User login
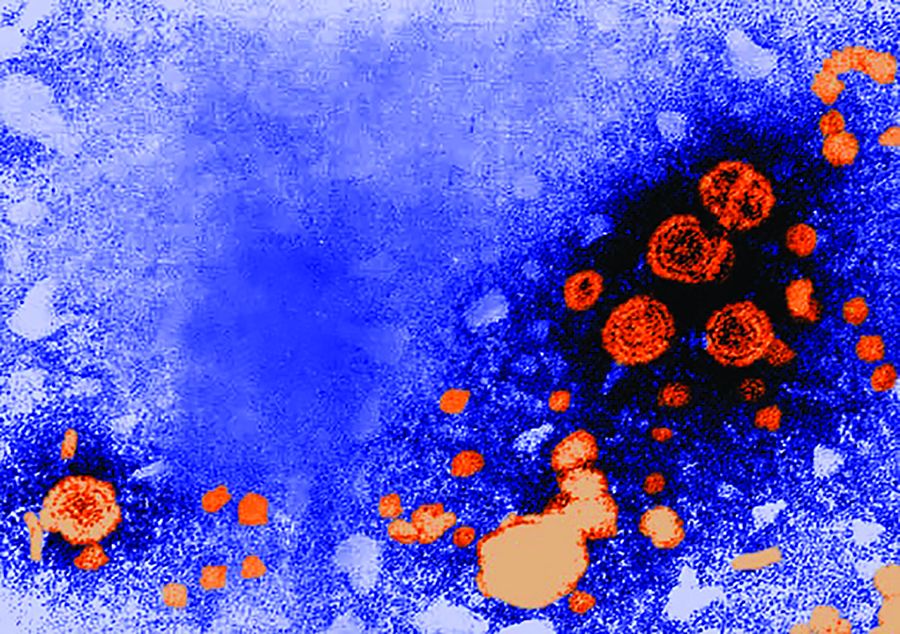
CDC: Zika-exposed newborns need intensified eye, hearing, and neurological testing
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
FROM MMWR
Rapid genomic testing can diagnose critically ill infants
Rapid, targeted genomic sequencing shows promise in quickly diagnosing critically ill infants for whom standard clinical work-ups were unsuccessful, according to Cleo C. van Diemen, PhD, of the University of Groningen (the Netherlands), and associates.
Over the course of 1 year, 23 critically ill infants younger than 12 months who had no clear diagnosis after standard clinical work-ups underwent rapid, targeted genomics, with 7 receiving a genetic diagnosis. The median turnaround time was 12 days, falling from roughly 3 weeks at the beginning of the study to a maximum of 8 days by the end of the study.
Compound heterozygous mutations in the EPG5, RMND1, and EIF2B5 genes allowed for diagnoses of Vici syndrome, combined oxidative phosphorylation deficiency-11, and vanishing white matter, respectively. Homozygous mutations in the KLHL41, GFER, and GLB1 genes allowed for diagnoses of nemaline myopathy, progressive mitochondrial myopathy, and GM1-gangliosidosis, respectively. In addition, a 1p36.33p36.32 microdeletion was discovered in an infant with cardiomyopathy.
“The clinical relevance of rapid genome diagnostics lies in the fact that these results can be used in the clinical decisions made in caring for critically ill children in ICUs, in better genetic counseling of the parents, and in guiding their future reproductive choices,” the investigators noted.
Find the full study in Pediatrics (2017 Sep 22. doi: 10.1542/ peds.2016-2854).
Rapid, targeted genomic sequencing shows promise in quickly diagnosing critically ill infants for whom standard clinical work-ups were unsuccessful, according to Cleo C. van Diemen, PhD, of the University of Groningen (the Netherlands), and associates.
Over the course of 1 year, 23 critically ill infants younger than 12 months who had no clear diagnosis after standard clinical work-ups underwent rapid, targeted genomics, with 7 receiving a genetic diagnosis. The median turnaround time was 12 days, falling from roughly 3 weeks at the beginning of the study to a maximum of 8 days by the end of the study.
Compound heterozygous mutations in the EPG5, RMND1, and EIF2B5 genes allowed for diagnoses of Vici syndrome, combined oxidative phosphorylation deficiency-11, and vanishing white matter, respectively. Homozygous mutations in the KLHL41, GFER, and GLB1 genes allowed for diagnoses of nemaline myopathy, progressive mitochondrial myopathy, and GM1-gangliosidosis, respectively. In addition, a 1p36.33p36.32 microdeletion was discovered in an infant with cardiomyopathy.
“The clinical relevance of rapid genome diagnostics lies in the fact that these results can be used in the clinical decisions made in caring for critically ill children in ICUs, in better genetic counseling of the parents, and in guiding their future reproductive choices,” the investigators noted.
Find the full study in Pediatrics (2017 Sep 22. doi: 10.1542/ peds.2016-2854).
Rapid, targeted genomic sequencing shows promise in quickly diagnosing critically ill infants for whom standard clinical work-ups were unsuccessful, according to Cleo C. van Diemen, PhD, of the University of Groningen (the Netherlands), and associates.
Over the course of 1 year, 23 critically ill infants younger than 12 months who had no clear diagnosis after standard clinical work-ups underwent rapid, targeted genomics, with 7 receiving a genetic diagnosis. The median turnaround time was 12 days, falling from roughly 3 weeks at the beginning of the study to a maximum of 8 days by the end of the study.
Compound heterozygous mutations in the EPG5, RMND1, and EIF2B5 genes allowed for diagnoses of Vici syndrome, combined oxidative phosphorylation deficiency-11, and vanishing white matter, respectively. Homozygous mutations in the KLHL41, GFER, and GLB1 genes allowed for diagnoses of nemaline myopathy, progressive mitochondrial myopathy, and GM1-gangliosidosis, respectively. In addition, a 1p36.33p36.32 microdeletion was discovered in an infant with cardiomyopathy.
“The clinical relevance of rapid genome diagnostics lies in the fact that these results can be used in the clinical decisions made in caring for critically ill children in ICUs, in better genetic counseling of the parents, and in guiding their future reproductive choices,” the investigators noted.
Find the full study in Pediatrics (2017 Sep 22. doi: 10.1542/ peds.2016-2854).
FROM PEDIATRICS
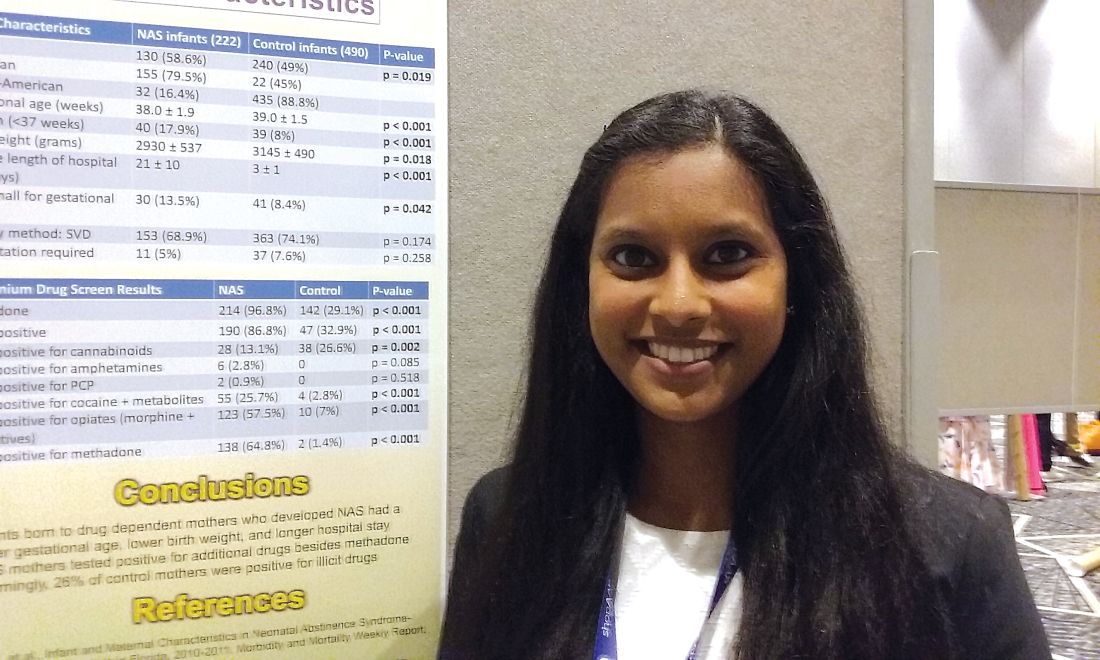
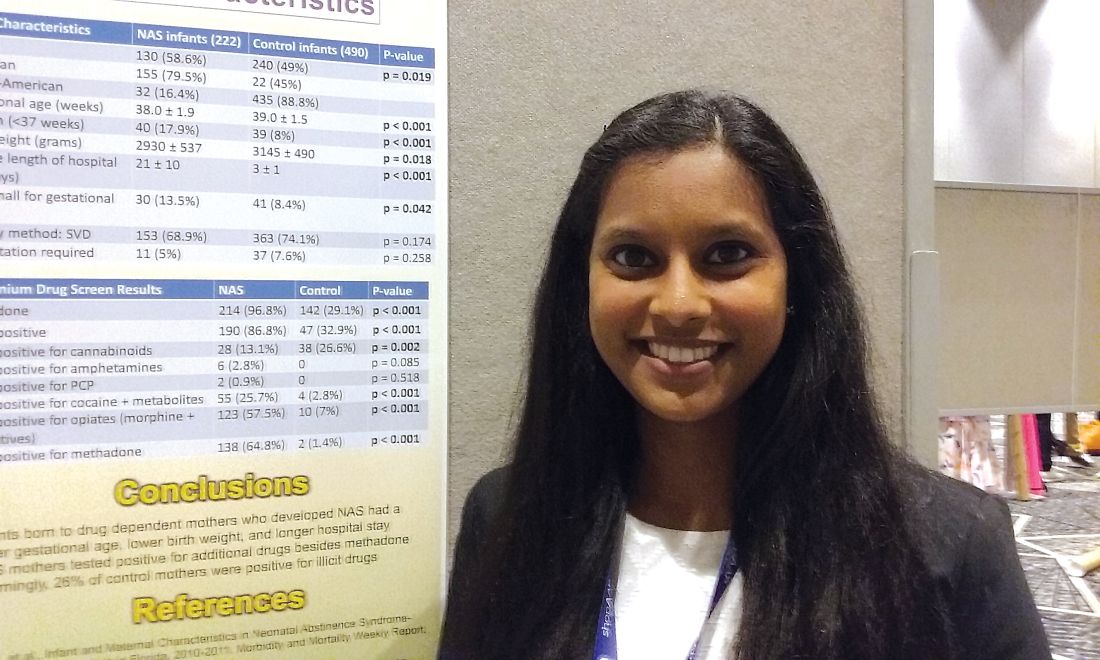
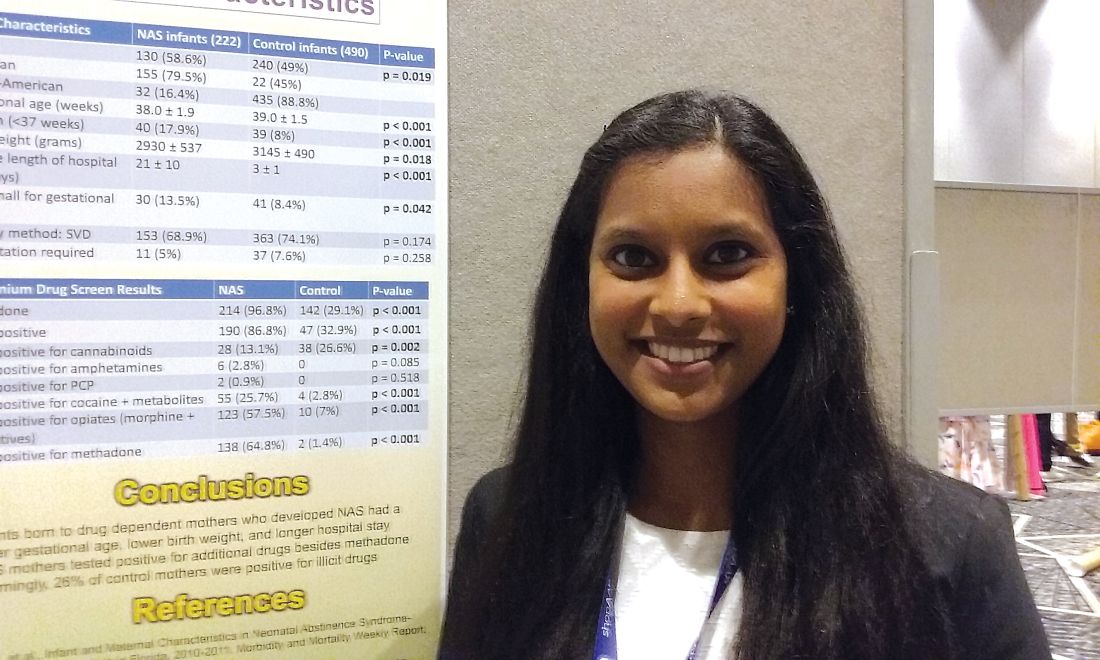
One in four ‘control’ mothers in NAS study tests positive for drug use
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
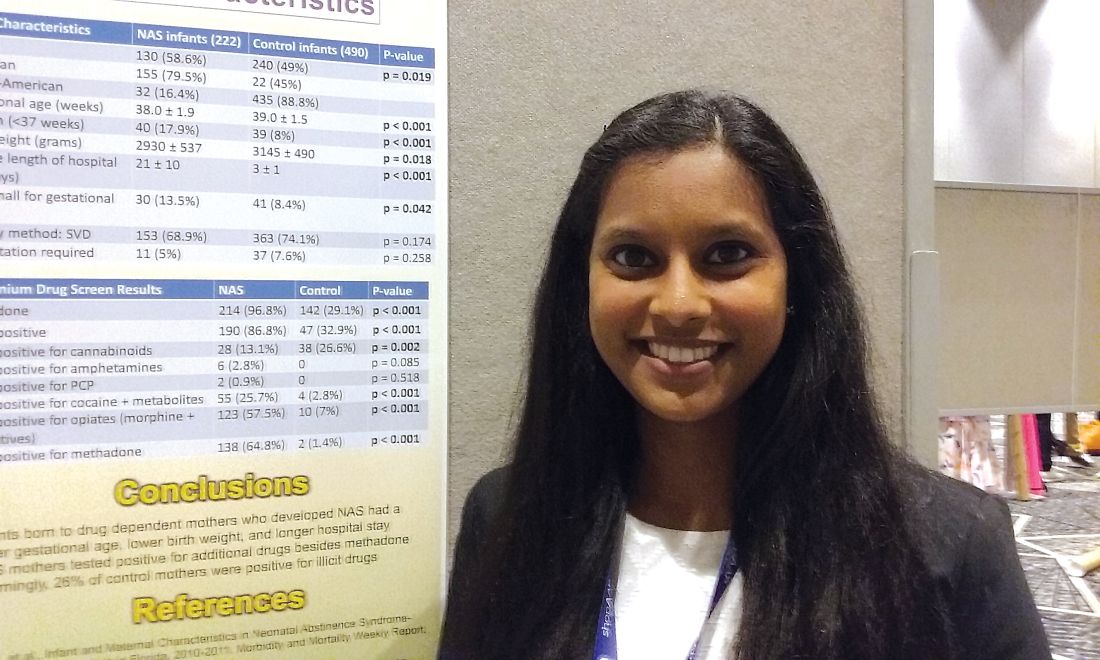
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Investigators studied mothers whose babies developed NAS and were surprised when almost 25% of women in the control group also tested positive for illicit drug use.
Major finding: Among the control mothers, drug use included marijuana 20.4%, opioids 1.8%, cocaine 1.2%, benzodiazepines 0.6%, heroin 0.2%, and barbiturates 0.2%.
Data source: Chart review of 222 infants who developed neonatal abstinence syndrome, compared with 490 controls.
Disclosures: Dr. Karunakaran had no relevant financial disclosures.
Breastfeeding practices have improved, but some attitudes are concerning
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: The percentage of surveyed physicians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05).
Data source: An analysis of data from three AAP Periodic Surveys of Fellows.
Disclosures: The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
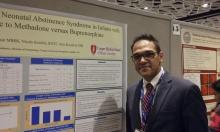
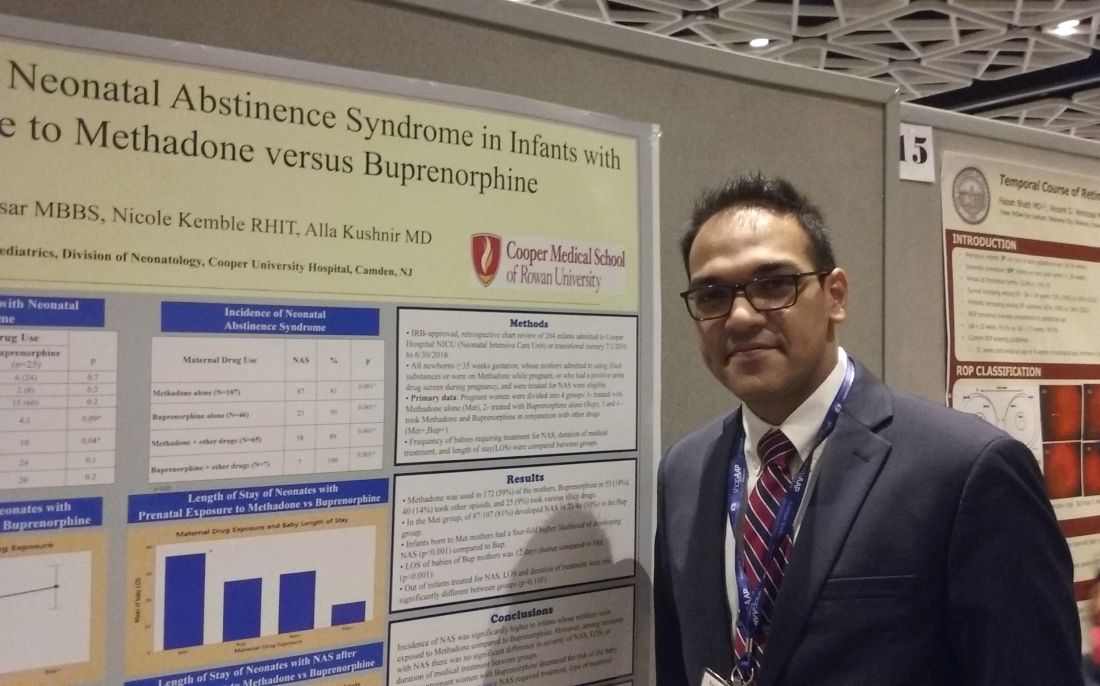
Buprenorphine linked to less neonatal abstinence syndrome than methadone
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
AT AAP 2017
Key clinical point: .
Major finding: 81% of infants in the methadone group developed NAS, compared with 50% of the buprenorphine group.
Data source: Retrospective study of 204 babies admitted to a NICU between July 2010 to June 2016 whose mothers admitted or tested positive for opioid maintenance therapy.
Disclosures: Dr. Kushnir and Dr. Bhaysar reported having no relevant financial disclosures.
Domperidone appears safe galactagogue for mothers and infants
Denver – Prescribing domperidone to support breastfeeding effectively reduced the use of infant formula without significant adverse effects in mothers and infants in a large retrospective study, Mitko Madjunkov, MD, reported at the annual meeting of the Teratology Society.
His study included 985 mothers who began taking domperidone to initiate and support breastfeeding after a visit to the International Breastfeeding Centre in Toronto. Collectively, the women had 1,005 infants.
The study was undertaken because few data exist on the dosing and safety of domperidone during lactation. Additionally, the Food and Drug Administration issued a warning in 2004 regarding the use of domperidone as a galactagogue in response to reports of cardiac arrhythmias and sudden deaths when the drug was prescribed as an antiemetic, explained Dr. Madjunkov of the Hospital for Sick Children in Toronto.
The FDA has not approved domperidone for any indication in the United States, though it is available in Canada and other countries.
Domperidone was used by the Toronto women for a median of 20 days. The maximum daily dose was 107 mg. The infants were an average of 38 days old at the time of the visit when domperidone was prescribed and 72 days of age at their last follow-up visit related to the study.
The drug was effective as a galactagogue: 63% of women were using infant formula before going on domperidone; after using the drug, 41% were still using formula, for an absolute 22% reduction. The drug was similarly effective in promoting breastfeeding in infants with or without tongue-tie/lip-tie defects.
In total, 18% of mothers reported minor side effects. Headaches were the most common, reported by 9.2% of domperidone users. Dose reduction was employed in just 0.6% of women in the study; 0.4% of participants discontinued treatment. Rapid heart rate and other minor cardiac side effects were reported by 0.7% of women, uniformly in conjunction with trigger factors such as anxiety or caffeine use, but none of these women discontinued treatment. No treatment-associated adverse effects occurred in the infants.
Dr. Madjunkov reported having no financial conflicts related to his study.
Denver – Prescribing domperidone to support breastfeeding effectively reduced the use of infant formula without significant adverse effects in mothers and infants in a large retrospective study, Mitko Madjunkov, MD, reported at the annual meeting of the Teratology Society.
His study included 985 mothers who began taking domperidone to initiate and support breastfeeding after a visit to the International Breastfeeding Centre in Toronto. Collectively, the women had 1,005 infants.
The study was undertaken because few data exist on the dosing and safety of domperidone during lactation. Additionally, the Food and Drug Administration issued a warning in 2004 regarding the use of domperidone as a galactagogue in response to reports of cardiac arrhythmias and sudden deaths when the drug was prescribed as an antiemetic, explained Dr. Madjunkov of the Hospital for Sick Children in Toronto.
The FDA has not approved domperidone for any indication in the United States, though it is available in Canada and other countries.
Domperidone was used by the Toronto women for a median of 20 days. The maximum daily dose was 107 mg. The infants were an average of 38 days old at the time of the visit when domperidone was prescribed and 72 days of age at their last follow-up visit related to the study.
The drug was effective as a galactagogue: 63% of women were using infant formula before going on domperidone; after using the drug, 41% were still using formula, for an absolute 22% reduction. The drug was similarly effective in promoting breastfeeding in infants with or without tongue-tie/lip-tie defects.
In total, 18% of mothers reported minor side effects. Headaches were the most common, reported by 9.2% of domperidone users. Dose reduction was employed in just 0.6% of women in the study; 0.4% of participants discontinued treatment. Rapid heart rate and other minor cardiac side effects were reported by 0.7% of women, uniformly in conjunction with trigger factors such as anxiety or caffeine use, but none of these women discontinued treatment. No treatment-associated adverse effects occurred in the infants.
Dr. Madjunkov reported having no financial conflicts related to his study.
Denver – Prescribing domperidone to support breastfeeding effectively reduced the use of infant formula without significant adverse effects in mothers and infants in a large retrospective study, Mitko Madjunkov, MD, reported at the annual meeting of the Teratology Society.
His study included 985 mothers who began taking domperidone to initiate and support breastfeeding after a visit to the International Breastfeeding Centre in Toronto. Collectively, the women had 1,005 infants.
The study was undertaken because few data exist on the dosing and safety of domperidone during lactation. Additionally, the Food and Drug Administration issued a warning in 2004 regarding the use of domperidone as a galactagogue in response to reports of cardiac arrhythmias and sudden deaths when the drug was prescribed as an antiemetic, explained Dr. Madjunkov of the Hospital for Sick Children in Toronto.
The FDA has not approved domperidone for any indication in the United States, though it is available in Canada and other countries.
Domperidone was used by the Toronto women for a median of 20 days. The maximum daily dose was 107 mg. The infants were an average of 38 days old at the time of the visit when domperidone was prescribed and 72 days of age at their last follow-up visit related to the study.
The drug was effective as a galactagogue: 63% of women were using infant formula before going on domperidone; after using the drug, 41% were still using formula, for an absolute 22% reduction. The drug was similarly effective in promoting breastfeeding in infants with or without tongue-tie/lip-tie defects.
In total, 18% of mothers reported minor side effects. Headaches were the most common, reported by 9.2% of domperidone users. Dose reduction was employed in just 0.6% of women in the study; 0.4% of participants discontinued treatment. Rapid heart rate and other minor cardiac side effects were reported by 0.7% of women, uniformly in conjunction with trigger factors such as anxiety or caffeine use, but none of these women discontinued treatment. No treatment-associated adverse effects occurred in the infants.
Dr. Madjunkov reported having no financial conflicts related to his study.
EXPERT ANALYSIS FROM TERATOLOGY SOCIETY 2017
Key clinical point:
Major finding: The use of the domperidone reduced the proportion of women using infant formula by an absolute 22%.
Data source: A retrospective study of 985 women who were prescribed domperidone as a galactagogue at the International Breastfeeding Centre in Toronto.
Disclosures: Dr. Madjunkov reported having no financial conflicts of interest related to the study.
Study: Don’t separate NAS infants from moms
NASHVILLE, TENN. – When newborns withdrawing from opioids stay with their mothers after delivery instead of going to the NICU, they are far less likely to receive morphine and other drugs and leave the hospital days sooner; they also are more likely to go home with their mother, a meta-analysis showed.
The analysis likely is the first to pool results from studies of rooming-in for infants with neonatal abstinence syndrome (NAS). A strong case has been building in the literature for several years that newborns do better with rooming-in, instead of the traditional approach for NAS – NICU housing and opioid dosing based on a symptom checklist.
“We found consistent emerging evidence that rooming-in is more effective than standard care in the NICU for infants with NAS. Based on these findings, we believe rooming-in should be established as the new evidence-based standard of care for this patient population,” said investigator Kanak Verma, a medical student at Dartmouth College, Hanover, N.H.
Rooming-in was associated with a 63% reduction in the need for pharmacotherapy, a decrease in hospital length of stay by more than 10 days, and a substantial, statistically significant decrease in cost from – in one study – a mean of almost $45,000 per NAS infant stay to just over $10,000.
“We were worried that by rooming-in we would be undertreating infants with NAS, and that they would be at increased risk for readmission, but there was no statistically significant increase in readmission rates for infants rooming in with their mothers,” Ms. Verma said at the Pediatric Hospital Medical annual meeting.
Infants also were more likely to go home with their mother or a family member. “Mothers who use opioid replacements have decreased ability to bond” with their infants. Rooming-in helps create that bond, and probably made discharge with a family member more likely, said coinvestigator Cassandra Rendon, also a Dartmouth medical student.
It’s unclear what exactly accounts for the better results, but “having a baby stay with [its] mom creates an opportunity for a lot of things that we know are effective,” including skin-to-skin contact, breastfeeding, and involvement of mothers in the care and monitoring of their infants, Ms. Rendon said.
Also, “we know that in babies with NAS, a low-stimulation environment is ideal,” Ms. Verma said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association. That’s a challenge in a busy NICU, but “we can create that in an isolated room with just the mother,” she added.
At least one of the studies used a new, more holistic approach to assess the need for pharmacologic management in NAS. Symptom scores still are considered, but how well the infant is eating, sleeping, and able to be consoled are considered as well. With the traditional symptom checklist, “we end up just treating the number, instead of treating the baby. What Dartmouth and other facilities are doing is looking at” how well the baby is doing overall, Ms. Rendon said.
If the baby is otherwise doing well, providers are less likely to give opioids for a little jitteriness or sweating. The decreased use of opioids leads, in turn, to shorter hospital stays.
Dartmouth is collaborating with Yale University in New Haven , Conn., and the Boston Medical Center to integrate the new treatment model into standard practice. For other centers interested in doing the same, Ms. Verma noted that nursery staff buy-in is essential. Nurses and others have to be comfortable “taking these patients out of the NICU” and treating them in a new way.
The investigators had no relevant financial disclosures.
NASHVILLE, TENN. – When newborns withdrawing from opioids stay with their mothers after delivery instead of going to the NICU, they are far less likely to receive morphine and other drugs and leave the hospital days sooner; they also are more likely to go home with their mother, a meta-analysis showed.
The analysis likely is the first to pool results from studies of rooming-in for infants with neonatal abstinence syndrome (NAS). A strong case has been building in the literature for several years that newborns do better with rooming-in, instead of the traditional approach for NAS – NICU housing and opioid dosing based on a symptom checklist.
“We found consistent emerging evidence that rooming-in is more effective than standard care in the NICU for infants with NAS. Based on these findings, we believe rooming-in should be established as the new evidence-based standard of care for this patient population,” said investigator Kanak Verma, a medical student at Dartmouth College, Hanover, N.H.
Rooming-in was associated with a 63% reduction in the need for pharmacotherapy, a decrease in hospital length of stay by more than 10 days, and a substantial, statistically significant decrease in cost from – in one study – a mean of almost $45,000 per NAS infant stay to just over $10,000.
“We were worried that by rooming-in we would be undertreating infants with NAS, and that they would be at increased risk for readmission, but there was no statistically significant increase in readmission rates for infants rooming in with their mothers,” Ms. Verma said at the Pediatric Hospital Medical annual meeting.
Infants also were more likely to go home with their mother or a family member. “Mothers who use opioid replacements have decreased ability to bond” with their infants. Rooming-in helps create that bond, and probably made discharge with a family member more likely, said coinvestigator Cassandra Rendon, also a Dartmouth medical student.
It’s unclear what exactly accounts for the better results, but “having a baby stay with [its] mom creates an opportunity for a lot of things that we know are effective,” including skin-to-skin contact, breastfeeding, and involvement of mothers in the care and monitoring of their infants, Ms. Rendon said.
Also, “we know that in babies with NAS, a low-stimulation environment is ideal,” Ms. Verma said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association. That’s a challenge in a busy NICU, but “we can create that in an isolated room with just the mother,” she added.
At least one of the studies used a new, more holistic approach to assess the need for pharmacologic management in NAS. Symptom scores still are considered, but how well the infant is eating, sleeping, and able to be consoled are considered as well. With the traditional symptom checklist, “we end up just treating the number, instead of treating the baby. What Dartmouth and other facilities are doing is looking at” how well the baby is doing overall, Ms. Rendon said.
If the baby is otherwise doing well, providers are less likely to give opioids for a little jitteriness or sweating. The decreased use of opioids leads, in turn, to shorter hospital stays.
Dartmouth is collaborating with Yale University in New Haven , Conn., and the Boston Medical Center to integrate the new treatment model into standard practice. For other centers interested in doing the same, Ms. Verma noted that nursery staff buy-in is essential. Nurses and others have to be comfortable “taking these patients out of the NICU” and treating them in a new way.
The investigators had no relevant financial disclosures.
NASHVILLE, TENN. – When newborns withdrawing from opioids stay with their mothers after delivery instead of going to the NICU, they are far less likely to receive morphine and other drugs and leave the hospital days sooner; they also are more likely to go home with their mother, a meta-analysis showed.
The analysis likely is the first to pool results from studies of rooming-in for infants with neonatal abstinence syndrome (NAS). A strong case has been building in the literature for several years that newborns do better with rooming-in, instead of the traditional approach for NAS – NICU housing and opioid dosing based on a symptom checklist.
“We found consistent emerging evidence that rooming-in is more effective than standard care in the NICU for infants with NAS. Based on these findings, we believe rooming-in should be established as the new evidence-based standard of care for this patient population,” said investigator Kanak Verma, a medical student at Dartmouth College, Hanover, N.H.
Rooming-in was associated with a 63% reduction in the need for pharmacotherapy, a decrease in hospital length of stay by more than 10 days, and a substantial, statistically significant decrease in cost from – in one study – a mean of almost $45,000 per NAS infant stay to just over $10,000.
“We were worried that by rooming-in we would be undertreating infants with NAS, and that they would be at increased risk for readmission, but there was no statistically significant increase in readmission rates for infants rooming in with their mothers,” Ms. Verma said at the Pediatric Hospital Medical annual meeting.
Infants also were more likely to go home with their mother or a family member. “Mothers who use opioid replacements have decreased ability to bond” with their infants. Rooming-in helps create that bond, and probably made discharge with a family member more likely, said coinvestigator Cassandra Rendon, also a Dartmouth medical student.
It’s unclear what exactly accounts for the better results, but “having a baby stay with [its] mom creates an opportunity for a lot of things that we know are effective,” including skin-to-skin contact, breastfeeding, and involvement of mothers in the care and monitoring of their infants, Ms. Rendon said.
Also, “we know that in babies with NAS, a low-stimulation environment is ideal,” Ms. Verma said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association. That’s a challenge in a busy NICU, but “we can create that in an isolated room with just the mother,” she added.
At least one of the studies used a new, more holistic approach to assess the need for pharmacologic management in NAS. Symptom scores still are considered, but how well the infant is eating, sleeping, and able to be consoled are considered as well. With the traditional symptom checklist, “we end up just treating the number, instead of treating the baby. What Dartmouth and other facilities are doing is looking at” how well the baby is doing overall, Ms. Rendon said.
If the baby is otherwise doing well, providers are less likely to give opioids for a little jitteriness or sweating. The decreased use of opioids leads, in turn, to shorter hospital stays.
Dartmouth is collaborating with Yale University in New Haven , Conn., and the Boston Medical Center to integrate the new treatment model into standard practice. For other centers interested in doing the same, Ms. Verma noted that nursery staff buy-in is essential. Nurses and others have to be comfortable “taking these patients out of the NICU” and treating them in a new way.
The investigators had no relevant financial disclosures.
AT PHM 2017
Key clinical point:
Major finding: Rooming-in was associated with a 63% reduction in the need for pharmacotherapy, a decrease in hospital length of stay by more than 10 days, and a substantial, statistically significant decrease in cost from, in one study, a mean of almost $45,000 per NAS infant stay to just over $10,000.
Data source: A meta-analysis of six studies.
Disclosures: The investigators had no relevant financial disclosures.
Postpartum depression screening in well-child care appears promising
, according to results of a study from the Netherlands.
“This promising finding warrants wider implementation of screening for postpartum depression,” said Dr. Angarath I. Van der Zee-van den Berg of the University of Twente, Enschede, the Netherlands, and associates.
Results showed significantly fewer mothers in the intervention group were depressed at 9 months post partum, compared with the CAU group (0.6% of 1,843 vs. 2.5% 1,246 for major depression), with an adjusted odds ratio of 0.28 (95% confidence interval, 0.12-0.63). The difference also was significant for minor and major depression, with 3.0% of the intervention group affected vs. 8.4% of the CAU group, and the adjusted odds ratio was 0.40 (95% confidence interval, 0.27-0.58). For parenting, anxiety symptoms, and mental health functioning, the intervention resulted in effect sizes ranging from 0.23 to 0.27.
“We found screening for postpartum depression to have a negligible effect on socioemotional development of the child with no former evidence to compare with,” Dr. Van der Zee-van den Berg and his associates said. “Attention for the mother-child interaction in the trajectory after screening may improve child outcomes; this evidently requires further study.”
To find out more information see Pediatrics (2017;140[4]:e20170110).
, according to results of a study from the Netherlands.
“This promising finding warrants wider implementation of screening for postpartum depression,” said Dr. Angarath I. Van der Zee-van den Berg of the University of Twente, Enschede, the Netherlands, and associates.
Results showed significantly fewer mothers in the intervention group were depressed at 9 months post partum, compared with the CAU group (0.6% of 1,843 vs. 2.5% 1,246 for major depression), with an adjusted odds ratio of 0.28 (95% confidence interval, 0.12-0.63). The difference also was significant for minor and major depression, with 3.0% of the intervention group affected vs. 8.4% of the CAU group, and the adjusted odds ratio was 0.40 (95% confidence interval, 0.27-0.58). For parenting, anxiety symptoms, and mental health functioning, the intervention resulted in effect sizes ranging from 0.23 to 0.27.
“We found screening for postpartum depression to have a negligible effect on socioemotional development of the child with no former evidence to compare with,” Dr. Van der Zee-van den Berg and his associates said. “Attention for the mother-child interaction in the trajectory after screening may improve child outcomes; this evidently requires further study.”
To find out more information see Pediatrics (2017;140[4]:e20170110).
, according to results of a study from the Netherlands.
“This promising finding warrants wider implementation of screening for postpartum depression,” said Dr. Angarath I. Van der Zee-van den Berg of the University of Twente, Enschede, the Netherlands, and associates.
Results showed significantly fewer mothers in the intervention group were depressed at 9 months post partum, compared with the CAU group (0.6% of 1,843 vs. 2.5% 1,246 for major depression), with an adjusted odds ratio of 0.28 (95% confidence interval, 0.12-0.63). The difference also was significant for minor and major depression, with 3.0% of the intervention group affected vs. 8.4% of the CAU group, and the adjusted odds ratio was 0.40 (95% confidence interval, 0.27-0.58). For parenting, anxiety symptoms, and mental health functioning, the intervention resulted in effect sizes ranging from 0.23 to 0.27.
“We found screening for postpartum depression to have a negligible effect on socioemotional development of the child with no former evidence to compare with,” Dr. Van der Zee-van den Berg and his associates said. “Attention for the mother-child interaction in the trajectory after screening may improve child outcomes; this evidently requires further study.”
To find out more information see Pediatrics (2017;140[4]:e20170110).
FROM PEDIATRICS
AAP recommends hepatitis B vaccine within 24 hours of birth for all infants
All newborns with a birth weight of at least 2,000 grams (4.4 pounds) should receive the hepatitis B vaccine within 24 hours of birth, according to a new policy statement by the American Academy of Pediatrics that brings its recommendations in line with those of the Advisory Committee on Immunization Practices at the Centers for Disease Control and Prevention.
“The birth dose can prevent infection of infants born to infected mothers in situations in which the mother’s results are never obtained, are misinterpreted, are falsely negative, are transcribed or reported to the infant care team inaccurately, or simply not communicated to the nursery,” announced the new statement from the AAP Committee on Infectious Diseases and the Committee on Fetus and Newborn (Pediatrics. 2017 Aug 28. doi: 10.1542/peds.2017-1870).
A dose of the hepatitis B vaccine within 24 hours of birth is 75%-95% effective at preventing perinatal hepatitis B transmission. “When postexposure prophylaxis with both hepatitis B vaccine and hepatitis B immune globulin (HBIG) is given, is timed appropriately, and is followed by completion of the infant hepatitis B immunization series, perinatal infection rates range from 0.7% to 1.1%,” according to the statement.
Approximately 1,000 newborns still contract perinatal hepatitis B infections every year. Of these, 90% will develop chronic hepatitis B infections, and a quarter of those who don’t receive treatment will die from liver cirrhosis or cancer. There has been an increase in the incidence of new hepatitis B infections in some states because of opioid epidemic in the United States, according to MMWR reports.
The cost effectiveness of preventing hepatitis B with the vaccine and, when necessary, HBIG, is estimated at $2,600 per quality-adjusted year of life. The most common side effects reported after hepatitis B administration are pain (3%-29%), erythema (3%), swelling (3%), fever (1%-6%) and headache (3%).
There has been extensive analysis of the safety of hepatitis B vaccines, the policy statement indicated. Analysis of Vaccine Safety Datalink data has found no causal link between administration of the hepatitis B vaccine and the following: neonatal sepsis or death, rheumatoid arthritis, Bell’s palsy, autoimmune thyroid disease, hemolytic anemia in children, anaphylaxis, optic neuritis, Guillain-Barré syndrome, sudden-onset sensorineural hearing loss, or other chronic illnesses.
Specific recommendations
• Infants born to mothers who test positive for hepatitis B surface antigen (HBsAg): Administer the hepatitis B vaccine and HBIG within 12 hours of birth.
• Infants weighing at least 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine within 24 hours of birth.
• Infants weighing less than 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine at hospital discharge or at age 1 month (whichever is first).
• Infants weighing at least 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and HBIG by hospital discharge or age 7 days (whichever is first) if HBsAg status remains unknown or is confirmed positive.
• Infants weighing less than 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and then HBIG within 12 hours unless the mother tests negative for HBsAg by then.
All newborns with a birth weight of at least 2,000 grams (4.4 pounds) should receive the hepatitis B vaccine within 24 hours of birth, according to a new policy statement by the American Academy of Pediatrics that brings its recommendations in line with those of the Advisory Committee on Immunization Practices at the Centers for Disease Control and Prevention.
“The birth dose can prevent infection of infants born to infected mothers in situations in which the mother’s results are never obtained, are misinterpreted, are falsely negative, are transcribed or reported to the infant care team inaccurately, or simply not communicated to the nursery,” announced the new statement from the AAP Committee on Infectious Diseases and the Committee on Fetus and Newborn (Pediatrics. 2017 Aug 28. doi: 10.1542/peds.2017-1870).
A dose of the hepatitis B vaccine within 24 hours of birth is 75%-95% effective at preventing perinatal hepatitis B transmission. “When postexposure prophylaxis with both hepatitis B vaccine and hepatitis B immune globulin (HBIG) is given, is timed appropriately, and is followed by completion of the infant hepatitis B immunization series, perinatal infection rates range from 0.7% to 1.1%,” according to the statement.
Approximately 1,000 newborns still contract perinatal hepatitis B infections every year. Of these, 90% will develop chronic hepatitis B infections, and a quarter of those who don’t receive treatment will die from liver cirrhosis or cancer. There has been an increase in the incidence of new hepatitis B infections in some states because of opioid epidemic in the United States, according to MMWR reports.
The cost effectiveness of preventing hepatitis B with the vaccine and, when necessary, HBIG, is estimated at $2,600 per quality-adjusted year of life. The most common side effects reported after hepatitis B administration are pain (3%-29%), erythema (3%), swelling (3%), fever (1%-6%) and headache (3%).
There has been extensive analysis of the safety of hepatitis B vaccines, the policy statement indicated. Analysis of Vaccine Safety Datalink data has found no causal link between administration of the hepatitis B vaccine and the following: neonatal sepsis or death, rheumatoid arthritis, Bell’s palsy, autoimmune thyroid disease, hemolytic anemia in children, anaphylaxis, optic neuritis, Guillain-Barré syndrome, sudden-onset sensorineural hearing loss, or other chronic illnesses.
Specific recommendations
• Infants born to mothers who test positive for hepatitis B surface antigen (HBsAg): Administer the hepatitis B vaccine and HBIG within 12 hours of birth.
• Infants weighing at least 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine within 24 hours of birth.
• Infants weighing less than 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine at hospital discharge or at age 1 month (whichever is first).
• Infants weighing at least 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and HBIG by hospital discharge or age 7 days (whichever is first) if HBsAg status remains unknown or is confirmed positive.
• Infants weighing less than 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and then HBIG within 12 hours unless the mother tests negative for HBsAg by then.
All newborns with a birth weight of at least 2,000 grams (4.4 pounds) should receive the hepatitis B vaccine within 24 hours of birth, according to a new policy statement by the American Academy of Pediatrics that brings its recommendations in line with those of the Advisory Committee on Immunization Practices at the Centers for Disease Control and Prevention.
“The birth dose can prevent infection of infants born to infected mothers in situations in which the mother’s results are never obtained, are misinterpreted, are falsely negative, are transcribed or reported to the infant care team inaccurately, or simply not communicated to the nursery,” announced the new statement from the AAP Committee on Infectious Diseases and the Committee on Fetus and Newborn (Pediatrics. 2017 Aug 28. doi: 10.1542/peds.2017-1870).
A dose of the hepatitis B vaccine within 24 hours of birth is 75%-95% effective at preventing perinatal hepatitis B transmission. “When postexposure prophylaxis with both hepatitis B vaccine and hepatitis B immune globulin (HBIG) is given, is timed appropriately, and is followed by completion of the infant hepatitis B immunization series, perinatal infection rates range from 0.7% to 1.1%,” according to the statement.
Approximately 1,000 newborns still contract perinatal hepatitis B infections every year. Of these, 90% will develop chronic hepatitis B infections, and a quarter of those who don’t receive treatment will die from liver cirrhosis or cancer. There has been an increase in the incidence of new hepatitis B infections in some states because of opioid epidemic in the United States, according to MMWR reports.
The cost effectiveness of preventing hepatitis B with the vaccine and, when necessary, HBIG, is estimated at $2,600 per quality-adjusted year of life. The most common side effects reported after hepatitis B administration are pain (3%-29%), erythema (3%), swelling (3%), fever (1%-6%) and headache (3%).
There has been extensive analysis of the safety of hepatitis B vaccines, the policy statement indicated. Analysis of Vaccine Safety Datalink data has found no causal link between administration of the hepatitis B vaccine and the following: neonatal sepsis or death, rheumatoid arthritis, Bell’s palsy, autoimmune thyroid disease, hemolytic anemia in children, anaphylaxis, optic neuritis, Guillain-Barré syndrome, sudden-onset sensorineural hearing loss, or other chronic illnesses.
Specific recommendations
• Infants born to mothers who test positive for hepatitis B surface antigen (HBsAg): Administer the hepatitis B vaccine and HBIG within 12 hours of birth.
• Infants weighing at least 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine within 24 hours of birth.
• Infants weighing less than 2,000 g and born to mothers who are HBsAg negative: Administer the hepatitis B vaccine at hospital discharge or at age 1 month (whichever is first).
• Infants weighing at least 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and HBIG by hospital discharge or age 7 days (whichever is first) if HBsAg status remains unknown or is confirmed positive.
• Infants weighing less than 2,000 g and born to mothers with an unknown HBsAg status: Administer the hepatitis B vaccine within 12 hours of birth and then HBIG within 12 hours unless the mother tests negative for HBsAg by then.
FROM PEDIATRICS
Key clinical point: All infants should receive hepatitis B vaccine within 24 hours of birth.
Major finding: Hepatitis B vaccine prevents 75%-95% of perinatal hepatitis B infections.
Data source: A literature review of data on hepatitis B epidemiology in the United States.
Disclosures: The statement did not receive external funding, and the authors stated that they have no conflicts of interest.
How to reduce NICU transfers for asymptomatic hypoglycemia
NASHVILLE, TENN. – At the University of North Carolina at Chapel Hill, many infants who would previously have been transferred to the NICU for asymptomatic hypoglycemia now are staying with their moms, thanks to a new protocol that holds off on blood glucose testing until infants are fed for the first time and glucose homeostasis can begin.
Not too long ago, the university realized it had a problem that’s probably familiar to other institutions: Its system to monitor newborns at risk for hypoglycemia – those born to diabetic mothers, or who are small or large for gestational age – put too many infants with asymptomatic hypoglycemia into the NICU when they didn’t really need to be there.
Nurse practitioners “were tired of transferring babies they felt were responsive to feeding and did not actually require NICU care,” and “a growing number of families were unhappy with being separated from infants that were well-appearing and feeding well at a time when moms were trying to establish breast feeding and bonding. There was frustration with our protocol,” which “seemed rigid and outdated,” said Ashley Sutton, MD, a pediatric hospitalist at the university.
To fix the problem, Dr. Sutton and others on a multidisciplinary team implemented the American Academy of Pediatrics’ 2011 guidelines for monitoring glucose homeostasis in late-preterm and term newborns at-risk for hypoglycemia, with an additional mandate to initiate immediate, continual skin-to-skin contact at delivery (Pediatrics. 2011 Mar;127[3]:575-9).
Under the new system, children are fed with either their mom’s or a donor’s breast milk within an hour of birth, and the initial glucose check comes at 90 minutes; infants are transferred if blood glucose remains below 25 mg/dL after the second feeding. After 4 hours of life, glucose levels below 35 mg/dL trigger an evaluation for symptoms, not necessarily an automatic NICU transfer.
Labor and delivery nurses also are empowered “to immediately feed the baby no matter what number [they are] seeing,” Dr. Sutton said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The efforts have made a difference. The transfer rate for at-risk infants has fallen from 17% to 3%, and skin-to-skin contact is initiated within the first hour of life in 64%, up from 45%. Feeding of at-risk infants within the first hour has increased from 43% to 61%, and the first glucose check comes at an average of 97 minutes. The number of unnecessary NICU transfers of at-risk infants has fallen sharply.
Meanwhile, there’s been no increase in sepsis evaluations, adverse events, readmissions, and the rates of symptomatic hypoglycemia.
Dr. Sutton and her colleagues had no industry disclosures. The work was funded by the National Institutes of Health.
NASHVILLE, TENN. – At the University of North Carolina at Chapel Hill, many infants who would previously have been transferred to the NICU for asymptomatic hypoglycemia now are staying with their moms, thanks to a new protocol that holds off on blood glucose testing until infants are fed for the first time and glucose homeostasis can begin.
Not too long ago, the university realized it had a problem that’s probably familiar to other institutions: Its system to monitor newborns at risk for hypoglycemia – those born to diabetic mothers, or who are small or large for gestational age – put too many infants with asymptomatic hypoglycemia into the NICU when they didn’t really need to be there.
Nurse practitioners “were tired of transferring babies they felt were responsive to feeding and did not actually require NICU care,” and “a growing number of families were unhappy with being separated from infants that were well-appearing and feeding well at a time when moms were trying to establish breast feeding and bonding. There was frustration with our protocol,” which “seemed rigid and outdated,” said Ashley Sutton, MD, a pediatric hospitalist at the university.
To fix the problem, Dr. Sutton and others on a multidisciplinary team implemented the American Academy of Pediatrics’ 2011 guidelines for monitoring glucose homeostasis in late-preterm and term newborns at-risk for hypoglycemia, with an additional mandate to initiate immediate, continual skin-to-skin contact at delivery (Pediatrics. 2011 Mar;127[3]:575-9).
Under the new system, children are fed with either their mom’s or a donor’s breast milk within an hour of birth, and the initial glucose check comes at 90 minutes; infants are transferred if blood glucose remains below 25 mg/dL after the second feeding. After 4 hours of life, glucose levels below 35 mg/dL trigger an evaluation for symptoms, not necessarily an automatic NICU transfer.
Labor and delivery nurses also are empowered “to immediately feed the baby no matter what number [they are] seeing,” Dr. Sutton said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The efforts have made a difference. The transfer rate for at-risk infants has fallen from 17% to 3%, and skin-to-skin contact is initiated within the first hour of life in 64%, up from 45%. Feeding of at-risk infants within the first hour has increased from 43% to 61%, and the first glucose check comes at an average of 97 minutes. The number of unnecessary NICU transfers of at-risk infants has fallen sharply.
Meanwhile, there’s been no increase in sepsis evaluations, adverse events, readmissions, and the rates of symptomatic hypoglycemia.
Dr. Sutton and her colleagues had no industry disclosures. The work was funded by the National Institutes of Health.
NASHVILLE, TENN. – At the University of North Carolina at Chapel Hill, many infants who would previously have been transferred to the NICU for asymptomatic hypoglycemia now are staying with their moms, thanks to a new protocol that holds off on blood glucose testing until infants are fed for the first time and glucose homeostasis can begin.
Not too long ago, the university realized it had a problem that’s probably familiar to other institutions: Its system to monitor newborns at risk for hypoglycemia – those born to diabetic mothers, or who are small or large for gestational age – put too many infants with asymptomatic hypoglycemia into the NICU when they didn’t really need to be there.
Nurse practitioners “were tired of transferring babies they felt were responsive to feeding and did not actually require NICU care,” and “a growing number of families were unhappy with being separated from infants that were well-appearing and feeding well at a time when moms were trying to establish breast feeding and bonding. There was frustration with our protocol,” which “seemed rigid and outdated,” said Ashley Sutton, MD, a pediatric hospitalist at the university.
To fix the problem, Dr. Sutton and others on a multidisciplinary team implemented the American Academy of Pediatrics’ 2011 guidelines for monitoring glucose homeostasis in late-preterm and term newborns at-risk for hypoglycemia, with an additional mandate to initiate immediate, continual skin-to-skin contact at delivery (Pediatrics. 2011 Mar;127[3]:575-9).
Under the new system, children are fed with either their mom’s or a donor’s breast milk within an hour of birth, and the initial glucose check comes at 90 minutes; infants are transferred if blood glucose remains below 25 mg/dL after the second feeding. After 4 hours of life, glucose levels below 35 mg/dL trigger an evaluation for symptoms, not necessarily an automatic NICU transfer.
Labor and delivery nurses also are empowered “to immediately feed the baby no matter what number [they are] seeing,” Dr. Sutton said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The efforts have made a difference. The transfer rate for at-risk infants has fallen from 17% to 3%, and skin-to-skin contact is initiated within the first hour of life in 64%, up from 45%. Feeding of at-risk infants within the first hour has increased from 43% to 61%, and the first glucose check comes at an average of 97 minutes. The number of unnecessary NICU transfers of at-risk infants has fallen sharply.
Meanwhile, there’s been no increase in sepsis evaluations, adverse events, readmissions, and the rates of symptomatic hypoglycemia.
Dr. Sutton and her colleagues had no industry disclosures. The work was funded by the National Institutes of Health.
AT PHM 2017
Key clinical point:
Major finding: After making that and other changes, the transfer rate for at-risk infants at a major academic center fell from 17% to 3%, without an increase in rates of symptomatic hypoglycemia and adverse events.
Data source: Quality improvement project at the University of North Carolina at Chapel Hill.
Disclosures: The investigators had no financial disclosures. The work was funded by the National Institutes of Health.