User login
The Images Are Great, But Do They Help?
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
DeFACTO Propels CT Fractional Flow Reserve Closer to Clinical Practice
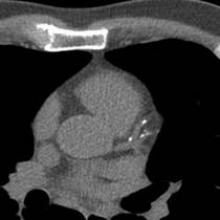
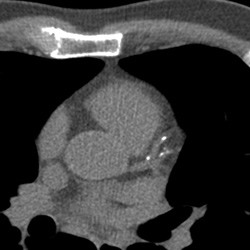
The addition of CT-based fractional flow reserve information to CT alone improved the diagnostic accuracy of stenoses, allowing noninvasive assessment of the physiologic consequences of lesions, according to the long-awaited results of the Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography (DeFACTO) study.
However, CT fractional flow reserve (FFR-CT) plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval. Per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone, in all patients, in all vessels, and also in vessels of intermediate stenosis severity," lead author Dr. James K. Min said during a press conference.
The results of the study were released in JAMA on Aug. 26th to coincide with the presentation of the study at the European Society of Cardiology meeting (JAMA 2012;308 [doi: 10.1001/2012.jama.11274]).
Fractional flow reserve (FFR) is currently assessed during invasive coronary angiography (ICA) to determine whether a coronary stenosis results in ischemia, and is the currently accepted reference standard for determining lesion-specific ischemia. FFR is the ratio of the mean coronary pressure distal to a coronary stenosis to the mean aortic pressure during maximal coronary blood flow. This value describes coronary flow still attainable despite the presence of a stenotic lesion.
While CT angiography has long been used to accurately and noninvasively assess the anatomic severity of stenoses, the technique has been criticized because it does not yield functional information about the hemodynamic effect of lesions.
Noninvasive calculation of FFR from CT "is a novel method that applies computational fluid dynamics to determine the physiologic significance of CAD [coronary artery disease]. Fractional flow reserve from CT enables calculation of rest and hyperemic pressure fields in coronary arteries without additional imaging, modification of CT acquisition protocols, or administration of medications," the investigators wrote.
"Taken together, these study results suggest the potential of FFR-CT as a promising noninvasive method for identification of individuals with ischemia. The present study findings can be considered proof of concept of the feasibility of this novel technology."
A total of 252 patients were included in the final analysis of the DeFACTO study. These patients had CAD and underwent clinically indicated ICA after CT with no intervening coronary event. Patients were not eligible if they had a history of coronary artery bypass graft (CABG) surgery or percutaneous coronary intervention. About 77% of patients had experienced angina within the past month.
Among 615 study vessels, 271 had less than 30% stenosis and 101 had at least 90% stenosis. In all, 407 vessels were directly assessed by both FFR and FFR-CT.
Computed tomographic angiography was performed on 64- or greater detector scanners with prospective or retrospective electrocardiographic gating.
The investigators evaluated CTs for maximal patient-, vessel-, and segment-based diameter stenosis (characterized as 0%, 1%-29%, 30%-49%, or 50% or larger).
Per-patient and per-vessel CAD stenosis were the maximal stenoses identified in all segments or in all segments within a vessel distribution, respectively. Vessel distributions were categorized for the left anterior descending, left circumflex, and right coronary artery. Computed tomographic angiograms (CTAs) were judged as excellent, good, adequate, or nondiagnostic.
Selective ICA was performed by standard protocol, and FFR was performed at the time of ICA. Fractional flow reserve was considered diagnostic of ischemia at a threshold of 0.80 or less. Computation of FFR-CT was performed in blinded fashion by the FFR-CT core laboratory at HeartFlow, the study’s sponsor.
Per-patient diagnostic accuracy for FFR-CT plus CT was 73%. By comparison, diagnostic accuracy of CT alone was 64%.
FFR-CT also demonstrated greater discriminatory power than CT alone for vessels directly assessed by invasive FFR. For these vessels, the diagnostic sensitivity and specificity of FFR-CT alone were 80% and 61%, respectively.
Importantly, the researchers performed a secondary analysis of patients with an intermediate stenosis ranging from 30% to 70%, "wherein the clinical utility of FFR-CT would be most commonly expected for use." Diagnostic accuracy (73% for FFR-CT and 57% for CT), sensitivity (82% and 37%, respectively), positive predictive value (54% and 34%) and negative predictive value (88% and 68%) were greater for FFR-CT than for CT, though specificity was similar at 66%.
This intermediate group is an important patient population. "We know that patients with 30%-70% stenosis – even though they don’t look high-risk anatomically – actually, some of them experience ischemia and physiologic consequences of their coronary artery disease," said Dr. Min, director of cardiac imaging research and co-director of cardiac imaging at the Cedars-Sinai Heart Institute in Los Angeles.
High sensitivity/low specificity among patients with intermediate stenoses suggests "a low false-negative rate if assessments by FFR-CT were used to identify ischemia causing intermediate lesions, with negligible effects on reductions of false positive results. In this regard, the use of FFR-CT may significantly advance clinical assessment of patients without conventional measures of anatomic high-grade coronary stenosis, largely by proper identification of a significantly greater proportion of patients with manifest ischemia rather than as a safeguard to further invasive evaluation," the researchers noted.
They also pointed out that the prespecified primary end point for FFR-CT – a lower bound of the 95% confidence interval greater than 70% – "represents a 15% increase over traditional noninvasive histologic imaging methods, including myocardial perfusion imaging by SPECT or stress echocardiography," Dr. Min said.
Dr. Min and several of his coauthors reported significant financial relationships with GE Healthcare and Philips Medical, as well as other medical imaging/pharmaceutical companies. Dr. Jason H. Cole reported a grant for research support from HeartFlow. Dr. John Mancini reported a grant to his institution from HeartFlow. This study was funded by HeartFlow.
"Technologies that provide both a highly sensitive anatomic evaluation for obstructive disease and a highly specific physiologic evaluation for ischemia represent the ‘Holy Grail’ for noninvasive imaging for CAD," Dr. Manesh R. Patel wrote in an accompanying editorial (JAMA 2012 Aug. 26 [doi: 10.1001/2012.jama.11383]).
One possible investigational approach is the combination of anatomic analysis using CT and functional analysis using fractional flow reserve based on CT data (FFR-CT).
The DeFACTO investigators "raise the bar by comparing this diagnostic technology with a reference standard of both invasive angiography and invasive FFR. This change in reference standard may in part explain some of the accuracy findings. So how should these findings be considered with regard to current clinical evaluation for chest pain?" asked Dr. Patel.
It’s important to put the findings on the performance of CT angiography into context, he wrote. "Several recent multicenter studies have reported diagnostic performance of CT angiography to have high sensitivity (i.e., between 85%-95%) compared with conventional invasive angiography for stenoses of 50% or greater." The high sensitivity of CTA has been used to triage low-risk patients in acute settings.
"However, in stable intermediate-risk patients, for whom a higher degree of specificity (low rate of false positive results) may be desirable to reduce referrals for invasive angiography, concerns exist about the specificity of CT angiography," Dr. Patel noted. In the present study, CT angiography had a sensitivity of 84% but a specificity of only 42% with the more rigorous reference standard.
"It is in this context that FFR-CT represents a novel and important innovation, with the possibility not only to diagnose but also to help direct invasive treatment. The current ... multicenter report by Min et al. confirms a high sensitivity (90%) but demonstrates modest specificity (54%), albeit better than CTA alone," he wrote.
"At first glance, readers of the study may consider FFR-CT technology to be limited based on the results presented. However, this would be a naive conclusion, likely based on the published diagnostic performance of noninvasive tests compared only with invasive angiography," Dr. Patel warned. By comparing existing noninvasive imaging technologies with invasive angiography plus FFR, it is highly likely that the published diagnostic performance would be reduced. "In fact, in clinical practice, the sole use of invasive angiography for lesion evaluation has decreased. Additionally, in real-world practice, the current noninvasive technologies used for diagnosis and risk stratification in stable elective patients prior to invasive angiography do not perform at the published diagnostic levels, as evidenced by the low rates of obstructive CAD at elective catheterization. Hence, the current report describes an important noninvasive technology that may improve existing care and has the potential to outperform established noninvasive technologies," according to Dr. Patel.
DR. PATEL is the cardiology section leader in the peripheral vascular program at Duke University in Durham, N.C., and is assistant director of the cardiac catheterization laboratory. Dr. Patel reports consultancy for Bayer, Jansen, Baxter, and Otsuka, and grants from Johnson & Johnson and AstraZeneca.
"Technologies that provide both a highly sensitive anatomic evaluation for obstructive disease and a highly specific physiologic evaluation for ischemia represent the ‘Holy Grail’ for noninvasive imaging for CAD," Dr. Manesh R. Patel wrote in an accompanying editorial (JAMA 2012 Aug. 26 [doi: 10.1001/2012.jama.11383]).
One possible investigational approach is the combination of anatomic analysis using CT and functional analysis using fractional flow reserve based on CT data (FFR-CT).
The DeFACTO investigators "raise the bar by comparing this diagnostic technology with a reference standard of both invasive angiography and invasive FFR. This change in reference standard may in part explain some of the accuracy findings. So how should these findings be considered with regard to current clinical evaluation for chest pain?" asked Dr. Patel.
It’s important to put the findings on the performance of CT angiography into context, he wrote. "Several recent multicenter studies have reported diagnostic performance of CT angiography to have high sensitivity (i.e., between 85%-95%) compared with conventional invasive angiography for stenoses of 50% or greater." The high sensitivity of CTA has been used to triage low-risk patients in acute settings.
"However, in stable intermediate-risk patients, for whom a higher degree of specificity (low rate of false positive results) may be desirable to reduce referrals for invasive angiography, concerns exist about the specificity of CT angiography," Dr. Patel noted. In the present study, CT angiography had a sensitivity of 84% but a specificity of only 42% with the more rigorous reference standard.
"It is in this context that FFR-CT represents a novel and important innovation, with the possibility not only to diagnose but also to help direct invasive treatment. The current ... multicenter report by Min et al. confirms a high sensitivity (90%) but demonstrates modest specificity (54%), albeit better than CTA alone," he wrote.
"At first glance, readers of the study may consider FFR-CT technology to be limited based on the results presented. However, this would be a naive conclusion, likely based on the published diagnostic performance of noninvasive tests compared only with invasive angiography," Dr. Patel warned. By comparing existing noninvasive imaging technologies with invasive angiography plus FFR, it is highly likely that the published diagnostic performance would be reduced. "In fact, in clinical practice, the sole use of invasive angiography for lesion evaluation has decreased. Additionally, in real-world practice, the current noninvasive technologies used for diagnosis and risk stratification in stable elective patients prior to invasive angiography do not perform at the published diagnostic levels, as evidenced by the low rates of obstructive CAD at elective catheterization. Hence, the current report describes an important noninvasive technology that may improve existing care and has the potential to outperform established noninvasive technologies," according to Dr. Patel.
DR. PATEL is the cardiology section leader in the peripheral vascular program at Duke University in Durham, N.C., and is assistant director of the cardiac catheterization laboratory. Dr. Patel reports consultancy for Bayer, Jansen, Baxter, and Otsuka, and grants from Johnson & Johnson and AstraZeneca.
"Technologies that provide both a highly sensitive anatomic evaluation for obstructive disease and a highly specific physiologic evaluation for ischemia represent the ‘Holy Grail’ for noninvasive imaging for CAD," Dr. Manesh R. Patel wrote in an accompanying editorial (JAMA 2012 Aug. 26 [doi: 10.1001/2012.jama.11383]).
One possible investigational approach is the combination of anatomic analysis using CT and functional analysis using fractional flow reserve based on CT data (FFR-CT).
The DeFACTO investigators "raise the bar by comparing this diagnostic technology with a reference standard of both invasive angiography and invasive FFR. This change in reference standard may in part explain some of the accuracy findings. So how should these findings be considered with regard to current clinical evaluation for chest pain?" asked Dr. Patel.
It’s important to put the findings on the performance of CT angiography into context, he wrote. "Several recent multicenter studies have reported diagnostic performance of CT angiography to have high sensitivity (i.e., between 85%-95%) compared with conventional invasive angiography for stenoses of 50% or greater." The high sensitivity of CTA has been used to triage low-risk patients in acute settings.
"However, in stable intermediate-risk patients, for whom a higher degree of specificity (low rate of false positive results) may be desirable to reduce referrals for invasive angiography, concerns exist about the specificity of CT angiography," Dr. Patel noted. In the present study, CT angiography had a sensitivity of 84% but a specificity of only 42% with the more rigorous reference standard.
"It is in this context that FFR-CT represents a novel and important innovation, with the possibility not only to diagnose but also to help direct invasive treatment. The current ... multicenter report by Min et al. confirms a high sensitivity (90%) but demonstrates modest specificity (54%), albeit better than CTA alone," he wrote.
"At first glance, readers of the study may consider FFR-CT technology to be limited based on the results presented. However, this would be a naive conclusion, likely based on the published diagnostic performance of noninvasive tests compared only with invasive angiography," Dr. Patel warned. By comparing existing noninvasive imaging technologies with invasive angiography plus FFR, it is highly likely that the published diagnostic performance would be reduced. "In fact, in clinical practice, the sole use of invasive angiography for lesion evaluation has decreased. Additionally, in real-world practice, the current noninvasive technologies used for diagnosis and risk stratification in stable elective patients prior to invasive angiography do not perform at the published diagnostic levels, as evidenced by the low rates of obstructive CAD at elective catheterization. Hence, the current report describes an important noninvasive technology that may improve existing care and has the potential to outperform established noninvasive technologies," according to Dr. Patel.
DR. PATEL is the cardiology section leader in the peripheral vascular program at Duke University in Durham, N.C., and is assistant director of the cardiac catheterization laboratory. Dr. Patel reports consultancy for Bayer, Jansen, Baxter, and Otsuka, and grants from Johnson & Johnson and AstraZeneca.
The addition of CT-based fractional flow reserve information to CT alone improved the diagnostic accuracy of stenoses, allowing noninvasive assessment of the physiologic consequences of lesions, according to the long-awaited results of the Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography (DeFACTO) study.
However, CT fractional flow reserve (FFR-CT) plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval. Per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone, in all patients, in all vessels, and also in vessels of intermediate stenosis severity," lead author Dr. James K. Min said during a press conference.
The results of the study were released in JAMA on Aug. 26th to coincide with the presentation of the study at the European Society of Cardiology meeting (JAMA 2012;308 [doi: 10.1001/2012.jama.11274]).
Fractional flow reserve (FFR) is currently assessed during invasive coronary angiography (ICA) to determine whether a coronary stenosis results in ischemia, and is the currently accepted reference standard for determining lesion-specific ischemia. FFR is the ratio of the mean coronary pressure distal to a coronary stenosis to the mean aortic pressure during maximal coronary blood flow. This value describes coronary flow still attainable despite the presence of a stenotic lesion.
While CT angiography has long been used to accurately and noninvasively assess the anatomic severity of stenoses, the technique has been criticized because it does not yield functional information about the hemodynamic effect of lesions.
Noninvasive calculation of FFR from CT "is a novel method that applies computational fluid dynamics to determine the physiologic significance of CAD [coronary artery disease]. Fractional flow reserve from CT enables calculation of rest and hyperemic pressure fields in coronary arteries without additional imaging, modification of CT acquisition protocols, or administration of medications," the investigators wrote.
"Taken together, these study results suggest the potential of FFR-CT as a promising noninvasive method for identification of individuals with ischemia. The present study findings can be considered proof of concept of the feasibility of this novel technology."
A total of 252 patients were included in the final analysis of the DeFACTO study. These patients had CAD and underwent clinically indicated ICA after CT with no intervening coronary event. Patients were not eligible if they had a history of coronary artery bypass graft (CABG) surgery or percutaneous coronary intervention. About 77% of patients had experienced angina within the past month.
Among 615 study vessels, 271 had less than 30% stenosis and 101 had at least 90% stenosis. In all, 407 vessels were directly assessed by both FFR and FFR-CT.
Computed tomographic angiography was performed on 64- or greater detector scanners with prospective or retrospective electrocardiographic gating.
The investigators evaluated CTs for maximal patient-, vessel-, and segment-based diameter stenosis (characterized as 0%, 1%-29%, 30%-49%, or 50% or larger).
Per-patient and per-vessel CAD stenosis were the maximal stenoses identified in all segments or in all segments within a vessel distribution, respectively. Vessel distributions were categorized for the left anterior descending, left circumflex, and right coronary artery. Computed tomographic angiograms (CTAs) were judged as excellent, good, adequate, or nondiagnostic.
Selective ICA was performed by standard protocol, and FFR was performed at the time of ICA. Fractional flow reserve was considered diagnostic of ischemia at a threshold of 0.80 or less. Computation of FFR-CT was performed in blinded fashion by the FFR-CT core laboratory at HeartFlow, the study’s sponsor.
Per-patient diagnostic accuracy for FFR-CT plus CT was 73%. By comparison, diagnostic accuracy of CT alone was 64%.
FFR-CT also demonstrated greater discriminatory power than CT alone for vessels directly assessed by invasive FFR. For these vessels, the diagnostic sensitivity and specificity of FFR-CT alone were 80% and 61%, respectively.
Importantly, the researchers performed a secondary analysis of patients with an intermediate stenosis ranging from 30% to 70%, "wherein the clinical utility of FFR-CT would be most commonly expected for use." Diagnostic accuracy (73% for FFR-CT and 57% for CT), sensitivity (82% and 37%, respectively), positive predictive value (54% and 34%) and negative predictive value (88% and 68%) were greater for FFR-CT than for CT, though specificity was similar at 66%.
This intermediate group is an important patient population. "We know that patients with 30%-70% stenosis – even though they don’t look high-risk anatomically – actually, some of them experience ischemia and physiologic consequences of their coronary artery disease," said Dr. Min, director of cardiac imaging research and co-director of cardiac imaging at the Cedars-Sinai Heart Institute in Los Angeles.
High sensitivity/low specificity among patients with intermediate stenoses suggests "a low false-negative rate if assessments by FFR-CT were used to identify ischemia causing intermediate lesions, with negligible effects on reductions of false positive results. In this regard, the use of FFR-CT may significantly advance clinical assessment of patients without conventional measures of anatomic high-grade coronary stenosis, largely by proper identification of a significantly greater proportion of patients with manifest ischemia rather than as a safeguard to further invasive evaluation," the researchers noted.
They also pointed out that the prespecified primary end point for FFR-CT – a lower bound of the 95% confidence interval greater than 70% – "represents a 15% increase over traditional noninvasive histologic imaging methods, including myocardial perfusion imaging by SPECT or stress echocardiography," Dr. Min said.
Dr. Min and several of his coauthors reported significant financial relationships with GE Healthcare and Philips Medical, as well as other medical imaging/pharmaceutical companies. Dr. Jason H. Cole reported a grant for research support from HeartFlow. Dr. John Mancini reported a grant to his institution from HeartFlow. This study was funded by HeartFlow.
The addition of CT-based fractional flow reserve information to CT alone improved the diagnostic accuracy of stenoses, allowing noninvasive assessment of the physiologic consequences of lesions, according to the long-awaited results of the Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography (DeFACTO) study.
However, CT fractional flow reserve (FFR-CT) plus CT narrowly failed to meet the trial’s primary end point – diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval. Per-patient performance diagnostic accuracy of FFR-CT plus CT was 73% with a 95% CI of 67%-78%.
Nevertheless, the addition of FFR-CT "demonstrated superior diagnostic performance characteristics, as compared with CT stenosis alone, in all patients, in all vessels, and also in vessels of intermediate stenosis severity," lead author Dr. James K. Min said during a press conference.
The results of the study were released in JAMA on Aug. 26th to coincide with the presentation of the study at the European Society of Cardiology meeting (JAMA 2012;308 [doi: 10.1001/2012.jama.11274]).
Fractional flow reserve (FFR) is currently assessed during invasive coronary angiography (ICA) to determine whether a coronary stenosis results in ischemia, and is the currently accepted reference standard for determining lesion-specific ischemia. FFR is the ratio of the mean coronary pressure distal to a coronary stenosis to the mean aortic pressure during maximal coronary blood flow. This value describes coronary flow still attainable despite the presence of a stenotic lesion.
While CT angiography has long been used to accurately and noninvasively assess the anatomic severity of stenoses, the technique has been criticized because it does not yield functional information about the hemodynamic effect of lesions.
Noninvasive calculation of FFR from CT "is a novel method that applies computational fluid dynamics to determine the physiologic significance of CAD [coronary artery disease]. Fractional flow reserve from CT enables calculation of rest and hyperemic pressure fields in coronary arteries without additional imaging, modification of CT acquisition protocols, or administration of medications," the investigators wrote.
"Taken together, these study results suggest the potential of FFR-CT as a promising noninvasive method for identification of individuals with ischemia. The present study findings can be considered proof of concept of the feasibility of this novel technology."
A total of 252 patients were included in the final analysis of the DeFACTO study. These patients had CAD and underwent clinically indicated ICA after CT with no intervening coronary event. Patients were not eligible if they had a history of coronary artery bypass graft (CABG) surgery or percutaneous coronary intervention. About 77% of patients had experienced angina within the past month.
Among 615 study vessels, 271 had less than 30% stenosis and 101 had at least 90% stenosis. In all, 407 vessels were directly assessed by both FFR and FFR-CT.
Computed tomographic angiography was performed on 64- or greater detector scanners with prospective or retrospective electrocardiographic gating.
The investigators evaluated CTs for maximal patient-, vessel-, and segment-based diameter stenosis (characterized as 0%, 1%-29%, 30%-49%, or 50% or larger).
Per-patient and per-vessel CAD stenosis were the maximal stenoses identified in all segments or in all segments within a vessel distribution, respectively. Vessel distributions were categorized for the left anterior descending, left circumflex, and right coronary artery. Computed tomographic angiograms (CTAs) were judged as excellent, good, adequate, or nondiagnostic.
Selective ICA was performed by standard protocol, and FFR was performed at the time of ICA. Fractional flow reserve was considered diagnostic of ischemia at a threshold of 0.80 or less. Computation of FFR-CT was performed in blinded fashion by the FFR-CT core laboratory at HeartFlow, the study’s sponsor.
Per-patient diagnostic accuracy for FFR-CT plus CT was 73%. By comparison, diagnostic accuracy of CT alone was 64%.
FFR-CT also demonstrated greater discriminatory power than CT alone for vessels directly assessed by invasive FFR. For these vessels, the diagnostic sensitivity and specificity of FFR-CT alone were 80% and 61%, respectively.
Importantly, the researchers performed a secondary analysis of patients with an intermediate stenosis ranging from 30% to 70%, "wherein the clinical utility of FFR-CT would be most commonly expected for use." Diagnostic accuracy (73% for FFR-CT and 57% for CT), sensitivity (82% and 37%, respectively), positive predictive value (54% and 34%) and negative predictive value (88% and 68%) were greater for FFR-CT than for CT, though specificity was similar at 66%.
This intermediate group is an important patient population. "We know that patients with 30%-70% stenosis – even though they don’t look high-risk anatomically – actually, some of them experience ischemia and physiologic consequences of their coronary artery disease," said Dr. Min, director of cardiac imaging research and co-director of cardiac imaging at the Cedars-Sinai Heart Institute in Los Angeles.
High sensitivity/low specificity among patients with intermediate stenoses suggests "a low false-negative rate if assessments by FFR-CT were used to identify ischemia causing intermediate lesions, with negligible effects on reductions of false positive results. In this regard, the use of FFR-CT may significantly advance clinical assessment of patients without conventional measures of anatomic high-grade coronary stenosis, largely by proper identification of a significantly greater proportion of patients with manifest ischemia rather than as a safeguard to further invasive evaluation," the researchers noted.
They also pointed out that the prespecified primary end point for FFR-CT – a lower bound of the 95% confidence interval greater than 70% – "represents a 15% increase over traditional noninvasive histologic imaging methods, including myocardial perfusion imaging by SPECT or stress echocardiography," Dr. Min said.
Dr. Min and several of his coauthors reported significant financial relationships with GE Healthcare and Philips Medical, as well as other medical imaging/pharmaceutical companies. Dr. Jason H. Cole reported a grant for research support from HeartFlow. Dr. John Mancini reported a grant to his institution from HeartFlow. This study was funded by HeartFlow.
FROM JAMA
Major Finding: CT fractional flow reserve (FFR-CT) plus CT had a per-patient performance diagnostic accuracy of 73% with a 95% confidence interval of 67%-78% – narrowly failing to meet the trial’s primary end point of diagnostic accuracy greater than 70% for the lower bound of the 95% confidence interval.
Data Source: DeFACTO was a multicenter prospective study of 252 patients with CAD, who underwent clinically indicated invasive coronary angiography after CT.
Disclosures: Dr. Min and several of his coauthors reported significant financial relationships with GE Healthcare and Philips Medical, as well as other medical imaging/pharmaceutical companies. Dr. Jason H. Cole reported a grant for research support from HeartFlow. Dr. John Mancini reported a grant to his institution from HeartFlow. This study was funded by HeartFlow.
CCTA Helps Clear Emergency Departments, But Costs Remain High
The use of cardiac computed tomography angiography (CCTA) can help emergency department physicians make better decisions about which patients with symptoms suggestive of acute coronary syndromes can safely be sent home.
There were no undetected cases of acute coronary syndromes (ACS) in patients assessed with CCTA or standard evaluation, suggesting that the earlier and greater number of discharges in the CCTA group did not result in any missed diagnoses in a prospective, randomized trial of 1,000 patients.
"It’s really about what is the minimum testing that you can do to safely send someone home if you’re an emergency department physician," senior author Dr. James E. Udelson said in an interview. Each ED and each ED physician had their own criteria for when a patient could be discharged based on CCTA findings. "We’re really measuring not the performance of the test, but how the test affects decision making," he said.
Previous studies have suggested that CCTA may aid in safer and earlier triage of low-risk patients and that it can rule out coronary artery disease faster than stress myocardial-perfusion imaging. However, CCTA often can involve more follow-up procedures and greater costs than functional testing.
While the accuracy of CCTA was roughly equivalent to that of standard ED evaluation, the imaging technique also cost about the same. There was no difference in total costs between the two groups for the index visit and during 28-day follow-up in a subgroup of 649 patients from five of nine sites, in which complete billing data were available. Costs for patients with CCTA appeared to be driven by a greater use of additional diagnostic testing.
In ROMICAT-II (Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography II), researchers pitted CCTA – as a first diagnostic test, performed as early as possible – against standard ED evaluation in 1,000 patients with acute chest pain suggestive of ACS (N. Engl. J. Med. 2012;367:299-308).
The average length of the hospital stay – the primary end point – for patients who underwent CCTA was 7.6 hours less than that of the standard evaluation group.
Patient enrollment began in April 2010 and ended in January 2012 at nine U.S. hospitals. All sites were required to use at least 64-slice CT. Eligible patients were 40-74 years of age, and presented to the ED with chest pain (or the anginal equivalent) of at least 5 minutes’ duration within 24 hours before presentation in the ED. They also had to be in sinus rhythm and warranted further risk stratification to rule out acute coronary syndromes.
Patient care was not mandated by the study protocol in either group, but instead was at the discretion of local physicians. The discharge diagnosis also was based on the local physicians’ assessment.
Of 1,000 enrolled patients, 501 were randomized to CCTA and 499 were assigned to a standard evaluation. All patients were included in the intention-to-treat analysis. Overall, 987 patients (99%) had complete follow-up at 28 days.
After a complete evaluation, 75 patients (8%) had a final diagnosis of an acute coronary syndrome. In this subgroup of patients with a final diagnosis of ACS, the length of stay in the hospital was similar after CCTA and after standard evaluation in the ED.
In the overall cohort and also in patients without a final diagnosis of ACS, the mean time to diagnosis was significantly decreased with CCTA, compared with a standard evaluation. Patients in the CCTA group were more often directly discharged from the ED (47%, compared with 12% of patients in the standard-evaluation group), with fewer admissions to an observation unit.
Overall, there were eight major adverse cardiovascular events during the 28-day follow-up: six after standard evaluation in the ED and two after CCTA.
The results have important implications for some EDs. Not all EDs are the same: Some are overflowing with patients, while others have light traffic. For directors of busy and crowded EDs, the findings provide "an opportunity to get people out a lot sooner," said Dr. Udelson, chief of the cardiology division at Tufts Medical Center in Boston.
Half of patients who presented to the ED with symptoms suggestive of ACS and who underwent CCTA were discharged within 8.6 hours. In contrast, it took more than a day (26.7 hours) for half of the patients in the standard-evaluation group to be discharged. "If you’re in a supercrowded ED, that’s really worth something," he said.
The researchers did not measure additional follow-up in this study beyond major events that may have happened within 30 days. However, "one of the things about CT is that you identify early disease. You can potentially be comfortable that it doesn’t have anything to do with the chest pain." Primary care physicians should know about this early disease, in order to potentially start or change treatment.
One important question is what the yield is of subsequent testing following CCTA, said Dr. Udelson. "We’ll try to define the characteristics of the CT that mean that you’re not going to find anything else and not to test further."
In an accompanying editorial, Dr. Rita F. Redberg asserted that "with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided" (N. Engl. J. Med. 2012;367:375-6). Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. She is also on the editorial board of Cardiology News.
However, Dr. Udelson pointed out that "ED physicians struggle with this. They’re on the firing line. It’s their heads if they make a wrong decision."
"That’s our potential next step. ... Almost a quarter of the patients in the control group had no imaging tests. In other words, the physicians felt comfortable enough to discharge these patients with no [additional] testing." They will try to determine which individuals can safely go home and which patients need additional testing.
This study was supported by grants from the National Institutes of Health. Dr. Udelson reported that he is on the scientific advisory board of Lantheus Medical Imaging. Several of the coauthors reported financial ties to imaging and/or pharmaceutical companies and professional organizations.
"With no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided," Dr. Rita F. Redberg argued in an accompanying editorial (N. Engl. J. Med. 2012;367:375-6) on the findings.
"In short, the question is not which test leads to faster discharge of patients from the emergency department, but whether a test is needed at all."
ROMICAT-II builds on similar data from another study that also randomly assigned patients with suspected acute coronary syndromes to CCTA or traditional care (N. Engl. J. Med. 2012;366:1393-403).
While shorter lengths of stay in the hospital are highly desirable, "the ROMICAT-II study reveals a deeper flaw in the approach to chest pain in the emergency department. The underlying assumption of these two studies is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes," said Dr. Redberg.
She explained that rates of major adverse cardiac events among all patients in these two studies – regardless of whether the patients underwent CCTA, stress testing, or no testing at all – were so low (less than 1% had a myocardial infarction and no patients died) that it is impossible to know whether the CCTA groups received any benefit whatsoever.
Dr. Redberg pointed out several potential dangers associated with CCTA, such as the increased likelihood of downstream testing after CCTA that can lead to serious complications.
"In light of the certainty that the patients in the CCTA group were exposed to substantial doses of radiation (from both CCTA and nuclear stress tests) and were at risk for nephrotoxicity and adverse reactions from the CCTA contrast dye, clinicians may legitimately ask whether the tests did more harm than good," she observed.
"Patients who have normal electrocardiographic findings and negative troponin levels constitute a group at low risk for cardiac events, and multiple studies show no evidence that any additional testing further reduces that risk," she said.
The decision regarding the need for diagnostic testing in these patients usually can be safely deferred to outpatient follow-up within a few weeks after the visit to the emergency department. The vast majority of patients have no cardiac causes for their chest pain, and many need no further testing.
Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. Dr. Redberg is also on the editorial board of Cardiology News. She reported that she has no conflicts of interest.
"With no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided," Dr. Rita F. Redberg argued in an accompanying editorial (N. Engl. J. Med. 2012;367:375-6) on the findings.
"In short, the question is not which test leads to faster discharge of patients from the emergency department, but whether a test is needed at all."
ROMICAT-II builds on similar data from another study that also randomly assigned patients with suspected acute coronary syndromes to CCTA or traditional care (N. Engl. J. Med. 2012;366:1393-403).
While shorter lengths of stay in the hospital are highly desirable, "the ROMICAT-II study reveals a deeper flaw in the approach to chest pain in the emergency department. The underlying assumption of these two studies is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes," said Dr. Redberg.
She explained that rates of major adverse cardiac events among all patients in these two studies – regardless of whether the patients underwent CCTA, stress testing, or no testing at all – were so low (less than 1% had a myocardial infarction and no patients died) that it is impossible to know whether the CCTA groups received any benefit whatsoever.
Dr. Redberg pointed out several potential dangers associated with CCTA, such as the increased likelihood of downstream testing after CCTA that can lead to serious complications.
"In light of the certainty that the patients in the CCTA group were exposed to substantial doses of radiation (from both CCTA and nuclear stress tests) and were at risk for nephrotoxicity and adverse reactions from the CCTA contrast dye, clinicians may legitimately ask whether the tests did more harm than good," she observed.
"Patients who have normal electrocardiographic findings and negative troponin levels constitute a group at low risk for cardiac events, and multiple studies show no evidence that any additional testing further reduces that risk," she said.
The decision regarding the need for diagnostic testing in these patients usually can be safely deferred to outpatient follow-up within a few weeks after the visit to the emergency department. The vast majority of patients have no cardiac causes for their chest pain, and many need no further testing.
Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. Dr. Redberg is also on the editorial board of Cardiology News. She reported that she has no conflicts of interest.
"With no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided," Dr. Rita F. Redberg argued in an accompanying editorial (N. Engl. J. Med. 2012;367:375-6) on the findings.
"In short, the question is not which test leads to faster discharge of patients from the emergency department, but whether a test is needed at all."
ROMICAT-II builds on similar data from another study that also randomly assigned patients with suspected acute coronary syndromes to CCTA or traditional care (N. Engl. J. Med. 2012;366:1393-403).
While shorter lengths of stay in the hospital are highly desirable, "the ROMICAT-II study reveals a deeper flaw in the approach to chest pain in the emergency department. The underlying assumption of these two studies is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes," said Dr. Redberg.
She explained that rates of major adverse cardiac events among all patients in these two studies – regardless of whether the patients underwent CCTA, stress testing, or no testing at all – were so low (less than 1% had a myocardial infarction and no patients died) that it is impossible to know whether the CCTA groups received any benefit whatsoever.
Dr. Redberg pointed out several potential dangers associated with CCTA, such as the increased likelihood of downstream testing after CCTA that can lead to serious complications.
"In light of the certainty that the patients in the CCTA group were exposed to substantial doses of radiation (from both CCTA and nuclear stress tests) and were at risk for nephrotoxicity and adverse reactions from the CCTA contrast dye, clinicians may legitimately ask whether the tests did more harm than good," she observed.
"Patients who have normal electrocardiographic findings and negative troponin levels constitute a group at low risk for cardiac events, and multiple studies show no evidence that any additional testing further reduces that risk," she said.
The decision regarding the need for diagnostic testing in these patients usually can be safely deferred to outpatient follow-up within a few weeks after the visit to the emergency department. The vast majority of patients have no cardiac causes for their chest pain, and many need no further testing.
Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. Dr. Redberg is also on the editorial board of Cardiology News. She reported that she has no conflicts of interest.
The use of cardiac computed tomography angiography (CCTA) can help emergency department physicians make better decisions about which patients with symptoms suggestive of acute coronary syndromes can safely be sent home.
There were no undetected cases of acute coronary syndromes (ACS) in patients assessed with CCTA or standard evaluation, suggesting that the earlier and greater number of discharges in the CCTA group did not result in any missed diagnoses in a prospective, randomized trial of 1,000 patients.
"It’s really about what is the minimum testing that you can do to safely send someone home if you’re an emergency department physician," senior author Dr. James E. Udelson said in an interview. Each ED and each ED physician had their own criteria for when a patient could be discharged based on CCTA findings. "We’re really measuring not the performance of the test, but how the test affects decision making," he said.
Previous studies have suggested that CCTA may aid in safer and earlier triage of low-risk patients and that it can rule out coronary artery disease faster than stress myocardial-perfusion imaging. However, CCTA often can involve more follow-up procedures and greater costs than functional testing.
While the accuracy of CCTA was roughly equivalent to that of standard ED evaluation, the imaging technique also cost about the same. There was no difference in total costs between the two groups for the index visit and during 28-day follow-up in a subgroup of 649 patients from five of nine sites, in which complete billing data were available. Costs for patients with CCTA appeared to be driven by a greater use of additional diagnostic testing.
In ROMICAT-II (Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography II), researchers pitted CCTA – as a first diagnostic test, performed as early as possible – against standard ED evaluation in 1,000 patients with acute chest pain suggestive of ACS (N. Engl. J. Med. 2012;367:299-308).
The average length of the hospital stay – the primary end point – for patients who underwent CCTA was 7.6 hours less than that of the standard evaluation group.
Patient enrollment began in April 2010 and ended in January 2012 at nine U.S. hospitals. All sites were required to use at least 64-slice CT. Eligible patients were 40-74 years of age, and presented to the ED with chest pain (or the anginal equivalent) of at least 5 minutes’ duration within 24 hours before presentation in the ED. They also had to be in sinus rhythm and warranted further risk stratification to rule out acute coronary syndromes.
Patient care was not mandated by the study protocol in either group, but instead was at the discretion of local physicians. The discharge diagnosis also was based on the local physicians’ assessment.
Of 1,000 enrolled patients, 501 were randomized to CCTA and 499 were assigned to a standard evaluation. All patients were included in the intention-to-treat analysis. Overall, 987 patients (99%) had complete follow-up at 28 days.
After a complete evaluation, 75 patients (8%) had a final diagnosis of an acute coronary syndrome. In this subgroup of patients with a final diagnosis of ACS, the length of stay in the hospital was similar after CCTA and after standard evaluation in the ED.
In the overall cohort and also in patients without a final diagnosis of ACS, the mean time to diagnosis was significantly decreased with CCTA, compared with a standard evaluation. Patients in the CCTA group were more often directly discharged from the ED (47%, compared with 12% of patients in the standard-evaluation group), with fewer admissions to an observation unit.
Overall, there were eight major adverse cardiovascular events during the 28-day follow-up: six after standard evaluation in the ED and two after CCTA.
The results have important implications for some EDs. Not all EDs are the same: Some are overflowing with patients, while others have light traffic. For directors of busy and crowded EDs, the findings provide "an opportunity to get people out a lot sooner," said Dr. Udelson, chief of the cardiology division at Tufts Medical Center in Boston.
Half of patients who presented to the ED with symptoms suggestive of ACS and who underwent CCTA were discharged within 8.6 hours. In contrast, it took more than a day (26.7 hours) for half of the patients in the standard-evaluation group to be discharged. "If you’re in a supercrowded ED, that’s really worth something," he said.
The researchers did not measure additional follow-up in this study beyond major events that may have happened within 30 days. However, "one of the things about CT is that you identify early disease. You can potentially be comfortable that it doesn’t have anything to do with the chest pain." Primary care physicians should know about this early disease, in order to potentially start or change treatment.
One important question is what the yield is of subsequent testing following CCTA, said Dr. Udelson. "We’ll try to define the characteristics of the CT that mean that you’re not going to find anything else and not to test further."
In an accompanying editorial, Dr. Rita F. Redberg asserted that "with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided" (N. Engl. J. Med. 2012;367:375-6). Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. She is also on the editorial board of Cardiology News.
However, Dr. Udelson pointed out that "ED physicians struggle with this. They’re on the firing line. It’s their heads if they make a wrong decision."
"That’s our potential next step. ... Almost a quarter of the patients in the control group had no imaging tests. In other words, the physicians felt comfortable enough to discharge these patients with no [additional] testing." They will try to determine which individuals can safely go home and which patients need additional testing.
This study was supported by grants from the National Institutes of Health. Dr. Udelson reported that he is on the scientific advisory board of Lantheus Medical Imaging. Several of the coauthors reported financial ties to imaging and/or pharmaceutical companies and professional organizations.
The use of cardiac computed tomography angiography (CCTA) can help emergency department physicians make better decisions about which patients with symptoms suggestive of acute coronary syndromes can safely be sent home.
There were no undetected cases of acute coronary syndromes (ACS) in patients assessed with CCTA or standard evaluation, suggesting that the earlier and greater number of discharges in the CCTA group did not result in any missed diagnoses in a prospective, randomized trial of 1,000 patients.
"It’s really about what is the minimum testing that you can do to safely send someone home if you’re an emergency department physician," senior author Dr. James E. Udelson said in an interview. Each ED and each ED physician had their own criteria for when a patient could be discharged based on CCTA findings. "We’re really measuring not the performance of the test, but how the test affects decision making," he said.
Previous studies have suggested that CCTA may aid in safer and earlier triage of low-risk patients and that it can rule out coronary artery disease faster than stress myocardial-perfusion imaging. However, CCTA often can involve more follow-up procedures and greater costs than functional testing.
While the accuracy of CCTA was roughly equivalent to that of standard ED evaluation, the imaging technique also cost about the same. There was no difference in total costs between the two groups for the index visit and during 28-day follow-up in a subgroup of 649 patients from five of nine sites, in which complete billing data were available. Costs for patients with CCTA appeared to be driven by a greater use of additional diagnostic testing.
In ROMICAT-II (Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography II), researchers pitted CCTA – as a first diagnostic test, performed as early as possible – against standard ED evaluation in 1,000 patients with acute chest pain suggestive of ACS (N. Engl. J. Med. 2012;367:299-308).
The average length of the hospital stay – the primary end point – for patients who underwent CCTA was 7.6 hours less than that of the standard evaluation group.
Patient enrollment began in April 2010 and ended in January 2012 at nine U.S. hospitals. All sites were required to use at least 64-slice CT. Eligible patients were 40-74 years of age, and presented to the ED with chest pain (or the anginal equivalent) of at least 5 minutes’ duration within 24 hours before presentation in the ED. They also had to be in sinus rhythm and warranted further risk stratification to rule out acute coronary syndromes.
Patient care was not mandated by the study protocol in either group, but instead was at the discretion of local physicians. The discharge diagnosis also was based on the local physicians’ assessment.
Of 1,000 enrolled patients, 501 were randomized to CCTA and 499 were assigned to a standard evaluation. All patients were included in the intention-to-treat analysis. Overall, 987 patients (99%) had complete follow-up at 28 days.
After a complete evaluation, 75 patients (8%) had a final diagnosis of an acute coronary syndrome. In this subgroup of patients with a final diagnosis of ACS, the length of stay in the hospital was similar after CCTA and after standard evaluation in the ED.
In the overall cohort and also in patients without a final diagnosis of ACS, the mean time to diagnosis was significantly decreased with CCTA, compared with a standard evaluation. Patients in the CCTA group were more often directly discharged from the ED (47%, compared with 12% of patients in the standard-evaluation group), with fewer admissions to an observation unit.
Overall, there were eight major adverse cardiovascular events during the 28-day follow-up: six after standard evaluation in the ED and two after CCTA.
The results have important implications for some EDs. Not all EDs are the same: Some are overflowing with patients, while others have light traffic. For directors of busy and crowded EDs, the findings provide "an opportunity to get people out a lot sooner," said Dr. Udelson, chief of the cardiology division at Tufts Medical Center in Boston.
Half of patients who presented to the ED with symptoms suggestive of ACS and who underwent CCTA were discharged within 8.6 hours. In contrast, it took more than a day (26.7 hours) for half of the patients in the standard-evaluation group to be discharged. "If you’re in a supercrowded ED, that’s really worth something," he said.
The researchers did not measure additional follow-up in this study beyond major events that may have happened within 30 days. However, "one of the things about CT is that you identify early disease. You can potentially be comfortable that it doesn’t have anything to do with the chest pain." Primary care physicians should know about this early disease, in order to potentially start or change treatment.
One important question is what the yield is of subsequent testing following CCTA, said Dr. Udelson. "We’ll try to define the characteristics of the CT that mean that you’re not going to find anything else and not to test further."
In an accompanying editorial, Dr. Rita F. Redberg asserted that "with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided" (N. Engl. J. Med. 2012;367:375-6). Dr. Redberg is a professor of medicine and the director of Women’s Cardiovascular Services at the University of California, San Francisco. She is also on the editorial board of Cardiology News.
However, Dr. Udelson pointed out that "ED physicians struggle with this. They’re on the firing line. It’s their heads if they make a wrong decision."
"That’s our potential next step. ... Almost a quarter of the patients in the control group had no imaging tests. In other words, the physicians felt comfortable enough to discharge these patients with no [additional] testing." They will try to determine which individuals can safely go home and which patients need additional testing.
This study was supported by grants from the National Institutes of Health. Dr. Udelson reported that he is on the scientific advisory board of Lantheus Medical Imaging. Several of the coauthors reported financial ties to imaging and/or pharmaceutical companies and professional organizations.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Pretreatment ASPECTS Reading Affects Stroke Outcomes
SAN DIEGO – Interim results from an ongoing study demonstrated that that a higher pretreatment Alberta Stroke Program Early CT Score on computed tomography angiogram images is associated with better outcome following endovascular therapy.
"There is no standard imaging approach for endovascular therapy patient selection," Dr. Donald Frei said at the annual meeting of the Society of Neurointerventional Surgery. "We’re trying to improve time from door to CT imaging and time from imaging to groin puncture, but we also need to be a little bit more sophisticated about patient selection. That’s what we tried to do in this study."
For the analysis, Dr. Frei, director of neurointerventional surgery for Radiology Imaging Associates/Swedish Medical Center in Denver, and his associates at 15 centers evaluated the influence of pretreatment ASPECTS from CTA source image on outcomes following endovascular therapy in the START (Stroke Treatment and Revascularization Therapy) trial, a prospective, single-arm multicenter trial that set out to study the influence of pretreatment core infarct size in 147 patients undergoing endovascular stroke therapy with the Penumbra system.
Imaging methods were at the direction of each investigator and included noncontrast CT, CTA-SI (CTA source images), CT perfusion, or MRI diffuse imaging. The current analysis focused on the preliminary CTA-SI results. ASPECTS was graded in a blinded fashion and analyzed according to a prior classification (0-4, 5-7, or 8-10) and the entire scale. Clinical outcomes were dichotomized as 90-day modified Rankin Scale (mRS) scores of 0-2 (good) vs. 3-6.
Dr. Frei reported interim results from 77 patients who met study criteria. Their mean age was 66 years, 56% were women, and their mean National Institutes of Health Stroke Scale score was 19. The majority of target vessel occlusions were in the middle cerebral artery (75.3%), followed by internal carotid artery (22.1%), and other areas (2.6%). (Dr. Frei noted that results from all 147 patients are expected to be presented at the upcoming International Stroke Conference.)
The median pre-ASPECTS on CTA-SI was 6. Of the 77 patients, 20 (26%) had a score of 0-4, 43 (56%) had a score of 5-7, and 14 (18%) had a score of 8-10.
Dr. Frei, who is also a member of the SNIS Executive Committee, reported that the rate of TIMI (Thrombolysis in Myocardial Infarction) 2-3 revascularization was 85.3%, the median time from groin puncture to aspiration discontinuation was 71.5 minutes, and 48.1% of patients achieved a good 90-day clinical outcome.
The mortality rate was 28.6%, and 32.5% suffered from intracranial hemorrhage. Of these, 20.8% were asymptomatic.
In general, the higher the pretreatment ASPECTS on CTA-SI, the better the outcome. For example, the rate of good outcomes was 20% for those with a pretreatment ASPECTS of 0-4, 56% for 5-7, and 64% for 8-10 (P = .08 for all). After adjusting for age and stroke severity, the researchers determined that a pre-ASPECTS score of 5-10 was an independent predictor of good outcome (odds ratio, 6.8; P = .006).
Univariate analysis demonstrated the following significant predictors of good outcomes: pretreatment ASPECTS greater than 4 (P = .0043), younger age (P = .01), lower pretreatment NIHSS (P = .04), shorter time from groin puncture to discontinuation of aspiration (P = .0004), and revascularization time (P = .0001).
In a prepared statement, Dr. Frei noted that although thousands of men and women suffer a stroke every day, "only a small percentage of those affected are treated with endovascular therapy. This study strongly suggests that a simple ASPECTS reading from a fast, easy-to-obtain CTA source image can guide patient selection for endovascular therapy, particularly those most likely to benefit from the Penumbra System" beyond the 3- to 4.5-hour window.
The START trial was sponsored by Penumbra Inc.
Dr. Frei said that he had no relevant financial disclosures to make.
SAN DIEGO – Interim results from an ongoing study demonstrated that that a higher pretreatment Alberta Stroke Program Early CT Score on computed tomography angiogram images is associated with better outcome following endovascular therapy.
"There is no standard imaging approach for endovascular therapy patient selection," Dr. Donald Frei said at the annual meeting of the Society of Neurointerventional Surgery. "We’re trying to improve time from door to CT imaging and time from imaging to groin puncture, but we also need to be a little bit more sophisticated about patient selection. That’s what we tried to do in this study."
For the analysis, Dr. Frei, director of neurointerventional surgery for Radiology Imaging Associates/Swedish Medical Center in Denver, and his associates at 15 centers evaluated the influence of pretreatment ASPECTS from CTA source image on outcomes following endovascular therapy in the START (Stroke Treatment and Revascularization Therapy) trial, a prospective, single-arm multicenter trial that set out to study the influence of pretreatment core infarct size in 147 patients undergoing endovascular stroke therapy with the Penumbra system.
Imaging methods were at the direction of each investigator and included noncontrast CT, CTA-SI (CTA source images), CT perfusion, or MRI diffuse imaging. The current analysis focused on the preliminary CTA-SI results. ASPECTS was graded in a blinded fashion and analyzed according to a prior classification (0-4, 5-7, or 8-10) and the entire scale. Clinical outcomes were dichotomized as 90-day modified Rankin Scale (mRS) scores of 0-2 (good) vs. 3-6.
Dr. Frei reported interim results from 77 patients who met study criteria. Their mean age was 66 years, 56% were women, and their mean National Institutes of Health Stroke Scale score was 19. The majority of target vessel occlusions were in the middle cerebral artery (75.3%), followed by internal carotid artery (22.1%), and other areas (2.6%). (Dr. Frei noted that results from all 147 patients are expected to be presented at the upcoming International Stroke Conference.)
The median pre-ASPECTS on CTA-SI was 6. Of the 77 patients, 20 (26%) had a score of 0-4, 43 (56%) had a score of 5-7, and 14 (18%) had a score of 8-10.
Dr. Frei, who is also a member of the SNIS Executive Committee, reported that the rate of TIMI (Thrombolysis in Myocardial Infarction) 2-3 revascularization was 85.3%, the median time from groin puncture to aspiration discontinuation was 71.5 minutes, and 48.1% of patients achieved a good 90-day clinical outcome.
The mortality rate was 28.6%, and 32.5% suffered from intracranial hemorrhage. Of these, 20.8% were asymptomatic.
In general, the higher the pretreatment ASPECTS on CTA-SI, the better the outcome. For example, the rate of good outcomes was 20% for those with a pretreatment ASPECTS of 0-4, 56% for 5-7, and 64% for 8-10 (P = .08 for all). After adjusting for age and stroke severity, the researchers determined that a pre-ASPECTS score of 5-10 was an independent predictor of good outcome (odds ratio, 6.8; P = .006).
Univariate analysis demonstrated the following significant predictors of good outcomes: pretreatment ASPECTS greater than 4 (P = .0043), younger age (P = .01), lower pretreatment NIHSS (P = .04), shorter time from groin puncture to discontinuation of aspiration (P = .0004), and revascularization time (P = .0001).
In a prepared statement, Dr. Frei noted that although thousands of men and women suffer a stroke every day, "only a small percentage of those affected are treated with endovascular therapy. This study strongly suggests that a simple ASPECTS reading from a fast, easy-to-obtain CTA source image can guide patient selection for endovascular therapy, particularly those most likely to benefit from the Penumbra System" beyond the 3- to 4.5-hour window.
The START trial was sponsored by Penumbra Inc.
Dr. Frei said that he had no relevant financial disclosures to make.
SAN DIEGO – Interim results from an ongoing study demonstrated that that a higher pretreatment Alberta Stroke Program Early CT Score on computed tomography angiogram images is associated with better outcome following endovascular therapy.
"There is no standard imaging approach for endovascular therapy patient selection," Dr. Donald Frei said at the annual meeting of the Society of Neurointerventional Surgery. "We’re trying to improve time from door to CT imaging and time from imaging to groin puncture, but we also need to be a little bit more sophisticated about patient selection. That’s what we tried to do in this study."
For the analysis, Dr. Frei, director of neurointerventional surgery for Radiology Imaging Associates/Swedish Medical Center in Denver, and his associates at 15 centers evaluated the influence of pretreatment ASPECTS from CTA source image on outcomes following endovascular therapy in the START (Stroke Treatment and Revascularization Therapy) trial, a prospective, single-arm multicenter trial that set out to study the influence of pretreatment core infarct size in 147 patients undergoing endovascular stroke therapy with the Penumbra system.
Imaging methods were at the direction of each investigator and included noncontrast CT, CTA-SI (CTA source images), CT perfusion, or MRI diffuse imaging. The current analysis focused on the preliminary CTA-SI results. ASPECTS was graded in a blinded fashion and analyzed according to a prior classification (0-4, 5-7, or 8-10) and the entire scale. Clinical outcomes were dichotomized as 90-day modified Rankin Scale (mRS) scores of 0-2 (good) vs. 3-6.
Dr. Frei reported interim results from 77 patients who met study criteria. Their mean age was 66 years, 56% were women, and their mean National Institutes of Health Stroke Scale score was 19. The majority of target vessel occlusions were in the middle cerebral artery (75.3%), followed by internal carotid artery (22.1%), and other areas (2.6%). (Dr. Frei noted that results from all 147 patients are expected to be presented at the upcoming International Stroke Conference.)
The median pre-ASPECTS on CTA-SI was 6. Of the 77 patients, 20 (26%) had a score of 0-4, 43 (56%) had a score of 5-7, and 14 (18%) had a score of 8-10.
Dr. Frei, who is also a member of the SNIS Executive Committee, reported that the rate of TIMI (Thrombolysis in Myocardial Infarction) 2-3 revascularization was 85.3%, the median time from groin puncture to aspiration discontinuation was 71.5 minutes, and 48.1% of patients achieved a good 90-day clinical outcome.
The mortality rate was 28.6%, and 32.5% suffered from intracranial hemorrhage. Of these, 20.8% were asymptomatic.
In general, the higher the pretreatment ASPECTS on CTA-SI, the better the outcome. For example, the rate of good outcomes was 20% for those with a pretreatment ASPECTS of 0-4, 56% for 5-7, and 64% for 8-10 (P = .08 for all). After adjusting for age and stroke severity, the researchers determined that a pre-ASPECTS score of 5-10 was an independent predictor of good outcome (odds ratio, 6.8; P = .006).
Univariate analysis demonstrated the following significant predictors of good outcomes: pretreatment ASPECTS greater than 4 (P = .0043), younger age (P = .01), lower pretreatment NIHSS (P = .04), shorter time from groin puncture to discontinuation of aspiration (P = .0004), and revascularization time (P = .0001).
In a prepared statement, Dr. Frei noted that although thousands of men and women suffer a stroke every day, "only a small percentage of those affected are treated with endovascular therapy. This study strongly suggests that a simple ASPECTS reading from a fast, easy-to-obtain CTA source image can guide patient selection for endovascular therapy, particularly those most likely to benefit from the Penumbra System" beyond the 3- to 4.5-hour window.
The START trial was sponsored by Penumbra Inc.
Dr. Frei said that he had no relevant financial disclosures to make.
AT THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Major Finding: After adjustment for age and stroke severity, a pretreatment ASPECTS result of 5-10 was found to be an independent predictor of good stroke outcome after endovascular intervention (OR, 6.8; P = 0.006).
Data Source: This was based on interim results from a multicenter study of 77 patients that evaluated the influence of pretreatment ASPECTS from CTA-SI on outcomes following endovascular therapy in the START trial.
Disclosures: The START trial was sponsored by Penumbra Inc. Dr. Frei said that he had no relevant financial conflicts to disclose.
A Case of Suspected Appendicitis
Hypothenar Hammer Syndrome
Closed Sagittal Band Injury Due to Low Energy Trauma
Single-Detector Polarization-Sensitive Optical Coherence Tomography for Assessment of Rotator Cuff Tendon Integrity
Moving In on Invasive Coronary Angiography
Potentially practice-changing new techniques for improving cardiovascular CT imaging quality were hot topics at this years meeting of the Society of Cardiovascular Computed Tomography. Here’s a rundown of techniques that you can expect to see more frequently.
Fractional Flow Reserve CT
One problem with coronary CT angiography (CCTA) has been that it does not define the hemodynamic significance of coronary lesions. Cardiologists have relied on fractional flow reserve (FFR) measured at the time of invasive coronary angiography to determine specifically the hemodynamic significance of coronary artery lesions (lesion-specific ischemia). FFR is defined as the ratio of maximal myocardial flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. Values less than or equal to 0.80 or 0.75 are considered to be diagnostic of lesion-specific ischemia. Assessment of lesion-specific ischemia improves event-free survival.
CT FFR uses some very sophisticated and complex computational methods which are applied to data from a normal CCTA. This allows cardiologists to quantify the FFR for each lesion seen on CCTA with the data taken from the same image. The result is that they are able to identify which stenoses are causing ischemia and should be treated – all noninvasively.
Dual-Source CT
Calcium and motion artifacts have long been a bane to cardiologists and radiologists. Calcium plaques have been shown to appear larger on CCTA. When calcium plaque volume is overestimated, luminal diameter is underestimated and the percentage of diameter stenosis is overestimated.
Dual-source CT has recently received Food and Drug Administration 510k clearance for cardiac CT studies. Basically the detector switches very quickly between two energies, improving the clarity of image of calcium plaque (reducing artifacts) and increasing accuracy.
Snapshot Freeze
Coronary motion can occur at high and low heart rates, resulting in both false positives and false negatives. SnapShot Freeze was developed to help significantly reduce coronary motion. By precisely detecting vessel motion and velocity, the SnapShot Freeze algorithm can determine actual vessel position and corrects the effects of motion during cardiac CT exams. The reduction of coronary motion artifacts increases interpretability and improves accuracy.
CT Perfusion
The assessment of the luminal coronary artery narrowing with CCTA has been a poor predictor of myocardial ischemia and has required additional perfusion imaging to identify patients who might benefit from revascularization.
Several trials have shown that CT perfusion imaging has a high sensitivity and negative predictive value when compared against SPECT. CT perfusion also appears to be an affective technique for noninvasively evaluating patients with abnormal CT scans. Data are expected next year from several multicenter clinical trials.
--By Kerri Wachter (on twitter @knwachter)
Potentially practice-changing new techniques for improving cardiovascular CT imaging quality were hot topics at this years meeting of the Society of Cardiovascular Computed Tomography. Here’s a rundown of techniques that you can expect to see more frequently.
Fractional Flow Reserve CT
One problem with coronary CT angiography (CCTA) has been that it does not define the hemodynamic significance of coronary lesions. Cardiologists have relied on fractional flow reserve (FFR) measured at the time of invasive coronary angiography to determine specifically the hemodynamic significance of coronary artery lesions (lesion-specific ischemia). FFR is defined as the ratio of maximal myocardial flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. Values less than or equal to 0.80 or 0.75 are considered to be diagnostic of lesion-specific ischemia. Assessment of lesion-specific ischemia improves event-free survival.
CT FFR uses some very sophisticated and complex computational methods which are applied to data from a normal CCTA. This allows cardiologists to quantify the FFR for each lesion seen on CCTA with the data taken from the same image. The result is that they are able to identify which stenoses are causing ischemia and should be treated – all noninvasively.
Dual-Source CT
Calcium and motion artifacts have long been a bane to cardiologists and radiologists. Calcium plaques have been shown to appear larger on CCTA. When calcium plaque volume is overestimated, luminal diameter is underestimated and the percentage of diameter stenosis is overestimated.
Dual-source CT has recently received Food and Drug Administration 510k clearance for cardiac CT studies. Basically the detector switches very quickly between two energies, improving the clarity of image of calcium plaque (reducing artifacts) and increasing accuracy.
Snapshot Freeze
Coronary motion can occur at high and low heart rates, resulting in both false positives and false negatives. SnapShot Freeze was developed to help significantly reduce coronary motion. By precisely detecting vessel motion and velocity, the SnapShot Freeze algorithm can determine actual vessel position and corrects the effects of motion during cardiac CT exams. The reduction of coronary motion artifacts increases interpretability and improves accuracy.
CT Perfusion
The assessment of the luminal coronary artery narrowing with CCTA has been a poor predictor of myocardial ischemia and has required additional perfusion imaging to identify patients who might benefit from revascularization.
Several trials have shown that CT perfusion imaging has a high sensitivity and negative predictive value when compared against SPECT. CT perfusion also appears to be an affective technique for noninvasively evaluating patients with abnormal CT scans. Data are expected next year from several multicenter clinical trials.
--By Kerri Wachter (on twitter @knwachter)
Potentially practice-changing new techniques for improving cardiovascular CT imaging quality were hot topics at this years meeting of the Society of Cardiovascular Computed Tomography. Here’s a rundown of techniques that you can expect to see more frequently.
Fractional Flow Reserve CT
One problem with coronary CT angiography (CCTA) has been that it does not define the hemodynamic significance of coronary lesions. Cardiologists have relied on fractional flow reserve (FFR) measured at the time of invasive coronary angiography to determine specifically the hemodynamic significance of coronary artery lesions (lesion-specific ischemia). FFR is defined as the ratio of maximal myocardial flow through a diseased artery to the blood flow in the hypothetical case that this artery is normal. Values less than or equal to 0.80 or 0.75 are considered to be diagnostic of lesion-specific ischemia. Assessment of lesion-specific ischemia improves event-free survival.
CT FFR uses some very sophisticated and complex computational methods which are applied to data from a normal CCTA. This allows cardiologists to quantify the FFR for each lesion seen on CCTA with the data taken from the same image. The result is that they are able to identify which stenoses are causing ischemia and should be treated – all noninvasively.
Dual-Source CT
Calcium and motion artifacts have long been a bane to cardiologists and radiologists. Calcium plaques have been shown to appear larger on CCTA. When calcium plaque volume is overestimated, luminal diameter is underestimated and the percentage of diameter stenosis is overestimated.
Dual-source CT has recently received Food and Drug Administration 510k clearance for cardiac CT studies. Basically the detector switches very quickly between two energies, improving the clarity of image of calcium plaque (reducing artifacts) and increasing accuracy.
Snapshot Freeze
Coronary motion can occur at high and low heart rates, resulting in both false positives and false negatives. SnapShot Freeze was developed to help significantly reduce coronary motion. By precisely detecting vessel motion and velocity, the SnapShot Freeze algorithm can determine actual vessel position and corrects the effects of motion during cardiac CT exams. The reduction of coronary motion artifacts increases interpretability and improves accuracy.
CT Perfusion
The assessment of the luminal coronary artery narrowing with CCTA has been a poor predictor of myocardial ischemia and has required additional perfusion imaging to identify patients who might benefit from revascularization.
Several trials have shown that CT perfusion imaging has a high sensitivity and negative predictive value when compared against SPECT. CT perfusion also appears to be an affective technique for noninvasively evaluating patients with abnormal CT scans. Data are expected next year from several multicenter clinical trials.
--By Kerri Wachter (on twitter @knwachter)
CTA Tracks Plaque Volume Changes With Statin Therapy
BALTIMORE – Computed tomographic angiography can accurately and noninvasively measure the changes in overall and composition-specific plaque volume as a result of statin therapy.
At 1.2 years’ follow-up, there was a significant 38% decrease in total plaque volume in individuals on statin therapy compared with patients not on statin therapy. This difference remained significant after adjustment for age, gender, and conventional risk factors. Significant changes in noncalcified volume (a 73% decrease) and mixed-plaque volume (a 10% decrease) also were seen in those on statins compared with the nonstatin group. In addition, calcified plaque remained relatively stable, decreasing by 3.5% in the statin therapy group compared with the nonstatin group.
"Statin therapy was associated with a significant decrease in plaque volume, especially in noncalcified plaque volumes, and it was more prominent in women," Dr. Vahid Nabavi said at the annual meeting of the Society of Cardiovascular Computed Tomography.
Several cardiovascular imaging studies revealed that progression of coronary plaque volume over time is an independent predictor of cardiovascular mortality. Intravascular ultrasound (IVUS) provides high-resolution images capable of revealing early preclinical coronary artery disease. However, it is a highly invasive and expensive technique, and will be used only in conjunction with complex coronary interventions, noted Dr. Nabavi, who is a research fellow at the Los Angeles Biomedical Research Institute at Harbor–University of California, Los Angeles, Medical Center.
Quantitative measurements of coronary plaque made with cardiovascular CT angiography (CTA) correlate well with plaque measurements made using IVUS. Low-density noncalcified plaque on CTA correlates with necrotic core plus fibrofatty tissue on IVUS. CTA could be a less expensive, noninvasive alternative to IVUS, particularly for measuring changes in plaque associated with therapy, Dr. Nabavi noted.
In this study, 107 patients underwent serial, clinically indicated CTAs. Their mean age was 67 years, and 81% were men. The median follow-up was 1.2 years. The researchers collected data on risk factors, statin therapy, and laboratory findings.
They quantitatively measured the change in indexed total and composition-specific plaque volume of the target segment with luminal stenosis less than 50% in patients on statin therapy (40 mg of atorvastatin daily) or those with lifestyle changes only.
At baseline, there were no significant differences between groups in age, gender, clinical demographics, risk factors, or total and composition-specific plaque volumes. After adjustment, decreases in overall, mixed, calcified, and noncalcified plaque volumes between those on statins and those not on statins were 56%, 12%, 43%, and 144%. "More robust changes were seen in women," Dr. Nabavi said.
Dr. Nabavi did not report whether he had any conflicts of interest.
BALTIMORE – Computed tomographic angiography can accurately and noninvasively measure the changes in overall and composition-specific plaque volume as a result of statin therapy.
At 1.2 years’ follow-up, there was a significant 38% decrease in total plaque volume in individuals on statin therapy compared with patients not on statin therapy. This difference remained significant after adjustment for age, gender, and conventional risk factors. Significant changes in noncalcified volume (a 73% decrease) and mixed-plaque volume (a 10% decrease) also were seen in those on statins compared with the nonstatin group. In addition, calcified plaque remained relatively stable, decreasing by 3.5% in the statin therapy group compared with the nonstatin group.
"Statin therapy was associated with a significant decrease in plaque volume, especially in noncalcified plaque volumes, and it was more prominent in women," Dr. Vahid Nabavi said at the annual meeting of the Society of Cardiovascular Computed Tomography.
Several cardiovascular imaging studies revealed that progression of coronary plaque volume over time is an independent predictor of cardiovascular mortality. Intravascular ultrasound (IVUS) provides high-resolution images capable of revealing early preclinical coronary artery disease. However, it is a highly invasive and expensive technique, and will be used only in conjunction with complex coronary interventions, noted Dr. Nabavi, who is a research fellow at the Los Angeles Biomedical Research Institute at Harbor–University of California, Los Angeles, Medical Center.
Quantitative measurements of coronary plaque made with cardiovascular CT angiography (CTA) correlate well with plaque measurements made using IVUS. Low-density noncalcified plaque on CTA correlates with necrotic core plus fibrofatty tissue on IVUS. CTA could be a less expensive, noninvasive alternative to IVUS, particularly for measuring changes in plaque associated with therapy, Dr. Nabavi noted.
In this study, 107 patients underwent serial, clinically indicated CTAs. Their mean age was 67 years, and 81% were men. The median follow-up was 1.2 years. The researchers collected data on risk factors, statin therapy, and laboratory findings.
They quantitatively measured the change in indexed total and composition-specific plaque volume of the target segment with luminal stenosis less than 50% in patients on statin therapy (40 mg of atorvastatin daily) or those with lifestyle changes only.
At baseline, there were no significant differences between groups in age, gender, clinical demographics, risk factors, or total and composition-specific plaque volumes. After adjustment, decreases in overall, mixed, calcified, and noncalcified plaque volumes between those on statins and those not on statins were 56%, 12%, 43%, and 144%. "More robust changes were seen in women," Dr. Nabavi said.
Dr. Nabavi did not report whether he had any conflicts of interest.
BALTIMORE – Computed tomographic angiography can accurately and noninvasively measure the changes in overall and composition-specific plaque volume as a result of statin therapy.
At 1.2 years’ follow-up, there was a significant 38% decrease in total plaque volume in individuals on statin therapy compared with patients not on statin therapy. This difference remained significant after adjustment for age, gender, and conventional risk factors. Significant changes in noncalcified volume (a 73% decrease) and mixed-plaque volume (a 10% decrease) also were seen in those on statins compared with the nonstatin group. In addition, calcified plaque remained relatively stable, decreasing by 3.5% in the statin therapy group compared with the nonstatin group.
"Statin therapy was associated with a significant decrease in plaque volume, especially in noncalcified plaque volumes, and it was more prominent in women," Dr. Vahid Nabavi said at the annual meeting of the Society of Cardiovascular Computed Tomography.
Several cardiovascular imaging studies revealed that progression of coronary plaque volume over time is an independent predictor of cardiovascular mortality. Intravascular ultrasound (IVUS) provides high-resolution images capable of revealing early preclinical coronary artery disease. However, it is a highly invasive and expensive technique, and will be used only in conjunction with complex coronary interventions, noted Dr. Nabavi, who is a research fellow at the Los Angeles Biomedical Research Institute at Harbor–University of California, Los Angeles, Medical Center.
Quantitative measurements of coronary plaque made with cardiovascular CT angiography (CTA) correlate well with plaque measurements made using IVUS. Low-density noncalcified plaque on CTA correlates with necrotic core plus fibrofatty tissue on IVUS. CTA could be a less expensive, noninvasive alternative to IVUS, particularly for measuring changes in plaque associated with therapy, Dr. Nabavi noted.
In this study, 107 patients underwent serial, clinically indicated CTAs. Their mean age was 67 years, and 81% were men. The median follow-up was 1.2 years. The researchers collected data on risk factors, statin therapy, and laboratory findings.
They quantitatively measured the change in indexed total and composition-specific plaque volume of the target segment with luminal stenosis less than 50% in patients on statin therapy (40 mg of atorvastatin daily) or those with lifestyle changes only.
At baseline, there were no significant differences between groups in age, gender, clinical demographics, risk factors, or total and composition-specific plaque volumes. After adjustment, decreases in overall, mixed, calcified, and noncalcified plaque volumes between those on statins and those not on statins were 56%, 12%, 43%, and 144%. "More robust changes were seen in women," Dr. Nabavi said.
Dr. Nabavi did not report whether he had any conflicts of interest.
AT THE ANNUAL MEETING OF THE SOCIETY OF CARDIOVASCULAR COMPUTED TOMOGRAPHY