User login
It’s time to rethink your approach to C diff infection
CASE 1
Beth O, a 63-year-old woman, presents to the emergency department (ED) with a 2-week history of diarrhea (6 very loose, watery stools per day) and lower abdominal pain. The patient denies any vomiting, sick contacts, or recent travel. Past medical history includes varicose veins. Her only active medication is loperamide, as needed, for the past 2 weeks. Ms. O also recently completed a 10-day course of clindamycin for an infected laceration on her finger.
Ms. O’s laboratory values are unremarkable, with a normal white blood cell (WBC) count and serum creatinine (SCr) level. Abdominal computed tomography (CT) reveals some abnormal bowel dilatation and a slight increase in colon wall thickness. There is a high suspicion for Clostridioides difficile (formerly Clostridium difficile) infection (CDI), and stool sent for polymerase chain reaction (PCR) testing comes back positive for C difficile toxin B. It is revealed to be a strain other than the BI/NAP1/027 epidemic strain (which has a higher mortality rate).
How should this patient be treated?
CASE 2
Sixty-eight-year-old Barbara Z presents to the ED from her skilled nursing facility with persistent diarrhea and abdominal cramping. She was diagnosed with CDI about 2 months ago and reports that her symptoms resolved within 4 to 5 days after starting a 14-day course of oral metronidazole.
Her past medical history is notable for multiple myeloma with bone metastasis, for which she is actively undergoing chemotherapy treatment. She also has chronic kidney disease (baseline SCr, 2.2 mg/dL), hypertension, and anemia of chronic disease. The patient’s medications include amlodipine and cholecalciferol. Her chemotherapy regimen consists of bortezomib, lenalidomide, and dexamethasone. CT of the abdomen shows diffuse colon wall thickening with surrounding inflammatory stranding—concerning for pancolitis. There is no evidence of toxic megacolon or ileus.
Ms. Z’s laboratory values are notable for a WBC count of 15,900 cells/mL and an SCr of 4.1 mg/dL. She is started on oral levofloxacin and metronidazole due to concern for an intra-abdominal infection. PCR testing is positive for C difficile, and an enzyme immunoassay (EIA) for C difficile toxin is positive.
What factors put Ms. Z at risk for C difficile, and how should she be treated?
Continue to: C difficile is one of the most...
C difficile is one of the most commonly reported pathogens in health care–associated infections and affects almost 1% of all hospitalized patients in the United States each year.1 From 2001 to 2010, the incidence of CDI doubled in patients discharged from hospitals,2 with an estimated cost of more than $5 billion annually.3 Furthermore, rates of community-associated CDI continue to increase and account for about 40% of cases.4
After colonization in the intestine, C difficile releases 2 toxins (TcdA and TcdB) that cause colitis.5 Patients may present with mild diarrhea that can progress to abdominal pain, cramping, fever, and leukocytosis. Fulminant CDI can lead to the formation of pseudomembranes in the colon, toxic megacolon, bowel perforation, shock, and death.2
Beginning in the early 2000s, hospitals reported increases in severe cases of CDI.6 A specific strain known as BI/NAP1/027 was identified and characterized by fluoroquinolone resistance, increased spore formation, and a higher mortality rate.6
Further complicating matters … Recurrent CDI occurs in up to 10% to 30% of patients,7 typically within 14 to 45 days of completion of antibiotic pharmacotherapy for CDI.8 Recurrence is characterized by new-onset diarrhea or abdominal symptoms after completion of treatment for CDI.5
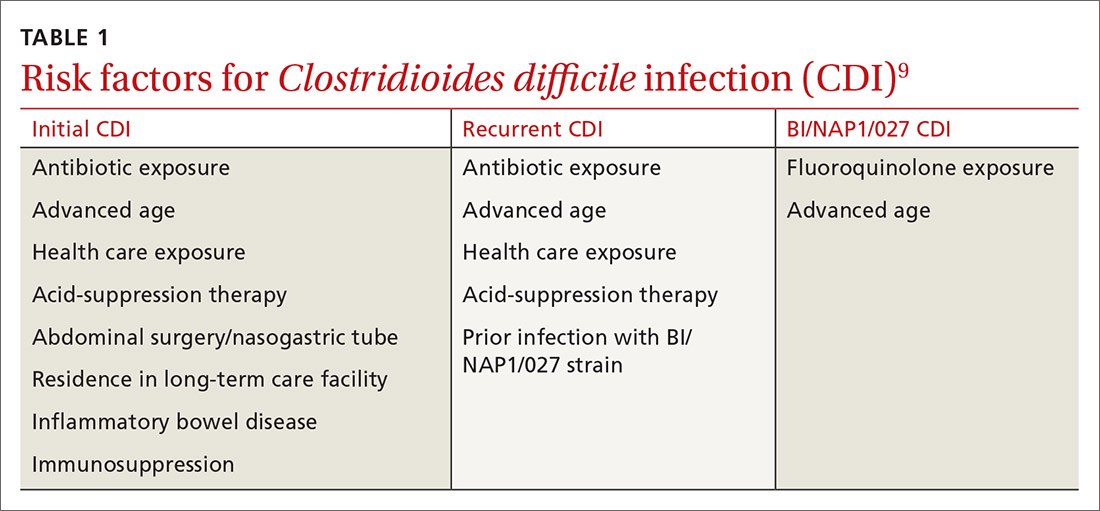
It typically begins with an antibiotic
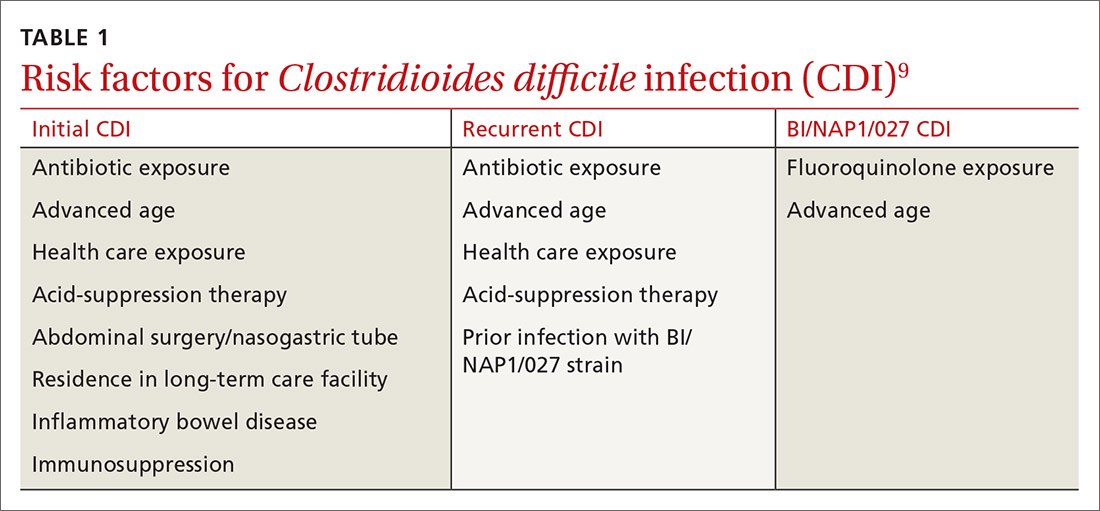
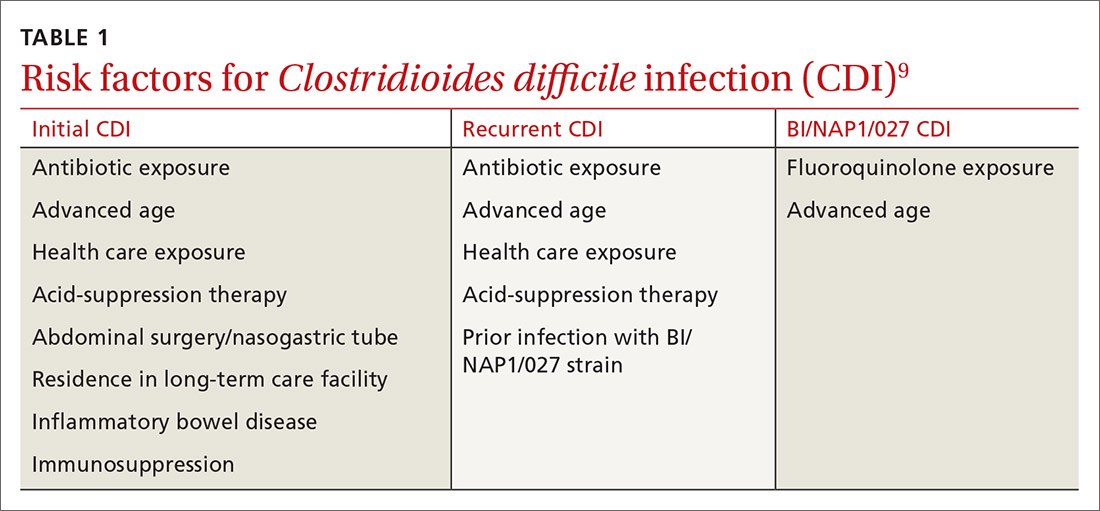
Risk factors for CDI are listed in TABLE 1.9 The most important modifiable risk factor for initial and recurrent CDI is recent use of antibiotics.10 Most antibiotics can disrupt normal intestinal flora, causing colonization of C difficile, but the strongest association seems to be with third- and fourth-generation cephalosporins, fluoroquinolones, carbapenems, and clindamycin.11 The risk for CDI occurs during antibiotic treatment, as well as up to 3 months after completion of antibiotic therapy.7 Exposure to multiple antibiotics and extended duration of antibacterial therapy can greatly increase the risk for CDI, so antimicrobial stewardship is key.11
Continue to: Continuing antibiotics while attempting...
Continuing antibiotics while attempting to treat CDI reduces the patient’s clinical response to CDI treatment, which can lead to recurrence.12 The Infectious Diseases Society of America (IDSA) guidelines include a strong recommendation to discontinue concurrent antibiotics as soon as possible in these scenarios.11
Acid-suppression therapy has also been associated with CDI. The mechanism is thought to be an interruption in the protection provided by stomach acid, and use over time may reduce the diversity of flora within the gut microbiome.13 The data demonstrating an association between acid-suppression therapy and CDI is conflicting, which may be a result of confounding factors such as the severity of CDI illness and diarrhea induced by use of proton pump inhibitors (PPIs).4 IDSA guidelines do not provide a recommendation regarding discontinuation of PPI therapy for the prevention of CDI, although inappropriate PPI therapy should always be discontinued.11
Advanced age is an important nonmodifiable risk factor for CDI. Older adults who live in long-term care facilities are at a higher risk for CDI, and these facilities have colonization rates as high as 50%.12
Community-associated risk. In an analysis of community-associated cases of CDI, 82% of patients reported some sort of health care exposure (ranging from physician office visit to surgery admission), 64% reported the receipt of antimicrobial therapy, and 31% reported the use of PPIs.14 Inflammatory bowel disease (IBD) may also put community dwellers at higher risk for CDI and its complications.15
CASES 1 & 2
Both CASE patients have risk factors for CDI. Ms. O (CASE 1) is likely at risk for CDI after completion of her recent course of clindamycin. Ms. Z (CASE 2) has several risk factors for recurrent CDI, including advanced age (≥ 65 years), residence in a long-term care facility, prior antibiotic exposure, and immunodeficiency because of chemotherapy/steroid use.
Continue to: Diagnosis
Diagnosis: Who and how to test
CDI should be both a clinical and laboratory-confirmed diagnosis. Patients should be tested for CDI if they have 3 or more episodes of unexplainable, new-onset unformed stools in 24 hours.11 Asymptomatic patients should not be tested to avoid unnecessary testing and treatment of those who are colonized but not infected.11 It is not recommended to routinely test patients who have taken laxatives within the previous 48 hours.11
There are several stool-based laboratory test options for the diagnosis of CDI (TABLE 211,12,16) but no definitive recommendation for all institutions.11 Many institutions have now implemented PCR testing for the diagnosis of CDI. However, while the benefits of this test include reduced need for repeat testing and possible identification of carriers, it’s estimated that reports of CDI increase more than 50% when an institution switches to PCR testing.1 Nonetheless, a one-step, highly sensitive test such as PCR may be used if strict criteria are implemented and followed.
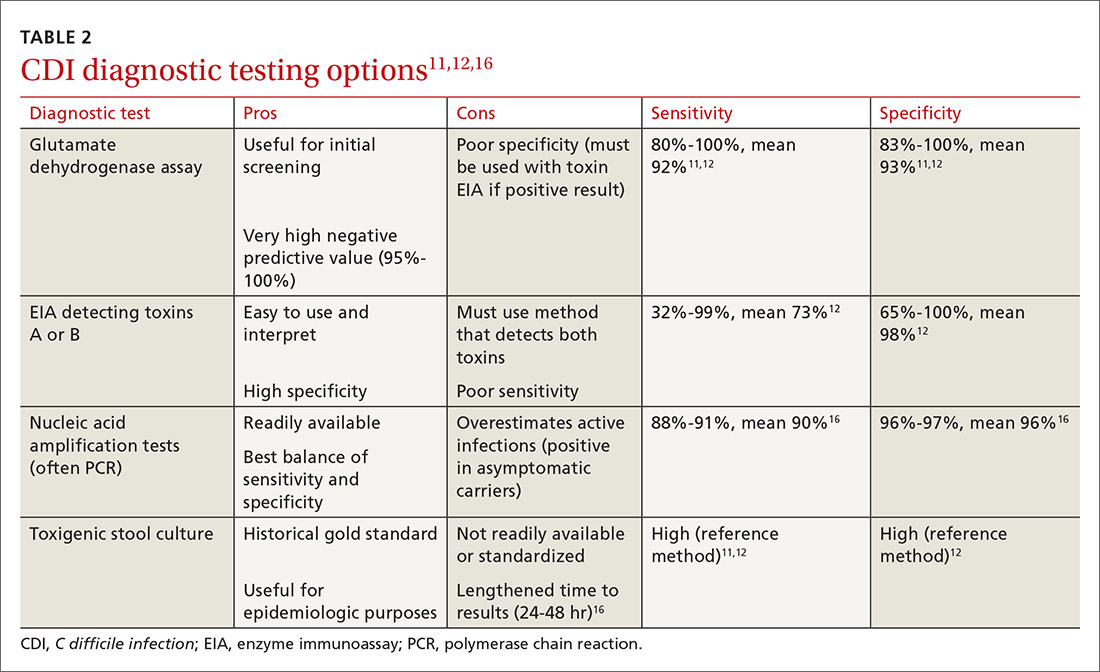
The increase in positive PCR tests has prompted evaluation of using another test in addition to or in place of PCR. Multistep testing options include a glutamate dehydrogenase assay (GDH) with a toxin EIA, GDH with a toxin EIA and final decision via PCR, or PCR with toxin EIA.11 Use of a multistep diagnostic algorithm may increase overall specificity up to 100%, which may improve determination of asymptomatic colonization vs active infection.16 (Patients who have negative toxin results with positive PCR likely have colonization but not infection and often do not require treatment.) IDSA guidelines recommend that the stool toxin test should be part of a multistep algorithm for diagnosis, rather than PCR alone, if strict criteria are not implemented for stool test submission.11
There is no need to perform a test of cure after a patient has been treated for CDI, and no repeat testing should be performed within 7 days of the previous test.11 After successful treatment, patients will continue to shed spores and test positively via PCR for weeks to months.11 When patients have a positive PCR test, there are several important infection control efforts that institutions should consider; see “IDSA weighs in on measures to combat C difficile.”
SIDEBAR
IDSA weighs in on measures to combat C difficile
The spores produced by Clostridioides difficile can survive for 5 months or longer on dry surfaces because of resistance to heat, acid, antibiotics, and many cleaning products.38 Unfortunately, spores transmitted from health care workers and the environment are the most likely cause of infection spreading in health care institutions. To prevent transmission of C difficile infection (CDI) throughout institutions, appropriate infection control measures are necessary.
Clinical practice guidelines from the Infectious Diseases Society of America (IDSA) recommend that patients with CDI be isolated to a private room with a dedicated toilet. Health care staff should wear gloves and gowns when entering the room of, or taking care of, a patient with CDI. For patients who are suspected of having CDI, contact precautions should be implemented while awaiting test results. When the diagnosis is confirmed, contact precautions should remain in place for at least 48 hours after resolution of diarrhea but may be continued until discharge.11
Practicing good hand hygiene is essential, especially in institutions with high rates of CDI or if fecal contamination is likely.11 Hand hygiene with soap and water is preferred, due to evidence of a higher spore removal rate, but alcohol-based alternatives may be used if necessary.11 In institutions with high rates of CDI, terminal (post-discharge) cleaning of rooms with a sporicidal agent should be considered.11
Asymptomatic carriers are also a concern for transmission of CDI in institutional settings. Screening and isolating patients who are carriers may prevent transmission, and some institutions have implemented this process to reduce the risk for CDI that originates in a health care facility.39 The IDSA guidelines do not make a recommendation regarding screening or isolation of asymptomatic carriers, so the decision is institution specific.11 These guidelines also recommend that patients presenting with similar infectious organisms be housed in the same room, if needed, to avoid cross-contamination to others or additional surfaces.11
For pediatric patients, testing recommendations vary by age. Testing is not generally recommended for neonates or infants ≤ 2 years of age with diarrhea because of the prevalence of colonization with C difficile.11 For children older than 2 years, testing for CDI is only recommended in the setting of prolonged or worsening diarrhea and if the patient has risk factors such as IBD, immunocompromised state, health care exposure, or recent antibiotic use.11 In addition, testing in this population should only be considered once other infectious and noninfectious causes of diarrhea have been excluded.11
Continue to: First-line treatment? Drug of choice has changed
First-line treatment? Drug of choice has changed
In 2018, the IDSA published new treatment guidelines that provide important updates from the 2010 guidelines.11 Chief among these was the elimination of metronidazole as a first-line therapy. Vancomycin or fidaxomicin are now recommended as first-line treatment options because of superior eradication of C difficile when compared with metronidazole.11 In the opinion of the authors, vancomycin should be considered the drug of choice because of cost. (See “The case for vancomycin.”)
SIDEBAR
The case for vancomycin
The majority of studies conducted prior to publication of the 2010 Infectious Diseases Society of America guidelines described numerically worse eradication rates of Clostridioides difficile infection (CDI) with metronidazole compared with vancomycin for all severities of infection, but statistical significance was not achieved. These studies also showed a nonsignificant increase in CDI recurrence with metronidazole.17,40,41
A 2005 systematic review demonstrated increased treatment failure rates with metronidazole.42 The rates of metronidazole discontinuation and transition to alternative options more than doubled in 2003-2004, to 25.7% of patients compared with 9.6% in earlier years.42 Metronidazole efficacy was further questioned in a prospective observational study conducted in 2005, in which only 50% of patients were cured after an initial course of treatment, while 28% had recurrence within 90 days.43
Vancomycin was found to be the superior treatment option to metronidazole and tolevamer in a 2014 randomized controlled trial.18 This study also demonstrated that vancomycin was the superior therapy when comparing treatment-naïve vs experienced patients and severity of CDI.18 A 2017 retrospective cohort study demonstrated decreased 30-day all-cause mortality for patients taking vancomycin vs metronidazole (adjusted relative risk = 0.86; 95% confidence interval, 0.74-0.98), although it should be noted that this difference was driven by those with severe CDI, and there was no statistically significant difference in mortality for patients with mild-to-moderate CDI.44
The results of these studies led to the recommendation of vancomycin over metronidazole as first-line pharmacotherapy for CDI in practice, despite the historical perspective that overutilization of oral vancomycin could potentially increase rates of vancomycinresistant Enterococcus.11
Metronidazole should only be used in the treatment of CDI as a lastresort medication because of cost or insurance coverage. Although the price of oral vancomycin is higher, favorable patient outcomes are substantially greater, and recent analyses have shown that vancomycin is actually more cost-effective than metronidazole as a result.24 Adverse effects for metronidazole include neurotoxicity, gastrointestinal discomfort, and disulfiram-like reaction.
Vancomycin does not harbor as many adverse effects because of extremely low systemic absorption when taken orally, but patients may experience gastrointestinal discomfort.45 While systemic exposure with oral administration of vancomycin is very low (< 1%), there have been case reports of nephrotoxicity and “red man syndrome” that are more typically seen with intravenous vancomycin.44
Given the low rate of systemic exposure, routine monitoring of renal function and serum drug levels is not usually necessary during oral vancomycin therapy. However, it may be appropriate to monitor renal function and serum levels of vancomycin in patients who have renal failure, have altered intestinal integrity, are age ≥ 65 years, or are receiving high doses of vancomycin.46
10-day vs 14-day treatment of CDI. Most studies for the treatment of CDI have used a 10-day regimen rather than increasing the duration to a 14-day regimen, and nearly all studies conducted have displayed high rates of symptom resolution at the end of 10 days of treatment.17,18 Thus, treatment duration beyond 10 days should only be considered for patients who continue to have symptoms or complications with CDI on Day 10 of treatment.
First recurrence. Metronidazole is no longer the recommended treatment for first recurrence of CDI treated initially with metronidazole; instead, a 10-day course of vancomycin should be used.11 For recurrent cases in patients initially treated with vancomycin, a tapered and pulsed regimen of vancomycin is recommended11:
- vancomycin PO 125 mg four times daily for 10 to 14 days followed by
- vancomycin PO 125 mg twice daily for 7 days, then
- vancomycin PO 125 mg once daily for 7 days, then
- vancomycin PO 125 mg every 2 to 3 days for 2 to 8 weeks.
Pediatric patients. The IDSA guidelines recommend use of metronidazole or vancomycin to treat an initial case or first recurrence of mild-to-moderate CDI in this population.11 Due to a lack of quality evidence, the drug of choice for initial treatment is inconclusive, so patient-specific factors and cost should be considered when choosing an agent.11 If not cost prohibitive, vancomycin should be the drug of choice for most cases of pediatric CDI, and for severe cases or multiple recurrences of CDI, vancomycin is clearly the drug of choice.
Recommended agents: A closer look
Oral vancomycin products. Vancocin, a capsule, and Firvanq, an oral solution, are 2 vancomycin products currently on the market for CDI. Although the capsules are a readily available treatment option, the cost of the full course of treatment can be a barrier for patients without insurance, or with high copays or deductibles (brand name, $4000; generic, $1252).19
Continue to: Historically, in an effort to keep costs down...
Historically, in an effort to keep costs down, an oral solution was often inexpensively compounded at hospitals or pharmacies.20
Fidaxomicin, an oral macrocyclic antibiotic with minimal systemic absorption, was first approved by the US Food and Drug Administration (FDA) for CDI in 2011.21 The IDSA guidelines recommend fidaxomicin for initial, and recurrent, cases of CDI as an alternative to vancomycin.11 This recommendation is based on 2 randomized double-blind trials comparing fidaxomicin to standard-dose oral vancomycin for initial or recurrent CDI.21,22
Pooled data from these 2 similar studies found that fidaxomicin was noninferior (10% noninferiority margin) to vancomycin for the primary outcome of clinical cure.23 Fidaxomicin was shown to be superior to vancomycin regarding rate of CDI recurrence (relative risk [RR] = 0.61; 95% confidence interval [CI], 0.43-0.87). These results were similar regardless of whether the CDI was an initial or recurrent case.23
Given the lack of systemic absorption, fidaxomicin is generally very well tolerated. The largest downside to fidaxomicin is its cost, which can be nearly $5000 for a standard 10-day course (vs as little as $165 for oral vancomycin).19 As a result, oral vancomycin solution is likely the most cost-effective therapy for initial cases of CDI.24 In patients with poor medication adherence, fidaxomicin offers the advantage of less-frequent dosing (twice daily vs 4 times daily with vancomycin).
For cases of recurrent CDI, when treatment failure occurred with vancomycin, fidaxomicin should be considered as an efficacious alternative. If fidaxomicin is used, it is advisable to verify coverage with the patient’s insurance plan, since prior authorization is frequently required.
Continue to: When meds fail, consider a fecal microbiota transplant
When meds fail, consider a fecal microbiota transplant
Another important change in the IDSA guidelines for CDI management is the strong recommendation for fecal microbiota transplantation (FMT) in patients with multiple recurrences of CDI for whom appropriate antibiotic treatment courses have failed.11,25 The goal of FMT is to “normalize” an abnormal gut microbiome by transplanting donor stool into a recipient.26
FMT has been shown to be highly effective in 5 randomized clinical trials conducted since 2013, with CDI cure rates between 85% and 94%.11 This rate of cure is particularly impressive given that the studies only included patients with refractory CDI.
Patients with recurrent CDI who may be candidates for FMT should be referred to a center or specialist with experience in FMT. These transplants can be expensive because of the screening process involved in obtaining donor samples. (Historically, a single FMT has cost $3000-$5000, and it is seldom covered by insurance.27) The emergence of universal stool banks offers a streamlined solution to this process.26
Fresh or frozen stool is considered equally effective in treating refractory CDI.26 Oral capsule and freeze-dried stool formulations have been studied, but their use is considered investigational at this time.26
Delivery via colonoscopy to the right colon is the preferred route of infusion; however, delivery via enema or nasogastric, nasojejunal, or nasoduodenal infusion can be considered as well.26
Continue to: In preparing for stool transplantation...
In preparing for stool transplantation, patients should be treated with standard doses of oral vancomycin or fidaxomicin for 3 days before the procedure to suppress intestinal C difficile, and the last dose of antibiotics should be given 12 to 48 hours before the procedure.26 Bowel lavage with polyethylene glycol is recommended, regardless of whether stool is delivered via colonoscopy or upper GI route.
Short-term adverse events associated with FMT appear to be minimal; data is lacking for long-term safety outcomes.28 While only recommended currently for cases of recurrent CDI, there is promising data emerging for use of FMT for severe cases, even without recurrence.29
The role of probiotics remains unclear
Probiotics have been explored in numerous trials to determine if they are effective in preventing CDI in patients who have been prescribed antibiotics.11 While no randomized trials have conclusively shown benefit, several meta-analyses have shown that the use of probiotics may result in a 60% to 65% relative risk reduction in CDI incidence.30,31
One proviso to these meta-analyses is that the incorporated studies have typically included patients at very high risk for CDI, and subanalyses have only found a reduction in CDI incidence when patients are at a very high baseline risk. In addition, there are many differences in probiotic types, formulations, treatment durations, and follow-up. As a result, the IDSA guidelines state that there is “insufficient data at this time” to recommend routine administration of probiotics for either primary or secondary CDI prophylaxis.11
Due to insufficient high-quality data, the IDSA guidelines do not provide a recommendation regarding use as an adjunct treatment option for acute CDI.11 Probiotics should not be routinely used to prevent CDI; however, they may provide benefit if reserved for patients at the highest risk for CDI (eg, history of CDI, prolonged use of broad-spectrum antibiotics, high local incidence).
Continue to: What about surgical intervention?
What about surgical intervention?
In severe cases of CDI, surgery may be necessary and can reduce mortality.32 The surgical procedure with the strongest recommendation in the IDSA guidelines is the subtotal colectomy, though the diverting loop ileostomy is an alternative option.11 Patients who may benefit from surgery include those with a WBC count ≥ 25,000; lactate > 5 mmol/L11; altered mental status; megacolon; perforation of the colon; acute abdomen on physical examination; or septic shock due to CDI.33 Although surgery can be beneficial, the mortality rate remains high for those with CDI who undergo colectomy.33
Reserve bezlotoxumab for prevention of recurrence
Bezlotoxumab, a human monoclonal immunoglobulin GI/kappa antibody, was approved by the FDA in 2016 for the prevention of recurrent CDI. Its mechanism of action is to bind and neutralize C difficile toxin B. It was approved as a single infusion for adults who are receiving active antibiotic therapy for CDI and are considered to be at high risk for recurrence.34
This approval was based on 2 trials of more than 2500 patients, in which participants received bezlotoxumab or placebo while receiving treatment for primary or recurrent CDI. The primary outcome of these studies was recurrent infection within 12 weeks after infusion, which was significantly lower for bezlotoxumab in both studies: 17% vs 28% (P < 0.001) in one trial and 16% vs 26% (P < 0.001) in the other trial.35
Bezlotoxumab should only be used as an adjunct to prevent recurrence.32 There is no recommendation for or against bezlotoxumab in the IDSA guidelines because of the recent date of the drug’s approval. Its frequency of use will likely depend on the number of patients who meet criteria as high risk for recurrence and its estimated cost of $4560 per dose.34,36
CASES
CASE 1: In light of Ms. O’s recent completion of a course of clindamycin and unremarkable lab work, she should be treated for mild-to-moderate CDI. She has no comorbid conditions to warrant fidaxomicin, and thus vancomycin (capsules or oral solution) would be the best treatment option. Ms. O is started on vancomycin PO 125 mg qid for 10 days. She is also advised to discontinue loperamide as soon as possible, based on poor outcomes data seen with the use of antimotility agents in CDI.37
Continue to: CASE 2
CASE 2: Ms. Z has several risk factors for recurrent CDI and has an elevated WBC count and SCr level (WBC ≥ 15,000 and SCr > 1.5 mg/dL). Thus, she is classified as having severe, recurrent CDI. Oral levofloxacin and metronidazole should be discontinued, because they increase the risk for treatment failure and development of more virulent CDI strains, such as BI/NAP1/027. Since Ms. Z used metronidazole for treatment of her initial CDI, vancomycin or fidaxomicin should be used at this time. Either vancomycin PO 125 mg qid for 10 days or fidaxomicin 200 mg bid for 10 days would be an appropriate regimen; however, because of cost and unknown insurance coverage, vancomycin is the most appropriate regimen.
CORRESPONDENCE
Jeremy Vandiver, PharmD, BCPS, University of Wyoming School of Pharmacy, Saint Joseph Family Medicine Residency, 1000 E. University Avenue, Dept 3375, Laramie, WY 82071; [email protected]
1. Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med. 2015;175:1792-1801.
2. Reveles KR, Lee GC, Boyd NK, et al. The rise in Clostridium difficile infection incidence among hospitalized adults in the United States: 2001-2010. Am J Infect Control. 2014;42:1028-1032.
3. Dubberke ER, Olsen MA. Burden of Clostridium difficile on the healthcare system. Clin Infect Dis. 2012;55(suppl 2):S88-S92.
4. Tariq R, Singh S, Gupta A, et al. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:784-791.
5. Kachrimanidou M, Malisiovas N. Clostridium difficile infection: a comprehensive review. Crit Rev Microbiol. 2011;37:178-187.
6. O’Connor JR, Johnson S, Gerding DN. Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology. 2009;136:1913-1924.
7. Kelly CP. A 76-year-old man with recurrent Clostridium difficile-associated diarrhea: review of C difficile infection. JAMA. 2009;301:954-962.
8. Cornely OA, Miller MA, Louie TJ, et al. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):S154-S161.
9. Napolitano LM, Edmiston CE Jr. Clostridium difficile disease: diagnosis, pathogenesis, and treatment update. Surgery 2017;162:325-348.
10. Deshpande A, Pasupuleti V, Thota P, et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452-460.
11. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66:e1-e48.
12. Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478-498; quiz 499.
13. Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42.
14. Chitnis AS, Holzbauer SM, Belflower RM, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013;173:1359-1367.
15. Negrón ME, Rezaie A, Barkema HW, et al. Ulcerative colitis patients with Clostridium difficile are at increased risk of death, colectomy, and postoperative complications: a population-based inception cohort study. Am J Gastroenterol. 2016;111:691-704.
16. Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313:398-408.
17. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
18. Johnson S, Louie TJ, Gerding DN, et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59:345-354.
19. Vancomycin: product details. Redbook Online. www.micromedexsolutions.com. Published 2018. Accessed June 13, 2020.
20. Mergenhagen KA, Wojciechowski AL, Paladino JA. A review of the economics of treating Clostridium difficile infection. Pharmacoeconomics. 2014;32:639-650.
21. Louie TJ, Miller MA, Mullane KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422-431.
22. Cornely OA, Crook DW, Esposito R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12:281-289.
23. Crook DW, Walker AS, Kean Y, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection: meta-analysis of pivotal randomized controlled trials. Clin Infect Dis. 2012;55 suppl 2:S93-103.
24. Ford DC, Schroeder MC, Ince D, et al. Cost-effectiveness analysis of initial treatment strategies for mild-to-moderate Clostridium difficile infection in hospitalized patients. Am J Health Syst Pharm. 2018;75:1110-1121.
25. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
26. Panchal P, Budree S, Scheeler A, et al. Scaling safe access to fecal microbiota transplantation: past, present, and future. Curr Gastroenterol Rep. 2018;20:14.
27. Arbel LT, Hsu E, McNally K. Cost-effectiveness of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection: a literature review. Cureus. 2017;9:e1599.
28. Cammarota G, Ianiro G, Tilg H, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569-580.
29. Hocquart M, Lagier JC, Cassir N, et al. Early fecal microbiota transplantation improves survival in severe Clostridium difficile infections. Clin Infect Dis. 2018;66:645-650.
30. Goldenberg JZ, Yap C, Lytvyn L, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2017;12:CD006095.
31. Johnston BC, Lytvyn L, Lo CK, et al. Microbial preparations (probiotics) for the prevention of Clostridium difficile infection in adults and children: an individual patient data meta-analysis of 6,851 participants. Infect Control Hosp Epidemiol. 2018:1-11.
32. Stewart DB, Hollenbeak CS, Wilson MZ. Is colectomy for fulminant Clostridium difficile colitis life saving? A systematic review. Colorectal Dis. 2013;15:798-804.
33. Julien M, Wild JL, Blansfield J, et al. Severe complicated Clostridium difficile infection: can the UPMC proposed scoring system predict the need for surgery? J Trauma Acute Care Surg. 2016;81:221-228.
34. Merck & Co, Inc. Sharp M. ZinplavaTM (bezlotoxumab [package insert] US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2016/761046s000lbl.pdf. Revised October 2016. Accessed May 29, 2020.
35. Wilcox MH, Gerding DN, Poxton IR, et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med. 2017;376:305-317.
36. Chahine EB, Cho JC, Worley MV. Bezlotoxumab for the Prevention of Clostridium difficile recurrence. Consult Pharm. 2018;33:89-97.
37. Koo HL, Koo DC, Musher DM, et al. Antimotility agents for the treatment of Clostridium difficile diarrhea and colitis. Clin Infect Dis. 2009;48:598-605.
38. Rupnik M, Wilcox MH, Gerding DN. Clostridium difficile infection: new developments in epidemiology and pathogenesis. Nat Rev Microbiol. 2009;7:526-536.
39. Longtin Y, Paquet-Bolduc B, Gilca R, et al. Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med. 2016;176:796-804.
40. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet. 1983;2:1043-1046.
41. Wenisch C, Parschalk B, Hasenhündl M, et al. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis. 1996;22:813-818.
42. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
43. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
44. Stevens VW, Nelson RE, Schwab-Daugherty EM, et al. Comparative effectiveness of vancomycin and metronidazole for the prevention of recurrence and death in patients with Clostridium difficile infection. JAMA Intern Med. 2017;177:546-553.
45. CutisPharma. FirvanqTM (vancomycin hydrochloride) for oral solution [package insert]. US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2018/208910s000lbl.pdf. Revised January 2018. Accessed May 29, 2020.
46.
CASE 1
Beth O, a 63-year-old woman, presents to the emergency department (ED) with a 2-week history of diarrhea (6 very loose, watery stools per day) and lower abdominal pain. The patient denies any vomiting, sick contacts, or recent travel. Past medical history includes varicose veins. Her only active medication is loperamide, as needed, for the past 2 weeks. Ms. O also recently completed a 10-day course of clindamycin for an infected laceration on her finger.
Ms. O’s laboratory values are unremarkable, with a normal white blood cell (WBC) count and serum creatinine (SCr) level. Abdominal computed tomography (CT) reveals some abnormal bowel dilatation and a slight increase in colon wall thickness. There is a high suspicion for Clostridioides difficile (formerly Clostridium difficile) infection (CDI), and stool sent for polymerase chain reaction (PCR) testing comes back positive for C difficile toxin B. It is revealed to be a strain other than the BI/NAP1/027 epidemic strain (which has a higher mortality rate).
How should this patient be treated?
CASE 2
Sixty-eight-year-old Barbara Z presents to the ED from her skilled nursing facility with persistent diarrhea and abdominal cramping. She was diagnosed with CDI about 2 months ago and reports that her symptoms resolved within 4 to 5 days after starting a 14-day course of oral metronidazole.
Her past medical history is notable for multiple myeloma with bone metastasis, for which she is actively undergoing chemotherapy treatment. She also has chronic kidney disease (baseline SCr, 2.2 mg/dL), hypertension, and anemia of chronic disease. The patient’s medications include amlodipine and cholecalciferol. Her chemotherapy regimen consists of bortezomib, lenalidomide, and dexamethasone. CT of the abdomen shows diffuse colon wall thickening with surrounding inflammatory stranding—concerning for pancolitis. There is no evidence of toxic megacolon or ileus.
Ms. Z’s laboratory values are notable for a WBC count of 15,900 cells/mL and an SCr of 4.1 mg/dL. She is started on oral levofloxacin and metronidazole due to concern for an intra-abdominal infection. PCR testing is positive for C difficile, and an enzyme immunoassay (EIA) for C difficile toxin is positive.
What factors put Ms. Z at risk for C difficile, and how should she be treated?
Continue to: C difficile is one of the most...
C difficile is one of the most commonly reported pathogens in health care–associated infections and affects almost 1% of all hospitalized patients in the United States each year.1 From 2001 to 2010, the incidence of CDI doubled in patients discharged from hospitals,2 with an estimated cost of more than $5 billion annually.3 Furthermore, rates of community-associated CDI continue to increase and account for about 40% of cases.4
After colonization in the intestine, C difficile releases 2 toxins (TcdA and TcdB) that cause colitis.5 Patients may present with mild diarrhea that can progress to abdominal pain, cramping, fever, and leukocytosis. Fulminant CDI can lead to the formation of pseudomembranes in the colon, toxic megacolon, bowel perforation, shock, and death.2
Beginning in the early 2000s, hospitals reported increases in severe cases of CDI.6 A specific strain known as BI/NAP1/027 was identified and characterized by fluoroquinolone resistance, increased spore formation, and a higher mortality rate.6
Further complicating matters … Recurrent CDI occurs in up to 10% to 30% of patients,7 typically within 14 to 45 days of completion of antibiotic pharmacotherapy for CDI.8 Recurrence is characterized by new-onset diarrhea or abdominal symptoms after completion of treatment for CDI.5
It typically begins with an antibiotic
Risk factors for CDI are listed in TABLE 1.9 The most important modifiable risk factor for initial and recurrent CDI is recent use of antibiotics.10 Most antibiotics can disrupt normal intestinal flora, causing colonization of C difficile, but the strongest association seems to be with third- and fourth-generation cephalosporins, fluoroquinolones, carbapenems, and clindamycin.11 The risk for CDI occurs during antibiotic treatment, as well as up to 3 months after completion of antibiotic therapy.7 Exposure to multiple antibiotics and extended duration of antibacterial therapy can greatly increase the risk for CDI, so antimicrobial stewardship is key.11
Continue to: Continuing antibiotics while attempting...
Continuing antibiotics while attempting to treat CDI reduces the patient’s clinical response to CDI treatment, which can lead to recurrence.12 The Infectious Diseases Society of America (IDSA) guidelines include a strong recommendation to discontinue concurrent antibiotics as soon as possible in these scenarios.11
Acid-suppression therapy has also been associated with CDI. The mechanism is thought to be an interruption in the protection provided by stomach acid, and use over time may reduce the diversity of flora within the gut microbiome.13 The data demonstrating an association between acid-suppression therapy and CDI is conflicting, which may be a result of confounding factors such as the severity of CDI illness and diarrhea induced by use of proton pump inhibitors (PPIs).4 IDSA guidelines do not provide a recommendation regarding discontinuation of PPI therapy for the prevention of CDI, although inappropriate PPI therapy should always be discontinued.11
Advanced age is an important nonmodifiable risk factor for CDI. Older adults who live in long-term care facilities are at a higher risk for CDI, and these facilities have colonization rates as high as 50%.12
Community-associated risk. In an analysis of community-associated cases of CDI, 82% of patients reported some sort of health care exposure (ranging from physician office visit to surgery admission), 64% reported the receipt of antimicrobial therapy, and 31% reported the use of PPIs.14 Inflammatory bowel disease (IBD) may also put community dwellers at higher risk for CDI and its complications.15
CASES 1 & 2
Both CASE patients have risk factors for CDI. Ms. O (CASE 1) is likely at risk for CDI after completion of her recent course of clindamycin. Ms. Z (CASE 2) has several risk factors for recurrent CDI, including advanced age (≥ 65 years), residence in a long-term care facility, prior antibiotic exposure, and immunodeficiency because of chemotherapy/steroid use.
Continue to: Diagnosis
Diagnosis: Who and how to test
CDI should be both a clinical and laboratory-confirmed diagnosis. Patients should be tested for CDI if they have 3 or more episodes of unexplainable, new-onset unformed stools in 24 hours.11 Asymptomatic patients should not be tested to avoid unnecessary testing and treatment of those who are colonized but not infected.11 It is not recommended to routinely test patients who have taken laxatives within the previous 48 hours.11
There are several stool-based laboratory test options for the diagnosis of CDI (TABLE 211,12,16) but no definitive recommendation for all institutions.11 Many institutions have now implemented PCR testing for the diagnosis of CDI. However, while the benefits of this test include reduced need for repeat testing and possible identification of carriers, it’s estimated that reports of CDI increase more than 50% when an institution switches to PCR testing.1 Nonetheless, a one-step, highly sensitive test such as PCR may be used if strict criteria are implemented and followed.
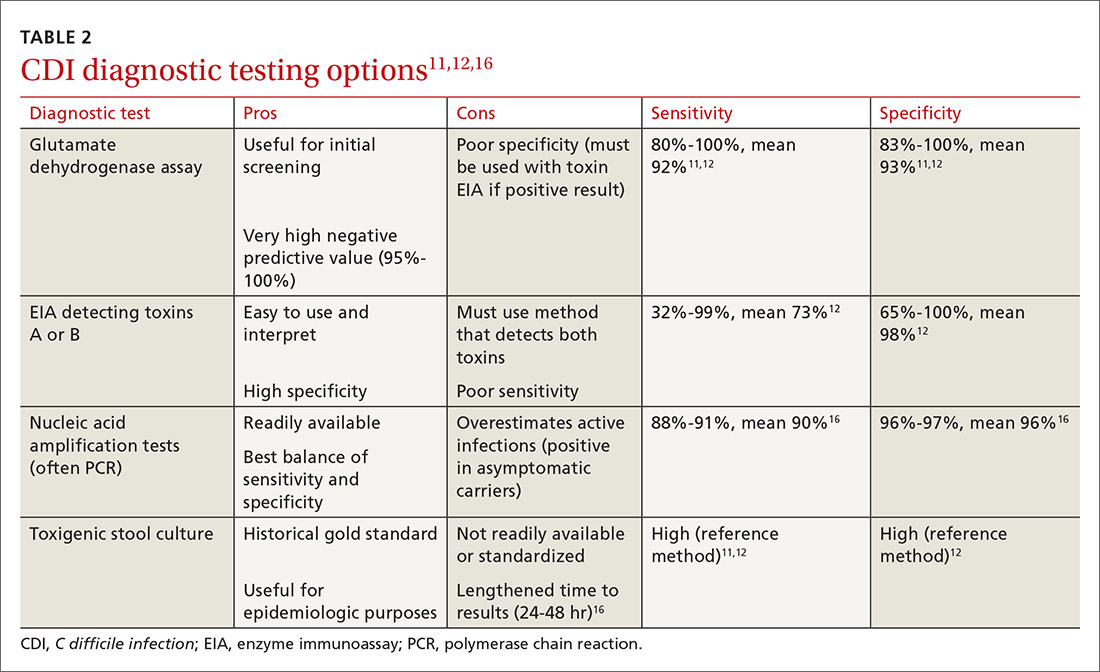
The increase in positive PCR tests has prompted evaluation of using another test in addition to or in place of PCR. Multistep testing options include a glutamate dehydrogenase assay (GDH) with a toxin EIA, GDH with a toxin EIA and final decision via PCR, or PCR with toxin EIA.11 Use of a multistep diagnostic algorithm may increase overall specificity up to 100%, which may improve determination of asymptomatic colonization vs active infection.16 (Patients who have negative toxin results with positive PCR likely have colonization but not infection and often do not require treatment.) IDSA guidelines recommend that the stool toxin test should be part of a multistep algorithm for diagnosis, rather than PCR alone, if strict criteria are not implemented for stool test submission.11
There is no need to perform a test of cure after a patient has been treated for CDI, and no repeat testing should be performed within 7 days of the previous test.11 After successful treatment, patients will continue to shed spores and test positively via PCR for weeks to months.11 When patients have a positive PCR test, there are several important infection control efforts that institutions should consider; see “IDSA weighs in on measures to combat C difficile.”
SIDEBAR
IDSA weighs in on measures to combat C difficile
The spores produced by Clostridioides difficile can survive for 5 months or longer on dry surfaces because of resistance to heat, acid, antibiotics, and many cleaning products.38 Unfortunately, spores transmitted from health care workers and the environment are the most likely cause of infection spreading in health care institutions. To prevent transmission of C difficile infection (CDI) throughout institutions, appropriate infection control measures are necessary.
Clinical practice guidelines from the Infectious Diseases Society of America (IDSA) recommend that patients with CDI be isolated to a private room with a dedicated toilet. Health care staff should wear gloves and gowns when entering the room of, or taking care of, a patient with CDI. For patients who are suspected of having CDI, contact precautions should be implemented while awaiting test results. When the diagnosis is confirmed, contact precautions should remain in place for at least 48 hours after resolution of diarrhea but may be continued until discharge.11
Practicing good hand hygiene is essential, especially in institutions with high rates of CDI or if fecal contamination is likely.11 Hand hygiene with soap and water is preferred, due to evidence of a higher spore removal rate, but alcohol-based alternatives may be used if necessary.11 In institutions with high rates of CDI, terminal (post-discharge) cleaning of rooms with a sporicidal agent should be considered.11
Asymptomatic carriers are also a concern for transmission of CDI in institutional settings. Screening and isolating patients who are carriers may prevent transmission, and some institutions have implemented this process to reduce the risk for CDI that originates in a health care facility.39 The IDSA guidelines do not make a recommendation regarding screening or isolation of asymptomatic carriers, so the decision is institution specific.11 These guidelines also recommend that patients presenting with similar infectious organisms be housed in the same room, if needed, to avoid cross-contamination to others or additional surfaces.11
For pediatric patients, testing recommendations vary by age. Testing is not generally recommended for neonates or infants ≤ 2 years of age with diarrhea because of the prevalence of colonization with C difficile.11 For children older than 2 years, testing for CDI is only recommended in the setting of prolonged or worsening diarrhea and if the patient has risk factors such as IBD, immunocompromised state, health care exposure, or recent antibiotic use.11 In addition, testing in this population should only be considered once other infectious and noninfectious causes of diarrhea have been excluded.11
Continue to: First-line treatment? Drug of choice has changed
First-line treatment? Drug of choice has changed
In 2018, the IDSA published new treatment guidelines that provide important updates from the 2010 guidelines.11 Chief among these was the elimination of metronidazole as a first-line therapy. Vancomycin or fidaxomicin are now recommended as first-line treatment options because of superior eradication of C difficile when compared with metronidazole.11 In the opinion of the authors, vancomycin should be considered the drug of choice because of cost. (See “The case for vancomycin.”)
SIDEBAR
The case for vancomycin
The majority of studies conducted prior to publication of the 2010 Infectious Diseases Society of America guidelines described numerically worse eradication rates of Clostridioides difficile infection (CDI) with metronidazole compared with vancomycin for all severities of infection, but statistical significance was not achieved. These studies also showed a nonsignificant increase in CDI recurrence with metronidazole.17,40,41
A 2005 systematic review demonstrated increased treatment failure rates with metronidazole.42 The rates of metronidazole discontinuation and transition to alternative options more than doubled in 2003-2004, to 25.7% of patients compared with 9.6% in earlier years.42 Metronidazole efficacy was further questioned in a prospective observational study conducted in 2005, in which only 50% of patients were cured after an initial course of treatment, while 28% had recurrence within 90 days.43
Vancomycin was found to be the superior treatment option to metronidazole and tolevamer in a 2014 randomized controlled trial.18 This study also demonstrated that vancomycin was the superior therapy when comparing treatment-naïve vs experienced patients and severity of CDI.18 A 2017 retrospective cohort study demonstrated decreased 30-day all-cause mortality for patients taking vancomycin vs metronidazole (adjusted relative risk = 0.86; 95% confidence interval, 0.74-0.98), although it should be noted that this difference was driven by those with severe CDI, and there was no statistically significant difference in mortality for patients with mild-to-moderate CDI.44
The results of these studies led to the recommendation of vancomycin over metronidazole as first-line pharmacotherapy for CDI in practice, despite the historical perspective that overutilization of oral vancomycin could potentially increase rates of vancomycinresistant Enterococcus.11
Metronidazole should only be used in the treatment of CDI as a lastresort medication because of cost or insurance coverage. Although the price of oral vancomycin is higher, favorable patient outcomes are substantially greater, and recent analyses have shown that vancomycin is actually more cost-effective than metronidazole as a result.24 Adverse effects for metronidazole include neurotoxicity, gastrointestinal discomfort, and disulfiram-like reaction.
Vancomycin does not harbor as many adverse effects because of extremely low systemic absorption when taken orally, but patients may experience gastrointestinal discomfort.45 While systemic exposure with oral administration of vancomycin is very low (< 1%), there have been case reports of nephrotoxicity and “red man syndrome” that are more typically seen with intravenous vancomycin.44
Given the low rate of systemic exposure, routine monitoring of renal function and serum drug levels is not usually necessary during oral vancomycin therapy. However, it may be appropriate to monitor renal function and serum levels of vancomycin in patients who have renal failure, have altered intestinal integrity, are age ≥ 65 years, or are receiving high doses of vancomycin.46
10-day vs 14-day treatment of CDI. Most studies for the treatment of CDI have used a 10-day regimen rather than increasing the duration to a 14-day regimen, and nearly all studies conducted have displayed high rates of symptom resolution at the end of 10 days of treatment.17,18 Thus, treatment duration beyond 10 days should only be considered for patients who continue to have symptoms or complications with CDI on Day 10 of treatment.
First recurrence. Metronidazole is no longer the recommended treatment for first recurrence of CDI treated initially with metronidazole; instead, a 10-day course of vancomycin should be used.11 For recurrent cases in patients initially treated with vancomycin, a tapered and pulsed regimen of vancomycin is recommended11:
- vancomycin PO 125 mg four times daily for 10 to 14 days followed by
- vancomycin PO 125 mg twice daily for 7 days, then
- vancomycin PO 125 mg once daily for 7 days, then
- vancomycin PO 125 mg every 2 to 3 days for 2 to 8 weeks.
Pediatric patients. The IDSA guidelines recommend use of metronidazole or vancomycin to treat an initial case or first recurrence of mild-to-moderate CDI in this population.11 Due to a lack of quality evidence, the drug of choice for initial treatment is inconclusive, so patient-specific factors and cost should be considered when choosing an agent.11 If not cost prohibitive, vancomycin should be the drug of choice for most cases of pediatric CDI, and for severe cases or multiple recurrences of CDI, vancomycin is clearly the drug of choice.
Recommended agents: A closer look
Oral vancomycin products. Vancocin, a capsule, and Firvanq, an oral solution, are 2 vancomycin products currently on the market for CDI. Although the capsules are a readily available treatment option, the cost of the full course of treatment can be a barrier for patients without insurance, or with high copays or deductibles (brand name, $4000; generic, $1252).19
Continue to: Historically, in an effort to keep costs down...
Historically, in an effort to keep costs down, an oral solution was often inexpensively compounded at hospitals or pharmacies.20
Fidaxomicin, an oral macrocyclic antibiotic with minimal systemic absorption, was first approved by the US Food and Drug Administration (FDA) for CDI in 2011.21 The IDSA guidelines recommend fidaxomicin for initial, and recurrent, cases of CDI as an alternative to vancomycin.11 This recommendation is based on 2 randomized double-blind trials comparing fidaxomicin to standard-dose oral vancomycin for initial or recurrent CDI.21,22
Pooled data from these 2 similar studies found that fidaxomicin was noninferior (10% noninferiority margin) to vancomycin for the primary outcome of clinical cure.23 Fidaxomicin was shown to be superior to vancomycin regarding rate of CDI recurrence (relative risk [RR] = 0.61; 95% confidence interval [CI], 0.43-0.87). These results were similar regardless of whether the CDI was an initial or recurrent case.23
Given the lack of systemic absorption, fidaxomicin is generally very well tolerated. The largest downside to fidaxomicin is its cost, which can be nearly $5000 for a standard 10-day course (vs as little as $165 for oral vancomycin).19 As a result, oral vancomycin solution is likely the most cost-effective therapy for initial cases of CDI.24 In patients with poor medication adherence, fidaxomicin offers the advantage of less-frequent dosing (twice daily vs 4 times daily with vancomycin).
For cases of recurrent CDI, when treatment failure occurred with vancomycin, fidaxomicin should be considered as an efficacious alternative. If fidaxomicin is used, it is advisable to verify coverage with the patient’s insurance plan, since prior authorization is frequently required.
Continue to: When meds fail, consider a fecal microbiota transplant
When meds fail, consider a fecal microbiota transplant
Another important change in the IDSA guidelines for CDI management is the strong recommendation for fecal microbiota transplantation (FMT) in patients with multiple recurrences of CDI for whom appropriate antibiotic treatment courses have failed.11,25 The goal of FMT is to “normalize” an abnormal gut microbiome by transplanting donor stool into a recipient.26
FMT has been shown to be highly effective in 5 randomized clinical trials conducted since 2013, with CDI cure rates between 85% and 94%.11 This rate of cure is particularly impressive given that the studies only included patients with refractory CDI.
Patients with recurrent CDI who may be candidates for FMT should be referred to a center or specialist with experience in FMT. These transplants can be expensive because of the screening process involved in obtaining donor samples. (Historically, a single FMT has cost $3000-$5000, and it is seldom covered by insurance.27) The emergence of universal stool banks offers a streamlined solution to this process.26
Fresh or frozen stool is considered equally effective in treating refractory CDI.26 Oral capsule and freeze-dried stool formulations have been studied, but their use is considered investigational at this time.26
Delivery via colonoscopy to the right colon is the preferred route of infusion; however, delivery via enema or nasogastric, nasojejunal, or nasoduodenal infusion can be considered as well.26
Continue to: In preparing for stool transplantation...
In preparing for stool transplantation, patients should be treated with standard doses of oral vancomycin or fidaxomicin for 3 days before the procedure to suppress intestinal C difficile, and the last dose of antibiotics should be given 12 to 48 hours before the procedure.26 Bowel lavage with polyethylene glycol is recommended, regardless of whether stool is delivered via colonoscopy or upper GI route.
Short-term adverse events associated with FMT appear to be minimal; data is lacking for long-term safety outcomes.28 While only recommended currently for cases of recurrent CDI, there is promising data emerging for use of FMT for severe cases, even without recurrence.29
The role of probiotics remains unclear
Probiotics have been explored in numerous trials to determine if they are effective in preventing CDI in patients who have been prescribed antibiotics.11 While no randomized trials have conclusively shown benefit, several meta-analyses have shown that the use of probiotics may result in a 60% to 65% relative risk reduction in CDI incidence.30,31
One proviso to these meta-analyses is that the incorporated studies have typically included patients at very high risk for CDI, and subanalyses have only found a reduction in CDI incidence when patients are at a very high baseline risk. In addition, there are many differences in probiotic types, formulations, treatment durations, and follow-up. As a result, the IDSA guidelines state that there is “insufficient data at this time” to recommend routine administration of probiotics for either primary or secondary CDI prophylaxis.11
Due to insufficient high-quality data, the IDSA guidelines do not provide a recommendation regarding use as an adjunct treatment option for acute CDI.11 Probiotics should not be routinely used to prevent CDI; however, they may provide benefit if reserved for patients at the highest risk for CDI (eg, history of CDI, prolonged use of broad-spectrum antibiotics, high local incidence).
Continue to: What about surgical intervention?
What about surgical intervention?
In severe cases of CDI, surgery may be necessary and can reduce mortality.32 The surgical procedure with the strongest recommendation in the IDSA guidelines is the subtotal colectomy, though the diverting loop ileostomy is an alternative option.11 Patients who may benefit from surgery include those with a WBC count ≥ 25,000; lactate > 5 mmol/L11; altered mental status; megacolon; perforation of the colon; acute abdomen on physical examination; or septic shock due to CDI.33 Although surgery can be beneficial, the mortality rate remains high for those with CDI who undergo colectomy.33
Reserve bezlotoxumab for prevention of recurrence
Bezlotoxumab, a human monoclonal immunoglobulin GI/kappa antibody, was approved by the FDA in 2016 for the prevention of recurrent CDI. Its mechanism of action is to bind and neutralize C difficile toxin B. It was approved as a single infusion for adults who are receiving active antibiotic therapy for CDI and are considered to be at high risk for recurrence.34
This approval was based on 2 trials of more than 2500 patients, in which participants received bezlotoxumab or placebo while receiving treatment for primary or recurrent CDI. The primary outcome of these studies was recurrent infection within 12 weeks after infusion, which was significantly lower for bezlotoxumab in both studies: 17% vs 28% (P < 0.001) in one trial and 16% vs 26% (P < 0.001) in the other trial.35
Bezlotoxumab should only be used as an adjunct to prevent recurrence.32 There is no recommendation for or against bezlotoxumab in the IDSA guidelines because of the recent date of the drug’s approval. Its frequency of use will likely depend on the number of patients who meet criteria as high risk for recurrence and its estimated cost of $4560 per dose.34,36
CASES
CASE 1: In light of Ms. O’s recent completion of a course of clindamycin and unremarkable lab work, she should be treated for mild-to-moderate CDI. She has no comorbid conditions to warrant fidaxomicin, and thus vancomycin (capsules or oral solution) would be the best treatment option. Ms. O is started on vancomycin PO 125 mg qid for 10 days. She is also advised to discontinue loperamide as soon as possible, based on poor outcomes data seen with the use of antimotility agents in CDI.37
Continue to: CASE 2
CASE 2: Ms. Z has several risk factors for recurrent CDI and has an elevated WBC count and SCr level (WBC ≥ 15,000 and SCr > 1.5 mg/dL). Thus, she is classified as having severe, recurrent CDI. Oral levofloxacin and metronidazole should be discontinued, because they increase the risk for treatment failure and development of more virulent CDI strains, such as BI/NAP1/027. Since Ms. Z used metronidazole for treatment of her initial CDI, vancomycin or fidaxomicin should be used at this time. Either vancomycin PO 125 mg qid for 10 days or fidaxomicin 200 mg bid for 10 days would be an appropriate regimen; however, because of cost and unknown insurance coverage, vancomycin is the most appropriate regimen.
CORRESPONDENCE
Jeremy Vandiver, PharmD, BCPS, University of Wyoming School of Pharmacy, Saint Joseph Family Medicine Residency, 1000 E. University Avenue, Dept 3375, Laramie, WY 82071; [email protected]
CASE 1
Beth O, a 63-year-old woman, presents to the emergency department (ED) with a 2-week history of diarrhea (6 very loose, watery stools per day) and lower abdominal pain. The patient denies any vomiting, sick contacts, or recent travel. Past medical history includes varicose veins. Her only active medication is loperamide, as needed, for the past 2 weeks. Ms. O also recently completed a 10-day course of clindamycin for an infected laceration on her finger.
Ms. O’s laboratory values are unremarkable, with a normal white blood cell (WBC) count and serum creatinine (SCr) level. Abdominal computed tomography (CT) reveals some abnormal bowel dilatation and a slight increase in colon wall thickness. There is a high suspicion for Clostridioides difficile (formerly Clostridium difficile) infection (CDI), and stool sent for polymerase chain reaction (PCR) testing comes back positive for C difficile toxin B. It is revealed to be a strain other than the BI/NAP1/027 epidemic strain (which has a higher mortality rate).
How should this patient be treated?
CASE 2
Sixty-eight-year-old Barbara Z presents to the ED from her skilled nursing facility with persistent diarrhea and abdominal cramping. She was diagnosed with CDI about 2 months ago and reports that her symptoms resolved within 4 to 5 days after starting a 14-day course of oral metronidazole.
Her past medical history is notable for multiple myeloma with bone metastasis, for which she is actively undergoing chemotherapy treatment. She also has chronic kidney disease (baseline SCr, 2.2 mg/dL), hypertension, and anemia of chronic disease. The patient’s medications include amlodipine and cholecalciferol. Her chemotherapy regimen consists of bortezomib, lenalidomide, and dexamethasone. CT of the abdomen shows diffuse colon wall thickening with surrounding inflammatory stranding—concerning for pancolitis. There is no evidence of toxic megacolon or ileus.
Ms. Z’s laboratory values are notable for a WBC count of 15,900 cells/mL and an SCr of 4.1 mg/dL. She is started on oral levofloxacin and metronidazole due to concern for an intra-abdominal infection. PCR testing is positive for C difficile, and an enzyme immunoassay (EIA) for C difficile toxin is positive.
What factors put Ms. Z at risk for C difficile, and how should she be treated?
Continue to: C difficile is one of the most...
C difficile is one of the most commonly reported pathogens in health care–associated infections and affects almost 1% of all hospitalized patients in the United States each year.1 From 2001 to 2010, the incidence of CDI doubled in patients discharged from hospitals,2 with an estimated cost of more than $5 billion annually.3 Furthermore, rates of community-associated CDI continue to increase and account for about 40% of cases.4
After colonization in the intestine, C difficile releases 2 toxins (TcdA and TcdB) that cause colitis.5 Patients may present with mild diarrhea that can progress to abdominal pain, cramping, fever, and leukocytosis. Fulminant CDI can lead to the formation of pseudomembranes in the colon, toxic megacolon, bowel perforation, shock, and death.2
Beginning in the early 2000s, hospitals reported increases in severe cases of CDI.6 A specific strain known as BI/NAP1/027 was identified and characterized by fluoroquinolone resistance, increased spore formation, and a higher mortality rate.6
Further complicating matters … Recurrent CDI occurs in up to 10% to 30% of patients,7 typically within 14 to 45 days of completion of antibiotic pharmacotherapy for CDI.8 Recurrence is characterized by new-onset diarrhea or abdominal symptoms after completion of treatment for CDI.5
It typically begins with an antibiotic
Risk factors for CDI are listed in TABLE 1.9 The most important modifiable risk factor for initial and recurrent CDI is recent use of antibiotics.10 Most antibiotics can disrupt normal intestinal flora, causing colonization of C difficile, but the strongest association seems to be with third- and fourth-generation cephalosporins, fluoroquinolones, carbapenems, and clindamycin.11 The risk for CDI occurs during antibiotic treatment, as well as up to 3 months after completion of antibiotic therapy.7 Exposure to multiple antibiotics and extended duration of antibacterial therapy can greatly increase the risk for CDI, so antimicrobial stewardship is key.11
Continue to: Continuing antibiotics while attempting...
Continuing antibiotics while attempting to treat CDI reduces the patient’s clinical response to CDI treatment, which can lead to recurrence.12 The Infectious Diseases Society of America (IDSA) guidelines include a strong recommendation to discontinue concurrent antibiotics as soon as possible in these scenarios.11
Acid-suppression therapy has also been associated with CDI. The mechanism is thought to be an interruption in the protection provided by stomach acid, and use over time may reduce the diversity of flora within the gut microbiome.13 The data demonstrating an association between acid-suppression therapy and CDI is conflicting, which may be a result of confounding factors such as the severity of CDI illness and diarrhea induced by use of proton pump inhibitors (PPIs).4 IDSA guidelines do not provide a recommendation regarding discontinuation of PPI therapy for the prevention of CDI, although inappropriate PPI therapy should always be discontinued.11
Advanced age is an important nonmodifiable risk factor for CDI. Older adults who live in long-term care facilities are at a higher risk for CDI, and these facilities have colonization rates as high as 50%.12
Community-associated risk. In an analysis of community-associated cases of CDI, 82% of patients reported some sort of health care exposure (ranging from physician office visit to surgery admission), 64% reported the receipt of antimicrobial therapy, and 31% reported the use of PPIs.14 Inflammatory bowel disease (IBD) may also put community dwellers at higher risk for CDI and its complications.15
CASES 1 & 2
Both CASE patients have risk factors for CDI. Ms. O (CASE 1) is likely at risk for CDI after completion of her recent course of clindamycin. Ms. Z (CASE 2) has several risk factors for recurrent CDI, including advanced age (≥ 65 years), residence in a long-term care facility, prior antibiotic exposure, and immunodeficiency because of chemotherapy/steroid use.
Continue to: Diagnosis
Diagnosis: Who and how to test
CDI should be both a clinical and laboratory-confirmed diagnosis. Patients should be tested for CDI if they have 3 or more episodes of unexplainable, new-onset unformed stools in 24 hours.11 Asymptomatic patients should not be tested to avoid unnecessary testing and treatment of those who are colonized but not infected.11 It is not recommended to routinely test patients who have taken laxatives within the previous 48 hours.11
There are several stool-based laboratory test options for the diagnosis of CDI (TABLE 211,12,16) but no definitive recommendation for all institutions.11 Many institutions have now implemented PCR testing for the diagnosis of CDI. However, while the benefits of this test include reduced need for repeat testing and possible identification of carriers, it’s estimated that reports of CDI increase more than 50% when an institution switches to PCR testing.1 Nonetheless, a one-step, highly sensitive test such as PCR may be used if strict criteria are implemented and followed.
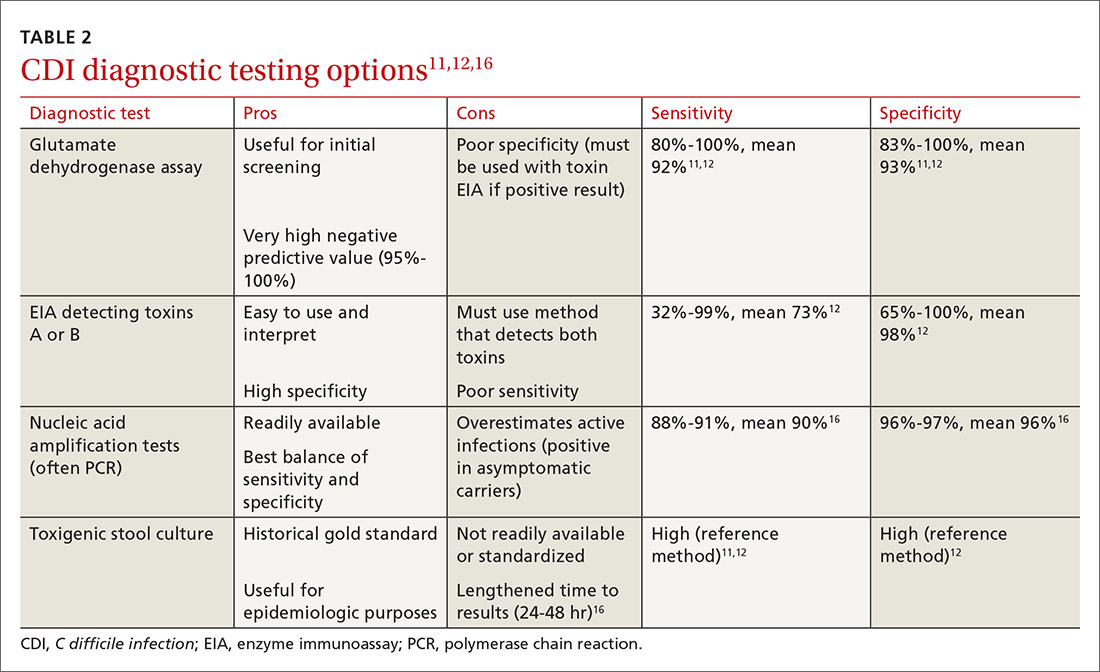
The increase in positive PCR tests has prompted evaluation of using another test in addition to or in place of PCR. Multistep testing options include a glutamate dehydrogenase assay (GDH) with a toxin EIA, GDH with a toxin EIA and final decision via PCR, or PCR with toxin EIA.11 Use of a multistep diagnostic algorithm may increase overall specificity up to 100%, which may improve determination of asymptomatic colonization vs active infection.16 (Patients who have negative toxin results with positive PCR likely have colonization but not infection and often do not require treatment.) IDSA guidelines recommend that the stool toxin test should be part of a multistep algorithm for diagnosis, rather than PCR alone, if strict criteria are not implemented for stool test submission.11
There is no need to perform a test of cure after a patient has been treated for CDI, and no repeat testing should be performed within 7 days of the previous test.11 After successful treatment, patients will continue to shed spores and test positively via PCR for weeks to months.11 When patients have a positive PCR test, there are several important infection control efforts that institutions should consider; see “IDSA weighs in on measures to combat C difficile.”
SIDEBAR
IDSA weighs in on measures to combat C difficile
The spores produced by Clostridioides difficile can survive for 5 months or longer on dry surfaces because of resistance to heat, acid, antibiotics, and many cleaning products.38 Unfortunately, spores transmitted from health care workers and the environment are the most likely cause of infection spreading in health care institutions. To prevent transmission of C difficile infection (CDI) throughout institutions, appropriate infection control measures are necessary.
Clinical practice guidelines from the Infectious Diseases Society of America (IDSA) recommend that patients with CDI be isolated to a private room with a dedicated toilet. Health care staff should wear gloves and gowns when entering the room of, or taking care of, a patient with CDI. For patients who are suspected of having CDI, contact precautions should be implemented while awaiting test results. When the diagnosis is confirmed, contact precautions should remain in place for at least 48 hours after resolution of diarrhea but may be continued until discharge.11
Practicing good hand hygiene is essential, especially in institutions with high rates of CDI or if fecal contamination is likely.11 Hand hygiene with soap and water is preferred, due to evidence of a higher spore removal rate, but alcohol-based alternatives may be used if necessary.11 In institutions with high rates of CDI, terminal (post-discharge) cleaning of rooms with a sporicidal agent should be considered.11
Asymptomatic carriers are also a concern for transmission of CDI in institutional settings. Screening and isolating patients who are carriers may prevent transmission, and some institutions have implemented this process to reduce the risk for CDI that originates in a health care facility.39 The IDSA guidelines do not make a recommendation regarding screening or isolation of asymptomatic carriers, so the decision is institution specific.11 These guidelines also recommend that patients presenting with similar infectious organisms be housed in the same room, if needed, to avoid cross-contamination to others or additional surfaces.11
For pediatric patients, testing recommendations vary by age. Testing is not generally recommended for neonates or infants ≤ 2 years of age with diarrhea because of the prevalence of colonization with C difficile.11 For children older than 2 years, testing for CDI is only recommended in the setting of prolonged or worsening diarrhea and if the patient has risk factors such as IBD, immunocompromised state, health care exposure, or recent antibiotic use.11 In addition, testing in this population should only be considered once other infectious and noninfectious causes of diarrhea have been excluded.11
Continue to: First-line treatment? Drug of choice has changed
First-line treatment? Drug of choice has changed
In 2018, the IDSA published new treatment guidelines that provide important updates from the 2010 guidelines.11 Chief among these was the elimination of metronidazole as a first-line therapy. Vancomycin or fidaxomicin are now recommended as first-line treatment options because of superior eradication of C difficile when compared with metronidazole.11 In the opinion of the authors, vancomycin should be considered the drug of choice because of cost. (See “The case for vancomycin.”)
SIDEBAR
The case for vancomycin
The majority of studies conducted prior to publication of the 2010 Infectious Diseases Society of America guidelines described numerically worse eradication rates of Clostridioides difficile infection (CDI) with metronidazole compared with vancomycin for all severities of infection, but statistical significance was not achieved. These studies also showed a nonsignificant increase in CDI recurrence with metronidazole.17,40,41
A 2005 systematic review demonstrated increased treatment failure rates with metronidazole.42 The rates of metronidazole discontinuation and transition to alternative options more than doubled in 2003-2004, to 25.7% of patients compared with 9.6% in earlier years.42 Metronidazole efficacy was further questioned in a prospective observational study conducted in 2005, in which only 50% of patients were cured after an initial course of treatment, while 28% had recurrence within 90 days.43
Vancomycin was found to be the superior treatment option to metronidazole and tolevamer in a 2014 randomized controlled trial.18 This study also demonstrated that vancomycin was the superior therapy when comparing treatment-naïve vs experienced patients and severity of CDI.18 A 2017 retrospective cohort study demonstrated decreased 30-day all-cause mortality for patients taking vancomycin vs metronidazole (adjusted relative risk = 0.86; 95% confidence interval, 0.74-0.98), although it should be noted that this difference was driven by those with severe CDI, and there was no statistically significant difference in mortality for patients with mild-to-moderate CDI.44
The results of these studies led to the recommendation of vancomycin over metronidazole as first-line pharmacotherapy for CDI in practice, despite the historical perspective that overutilization of oral vancomycin could potentially increase rates of vancomycinresistant Enterococcus.11
Metronidazole should only be used in the treatment of CDI as a lastresort medication because of cost or insurance coverage. Although the price of oral vancomycin is higher, favorable patient outcomes are substantially greater, and recent analyses have shown that vancomycin is actually more cost-effective than metronidazole as a result.24 Adverse effects for metronidazole include neurotoxicity, gastrointestinal discomfort, and disulfiram-like reaction.
Vancomycin does not harbor as many adverse effects because of extremely low systemic absorption when taken orally, but patients may experience gastrointestinal discomfort.45 While systemic exposure with oral administration of vancomycin is very low (< 1%), there have been case reports of nephrotoxicity and “red man syndrome” that are more typically seen with intravenous vancomycin.44
Given the low rate of systemic exposure, routine monitoring of renal function and serum drug levels is not usually necessary during oral vancomycin therapy. However, it may be appropriate to monitor renal function and serum levels of vancomycin in patients who have renal failure, have altered intestinal integrity, are age ≥ 65 years, or are receiving high doses of vancomycin.46
10-day vs 14-day treatment of CDI. Most studies for the treatment of CDI have used a 10-day regimen rather than increasing the duration to a 14-day regimen, and nearly all studies conducted have displayed high rates of symptom resolution at the end of 10 days of treatment.17,18 Thus, treatment duration beyond 10 days should only be considered for patients who continue to have symptoms or complications with CDI on Day 10 of treatment.
First recurrence. Metronidazole is no longer the recommended treatment for first recurrence of CDI treated initially with metronidazole; instead, a 10-day course of vancomycin should be used.11 For recurrent cases in patients initially treated with vancomycin, a tapered and pulsed regimen of vancomycin is recommended11:
- vancomycin PO 125 mg four times daily for 10 to 14 days followed by
- vancomycin PO 125 mg twice daily for 7 days, then
- vancomycin PO 125 mg once daily for 7 days, then
- vancomycin PO 125 mg every 2 to 3 days for 2 to 8 weeks.
Pediatric patients. The IDSA guidelines recommend use of metronidazole or vancomycin to treat an initial case or first recurrence of mild-to-moderate CDI in this population.11 Due to a lack of quality evidence, the drug of choice for initial treatment is inconclusive, so patient-specific factors and cost should be considered when choosing an agent.11 If not cost prohibitive, vancomycin should be the drug of choice for most cases of pediatric CDI, and for severe cases or multiple recurrences of CDI, vancomycin is clearly the drug of choice.
Recommended agents: A closer look
Oral vancomycin products. Vancocin, a capsule, and Firvanq, an oral solution, are 2 vancomycin products currently on the market for CDI. Although the capsules are a readily available treatment option, the cost of the full course of treatment can be a barrier for patients without insurance, or with high copays or deductibles (brand name, $4000; generic, $1252).19
Continue to: Historically, in an effort to keep costs down...
Historically, in an effort to keep costs down, an oral solution was often inexpensively compounded at hospitals or pharmacies.20
Fidaxomicin, an oral macrocyclic antibiotic with minimal systemic absorption, was first approved by the US Food and Drug Administration (FDA) for CDI in 2011.21 The IDSA guidelines recommend fidaxomicin for initial, and recurrent, cases of CDI as an alternative to vancomycin.11 This recommendation is based on 2 randomized double-blind trials comparing fidaxomicin to standard-dose oral vancomycin for initial or recurrent CDI.21,22
Pooled data from these 2 similar studies found that fidaxomicin was noninferior (10% noninferiority margin) to vancomycin for the primary outcome of clinical cure.23 Fidaxomicin was shown to be superior to vancomycin regarding rate of CDI recurrence (relative risk [RR] = 0.61; 95% confidence interval [CI], 0.43-0.87). These results were similar regardless of whether the CDI was an initial or recurrent case.23
Given the lack of systemic absorption, fidaxomicin is generally very well tolerated. The largest downside to fidaxomicin is its cost, which can be nearly $5000 for a standard 10-day course (vs as little as $165 for oral vancomycin).19 As a result, oral vancomycin solution is likely the most cost-effective therapy for initial cases of CDI.24 In patients with poor medication adherence, fidaxomicin offers the advantage of less-frequent dosing (twice daily vs 4 times daily with vancomycin).
For cases of recurrent CDI, when treatment failure occurred with vancomycin, fidaxomicin should be considered as an efficacious alternative. If fidaxomicin is used, it is advisable to verify coverage with the patient’s insurance plan, since prior authorization is frequently required.
Continue to: When meds fail, consider a fecal microbiota transplant
When meds fail, consider a fecal microbiota transplant
Another important change in the IDSA guidelines for CDI management is the strong recommendation for fecal microbiota transplantation (FMT) in patients with multiple recurrences of CDI for whom appropriate antibiotic treatment courses have failed.11,25 The goal of FMT is to “normalize” an abnormal gut microbiome by transplanting donor stool into a recipient.26
FMT has been shown to be highly effective in 5 randomized clinical trials conducted since 2013, with CDI cure rates between 85% and 94%.11 This rate of cure is particularly impressive given that the studies only included patients with refractory CDI.
Patients with recurrent CDI who may be candidates for FMT should be referred to a center or specialist with experience in FMT. These transplants can be expensive because of the screening process involved in obtaining donor samples. (Historically, a single FMT has cost $3000-$5000, and it is seldom covered by insurance.27) The emergence of universal stool banks offers a streamlined solution to this process.26
Fresh or frozen stool is considered equally effective in treating refractory CDI.26 Oral capsule and freeze-dried stool formulations have been studied, but their use is considered investigational at this time.26
Delivery via colonoscopy to the right colon is the preferred route of infusion; however, delivery via enema or nasogastric, nasojejunal, or nasoduodenal infusion can be considered as well.26
Continue to: In preparing for stool transplantation...
In preparing for stool transplantation, patients should be treated with standard doses of oral vancomycin or fidaxomicin for 3 days before the procedure to suppress intestinal C difficile, and the last dose of antibiotics should be given 12 to 48 hours before the procedure.26 Bowel lavage with polyethylene glycol is recommended, regardless of whether stool is delivered via colonoscopy or upper GI route.
Short-term adverse events associated with FMT appear to be minimal; data is lacking for long-term safety outcomes.28 While only recommended currently for cases of recurrent CDI, there is promising data emerging for use of FMT for severe cases, even without recurrence.29
The role of probiotics remains unclear
Probiotics have been explored in numerous trials to determine if they are effective in preventing CDI in patients who have been prescribed antibiotics.11 While no randomized trials have conclusively shown benefit, several meta-analyses have shown that the use of probiotics may result in a 60% to 65% relative risk reduction in CDI incidence.30,31
One proviso to these meta-analyses is that the incorporated studies have typically included patients at very high risk for CDI, and subanalyses have only found a reduction in CDI incidence when patients are at a very high baseline risk. In addition, there are many differences in probiotic types, formulations, treatment durations, and follow-up. As a result, the IDSA guidelines state that there is “insufficient data at this time” to recommend routine administration of probiotics for either primary or secondary CDI prophylaxis.11
Due to insufficient high-quality data, the IDSA guidelines do not provide a recommendation regarding use as an adjunct treatment option for acute CDI.11 Probiotics should not be routinely used to prevent CDI; however, they may provide benefit if reserved for patients at the highest risk for CDI (eg, history of CDI, prolonged use of broad-spectrum antibiotics, high local incidence).
Continue to: What about surgical intervention?
What about surgical intervention?
In severe cases of CDI, surgery may be necessary and can reduce mortality.32 The surgical procedure with the strongest recommendation in the IDSA guidelines is the subtotal colectomy, though the diverting loop ileostomy is an alternative option.11 Patients who may benefit from surgery include those with a WBC count ≥ 25,000; lactate > 5 mmol/L11; altered mental status; megacolon; perforation of the colon; acute abdomen on physical examination; or septic shock due to CDI.33 Although surgery can be beneficial, the mortality rate remains high for those with CDI who undergo colectomy.33
Reserve bezlotoxumab for prevention of recurrence
Bezlotoxumab, a human monoclonal immunoglobulin GI/kappa antibody, was approved by the FDA in 2016 for the prevention of recurrent CDI. Its mechanism of action is to bind and neutralize C difficile toxin B. It was approved as a single infusion for adults who are receiving active antibiotic therapy for CDI and are considered to be at high risk for recurrence.34
This approval was based on 2 trials of more than 2500 patients, in which participants received bezlotoxumab or placebo while receiving treatment for primary or recurrent CDI. The primary outcome of these studies was recurrent infection within 12 weeks after infusion, which was significantly lower for bezlotoxumab in both studies: 17% vs 28% (P < 0.001) in one trial and 16% vs 26% (P < 0.001) in the other trial.35
Bezlotoxumab should only be used as an adjunct to prevent recurrence.32 There is no recommendation for or against bezlotoxumab in the IDSA guidelines because of the recent date of the drug’s approval. Its frequency of use will likely depend on the number of patients who meet criteria as high risk for recurrence and its estimated cost of $4560 per dose.34,36
CASES
CASE 1: In light of Ms. O’s recent completion of a course of clindamycin and unremarkable lab work, she should be treated for mild-to-moderate CDI. She has no comorbid conditions to warrant fidaxomicin, and thus vancomycin (capsules or oral solution) would be the best treatment option. Ms. O is started on vancomycin PO 125 mg qid for 10 days. She is also advised to discontinue loperamide as soon as possible, based on poor outcomes data seen with the use of antimotility agents in CDI.37
Continue to: CASE 2
CASE 2: Ms. Z has several risk factors for recurrent CDI and has an elevated WBC count and SCr level (WBC ≥ 15,000 and SCr > 1.5 mg/dL). Thus, she is classified as having severe, recurrent CDI. Oral levofloxacin and metronidazole should be discontinued, because they increase the risk for treatment failure and development of more virulent CDI strains, such as BI/NAP1/027. Since Ms. Z used metronidazole for treatment of her initial CDI, vancomycin or fidaxomicin should be used at this time. Either vancomycin PO 125 mg qid for 10 days or fidaxomicin 200 mg bid for 10 days would be an appropriate regimen; however, because of cost and unknown insurance coverage, vancomycin is the most appropriate regimen.
CORRESPONDENCE
Jeremy Vandiver, PharmD, BCPS, University of Wyoming School of Pharmacy, Saint Joseph Family Medicine Residency, 1000 E. University Avenue, Dept 3375, Laramie, WY 82071; [email protected]
1. Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med. 2015;175:1792-1801.
2. Reveles KR, Lee GC, Boyd NK, et al. The rise in Clostridium difficile infection incidence among hospitalized adults in the United States: 2001-2010. Am J Infect Control. 2014;42:1028-1032.
3. Dubberke ER, Olsen MA. Burden of Clostridium difficile on the healthcare system. Clin Infect Dis. 2012;55(suppl 2):S88-S92.
4. Tariq R, Singh S, Gupta A, et al. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:784-791.
5. Kachrimanidou M, Malisiovas N. Clostridium difficile infection: a comprehensive review. Crit Rev Microbiol. 2011;37:178-187.
6. O’Connor JR, Johnson S, Gerding DN. Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology. 2009;136:1913-1924.
7. Kelly CP. A 76-year-old man with recurrent Clostridium difficile-associated diarrhea: review of C difficile infection. JAMA. 2009;301:954-962.
8. Cornely OA, Miller MA, Louie TJ, et al. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):S154-S161.
9. Napolitano LM, Edmiston CE Jr. Clostridium difficile disease: diagnosis, pathogenesis, and treatment update. Surgery 2017;162:325-348.
10. Deshpande A, Pasupuleti V, Thota P, et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452-460.
11. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66:e1-e48.
12. Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478-498; quiz 499.
13. Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42.
14. Chitnis AS, Holzbauer SM, Belflower RM, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013;173:1359-1367.
15. Negrón ME, Rezaie A, Barkema HW, et al. Ulcerative colitis patients with Clostridium difficile are at increased risk of death, colectomy, and postoperative complications: a population-based inception cohort study. Am J Gastroenterol. 2016;111:691-704.
16. Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313:398-408.
17. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
18. Johnson S, Louie TJ, Gerding DN, et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59:345-354.
19. Vancomycin: product details. Redbook Online. www.micromedexsolutions.com. Published 2018. Accessed June 13, 2020.
20. Mergenhagen KA, Wojciechowski AL, Paladino JA. A review of the economics of treating Clostridium difficile infection. Pharmacoeconomics. 2014;32:639-650.
21. Louie TJ, Miller MA, Mullane KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422-431.
22. Cornely OA, Crook DW, Esposito R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12:281-289.
23. Crook DW, Walker AS, Kean Y, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection: meta-analysis of pivotal randomized controlled trials. Clin Infect Dis. 2012;55 suppl 2:S93-103.
24. Ford DC, Schroeder MC, Ince D, et al. Cost-effectiveness analysis of initial treatment strategies for mild-to-moderate Clostridium difficile infection in hospitalized patients. Am J Health Syst Pharm. 2018;75:1110-1121.
25. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
26. Panchal P, Budree S, Scheeler A, et al. Scaling safe access to fecal microbiota transplantation: past, present, and future. Curr Gastroenterol Rep. 2018;20:14.
27. Arbel LT, Hsu E, McNally K. Cost-effectiveness of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection: a literature review. Cureus. 2017;9:e1599.
28. Cammarota G, Ianiro G, Tilg H, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569-580.
29. Hocquart M, Lagier JC, Cassir N, et al. Early fecal microbiota transplantation improves survival in severe Clostridium difficile infections. Clin Infect Dis. 2018;66:645-650.
30. Goldenberg JZ, Yap C, Lytvyn L, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2017;12:CD006095.
31. Johnston BC, Lytvyn L, Lo CK, et al. Microbial preparations (probiotics) for the prevention of Clostridium difficile infection in adults and children: an individual patient data meta-analysis of 6,851 participants. Infect Control Hosp Epidemiol. 2018:1-11.
32. Stewart DB, Hollenbeak CS, Wilson MZ. Is colectomy for fulminant Clostridium difficile colitis life saving? A systematic review. Colorectal Dis. 2013;15:798-804.
33. Julien M, Wild JL, Blansfield J, et al. Severe complicated Clostridium difficile infection: can the UPMC proposed scoring system predict the need for surgery? J Trauma Acute Care Surg. 2016;81:221-228.
34. Merck & Co, Inc. Sharp M. ZinplavaTM (bezlotoxumab [package insert] US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2016/761046s000lbl.pdf. Revised October 2016. Accessed May 29, 2020.
35. Wilcox MH, Gerding DN, Poxton IR, et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med. 2017;376:305-317.
36. Chahine EB, Cho JC, Worley MV. Bezlotoxumab for the Prevention of Clostridium difficile recurrence. Consult Pharm. 2018;33:89-97.
37. Koo HL, Koo DC, Musher DM, et al. Antimotility agents for the treatment of Clostridium difficile diarrhea and colitis. Clin Infect Dis. 2009;48:598-605.
38. Rupnik M, Wilcox MH, Gerding DN. Clostridium difficile infection: new developments in epidemiology and pathogenesis. Nat Rev Microbiol. 2009;7:526-536.
39. Longtin Y, Paquet-Bolduc B, Gilca R, et al. Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med. 2016;176:796-804.
40. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet. 1983;2:1043-1046.
41. Wenisch C, Parschalk B, Hasenhündl M, et al. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis. 1996;22:813-818.
42. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
43. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
44. Stevens VW, Nelson RE, Schwab-Daugherty EM, et al. Comparative effectiveness of vancomycin and metronidazole for the prevention of recurrence and death in patients with Clostridium difficile infection. JAMA Intern Med. 2017;177:546-553.
45. CutisPharma. FirvanqTM (vancomycin hydrochloride) for oral solution [package insert]. US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2018/208910s000lbl.pdf. Revised January 2018. Accessed May 29, 2020.
46.
1. Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med. 2015;175:1792-1801.
2. Reveles KR, Lee GC, Boyd NK, et al. The rise in Clostridium difficile infection incidence among hospitalized adults in the United States: 2001-2010. Am J Infect Control. 2014;42:1028-1032.
3. Dubberke ER, Olsen MA. Burden of Clostridium difficile on the healthcare system. Clin Infect Dis. 2012;55(suppl 2):S88-S92.
4. Tariq R, Singh S, Gupta A, et al. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:784-791.
5. Kachrimanidou M, Malisiovas N. Clostridium difficile infection: a comprehensive review. Crit Rev Microbiol. 2011;37:178-187.
6. O’Connor JR, Johnson S, Gerding DN. Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology. 2009;136:1913-1924.
7. Kelly CP. A 76-year-old man with recurrent Clostridium difficile-associated diarrhea: review of C difficile infection. JAMA. 2009;301:954-962.
8. Cornely OA, Miller MA, Louie TJ, et al. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):S154-S161.
9. Napolitano LM, Edmiston CE Jr. Clostridium difficile disease: diagnosis, pathogenesis, and treatment update. Surgery 2017;162:325-348.
10. Deshpande A, Pasupuleti V, Thota P, et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452-460.
11. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66:e1-e48.
12. Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478-498; quiz 499.
13. Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42.
14. Chitnis AS, Holzbauer SM, Belflower RM, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013;173:1359-1367.
15. Negrón ME, Rezaie A, Barkema HW, et al. Ulcerative colitis patients with Clostridium difficile are at increased risk of death, colectomy, and postoperative complications: a population-based inception cohort study. Am J Gastroenterol. 2016;111:691-704.
16. Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313:398-408.
17. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-307.
18. Johnson S, Louie TJ, Gerding DN, et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59:345-354.
19. Vancomycin: product details. Redbook Online. www.micromedexsolutions.com. Published 2018. Accessed June 13, 2020.
20. Mergenhagen KA, Wojciechowski AL, Paladino JA. A review of the economics of treating Clostridium difficile infection. Pharmacoeconomics. 2014;32:639-650.
21. Louie TJ, Miller MA, Mullane KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422-431.
22. Cornely OA, Crook DW, Esposito R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12:281-289.
23. Crook DW, Walker AS, Kean Y, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection: meta-analysis of pivotal randomized controlled trials. Clin Infect Dis. 2012;55 suppl 2:S93-103.
24. Ford DC, Schroeder MC, Ince D, et al. Cost-effectiveness analysis of initial treatment strategies for mild-to-moderate Clostridium difficile infection in hospitalized patients. Am J Health Syst Pharm. 2018;75:1110-1121.
25. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431-455.
26. Panchal P, Budree S, Scheeler A, et al. Scaling safe access to fecal microbiota transplantation: past, present, and future. Curr Gastroenterol Rep. 2018;20:14.
27. Arbel LT, Hsu E, McNally K. Cost-effectiveness of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection: a literature review. Cureus. 2017;9:e1599.
28. Cammarota G, Ianiro G, Tilg H, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569-580.
29. Hocquart M, Lagier JC, Cassir N, et al. Early fecal microbiota transplantation improves survival in severe Clostridium difficile infections. Clin Infect Dis. 2018;66:645-650.
30. Goldenberg JZ, Yap C, Lytvyn L, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2017;12:CD006095.
31. Johnston BC, Lytvyn L, Lo CK, et al. Microbial preparations (probiotics) for the prevention of Clostridium difficile infection in adults and children: an individual patient data meta-analysis of 6,851 participants. Infect Control Hosp Epidemiol. 2018:1-11.
32. Stewart DB, Hollenbeak CS, Wilson MZ. Is colectomy for fulminant Clostridium difficile colitis life saving? A systematic review. Colorectal Dis. 2013;15:798-804.
33. Julien M, Wild JL, Blansfield J, et al. Severe complicated Clostridium difficile infection: can the UPMC proposed scoring system predict the need for surgery? J Trauma Acute Care Surg. 2016;81:221-228.
34. Merck & Co, Inc. Sharp M. ZinplavaTM (bezlotoxumab [package insert] US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2016/761046s000lbl.pdf. Revised October 2016. Accessed May 29, 2020.
35. Wilcox MH, Gerding DN, Poxton IR, et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med. 2017;376:305-317.
36. Chahine EB, Cho JC, Worley MV. Bezlotoxumab for the Prevention of Clostridium difficile recurrence. Consult Pharm. 2018;33:89-97.
37. Koo HL, Koo DC, Musher DM, et al. Antimotility agents for the treatment of Clostridium difficile diarrhea and colitis. Clin Infect Dis. 2009;48:598-605.
38. Rupnik M, Wilcox MH, Gerding DN. Clostridium difficile infection: new developments in epidemiology and pathogenesis. Nat Rev Microbiol. 2009;7:526-536.
39. Longtin Y, Paquet-Bolduc B, Gilca R, et al. Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med. 2016;176:796-804.
40. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet. 1983;2:1043-1046.
41. Wenisch C, Parschalk B, Hasenhündl M, et al. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis. 1996;22:813-818.
42. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591-1597.
43. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005;40:1586-1590.
44. Stevens VW, Nelson RE, Schwab-Daugherty EM, et al. Comparative effectiveness of vancomycin and metronidazole for the prevention of recurrence and death in patients with Clostridium difficile infection. JAMA Intern Med. 2017;177:546-553.
45. CutisPharma. FirvanqTM (vancomycin hydrochloride) for oral solution [package insert]. US Food and Drug Administration Web site. www.accessdata.fda.gov/drugsatfda_docs/label/2018/208910s000lbl.pdf. Revised January 2018. Accessed May 29, 2020.
46.
PRACTICE RECOMMENDATIONS
› Keep in mind that previous exposure to antibiotics is the most important risk factor for initial and recurrent Clostridioides difficile infection (CDI). Thus, appropriate antimicrobial stewardship is key to prevention. C
› Begin with vancomycin or fidaxomicin (over metronidazole) for first-line treatment of CDI in adults. A
› Consider fecal microbiota transplantation in high-risk patients with recurrent CDI for whom antimicrobial therapy has failed. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Simplifying the antibiotic selection process
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
Get updated: Latest ATS/ISDA guidelines for pneumonia
according to Joanna M. Bonsall, MD, PhD, SFHM, chief of hospital medicine at Grady Memorial Hospital and associate professor of medicine at Emory University, both in Atlanta.
Last year, the American Thoracic Society and the Infectious Diseases Society of America updated their clinical guidelines on community-acquired pneumonia (CAP) for the first time since 2007. The guidelines were published in the Oct. 1, 2019 issue of the American Journal of Respiratory and Critical Care Medicine.
CAP is one of the most common reasons for hospitalization in the United States, and it is estimated that CAP comprises over 4.5 million outpatient and ED visits each year, according to the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey in 2009-2010. It is also the most common cause of death from infection disease, according to the Centers for Disease Control and Prevention.
Dr. Bonsall will present “Updates in Pneumonia” at HM20 Virtual, the virtual annual meeting of the Society of Hospital Medicine; a live question-and-answer session will be held online Aug. 20. In her session, Dr. Bonsall said she plans to cover the new ATS/IDSA guidelines for CAP, which will include what initial testing to order, which empiric antibiotics to use, and how to manage patients at risk for resistant organisms, formerly known as health care–associated pneumonia (HCAP). Dr. Bonsall also will outline the evidence for use of steroids, especially in cases of severe pneumonia, and review the 2016 ATS/IDSA guidelines for hospital-acquired pneumonia with a focus on antibiotic selection.
One major change for 2019: The ATS/IDSA CAP guideline authors issued a strong recommendation to abandon use of the term HCAP as a “distinct clinical entity” when considering antibiotics for patients with CAP. In addition, methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa should only be empirically covered in patients with CAP if they present with locally validated risk factors for either pathogen, according to the guidelines.
“Order pretreatment testing based on severity of illness as well as risk factors for drug-resistant pathogens,” Dr. Bonsall said. Hospitalists also should avoid using procalcitonin levels as a benchmark for whether a patient should be started on antibiotics. Once the recommended antibiotic treatment has been initiated, attendees should use culture results to narrow down the possibilities, especially in cases of drug-resistant pathogens.
The ATS/IDSA guidelines also state that corticosteroids should not be routinely used for patients with nonsevere CAP, but attendees should also be aware of the limitations and interpretations of the evidence, Dr. Bonsall said. Avoiding routine corticosteroid use in patients with severe CAP or in patients with severe influenza pneumonia carries a conditional recommendation with a moderate and low quality of evidence, respectively. In general, cases of CAP should be treated for no more than 5 days, or 3 days of treatment after the patient becomes clinically stable.
Attendees at HM20 Virtual should walk away from the session knowing what testing is necessary and what testing is unnecessary, and how to reduce antibiotic exposure for both broad spectrum use and duration. “At the end of the session, you should feel comfortable using both the CAP and HAP guidelines,” Dr. Bonsall said.
Dr. Bonsall reported no relevant financial disclosures.
Updates in Pneumonia
Live Q&A: Thursday, Aug. 20, 2:15 p.m to 3:15 p.m.
according to Joanna M. Bonsall, MD, PhD, SFHM, chief of hospital medicine at Grady Memorial Hospital and associate professor of medicine at Emory University, both in Atlanta.
Last year, the American Thoracic Society and the Infectious Diseases Society of America updated their clinical guidelines on community-acquired pneumonia (CAP) for the first time since 2007. The guidelines were published in the Oct. 1, 2019 issue of the American Journal of Respiratory and Critical Care Medicine.
CAP is one of the most common reasons for hospitalization in the United States, and it is estimated that CAP comprises over 4.5 million outpatient and ED visits each year, according to the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey in 2009-2010. It is also the most common cause of death from infection disease, according to the Centers for Disease Control and Prevention.
Dr. Bonsall will present “Updates in Pneumonia” at HM20 Virtual, the virtual annual meeting of the Society of Hospital Medicine; a live question-and-answer session will be held online Aug. 20. In her session, Dr. Bonsall said she plans to cover the new ATS/IDSA guidelines for CAP, which will include what initial testing to order, which empiric antibiotics to use, and how to manage patients at risk for resistant organisms, formerly known as health care–associated pneumonia (HCAP). Dr. Bonsall also will outline the evidence for use of steroids, especially in cases of severe pneumonia, and review the 2016 ATS/IDSA guidelines for hospital-acquired pneumonia with a focus on antibiotic selection.
One major change for 2019: The ATS/IDSA CAP guideline authors issued a strong recommendation to abandon use of the term HCAP as a “distinct clinical entity” when considering antibiotics for patients with CAP. In addition, methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa should only be empirically covered in patients with CAP if they present with locally validated risk factors for either pathogen, according to the guidelines.
“Order pretreatment testing based on severity of illness as well as risk factors for drug-resistant pathogens,” Dr. Bonsall said. Hospitalists also should avoid using procalcitonin levels as a benchmark for whether a patient should be started on antibiotics. Once the recommended antibiotic treatment has been initiated, attendees should use culture results to narrow down the possibilities, especially in cases of drug-resistant pathogens.
The ATS/IDSA guidelines also state that corticosteroids should not be routinely used for patients with nonsevere CAP, but attendees should also be aware of the limitations and interpretations of the evidence, Dr. Bonsall said. Avoiding routine corticosteroid use in patients with severe CAP or in patients with severe influenza pneumonia carries a conditional recommendation with a moderate and low quality of evidence, respectively. In general, cases of CAP should be treated for no more than 5 days, or 3 days of treatment after the patient becomes clinically stable.
Attendees at HM20 Virtual should walk away from the session knowing what testing is necessary and what testing is unnecessary, and how to reduce antibiotic exposure for both broad spectrum use and duration. “At the end of the session, you should feel comfortable using both the CAP and HAP guidelines,” Dr. Bonsall said.
Dr. Bonsall reported no relevant financial disclosures.
Updates in Pneumonia
Live Q&A: Thursday, Aug. 20, 2:15 p.m to 3:15 p.m.
according to Joanna M. Bonsall, MD, PhD, SFHM, chief of hospital medicine at Grady Memorial Hospital and associate professor of medicine at Emory University, both in Atlanta.
Last year, the American Thoracic Society and the Infectious Diseases Society of America updated their clinical guidelines on community-acquired pneumonia (CAP) for the first time since 2007. The guidelines were published in the Oct. 1, 2019 issue of the American Journal of Respiratory and Critical Care Medicine.
CAP is one of the most common reasons for hospitalization in the United States, and it is estimated that CAP comprises over 4.5 million outpatient and ED visits each year, according to the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey in 2009-2010. It is also the most common cause of death from infection disease, according to the Centers for Disease Control and Prevention.
Dr. Bonsall will present “Updates in Pneumonia” at HM20 Virtual, the virtual annual meeting of the Society of Hospital Medicine; a live question-and-answer session will be held online Aug. 20. In her session, Dr. Bonsall said she plans to cover the new ATS/IDSA guidelines for CAP, which will include what initial testing to order, which empiric antibiotics to use, and how to manage patients at risk for resistant organisms, formerly known as health care–associated pneumonia (HCAP). Dr. Bonsall also will outline the evidence for use of steroids, especially in cases of severe pneumonia, and review the 2016 ATS/IDSA guidelines for hospital-acquired pneumonia with a focus on antibiotic selection.
One major change for 2019: The ATS/IDSA CAP guideline authors issued a strong recommendation to abandon use of the term HCAP as a “distinct clinical entity” when considering antibiotics for patients with CAP. In addition, methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa should only be empirically covered in patients with CAP if they present with locally validated risk factors for either pathogen, according to the guidelines.
“Order pretreatment testing based on severity of illness as well as risk factors for drug-resistant pathogens,” Dr. Bonsall said. Hospitalists also should avoid using procalcitonin levels as a benchmark for whether a patient should be started on antibiotics. Once the recommended antibiotic treatment has been initiated, attendees should use culture results to narrow down the possibilities, especially in cases of drug-resistant pathogens.
The ATS/IDSA guidelines also state that corticosteroids should not be routinely used for patients with nonsevere CAP, but attendees should also be aware of the limitations and interpretations of the evidence, Dr. Bonsall said. Avoiding routine corticosteroid use in patients with severe CAP or in patients with severe influenza pneumonia carries a conditional recommendation with a moderate and low quality of evidence, respectively. In general, cases of CAP should be treated for no more than 5 days, or 3 days of treatment after the patient becomes clinically stable.
Attendees at HM20 Virtual should walk away from the session knowing what testing is necessary and what testing is unnecessary, and how to reduce antibiotic exposure for both broad spectrum use and duration. “At the end of the session, you should feel comfortable using both the CAP and HAP guidelines,” Dr. Bonsall said.
Dr. Bonsall reported no relevant financial disclosures.
Updates in Pneumonia
Live Q&A: Thursday, Aug. 20, 2:15 p.m to 3:15 p.m.
Sepsis: Vitamin C, thiamine, glucocorticoids remain controversial
Sepsis is the number one killer in U.S. hospitals. About one in three patient deaths in a hospital are attributable to sepsis, according to the Centers for Disease Control and Prevention, and it is the leading cause of readmission for U.S. hospitals as well.
Patricia Kritek MD, EdM, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, hopes to bring attendees up to speed on sepsis with her presentation, “Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis” at HM20 Virtual.
Each year, approximately 1.7 million American adults develop sepsis, and nearly 270,000 Americans will die from sepsis annually. Although sepsis disproportionately affects young children, older adults, patients with chronic diseases, and those with a weak immune system, the disease can affect anyone.
With that reputation, sepsis is on the forefront of hospitalists’ minds. Hospitalists are traditionally well versed in current sepsis guidelines, but time to treatment is paramount, and it can be difficult to stay up to date on the latest studies in the field.
The title of Dr. Kritek’s presentation hints at the theme: Hospitalists may have learned the systemic inflammatory response syndrome (SIRS) criteria for diagnosing sepsis, but the Sequential Organ Failure Assessment (SOFA) Score developed by the Third International Consensus Definitions for Sepsis and Septic Shock – previously known as the sepsis-related organ failure assessment score – has been the new method since 2016 to assess the clinical outcomes of patients with sepsis.
The quick SOFA score (qSOFA), developed by the Society of Critical Care and European Society of Intensive Care Medicine in 2016 guidelines, further helps hospitalists and other hospital physicians identify those patients at highest risk of mortality from sepsis outside an intensive care unit setting.
Dr. Kritek, who is a board-certified critical care medicine physician, has previously presented this talk at the Society for Hospital Medicine Annual Conference in the past. This year the presentation will include a number of studies that examine what role vitamin C, thiamine, and glucocorticoids have in treating patients with sepsis, she said. For example, it is thought that parenteral administration of vitamin C could raise plasma levels and reduce multiorgan failure. Thiamine could be useful in sepsis treatment because of its role in glucose metabolism and lactate production, while glucocorticoids could help improve the mortality rate of patients with sepsis.
While Dr. Kritek said she is not going to be advocating for the benefit of vitamin C and thiamine during the session, “this is an area of ongoing debate, and we will walk through the most recent data to try to make sense of it,” she said.
Dr. Kritek noted that the role of balanced crystalloids in resuscitation will be discussed versus when to use saline, as well as the potential of new vasopressors for the treatment of septic shock.
“Our goal will be to integrate the most recent literature into day-to-day practice,” Dr. Kritek said.Dr. Kritek reports no conflicts of interest.
“Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis”
Sepsis is the number one killer in U.S. hospitals. About one in three patient deaths in a hospital are attributable to sepsis, according to the Centers for Disease Control and Prevention, and it is the leading cause of readmission for U.S. hospitals as well.
Patricia Kritek MD, EdM, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, hopes to bring attendees up to speed on sepsis with her presentation, “Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis” at HM20 Virtual.
Each year, approximately 1.7 million American adults develop sepsis, and nearly 270,000 Americans will die from sepsis annually. Although sepsis disproportionately affects young children, older adults, patients with chronic diseases, and those with a weak immune system, the disease can affect anyone.
With that reputation, sepsis is on the forefront of hospitalists’ minds. Hospitalists are traditionally well versed in current sepsis guidelines, but time to treatment is paramount, and it can be difficult to stay up to date on the latest studies in the field.
The title of Dr. Kritek’s presentation hints at the theme: Hospitalists may have learned the systemic inflammatory response syndrome (SIRS) criteria for diagnosing sepsis, but the Sequential Organ Failure Assessment (SOFA) Score developed by the Third International Consensus Definitions for Sepsis and Septic Shock – previously known as the sepsis-related organ failure assessment score – has been the new method since 2016 to assess the clinical outcomes of patients with sepsis.
The quick SOFA score (qSOFA), developed by the Society of Critical Care and European Society of Intensive Care Medicine in 2016 guidelines, further helps hospitalists and other hospital physicians identify those patients at highest risk of mortality from sepsis outside an intensive care unit setting.
Dr. Kritek, who is a board-certified critical care medicine physician, has previously presented this talk at the Society for Hospital Medicine Annual Conference in the past. This year the presentation will include a number of studies that examine what role vitamin C, thiamine, and glucocorticoids have in treating patients with sepsis, she said. For example, it is thought that parenteral administration of vitamin C could raise plasma levels and reduce multiorgan failure. Thiamine could be useful in sepsis treatment because of its role in glucose metabolism and lactate production, while glucocorticoids could help improve the mortality rate of patients with sepsis.
While Dr. Kritek said she is not going to be advocating for the benefit of vitamin C and thiamine during the session, “this is an area of ongoing debate, and we will walk through the most recent data to try to make sense of it,” she said.
Dr. Kritek noted that the role of balanced crystalloids in resuscitation will be discussed versus when to use saline, as well as the potential of new vasopressors for the treatment of septic shock.
“Our goal will be to integrate the most recent literature into day-to-day practice,” Dr. Kritek said.Dr. Kritek reports no conflicts of interest.
“Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis”
Sepsis is the number one killer in U.S. hospitals. About one in three patient deaths in a hospital are attributable to sepsis, according to the Centers for Disease Control and Prevention, and it is the leading cause of readmission for U.S. hospitals as well.
Patricia Kritek MD, EdM, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, hopes to bring attendees up to speed on sepsis with her presentation, “Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis” at HM20 Virtual.
Each year, approximately 1.7 million American adults develop sepsis, and nearly 270,000 Americans will die from sepsis annually. Although sepsis disproportionately affects young children, older adults, patients with chronic diseases, and those with a weak immune system, the disease can affect anyone.
With that reputation, sepsis is on the forefront of hospitalists’ minds. Hospitalists are traditionally well versed in current sepsis guidelines, but time to treatment is paramount, and it can be difficult to stay up to date on the latest studies in the field.
The title of Dr. Kritek’s presentation hints at the theme: Hospitalists may have learned the systemic inflammatory response syndrome (SIRS) criteria for diagnosing sepsis, but the Sequential Organ Failure Assessment (SOFA) Score developed by the Third International Consensus Definitions for Sepsis and Septic Shock – previously known as the sepsis-related organ failure assessment score – has been the new method since 2016 to assess the clinical outcomes of patients with sepsis.
The quick SOFA score (qSOFA), developed by the Society of Critical Care and European Society of Intensive Care Medicine in 2016 guidelines, further helps hospitalists and other hospital physicians identify those patients at highest risk of mortality from sepsis outside an intensive care unit setting.
Dr. Kritek, who is a board-certified critical care medicine physician, has previously presented this talk at the Society for Hospital Medicine Annual Conference in the past. This year the presentation will include a number of studies that examine what role vitamin C, thiamine, and glucocorticoids have in treating patients with sepsis, she said. For example, it is thought that parenteral administration of vitamin C could raise plasma levels and reduce multiorgan failure. Thiamine could be useful in sepsis treatment because of its role in glucose metabolism and lactate production, while glucocorticoids could help improve the mortality rate of patients with sepsis.
While Dr. Kritek said she is not going to be advocating for the benefit of vitamin C and thiamine during the session, “this is an area of ongoing debate, and we will walk through the most recent data to try to make sense of it,” she said.
Dr. Kritek noted that the role of balanced crystalloids in resuscitation will be discussed versus when to use saline, as well as the potential of new vasopressors for the treatment of septic shock.
“Our goal will be to integrate the most recent literature into day-to-day practice,” Dr. Kritek said.Dr. Kritek reports no conflicts of interest.
“Put SIRS on the SOFA and Let’s get Septic! Update in Sepsis”
Schools can reopen safely with precautions, experts say
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
Why doctors keep monitoring kids who recover from mysterious COVID-linked illness
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
Proton pump inhibitors tied to COVID-19 risk
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Easy access to PrEP reduces rates of HIV acquisition
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
Zika virus syndrome may adversely affect children normocephalic at birth
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
FROM JAMA NETWORK OPEN
HSCT or systemic treatment should be offered to HIV+ patients with lymphoma
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA