prior employment, and other support from the pharmaceutical sector.
SOURCE: Greenup RA et al. J Oncol Pract. 2019 Jul 29. doi: 10.1200/JOP.18.00796.
Treatment costs are a significant factor in women’s decision making around breast cancer surgery, investigators reported.
With the health care costs of breast cancer estimated to reach $20 billion by 2020 in the United States, many of those costs are being shifted onto patients themselves, wrote Rachel A. Greenup, MD, from Duke University, Durham, N.C., and coauthors in the Journal of Oncology Practice.
“This financial hardship is now recognized as a major adverse effect of cancer care and has been associated with reduced quality of life, nonadherence, and an increased risk of early mortality,” they wrote.
Researchers surveyed 607 women with a history of breast cancer to examine the impact that cost had on their decisions about surgery and what financial harm they had experienced after breast cancer surgery.
Overall, 43% of women said they considered costs when making decisions about breast cancer treatment, 28% said cost influenced their decision making around breast cancer surgery, and 14% said costs were extremely important in that decision.
Women in the lowest income bracket – earning at or below $45,000 per year – identified cost as the most influential factor in their decision about breast cancer surgery, above loss of sensation, breast preservation or appearance, the need for long-term surveillance, or avoiding radiation.
However, more than three-quarters of women said they never discussed costs with their medical team.
Bilateral mastectomy, with and without reconstruction, was associated with higher patient-reported out-of-pocket costs, higher debt, higher rates of cancer-induced financial hardship, and higher rates of altered or reduced employment, compared with breast-conserving surgery.
More than one-third of participants reported significant to catastrophic financial burden because of their breast cancer care.
Even in the highest income brackets, two-thirds of women were financially unprepared for the cost of treatment, and 26% said their treatment costs were higher than expected.
The authors commented that “cost transparency” was uncommon between oncologically equivalent surgical treatments, “thus, patients with breast cancer may unknowingly be guiding therapeutic decisions that increase the risk of financial harm.”
“To date, patient out-of-pocket costs and subsequent risk of financial harm have not been routinely incorporated into shared decisions for breast cancer surgery, a process that has otherwise highly revered patient values,” they wrote.
The investigators suggested that revealing the greater risk for financial burden associated with treatments like bilateral mastectomy could help inform surgical treatment decisions.
The study was supported by the National Institutes of Health and the Duke Cancer Institute. Six authors reported honoraria, research funding, prior employment, and other support from the pharmaceutical sector.
SOURCE: Greenup RA et al. J Oncol Pract. 2019 Jul 29. doi: 10.1200/JOP.18.00796.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Illusion of options
Mr. M wanted a second opinion. He was almost 80 years old and had been healthy his entire life. But recent abdominal discomfort prompted a CT scan, which prompted a biopsy. It appeared the tumor had started in his pancreas and then spread to the lymph nodes and the wall of his abdomen.
He asked his doctor to “give it to him straight,” and she did. She told him that it was incurable, but that chemotherapy might slow it down. He asked how long he had, and she said less than a year.
He wanted a straight answer, but that wasn’t the answer he wanted. Who would? So he did some reading and decided to come to a large academic hospital an hour away for a second opinion.
I interviewed him and then scrolled through his CT scans outside the room. There were a few things we could do, the attending and I discussed. We would send his tumor for genetic testing to see if there were any cancer mutations that could be targeted with drugs more specific than standard chemotherapy. We would also refer him to our cancer genetics clinic to get his blood tested for inherited mutations.
But mostly, all of that would likely turn up negative. Mostly, we agreed with his local oncologist.
We went back in the room. Explaining the genetic testing took the length of the visit because this is not a straightforward concept. We explained the difference between tumor mutations and inherited mutations. We wrote down a list of genetic variations we could discover. We discussed treatment options that could go along with each.
Do you have any questions?
He broke down. He reached for the tissue box sitting on the exam room table. “I feel so much better,” he said. “This is why I came here.” He felt safe, reassured, and hopeful.
I was happy to be helpful, but later, as I wrote my clinic note about him, I felt uneasy about the visit.
Everything we said was true. But somehow, it still felt as though we left him with an overly optimistic view of his illness. Did our emphasis on what could be done overshadow that it was unlikely to change the big picture? Did our in-depth discussion of slim possibilities mask that his prognosis was, in fact, still grim?
Working at a large academic medical center, I see many patients who come for a second opinion. I’m incredibly fortunate to learn at a place that is not just up to date in the most cutting-edge treatments but often leading in innovation.
And so we offer patients these options. They sound novel and exciting. They fill patients with hope because they fill the field with hope. I, too, get enraptured with the possibilities – circulating tumor DNA and clinical trials and targeted therapies.
At big cancer meetings every year, oncologists come together and speak about cancer therapies with enthusiasm and hope. Advances have exploded; it’s an exciting time to be learning and practicing.
And yet, the reality for many patients is very different. We are still discussing hospice after one line of chemotherapy has failed. We are still gently holding hands and saying that we have no more options to treat their aggressive cancers.
How can both of these worlds coexist? How can both be true?
A few years ago, a friend was diagnosed with a devastating neurologic condition. I went to a clinical trials website and typed in her disease. Immediately, hundreds of options popped up. I felt hopeful. The field is moving forward, I thought. There are options.
But in the exam room, there were none. When I asked about what I had read, the neurologist explained how many of these possibilities were being investigated. But in the end, my friend really had no good options.
After my visit with Mr. M, I thought about how commonly this story plays out in my field of hematology and oncology. Yes, there are instances in which we find a mutation that drastically changes management. It’s wonderful to witness: patients handed an ominous diagnosis and then living their normal lives, in remission or with stable disease, years later.
We all hope for that. But we rarely get it. The challenge comes when we spend 95% of a visit talking about something with a 1% chance of working. The numbers don’t add up – it’s an equation that easily results in false understanding. Cancer can be glossed with a veneer of innovative options, obscuring the reality that none are likely to work.
Weaving both truths into the conversation is a difficult skill, but one I decided to be more cognizant of after my encounter with Mr. M.
At our next visit, we were still waiting on the test results. But I decided to speak with him candidly. It’s important to have a plan B, I said, and asked what would be important to him if his time were limited. He nodded, thinking about this. “I’ve just been holding out hope for the mutation,” he admitted.
The next week his genetic testing came back negative, and he decided to get palliative chemotherapy closer to home. He had no reason to come to a large academic hospital anymore. With nothing special to offer him, I never saw him again.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz and listen to her each week on the Blood & Cancer podcast.
Mr. M wanted a second opinion. He was almost 80 years old and had been healthy his entire life. But recent abdominal discomfort prompted a CT scan, which prompted a biopsy. It appeared the tumor had started in his pancreas and then spread to the lymph nodes and the wall of his abdomen.
He asked his doctor to “give it to him straight,” and she did. She told him that it was incurable, but that chemotherapy might slow it down. He asked how long he had, and she said less than a year.
He wanted a straight answer, but that wasn’t the answer he wanted. Who would? So he did some reading and decided to come to a large academic hospital an hour away for a second opinion.
I interviewed him and then scrolled through his CT scans outside the room. There were a few things we could do, the attending and I discussed. We would send his tumor for genetic testing to see if there were any cancer mutations that could be targeted with drugs more specific than standard chemotherapy. We would also refer him to our cancer genetics clinic to get his blood tested for inherited mutations.
But mostly, all of that would likely turn up negative. Mostly, we agreed with his local oncologist.
We went back in the room. Explaining the genetic testing took the length of the visit because this is not a straightforward concept. We explained the difference between tumor mutations and inherited mutations. We wrote down a list of genetic variations we could discover. We discussed treatment options that could go along with each.
Do you have any questions?
He broke down. He reached for the tissue box sitting on the exam room table. “I feel so much better,” he said. “This is why I came here.” He felt safe, reassured, and hopeful.
I was happy to be helpful, but later, as I wrote my clinic note about him, I felt uneasy about the visit.
Everything we said was true. But somehow, it still felt as though we left him with an overly optimistic view of his illness. Did our emphasis on what could be done overshadow that it was unlikely to change the big picture? Did our in-depth discussion of slim possibilities mask that his prognosis was, in fact, still grim?
Working at a large academic medical center, I see many patients who come for a second opinion. I’m incredibly fortunate to learn at a place that is not just up to date in the most cutting-edge treatments but often leading in innovation.
And so we offer patients these options. They sound novel and exciting. They fill patients with hope because they fill the field with hope. I, too, get enraptured with the possibilities – circulating tumor DNA and clinical trials and targeted therapies.
At big cancer meetings every year, oncologists come together and speak about cancer therapies with enthusiasm and hope. Advances have exploded; it’s an exciting time to be learning and practicing.
And yet, the reality for many patients is very different. We are still discussing hospice after one line of chemotherapy has failed. We are still gently holding hands and saying that we have no more options to treat their aggressive cancers.
How can both of these worlds coexist? How can both be true?
A few years ago, a friend was diagnosed with a devastating neurologic condition. I went to a clinical trials website and typed in her disease. Immediately, hundreds of options popped up. I felt hopeful. The field is moving forward, I thought. There are options.
But in the exam room, there were none. When I asked about what I had read, the neurologist explained how many of these possibilities were being investigated. But in the end, my friend really had no good options.
After my visit with Mr. M, I thought about how commonly this story plays out in my field of hematology and oncology. Yes, there are instances in which we find a mutation that drastically changes management. It’s wonderful to witness: patients handed an ominous diagnosis and then living their normal lives, in remission or with stable disease, years later.
We all hope for that. But we rarely get it. The challenge comes when we spend 95% of a visit talking about something with a 1% chance of working. The numbers don’t add up – it’s an equation that easily results in false understanding. Cancer can be glossed with a veneer of innovative options, obscuring the reality that none are likely to work.
Weaving both truths into the conversation is a difficult skill, but one I decided to be more cognizant of after my encounter with Mr. M.
At our next visit, we were still waiting on the test results. But I decided to speak with him candidly. It’s important to have a plan B, I said, and asked what would be important to him if his time were limited. He nodded, thinking about this. “I’ve just been holding out hope for the mutation,” he admitted.
The next week his genetic testing came back negative, and he decided to get palliative chemotherapy closer to home. He had no reason to come to a large academic hospital anymore. With nothing special to offer him, I never saw him again.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz and listen to her each week on the Blood & Cancer podcast.
Mr. M wanted a second opinion. He was almost 80 years old and had been healthy his entire life. But recent abdominal discomfort prompted a CT scan, which prompted a biopsy. It appeared the tumor had started in his pancreas and then spread to the lymph nodes and the wall of his abdomen.
He asked his doctor to “give it to him straight,” and she did. She told him that it was incurable, but that chemotherapy might slow it down. He asked how long he had, and she said less than a year.
He wanted a straight answer, but that wasn’t the answer he wanted. Who would? So he did some reading and decided to come to a large academic hospital an hour away for a second opinion.
I interviewed him and then scrolled through his CT scans outside the room. There were a few things we could do, the attending and I discussed. We would send his tumor for genetic testing to see if there were any cancer mutations that could be targeted with drugs more specific than standard chemotherapy. We would also refer him to our cancer genetics clinic to get his blood tested for inherited mutations.
But mostly, all of that would likely turn up negative. Mostly, we agreed with his local oncologist.
We went back in the room. Explaining the genetic testing took the length of the visit because this is not a straightforward concept. We explained the difference between tumor mutations and inherited mutations. We wrote down a list of genetic variations we could discover. We discussed treatment options that could go along with each.
Do you have any questions?
He broke down. He reached for the tissue box sitting on the exam room table. “I feel so much better,” he said. “This is why I came here.” He felt safe, reassured, and hopeful.
I was happy to be helpful, but later, as I wrote my clinic note about him, I felt uneasy about the visit.
Everything we said was true. But somehow, it still felt as though we left him with an overly optimistic view of his illness. Did our emphasis on what could be done overshadow that it was unlikely to change the big picture? Did our in-depth discussion of slim possibilities mask that his prognosis was, in fact, still grim?
Working at a large academic medical center, I see many patients who come for a second opinion. I’m incredibly fortunate to learn at a place that is not just up to date in the most cutting-edge treatments but often leading in innovation.
And so we offer patients these options. They sound novel and exciting. They fill patients with hope because they fill the field with hope. I, too, get enraptured with the possibilities – circulating tumor DNA and clinical trials and targeted therapies.
At big cancer meetings every year, oncologists come together and speak about cancer therapies with enthusiasm and hope. Advances have exploded; it’s an exciting time to be learning and practicing.
And yet, the reality for many patients is very different. We are still discussing hospice after one line of chemotherapy has failed. We are still gently holding hands and saying that we have no more options to treat their aggressive cancers.
How can both of these worlds coexist? How can both be true?
A few years ago, a friend was diagnosed with a devastating neurologic condition. I went to a clinical trials website and typed in her disease. Immediately, hundreds of options popped up. I felt hopeful. The field is moving forward, I thought. There are options.
But in the exam room, there were none. When I asked about what I had read, the neurologist explained how many of these possibilities were being investigated. But in the end, my friend really had no good options.
After my visit with Mr. M, I thought about how commonly this story plays out in my field of hematology and oncology. Yes, there are instances in which we find a mutation that drastically changes management. It’s wonderful to witness: patients handed an ominous diagnosis and then living their normal lives, in remission or with stable disease, years later.
We all hope for that. But we rarely get it. The challenge comes when we spend 95% of a visit talking about something with a 1% chance of working. The numbers don’t add up – it’s an equation that easily results in false understanding. Cancer can be glossed with a veneer of innovative options, obscuring the reality that none are likely to work.
Weaving both truths into the conversation is a difficult skill, but one I decided to be more cognizant of after my encounter with Mr. M.
At our next visit, we were still waiting on the test results. But I decided to speak with him candidly. It’s important to have a plan B, I said, and asked what would be important to him if his time were limited. He nodded, thinking about this. “I’ve just been holding out hope for the mutation,” he admitted.
The next week his genetic testing came back negative, and he decided to get palliative chemotherapy closer to home. He had no reason to come to a large academic hospital anymore. With nothing special to offer him, I never saw him again.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz and listen to her each week on the Blood & Cancer podcast.
HHS proposes pathways for drug importation
Officials at the U.S. Department of Health and Human Services have announced a new plan that they say would lay the foundation for safe importation of certain medications, with the aim of expanding drug access and lowering prescription costs for patients.
The action plan, unveiled July 31, outlines two pathways for drug importation from foreign markets. The first route would authorize states, wholesalers, or pharmacists to propose pilot demonstrations on how they would import drugs from Canada into the United States, provided these are versions of drugs already approved by the Food and Drug Administration. Similarly, a second pathway would allow manufacturers that sell in foreign countries the opportunity to import drugs that are versions of FDA-approved medications.
HHS Secretary Alex M. Azar II said the action plan is part of President Trump’s drug-pricing blueprint and is intended to combat the sky-high price tags on many prescription medications.
“President Trump has been clear: For too long American patients have been paying exorbitantly high prices for prescription drugs that are made available to other countries at lower prices,” Mr. Azar said in a statement. “[The] announcement outlines the pathways the administration intends to explore to allow safe importation of certain prescription drugs to lower prices and reduce out of pocket costs for American patients. This is the next important step in the administration’s work to end foreign freeloading and put American patients first.”
Under the first pathway, HHS would review plans submitted by states, pharmacists, or drugmakers that outline how the entities would import Health Canada–approved drugs that are in compliance with the federal Food, Drug, and Cosmetic Act. The importation would occur in a manner that assures the drug’s validity and meets the cost requirements of federal rule making, according to an HHS fact sheet.
Demonstration projects would be time-limited and require regular reporting to ensure safety and cost conditions are being met.
Under the second pathway, manufacturers of FDA-approved drug products would be able to import versions of those drugs that they sell in foreign countries through a special process to be outlined by the agency. As part of the process, drugmakers would need to establish that the foreign version is the same as the U.S. version. The FDA would then allow the drug to be labeled for sale in the U.S. and imported, according to the fact sheet. HHS officials said they believe that manufacturers would use this pathway to offer U.S. patients lower-cost versions of their drugs and the medications affected could potentially include those used to treat diabetes, rheumatoid arthritis, cardiovascular disorders, and cancer.
“In recent years, multiple manufacturers have stated (either publicly or in statements to the Administration) that they wanted to offer lower cost versions but could not readily do so because they were locked into contracts with other parties in the supply chain,” HHS officials stated in the fact sheet. “This pathway would highlight an opportunity for manufacturers to use importation to offer lower-cost versions of their drugs.”
HHS plans to introduce its action plan through a formal notice of proposed rulemaking, which has not yet been finalized. Some elements of the final proposal may differ from its initial descriptions to reflect further consideration of the relevant issues, the agency noted.
Acting FDA Commissioner Ned Sharpless, MD, said the agency has a unique role to play in promoting competition that can help reduce drug prices and improve access to medicine for Americans.
“Driving down drug prices requires a comprehensive approach and we must continue to look at all innovative solutions to this challenge,” Dr. Sharpless said in a statement. “[The] proposal is the result of the hard work by the dedicated staff of the FDA, in close collaboration with HHS and the White House, to identify potential pathways we can pursue to support the safe importation of certain prescription drugs.”
Sen. Lamar Alexander (R-Tenn.), chair of the Health, Education, Labor and Pensions committee, said the administration’s proposal sounds promising as long as the plan ensures the safety and efficacy of imported medications.
“This is the first administration to take concrete steps to allow importation of prescription drugs to reduce their cost and I welcome it,” Sen. Alexander said in a statement. “The key for me is whether this plan preserves the Food and Drug Administration’s gold standard for safety and effectiveness. Millions of Americans every day buy prescription drugs relying on the FDA’s guarantee of quality.”
Officials at the U.S. Department of Health and Human Services have announced a new plan that they say would lay the foundation for safe importation of certain medications, with the aim of expanding drug access and lowering prescription costs for patients.
The action plan, unveiled July 31, outlines two pathways for drug importation from foreign markets. The first route would authorize states, wholesalers, or pharmacists to propose pilot demonstrations on how they would import drugs from Canada into the United States, provided these are versions of drugs already approved by the Food and Drug Administration. Similarly, a second pathway would allow manufacturers that sell in foreign countries the opportunity to import drugs that are versions of FDA-approved medications.
HHS Secretary Alex M. Azar II said the action plan is part of President Trump’s drug-pricing blueprint and is intended to combat the sky-high price tags on many prescription medications.
“President Trump has been clear: For too long American patients have been paying exorbitantly high prices for prescription drugs that are made available to other countries at lower prices,” Mr. Azar said in a statement. “[The] announcement outlines the pathways the administration intends to explore to allow safe importation of certain prescription drugs to lower prices and reduce out of pocket costs for American patients. This is the next important step in the administration’s work to end foreign freeloading and put American patients first.”
Under the first pathway, HHS would review plans submitted by states, pharmacists, or drugmakers that outline how the entities would import Health Canada–approved drugs that are in compliance with the federal Food, Drug, and Cosmetic Act. The importation would occur in a manner that assures the drug’s validity and meets the cost requirements of federal rule making, according to an HHS fact sheet.
Demonstration projects would be time-limited and require regular reporting to ensure safety and cost conditions are being met.
Under the second pathway, manufacturers of FDA-approved drug products would be able to import versions of those drugs that they sell in foreign countries through a special process to be outlined by the agency. As part of the process, drugmakers would need to establish that the foreign version is the same as the U.S. version. The FDA would then allow the drug to be labeled for sale in the U.S. and imported, according to the fact sheet. HHS officials said they believe that manufacturers would use this pathway to offer U.S. patients lower-cost versions of their drugs and the medications affected could potentially include those used to treat diabetes, rheumatoid arthritis, cardiovascular disorders, and cancer.
“In recent years, multiple manufacturers have stated (either publicly or in statements to the Administration) that they wanted to offer lower cost versions but could not readily do so because they were locked into contracts with other parties in the supply chain,” HHS officials stated in the fact sheet. “This pathway would highlight an opportunity for manufacturers to use importation to offer lower-cost versions of their drugs.”
HHS plans to introduce its action plan through a formal notice of proposed rulemaking, which has not yet been finalized. Some elements of the final proposal may differ from its initial descriptions to reflect further consideration of the relevant issues, the agency noted.
Acting FDA Commissioner Ned Sharpless, MD, said the agency has a unique role to play in promoting competition that can help reduce drug prices and improve access to medicine for Americans.
“Driving down drug prices requires a comprehensive approach and we must continue to look at all innovative solutions to this challenge,” Dr. Sharpless said in a statement. “[The] proposal is the result of the hard work by the dedicated staff of the FDA, in close collaboration with HHS and the White House, to identify potential pathways we can pursue to support the safe importation of certain prescription drugs.”
Sen. Lamar Alexander (R-Tenn.), chair of the Health, Education, Labor and Pensions committee, said the administration’s proposal sounds promising as long as the plan ensures the safety and efficacy of imported medications.
“This is the first administration to take concrete steps to allow importation of prescription drugs to reduce their cost and I welcome it,” Sen. Alexander said in a statement. “The key for me is whether this plan preserves the Food and Drug Administration’s gold standard for safety and effectiveness. Millions of Americans every day buy prescription drugs relying on the FDA’s guarantee of quality.”
Officials at the U.S. Department of Health and Human Services have announced a new plan that they say would lay the foundation for safe importation of certain medications, with the aim of expanding drug access and lowering prescription costs for patients.
The action plan, unveiled July 31, outlines two pathways for drug importation from foreign markets. The first route would authorize states, wholesalers, or pharmacists to propose pilot demonstrations on how they would import drugs from Canada into the United States, provided these are versions of drugs already approved by the Food and Drug Administration. Similarly, a second pathway would allow manufacturers that sell in foreign countries the opportunity to import drugs that are versions of FDA-approved medications.
HHS Secretary Alex M. Azar II said the action plan is part of President Trump’s drug-pricing blueprint and is intended to combat the sky-high price tags on many prescription medications.
“President Trump has been clear: For too long American patients have been paying exorbitantly high prices for prescription drugs that are made available to other countries at lower prices,” Mr. Azar said in a statement. “[The] announcement outlines the pathways the administration intends to explore to allow safe importation of certain prescription drugs to lower prices and reduce out of pocket costs for American patients. This is the next important step in the administration’s work to end foreign freeloading and put American patients first.”
Under the first pathway, HHS would review plans submitted by states, pharmacists, or drugmakers that outline how the entities would import Health Canada–approved drugs that are in compliance with the federal Food, Drug, and Cosmetic Act. The importation would occur in a manner that assures the drug’s validity and meets the cost requirements of federal rule making, according to an HHS fact sheet.
Demonstration projects would be time-limited and require regular reporting to ensure safety and cost conditions are being met.
Under the second pathway, manufacturers of FDA-approved drug products would be able to import versions of those drugs that they sell in foreign countries through a special process to be outlined by the agency. As part of the process, drugmakers would need to establish that the foreign version is the same as the U.S. version. The FDA would then allow the drug to be labeled for sale in the U.S. and imported, according to the fact sheet. HHS officials said they believe that manufacturers would use this pathway to offer U.S. patients lower-cost versions of their drugs and the medications affected could potentially include those used to treat diabetes, rheumatoid arthritis, cardiovascular disorders, and cancer.
“In recent years, multiple manufacturers have stated (either publicly or in statements to the Administration) that they wanted to offer lower cost versions but could not readily do so because they were locked into contracts with other parties in the supply chain,” HHS officials stated in the fact sheet. “This pathway would highlight an opportunity for manufacturers to use importation to offer lower-cost versions of their drugs.”
HHS plans to introduce its action plan through a formal notice of proposed rulemaking, which has not yet been finalized. Some elements of the final proposal may differ from its initial descriptions to reflect further consideration of the relevant issues, the agency noted.
Acting FDA Commissioner Ned Sharpless, MD, said the agency has a unique role to play in promoting competition that can help reduce drug prices and improve access to medicine for Americans.
“Driving down drug prices requires a comprehensive approach and we must continue to look at all innovative solutions to this challenge,” Dr. Sharpless said in a statement. “[The] proposal is the result of the hard work by the dedicated staff of the FDA, in close collaboration with HHS and the White House, to identify potential pathways we can pursue to support the safe importation of certain prescription drugs.”
Sen. Lamar Alexander (R-Tenn.), chair of the Health, Education, Labor and Pensions committee, said the administration’s proposal sounds promising as long as the plan ensures the safety and efficacy of imported medications.
“This is the first administration to take concrete steps to allow importation of prescription drugs to reduce their cost and I welcome it,” Sen. Alexander said in a statement. “The key for me is whether this plan preserves the Food and Drug Administration’s gold standard for safety and effectiveness. Millions of Americans every day buy prescription drugs relying on the FDA’s guarantee of quality.”
Lichenoid dermatitis with mycosis fungoides features linked to checkpoint inhibitor therapy
A patient treated with immune checkpoint inhibitor therapy for thyroid carcinoma presented with lichenoid dermatitis that resembled mycosis fungoides and also showed with monoclonal T-cell receptor gene rearrangement.
A case report published in the Journal of Cutaneous Pathology describes the “unusual” case and highlights another form of lichenoid dermatitis that may occur with immune checkpoint inhibitor therapy.
The patient was a 66-year-old man with BRAFV600E-mutated anaplastic thyroid carcinoma, who was enrolled in a clinical trial of the checkpoint inhibitor atezolizumab, in combination with the BRAF inhibitor vemurafenib and MEK inhibitor cobimetinib.
Around 11 months after starting treatment, he presented to a dermatology department with a 1.5-cm x 1.2-cm crusted, erythematous plaque on his abdomen that had appeared 3 weeks earlier. He also had several follicular-based erythematous papules on his extremities and a single verrucous papule on his index finger, which the authors wrote were likely associated with the vemurafenib therapy.
The patient had previously had a squamous cell carcinoma removed but had no history of cutaneous lymphoma.
A punch biopsy of the abdominal lesion showed dense lichenoid, lymphohistiocytic infiltrate with papillary dermal fibrosis, and scattered multinucleated giant histiocytes. Immunohistochemical studies showed the lesion had an abnormal immunophenotype in which CD4+ cells were four to five times more common than CD8+ cells, and there was partial loss of CD7 expression.
The lesion was treated with 0.05% clobetasol cream and monitored without interrupting the cancer therapy. The lesion gradually reduced in size, but 4 months later, another lesion appeared on the patient’s right clavicle.
A skin biopsy revealed lichenoid lymphohistiocytic infiltrate with occasional giant cells in the superficial dermis, as well as atypical, hyperchromatic lymphocytes with clear halos. Immunohistochemical studies showed that the new lesion was similar to the earlier abdominal lesion.
T-cell receptor gene rearrangement studies on both lesions showed that the abdominal lesion had both monoclonal TCR-gamma and TCR-beta gene rearrangements. The clavicle lesion showed the same monoclonal TCR-gamma rearrangement as the abdominal lesion, but lacked the TCR-beta gene rearrangement.
The lesions continued to be treated with clobetasol cream (0.05%), and the patient remained on the anticancer treatment regimen.
Michael T. Tetzlaff, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and coauthors wrote that up to half of all patients treated with immune checkpoint inhibitors develop some kind of cutaneous immune-related adverse event, and lichenoid dermatitis is one of the most common seen in biopsies.
“Clinical and pathological recognition of monoclonal [lichenoid dermatitis associated with immune checkpoint inhibitors] in the context of [immune checkpoint inhibitor] therapy will be important for accurate diagnosis and patient care,” they wrote.
The researchers did not report financial disclosures.
SOURCE: Tetzlaff MT et al. J Cutan Pathol. 2019 Jun 29. doi: 10.1111/cup.13536.
A patient treated with immune checkpoint inhibitor therapy for thyroid carcinoma presented with lichenoid dermatitis that resembled mycosis fungoides and also showed with monoclonal T-cell receptor gene rearrangement.
A case report published in the Journal of Cutaneous Pathology describes the “unusual” case and highlights another form of lichenoid dermatitis that may occur with immune checkpoint inhibitor therapy.
The patient was a 66-year-old man with BRAFV600E-mutated anaplastic thyroid carcinoma, who was enrolled in a clinical trial of the checkpoint inhibitor atezolizumab, in combination with the BRAF inhibitor vemurafenib and MEK inhibitor cobimetinib.
Around 11 months after starting treatment, he presented to a dermatology department with a 1.5-cm x 1.2-cm crusted, erythematous plaque on his abdomen that had appeared 3 weeks earlier. He also had several follicular-based erythematous papules on his extremities and a single verrucous papule on his index finger, which the authors wrote were likely associated with the vemurafenib therapy.
The patient had previously had a squamous cell carcinoma removed but had no history of cutaneous lymphoma.
A punch biopsy of the abdominal lesion showed dense lichenoid, lymphohistiocytic infiltrate with papillary dermal fibrosis, and scattered multinucleated giant histiocytes. Immunohistochemical studies showed the lesion had an abnormal immunophenotype in which CD4+ cells were four to five times more common than CD8+ cells, and there was partial loss of CD7 expression.
The lesion was treated with 0.05% clobetasol cream and monitored without interrupting the cancer therapy. The lesion gradually reduced in size, but 4 months later, another lesion appeared on the patient’s right clavicle.
A skin biopsy revealed lichenoid lymphohistiocytic infiltrate with occasional giant cells in the superficial dermis, as well as atypical, hyperchromatic lymphocytes with clear halos. Immunohistochemical studies showed that the new lesion was similar to the earlier abdominal lesion.
T-cell receptor gene rearrangement studies on both lesions showed that the abdominal lesion had both monoclonal TCR-gamma and TCR-beta gene rearrangements. The clavicle lesion showed the same monoclonal TCR-gamma rearrangement as the abdominal lesion, but lacked the TCR-beta gene rearrangement.
The lesions continued to be treated with clobetasol cream (0.05%), and the patient remained on the anticancer treatment regimen.
Michael T. Tetzlaff, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and coauthors wrote that up to half of all patients treated with immune checkpoint inhibitors develop some kind of cutaneous immune-related adverse event, and lichenoid dermatitis is one of the most common seen in biopsies.
“Clinical and pathological recognition of monoclonal [lichenoid dermatitis associated with immune checkpoint inhibitors] in the context of [immune checkpoint inhibitor] therapy will be important for accurate diagnosis and patient care,” they wrote.
The researchers did not report financial disclosures.
SOURCE: Tetzlaff MT et al. J Cutan Pathol. 2019 Jun 29. doi: 10.1111/cup.13536.
A patient treated with immune checkpoint inhibitor therapy for thyroid carcinoma presented with lichenoid dermatitis that resembled mycosis fungoides and also showed with monoclonal T-cell receptor gene rearrangement.
A case report published in the Journal of Cutaneous Pathology describes the “unusual” case and highlights another form of lichenoid dermatitis that may occur with immune checkpoint inhibitor therapy.
The patient was a 66-year-old man with BRAFV600E-mutated anaplastic thyroid carcinoma, who was enrolled in a clinical trial of the checkpoint inhibitor atezolizumab, in combination with the BRAF inhibitor vemurafenib and MEK inhibitor cobimetinib.
Around 11 months after starting treatment, he presented to a dermatology department with a 1.5-cm x 1.2-cm crusted, erythematous plaque on his abdomen that had appeared 3 weeks earlier. He also had several follicular-based erythematous papules on his extremities and a single verrucous papule on his index finger, which the authors wrote were likely associated with the vemurafenib therapy.
The patient had previously had a squamous cell carcinoma removed but had no history of cutaneous lymphoma.
A punch biopsy of the abdominal lesion showed dense lichenoid, lymphohistiocytic infiltrate with papillary dermal fibrosis, and scattered multinucleated giant histiocytes. Immunohistochemical studies showed the lesion had an abnormal immunophenotype in which CD4+ cells were four to five times more common than CD8+ cells, and there was partial loss of CD7 expression.
The lesion was treated with 0.05% clobetasol cream and monitored without interrupting the cancer therapy. The lesion gradually reduced in size, but 4 months later, another lesion appeared on the patient’s right clavicle.
A skin biopsy revealed lichenoid lymphohistiocytic infiltrate with occasional giant cells in the superficial dermis, as well as atypical, hyperchromatic lymphocytes with clear halos. Immunohistochemical studies showed that the new lesion was similar to the earlier abdominal lesion.
T-cell receptor gene rearrangement studies on both lesions showed that the abdominal lesion had both monoclonal TCR-gamma and TCR-beta gene rearrangements. The clavicle lesion showed the same monoclonal TCR-gamma rearrangement as the abdominal lesion, but lacked the TCR-beta gene rearrangement.
The lesions continued to be treated with clobetasol cream (0.05%), and the patient remained on the anticancer treatment regimen.
Michael T. Tetzlaff, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, and coauthors wrote that up to half of all patients treated with immune checkpoint inhibitors develop some kind of cutaneous immune-related adverse event, and lichenoid dermatitis is one of the most common seen in biopsies.
“Clinical and pathological recognition of monoclonal [lichenoid dermatitis associated with immune checkpoint inhibitors] in the context of [immune checkpoint inhibitor] therapy will be important for accurate diagnosis and patient care,” they wrote.
The researchers did not report financial disclosures.
SOURCE: Tetzlaff MT et al. J Cutan Pathol. 2019 Jun 29. doi: 10.1111/cup.13536.
FROM THE JOURNAL OF CUTANEOUS PATHOLOGY
Key clinical point:
Major finding: Checkpoint inhibitor therapy can trigger lichenoid dermatitis with mycosis fungoides–like features.
Study details: A case report involving a 66-year-old man with BRAFV600E-mutated anaplastic thyroid carcinoma.
Disclosures: The researchers did not report financial disclosures.
Source: Tetzlaff MT et al. J Cutan Pathol. 2019 Jun 29. doi: 10.1111/cup.13536.