User login
Increased risk of second cancers in mycosis fungoides
LA JOLLA, CALIF. – A retrospective study suggests patients with mycosis fungoides (MF) have an increased risk of developing hematologic and solid tumor malignancies.

Researchers found the risk of second malignancy was highest among MF patients aged 30 to 50 years and patients who had tumor stage or advanced stage MF.
The increased risk was present during the entire period after MF diagnosis, but it was greatest in the first 6 months after diagnosis and roughly a dozen years later.
Amrita Goyal, MD, of the University of Minnesota in Minneapolis, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The researchers first assessed the risk of second malignancy in 172 MF patients treated at UMN from 2005 to 2017, comparing this cohort to a control group of 172 patients with seborrheic dermatitis.
Second malignancies occurred in 24 MF patients and three controls, which was a significant difference (P = .0045). The most common second malignancies among the MF patients were melanoma (n = 4), prostate cancer (n = 3), and renal cell carcinoma (n = 3).
Further analyses revealed that MF patients were more likely to develop a second malignancy if they had tumor stage disease (P = .0024) or stage IIB or higher disease (P = .03).
To corroborate and expand upon these results, Dr. Goyal and her colleagues analyzed data from the Surveillance, Epidemiology, and End Results (SEER) database on patients diagnosed with MF from 2000 to 2014.
Among the 6,196 MF patients in this cohort, there were 514 second cancers.
“We found that MF patients were, overall, 10 times more likely to develop a second malignancy [compared with the general population],” Dr. Goyal said.
Specifically, the standardized incidence ratio was 10.15 for all malignancies, 7.33 for solid tumors, and 41.72 for hematologic malignancies.
Standardized incidence ratios for individual malignancies were:
- 69.8 for Hodgkin lymphoma.
- 46.5 for non-Hodgkin lymphoma.
- 8.6 for leukemia.
- 7.2 for melanoma.
- 6.2 for lung cancer.
- 7.9 for female breast cancer.
- 5.2 for colon cancer.
- 4.1 for prostate cancer.
- 3.9 for renal cell carcinoma.
- 3.8 for pancreatic cancer.
- 3.6 for bladder cancer.
“We found there is an increased risk [of second malignancy] during the first 6 months after diagnosis of MF, likely related to patients being in contact with the health care system more,” Dr. Goyal said. “Over time, patients have about a 7- to 10-fold increased risk over baseline, until they reach about 12 or 13 years after diagnosis, at which point, there is an increase in risk.”
The researchers found the greatest risk of second malignancy was among patients aged 30 to 50 years, although there was an increased risk for all age groups.
“The reason we think patients are experiencing an increased risk of cancers is we believe this may be due to immune suppression secondary to the mycosis fungoides, although further studies need to be performed to determine if that’s accurate,” Dr. Goyal said.
To that end, she and her colleagues are planning gene expression studies in patients from the UMN cohort. The researchers plan to examine genes involved in the pathogenesis of second malignancies and MF progression in tissue samples from 36 MF patients, 12 who developed second malignancies and 24 who did not.
The current research was funded by the American Society of Hematology. Dr. Goyal reported having no relevant financial disclosures. The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – A retrospective study suggests patients with mycosis fungoides (MF) have an increased risk of developing hematologic and solid tumor malignancies.

Researchers found the risk of second malignancy was highest among MF patients aged 30 to 50 years and patients who had tumor stage or advanced stage MF.
The increased risk was present during the entire period after MF diagnosis, but it was greatest in the first 6 months after diagnosis and roughly a dozen years later.
Amrita Goyal, MD, of the University of Minnesota in Minneapolis, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The researchers first assessed the risk of second malignancy in 172 MF patients treated at UMN from 2005 to 2017, comparing this cohort to a control group of 172 patients with seborrheic dermatitis.
Second malignancies occurred in 24 MF patients and three controls, which was a significant difference (P = .0045). The most common second malignancies among the MF patients were melanoma (n = 4), prostate cancer (n = 3), and renal cell carcinoma (n = 3).
Further analyses revealed that MF patients were more likely to develop a second malignancy if they had tumor stage disease (P = .0024) or stage IIB or higher disease (P = .03).
To corroborate and expand upon these results, Dr. Goyal and her colleagues analyzed data from the Surveillance, Epidemiology, and End Results (SEER) database on patients diagnosed with MF from 2000 to 2014.
Among the 6,196 MF patients in this cohort, there were 514 second cancers.
“We found that MF patients were, overall, 10 times more likely to develop a second malignancy [compared with the general population],” Dr. Goyal said.
Specifically, the standardized incidence ratio was 10.15 for all malignancies, 7.33 for solid tumors, and 41.72 for hematologic malignancies.
Standardized incidence ratios for individual malignancies were:
- 69.8 for Hodgkin lymphoma.
- 46.5 for non-Hodgkin lymphoma.
- 8.6 for leukemia.
- 7.2 for melanoma.
- 6.2 for lung cancer.
- 7.9 for female breast cancer.
- 5.2 for colon cancer.
- 4.1 for prostate cancer.
- 3.9 for renal cell carcinoma.
- 3.8 for pancreatic cancer.
- 3.6 for bladder cancer.
“We found there is an increased risk [of second malignancy] during the first 6 months after diagnosis of MF, likely related to patients being in contact with the health care system more,” Dr. Goyal said. “Over time, patients have about a 7- to 10-fold increased risk over baseline, until they reach about 12 or 13 years after diagnosis, at which point, there is an increase in risk.”
The researchers found the greatest risk of second malignancy was among patients aged 30 to 50 years, although there was an increased risk for all age groups.
“The reason we think patients are experiencing an increased risk of cancers is we believe this may be due to immune suppression secondary to the mycosis fungoides, although further studies need to be performed to determine if that’s accurate,” Dr. Goyal said.
To that end, she and her colleagues are planning gene expression studies in patients from the UMN cohort. The researchers plan to examine genes involved in the pathogenesis of second malignancies and MF progression in tissue samples from 36 MF patients, 12 who developed second malignancies and 24 who did not.
The current research was funded by the American Society of Hematology. Dr. Goyal reported having no relevant financial disclosures. The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – A retrospective study suggests patients with mycosis fungoides (MF) have an increased risk of developing hematologic and solid tumor malignancies.

Researchers found the risk of second malignancy was highest among MF patients aged 30 to 50 years and patients who had tumor stage or advanced stage MF.
The increased risk was present during the entire period after MF diagnosis, but it was greatest in the first 6 months after diagnosis and roughly a dozen years later.
Amrita Goyal, MD, of the University of Minnesota in Minneapolis, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The researchers first assessed the risk of second malignancy in 172 MF patients treated at UMN from 2005 to 2017, comparing this cohort to a control group of 172 patients with seborrheic dermatitis.
Second malignancies occurred in 24 MF patients and three controls, which was a significant difference (P = .0045). The most common second malignancies among the MF patients were melanoma (n = 4), prostate cancer (n = 3), and renal cell carcinoma (n = 3).
Further analyses revealed that MF patients were more likely to develop a second malignancy if they had tumor stage disease (P = .0024) or stage IIB or higher disease (P = .03).
To corroborate and expand upon these results, Dr. Goyal and her colleagues analyzed data from the Surveillance, Epidemiology, and End Results (SEER) database on patients diagnosed with MF from 2000 to 2014.
Among the 6,196 MF patients in this cohort, there were 514 second cancers.
“We found that MF patients were, overall, 10 times more likely to develop a second malignancy [compared with the general population],” Dr. Goyal said.
Specifically, the standardized incidence ratio was 10.15 for all malignancies, 7.33 for solid tumors, and 41.72 for hematologic malignancies.
Standardized incidence ratios for individual malignancies were:
- 69.8 for Hodgkin lymphoma.
- 46.5 for non-Hodgkin lymphoma.
- 8.6 for leukemia.
- 7.2 for melanoma.
- 6.2 for lung cancer.
- 7.9 for female breast cancer.
- 5.2 for colon cancer.
- 4.1 for prostate cancer.
- 3.9 for renal cell carcinoma.
- 3.8 for pancreatic cancer.
- 3.6 for bladder cancer.
“We found there is an increased risk [of second malignancy] during the first 6 months after diagnosis of MF, likely related to patients being in contact with the health care system more,” Dr. Goyal said. “Over time, patients have about a 7- to 10-fold increased risk over baseline, until they reach about 12 or 13 years after diagnosis, at which point, there is an increase in risk.”
The researchers found the greatest risk of second malignancy was among patients aged 30 to 50 years, although there was an increased risk for all age groups.
“The reason we think patients are experiencing an increased risk of cancers is we believe this may be due to immune suppression secondary to the mycosis fungoides, although further studies need to be performed to determine if that’s accurate,” Dr. Goyal said.
To that end, she and her colleagues are planning gene expression studies in patients from the UMN cohort. The researchers plan to examine genes involved in the pathogenesis of second malignancies and MF progression in tissue samples from 36 MF patients, 12 who developed second malignancies and 24 who did not.
The current research was funded by the American Society of Hematology. Dr. Goyal reported having no relevant financial disclosures. The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: In a cohort of MF patients from the SEER database, the standardized incidence ratio was 10.15 for all malignancies, 7.33 for solid tumors, and 41.72 for hematologic malignancies.
Study details: Retrospective study of 6,196 MF patients from the SEER database, and a single-center cohort of 172 MF patients who were matched to 172 patients with seborrheic dermatitis.
Disclosures: This research was funded by the American Society of Hematology. Dr. Goyal reported having no relevant financial disclosures.
New findings raise questions about the role of ANAs in SLE
Antinuclear antibodies (ANAs) have long been considered an important marker in rheumatologic conditions, particularly for the diagnosis and classification of patients with systemic lupus erythematosus, but recent findings are raising new questions about their role.
“We’ve measured ANAs for a long time – it’s a very important test in rheumatology,” David S. Pisetsky, MD, PhD, explained in an interview.
However, even though this test has been around for decades, “some interesting things have developed around it that have made a lot of people, including me, take a second look,” said Dr. Pisetsky, professor of medicine and immunology at Duke University, Durham, N.C.
He elaborated on those recent findings, which relate to the findings of ANA negativity in patients with an established diagnosis of systemic lupus erythematosus (SLE) and to variability among ANA test kit findings, during a presentation at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“Screening of patients during clinical trials for new treatments of SLE suggest that a significant number of people with lupus – 20%-30%, in fact – are ANA negative despite disease activity at the time the test is done,” he said.
For example, unpublished (but recently submitted) data from a phase 2 trial looking at the efficacy and safety of an interleukin-6 monoclonal antibody for the treatment of SLE showed that 23.8% of baseline samples from 183 SLE patients with positive historical ANA and clinically active lupus prior to randomization were ANA negative.
A particular concern with respect to such findings is that ANA positivity is typically a criterion for entry into clinical trials of therapies for lupus and prescription of medications approved for active lupus, Dr. Pisetsky said.
“On the other hand, about 20% of otherwise healthy people – especially women – can be ANA positive, so it’s always been problematic as a screening test due to these false positives, but these new findings suggest that in lupus a real concern is false negatives,” he said. “It’s quite a surprise.”
The findings raise questions about whether ANA negativity in SLE reflects the natural history of the disease, an effect of treatments, or a problem with the assays.
It appears an important problem relates to test kit variability, he said.
“There are lots of different ANA test kits. Their performance characteristics are very different. The performance of ANA tests is much more variable than people realize,” he said, citing data from an analysis that he and his colleagues conducted using 103 samples from a cohort of patients with established SLE.
In that 2017 study, an ANA enzyme-linked immunosorbent assay showed an ANA-negativity rate of 11.7% with zero indeterminate tests, whereas three different test kits showed ANA-negativity rates of 22.3% (with 8.7% of samples reported as indeterminate), 9.7% (with another 9.7% indeterminate), and 4.9% (with another 1.9% indeterminate), respectively. Multiplex testing showed a 13.6% ANA-negativity rate and an indeterminate rate of 7.8% (Ann Rheum Dis. 2018;77:911-3).
Only one sample tested negative for ANA on all three test kits, and disagreement about ANA negativity occurred in one-third of the samples, he said.
Anti–double-stranded DNA assays
Recent findings also raise questions about the use of assays that specifically assess for anti–double-stranded DNA (anti-dsDNA) antibodies, which are highly associated with SLE and have been used as a biomarker for the disease, Dr. Pisetsky said.
For example, a comparison of two anti-dsDNA assays showed discordant results with respect to negativity for anti-dsDNA antibodies in 64 of 181 samples from SLE patients. One assay showed a 70.7% rate of anti-dsDNA negativity and the other showed a 37.6% rate.
The concern regarding test variability relates to the issue of ANA positivity and eligibility for study enrollment and certain treatments; test variability can affect the diagnosis of patients with SLE because ANA positivity is an important finding in routine clinical care, and for anti-dsDNA, test variability can affect assessment of disease activity, he explained.
Tests may differ in a number of ways, such as in their specificity, sensitivity, avidity, and range of epitopes detected. Unfortunately, not enough is known at this point to make specific recommendations regarding best test kits, and while there are alternative technologies that could be useful for ANA testing, none has been validated for particular use in the assessment of trial eligibility, Dr. Pisetsky said.
Nonetheless, awareness of the test variability is important, especially when it comes to assessing patients for trial eligibility and prescribing medications, he added. “For practical, real-world utilization, people need to know about this.”
Dr. Pisetsky reported receiving ANA-related research support from Pfizer, conducting collaborative research with Bio-Rad and EuroImmun, and serving as an adviser to ImmunArray.
Antinuclear antibodies (ANAs) have long been considered an important marker in rheumatologic conditions, particularly for the diagnosis and classification of patients with systemic lupus erythematosus, but recent findings are raising new questions about their role.
“We’ve measured ANAs for a long time – it’s a very important test in rheumatology,” David S. Pisetsky, MD, PhD, explained in an interview.
However, even though this test has been around for decades, “some interesting things have developed around it that have made a lot of people, including me, take a second look,” said Dr. Pisetsky, professor of medicine and immunology at Duke University, Durham, N.C.
He elaborated on those recent findings, which relate to the findings of ANA negativity in patients with an established diagnosis of systemic lupus erythematosus (SLE) and to variability among ANA test kit findings, during a presentation at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“Screening of patients during clinical trials for new treatments of SLE suggest that a significant number of people with lupus – 20%-30%, in fact – are ANA negative despite disease activity at the time the test is done,” he said.
For example, unpublished (but recently submitted) data from a phase 2 trial looking at the efficacy and safety of an interleukin-6 monoclonal antibody for the treatment of SLE showed that 23.8% of baseline samples from 183 SLE patients with positive historical ANA and clinically active lupus prior to randomization were ANA negative.
A particular concern with respect to such findings is that ANA positivity is typically a criterion for entry into clinical trials of therapies for lupus and prescription of medications approved for active lupus, Dr. Pisetsky said.
“On the other hand, about 20% of otherwise healthy people – especially women – can be ANA positive, so it’s always been problematic as a screening test due to these false positives, but these new findings suggest that in lupus a real concern is false negatives,” he said. “It’s quite a surprise.”
The findings raise questions about whether ANA negativity in SLE reflects the natural history of the disease, an effect of treatments, or a problem with the assays.
It appears an important problem relates to test kit variability, he said.
“There are lots of different ANA test kits. Their performance characteristics are very different. The performance of ANA tests is much more variable than people realize,” he said, citing data from an analysis that he and his colleagues conducted using 103 samples from a cohort of patients with established SLE.
In that 2017 study, an ANA enzyme-linked immunosorbent assay showed an ANA-negativity rate of 11.7% with zero indeterminate tests, whereas three different test kits showed ANA-negativity rates of 22.3% (with 8.7% of samples reported as indeterminate), 9.7% (with another 9.7% indeterminate), and 4.9% (with another 1.9% indeterminate), respectively. Multiplex testing showed a 13.6% ANA-negativity rate and an indeterminate rate of 7.8% (Ann Rheum Dis. 2018;77:911-3).
Only one sample tested negative for ANA on all three test kits, and disagreement about ANA negativity occurred in one-third of the samples, he said.
Anti–double-stranded DNA assays
Recent findings also raise questions about the use of assays that specifically assess for anti–double-stranded DNA (anti-dsDNA) antibodies, which are highly associated with SLE and have been used as a biomarker for the disease, Dr. Pisetsky said.
For example, a comparison of two anti-dsDNA assays showed discordant results with respect to negativity for anti-dsDNA antibodies in 64 of 181 samples from SLE patients. One assay showed a 70.7% rate of anti-dsDNA negativity and the other showed a 37.6% rate.
The concern regarding test variability relates to the issue of ANA positivity and eligibility for study enrollment and certain treatments; test variability can affect the diagnosis of patients with SLE because ANA positivity is an important finding in routine clinical care, and for anti-dsDNA, test variability can affect assessment of disease activity, he explained.
Tests may differ in a number of ways, such as in their specificity, sensitivity, avidity, and range of epitopes detected. Unfortunately, not enough is known at this point to make specific recommendations regarding best test kits, and while there are alternative technologies that could be useful for ANA testing, none has been validated for particular use in the assessment of trial eligibility, Dr. Pisetsky said.
Nonetheless, awareness of the test variability is important, especially when it comes to assessing patients for trial eligibility and prescribing medications, he added. “For practical, real-world utilization, people need to know about this.”
Dr. Pisetsky reported receiving ANA-related research support from Pfizer, conducting collaborative research with Bio-Rad and EuroImmun, and serving as an adviser to ImmunArray.
Antinuclear antibodies (ANAs) have long been considered an important marker in rheumatologic conditions, particularly for the diagnosis and classification of patients with systemic lupus erythematosus, but recent findings are raising new questions about their role.
“We’ve measured ANAs for a long time – it’s a very important test in rheumatology,” David S. Pisetsky, MD, PhD, explained in an interview.
However, even though this test has been around for decades, “some interesting things have developed around it that have made a lot of people, including me, take a second look,” said Dr. Pisetsky, professor of medicine and immunology at Duke University, Durham, N.C.
He elaborated on those recent findings, which relate to the findings of ANA negativity in patients with an established diagnosis of systemic lupus erythematosus (SLE) and to variability among ANA test kit findings, during a presentation at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“Screening of patients during clinical trials for new treatments of SLE suggest that a significant number of people with lupus – 20%-30%, in fact – are ANA negative despite disease activity at the time the test is done,” he said.
For example, unpublished (but recently submitted) data from a phase 2 trial looking at the efficacy and safety of an interleukin-6 monoclonal antibody for the treatment of SLE showed that 23.8% of baseline samples from 183 SLE patients with positive historical ANA and clinically active lupus prior to randomization were ANA negative.
A particular concern with respect to such findings is that ANA positivity is typically a criterion for entry into clinical trials of therapies for lupus and prescription of medications approved for active lupus, Dr. Pisetsky said.
“On the other hand, about 20% of otherwise healthy people – especially women – can be ANA positive, so it’s always been problematic as a screening test due to these false positives, but these new findings suggest that in lupus a real concern is false negatives,” he said. “It’s quite a surprise.”
The findings raise questions about whether ANA negativity in SLE reflects the natural history of the disease, an effect of treatments, or a problem with the assays.
It appears an important problem relates to test kit variability, he said.
“There are lots of different ANA test kits. Their performance characteristics are very different. The performance of ANA tests is much more variable than people realize,” he said, citing data from an analysis that he and his colleagues conducted using 103 samples from a cohort of patients with established SLE.
In that 2017 study, an ANA enzyme-linked immunosorbent assay showed an ANA-negativity rate of 11.7% with zero indeterminate tests, whereas three different test kits showed ANA-negativity rates of 22.3% (with 8.7% of samples reported as indeterminate), 9.7% (with another 9.7% indeterminate), and 4.9% (with another 1.9% indeterminate), respectively. Multiplex testing showed a 13.6% ANA-negativity rate and an indeterminate rate of 7.8% (Ann Rheum Dis. 2018;77:911-3).
Only one sample tested negative for ANA on all three test kits, and disagreement about ANA negativity occurred in one-third of the samples, he said.
Anti–double-stranded DNA assays
Recent findings also raise questions about the use of assays that specifically assess for anti–double-stranded DNA (anti-dsDNA) antibodies, which are highly associated with SLE and have been used as a biomarker for the disease, Dr. Pisetsky said.
For example, a comparison of two anti-dsDNA assays showed discordant results with respect to negativity for anti-dsDNA antibodies in 64 of 181 samples from SLE patients. One assay showed a 70.7% rate of anti-dsDNA negativity and the other showed a 37.6% rate.
The concern regarding test variability relates to the issue of ANA positivity and eligibility for study enrollment and certain treatments; test variability can affect the diagnosis of patients with SLE because ANA positivity is an important finding in routine clinical care, and for anti-dsDNA, test variability can affect assessment of disease activity, he explained.
Tests may differ in a number of ways, such as in their specificity, sensitivity, avidity, and range of epitopes detected. Unfortunately, not enough is known at this point to make specific recommendations regarding best test kits, and while there are alternative technologies that could be useful for ANA testing, none has been validated for particular use in the assessment of trial eligibility, Dr. Pisetsky said.
Nonetheless, awareness of the test variability is important, especially when it comes to assessing patients for trial eligibility and prescribing medications, he added. “For practical, real-world utilization, people need to know about this.”
Dr. Pisetsky reported receiving ANA-related research support from Pfizer, conducting collaborative research with Bio-Rad and EuroImmun, and serving as an adviser to ImmunArray.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
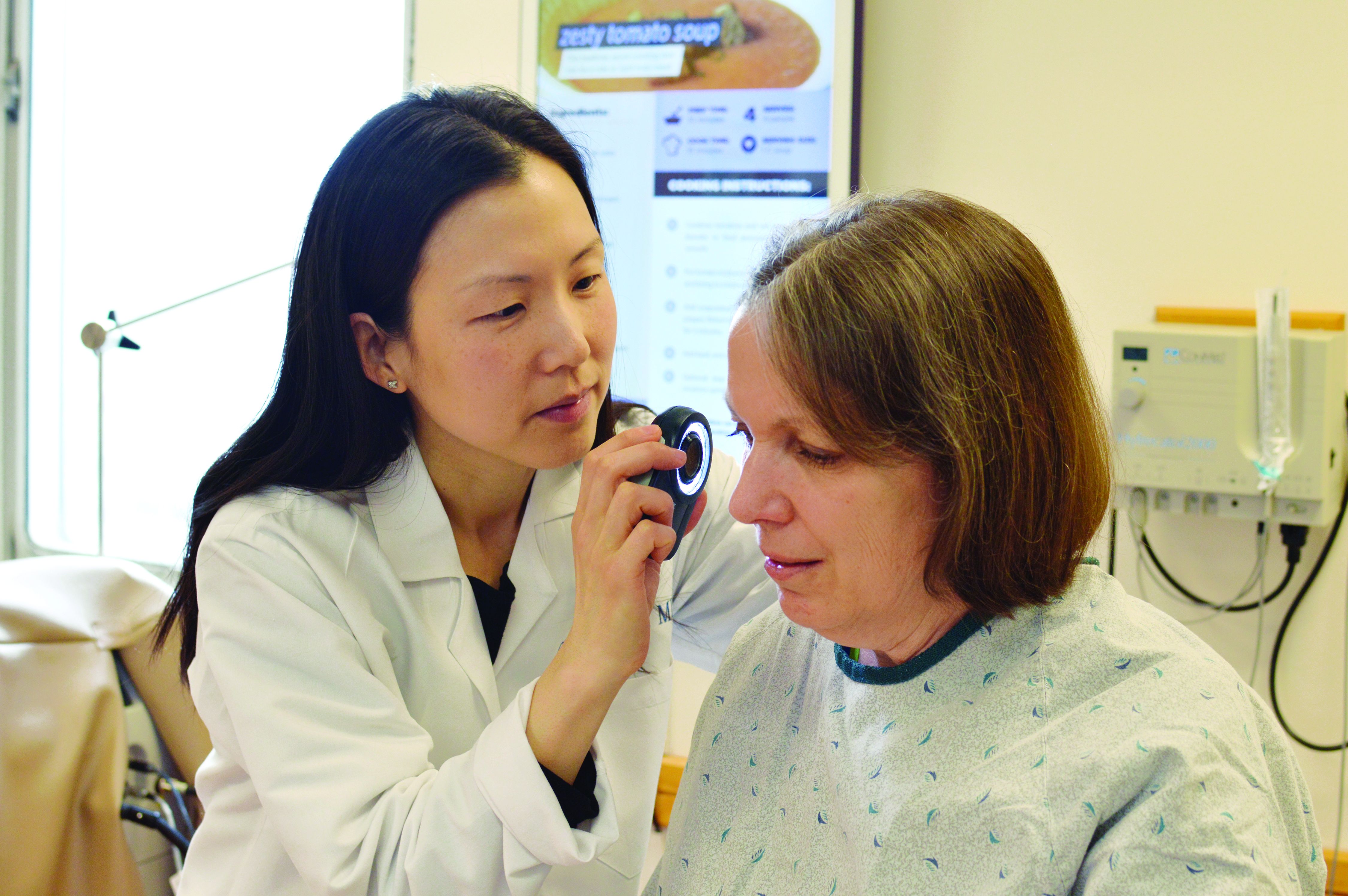
Antibiotic use in dermatology declining, with one exception
Dermatologists are prescribing fewer antibiotics for acne and rosacea, but prescribing after dermatologic surgery has increased in the past decade.
In a study published online Jan. 16 in JAMA Dermatology, researchers report the results of a cross-sectional analysis of antibiotic prescribing by 11,986 dermatologists between 2008 and 2016, using commercial claims data.
The analysis showed that, over this period of time, the overall rate of antibiotic prescribing by dermatologists decreased by 36.6%, from 3.36 courses per 100 dermatologist visits to 2.13 courses. In particular, antibiotic prescribing for acne decreased by 28.1%, from 11.76 courses per 100 visits to 8.45 courses, and for rosacea it decreased by 18.1%, from 10.89 courses per 100 visits to 8.92 courses.
John S. Barbieri, MD, of the department of dermatology, University of Pennsylvania, and his coauthors described the overall decline in antibiotic prescribing as “encouraging,” considering that in 2013 dermatologists were identified as the “most frequent prescribers of oral antibiotics per clinician.” The decline resulted in an estimated 480,000 fewer antibiotic courses a year, they noted.
“Much of the decrease in extended courses of antibiotic therapy is associated with visits for acne and rosacea,” they wrote. “Although recent guidelines suggest limiting the duration of therapy in this patient population, course duration has remained stable over time, suggesting that this decrease may be due to fewer patients being treated with antibiotics rather than patients being treated for a shorter duration.”
However, the rate of oral antibiotic prescriptions associated with surgical visits increased by 69.6%, from 3.92 courses per 100 visits to 6.65. This increase was concerning, given the risk of surgical-site infections was low, the authors pointed out. “In addition, a 2008 advisory statement on antibiotic prophylaxis recommends single-dose perioperative antibiotics for patients at increased risk of surgical-site infection,” they added.
The study also noted a 35.3% increase in antibiotic prescribing for cysts and a 3.2% increase for hidradenitis suppurativa.
Over the entire study period, nearly 1 million courses of oral antibiotics were prescribed. Doxycycline hyclate accounted for around one quarter of prescriptions, as did minocycline, while 19.9% of prescriptions were for cephalexin.
“Given the low rate of infectious complications, even for Mohs surgery, and the lack of evidence to support the use of prolonged rather than single-dose perioperative regimens, the postoperative courses of antibiotics identified in this study may increase risks to patients without substantial benefits,” they added.
The study was partly supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases. No conflicts of interest were declared.
SOURCE: Barbieri J et al. JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4944.
Reducing antibiotic prescribing in dermatology – as in so many other areas of medical practice – is a challenge, but there are a number of strategies that can help.
The first is to take a wait-and-see approach, which has been shown to be effective for childhood otitis media. Communication training for physicians can also help them to manage patient requests for antibiotics by working out the patient’s level of understanding of their condition and treatment options, and their expectations, and getting them to agree to keep antibiotics as a contingency plan. There are clinical decision support tools available to help physicians identify high-risk surgical patients who may require postoperative antibiotics.
It will help to have alternative treatment options for conditions such as acne and rosacea, such as better topical therapies, and an increase in clinical trials for these therapies will hopefully provide more options for patients.
Joslyn S. Kirby, MD, and Jordan S. Lim, MB, are in the department of dermatology, Penn State University, Hershey. These comments are taken from an accompanying editorial (JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4877). They had no disclosures.
Reducing antibiotic prescribing in dermatology – as in so many other areas of medical practice – is a challenge, but there are a number of strategies that can help.
The first is to take a wait-and-see approach, which has been shown to be effective for childhood otitis media. Communication training for physicians can also help them to manage patient requests for antibiotics by working out the patient’s level of understanding of their condition and treatment options, and their expectations, and getting them to agree to keep antibiotics as a contingency plan. There are clinical decision support tools available to help physicians identify high-risk surgical patients who may require postoperative antibiotics.
It will help to have alternative treatment options for conditions such as acne and rosacea, such as better topical therapies, and an increase in clinical trials for these therapies will hopefully provide more options for patients.
Joslyn S. Kirby, MD, and Jordan S. Lim, MB, are in the department of dermatology, Penn State University, Hershey. These comments are taken from an accompanying editorial (JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4877). They had no disclosures.
Reducing antibiotic prescribing in dermatology – as in so many other areas of medical practice – is a challenge, but there are a number of strategies that can help.
The first is to take a wait-and-see approach, which has been shown to be effective for childhood otitis media. Communication training for physicians can also help them to manage patient requests for antibiotics by working out the patient’s level of understanding of their condition and treatment options, and their expectations, and getting them to agree to keep antibiotics as a contingency plan. There are clinical decision support tools available to help physicians identify high-risk surgical patients who may require postoperative antibiotics.
It will help to have alternative treatment options for conditions such as acne and rosacea, such as better topical therapies, and an increase in clinical trials for these therapies will hopefully provide more options for patients.
Joslyn S. Kirby, MD, and Jordan S. Lim, MB, are in the department of dermatology, Penn State University, Hershey. These comments are taken from an accompanying editorial (JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4877). They had no disclosures.
Dermatologists are prescribing fewer antibiotics for acne and rosacea, but prescribing after dermatologic surgery has increased in the past decade.
In a study published online Jan. 16 in JAMA Dermatology, researchers report the results of a cross-sectional analysis of antibiotic prescribing by 11,986 dermatologists between 2008 and 2016, using commercial claims data.
The analysis showed that, over this period of time, the overall rate of antibiotic prescribing by dermatologists decreased by 36.6%, from 3.36 courses per 100 dermatologist visits to 2.13 courses. In particular, antibiotic prescribing for acne decreased by 28.1%, from 11.76 courses per 100 visits to 8.45 courses, and for rosacea it decreased by 18.1%, from 10.89 courses per 100 visits to 8.92 courses.
John S. Barbieri, MD, of the department of dermatology, University of Pennsylvania, and his coauthors described the overall decline in antibiotic prescribing as “encouraging,” considering that in 2013 dermatologists were identified as the “most frequent prescribers of oral antibiotics per clinician.” The decline resulted in an estimated 480,000 fewer antibiotic courses a year, they noted.
“Much of the decrease in extended courses of antibiotic therapy is associated with visits for acne and rosacea,” they wrote. “Although recent guidelines suggest limiting the duration of therapy in this patient population, course duration has remained stable over time, suggesting that this decrease may be due to fewer patients being treated with antibiotics rather than patients being treated for a shorter duration.”
However, the rate of oral antibiotic prescriptions associated with surgical visits increased by 69.6%, from 3.92 courses per 100 visits to 6.65. This increase was concerning, given the risk of surgical-site infections was low, the authors pointed out. “In addition, a 2008 advisory statement on antibiotic prophylaxis recommends single-dose perioperative antibiotics for patients at increased risk of surgical-site infection,” they added.
The study also noted a 35.3% increase in antibiotic prescribing for cysts and a 3.2% increase for hidradenitis suppurativa.
Over the entire study period, nearly 1 million courses of oral antibiotics were prescribed. Doxycycline hyclate accounted for around one quarter of prescriptions, as did minocycline, while 19.9% of prescriptions were for cephalexin.
“Given the low rate of infectious complications, even for Mohs surgery, and the lack of evidence to support the use of prolonged rather than single-dose perioperative regimens, the postoperative courses of antibiotics identified in this study may increase risks to patients without substantial benefits,” they added.
The study was partly supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases. No conflicts of interest were declared.
SOURCE: Barbieri J et al. JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4944.
Dermatologists are prescribing fewer antibiotics for acne and rosacea, but prescribing after dermatologic surgery has increased in the past decade.
In a study published online Jan. 16 in JAMA Dermatology, researchers report the results of a cross-sectional analysis of antibiotic prescribing by 11,986 dermatologists between 2008 and 2016, using commercial claims data.
The analysis showed that, over this period of time, the overall rate of antibiotic prescribing by dermatologists decreased by 36.6%, from 3.36 courses per 100 dermatologist visits to 2.13 courses. In particular, antibiotic prescribing for acne decreased by 28.1%, from 11.76 courses per 100 visits to 8.45 courses, and for rosacea it decreased by 18.1%, from 10.89 courses per 100 visits to 8.92 courses.
John S. Barbieri, MD, of the department of dermatology, University of Pennsylvania, and his coauthors described the overall decline in antibiotic prescribing as “encouraging,” considering that in 2013 dermatologists were identified as the “most frequent prescribers of oral antibiotics per clinician.” The decline resulted in an estimated 480,000 fewer antibiotic courses a year, they noted.
“Much of the decrease in extended courses of antibiotic therapy is associated with visits for acne and rosacea,” they wrote. “Although recent guidelines suggest limiting the duration of therapy in this patient population, course duration has remained stable over time, suggesting that this decrease may be due to fewer patients being treated with antibiotics rather than patients being treated for a shorter duration.”
However, the rate of oral antibiotic prescriptions associated with surgical visits increased by 69.6%, from 3.92 courses per 100 visits to 6.65. This increase was concerning, given the risk of surgical-site infections was low, the authors pointed out. “In addition, a 2008 advisory statement on antibiotic prophylaxis recommends single-dose perioperative antibiotics for patients at increased risk of surgical-site infection,” they added.
The study also noted a 35.3% increase in antibiotic prescribing for cysts and a 3.2% increase for hidradenitis suppurativa.
Over the entire study period, nearly 1 million courses of oral antibiotics were prescribed. Doxycycline hyclate accounted for around one quarter of prescriptions, as did minocycline, while 19.9% of prescriptions were for cephalexin.
“Given the low rate of infectious complications, even for Mohs surgery, and the lack of evidence to support the use of prolonged rather than single-dose perioperative regimens, the postoperative courses of antibiotics identified in this study may increase risks to patients without substantial benefits,” they added.
The study was partly supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases. No conflicts of interest were declared.
SOURCE: Barbieri J et al. JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4944.
FROM JAMA DERMATOLOGY
Key clinical point: Antibiotic prescriptions by dermatologists have decreased since 2008.
Major finding: Between 2008 and 2016, antibiotic prescriptions by dermatologists dropped by 36.6%.
Study details: Cross-sectional analysis of antibiotic prescribing by 11,986 dermatologists from 2008 to 2016.
Disclosures: The study was partly supported by the National Institute of Arthritis and Musculoskeletal Skin Diseases. The authors had no disclosures.
Source: Barbieri J et al. JAMA Dermatology. 2019 Jan 16. doi: 10.1001/jamadermatol.2018.4944.
Will microneedling enhance the impact of photodynamic therapy?
ORLANDO –
Dr. Spencer, who practices in St. Petersburg, Fla., and is cochair of the conference, gave attendees a roundup of what’s new in adjuncts and delivery methods for photodynamic therapy (PDT). Among the updates is the promise of PDT delivered by means of an ultrashort incubation time of 10-20 minutes, followed by prolonged blue light exposure time of 1 hour. “The idea is that the enzymatic conversion is occurring during the light exposure,” Dr. Spencer said, adding that reports of this approach are mostly anecdotal.
A variation on the ultrashort incubation adds microneedling, he said. In one recent study, 33 patients who had facial actinic keratoses (AKs) were randomized to 10 or 20 minutes of incubation after application of aminolevulinic acid (ALA), followed by 1,000 seconds of exposure to blue light. However, in this split-face study, participants each had one side of their faces treated with microneedling and the other half with a sham treatment before ALA was applied.
Those who had the shorter incubation time had 43% of AKs cleared on the side that received microneedling, compared with 38% on the sham side. For those who received 20 minutes of ALA incubation, rates were higher, with 76% AK clearance on the treated side and 58% on the sham side. “Patients reported that the procedure was virtually painless on both sides,” said Dr. Spencer.
Though the addition of microneedling to PDT is a newer trend, there’s one that’s been a mainstay in Europe for some time: daylight PDT. He cited a review article published in 2016, which identified 17 studies on the use of daylight PDT (Dermatol Surg. 2016 Mar;42[3]:286-95).
Advantages of daylight PDT, he said, include less time in the office for patients and “supposedly less pain.” European protocols vary, but most use methyl aminolevulinate, which he said is a “little more lipophilic than ALA,” with incubation times ranging from 0 to 30 minutes. Exposure time is also variable, but will usually range from 1.5 to 2.5 hours. Most patients receive just one treatment, but some protocols will include up to three treatments.
Overall, studies show a range from 46% to almost 90% complete response rates when AKs are treated with daylight PDT. One study that looked at daylight PDT for small basal cell carcinomas showed that 94% of patients had clinical clearance of their lesions after two treatment sessions; however, the recurrence rate at 12 months post therapy was 21%, Dr. Spencer said.
He shared results of a recent head-to-head study of conventional and daylight PDT; conducted in Greece, the study enrolled patients with “high sun exposure” and used a split-face design.
Of the 46 patients who received MAL on both sides of their faces, response rates were similar at both 3 and 12 months, with slightly numerically higher clearance rates for conventional versus daylight PDT. The 3-month clearance rate for conventional PDT was 80.6%, compared with 78.0% for daylight PDT. At 12 months, the respective clearance rates were 73.7% and 71.8% (J Eur Acad Dermatol Venereol. 2018 Apr;32[4]:595-600). However, “significantly less pain was reported with daylight PDT,” Dr. Spencer said.
Daylight PDT hasn’t caught on the United States. Physicians have concern about the lack of control of UV dosing, and, he pointed out, “this, of course, is not billable.”
Dr. Spencer reported that he serves on the speakers bureau for Genentech.
ORLANDO –
Dr. Spencer, who practices in St. Petersburg, Fla., and is cochair of the conference, gave attendees a roundup of what’s new in adjuncts and delivery methods for photodynamic therapy (PDT). Among the updates is the promise of PDT delivered by means of an ultrashort incubation time of 10-20 minutes, followed by prolonged blue light exposure time of 1 hour. “The idea is that the enzymatic conversion is occurring during the light exposure,” Dr. Spencer said, adding that reports of this approach are mostly anecdotal.
A variation on the ultrashort incubation adds microneedling, he said. In one recent study, 33 patients who had facial actinic keratoses (AKs) were randomized to 10 or 20 minutes of incubation after application of aminolevulinic acid (ALA), followed by 1,000 seconds of exposure to blue light. However, in this split-face study, participants each had one side of their faces treated with microneedling and the other half with a sham treatment before ALA was applied.
Those who had the shorter incubation time had 43% of AKs cleared on the side that received microneedling, compared with 38% on the sham side. For those who received 20 minutes of ALA incubation, rates were higher, with 76% AK clearance on the treated side and 58% on the sham side. “Patients reported that the procedure was virtually painless on both sides,” said Dr. Spencer.
Though the addition of microneedling to PDT is a newer trend, there’s one that’s been a mainstay in Europe for some time: daylight PDT. He cited a review article published in 2016, which identified 17 studies on the use of daylight PDT (Dermatol Surg. 2016 Mar;42[3]:286-95).
Advantages of daylight PDT, he said, include less time in the office for patients and “supposedly less pain.” European protocols vary, but most use methyl aminolevulinate, which he said is a “little more lipophilic than ALA,” with incubation times ranging from 0 to 30 minutes. Exposure time is also variable, but will usually range from 1.5 to 2.5 hours. Most patients receive just one treatment, but some protocols will include up to three treatments.
Overall, studies show a range from 46% to almost 90% complete response rates when AKs are treated with daylight PDT. One study that looked at daylight PDT for small basal cell carcinomas showed that 94% of patients had clinical clearance of their lesions after two treatment sessions; however, the recurrence rate at 12 months post therapy was 21%, Dr. Spencer said.
He shared results of a recent head-to-head study of conventional and daylight PDT; conducted in Greece, the study enrolled patients with “high sun exposure” and used a split-face design.
Of the 46 patients who received MAL on both sides of their faces, response rates were similar at both 3 and 12 months, with slightly numerically higher clearance rates for conventional versus daylight PDT. The 3-month clearance rate for conventional PDT was 80.6%, compared with 78.0% for daylight PDT. At 12 months, the respective clearance rates were 73.7% and 71.8% (J Eur Acad Dermatol Venereol. 2018 Apr;32[4]:595-600). However, “significantly less pain was reported with daylight PDT,” Dr. Spencer said.
Daylight PDT hasn’t caught on the United States. Physicians have concern about the lack of control of UV dosing, and, he pointed out, “this, of course, is not billable.”
Dr. Spencer reported that he serves on the speakers bureau for Genentech.
ORLANDO –
Dr. Spencer, who practices in St. Petersburg, Fla., and is cochair of the conference, gave attendees a roundup of what’s new in adjuncts and delivery methods for photodynamic therapy (PDT). Among the updates is the promise of PDT delivered by means of an ultrashort incubation time of 10-20 minutes, followed by prolonged blue light exposure time of 1 hour. “The idea is that the enzymatic conversion is occurring during the light exposure,” Dr. Spencer said, adding that reports of this approach are mostly anecdotal.
A variation on the ultrashort incubation adds microneedling, he said. In one recent study, 33 patients who had facial actinic keratoses (AKs) were randomized to 10 or 20 minutes of incubation after application of aminolevulinic acid (ALA), followed by 1,000 seconds of exposure to blue light. However, in this split-face study, participants each had one side of their faces treated with microneedling and the other half with a sham treatment before ALA was applied.
Those who had the shorter incubation time had 43% of AKs cleared on the side that received microneedling, compared with 38% on the sham side. For those who received 20 minutes of ALA incubation, rates were higher, with 76% AK clearance on the treated side and 58% on the sham side. “Patients reported that the procedure was virtually painless on both sides,” said Dr. Spencer.
Though the addition of microneedling to PDT is a newer trend, there’s one that’s been a mainstay in Europe for some time: daylight PDT. He cited a review article published in 2016, which identified 17 studies on the use of daylight PDT (Dermatol Surg. 2016 Mar;42[3]:286-95).
Advantages of daylight PDT, he said, include less time in the office for patients and “supposedly less pain.” European protocols vary, but most use methyl aminolevulinate, which he said is a “little more lipophilic than ALA,” with incubation times ranging from 0 to 30 minutes. Exposure time is also variable, but will usually range from 1.5 to 2.5 hours. Most patients receive just one treatment, but some protocols will include up to three treatments.
Overall, studies show a range from 46% to almost 90% complete response rates when AKs are treated with daylight PDT. One study that looked at daylight PDT for small basal cell carcinomas showed that 94% of patients had clinical clearance of their lesions after two treatment sessions; however, the recurrence rate at 12 months post therapy was 21%, Dr. Spencer said.
He shared results of a recent head-to-head study of conventional and daylight PDT; conducted in Greece, the study enrolled patients with “high sun exposure” and used a split-face design.
Of the 46 patients who received MAL on both sides of their faces, response rates were similar at both 3 and 12 months, with slightly numerically higher clearance rates for conventional versus daylight PDT. The 3-month clearance rate for conventional PDT was 80.6%, compared with 78.0% for daylight PDT. At 12 months, the respective clearance rates were 73.7% and 71.8% (J Eur Acad Dermatol Venereol. 2018 Apr;32[4]:595-600). However, “significantly less pain was reported with daylight PDT,” Dr. Spencer said.
Daylight PDT hasn’t caught on the United States. Physicians have concern about the lack of control of UV dosing, and, he pointed out, “this, of course, is not billable.”
Dr. Spencer reported that he serves on the speakers bureau for Genentech.
EXPERT ANALYSIS FROM ODAC 2019
When sweaty palms are more than just sweaty palms
ORLANDO – When you extend your hand to a new patient, and he reflexively wipes his palm before shaking hands, be alert. It’s possible you’re seeing primary hyperhidrosis, a condition that’s both more common and more disabling than once thought.
“Looking at the biology of sweating, normally, it’s a good thing – we need it to survive. However, hyperhidrosis is too much of a good thing – it’s an excess of what is needed for normal biology,” said Adam Friedman, MD, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
Recent data, he pointed out, show that hyperhidrosis is more prevalent than previously thought – about 4.8% of individuals may have the condition, with about half having axillary hyperhidrosis. Symptoms peak in early adulthood, with adults aged 18-54 most affected. “These are the prime working years,” he said.
About 2% of teens are affected, and many adults report that symptoms began before they were 12 years old. Hand hyperhidrosis is a factor for computer and electronic device work, sports, and even handling paper and pencils, noted Dr. Friedman, professor of dermatology at George Washington University, Washington.
“Does it affect quality of life? Yes. We have data to support the impact. The adverse impact is actually greater than that of eczema and psoriasis,” he said, adding that patients won’t always bring up their concerns about sweating. “Often, it’s the patient who apologizes for having sweaty palms or who sticks to the paper on the exam table. It’s worth asking these patients if they are bothered by excessive sweating.”
Is it hyperhidrosis?
A 2016 paper defined hyperhidrosis as “a condition that involves chronic excessive sweating of the underarms, hands, feet, face, groin, or other bodily areas, which is much more than what is normal, and occurs regardless of temperature, exercise, or situation, and may have an impact on quality of life” (Arch Dermatol Res. 2016 Dec;308[10]:743-9). The amount of sweating can be four to five times that seen in healthy controls.
Other clues that excess sweating might be hyperhidrosis? General hyperhidrosis is a secondary syndrome that can be caused by a variety of conditions including endocrine and metabolic disorders and malignancies. Drugs and toxins can also cause generalized excessive sweating.
Focal hyperhidrosis can be primary idiopathic disease; some neuropathies and certain spinal diseases and spinal cord injury can also cause focal hyperhidrosis, though not usually in the axillary/palmar/plantar distribution seen in primary hyperhidrosis.
Before settling on primary hyperhidrosis, the history and exam should also account for other possibilities in the differential: social anxiety disorder, eccrine nevus, gustatory sweating, Frey syndrome, and impaired evaporation could all account for excess sweating, which is also a postsurgical phenomenon for some patients.
Diagnostic criteria call for “focal, visible, excessive sweating” persisting for at least 6 months with no apparent cause. Additionally, patients must have at least two of the additional following criteria: sweating that is bilateral and symmetric, occurs at least once weekly, impairs daily activities, and starts before age 25 years, as well as a positive family history of hyperhidrosis and cessation of sweating during sleep.
The last point is critical, Dr. Friedman said. “If you sweat a lot at night, it’s not hyperhidrosis!”
Though gravimetric evaluation is used in hyperhidrosis research, the history and exam are really where the diagnosis is made in practice, he noted. The Hyperhidrosis Disease Severity Scale is a brief, useful clinical tool that asks patients to peg the extent to which their sweating interferes with daily life.
Topical treatments to try
Topical antiperspirants and other topical agents are a logical place to start and may be required as part of step therapy by insurers. Many patients will already have tried clinical strength over-the-counter antiperspirants containing aluminum zirconium trichlorohydrex, but these products rate low in patient satisfaction among those with primary hyperhidrosis.
Prescription aluminum salts can be compounded to various strengths, with 10%-20% concentration appropriate for axillae and 30%-40% a good strength for palms and soles, according to Dr. Friedman. All of these agents work by precipitating out solids that form a shallow plug in sweat ducts, slowing the flow of perspiration.
Pearls for topical treatment include the need for the product to be on the skin for 6-8 hours overnight. “Remember hyperhidrosis patients do not sweat at night,” so this is the time when the occlusive plugs can form. Then residue can be washed off in the morning, and patients can apply a deodorant. “I remind my patients that antiperspirants are for sweating, and deodorants are for odor,” said Dr. Friedman. These products can damage fabric, and they can be irritating, a problem addressed with low-potency topical steroids.
Topical regimens don’t need to be adjusted for pediatric patients, said Dr. Friedman.
Iontophoresis has been around since the 1950s, is effective, has few side effects, and is considered first-line treatment for severe palmar and plantar hyperhidrosis. But he said there’s one big rub: time. To be effective, patients need 20-30 minutes of application of 15-20 milliamperes of current 3-4 times weekly, not a schedule that works for most patients or practitioners, Dr. Friedman noted.
A treatment recently approved by the Food and Drug Administration for primary axillary hyperhidrosis is a topical anticholinergic, glycopyrronium tosylate, applied with wipes impregnated with glycopyrronium solution. This product significantly outperformed placebo in two clinical trials, with up to 64% of users meeting the primary endpoint of improving by at least 4 points on the Axillary Sweating Daily Diary (ASDD) scale. This product significantly outperformed placebo in two clinical trials, with 53% and 66% of users meeting the primary endpoint, improvement of at least 4 points from baseline in the weekly mean ASDD Item #2. It was approved in those aged 9 years and older.
“You can use this in kids, but you need to educate the kid and the parent or adult,” he said. “This is the last thing you do before bed, after brushing your teeth and after washing your face.”
Patients should apply one swipe to the clean skin of each underarm, and then wash their hands thoroughly. Clinical trials saw a greater proportion of off-target effects such as dry eyes and mouth and mydriasis in the active arm; unilateral mydriasis was more common than bilateral, underscoring the importance of hand washing as this was probably secondary transfer from hands to face during sleep, said Dr. Friedman. Patients can expect results in 2-3 weeks, and doses can be held as needed for anticholinergic side effects.
Systemic choices are limited
There are no FDA-approved systemic agents for hyperhidrosis, and the literature holds only case reports or small series, Dr. Friedman pointed out.
Though systemic treatment may be more effective in generalized hyperhidrosis and for patients with dysautonomia-associated hyperhidrosis, glycopyrrolate is a logical choice if a systemic anticholinergic is desired. A starting dose of 1 mg twice daily can be titrated for effect to about 6 mg daily. Though off-target effects may be a dose-limiting factor, glycopyrrolate is not very lipid soluble, so it penetrates the blood-brain barrier relatively poorly, he said.
Oxybutynin is available in many forms, including a slow-release tablet that permits once-daily dosing. Starting at 5-10 mg daily is a good idea, but dosing may need to be increased to as high as 20 mg daily to be effective. However, patients will often experience “major side effects” with oxybutynin, including significant xerostomia, constipation, blurred vision, and difficulty urinating.
For children, small studies have seen improvement with glycopyrrolate at an average dose of about 2 mg/day. Oxybutynin, which has been extensively studied in the pediatric population, was also effective, but central nervous system adverse events were common.
For some, beta-adrenergic blockade can be an extremely valuable tool, said Dr. Friedman. When sweating is linked to social phobia or performance anxiety, 10-20 mg of atenolol about an hour before the performance or public appearance can make a big difference. Bradycardia, atrioventricular block, and asthma are all contraindications, and the usual precautions should be taken with a host of other comorbidities, he noted.
It’s a good idea to check resting blood pressure and heart rate and take body mass into consideration, and adjust the dose downward appropriately. A key pearl: “Have them do a test run at home, to make sure they don’t keel over on the podium!” said Dr. Friedman.
Botulinum toxin tips and tricks
Botulinum toxin can be very effective and works directly by blocking acetylcholine release at the junction of the sympathetic sudomotor neuron and the sweat gland.
Before treatment, make sure the patient prepares correctly by abstaining from over-the-counter deodorants or antiperspirants, and resting without exertion or drinking hot beverages for about 30 minutes before the procedure.
To ascertain the follicular outline of the area to be injected, the iodine starch test can be used: Paint the axilla with iodine, allow it to dry, and then dust corn starch over the area. The follicular outline is mapped by the purple-blue reaction of the starch and iodine in the presence of moisture from perspiration, Dr. Friedman said.
Applying topical analgesia 30 minutes prior to the procedure helps with patient discomfort with axillary injections. When it comes time to inject, a shallow approach with the bevel side up works well, with a goal of blanketing the field identified by the iodine starch test with small aliquots of toxin placed 1-2 centimeters apart, said Dr. Friedman. However, for patients who might have tattoos that extend to the axillary area, “Avoid the ink!”
Patients will start to see improvement within 2-4 days, and although the literature says a toxin treatment can last 6-9 months, Dr. Friedman said he sees patients coming back in 4-5 months.
Obtaining botulinum toxin can be done in one of two ways: the “buy and bill” approach has the dermatologist purchasing the medication, using CPT 64650 and J code J0585 – “Remember the units!” said Dr. Friedman, because reimbursement will be based on the volume of toxin purchased.. This route may be cheaper for the patient because it avoids a medication copay. The physician obtains preauthorization for both the medication and procedure with this strategy.
The other route is to have the provider prescribe botulinum toxin and the patient purchase it at a regular or specialty pharmacy. In this case, the pharmacist obtains precertification for the medication, but the physician still needs to be precertified – and bill – for the injection procedure itself. This scenario is less risky for the physician but may trigger two separate copays for the patient.
Botulinum toxin can be effective for up to 90% of patients, but at a cost: Without insurance reimbursement, treatments can cost in the neighborhood of $1,500.
A good resource for patients and clinicians is the International Hyperhidrosis Society’s website (sweathelp.org), said Dr. Friedman.
Dr. Friedman disclosed relationships with multiple pharmaceutical and cosmetic companies, including Dermira, which markets topical glycopyrronium tosylate as Qbrexza.
ORLANDO – When you extend your hand to a new patient, and he reflexively wipes his palm before shaking hands, be alert. It’s possible you’re seeing primary hyperhidrosis, a condition that’s both more common and more disabling than once thought.
“Looking at the biology of sweating, normally, it’s a good thing – we need it to survive. However, hyperhidrosis is too much of a good thing – it’s an excess of what is needed for normal biology,” said Adam Friedman, MD, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
Recent data, he pointed out, show that hyperhidrosis is more prevalent than previously thought – about 4.8% of individuals may have the condition, with about half having axillary hyperhidrosis. Symptoms peak in early adulthood, with adults aged 18-54 most affected. “These are the prime working years,” he said.
About 2% of teens are affected, and many adults report that symptoms began before they were 12 years old. Hand hyperhidrosis is a factor for computer and electronic device work, sports, and even handling paper and pencils, noted Dr. Friedman, professor of dermatology at George Washington University, Washington.
“Does it affect quality of life? Yes. We have data to support the impact. The adverse impact is actually greater than that of eczema and psoriasis,” he said, adding that patients won’t always bring up their concerns about sweating. “Often, it’s the patient who apologizes for having sweaty palms or who sticks to the paper on the exam table. It’s worth asking these patients if they are bothered by excessive sweating.”
Is it hyperhidrosis?
A 2016 paper defined hyperhidrosis as “a condition that involves chronic excessive sweating of the underarms, hands, feet, face, groin, or other bodily areas, which is much more than what is normal, and occurs regardless of temperature, exercise, or situation, and may have an impact on quality of life” (Arch Dermatol Res. 2016 Dec;308[10]:743-9). The amount of sweating can be four to five times that seen in healthy controls.
Other clues that excess sweating might be hyperhidrosis? General hyperhidrosis is a secondary syndrome that can be caused by a variety of conditions including endocrine and metabolic disorders and malignancies. Drugs and toxins can also cause generalized excessive sweating.
Focal hyperhidrosis can be primary idiopathic disease; some neuropathies and certain spinal diseases and spinal cord injury can also cause focal hyperhidrosis, though not usually in the axillary/palmar/plantar distribution seen in primary hyperhidrosis.
Before settling on primary hyperhidrosis, the history and exam should also account for other possibilities in the differential: social anxiety disorder, eccrine nevus, gustatory sweating, Frey syndrome, and impaired evaporation could all account for excess sweating, which is also a postsurgical phenomenon for some patients.
Diagnostic criteria call for “focal, visible, excessive sweating” persisting for at least 6 months with no apparent cause. Additionally, patients must have at least two of the additional following criteria: sweating that is bilateral and symmetric, occurs at least once weekly, impairs daily activities, and starts before age 25 years, as well as a positive family history of hyperhidrosis and cessation of sweating during sleep.
The last point is critical, Dr. Friedman said. “If you sweat a lot at night, it’s not hyperhidrosis!”
Though gravimetric evaluation is used in hyperhidrosis research, the history and exam are really where the diagnosis is made in practice, he noted. The Hyperhidrosis Disease Severity Scale is a brief, useful clinical tool that asks patients to peg the extent to which their sweating interferes with daily life.
Topical treatments to try
Topical antiperspirants and other topical agents are a logical place to start and may be required as part of step therapy by insurers. Many patients will already have tried clinical strength over-the-counter antiperspirants containing aluminum zirconium trichlorohydrex, but these products rate low in patient satisfaction among those with primary hyperhidrosis.
Prescription aluminum salts can be compounded to various strengths, with 10%-20% concentration appropriate for axillae and 30%-40% a good strength for palms and soles, according to Dr. Friedman. All of these agents work by precipitating out solids that form a shallow plug in sweat ducts, slowing the flow of perspiration.
Pearls for topical treatment include the need for the product to be on the skin for 6-8 hours overnight. “Remember hyperhidrosis patients do not sweat at night,” so this is the time when the occlusive plugs can form. Then residue can be washed off in the morning, and patients can apply a deodorant. “I remind my patients that antiperspirants are for sweating, and deodorants are for odor,” said Dr. Friedman. These products can damage fabric, and they can be irritating, a problem addressed with low-potency topical steroids.
Topical regimens don’t need to be adjusted for pediatric patients, said Dr. Friedman.
Iontophoresis has been around since the 1950s, is effective, has few side effects, and is considered first-line treatment for severe palmar and plantar hyperhidrosis. But he said there’s one big rub: time. To be effective, patients need 20-30 minutes of application of 15-20 milliamperes of current 3-4 times weekly, not a schedule that works for most patients or practitioners, Dr. Friedman noted.
A treatment recently approved by the Food and Drug Administration for primary axillary hyperhidrosis is a topical anticholinergic, glycopyrronium tosylate, applied with wipes impregnated with glycopyrronium solution. This product significantly outperformed placebo in two clinical trials, with up to 64% of users meeting the primary endpoint of improving by at least 4 points on the Axillary Sweating Daily Diary (ASDD) scale. This product significantly outperformed placebo in two clinical trials, with 53% and 66% of users meeting the primary endpoint, improvement of at least 4 points from baseline in the weekly mean ASDD Item #2. It was approved in those aged 9 years and older.
“You can use this in kids, but you need to educate the kid and the parent or adult,” he said. “This is the last thing you do before bed, after brushing your teeth and after washing your face.”
Patients should apply one swipe to the clean skin of each underarm, and then wash their hands thoroughly. Clinical trials saw a greater proportion of off-target effects such as dry eyes and mouth and mydriasis in the active arm; unilateral mydriasis was more common than bilateral, underscoring the importance of hand washing as this was probably secondary transfer from hands to face during sleep, said Dr. Friedman. Patients can expect results in 2-3 weeks, and doses can be held as needed for anticholinergic side effects.
Systemic choices are limited
There are no FDA-approved systemic agents for hyperhidrosis, and the literature holds only case reports or small series, Dr. Friedman pointed out.
Though systemic treatment may be more effective in generalized hyperhidrosis and for patients with dysautonomia-associated hyperhidrosis, glycopyrrolate is a logical choice if a systemic anticholinergic is desired. A starting dose of 1 mg twice daily can be titrated for effect to about 6 mg daily. Though off-target effects may be a dose-limiting factor, glycopyrrolate is not very lipid soluble, so it penetrates the blood-brain barrier relatively poorly, he said.
Oxybutynin is available in many forms, including a slow-release tablet that permits once-daily dosing. Starting at 5-10 mg daily is a good idea, but dosing may need to be increased to as high as 20 mg daily to be effective. However, patients will often experience “major side effects” with oxybutynin, including significant xerostomia, constipation, blurred vision, and difficulty urinating.
For children, small studies have seen improvement with glycopyrrolate at an average dose of about 2 mg/day. Oxybutynin, which has been extensively studied in the pediatric population, was also effective, but central nervous system adverse events were common.
For some, beta-adrenergic blockade can be an extremely valuable tool, said Dr. Friedman. When sweating is linked to social phobia or performance anxiety, 10-20 mg of atenolol about an hour before the performance or public appearance can make a big difference. Bradycardia, atrioventricular block, and asthma are all contraindications, and the usual precautions should be taken with a host of other comorbidities, he noted.
It’s a good idea to check resting blood pressure and heart rate and take body mass into consideration, and adjust the dose downward appropriately. A key pearl: “Have them do a test run at home, to make sure they don’t keel over on the podium!” said Dr. Friedman.
Botulinum toxin tips and tricks
Botulinum toxin can be very effective and works directly by blocking acetylcholine release at the junction of the sympathetic sudomotor neuron and the sweat gland.
Before treatment, make sure the patient prepares correctly by abstaining from over-the-counter deodorants or antiperspirants, and resting without exertion or drinking hot beverages for about 30 minutes before the procedure.
To ascertain the follicular outline of the area to be injected, the iodine starch test can be used: Paint the axilla with iodine, allow it to dry, and then dust corn starch over the area. The follicular outline is mapped by the purple-blue reaction of the starch and iodine in the presence of moisture from perspiration, Dr. Friedman said.
Applying topical analgesia 30 minutes prior to the procedure helps with patient discomfort with axillary injections. When it comes time to inject, a shallow approach with the bevel side up works well, with a goal of blanketing the field identified by the iodine starch test with small aliquots of toxin placed 1-2 centimeters apart, said Dr. Friedman. However, for patients who might have tattoos that extend to the axillary area, “Avoid the ink!”
Patients will start to see improvement within 2-4 days, and although the literature says a toxin treatment can last 6-9 months, Dr. Friedman said he sees patients coming back in 4-5 months.
Obtaining botulinum toxin can be done in one of two ways: the “buy and bill” approach has the dermatologist purchasing the medication, using CPT 64650 and J code J0585 – “Remember the units!” said Dr. Friedman, because reimbursement will be based on the volume of toxin purchased.. This route may be cheaper for the patient because it avoids a medication copay. The physician obtains preauthorization for both the medication and procedure with this strategy.
The other route is to have the provider prescribe botulinum toxin and the patient purchase it at a regular or specialty pharmacy. In this case, the pharmacist obtains precertification for the medication, but the physician still needs to be precertified – and bill – for the injection procedure itself. This scenario is less risky for the physician but may trigger two separate copays for the patient.
Botulinum toxin can be effective for up to 90% of patients, but at a cost: Without insurance reimbursement, treatments can cost in the neighborhood of $1,500.
A good resource for patients and clinicians is the International Hyperhidrosis Society’s website (sweathelp.org), said Dr. Friedman.
Dr. Friedman disclosed relationships with multiple pharmaceutical and cosmetic companies, including Dermira, which markets topical glycopyrronium tosylate as Qbrexza.
ORLANDO – When you extend your hand to a new patient, and he reflexively wipes his palm before shaking hands, be alert. It’s possible you’re seeing primary hyperhidrosis, a condition that’s both more common and more disabling than once thought.
“Looking at the biology of sweating, normally, it’s a good thing – we need it to survive. However, hyperhidrosis is too much of a good thing – it’s an excess of what is needed for normal biology,” said Adam Friedman, MD, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
Recent data, he pointed out, show that hyperhidrosis is more prevalent than previously thought – about 4.8% of individuals may have the condition, with about half having axillary hyperhidrosis. Symptoms peak in early adulthood, with adults aged 18-54 most affected. “These are the prime working years,” he said.
About 2% of teens are affected, and many adults report that symptoms began before they were 12 years old. Hand hyperhidrosis is a factor for computer and electronic device work, sports, and even handling paper and pencils, noted Dr. Friedman, professor of dermatology at George Washington University, Washington.
“Does it affect quality of life? Yes. We have data to support the impact. The adverse impact is actually greater than that of eczema and psoriasis,” he said, adding that patients won’t always bring up their concerns about sweating. “Often, it’s the patient who apologizes for having sweaty palms or who sticks to the paper on the exam table. It’s worth asking these patients if they are bothered by excessive sweating.”
Is it hyperhidrosis?
A 2016 paper defined hyperhidrosis as “a condition that involves chronic excessive sweating of the underarms, hands, feet, face, groin, or other bodily areas, which is much more than what is normal, and occurs regardless of temperature, exercise, or situation, and may have an impact on quality of life” (Arch Dermatol Res. 2016 Dec;308[10]:743-9). The amount of sweating can be four to five times that seen in healthy controls.
Other clues that excess sweating might be hyperhidrosis? General hyperhidrosis is a secondary syndrome that can be caused by a variety of conditions including endocrine and metabolic disorders and malignancies. Drugs and toxins can also cause generalized excessive sweating.
Focal hyperhidrosis can be primary idiopathic disease; some neuropathies and certain spinal diseases and spinal cord injury can also cause focal hyperhidrosis, though not usually in the axillary/palmar/plantar distribution seen in primary hyperhidrosis.
Before settling on primary hyperhidrosis, the history and exam should also account for other possibilities in the differential: social anxiety disorder, eccrine nevus, gustatory sweating, Frey syndrome, and impaired evaporation could all account for excess sweating, which is also a postsurgical phenomenon for some patients.
Diagnostic criteria call for “focal, visible, excessive sweating” persisting for at least 6 months with no apparent cause. Additionally, patients must have at least two of the additional following criteria: sweating that is bilateral and symmetric, occurs at least once weekly, impairs daily activities, and starts before age 25 years, as well as a positive family history of hyperhidrosis and cessation of sweating during sleep.
The last point is critical, Dr. Friedman said. “If you sweat a lot at night, it’s not hyperhidrosis!”
Though gravimetric evaluation is used in hyperhidrosis research, the history and exam are really where the diagnosis is made in practice, he noted. The Hyperhidrosis Disease Severity Scale is a brief, useful clinical tool that asks patients to peg the extent to which their sweating interferes with daily life.
Topical treatments to try
Topical antiperspirants and other topical agents are a logical place to start and may be required as part of step therapy by insurers. Many patients will already have tried clinical strength over-the-counter antiperspirants containing aluminum zirconium trichlorohydrex, but these products rate low in patient satisfaction among those with primary hyperhidrosis.
Prescription aluminum salts can be compounded to various strengths, with 10%-20% concentration appropriate for axillae and 30%-40% a good strength for palms and soles, according to Dr. Friedman. All of these agents work by precipitating out solids that form a shallow plug in sweat ducts, slowing the flow of perspiration.
Pearls for topical treatment include the need for the product to be on the skin for 6-8 hours overnight. “Remember hyperhidrosis patients do not sweat at night,” so this is the time when the occlusive plugs can form. Then residue can be washed off in the morning, and patients can apply a deodorant. “I remind my patients that antiperspirants are for sweating, and deodorants are for odor,” said Dr. Friedman. These products can damage fabric, and they can be irritating, a problem addressed with low-potency topical steroids.
Topical regimens don’t need to be adjusted for pediatric patients, said Dr. Friedman.
Iontophoresis has been around since the 1950s, is effective, has few side effects, and is considered first-line treatment for severe palmar and plantar hyperhidrosis. But he said there’s one big rub: time. To be effective, patients need 20-30 minutes of application of 15-20 milliamperes of current 3-4 times weekly, not a schedule that works for most patients or practitioners, Dr. Friedman noted.
A treatment recently approved by the Food and Drug Administration for primary axillary hyperhidrosis is a topical anticholinergic, glycopyrronium tosylate, applied with wipes impregnated with glycopyrronium solution. This product significantly outperformed placebo in two clinical trials, with up to 64% of users meeting the primary endpoint of improving by at least 4 points on the Axillary Sweating Daily Diary (ASDD) scale. This product significantly outperformed placebo in two clinical trials, with 53% and 66% of users meeting the primary endpoint, improvement of at least 4 points from baseline in the weekly mean ASDD Item #2. It was approved in those aged 9 years and older.
“You can use this in kids, but you need to educate the kid and the parent or adult,” he said. “This is the last thing you do before bed, after brushing your teeth and after washing your face.”
Patients should apply one swipe to the clean skin of each underarm, and then wash their hands thoroughly. Clinical trials saw a greater proportion of off-target effects such as dry eyes and mouth and mydriasis in the active arm; unilateral mydriasis was more common than bilateral, underscoring the importance of hand washing as this was probably secondary transfer from hands to face during sleep, said Dr. Friedman. Patients can expect results in 2-3 weeks, and doses can be held as needed for anticholinergic side effects.
Systemic choices are limited
There are no FDA-approved systemic agents for hyperhidrosis, and the literature holds only case reports or small series, Dr. Friedman pointed out.
Though systemic treatment may be more effective in generalized hyperhidrosis and for patients with dysautonomia-associated hyperhidrosis, glycopyrrolate is a logical choice if a systemic anticholinergic is desired. A starting dose of 1 mg twice daily can be titrated for effect to about 6 mg daily. Though off-target effects may be a dose-limiting factor, glycopyrrolate is not very lipid soluble, so it penetrates the blood-brain barrier relatively poorly, he said.
Oxybutynin is available in many forms, including a slow-release tablet that permits once-daily dosing. Starting at 5-10 mg daily is a good idea, but dosing may need to be increased to as high as 20 mg daily to be effective. However, patients will often experience “major side effects” with oxybutynin, including significant xerostomia, constipation, blurred vision, and difficulty urinating.
For children, small studies have seen improvement with glycopyrrolate at an average dose of about 2 mg/day. Oxybutynin, which has been extensively studied in the pediatric population, was also effective, but central nervous system adverse events were common.
For some, beta-adrenergic blockade can be an extremely valuable tool, said Dr. Friedman. When sweating is linked to social phobia or performance anxiety, 10-20 mg of atenolol about an hour before the performance or public appearance can make a big difference. Bradycardia, atrioventricular block, and asthma are all contraindications, and the usual precautions should be taken with a host of other comorbidities, he noted.
It’s a good idea to check resting blood pressure and heart rate and take body mass into consideration, and adjust the dose downward appropriately. A key pearl: “Have them do a test run at home, to make sure they don’t keel over on the podium!” said Dr. Friedman.
Botulinum toxin tips and tricks
Botulinum toxin can be very effective and works directly by blocking acetylcholine release at the junction of the sympathetic sudomotor neuron and the sweat gland.
Before treatment, make sure the patient prepares correctly by abstaining from over-the-counter deodorants or antiperspirants, and resting without exertion or drinking hot beverages for about 30 minutes before the procedure.
To ascertain the follicular outline of the area to be injected, the iodine starch test can be used: Paint the axilla with iodine, allow it to dry, and then dust corn starch over the area. The follicular outline is mapped by the purple-blue reaction of the starch and iodine in the presence of moisture from perspiration, Dr. Friedman said.
Applying topical analgesia 30 minutes prior to the procedure helps with patient discomfort with axillary injections. When it comes time to inject, a shallow approach with the bevel side up works well, with a goal of blanketing the field identified by the iodine starch test with small aliquots of toxin placed 1-2 centimeters apart, said Dr. Friedman. However, for patients who might have tattoos that extend to the axillary area, “Avoid the ink!”
Patients will start to see improvement within 2-4 days, and although the literature says a toxin treatment can last 6-9 months, Dr. Friedman said he sees patients coming back in 4-5 months.
Obtaining botulinum toxin can be done in one of two ways: the “buy and bill” approach has the dermatologist purchasing the medication, using CPT 64650 and J code J0585 – “Remember the units!” said Dr. Friedman, because reimbursement will be based on the volume of toxin purchased.. This route may be cheaper for the patient because it avoids a medication copay. The physician obtains preauthorization for both the medication and procedure with this strategy.
The other route is to have the provider prescribe botulinum toxin and the patient purchase it at a regular or specialty pharmacy. In this case, the pharmacist obtains precertification for the medication, but the physician still needs to be precertified – and bill – for the injection procedure itself. This scenario is less risky for the physician but may trigger two separate copays for the patient.
Botulinum toxin can be effective for up to 90% of patients, but at a cost: Without insurance reimbursement, treatments can cost in the neighborhood of $1,500.
A good resource for patients and clinicians is the International Hyperhidrosis Society’s website (sweathelp.org), said Dr. Friedman.
Dr. Friedman disclosed relationships with multiple pharmaceutical and cosmetic companies, including Dermira, which markets topical glycopyrronium tosylate as Qbrexza.
EXPERT ANALYSIS FROM ODAC 2019
Combo treatment may improve quality of life in CTCL
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Five of six evaluable CTCL patients had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment.
Study details: A phase 2 study with results reported for 10 patients.
Disclosures: The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. The principal investigator reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
How not to miss the ‘invisible gorilla’: Visual intelligence in dermatology
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Plerixafor produced dramatic responses in severe WHIM syndrome
Low-dose treatment with plerixafor, a CXC chemokine receptor 4 antagonist, was well tolerated and markedly improved severe presentations of warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) syndrome in three patients who could not receive granulocyte colony-stimulating factor therapy, investigators reported.
“Myelofibrosis, panleukopenia, anemia, and thrombocytopenia were ameliorated, the wart burden and frequency of infection declined, human papillomavirus–associated oropharyngeal squamous-cell carcinoma stabilized, and quality of life improved markedly,” David H. McDermott, MD, of the National Institute of Allergy and Infectious Diseases and his colleagues wrote in the New England Journal of Medicine.
WHIM syndrome is a primary immunodeficiency disorder characterized by panleukopenia and caused by autosomal dominant gain-of-function mutations in CXC chemokine receptor 4 (CXCR4). Granulocyte colony-stimulating factor (G-CSF) therapy improves neutropenia in these patients, but not other cytopenias.
Previously, the investigators treated three WHIM syndrome patients with plerixafor (Mozobil), which was well tolerated and led to sustained increases in circulating neutrophils, lymphocytes, and monocytes. The current report is of three patients with advanced WHIM syndrome who received open-label plerixafor because they were ineligible for a randomized trial of this drug.
After treatment initiation, infection frequency dropped by 85% in one patient and declined markedly in all three patients. Lymphocyte counts improved the most in two patients while neutrophils were most responsive in the third patient. Warts partially resolved in two patients, of which one patient also experienced partial resolution of head and neck squamous cell carcinoma. This patient later died of a multidrug-resistant Pseudomonas aeruginosa infection after undergoing a 9-hour surgery.
In the third patient, plerixafor therapy led to clearance of TSPyV and 17 human papillomavirus (HPV) infections, with consequent resolution of chronic, progressive, multifocal eczematoid and follicular lesions, the researchers reported. The study dose was relatively low – about 10% of the stem-cell mobilization dose – and did not cause bone pain or other treatment-emergent adverse events, despite the relatively long treatment course (19-52 months).
A separate, phase 3 trial (NCT02231879) has enrolled 19 patients. Primary results are expected in 2020.
The National Institutes of Health funded the work. Dr. McDermott reported a pending patent to reduce CXCR4 expression and/or function to enhance engraftment of hematopoietic stem cells.
SOURCE: McDermott DH et al. N Engl J Med. 2019;380:163-70.
Low-dose treatment with plerixafor, a CXC chemokine receptor 4 antagonist, was well tolerated and markedly improved severe presentations of warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) syndrome in three patients who could not receive granulocyte colony-stimulating factor therapy, investigators reported.
“Myelofibrosis, panleukopenia, anemia, and thrombocytopenia were ameliorated, the wart burden and frequency of infection declined, human papillomavirus–associated oropharyngeal squamous-cell carcinoma stabilized, and quality of life improved markedly,” David H. McDermott, MD, of the National Institute of Allergy and Infectious Diseases and his colleagues wrote in the New England Journal of Medicine.
WHIM syndrome is a primary immunodeficiency disorder characterized by panleukopenia and caused by autosomal dominant gain-of-function mutations in CXC chemokine receptor 4 (CXCR4). Granulocyte colony-stimulating factor (G-CSF) therapy improves neutropenia in these patients, but not other cytopenias.
Previously, the investigators treated three WHIM syndrome patients with plerixafor (Mozobil), which was well tolerated and led to sustained increases in circulating neutrophils, lymphocytes, and monocytes. The current report is of three patients with advanced WHIM syndrome who received open-label plerixafor because they were ineligible for a randomized trial of this drug.
After treatment initiation, infection frequency dropped by 85% in one patient and declined markedly in all three patients. Lymphocyte counts improved the most in two patients while neutrophils were most responsive in the third patient. Warts partially resolved in two patients, of which one patient also experienced partial resolution of head and neck squamous cell carcinoma. This patient later died of a multidrug-resistant Pseudomonas aeruginosa infection after undergoing a 9-hour surgery.
In the third patient, plerixafor therapy led to clearance of TSPyV and 17 human papillomavirus (HPV) infections, with consequent resolution of chronic, progressive, multifocal eczematoid and follicular lesions, the researchers reported. The study dose was relatively low – about 10% of the stem-cell mobilization dose – and did not cause bone pain or other treatment-emergent adverse events, despite the relatively long treatment course (19-52 months).
A separate, phase 3 trial (NCT02231879) has enrolled 19 patients. Primary results are expected in 2020.
The National Institutes of Health funded the work. Dr. McDermott reported a pending patent to reduce CXCR4 expression and/or function to enhance engraftment of hematopoietic stem cells.
SOURCE: McDermott DH et al. N Engl J Med. 2019;380:163-70.
Low-dose treatment with plerixafor, a CXC chemokine receptor 4 antagonist, was well tolerated and markedly improved severe presentations of warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) syndrome in three patients who could not receive granulocyte colony-stimulating factor therapy, investigators reported.
“Myelofibrosis, panleukopenia, anemia, and thrombocytopenia were ameliorated, the wart burden and frequency of infection declined, human papillomavirus–associated oropharyngeal squamous-cell carcinoma stabilized, and quality of life improved markedly,” David H. McDermott, MD, of the National Institute of Allergy and Infectious Diseases and his colleagues wrote in the New England Journal of Medicine.
WHIM syndrome is a primary immunodeficiency disorder characterized by panleukopenia and caused by autosomal dominant gain-of-function mutations in CXC chemokine receptor 4 (CXCR4). Granulocyte colony-stimulating factor (G-CSF) therapy improves neutropenia in these patients, but not other cytopenias.
Previously, the investigators treated three WHIM syndrome patients with plerixafor (Mozobil), which was well tolerated and led to sustained increases in circulating neutrophils, lymphocytes, and monocytes. The current report is of three patients with advanced WHIM syndrome who received open-label plerixafor because they were ineligible for a randomized trial of this drug.
After treatment initiation, infection frequency dropped by 85% in one patient and declined markedly in all three patients. Lymphocyte counts improved the most in two patients while neutrophils were most responsive in the third patient. Warts partially resolved in two patients, of which one patient also experienced partial resolution of head and neck squamous cell carcinoma. This patient later died of a multidrug-resistant Pseudomonas aeruginosa infection after undergoing a 9-hour surgery.
In the third patient, plerixafor therapy led to clearance of TSPyV and 17 human papillomavirus (HPV) infections, with consequent resolution of chronic, progressive, multifocal eczematoid and follicular lesions, the researchers reported. The study dose was relatively low – about 10% of the stem-cell mobilization dose – and did not cause bone pain or other treatment-emergent adverse events, despite the relatively long treatment course (19-52 months).
A separate, phase 3 trial (NCT02231879) has enrolled 19 patients. Primary results are expected in 2020.
The National Institutes of Health funded the work. Dr. McDermott reported a pending patent to reduce CXCR4 expression and/or function to enhance engraftment of hematopoietic stem cells.
SOURCE: McDermott DH et al. N Engl J Med. 2019;380:163-70.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Infection frequency dropped by 85% in one patient and showed marked declines in all three patients.
Study details: Open-label study of three patients who were ineligible to receive G-CSF therapy.
Disclosures: The National Institutes of Health funded the work. Dr. McDermott reported a pending patent on reducing CXCR4 expression and/or function to enhance engraftment of hematopoietic stem cells.
Source: McDermott DH et al. N Engl J Med. 2019;380:163-70.
Difelikefalin shows promise for hemodialysis-associated itch
PARIS – while achieving across-the-board clinically meaningful improvements in quality of life measures in patients with hemodialysis-associated pruritus in a phase 2 study, Frédérique Menzaghi, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
At present there is no approved medication in the United States or Europe for the often intense itching associated with chronic kidney disease. Off-label treatments have limited efficacy.
Dr. Menzaghi is senior vice president for research and development at Cara Therapeutics, which is developing difelikefalin.
More than half – 60% to 70% – of patients on hemodialysis for end-stage renal disease experience chronic pruritus, as do a smaller proportion of individuals with chronic kidney disease (CKD) not requiring dialysis. CKD-associated pruritus is a day-and-night itch that makes life miserable for affected patients. Not only must they endure the predictable complications of skin excoriation, including impetigo, ulcerations, papules, and prurigo nodularis, but they also experience sleep disruption, depressed mood, and a 10%-20% increased mortality risk compared with CKD patients without pruritus.
Difelikefalin is a potent and selective peripheral kappa opioid receptor agonist that doesn’t activate mu or delta opioid receptors. It’s a synthetic drug that mimics endogenous dynorphin. Its key attribute is that it doesn’t cross the blood/brain barrier, so it doesn’t pose a risk for adverse events caused by activation of central opioid receptors. Difelikefalin has two mechanisms of action in CKD-associated pruritus: an antipruritic effect due to inhibition of ion channels responsible for afferent peripheral nerve activity; and an anti-inflammatory effect mediated by activation of kappa opioid receptors expressed by immune system cells, according to Dr. Menzaghi.
She reported on 174 hemodialysis patients with moderate to severe CKD-associated pruritus who were randomized to a double-blind, phase 2, dose-ranging study featuring an intravenous bolus of difelikefalin at 0.5, 1.0, or 1.5 mcg/kg or placebo given immediately after each of the thrice-weekly hemodialysis sessions for 8 weeks.
An oral formulation of difelikefalin is also under investigation for treatment of CKD-associated pruritus. The IV version is being developed for hemodialysis patients because difelikefalin is renally excreted.
“We’re taking advantage of the fact that their kidneys aren’t working. The drug stays in the system until the next dialysis because it can’t be eliminated. It’s quite convenient for these patients,” she explained.
The primary endpoint in the phase 2 study was change from baseline through week 8 in the weekly average of a patient’s daily self-rated 0-10 worst itching intensity numeric rating scale (NRS) scores. All participants had to have a baseline NRS score of at least 4, considered the lower threshold for moderate itch. In fact, the mean baseline score was 6.7-7.1 in the four study arms.
The results
Sixty-four percent of patients on difelikefalin 0.5 mcg/kg – the most effective dose – experienced at least a 3-point reduction, compared with 29% of placebo-treated controls. And a 4-point or greater reduction in NRS from baseline was documented in 51% of patients on difelikefalin at 0.5 mcg/kg, compared with 24% of controls.
Although a 4-point difference is widely considered to represent clinically meaningful improvement in atopic dermatitis studies, Dr. Menzaghi said psychometric analyses of the difelikefalin trial data indicated that a 3-point or greater improvement in NRS score was associated with clinically meaningful change.
“Our data suggest that a 4-point change may not be generalizable to all conditions,” she said.
Hemodialysis patients with severe baseline itch typically improved to moderate itch on difelikefalin, while those with baseline moderate itch – that is, an NRS of 4-6 – dropped down to mild or no itch while on the drug.
“But that’s just a number. The question is, is that really clinically meaningful?” Dr. Menzaghi noted.
The answer, she continued, is yes. A high correlation was seen between reduction in itch intensity and improvement in quality of life. Scores on the 5-D Itch Scale and Skindex-10 improved two- to threefold more in the difelikefalin 0.5-mcg group than in controls. So did scores on the 12-item Medical Outcomes Study Sleep Scale assessing sleep restlessness, awakening during sleep, and trouble falling asleep.
“We think these results suggest that peripheral kappa opioid receptors play an integral role in the modulation of itch signals and represent a primary target for the development of antipruritic agents,” said Dr. Menzaghi.
Indeed, a phase 3 randomized trial of difelikefalin 0.5 mcg/kg versus placebo in 350 hemodialysis patients with CKD-associated itch is ongoing in the United States, Europe, Australia, and Korea. Also ongoing is a phase 2 U.S. study of oral difelikefalin in patients with CKD-associated pruritus, many of whom are not on hemodialysis. In January, the company announced that enrollment in a phase 3 U.S. study of difelikefalin injection (0.5 mcg/kg) in hemodialysis patients with moderate to severe CKD-associated pruritus had been completed. The trials are funded by Cara Therapeutics.
SOURCE: Menzaghi F. EADV Congress, Abstract FC0.4.7.
PARIS – while achieving across-the-board clinically meaningful improvements in quality of life measures in patients with hemodialysis-associated pruritus in a phase 2 study, Frédérique Menzaghi, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
At present there is no approved medication in the United States or Europe for the often intense itching associated with chronic kidney disease. Off-label treatments have limited efficacy.
Dr. Menzaghi is senior vice president for research and development at Cara Therapeutics, which is developing difelikefalin.
More than half – 60% to 70% – of patients on hemodialysis for end-stage renal disease experience chronic pruritus, as do a smaller proportion of individuals with chronic kidney disease (CKD) not requiring dialysis. CKD-associated pruritus is a day-and-night itch that makes life miserable for affected patients. Not only must they endure the predictable complications of skin excoriation, including impetigo, ulcerations, papules, and prurigo nodularis, but they also experience sleep disruption, depressed mood, and a 10%-20% increased mortality risk compared with CKD patients without pruritus.
Difelikefalin is a potent and selective peripheral kappa opioid receptor agonist that doesn’t activate mu or delta opioid receptors. It’s a synthetic drug that mimics endogenous dynorphin. Its key attribute is that it doesn’t cross the blood/brain barrier, so it doesn’t pose a risk for adverse events caused by activation of central opioid receptors. Difelikefalin has two mechanisms of action in CKD-associated pruritus: an antipruritic effect due to inhibition of ion channels responsible for afferent peripheral nerve activity; and an anti-inflammatory effect mediated by activation of kappa opioid receptors expressed by immune system cells, according to Dr. Menzaghi.
She reported on 174 hemodialysis patients with moderate to severe CKD-associated pruritus who were randomized to a double-blind, phase 2, dose-ranging study featuring an intravenous bolus of difelikefalin at 0.5, 1.0, or 1.5 mcg/kg or placebo given immediately after each of the thrice-weekly hemodialysis sessions for 8 weeks.
An oral formulation of difelikefalin is also under investigation for treatment of CKD-associated pruritus. The IV version is being developed for hemodialysis patients because difelikefalin is renally excreted.
“We’re taking advantage of the fact that their kidneys aren’t working. The drug stays in the system until the next dialysis because it can’t be eliminated. It’s quite convenient for these patients,” she explained.
The primary endpoint in the phase 2 study was change from baseline through week 8 in the weekly average of a patient’s daily self-rated 0-10 worst itching intensity numeric rating scale (NRS) scores. All participants had to have a baseline NRS score of at least 4, considered the lower threshold for moderate itch. In fact, the mean baseline score was 6.7-7.1 in the four study arms.
The results
Sixty-four percent of patients on difelikefalin 0.5 mcg/kg – the most effective dose – experienced at least a 3-point reduction, compared with 29% of placebo-treated controls. And a 4-point or greater reduction in NRS from baseline was documented in 51% of patients on difelikefalin at 0.5 mcg/kg, compared with 24% of controls.
Although a 4-point difference is widely considered to represent clinically meaningful improvement in atopic dermatitis studies, Dr. Menzaghi said psychometric analyses of the difelikefalin trial data indicated that a 3-point or greater improvement in NRS score was associated with clinically meaningful change.
“Our data suggest that a 4-point change may not be generalizable to all conditions,” she said.
Hemodialysis patients with severe baseline itch typically improved to moderate itch on difelikefalin, while those with baseline moderate itch – that is, an NRS of 4-6 – dropped down to mild or no itch while on the drug.
“But that’s just a number. The question is, is that really clinically meaningful?” Dr. Menzaghi noted.
The answer, she continued, is yes. A high correlation was seen between reduction in itch intensity and improvement in quality of life. Scores on the 5-D Itch Scale and Skindex-10 improved two- to threefold more in the difelikefalin 0.5-mcg group than in controls. So did scores on the 12-item Medical Outcomes Study Sleep Scale assessing sleep restlessness, awakening during sleep, and trouble falling asleep.
“We think these results suggest that peripheral kappa opioid receptors play an integral role in the modulation of itch signals and represent a primary target for the development of antipruritic agents,” said Dr. Menzaghi.
Indeed, a phase 3 randomized trial of difelikefalin 0.5 mcg/kg versus placebo in 350 hemodialysis patients with CKD-associated itch is ongoing in the United States, Europe, Australia, and Korea. Also ongoing is a phase 2 U.S. study of oral difelikefalin in patients with CKD-associated pruritus, many of whom are not on hemodialysis. In January, the company announced that enrollment in a phase 3 U.S. study of difelikefalin injection (0.5 mcg/kg) in hemodialysis patients with moderate to severe CKD-associated pruritus had been completed. The trials are funded by Cara Therapeutics.
SOURCE: Menzaghi F. EADV Congress, Abstract FC0.4.7.
PARIS – while achieving across-the-board clinically meaningful improvements in quality of life measures in patients with hemodialysis-associated pruritus in a phase 2 study, Frédérique Menzaghi, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
At present there is no approved medication in the United States or Europe for the often intense itching associated with chronic kidney disease. Off-label treatments have limited efficacy.
Dr. Menzaghi is senior vice president for research and development at Cara Therapeutics, which is developing difelikefalin.
More than half – 60% to 70% – of patients on hemodialysis for end-stage renal disease experience chronic pruritus, as do a smaller proportion of individuals with chronic kidney disease (CKD) not requiring dialysis. CKD-associated pruritus is a day-and-night itch that makes life miserable for affected patients. Not only must they endure the predictable complications of skin excoriation, including impetigo, ulcerations, papules, and prurigo nodularis, but they also experience sleep disruption, depressed mood, and a 10%-20% increased mortality risk compared with CKD patients without pruritus.
Difelikefalin is a potent and selective peripheral kappa opioid receptor agonist that doesn’t activate mu or delta opioid receptors. It’s a synthetic drug that mimics endogenous dynorphin. Its key attribute is that it doesn’t cross the blood/brain barrier, so it doesn’t pose a risk for adverse events caused by activation of central opioid receptors. Difelikefalin has two mechanisms of action in CKD-associated pruritus: an antipruritic effect due to inhibition of ion channels responsible for afferent peripheral nerve activity; and an anti-inflammatory effect mediated by activation of kappa opioid receptors expressed by immune system cells, according to Dr. Menzaghi.
She reported on 174 hemodialysis patients with moderate to severe CKD-associated pruritus who were randomized to a double-blind, phase 2, dose-ranging study featuring an intravenous bolus of difelikefalin at 0.5, 1.0, or 1.5 mcg/kg or placebo given immediately after each of the thrice-weekly hemodialysis sessions for 8 weeks.
An oral formulation of difelikefalin is also under investigation for treatment of CKD-associated pruritus. The IV version is being developed for hemodialysis patients because difelikefalin is renally excreted.
“We’re taking advantage of the fact that their kidneys aren’t working. The drug stays in the system until the next dialysis because it can’t be eliminated. It’s quite convenient for these patients,” she explained.
The primary endpoint in the phase 2 study was change from baseline through week 8 in the weekly average of a patient’s daily self-rated 0-10 worst itching intensity numeric rating scale (NRS) scores. All participants had to have a baseline NRS score of at least 4, considered the lower threshold for moderate itch. In fact, the mean baseline score was 6.7-7.1 in the four study arms.
The results
Sixty-four percent of patients on difelikefalin 0.5 mcg/kg – the most effective dose – experienced at least a 3-point reduction, compared with 29% of placebo-treated controls. And a 4-point or greater reduction in NRS from baseline was documented in 51% of patients on difelikefalin at 0.5 mcg/kg, compared with 24% of controls.
Although a 4-point difference is widely considered to represent clinically meaningful improvement in atopic dermatitis studies, Dr. Menzaghi said psychometric analyses of the difelikefalin trial data indicated that a 3-point or greater improvement in NRS score was associated with clinically meaningful change.
“Our data suggest that a 4-point change may not be generalizable to all conditions,” she said.
Hemodialysis patients with severe baseline itch typically improved to moderate itch on difelikefalin, while those with baseline moderate itch – that is, an NRS of 4-6 – dropped down to mild or no itch while on the drug.
“But that’s just a number. The question is, is that really clinically meaningful?” Dr. Menzaghi noted.
The answer, she continued, is yes. A high correlation was seen between reduction in itch intensity and improvement in quality of life. Scores on the 5-D Itch Scale and Skindex-10 improved two- to threefold more in the difelikefalin 0.5-mcg group than in controls. So did scores on the 12-item Medical Outcomes Study Sleep Scale assessing sleep restlessness, awakening during sleep, and trouble falling asleep.
“We think these results suggest that peripheral kappa opioid receptors play an integral role in the modulation of itch signals and represent a primary target for the development of antipruritic agents,” said Dr. Menzaghi.
Indeed, a phase 3 randomized trial of difelikefalin 0.5 mcg/kg versus placebo in 350 hemodialysis patients with CKD-associated itch is ongoing in the United States, Europe, Australia, and Korea. Also ongoing is a phase 2 U.S. study of oral difelikefalin in patients with CKD-associated pruritus, many of whom are not on hemodialysis. In January, the company announced that enrollment in a phase 3 U.S. study of difelikefalin injection (0.5 mcg/kg) in hemodialysis patients with moderate to severe CKD-associated pruritus had been completed. The trials are funded by Cara Therapeutics.
SOURCE: Menzaghi F. EADV Congress, Abstract FC0.4.7.
REPORTING FROM THE EADV CONGRESS
Key clinical point: Moderate to severe chronic itching associated with chronic kidney disease is a common and underrecognized problem with a huge quality of life impact.
Major finding: Sixty-four percent of hemodialysis patients on difelikefalin 0.5 mcg/kg experienced at least a 3-point reduction on a 0-10 worst daily itch numeric rating scale, compared with 29% of placebo-treated controls.
Study details: This phase 2, multicenter, 8-week, double-blind study comprised 174 patients with moderate to severe hemodialysis-related itching.
Disclosures: The study was sponsored by Cara Therapeutics and presented by a company officer.
Source: Menzaghi F. EADV Congress, Abstract FC0.4.7.
Tofacitinib tackles cutaneous sarcoidosis
Tofacitinib significantly improved skin lesions associated with cutaneous sarcoidosis, according to a case report published in the New England Journal of Medicine.
Treatment options for cutaneous sarcoidosis are limited, as are data on the effectiveness of alternatives to prednisone, which is often the first choice despite adverse effects, wrote William Damsky, MD, of Yale University in New Haven, Conn., and his colleagues.
Previous studies have suggested involvement of the JAK-STAT pathway in sarcoidosis; therefore, the researchers treated a patient who had refractory cutaneous sarcoidosis with oral tofacitinib. The treatment significantly improved the patient’s skin lesions both clinically and histologically.
The patient was a 48-year-old woman with a history of cutaneous and pulmonary sarcoidosis and treatment-resistant skin lesions. At the time of the case report, she had no pulmonary symptoms and no ophthalmologic issues, but presented with pink-brown indurated papules and plaques, and some alopecia on her scalp (N Engl J Med. 2018;379:2540-6).
The patient had not responded to other medications including glucocorticoids, minocycline, hydroxychloroquine, methotrexate, adalimumab, tacrolimus, and apremilast. With her consent, the patient received off-label tofacitinib at 5 mg twice daily. The lesions began to improve, but treatment was discontinued because of insurance issues. When treatment resumed, the patient’s Cutaneous Sarcoidosis Activity and Morphology Instrument (CSAMI) score, used to assess disease activity, was 85 on a scale of 0 to 165; this score dropped to 53 after 4 months of treatment.
In addition, two samples collected after 10 months of treatment showed histologic resolution of granulomas.
Although the findings must be replicated in other patients, the results suggest that “the dysregulation of JAK-STAT–dependent cytokines (e.g., interferon-gamma) is pathogenically involved in cutaneous sarcoidosis and, probably, in sarcoidosis in general,” the researchers said.
Dr. Damsky disclosed a financial relationship with Eli Lilly, and research funding from the Dermatology Foundation and the National Institutes of Health. The study was supported by the Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research, the National Institutes of Health, and the Dermatology Foundation.
SOURCE: Damsky W et al. N Engl J Med. 2018;379:2540-6.
Tofacitinib significantly improved skin lesions associated with cutaneous sarcoidosis, according to a case report published in the New England Journal of Medicine.
Treatment options for cutaneous sarcoidosis are limited, as are data on the effectiveness of alternatives to prednisone, which is often the first choice despite adverse effects, wrote William Damsky, MD, of Yale University in New Haven, Conn., and his colleagues.
Previous studies have suggested involvement of the JAK-STAT pathway in sarcoidosis; therefore, the researchers treated a patient who had refractory cutaneous sarcoidosis with oral tofacitinib. The treatment significantly improved the patient’s skin lesions both clinically and histologically.
The patient was a 48-year-old woman with a history of cutaneous and pulmonary sarcoidosis and treatment-resistant skin lesions. At the time of the case report, she had no pulmonary symptoms and no ophthalmologic issues, but presented with pink-brown indurated papules and plaques, and some alopecia on her scalp (N Engl J Med. 2018;379:2540-6).
The patient had not responded to other medications including glucocorticoids, minocycline, hydroxychloroquine, methotrexate, adalimumab, tacrolimus, and apremilast. With her consent, the patient received off-label tofacitinib at 5 mg twice daily. The lesions began to improve, but treatment was discontinued because of insurance issues. When treatment resumed, the patient’s Cutaneous Sarcoidosis Activity and Morphology Instrument (CSAMI) score, used to assess disease activity, was 85 on a scale of 0 to 165; this score dropped to 53 after 4 months of treatment.
In addition, two samples collected after 10 months of treatment showed histologic resolution of granulomas.
Although the findings must be replicated in other patients, the results suggest that “the dysregulation of JAK-STAT–dependent cytokines (e.g., interferon-gamma) is pathogenically involved in cutaneous sarcoidosis and, probably, in sarcoidosis in general,” the researchers said.
Dr. Damsky disclosed a financial relationship with Eli Lilly, and research funding from the Dermatology Foundation and the National Institutes of Health. The study was supported by the Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research, the National Institutes of Health, and the Dermatology Foundation.
SOURCE: Damsky W et al. N Engl J Med. 2018;379:2540-6.
Tofacitinib significantly improved skin lesions associated with cutaneous sarcoidosis, according to a case report published in the New England Journal of Medicine.
Treatment options for cutaneous sarcoidosis are limited, as are data on the effectiveness of alternatives to prednisone, which is often the first choice despite adverse effects, wrote William Damsky, MD, of Yale University in New Haven, Conn., and his colleagues.
Previous studies have suggested involvement of the JAK-STAT pathway in sarcoidosis; therefore, the researchers treated a patient who had refractory cutaneous sarcoidosis with oral tofacitinib. The treatment significantly improved the patient’s skin lesions both clinically and histologically.
The patient was a 48-year-old woman with a history of cutaneous and pulmonary sarcoidosis and treatment-resistant skin lesions. At the time of the case report, she had no pulmonary symptoms and no ophthalmologic issues, but presented with pink-brown indurated papules and plaques, and some alopecia on her scalp (N Engl J Med. 2018;379:2540-6).
The patient had not responded to other medications including glucocorticoids, minocycline, hydroxychloroquine, methotrexate, adalimumab, tacrolimus, and apremilast. With her consent, the patient received off-label tofacitinib at 5 mg twice daily. The lesions began to improve, but treatment was discontinued because of insurance issues. When treatment resumed, the patient’s Cutaneous Sarcoidosis Activity and Morphology Instrument (CSAMI) score, used to assess disease activity, was 85 on a scale of 0 to 165; this score dropped to 53 after 4 months of treatment.
In addition, two samples collected after 10 months of treatment showed histologic resolution of granulomas.
Although the findings must be replicated in other patients, the results suggest that “the dysregulation of JAK-STAT–dependent cytokines (e.g., interferon-gamma) is pathogenically involved in cutaneous sarcoidosis and, probably, in sarcoidosis in general,” the researchers said.
Dr. Damsky disclosed a financial relationship with Eli Lilly, and research funding from the Dermatology Foundation and the National Institutes of Health. The study was supported by the Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research, the National Institutes of Health, and the Dermatology Foundation.
SOURCE: Damsky W et al. N Engl J Med. 2018;379:2540-6.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A 48-year-old woman with sarcoidosis showed significant improvement in her skin on treatment with tofacitinib.
Major finding: The patient’s disease activity score on the CSAMI went from 85 to 53 after 4 months of therapy.
Study details: Case report of a 48-year-old woman with cutaneous and pulmonary sarcoidosis and treatment-resistant skin lesions.
Disclosures: Dr. Damsky disclosed a financial relationship with Eli Lilly, and research funding from the Dermatology Foundation and the National Institutes of Health. The study was supported by the Ranjini and Ajay Poddar Resource Fund for Dermatologic Diseases Research, the National Institutes of Health, and the Dermatology Foundation.
Source: Damsky W et al. N Engl J Med. 2018;379:2540-6.