User login
EULAR's Lupus Nephritis Guidelines Emphasize Early Biopsy
The European League Against Rheumatism has issued its first guidelines on management of lupus nephritis, and they advise renal biopsy at the first sign of kidney involvement, unlike the guidance issued by the American College of Rheumatology, which leaves timing of that testing up to the clinician’s judgment.
Other bright spots in EULAR’s guidelines, which it issued jointly with the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) are their position that mycophenolic acid should be the first choice for immunosuppressive therapy, the precise recommendations for steroid dosage, stratification of treatment plans according to disease severity, and explicit advice on switching therapies after one drug has failed.
The European guidelines were published in the November issue of Annals of the Rheumatic Diseases (2012;71:1771-82) and are intended for rheumatologists, nephrologists, and internists managing adult and pediatric patients with lupus nephritis. The EULAR guidelines differ in several key ways from those issued by the American College of Rheumatology (ACR) in June (Arthritis Care Res. 2012;64:797-808).
The EULAR guidelines are unequivocal in their support for renal biopsy at any sign of renal involvement, including when unexplained renal insufficiency is accompanied by normal urinary findings. The ACR guidelines, by contrast, allow for more physician latitude in determining whether to biopsy.
"This can be an emotional issue because rheumatologists do not do biopsies and may try to avoid them," said the EULAR guidelines’ lead author, rheumatologist Dr. Dimitrios T. Boumpas, who is professor of medicine and director of internal medicine/rheumatology at the University of Crete in Heraklion, Greece, in an interview. "We felt that someone should make a position statement. Biopsy is simply best care. If you’re dealing with something severe like LN [lupus nephritis] and you avoid biopsy, that’s not good medicine."
Dr. Boumpas said the EULAR task force had also moved to put mycophenolic acid in the first position as an initial immunosuppressant treatment for most cases of class III-IV LN. Low-dose intravenous cyclophosphamide in combination with steroids is also recommended for this patient group.
There are no 5-year data for mycophenolic acid as there are for cyclophosphamide, Dr. Boumpas said. But the task force that developed the guidelines weighed data on safety and efficacy and found mycophenolic acid "as the clear first choice, while at the same time recognizing the limitations of the studies," he noted.
The ACR guidelines do not recommend use of azathioprine (AZA) as induction treatment. The EULAR recommendations acknowledge that AZA has been associated with a higher risk of renal flares, and call for its use in certain patients who have no adverse clinical or histological risk factors. Patients treated with AZA need close follow-up. "This is particularly important for countries without access to MPA [mycophenolic acid]," Dr. Boumpas said.
The EULAR guidelines also recommend switching to an alternative agent when patients fail to improve in 3-4 months or do not achieve partial response after 6-12 months, or a complete response after 2 years.
"This is based on evidence from both controlled trials and observational cohort studies, which highlight the fact that immunosuppressive agents, particularly cyclophosphamide, may take up to 2 years to achieve complete renal response," Dr. George K. Bertsias, also of the University of Crete in Heraklion and the first author of the guidelines, said in an interview. "On the other hand, lack of improvement at early time points (3-6 months) is associated with adverse prognosis and should evoke discussions for treatment intensification or switch."
This is a different timetable from that described in the ACR guidelines, which advocate switching after patients fail to respond after 6 months of treatment based on the treating physician’s clinical impression.
For patients not responding to mycophenolic acid or cyclophosphamide, treatment may be switched from mycophenolic acid to cyclophosphamide or from cyclophosphamide to mycophenolic acid, according to the guidelines.
If switching fails, rituximab, a biological agent, may be given either as an add-on treatment or as monotherapy. Although randomized controlled trials have failed to demonstrate the superiority of rituximab over standard treatment in lupus nephritis, "there is culminating evidence from several uncontrolled studies and several groups worldwide that rituximab works in about half of patients with nephritis refractory to conventional immunosuppressive therapy," Dr. Boumpas said. "Since rituximab does not have adverse effects on the gonads – a significant issue in the care of young women with lupus – the committee decided to recommend it as an additional treatment resource."
The EULAR guidelines, in contrast to the ACR guidelines, contain specific dosing advice on steroids, advocating pulse steroids (500-1,000 mg of methylprednisolone daily for three doses) in combination with initial immunosuppressive therapy, followed by daily oral glucocorticoids (0.5-1.0 mg/kg per day), afterward tapering to the minimal amount necessary to control disease.
The EULAR guidelines also contain specific recommendations for patients planning pregnancy. In addition, they cover diagnosis and management of pediatric lupus nephritis, which largely follow adult recommendations. The pediatric recommendations are based on evidence in adults, and on nonrandomized evidence in children.
Work on the recommendations was funded by EULAR and the ERA-EDTA. The authors declared no conflicts of interest.
European Renal Association-European Dialysis and Transplant Association, ERA-EDTA, mycophenolic acid, immunosuppressive therapy, Annals of the Rheumatic Diseases, Dr. Dimitrios T. Boumpas,
The European League Against Rheumatism has issued its first guidelines on management of lupus nephritis, and they advise renal biopsy at the first sign of kidney involvement, unlike the guidance issued by the American College of Rheumatology, which leaves timing of that testing up to the clinician’s judgment.
Other bright spots in EULAR’s guidelines, which it issued jointly with the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) are their position that mycophenolic acid should be the first choice for immunosuppressive therapy, the precise recommendations for steroid dosage, stratification of treatment plans according to disease severity, and explicit advice on switching therapies after one drug has failed.
The European guidelines were published in the November issue of Annals of the Rheumatic Diseases (2012;71:1771-82) and are intended for rheumatologists, nephrologists, and internists managing adult and pediatric patients with lupus nephritis. The EULAR guidelines differ in several key ways from those issued by the American College of Rheumatology (ACR) in June (Arthritis Care Res. 2012;64:797-808).
The EULAR guidelines are unequivocal in their support for renal biopsy at any sign of renal involvement, including when unexplained renal insufficiency is accompanied by normal urinary findings. The ACR guidelines, by contrast, allow for more physician latitude in determining whether to biopsy.
"This can be an emotional issue because rheumatologists do not do biopsies and may try to avoid them," said the EULAR guidelines’ lead author, rheumatologist Dr. Dimitrios T. Boumpas, who is professor of medicine and director of internal medicine/rheumatology at the University of Crete in Heraklion, Greece, in an interview. "We felt that someone should make a position statement. Biopsy is simply best care. If you’re dealing with something severe like LN [lupus nephritis] and you avoid biopsy, that’s not good medicine."
Dr. Boumpas said the EULAR task force had also moved to put mycophenolic acid in the first position as an initial immunosuppressant treatment for most cases of class III-IV LN. Low-dose intravenous cyclophosphamide in combination with steroids is also recommended for this patient group.
There are no 5-year data for mycophenolic acid as there are for cyclophosphamide, Dr. Boumpas said. But the task force that developed the guidelines weighed data on safety and efficacy and found mycophenolic acid "as the clear first choice, while at the same time recognizing the limitations of the studies," he noted.
The ACR guidelines do not recommend use of azathioprine (AZA) as induction treatment. The EULAR recommendations acknowledge that AZA has been associated with a higher risk of renal flares, and call for its use in certain patients who have no adverse clinical or histological risk factors. Patients treated with AZA need close follow-up. "This is particularly important for countries without access to MPA [mycophenolic acid]," Dr. Boumpas said.
The EULAR guidelines also recommend switching to an alternative agent when patients fail to improve in 3-4 months or do not achieve partial response after 6-12 months, or a complete response after 2 years.
"This is based on evidence from both controlled trials and observational cohort studies, which highlight the fact that immunosuppressive agents, particularly cyclophosphamide, may take up to 2 years to achieve complete renal response," Dr. George K. Bertsias, also of the University of Crete in Heraklion and the first author of the guidelines, said in an interview. "On the other hand, lack of improvement at early time points (3-6 months) is associated with adverse prognosis and should evoke discussions for treatment intensification or switch."
This is a different timetable from that described in the ACR guidelines, which advocate switching after patients fail to respond after 6 months of treatment based on the treating physician’s clinical impression.
For patients not responding to mycophenolic acid or cyclophosphamide, treatment may be switched from mycophenolic acid to cyclophosphamide or from cyclophosphamide to mycophenolic acid, according to the guidelines.
If switching fails, rituximab, a biological agent, may be given either as an add-on treatment or as monotherapy. Although randomized controlled trials have failed to demonstrate the superiority of rituximab over standard treatment in lupus nephritis, "there is culminating evidence from several uncontrolled studies and several groups worldwide that rituximab works in about half of patients with nephritis refractory to conventional immunosuppressive therapy," Dr. Boumpas said. "Since rituximab does not have adverse effects on the gonads – a significant issue in the care of young women with lupus – the committee decided to recommend it as an additional treatment resource."
The EULAR guidelines, in contrast to the ACR guidelines, contain specific dosing advice on steroids, advocating pulse steroids (500-1,000 mg of methylprednisolone daily for three doses) in combination with initial immunosuppressive therapy, followed by daily oral glucocorticoids (0.5-1.0 mg/kg per day), afterward tapering to the minimal amount necessary to control disease.
The EULAR guidelines also contain specific recommendations for patients planning pregnancy. In addition, they cover diagnosis and management of pediatric lupus nephritis, which largely follow adult recommendations. The pediatric recommendations are based on evidence in adults, and on nonrandomized evidence in children.
Work on the recommendations was funded by EULAR and the ERA-EDTA. The authors declared no conflicts of interest.
The European League Against Rheumatism has issued its first guidelines on management of lupus nephritis, and they advise renal biopsy at the first sign of kidney involvement, unlike the guidance issued by the American College of Rheumatology, which leaves timing of that testing up to the clinician’s judgment.
Other bright spots in EULAR’s guidelines, which it issued jointly with the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) are their position that mycophenolic acid should be the first choice for immunosuppressive therapy, the precise recommendations for steroid dosage, stratification of treatment plans according to disease severity, and explicit advice on switching therapies after one drug has failed.
The European guidelines were published in the November issue of Annals of the Rheumatic Diseases (2012;71:1771-82) and are intended for rheumatologists, nephrologists, and internists managing adult and pediatric patients with lupus nephritis. The EULAR guidelines differ in several key ways from those issued by the American College of Rheumatology (ACR) in June (Arthritis Care Res. 2012;64:797-808).
The EULAR guidelines are unequivocal in their support for renal biopsy at any sign of renal involvement, including when unexplained renal insufficiency is accompanied by normal urinary findings. The ACR guidelines, by contrast, allow for more physician latitude in determining whether to biopsy.
"This can be an emotional issue because rheumatologists do not do biopsies and may try to avoid them," said the EULAR guidelines’ lead author, rheumatologist Dr. Dimitrios T. Boumpas, who is professor of medicine and director of internal medicine/rheumatology at the University of Crete in Heraklion, Greece, in an interview. "We felt that someone should make a position statement. Biopsy is simply best care. If you’re dealing with something severe like LN [lupus nephritis] and you avoid biopsy, that’s not good medicine."
Dr. Boumpas said the EULAR task force had also moved to put mycophenolic acid in the first position as an initial immunosuppressant treatment for most cases of class III-IV LN. Low-dose intravenous cyclophosphamide in combination with steroids is also recommended for this patient group.
There are no 5-year data for mycophenolic acid as there are for cyclophosphamide, Dr. Boumpas said. But the task force that developed the guidelines weighed data on safety and efficacy and found mycophenolic acid "as the clear first choice, while at the same time recognizing the limitations of the studies," he noted.
The ACR guidelines do not recommend use of azathioprine (AZA) as induction treatment. The EULAR recommendations acknowledge that AZA has been associated with a higher risk of renal flares, and call for its use in certain patients who have no adverse clinical or histological risk factors. Patients treated with AZA need close follow-up. "This is particularly important for countries without access to MPA [mycophenolic acid]," Dr. Boumpas said.
The EULAR guidelines also recommend switching to an alternative agent when patients fail to improve in 3-4 months or do not achieve partial response after 6-12 months, or a complete response after 2 years.
"This is based on evidence from both controlled trials and observational cohort studies, which highlight the fact that immunosuppressive agents, particularly cyclophosphamide, may take up to 2 years to achieve complete renal response," Dr. George K. Bertsias, also of the University of Crete in Heraklion and the first author of the guidelines, said in an interview. "On the other hand, lack of improvement at early time points (3-6 months) is associated with adverse prognosis and should evoke discussions for treatment intensification or switch."
This is a different timetable from that described in the ACR guidelines, which advocate switching after patients fail to respond after 6 months of treatment based on the treating physician’s clinical impression.
For patients not responding to mycophenolic acid or cyclophosphamide, treatment may be switched from mycophenolic acid to cyclophosphamide or from cyclophosphamide to mycophenolic acid, according to the guidelines.
If switching fails, rituximab, a biological agent, may be given either as an add-on treatment or as monotherapy. Although randomized controlled trials have failed to demonstrate the superiority of rituximab over standard treatment in lupus nephritis, "there is culminating evidence from several uncontrolled studies and several groups worldwide that rituximab works in about half of patients with nephritis refractory to conventional immunosuppressive therapy," Dr. Boumpas said. "Since rituximab does not have adverse effects on the gonads – a significant issue in the care of young women with lupus – the committee decided to recommend it as an additional treatment resource."
The EULAR guidelines, in contrast to the ACR guidelines, contain specific dosing advice on steroids, advocating pulse steroids (500-1,000 mg of methylprednisolone daily for three doses) in combination with initial immunosuppressive therapy, followed by daily oral glucocorticoids (0.5-1.0 mg/kg per day), afterward tapering to the minimal amount necessary to control disease.
The EULAR guidelines also contain specific recommendations for patients planning pregnancy. In addition, they cover diagnosis and management of pediatric lupus nephritis, which largely follow adult recommendations. The pediatric recommendations are based on evidence in adults, and on nonrandomized evidence in children.
Work on the recommendations was funded by EULAR and the ERA-EDTA. The authors declared no conflicts of interest.
European Renal Association-European Dialysis and Transplant Association, ERA-EDTA, mycophenolic acid, immunosuppressive therapy, Annals of the Rheumatic Diseases, Dr. Dimitrios T. Boumpas,
European Renal Association-European Dialysis and Transplant Association, ERA-EDTA, mycophenolic acid, immunosuppressive therapy, Annals of the Rheumatic Diseases, Dr. Dimitrios T. Boumpas,
FROM ANNALS OF THE RHEUMATIC DISEASES
CTA Lacks Accuracy for Assessing In-Stent Restenosis
BALTIMORE – CT angiography is not accurate enough to assess in-stent restenosis, compared with invasive coronary angiography, based on the results of a meta-analysis.
In 11 studies with data on the patient level (804 patients with 1,295 stents), the pooled sensitivity of CT was 94% and the specificity was 92%. In six studies using 64-row or greater CT, the pooled sensitivity of CT was 94% and specificity of CT was 94%. However, the difference compared with all 11 patient-level studies was not significant.
They also looked at the influence of stent size on CT accuracy in eight studies with 1,246 stents. Sensitivity was 81% for stents less than 3 mm and 92% for stents at least 3 mm in size. Specificity was 84% for stents less than 3 mm and 98% for stents at least 3 mm in size.
"In other words, the type of stent and the characteristics that the patient brings with him or her is much more important than the type of scanner that you have sitting there," said Dr. Marc Dewey of Charité – Universitätsmedizin Berlin. The findings were presented at the annual meeting of the Society of Cardiovascular Computed Tomography.
The researchers included prospective studies using at least 12-row CT scanners. Patients were assessed for 50% diameter in-stent restenosis as clinically relevant. All patients had to have coronary angiography.
The researchers included several databases: MEDLINE, EMBASE, ISI’s Web of Science (now Thomson Reuters Web of Knowledge) and the Cochrane Library. Search terms included "computed tomography," "coronary angiography," and "stent." Overall, they identified 33 studies with stent-level data.
Based on likelihood ratios, "we couldn’t conclude that CT was reliable in ruling in and ruling out coronary stent restenosis," said Dr. Dewey.
The investigators also looked at nondiagnostic studies. There were 30 studies with information on the stent level and 17 studies with information on the patient level. They used a missing data technique to assess for less-than-perfect reporting on the study level. The nondiagnostic rate on the patient level was 6% on average, based on the reported results, but the confidence intervals went up to more than 13%. "So almost every six or seven patients would be nondiagnostic."
"Coronary stent imaging by CT is slightly better using 64-row CT and above, though this was not significant. On the other hand, patients with stents that were at least 3 mm or larger could be significantly better assessed. Specificity in particular was significantly improved," said Dr. Dewey.
On the basis of these findings, CT should not be recommended for the assessment of coronary stent restenosis.
The study was funded by the German Research Foundation. The investigators did not report whether they have any significant conflicts of interest.
BALTIMORE – CT angiography is not accurate enough to assess in-stent restenosis, compared with invasive coronary angiography, based on the results of a meta-analysis.
In 11 studies with data on the patient level (804 patients with 1,295 stents), the pooled sensitivity of CT was 94% and the specificity was 92%. In six studies using 64-row or greater CT, the pooled sensitivity of CT was 94% and specificity of CT was 94%. However, the difference compared with all 11 patient-level studies was not significant.
They also looked at the influence of stent size on CT accuracy in eight studies with 1,246 stents. Sensitivity was 81% for stents less than 3 mm and 92% for stents at least 3 mm in size. Specificity was 84% for stents less than 3 mm and 98% for stents at least 3 mm in size.
"In other words, the type of stent and the characteristics that the patient brings with him or her is much more important than the type of scanner that you have sitting there," said Dr. Marc Dewey of Charité – Universitätsmedizin Berlin. The findings were presented at the annual meeting of the Society of Cardiovascular Computed Tomography.
The researchers included prospective studies using at least 12-row CT scanners. Patients were assessed for 50% diameter in-stent restenosis as clinically relevant. All patients had to have coronary angiography.
The researchers included several databases: MEDLINE, EMBASE, ISI’s Web of Science (now Thomson Reuters Web of Knowledge) and the Cochrane Library. Search terms included "computed tomography," "coronary angiography," and "stent." Overall, they identified 33 studies with stent-level data.
Based on likelihood ratios, "we couldn’t conclude that CT was reliable in ruling in and ruling out coronary stent restenosis," said Dr. Dewey.
The investigators also looked at nondiagnostic studies. There were 30 studies with information on the stent level and 17 studies with information on the patient level. They used a missing data technique to assess for less-than-perfect reporting on the study level. The nondiagnostic rate on the patient level was 6% on average, based on the reported results, but the confidence intervals went up to more than 13%. "So almost every six or seven patients would be nondiagnostic."
"Coronary stent imaging by CT is slightly better using 64-row CT and above, though this was not significant. On the other hand, patients with stents that were at least 3 mm or larger could be significantly better assessed. Specificity in particular was significantly improved," said Dr. Dewey.
On the basis of these findings, CT should not be recommended for the assessment of coronary stent restenosis.
The study was funded by the German Research Foundation. The investigators did not report whether they have any significant conflicts of interest.
BALTIMORE – CT angiography is not accurate enough to assess in-stent restenosis, compared with invasive coronary angiography, based on the results of a meta-analysis.
In 11 studies with data on the patient level (804 patients with 1,295 stents), the pooled sensitivity of CT was 94% and the specificity was 92%. In six studies using 64-row or greater CT, the pooled sensitivity of CT was 94% and specificity of CT was 94%. However, the difference compared with all 11 patient-level studies was not significant.
They also looked at the influence of stent size on CT accuracy in eight studies with 1,246 stents. Sensitivity was 81% for stents less than 3 mm and 92% for stents at least 3 mm in size. Specificity was 84% for stents less than 3 mm and 98% for stents at least 3 mm in size.
"In other words, the type of stent and the characteristics that the patient brings with him or her is much more important than the type of scanner that you have sitting there," said Dr. Marc Dewey of Charité – Universitätsmedizin Berlin. The findings were presented at the annual meeting of the Society of Cardiovascular Computed Tomography.
The researchers included prospective studies using at least 12-row CT scanners. Patients were assessed for 50% diameter in-stent restenosis as clinically relevant. All patients had to have coronary angiography.
The researchers included several databases: MEDLINE, EMBASE, ISI’s Web of Science (now Thomson Reuters Web of Knowledge) and the Cochrane Library. Search terms included "computed tomography," "coronary angiography," and "stent." Overall, they identified 33 studies with stent-level data.
Based on likelihood ratios, "we couldn’t conclude that CT was reliable in ruling in and ruling out coronary stent restenosis," said Dr. Dewey.
The investigators also looked at nondiagnostic studies. There were 30 studies with information on the stent level and 17 studies with information on the patient level. They used a missing data technique to assess for less-than-perfect reporting on the study level. The nondiagnostic rate on the patient level was 6% on average, based on the reported results, but the confidence intervals went up to more than 13%. "So almost every six or seven patients would be nondiagnostic."
"Coronary stent imaging by CT is slightly better using 64-row CT and above, though this was not significant. On the other hand, patients with stents that were at least 3 mm or larger could be significantly better assessed. Specificity in particular was significantly improved," said Dr. Dewey.
On the basis of these findings, CT should not be recommended for the assessment of coronary stent restenosis.
The study was funded by the German Research Foundation. The investigators did not report whether they have any significant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SOCIETY OF CARDIOVASCULAR COMPUTED TOMOGRAPHY
Major Finding: In 11 studies with data on the patient level (804 patients with 1,295 stents), the pooled sensitivity of CT was 94% and the specificity was 92%, compared with coronary angiography. In six studies using 64-row or greater CT, the pooled sensitivity of CT was 94% and specificity of CT was 94%.
Data Source: A meta-analysis of 33 prospective studies in which at least 12-row CT scanners were used. Patients were assessed for 50% diameter in-stent restenosis as clinically relevant. All patients had to have coronary angiography.
Disclosures: The study was funded by the German Research Foundation. The investigators did not report whether they have any significant conflicts of interest.
Severe, Sharp Right Upper Quadrant and Epigastric Pain
Simultaneous Use of 2 C-Arm Devices Facilitates Percutaneous Treatment of Proximal Humerus Fractures
Cardiovascular CT Poised to Take Imaging Center Stage
New technologies that solve some old problems could make cardiovascular CT the go-to imaging tool to assess both anatomy and function.
Cardiovascular CT imaging has been a welcome tool in patient assessment due to its noninvasive nature, ease, and quickness. Likewise, cardiovascular CT angiography (CCTA) has provided noninvasive information about vessel stenoses, with lower costs and radiation exposure compared with invasive angiography.
Perhaps the biggest criticism about cardiovascular CT is that, while it provides very good anatomic detail, functional information – a crucial piece to the overall picture – is not discernable.
"Historically, coronary CT angiography has been an extremely anatomic method for documenting the severity of coronary artery stenoses or luminal compromise," said Dr. James K. Min, immediate past president of SCCT. This has left CTA open to the criticism that the more useful evaluation of coronary artery disease is not only to document high-grade stenoses – as with coronary CT angiography – but also to determine the physiologic significance of those stenoses.
However, at this year’s meeting of the Society of Cardiovascular Computed Tomography in Baltimore, "we saw the emergence of two robust methods for physiologic assessment of coronary disease by cardiac CT," he said. These are fractional flow reserve CT and CT-based myocardial perfusion imaging.
Evidence regarding these methods was then bolstered at the annual congress of the European Society of Cardiology in Munich, with the presentation of two imaging trials. The DeFACTO study, comparing CT-based FFR with FFR obtained by conventional angiography, did not show diagnostic superiority of CT-based FFR over angiography, but it did enhance diagnoses compared with CT without FFR. The CORE320 trial, assessing the diagnostic accuracy CT-based myocardial perfusion imaging in patients with suspected coronary artery disease, showed that CT-based myocardial perfusion imaging significantly increased the diagnostic accuracy of CTA alone to delineate flow-limiting disease.
Cardiovascular CT also has been hamstrung by a number of technical limitations. Calcium blooming artifacts make it difficult to get an accurate measurement of calcium lesion components and lumen size and motion artifacts also limit the clarity of CT images, leaving some vessels simply unreadable.
Two new technological advances – dual-energy CT and intelligent motion correction using snapshot freeze – are already changing practice, according to leaders at this year’s annual meeting of the SCCT.
CT Fractional Flow Reserve
Fractional flow reserve (FFR) is defined as the maximal blood flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. CT-based FFR relies on the use of some complicated math and modeling to calculate FFR from CT data and actually traces its roots back to the air flow modeling that goes into designing airplane wings.
All of the data needed can be gleaned from a single-phase static CT image. Geometry can be extracted from CCTA anatomic data. Boundary conditions can also be determined. Resting coronary blood flow can be calculated from myocardial mass. Mean blood pressure can be estimated from brachial artery pressure. Coronary microcirculatory resistance can be derived from morphometry data. Lastly, fluid properties include the viscosity and density of blood. "Putting it all together, we can come out with a calculated assessment of things like coronary flow and FFR ... now, we can do anatomy and function," said Dr. Matthew J. Budoff, director of cardiology at the University of California at Los Angeles School of Medicine in Torrance.
Until now, FFR was determined through invasive coronary angiography, which was the only method for specific determination of coronary artery lesions (lesion-specific ischemia). Values of 0.80 and lower or 0.75 and lower are considered diagnostic of lesion-specific ischemia. "It tells us whether there is a physiologic significance of the lesion," Dr. Budoff said.
At the same time, stenosis seen on CCTA has been an unreliable predictor of lesion-specific ischemia in trials. "Just seeing that anatomical stenosis doesn’t mean it’s functionally significant," said Dr. Budoff. CCTA results in a lot of false positives when it comes to physiologic significance.
FFR estimates throughout the entire coronary tree. "Because it relies on the entire coronary anatomy, it’s actually less sensitive to artifacts and less sensitive to things like calcification than individual segment assessment."
The first trial of FFR-CT was in the Diagnosis of Ischemia-Causing Stenoses Obtained via Noninvasive Fractional Flow Reserve (DISCOVER-FLOW) trial. In the study, the researchers compared the accuracy of CCTA with FFR-CT (invasive FFR served as the reference).
The results showed that the coronary stenoses that cause ischemia can be identified noninvasively with computer analysis of CCTA to construct FFR for specific lesions (Eur. Heart J. Cardiovasc. Imaging 2012 Jul 15 [doi: 10.1093/ehjci/jes130]).
The upshot of this study is that "when we think it’s a high-grade stenosis [with FFR-CT], it is a physiologically significant stenosis," Dr. Budoff said. "So we’ve dramatically improved the ability of CT to correlate with the most invasive and probably the most definitive way, currently, of assessing physiologic significance, and that’s FFR."
CT-based fractional flow reserve (FFR) is now a step closer to clinical use with the results of the Determination of FFR by Anatomic CT Angiography (DeFACTO) trial presented at the ESC meeting and simultaneously published (JAMA 2012 Aug. 26 [doi:10.1001/2012.jama.11274]). The addition of CT-based FFR information to CT alone improved diagnostic accuracy of stenoses, compared with invasive angiography and FFR.
"We’ve dramatically improved the ability of CT to correlate with ... FFR," said Dr. Matthew J. Budoff.
Although FFR-CT plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval, the per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone in all patients, in all vessels and also in vessels of intermediate stenosis severity," Dr. Min said during a press conference.
Myocardial Perfusion
"The second method of physiologic assessment of coronary disease, which is emerging, is myocardial perfusion imaging – performing a typical stress test with a CT angiogram," said Dr. Min.
This allows the visualization of perfusion/ischemia at specific lesions identified by CTA, providing functional and anatomic information. The data for perfusion images are extracted from a standard CTA scan.
With CT perfusion, a rest CT angiogram is performed to document the coronary artery stenoses that are within the coronary artery bed and also to look at the rest perfusion of the myocardium to determine whether it’s normal or abnormal, according to Dr. Min.
Before or after the rest CTA, a stress CT would be performed via pharmacologic means using a traditional 64-row cardiac CT.
It’s known that patients who have a normal SPECT myocardial perfusion examination have a very low rate of cardiovascular events over the next year, according to Dr. Richard T. George. "However, those patients with an abnormal nuclear scan actually have a quite high event rate over the next year."
In addition, it’s also known that CCTA has great prognostic value "and probably for a longer period than SPECT does, but SPECT myocardial perfusion imaging probably tells you more about the intermediate time period in the future about the event rate in the patient," he said.
Several studies have looked at the additional value of CT perfusion testing.
One of the first studies that compared CCTA and CT perfusion (CTP) with quantitative coronary angiography and SPECT perfusion showed a sensitivity with CTA/CTP of 88% and a specificity of 91% (Circ. Cardiovasc. Imaging 2009;2:174-82). "This study demonstrates some of the additional value of stress CT myocardial perfusion imaging," said Dr. George, assistant professor of medicine at the Heart and Vascular Institute at Johns Hopkins Hospital in Baltimore.
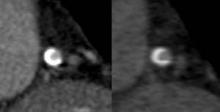
In another study, researchers assessed the additional value of dipyridamole stress myocardial perfusion by 64-row CT in patients with coronary stents (J. Cardiovasc. Comput. Tomogr. 2011;5:449-58). It is often difficult in many of these patients to assess whether in-stent restenosis is present, said Dr. George. The researchers in this study found that the addition of CT myocardial perfusion imaging to CCTA improved accuracy.
In a study targeting reversible ischemia, researchers assessed CT myocardial perfusion imaging with 320-row detector CT in 50 patients with an intermediate- to high-risk for CAD (Circ. Cardiovasc. Imaging 2012;5:333-40).
"The important part of this study is that they actually looked at reversible ischemia. A lot of our studies with CT perfusion imaging just lump all perfusion deficits together." In it, 40% of patients had an abnormal SPECT scan; 90% of those abnormal scans were reversible ischemia," said Dr. George.
In a per-patient analysis of CT perfusion imaging vs. CTA stenosis greater than 50% in the setting of a territorial SPECT myocardial perfusion deficit, sensitivity was 100% and specificity was 81%. The study shows the effectiveness of CT perfusion for assessing lesion-specific ischemia, Dr. George noted.
"What we’re finding is that CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing methods that we’ve used until this day," Dr. Min said.
"CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing method," said Dr. James K. Min.
In the Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320 Detector Computed Tomography (Core320) trial, researchers compared the diagnostic accuracy of CTA plus CT-based myocardial perfusion against ICA plus SPECT myocardial perfusion imaging in 381 patients with suspected or diagnosed coronary artery disease with a clinical indication for coronary angiography.
"When we add perfusion [to CTA alone] we gain power to diagnose flow-limiting stenosis," lead author Dr. Joao A.C. Lima said at the ESC meeting. Together, "they have the same power as invasive angiography and SPECT MPI in defining who are the patients who end up going through revascularization," he said.
The area under the receiver operating characteristic curve (ROC) – an effective method of evaluating the performance of diagnostic tests – was 0.79 for CTA-CTP and 0.81 for ICA-SPECT.
"At this point, the [CT perfusion] technology could be used precisely to find the patients who have flow-limiting disease and, therefore, are going to need revascularization," said Dr. Lima, director of cardiovascular imaging at the Johns Hopkins University in Baltimore.
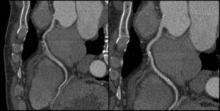
Dual-Energy CT
Dual-energy CT (also known as dual-source CT) "interleaves sets of high- and low-keV images. The energy alternates between two energies (80 keV to 140 keV) every 0.5 msec," said Dr. James P. Earls. The result is two competing sets that can be used simultaneously. The importance of this dual-energy approach is that with higher energies and a software algorithm, calcium blooming is decreased. This means a more accurate size of calcium in lesions and lumen size.
Back-end software produces a range of monochromatic images (images at a single energy). "In terms of calcium reduction, the monochromatic images are probably more important," said Dr. Earls, codirector of the cardiac CT program at Inova Heart and Vascular Institute in Falls Church, Va.
Monochromatic images range from 40 keV to 140 keV. "At 40 keV you’re very close to the k-edge of iodine, so you have significant attenuation of anything that is enhancing ... at about 75 keV you have something that looks akin to a 120-keV image that we would normally get." As the energy increases, "you get away from what we would do on a routine clinical basis."
The ATLANTA I study (Assessment of Tissue Characteristics, Lesion Morphology, and Hemodynamics by Angiography With Fractional Flow Reserve, Intravascular Ultrasound and Virtual Histology, and Noninvasive Computed Tomography in Atherosclerotic Plaques) showed that with conventional single-energy CT calcium, plaque is overestimated and lumen size is therefore underestimated (J. Am. Coll. Cardiol. Intv. 2011;4:198-208 [doi:10.1016/j.jcin.2010.10.008]).
The ATLANTA I study tells us that "when we do routine single-energy CT, calcium plaques are significantly overportrayed." In this study, researchers found that calcified plaque volume is 104% greater than its true volume as determined by intravascular ultrasound. As a result, the minimal luminal diameter is underestimated by 21% and the percentage diameter stenosis is overrepresented by 39%. "Lots of false positives [are] caused by calcified plaque in the area," Dr. Earls observed.
The reason for this is that as energy increases, the calcium blooming decreases. This accounts for the enlargement of the lumen.
Noncalcified plaques don’t show as dramatic an effect, though. Soft plaque size does not change much when seen at different energies, Dr. Earls noted. "Ultimately it may be that we use a combination of monochromatic images and material density images, as we approach this going forward. These are both available every time that you do a scan," said Dr. Earls.
Dual-source CT does have limitations, though. There is no retrospective gating; there are limited milliAmpere (electrical charge) presets, and there is no high-resolution mode.
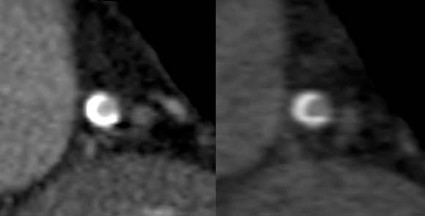
Intelligent Motion Correction
Motion artifacts make it difficult or impossible to evaluate vessels, leaving clinicians to treat the vessels as narrowed by default. A new technology is designed to overcome the problem of motion artifacts in cardiovascular CT.
"The images are acquired in a standard fashion, but instead of reconstructing them in a standard fashion, there is integration of this intelligent motion correction that tracks the motion of the vessel over two or three phases of the cardiac cycle," Dr. Jonathon A. Leipsic said in an interview. "When we acquire the study, we get a couple of phases beyond just the minimal acquisition – which is standard. It sees where the vessel is over a couple of phases and how it looks. Based on the known velocity of the artery, how it appears, and the patient’s known heart rate, [the algorithm] then corrects for the expected motion."
The technology is already changing practice. It is used on Europe and Japan; it is also being used in many centers in the United States. The motion correction algorithm has wide range of applications. "Anywhere there is motion, anyone with a sudden ectopic pace or premature ventricular contraction, anyone with an arrhythmia – all of those patients will benefit from this motion correction," said Dr. Leipsic, chairman of the department of radiology for Providence Health Care and vice chairman of research for the department of radiology at the University of British Columbia, Vancouver.
Importantly, the scan time and radiation dose don’t increase appreciably with the acquisition of vessel velocity data. "It doesn’t change the acquisition. You can just wait and see. If you have a study that has no motion, then you don’t need to use [motion correction]. But if you have a study with motion, then you can use it. You can make that choice after you see the initial data," Dr. Leipsic explained.
Dr. Leipsic was the lead author on one of the first studies to assess the accuracy this of this method (J. Cardiovasc. Comput. Tomography 2012;6:164-71. Epub 2012 Apr 6). In the study, "we looked at a population of convenience patients that happened to be going to the cath lab. We chose very difficult patients – patients undergoing transcatheter valve replacement – who have very high heart rates. We saw a significant improvement in interpretability, overall image quality, and diagnostic accuracy" with this technology. The researchers also noted significant improvements in right coronary evaluation, as well as other coronary territories.
Some have argued that all that is needed to avoid motion artifacts is to rate-control patients. However, "we aggressively rate-controlled patients ... there’s just too much motion," Dr. Leipsic countered. "It’s hard to anticipate some problems – an irregular beat or some irregular rhythm – and having this in your back pocket ... has exciting potential."
Additional trials to assess accuracy are expected, perhaps most prominently the VICTORY trial (Validation of an Intracycle CT Motion Correction Algorithm for Diagnostic Accuracy: A Prospective Multicenter Study). In the study, CCTA will be compared with invasive coronary angiography (ICA) for diagnostic sensitivity and specificity, positive predictive value, negative predictive value, diagnostic accuracy, and positive and negative likelihood ratios.
Coronary segments will be assessed for "significance" of coronary artery luminal diameter obstruction. Individual segments will be graded based on image quality, with the third reader used to achieve consensus. Dr. Leipsic and Dr. James Min are the principal investigators for the study.
For now, the intelligent motion correction algorithm, called SnapShot Freez4e, is available only from GE Healthcare, as part of its Discovery CT750 HD FREEdom Edition, which was granted 510(k) clearance in June. "I think that other companies are going to come up with something similar but I think that each type will be adequately different enough that [these technologies] will require their own validation studies," said Dr. Leipsic.
Siemens is reportedly developing a similar technology.
Dr. Min is a speaker for GE Healthcare. Dr. Budoff receives grant support from HeartFlow. Dr. George has received research support from Toshiba Medical Systems and GE Healthcare, is on the advisory board of GE Healthcare, and is a consultant to ICON Medical Imaging. Dr. Earls is on the speakers bureau for and has research funded by GE Healthcare. Dr. Leipsic is a consultant/speaker for Edwards Lifesciences and GE Healthcare.
New technologies that solve some old problems could make cardiovascular CT the go-to imaging tool to assess both anatomy and function.
Cardiovascular CT imaging has been a welcome tool in patient assessment due to its noninvasive nature, ease, and quickness. Likewise, cardiovascular CT angiography (CCTA) has provided noninvasive information about vessel stenoses, with lower costs and radiation exposure compared with invasive angiography.
Perhaps the biggest criticism about cardiovascular CT is that, while it provides very good anatomic detail, functional information – a crucial piece to the overall picture – is not discernable.
"Historically, coronary CT angiography has been an extremely anatomic method for documenting the severity of coronary artery stenoses or luminal compromise," said Dr. James K. Min, immediate past president of SCCT. This has left CTA open to the criticism that the more useful evaluation of coronary artery disease is not only to document high-grade stenoses – as with coronary CT angiography – but also to determine the physiologic significance of those stenoses.
However, at this year’s meeting of the Society of Cardiovascular Computed Tomography in Baltimore, "we saw the emergence of two robust methods for physiologic assessment of coronary disease by cardiac CT," he said. These are fractional flow reserve CT and CT-based myocardial perfusion imaging.
Evidence regarding these methods was then bolstered at the annual congress of the European Society of Cardiology in Munich, with the presentation of two imaging trials. The DeFACTO study, comparing CT-based FFR with FFR obtained by conventional angiography, did not show diagnostic superiority of CT-based FFR over angiography, but it did enhance diagnoses compared with CT without FFR. The CORE320 trial, assessing the diagnostic accuracy CT-based myocardial perfusion imaging in patients with suspected coronary artery disease, showed that CT-based myocardial perfusion imaging significantly increased the diagnostic accuracy of CTA alone to delineate flow-limiting disease.
Cardiovascular CT also has been hamstrung by a number of technical limitations. Calcium blooming artifacts make it difficult to get an accurate measurement of calcium lesion components and lumen size and motion artifacts also limit the clarity of CT images, leaving some vessels simply unreadable.
Two new technological advances – dual-energy CT and intelligent motion correction using snapshot freeze – are already changing practice, according to leaders at this year’s annual meeting of the SCCT.
CT Fractional Flow Reserve
Fractional flow reserve (FFR) is defined as the maximal blood flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. CT-based FFR relies on the use of some complicated math and modeling to calculate FFR from CT data and actually traces its roots back to the air flow modeling that goes into designing airplane wings.
All of the data needed can be gleaned from a single-phase static CT image. Geometry can be extracted from CCTA anatomic data. Boundary conditions can also be determined. Resting coronary blood flow can be calculated from myocardial mass. Mean blood pressure can be estimated from brachial artery pressure. Coronary microcirculatory resistance can be derived from morphometry data. Lastly, fluid properties include the viscosity and density of blood. "Putting it all together, we can come out with a calculated assessment of things like coronary flow and FFR ... now, we can do anatomy and function," said Dr. Matthew J. Budoff, director of cardiology at the University of California at Los Angeles School of Medicine in Torrance.
Until now, FFR was determined through invasive coronary angiography, which was the only method for specific determination of coronary artery lesions (lesion-specific ischemia). Values of 0.80 and lower or 0.75 and lower are considered diagnostic of lesion-specific ischemia. "It tells us whether there is a physiologic significance of the lesion," Dr. Budoff said.
At the same time, stenosis seen on CCTA has been an unreliable predictor of lesion-specific ischemia in trials. "Just seeing that anatomical stenosis doesn’t mean it’s functionally significant," said Dr. Budoff. CCTA results in a lot of false positives when it comes to physiologic significance.
FFR estimates throughout the entire coronary tree. "Because it relies on the entire coronary anatomy, it’s actually less sensitive to artifacts and less sensitive to things like calcification than individual segment assessment."
The first trial of FFR-CT was in the Diagnosis of Ischemia-Causing Stenoses Obtained via Noninvasive Fractional Flow Reserve (DISCOVER-FLOW) trial. In the study, the researchers compared the accuracy of CCTA with FFR-CT (invasive FFR served as the reference).
The results showed that the coronary stenoses that cause ischemia can be identified noninvasively with computer analysis of CCTA to construct FFR for specific lesions (Eur. Heart J. Cardiovasc. Imaging 2012 Jul 15 [doi: 10.1093/ehjci/jes130]).
The upshot of this study is that "when we think it’s a high-grade stenosis [with FFR-CT], it is a physiologically significant stenosis," Dr. Budoff said. "So we’ve dramatically improved the ability of CT to correlate with the most invasive and probably the most definitive way, currently, of assessing physiologic significance, and that’s FFR."
CT-based fractional flow reserve (FFR) is now a step closer to clinical use with the results of the Determination of FFR by Anatomic CT Angiography (DeFACTO) trial presented at the ESC meeting and simultaneously published (JAMA 2012 Aug. 26 [doi:10.1001/2012.jama.11274]). The addition of CT-based FFR information to CT alone improved diagnostic accuracy of stenoses, compared with invasive angiography and FFR.
"We’ve dramatically improved the ability of CT to correlate with ... FFR," said Dr. Matthew J. Budoff.
Although FFR-CT plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval, the per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone in all patients, in all vessels and also in vessels of intermediate stenosis severity," Dr. Min said during a press conference.
Myocardial Perfusion
"The second method of physiologic assessment of coronary disease, which is emerging, is myocardial perfusion imaging – performing a typical stress test with a CT angiogram," said Dr. Min.
This allows the visualization of perfusion/ischemia at specific lesions identified by CTA, providing functional and anatomic information. The data for perfusion images are extracted from a standard CTA scan.
With CT perfusion, a rest CT angiogram is performed to document the coronary artery stenoses that are within the coronary artery bed and also to look at the rest perfusion of the myocardium to determine whether it’s normal or abnormal, according to Dr. Min.
Before or after the rest CTA, a stress CT would be performed via pharmacologic means using a traditional 64-row cardiac CT.
It’s known that patients who have a normal SPECT myocardial perfusion examination have a very low rate of cardiovascular events over the next year, according to Dr. Richard T. George. "However, those patients with an abnormal nuclear scan actually have a quite high event rate over the next year."
In addition, it’s also known that CCTA has great prognostic value "and probably for a longer period than SPECT does, but SPECT myocardial perfusion imaging probably tells you more about the intermediate time period in the future about the event rate in the patient," he said.
Several studies have looked at the additional value of CT perfusion testing.
One of the first studies that compared CCTA and CT perfusion (CTP) with quantitative coronary angiography and SPECT perfusion showed a sensitivity with CTA/CTP of 88% and a specificity of 91% (Circ. Cardiovasc. Imaging 2009;2:174-82). "This study demonstrates some of the additional value of stress CT myocardial perfusion imaging," said Dr. George, assistant professor of medicine at the Heart and Vascular Institute at Johns Hopkins Hospital in Baltimore.
In another study, researchers assessed the additional value of dipyridamole stress myocardial perfusion by 64-row CT in patients with coronary stents (J. Cardiovasc. Comput. Tomogr. 2011;5:449-58). It is often difficult in many of these patients to assess whether in-stent restenosis is present, said Dr. George. The researchers in this study found that the addition of CT myocardial perfusion imaging to CCTA improved accuracy.
In a study targeting reversible ischemia, researchers assessed CT myocardial perfusion imaging with 320-row detector CT in 50 patients with an intermediate- to high-risk for CAD (Circ. Cardiovasc. Imaging 2012;5:333-40).
"The important part of this study is that they actually looked at reversible ischemia. A lot of our studies with CT perfusion imaging just lump all perfusion deficits together." In it, 40% of patients had an abnormal SPECT scan; 90% of those abnormal scans were reversible ischemia," said Dr. George.
In a per-patient analysis of CT perfusion imaging vs. CTA stenosis greater than 50% in the setting of a territorial SPECT myocardial perfusion deficit, sensitivity was 100% and specificity was 81%. The study shows the effectiveness of CT perfusion for assessing lesion-specific ischemia, Dr. George noted.
"What we’re finding is that CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing methods that we’ve used until this day," Dr. Min said.
"CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing method," said Dr. James K. Min.
In the Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320 Detector Computed Tomography (Core320) trial, researchers compared the diagnostic accuracy of CTA plus CT-based myocardial perfusion against ICA plus SPECT myocardial perfusion imaging in 381 patients with suspected or diagnosed coronary artery disease with a clinical indication for coronary angiography.
"When we add perfusion [to CTA alone] we gain power to diagnose flow-limiting stenosis," lead author Dr. Joao A.C. Lima said at the ESC meeting. Together, "they have the same power as invasive angiography and SPECT MPI in defining who are the patients who end up going through revascularization," he said.
The area under the receiver operating characteristic curve (ROC) – an effective method of evaluating the performance of diagnostic tests – was 0.79 for CTA-CTP and 0.81 for ICA-SPECT.
"At this point, the [CT perfusion] technology could be used precisely to find the patients who have flow-limiting disease and, therefore, are going to need revascularization," said Dr. Lima, director of cardiovascular imaging at the Johns Hopkins University in Baltimore.
Dual-Energy CT
Dual-energy CT (also known as dual-source CT) "interleaves sets of high- and low-keV images. The energy alternates between two energies (80 keV to 140 keV) every 0.5 msec," said Dr. James P. Earls. The result is two competing sets that can be used simultaneously. The importance of this dual-energy approach is that with higher energies and a software algorithm, calcium blooming is decreased. This means a more accurate size of calcium in lesions and lumen size.
Back-end software produces a range of monochromatic images (images at a single energy). "In terms of calcium reduction, the monochromatic images are probably more important," said Dr. Earls, codirector of the cardiac CT program at Inova Heart and Vascular Institute in Falls Church, Va.
Monochromatic images range from 40 keV to 140 keV. "At 40 keV you’re very close to the k-edge of iodine, so you have significant attenuation of anything that is enhancing ... at about 75 keV you have something that looks akin to a 120-keV image that we would normally get." As the energy increases, "you get away from what we would do on a routine clinical basis."
The ATLANTA I study (Assessment of Tissue Characteristics, Lesion Morphology, and Hemodynamics by Angiography With Fractional Flow Reserve, Intravascular Ultrasound and Virtual Histology, and Noninvasive Computed Tomography in Atherosclerotic Plaques) showed that with conventional single-energy CT calcium, plaque is overestimated and lumen size is therefore underestimated (J. Am. Coll. Cardiol. Intv. 2011;4:198-208 [doi:10.1016/j.jcin.2010.10.008]).
The ATLANTA I study tells us that "when we do routine single-energy CT, calcium plaques are significantly overportrayed." In this study, researchers found that calcified plaque volume is 104% greater than its true volume as determined by intravascular ultrasound. As a result, the minimal luminal diameter is underestimated by 21% and the percentage diameter stenosis is overrepresented by 39%. "Lots of false positives [are] caused by calcified plaque in the area," Dr. Earls observed.
The reason for this is that as energy increases, the calcium blooming decreases. This accounts for the enlargement of the lumen.
Noncalcified plaques don’t show as dramatic an effect, though. Soft plaque size does not change much when seen at different energies, Dr. Earls noted. "Ultimately it may be that we use a combination of monochromatic images and material density images, as we approach this going forward. These are both available every time that you do a scan," said Dr. Earls.
Dual-source CT does have limitations, though. There is no retrospective gating; there are limited milliAmpere (electrical charge) presets, and there is no high-resolution mode.
Intelligent Motion Correction
Motion artifacts make it difficult or impossible to evaluate vessels, leaving clinicians to treat the vessels as narrowed by default. A new technology is designed to overcome the problem of motion artifacts in cardiovascular CT.
"The images are acquired in a standard fashion, but instead of reconstructing them in a standard fashion, there is integration of this intelligent motion correction that tracks the motion of the vessel over two or three phases of the cardiac cycle," Dr. Jonathon A. Leipsic said in an interview. "When we acquire the study, we get a couple of phases beyond just the minimal acquisition – which is standard. It sees where the vessel is over a couple of phases and how it looks. Based on the known velocity of the artery, how it appears, and the patient’s known heart rate, [the algorithm] then corrects for the expected motion."
The technology is already changing practice. It is used on Europe and Japan; it is also being used in many centers in the United States. The motion correction algorithm has wide range of applications. "Anywhere there is motion, anyone with a sudden ectopic pace or premature ventricular contraction, anyone with an arrhythmia – all of those patients will benefit from this motion correction," said Dr. Leipsic, chairman of the department of radiology for Providence Health Care and vice chairman of research for the department of radiology at the University of British Columbia, Vancouver.
Importantly, the scan time and radiation dose don’t increase appreciably with the acquisition of vessel velocity data. "It doesn’t change the acquisition. You can just wait and see. If you have a study that has no motion, then you don’t need to use [motion correction]. But if you have a study with motion, then you can use it. You can make that choice after you see the initial data," Dr. Leipsic explained.
Dr. Leipsic was the lead author on one of the first studies to assess the accuracy this of this method (J. Cardiovasc. Comput. Tomography 2012;6:164-71. Epub 2012 Apr 6). In the study, "we looked at a population of convenience patients that happened to be going to the cath lab. We chose very difficult patients – patients undergoing transcatheter valve replacement – who have very high heart rates. We saw a significant improvement in interpretability, overall image quality, and diagnostic accuracy" with this technology. The researchers also noted significant improvements in right coronary evaluation, as well as other coronary territories.
Some have argued that all that is needed to avoid motion artifacts is to rate-control patients. However, "we aggressively rate-controlled patients ... there’s just too much motion," Dr. Leipsic countered. "It’s hard to anticipate some problems – an irregular beat or some irregular rhythm – and having this in your back pocket ... has exciting potential."
Additional trials to assess accuracy are expected, perhaps most prominently the VICTORY trial (Validation of an Intracycle CT Motion Correction Algorithm for Diagnostic Accuracy: A Prospective Multicenter Study). In the study, CCTA will be compared with invasive coronary angiography (ICA) for diagnostic sensitivity and specificity, positive predictive value, negative predictive value, diagnostic accuracy, and positive and negative likelihood ratios.
Coronary segments will be assessed for "significance" of coronary artery luminal diameter obstruction. Individual segments will be graded based on image quality, with the third reader used to achieve consensus. Dr. Leipsic and Dr. James Min are the principal investigators for the study.
For now, the intelligent motion correction algorithm, called SnapShot Freez4e, is available only from GE Healthcare, as part of its Discovery CT750 HD FREEdom Edition, which was granted 510(k) clearance in June. "I think that other companies are going to come up with something similar but I think that each type will be adequately different enough that [these technologies] will require their own validation studies," said Dr. Leipsic.
Siemens is reportedly developing a similar technology.
Dr. Min is a speaker for GE Healthcare. Dr. Budoff receives grant support from HeartFlow. Dr. George has received research support from Toshiba Medical Systems and GE Healthcare, is on the advisory board of GE Healthcare, and is a consultant to ICON Medical Imaging. Dr. Earls is on the speakers bureau for and has research funded by GE Healthcare. Dr. Leipsic is a consultant/speaker for Edwards Lifesciences and GE Healthcare.
New technologies that solve some old problems could make cardiovascular CT the go-to imaging tool to assess both anatomy and function.
Cardiovascular CT imaging has been a welcome tool in patient assessment due to its noninvasive nature, ease, and quickness. Likewise, cardiovascular CT angiography (CCTA) has provided noninvasive information about vessel stenoses, with lower costs and radiation exposure compared with invasive angiography.
Perhaps the biggest criticism about cardiovascular CT is that, while it provides very good anatomic detail, functional information – a crucial piece to the overall picture – is not discernable.
"Historically, coronary CT angiography has been an extremely anatomic method for documenting the severity of coronary artery stenoses or luminal compromise," said Dr. James K. Min, immediate past president of SCCT. This has left CTA open to the criticism that the more useful evaluation of coronary artery disease is not only to document high-grade stenoses – as with coronary CT angiography – but also to determine the physiologic significance of those stenoses.
However, at this year’s meeting of the Society of Cardiovascular Computed Tomography in Baltimore, "we saw the emergence of two robust methods for physiologic assessment of coronary disease by cardiac CT," he said. These are fractional flow reserve CT and CT-based myocardial perfusion imaging.
Evidence regarding these methods was then bolstered at the annual congress of the European Society of Cardiology in Munich, with the presentation of two imaging trials. The DeFACTO study, comparing CT-based FFR with FFR obtained by conventional angiography, did not show diagnostic superiority of CT-based FFR over angiography, but it did enhance diagnoses compared with CT without FFR. The CORE320 trial, assessing the diagnostic accuracy CT-based myocardial perfusion imaging in patients with suspected coronary artery disease, showed that CT-based myocardial perfusion imaging significantly increased the diagnostic accuracy of CTA alone to delineate flow-limiting disease.
Cardiovascular CT also has been hamstrung by a number of technical limitations. Calcium blooming artifacts make it difficult to get an accurate measurement of calcium lesion components and lumen size and motion artifacts also limit the clarity of CT images, leaving some vessels simply unreadable.
Two new technological advances – dual-energy CT and intelligent motion correction using snapshot freeze – are already changing practice, according to leaders at this year’s annual meeting of the SCCT.
CT Fractional Flow Reserve
Fractional flow reserve (FFR) is defined as the maximal blood flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. CT-based FFR relies on the use of some complicated math and modeling to calculate FFR from CT data and actually traces its roots back to the air flow modeling that goes into designing airplane wings.
All of the data needed can be gleaned from a single-phase static CT image. Geometry can be extracted from CCTA anatomic data. Boundary conditions can also be determined. Resting coronary blood flow can be calculated from myocardial mass. Mean blood pressure can be estimated from brachial artery pressure. Coronary microcirculatory resistance can be derived from morphometry data. Lastly, fluid properties include the viscosity and density of blood. "Putting it all together, we can come out with a calculated assessment of things like coronary flow and FFR ... now, we can do anatomy and function," said Dr. Matthew J. Budoff, director of cardiology at the University of California at Los Angeles School of Medicine in Torrance.
Until now, FFR was determined through invasive coronary angiography, which was the only method for specific determination of coronary artery lesions (lesion-specific ischemia). Values of 0.80 and lower or 0.75 and lower are considered diagnostic of lesion-specific ischemia. "It tells us whether there is a physiologic significance of the lesion," Dr. Budoff said.
At the same time, stenosis seen on CCTA has been an unreliable predictor of lesion-specific ischemia in trials. "Just seeing that anatomical stenosis doesn’t mean it’s functionally significant," said Dr. Budoff. CCTA results in a lot of false positives when it comes to physiologic significance.
FFR estimates throughout the entire coronary tree. "Because it relies on the entire coronary anatomy, it’s actually less sensitive to artifacts and less sensitive to things like calcification than individual segment assessment."
The first trial of FFR-CT was in the Diagnosis of Ischemia-Causing Stenoses Obtained via Noninvasive Fractional Flow Reserve (DISCOVER-FLOW) trial. In the study, the researchers compared the accuracy of CCTA with FFR-CT (invasive FFR served as the reference).
The results showed that the coronary stenoses that cause ischemia can be identified noninvasively with computer analysis of CCTA to construct FFR for specific lesions (Eur. Heart J. Cardiovasc. Imaging 2012 Jul 15 [doi: 10.1093/ehjci/jes130]).
The upshot of this study is that "when we think it’s a high-grade stenosis [with FFR-CT], it is a physiologically significant stenosis," Dr. Budoff said. "So we’ve dramatically improved the ability of CT to correlate with the most invasive and probably the most definitive way, currently, of assessing physiologic significance, and that’s FFR."
CT-based fractional flow reserve (FFR) is now a step closer to clinical use with the results of the Determination of FFR by Anatomic CT Angiography (DeFACTO) trial presented at the ESC meeting and simultaneously published (JAMA 2012 Aug. 26 [doi:10.1001/2012.jama.11274]). The addition of CT-based FFR information to CT alone improved diagnostic accuracy of stenoses, compared with invasive angiography and FFR.
"We’ve dramatically improved the ability of CT to correlate with ... FFR," said Dr. Matthew J. Budoff.
Although FFR-CT plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval, the per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone in all patients, in all vessels and also in vessels of intermediate stenosis severity," Dr. Min said during a press conference.
Myocardial Perfusion
"The second method of physiologic assessment of coronary disease, which is emerging, is myocardial perfusion imaging – performing a typical stress test with a CT angiogram," said Dr. Min.
This allows the visualization of perfusion/ischemia at specific lesions identified by CTA, providing functional and anatomic information. The data for perfusion images are extracted from a standard CTA scan.
With CT perfusion, a rest CT angiogram is performed to document the coronary artery stenoses that are within the coronary artery bed and also to look at the rest perfusion of the myocardium to determine whether it’s normal or abnormal, according to Dr. Min.
Before or after the rest CTA, a stress CT would be performed via pharmacologic means using a traditional 64-row cardiac CT.
It’s known that patients who have a normal SPECT myocardial perfusion examination have a very low rate of cardiovascular events over the next year, according to Dr. Richard T. George. "However, those patients with an abnormal nuclear scan actually have a quite high event rate over the next year."
In addition, it’s also known that CCTA has great prognostic value "and probably for a longer period than SPECT does, but SPECT myocardial perfusion imaging probably tells you more about the intermediate time period in the future about the event rate in the patient," he said.
Several studies have looked at the additional value of CT perfusion testing.
One of the first studies that compared CCTA and CT perfusion (CTP) with quantitative coronary angiography and SPECT perfusion showed a sensitivity with CTA/CTP of 88% and a specificity of 91% (Circ. Cardiovasc. Imaging 2009;2:174-82). "This study demonstrates some of the additional value of stress CT myocardial perfusion imaging," said Dr. George, assistant professor of medicine at the Heart and Vascular Institute at Johns Hopkins Hospital in Baltimore.
In another study, researchers assessed the additional value of dipyridamole stress myocardial perfusion by 64-row CT in patients with coronary stents (J. Cardiovasc. Comput. Tomogr. 2011;5:449-58). It is often difficult in many of these patients to assess whether in-stent restenosis is present, said Dr. George. The researchers in this study found that the addition of CT myocardial perfusion imaging to CCTA improved accuracy.
In a study targeting reversible ischemia, researchers assessed CT myocardial perfusion imaging with 320-row detector CT in 50 patients with an intermediate- to high-risk for CAD (Circ. Cardiovasc. Imaging 2012;5:333-40).
"The important part of this study is that they actually looked at reversible ischemia. A lot of our studies with CT perfusion imaging just lump all perfusion deficits together." In it, 40% of patients had an abnormal SPECT scan; 90% of those abnormal scans were reversible ischemia," said Dr. George.
In a per-patient analysis of CT perfusion imaging vs. CTA stenosis greater than 50% in the setting of a territorial SPECT myocardial perfusion deficit, sensitivity was 100% and specificity was 81%. The study shows the effectiveness of CT perfusion for assessing lesion-specific ischemia, Dr. George noted.
"What we’re finding is that CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing methods that we’ve used until this day," Dr. Min said.
"CT perfusion or stress testing with CT can be as accurate, if not more accurate, than the conventional stress testing method," said Dr. James K. Min.
In the Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320 Detector Computed Tomography (Core320) trial, researchers compared the diagnostic accuracy of CTA plus CT-based myocardial perfusion against ICA plus SPECT myocardial perfusion imaging in 381 patients with suspected or diagnosed coronary artery disease with a clinical indication for coronary angiography.
"When we add perfusion [to CTA alone] we gain power to diagnose flow-limiting stenosis," lead author Dr. Joao A.C. Lima said at the ESC meeting. Together, "they have the same power as invasive angiography and SPECT MPI in defining who are the patients who end up going through revascularization," he said.
The area under the receiver operating characteristic curve (ROC) – an effective method of evaluating the performance of diagnostic tests – was 0.79 for CTA-CTP and 0.81 for ICA-SPECT.
"At this point, the [CT perfusion] technology could be used precisely to find the patients who have flow-limiting disease and, therefore, are going to need revascularization," said Dr. Lima, director of cardiovascular imaging at the Johns Hopkins University in Baltimore.
Dual-Energy CT
Dual-energy CT (also known as dual-source CT) "interleaves sets of high- and low-keV images. The energy alternates between two energies (80 keV to 140 keV) every 0.5 msec," said Dr. James P. Earls. The result is two competing sets that can be used simultaneously. The importance of this dual-energy approach is that with higher energies and a software algorithm, calcium blooming is decreased. This means a more accurate size of calcium in lesions and lumen size.
Back-end software produces a range of monochromatic images (images at a single energy). "In terms of calcium reduction, the monochromatic images are probably more important," said Dr. Earls, codirector of the cardiac CT program at Inova Heart and Vascular Institute in Falls Church, Va.
Monochromatic images range from 40 keV to 140 keV. "At 40 keV you’re very close to the k-edge of iodine, so you have significant attenuation of anything that is enhancing ... at about 75 keV you have something that looks akin to a 120-keV image that we would normally get." As the energy increases, "you get away from what we would do on a routine clinical basis."
The ATLANTA I study (Assessment of Tissue Characteristics, Lesion Morphology, and Hemodynamics by Angiography With Fractional Flow Reserve, Intravascular Ultrasound and Virtual Histology, and Noninvasive Computed Tomography in Atherosclerotic Plaques) showed that with conventional single-energy CT calcium, plaque is overestimated and lumen size is therefore underestimated (J. Am. Coll. Cardiol. Intv. 2011;4:198-208 [doi:10.1016/j.jcin.2010.10.008]).
The ATLANTA I study tells us that "when we do routine single-energy CT, calcium plaques are significantly overportrayed." In this study, researchers found that calcified plaque volume is 104% greater than its true volume as determined by intravascular ultrasound. As a result, the minimal luminal diameter is underestimated by 21% and the percentage diameter stenosis is overrepresented by 39%. "Lots of false positives [are] caused by calcified plaque in the area," Dr. Earls observed.
The reason for this is that as energy increases, the calcium blooming decreases. This accounts for the enlargement of the lumen.
Noncalcified plaques don’t show as dramatic an effect, though. Soft plaque size does not change much when seen at different energies, Dr. Earls noted. "Ultimately it may be that we use a combination of monochromatic images and material density images, as we approach this going forward. These are both available every time that you do a scan," said Dr. Earls.
Dual-source CT does have limitations, though. There is no retrospective gating; there are limited milliAmpere (electrical charge) presets, and there is no high-resolution mode.
Intelligent Motion Correction
Motion artifacts make it difficult or impossible to evaluate vessels, leaving clinicians to treat the vessels as narrowed by default. A new technology is designed to overcome the problem of motion artifacts in cardiovascular CT.
"The images are acquired in a standard fashion, but instead of reconstructing them in a standard fashion, there is integration of this intelligent motion correction that tracks the motion of the vessel over two or three phases of the cardiac cycle," Dr. Jonathon A. Leipsic said in an interview. "When we acquire the study, we get a couple of phases beyond just the minimal acquisition – which is standard. It sees where the vessel is over a couple of phases and how it looks. Based on the known velocity of the artery, how it appears, and the patient’s known heart rate, [the algorithm] then corrects for the expected motion."
The technology is already changing practice. It is used on Europe and Japan; it is also being used in many centers in the United States. The motion correction algorithm has wide range of applications. "Anywhere there is motion, anyone with a sudden ectopic pace or premature ventricular contraction, anyone with an arrhythmia – all of those patients will benefit from this motion correction," said Dr. Leipsic, chairman of the department of radiology for Providence Health Care and vice chairman of research for the department of radiology at the University of British Columbia, Vancouver.
Importantly, the scan time and radiation dose don’t increase appreciably with the acquisition of vessel velocity data. "It doesn’t change the acquisition. You can just wait and see. If you have a study that has no motion, then you don’t need to use [motion correction]. But if you have a study with motion, then you can use it. You can make that choice after you see the initial data," Dr. Leipsic explained.
Dr. Leipsic was the lead author on one of the first studies to assess the accuracy this of this method (J. Cardiovasc. Comput. Tomography 2012;6:164-71. Epub 2012 Apr 6). In the study, "we looked at a population of convenience patients that happened to be going to the cath lab. We chose very difficult patients – patients undergoing transcatheter valve replacement – who have very high heart rates. We saw a significant improvement in interpretability, overall image quality, and diagnostic accuracy" with this technology. The researchers also noted significant improvements in right coronary evaluation, as well as other coronary territories.
Some have argued that all that is needed to avoid motion artifacts is to rate-control patients. However, "we aggressively rate-controlled patients ... there’s just too much motion," Dr. Leipsic countered. "It’s hard to anticipate some problems – an irregular beat or some irregular rhythm – and having this in your back pocket ... has exciting potential."
Additional trials to assess accuracy are expected, perhaps most prominently the VICTORY trial (Validation of an Intracycle CT Motion Correction Algorithm for Diagnostic Accuracy: A Prospective Multicenter Study). In the study, CCTA will be compared with invasive coronary angiography (ICA) for diagnostic sensitivity and specificity, positive predictive value, negative predictive value, diagnostic accuracy, and positive and negative likelihood ratios.
Coronary segments will be assessed for "significance" of coronary artery luminal diameter obstruction. Individual segments will be graded based on image quality, with the third reader used to achieve consensus. Dr. Leipsic and Dr. James Min are the principal investigators for the study.
For now, the intelligent motion correction algorithm, called SnapShot Freez4e, is available only from GE Healthcare, as part of its Discovery CT750 HD FREEdom Edition, which was granted 510(k) clearance in June. "I think that other companies are going to come up with something similar but I think that each type will be adequately different enough that [these technologies] will require their own validation studies," said Dr. Leipsic.
Siemens is reportedly developing a similar technology.
Dr. Min is a speaker for GE Healthcare. Dr. Budoff receives grant support from HeartFlow. Dr. George has received research support from Toshiba Medical Systems and GE Healthcare, is on the advisory board of GE Healthcare, and is a consultant to ICON Medical Imaging. Dr. Earls is on the speakers bureau for and has research funded by GE Healthcare. Dr. Leipsic is a consultant/speaker for Edwards Lifesciences and GE Healthcare.
A Cycling Accident Results in Shoulder Pain
Sudden Ankle Pain During Activity
The Spectrum of Traumatic Schmorl's Nodes: Identification and Treatment Options in 3 Patients
Massive Subacromial-Subdeltoid Bursitis With Rice Bodies Secondary to an Orthopedic Implant
FAME 2 Favorable PCI Results Driven by Revascularization
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in patients who underwent FFR-guided PCI than in patients who received best medical management alone (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical therapy group.
Data Source: Data are from the FAME 2 trial, in 1,220 stable patients who had angiographically assessed coronary artery disease and were appropriate candidates for PCI. The trial was stopped early because of a highly significant difference in the primary outcome.
Disclosures: The study was sponsored by St. Jude Medical. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.