User login
Palonosetron and netupitant for prevention of chemotherapy-induced nausea and vomiting
The US Food and Drug Administration (FDA) recently approved NEPA, an oral fixed-dose combination of netupitant and palonosetron for treatment of chemotherapy-induced nausea and vomiting (CINV). Palonosetron is a pharmacologically distinct, best-in-class serotonin (5-hydroxytryptamine) type 3 (5-HT3) receptor antagonist, which prevents CINV during the acute phase (0-24 h) after administration of chemotherapy, and netupitant is a potent and selective neurokinin-1 (NK-1) receptor antagonist, which prevents CINV during both the acute and delayed (25-120 h) phases. The 2 agents have also been shown potentially to act synergistically in inhibiting NK-1 receptor activity.
Click on the PDF icon at the top of this introduction to read the full article.
The US Food and Drug Administration (FDA) recently approved NEPA, an oral fixed-dose combination of netupitant and palonosetron for treatment of chemotherapy-induced nausea and vomiting (CINV). Palonosetron is a pharmacologically distinct, best-in-class serotonin (5-hydroxytryptamine) type 3 (5-HT3) receptor antagonist, which prevents CINV during the acute phase (0-24 h) after administration of chemotherapy, and netupitant is a potent and selective neurokinin-1 (NK-1) receptor antagonist, which prevents CINV during both the acute and delayed (25-120 h) phases. The 2 agents have also been shown potentially to act synergistically in inhibiting NK-1 receptor activity.
Click on the PDF icon at the top of this introduction to read the full article.
The US Food and Drug Administration (FDA) recently approved NEPA, an oral fixed-dose combination of netupitant and palonosetron for treatment of chemotherapy-induced nausea and vomiting (CINV). Palonosetron is a pharmacologically distinct, best-in-class serotonin (5-hydroxytryptamine) type 3 (5-HT3) receptor antagonist, which prevents CINV during the acute phase (0-24 h) after administration of chemotherapy, and netupitant is a potent and selective neurokinin-1 (NK-1) receptor antagonist, which prevents CINV during both the acute and delayed (25-120 h) phases. The 2 agents have also been shown potentially to act synergistically in inhibiting NK-1 receptor activity.
Click on the PDF icon at the top of this introduction to read the full article.
Managing change in oncology
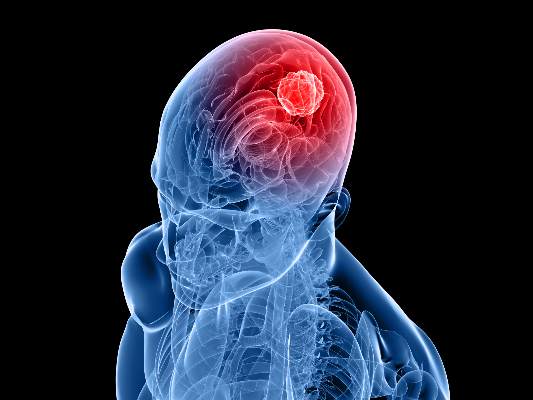
Alzheimer’s drug improves cognitive function after RT for brain tumors
Adult brain tumor survivors taking donepezil, a drug approved for the treatment of Alzheimer’s disease, showed significant improvements in the cognitive functions of memory, motor speed, and dexterity, compared with those taking a placebo. However, improvements in the primary outcome of composite cognitive function were similar for the two arms, investigators reported.
The study results were published online April 20 in the Journal of Clinical Oncology.
Patients with greater pretreatment deficits saw greater improvements in cognitive functioning with donepezil treatment, reported Stephen Rapp, Ph.D., professor of psychiatry and behavioral medicine at Wake Forest School of Medicine, Winston-Salem, N.C., and associates.
“This suggests that treatment with a daily dose of donepezil can provide benefit to some adult long-term brain tumor survivors after PBI or WBI [partial- or whole-brain irradiation], particularly those with greater pretreatment cognitive impairment,” they wrote (J. Clin. Oncol. 2015 Apr. 20 [doi: 10.1200/JCO.2014.58.4508]).
The phase III trial enrolled 198 primary or metastatic brain tumor survivors who underwent fractionated PBI or WBI at least 6 months previously. Patients received either donepezil at 5 mg daily for 6 weeks, followed by 10 mg daily for 18 weeks if well tolerated, or placebo for 24 weeks. Composite cognitive scores improved for both arms and did not differ significantly. Donepezil treatment resulted in significantly greater improvements in memory (recognition, P = .027; discrimination, P = .007) and motor speed and dexterity (P = .016).
Donepezil was generally well tolerated, except for diarrhea in 25% of the active arm vs. 9% in the placebo arm (P = .005). The study retention rate was 74% at 24 weeks for both groups.
Although enrolled patients had a high level of cognitive impairment relative to noncancer controls, with 91% having at least one test score at least 1.5 standard deviations below the normal comparison group, scores across most measures varied widely from significantly lower to higher than the comparison group. This heterogeneity may underlie the less than significant improvement observed with the study treatment. Patients with greater cognitive deficits saw greater benefits.
“This indicates that brain tumors and their treatments, including cranial irradiation, are associated with clinically significant cognitive impairment among some but not all patients. In future studies, demonstrable cognitive impairment should be an inclusion criterion for enrollment,” Dr. Rapp and associates wrote.
The study by Rapp et al. suggests that for brain tumor survivors experiencing cognitive difficulties, intervention with donepezil, a drug approved for use in Alzheimer’s disease (AD), may be helpful. Although average improvements were small, the trial indicates clear benefit for some patients, especially those most impaired. The study followed patients taking the drug for 6 months, but patients who responded to treatment likely will continue with lifelong therapy, based on experience with donepezil in AD. After cessation of the agent, neurocognitive function of treated AD patients declined to the level of untreated patients.
The results of the current study justify administering the drug to affected patients and monitoring for effects. In the absence of evidence of clinical benefit, the data do not support continuing treatment. Donepezil use in AD is continued for some patients even without signs of improvement, on the basis of slowing expected decline. However, cognitive declines due to tumor and treatment injury do not progress over time, and donepezil use in this population is supported only with evidence of benefit.
Optimal dosing for cancer patients requires further study, but studies with AD patients showed no clear benefit of dose escalation that outweighed GI adverse effects.
Maintaining maximal cognitive functioning in patients who often begin treatment with brain injury due to the tumor and unrelated illnesses, requires first the prevention of further damage. Strategies include functional image-guided surgery, limiting daily radiation fraction size, improved image-guided radiotherapy target definition, highly conformal radiotherapy administration techniques, and highly focused stereotactic radiosurgery in place of whole-brain radiotherapy for many patients with brain metastasis. Research on improvements in imaging of tumor and functional brain to better guide surgery and radiation is worthwhile.
Neurocognitive rehabilitation is recommended for patients with cognitive deficits that persist after therapy had ended. A recent randomized study showed clear benefit of rehabilitation for attention, verbal memory, and mental fatigue.
By taking steps to prevent injury, rehabilitate patients with deficits, and administer drug therapies while monitoring for benefit, improvements to cognitive function in brain tumor survivors may begin to increase. To best employ these strategies, a validated, easy-to-use instrument that measures mild to moderate impairment is needed for routine oncology practice.
Dr. Lawrence Kleinberg is associate professor of radiation oncology and molecular radiation sciences at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore. These comments were excerpted from the editorial accompanying the report by Dr. Rapp et al. (J. Clin. Oncol. 2015 April 20 [doi: 10.1200/JCO.2014.60.2805]).
The study by Rapp et al. suggests that for brain tumor survivors experiencing cognitive difficulties, intervention with donepezil, a drug approved for use in Alzheimer’s disease (AD), may be helpful. Although average improvements were small, the trial indicates clear benefit for some patients, especially those most impaired. The study followed patients taking the drug for 6 months, but patients who responded to treatment likely will continue with lifelong therapy, based on experience with donepezil in AD. After cessation of the agent, neurocognitive function of treated AD patients declined to the level of untreated patients.
The results of the current study justify administering the drug to affected patients and monitoring for effects. In the absence of evidence of clinical benefit, the data do not support continuing treatment. Donepezil use in AD is continued for some patients even without signs of improvement, on the basis of slowing expected decline. However, cognitive declines due to tumor and treatment injury do not progress over time, and donepezil use in this population is supported only with evidence of benefit.
Optimal dosing for cancer patients requires further study, but studies with AD patients showed no clear benefit of dose escalation that outweighed GI adverse effects.
Maintaining maximal cognitive functioning in patients who often begin treatment with brain injury due to the tumor and unrelated illnesses, requires first the prevention of further damage. Strategies include functional image-guided surgery, limiting daily radiation fraction size, improved image-guided radiotherapy target definition, highly conformal radiotherapy administration techniques, and highly focused stereotactic radiosurgery in place of whole-brain radiotherapy for many patients with brain metastasis. Research on improvements in imaging of tumor and functional brain to better guide surgery and radiation is worthwhile.
Neurocognitive rehabilitation is recommended for patients with cognitive deficits that persist after therapy had ended. A recent randomized study showed clear benefit of rehabilitation for attention, verbal memory, and mental fatigue.
By taking steps to prevent injury, rehabilitate patients with deficits, and administer drug therapies while monitoring for benefit, improvements to cognitive function in brain tumor survivors may begin to increase. To best employ these strategies, a validated, easy-to-use instrument that measures mild to moderate impairment is needed for routine oncology practice.
Dr. Lawrence Kleinberg is associate professor of radiation oncology and molecular radiation sciences at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore. These comments were excerpted from the editorial accompanying the report by Dr. Rapp et al. (J. Clin. Oncol. 2015 April 20 [doi: 10.1200/JCO.2014.60.2805]).
The study by Rapp et al. suggests that for brain tumor survivors experiencing cognitive difficulties, intervention with donepezil, a drug approved for use in Alzheimer’s disease (AD), may be helpful. Although average improvements were small, the trial indicates clear benefit for some patients, especially those most impaired. The study followed patients taking the drug for 6 months, but patients who responded to treatment likely will continue with lifelong therapy, based on experience with donepezil in AD. After cessation of the agent, neurocognitive function of treated AD patients declined to the level of untreated patients.
The results of the current study justify administering the drug to affected patients and monitoring for effects. In the absence of evidence of clinical benefit, the data do not support continuing treatment. Donepezil use in AD is continued for some patients even without signs of improvement, on the basis of slowing expected decline. However, cognitive declines due to tumor and treatment injury do not progress over time, and donepezil use in this population is supported only with evidence of benefit.
Optimal dosing for cancer patients requires further study, but studies with AD patients showed no clear benefit of dose escalation that outweighed GI adverse effects.
Maintaining maximal cognitive functioning in patients who often begin treatment with brain injury due to the tumor and unrelated illnesses, requires first the prevention of further damage. Strategies include functional image-guided surgery, limiting daily radiation fraction size, improved image-guided radiotherapy target definition, highly conformal radiotherapy administration techniques, and highly focused stereotactic radiosurgery in place of whole-brain radiotherapy for many patients with brain metastasis. Research on improvements in imaging of tumor and functional brain to better guide surgery and radiation is worthwhile.
Neurocognitive rehabilitation is recommended for patients with cognitive deficits that persist after therapy had ended. A recent randomized study showed clear benefit of rehabilitation for attention, verbal memory, and mental fatigue.
By taking steps to prevent injury, rehabilitate patients with deficits, and administer drug therapies while monitoring for benefit, improvements to cognitive function in brain tumor survivors may begin to increase. To best employ these strategies, a validated, easy-to-use instrument that measures mild to moderate impairment is needed for routine oncology practice.
Dr. Lawrence Kleinberg is associate professor of radiation oncology and molecular radiation sciences at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore. These comments were excerpted from the editorial accompanying the report by Dr. Rapp et al. (J. Clin. Oncol. 2015 April 20 [doi: 10.1200/JCO.2014.60.2805]).
Adult brain tumor survivors taking donepezil, a drug approved for the treatment of Alzheimer’s disease, showed significant improvements in the cognitive functions of memory, motor speed, and dexterity, compared with those taking a placebo. However, improvements in the primary outcome of composite cognitive function were similar for the two arms, investigators reported.
The study results were published online April 20 in the Journal of Clinical Oncology.
Patients with greater pretreatment deficits saw greater improvements in cognitive functioning with donepezil treatment, reported Stephen Rapp, Ph.D., professor of psychiatry and behavioral medicine at Wake Forest School of Medicine, Winston-Salem, N.C., and associates.
“This suggests that treatment with a daily dose of donepezil can provide benefit to some adult long-term brain tumor survivors after PBI or WBI [partial- or whole-brain irradiation], particularly those with greater pretreatment cognitive impairment,” they wrote (J. Clin. Oncol. 2015 Apr. 20 [doi: 10.1200/JCO.2014.58.4508]).
The phase III trial enrolled 198 primary or metastatic brain tumor survivors who underwent fractionated PBI or WBI at least 6 months previously. Patients received either donepezil at 5 mg daily for 6 weeks, followed by 10 mg daily for 18 weeks if well tolerated, or placebo for 24 weeks. Composite cognitive scores improved for both arms and did not differ significantly. Donepezil treatment resulted in significantly greater improvements in memory (recognition, P = .027; discrimination, P = .007) and motor speed and dexterity (P = .016).
Donepezil was generally well tolerated, except for diarrhea in 25% of the active arm vs. 9% in the placebo arm (P = .005). The study retention rate was 74% at 24 weeks for both groups.
Although enrolled patients had a high level of cognitive impairment relative to noncancer controls, with 91% having at least one test score at least 1.5 standard deviations below the normal comparison group, scores across most measures varied widely from significantly lower to higher than the comparison group. This heterogeneity may underlie the less than significant improvement observed with the study treatment. Patients with greater cognitive deficits saw greater benefits.
“This indicates that brain tumors and their treatments, including cranial irradiation, are associated with clinically significant cognitive impairment among some but not all patients. In future studies, demonstrable cognitive impairment should be an inclusion criterion for enrollment,” Dr. Rapp and associates wrote.
Adult brain tumor survivors taking donepezil, a drug approved for the treatment of Alzheimer’s disease, showed significant improvements in the cognitive functions of memory, motor speed, and dexterity, compared with those taking a placebo. However, improvements in the primary outcome of composite cognitive function were similar for the two arms, investigators reported.
The study results were published online April 20 in the Journal of Clinical Oncology.
Patients with greater pretreatment deficits saw greater improvements in cognitive functioning with donepezil treatment, reported Stephen Rapp, Ph.D., professor of psychiatry and behavioral medicine at Wake Forest School of Medicine, Winston-Salem, N.C., and associates.
“This suggests that treatment with a daily dose of donepezil can provide benefit to some adult long-term brain tumor survivors after PBI or WBI [partial- or whole-brain irradiation], particularly those with greater pretreatment cognitive impairment,” they wrote (J. Clin. Oncol. 2015 Apr. 20 [doi: 10.1200/JCO.2014.58.4508]).
The phase III trial enrolled 198 primary or metastatic brain tumor survivors who underwent fractionated PBI or WBI at least 6 months previously. Patients received either donepezil at 5 mg daily for 6 weeks, followed by 10 mg daily for 18 weeks if well tolerated, or placebo for 24 weeks. Composite cognitive scores improved for both arms and did not differ significantly. Donepezil treatment resulted in significantly greater improvements in memory (recognition, P = .027; discrimination, P = .007) and motor speed and dexterity (P = .016).
Donepezil was generally well tolerated, except for diarrhea in 25% of the active arm vs. 9% in the placebo arm (P = .005). The study retention rate was 74% at 24 weeks for both groups.
Although enrolled patients had a high level of cognitive impairment relative to noncancer controls, with 91% having at least one test score at least 1.5 standard deviations below the normal comparison group, scores across most measures varied widely from significantly lower to higher than the comparison group. This heterogeneity may underlie the less than significant improvement observed with the study treatment. Patients with greater cognitive deficits saw greater benefits.
“This indicates that brain tumors and their treatments, including cranial irradiation, are associated with clinically significant cognitive impairment among some but not all patients. In future studies, demonstrable cognitive impairment should be an inclusion criterion for enrollment,” Dr. Rapp and associates wrote.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Among adult brain tumor survivors who underwent partial- or whole-brain irradiation, treatment with donepezil compared with placebo was associated with significant improvements in memory and motor speed and dexterity, but composite cognitive scores were similar.
Major finding: After 24 weeks of treatment, patients taking donepezil (vs. placebo) had significantly more improvement in memory (recognition, P = .027; discrimination, P = .007) and motor speed and dexterity (P = .016).
Data source: A double-blind phase III trial that randomized 198 patients who had undergone irradiation at least 6 months previously to receive donepezil (5 mg for 6 weeks followed by 10 mg for 18 weeks) or placebo (24 weeks).
Disclosures: Dr. Rapp reported having no financial disclosures.
Sleep disorders in patients with cancer
Sleep disturbances are common among patients with cancer for many reasons. Sleep problems can be present at any stage during treatment for cancer and in some patients, sleep disturbance may be the presenting symptoms that lead to the diagnosis of some types of cancer. Poor sleep impairs quality of life In people with cancer, but most do not specifically complain of sleep problems unless they are explicitly asked. Insomnia and fatigue are most common sleep disorders in this cohort, although primary sleep disorders, including obstructive sleep apnea and restless legs syndrome, which are common in the general population, have not been carefully studied in the oncology setting despite significant their impairment of quality of life.
Click on the PDF icon at the top of this introduction to read the full article.
disorder
Sleep disturbances are common among patients with cancer for many reasons. Sleep problems can be present at any stage during treatment for cancer and in some patients, sleep disturbance may be the presenting symptoms that lead to the diagnosis of some types of cancer. Poor sleep impairs quality of life In people with cancer, but most do not specifically complain of sleep problems unless they are explicitly asked. Insomnia and fatigue are most common sleep disorders in this cohort, although primary sleep disorders, including obstructive sleep apnea and restless legs syndrome, which are common in the general population, have not been carefully studied in the oncology setting despite significant their impairment of quality of life.
Click on the PDF icon at the top of this introduction to read the full article.
Sleep disturbances are common among patients with cancer for many reasons. Sleep problems can be present at any stage during treatment for cancer and in some patients, sleep disturbance may be the presenting symptoms that lead to the diagnosis of some types of cancer. Poor sleep impairs quality of life In people with cancer, but most do not specifically complain of sleep problems unless they are explicitly asked. Insomnia and fatigue are most common sleep disorders in this cohort, although primary sleep disorders, including obstructive sleep apnea and restless legs syndrome, which are common in the general population, have not been carefully studied in the oncology setting despite significant their impairment of quality of life.
Click on the PDF icon at the top of this introduction to read the full article.
disorder
disorder
SSIs a factor in postop colon cancer survival
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
AT SSO 2015
Key clinical point: Surgical site infections in patients with colon cancer are associated with both worse overall survival and lower chance of receiving adjuvant chemotherapy.
Major finding: Median overall survival for stage III patients with SSIs was 29 months, vs. 33 for no SSIs.
Data source: Retrospective cohort study of 9,946 patients who underwent radical colon cancer resection with curative intent.
Disclosures: The study was internally supported. Dr. Barden reported having no conflicts of interest.
Palliative surgery eases pain at end of life
HOUSTON – Palliative surgery can alleviate pain and improve the quality of life for patients dying from advanced cancers, without compromising performance status, a study showed.
Among 202 patients with stage III or IV cancers who underwent surgery with palliation as the goal, pain scores were significantly improved after surgery, while Karnofsky Performance Status (KPS) scores remained unchanged, said Dr. Anne Falor, a surgical oncology fellow at City of Hope in Duarte, Calif.
“Surgical oncology has not been historically involved in palliative care. If a patient is deemed unresectable, his or her treatment is often the purview of medical or radiation oncology,” she said at the annual Society of Surgical Oncology Cancer Symposium.
But for patients who are likely to have prolonged disease-free intervals, palliative surgery can be performed with low morbidity, she said.
Dr. Falor and her colleagues reviewed their center’s experience with palliative surgery in 2011, during which time 202 patients with a predicted 5-year survival of less than 5% underwent a total of 247 palliative procedures.
The patients had malignancies at various sites, including the large intestine, lung, stomach, breast, prostate, lymph nodes, esophagus, pancreas, and ovaries.
The primary indications for the procedure included dysphagia, pain/wound problems, dyspnea, nausea and vomiting, and dysuria.
Most of the patients (83%) had a single procedure, but 13% had two operations, 4% had three operations, 1% had four procedures, and 0.4% had five or more interventions.
The majority of procedures performed were endoscopic interventions characterized as minor in nature, followed by minor genitourinary and thoracic interventions, although a nearly equal proportion of thoracic interventions (about 28%) were major procedures such as diverting ostomy.
When the investigators looked at 30-day outcomes following palliative surgery, they found that only 13% of patients needed an urgent care visit, 2% required a triage call, 22% were readmitted, and 60% had an institutional supportive care referral.
Total 30-day morbidity of any kind was seen in 37% of patients; 15% of patients died within 30 days of surgery.
Looking at quality of life outcomes, the investigators found no differences in the percentage of patients with KPS scores from 80 to 100 between the presurgery and postsurgery periods (78% and 70%, respectively, P = ns).
There were significant improvements, however, in pain scores, which dropped by a mean of 1.2 points from the preoperative period to discharge (P < .0001), and decreased by 0.6 points before surgery to the first follow-up visit (P = .0037).
Dr. Falor said that it’s important for patients and their care team to have a discussion regarding expectations for surgery and the goals of care.
The study was internally funded. Dr. Falor reported having no conflicts of interest.
Over the past decade palliative surgery has been increasingly discussed and scrutinized, as the concept of palliative care has gained greater traction with medical professionals and the public. Not too long ago the designation “palliative” when applied to a surgical procedure had an apologetic connotation because the operation would fail to heal. In some cases the term was even used to describe positive tumor margins at the conclusion of a resection – something totally irrelevant when assessing the direct impact of the operation upon a patient’s self-designated symptoms.
Only recently has a more positive perspective emerged, helped by data such as these researchers have presented. Palliative surgery now is not failing to cure, but succeeding to comfort.
New perspectives, however, will raise new and necessary questions to better define the role of surgery in the greater context of relief of suffering in all its manifestations. In our wish to respond surgically to pain and other symptoms we must be vigilant against the temptation to “do something” when surgery for cure or palliation is unlikely to help in order to assuage our feelings of hopelessness. Hopelessness is not an indication for surgery – pain, obstruction, and saving life are. Indications for surgery must be more specific, as this article points out, and it is more likely to help with localized and pressing symptoms. A rule of thumb passed down to me from my surgeon grandfather who practiced in an era when the vast majority of operations were palliative, the more pressing and clear the indication for surgery, the better the result.
Dr. Geoffrey Dunn, an ACS Fellow based in Erie, Pa.
Over the past decade palliative surgery has been increasingly discussed and scrutinized, as the concept of palliative care has gained greater traction with medical professionals and the public. Not too long ago the designation “palliative” when applied to a surgical procedure had an apologetic connotation because the operation would fail to heal. In some cases the term was even used to describe positive tumor margins at the conclusion of a resection – something totally irrelevant when assessing the direct impact of the operation upon a patient’s self-designated symptoms.
Only recently has a more positive perspective emerged, helped by data such as these researchers have presented. Palliative surgery now is not failing to cure, but succeeding to comfort.
New perspectives, however, will raise new and necessary questions to better define the role of surgery in the greater context of relief of suffering in all its manifestations. In our wish to respond surgically to pain and other symptoms we must be vigilant against the temptation to “do something” when surgery for cure or palliation is unlikely to help in order to assuage our feelings of hopelessness. Hopelessness is not an indication for surgery – pain, obstruction, and saving life are. Indications for surgery must be more specific, as this article points out, and it is more likely to help with localized and pressing symptoms. A rule of thumb passed down to me from my surgeon grandfather who practiced in an era when the vast majority of operations were palliative, the more pressing and clear the indication for surgery, the better the result.
Dr. Geoffrey Dunn, an ACS Fellow based in Erie, Pa.
Over the past decade palliative surgery has been increasingly discussed and scrutinized, as the concept of palliative care has gained greater traction with medical professionals and the public. Not too long ago the designation “palliative” when applied to a surgical procedure had an apologetic connotation because the operation would fail to heal. In some cases the term was even used to describe positive tumor margins at the conclusion of a resection – something totally irrelevant when assessing the direct impact of the operation upon a patient’s self-designated symptoms.
Only recently has a more positive perspective emerged, helped by data such as these researchers have presented. Palliative surgery now is not failing to cure, but succeeding to comfort.
New perspectives, however, will raise new and necessary questions to better define the role of surgery in the greater context of relief of suffering in all its manifestations. In our wish to respond surgically to pain and other symptoms we must be vigilant against the temptation to “do something” when surgery for cure or palliation is unlikely to help in order to assuage our feelings of hopelessness. Hopelessness is not an indication for surgery – pain, obstruction, and saving life are. Indications for surgery must be more specific, as this article points out, and it is more likely to help with localized and pressing symptoms. A rule of thumb passed down to me from my surgeon grandfather who practiced in an era when the vast majority of operations were palliative, the more pressing and clear the indication for surgery, the better the result.
Dr. Geoffrey Dunn, an ACS Fellow based in Erie, Pa.
HOUSTON – Palliative surgery can alleviate pain and improve the quality of life for patients dying from advanced cancers, without compromising performance status, a study showed.
Among 202 patients with stage III or IV cancers who underwent surgery with palliation as the goal, pain scores were significantly improved after surgery, while Karnofsky Performance Status (KPS) scores remained unchanged, said Dr. Anne Falor, a surgical oncology fellow at City of Hope in Duarte, Calif.
“Surgical oncology has not been historically involved in palliative care. If a patient is deemed unresectable, his or her treatment is often the purview of medical or radiation oncology,” she said at the annual Society of Surgical Oncology Cancer Symposium.
But for patients who are likely to have prolonged disease-free intervals, palliative surgery can be performed with low morbidity, she said.
Dr. Falor and her colleagues reviewed their center’s experience with palliative surgery in 2011, during which time 202 patients with a predicted 5-year survival of less than 5% underwent a total of 247 palliative procedures.
The patients had malignancies at various sites, including the large intestine, lung, stomach, breast, prostate, lymph nodes, esophagus, pancreas, and ovaries.
The primary indications for the procedure included dysphagia, pain/wound problems, dyspnea, nausea and vomiting, and dysuria.
Most of the patients (83%) had a single procedure, but 13% had two operations, 4% had three operations, 1% had four procedures, and 0.4% had five or more interventions.
The majority of procedures performed were endoscopic interventions characterized as minor in nature, followed by minor genitourinary and thoracic interventions, although a nearly equal proportion of thoracic interventions (about 28%) were major procedures such as diverting ostomy.
When the investigators looked at 30-day outcomes following palliative surgery, they found that only 13% of patients needed an urgent care visit, 2% required a triage call, 22% were readmitted, and 60% had an institutional supportive care referral.
Total 30-day morbidity of any kind was seen in 37% of patients; 15% of patients died within 30 days of surgery.
Looking at quality of life outcomes, the investigators found no differences in the percentage of patients with KPS scores from 80 to 100 between the presurgery and postsurgery periods (78% and 70%, respectively, P = ns).
There were significant improvements, however, in pain scores, which dropped by a mean of 1.2 points from the preoperative period to discharge (P < .0001), and decreased by 0.6 points before surgery to the first follow-up visit (P = .0037).
Dr. Falor said that it’s important for patients and their care team to have a discussion regarding expectations for surgery and the goals of care.
The study was internally funded. Dr. Falor reported having no conflicts of interest.
HOUSTON – Palliative surgery can alleviate pain and improve the quality of life for patients dying from advanced cancers, without compromising performance status, a study showed.
Among 202 patients with stage III or IV cancers who underwent surgery with palliation as the goal, pain scores were significantly improved after surgery, while Karnofsky Performance Status (KPS) scores remained unchanged, said Dr. Anne Falor, a surgical oncology fellow at City of Hope in Duarte, Calif.
“Surgical oncology has not been historically involved in palliative care. If a patient is deemed unresectable, his or her treatment is often the purview of medical or radiation oncology,” she said at the annual Society of Surgical Oncology Cancer Symposium.
But for patients who are likely to have prolonged disease-free intervals, palliative surgery can be performed with low morbidity, she said.
Dr. Falor and her colleagues reviewed their center’s experience with palliative surgery in 2011, during which time 202 patients with a predicted 5-year survival of less than 5% underwent a total of 247 palliative procedures.
The patients had malignancies at various sites, including the large intestine, lung, stomach, breast, prostate, lymph nodes, esophagus, pancreas, and ovaries.
The primary indications for the procedure included dysphagia, pain/wound problems, dyspnea, nausea and vomiting, and dysuria.
Most of the patients (83%) had a single procedure, but 13% had two operations, 4% had three operations, 1% had four procedures, and 0.4% had five or more interventions.
The majority of procedures performed were endoscopic interventions characterized as minor in nature, followed by minor genitourinary and thoracic interventions, although a nearly equal proportion of thoracic interventions (about 28%) were major procedures such as diverting ostomy.
When the investigators looked at 30-day outcomes following palliative surgery, they found that only 13% of patients needed an urgent care visit, 2% required a triage call, 22% were readmitted, and 60% had an institutional supportive care referral.
Total 30-day morbidity of any kind was seen in 37% of patients; 15% of patients died within 30 days of surgery.
Looking at quality of life outcomes, the investigators found no differences in the percentage of patients with KPS scores from 80 to 100 between the presurgery and postsurgery periods (78% and 70%, respectively, P = ns).
There were significant improvements, however, in pain scores, which dropped by a mean of 1.2 points from the preoperative period to discharge (P < .0001), and decreased by 0.6 points before surgery to the first follow-up visit (P = .0037).
Dr. Falor said that it’s important for patients and their care team to have a discussion regarding expectations for surgery and the goals of care.
The study was internally funded. Dr. Falor reported having no conflicts of interest.
Key clinical point: Palliative surgery in patients with advanced cancers can relieve pain with minimal morbidity.
Major finding: Pain scores improved significantly from the pre- to postoperative periods, without a significant decline in performance status scores.
Data source: Case series of 202 patients with stage III or IV malignancies who underwent 247 palliative procedures.
Disclosures: The study was internally funded. Dr. Falor reported having no conflicts of interest.
More children surviving cancer, but they still face chronic conditions
The number of childhood cancer survivors has increased significantly since 2005, but the majority of survivors have some sort of morbidity, according to Dr. Siobhan M. Phillips of Northwestern University, Chicago, and her associates.
Investigators used cancer incidence and survival data from Surveillance, Epidemiology, and End Results registries, and data from the Childhood Cancer Survivor Study cohort that had information on potential adverse and late effects of cancer treatment from more than 14,000 long-term survivors of childhood cancers. There were nearly 590,000 childhood cancer survivors in the United States in 2011, an increase of about 60,000 from 2005. More than 80% had lived longer than 5 years post diagnosis. However, 70% of survivors had a mild to moderate chronic condition, with nearly a third having a severe, disabling, or life-threatening condition. The most common morbidity was neurocognitive dysfunction, Dr. Phillips and her associates reported.
“Our study findings highlight that a singular focus on curing cancer yields an incomplete picture of childhood cancer survivorship. The burden of chronic conditions in this population is profound, both in occurrence and severity. Efforts to understand how to effectively decrease morbidity burden and incorporate effective care coordination and rehabilitation models to optimize longevity and well-being in this population should be a priority,” Dr. Phillips said in a press release from the American Association for Cancer Research. Find the full study in Cancer Epidemiology, Biomarkers and Prevention (doi: 10.1158/1055-9965.EPI-14-1418).
The number of childhood cancer survivors has increased significantly since 2005, but the majority of survivors have some sort of morbidity, according to Dr. Siobhan M. Phillips of Northwestern University, Chicago, and her associates.
Investigators used cancer incidence and survival data from Surveillance, Epidemiology, and End Results registries, and data from the Childhood Cancer Survivor Study cohort that had information on potential adverse and late effects of cancer treatment from more than 14,000 long-term survivors of childhood cancers. There were nearly 590,000 childhood cancer survivors in the United States in 2011, an increase of about 60,000 from 2005. More than 80% had lived longer than 5 years post diagnosis. However, 70% of survivors had a mild to moderate chronic condition, with nearly a third having a severe, disabling, or life-threatening condition. The most common morbidity was neurocognitive dysfunction, Dr. Phillips and her associates reported.
“Our study findings highlight that a singular focus on curing cancer yields an incomplete picture of childhood cancer survivorship. The burden of chronic conditions in this population is profound, both in occurrence and severity. Efforts to understand how to effectively decrease morbidity burden and incorporate effective care coordination and rehabilitation models to optimize longevity and well-being in this population should be a priority,” Dr. Phillips said in a press release from the American Association for Cancer Research. Find the full study in Cancer Epidemiology, Biomarkers and Prevention (doi: 10.1158/1055-9965.EPI-14-1418).
The number of childhood cancer survivors has increased significantly since 2005, but the majority of survivors have some sort of morbidity, according to Dr. Siobhan M. Phillips of Northwestern University, Chicago, and her associates.
Investigators used cancer incidence and survival data from Surveillance, Epidemiology, and End Results registries, and data from the Childhood Cancer Survivor Study cohort that had information on potential adverse and late effects of cancer treatment from more than 14,000 long-term survivors of childhood cancers. There were nearly 590,000 childhood cancer survivors in the United States in 2011, an increase of about 60,000 from 2005. More than 80% had lived longer than 5 years post diagnosis. However, 70% of survivors had a mild to moderate chronic condition, with nearly a third having a severe, disabling, or life-threatening condition. The most common morbidity was neurocognitive dysfunction, Dr. Phillips and her associates reported.
“Our study findings highlight that a singular focus on curing cancer yields an incomplete picture of childhood cancer survivorship. The burden of chronic conditions in this population is profound, both in occurrence and severity. Efforts to understand how to effectively decrease morbidity burden and incorporate effective care coordination and rehabilitation models to optimize longevity and well-being in this population should be a priority,” Dr. Phillips said in a press release from the American Association for Cancer Research. Find the full study in Cancer Epidemiology, Biomarkers and Prevention (doi: 10.1158/1055-9965.EPI-14-1418).
Gynecologic cancers predict coexisting pelvic floor disorders
ORLANDO – Women diagnosed with a gynecologic malignancy have a strong likelihood of presenting with a coexisting pelvic floor disorder, according to data collected prospectively from a cancer survivorship cohort.
Bladder symptoms on validated questionnaires completed soon after diagnosis and prior to surgical treatment were especially common, with an overall urinary incontinence rate of 46.1% and a stress incontinence (SUI) rate of 59.5%, Dr. C. Emi Bretschneider reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“We think increased awareness of pelvic health issues will allow for more individualized and comprehensive counseling and care of these women,” said Dr. Bretschneider of the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill.
She identified pelvic floor disorders as a major potential source of diminished quality of life in women with gynecologic malignancies.
Dr. C. Bryce Bowling, a urogynecologist at the University of Tennessee, Knoxville, agreed. Although he observed that the risk of both pelvic floor disorders and gynecologic malignancies increase with age, he said the reported rates at which they coexist is “sobering.”
“These are important data for those who are not already aware of this relationship,” Dr. Bowling, a discussant invited by the Society of Gynecologic Surgeons, said in an interview.
At many institutions, including his own, screening for pelvic floor disorders in women with gynecologic malignancies is already routine.
“Screening for incontinence is a very important consideration even for those with a poor prognosis,” he said. “Control of urinary symptoms over the course of the woman’s survival will have a very positive impact on quality of life.”
The data on pelvic floor disorders was drawn from 154 women with gynecologic cancers who completed baseline evaluations of bowel and bladder symptoms using two validated questionnaires in a recent 10-month period. Most (62%) had endometrial cancer, but other cancers, such as ovarian (17%) and cervical (11%) were represented. There were no significant differences in the rates of pelvic floor disorders among the cancer types.
In addition to the substantial rates of urinary incontinence and SUI, 40.8% of patients reported urinary incontinence with urgency and 21.5% reported nocturia most or every night. The rate of enuresis was 7.2%. In addition, 3.9% reported fecal incontinence.
Complaints of abdominal pain (46.8%), constipation (42.2%), and diarrhea (20.1%) were also common, Dr. Bretschneider reported at the meeting, jointly sponsored by the American College of Surgeons.
When women older than 50 years were compared to younger women, the rates of nearly every indicator of a pelvic floor disorder were higher. Most differences, such as overall urinary incontinence (P = .009), SUI (P = .005), and abdominal pain (P = .002) had a high degree of statistical significance. However, overall urinary incontinence and SUI were not significantly associated with age when modeled as a continuous variable.
Recognizing pelvic floor disorders at the time of the diagnosis of gynecologic malignancy can be relevant to planning cancer treatment, according to Dr. Bretschnieder. The study results highlight the need for a proactive approach that includes screening at the time of diagnosis, she said.
ORLANDO – Women diagnosed with a gynecologic malignancy have a strong likelihood of presenting with a coexisting pelvic floor disorder, according to data collected prospectively from a cancer survivorship cohort.
Bladder symptoms on validated questionnaires completed soon after diagnosis and prior to surgical treatment were especially common, with an overall urinary incontinence rate of 46.1% and a stress incontinence (SUI) rate of 59.5%, Dr. C. Emi Bretschneider reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“We think increased awareness of pelvic health issues will allow for more individualized and comprehensive counseling and care of these women,” said Dr. Bretschneider of the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill.
She identified pelvic floor disorders as a major potential source of diminished quality of life in women with gynecologic malignancies.
Dr. C. Bryce Bowling, a urogynecologist at the University of Tennessee, Knoxville, agreed. Although he observed that the risk of both pelvic floor disorders and gynecologic malignancies increase with age, he said the reported rates at which they coexist is “sobering.”
“These are important data for those who are not already aware of this relationship,” Dr. Bowling, a discussant invited by the Society of Gynecologic Surgeons, said in an interview.
At many institutions, including his own, screening for pelvic floor disorders in women with gynecologic malignancies is already routine.
“Screening for incontinence is a very important consideration even for those with a poor prognosis,” he said. “Control of urinary symptoms over the course of the woman’s survival will have a very positive impact on quality of life.”
The data on pelvic floor disorders was drawn from 154 women with gynecologic cancers who completed baseline evaluations of bowel and bladder symptoms using two validated questionnaires in a recent 10-month period. Most (62%) had endometrial cancer, but other cancers, such as ovarian (17%) and cervical (11%) were represented. There were no significant differences in the rates of pelvic floor disorders among the cancer types.
In addition to the substantial rates of urinary incontinence and SUI, 40.8% of patients reported urinary incontinence with urgency and 21.5% reported nocturia most or every night. The rate of enuresis was 7.2%. In addition, 3.9% reported fecal incontinence.
Complaints of abdominal pain (46.8%), constipation (42.2%), and diarrhea (20.1%) were also common, Dr. Bretschneider reported at the meeting, jointly sponsored by the American College of Surgeons.
When women older than 50 years were compared to younger women, the rates of nearly every indicator of a pelvic floor disorder were higher. Most differences, such as overall urinary incontinence (P = .009), SUI (P = .005), and abdominal pain (P = .002) had a high degree of statistical significance. However, overall urinary incontinence and SUI were not significantly associated with age when modeled as a continuous variable.
Recognizing pelvic floor disorders at the time of the diagnosis of gynecologic malignancy can be relevant to planning cancer treatment, according to Dr. Bretschnieder. The study results highlight the need for a proactive approach that includes screening at the time of diagnosis, she said.
ORLANDO – Women diagnosed with a gynecologic malignancy have a strong likelihood of presenting with a coexisting pelvic floor disorder, according to data collected prospectively from a cancer survivorship cohort.
Bladder symptoms on validated questionnaires completed soon after diagnosis and prior to surgical treatment were especially common, with an overall urinary incontinence rate of 46.1% and a stress incontinence (SUI) rate of 59.5%, Dr. C. Emi Bretschneider reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
“We think increased awareness of pelvic health issues will allow for more individualized and comprehensive counseling and care of these women,” said Dr. Bretschneider of the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill.
She identified pelvic floor disorders as a major potential source of diminished quality of life in women with gynecologic malignancies.
Dr. C. Bryce Bowling, a urogynecologist at the University of Tennessee, Knoxville, agreed. Although he observed that the risk of both pelvic floor disorders and gynecologic malignancies increase with age, he said the reported rates at which they coexist is “sobering.”
“These are important data for those who are not already aware of this relationship,” Dr. Bowling, a discussant invited by the Society of Gynecologic Surgeons, said in an interview.
At many institutions, including his own, screening for pelvic floor disorders in women with gynecologic malignancies is already routine.
“Screening for incontinence is a very important consideration even for those with a poor prognosis,” he said. “Control of urinary symptoms over the course of the woman’s survival will have a very positive impact on quality of life.”
The data on pelvic floor disorders was drawn from 154 women with gynecologic cancers who completed baseline evaluations of bowel and bladder symptoms using two validated questionnaires in a recent 10-month period. Most (62%) had endometrial cancer, but other cancers, such as ovarian (17%) and cervical (11%) were represented. There were no significant differences in the rates of pelvic floor disorders among the cancer types.
In addition to the substantial rates of urinary incontinence and SUI, 40.8% of patients reported urinary incontinence with urgency and 21.5% reported nocturia most or every night. The rate of enuresis was 7.2%. In addition, 3.9% reported fecal incontinence.
Complaints of abdominal pain (46.8%), constipation (42.2%), and diarrhea (20.1%) were also common, Dr. Bretschneider reported at the meeting, jointly sponsored by the American College of Surgeons.
When women older than 50 years were compared to younger women, the rates of nearly every indicator of a pelvic floor disorder were higher. Most differences, such as overall urinary incontinence (P = .009), SUI (P = .005), and abdominal pain (P = .002) had a high degree of statistical significance. However, overall urinary incontinence and SUI were not significantly associated with age when modeled as a continuous variable.
Recognizing pelvic floor disorders at the time of the diagnosis of gynecologic malignancy can be relevant to planning cancer treatment, according to Dr. Bretschnieder. The study results highlight the need for a proactive approach that includes screening at the time of diagnosis, she said.
Key clinical point: A substantial proportion of women with gynecologic cancers have coexisting pelvic floor disorders that, if not addressed, threaten efforts to achieve optimal improvements in quality of life.
Major finding: In an evaluation of 154 women with gynecologic cancers, more than half had some degree of urinary incontinence, indicating that coexisting pelvic floor disorders are common.
Data source: Abstracted data from a prospectively enrolled cohort of cancer patients.
Disclosures: Dr. C. Emi Bretschneider reported having no financial disclosures.
FDA strengthens allergy warning for IV anemia therapy ferumoxytol
The warning about potentially life-threatening allergic reactions with the intravenous anemia drug ferumoxytol is being strengthened to reflect cases of allergic reactions, including fatalities, associated with this drug since approval, the Food and Drug Administration announced on March 30.
Information about the risk of potentially life-threatening allergic reactions was included in the warnings and precautions section of the prescribing information for ferumoxytol (Feraheme) when it was approved in 2009, and this risk is associated with all IV iron therapies. Since approval of ferumoxytol, however, “serious reactions, including deaths, have occurred despite the proper use of therapies to treat these reactions and emergency resuscitation measures,” according to the FDA’s statement, a drug safety communication.
Ways to reduce this risk have been identified and “health care professionals should follow the new recommendations in the drug label,” which includes the new contraindication, a “strong recommendation against use of Feraheme in patients who have had an allergic reaction to any intravenous (IV) iron replacement product,” the statement said.
Other recommendations included in the revised prescribing information include instructions to administer diluted ferumoxytol in an IV infusion administered over at least 15 minutes and to never administer it as an undiluted solution; to closely monitor patients for signs and symptoms of serious allergic reactions, which includes monitoring pulse and blood pressure during administration and for at least 30 minutes after each infusion; and to “carefully consider the potential risks and benefits” of the drug in elderly patients and in patients who have multiple drug allergies, two groups of patients who may be at increased risk for serious reactions.
Between June 2009 and June 30, 2014, 79 reports of anaphylactic reactions associated with ferumoxytol were identified in people from aged 19-96 years in the FDA Adverse Event Reporting System database, of which 18 were fatal, “despite immediate medical intervention and emergency resuscitation attempts. Almost half were reported with the first dose and 60 cases – about 75% – were reported to have started during the infusion or within 5 minutes after it had been fully infused.
Of the 79 cases, 34 (43%) were reported in people with a history of drug allergy; and 24% had a history of multiple drug allergies. Cardiac arrest, hypotension, dyspnea, nausea, vomiting, and flushing were among the common symptoms described.
Serious adverse events associated with ferumoxytol or other IV iron therapies should be reported to the FDA’s MedWatch program at 800-332-1099 or on-line at https://www.accessdata.fda.gov/scripts/medwatch/.
The warning about potentially life-threatening allergic reactions with the intravenous anemia drug ferumoxytol is being strengthened to reflect cases of allergic reactions, including fatalities, associated with this drug since approval, the Food and Drug Administration announced on March 30.
Information about the risk of potentially life-threatening allergic reactions was included in the warnings and precautions section of the prescribing information for ferumoxytol (Feraheme) when it was approved in 2009, and this risk is associated with all IV iron therapies. Since approval of ferumoxytol, however, “serious reactions, including deaths, have occurred despite the proper use of therapies to treat these reactions and emergency resuscitation measures,” according to the FDA’s statement, a drug safety communication.
Ways to reduce this risk have been identified and “health care professionals should follow the new recommendations in the drug label,” which includes the new contraindication, a “strong recommendation against use of Feraheme in patients who have had an allergic reaction to any intravenous (IV) iron replacement product,” the statement said.
Other recommendations included in the revised prescribing information include instructions to administer diluted ferumoxytol in an IV infusion administered over at least 15 minutes and to never administer it as an undiluted solution; to closely monitor patients for signs and symptoms of serious allergic reactions, which includes monitoring pulse and blood pressure during administration and for at least 30 minutes after each infusion; and to “carefully consider the potential risks and benefits” of the drug in elderly patients and in patients who have multiple drug allergies, two groups of patients who may be at increased risk for serious reactions.
Between June 2009 and June 30, 2014, 79 reports of anaphylactic reactions associated with ferumoxytol were identified in people from aged 19-96 years in the FDA Adverse Event Reporting System database, of which 18 were fatal, “despite immediate medical intervention and emergency resuscitation attempts. Almost half were reported with the first dose and 60 cases – about 75% – were reported to have started during the infusion or within 5 minutes after it had been fully infused.
Of the 79 cases, 34 (43%) were reported in people with a history of drug allergy; and 24% had a history of multiple drug allergies. Cardiac arrest, hypotension, dyspnea, nausea, vomiting, and flushing were among the common symptoms described.
Serious adverse events associated with ferumoxytol or other IV iron therapies should be reported to the FDA’s MedWatch program at 800-332-1099 or on-line at https://www.accessdata.fda.gov/scripts/medwatch/.
The warning about potentially life-threatening allergic reactions with the intravenous anemia drug ferumoxytol is being strengthened to reflect cases of allergic reactions, including fatalities, associated with this drug since approval, the Food and Drug Administration announced on March 30.
Information about the risk of potentially life-threatening allergic reactions was included in the warnings and precautions section of the prescribing information for ferumoxytol (Feraheme) when it was approved in 2009, and this risk is associated with all IV iron therapies. Since approval of ferumoxytol, however, “serious reactions, including deaths, have occurred despite the proper use of therapies to treat these reactions and emergency resuscitation measures,” according to the FDA’s statement, a drug safety communication.
Ways to reduce this risk have been identified and “health care professionals should follow the new recommendations in the drug label,” which includes the new contraindication, a “strong recommendation against use of Feraheme in patients who have had an allergic reaction to any intravenous (IV) iron replacement product,” the statement said.
Other recommendations included in the revised prescribing information include instructions to administer diluted ferumoxytol in an IV infusion administered over at least 15 minutes and to never administer it as an undiluted solution; to closely monitor patients for signs and symptoms of serious allergic reactions, which includes monitoring pulse and blood pressure during administration and for at least 30 minutes after each infusion; and to “carefully consider the potential risks and benefits” of the drug in elderly patients and in patients who have multiple drug allergies, two groups of patients who may be at increased risk for serious reactions.
Between June 2009 and June 30, 2014, 79 reports of anaphylactic reactions associated with ferumoxytol were identified in people from aged 19-96 years in the FDA Adverse Event Reporting System database, of which 18 were fatal, “despite immediate medical intervention and emergency resuscitation attempts. Almost half were reported with the first dose and 60 cases – about 75% – were reported to have started during the infusion or within 5 minutes after it had been fully infused.
Of the 79 cases, 34 (43%) were reported in people with a history of drug allergy; and 24% had a history of multiple drug allergies. Cardiac arrest, hypotension, dyspnea, nausea, vomiting, and flushing were among the common symptoms described.
Serious adverse events associated with ferumoxytol or other IV iron therapies should be reported to the FDA’s MedWatch program at 800-332-1099 or on-line at https://www.accessdata.fda.gov/scripts/medwatch/.
Long-term endocrine effects common after reduced-intensity chemotherapy in children
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
AT ENDO 2015
Key clinical point: Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Major finding: Of the 77 children assessed for thyroid function after HSCT with reduced-intensity conditioning, 11 had evidence of primary hypothyroidism, five had central hypothyroidism, and two had evidence of primary hyperthyroidism.
Data source: Review of 120 pediatric hematopoietic stem cell transplants at the Cincinnati Children’s Hospital Medical Center.
Disclosures: The investigators had no disclosures and no external funding for their work.