User login
Survey finds Black, Hispanic patients may prefer race-concordant dermatologists, highlighting opportunities for changes in education and practice
, according to a patient survey.
In the survey, 42% of self-identified Black patients and 44% of self-identified Hispanic patients assigned some level of importance to the race or ethnicity of their dermatologist. Of patients self-identified as White, the figure was 2%, which was significantly lower (P less than .001).
Responses to the survey indicated that there is concern among non-White patients that White physicians are not fully sensitive to the clinical issues presented by their skin type. For example, 22% of Hispanic patients and 21% of Black patients agreed that a race-concordant physician would be better trained to treat their skin.
The results of the survey were recently published in a Research Letter in the Journal of the American Academy of Dermatology.
When patients were asked to agree or disagree with the statement that non-White patients receive the same quality of care as White patients, about a third disagreed, “but about half said they were unsure, which I interpret basically as a negative answer,” reported the lead author, Adam Friedman, MD, professor and interim chair of the department of dermatology at George Washington University, Washington.
“These data are a call to action. Certainly, we need to diversify our workforce to mirror the overall population, but we can also do more to improve training for dermatologic diseases across skin types,” Dr. Friedman said in an interview.
“Ensuring all skin types are represented in all dermatologic education, from resident book clubs to the national stage is but one step to making dermatology more inclusive and prepared to care for all patients,” he added.
Ninety-two patients receiving dermatology care at Dr. Friedman’s institution completed the survey. Fifty identified themselves as White, nine as Hispanic, and 33 as Black. Allowing patients to self-identify race was an important feature of this survey, according to Dr. Friedman.
“Something I really struggle with is terminology. Are race and ethnicity the appropriate terms when discussing different skin types and tones? It is so easy to misuse even validated tools. The Fitzpatrick Scale, for example, requires patients to relay how easily they burn, but reveals nothing about how patients refer to their skin tone,” Dr. Friedman explained. “We need to reset how we characterize and categorize skin types.”
Among those who assigned at least some importance to having a dermatologist of the same race or ethnicity, the most common reason was that such physicians “are better able to listen and relate to me.” Thirty percent of Black patients and 22% of Hispanic patients agreed with this statement. The perception that such physicians are better trained to treat non-White skin was the next most common reason.
The results of the survey emphasize the importance of ensuring that there is comprehensive training in managing all skin types and that physicians receive rigorous implicit bias and cultural sensitivity training in order to win patient trust, according to Dr. Friedman. He suggested that the perception that White physicians might not provide optimal care to non-White patients by study participants “has some validity. Structural racism in medicine is well-documented, and dermatologists have already begun to combat this on several fronts.”
In fact, the process of conducting and analyzing data from this survey proved to be its own lesson in sociocultural sensitivity, he said.
After a draft completed peer review and was accepted for publication, Dr. Friedman was confronted with numerous criticisms of the language that was used. In particular, one of his former residents, Misty Eleryan, MD, who is now a Mohs Fellow at the University of California, Los Angeles, was instrumental in pointing out problems. Ultimately, he withdrew the paper to rephrase the findings.
“It was not until then that I also learned that there is a JAAD Sensitivity Workgroup, which was very helpful in identifying issues we had overlooked,” Dr. Friedman said. For example, he had used the term “minorities” for non-White populations, which is not only inaccurate in many situations but has a pejorative undertone.
“It is important to recognize that the impact is more important than the intention,” said Dr. Friedman, who reported that he learned a lot in this process.
It is the need for this type of augmented sensitivity that the survey underscores, he added. He called for cultural sensitivity to be part of medical training to undo unrecognized bias, and said, “We need to understand how our patients perceive us.”
SOURCE: Friedman A et al. J Am Acad Dermatol. 2020 Sep 16;S0190-9622(20)32620-7. doi: 10.1016/j.jaad.2020.09.032.
, according to a patient survey.
In the survey, 42% of self-identified Black patients and 44% of self-identified Hispanic patients assigned some level of importance to the race or ethnicity of their dermatologist. Of patients self-identified as White, the figure was 2%, which was significantly lower (P less than .001).
Responses to the survey indicated that there is concern among non-White patients that White physicians are not fully sensitive to the clinical issues presented by their skin type. For example, 22% of Hispanic patients and 21% of Black patients agreed that a race-concordant physician would be better trained to treat their skin.
The results of the survey were recently published in a Research Letter in the Journal of the American Academy of Dermatology.
When patients were asked to agree or disagree with the statement that non-White patients receive the same quality of care as White patients, about a third disagreed, “but about half said they were unsure, which I interpret basically as a negative answer,” reported the lead author, Adam Friedman, MD, professor and interim chair of the department of dermatology at George Washington University, Washington.
“These data are a call to action. Certainly, we need to diversify our workforce to mirror the overall population, but we can also do more to improve training for dermatologic diseases across skin types,” Dr. Friedman said in an interview.
“Ensuring all skin types are represented in all dermatologic education, from resident book clubs to the national stage is but one step to making dermatology more inclusive and prepared to care for all patients,” he added.
Ninety-two patients receiving dermatology care at Dr. Friedman’s institution completed the survey. Fifty identified themselves as White, nine as Hispanic, and 33 as Black. Allowing patients to self-identify race was an important feature of this survey, according to Dr. Friedman.
“Something I really struggle with is terminology. Are race and ethnicity the appropriate terms when discussing different skin types and tones? It is so easy to misuse even validated tools. The Fitzpatrick Scale, for example, requires patients to relay how easily they burn, but reveals nothing about how patients refer to their skin tone,” Dr. Friedman explained. “We need to reset how we characterize and categorize skin types.”
Among those who assigned at least some importance to having a dermatologist of the same race or ethnicity, the most common reason was that such physicians “are better able to listen and relate to me.” Thirty percent of Black patients and 22% of Hispanic patients agreed with this statement. The perception that such physicians are better trained to treat non-White skin was the next most common reason.
The results of the survey emphasize the importance of ensuring that there is comprehensive training in managing all skin types and that physicians receive rigorous implicit bias and cultural sensitivity training in order to win patient trust, according to Dr. Friedman. He suggested that the perception that White physicians might not provide optimal care to non-White patients by study participants “has some validity. Structural racism in medicine is well-documented, and dermatologists have already begun to combat this on several fronts.”
In fact, the process of conducting and analyzing data from this survey proved to be its own lesson in sociocultural sensitivity, he said.
After a draft completed peer review and was accepted for publication, Dr. Friedman was confronted with numerous criticisms of the language that was used. In particular, one of his former residents, Misty Eleryan, MD, who is now a Mohs Fellow at the University of California, Los Angeles, was instrumental in pointing out problems. Ultimately, he withdrew the paper to rephrase the findings.
“It was not until then that I also learned that there is a JAAD Sensitivity Workgroup, which was very helpful in identifying issues we had overlooked,” Dr. Friedman said. For example, he had used the term “minorities” for non-White populations, which is not only inaccurate in many situations but has a pejorative undertone.
“It is important to recognize that the impact is more important than the intention,” said Dr. Friedman, who reported that he learned a lot in this process.
It is the need for this type of augmented sensitivity that the survey underscores, he added. He called for cultural sensitivity to be part of medical training to undo unrecognized bias, and said, “We need to understand how our patients perceive us.”
SOURCE: Friedman A et al. J Am Acad Dermatol. 2020 Sep 16;S0190-9622(20)32620-7. doi: 10.1016/j.jaad.2020.09.032.
, according to a patient survey.
In the survey, 42% of self-identified Black patients and 44% of self-identified Hispanic patients assigned some level of importance to the race or ethnicity of their dermatologist. Of patients self-identified as White, the figure was 2%, which was significantly lower (P less than .001).
Responses to the survey indicated that there is concern among non-White patients that White physicians are not fully sensitive to the clinical issues presented by their skin type. For example, 22% of Hispanic patients and 21% of Black patients agreed that a race-concordant physician would be better trained to treat their skin.
The results of the survey were recently published in a Research Letter in the Journal of the American Academy of Dermatology.
When patients were asked to agree or disagree with the statement that non-White patients receive the same quality of care as White patients, about a third disagreed, “but about half said they were unsure, which I interpret basically as a negative answer,” reported the lead author, Adam Friedman, MD, professor and interim chair of the department of dermatology at George Washington University, Washington.
“These data are a call to action. Certainly, we need to diversify our workforce to mirror the overall population, but we can also do more to improve training for dermatologic diseases across skin types,” Dr. Friedman said in an interview.
“Ensuring all skin types are represented in all dermatologic education, from resident book clubs to the national stage is but one step to making dermatology more inclusive and prepared to care for all patients,” he added.
Ninety-two patients receiving dermatology care at Dr. Friedman’s institution completed the survey. Fifty identified themselves as White, nine as Hispanic, and 33 as Black. Allowing patients to self-identify race was an important feature of this survey, according to Dr. Friedman.
“Something I really struggle with is terminology. Are race and ethnicity the appropriate terms when discussing different skin types and tones? It is so easy to misuse even validated tools. The Fitzpatrick Scale, for example, requires patients to relay how easily they burn, but reveals nothing about how patients refer to their skin tone,” Dr. Friedman explained. “We need to reset how we characterize and categorize skin types.”
Among those who assigned at least some importance to having a dermatologist of the same race or ethnicity, the most common reason was that such physicians “are better able to listen and relate to me.” Thirty percent of Black patients and 22% of Hispanic patients agreed with this statement. The perception that such physicians are better trained to treat non-White skin was the next most common reason.
The results of the survey emphasize the importance of ensuring that there is comprehensive training in managing all skin types and that physicians receive rigorous implicit bias and cultural sensitivity training in order to win patient trust, according to Dr. Friedman. He suggested that the perception that White physicians might not provide optimal care to non-White patients by study participants “has some validity. Structural racism in medicine is well-documented, and dermatologists have already begun to combat this on several fronts.”
In fact, the process of conducting and analyzing data from this survey proved to be its own lesson in sociocultural sensitivity, he said.
After a draft completed peer review and was accepted for publication, Dr. Friedman was confronted with numerous criticisms of the language that was used. In particular, one of his former residents, Misty Eleryan, MD, who is now a Mohs Fellow at the University of California, Los Angeles, was instrumental in pointing out problems. Ultimately, he withdrew the paper to rephrase the findings.
“It was not until then that I also learned that there is a JAAD Sensitivity Workgroup, which was very helpful in identifying issues we had overlooked,” Dr. Friedman said. For example, he had used the term “minorities” for non-White populations, which is not only inaccurate in many situations but has a pejorative undertone.
“It is important to recognize that the impact is more important than the intention,” said Dr. Friedman, who reported that he learned a lot in this process.
It is the need for this type of augmented sensitivity that the survey underscores, he added. He called for cultural sensitivity to be part of medical training to undo unrecognized bias, and said, “We need to understand how our patients perceive us.”
SOURCE: Friedman A et al. J Am Acad Dermatol. 2020 Sep 16;S0190-9622(20)32620-7. doi: 10.1016/j.jaad.2020.09.032.
Equitable Post-COVID-19 Care: A Practical Framework to Integrate Health Equity in Diabetes Management
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
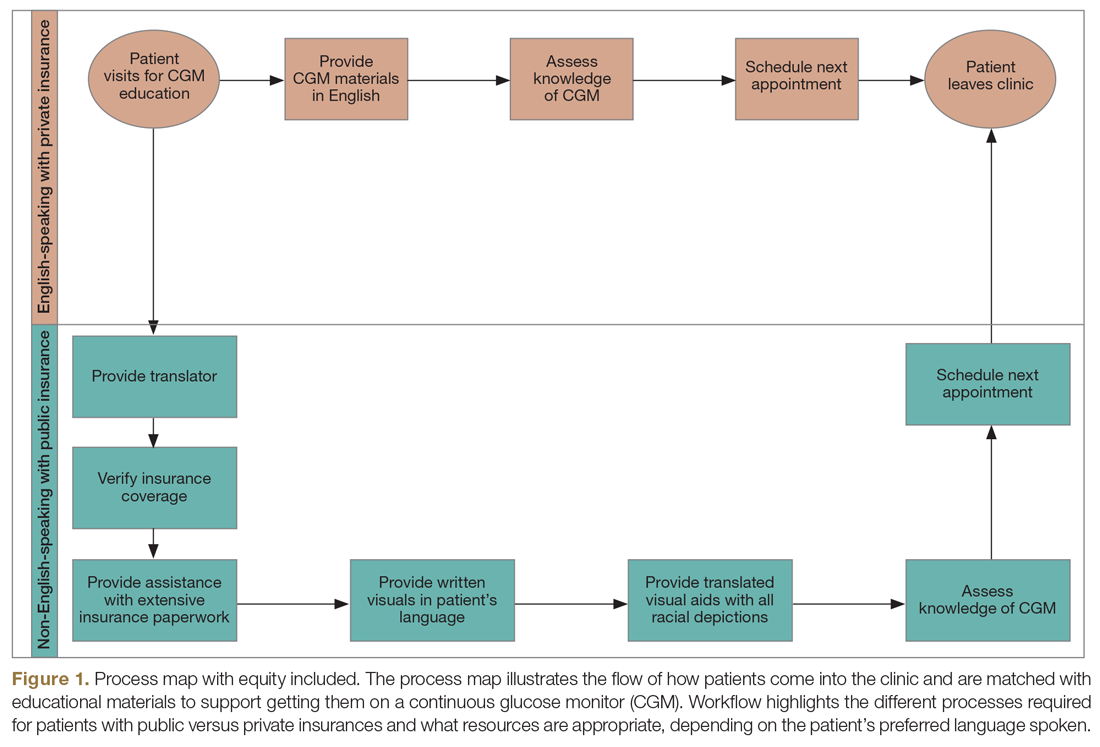
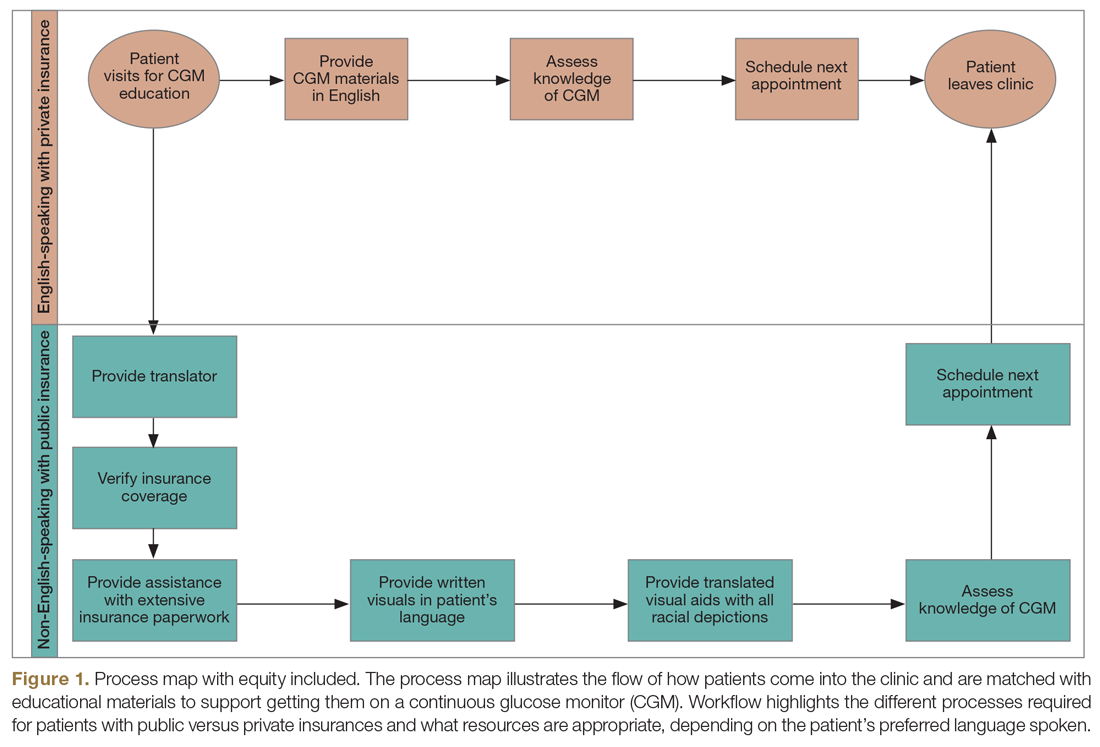
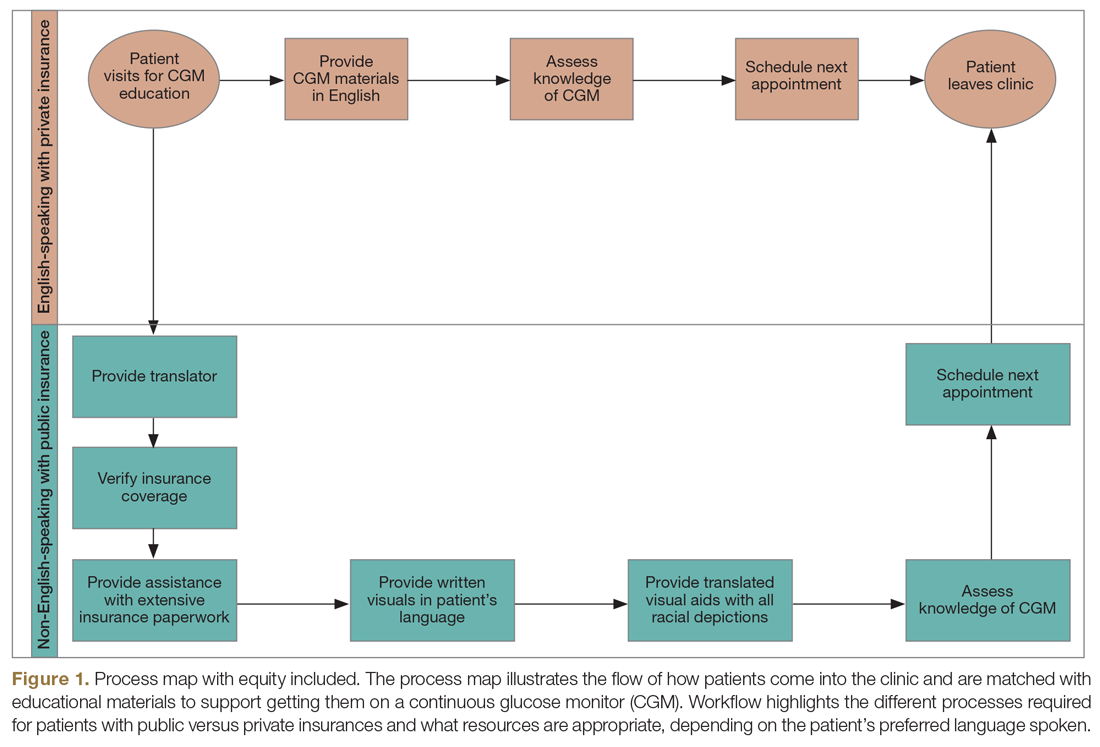
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
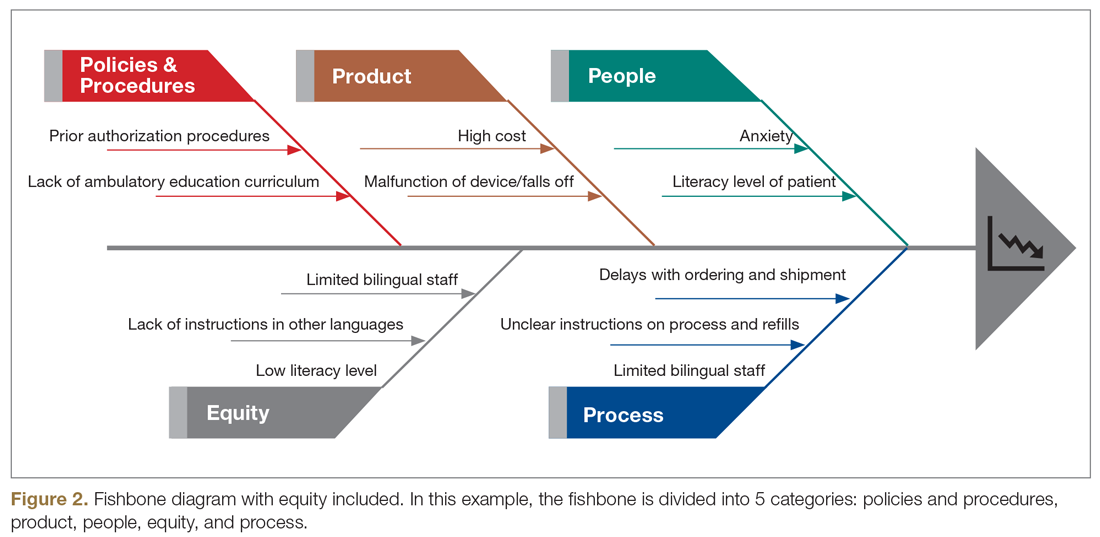
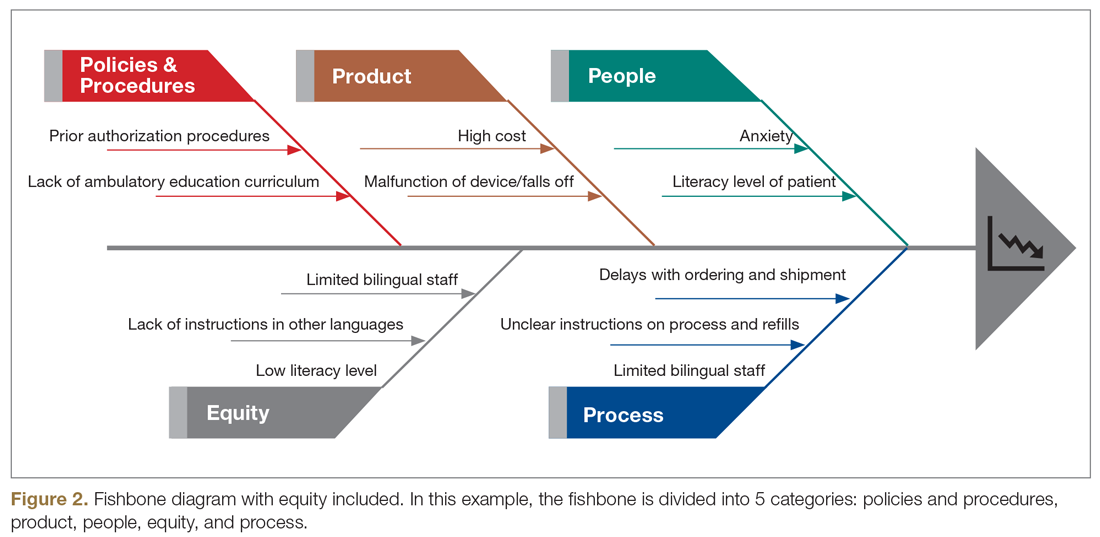
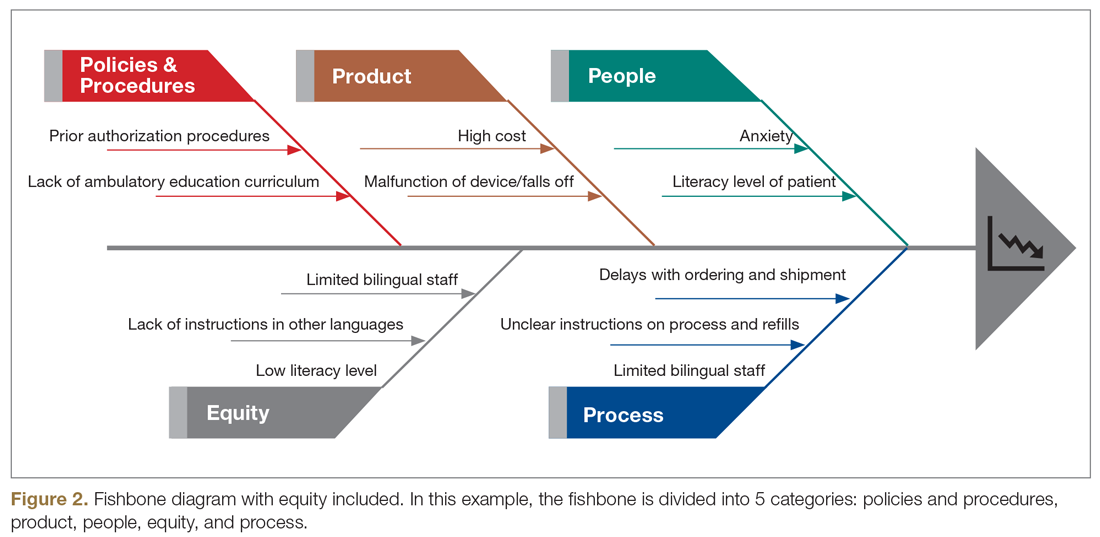
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; [email protected].
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; [email protected].
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
From T1D Exchange, Boston, MA (Dr. Ebekozien, Dr. Odugbesan, and Nicole Rioles); Barbara Davis Center, University of Colorado, Boulder, CO (Dr. Majidi); Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (Dr. Jones); and Nationwide Children’s Hospital, Columbus, OH (Dr. Kamboj)
Health equity has been described as the opportunity for all persons to obtain their highest level of health possible.1 Unfortunately, even with advances in technology and care practices, disparities persist in health care outcomes. Disparities in prevalence, prognosis, and outcomes still exist in diabetes management.2 Non-Hispanic Black and/or Hispanic populations are more likely to have worse glycemic control,3,4 to encounter more barriers in access to care,5 and to have higher levels of acute complications,4 and to use advanced technologies less frequently.4 Diabetes is one of the preexisting conditions that increase morbidity and mortality in COVID-19.6,7 Unfortunately, adverse outcomes from COVID-19 also disproportionately impact a specific vulnerable population.8,9 The urgent transition to managing diabetes remotely during the COVID-19 pandemic may exacerbate long-term inequities because some vulnerable patients might not have access to technology devices necessary for effective remote management.
Here, we describe how quality improvement (QI) tools and principles can be adapted into a framework for advancing health equity. Specifically, we describe a 10-step framework that may be applied in diabetes care management to achieve improvement, using a hypothetical example of increasing use of continuous glucose monitors (CGMs) among patients with type 1 diabetes mellitus.10 This framework was developed to address the literature gap on practical ways health care providers can address inequities using QI principles, and was implemented by 1 of the authors at a local public health department.11 The framework’s iterative and comprehensive design makes it ideal for addressing inequities in chronic diseases like diabetes, which have multiple root causes with no easy solutions. The improvement program pilot received a national model practice award.11,12
10-Step Framework
Step 1: Review program/project baseline data for existing disparities. Diabetes programs and routine QI processes encourage existing data review to determine how effective the current system is working and if the existing process has a predictable pattern.13,14 Our equity-revised framework proposes a more in-depth review to stratify baseline data based on factors that might contribute to inequities, including race, age, income levels, ethnicity, language, sexual orientation, insurance type, and zip code. This process will identify patients not served or unfairly impacted due to socioeconomic factors. For example, using the hypothetical example of improving CGM use, a team completes a preliminary data review and determines that baseline CGM use is 30% in the clinic population. However, in a review to assess for disparities, they also identify that patients on public insurance have a significantly lower CGM uptake of only 15%.
Step 2: Build an equitable project team, including patients with lived experiences. Routine projects typically have clinicians, administrative staff, and analytic staff as members of their team. In a post-COVID-19 world, every team needs to learn directly from people impacted and share decision-making power. The traditional approach to receiving feedback has generally been to collect responses using surveys or focus groups. We propose that individuals/families who are disproportionately impacted be included as active members on QI teams. For example, in the hypothetical example of the CGM project, team members would include patients with type 1 diabetes who are on public insurance and their families.
Step 3: Develop equity-focused goals. The traditional program involves the development of aims that are SMART (specific, measurable, achievable, realistic, time-bound).15 The proposed framework encourages the inclusion of equity-revised goals (SMARTer) using insights from Steps 1 and 2. For example, your typical smart goal might be to increase the percentage of patients using CGM by 20% in 6 months, while a SMARTer goal would be to increase the proportion of patients using CGM by 20% and reduce the disparities among public and private insurance patients by 30% in 6 months.
Step 4: Identify inequitable processes/pathways. Traditional QI programs might use a process map or flow diagram to depict the current state of a process visually.16 For example, in Figure 1, the process map diagram depicts some differences in the process for patients with public insurance as opposed to those with private insurance. The framework also advocates for using visual tools like process maps to depict how there might be inequitable pathways in a system. Visually identifying inequitable processes/pathways can help a team see barriers, address challenges, and pilot innovative solutions.
Step 5: Identify how socioeconomic factors are contributing to the current outcome. A good understanding of factors that contribute to the problem is an essential part of finding fundamental solutions. The fishbone diagram16 is a visualization tool used to identify contributing factors. When investigating contributing factors, it is commonplace to identify factors that fit into 1 of 5 categories: people, process, place, product, and policies (5 Ps). An equity-focused process will include equity as a new major factor category, and the socioeconomic impacts that contribute to inequities will be brainstormed and visually represented. For example, in the hypothetical CGM improvement example, an equity contributing factor is extensive CGM application paperwork for patients on public insurance as compared to those on private insurance. Figure 2 shows equity integrated into a fishbone diagram.
Step 6: Brainstorm possible improvements. Potential improvement ideas for the hypothetical CGM example might include redesigning the existing workflow, piloting CGM educational classes, and using a CGM barrier assessment tool to identify and address barriers to adoption.
Step 7: Use the decision matrix with equity as a criterion to prioritize improvement ideas. Decision matrix15 is a great tool that is frequently used to help teams prioritize potential ideas. Project team members must decide what criteria are important in prioritizing ideas to implement. Common criteria include implementation cost, time, and resources, but in addition to the common criteria, the team can specify ”impact on equity” as one of their criteria, alongside other standard criteria like impact.
Step 8: Test one small change at a time. This step is consistent with other traditional improvement models using the Plan, Do, Study, Act (PDSA) model for improvement.17 During this phase, the team should make predictions on the expected impact of the intervention on outcomes. For example, in the hypothetical example, the team predicts that testing and expanding CGM classes will reduce disparities among public versus private health insurance users by 5% and increase overall CGM uptake by 10%.
Step 9: Measure and compare results with predictions to identify inequitable practices or consequences. After each test of change, the team should review the results, including implementation cost considerations, and compare them to the predictions in the earlier step. The team should also document the potential reasons why their predictions were correct or inaccurate, and whether there were any unforeseen outcomes from the intervention.
Step 10: Celebrate small wins and repeat the process. Making fundamental and equitable changes takes time. This framework aimed at undoing inequities, particularly those inequities that have been amplified by the COVID-19 pandemic, is iterative and ongoing.18,19 Not every test of change will impact the outcome or reduce inequity, but over time, each change will impact the next, generating sustainable effects.
Conclusion
There are ongoing studies examining the adverse outcomes and potential health inequities for patients with diabetes impacted by COVID-19.20 Health care providers need to plan for post-COVID-19 care, keeping in mind that the pandemic might worsen already existing health disparities in diabetes management.3,4,21 This work will involve an intentional approach to address structural and systemic racism.22 Therefore, the work of building health equity solutions must be rooted in racial justice, economic equity, and equitable access to health care and education.
Initiatives like this are currently being funded through foundation grants as well as state and federal research or program grants. Regional and national payors, including the Centers for Medicare & Medicaid Services, are currently piloting long-term sustainable funding models through programs like accountable care organizations and the Accountable Health Communities Model.23
Health systems can successfully address health equity and racial justice, using a framework as described above, to identify determinants of health, develop policies to expand access to care for the most vulnerable patients, distribute decision-making power, and train staff by naming structural racism as a driver of health inequities.
Acknowledgment: The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1D Exchange Quality Improvement Collaborative, who continually seek to improve care and outcomes for people living with diabetes.
Corresponding author: Osagie Ebekozien, MD, 11 Avenue De La Fayette, Boston, MA 02115; [email protected].
Financial disclosures: None.
Funding: T1D Exchange QI Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust. No specific funding was received for this manuscript or the development of this framework.
Keywords: type 1 diabetes; quality improvement; QI framework; racial justice; health disparities.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
1. American Public Health Association Health Equity web site. https://www.apha.org/topics-and-issues/health-equity. Accessed June 4, 2020.
2. Lado J, Lipman T. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am. 2016;45:453-461.
3. Kahkoska AR, Shay CM, Crandell J, et al. Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open. 2018;1:e181851.
4. Willi SM, Miller KM, DiMeglio LA, et al; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434.
5. Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164:1369-1375.
6. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142.
7. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020;382:2012-2022.
8. Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398-402.
9. Shah M, Sachdeva M, Dodiuk-Gad RP. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35.
10. Ebekozien O, Rioles N, DeSalvo D, et al. Improving continuous glucose monitoring (CGM) use across national centers: results from the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Diabetes. 2020;69(Supplement 1):145-LB.
11. Ebekozien O. QI methodology to address health equity. Presented at American Society of Quality BOSCON 2018; Boston, MA; March 19 and 20, 2018.
12. 2019 Model Practice Award, Building A Culture of Improvement. National Association of County and City Health Officials web site. www.naccho.org/membership/awards/model-practices. Accessed June 4, 2020.
13. Nuckols TK, Keeler E, Anderson LJ, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41:985‐993.
14. Rossi MC, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166‐2168.
15. McQuillan RF, Silver SA, Harel Z, et al. How to measure and interpret quality improvement data. Clin J Am Soc Nephrol. 2016;11:908-914.
16. Siddiqi FS. Quality improvement in diabetes care: time for us to step up? Can J Diabetes. 2019;43:233.
17. Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290‐298.
18. Ferdinand KC, Nasser SA. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746-2748..
19. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318:E736-E741.
20. Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83-e85.
21. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes among patients in the T1D Exchange-QI Collaborative. Diabetes. 2020;69(Supplement 1):1220-P. https://doi.org/10.2337/ db20-1220.-P.
22. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20-47.
23. Centers for Medicare & Medicaid Services. Accountable Health Communities Model. CMS.gov web site. https://innovation.cms.gov/innovation-models/ahcm. Accessed October 10, 2020.
AMA takes on vaccine misinformation, physician vaccines, racism
The American Medical Association House of Delegates has adopted a policy to educate physicians on how to speak with patients about COVID-19 vaccination to counteract widespread misinformation about the vaccine development process.
Other highlights of the AMA’s recent special meeting include a new policy on the ethics of physicians getting immunized against COVID-19 and a far-reaching statement about racism.
Under the organization’s new vaccination education policy, the AMA will provide physicians with “culturally appropriate patient education materials,” according to a news release.
This campaign will be conducted “bearing in mind the historical context of ‘experimentation’ with vaccines and other medication in communities of color,” the AMA said, apparently alluding to the infamous Tuskegee study of syphilis in Black men.
Educating the public about the safety and efficacy of the COVID-19 vaccine programs is an “urgent priority,” the AMA said. This is especially true among populations that have been disproportionately affected by the disease. Black and Latino people are being hospitalized for COVID-19 at far higher rates than White Americans.
“Under the new policy, the AMA will help address patient concerns, dispel misinformation, and build confidence in COVID-19 vaccination,” the release states. The AMA also plans to build a coalition of health care and public health organizations to develop and implement a joint public education program.
Polls have indicated that many people will not get vaccinated when supplies of the new COVID-19 vaccines are available, although public support is rising. A recent Gallup poll found that 58% of surveyed adults were willing to be inoculated, up from 50% in September.
A Kaiser Family Foundation survey in September found that a majority of Americans were skeptical of a rushed vaccine, because they were concerned that the Trump administration was pressuring the Food and Drug Administration to approve a vaccine before the election.
“Given the unprecedented situation with COVID-19 and with vaccine development moving at a rapid pace, many of our patients and the public have questions and concerns,” said AMA President Susan R. Bailey, MD, in the release. “It is essential that we speak together as a strong, unified voice across health care and public health, inclusive of organizations respected in communities of color; to use scientific, fact-based evidence to help allay public concerns; and build confidence in COVID-19 vaccine candidates that are determined to be safe and effective.”
Physician, immunize thyself
The AMA also adopted a new ethics policy about physician immunization. On Monday, the AMA House of Delegates stated that physicians who are not immunized from a vaccine-preventable disease have an ethical responsibility to take appropriate actions to protect patients and colleagues.
The AMA code of ethics has long maintained that physicians have a strong ethical duty to accept immunizations when a safe, effective vaccine is available. However, the organization said in a news release, “it is not ethically problematic to exempt individuals when a specific vaccine poses a risk due to underlying medical conditions.”
Ethical concerns arise when physicians are allowed to decline vaccinations for nonmedical reasons, according to a report presented to the House of Delegates by the AMA Council on Ethical and Judicial Affairs.
According to the newly amended AMA ethical guidance, “physicians who are not or cannot be immunized have a responsibility to voluntarily take appropriate actions to protect patients, fellow health care workers and others.” This includes refraining from direct patient contact.
The delegates also approved a guidance asserting that physician practices and health care institutions are responsible for developing policies and procedures for responding to pandemics and epidemics. These policies and procedures should outline appropriate protective equipment allocation, staff immunization programs, and infection control practices.
Combating systemic racism
In an effort to reduce racial disparities in healthcare, the AMA House of Delegates adopted new policies recognizing race as a social construct, rather than a biological construct.
“The policies aim to advance data-driven, antiracist concepts challenging the current clinical application of race and its effects on vulnerable patient populations,” an AMA statement said.
The new AMA policies “reflect an understanding of race as a socially constructed category different from ethnicity, genetic ancestry, or biology, and aim to end the misinterpretation of race as a biological category defined by genetic traits or biological differences,” the AMA said.
According to the AMA, the practice of accepting race as a biological construct “exacerbates health disparities and results in detrimental health outcomes for marginalized and minoritized communities.”
Specifically, the AMA said it supports ending the practice of using race as a proxy for biology in medical education, research, and clinical practice. It also encourages medical education programs to recognize the harmful effects of this approach. It recommends that clinicians and researchers focus on genetics and biology, the experience of racism, and social determinants of health when describing risk factors for disease.
“The AMA is dedicated to dismantling racist and discriminatory policies and practices across all of health care, and that includes the way we define race in medicine,” said AMA board member Michael Suk, MD, in its statement. “We believe it is not sufficient for medicine to be nonracist, which is why the AMA is committed to pushing for a shift in thinking from race as a biological risk factor to a deeper understanding of racism as a determinant of health.”
The AMA also plans to partner with physician organizations and other stakeholders “to identify any problematic aspects of medical education that may perpetuate institutional and structural racism.” For example, the AMA will work with other organizations to improve clinical algorithms that incorrectly adjust for race and lead to less-than-optimal care for minority patients.
A version of this article originally appeared on Medscape.com.
The American Medical Association House of Delegates has adopted a policy to educate physicians on how to speak with patients about COVID-19 vaccination to counteract widespread misinformation about the vaccine development process.
Other highlights of the AMA’s recent special meeting include a new policy on the ethics of physicians getting immunized against COVID-19 and a far-reaching statement about racism.
Under the organization’s new vaccination education policy, the AMA will provide physicians with “culturally appropriate patient education materials,” according to a news release.
This campaign will be conducted “bearing in mind the historical context of ‘experimentation’ with vaccines and other medication in communities of color,” the AMA said, apparently alluding to the infamous Tuskegee study of syphilis in Black men.
Educating the public about the safety and efficacy of the COVID-19 vaccine programs is an “urgent priority,” the AMA said. This is especially true among populations that have been disproportionately affected by the disease. Black and Latino people are being hospitalized for COVID-19 at far higher rates than White Americans.
“Under the new policy, the AMA will help address patient concerns, dispel misinformation, and build confidence in COVID-19 vaccination,” the release states. The AMA also plans to build a coalition of health care and public health organizations to develop and implement a joint public education program.
Polls have indicated that many people will not get vaccinated when supplies of the new COVID-19 vaccines are available, although public support is rising. A recent Gallup poll found that 58% of surveyed adults were willing to be inoculated, up from 50% in September.
A Kaiser Family Foundation survey in September found that a majority of Americans were skeptical of a rushed vaccine, because they were concerned that the Trump administration was pressuring the Food and Drug Administration to approve a vaccine before the election.
“Given the unprecedented situation with COVID-19 and with vaccine development moving at a rapid pace, many of our patients and the public have questions and concerns,” said AMA President Susan R. Bailey, MD, in the release. “It is essential that we speak together as a strong, unified voice across health care and public health, inclusive of organizations respected in communities of color; to use scientific, fact-based evidence to help allay public concerns; and build confidence in COVID-19 vaccine candidates that are determined to be safe and effective.”
Physician, immunize thyself
The AMA also adopted a new ethics policy about physician immunization. On Monday, the AMA House of Delegates stated that physicians who are not immunized from a vaccine-preventable disease have an ethical responsibility to take appropriate actions to protect patients and colleagues.
The AMA code of ethics has long maintained that physicians have a strong ethical duty to accept immunizations when a safe, effective vaccine is available. However, the organization said in a news release, “it is not ethically problematic to exempt individuals when a specific vaccine poses a risk due to underlying medical conditions.”
Ethical concerns arise when physicians are allowed to decline vaccinations for nonmedical reasons, according to a report presented to the House of Delegates by the AMA Council on Ethical and Judicial Affairs.
According to the newly amended AMA ethical guidance, “physicians who are not or cannot be immunized have a responsibility to voluntarily take appropriate actions to protect patients, fellow health care workers and others.” This includes refraining from direct patient contact.
The delegates also approved a guidance asserting that physician practices and health care institutions are responsible for developing policies and procedures for responding to pandemics and epidemics. These policies and procedures should outline appropriate protective equipment allocation, staff immunization programs, and infection control practices.
Combating systemic racism
In an effort to reduce racial disparities in healthcare, the AMA House of Delegates adopted new policies recognizing race as a social construct, rather than a biological construct.
“The policies aim to advance data-driven, antiracist concepts challenging the current clinical application of race and its effects on vulnerable patient populations,” an AMA statement said.
The new AMA policies “reflect an understanding of race as a socially constructed category different from ethnicity, genetic ancestry, or biology, and aim to end the misinterpretation of race as a biological category defined by genetic traits or biological differences,” the AMA said.
According to the AMA, the practice of accepting race as a biological construct “exacerbates health disparities and results in detrimental health outcomes for marginalized and minoritized communities.”
Specifically, the AMA said it supports ending the practice of using race as a proxy for biology in medical education, research, and clinical practice. It also encourages medical education programs to recognize the harmful effects of this approach. It recommends that clinicians and researchers focus on genetics and biology, the experience of racism, and social determinants of health when describing risk factors for disease.
“The AMA is dedicated to dismantling racist and discriminatory policies and practices across all of health care, and that includes the way we define race in medicine,” said AMA board member Michael Suk, MD, in its statement. “We believe it is not sufficient for medicine to be nonracist, which is why the AMA is committed to pushing for a shift in thinking from race as a biological risk factor to a deeper understanding of racism as a determinant of health.”
The AMA also plans to partner with physician organizations and other stakeholders “to identify any problematic aspects of medical education that may perpetuate institutional and structural racism.” For example, the AMA will work with other organizations to improve clinical algorithms that incorrectly adjust for race and lead to less-than-optimal care for minority patients.
A version of this article originally appeared on Medscape.com.
The American Medical Association House of Delegates has adopted a policy to educate physicians on how to speak with patients about COVID-19 vaccination to counteract widespread misinformation about the vaccine development process.
Other highlights of the AMA’s recent special meeting include a new policy on the ethics of physicians getting immunized against COVID-19 and a far-reaching statement about racism.
Under the organization’s new vaccination education policy, the AMA will provide physicians with “culturally appropriate patient education materials,” according to a news release.
This campaign will be conducted “bearing in mind the historical context of ‘experimentation’ with vaccines and other medication in communities of color,” the AMA said, apparently alluding to the infamous Tuskegee study of syphilis in Black men.
Educating the public about the safety and efficacy of the COVID-19 vaccine programs is an “urgent priority,” the AMA said. This is especially true among populations that have been disproportionately affected by the disease. Black and Latino people are being hospitalized for COVID-19 at far higher rates than White Americans.
“Under the new policy, the AMA will help address patient concerns, dispel misinformation, and build confidence in COVID-19 vaccination,” the release states. The AMA also plans to build a coalition of health care and public health organizations to develop and implement a joint public education program.
Polls have indicated that many people will not get vaccinated when supplies of the new COVID-19 vaccines are available, although public support is rising. A recent Gallup poll found that 58% of surveyed adults were willing to be inoculated, up from 50% in September.
A Kaiser Family Foundation survey in September found that a majority of Americans were skeptical of a rushed vaccine, because they were concerned that the Trump administration was pressuring the Food and Drug Administration to approve a vaccine before the election.
“Given the unprecedented situation with COVID-19 and with vaccine development moving at a rapid pace, many of our patients and the public have questions and concerns,” said AMA President Susan R. Bailey, MD, in the release. “It is essential that we speak together as a strong, unified voice across health care and public health, inclusive of organizations respected in communities of color; to use scientific, fact-based evidence to help allay public concerns; and build confidence in COVID-19 vaccine candidates that are determined to be safe and effective.”
Physician, immunize thyself
The AMA also adopted a new ethics policy about physician immunization. On Monday, the AMA House of Delegates stated that physicians who are not immunized from a vaccine-preventable disease have an ethical responsibility to take appropriate actions to protect patients and colleagues.
The AMA code of ethics has long maintained that physicians have a strong ethical duty to accept immunizations when a safe, effective vaccine is available. However, the organization said in a news release, “it is not ethically problematic to exempt individuals when a specific vaccine poses a risk due to underlying medical conditions.”
Ethical concerns arise when physicians are allowed to decline vaccinations for nonmedical reasons, according to a report presented to the House of Delegates by the AMA Council on Ethical and Judicial Affairs.
According to the newly amended AMA ethical guidance, “physicians who are not or cannot be immunized have a responsibility to voluntarily take appropriate actions to protect patients, fellow health care workers and others.” This includes refraining from direct patient contact.
The delegates also approved a guidance asserting that physician practices and health care institutions are responsible for developing policies and procedures for responding to pandemics and epidemics. These policies and procedures should outline appropriate protective equipment allocation, staff immunization programs, and infection control practices.
Combating systemic racism
In an effort to reduce racial disparities in healthcare, the AMA House of Delegates adopted new policies recognizing race as a social construct, rather than a biological construct.
“The policies aim to advance data-driven, antiracist concepts challenging the current clinical application of race and its effects on vulnerable patient populations,” an AMA statement said.
The new AMA policies “reflect an understanding of race as a socially constructed category different from ethnicity, genetic ancestry, or biology, and aim to end the misinterpretation of race as a biological category defined by genetic traits or biological differences,” the AMA said.
According to the AMA, the practice of accepting race as a biological construct “exacerbates health disparities and results in detrimental health outcomes for marginalized and minoritized communities.”
Specifically, the AMA said it supports ending the practice of using race as a proxy for biology in medical education, research, and clinical practice. It also encourages medical education programs to recognize the harmful effects of this approach. It recommends that clinicians and researchers focus on genetics and biology, the experience of racism, and social determinants of health when describing risk factors for disease.
“The AMA is dedicated to dismantling racist and discriminatory policies and practices across all of health care, and that includes the way we define race in medicine,” said AMA board member Michael Suk, MD, in its statement. “We believe it is not sufficient for medicine to be nonracist, which is why the AMA is committed to pushing for a shift in thinking from race as a biological risk factor to a deeper understanding of racism as a determinant of health.”
The AMA also plans to partner with physician organizations and other stakeholders “to identify any problematic aspects of medical education that may perpetuate institutional and structural racism.” For example, the AMA will work with other organizations to improve clinical algorithms that incorrectly adjust for race and lead to less-than-optimal care for minority patients.
A version of this article originally appeared on Medscape.com.
Employment protections now include sexual orientation, but our role in LGBTQIA+ equality continues
The state of Tennessee, where I worked and attended medical school, did not have legislation in place prohibiting termination of employment based on sexual orientation alone. As a lesbian, I never felt safe at work knowing that I could be fired at any time simply because of who I loved and how I identified. When I started medical school in rural Appalachia, I decided I would be “out” but remained cautious. That meant inspecting everyone I encountered for signs of acceptance and safety before sharing details about my life. As a third-year medical student, I started wearing a rainbow triangle on my white coat. One of the first patients I cared for cried and thanked me for wearing the pin. She then proceeded to tell me about her partner, her own struggles with depression, and the secrets she had to keep from her community. It was overwhelming and, yet, so familiar. I was struck by how wearing this pin, a small gesture, made this patient feel safe enough to come out to me and seek help for her depression. Although I found a supportive community in Tennessee, it was only after I moved to Massachusetts for residency—where antidiscrimination laws protected lesbian, gay, bisexual, transgender, queer/questioning, intersex, asexual, plus all other gender and sexual minority (LGBTQIA+) identified people—did I feel safe to freely share about my partner and our life together.
A landmark decision in the Supreme Court
This past June, in a 6 to 3 decision, the US Supreme Court ruled in the case of Bostock v Clayton County that Title VII’s ban on discrimination also protects LGBTQIA+ employees. Title VII is a federal law that protects employees from discrimination based on race, color, national origin, sex, and religion.1 In this decision, the court determined that “sex” cannot be differentiated from sexual orientation. Justice Neil Gorsuch, who wrote the majority opinion, stated, “It is impossible… to discriminate against a person for being homosexual or transgender without discriminating against that individual based on sex.”2 Title VII not only protects employees in hiring and firing practices but also protects against harassment and retaliation. Prior to this ruling, there were no federal antidiscrimination laws for LGBTQIA+ individuals, and only 22 states and the District of Columbia had laws in place that specified antidiscrimination protection for this community.3 Because of this landmark decision, Title VII now protects all employees in all states from discrimination, including due to an individual’s sexual orientation.
This is a huge victory in the battle for equality; however, the fight is not over. Justice Gorsuch stated, “We do not purport to address bathrooms, locker rooms or anything else of the kind…whether other policies and practices might or might not qualify as unlawful discrimination or find justifications under other provisions of Title VII are questions for future cases, not these.”2 This victory sets a new precedent and will continue to be further defined with more court cases as states and employers push back against these protections.
Continue to: A worrying shift in the Court...
A worrying shift in the Court
We have already started to see the repercussions of this ruling from Supreme Court justices themselves. Justice Clarence Thomas, who dissented in the Obergefell v Hodges decision in 2015, which established the constitutional right for marriage equality, recently wrote a petition to have the Supreme Court reconsider that ruling. He wrote “Obergefell enables courts and governments to brand religious adherents who believe that marriage is between one man and one woman as bigots, making their religious liberty concerns that much easier to dismiss.”3 After the passing of Justice Ruth Bader Ginsburg, the Supreme Court became decidedly more conservative with the appointment of Judge Amy Coney Barrett, whose mentor was the late Justice Antonin Scalia, who also dissented in the 2015 case.
As we celebrate this huge win for equality in this June decision, we also must recognize that LGBTQIA+ rights are still at risk.
LGBTQIA+ patients at higher risk for litany of conditions
Even with the Bostock v Clayton County ruling, we must not forget that discrimination will continue to exist. As health care providers, we have a responsibility to advocate on behalf of our LGBTQIA+ colleagues and patients. According to the Healthy People 2020 survey, there are higher rates of obesity, tobacco dependence, and sexually transmitted infection, as well as lower adherence to cancer screening recommendations in the LGBTQIA+ community.4 These disparities are a result of systemic, legal, and social factors, including limited access to affirming and inclusive health care.5 The LGBTQIA+ community deserves better.
Take action
In the coming months and years, as the US Supreme Court hears more cases that will threaten the rights of the LGBTQIA+ community, I challenge all clinicians to take action. Even the smallest of gestures, such as wearing a rainbow pin, can be transformative for our patients and within our communities.
- Advocate for your state to enact nondiscrimination laws protecting the LGBTQIA+ community. Find out if your state has a law.
- Support your LGBTQIA+ colleagues by establishing an employee support group.
- Educate yourself and your colleagues on LGBTQIA+ inclusive medical practices.
- US Equal Employment Opportunity Commission. Title VII of the Civil Rights Act of 1964. https://www.eeoc.gov/statutes/title-vii-civil-rights-act-1964. Accessed November 4, 2020.
- Bostock v Clayton County, 590 US ___ (2020).
- Petition for Writ of Certiorari, Clarence Thomas. October 2020. https://www.supremecourt.gov/orders/courtorders/100520zor_3204.pdf. Accessed November 11, 2020.
- US Department of Health and Human Services. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. Accessed November 4, 2020.
- Ard KL, Makadon HJ. Improving the health of lesbian, gay, bisexual and transgender people: understanding and eliminating health disparities. The National LGBT Health Education Center website. https://www.lgbtqiahealtheducation.org/wp-content/uploads/Improving-the-Health-of-LGBT-People.pdf. Accessed November 4, 2020.
The state of Tennessee, where I worked and attended medical school, did not have legislation in place prohibiting termination of employment based on sexual orientation alone. As a lesbian, I never felt safe at work knowing that I could be fired at any time simply because of who I loved and how I identified. When I started medical school in rural Appalachia, I decided I would be “out” but remained cautious. That meant inspecting everyone I encountered for signs of acceptance and safety before sharing details about my life. As a third-year medical student, I started wearing a rainbow triangle on my white coat. One of the first patients I cared for cried and thanked me for wearing the pin. She then proceeded to tell me about her partner, her own struggles with depression, and the secrets she had to keep from her community. It was overwhelming and, yet, so familiar. I was struck by how wearing this pin, a small gesture, made this patient feel safe enough to come out to me and seek help for her depression. Although I found a supportive community in Tennessee, it was only after I moved to Massachusetts for residency—where antidiscrimination laws protected lesbian, gay, bisexual, transgender, queer/questioning, intersex, asexual, plus all other gender and sexual minority (LGBTQIA+) identified people—did I feel safe to freely share about my partner and our life together.
A landmark decision in the Supreme Court
This past June, in a 6 to 3 decision, the US Supreme Court ruled in the case of Bostock v Clayton County that Title VII’s ban on discrimination also protects LGBTQIA+ employees. Title VII is a federal law that protects employees from discrimination based on race, color, national origin, sex, and religion.1 In this decision, the court determined that “sex” cannot be differentiated from sexual orientation. Justice Neil Gorsuch, who wrote the majority opinion, stated, “It is impossible… to discriminate against a person for being homosexual or transgender without discriminating against that individual based on sex.”2 Title VII not only protects employees in hiring and firing practices but also protects against harassment and retaliation. Prior to this ruling, there were no federal antidiscrimination laws for LGBTQIA+ individuals, and only 22 states and the District of Columbia had laws in place that specified antidiscrimination protection for this community.3 Because of this landmark decision, Title VII now protects all employees in all states from discrimination, including due to an individual’s sexual orientation.
This is a huge victory in the battle for equality; however, the fight is not over. Justice Gorsuch stated, “We do not purport to address bathrooms, locker rooms or anything else of the kind…whether other policies and practices might or might not qualify as unlawful discrimination or find justifications under other provisions of Title VII are questions for future cases, not these.”2 This victory sets a new precedent and will continue to be further defined with more court cases as states and employers push back against these protections.
Continue to: A worrying shift in the Court...
A worrying shift in the Court
We have already started to see the repercussions of this ruling from Supreme Court justices themselves. Justice Clarence Thomas, who dissented in the Obergefell v Hodges decision in 2015, which established the constitutional right for marriage equality, recently wrote a petition to have the Supreme Court reconsider that ruling. He wrote “Obergefell enables courts and governments to brand religious adherents who believe that marriage is between one man and one woman as bigots, making their religious liberty concerns that much easier to dismiss.”3 After the passing of Justice Ruth Bader Ginsburg, the Supreme Court became decidedly more conservative with the appointment of Judge Amy Coney Barrett, whose mentor was the late Justice Antonin Scalia, who also dissented in the 2015 case.
As we celebrate this huge win for equality in this June decision, we also must recognize that LGBTQIA+ rights are still at risk.
LGBTQIA+ patients at higher risk for litany of conditions
Even with the Bostock v Clayton County ruling, we must not forget that discrimination will continue to exist. As health care providers, we have a responsibility to advocate on behalf of our LGBTQIA+ colleagues and patients. According to the Healthy People 2020 survey, there are higher rates of obesity, tobacco dependence, and sexually transmitted infection, as well as lower adherence to cancer screening recommendations in the LGBTQIA+ community.4 These disparities are a result of systemic, legal, and social factors, including limited access to affirming and inclusive health care.5 The LGBTQIA+ community deserves better.
Take action
In the coming months and years, as the US Supreme Court hears more cases that will threaten the rights of the LGBTQIA+ community, I challenge all clinicians to take action. Even the smallest of gestures, such as wearing a rainbow pin, can be transformative for our patients and within our communities.
- Advocate for your state to enact nondiscrimination laws protecting the LGBTQIA+ community. Find out if your state has a law.
- Support your LGBTQIA+ colleagues by establishing an employee support group.
- Educate yourself and your colleagues on LGBTQIA+ inclusive medical practices.
The state of Tennessee, where I worked and attended medical school, did not have legislation in place prohibiting termination of employment based on sexual orientation alone. As a lesbian, I never felt safe at work knowing that I could be fired at any time simply because of who I loved and how I identified. When I started medical school in rural Appalachia, I decided I would be “out” but remained cautious. That meant inspecting everyone I encountered for signs of acceptance and safety before sharing details about my life. As a third-year medical student, I started wearing a rainbow triangle on my white coat. One of the first patients I cared for cried and thanked me for wearing the pin. She then proceeded to tell me about her partner, her own struggles with depression, and the secrets she had to keep from her community. It was overwhelming and, yet, so familiar. I was struck by how wearing this pin, a small gesture, made this patient feel safe enough to come out to me and seek help for her depression. Although I found a supportive community in Tennessee, it was only after I moved to Massachusetts for residency—where antidiscrimination laws protected lesbian, gay, bisexual, transgender, queer/questioning, intersex, asexual, plus all other gender and sexual minority (LGBTQIA+) identified people—did I feel safe to freely share about my partner and our life together.
A landmark decision in the Supreme Court
This past June, in a 6 to 3 decision, the US Supreme Court ruled in the case of Bostock v Clayton County that Title VII’s ban on discrimination also protects LGBTQIA+ employees. Title VII is a federal law that protects employees from discrimination based on race, color, national origin, sex, and religion.1 In this decision, the court determined that “sex” cannot be differentiated from sexual orientation. Justice Neil Gorsuch, who wrote the majority opinion, stated, “It is impossible… to discriminate against a person for being homosexual or transgender without discriminating against that individual based on sex.”2 Title VII not only protects employees in hiring and firing practices but also protects against harassment and retaliation. Prior to this ruling, there were no federal antidiscrimination laws for LGBTQIA+ individuals, and only 22 states and the District of Columbia had laws in place that specified antidiscrimination protection for this community.3 Because of this landmark decision, Title VII now protects all employees in all states from discrimination, including due to an individual’s sexual orientation.
This is a huge victory in the battle for equality; however, the fight is not over. Justice Gorsuch stated, “We do not purport to address bathrooms, locker rooms or anything else of the kind…whether other policies and practices might or might not qualify as unlawful discrimination or find justifications under other provisions of Title VII are questions for future cases, not these.”2 This victory sets a new precedent and will continue to be further defined with more court cases as states and employers push back against these protections.
Continue to: A worrying shift in the Court...
A worrying shift in the Court
We have already started to see the repercussions of this ruling from Supreme Court justices themselves. Justice Clarence Thomas, who dissented in the Obergefell v Hodges decision in 2015, which established the constitutional right for marriage equality, recently wrote a petition to have the Supreme Court reconsider that ruling. He wrote “Obergefell enables courts and governments to brand religious adherents who believe that marriage is between one man and one woman as bigots, making their religious liberty concerns that much easier to dismiss.”3 After the passing of Justice Ruth Bader Ginsburg, the Supreme Court became decidedly more conservative with the appointment of Judge Amy Coney Barrett, whose mentor was the late Justice Antonin Scalia, who also dissented in the 2015 case.
As we celebrate this huge win for equality in this June decision, we also must recognize that LGBTQIA+ rights are still at risk.
LGBTQIA+ patients at higher risk for litany of conditions
Even with the Bostock v Clayton County ruling, we must not forget that discrimination will continue to exist. As health care providers, we have a responsibility to advocate on behalf of our LGBTQIA+ colleagues and patients. According to the Healthy People 2020 survey, there are higher rates of obesity, tobacco dependence, and sexually transmitted infection, as well as lower adherence to cancer screening recommendations in the LGBTQIA+ community.4 These disparities are a result of systemic, legal, and social factors, including limited access to affirming and inclusive health care.5 The LGBTQIA+ community deserves better.
Take action
In the coming months and years, as the US Supreme Court hears more cases that will threaten the rights of the LGBTQIA+ community, I challenge all clinicians to take action. Even the smallest of gestures, such as wearing a rainbow pin, can be transformative for our patients and within our communities.
- Advocate for your state to enact nondiscrimination laws protecting the LGBTQIA+ community. Find out if your state has a law.
- Support your LGBTQIA+ colleagues by establishing an employee support group.
- Educate yourself and your colleagues on LGBTQIA+ inclusive medical practices.
- US Equal Employment Opportunity Commission. Title VII of the Civil Rights Act of 1964. https://www.eeoc.gov/statutes/title-vii-civil-rights-act-1964. Accessed November 4, 2020.
- Bostock v Clayton County, 590 US ___ (2020).
- Petition for Writ of Certiorari, Clarence Thomas. October 2020. https://www.supremecourt.gov/orders/courtorders/100520zor_3204.pdf. Accessed November 11, 2020.
- US Department of Health and Human Services. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. Accessed November 4, 2020.
- Ard KL, Makadon HJ. Improving the health of lesbian, gay, bisexual and transgender people: understanding and eliminating health disparities. The National LGBT Health Education Center website. https://www.lgbtqiahealtheducation.org/wp-content/uploads/Improving-the-Health-of-LGBT-People.pdf. Accessed November 4, 2020.
- US Equal Employment Opportunity Commission. Title VII of the Civil Rights Act of 1964. https://www.eeoc.gov/statutes/title-vii-civil-rights-act-1964. Accessed November 4, 2020.
- Bostock v Clayton County, 590 US ___ (2020).
- Petition for Writ of Certiorari, Clarence Thomas. October 2020. https://www.supremecourt.gov/orders/courtorders/100520zor_3204.pdf. Accessed November 11, 2020.
- US Department of Health and Human Services. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. Accessed November 4, 2020.
- Ard KL, Makadon HJ. Improving the health of lesbian, gay, bisexual and transgender people: understanding and eliminating health disparities. The National LGBT Health Education Center website. https://www.lgbtqiahealtheducation.org/wp-content/uploads/Improving-the-Health-of-LGBT-People.pdf. Accessed November 4, 2020.
The case for a new skin typing system
Even though the popular classification system added skin types V and VI in 1988 to the first iteration established in 1975, it was never intended for categorizing skin color, according to Karen C. Kagha, MD.
“This topic is going to become more relevant in our clinical practices, especially when you look at the current population trends in the U.S.,” Dr. Kagha, MD, a dermatologist and cosmetic and laser fellow in the department of dermatology at Massachusetts General Hospital and a research fellow at Wellman Center for Photomedicine, both in Boston, said during a virtual course on laser and aesthetic skin therapy. “Minority groups continue to increase. According to the U.S. Census Bureau, by the year 2050, we can expect that the majority of the population will be of non-European descent.”
The original intent of the Fitzpatrick Skin Typing (FST) system was to establish a minimal erythema dose, or likelihood to burn for patients receiving phototherapy, she continued. However, a recently published survey of 141 board-certified dermatologists and trainees found that 31% of respondents said that they used the Fitzpatrick Skin Typing System to describe the patient’s race or ethnicity, 47% used it to describe the patients’ constitutive skin color, and 22% used it in both scenarios.
“There also have been inconsistencies reported with the Fitzpatrick Skin Typing System,” Dr. Kagha said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Some studies show that there are inconsistent correlations between self-reported Fitzpatrick Skin Type and burn risk, and between self-reported FST and physician-reported FST. This means that some patients self-identify differently from how their physicians identify them.” There have also been some inconsistent correlations between race and objective measures of pigmentation, and also between race and self-reported FST.
Several classification systems have surfaced to try to bridge some of these gaps, including the Fanous classification, the Roberts Skin Type Classification System, and the Lancer Ethnicity Scale. Some of these have focused more on expanding the racial and ethnic categories to help predict response to procedures, she said, while others have focused more on hyperpigmentation, photoaging, and risk of scarring. “Others have suggested having different color matching systems to expand on a number of color-matched hues with regard to hyperpigmentation or race,” Dr. Kagha added. “In spite of all these efforts, it seems that the FST system remains the most widely used classification system in dermatology. I think that’s likely because we haven’t established a new consensus on a different system to use.”
She went on to postulate that there is likely “an infinite number of skin colors that are also impacted by geographic and cultural factors. Perhaps we should restructure how we think about skin typing. We need to establish a new consensus on skin typing, one that respects the variability in skin color but also one that’s clear, concise, objective, practical, and can be universally accepted.”
Dr. Kagha concluded her remarks by encouraging dermatologists to become more comfortable with treating all skin types. “This is going to be in line with the current population trends in the U.S., and also in line with the patients that we serve. Finally, I think we as physicians are in a unique position. Our patients’ frustrations and unsolved mysteries can drive our passion and our patient-centered innovation. For me, a common theme and a common source of frustration that I’ve seen in patients with increased melanin in their skin is figuring out how to effectively remove or prevent unwanted marks or unwanted pigment without disturbing the baseline pigment.”
Dr. Kagha reported having no financial disclosures.
Even though the popular classification system added skin types V and VI in 1988 to the first iteration established in 1975, it was never intended for categorizing skin color, according to Karen C. Kagha, MD.
“This topic is going to become more relevant in our clinical practices, especially when you look at the current population trends in the U.S.,” Dr. Kagha, MD, a dermatologist and cosmetic and laser fellow in the department of dermatology at Massachusetts General Hospital and a research fellow at Wellman Center for Photomedicine, both in Boston, said during a virtual course on laser and aesthetic skin therapy. “Minority groups continue to increase. According to the U.S. Census Bureau, by the year 2050, we can expect that the majority of the population will be of non-European descent.”
The original intent of the Fitzpatrick Skin Typing (FST) system was to establish a minimal erythema dose, or likelihood to burn for patients receiving phototherapy, she continued. However, a recently published survey of 141 board-certified dermatologists and trainees found that 31% of respondents said that they used the Fitzpatrick Skin Typing System to describe the patient’s race or ethnicity, 47% used it to describe the patients’ constitutive skin color, and 22% used it in both scenarios.
“There also have been inconsistencies reported with the Fitzpatrick Skin Typing System,” Dr. Kagha said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Some studies show that there are inconsistent correlations between self-reported Fitzpatrick Skin Type and burn risk, and between self-reported FST and physician-reported FST. This means that some patients self-identify differently from how their physicians identify them.” There have also been some inconsistent correlations between race and objective measures of pigmentation, and also between race and self-reported FST.
Several classification systems have surfaced to try to bridge some of these gaps, including the Fanous classification, the Roberts Skin Type Classification System, and the Lancer Ethnicity Scale. Some of these have focused more on expanding the racial and ethnic categories to help predict response to procedures, she said, while others have focused more on hyperpigmentation, photoaging, and risk of scarring. “Others have suggested having different color matching systems to expand on a number of color-matched hues with regard to hyperpigmentation or race,” Dr. Kagha added. “In spite of all these efforts, it seems that the FST system remains the most widely used classification system in dermatology. I think that’s likely because we haven’t established a new consensus on a different system to use.”
She went on to postulate that there is likely “an infinite number of skin colors that are also impacted by geographic and cultural factors. Perhaps we should restructure how we think about skin typing. We need to establish a new consensus on skin typing, one that respects the variability in skin color but also one that’s clear, concise, objective, practical, and can be universally accepted.”
Dr. Kagha concluded her remarks by encouraging dermatologists to become more comfortable with treating all skin types. “This is going to be in line with the current population trends in the U.S., and also in line with the patients that we serve. Finally, I think we as physicians are in a unique position. Our patients’ frustrations and unsolved mysteries can drive our passion and our patient-centered innovation. For me, a common theme and a common source of frustration that I’ve seen in patients with increased melanin in their skin is figuring out how to effectively remove or prevent unwanted marks or unwanted pigment without disturbing the baseline pigment.”
Dr. Kagha reported having no financial disclosures.
Even though the popular classification system added skin types V and VI in 1988 to the first iteration established in 1975, it was never intended for categorizing skin color, according to Karen C. Kagha, MD.
“This topic is going to become more relevant in our clinical practices, especially when you look at the current population trends in the U.S.,” Dr. Kagha, MD, a dermatologist and cosmetic and laser fellow in the department of dermatology at Massachusetts General Hospital and a research fellow at Wellman Center for Photomedicine, both in Boston, said during a virtual course on laser and aesthetic skin therapy. “Minority groups continue to increase. According to the U.S. Census Bureau, by the year 2050, we can expect that the majority of the population will be of non-European descent.”
The original intent of the Fitzpatrick Skin Typing (FST) system was to establish a minimal erythema dose, or likelihood to burn for patients receiving phototherapy, she continued. However, a recently published survey of 141 board-certified dermatologists and trainees found that 31% of respondents said that they used the Fitzpatrick Skin Typing System to describe the patient’s race or ethnicity, 47% used it to describe the patients’ constitutive skin color, and 22% used it in both scenarios.
“There also have been inconsistencies reported with the Fitzpatrick Skin Typing System,” Dr. Kagha said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Some studies show that there are inconsistent correlations between self-reported Fitzpatrick Skin Type and burn risk, and between self-reported FST and physician-reported FST. This means that some patients self-identify differently from how their physicians identify them.” There have also been some inconsistent correlations between race and objective measures of pigmentation, and also between race and self-reported FST.
Several classification systems have surfaced to try to bridge some of these gaps, including the Fanous classification, the Roberts Skin Type Classification System, and the Lancer Ethnicity Scale. Some of these have focused more on expanding the racial and ethnic categories to help predict response to procedures, she said, while others have focused more on hyperpigmentation, photoaging, and risk of scarring. “Others have suggested having different color matching systems to expand on a number of color-matched hues with regard to hyperpigmentation or race,” Dr. Kagha added. “In spite of all these efforts, it seems that the FST system remains the most widely used classification system in dermatology. I think that’s likely because we haven’t established a new consensus on a different system to use.”
She went on to postulate that there is likely “an infinite number of skin colors that are also impacted by geographic and cultural factors. Perhaps we should restructure how we think about skin typing. We need to establish a new consensus on skin typing, one that respects the variability in skin color but also one that’s clear, concise, objective, practical, and can be universally accepted.”
Dr. Kagha concluded her remarks by encouraging dermatologists to become more comfortable with treating all skin types. “This is going to be in line with the current population trends in the U.S., and also in line with the patients that we serve. Finally, I think we as physicians are in a unique position. Our patients’ frustrations and unsolved mysteries can drive our passion and our patient-centered innovation. For me, a common theme and a common source of frustration that I’ve seen in patients with increased melanin in their skin is figuring out how to effectively remove or prevent unwanted marks or unwanted pigment without disturbing the baseline pigment.”
Dr. Kagha reported having no financial disclosures.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Black patients less likely to receive H. pylori eradication testing
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
FROM ACG 2020
Primary care journals address systemic racism in medicine
Sumi Sexton, MD, editor in chief of American Family Physician (AFP), said in an interview she had been working on changes at her journal that would answer the need for action that was made clear by this summer’s Black Lives Matter protests and realized the issue was much bigger than one journal. She proposed the collaboration with the other editors.
The editors wrote a joint statement explaining what they plan to do collectively. It was published online Oct. 15 ahead of print and will be published in all 10 journals at the beginning of the year.
Following the action by family medicine editors, the American College of Physicians issued a statement expressing commitment to being an antiracist organization. It calls on all doctors to speak out against hate and discrimination and to act against institutional and systemic racism. The statement also apologizes for the organization’s own past actions: “ACP acknowledges and regrets its own historical organizational injustices and inequities, and past racism, discrimination and exclusionary practices throughout its history, whether intentional or unintentional, by act or omission.”
Family medicine journals plan changes
Changes will differ at each family medicine publication, according to Sexton and other interviewees. Some specific changes at AFP, for example, include creating a medical editor role dedicated to diversity, equity, and inclusion to ensure that content is not only accurate but also that more content addresses racism, Dr. Sexton said.
AFP is creating a Web page dedicated to diversity and will now capitalize the word “Black” in racial and cultural references. Recent calls for papers have included emphasis on finding authors from underrepresented groups and on mentoring new authors.
“We really need to enable our colleagues,” Dr. Sexton said.
The journals are also pooling their published research on topics of racism and inclusion and have established a joint bibliography.
The steps are important, Dr. Sexton said, because reform in research will start a “cascade of action” that will result in better patient care.
“Our mission is to care for the individual as a whole person,” Dr. Sexton said. “This is part of that mission.”
Increasing diversity on editorial boards
Family physician Kameron Leigh Matthews, MD, chief medical officer for the Veterans Health Administration, praised the journals’ plan.
She noted that the groups are addressing diversity on their editorial boards, as well as evaluating content. Effective change must also happen regarding the people reviewing the content, she said in an interview. “It has to be both.
“I’m very proud as a family physician that our editors came together and are giving the right response. It’s not enough to say we stand against racism. They’re actually offering concrete actions that they will take as editors, and that will influence health care,” she said.
Dr. Matthews pointed to an example of what can happen when the editorial process fails and racism is introduced in research.
She cited the retraction of an article in the Journal of the American Heart Association entitled, “Evolution of Race and Ethnicity Considerations for the Cardiology Workforce.” The article advocated for ending racial and ethnic preferences in undergraduate and medical school admissions.
The American Heart Association said the article concluded “incorrectly that Black and Hispanic trainees in medicine are less qualified than White and Asian trainees.” The article had “rightfully drawn criticism for its misrepresentations and conclusions,” the AHA said, adding that it would launch an investigation into how the article came to be published.
Dr. Matthews says that’s why it’s so important that, in their statement, the family medicine editors vow to address not only the content but also the editing process to avoid similar systemic lapses.
Dr. Matthews added that, because the proportion of physicians from underrepresented groups is small – only 5% of physicians are Black and 6% are Hispanic – it is vital, as recommended in the editors’ statement, to mentor researchers from underrepresented groups and to reach out to students and residents to be coauthors.
“To sit back and say there’s not enough to recruit from is not sufficient,” Dr. Matthews said. “You need to recognize that you need to assist with expanding the pool.”
She also said she would like to see the journals focus more heavily on solutions to racial disparities in health care rather than on pointing them out.
At the Journal of Family Practice (JFP), Editor in Chief John Hickner, MD, said adding diversity to the editorial board is a top priority. He also reiterated that diversity in top leadership is a concern across all the journals, inasmuch as only 1 of the 10 editors in chief is a person of color.
As an editor, he said, he will personally, as well as through family medicine department chairs, be seeking authors who are members of underrepresented groups and that he will be assisting those who need help.
“I’m committed to giving them special attention in the editorial process,” he said.
Dr. Hickner said the 10 journals have also committed to periodically evaluate whether their approaches are making substantial changes. He said the editors have vowed to meet at least once a year to review progress “and hold each other accountable.”
Statement authors, in addition to Dr. Sexton and Dr. Hickner, include these editors in chief: Caroline R. Richardson, MD, Annals of Family Medicine; Sarina B. Schrager, MD, FPM; Marjorie A. Bowman, MD, The Journal of the American Board of Family Medicine; Christopher P. Morley, PhD, PRiMER; Nicholas Pimlott, MD, PhD, Canadian Family Physician; John W. Saultz, MD, Family Medicine; and Barry D. Weiss, MD, FP Essentials.
The authors have disclosed no relevant financial relationships. The Journal of Family Practice is owned by the same news organization as this publication.
A version of this article originally appeared on Medscape.com.
Sumi Sexton, MD, editor in chief of American Family Physician (AFP), said in an interview she had been working on changes at her journal that would answer the need for action that was made clear by this summer’s Black Lives Matter protests and realized the issue was much bigger than one journal. She proposed the collaboration with the other editors.
The editors wrote a joint statement explaining what they plan to do collectively. It was published online Oct. 15 ahead of print and will be published in all 10 journals at the beginning of the year.
Following the action by family medicine editors, the American College of Physicians issued a statement expressing commitment to being an antiracist organization. It calls on all doctors to speak out against hate and discrimination and to act against institutional and systemic racism. The statement also apologizes for the organization’s own past actions: “ACP acknowledges and regrets its own historical organizational injustices and inequities, and past racism, discrimination and exclusionary practices throughout its history, whether intentional or unintentional, by act or omission.”
Family medicine journals plan changes
Changes will differ at each family medicine publication, according to Sexton and other interviewees. Some specific changes at AFP, for example, include creating a medical editor role dedicated to diversity, equity, and inclusion to ensure that content is not only accurate but also that more content addresses racism, Dr. Sexton said.
AFP is creating a Web page dedicated to diversity and will now capitalize the word “Black” in racial and cultural references. Recent calls for papers have included emphasis on finding authors from underrepresented groups and on mentoring new authors.
“We really need to enable our colleagues,” Dr. Sexton said.
The journals are also pooling their published research on topics of racism and inclusion and have established a joint bibliography.
The steps are important, Dr. Sexton said, because reform in research will start a “cascade of action” that will result in better patient care.
“Our mission is to care for the individual as a whole person,” Dr. Sexton said. “This is part of that mission.”
Increasing diversity on editorial boards
Family physician Kameron Leigh Matthews, MD, chief medical officer for the Veterans Health Administration, praised the journals’ plan.
She noted that the groups are addressing diversity on their editorial boards, as well as evaluating content. Effective change must also happen regarding the people reviewing the content, she said in an interview. “It has to be both.
“I’m very proud as a family physician that our editors came together and are giving the right response. It’s not enough to say we stand against racism. They’re actually offering concrete actions that they will take as editors, and that will influence health care,” she said.
Dr. Matthews pointed to an example of what can happen when the editorial process fails and racism is introduced in research.
She cited the retraction of an article in the Journal of the American Heart Association entitled, “Evolution of Race and Ethnicity Considerations for the Cardiology Workforce.” The article advocated for ending racial and ethnic preferences in undergraduate and medical school admissions.
The American Heart Association said the article concluded “incorrectly that Black and Hispanic trainees in medicine are less qualified than White and Asian trainees.” The article had “rightfully drawn criticism for its misrepresentations and conclusions,” the AHA said, adding that it would launch an investigation into how the article came to be published.
Dr. Matthews says that’s why it’s so important that, in their statement, the family medicine editors vow to address not only the content but also the editing process to avoid similar systemic lapses.
Dr. Matthews added that, because the proportion of physicians from underrepresented groups is small – only 5% of physicians are Black and 6% are Hispanic – it is vital, as recommended in the editors’ statement, to mentor researchers from underrepresented groups and to reach out to students and residents to be coauthors.
“To sit back and say there’s not enough to recruit from is not sufficient,” Dr. Matthews said. “You need to recognize that you need to assist with expanding the pool.”
She also said she would like to see the journals focus more heavily on solutions to racial disparities in health care rather than on pointing them out.
At the Journal of Family Practice (JFP), Editor in Chief John Hickner, MD, said adding diversity to the editorial board is a top priority. He also reiterated that diversity in top leadership is a concern across all the journals, inasmuch as only 1 of the 10 editors in chief is a person of color.
As an editor, he said, he will personally, as well as through family medicine department chairs, be seeking authors who are members of underrepresented groups and that he will be assisting those who need help.
“I’m committed to giving them special attention in the editorial process,” he said.
Dr. Hickner said the 10 journals have also committed to periodically evaluate whether their approaches are making substantial changes. He said the editors have vowed to meet at least once a year to review progress “and hold each other accountable.”
Statement authors, in addition to Dr. Sexton and Dr. Hickner, include these editors in chief: Caroline R. Richardson, MD, Annals of Family Medicine; Sarina B. Schrager, MD, FPM; Marjorie A. Bowman, MD, The Journal of the American Board of Family Medicine; Christopher P. Morley, PhD, PRiMER; Nicholas Pimlott, MD, PhD, Canadian Family Physician; John W. Saultz, MD, Family Medicine; and Barry D. Weiss, MD, FP Essentials.
The authors have disclosed no relevant financial relationships. The Journal of Family Practice is owned by the same news organization as this publication.
A version of this article originally appeared on Medscape.com.
Sumi Sexton, MD, editor in chief of American Family Physician (AFP), said in an interview she had been working on changes at her journal that would answer the need for action that was made clear by this summer’s Black Lives Matter protests and realized the issue was much bigger than one journal. She proposed the collaboration with the other editors.
The editors wrote a joint statement explaining what they plan to do collectively. It was published online Oct. 15 ahead of print and will be published in all 10 journals at the beginning of the year.
Following the action by family medicine editors, the American College of Physicians issued a statement expressing commitment to being an antiracist organization. It calls on all doctors to speak out against hate and discrimination and to act against institutional and systemic racism. The statement also apologizes for the organization’s own past actions: “ACP acknowledges and regrets its own historical organizational injustices and inequities, and past racism, discrimination and exclusionary practices throughout its history, whether intentional or unintentional, by act or omission.”
Family medicine journals plan changes
Changes will differ at each family medicine publication, according to Sexton and other interviewees. Some specific changes at AFP, for example, include creating a medical editor role dedicated to diversity, equity, and inclusion to ensure that content is not only accurate but also that more content addresses racism, Dr. Sexton said.
AFP is creating a Web page dedicated to diversity and will now capitalize the word “Black” in racial and cultural references. Recent calls for papers have included emphasis on finding authors from underrepresented groups and on mentoring new authors.
“We really need to enable our colleagues,” Dr. Sexton said.
The journals are also pooling their published research on topics of racism and inclusion and have established a joint bibliography.
The steps are important, Dr. Sexton said, because reform in research will start a “cascade of action” that will result in better patient care.
“Our mission is to care for the individual as a whole person,” Dr. Sexton said. “This is part of that mission.”
Increasing diversity on editorial boards
Family physician Kameron Leigh Matthews, MD, chief medical officer for the Veterans Health Administration, praised the journals’ plan.
She noted that the groups are addressing diversity on their editorial boards, as well as evaluating content. Effective change must also happen regarding the people reviewing the content, she said in an interview. “It has to be both.
“I’m very proud as a family physician that our editors came together and are giving the right response. It’s not enough to say we stand against racism. They’re actually offering concrete actions that they will take as editors, and that will influence health care,” she said.
Dr. Matthews pointed to an example of what can happen when the editorial process fails and racism is introduced in research.
She cited the retraction of an article in the Journal of the American Heart Association entitled, “Evolution of Race and Ethnicity Considerations for the Cardiology Workforce.” The article advocated for ending racial and ethnic preferences in undergraduate and medical school admissions.
The American Heart Association said the article concluded “incorrectly that Black and Hispanic trainees in medicine are less qualified than White and Asian trainees.” The article had “rightfully drawn criticism for its misrepresentations and conclusions,” the AHA said, adding that it would launch an investigation into how the article came to be published.
Dr. Matthews says that’s why it’s so important that, in their statement, the family medicine editors vow to address not only the content but also the editing process to avoid similar systemic lapses.
Dr. Matthews added that, because the proportion of physicians from underrepresented groups is small – only 5% of physicians are Black and 6% are Hispanic – it is vital, as recommended in the editors’ statement, to mentor researchers from underrepresented groups and to reach out to students and residents to be coauthors.
“To sit back and say there’s not enough to recruit from is not sufficient,” Dr. Matthews said. “You need to recognize that you need to assist with expanding the pool.”
She also said she would like to see the journals focus more heavily on solutions to racial disparities in health care rather than on pointing them out.
At the Journal of Family Practice (JFP), Editor in Chief John Hickner, MD, said adding diversity to the editorial board is a top priority. He also reiterated that diversity in top leadership is a concern across all the journals, inasmuch as only 1 of the 10 editors in chief is a person of color.
As an editor, he said, he will personally, as well as through family medicine department chairs, be seeking authors who are members of underrepresented groups and that he will be assisting those who need help.
“I’m committed to giving them special attention in the editorial process,” he said.
Dr. Hickner said the 10 journals have also committed to periodically evaluate whether their approaches are making substantial changes. He said the editors have vowed to meet at least once a year to review progress “and hold each other accountable.”
Statement authors, in addition to Dr. Sexton and Dr. Hickner, include these editors in chief: Caroline R. Richardson, MD, Annals of Family Medicine; Sarina B. Schrager, MD, FPM; Marjorie A. Bowman, MD, The Journal of the American Board of Family Medicine; Christopher P. Morley, PhD, PRiMER; Nicholas Pimlott, MD, PhD, Canadian Family Physician; John W. Saultz, MD, Family Medicine; and Barry D. Weiss, MD, FP Essentials.
The authors have disclosed no relevant financial relationships. The Journal of Family Practice is owned by the same news organization as this publication.
A version of this article originally appeared on Medscape.com.
Family planning issues loom large for female radiation oncologists
Results from the survey were reported at the American Society for Radiation Oncology Annual Meeting 2020.
“Female radiation oncologists often spend their childbearing years in training and establishing careers,” commented lead investigator Anna Lee, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Currently, physician fertility and family planning are rarely discussed or taught in medical school or postgraduate training,” Dr. Lee said.
Dr. Lee and colleagues conducted a national anonymous cross-sectional online survey of female oncologists of all types and all career levels (including trainees). The team circulated a 39-item questionnaire exploring attitudes toward and experiences related to family planning and assisted reproductive technology (ART) by email and social media channels.
A total of 351 radiation oncologists participated, representing one-fifth of the specialty’s entire female workforce nationally and making this study the largest to date on family planning among these physicians.
Most respondents were aged 31-40 years (60%) and married (79%), had children (68%), and were in training (26%) or academic practice (48%).
Survey results
Fully 74% of respondents reported that their career plans strongly influenced the timing of when to start a family, and 29% said family planning considerations influenced their decision regarding their choice of academia versus private practice, Dr. Lee reported.
Overall, 24% of respondents indicated that they had difficulty with infertility or required fertility counseling/treatment, 66% said they wished fertility preservation was discussed at some point during their training, and 22% said either that ART would have benefited them if it had been available or that they were planning to or had already used fertility preservation.
On the topic of maternity leave, some respondents reported that their institution either had no formal leave policy during training or provided less than 1 month of leave (23%) and that they felt pressure to take less time off than was policy (15%).
“Of note, 32 women in our survey were not offered non–radiation-exposing assignments during pregnancy, and an additional 57 had to specifically ask for them,” Dr. Lee remarked.
About one-third of respondents each reported that they did not feel supported during training for issues related to fertility and/or pregnancy (33%) and that they experienced discrimination for being pregnant (32%) and taking maternity leave (30%).
“Systemic changes are necessary early in medical education and training to ensure women are supported and able to advance equitably in the field. As less than a third of the current radiation oncology workforce are women, improvement upon these issues will be necessary to draw more women into the field,” Dr. Lee commented. “Education on ART risks, benefits, and success rates can help physicians and those in training in their family planning, while the lack of education and structured policy can exacerbate the emotional, physical, and financial impact of infertility.
“Until recently, there has been a dearth of policy at the programmatic, institutional, and national level allowing time and protection for pregnancy and maternity leave,” she added. “Thankfully, this summer, the American Board of Medical Specialties announced a progressive leave policy for residents and fellows.”
The new policy, which goes into effect July 2021, allows a minimum of 6 weeks away without exhausting time allowed for vacation or sick leave and without requiring an extension in training.
When career and biology collide
“The collision of professional and biological clocks for women in medicine is an important issue highlighted by this study,” Reshma Jagsi, MD, DPhil, of the University of Michigan in Ann Arbor, said in an interview.
“Prior work focused on women in medicine more generally. A deeper dive into the experiences of women in a specific field may be even more compelling to drive change on the part of professional societies and organizations,” Dr. Jagsi added.
The infertility rate observed in the study could have potentially been skewed by the preponderance of younger respondents (resulting in underestimation) or by greater participation of those interested in the subject (resulting in overestimation), she noted. However, it aligns well with the rate in a study Dr. Jagsi and colleagues conducted among female physicians generally using somewhat different methods. That study was published in the Journal of Women’s Health.
Concern about radiation exposure and its potential reproductive health effects should not deter women from choosing radiation oncology as a specialty, according to Dr. Jagsi.
“Radiation exposure is actually very low in radiation oncology, much lower than in specialties like interventional cardiology, where physicians are in the room where fluoroscopy is being used. It is actually an important misconception about this field that merits correction,” she stressed. “Rather, the fertility concerns are related to the expectations of training and demands of work during the prime childbearing years more generally that can lead women to delay pregnancy, which is an issue common to all medical specialties.”
“The investigators’ conclusions are very reasonable,” Dr. Jagsi said. “Although one might quibble whether the exact proportions reflect the experiences of all women in the field perfectly due to the possibility of selection bias, one cannot question whether a substantial number of women are experiencing these challenges and that they merit intervention.”
The study did not receive specific funding. Dr. Lee and Dr. Jagsi disclosed no relevant conflicts of interest.
SOURCE: Lee A et al. ASTRO 2020, Abstract LBA 6.
Results from the survey were reported at the American Society for Radiation Oncology Annual Meeting 2020.
“Female radiation oncologists often spend their childbearing years in training and establishing careers,” commented lead investigator Anna Lee, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Currently, physician fertility and family planning are rarely discussed or taught in medical school or postgraduate training,” Dr. Lee said.
Dr. Lee and colleagues conducted a national anonymous cross-sectional online survey of female oncologists of all types and all career levels (including trainees). The team circulated a 39-item questionnaire exploring attitudes toward and experiences related to family planning and assisted reproductive technology (ART) by email and social media channels.
A total of 351 radiation oncologists participated, representing one-fifth of the specialty’s entire female workforce nationally and making this study the largest to date on family planning among these physicians.
Most respondents were aged 31-40 years (60%) and married (79%), had children (68%), and were in training (26%) or academic practice (48%).
Survey results
Fully 74% of respondents reported that their career plans strongly influenced the timing of when to start a family, and 29% said family planning considerations influenced their decision regarding their choice of academia versus private practice, Dr. Lee reported.
Overall, 24% of respondents indicated that they had difficulty with infertility or required fertility counseling/treatment, 66% said they wished fertility preservation was discussed at some point during their training, and 22% said either that ART would have benefited them if it had been available or that they were planning to or had already used fertility preservation.
On the topic of maternity leave, some respondents reported that their institution either had no formal leave policy during training or provided less than 1 month of leave (23%) and that they felt pressure to take less time off than was policy (15%).
“Of note, 32 women in our survey were not offered non–radiation-exposing assignments during pregnancy, and an additional 57 had to specifically ask for them,” Dr. Lee remarked.
About one-third of respondents each reported that they did not feel supported during training for issues related to fertility and/or pregnancy (33%) and that they experienced discrimination for being pregnant (32%) and taking maternity leave (30%).
“Systemic changes are necessary early in medical education and training to ensure women are supported and able to advance equitably in the field. As less than a third of the current radiation oncology workforce are women, improvement upon these issues will be necessary to draw more women into the field,” Dr. Lee commented. “Education on ART risks, benefits, and success rates can help physicians and those in training in their family planning, while the lack of education and structured policy can exacerbate the emotional, physical, and financial impact of infertility.
“Until recently, there has been a dearth of policy at the programmatic, institutional, and national level allowing time and protection for pregnancy and maternity leave,” she added. “Thankfully, this summer, the American Board of Medical Specialties announced a progressive leave policy for residents and fellows.”
The new policy, which goes into effect July 2021, allows a minimum of 6 weeks away without exhausting time allowed for vacation or sick leave and without requiring an extension in training.
When career and biology collide
“The collision of professional and biological clocks for women in medicine is an important issue highlighted by this study,” Reshma Jagsi, MD, DPhil, of the University of Michigan in Ann Arbor, said in an interview.
“Prior work focused on women in medicine more generally. A deeper dive into the experiences of women in a specific field may be even more compelling to drive change on the part of professional societies and organizations,” Dr. Jagsi added.
The infertility rate observed in the study could have potentially been skewed by the preponderance of younger respondents (resulting in underestimation) or by greater participation of those interested in the subject (resulting in overestimation), she noted. However, it aligns well with the rate in a study Dr. Jagsi and colleagues conducted among female physicians generally using somewhat different methods. That study was published in the Journal of Women’s Health.
Concern about radiation exposure and its potential reproductive health effects should not deter women from choosing radiation oncology as a specialty, according to Dr. Jagsi.
“Radiation exposure is actually very low in radiation oncology, much lower than in specialties like interventional cardiology, where physicians are in the room where fluoroscopy is being used. It is actually an important misconception about this field that merits correction,” she stressed. “Rather, the fertility concerns are related to the expectations of training and demands of work during the prime childbearing years more generally that can lead women to delay pregnancy, which is an issue common to all medical specialties.”
“The investigators’ conclusions are very reasonable,” Dr. Jagsi said. “Although one might quibble whether the exact proportions reflect the experiences of all women in the field perfectly due to the possibility of selection bias, one cannot question whether a substantial number of women are experiencing these challenges and that they merit intervention.”
The study did not receive specific funding. Dr. Lee and Dr. Jagsi disclosed no relevant conflicts of interest.
SOURCE: Lee A et al. ASTRO 2020, Abstract LBA 6.
Results from the survey were reported at the American Society for Radiation Oncology Annual Meeting 2020.
“Female radiation oncologists often spend their childbearing years in training and establishing careers,” commented lead investigator Anna Lee, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Currently, physician fertility and family planning are rarely discussed or taught in medical school or postgraduate training,” Dr. Lee said.
Dr. Lee and colleagues conducted a national anonymous cross-sectional online survey of female oncologists of all types and all career levels (including trainees). The team circulated a 39-item questionnaire exploring attitudes toward and experiences related to family planning and assisted reproductive technology (ART) by email and social media channels.
A total of 351 radiation oncologists participated, representing one-fifth of the specialty’s entire female workforce nationally and making this study the largest to date on family planning among these physicians.
Most respondents were aged 31-40 years (60%) and married (79%), had children (68%), and were in training (26%) or academic practice (48%).
Survey results
Fully 74% of respondents reported that their career plans strongly influenced the timing of when to start a family, and 29% said family planning considerations influenced their decision regarding their choice of academia versus private practice, Dr. Lee reported.
Overall, 24% of respondents indicated that they had difficulty with infertility or required fertility counseling/treatment, 66% said they wished fertility preservation was discussed at some point during their training, and 22% said either that ART would have benefited them if it had been available or that they were planning to or had already used fertility preservation.
On the topic of maternity leave, some respondents reported that their institution either had no formal leave policy during training or provided less than 1 month of leave (23%) and that they felt pressure to take less time off than was policy (15%).
“Of note, 32 women in our survey were not offered non–radiation-exposing assignments during pregnancy, and an additional 57 had to specifically ask for them,” Dr. Lee remarked.
About one-third of respondents each reported that they did not feel supported during training for issues related to fertility and/or pregnancy (33%) and that they experienced discrimination for being pregnant (32%) and taking maternity leave (30%).
“Systemic changes are necessary early in medical education and training to ensure women are supported and able to advance equitably in the field. As less than a third of the current radiation oncology workforce are women, improvement upon these issues will be necessary to draw more women into the field,” Dr. Lee commented. “Education on ART risks, benefits, and success rates can help physicians and those in training in their family planning, while the lack of education and structured policy can exacerbate the emotional, physical, and financial impact of infertility.
“Until recently, there has been a dearth of policy at the programmatic, institutional, and national level allowing time and protection for pregnancy and maternity leave,” she added. “Thankfully, this summer, the American Board of Medical Specialties announced a progressive leave policy for residents and fellows.”
The new policy, which goes into effect July 2021, allows a minimum of 6 weeks away without exhausting time allowed for vacation or sick leave and without requiring an extension in training.
When career and biology collide
“The collision of professional and biological clocks for women in medicine is an important issue highlighted by this study,” Reshma Jagsi, MD, DPhil, of the University of Michigan in Ann Arbor, said in an interview.
“Prior work focused on women in medicine more generally. A deeper dive into the experiences of women in a specific field may be even more compelling to drive change on the part of professional societies and organizations,” Dr. Jagsi added.
The infertility rate observed in the study could have potentially been skewed by the preponderance of younger respondents (resulting in underestimation) or by greater participation of those interested in the subject (resulting in overestimation), she noted. However, it aligns well with the rate in a study Dr. Jagsi and colleagues conducted among female physicians generally using somewhat different methods. That study was published in the Journal of Women’s Health.
Concern about radiation exposure and its potential reproductive health effects should not deter women from choosing radiation oncology as a specialty, according to Dr. Jagsi.
“Radiation exposure is actually very low in radiation oncology, much lower than in specialties like interventional cardiology, where physicians are in the room where fluoroscopy is being used. It is actually an important misconception about this field that merits correction,” she stressed. “Rather, the fertility concerns are related to the expectations of training and demands of work during the prime childbearing years more generally that can lead women to delay pregnancy, which is an issue common to all medical specialties.”
“The investigators’ conclusions are very reasonable,” Dr. Jagsi said. “Although one might quibble whether the exact proportions reflect the experiences of all women in the field perfectly due to the possibility of selection bias, one cannot question whether a substantial number of women are experiencing these challenges and that they merit intervention.”
The study did not receive specific funding. Dr. Lee and Dr. Jagsi disclosed no relevant conflicts of interest.
SOURCE: Lee A et al. ASTRO 2020, Abstract LBA 6.
FROM ASTRO 2020
For acne in darker skin, judicious use of peeling agents can speed resolution
according to an expert, who cited both published data and empirical experience at the virtual Skin of Color Update 2020.
Because of the risk of exacerbating hyperpigmentation, superficial peels must be used judiciously, but “peels do add some benefit in terms of resolving the hyperpigmentation more rapidly,” Andrew Alexis, MD, chair of the department of dermatology at Mount Sinai Morningside and Mount Sinai West, New York, said at the meeting.
Addressing hyperpigmentation in skin of color is a critical goal. For many patients, the postinflammatory hyperpigmentation (PIH) that accompanies acne in Fitzpatrick skin types IV or higher imposes a greater burden than the acne itself.
“PIH is one of the driving forces among patients with darker skin coming to a dermatologist,” said Dr. Alexis, who is also professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York. “Patients often describe these hyperpigmented macules as scars, and they are concerned that they are not reversible.”
In darker skin, the combination of treatments used for acne should address the pathogenic factors that contribute to acne and PIH at the same time, according to Dr. Alexis. He advised describing the goals and the timeline of acne and PIH resolution at the very first visit.
Of these two goals, resolution of PIH is often the more challenging. First-line topical retinoids have anti-inflammatory effects, but Dr. Alexis suggested that additional agents, such as topical antibiotics, topical dapsone, and benzoyl peroxide, are commonly needed to fully control inflammation.
“Topical retinoids serve as the foundation of acne treatment, especially in skin of color due to their dual action on acne and PIH,” he said. However, he added that this needs support with a “well-rounded combination therapy to address as many pathogenic factors as possible.”
One of these factors is subclinical inflammation. Citing studies first initiated at Howard University, Washington, Dr. Alexis said there are now compelling data showing T lymphocyte infiltration and increased expression of proinflammatory cytokines even in clinically uninvolved skin in acne patients with darker skin.
In patients with significant PIH, he considers oral antibiotics for their systemic anti-inflammatory effects, singling out sarecycline as a narrow-spectrum agent with a potent effect on Cutibacterium acnes. This tetracycline, a relatively recent addition to acne treatment options, has specifically been shown to be “superior to placebo across a diverse patient population” that includes those with darker skin tones.
“Another addition that can be leveraged for anti-inflammatory effects is topical minocycline foam. This has also been studied in diverse patient populations and shown to be superior to vehicle,” Dr. Alexis said.
For acne, the response to most of these therapies is relatively rapid, but control of PIH takes longer. After resolution of acne, he considers superficial chemical peels to speed the healing of PIH.
In a small randomized trial he cited, superficial glycolic acid peel added to a modified Kligman formula (hydroquinone 2%, tretinoin 0.05%, and hydrocortisone 1%) provided significantly lower scores in the mean Hyperpigmentation Area and Severity Index at 12 weeks (P = .004) and 21 weeks (P < .001 relative to the Kligman formula alone). Dr. Alexis said he has had the same clinical experience with chemical peels
For many acne patients with darker skin, good results are achieved after four weeks on a multidrug combination with a topical retinoid backbone. One week after stopping the combination, the superficial chemical peel can be started at a very low dose on an every-other-night schedule. If tolerated, the dose can be slowly increased.
Slow up-titration of all topical agents in skin of color, not just superficial chemical peels, is prudent, according to Dr. Alexis. For patients new to retinoids, he also recommended every-other-night dosing to avoid the irritation that might exacerbate PIH. He said the risks of adverse reactions come early. “We need to hold the hands of our patients through the first 2 weeks. Warn of dryness and pealing. Recommend moisturizers and keep the doses low.”
The benefits and risks of acne treatment are different in dark relative to light skin, Dr. Alexis emphasized. He added that a measured approach that includes specific strategies for PIH delivers results.
Providing treatment with a strategy that addresses both acne and PIH, he said, “we can have excellent outcomes time and time again for acne in patients with darker skin types.”
There is an evidence basis for making effective treatment of PIH a specific goal in the treatment of acne. In a study that evaluated the psychosocial impact of PIH in 50 patients with acne, 54% responded that PIH was a source of embarrassment. The study was one of the first to evaluate the impact of PIH as a separate source of impaired quality of life in acne patients.
“To improve the patient’s quality of life, the dermatologist should treat acne and postinflammatory hyperpigmentation at the same time,” said Katlein Franca, MD, PhD, assistant professor of dermatology, University of Miami.
In particular, Dr. Franca, who led the PIH study, suggested that PIH, like acne, is a source of low self-esteem. In regard to PIH, “most patients feel embarrassed about the spots,” she said in an interview.
“Strategies to hide the hyperpigmented spots include the use of makeup and even different hairstyles to cover the affected areas,” she added, indicating that treatments provided to clear PIH as well as acne can remove a source of stress and threat to a sense of well-being.
Dr. Alexis reports financial relationships with many pharmaceutical companies, including those that make acne drugs.
according to an expert, who cited both published data and empirical experience at the virtual Skin of Color Update 2020.
Because of the risk of exacerbating hyperpigmentation, superficial peels must be used judiciously, but “peels do add some benefit in terms of resolving the hyperpigmentation more rapidly,” Andrew Alexis, MD, chair of the department of dermatology at Mount Sinai Morningside and Mount Sinai West, New York, said at the meeting.
Addressing hyperpigmentation in skin of color is a critical goal. For many patients, the postinflammatory hyperpigmentation (PIH) that accompanies acne in Fitzpatrick skin types IV or higher imposes a greater burden than the acne itself.
“PIH is one of the driving forces among patients with darker skin coming to a dermatologist,” said Dr. Alexis, who is also professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York. “Patients often describe these hyperpigmented macules as scars, and they are concerned that they are not reversible.”
In darker skin, the combination of treatments used for acne should address the pathogenic factors that contribute to acne and PIH at the same time, according to Dr. Alexis. He advised describing the goals and the timeline of acne and PIH resolution at the very first visit.
Of these two goals, resolution of PIH is often the more challenging. First-line topical retinoids have anti-inflammatory effects, but Dr. Alexis suggested that additional agents, such as topical antibiotics, topical dapsone, and benzoyl peroxide, are commonly needed to fully control inflammation.
“Topical retinoids serve as the foundation of acne treatment, especially in skin of color due to their dual action on acne and PIH,” he said. However, he added that this needs support with a “well-rounded combination therapy to address as many pathogenic factors as possible.”
One of these factors is subclinical inflammation. Citing studies first initiated at Howard University, Washington, Dr. Alexis said there are now compelling data showing T lymphocyte infiltration and increased expression of proinflammatory cytokines even in clinically uninvolved skin in acne patients with darker skin.
In patients with significant PIH, he considers oral antibiotics for their systemic anti-inflammatory effects, singling out sarecycline as a narrow-spectrum agent with a potent effect on Cutibacterium acnes. This tetracycline, a relatively recent addition to acne treatment options, has specifically been shown to be “superior to placebo across a diverse patient population” that includes those with darker skin tones.
“Another addition that can be leveraged for anti-inflammatory effects is topical minocycline foam. This has also been studied in diverse patient populations and shown to be superior to vehicle,” Dr. Alexis said.
For acne, the response to most of these therapies is relatively rapid, but control of PIH takes longer. After resolution of acne, he considers superficial chemical peels to speed the healing of PIH.
In a small randomized trial he cited, superficial glycolic acid peel added to a modified Kligman formula (hydroquinone 2%, tretinoin 0.05%, and hydrocortisone 1%) provided significantly lower scores in the mean Hyperpigmentation Area and Severity Index at 12 weeks (P = .004) and 21 weeks (P < .001 relative to the Kligman formula alone). Dr. Alexis said he has had the same clinical experience with chemical peels
For many acne patients with darker skin, good results are achieved after four weeks on a multidrug combination with a topical retinoid backbone. One week after stopping the combination, the superficial chemical peel can be started at a very low dose on an every-other-night schedule. If tolerated, the dose can be slowly increased.
Slow up-titration of all topical agents in skin of color, not just superficial chemical peels, is prudent, according to Dr. Alexis. For patients new to retinoids, he also recommended every-other-night dosing to avoid the irritation that might exacerbate PIH. He said the risks of adverse reactions come early. “We need to hold the hands of our patients through the first 2 weeks. Warn of dryness and pealing. Recommend moisturizers and keep the doses low.”
The benefits and risks of acne treatment are different in dark relative to light skin, Dr. Alexis emphasized. He added that a measured approach that includes specific strategies for PIH delivers results.
Providing treatment with a strategy that addresses both acne and PIH, he said, “we can have excellent outcomes time and time again for acne in patients with darker skin types.”
There is an evidence basis for making effective treatment of PIH a specific goal in the treatment of acne. In a study that evaluated the psychosocial impact of PIH in 50 patients with acne, 54% responded that PIH was a source of embarrassment. The study was one of the first to evaluate the impact of PIH as a separate source of impaired quality of life in acne patients.
“To improve the patient’s quality of life, the dermatologist should treat acne and postinflammatory hyperpigmentation at the same time,” said Katlein Franca, MD, PhD, assistant professor of dermatology, University of Miami.
In particular, Dr. Franca, who led the PIH study, suggested that PIH, like acne, is a source of low self-esteem. In regard to PIH, “most patients feel embarrassed about the spots,” she said in an interview.
“Strategies to hide the hyperpigmented spots include the use of makeup and even different hairstyles to cover the affected areas,” she added, indicating that treatments provided to clear PIH as well as acne can remove a source of stress and threat to a sense of well-being.
Dr. Alexis reports financial relationships with many pharmaceutical companies, including those that make acne drugs.
according to an expert, who cited both published data and empirical experience at the virtual Skin of Color Update 2020.
Because of the risk of exacerbating hyperpigmentation, superficial peels must be used judiciously, but “peels do add some benefit in terms of resolving the hyperpigmentation more rapidly,” Andrew Alexis, MD, chair of the department of dermatology at Mount Sinai Morningside and Mount Sinai West, New York, said at the meeting.
Addressing hyperpigmentation in skin of color is a critical goal. For many patients, the postinflammatory hyperpigmentation (PIH) that accompanies acne in Fitzpatrick skin types IV or higher imposes a greater burden than the acne itself.
“PIH is one of the driving forces among patients with darker skin coming to a dermatologist,” said Dr. Alexis, who is also professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York. “Patients often describe these hyperpigmented macules as scars, and they are concerned that they are not reversible.”
In darker skin, the combination of treatments used for acne should address the pathogenic factors that contribute to acne and PIH at the same time, according to Dr. Alexis. He advised describing the goals and the timeline of acne and PIH resolution at the very first visit.
Of these two goals, resolution of PIH is often the more challenging. First-line topical retinoids have anti-inflammatory effects, but Dr. Alexis suggested that additional agents, such as topical antibiotics, topical dapsone, and benzoyl peroxide, are commonly needed to fully control inflammation.
“Topical retinoids serve as the foundation of acne treatment, especially in skin of color due to their dual action on acne and PIH,” he said. However, he added that this needs support with a “well-rounded combination therapy to address as many pathogenic factors as possible.”
One of these factors is subclinical inflammation. Citing studies first initiated at Howard University, Washington, Dr. Alexis said there are now compelling data showing T lymphocyte infiltration and increased expression of proinflammatory cytokines even in clinically uninvolved skin in acne patients with darker skin.
In patients with significant PIH, he considers oral antibiotics for their systemic anti-inflammatory effects, singling out sarecycline as a narrow-spectrum agent with a potent effect on Cutibacterium acnes. This tetracycline, a relatively recent addition to acne treatment options, has specifically been shown to be “superior to placebo across a diverse patient population” that includes those with darker skin tones.
“Another addition that can be leveraged for anti-inflammatory effects is topical minocycline foam. This has also been studied in diverse patient populations and shown to be superior to vehicle,” Dr. Alexis said.
For acne, the response to most of these therapies is relatively rapid, but control of PIH takes longer. After resolution of acne, he considers superficial chemical peels to speed the healing of PIH.
In a small randomized trial he cited, superficial glycolic acid peel added to a modified Kligman formula (hydroquinone 2%, tretinoin 0.05%, and hydrocortisone 1%) provided significantly lower scores in the mean Hyperpigmentation Area and Severity Index at 12 weeks (P = .004) and 21 weeks (P < .001 relative to the Kligman formula alone). Dr. Alexis said he has had the same clinical experience with chemical peels
For many acne patients with darker skin, good results are achieved after four weeks on a multidrug combination with a topical retinoid backbone. One week after stopping the combination, the superficial chemical peel can be started at a very low dose on an every-other-night schedule. If tolerated, the dose can be slowly increased.
Slow up-titration of all topical agents in skin of color, not just superficial chemical peels, is prudent, according to Dr. Alexis. For patients new to retinoids, he also recommended every-other-night dosing to avoid the irritation that might exacerbate PIH. He said the risks of adverse reactions come early. “We need to hold the hands of our patients through the first 2 weeks. Warn of dryness and pealing. Recommend moisturizers and keep the doses low.”
The benefits and risks of acne treatment are different in dark relative to light skin, Dr. Alexis emphasized. He added that a measured approach that includes specific strategies for PIH delivers results.
Providing treatment with a strategy that addresses both acne and PIH, he said, “we can have excellent outcomes time and time again for acne in patients with darker skin types.”
There is an evidence basis for making effective treatment of PIH a specific goal in the treatment of acne. In a study that evaluated the psychosocial impact of PIH in 50 patients with acne, 54% responded that PIH was a source of embarrassment. The study was one of the first to evaluate the impact of PIH as a separate source of impaired quality of life in acne patients.
“To improve the patient’s quality of life, the dermatologist should treat acne and postinflammatory hyperpigmentation at the same time,” said Katlein Franca, MD, PhD, assistant professor of dermatology, University of Miami.
In particular, Dr. Franca, who led the PIH study, suggested that PIH, like acne, is a source of low self-esteem. In regard to PIH, “most patients feel embarrassed about the spots,” she said in an interview.
“Strategies to hide the hyperpigmented spots include the use of makeup and even different hairstyles to cover the affected areas,” she added, indicating that treatments provided to clear PIH as well as acne can remove a source of stress and threat to a sense of well-being.
Dr. Alexis reports financial relationships with many pharmaceutical companies, including those that make acne drugs.
FROM SOC 2020
Chinese American families suffer discrimination related to COVID-19
according to results from a survey study.
In the United States, where public officials continue to refer to SARS-CoV-2 as the “China virus” and have often sought to draw attention to its origins in Wuhan, China, “the associations between discrimination triggered by the racialization of this acute public health crisis and mental health are unknown,” Charissa S.L. Cheah, PhD, of the University of Maryland, Baltimore County, and colleagues wrote.
For their research published Oct. 29 in Pediatrics, Dr. Cheah and colleagues recruited a cohort of 543 Chinese American parents of school-age children, and 230 of their children aged 10-18 years, to complete online surveys between mid-March and late May 2020. Parents in the cohort were largely foreign born, with all identifying as ethnically Chinese, while their children were mostly U.S. born.
Evidence of discrimination against Chinese Americans
Half of parents and their children (51% of parents and 50% of youth) reported experiencing at least one in-person incident of direct discrimination (assessed using questions derived from a validated scale of racial aggression) related to the pandemic. Dr. Cheah and colleagues also reported a high incidence of direct discrimination online (32% of parents and 46% of youth). Additionally, the researchers measured reports of vicarious or indirect discrimination – such as hearing jokes or disparaging remarks about one’s ethnic group – which they used a different adapted scale to capture. More than three-quarters of the cohort reported such experiences.
The experiences of discrimination likely bore on the mental health of both parents and youth. Using a series of instruments designed to measure overall psychological well-being as well as symptoms of depression, anxiety, and certain emotional and behavioral outcomes, Dr. Cheah and colleagues reported significant negative associations between direct online or in-person discrimination and psychological health. For parents and children alike, anxiety and depressive symptoms were positively associated with all varieties of discrimination experiences measured in the study.
About a fifth of the youth in the study were deemed, based on the symptom scales used in the study, to have an elevated risk of clinically significant mental health problems, higher than the 10%-15% that would be expected for these age groups in the United States.
“This study revealed that a high percentage of Chinese American parents and their children personally experienced or witnessed anti-Chinese or anti–Asian American racial discrimination both online and in person due to the COVID-19 pandemic,” the investigators wrote. “Most respondents reported directly experiencing or witnessing racial discrimination against other Chinese or Asian American individuals due to COVID-19 at least once.”
Dr. Cheah and colleagues noted that their cross-sectional study did not lend itself to causal interpretations and was vulnerable to certain types of reporting bias. Nonetheless, they argued, as the pandemic continues, “pediatricians should be sensitive to the potential mental health needs of Chinese American youth and their parents related to various forms of racism, in addition to other stressors, as the foundations of perceptions of racial-ethnic discrimination and their consequences may be set during this period.”
COVID-19 didn’t only bring infection
In an accompanying editorial, Tina L. Cheng, MD, of Johns Hopkins University, Baltimore, and her daughter Alison M. Conca-Cheng, a medical student at Brown University, Providence, R.I., remarked that the study’s findings were consistent with recent research that found “4 in 10 Americans reported that it has become more common since COVID-19 for people to express racist views about Asian Americans,” and also described an increase in complaints of discriminatory experiences by Asian Americans.
In this context, a link to poor mental health “should be no surprise,” Dr. Cheng and Ms. Conca-Cheng argued, and urged pediatricians to consult the American Academy of Pediatrics’ 2019 policy statement on racism and on child and adolescent health. “It calls for us to optimize clinical practice, improve workforce development and professional education, strengthen research, and deploy systems through community engagement, advocacy, and public policy.”
David Rettew, MD, a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington, called the study’s main points “clear and disturbing.”
“While it is difficult to find much in the way here of a silver lining, these alarming reports have helped people working in health care and mental health to understand racism as another form of trauma and abuse which, like other types, can have real negative effects on health,” Dr. Rettew said in an interview. “The more we as mental health professions ask about racism and offer resources for people who have experienced it, just as we would people who have endured other types of trauma, the more we can help people heal. That said, it would be better just to stop this from happening in the first place.”
Dr. Cheah and colleagues’ study was supported by a National Science Foundation grant. The investigators disclosed no conflicts of interest. Dr. Cheng and Ms. Conca-Cheng disclosed no financial conflicts of interest related to their editorial. Dr. Rettew said he had no relevant financial disclosures.
SOURCE: Cheah CSL et al. Pediatrics. 2020;146(5):e2020021816.
according to results from a survey study.
In the United States, where public officials continue to refer to SARS-CoV-2 as the “China virus” and have often sought to draw attention to its origins in Wuhan, China, “the associations between discrimination triggered by the racialization of this acute public health crisis and mental health are unknown,” Charissa S.L. Cheah, PhD, of the University of Maryland, Baltimore County, and colleagues wrote.
For their research published Oct. 29 in Pediatrics, Dr. Cheah and colleagues recruited a cohort of 543 Chinese American parents of school-age children, and 230 of their children aged 10-18 years, to complete online surveys between mid-March and late May 2020. Parents in the cohort were largely foreign born, with all identifying as ethnically Chinese, while their children were mostly U.S. born.
Evidence of discrimination against Chinese Americans
Half of parents and their children (51% of parents and 50% of youth) reported experiencing at least one in-person incident of direct discrimination (assessed using questions derived from a validated scale of racial aggression) related to the pandemic. Dr. Cheah and colleagues also reported a high incidence of direct discrimination online (32% of parents and 46% of youth). Additionally, the researchers measured reports of vicarious or indirect discrimination – such as hearing jokes or disparaging remarks about one’s ethnic group – which they used a different adapted scale to capture. More than three-quarters of the cohort reported such experiences.
The experiences of discrimination likely bore on the mental health of both parents and youth. Using a series of instruments designed to measure overall psychological well-being as well as symptoms of depression, anxiety, and certain emotional and behavioral outcomes, Dr. Cheah and colleagues reported significant negative associations between direct online or in-person discrimination and psychological health. For parents and children alike, anxiety and depressive symptoms were positively associated with all varieties of discrimination experiences measured in the study.
About a fifth of the youth in the study were deemed, based on the symptom scales used in the study, to have an elevated risk of clinically significant mental health problems, higher than the 10%-15% that would be expected for these age groups in the United States.
“This study revealed that a high percentage of Chinese American parents and their children personally experienced or witnessed anti-Chinese or anti–Asian American racial discrimination both online and in person due to the COVID-19 pandemic,” the investigators wrote. “Most respondents reported directly experiencing or witnessing racial discrimination against other Chinese or Asian American individuals due to COVID-19 at least once.”
Dr. Cheah and colleagues noted that their cross-sectional study did not lend itself to causal interpretations and was vulnerable to certain types of reporting bias. Nonetheless, they argued, as the pandemic continues, “pediatricians should be sensitive to the potential mental health needs of Chinese American youth and their parents related to various forms of racism, in addition to other stressors, as the foundations of perceptions of racial-ethnic discrimination and their consequences may be set during this period.”
COVID-19 didn’t only bring infection
In an accompanying editorial, Tina L. Cheng, MD, of Johns Hopkins University, Baltimore, and her daughter Alison M. Conca-Cheng, a medical student at Brown University, Providence, R.I., remarked that the study’s findings were consistent with recent research that found “4 in 10 Americans reported that it has become more common since COVID-19 for people to express racist views about Asian Americans,” and also described an increase in complaints of discriminatory experiences by Asian Americans.
In this context, a link to poor mental health “should be no surprise,” Dr. Cheng and Ms. Conca-Cheng argued, and urged pediatricians to consult the American Academy of Pediatrics’ 2019 policy statement on racism and on child and adolescent health. “It calls for us to optimize clinical practice, improve workforce development and professional education, strengthen research, and deploy systems through community engagement, advocacy, and public policy.”
David Rettew, MD, a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington, called the study’s main points “clear and disturbing.”
“While it is difficult to find much in the way here of a silver lining, these alarming reports have helped people working in health care and mental health to understand racism as another form of trauma and abuse which, like other types, can have real negative effects on health,” Dr. Rettew said in an interview. “The more we as mental health professions ask about racism and offer resources for people who have experienced it, just as we would people who have endured other types of trauma, the more we can help people heal. That said, it would be better just to stop this from happening in the first place.”
Dr. Cheah and colleagues’ study was supported by a National Science Foundation grant. The investigators disclosed no conflicts of interest. Dr. Cheng and Ms. Conca-Cheng disclosed no financial conflicts of interest related to their editorial. Dr. Rettew said he had no relevant financial disclosures.
SOURCE: Cheah CSL et al. Pediatrics. 2020;146(5):e2020021816.
according to results from a survey study.
In the United States, where public officials continue to refer to SARS-CoV-2 as the “China virus” and have often sought to draw attention to its origins in Wuhan, China, “the associations between discrimination triggered by the racialization of this acute public health crisis and mental health are unknown,” Charissa S.L. Cheah, PhD, of the University of Maryland, Baltimore County, and colleagues wrote.
For their research published Oct. 29 in Pediatrics, Dr. Cheah and colleagues recruited a cohort of 543 Chinese American parents of school-age children, and 230 of their children aged 10-18 years, to complete online surveys between mid-March and late May 2020. Parents in the cohort were largely foreign born, with all identifying as ethnically Chinese, while their children were mostly U.S. born.
Evidence of discrimination against Chinese Americans
Half of parents and their children (51% of parents and 50% of youth) reported experiencing at least one in-person incident of direct discrimination (assessed using questions derived from a validated scale of racial aggression) related to the pandemic. Dr. Cheah and colleagues also reported a high incidence of direct discrimination online (32% of parents and 46% of youth). Additionally, the researchers measured reports of vicarious or indirect discrimination – such as hearing jokes or disparaging remarks about one’s ethnic group – which they used a different adapted scale to capture. More than three-quarters of the cohort reported such experiences.
The experiences of discrimination likely bore on the mental health of both parents and youth. Using a series of instruments designed to measure overall psychological well-being as well as symptoms of depression, anxiety, and certain emotional and behavioral outcomes, Dr. Cheah and colleagues reported significant negative associations between direct online or in-person discrimination and psychological health. For parents and children alike, anxiety and depressive symptoms were positively associated with all varieties of discrimination experiences measured in the study.
About a fifth of the youth in the study were deemed, based on the symptom scales used in the study, to have an elevated risk of clinically significant mental health problems, higher than the 10%-15% that would be expected for these age groups in the United States.
“This study revealed that a high percentage of Chinese American parents and their children personally experienced or witnessed anti-Chinese or anti–Asian American racial discrimination both online and in person due to the COVID-19 pandemic,” the investigators wrote. “Most respondents reported directly experiencing or witnessing racial discrimination against other Chinese or Asian American individuals due to COVID-19 at least once.”
Dr. Cheah and colleagues noted that their cross-sectional study did not lend itself to causal interpretations and was vulnerable to certain types of reporting bias. Nonetheless, they argued, as the pandemic continues, “pediatricians should be sensitive to the potential mental health needs of Chinese American youth and their parents related to various forms of racism, in addition to other stressors, as the foundations of perceptions of racial-ethnic discrimination and their consequences may be set during this period.”
COVID-19 didn’t only bring infection
In an accompanying editorial, Tina L. Cheng, MD, of Johns Hopkins University, Baltimore, and her daughter Alison M. Conca-Cheng, a medical student at Brown University, Providence, R.I., remarked that the study’s findings were consistent with recent research that found “4 in 10 Americans reported that it has become more common since COVID-19 for people to express racist views about Asian Americans,” and also described an increase in complaints of discriminatory experiences by Asian Americans.
In this context, a link to poor mental health “should be no surprise,” Dr. Cheng and Ms. Conca-Cheng argued, and urged pediatricians to consult the American Academy of Pediatrics’ 2019 policy statement on racism and on child and adolescent health. “It calls for us to optimize clinical practice, improve workforce development and professional education, strengthen research, and deploy systems through community engagement, advocacy, and public policy.”
David Rettew, MD, a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington, called the study’s main points “clear and disturbing.”
“While it is difficult to find much in the way here of a silver lining, these alarming reports have helped people working in health care and mental health to understand racism as another form of trauma and abuse which, like other types, can have real negative effects on health,” Dr. Rettew said in an interview. “The more we as mental health professions ask about racism and offer resources for people who have experienced it, just as we would people who have endured other types of trauma, the more we can help people heal. That said, it would be better just to stop this from happening in the first place.”
Dr. Cheah and colleagues’ study was supported by a National Science Foundation grant. The investigators disclosed no conflicts of interest. Dr. Cheng and Ms. Conca-Cheng disclosed no financial conflicts of interest related to their editorial. Dr. Rettew said he had no relevant financial disclosures.
SOURCE: Cheah CSL et al. Pediatrics. 2020;146(5):e2020021816.
FROM PEDIATRICS