User login
For MD-IQ use only
December 2020 - Quick Quiz Question 2
Q2. Correct answer: D
Rationale
Deficient intake of fiber and folate may originate in the food choice of the individual, whereas some deficiencies of intake, such as thiamine, appear to be celiac specific. The provider should encourage intake of nutrient-dense foods including wholegrain foods, enriched if possible, legumes, fruits, vegetables, lean meat, fish, chicken, and eggs. It is not necessary to prioritize micronutrient supplements over achieving nutritional adequacy through dietary intake. Iron deficiency is an effect of untreated celiac disease.
Reference
1. Shepherd SJ, Gibson PR. J Human Nutr Dietet. 2012;26:349-58.
Q2. Correct answer: D
Rationale
Deficient intake of fiber and folate may originate in the food choice of the individual, whereas some deficiencies of intake, such as thiamine, appear to be celiac specific. The provider should encourage intake of nutrient-dense foods including wholegrain foods, enriched if possible, legumes, fruits, vegetables, lean meat, fish, chicken, and eggs. It is not necessary to prioritize micronutrient supplements over achieving nutritional adequacy through dietary intake. Iron deficiency is an effect of untreated celiac disease.
Reference
1. Shepherd SJ, Gibson PR. J Human Nutr Dietet. 2012;26:349-58.
Q2. Correct answer: D
Rationale
Deficient intake of fiber and folate may originate in the food choice of the individual, whereas some deficiencies of intake, such as thiamine, appear to be celiac specific. The provider should encourage intake of nutrient-dense foods including wholegrain foods, enriched if possible, legumes, fruits, vegetables, lean meat, fish, chicken, and eggs. It is not necessary to prioritize micronutrient supplements over achieving nutritional adequacy through dietary intake. Iron deficiency is an effect of untreated celiac disease.
Reference
1. Shepherd SJ, Gibson PR. J Human Nutr Dietet. 2012;26:349-58.
Question 2
December 2020 - Quick Quiz Question 1
Correct answer: C
Rationale
According to the Multi-Society Task Force on Colorectal Cancer, colonoscopy should be performed 1 year after resection, and again 3 years later, in order to decrease the risk of metachronous colorectal cancer.
Reference
1. Kahi CJ, Boland CR, Dominitz JA. Gastroenterology. 2016. 150(3):758-68.e11.
Correct answer: C
Rationale
According to the Multi-Society Task Force on Colorectal Cancer, colonoscopy should be performed 1 year after resection, and again 3 years later, in order to decrease the risk of metachronous colorectal cancer.
Reference
1. Kahi CJ, Boland CR, Dominitz JA. Gastroenterology. 2016. 150(3):758-68.e11.
Correct answer: C
Rationale
According to the Multi-Society Task Force on Colorectal Cancer, colonoscopy should be performed 1 year after resection, and again 3 years later, in order to decrease the risk of metachronous colorectal cancer.
Reference
1. Kahi CJ, Boland CR, Dominitz JA. Gastroenterology. 2016. 150(3):758-68.e11.
You perform a colonoscopy for a patient who underwent sigmoid resection for stage 2 colorectal cancer 1 year ago. The colonoscopy reveals one diminutive adenoma in the cecum, which you remove with a cold snare.
Pigment traits, sun sensitivity associated with risk of non-Hodgkin lymphomas and chronic lymphocytic leukemia
Risk factors for keratinocyte carcinomas, primarily pigment traits and sun sensitivity, were associated with the risk of developing non-Hodgkin lymphomas (NHL) and chronic lymphocytic leukemia (CLL) in an analysis of 92,097 women in France.
The presence of “many or very many nevi [moles]” was particularly associated with the risk of CLL among individuals in the E3N cohort, according to a report published online in Cancer Medicine. E3N is a prospective cohort of French women aged 40-65 years at inclusion in 1990. Researchers collected cancer data at baseline and every 2-3 years.
Hazard ratios and 95% confidence intervals for associations between patients pigmentary traits and sun exposure and their risk for CLL/NHL were estimated using Cox models, according to study author Louis-Marie Garcin, MD, of the Université Paris-Saclay, Villejuif, and colleagues.
Common etiology?
Among the 92,097 women included in the study, 622 incident cases of CLL/NHL were observed over a median of 24-years’ follow-up.
The presence of nevi was associated with CLL/NHL risk. The HR for “many or very many nevi” relative to “no nevi” was 1.56. The association with number of nevi was strongest for the risk of CLL, with an HR for “many or very many nevi” of 3.00 vs. 1.32 for NHL. In addition, the researchers found that women whose skin was highly sensitive to sunburn also had a higher risk of CLL (HR, 1.96), while no increased risk of NHL was observed. All HR values were within their respective 95% confidence intervals.
Relevant characteristics that were found to not be associated with added CLL/NHL risk were skin or hair color, number of freckles, and average daily UV dose during spring and summer in the location of residence at birth or at inclusion.
These observations suggest that CLL in particular may share some constitutional risk factors with keratinocyte cancers, according to the researchers.
“We report an association between nevi frequency and CLL/NHL risk, suggesting a partly common genetic etiology of these tumors. Future research should investigate common pathophysiological pathways that could promote the development of both skin carcinoma and CLL/NHL,” the researchers concluded.
The study was sponsored by the French government. The authors stated that they had no conflicts of interest.
SOURCE: Garcin L-M et al. Cancer Med. 2020. doi: 10.1002/cam4.3586.
Risk factors for keratinocyte carcinomas, primarily pigment traits and sun sensitivity, were associated with the risk of developing non-Hodgkin lymphomas (NHL) and chronic lymphocytic leukemia (CLL) in an analysis of 92,097 women in France.
The presence of “many or very many nevi [moles]” was particularly associated with the risk of CLL among individuals in the E3N cohort, according to a report published online in Cancer Medicine. E3N is a prospective cohort of French women aged 40-65 years at inclusion in 1990. Researchers collected cancer data at baseline and every 2-3 years.
Hazard ratios and 95% confidence intervals for associations between patients pigmentary traits and sun exposure and their risk for CLL/NHL were estimated using Cox models, according to study author Louis-Marie Garcin, MD, of the Université Paris-Saclay, Villejuif, and colleagues.
Common etiology?
Among the 92,097 women included in the study, 622 incident cases of CLL/NHL were observed over a median of 24-years’ follow-up.
The presence of nevi was associated with CLL/NHL risk. The HR for “many or very many nevi” relative to “no nevi” was 1.56. The association with number of nevi was strongest for the risk of CLL, with an HR for “many or very many nevi” of 3.00 vs. 1.32 for NHL. In addition, the researchers found that women whose skin was highly sensitive to sunburn also had a higher risk of CLL (HR, 1.96), while no increased risk of NHL was observed. All HR values were within their respective 95% confidence intervals.
Relevant characteristics that were found to not be associated with added CLL/NHL risk were skin or hair color, number of freckles, and average daily UV dose during spring and summer in the location of residence at birth or at inclusion.
These observations suggest that CLL in particular may share some constitutional risk factors with keratinocyte cancers, according to the researchers.
“We report an association between nevi frequency and CLL/NHL risk, suggesting a partly common genetic etiology of these tumors. Future research should investigate common pathophysiological pathways that could promote the development of both skin carcinoma and CLL/NHL,” the researchers concluded.
The study was sponsored by the French government. The authors stated that they had no conflicts of interest.
SOURCE: Garcin L-M et al. Cancer Med. 2020. doi: 10.1002/cam4.3586.
Risk factors for keratinocyte carcinomas, primarily pigment traits and sun sensitivity, were associated with the risk of developing non-Hodgkin lymphomas (NHL) and chronic lymphocytic leukemia (CLL) in an analysis of 92,097 women in France.
The presence of “many or very many nevi [moles]” was particularly associated with the risk of CLL among individuals in the E3N cohort, according to a report published online in Cancer Medicine. E3N is a prospective cohort of French women aged 40-65 years at inclusion in 1990. Researchers collected cancer data at baseline and every 2-3 years.
Hazard ratios and 95% confidence intervals for associations between patients pigmentary traits and sun exposure and their risk for CLL/NHL were estimated using Cox models, according to study author Louis-Marie Garcin, MD, of the Université Paris-Saclay, Villejuif, and colleagues.
Common etiology?
Among the 92,097 women included in the study, 622 incident cases of CLL/NHL were observed over a median of 24-years’ follow-up.
The presence of nevi was associated with CLL/NHL risk. The HR for “many or very many nevi” relative to “no nevi” was 1.56. The association with number of nevi was strongest for the risk of CLL, with an HR for “many or very many nevi” of 3.00 vs. 1.32 for NHL. In addition, the researchers found that women whose skin was highly sensitive to sunburn also had a higher risk of CLL (HR, 1.96), while no increased risk of NHL was observed. All HR values were within their respective 95% confidence intervals.
Relevant characteristics that were found to not be associated with added CLL/NHL risk were skin or hair color, number of freckles, and average daily UV dose during spring and summer in the location of residence at birth or at inclusion.
These observations suggest that CLL in particular may share some constitutional risk factors with keratinocyte cancers, according to the researchers.
“We report an association between nevi frequency and CLL/NHL risk, suggesting a partly common genetic etiology of these tumors. Future research should investigate common pathophysiological pathways that could promote the development of both skin carcinoma and CLL/NHL,” the researchers concluded.
The study was sponsored by the French government. The authors stated that they had no conflicts of interest.
SOURCE: Garcin L-M et al. Cancer Med. 2020. doi: 10.1002/cam4.3586.
FROM CANCER MEDICINE
Photosensitivity diagnosis made simple
of the University of Southern California, Los Angeles.
“When a patient comes in who makes you suspect a photosensitivity, there will be two different presentations,” he said in a virtual presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
In some cases, the patient presents with a reaction they believe is sun related, although they don’t have a rash currently, he said. In other cases, “you as a good clinician suspect photosensitivity because the eruption is in a photo distribution,” although the patient may or may not relate it to sun exposure, he added.
Dr. DeLeo noted a few key points to include when taking the history in patients with likely photosensitivity, whether or not they present with a rash.
“I always ask patients when did the episode occur? Is it chronic?” Also ask about timing: Does the reaction occur in the sun, or later? Does it occur quickly and go away within hours, or occur within days or weeks of exposure?
“Always take a good drug history, as photosensitivity can often be related to drugs,” Dr. DeLeo noted. For example, approximately 50% of individuals on amiodarone will have some type of photosensitivity, he said.
Other drug-induced photosensitive conditions include drug-induced subacute cutaneous lupus and pseudoporphyria from NSAIDs, as well as hyperpigmentation from diltiazem, which most often occurs in Black women, he said.
“Photodrug reactions are usually related to UVA radiation, and that is important because you can develop it through the window while driving in your car”: The car windows do not protect against UVA, Dr. DeLeo said. If you have a patient who tells you about a photosensitivity or has a rash and they are on a photosensitizing drug, first rule out connective tissue disease, then discontinue the drug in collaboration with the patient’s internist and wait for the reaction to disappear, and it should, he said.
Some photosensitivity rashes have characteristic patterns, notably connective tissue disease patterns in lupus and dermatomyositis patients, bullous eruptions in cases of porphyria or phototoxic contact dermatitis, and eczematous eruptions, Dr. DeLeo noted.
Patients who present without a rash, but report a history of a reaction that they believe is related to sun exposure, fall into two categories: some had a rash that occurred while in the sun and disappeared quickly, and some had one that occurred hours or days after exposure and lasted a few days to weeks, said Dr. DeLeo.
The differential diagnosis in the patient with immediate photosensitivity is fairly clear: These patients usually have solar urticaria, he said. However, some lupus patients may report this reaction so it is important to rule out connective tissue disease. The diagnosis can be made with phototesting or do a simple test by having the patient sit out in the sunshine, he said.
For the patient who has a delayed reactivity after sun exposure, and doesn’t have the reaction when they come to the office, the differential diagnosis in a simply applied way is that, if the reaction spared the face, it is likely polymorphous light eruption (PMLE); but if the face is involved, the patient likely has photoallergic contact dermatitis, Dr. DeLeo explained. However, always consider the alternatives of connective tissue disease, drug reactions, and contact dermatitis that is not photoallergic, he noted.
PMLE “is the most common photosensitivity reaction that we see in the United States,” and it almost always occurs when people are away from home, usually on vacation, said Dr. DeLeo. The differential diagnosis for patients with recurrent or delayed rash involving the face could be photoallergic contact dermatitis, but rule out airborne contact dermatitis, personal care product contact dermatitis, and chronic actinic dermatitis, he said. A work-up for these patients could include a photo test, photopatch test, or patch test.
Dr. DeLeo disclosed serving as a consultant for Estee Lauder.
MedscapeLive and this news organization are owned by the same parent company.
of the University of Southern California, Los Angeles.
“When a patient comes in who makes you suspect a photosensitivity, there will be two different presentations,” he said in a virtual presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
In some cases, the patient presents with a reaction they believe is sun related, although they don’t have a rash currently, he said. In other cases, “you as a good clinician suspect photosensitivity because the eruption is in a photo distribution,” although the patient may or may not relate it to sun exposure, he added.
Dr. DeLeo noted a few key points to include when taking the history in patients with likely photosensitivity, whether or not they present with a rash.
“I always ask patients when did the episode occur? Is it chronic?” Also ask about timing: Does the reaction occur in the sun, or later? Does it occur quickly and go away within hours, or occur within days or weeks of exposure?
“Always take a good drug history, as photosensitivity can often be related to drugs,” Dr. DeLeo noted. For example, approximately 50% of individuals on amiodarone will have some type of photosensitivity, he said.
Other drug-induced photosensitive conditions include drug-induced subacute cutaneous lupus and pseudoporphyria from NSAIDs, as well as hyperpigmentation from diltiazem, which most often occurs in Black women, he said.
“Photodrug reactions are usually related to UVA radiation, and that is important because you can develop it through the window while driving in your car”: The car windows do not protect against UVA, Dr. DeLeo said. If you have a patient who tells you about a photosensitivity or has a rash and they are on a photosensitizing drug, first rule out connective tissue disease, then discontinue the drug in collaboration with the patient’s internist and wait for the reaction to disappear, and it should, he said.
Some photosensitivity rashes have characteristic patterns, notably connective tissue disease patterns in lupus and dermatomyositis patients, bullous eruptions in cases of porphyria or phototoxic contact dermatitis, and eczematous eruptions, Dr. DeLeo noted.
Patients who present without a rash, but report a history of a reaction that they believe is related to sun exposure, fall into two categories: some had a rash that occurred while in the sun and disappeared quickly, and some had one that occurred hours or days after exposure and lasted a few days to weeks, said Dr. DeLeo.
The differential diagnosis in the patient with immediate photosensitivity is fairly clear: These patients usually have solar urticaria, he said. However, some lupus patients may report this reaction so it is important to rule out connective tissue disease. The diagnosis can be made with phototesting or do a simple test by having the patient sit out in the sunshine, he said.
For the patient who has a delayed reactivity after sun exposure, and doesn’t have the reaction when they come to the office, the differential diagnosis in a simply applied way is that, if the reaction spared the face, it is likely polymorphous light eruption (PMLE); but if the face is involved, the patient likely has photoallergic contact dermatitis, Dr. DeLeo explained. However, always consider the alternatives of connective tissue disease, drug reactions, and contact dermatitis that is not photoallergic, he noted.
PMLE “is the most common photosensitivity reaction that we see in the United States,” and it almost always occurs when people are away from home, usually on vacation, said Dr. DeLeo. The differential diagnosis for patients with recurrent or delayed rash involving the face could be photoallergic contact dermatitis, but rule out airborne contact dermatitis, personal care product contact dermatitis, and chronic actinic dermatitis, he said. A work-up for these patients could include a photo test, photopatch test, or patch test.
Dr. DeLeo disclosed serving as a consultant for Estee Lauder.
MedscapeLive and this news organization are owned by the same parent company.
of the University of Southern California, Los Angeles.
“When a patient comes in who makes you suspect a photosensitivity, there will be two different presentations,” he said in a virtual presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
In some cases, the patient presents with a reaction they believe is sun related, although they don’t have a rash currently, he said. In other cases, “you as a good clinician suspect photosensitivity because the eruption is in a photo distribution,” although the patient may or may not relate it to sun exposure, he added.
Dr. DeLeo noted a few key points to include when taking the history in patients with likely photosensitivity, whether or not they present with a rash.
“I always ask patients when did the episode occur? Is it chronic?” Also ask about timing: Does the reaction occur in the sun, or later? Does it occur quickly and go away within hours, or occur within days or weeks of exposure?
“Always take a good drug history, as photosensitivity can often be related to drugs,” Dr. DeLeo noted. For example, approximately 50% of individuals on amiodarone will have some type of photosensitivity, he said.
Other drug-induced photosensitive conditions include drug-induced subacute cutaneous lupus and pseudoporphyria from NSAIDs, as well as hyperpigmentation from diltiazem, which most often occurs in Black women, he said.
“Photodrug reactions are usually related to UVA radiation, and that is important because you can develop it through the window while driving in your car”: The car windows do not protect against UVA, Dr. DeLeo said. If you have a patient who tells you about a photosensitivity or has a rash and they are on a photosensitizing drug, first rule out connective tissue disease, then discontinue the drug in collaboration with the patient’s internist and wait for the reaction to disappear, and it should, he said.
Some photosensitivity rashes have characteristic patterns, notably connective tissue disease patterns in lupus and dermatomyositis patients, bullous eruptions in cases of porphyria or phototoxic contact dermatitis, and eczematous eruptions, Dr. DeLeo noted.
Patients who present without a rash, but report a history of a reaction that they believe is related to sun exposure, fall into two categories: some had a rash that occurred while in the sun and disappeared quickly, and some had one that occurred hours or days after exposure and lasted a few days to weeks, said Dr. DeLeo.
The differential diagnosis in the patient with immediate photosensitivity is fairly clear: These patients usually have solar urticaria, he said. However, some lupus patients may report this reaction so it is important to rule out connective tissue disease. The diagnosis can be made with phototesting or do a simple test by having the patient sit out in the sunshine, he said.
For the patient who has a delayed reactivity after sun exposure, and doesn’t have the reaction when they come to the office, the differential diagnosis in a simply applied way is that, if the reaction spared the face, it is likely polymorphous light eruption (PMLE); but if the face is involved, the patient likely has photoallergic contact dermatitis, Dr. DeLeo explained. However, always consider the alternatives of connective tissue disease, drug reactions, and contact dermatitis that is not photoallergic, he noted.
PMLE “is the most common photosensitivity reaction that we see in the United States,” and it almost always occurs when people are away from home, usually on vacation, said Dr. DeLeo. The differential diagnosis for patients with recurrent or delayed rash involving the face could be photoallergic contact dermatitis, but rule out airborne contact dermatitis, personal care product contact dermatitis, and chronic actinic dermatitis, he said. A work-up for these patients could include a photo test, photopatch test, or patch test.
Dr. DeLeo disclosed serving as a consultant for Estee Lauder.
MedscapeLive and this news organization are owned by the same parent company.
FROM MEDSCAPELIVE LAS VEGAS DERMATOLOGY SEMINAR
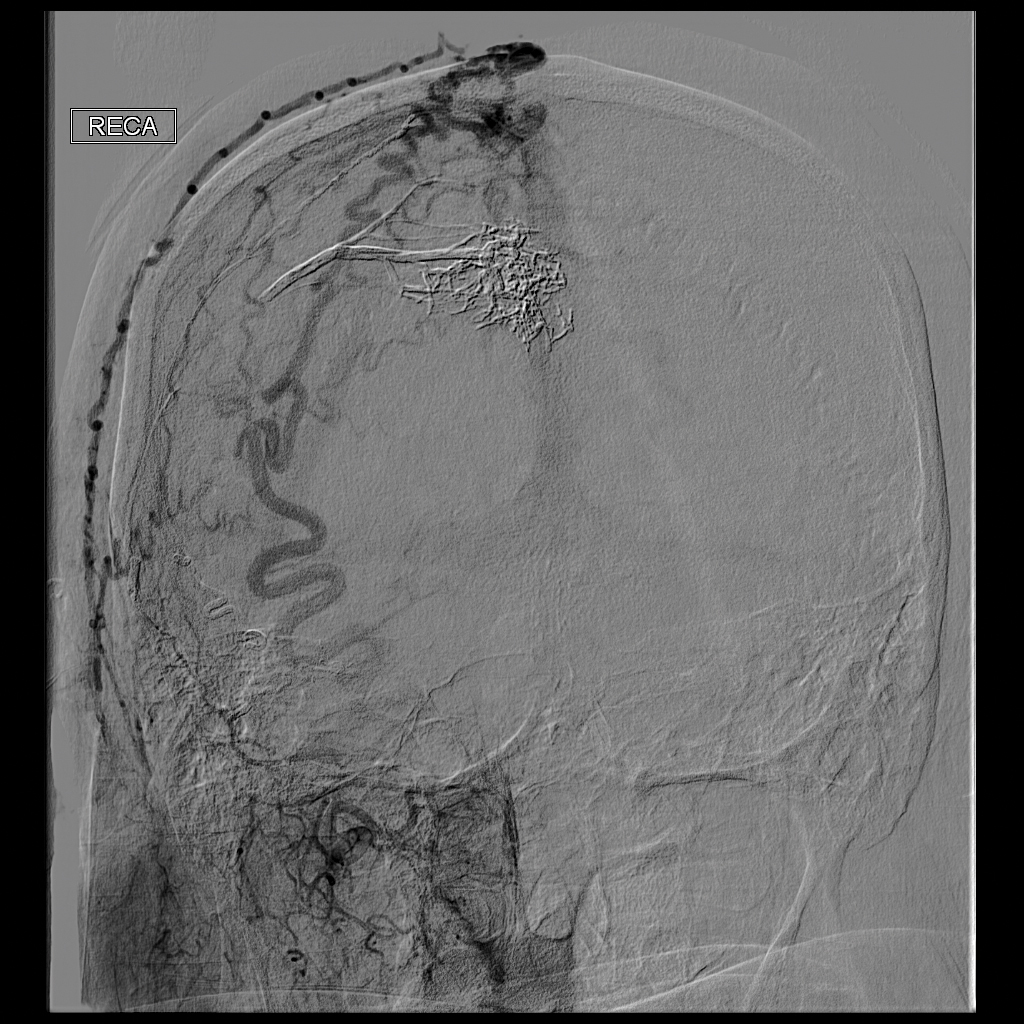
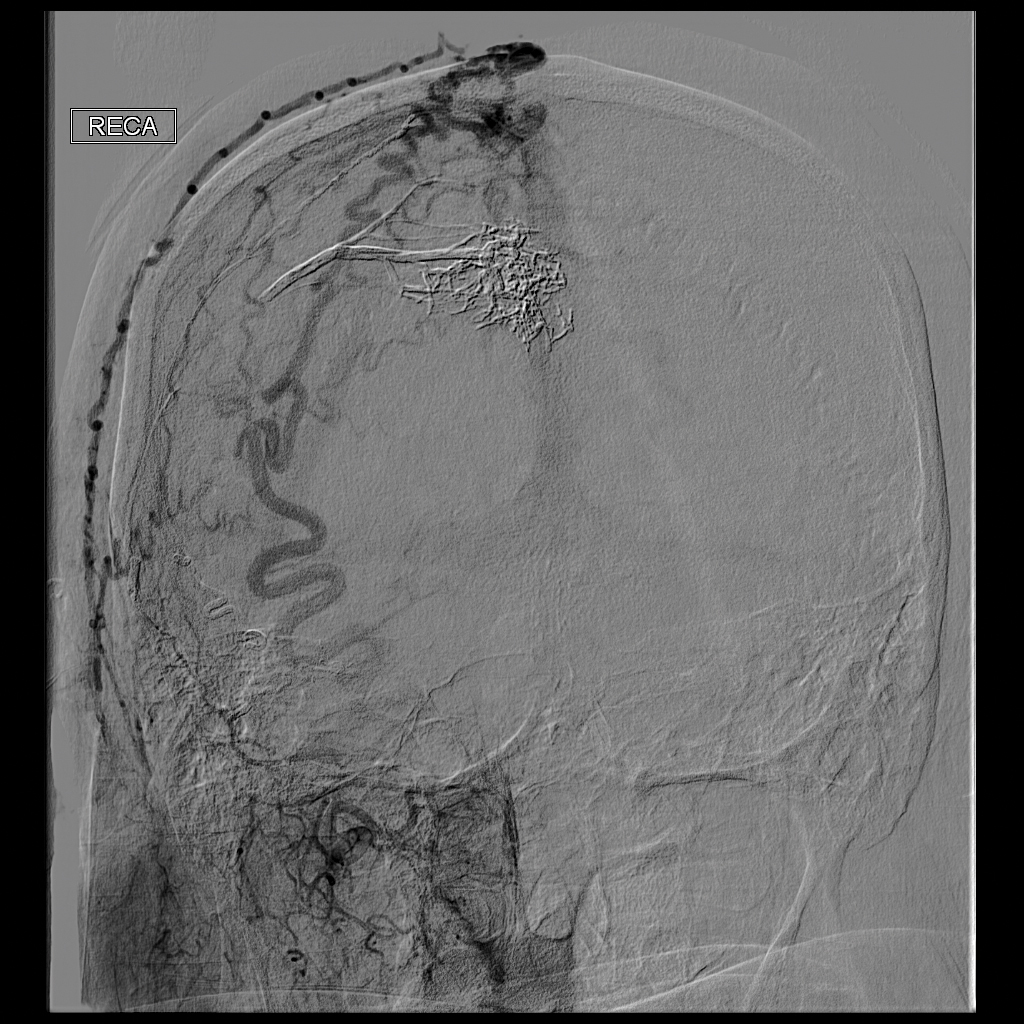
Scalp Arteriovenous Fistula With Intracranial Communication
To the Editor:
A 71-year-old man presented with a nodule on the vertex of the scalp of 1 year’s duration. The lesion had become soft and tender during the week prior to presentation. He noted that he was experiencing headaches and a buzzing sound in his head. He denied all other neurologic symptoms. The patient was given amoxicillin from a primary care physician and was referred to our institution for evaluation of a presumed inflamed cyst.
The patient’s medical history included an intracranial arteriovenous fistula (AVF) treated with endovascular embolization 1 year prior to presentation, 2 substantial falls in childhood with head trauma and loss of consciousness, essential hypertension, and an aortic aneurysm. His medications included amlodipine, lisinopril, amoxicillin, a multivitamin, and grape seed extract.
Physical examination revealed a 2-cm, pink, somewhat rubbery, subcutaneous, nonmobile nodule on the vertex of the scalp (Figure 1). The lesion was not consistent with a common pilar cyst, and an excisional biopsy was performed to exclude malignancy. Upon superficial incision, the lesion bled moderately, and the procedure was immediately discontinued. Hemostasis was obtained, and the patient was sent for ultrasonography of the lesion.

Ultrasonography demonstrated a small hypoechoic nodule measuring up to 0.5 cm containing a tangle of vessels in the subcutaneous soft tissue corresponding to the palpable abnormality. A cerebral angiogram demonstrated a dural AVF of the superior sagittal sinus with multifocal supply that connected with this scalp nodule (Figure 2). The patient was treated by interventional neuroradiology with endovascular embolization, which resulted in complete resolution of the scalp nodule.
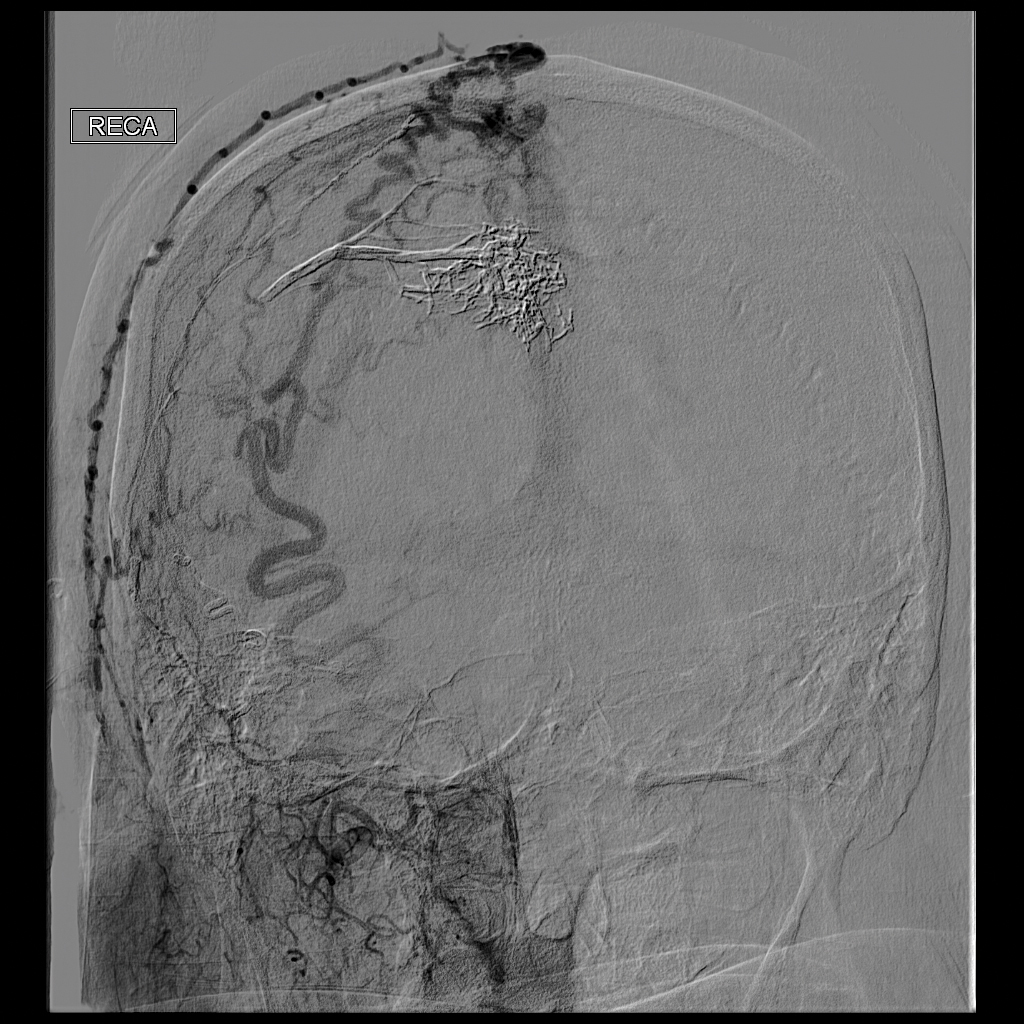
Scalp arteriovenous fistulas (S-AVFs) are characterized by abnormal connections between supplying arteries and draining veins in the subcutaneous plane of the scalp.1,2 The veins of an S-AVF undergo progressive aneurysmal dilatation from abnormal hemodynamics.1-3 Scalp arteriovenous fistulas are rare and may present as either an innocuous-looking scalp nodule or a progressively enlarging pulsatile mass on the scalp.2-4 Associated symptoms often include headache, local pain, bruits, tinnitus, and thrill.1,3,4 Recurrent hemorrhage, scalp necrosis, congestive heart failure, epilepsy, mental retardation, and intracranial ischemia also may occur.4
Scalp AVFs may occur with or without intracranial communication.4 Spontaneous S-AVFs with intracranial communication are uncommon, and their etiology is unclear. They may form as congenital malformations or may be idiopathic. Factors increasing circulation through the S-AVF such as trauma, pregnancy, hormonal changes, and inflammation prompt the development of symptoms.4 Scalp AVFs also may be caused by trauma.3 Scalp AVFs without intracranial communication have been reported following hair transplantation.1 Scalp AVFs with intracranial communication have been reported months to years after skull fracture or craniotomy.2 True spontaneous S-AVFs are difficult to differentiate from traumatic S-AVFs other than by history alone.2
Increased venous pressure has been shown to generate AVFs in rats.5 It has been suggested that S-AVFs can become enlarged by capturing subcutaneous or intracranial feeder vessels and that the consequent hemodynamic stress may induce de novo aneurysms in S-AVFs. Additionally, intracranial AVFs may alter the intracranial hemodynamics, leading to increased venous pressure in the superior sagittal sinus and the formation of communicating S-AVFs.5 Interestingly, our patient had an intracranial AVF treated with endovascular embolization 1 year prior to the formation of the S-AVF. An angiogram at the time of this embolization procedure did not demonstrate any S-AVFs. Furthermore, our patient has a history of 2 substantial falls in childhood with head trauma and loss of consciousness. Perhaps these traumas initiated a channel through the cranium where an S-AVF with intracranial communication was able to form and may have only become clinically or radiographically detectable once it enlarged due to the altered hemodynamics caused by the intracranial AVF 1 year prior.
The diagnosis of an S-AVF is confirmed with imaging studies. Doppler ultrasonography initially will help to detect that a lesion is vascular in nature. Intra-arterial digital subtraction angiography is the gold-standard imaging technique and is necessary to delineate the feeding arteries and the draining channels as well as possible communication with intracranial vasculature.1,2 There is controversy regarding the appropriate treatment of S-AVFs.2 Each S-AVF possesses unique anatomic features that dictate appropriate management. The prognosis for an S-AVF is extremely variable, and the decision to treat is based on the patient’s symptoms and risk for exsanguinating hemorrhage.2,4 Neurosurgical approaches include ligation of the feeding arteries, surgical resection, electrothrombosis, direct intralesional injection of sclerosing agents, and endovascular embolization. Endovascular intervention increasingly is utilized as a primary treatment or as a preoperative adjunct to surgery.2,4 Large S-AVFs have a high risk for recurrence after treatment with endovascular embolization alone. In cases with intracranial communication, the intracranial component is treated first.2
This case emphasizes the importance of including S-AVFs on the dermatologic differential diagnosis of a scalp nodule, especially in patients with any history of intracranial AVF. A thorough history, detailed intake of potential signs and symptoms of AVF, and palpation for bruits is recommended as part of the surgical evaluation of a scalp nodule. Imaging of scalp nodules also should be considered for patients with any history of intracranial AVF; S-AVFs should be referred to neurosurgery or interventional neuroradiology for evaluation and possible treatment.
- Bernstein J, Podnos S, Leavitt M. Arteriovenous fistula following hair transplantation. Dermatol Surg. 2011;37:873-875.
- Kumar R, Sharma G, Sharma BS. Management of scalp arterio-venous malformation: case series and review of literature. Br J Neurosurg. 2012;26:371-377.
- Gurkanlar D, Gonul M, Solmaz I, et al. Cirsoid aneurysms of the scalp. Neurosurg Rev. 2006;29:208-212.
- Senoglu M, Yasim A, Gokce M, et al. Nontraumatic scalp arteriovenous fistula in an adult: technical report on an illustrative case. Surg Neurol. 2008;70:194-197.
- Lanzino G, Passacantilli E, Lemole G, et al. Scalp arteriovenous malformation draining into the superior sagittal sinus associated with an intracranial arteriovenous malformation: just a coincidence? case report. Neurosurgery. 2003;52:440-443.
To the Editor:
A 71-year-old man presented with a nodule on the vertex of the scalp of 1 year’s duration. The lesion had become soft and tender during the week prior to presentation. He noted that he was experiencing headaches and a buzzing sound in his head. He denied all other neurologic symptoms. The patient was given amoxicillin from a primary care physician and was referred to our institution for evaluation of a presumed inflamed cyst.
The patient’s medical history included an intracranial arteriovenous fistula (AVF) treated with endovascular embolization 1 year prior to presentation, 2 substantial falls in childhood with head trauma and loss of consciousness, essential hypertension, and an aortic aneurysm. His medications included amlodipine, lisinopril, amoxicillin, a multivitamin, and grape seed extract.
Physical examination revealed a 2-cm, pink, somewhat rubbery, subcutaneous, nonmobile nodule on the vertex of the scalp (Figure 1). The lesion was not consistent with a common pilar cyst, and an excisional biopsy was performed to exclude malignancy. Upon superficial incision, the lesion bled moderately, and the procedure was immediately discontinued. Hemostasis was obtained, and the patient was sent for ultrasonography of the lesion.

Ultrasonography demonstrated a small hypoechoic nodule measuring up to 0.5 cm containing a tangle of vessels in the subcutaneous soft tissue corresponding to the palpable abnormality. A cerebral angiogram demonstrated a dural AVF of the superior sagittal sinus with multifocal supply that connected with this scalp nodule (Figure 2). The patient was treated by interventional neuroradiology with endovascular embolization, which resulted in complete resolution of the scalp nodule.
Scalp arteriovenous fistulas (S-AVFs) are characterized by abnormal connections between supplying arteries and draining veins in the subcutaneous plane of the scalp.1,2 The veins of an S-AVF undergo progressive aneurysmal dilatation from abnormal hemodynamics.1-3 Scalp arteriovenous fistulas are rare and may present as either an innocuous-looking scalp nodule or a progressively enlarging pulsatile mass on the scalp.2-4 Associated symptoms often include headache, local pain, bruits, tinnitus, and thrill.1,3,4 Recurrent hemorrhage, scalp necrosis, congestive heart failure, epilepsy, mental retardation, and intracranial ischemia also may occur.4
Scalp AVFs may occur with or without intracranial communication.4 Spontaneous S-AVFs with intracranial communication are uncommon, and their etiology is unclear. They may form as congenital malformations or may be idiopathic. Factors increasing circulation through the S-AVF such as trauma, pregnancy, hormonal changes, and inflammation prompt the development of symptoms.4 Scalp AVFs also may be caused by trauma.3 Scalp AVFs without intracranial communication have been reported following hair transplantation.1 Scalp AVFs with intracranial communication have been reported months to years after skull fracture or craniotomy.2 True spontaneous S-AVFs are difficult to differentiate from traumatic S-AVFs other than by history alone.2
Increased venous pressure has been shown to generate AVFs in rats.5 It has been suggested that S-AVFs can become enlarged by capturing subcutaneous or intracranial feeder vessels and that the consequent hemodynamic stress may induce de novo aneurysms in S-AVFs. Additionally, intracranial AVFs may alter the intracranial hemodynamics, leading to increased venous pressure in the superior sagittal sinus and the formation of communicating S-AVFs.5 Interestingly, our patient had an intracranial AVF treated with endovascular embolization 1 year prior to the formation of the S-AVF. An angiogram at the time of this embolization procedure did not demonstrate any S-AVFs. Furthermore, our patient has a history of 2 substantial falls in childhood with head trauma and loss of consciousness. Perhaps these traumas initiated a channel through the cranium where an S-AVF with intracranial communication was able to form and may have only become clinically or radiographically detectable once it enlarged due to the altered hemodynamics caused by the intracranial AVF 1 year prior.
The diagnosis of an S-AVF is confirmed with imaging studies. Doppler ultrasonography initially will help to detect that a lesion is vascular in nature. Intra-arterial digital subtraction angiography is the gold-standard imaging technique and is necessary to delineate the feeding arteries and the draining channels as well as possible communication with intracranial vasculature.1,2 There is controversy regarding the appropriate treatment of S-AVFs.2 Each S-AVF possesses unique anatomic features that dictate appropriate management. The prognosis for an S-AVF is extremely variable, and the decision to treat is based on the patient’s symptoms and risk for exsanguinating hemorrhage.2,4 Neurosurgical approaches include ligation of the feeding arteries, surgical resection, electrothrombosis, direct intralesional injection of sclerosing agents, and endovascular embolization. Endovascular intervention increasingly is utilized as a primary treatment or as a preoperative adjunct to surgery.2,4 Large S-AVFs have a high risk for recurrence after treatment with endovascular embolization alone. In cases with intracranial communication, the intracranial component is treated first.2
This case emphasizes the importance of including S-AVFs on the dermatologic differential diagnosis of a scalp nodule, especially in patients with any history of intracranial AVF. A thorough history, detailed intake of potential signs and symptoms of AVF, and palpation for bruits is recommended as part of the surgical evaluation of a scalp nodule. Imaging of scalp nodules also should be considered for patients with any history of intracranial AVF; S-AVFs should be referred to neurosurgery or interventional neuroradiology for evaluation and possible treatment.
To the Editor:
A 71-year-old man presented with a nodule on the vertex of the scalp of 1 year’s duration. The lesion had become soft and tender during the week prior to presentation. He noted that he was experiencing headaches and a buzzing sound in his head. He denied all other neurologic symptoms. The patient was given amoxicillin from a primary care physician and was referred to our institution for evaluation of a presumed inflamed cyst.
The patient’s medical history included an intracranial arteriovenous fistula (AVF) treated with endovascular embolization 1 year prior to presentation, 2 substantial falls in childhood with head trauma and loss of consciousness, essential hypertension, and an aortic aneurysm. His medications included amlodipine, lisinopril, amoxicillin, a multivitamin, and grape seed extract.
Physical examination revealed a 2-cm, pink, somewhat rubbery, subcutaneous, nonmobile nodule on the vertex of the scalp (Figure 1). The lesion was not consistent with a common pilar cyst, and an excisional biopsy was performed to exclude malignancy. Upon superficial incision, the lesion bled moderately, and the procedure was immediately discontinued. Hemostasis was obtained, and the patient was sent for ultrasonography of the lesion.

Ultrasonography demonstrated a small hypoechoic nodule measuring up to 0.5 cm containing a tangle of vessels in the subcutaneous soft tissue corresponding to the palpable abnormality. A cerebral angiogram demonstrated a dural AVF of the superior sagittal sinus with multifocal supply that connected with this scalp nodule (Figure 2). The patient was treated by interventional neuroradiology with endovascular embolization, which resulted in complete resolution of the scalp nodule.
Scalp arteriovenous fistulas (S-AVFs) are characterized by abnormal connections between supplying arteries and draining veins in the subcutaneous plane of the scalp.1,2 The veins of an S-AVF undergo progressive aneurysmal dilatation from abnormal hemodynamics.1-3 Scalp arteriovenous fistulas are rare and may present as either an innocuous-looking scalp nodule or a progressively enlarging pulsatile mass on the scalp.2-4 Associated symptoms often include headache, local pain, bruits, tinnitus, and thrill.1,3,4 Recurrent hemorrhage, scalp necrosis, congestive heart failure, epilepsy, mental retardation, and intracranial ischemia also may occur.4
Scalp AVFs may occur with or without intracranial communication.4 Spontaneous S-AVFs with intracranial communication are uncommon, and their etiology is unclear. They may form as congenital malformations or may be idiopathic. Factors increasing circulation through the S-AVF such as trauma, pregnancy, hormonal changes, and inflammation prompt the development of symptoms.4 Scalp AVFs also may be caused by trauma.3 Scalp AVFs without intracranial communication have been reported following hair transplantation.1 Scalp AVFs with intracranial communication have been reported months to years after skull fracture or craniotomy.2 True spontaneous S-AVFs are difficult to differentiate from traumatic S-AVFs other than by history alone.2
Increased venous pressure has been shown to generate AVFs in rats.5 It has been suggested that S-AVFs can become enlarged by capturing subcutaneous or intracranial feeder vessels and that the consequent hemodynamic stress may induce de novo aneurysms in S-AVFs. Additionally, intracranial AVFs may alter the intracranial hemodynamics, leading to increased venous pressure in the superior sagittal sinus and the formation of communicating S-AVFs.5 Interestingly, our patient had an intracranial AVF treated with endovascular embolization 1 year prior to the formation of the S-AVF. An angiogram at the time of this embolization procedure did not demonstrate any S-AVFs. Furthermore, our patient has a history of 2 substantial falls in childhood with head trauma and loss of consciousness. Perhaps these traumas initiated a channel through the cranium where an S-AVF with intracranial communication was able to form and may have only become clinically or radiographically detectable once it enlarged due to the altered hemodynamics caused by the intracranial AVF 1 year prior.
The diagnosis of an S-AVF is confirmed with imaging studies. Doppler ultrasonography initially will help to detect that a lesion is vascular in nature. Intra-arterial digital subtraction angiography is the gold-standard imaging technique and is necessary to delineate the feeding arteries and the draining channels as well as possible communication with intracranial vasculature.1,2 There is controversy regarding the appropriate treatment of S-AVFs.2 Each S-AVF possesses unique anatomic features that dictate appropriate management. The prognosis for an S-AVF is extremely variable, and the decision to treat is based on the patient’s symptoms and risk for exsanguinating hemorrhage.2,4 Neurosurgical approaches include ligation of the feeding arteries, surgical resection, electrothrombosis, direct intralesional injection of sclerosing agents, and endovascular embolization. Endovascular intervention increasingly is utilized as a primary treatment or as a preoperative adjunct to surgery.2,4 Large S-AVFs have a high risk for recurrence after treatment with endovascular embolization alone. In cases with intracranial communication, the intracranial component is treated first.2
This case emphasizes the importance of including S-AVFs on the dermatologic differential diagnosis of a scalp nodule, especially in patients with any history of intracranial AVF. A thorough history, detailed intake of potential signs and symptoms of AVF, and palpation for bruits is recommended as part of the surgical evaluation of a scalp nodule. Imaging of scalp nodules also should be considered for patients with any history of intracranial AVF; S-AVFs should be referred to neurosurgery or interventional neuroradiology for evaluation and possible treatment.
- Bernstein J, Podnos S, Leavitt M. Arteriovenous fistula following hair transplantation. Dermatol Surg. 2011;37:873-875.
- Kumar R, Sharma G, Sharma BS. Management of scalp arterio-venous malformation: case series and review of literature. Br J Neurosurg. 2012;26:371-377.
- Gurkanlar D, Gonul M, Solmaz I, et al. Cirsoid aneurysms of the scalp. Neurosurg Rev. 2006;29:208-212.
- Senoglu M, Yasim A, Gokce M, et al. Nontraumatic scalp arteriovenous fistula in an adult: technical report on an illustrative case. Surg Neurol. 2008;70:194-197.
- Lanzino G, Passacantilli E, Lemole G, et al. Scalp arteriovenous malformation draining into the superior sagittal sinus associated with an intracranial arteriovenous malformation: just a coincidence? case report. Neurosurgery. 2003;52:440-443.
- Bernstein J, Podnos S, Leavitt M. Arteriovenous fistula following hair transplantation. Dermatol Surg. 2011;37:873-875.
- Kumar R, Sharma G, Sharma BS. Management of scalp arterio-venous malformation: case series and review of literature. Br J Neurosurg. 2012;26:371-377.
- Gurkanlar D, Gonul M, Solmaz I, et al. Cirsoid aneurysms of the scalp. Neurosurg Rev. 2006;29:208-212.
- Senoglu M, Yasim A, Gokce M, et al. Nontraumatic scalp arteriovenous fistula in an adult: technical report on an illustrative case. Surg Neurol. 2008;70:194-197.
- Lanzino G, Passacantilli E, Lemole G, et al. Scalp arteriovenous malformation draining into the superior sagittal sinus associated with an intracranial arteriovenous malformation: just a coincidence? case report. Neurosurgery. 2003;52:440-443.
Practice Points
- Scalp arteriovenous fistulas may be traumatic or spontaneous and present as either an innocuous-looking scalp nodule or as a progressively enlarging pulsatile mass on the scalp.
- Clinical detection followed by appropriate imaging and referral to neurosurgery or interventional neuroradiology is vital to patient safety.
@GiJournal: An online platform to discuss the latest gastroenterology and hepatology publications
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
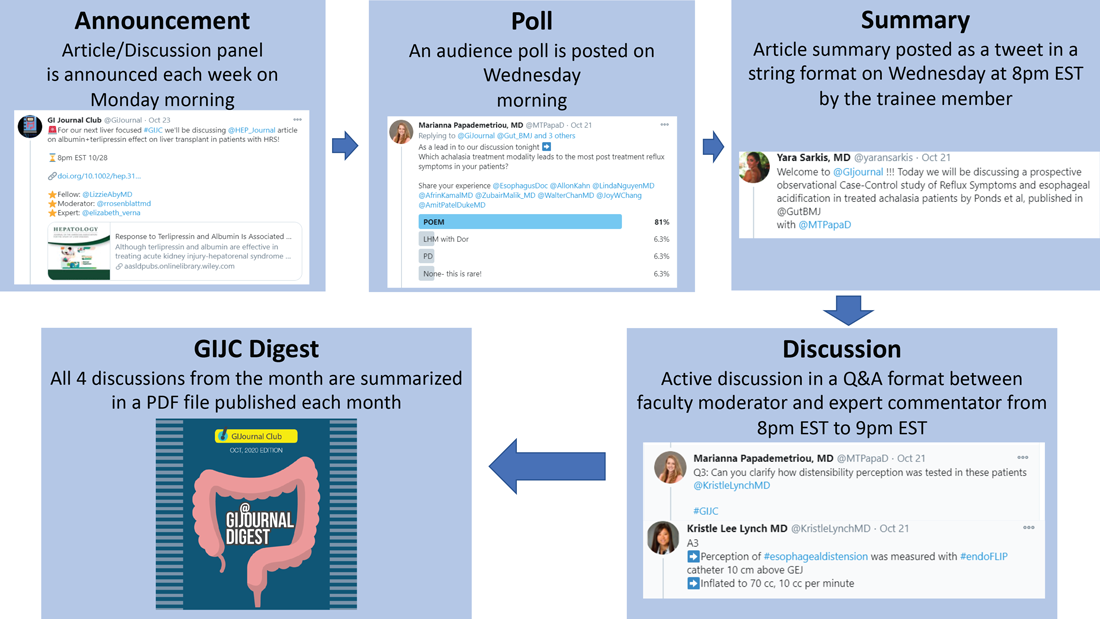
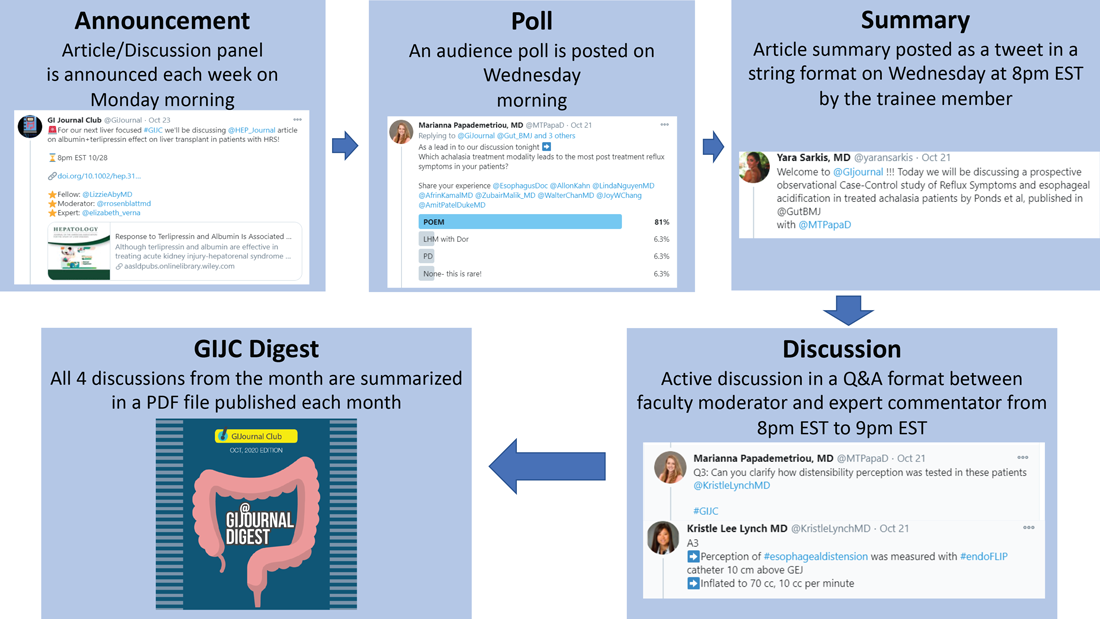
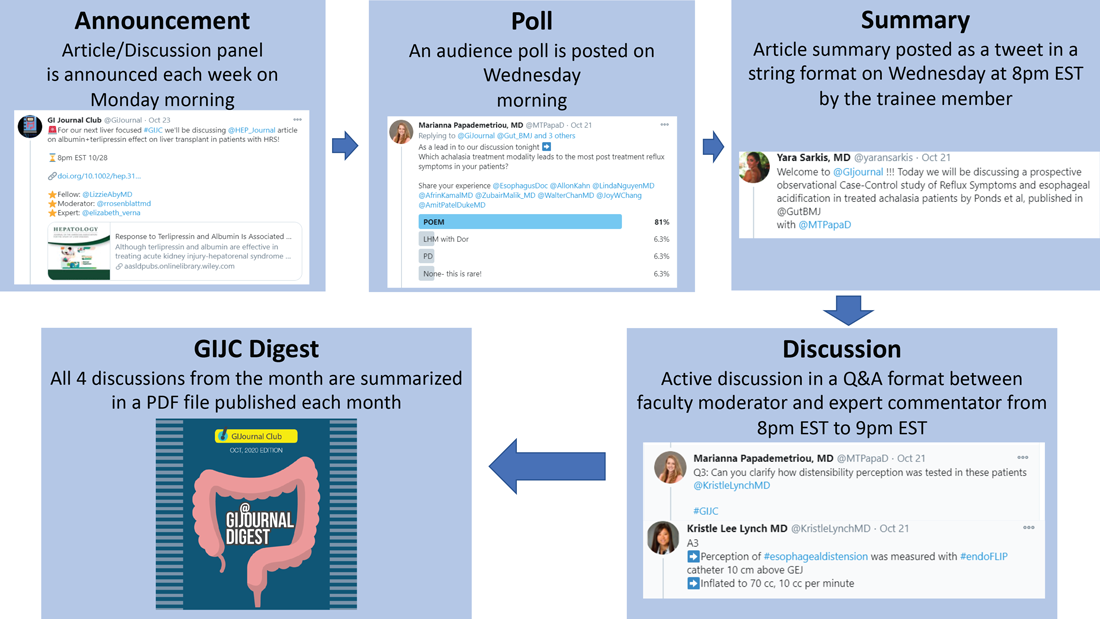
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
Abnormal anal paps in people with HIV can go more than a year without follow-up
That delay “revealed missed opportunities for a better experience on the patient, clinic, and provider level,” Jessica Wells, PhD, research assistant professor at the Nell Hodgson Woodruff School of Nursing at Emory University, Atlanta, said in an interview. After all, “a lot can happen in that 1 year,” including early development of human papillomavirus (HPV)–associated anal cancer.
Although it’s too soon to say how significant that delay is with respect to the natural history of anal cancer, Dr. Wells said the data are a potential signal of disparities.
“The findings from my study may foreshadow potential disparities if we don’t have the necessary resources in place to promote follow-up care after an abnormal Pap test, similar to the disparities that we see in cervical cancer,” she said during the virtual Association of Nurses in AIDS Care 2020 Annual Meeting.
Single-center study
In the United States, people living with HIV are 19 times more likely to develop anal cancer than the general population, according to a 2018 article in the Journal of Clinical Oncology. Another single-center study from Yale University found that, in minority communities, anal cancer rates were 75% higher than in White communities. Anal cancer rates were 72% higher in communities with greater poverty. As a result, many clinics are beginning to administer Pap tests to determine early signs of HPV infection and associated changes.
In Dr. Wells’ study, which was conducted from 2012 to 2015, 150 adults with HIV who were aged 21 and older were recruited from Grady Ponce De Leon Center in Atlanta. According to a 2018 study from that center, a large minority of participants had late-stage HIV and suppressed immune systems.
All participants had been referred for HRA after a recent abnormal anal Pap test. Participants filled out questionnaires on sociodemographics, internalized HIV-related stigma, depression, risk behaviors, social support, and knowledge about HPV and anal cancer.
Participants were disproportionately older (mean age, 50.9 years); cisgender (86.7%), Black (78%); and gay, lesbian, or bisexual (84.3%). Slightly more than 1 in 10 participants (11.3%) were transgender women.
Although for 6% of participants, Pap test results indicated high-grade squamous intraepithelial lesions (HSIL), an additional 8% had atypical Pap findings that couldn’t exclude HSIL – the kinds of results that are one step away from a cancer diagnosis. More than 80% of participants had low-grade or inconclusive results. Nearly half (44%) of participants’ Pap tests revealed low-grade squamous cell intraepithelial cell lesions (LSIL); 42% indicated atypical squamous cells of undetermined significance.
When Dr. Wells looked at how long participants had waited to undergo HRA, she found something that surprised her: although some participants underwent follow-up assessment in 17 days, for many, it took much longer. The longest wait was 2,350 days – more than 6 years.
“There were quite a few patients who had follow-up beyond 1,000-plus days,” Dr. Wells said in an interview. “I didn›t think the delays were that long — at most, I would say that patients will get scheduled and come back within a few weeks or months.”
What’s more, she discovered through the HPV knowledge questionnaire that many participants did not understand why they were having a follow-up appointment. Anecdotally, some confused HPV with HIV.
“There’s education to be done to inform this target population that those living with HIV are more prone or at increased risk of this virus causing cancer later,” she said. “There are a lot of campaigns around women living with HIV, that they need to do cervical cancer screening. I think we need to really expand this campaign to include that HPV can also cause anal cancer.”
Dr. Wells had planned to primarily investigate the impact of psychosocial factors on wait time to follow-up, but none of those factors were associated with longer wait times.
Systems-level factors
That led Ann Gakumo, PhD, chair of nursing at the College of Nursing and Health Sciences of the University of Massachusetts, Boston, to ask what other factors could account for the delay.
There were several, Dr. Wells said. Precarious housing, for example, could have influenced this lag in follow-up. About one in four participants were in transient housing, and one participant reported having been incarcerated. She gathered street addresses and plans to analyze that data to see whether the cases occurred in clusters in specific neighborhoods, as the Yale data indicated.
In addition, the anoscopy clinic was only available to receive patients one day a week and was staffed with only one clinician who was trained to perform HRA. Wait times could stretch for hours. Sometimes, participants had to leave the clinic to attend to other business, and their appointments needed to be rescheduled, Wells said.
In addition to the sometimes poor understanding of the importance of the follow-up test, Dr. Wells said, “we start to see a layering of these barriers. That’s where we start seeing breakdowns. So I’m hoping in a larger study I can address some of these barriers on a multilevel approach.”
This resonated with Dr. Gakumo.
“Oftentimes, we put so much of the responsibility for this on the part of the client and not enough on the part of the provider or on the systems level,” she said.
Guiding guidelines
Guidelines on follow-up for abnormal anal Pap test results are scarce, mostly because, unlike cervical cancer, the natural history of HPV-related anal cancers hasn’t been established. The HIV Medical Association does recommend anal Pap tests, but only in cases in which “access to appropriate referral for follow-up, including high-resolution anoscopy, is available.”
In an interview, Cecile Lahiri, MD, assistant professor of infectious disease at Emory University, said that, at Ponce De Leon Center, they recommend an anal Pap for women with HIV who have a history of cervical dysplasia.
There is a reliable association between high-grade abnormal Pap tests and cervical cancer, although low-grade changes can resolve on their own. In the case of anal cancer, especially in patients with HIV, low-grade cell changes are predictive; moreover, for such patients, anal cancer is more likely to recur and is harder to treat, Dr. Lahiri said.
“The cervical environment and the anal environment are very different,” said Dr. Lahiri, who works at the Grady Ponce De Leon Center but was not involved in Dr. Wells’ study. Dr. Lahiri is also a coinvestigator of the multisite, randomized, controlled Anal Cancer HSIL Outcomes Research (ANCHOR) study, which seeks to establish whether early treatment of high-grade anal Pap changes is better than a watch-and-wait approach.
Dr. Lahiri said that when the results of that trial become available, they are more likely to know how important early anoscopy and treatment are. The findings should inform guidelines and insurance coverage of anal Pap tests and anoscopy.
In the meantime, she said, she suspected that, with the ANCHOR trial in 2015, many sites’ capacity for anoscopy may have increased, and the wait times may have gone down.
“One of the most important pieces of the study is actually the time period in which it was conducted,” said Dr. Lahiri, who in 2015 became the clinic’s second physician trained in anoscopy. Currently, more than 200 people at the Ponce De Leon Center are enrolled in the ANCHOR trial. In addition, the general capacity for performing anoscopies has gone up nationwide as a result of the trial, which required that more providers learn how to properly perform an HRA. Many clinicians are not routinely trained in performing HRA, including gastroenterologists and surgeons, Dr. Lahiri said.
“It would be interesting to look at the differences, with the start of ANCHOR being the time point for before and after,” she said.
This article first appeared on Medscape.com.
That delay “revealed missed opportunities for a better experience on the patient, clinic, and provider level,” Jessica Wells, PhD, research assistant professor at the Nell Hodgson Woodruff School of Nursing at Emory University, Atlanta, said in an interview. After all, “a lot can happen in that 1 year,” including early development of human papillomavirus (HPV)–associated anal cancer.
Although it’s too soon to say how significant that delay is with respect to the natural history of anal cancer, Dr. Wells said the data are a potential signal of disparities.
“The findings from my study may foreshadow potential disparities if we don’t have the necessary resources in place to promote follow-up care after an abnormal Pap test, similar to the disparities that we see in cervical cancer,” she said during the virtual Association of Nurses in AIDS Care 2020 Annual Meeting.
Single-center study
In the United States, people living with HIV are 19 times more likely to develop anal cancer than the general population, according to a 2018 article in the Journal of Clinical Oncology. Another single-center study from Yale University found that, in minority communities, anal cancer rates were 75% higher than in White communities. Anal cancer rates were 72% higher in communities with greater poverty. As a result, many clinics are beginning to administer Pap tests to determine early signs of HPV infection and associated changes.
In Dr. Wells’ study, which was conducted from 2012 to 2015, 150 adults with HIV who were aged 21 and older were recruited from Grady Ponce De Leon Center in Atlanta. According to a 2018 study from that center, a large minority of participants had late-stage HIV and suppressed immune systems.
All participants had been referred for HRA after a recent abnormal anal Pap test. Participants filled out questionnaires on sociodemographics, internalized HIV-related stigma, depression, risk behaviors, social support, and knowledge about HPV and anal cancer.
Participants were disproportionately older (mean age, 50.9 years); cisgender (86.7%), Black (78%); and gay, lesbian, or bisexual (84.3%). Slightly more than 1 in 10 participants (11.3%) were transgender women.
Although for 6% of participants, Pap test results indicated high-grade squamous intraepithelial lesions (HSIL), an additional 8% had atypical Pap findings that couldn’t exclude HSIL – the kinds of results that are one step away from a cancer diagnosis. More than 80% of participants had low-grade or inconclusive results. Nearly half (44%) of participants’ Pap tests revealed low-grade squamous cell intraepithelial cell lesions (LSIL); 42% indicated atypical squamous cells of undetermined significance.
When Dr. Wells looked at how long participants had waited to undergo HRA, she found something that surprised her: although some participants underwent follow-up assessment in 17 days, for many, it took much longer. The longest wait was 2,350 days – more than 6 years.
“There were quite a few patients who had follow-up beyond 1,000-plus days,” Dr. Wells said in an interview. “I didn›t think the delays were that long — at most, I would say that patients will get scheduled and come back within a few weeks or months.”
What’s more, she discovered through the HPV knowledge questionnaire that many participants did not understand why they were having a follow-up appointment. Anecdotally, some confused HPV with HIV.
“There’s education to be done to inform this target population that those living with HIV are more prone or at increased risk of this virus causing cancer later,” she said. “There are a lot of campaigns around women living with HIV, that they need to do cervical cancer screening. I think we need to really expand this campaign to include that HPV can also cause anal cancer.”
Dr. Wells had planned to primarily investigate the impact of psychosocial factors on wait time to follow-up, but none of those factors were associated with longer wait times.
Systems-level factors
That led Ann Gakumo, PhD, chair of nursing at the College of Nursing and Health Sciences of the University of Massachusetts, Boston, to ask what other factors could account for the delay.
There were several, Dr. Wells said. Precarious housing, for example, could have influenced this lag in follow-up. About one in four participants were in transient housing, and one participant reported having been incarcerated. She gathered street addresses and plans to analyze that data to see whether the cases occurred in clusters in specific neighborhoods, as the Yale data indicated.
In addition, the anoscopy clinic was only available to receive patients one day a week and was staffed with only one clinician who was trained to perform HRA. Wait times could stretch for hours. Sometimes, participants had to leave the clinic to attend to other business, and their appointments needed to be rescheduled, Wells said.
In addition to the sometimes poor understanding of the importance of the follow-up test, Dr. Wells said, “we start to see a layering of these barriers. That’s where we start seeing breakdowns. So I’m hoping in a larger study I can address some of these barriers on a multilevel approach.”
This resonated with Dr. Gakumo.
“Oftentimes, we put so much of the responsibility for this on the part of the client and not enough on the part of the provider or on the systems level,” she said.
Guiding guidelines
Guidelines on follow-up for abnormal anal Pap test results are scarce, mostly because, unlike cervical cancer, the natural history of HPV-related anal cancers hasn’t been established. The HIV Medical Association does recommend anal Pap tests, but only in cases in which “access to appropriate referral for follow-up, including high-resolution anoscopy, is available.”
In an interview, Cecile Lahiri, MD, assistant professor of infectious disease at Emory University, said that, at Ponce De Leon Center, they recommend an anal Pap for women with HIV who have a history of cervical dysplasia.
There is a reliable association between high-grade abnormal Pap tests and cervical cancer, although low-grade changes can resolve on their own. In the case of anal cancer, especially in patients with HIV, low-grade cell changes are predictive; moreover, for such patients, anal cancer is more likely to recur and is harder to treat, Dr. Lahiri said.
“The cervical environment and the anal environment are very different,” said Dr. Lahiri, who works at the Grady Ponce De Leon Center but was not involved in Dr. Wells’ study. Dr. Lahiri is also a coinvestigator of the multisite, randomized, controlled Anal Cancer HSIL Outcomes Research (ANCHOR) study, which seeks to establish whether early treatment of high-grade anal Pap changes is better than a watch-and-wait approach.
Dr. Lahiri said that when the results of that trial become available, they are more likely to know how important early anoscopy and treatment are. The findings should inform guidelines and insurance coverage of anal Pap tests and anoscopy.
In the meantime, she said, she suspected that, with the ANCHOR trial in 2015, many sites’ capacity for anoscopy may have increased, and the wait times may have gone down.
“One of the most important pieces of the study is actually the time period in which it was conducted,” said Dr. Lahiri, who in 2015 became the clinic’s second physician trained in anoscopy. Currently, more than 200 people at the Ponce De Leon Center are enrolled in the ANCHOR trial. In addition, the general capacity for performing anoscopies has gone up nationwide as a result of the trial, which required that more providers learn how to properly perform an HRA. Many clinicians are not routinely trained in performing HRA, including gastroenterologists and surgeons, Dr. Lahiri said.
“It would be interesting to look at the differences, with the start of ANCHOR being the time point for before and after,” she said.
This article first appeared on Medscape.com.
That delay “revealed missed opportunities for a better experience on the patient, clinic, and provider level,” Jessica Wells, PhD, research assistant professor at the Nell Hodgson Woodruff School of Nursing at Emory University, Atlanta, said in an interview. After all, “a lot can happen in that 1 year,” including early development of human papillomavirus (HPV)–associated anal cancer.
Although it’s too soon to say how significant that delay is with respect to the natural history of anal cancer, Dr. Wells said the data are a potential signal of disparities.
“The findings from my study may foreshadow potential disparities if we don’t have the necessary resources in place to promote follow-up care after an abnormal Pap test, similar to the disparities that we see in cervical cancer,” she said during the virtual Association of Nurses in AIDS Care 2020 Annual Meeting.
Single-center study
In the United States, people living with HIV are 19 times more likely to develop anal cancer than the general population, according to a 2018 article in the Journal of Clinical Oncology. Another single-center study from Yale University found that, in minority communities, anal cancer rates were 75% higher than in White communities. Anal cancer rates were 72% higher in communities with greater poverty. As a result, many clinics are beginning to administer Pap tests to determine early signs of HPV infection and associated changes.
In Dr. Wells’ study, which was conducted from 2012 to 2015, 150 adults with HIV who were aged 21 and older were recruited from Grady Ponce De Leon Center in Atlanta. According to a 2018 study from that center, a large minority of participants had late-stage HIV and suppressed immune systems.
All participants had been referred for HRA after a recent abnormal anal Pap test. Participants filled out questionnaires on sociodemographics, internalized HIV-related stigma, depression, risk behaviors, social support, and knowledge about HPV and anal cancer.
Participants were disproportionately older (mean age, 50.9 years); cisgender (86.7%), Black (78%); and gay, lesbian, or bisexual (84.3%). Slightly more than 1 in 10 participants (11.3%) were transgender women.
Although for 6% of participants, Pap test results indicated high-grade squamous intraepithelial lesions (HSIL), an additional 8% had atypical Pap findings that couldn’t exclude HSIL – the kinds of results that are one step away from a cancer diagnosis. More than 80% of participants had low-grade or inconclusive results. Nearly half (44%) of participants’ Pap tests revealed low-grade squamous cell intraepithelial cell lesions (LSIL); 42% indicated atypical squamous cells of undetermined significance.
When Dr. Wells looked at how long participants had waited to undergo HRA, she found something that surprised her: although some participants underwent follow-up assessment in 17 days, for many, it took much longer. The longest wait was 2,350 days – more than 6 years.
“There were quite a few patients who had follow-up beyond 1,000-plus days,” Dr. Wells said in an interview. “I didn›t think the delays were that long — at most, I would say that patients will get scheduled and come back within a few weeks or months.”
What’s more, she discovered through the HPV knowledge questionnaire that many participants did not understand why they were having a follow-up appointment. Anecdotally, some confused HPV with HIV.
“There’s education to be done to inform this target population that those living with HIV are more prone or at increased risk of this virus causing cancer later,” she said. “There are a lot of campaigns around women living with HIV, that they need to do cervical cancer screening. I think we need to really expand this campaign to include that HPV can also cause anal cancer.”
Dr. Wells had planned to primarily investigate the impact of psychosocial factors on wait time to follow-up, but none of those factors were associated with longer wait times.
Systems-level factors
That led Ann Gakumo, PhD, chair of nursing at the College of Nursing and Health Sciences of the University of Massachusetts, Boston, to ask what other factors could account for the delay.
There were several, Dr. Wells said. Precarious housing, for example, could have influenced this lag in follow-up. About one in four participants were in transient housing, and one participant reported having been incarcerated. She gathered street addresses and plans to analyze that data to see whether the cases occurred in clusters in specific neighborhoods, as the Yale data indicated.
In addition, the anoscopy clinic was only available to receive patients one day a week and was staffed with only one clinician who was trained to perform HRA. Wait times could stretch for hours. Sometimes, participants had to leave the clinic to attend to other business, and their appointments needed to be rescheduled, Wells said.
In addition to the sometimes poor understanding of the importance of the follow-up test, Dr. Wells said, “we start to see a layering of these barriers. That’s where we start seeing breakdowns. So I’m hoping in a larger study I can address some of these barriers on a multilevel approach.”
This resonated with Dr. Gakumo.
“Oftentimes, we put so much of the responsibility for this on the part of the client and not enough on the part of the provider or on the systems level,” she said.
Guiding guidelines
Guidelines on follow-up for abnormal anal Pap test results are scarce, mostly because, unlike cervical cancer, the natural history of HPV-related anal cancers hasn’t been established. The HIV Medical Association does recommend anal Pap tests, but only in cases in which “access to appropriate referral for follow-up, including high-resolution anoscopy, is available.”
In an interview, Cecile Lahiri, MD, assistant professor of infectious disease at Emory University, said that, at Ponce De Leon Center, they recommend an anal Pap for women with HIV who have a history of cervical dysplasia.
There is a reliable association between high-grade abnormal Pap tests and cervical cancer, although low-grade changes can resolve on their own. In the case of anal cancer, especially in patients with HIV, low-grade cell changes are predictive; moreover, for such patients, anal cancer is more likely to recur and is harder to treat, Dr. Lahiri said.
“The cervical environment and the anal environment are very different,” said Dr. Lahiri, who works at the Grady Ponce De Leon Center but was not involved in Dr. Wells’ study. Dr. Lahiri is also a coinvestigator of the multisite, randomized, controlled Anal Cancer HSIL Outcomes Research (ANCHOR) study, which seeks to establish whether early treatment of high-grade anal Pap changes is better than a watch-and-wait approach.
Dr. Lahiri said that when the results of that trial become available, they are more likely to know how important early anoscopy and treatment are. The findings should inform guidelines and insurance coverage of anal Pap tests and anoscopy.
In the meantime, she said, she suspected that, with the ANCHOR trial in 2015, many sites’ capacity for anoscopy may have increased, and the wait times may have gone down.
“One of the most important pieces of the study is actually the time period in which it was conducted,” said Dr. Lahiri, who in 2015 became the clinic’s second physician trained in anoscopy. Currently, more than 200 people at the Ponce De Leon Center are enrolled in the ANCHOR trial. In addition, the general capacity for performing anoscopies has gone up nationwide as a result of the trial, which required that more providers learn how to properly perform an HRA. Many clinicians are not routinely trained in performing HRA, including gastroenterologists and surgeons, Dr. Lahiri said.
“It would be interesting to look at the differences, with the start of ANCHOR being the time point for before and after,” she said.
This article first appeared on Medscape.com.
What hospitalists need to know about health care reimbursement and denial prevention
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
VTEs tied to immune checkpoint inhibitor cancer treatment
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
FROM AHA 2020
Oral Hairy Leukoplakia Associated With the Use of Adalimumab
To the Editor:
Oral hairy leukoplakia (OHL) is an Epstein-Barr virus (EBV)–mediated mucocutaneous disease that often involves the lingual epithelium. The lateral portions of the tongue are the most commonly affected sites. The lesions often are described as asymptomatic, white, corrugated patches or plaques that are unable to be scraped off.1 Oral hairy leukoplakia was first identified in 1984 and was considered to be associated with AIDS.2 An association between the presence of OHL and the degree of immunosuppression as well as the severity of human immunodeficiency virus (HIV) has been reported.3 Although OHL initially was considered to be pathognomonic for HIV, it has since been described in multiple other immunosuppressive conditions.4 Numerous medical conditions and combinations of immunosuppressive medications have been associated with OHL in patients who were HIV negative.5
Adalimumab is an injectable human IgG1 recombinant antibody to tumor necrosis factor α (TNF-α).6 It currently is approved by the US Food and Drug Administration for the treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn disease, ulcerative colitis, noninfectious uveitis, hidradenitis suppurativa, and plaque psoriasis.7 We report a case of OHL associated with the use of adalimumab.
A 47-year-old woman initially presented with chronic plaque-type psoriasis. Her medical history was notable for bipolar disorder, migraines, hypertension, and tobacco use. The patient’s psoriasis initially was well controlled on a regimen of topical steroids and methotrexate; however, methotrexate was stopped after 2.5 years due to a mildly elevated alanine aminotransferase level, as well as an abnormal liver biopsy showing mildly active (grade 1 of 3) steatohepatitis with portal chronic inflammation, pericellular fibrosis, and portal and focal periportal fibrosis (stage 1-2 of 4). The patient and her dermatologist were uncomfortable continuing methotrexate with these findings. After baseline screening including a negative purified protein derivative skin test, adalimumab was initiated. A loading dose of 80 mg subcutaneously (SQ) was given, followed by adalimumab 40 mg SQ 1 week later and 40 mg every other week as maintenance.
The patient’s psoriasis was well controlled with adalimumab for 22 months, but she then developed a thin white plaque on the right lateral tongue (Figure 1). An incisional biopsy of the tongue performed by an oral surgeon revealed hyperkeratosis with Candida colonization and viral cytopathic effect (Figure 2). An EBV DNA in situ hybridization stain revealed focal positivity within these cells (Figure 3), leading to a diagnosis of OHL. Laboratory evaluation demonstrated a normal complete blood cell count with differential and liver panel as well as a negative HIV test. The patient otherwise felt well and denied fevers, lymphadenopathy, and weight loss.

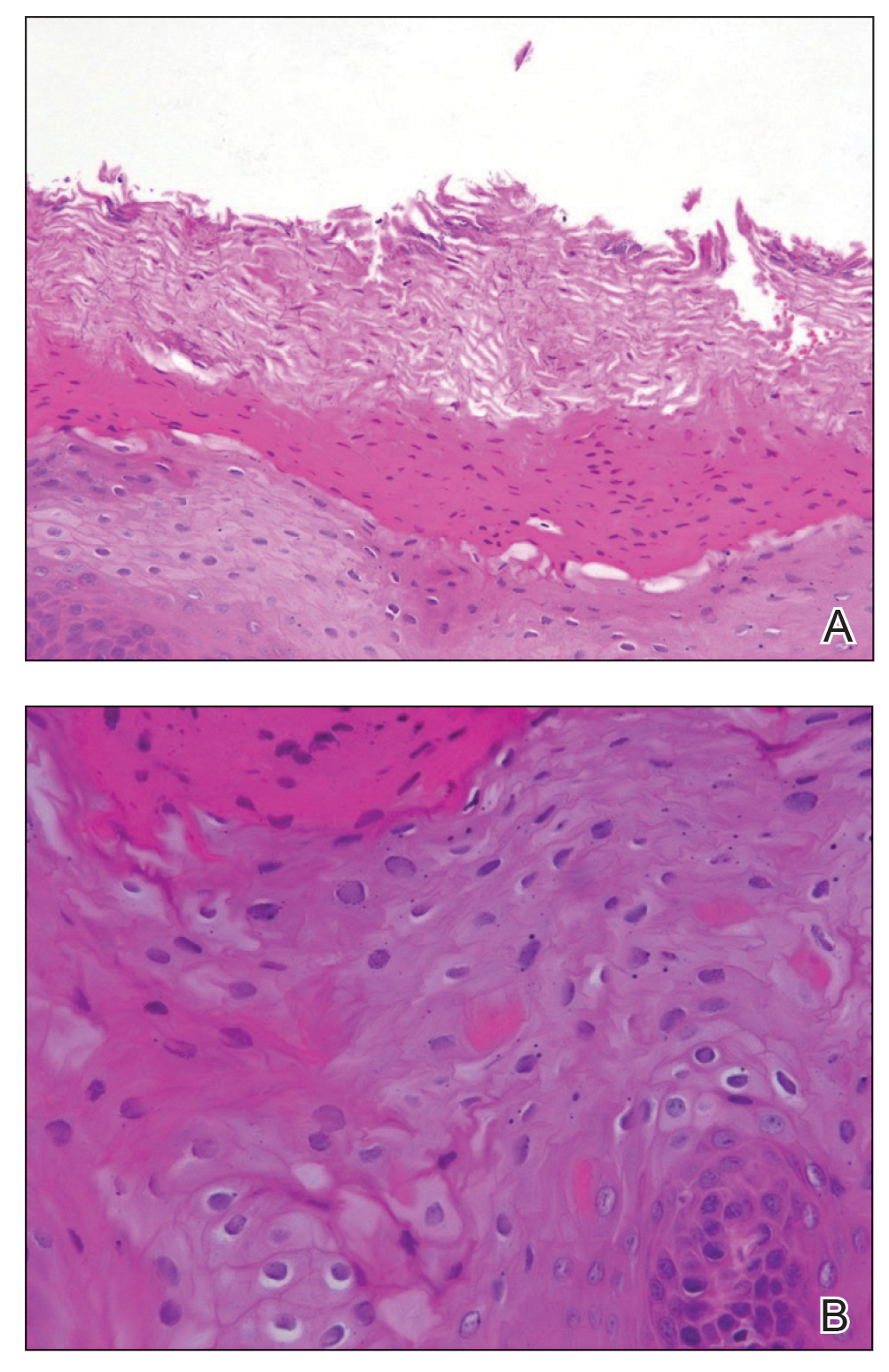
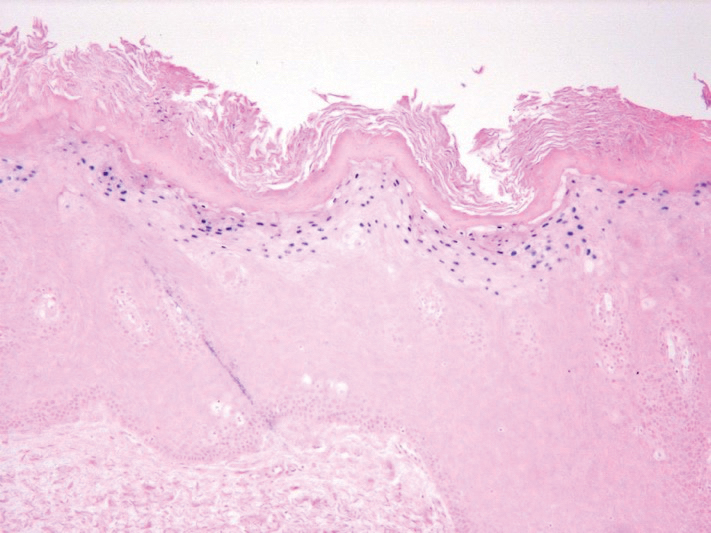
We consulted with an infectious disease and immunodeficiency specialist regarding the patient’s case. Before conducting further evaluation beyond HIV screening for immunodeficiency states, adalimumab was discontinued to see if the OHL would spontaneously resolve. Three months after discontinuation of adalimumab, the white plaque on the right lateral tongue was notably improved. The OHL continued to disappear and was completely resolved 1 year after discontinuation of adalimumab. The patient’s psoriasis had subsequently remained well controlled with diet and weight loss, smoking cessation, topical steroids, and apremilast without any recurrence of the OHL.
Oral hairy leukoplakia is associated with upregulated EBV replication and EBV-encoded proteins such as latent membrane protein 1.2 It often presents as white or gray patches on the lateral lingual margins with prominent folds and/or projections, giving a shaggy appearance. Oral hairy leukoplakia often is specific for HIV infection and rarely is associated with other immunodeficiencies.2 Prasad and Bilodeau5 performed a literature review of medical conditions and immunosuppressive medications associated with OHL in patients without HIV. Allogeneic transplant was associated with the highest incidence of OHL in HIV-negative patients (59.2% [45/76]).5 Various combinations of immunosuppressive medications (eg, prednisone, cyclosporine, azathioprine) also may be implicated in cases of HIV-negative patients with OHL. A case of OHL also has been reported with long-standing use of inhaled corticosteroids in an immunocompetent, HIV-negative patient.6 Another case was reported with long-term use of the aromatic antiepileptic lamotrigine, which resolved once stopping the medication.8 Although EBV is an oncovirus and has been associated with lymphoproliferative disorders and nasopharyngeal carcinoma, OHL is not considered to be a premalignant lesion.7 Despite the strong association between OHL and HIV, our patient was HIV negative. The only immunocompromising factor in our patient was the use of adalimumab to treat psoriasis. We did not conduct further testing for immunodeficiency states because the OHL spontaneously resolved when the adalimumab was discontinued.
PubMed and Ovid searches of articles indexed for MEDLINE using the terms adalimumab and oral hairy leukoplakia as well as TNF-alpha inhibitor and oral hairy leukoplakia with humans and English language as limitations revealed that no cases have been reported in the literature demonstrating an association between OHL and adalimumab or any other TNF-α inhibitor. However, Cetkovska et al9 reported a case of EBV hepatitis and subsequently chronic hepatitis as a complication of infliximab used for the treatment of chronic psoriasis. Because TNF-α and IFN-γ play an important role in controlling viral infections, there is an increased risk for reactivating a viral illness when depleting TNF through pharmacologic measures (ie, adalimumab, infliximab).8 Another case of EBV-associated plasmablastic lymphoma was reported after 1 year of adalimumab use in a patient with Crohn disease. The plasmablastic lymphoma resolved after 4 rounds of chemotherapy.10
The only contraindication for the use of adalimumab is a known hypersensitivity to the drug. Relative contraindications for use of adalimumab include active tuberculosis, demyelinating disease, hematologic diseases (ie, thrombocytopenia, pancytopenia), lymphoma, hepatitis C, and hepatitis B.11 The most common adverse effect of adalimumab is an injection-site reaction. Additional reported adverse effects of TNF-α inhibitors as a class are lymphoma, melanoma, nonmelanoma skin cancer, reactivation of latent tuberculosis, congestive heart failure, autoimmunity, and hematologic toxicity.11
This case demonstrates an association between adalimumab and OHL in an HIV-negative patient. Although the mechanism behind OHL and immunosuppression remains to be elucidated, this association is important to keep in mind when using adalimumab or other TNF-α inhibitors for the treatment of psoriasis or other medical conditions.
- Triantos D, Porter SR, Scully C, et al. Oral hairy leukoplakia: clinicopathologic features, pathogenesis, diagnosis, and clinical significance. Clin Infect Dis. 1997;25:1392-1396.
- Greenspan D, Greenspan JS, Conant M, et al. Oral “hairy” leucoplakia in male homosexuals: evidence of association with both papillomavirus and a herpes-group virus. Lancet. 1984;2:831-834.
- Glick M, Muzyka BC, Lurie D, et al. Oral manifestations associated with HIV-related disease as marks for immune suppression and AIDS. Oral Surg Oral Med Oral Pathol. 1994;77:344-349.
- Chambers AE, Conn B, Pemberton M, et al. Twenty-first-century oral hair leukoplakia—a non-HIV-associated entity. Oral Surg Oral Med Oral Patho Oral Radiol. 2015;119:326-332.
- Prasad JL, Bilodeau EA. Oral hairy leukoplakia in patients without HIV: presentation of 2 new cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:E151-E160.
- Moffat M, Jauhar S, Jones ME, et al. Oral hairy leukoplakia in an HIV-negative, immunocompetent patient. Oral Biosci Med. 2005;2:282-284.
- Greenspan JS, Greenspan D. Oral hairy leukoplakia: diagnosis and management. Oral Surg Oral Med Oral Pathol. 1989;67:396-403.
- Gordins P, Sloan P, Spickett GP, et al. Oral hairy leukoplakia in a patient on long-term anticonvulsant treatment with lamotrigine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:E17-E23.
- Cetkovska P, Lomicova I, Mukensnabl P, et al. Anti-tumour necrosis factor treatment of severe psoriasis complicated by Epstein-Barr virus hepatitis and subsequently by chronic hepatitis. Dermatol Ther. 2015;28:369-372.
- Liu L, Charabaty A, Ozdemirli M. EBV-associated plasmablastic lymphoma in a patient with Crohn’s disease after adalimumab treatment. J Crohns Colitis. 2013;7:E118-E119.
- Humira [package insert]. North Chicago, IL: AbbVie Inc; 2018.
To the Editor:
Oral hairy leukoplakia (OHL) is an Epstein-Barr virus (EBV)–mediated mucocutaneous disease that often involves the lingual epithelium. The lateral portions of the tongue are the most commonly affected sites. The lesions often are described as asymptomatic, white, corrugated patches or plaques that are unable to be scraped off.1 Oral hairy leukoplakia was first identified in 1984 and was considered to be associated with AIDS.2 An association between the presence of OHL and the degree of immunosuppression as well as the severity of human immunodeficiency virus (HIV) has been reported.3 Although OHL initially was considered to be pathognomonic for HIV, it has since been described in multiple other immunosuppressive conditions.4 Numerous medical conditions and combinations of immunosuppressive medications have been associated with OHL in patients who were HIV negative.5
Adalimumab is an injectable human IgG1 recombinant antibody to tumor necrosis factor α (TNF-α).6 It currently is approved by the US Food and Drug Administration for the treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn disease, ulcerative colitis, noninfectious uveitis, hidradenitis suppurativa, and plaque psoriasis.7 We report a case of OHL associated with the use of adalimumab.
A 47-year-old woman initially presented with chronic plaque-type psoriasis. Her medical history was notable for bipolar disorder, migraines, hypertension, and tobacco use. The patient’s psoriasis initially was well controlled on a regimen of topical steroids and methotrexate; however, methotrexate was stopped after 2.5 years due to a mildly elevated alanine aminotransferase level, as well as an abnormal liver biopsy showing mildly active (grade 1 of 3) steatohepatitis with portal chronic inflammation, pericellular fibrosis, and portal and focal periportal fibrosis (stage 1-2 of 4). The patient and her dermatologist were uncomfortable continuing methotrexate with these findings. After baseline screening including a negative purified protein derivative skin test, adalimumab was initiated. A loading dose of 80 mg subcutaneously (SQ) was given, followed by adalimumab 40 mg SQ 1 week later and 40 mg every other week as maintenance.
The patient’s psoriasis was well controlled with adalimumab for 22 months, but she then developed a thin white plaque on the right lateral tongue (Figure 1). An incisional biopsy of the tongue performed by an oral surgeon revealed hyperkeratosis with Candida colonization and viral cytopathic effect (Figure 2). An EBV DNA in situ hybridization stain revealed focal positivity within these cells (Figure 3), leading to a diagnosis of OHL. Laboratory evaluation demonstrated a normal complete blood cell count with differential and liver panel as well as a negative HIV test. The patient otherwise felt well and denied fevers, lymphadenopathy, and weight loss.

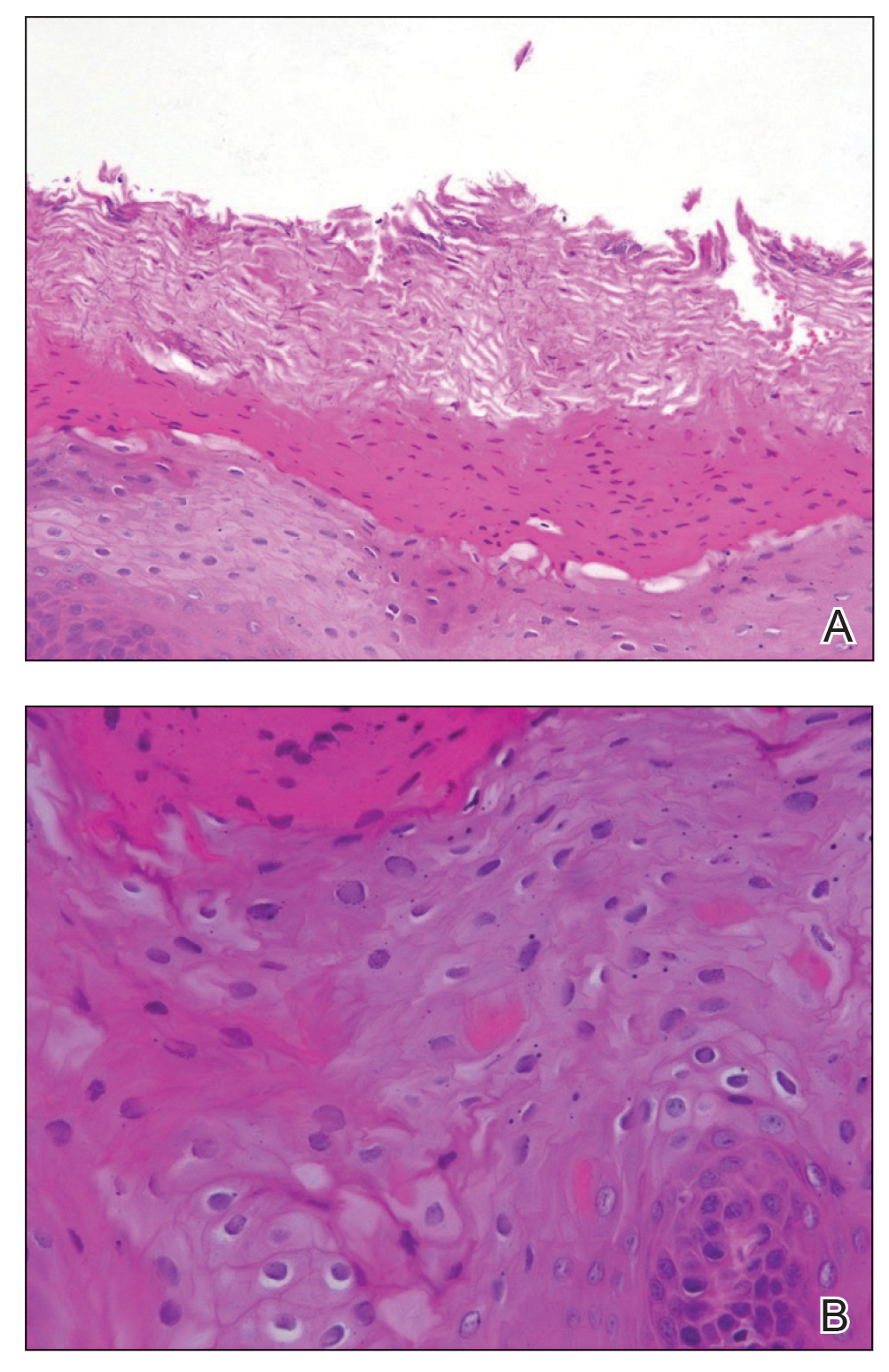
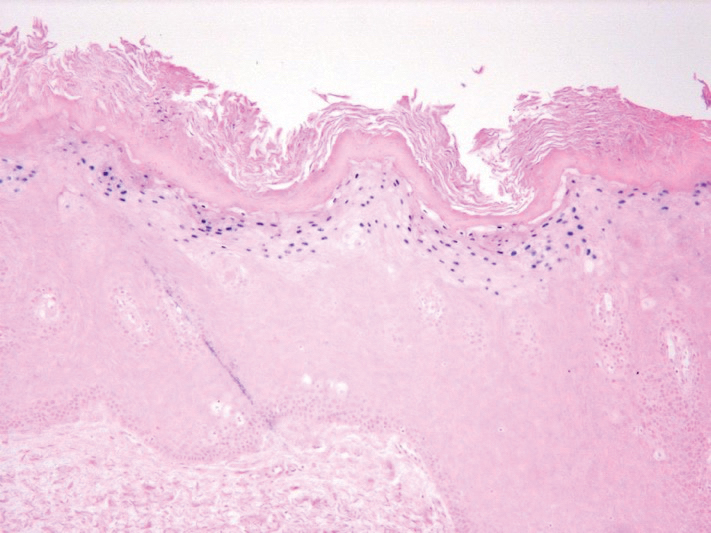
We consulted with an infectious disease and immunodeficiency specialist regarding the patient’s case. Before conducting further evaluation beyond HIV screening for immunodeficiency states, adalimumab was discontinued to see if the OHL would spontaneously resolve. Three months after discontinuation of adalimumab, the white plaque on the right lateral tongue was notably improved. The OHL continued to disappear and was completely resolved 1 year after discontinuation of adalimumab. The patient’s psoriasis had subsequently remained well controlled with diet and weight loss, smoking cessation, topical steroids, and apremilast without any recurrence of the OHL.
Oral hairy leukoplakia is associated with upregulated EBV replication and EBV-encoded proteins such as latent membrane protein 1.2 It often presents as white or gray patches on the lateral lingual margins with prominent folds and/or projections, giving a shaggy appearance. Oral hairy leukoplakia often is specific for HIV infection and rarely is associated with other immunodeficiencies.2 Prasad and Bilodeau5 performed a literature review of medical conditions and immunosuppressive medications associated with OHL in patients without HIV. Allogeneic transplant was associated with the highest incidence of OHL in HIV-negative patients (59.2% [45/76]).5 Various combinations of immunosuppressive medications (eg, prednisone, cyclosporine, azathioprine) also may be implicated in cases of HIV-negative patients with OHL. A case of OHL also has been reported with long-standing use of inhaled corticosteroids in an immunocompetent, HIV-negative patient.6 Another case was reported with long-term use of the aromatic antiepileptic lamotrigine, which resolved once stopping the medication.8 Although EBV is an oncovirus and has been associated with lymphoproliferative disorders and nasopharyngeal carcinoma, OHL is not considered to be a premalignant lesion.7 Despite the strong association between OHL and HIV, our patient was HIV negative. The only immunocompromising factor in our patient was the use of adalimumab to treat psoriasis. We did not conduct further testing for immunodeficiency states because the OHL spontaneously resolved when the adalimumab was discontinued.
PubMed and Ovid searches of articles indexed for MEDLINE using the terms adalimumab and oral hairy leukoplakia as well as TNF-alpha inhibitor and oral hairy leukoplakia with humans and English language as limitations revealed that no cases have been reported in the literature demonstrating an association between OHL and adalimumab or any other TNF-α inhibitor. However, Cetkovska et al9 reported a case of EBV hepatitis and subsequently chronic hepatitis as a complication of infliximab used for the treatment of chronic psoriasis. Because TNF-α and IFN-γ play an important role in controlling viral infections, there is an increased risk for reactivating a viral illness when depleting TNF through pharmacologic measures (ie, adalimumab, infliximab).8 Another case of EBV-associated plasmablastic lymphoma was reported after 1 year of adalimumab use in a patient with Crohn disease. The plasmablastic lymphoma resolved after 4 rounds of chemotherapy.10
The only contraindication for the use of adalimumab is a known hypersensitivity to the drug. Relative contraindications for use of adalimumab include active tuberculosis, demyelinating disease, hematologic diseases (ie, thrombocytopenia, pancytopenia), lymphoma, hepatitis C, and hepatitis B.11 The most common adverse effect of adalimumab is an injection-site reaction. Additional reported adverse effects of TNF-α inhibitors as a class are lymphoma, melanoma, nonmelanoma skin cancer, reactivation of latent tuberculosis, congestive heart failure, autoimmunity, and hematologic toxicity.11
This case demonstrates an association between adalimumab and OHL in an HIV-negative patient. Although the mechanism behind OHL and immunosuppression remains to be elucidated, this association is important to keep in mind when using adalimumab or other TNF-α inhibitors for the treatment of psoriasis or other medical conditions.
To the Editor:
Oral hairy leukoplakia (OHL) is an Epstein-Barr virus (EBV)–mediated mucocutaneous disease that often involves the lingual epithelium. The lateral portions of the tongue are the most commonly affected sites. The lesions often are described as asymptomatic, white, corrugated patches or plaques that are unable to be scraped off.1 Oral hairy leukoplakia was first identified in 1984 and was considered to be associated with AIDS.2 An association between the presence of OHL and the degree of immunosuppression as well as the severity of human immunodeficiency virus (HIV) has been reported.3 Although OHL initially was considered to be pathognomonic for HIV, it has since been described in multiple other immunosuppressive conditions.4 Numerous medical conditions and combinations of immunosuppressive medications have been associated with OHL in patients who were HIV negative.5
Adalimumab is an injectable human IgG1 recombinant antibody to tumor necrosis factor α (TNF-α).6 It currently is approved by the US Food and Drug Administration for the treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult and pediatric Crohn disease, ulcerative colitis, noninfectious uveitis, hidradenitis suppurativa, and plaque psoriasis.7 We report a case of OHL associated with the use of adalimumab.
A 47-year-old woman initially presented with chronic plaque-type psoriasis. Her medical history was notable for bipolar disorder, migraines, hypertension, and tobacco use. The patient’s psoriasis initially was well controlled on a regimen of topical steroids and methotrexate; however, methotrexate was stopped after 2.5 years due to a mildly elevated alanine aminotransferase level, as well as an abnormal liver biopsy showing mildly active (grade 1 of 3) steatohepatitis with portal chronic inflammation, pericellular fibrosis, and portal and focal periportal fibrosis (stage 1-2 of 4). The patient and her dermatologist were uncomfortable continuing methotrexate with these findings. After baseline screening including a negative purified protein derivative skin test, adalimumab was initiated. A loading dose of 80 mg subcutaneously (SQ) was given, followed by adalimumab 40 mg SQ 1 week later and 40 mg every other week as maintenance.
The patient’s psoriasis was well controlled with adalimumab for 22 months, but she then developed a thin white plaque on the right lateral tongue (Figure 1). An incisional biopsy of the tongue performed by an oral surgeon revealed hyperkeratosis with Candida colonization and viral cytopathic effect (Figure 2). An EBV DNA in situ hybridization stain revealed focal positivity within these cells (Figure 3), leading to a diagnosis of OHL. Laboratory evaluation demonstrated a normal complete blood cell count with differential and liver panel as well as a negative HIV test. The patient otherwise felt well and denied fevers, lymphadenopathy, and weight loss.

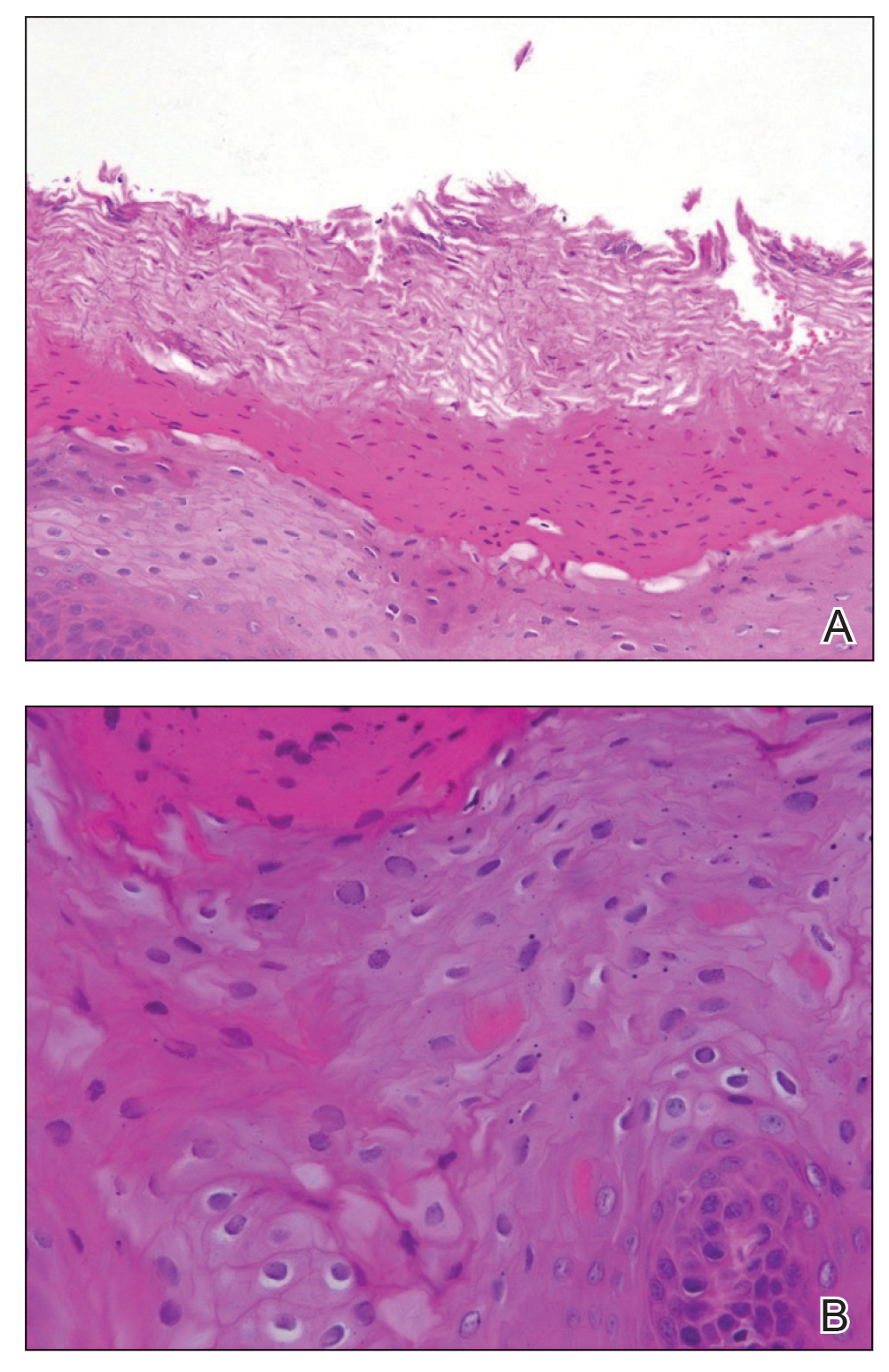
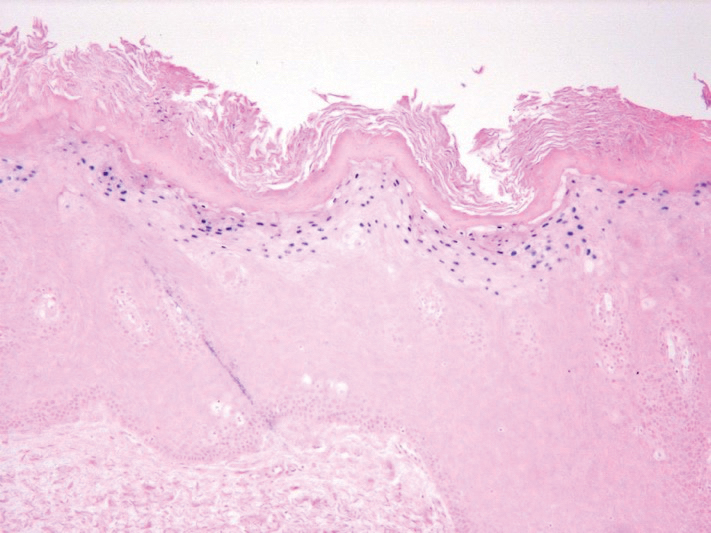
We consulted with an infectious disease and immunodeficiency specialist regarding the patient’s case. Before conducting further evaluation beyond HIV screening for immunodeficiency states, adalimumab was discontinued to see if the OHL would spontaneously resolve. Three months after discontinuation of adalimumab, the white plaque on the right lateral tongue was notably improved. The OHL continued to disappear and was completely resolved 1 year after discontinuation of adalimumab. The patient’s psoriasis had subsequently remained well controlled with diet and weight loss, smoking cessation, topical steroids, and apremilast without any recurrence of the OHL.
Oral hairy leukoplakia is associated with upregulated EBV replication and EBV-encoded proteins such as latent membrane protein 1.2 It often presents as white or gray patches on the lateral lingual margins with prominent folds and/or projections, giving a shaggy appearance. Oral hairy leukoplakia often is specific for HIV infection and rarely is associated with other immunodeficiencies.2 Prasad and Bilodeau5 performed a literature review of medical conditions and immunosuppressive medications associated with OHL in patients without HIV. Allogeneic transplant was associated with the highest incidence of OHL in HIV-negative patients (59.2% [45/76]).5 Various combinations of immunosuppressive medications (eg, prednisone, cyclosporine, azathioprine) also may be implicated in cases of HIV-negative patients with OHL. A case of OHL also has been reported with long-standing use of inhaled corticosteroids in an immunocompetent, HIV-negative patient.6 Another case was reported with long-term use of the aromatic antiepileptic lamotrigine, which resolved once stopping the medication.8 Although EBV is an oncovirus and has been associated with lymphoproliferative disorders and nasopharyngeal carcinoma, OHL is not considered to be a premalignant lesion.7 Despite the strong association between OHL and HIV, our patient was HIV negative. The only immunocompromising factor in our patient was the use of adalimumab to treat psoriasis. We did not conduct further testing for immunodeficiency states because the OHL spontaneously resolved when the adalimumab was discontinued.
PubMed and Ovid searches of articles indexed for MEDLINE using the terms adalimumab and oral hairy leukoplakia as well as TNF-alpha inhibitor and oral hairy leukoplakia with humans and English language as limitations revealed that no cases have been reported in the literature demonstrating an association between OHL and adalimumab or any other TNF-α inhibitor. However, Cetkovska et al9 reported a case of EBV hepatitis and subsequently chronic hepatitis as a complication of infliximab used for the treatment of chronic psoriasis. Because TNF-α and IFN-γ play an important role in controlling viral infections, there is an increased risk for reactivating a viral illness when depleting TNF through pharmacologic measures (ie, adalimumab, infliximab).8 Another case of EBV-associated plasmablastic lymphoma was reported after 1 year of adalimumab use in a patient with Crohn disease. The plasmablastic lymphoma resolved after 4 rounds of chemotherapy.10
The only contraindication for the use of adalimumab is a known hypersensitivity to the drug. Relative contraindications for use of adalimumab include active tuberculosis, demyelinating disease, hematologic diseases (ie, thrombocytopenia, pancytopenia), lymphoma, hepatitis C, and hepatitis B.11 The most common adverse effect of adalimumab is an injection-site reaction. Additional reported adverse effects of TNF-α inhibitors as a class are lymphoma, melanoma, nonmelanoma skin cancer, reactivation of latent tuberculosis, congestive heart failure, autoimmunity, and hematologic toxicity.11
This case demonstrates an association between adalimumab and OHL in an HIV-negative patient. Although the mechanism behind OHL and immunosuppression remains to be elucidated, this association is important to keep in mind when using adalimumab or other TNF-α inhibitors for the treatment of psoriasis or other medical conditions.
- Triantos D, Porter SR, Scully C, et al. Oral hairy leukoplakia: clinicopathologic features, pathogenesis, diagnosis, and clinical significance. Clin Infect Dis. 1997;25:1392-1396.
- Greenspan D, Greenspan JS, Conant M, et al. Oral “hairy” leucoplakia in male homosexuals: evidence of association with both papillomavirus and a herpes-group virus. Lancet. 1984;2:831-834.
- Glick M, Muzyka BC, Lurie D, et al. Oral manifestations associated with HIV-related disease as marks for immune suppression and AIDS. Oral Surg Oral Med Oral Pathol. 1994;77:344-349.
- Chambers AE, Conn B, Pemberton M, et al. Twenty-first-century oral hair leukoplakia—a non-HIV-associated entity. Oral Surg Oral Med Oral Patho Oral Radiol. 2015;119:326-332.
- Prasad JL, Bilodeau EA. Oral hairy leukoplakia in patients without HIV: presentation of 2 new cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:E151-E160.
- Moffat M, Jauhar S, Jones ME, et al. Oral hairy leukoplakia in an HIV-negative, immunocompetent patient. Oral Biosci Med. 2005;2:282-284.
- Greenspan JS, Greenspan D. Oral hairy leukoplakia: diagnosis and management. Oral Surg Oral Med Oral Pathol. 1989;67:396-403.
- Gordins P, Sloan P, Spickett GP, et al. Oral hairy leukoplakia in a patient on long-term anticonvulsant treatment with lamotrigine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:E17-E23.
- Cetkovska P, Lomicova I, Mukensnabl P, et al. Anti-tumour necrosis factor treatment of severe psoriasis complicated by Epstein-Barr virus hepatitis and subsequently by chronic hepatitis. Dermatol Ther. 2015;28:369-372.
- Liu L, Charabaty A, Ozdemirli M. EBV-associated plasmablastic lymphoma in a patient with Crohn’s disease after adalimumab treatment. J Crohns Colitis. 2013;7:E118-E119.
- Humira [package insert]. North Chicago, IL: AbbVie Inc; 2018.
- Triantos D, Porter SR, Scully C, et al. Oral hairy leukoplakia: clinicopathologic features, pathogenesis, diagnosis, and clinical significance. Clin Infect Dis. 1997;25:1392-1396.
- Greenspan D, Greenspan JS, Conant M, et al. Oral “hairy” leucoplakia in male homosexuals: evidence of association with both papillomavirus and a herpes-group virus. Lancet. 1984;2:831-834.
- Glick M, Muzyka BC, Lurie D, et al. Oral manifestations associated with HIV-related disease as marks for immune suppression and AIDS. Oral Surg Oral Med Oral Pathol. 1994;77:344-349.
- Chambers AE, Conn B, Pemberton M, et al. Twenty-first-century oral hair leukoplakia—a non-HIV-associated entity. Oral Surg Oral Med Oral Patho Oral Radiol. 2015;119:326-332.
- Prasad JL, Bilodeau EA. Oral hairy leukoplakia in patients without HIV: presentation of 2 new cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:E151-E160.
- Moffat M, Jauhar S, Jones ME, et al. Oral hairy leukoplakia in an HIV-negative, immunocompetent patient. Oral Biosci Med. 2005;2:282-284.
- Greenspan JS, Greenspan D. Oral hairy leukoplakia: diagnosis and management. Oral Surg Oral Med Oral Pathol. 1989;67:396-403.
- Gordins P, Sloan P, Spickett GP, et al. Oral hairy leukoplakia in a patient on long-term anticonvulsant treatment with lamotrigine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:E17-E23.
- Cetkovska P, Lomicova I, Mukensnabl P, et al. Anti-tumour necrosis factor treatment of severe psoriasis complicated by Epstein-Barr virus hepatitis and subsequently by chronic hepatitis. Dermatol Ther. 2015;28:369-372.
- Liu L, Charabaty A, Ozdemirli M. EBV-associated plasmablastic lymphoma in a patient with Crohn’s disease after adalimumab treatment. J Crohns Colitis. 2013;7:E118-E119.
- Humira [package insert]. North Chicago, IL: AbbVie Inc; 2018.
Practice Points
- Workup for new-onset oral hairy leukoplakia should include a comprehensive medication history.
- Oral hairy leukoplakia is an uncommon side effect of adalimumab.