User login
AHA/ACC guidance on ethics, professionalism in cardiovascular care
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.
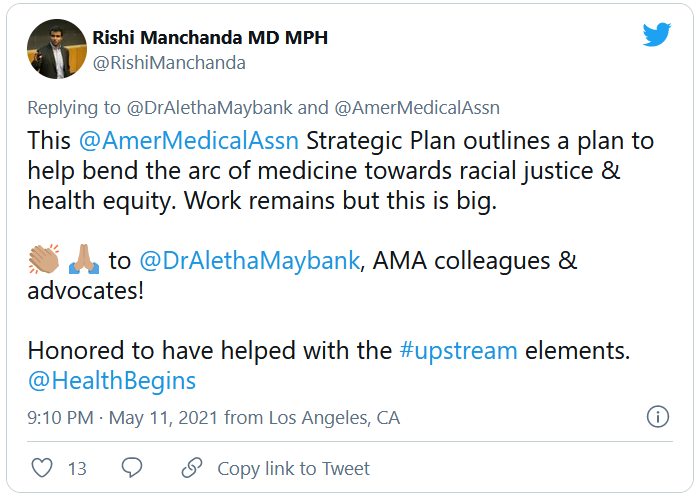
Addressing today’s racial health inequities requires understanding their roots
The health disparities seen in today’s high rates of Black infant and maternal morbidity and mortality are rooted in health inequities and generational stress dating back centuries in the United States, but today’s obstetricians can make changes in their own practices to address this inequity, according to Haywood L. Brown, MD, professor of ob.gyn. and associate dean of diversity at the Morsani College of Medicine and vice president of institutional equity at the University of South Florida, Tampa.
Dr. Brown delivered his remarks during the Benson and Pamela Harer Seminar on History at the annual meeting of the American College of Obstetricians and Gynecologists on May 2. His talk focused on the origins of perinatal and maternal health inequities and how those original factors play out today in increased maternal and neonatal morbidity and mortality among Black women and their babies.
“Racial and ethnic disparities and inequity in maternal and child health are prevalent and persistent. We have to move beyond the documentation,” Dr. Brown told attendees. “We have to adopt uniform care standards, recognizing our own biases and understanding that the contribution of social determinants of health are important in the care and outcome of women. And we have to work on decreasing the stress of women who give birth.”
Evelyn Nicole Mitchell, MD, faculty chair of the ob.gyn. diversity and inclusion committee at the University of Southern California, found Dr. Brown’s talk compelling and hopes it opens the eyes of others who attended.
“You really have to understand the why behind the problems we have, and it really goes back to slavery and this historical distrust that’s been here from the beginning,” Dr. Mitchell said in an interview. “I hope this allows people to open their eyes and think about this situation from their patients’ shoes, to really put their guard down and explore, ‘how can I contribute to fixing this system that has been here from the beginning?’ I think a lot of people get defensive and think: ‘Oh, I’m not a racist. I just don’t want to talk about this,’ but it’s about a system being racist.” The question then, Dr. Mitchell said, is: “So how do I contribute to that system?”
Dr. Brown frequently returned to the theme of high stress levels in Black mothers contributing to poorer outcomes, such as preterm birth. That stress arises originally from the generational stress brought on by racism and oppression over the centuries but has been compounded by poverty, racial injustice, lack of access to adequate nutrition, lower education levels, environmental factors, and other determinants of health.
“The bottom line, as Dr. Brown said, is that we need to decrease the stress level of Black mothers giving birth,” Dr. Mitchell said. “How can I, as a provider, decrease the stress level of my patients? Well, No. 1, I can identify and eliminate implicit bias that I may harbor.”
Slavery husbandry laid the groundwork for today
The most surprising aspect of Dr. Brown’s lecture for Dr. Mitchell was the fact that enslaved women received a measure of protection that other enslaved people did not to “ensure that they were healthy and that they were able to reproduce in the future,” Dr. Mitchell said. “It was for the wrong reasons – to keep slavery going – but in a sense they were prioritizing Black women to take advantage of their reproductive capacity, compared to nowadays where Black women are facing severe disparities.”
To safeguard enslaved women’s fecundity, plantation owners attempted to reduce stressors in the women’s lives, such as allowing them to cohabitate with a husband and nuclear family, though sexual assault and abuse still occurred. The owners also tracked the enslaved girls’ menstrual cycles after menarche to maximize their “breeding” potential, especially between the ages of 15 and 24. Slave owners delegated older enslaved women as maternity caregivers and midwives, leading to the passing down of midwifery skills through generations of Black American women.
“Pregnant women received the best medical care on the plantation because of the premium placed on reproduction,” Dr. Brown said. Wealthier planters called in doctors for complicated deliveries, which provided J. Marian Sims the ability conduct surgical experiments on Betsey, Lucy, and Anarcha to treat vesicovaginal fistula since fistula “limited her ability to do the maximum work she could in the house or on the plantation,” Dr. Brown said.
After slavery ended, health care access did not improve for Black people. In 1920, there was approximately 1 Black physician for every 3,000 Black people, compared with 1 in 500 for the White population, and grannie midwives continued to be the primary birthing attendants for Black women. Over the next several decades, however, both maternal and infant mortality across all races began steeply dropping. Reasons for the drop included the incorporation of the American Board of Obstetrics and Gynecology in 1930, a shift from home births to hospital births, and the legalization of abortion, which led to an 89% decline in deaths from septic illegal abortions from 1950 to 1973.
Still, Black maternal and infant mortality remained higher than White, and the poverty gap further exacerbated outcomes.
“Substandard maternity care really is the origin of many of the Black maternal and infant morbidity and mortality” complications, such as low birth weight, small for gestational age, growth restriction, and intrauterine starvation, “which we now believe are the origin of things like hypertension, diabetes, and obesity,” Dr. Brown said.
Today, inequities persist because of the systemic racism throughout this history.
“As we talk about health disparities, prematurity, growth restriction, and maternal morbidity, the fetal origins for adult disease in diabetes and hypertension and obesity have generational implications over the last 400 years,” Dr. Brown said. “Generational stress and stresses in lack women from slavery to present times are some of the origins of the things that we see today, including segregation, economic inequities, eugenic sterilizations, the quality of education, and of course, systemic racism on health care access and quality.”
It is this long arc of history that Dr. Mitchell hopes attendees will begin to grasp.
“If you don’t understand all that and have that depth, there’s no way for you to truly understand the problems that are going on and how to solve them,” Dr. Mitchell said. She hopes that especially those who have been more “resistant to accepting these truths” can start to see the big picture. “Hopefully, they can look at it as a systemic problem and then focus on how they can change the system.”
Dr Brown is a contributor to UpToDate and the Merck Manual and serves on the advisory boards of Merck for Mothers Global Women’s Health and BabyScripts. Dr. Mitchell has no disclosures.
The health disparities seen in today’s high rates of Black infant and maternal morbidity and mortality are rooted in health inequities and generational stress dating back centuries in the United States, but today’s obstetricians can make changes in their own practices to address this inequity, according to Haywood L. Brown, MD, professor of ob.gyn. and associate dean of diversity at the Morsani College of Medicine and vice president of institutional equity at the University of South Florida, Tampa.
Dr. Brown delivered his remarks during the Benson and Pamela Harer Seminar on History at the annual meeting of the American College of Obstetricians and Gynecologists on May 2. His talk focused on the origins of perinatal and maternal health inequities and how those original factors play out today in increased maternal and neonatal morbidity and mortality among Black women and their babies.
“Racial and ethnic disparities and inequity in maternal and child health are prevalent and persistent. We have to move beyond the documentation,” Dr. Brown told attendees. “We have to adopt uniform care standards, recognizing our own biases and understanding that the contribution of social determinants of health are important in the care and outcome of women. And we have to work on decreasing the stress of women who give birth.”
Evelyn Nicole Mitchell, MD, faculty chair of the ob.gyn. diversity and inclusion committee at the University of Southern California, found Dr. Brown’s talk compelling and hopes it opens the eyes of others who attended.
“You really have to understand the why behind the problems we have, and it really goes back to slavery and this historical distrust that’s been here from the beginning,” Dr. Mitchell said in an interview. “I hope this allows people to open their eyes and think about this situation from their patients’ shoes, to really put their guard down and explore, ‘how can I contribute to fixing this system that has been here from the beginning?’ I think a lot of people get defensive and think: ‘Oh, I’m not a racist. I just don’t want to talk about this,’ but it’s about a system being racist.” The question then, Dr. Mitchell said, is: “So how do I contribute to that system?”
Dr. Brown frequently returned to the theme of high stress levels in Black mothers contributing to poorer outcomes, such as preterm birth. That stress arises originally from the generational stress brought on by racism and oppression over the centuries but has been compounded by poverty, racial injustice, lack of access to adequate nutrition, lower education levels, environmental factors, and other determinants of health.
“The bottom line, as Dr. Brown said, is that we need to decrease the stress level of Black mothers giving birth,” Dr. Mitchell said. “How can I, as a provider, decrease the stress level of my patients? Well, No. 1, I can identify and eliminate implicit bias that I may harbor.”
Slavery husbandry laid the groundwork for today
The most surprising aspect of Dr. Brown’s lecture for Dr. Mitchell was the fact that enslaved women received a measure of protection that other enslaved people did not to “ensure that they were healthy and that they were able to reproduce in the future,” Dr. Mitchell said. “It was for the wrong reasons – to keep slavery going – but in a sense they were prioritizing Black women to take advantage of their reproductive capacity, compared to nowadays where Black women are facing severe disparities.”
To safeguard enslaved women’s fecundity, plantation owners attempted to reduce stressors in the women’s lives, such as allowing them to cohabitate with a husband and nuclear family, though sexual assault and abuse still occurred. The owners also tracked the enslaved girls’ menstrual cycles after menarche to maximize their “breeding” potential, especially between the ages of 15 and 24. Slave owners delegated older enslaved women as maternity caregivers and midwives, leading to the passing down of midwifery skills through generations of Black American women.
“Pregnant women received the best medical care on the plantation because of the premium placed on reproduction,” Dr. Brown said. Wealthier planters called in doctors for complicated deliveries, which provided J. Marian Sims the ability conduct surgical experiments on Betsey, Lucy, and Anarcha to treat vesicovaginal fistula since fistula “limited her ability to do the maximum work she could in the house or on the plantation,” Dr. Brown said.
After slavery ended, health care access did not improve for Black people. In 1920, there was approximately 1 Black physician for every 3,000 Black people, compared with 1 in 500 for the White population, and grannie midwives continued to be the primary birthing attendants for Black women. Over the next several decades, however, both maternal and infant mortality across all races began steeply dropping. Reasons for the drop included the incorporation of the American Board of Obstetrics and Gynecology in 1930, a shift from home births to hospital births, and the legalization of abortion, which led to an 89% decline in deaths from septic illegal abortions from 1950 to 1973.
Still, Black maternal and infant mortality remained higher than White, and the poverty gap further exacerbated outcomes.
“Substandard maternity care really is the origin of many of the Black maternal and infant morbidity and mortality” complications, such as low birth weight, small for gestational age, growth restriction, and intrauterine starvation, “which we now believe are the origin of things like hypertension, diabetes, and obesity,” Dr. Brown said.
Today, inequities persist because of the systemic racism throughout this history.
“As we talk about health disparities, prematurity, growth restriction, and maternal morbidity, the fetal origins for adult disease in diabetes and hypertension and obesity have generational implications over the last 400 years,” Dr. Brown said. “Generational stress and stresses in lack women from slavery to present times are some of the origins of the things that we see today, including segregation, economic inequities, eugenic sterilizations, the quality of education, and of course, systemic racism on health care access and quality.”
It is this long arc of history that Dr. Mitchell hopes attendees will begin to grasp.
“If you don’t understand all that and have that depth, there’s no way for you to truly understand the problems that are going on and how to solve them,” Dr. Mitchell said. She hopes that especially those who have been more “resistant to accepting these truths” can start to see the big picture. “Hopefully, they can look at it as a systemic problem and then focus on how they can change the system.”
Dr Brown is a contributor to UpToDate and the Merck Manual and serves on the advisory boards of Merck for Mothers Global Women’s Health and BabyScripts. Dr. Mitchell has no disclosures.
The health disparities seen in today’s high rates of Black infant and maternal morbidity and mortality are rooted in health inequities and generational stress dating back centuries in the United States, but today’s obstetricians can make changes in their own practices to address this inequity, according to Haywood L. Brown, MD, professor of ob.gyn. and associate dean of diversity at the Morsani College of Medicine and vice president of institutional equity at the University of South Florida, Tampa.
Dr. Brown delivered his remarks during the Benson and Pamela Harer Seminar on History at the annual meeting of the American College of Obstetricians and Gynecologists on May 2. His talk focused on the origins of perinatal and maternal health inequities and how those original factors play out today in increased maternal and neonatal morbidity and mortality among Black women and their babies.
“Racial and ethnic disparities and inequity in maternal and child health are prevalent and persistent. We have to move beyond the documentation,” Dr. Brown told attendees. “We have to adopt uniform care standards, recognizing our own biases and understanding that the contribution of social determinants of health are important in the care and outcome of women. And we have to work on decreasing the stress of women who give birth.”
Evelyn Nicole Mitchell, MD, faculty chair of the ob.gyn. diversity and inclusion committee at the University of Southern California, found Dr. Brown’s talk compelling and hopes it opens the eyes of others who attended.
“You really have to understand the why behind the problems we have, and it really goes back to slavery and this historical distrust that’s been here from the beginning,” Dr. Mitchell said in an interview. “I hope this allows people to open their eyes and think about this situation from their patients’ shoes, to really put their guard down and explore, ‘how can I contribute to fixing this system that has been here from the beginning?’ I think a lot of people get defensive and think: ‘Oh, I’m not a racist. I just don’t want to talk about this,’ but it’s about a system being racist.” The question then, Dr. Mitchell said, is: “So how do I contribute to that system?”
Dr. Brown frequently returned to the theme of high stress levels in Black mothers contributing to poorer outcomes, such as preterm birth. That stress arises originally from the generational stress brought on by racism and oppression over the centuries but has been compounded by poverty, racial injustice, lack of access to adequate nutrition, lower education levels, environmental factors, and other determinants of health.
“The bottom line, as Dr. Brown said, is that we need to decrease the stress level of Black mothers giving birth,” Dr. Mitchell said. “How can I, as a provider, decrease the stress level of my patients? Well, No. 1, I can identify and eliminate implicit bias that I may harbor.”
Slavery husbandry laid the groundwork for today
The most surprising aspect of Dr. Brown’s lecture for Dr. Mitchell was the fact that enslaved women received a measure of protection that other enslaved people did not to “ensure that they were healthy and that they were able to reproduce in the future,” Dr. Mitchell said. “It was for the wrong reasons – to keep slavery going – but in a sense they were prioritizing Black women to take advantage of their reproductive capacity, compared to nowadays where Black women are facing severe disparities.”
To safeguard enslaved women’s fecundity, plantation owners attempted to reduce stressors in the women’s lives, such as allowing them to cohabitate with a husband and nuclear family, though sexual assault and abuse still occurred. The owners also tracked the enslaved girls’ menstrual cycles after menarche to maximize their “breeding” potential, especially between the ages of 15 and 24. Slave owners delegated older enslaved women as maternity caregivers and midwives, leading to the passing down of midwifery skills through generations of Black American women.
“Pregnant women received the best medical care on the plantation because of the premium placed on reproduction,” Dr. Brown said. Wealthier planters called in doctors for complicated deliveries, which provided J. Marian Sims the ability conduct surgical experiments on Betsey, Lucy, and Anarcha to treat vesicovaginal fistula since fistula “limited her ability to do the maximum work she could in the house or on the plantation,” Dr. Brown said.
After slavery ended, health care access did not improve for Black people. In 1920, there was approximately 1 Black physician for every 3,000 Black people, compared with 1 in 500 for the White population, and grannie midwives continued to be the primary birthing attendants for Black women. Over the next several decades, however, both maternal and infant mortality across all races began steeply dropping. Reasons for the drop included the incorporation of the American Board of Obstetrics and Gynecology in 1930, a shift from home births to hospital births, and the legalization of abortion, which led to an 89% decline in deaths from septic illegal abortions from 1950 to 1973.
Still, Black maternal and infant mortality remained higher than White, and the poverty gap further exacerbated outcomes.
“Substandard maternity care really is the origin of many of the Black maternal and infant morbidity and mortality” complications, such as low birth weight, small for gestational age, growth restriction, and intrauterine starvation, “which we now believe are the origin of things like hypertension, diabetes, and obesity,” Dr. Brown said.
Today, inequities persist because of the systemic racism throughout this history.
“As we talk about health disparities, prematurity, growth restriction, and maternal morbidity, the fetal origins for adult disease in diabetes and hypertension and obesity have generational implications over the last 400 years,” Dr. Brown said. “Generational stress and stresses in lack women from slavery to present times are some of the origins of the things that we see today, including segregation, economic inequities, eugenic sterilizations, the quality of education, and of course, systemic racism on health care access and quality.”
It is this long arc of history that Dr. Mitchell hopes attendees will begin to grasp.
“If you don’t understand all that and have that depth, there’s no way for you to truly understand the problems that are going on and how to solve them,” Dr. Mitchell said. She hopes that especially those who have been more “resistant to accepting these truths” can start to see the big picture. “Hopefully, they can look at it as a systemic problem and then focus on how they can change the system.”
Dr Brown is a contributor to UpToDate and the Merck Manual and serves on the advisory boards of Merck for Mothers Global Women’s Health and BabyScripts. Dr. Mitchell has no disclosures.
FROM ACOG 2021
AMA announces major commitment to health equity
The 82-page report, which was created by the association’s Center for Health Equity, argues for both internal changes at the AMA and changes in how the association addresses race-based inequities in general.
The report was released just 2 months after this news organization reported that a podcast hosted by AMA’s top journal was lambasted as racist and out of touch. In the podcast – entitled “Stuctural Racism for Doctors – What Is It?” – one JAMA editor argued that structural racism doesn’t exist. He eventually resigned and the journal’s top editor was placed on administration leave.
The new AMA report’s strategic framework “is driven by the immense need for equity-centered solutions to confront harms produced by systemic racism and other forms of oppression for Black, Latinx, Indigenous, Asian, and other people of color, as well as people who identify as LGBTQ+ and people with disabilities,” the AMA said in a news release. “Its urgency is underscored by ongoing circumstances including inequities exacerbated by the COVID-19 pandemic, ongoing police brutality, and hate crimes targeting Asian, Black, and Brown communities.”
The plan includes five main approaches to addressing inequities in health care and the AMA:
- Implement antiracist equity strategies through AMA practices, programming, policies, and culture.
- Build alliances with marginalized doctors and other stakeholders to elevate the experiences and ideas of historically marginalized and minority health care leaders.
- Strengthen, empower, and equip doctors with the knowledge and tools to dismantle structural and social health inequities.
- Ensure equitable opportunities in innovation.
- Foster truth, racial healing, reconciliation, and transformation for AMA’s past by accounting for how policies and processes excluded, discriminated, and harmed communities.
As the report acknowledges, the AMA has a long history of exclusion of and discrimination against Black physicians, for which the association publicly apologized in 2008. Within the past year, the AMA has reaffirmed its commitment to addressing this legacy and to be proactive on health equity.
Among other things, the association has described racism as a public health crisis, stated that race has nothing to do with biology, said police brutality is a product of structural racism, and called on the federal government to collect and release COVID-19 race/ethnicity data. It also removed the name of AMA founder Nathan Davis, MD, from an annual award and display because of his contribution to explicit racist practices.
Equity-centered solutions
The AMA launched its Center for Health Equity in 2019 with a mandate “to embed health equity across the organization.” Aletha Maybank, MD, was named the AMA’s chief health equity officer to lead the center.
In the report that Dr. Maybank helped write, the AMA discusses the consequences of individual and systemic injustice toward minorities. Among these consequences, the report said, is “segregated and inequitable health care systems.”
The “equity-centered solutions” listed in the report include:
- End segregated health care.
- Establish national health care equity and racial justice standards.
- End the use of race-based clinical decision models.
- Eliminate all forms of discrimination, exclusion and oppression in medical and physician education, training, hiring, and promotion.
- Prevent exclusion of and ensure equal representation of Black, Indigenous and Latinx people in medical school admissions as well as medical school and hospital leadership ranks.
- Ensure equity in innovation, including design, development, implementation along with support for equitable innovation opportunities and entrepreneurship.
- Solidify connections and coordination between health care and public health.
- Acknowledge and repair past harms committed by institutions.
Changing medical education
In an exclusive interview, Gerald E. Harmon, MD, president-elect of the AMA, singled out medical education as an area that is ripe for change. “One of the most threatened phenotypes on the planet is the Black male physician,” he said. “Their numbers among medical school applicants continue to drop. We have increasing numbers of women in medical schools – over 50% of trainees are women – and more Black women are entering medical school, but Black men in medical school are an endangered species.
“We’re trying to get the physician workforce to look like the patient workforce.”
Dr. Harmon cited the “pipeline program” at the Morehouse School of Medicine in Atlanta and the AMA’s “doctors back to school” program as examples of efforts to attract minority high school students to health care careers. Much more needs to be done, he added. “We have to put equity and representation into our medical workforce so we can provide better high quality, more reliable care for underrepresented patients.”
Putting the AMA’s house in order
In its report, the AMA also makes recommendations about how it can improve equity within its own organization. Over the next 3 years, among other things, the association plans to improve the diversity of leadership at the AMA and its journal, JAMA; train all staff on equity requirements; and develop a plan to recruit more racial and ethnic minorities, LGBTQ+ people, and disabled people.
Dr. Maybank, the AMA’s chief health equity officer, said in an interview that she wouldn’t describe these efforts as affirmative action. “This is beyond affirmative action. It’s about intentional activity and action to ensure equity and justice within the AMA.”
The AMA has to thoroughly examine its own processes and determine “how inequity shows up on a day-to-day basis,” she said. “Whether it’s through hiring, innovation, publishing or communications, everybody needs to know how inequity shows up and how their own mental models can exacerbate inequities. People need tools to challenge themselves and ask themselves critical questions about racism in their processes and what they can do to mitigate those.”
A version of this article first appeared on WebMD.com.
The 82-page report, which was created by the association’s Center for Health Equity, argues for both internal changes at the AMA and changes in how the association addresses race-based inequities in general.
The report was released just 2 months after this news organization reported that a podcast hosted by AMA’s top journal was lambasted as racist and out of touch. In the podcast – entitled “Stuctural Racism for Doctors – What Is It?” – one JAMA editor argued that structural racism doesn’t exist. He eventually resigned and the journal’s top editor was placed on administration leave.
The new AMA report’s strategic framework “is driven by the immense need for equity-centered solutions to confront harms produced by systemic racism and other forms of oppression for Black, Latinx, Indigenous, Asian, and other people of color, as well as people who identify as LGBTQ+ and people with disabilities,” the AMA said in a news release. “Its urgency is underscored by ongoing circumstances including inequities exacerbated by the COVID-19 pandemic, ongoing police brutality, and hate crimes targeting Asian, Black, and Brown communities.”
The plan includes five main approaches to addressing inequities in health care and the AMA:
- Implement antiracist equity strategies through AMA practices, programming, policies, and culture.
- Build alliances with marginalized doctors and other stakeholders to elevate the experiences and ideas of historically marginalized and minority health care leaders.
- Strengthen, empower, and equip doctors with the knowledge and tools to dismantle structural and social health inequities.
- Ensure equitable opportunities in innovation.
- Foster truth, racial healing, reconciliation, and transformation for AMA’s past by accounting for how policies and processes excluded, discriminated, and harmed communities.
As the report acknowledges, the AMA has a long history of exclusion of and discrimination against Black physicians, for which the association publicly apologized in 2008. Within the past year, the AMA has reaffirmed its commitment to addressing this legacy and to be proactive on health equity.
Among other things, the association has described racism as a public health crisis, stated that race has nothing to do with biology, said police brutality is a product of structural racism, and called on the federal government to collect and release COVID-19 race/ethnicity data. It also removed the name of AMA founder Nathan Davis, MD, from an annual award and display because of his contribution to explicit racist practices.
Equity-centered solutions
The AMA launched its Center for Health Equity in 2019 with a mandate “to embed health equity across the organization.” Aletha Maybank, MD, was named the AMA’s chief health equity officer to lead the center.
In the report that Dr. Maybank helped write, the AMA discusses the consequences of individual and systemic injustice toward minorities. Among these consequences, the report said, is “segregated and inequitable health care systems.”
The “equity-centered solutions” listed in the report include:
- End segregated health care.
- Establish national health care equity and racial justice standards.
- End the use of race-based clinical decision models.
- Eliminate all forms of discrimination, exclusion and oppression in medical and physician education, training, hiring, and promotion.
- Prevent exclusion of and ensure equal representation of Black, Indigenous and Latinx people in medical school admissions as well as medical school and hospital leadership ranks.
- Ensure equity in innovation, including design, development, implementation along with support for equitable innovation opportunities and entrepreneurship.
- Solidify connections and coordination between health care and public health.
- Acknowledge and repair past harms committed by institutions.
Changing medical education
In an exclusive interview, Gerald E. Harmon, MD, president-elect of the AMA, singled out medical education as an area that is ripe for change. “One of the most threatened phenotypes on the planet is the Black male physician,” he said. “Their numbers among medical school applicants continue to drop. We have increasing numbers of women in medical schools – over 50% of trainees are women – and more Black women are entering medical school, but Black men in medical school are an endangered species.
“We’re trying to get the physician workforce to look like the patient workforce.”
Dr. Harmon cited the “pipeline program” at the Morehouse School of Medicine in Atlanta and the AMA’s “doctors back to school” program as examples of efforts to attract minority high school students to health care careers. Much more needs to be done, he added. “We have to put equity and representation into our medical workforce so we can provide better high quality, more reliable care for underrepresented patients.”
Putting the AMA’s house in order
In its report, the AMA also makes recommendations about how it can improve equity within its own organization. Over the next 3 years, among other things, the association plans to improve the diversity of leadership at the AMA and its journal, JAMA; train all staff on equity requirements; and develop a plan to recruit more racial and ethnic minorities, LGBTQ+ people, and disabled people.
Dr. Maybank, the AMA’s chief health equity officer, said in an interview that she wouldn’t describe these efforts as affirmative action. “This is beyond affirmative action. It’s about intentional activity and action to ensure equity and justice within the AMA.”
The AMA has to thoroughly examine its own processes and determine “how inequity shows up on a day-to-day basis,” she said. “Whether it’s through hiring, innovation, publishing or communications, everybody needs to know how inequity shows up and how their own mental models can exacerbate inequities. People need tools to challenge themselves and ask themselves critical questions about racism in their processes and what they can do to mitigate those.”
A version of this article first appeared on WebMD.com.
The 82-page report, which was created by the association’s Center for Health Equity, argues for both internal changes at the AMA and changes in how the association addresses race-based inequities in general.
The report was released just 2 months after this news organization reported that a podcast hosted by AMA’s top journal was lambasted as racist and out of touch. In the podcast – entitled “Stuctural Racism for Doctors – What Is It?” – one JAMA editor argued that structural racism doesn’t exist. He eventually resigned and the journal’s top editor was placed on administration leave.
The new AMA report’s strategic framework “is driven by the immense need for equity-centered solutions to confront harms produced by systemic racism and other forms of oppression for Black, Latinx, Indigenous, Asian, and other people of color, as well as people who identify as LGBTQ+ and people with disabilities,” the AMA said in a news release. “Its urgency is underscored by ongoing circumstances including inequities exacerbated by the COVID-19 pandemic, ongoing police brutality, and hate crimes targeting Asian, Black, and Brown communities.”
The plan includes five main approaches to addressing inequities in health care and the AMA:
- Implement antiracist equity strategies through AMA practices, programming, policies, and culture.
- Build alliances with marginalized doctors and other stakeholders to elevate the experiences and ideas of historically marginalized and minority health care leaders.
- Strengthen, empower, and equip doctors with the knowledge and tools to dismantle structural and social health inequities.
- Ensure equitable opportunities in innovation.
- Foster truth, racial healing, reconciliation, and transformation for AMA’s past by accounting for how policies and processes excluded, discriminated, and harmed communities.
As the report acknowledges, the AMA has a long history of exclusion of and discrimination against Black physicians, for which the association publicly apologized in 2008. Within the past year, the AMA has reaffirmed its commitment to addressing this legacy and to be proactive on health equity.
Among other things, the association has described racism as a public health crisis, stated that race has nothing to do with biology, said police brutality is a product of structural racism, and called on the federal government to collect and release COVID-19 race/ethnicity data. It also removed the name of AMA founder Nathan Davis, MD, from an annual award and display because of his contribution to explicit racist practices.
Equity-centered solutions
The AMA launched its Center for Health Equity in 2019 with a mandate “to embed health equity across the organization.” Aletha Maybank, MD, was named the AMA’s chief health equity officer to lead the center.
In the report that Dr. Maybank helped write, the AMA discusses the consequences of individual and systemic injustice toward minorities. Among these consequences, the report said, is “segregated and inequitable health care systems.”
The “equity-centered solutions” listed in the report include:
- End segregated health care.
- Establish national health care equity and racial justice standards.
- End the use of race-based clinical decision models.
- Eliminate all forms of discrimination, exclusion and oppression in medical and physician education, training, hiring, and promotion.
- Prevent exclusion of and ensure equal representation of Black, Indigenous and Latinx people in medical school admissions as well as medical school and hospital leadership ranks.
- Ensure equity in innovation, including design, development, implementation along with support for equitable innovation opportunities and entrepreneurship.
- Solidify connections and coordination between health care and public health.
- Acknowledge and repair past harms committed by institutions.
Changing medical education
In an exclusive interview, Gerald E. Harmon, MD, president-elect of the AMA, singled out medical education as an area that is ripe for change. “One of the most threatened phenotypes on the planet is the Black male physician,” he said. “Their numbers among medical school applicants continue to drop. We have increasing numbers of women in medical schools – over 50% of trainees are women – and more Black women are entering medical school, but Black men in medical school are an endangered species.
“We’re trying to get the physician workforce to look like the patient workforce.”
Dr. Harmon cited the “pipeline program” at the Morehouse School of Medicine in Atlanta and the AMA’s “doctors back to school” program as examples of efforts to attract minority high school students to health care careers. Much more needs to be done, he added. “We have to put equity and representation into our medical workforce so we can provide better high quality, more reliable care for underrepresented patients.”
Putting the AMA’s house in order
In its report, the AMA also makes recommendations about how it can improve equity within its own organization. Over the next 3 years, among other things, the association plans to improve the diversity of leadership at the AMA and its journal, JAMA; train all staff on equity requirements; and develop a plan to recruit more racial and ethnic minorities, LGBTQ+ people, and disabled people.
Dr. Maybank, the AMA’s chief health equity officer, said in an interview that she wouldn’t describe these efforts as affirmative action. “This is beyond affirmative action. It’s about intentional activity and action to ensure equity and justice within the AMA.”
The AMA has to thoroughly examine its own processes and determine “how inequity shows up on a day-to-day basis,” she said. “Whether it’s through hiring, innovation, publishing or communications, everybody needs to know how inequity shows up and how their own mental models can exacerbate inequities. People need tools to challenge themselves and ask themselves critical questions about racism in their processes and what they can do to mitigate those.”
A version of this article first appeared on WebMD.com.
Photoprotection recommended for people of color
and applying a tinted sunscreen with an SPF of 30 or greater to exposed areas, according to Henry W. Lim, MD.
In addition, “with rigorous photoprotection, vitamin D supplementation should be advised to patients,” Dr. Lim, a former chair of the department of dermatology at Henry Ford Health System, Detroit, said during the Society for Pediatric Dermatology pre-AAD meeting. “One multivitamin a day should be sufficient for most patients. This is especially relevant because we do know that skin of color patients tend to have lower vitamin D levels to start with.”
Photoprotection for people of color helps minimize the development of photodermatoses, postinflammatory hyperpigmentation, polymorphous light eruption, and chronic actinic dermatitis, he said. In a retrospective chart review of 1,080 people conducted at four academic medical centers in the United States, Dr. Lim and colleagues found a higher proportion of polymorphous light eruption and chronic actinic dermatitis in Black individuals, and a higher proportion of photoallergic contact dermatitis, phototoxic drug eruptions, phytophotodermatitis, porphyria, and solar urticaria in White individuals.
“Another pediatric photodermatosis, actinic prurigo, tends to occur most often in Mestizo individuals, patients of American Indian heritage,” he added. “This is a significant issue, especially in Latin America.”
In a systematic review of 20 studies in the medical literature, researchers assessed the quality of life and psychological impact of photodermatoses in affected patients. Studies included in the review drew from 2,487 adults and 119 children. Among adults, the self-administered Dermatology Life Quality Index (DLQI) revealed that photodermatoses adversely affected employment, education, and leisure activities in adults. Among children, the condition adversely affected outdoor activities and exacerbated symptoms in those with erythropoietic protoporphyria (EPP).
As for skin cancer risk, the association between UV light exposure and the development of melanoma is not as strong in people with skin of color, compared with light-skinned individuals. In a recent systematic review of 13 studies on the topic, 11 showed no association, one showed a small positive relationship in Black males and 1 showed a weak association in Hispanic males.
“The conclusion from this review is that UV protection for melanoma prevention in people of color is not supported by most studies,” said Dr. Lim, who was not affiliated with the review. “The authors also noted, however, that the evidence is of moderate to low quality. Larger studies should be done.”
The association between UV exposure and the development to squamous cell cancer in skin of color is also not strong. “However, we do know that sun exposure is associated with the development of basal cell carcinoma in this population,” he said.
Sunscreen ingredient studies
Dr. Lim also highlighted findings from two studies related to the effect of sunscreen application on plasma concentration of sunscreen active ingredients, both in adults. In the most recent analysis, scientists at the Food and Drug Administration and colleagues conducted a randomized clinical trial in 48 individuals with skin types II-IV.
Participants applied sunscreen at 2 mg/cm2 to 75% of body surface area at 0 hours on day 1 and 4 times on day 2 through day 4 at 2-hour intervals. Over the course of 21 days, the researchers collected 34 blood samples from each participant, and evaluated six active ingredients in four sunscreen products: avobenzone, oxybenzone, octocrylene, homosalate, octisalate, and octinoxate.
For all active ingredients, levels of greater than 0.5 ng/mL were detected after a single application on day 1. Levels of greater than 0.5 ng/mL were detected up to day 7, and up to day 21 for oxybenzone. All were detected in skin on days 7 and 14 via tape stripping. The authors called for further studies to determine the clinical significance of these findings and emphasized that the results “do not indicate that individuals should refrain from the use of sunscreen.”
The FDA is asking for additional studies on the safety of these 12 filters, noted Dr. Lim, who is a past president of the American Academy of Dermatology. On Feb. 26, 2019, the FDA issued a proposed rule regarding sunscreen drug products for over-the-counter human use. It proposes that the 16 UV filters be classified into one of 3 categories. Category I would include zinc oxide and titanium dioxide, which are generally recognized as safe and effective (GRASE). Category II would include PABA and trolamine salicylate, which are not used in the United States and are not GRASE. Category III would include 12 filters that lack insufficient safety data to make a determination regarding GRASE.
The final FDA rule was scheduled to be released in September of 2020, but a result of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, the FDA “will be moving from a laborious rulemaking process to an administrative order process, which means it should not take as long to implement a monograph,” Dr. Lim said. “The FDA has decided that there will not be a final rule regarding sunscreen drug products,” but is required to issue a proposed administrative order by Sept. 27, 2021, he said.
When the final administrative order has been issued, manufacturers would have at least 1 year to comply with sunscreen products offered in the United States. “The approximate timeline is probably going to be 2023,” he said.
Dr. Lim disclosed that he is an investigator for Incyte, L’Oreal, Pfizer, and the Patient-centered Outcomes Research Institute, and a consultant for Pierre Fabre, ISDIN, Ferndale, La Roche–Posay, and Beiersdorf. He has been a speaker at general educational sessions sponsored by La Roche–Posay and Cantabria Labs.
and applying a tinted sunscreen with an SPF of 30 or greater to exposed areas, according to Henry W. Lim, MD.
In addition, “with rigorous photoprotection, vitamin D supplementation should be advised to patients,” Dr. Lim, a former chair of the department of dermatology at Henry Ford Health System, Detroit, said during the Society for Pediatric Dermatology pre-AAD meeting. “One multivitamin a day should be sufficient for most patients. This is especially relevant because we do know that skin of color patients tend to have lower vitamin D levels to start with.”
Photoprotection for people of color helps minimize the development of photodermatoses, postinflammatory hyperpigmentation, polymorphous light eruption, and chronic actinic dermatitis, he said. In a retrospective chart review of 1,080 people conducted at four academic medical centers in the United States, Dr. Lim and colleagues found a higher proportion of polymorphous light eruption and chronic actinic dermatitis in Black individuals, and a higher proportion of photoallergic contact dermatitis, phototoxic drug eruptions, phytophotodermatitis, porphyria, and solar urticaria in White individuals.
“Another pediatric photodermatosis, actinic prurigo, tends to occur most often in Mestizo individuals, patients of American Indian heritage,” he added. “This is a significant issue, especially in Latin America.”
In a systematic review of 20 studies in the medical literature, researchers assessed the quality of life and psychological impact of photodermatoses in affected patients. Studies included in the review drew from 2,487 adults and 119 children. Among adults, the self-administered Dermatology Life Quality Index (DLQI) revealed that photodermatoses adversely affected employment, education, and leisure activities in adults. Among children, the condition adversely affected outdoor activities and exacerbated symptoms in those with erythropoietic protoporphyria (EPP).
As for skin cancer risk, the association between UV light exposure and the development of melanoma is not as strong in people with skin of color, compared with light-skinned individuals. In a recent systematic review of 13 studies on the topic, 11 showed no association, one showed a small positive relationship in Black males and 1 showed a weak association in Hispanic males.
“The conclusion from this review is that UV protection for melanoma prevention in people of color is not supported by most studies,” said Dr. Lim, who was not affiliated with the review. “The authors also noted, however, that the evidence is of moderate to low quality. Larger studies should be done.”
The association between UV exposure and the development to squamous cell cancer in skin of color is also not strong. “However, we do know that sun exposure is associated with the development of basal cell carcinoma in this population,” he said.
Sunscreen ingredient studies
Dr. Lim also highlighted findings from two studies related to the effect of sunscreen application on plasma concentration of sunscreen active ingredients, both in adults. In the most recent analysis, scientists at the Food and Drug Administration and colleagues conducted a randomized clinical trial in 48 individuals with skin types II-IV.
Participants applied sunscreen at 2 mg/cm2 to 75% of body surface area at 0 hours on day 1 and 4 times on day 2 through day 4 at 2-hour intervals. Over the course of 21 days, the researchers collected 34 blood samples from each participant, and evaluated six active ingredients in four sunscreen products: avobenzone, oxybenzone, octocrylene, homosalate, octisalate, and octinoxate.
For all active ingredients, levels of greater than 0.5 ng/mL were detected after a single application on day 1. Levels of greater than 0.5 ng/mL were detected up to day 7, and up to day 21 for oxybenzone. All were detected in skin on days 7 and 14 via tape stripping. The authors called for further studies to determine the clinical significance of these findings and emphasized that the results “do not indicate that individuals should refrain from the use of sunscreen.”
The FDA is asking for additional studies on the safety of these 12 filters, noted Dr. Lim, who is a past president of the American Academy of Dermatology. On Feb. 26, 2019, the FDA issued a proposed rule regarding sunscreen drug products for over-the-counter human use. It proposes that the 16 UV filters be classified into one of 3 categories. Category I would include zinc oxide and titanium dioxide, which are generally recognized as safe and effective (GRASE). Category II would include PABA and trolamine salicylate, which are not used in the United States and are not GRASE. Category III would include 12 filters that lack insufficient safety data to make a determination regarding GRASE.
The final FDA rule was scheduled to be released in September of 2020, but a result of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, the FDA “will be moving from a laborious rulemaking process to an administrative order process, which means it should not take as long to implement a monograph,” Dr. Lim said. “The FDA has decided that there will not be a final rule regarding sunscreen drug products,” but is required to issue a proposed administrative order by Sept. 27, 2021, he said.
When the final administrative order has been issued, manufacturers would have at least 1 year to comply with sunscreen products offered in the United States. “The approximate timeline is probably going to be 2023,” he said.
Dr. Lim disclosed that he is an investigator for Incyte, L’Oreal, Pfizer, and the Patient-centered Outcomes Research Institute, and a consultant for Pierre Fabre, ISDIN, Ferndale, La Roche–Posay, and Beiersdorf. He has been a speaker at general educational sessions sponsored by La Roche–Posay and Cantabria Labs.
and applying a tinted sunscreen with an SPF of 30 or greater to exposed areas, according to Henry W. Lim, MD.
In addition, “with rigorous photoprotection, vitamin D supplementation should be advised to patients,” Dr. Lim, a former chair of the department of dermatology at Henry Ford Health System, Detroit, said during the Society for Pediatric Dermatology pre-AAD meeting. “One multivitamin a day should be sufficient for most patients. This is especially relevant because we do know that skin of color patients tend to have lower vitamin D levels to start with.”
Photoprotection for people of color helps minimize the development of photodermatoses, postinflammatory hyperpigmentation, polymorphous light eruption, and chronic actinic dermatitis, he said. In a retrospective chart review of 1,080 people conducted at four academic medical centers in the United States, Dr. Lim and colleagues found a higher proportion of polymorphous light eruption and chronic actinic dermatitis in Black individuals, and a higher proportion of photoallergic contact dermatitis, phototoxic drug eruptions, phytophotodermatitis, porphyria, and solar urticaria in White individuals.
“Another pediatric photodermatosis, actinic prurigo, tends to occur most often in Mestizo individuals, patients of American Indian heritage,” he added. “This is a significant issue, especially in Latin America.”
In a systematic review of 20 studies in the medical literature, researchers assessed the quality of life and psychological impact of photodermatoses in affected patients. Studies included in the review drew from 2,487 adults and 119 children. Among adults, the self-administered Dermatology Life Quality Index (DLQI) revealed that photodermatoses adversely affected employment, education, and leisure activities in adults. Among children, the condition adversely affected outdoor activities and exacerbated symptoms in those with erythropoietic protoporphyria (EPP).
As for skin cancer risk, the association between UV light exposure and the development of melanoma is not as strong in people with skin of color, compared with light-skinned individuals. In a recent systematic review of 13 studies on the topic, 11 showed no association, one showed a small positive relationship in Black males and 1 showed a weak association in Hispanic males.
“The conclusion from this review is that UV protection for melanoma prevention in people of color is not supported by most studies,” said Dr. Lim, who was not affiliated with the review. “The authors also noted, however, that the evidence is of moderate to low quality. Larger studies should be done.”
The association between UV exposure and the development to squamous cell cancer in skin of color is also not strong. “However, we do know that sun exposure is associated with the development of basal cell carcinoma in this population,” he said.
Sunscreen ingredient studies
Dr. Lim also highlighted findings from two studies related to the effect of sunscreen application on plasma concentration of sunscreen active ingredients, both in adults. In the most recent analysis, scientists at the Food and Drug Administration and colleagues conducted a randomized clinical trial in 48 individuals with skin types II-IV.
Participants applied sunscreen at 2 mg/cm2 to 75% of body surface area at 0 hours on day 1 and 4 times on day 2 through day 4 at 2-hour intervals. Over the course of 21 days, the researchers collected 34 blood samples from each participant, and evaluated six active ingredients in four sunscreen products: avobenzone, oxybenzone, octocrylene, homosalate, octisalate, and octinoxate.
For all active ingredients, levels of greater than 0.5 ng/mL were detected after a single application on day 1. Levels of greater than 0.5 ng/mL were detected up to day 7, and up to day 21 for oxybenzone. All were detected in skin on days 7 and 14 via tape stripping. The authors called for further studies to determine the clinical significance of these findings and emphasized that the results “do not indicate that individuals should refrain from the use of sunscreen.”
The FDA is asking for additional studies on the safety of these 12 filters, noted Dr. Lim, who is a past president of the American Academy of Dermatology. On Feb. 26, 2019, the FDA issued a proposed rule regarding sunscreen drug products for over-the-counter human use. It proposes that the 16 UV filters be classified into one of 3 categories. Category I would include zinc oxide and titanium dioxide, which are generally recognized as safe and effective (GRASE). Category II would include PABA and trolamine salicylate, which are not used in the United States and are not GRASE. Category III would include 12 filters that lack insufficient safety data to make a determination regarding GRASE.
The final FDA rule was scheduled to be released in September of 2020, but a result of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, the FDA “will be moving from a laborious rulemaking process to an administrative order process, which means it should not take as long to implement a monograph,” Dr. Lim said. “The FDA has decided that there will not be a final rule regarding sunscreen drug products,” but is required to issue a proposed administrative order by Sept. 27, 2021, he said.
When the final administrative order has been issued, manufacturers would have at least 1 year to comply with sunscreen products offered in the United States. “The approximate timeline is probably going to be 2023,” he said.
Dr. Lim disclosed that he is an investigator for Incyte, L’Oreal, Pfizer, and the Patient-centered Outcomes Research Institute, and a consultant for Pierre Fabre, ISDIN, Ferndale, La Roche–Posay, and Beiersdorf. He has been a speaker at general educational sessions sponsored by La Roche–Posay and Cantabria Labs.
FROM THE SPD PRE-AAD MEETING
Systemic racism is a cause of health disparities
I applaud the joint statement by the editors of the family medicine journals to commit to the eradication of systemic racism in medicine ( J Fam Pract . 2021;70:3 -4). These are crucial times in our history, where proactive change is necessary. The leadership they have shown is important.

No one wants health disparities. So, to eliminate them, we need to know what they are and where they came from. In my presentations on health disparities to students, residents, and health care providers, I use 3 definitions of health disparities. My definitions are slightly different from those proposed in the seminal report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, from the National Academy of Medicine (then Institute of Medicine).1 I like to think that my definitions elicit the information needed to guide change.
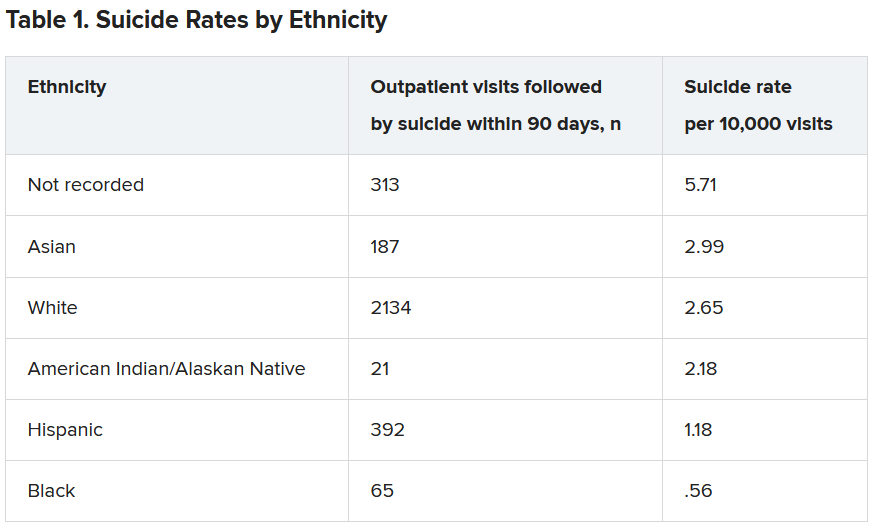
The first definition focuses on health statistics. When there are different outcomes for different demographic groups for the same disease, that is a disparity. This could be Black vs white, male vs female, or 1 zip code vs another.2 We owe ourselves an explanation for these differences if we are to be able to propose solutions.
Second, there are disparities in the provision of health care. If there are 2 individuals who present with the exact same symptoms, we need to ask ourselves why they would be treated differently. Even in systems where insurance status is the same, there are documented differences in care. A well-studied example of this is pain. In 1 such study, a meta-analysis showed that Blacks were less likely than whites to receive medication for acute pain in the emergency department (OR = 0.60 [95% CI, 0.43-0.83]).3 Other examples of differences by race include cardiac services,4 lung cancer screening,5 and stroke interventions.6
The third definition of health disparities involves differences in health-seeking behavior. This is not to blame the “victim,” but to understand the reason why the difference exists so that adequate interventions can be designed to improve outcomes. Traditionally, the concept of access referenced whether or not the patient had health insurance. But the provision of health insurance is insufficient to explain issues of access.7
Extrinsic and intrinsic factors at work. Factors related to insurance are an example of the extrinsic factors related to access. However, there are intrinsic factors related to access, most of which involve health literacy. We must ask ourselves: What are the best practices to educate patients to get the care they need? I will take this 1 step further; it is the duty of all health care professionals to improve health literacy 1 patient, 1 community at a time.
The next point that I make in my presentations on health disparities is that if you control for socioeconomic status, some of the health disparities go away. However, they rarely disappear. We measure socioeconomic status in a variety of ways: education, insurance status, income, and wealth. And as would be expected, these variables are usually correlated. We also know that these variables are not distributed equally by race. This is by design. This has been intentional. This has been, in many cases, our country’s policy. This is the result of systemic racism.
Continue to: It is necessary...
It is necessary for us to be willing to accept the toxicity of racism. This we can assess in 2 major ways. First, if we apply the Koch postulates or the Bradford Hill criteria for causation to racism, we can assess the degree to which racism is an explanation for health disparities. These principles offer methods for determining the relationship between risk and outcome.
Second, when we analyze the historical antecedents of health disparities, we find that racism is directly responsible not only for the current toxicity that Black people face today, but for the socioeconomic disparities that continue to exist. Let me give just a few examples.
- The Farm Security Administration was created in 1937 to avoid the collapse of the farming industry. As a compromise to southern legislators, a model was approved to allow local administration of support to farmers that essentially condoned the discrimination that had been occurring and would continue to occur—especially in the South.
- The National Housing Act of 1934 was created to provide stability to the banking industry at a time of national crisis. It subsidized a massive building program, and many of the units had restrictive covenants that prevented the sale to Blacks. It also codified redlining that prevented insured mortgages from being provided to Black communities.
- The Social Security Act of 1935 was created to provide benefits for the elderly and disabled. All workers were included except domestic workers and farm workers—the majority of whom were Black. This was another compromise that was made with southern congressman to get this act passed.
- The Servicemen’s Readjustment Act of 1944 (also known as the GI Bill) was passed to support veterans returning from World War II. Two major functions of the bill were to support educational opportunities for veterans and their families and to support the purchase of homes. From 1945 to 1954, the US added 13 million new homes. In 1946 and 1947, the Veterans Administration financed 40% of all single-family houses in the United States. Additionally, there were educational benefits for veterans to go to college or to learn a trade. These provisions, education, and housing were not equally available to Blacks. Columbia University professor Ira Katznelson called this act and others “affirmative action for whites.” 8
In 2019, the median income in white households was $76,057 and in Black households it was $46,073. 9 So, when we look at disparities of income, we must acknowledge this difference within the context of the current environment and the historical conditions that created these disparities. If we go 1 step further and look at disparities of wealth, we find that in 2019, the median wealth for white families was $188,200 and the median wealth for Black families was $24,100. 10
When one considers that a major contributor of wealth is home ownership, these differences seem logical—particularly related to points 1, 2, and 4 that I've just described. These economic disparities would not be as great today if the 4 examples given here (not to mention numerous other examples) had been administered equitably. The same applies to disparities in housing, employment, and education. Systemic racism is the causative agent. Systemic racism must be neutralized if we are to obtain anything close to health equity. 11
The Centers for Disease Control and Prevention (CDC) has recently taken new steps to recognize the role of racism in health. 12 The CDC plans to use “science to investigate and better understand the intersection of racism and health, and then to take action.” 13
It is time for the entire nation to recognize the links between racism and health outcomes and examine how we can design, implement, and evaluate interventions that will permanently correct these inequities.
1. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; 2003. Accessed April 22, 2021. https://doi.org/10.17226/10260
2. Life Expectancy: Could where you live influence how long you live? Robert Wood Johnson Foundation. Accessed April 22, 2021. www.rwjf.org/en/library/interactives/whereyouliveaffectshowlongyoulive.html
3. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med. 2019;37:1770-1777. doi: 10.1016/j.ajem.2019.06.014
4. Youmans QR, Hastings-Spaine L, Princewill O, et al. Disparities in cardiovascular care: past, present, and solutions. Cleve Clin J Med. 2019;86:621-632. doi: 10.3949/ccjm.86a.18088
5. Rivera MP, Katki HA, Tanner NT, et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society statement. Am J Respir Crit Care Med. 2020;202: e95-e112. doi: 10.1164/rccm.202008-3053ST
6. Rinaldo L, Rabinstein AA, Cloft H, et al. Racial and ethnic disparities in the utilization of thrombectomy for acute stroke. Stroke. 2019;50:2428-2432. doi:10.1161/STROKEAHA.118.024651
7. Hall AG, Lemak CH, Steingraber H, et al. Expanding the definition of access: it isn’t just about health insurance. J Health Care Poor Underserved. 2008;19:625-638. doi: 10.1353/hpu.0.0011
8. Katznelson I. When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth Century America. W. W. Norton & Co; 2006.
9. US Census Bureau. Households by Total Money Income, Race, and Hispanic Origin of Householder: 1967 to 2019. Accessed April 26, 2021. www.census.gov/data/tables/2020/demo/income-poverty/p60-270.html
10. Robb G. Long-standing wealth gap between Black and white Americans remains substantial, Fed data for 2019 show. MarketWatch. September 29, 2020. Accessed April 26, 2021. www.marketwatch.com/story/long-standing-wealth-gap-between-blacks-and-whites-remains-substantial-new-fed-data-for-2019-show-2020-09-28
11. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;9:1212-1215. doi: 10.2105/ajph.90.8.1212
12. CDC. Health equity: Director’s commentary. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/director-commentary.html
13. CDC. Health equity: CDC’s efforts. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/cdc-efforts.html
I applaud the joint statement by the editors of the family medicine journals to commit to the eradication of systemic racism in medicine ( J Fam Pract . 2021;70:3 -4). These are crucial times in our history, where proactive change is necessary. The leadership they have shown is important.

No one wants health disparities. So, to eliminate them, we need to know what they are and where they came from. In my presentations on health disparities to students, residents, and health care providers, I use 3 definitions of health disparities. My definitions are slightly different from those proposed in the seminal report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, from the National Academy of Medicine (then Institute of Medicine).1 I like to think that my definitions elicit the information needed to guide change.
The first definition focuses on health statistics. When there are different outcomes for different demographic groups for the same disease, that is a disparity. This could be Black vs white, male vs female, or 1 zip code vs another.2 We owe ourselves an explanation for these differences if we are to be able to propose solutions.
Second, there are disparities in the provision of health care. If there are 2 individuals who present with the exact same symptoms, we need to ask ourselves why they would be treated differently. Even in systems where insurance status is the same, there are documented differences in care. A well-studied example of this is pain. In 1 such study, a meta-analysis showed that Blacks were less likely than whites to receive medication for acute pain in the emergency department (OR = 0.60 [95% CI, 0.43-0.83]).3 Other examples of differences by race include cardiac services,4 lung cancer screening,5 and stroke interventions.6
The third definition of health disparities involves differences in health-seeking behavior. This is not to blame the “victim,” but to understand the reason why the difference exists so that adequate interventions can be designed to improve outcomes. Traditionally, the concept of access referenced whether or not the patient had health insurance. But the provision of health insurance is insufficient to explain issues of access.7
Extrinsic and intrinsic factors at work. Factors related to insurance are an example of the extrinsic factors related to access. However, there are intrinsic factors related to access, most of which involve health literacy. We must ask ourselves: What are the best practices to educate patients to get the care they need? I will take this 1 step further; it is the duty of all health care professionals to improve health literacy 1 patient, 1 community at a time.
The next point that I make in my presentations on health disparities is that if you control for socioeconomic status, some of the health disparities go away. However, they rarely disappear. We measure socioeconomic status in a variety of ways: education, insurance status, income, and wealth. And as would be expected, these variables are usually correlated. We also know that these variables are not distributed equally by race. This is by design. This has been intentional. This has been, in many cases, our country’s policy. This is the result of systemic racism.
Continue to: It is necessary...
It is necessary for us to be willing to accept the toxicity of racism. This we can assess in 2 major ways. First, if we apply the Koch postulates or the Bradford Hill criteria for causation to racism, we can assess the degree to which racism is an explanation for health disparities. These principles offer methods for determining the relationship between risk and outcome.
Second, when we analyze the historical antecedents of health disparities, we find that racism is directly responsible not only for the current toxicity that Black people face today, but for the socioeconomic disparities that continue to exist. Let me give just a few examples.
- The Farm Security Administration was created in 1937 to avoid the collapse of the farming industry. As a compromise to southern legislators, a model was approved to allow local administration of support to farmers that essentially condoned the discrimination that had been occurring and would continue to occur—especially in the South.
- The National Housing Act of 1934 was created to provide stability to the banking industry at a time of national crisis. It subsidized a massive building program, and many of the units had restrictive covenants that prevented the sale to Blacks. It also codified redlining that prevented insured mortgages from being provided to Black communities.
- The Social Security Act of 1935 was created to provide benefits for the elderly and disabled. All workers were included except domestic workers and farm workers—the majority of whom were Black. This was another compromise that was made with southern congressman to get this act passed.
- The Servicemen’s Readjustment Act of 1944 (also known as the GI Bill) was passed to support veterans returning from World War II. Two major functions of the bill were to support educational opportunities for veterans and their families and to support the purchase of homes. From 1945 to 1954, the US added 13 million new homes. In 1946 and 1947, the Veterans Administration financed 40% of all single-family houses in the United States. Additionally, there were educational benefits for veterans to go to college or to learn a trade. These provisions, education, and housing were not equally available to Blacks. Columbia University professor Ira Katznelson called this act and others “affirmative action for whites.” 8
In 2019, the median income in white households was $76,057 and in Black households it was $46,073. 9 So, when we look at disparities of income, we must acknowledge this difference within the context of the current environment and the historical conditions that created these disparities. If we go 1 step further and look at disparities of wealth, we find that in 2019, the median wealth for white families was $188,200 and the median wealth for Black families was $24,100. 10
When one considers that a major contributor of wealth is home ownership, these differences seem logical—particularly related to points 1, 2, and 4 that I've just described. These economic disparities would not be as great today if the 4 examples given here (not to mention numerous other examples) had been administered equitably. The same applies to disparities in housing, employment, and education. Systemic racism is the causative agent. Systemic racism must be neutralized if we are to obtain anything close to health equity. 11
The Centers for Disease Control and Prevention (CDC) has recently taken new steps to recognize the role of racism in health. 12 The CDC plans to use “science to investigate and better understand the intersection of racism and health, and then to take action.” 13
It is time for the entire nation to recognize the links between racism and health outcomes and examine how we can design, implement, and evaluate interventions that will permanently correct these inequities.
I applaud the joint statement by the editors of the family medicine journals to commit to the eradication of systemic racism in medicine ( J Fam Pract . 2021;70:3 -4). These are crucial times in our history, where proactive change is necessary. The leadership they have shown is important.

No one wants health disparities. So, to eliminate them, we need to know what they are and where they came from. In my presentations on health disparities to students, residents, and health care providers, I use 3 definitions of health disparities. My definitions are slightly different from those proposed in the seminal report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, from the National Academy of Medicine (then Institute of Medicine).1 I like to think that my definitions elicit the information needed to guide change.
The first definition focuses on health statistics. When there are different outcomes for different demographic groups for the same disease, that is a disparity. This could be Black vs white, male vs female, or 1 zip code vs another.2 We owe ourselves an explanation for these differences if we are to be able to propose solutions.
Second, there are disparities in the provision of health care. If there are 2 individuals who present with the exact same symptoms, we need to ask ourselves why they would be treated differently. Even in systems where insurance status is the same, there are documented differences in care. A well-studied example of this is pain. In 1 such study, a meta-analysis showed that Blacks were less likely than whites to receive medication for acute pain in the emergency department (OR = 0.60 [95% CI, 0.43-0.83]).3 Other examples of differences by race include cardiac services,4 lung cancer screening,5 and stroke interventions.6
The third definition of health disparities involves differences in health-seeking behavior. This is not to blame the “victim,” but to understand the reason why the difference exists so that adequate interventions can be designed to improve outcomes. Traditionally, the concept of access referenced whether or not the patient had health insurance. But the provision of health insurance is insufficient to explain issues of access.7
Extrinsic and intrinsic factors at work. Factors related to insurance are an example of the extrinsic factors related to access. However, there are intrinsic factors related to access, most of which involve health literacy. We must ask ourselves: What are the best practices to educate patients to get the care they need? I will take this 1 step further; it is the duty of all health care professionals to improve health literacy 1 patient, 1 community at a time.
The next point that I make in my presentations on health disparities is that if you control for socioeconomic status, some of the health disparities go away. However, they rarely disappear. We measure socioeconomic status in a variety of ways: education, insurance status, income, and wealth. And as would be expected, these variables are usually correlated. We also know that these variables are not distributed equally by race. This is by design. This has been intentional. This has been, in many cases, our country’s policy. This is the result of systemic racism.
Continue to: It is necessary...
It is necessary for us to be willing to accept the toxicity of racism. This we can assess in 2 major ways. First, if we apply the Koch postulates or the Bradford Hill criteria for causation to racism, we can assess the degree to which racism is an explanation for health disparities. These principles offer methods for determining the relationship between risk and outcome.
Second, when we analyze the historical antecedents of health disparities, we find that racism is directly responsible not only for the current toxicity that Black people face today, but for the socioeconomic disparities that continue to exist. Let me give just a few examples.
- The Farm Security Administration was created in 1937 to avoid the collapse of the farming industry. As a compromise to southern legislators, a model was approved to allow local administration of support to farmers that essentially condoned the discrimination that had been occurring and would continue to occur—especially in the South.
- The National Housing Act of 1934 was created to provide stability to the banking industry at a time of national crisis. It subsidized a massive building program, and many of the units had restrictive covenants that prevented the sale to Blacks. It also codified redlining that prevented insured mortgages from being provided to Black communities.
- The Social Security Act of 1935 was created to provide benefits for the elderly and disabled. All workers were included except domestic workers and farm workers—the majority of whom were Black. This was another compromise that was made with southern congressman to get this act passed.
- The Servicemen’s Readjustment Act of 1944 (also known as the GI Bill) was passed to support veterans returning from World War II. Two major functions of the bill were to support educational opportunities for veterans and their families and to support the purchase of homes. From 1945 to 1954, the US added 13 million new homes. In 1946 and 1947, the Veterans Administration financed 40% of all single-family houses in the United States. Additionally, there were educational benefits for veterans to go to college or to learn a trade. These provisions, education, and housing were not equally available to Blacks. Columbia University professor Ira Katznelson called this act and others “affirmative action for whites.” 8
In 2019, the median income in white households was $76,057 and in Black households it was $46,073. 9 So, when we look at disparities of income, we must acknowledge this difference within the context of the current environment and the historical conditions that created these disparities. If we go 1 step further and look at disparities of wealth, we find that in 2019, the median wealth for white families was $188,200 and the median wealth for Black families was $24,100. 10
When one considers that a major contributor of wealth is home ownership, these differences seem logical—particularly related to points 1, 2, and 4 that I've just described. These economic disparities would not be as great today if the 4 examples given here (not to mention numerous other examples) had been administered equitably. The same applies to disparities in housing, employment, and education. Systemic racism is the causative agent. Systemic racism must be neutralized if we are to obtain anything close to health equity. 11
The Centers for Disease Control and Prevention (CDC) has recently taken new steps to recognize the role of racism in health. 12 The CDC plans to use “science to investigate and better understand the intersection of racism and health, and then to take action.” 13
It is time for the entire nation to recognize the links between racism and health outcomes and examine how we can design, implement, and evaluate interventions that will permanently correct these inequities.
1. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; 2003. Accessed April 22, 2021. https://doi.org/10.17226/10260
2. Life Expectancy: Could where you live influence how long you live? Robert Wood Johnson Foundation. Accessed April 22, 2021. www.rwjf.org/en/library/interactives/whereyouliveaffectshowlongyoulive.html
3. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med. 2019;37:1770-1777. doi: 10.1016/j.ajem.2019.06.014
4. Youmans QR, Hastings-Spaine L, Princewill O, et al. Disparities in cardiovascular care: past, present, and solutions. Cleve Clin J Med. 2019;86:621-632. doi: 10.3949/ccjm.86a.18088
5. Rivera MP, Katki HA, Tanner NT, et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society statement. Am J Respir Crit Care Med. 2020;202: e95-e112. doi: 10.1164/rccm.202008-3053ST
6. Rinaldo L, Rabinstein AA, Cloft H, et al. Racial and ethnic disparities in the utilization of thrombectomy for acute stroke. Stroke. 2019;50:2428-2432. doi:10.1161/STROKEAHA.118.024651
7. Hall AG, Lemak CH, Steingraber H, et al. Expanding the definition of access: it isn’t just about health insurance. J Health Care Poor Underserved. 2008;19:625-638. doi: 10.1353/hpu.0.0011
8. Katznelson I. When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth Century America. W. W. Norton & Co; 2006.
9. US Census Bureau. Households by Total Money Income, Race, and Hispanic Origin of Householder: 1967 to 2019. Accessed April 26, 2021. www.census.gov/data/tables/2020/demo/income-poverty/p60-270.html
10. Robb G. Long-standing wealth gap between Black and white Americans remains substantial, Fed data for 2019 show. MarketWatch. September 29, 2020. Accessed April 26, 2021. www.marketwatch.com/story/long-standing-wealth-gap-between-blacks-and-whites-remains-substantial-new-fed-data-for-2019-show-2020-09-28
11. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;9:1212-1215. doi: 10.2105/ajph.90.8.1212
12. CDC. Health equity: Director’s commentary. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/director-commentary.html
13. CDC. Health equity: CDC’s efforts. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/cdc-efforts.html
1. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; 2003. Accessed April 22, 2021. https://doi.org/10.17226/10260
2. Life Expectancy: Could where you live influence how long you live? Robert Wood Johnson Foundation. Accessed April 22, 2021. www.rwjf.org/en/library/interactives/whereyouliveaffectshowlongyoulive.html
3. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med. 2019;37:1770-1777. doi: 10.1016/j.ajem.2019.06.014
4. Youmans QR, Hastings-Spaine L, Princewill O, et al. Disparities in cardiovascular care: past, present, and solutions. Cleve Clin J Med. 2019;86:621-632. doi: 10.3949/ccjm.86a.18088
5. Rivera MP, Katki HA, Tanner NT, et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society statement. Am J Respir Crit Care Med. 2020;202: e95-e112. doi: 10.1164/rccm.202008-3053ST
6. Rinaldo L, Rabinstein AA, Cloft H, et al. Racial and ethnic disparities in the utilization of thrombectomy for acute stroke. Stroke. 2019;50:2428-2432. doi:10.1161/STROKEAHA.118.024651
7. Hall AG, Lemak CH, Steingraber H, et al. Expanding the definition of access: it isn’t just about health insurance. J Health Care Poor Underserved. 2008;19:625-638. doi: 10.1353/hpu.0.0011
8. Katznelson I. When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth Century America. W. W. Norton & Co; 2006.
9. US Census Bureau. Households by Total Money Income, Race, and Hispanic Origin of Householder: 1967 to 2019. Accessed April 26, 2021. www.census.gov/data/tables/2020/demo/income-poverty/p60-270.html
10. Robb G. Long-standing wealth gap between Black and white Americans remains substantial, Fed data for 2019 show. MarketWatch. September 29, 2020. Accessed April 26, 2021. www.marketwatch.com/story/long-standing-wealth-gap-between-blacks-and-whites-remains-substantial-new-fed-data-for-2019-show-2020-09-28
11. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;9:1212-1215. doi: 10.2105/ajph.90.8.1212
12. CDC. Health equity: Director’s commentary. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/director-commentary.html
13. CDC. Health equity: CDC’s efforts. April 8, 2021. Accessed April 23, 2021. www.cdc.gov/healthequity/racism-disparities/cdc-efforts.html
Support group for Asian Americans uses theater to cope with COVID
An online, culturally based peer support group that uses theater and other creative outlets is helping Asian Americans cope with the COVID-19 pandemic, new research shows.
The findings of the qualitative study suggest that the program could be a model to support the mental health of other minority community groups during the COVID pandemic and beyond, say investigators from the Yale University Child Study Center, New Haven, Conn.
The Yale Compassionate Home, Action Together (CHATogether) group was created to promote emotional wellness among Asian American youth, young adults, and their families.
Early in the pandemic, it expanded its purpose to serve as a COVID-19 support group. Through social media outreach, CHATogether encourages members to cope with COVID-19 by using productive and creative outlets.
“We are a community education program serving Asian American families,” said Eunice Yuen, MD, PhD, the program’s founder and director, who is with the Yale University Child Study Center.
“ such as family conflict and xenophobic attacks,” said Dr. Yuen.
She discussed the program at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Skits, role playing
CHATogether groups consist of people with similar experiences and challenges who support each other through weekly online group meetings, she explained.
Group members work together to create family conflict scenarios and role-play dialogues on topics amplified during the COVID-19 pandemic, such as cross-cultural challenges among Asian Americans, academic expectations in home schooling, and Black Lives Matter and LGBTQ conflicts within Asian families.
Group members create skits that are based on their personal experiences and that allow them to work through their own internal conflicts and gain a sense of agency, said Dr. Yuen.
“CHATogether is really the interface of mental health, art, and theater, and we’re trying to create a vehicle that can be a lighthearted way for people to talk about mental health, especially for Asian American families,” said Dr. Yuen.
Preliminary results from a focus group with 10 CHATogether members who joined the program since the pandemic started identified four major ways in which the program has had a positive impact on the mental health and well-being of participants:
- It provides a safe and supportive environment, strengthens bonds between members, and increases the sense of belonging, thus encouraging engagement.
- It provides structural consistency/stability through regular meetings and consistent group functions. Weekly meetings provide a sense of control and hope in the midst of uncertainty during periods of sheltering in place.
- Through adapting the group to virtual platforms, group members experience the inherent strengths of a growth mindset and cognitive flexibility when facing challenges.
- It supports healthy coping skills through sublimation and altruism.
Looking ahead, Dr. Yuen said, the team plans to investigate the validity and effectiveness of this model and to expand the group to include other minorities, school educators, and medical education for trainees and medical students.
Commenting on the program, briefing moderator Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, described the initiative as a “great project that serves as a model that can be used not only for Asian Americans but for other groups.
“I think the key to it is that cultural sensitivity that we need to really take into account and cultural differences among people in order to best engage them and help support them. I think this program does that beautifully,” said Dr. Borenstein.
The work was supported by the APA’s Substance Abuse and Mental Health Services Administration Minority Fellowship, which provides a 1-year fellowship to psychiatry residents committed to addressing minority psychiatric mental health issues. Dr. Yuen and Dr. Borenstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An online, culturally based peer support group that uses theater and other creative outlets is helping Asian Americans cope with the COVID-19 pandemic, new research shows.
The findings of the qualitative study suggest that the program could be a model to support the mental health of other minority community groups during the COVID pandemic and beyond, say investigators from the Yale University Child Study Center, New Haven, Conn.
The Yale Compassionate Home, Action Together (CHATogether) group was created to promote emotional wellness among Asian American youth, young adults, and their families.
Early in the pandemic, it expanded its purpose to serve as a COVID-19 support group. Through social media outreach, CHATogether encourages members to cope with COVID-19 by using productive and creative outlets.
“We are a community education program serving Asian American families,” said Eunice Yuen, MD, PhD, the program’s founder and director, who is with the Yale University Child Study Center.
“ such as family conflict and xenophobic attacks,” said Dr. Yuen.
She discussed the program at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Skits, role playing
CHATogether groups consist of people with similar experiences and challenges who support each other through weekly online group meetings, she explained.
Group members work together to create family conflict scenarios and role-play dialogues on topics amplified during the COVID-19 pandemic, such as cross-cultural challenges among Asian Americans, academic expectations in home schooling, and Black Lives Matter and LGBTQ conflicts within Asian families.
Group members create skits that are based on their personal experiences and that allow them to work through their own internal conflicts and gain a sense of agency, said Dr. Yuen.
“CHATogether is really the interface of mental health, art, and theater, and we’re trying to create a vehicle that can be a lighthearted way for people to talk about mental health, especially for Asian American families,” said Dr. Yuen.
Preliminary results from a focus group with 10 CHATogether members who joined the program since the pandemic started identified four major ways in which the program has had a positive impact on the mental health and well-being of participants:
- It provides a safe and supportive environment, strengthens bonds between members, and increases the sense of belonging, thus encouraging engagement.
- It provides structural consistency/stability through regular meetings and consistent group functions. Weekly meetings provide a sense of control and hope in the midst of uncertainty during periods of sheltering in place.
- Through adapting the group to virtual platforms, group members experience the inherent strengths of a growth mindset and cognitive flexibility when facing challenges.
- It supports healthy coping skills through sublimation and altruism.
Looking ahead, Dr. Yuen said, the team plans to investigate the validity and effectiveness of this model and to expand the group to include other minorities, school educators, and medical education for trainees and medical students.
Commenting on the program, briefing moderator Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, described the initiative as a “great project that serves as a model that can be used not only for Asian Americans but for other groups.
“I think the key to it is that cultural sensitivity that we need to really take into account and cultural differences among people in order to best engage them and help support them. I think this program does that beautifully,” said Dr. Borenstein.
The work was supported by the APA’s Substance Abuse and Mental Health Services Administration Minority Fellowship, which provides a 1-year fellowship to psychiatry residents committed to addressing minority psychiatric mental health issues. Dr. Yuen and Dr. Borenstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An online, culturally based peer support group that uses theater and other creative outlets is helping Asian Americans cope with the COVID-19 pandemic, new research shows.
The findings of the qualitative study suggest that the program could be a model to support the mental health of other minority community groups during the COVID pandemic and beyond, say investigators from the Yale University Child Study Center, New Haven, Conn.
The Yale Compassionate Home, Action Together (CHATogether) group was created to promote emotional wellness among Asian American youth, young adults, and their families.
Early in the pandemic, it expanded its purpose to serve as a COVID-19 support group. Through social media outreach, CHATogether encourages members to cope with COVID-19 by using productive and creative outlets.
“We are a community education program serving Asian American families,” said Eunice Yuen, MD, PhD, the program’s founder and director, who is with the Yale University Child Study Center.
“ such as family conflict and xenophobic attacks,” said Dr. Yuen.
She discussed the program at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Skits, role playing
CHATogether groups consist of people with similar experiences and challenges who support each other through weekly online group meetings, she explained.
Group members work together to create family conflict scenarios and role-play dialogues on topics amplified during the COVID-19 pandemic, such as cross-cultural challenges among Asian Americans, academic expectations in home schooling, and Black Lives Matter and LGBTQ conflicts within Asian families.
Group members create skits that are based on their personal experiences and that allow them to work through their own internal conflicts and gain a sense of agency, said Dr. Yuen.
“CHATogether is really the interface of mental health, art, and theater, and we’re trying to create a vehicle that can be a lighthearted way for people to talk about mental health, especially for Asian American families,” said Dr. Yuen.
Preliminary results from a focus group with 10 CHATogether members who joined the program since the pandemic started identified four major ways in which the program has had a positive impact on the mental health and well-being of participants:
- It provides a safe and supportive environment, strengthens bonds between members, and increases the sense of belonging, thus encouraging engagement.
- It provides structural consistency/stability through regular meetings and consistent group functions. Weekly meetings provide a sense of control and hope in the midst of uncertainty during periods of sheltering in place.
- Through adapting the group to virtual platforms, group members experience the inherent strengths of a growth mindset and cognitive flexibility when facing challenges.
- It supports healthy coping skills through sublimation and altruism.
Looking ahead, Dr. Yuen said, the team plans to investigate the validity and effectiveness of this model and to expand the group to include other minorities, school educators, and medical education for trainees and medical students.
Commenting on the program, briefing moderator Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, described the initiative as a “great project that serves as a model that can be used not only for Asian Americans but for other groups.
“I think the key to it is that cultural sensitivity that we need to really take into account and cultural differences among people in order to best engage them and help support them. I think this program does that beautifully,” said Dr. Borenstein.
The work was supported by the APA’s Substance Abuse and Mental Health Services Administration Minority Fellowship, which provides a 1-year fellowship to psychiatry residents committed to addressing minority psychiatric mental health issues. Dr. Yuen and Dr. Borenstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Suicide risk prediction tools fail people of color
Current models used to predict suicide risk fall short for racialized populations including Black, Indigenous, and people of color (BIPOC), new research shows.
Investigators developed two suicide prediction models to examine whether these types of tools are accurate in their predictive abilities, or whether they are flawed.
They found both prediction models failed to identify high-risk BIPOC individuals. In the first model, nearly half of outpatient visits followed by suicide were identified in White patients versus only 7% of visits followed by suicide in BIPOC patients. The second model had a sensitivity of 41% for White patients, but just 3% for Black patients and 7% for American Indian/Alaskan Native patients.
“You don’t know whether a prediction model will be useful or harmful until it’s evaluated. The take-home message of our study is this: You have to look,” lead author Yates Coley, PhD, assistant investigator, Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The study was published online April 28, 2021, in JAMA Psychiatry.
Racial inequities
Suicide risk prediction models have been “developed and validated in several settings” and are now in regular use at the Veterans Health Administration, HealthPartners, and Kaiser Permanente, the authors wrote.
But the performance of suicide risk prediction models, while accurate in the overall population, “remains unexamined” in particular subpopulations, they noted.
“Health records data reflect existing racial and ethnic inequities in health care access, quality, and outcomes; and prediction models using health records data may perpetuate these disparities by presuming that past healthcare patterns accurately reflect actual needs,” Dr. Coley said.
Dr. Coley and associates “wanted to make sure that any suicide prediction model we implemented in clinical care reduced health disparities rather than exacerbated them.”
To investigate, researchers examined all outpatient mental health visits to seven large integrated health care systems by patients 13 years and older (n = 13,980,570 visits by 1,422,534 patients; 64% female, mean age, 42 years). The study spanned from Jan. 1, 2009, to Sept. 30, 2017, with follow-up through Dec. 31, 2017.
In particular, researchers looked at suicides that took place within 90 days following the outpatient visit.
Researchers used two prediction models: logistic regression with LASSO (Least Absolute Shrinkage and Selection Operator) variable selection and random forest technique, a “tree-based method that explores interactions between predictors (including those with race and ethnicity) in estimating probability of an outcome.”
The models considered prespecified interactions between predictors, including prior diagnoses, suicide attempts, and PHQ-9 [Patient Health Questionnaire–9] responses, and race and ethnicity data.
Researchers evaluated performance of the prediction models in the overall validation set and within subgroups defined by race/ethnicity.
The area under the curve measured model discrimination, and sensitivity was estimated for global and race/ethnicity-specific thresholds.
‘Unacceptable’ scenario
Within the total population, there were 768 deaths by suicide within 90 days of 3,143 visits. Suicide rates were highest for visits by patients with no recorded race/ethnicity, followed by visits by Asian, White, American Indian/Alaskan Native, Hispanic, and Black patients.
Both models showed “high” AUC sensitivity for White, Hispanic, and Asian patients but “poor” AUC sensitivity for BIPOC and patients without recorded race/ethnicity, the authors reported.
“Implementation of prediction models has to be considered in the broader context of unmet health care needs,” said Dr. Coley.
“In our specific example of suicide prediction, BIPOC populations already face substantial barriers in accessing quality mental health care and, as a result, have poorer outcomes, and using either of the suicide prediction models examined in our study will provide less benefit to already-underserved populations and widen existing care gaps,” a scenario Dr. Coley said is “unacceptable.”
“ she added.
Biased algorithms
Commenting on the study, Jonathan Singer, PhD, LCSW, associate professor at Loyola University, Chicago, described it as an “important contribution because it points to a systemic problem and also to the fact that the algorithms we create are biased, created by humans, and humans are biased.”
Although the study focused on the health care system, Dr. Singer believes the findings have implications for individual clinicians.
“If clinicians may be biased against identifying suicide risk in Black and Native American patients, they may attribute suicidal risk to something else. For example, we know that in Black Americans, expressions of intense emotions are oftentimes interpreted as aggression or being threatening, as opposed to indicators of sadness or fear,” noted Dr. Singer, who is also president of the American Academy of Suicidology and was not involved with the study,
“Clinicians who misinterpret these intense emotions are less likely to identify a Black client or patient who is suicidal,” Dr. Singer said.
The research was supported by the Mental Health Research Network from the National Institute of Mental Health. Dr. Coley has reported receiving support through a grant from the Agency for Healthcare Research and Quality. Dr. Singer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current models used to predict suicide risk fall short for racialized populations including Black, Indigenous, and people of color (BIPOC), new research shows.
Investigators developed two suicide prediction models to examine whether these types of tools are accurate in their predictive abilities, or whether they are flawed.
They found both prediction models failed to identify high-risk BIPOC individuals. In the first model, nearly half of outpatient visits followed by suicide were identified in White patients versus only 7% of visits followed by suicide in BIPOC patients. The second model had a sensitivity of 41% for White patients, but just 3% for Black patients and 7% for American Indian/Alaskan Native patients.
“You don’t know whether a prediction model will be useful or harmful until it’s evaluated. The take-home message of our study is this: You have to look,” lead author Yates Coley, PhD, assistant investigator, Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The study was published online April 28, 2021, in JAMA Psychiatry.
Racial inequities
Suicide risk prediction models have been “developed and validated in several settings” and are now in regular use at the Veterans Health Administration, HealthPartners, and Kaiser Permanente, the authors wrote.
But the performance of suicide risk prediction models, while accurate in the overall population, “remains unexamined” in particular subpopulations, they noted.
“Health records data reflect existing racial and ethnic inequities in health care access, quality, and outcomes; and prediction models using health records data may perpetuate these disparities by presuming that past healthcare patterns accurately reflect actual needs,” Dr. Coley said.
Dr. Coley and associates “wanted to make sure that any suicide prediction model we implemented in clinical care reduced health disparities rather than exacerbated them.”
To investigate, researchers examined all outpatient mental health visits to seven large integrated health care systems by patients 13 years and older (n = 13,980,570 visits by 1,422,534 patients; 64% female, mean age, 42 years). The study spanned from Jan. 1, 2009, to Sept. 30, 2017, with follow-up through Dec. 31, 2017.
In particular, researchers looked at suicides that took place within 90 days following the outpatient visit.
Researchers used two prediction models: logistic regression with LASSO (Least Absolute Shrinkage and Selection Operator) variable selection and random forest technique, a “tree-based method that explores interactions between predictors (including those with race and ethnicity) in estimating probability of an outcome.”
The models considered prespecified interactions between predictors, including prior diagnoses, suicide attempts, and PHQ-9 [Patient Health Questionnaire–9] responses, and race and ethnicity data.
Researchers evaluated performance of the prediction models in the overall validation set and within subgroups defined by race/ethnicity.
The area under the curve measured model discrimination, and sensitivity was estimated for global and race/ethnicity-specific thresholds.
‘Unacceptable’ scenario
Within the total population, there were 768 deaths by suicide within 90 days of 3,143 visits. Suicide rates were highest for visits by patients with no recorded race/ethnicity, followed by visits by Asian, White, American Indian/Alaskan Native, Hispanic, and Black patients.
Both models showed “high” AUC sensitivity for White, Hispanic, and Asian patients but “poor” AUC sensitivity for BIPOC and patients without recorded race/ethnicity, the authors reported.
“Implementation of prediction models has to be considered in the broader context of unmet health care needs,” said Dr. Coley.
“In our specific example of suicide prediction, BIPOC populations already face substantial barriers in accessing quality mental health care and, as a result, have poorer outcomes, and using either of the suicide prediction models examined in our study will provide less benefit to already-underserved populations and widen existing care gaps,” a scenario Dr. Coley said is “unacceptable.”
“ she added.
Biased algorithms
Commenting on the study, Jonathan Singer, PhD, LCSW, associate professor at Loyola University, Chicago, described it as an “important contribution because it points to a systemic problem and also to the fact that the algorithms we create are biased, created by humans, and humans are biased.”
Although the study focused on the health care system, Dr. Singer believes the findings have implications for individual clinicians.
“If clinicians may be biased against identifying suicide risk in Black and Native American patients, they may attribute suicidal risk to something else. For example, we know that in Black Americans, expressions of intense emotions are oftentimes interpreted as aggression or being threatening, as opposed to indicators of sadness or fear,” noted Dr. Singer, who is also president of the American Academy of Suicidology and was not involved with the study,
“Clinicians who misinterpret these intense emotions are less likely to identify a Black client or patient who is suicidal,” Dr. Singer said.
The research was supported by the Mental Health Research Network from the National Institute of Mental Health. Dr. Coley has reported receiving support through a grant from the Agency for Healthcare Research and Quality. Dr. Singer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current models used to predict suicide risk fall short for racialized populations including Black, Indigenous, and people of color (BIPOC), new research shows.
Investigators developed two suicide prediction models to examine whether these types of tools are accurate in their predictive abilities, or whether they are flawed.
They found both prediction models failed to identify high-risk BIPOC individuals. In the first model, nearly half of outpatient visits followed by suicide were identified in White patients versus only 7% of visits followed by suicide in BIPOC patients. The second model had a sensitivity of 41% for White patients, but just 3% for Black patients and 7% for American Indian/Alaskan Native patients.
“You don’t know whether a prediction model will be useful or harmful until it’s evaluated. The take-home message of our study is this: You have to look,” lead author Yates Coley, PhD, assistant investigator, Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The study was published online April 28, 2021, in JAMA Psychiatry.
Racial inequities
Suicide risk prediction models have been “developed and validated in several settings” and are now in regular use at the Veterans Health Administration, HealthPartners, and Kaiser Permanente, the authors wrote.
But the performance of suicide risk prediction models, while accurate in the overall population, “remains unexamined” in particular subpopulations, they noted.
“Health records data reflect existing racial and ethnic inequities in health care access, quality, and outcomes; and prediction models using health records data may perpetuate these disparities by presuming that past healthcare patterns accurately reflect actual needs,” Dr. Coley said.
Dr. Coley and associates “wanted to make sure that any suicide prediction model we implemented in clinical care reduced health disparities rather than exacerbated them.”
To investigate, researchers examined all outpatient mental health visits to seven large integrated health care systems by patients 13 years and older (n = 13,980,570 visits by 1,422,534 patients; 64% female, mean age, 42 years). The study spanned from Jan. 1, 2009, to Sept. 30, 2017, with follow-up through Dec. 31, 2017.
In particular, researchers looked at suicides that took place within 90 days following the outpatient visit.
Researchers used two prediction models: logistic regression with LASSO (Least Absolute Shrinkage and Selection Operator) variable selection and random forest technique, a “tree-based method that explores interactions between predictors (including those with race and ethnicity) in estimating probability of an outcome.”
The models considered prespecified interactions between predictors, including prior diagnoses, suicide attempts, and PHQ-9 [Patient Health Questionnaire–9] responses, and race and ethnicity data.
Researchers evaluated performance of the prediction models in the overall validation set and within subgroups defined by race/ethnicity.
The area under the curve measured model discrimination, and sensitivity was estimated for global and race/ethnicity-specific thresholds.
‘Unacceptable’ scenario
Within the total population, there were 768 deaths by suicide within 90 days of 3,143 visits. Suicide rates were highest for visits by patients with no recorded race/ethnicity, followed by visits by Asian, White, American Indian/Alaskan Native, Hispanic, and Black patients.
Both models showed “high” AUC sensitivity for White, Hispanic, and Asian patients but “poor” AUC sensitivity for BIPOC and patients without recorded race/ethnicity, the authors reported.
“Implementation of prediction models has to be considered in the broader context of unmet health care needs,” said Dr. Coley.
“In our specific example of suicide prediction, BIPOC populations already face substantial barriers in accessing quality mental health care and, as a result, have poorer outcomes, and using either of the suicide prediction models examined in our study will provide less benefit to already-underserved populations and widen existing care gaps,” a scenario Dr. Coley said is “unacceptable.”
“ she added.
Biased algorithms
Commenting on the study, Jonathan Singer, PhD, LCSW, associate professor at Loyola University, Chicago, described it as an “important contribution because it points to a systemic problem and also to the fact that the algorithms we create are biased, created by humans, and humans are biased.”
Although the study focused on the health care system, Dr. Singer believes the findings have implications for individual clinicians.
“If clinicians may be biased against identifying suicide risk in Black and Native American patients, they may attribute suicidal risk to something else. For example, we know that in Black Americans, expressions of intense emotions are oftentimes interpreted as aggression or being threatening, as opposed to indicators of sadness or fear,” noted Dr. Singer, who is also president of the American Academy of Suicidology and was not involved with the study,
“Clinicians who misinterpret these intense emotions are less likely to identify a Black client or patient who is suicidal,” Dr. Singer said.
The research was supported by the Mental Health Research Network from the National Institute of Mental Health. Dr. Coley has reported receiving support through a grant from the Agency for Healthcare Research and Quality. Dr. Singer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SGIM annual meeting focuses on inclusivity
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
FROM SGIM 2021
Structural racism tied to psychosis risk in Black people
Social and economic disparities are linked to an increased risk for psychosis in Black and Latino communities, new research shows.
Results of a literature review of social and economic disparities in mental illness suggest that “structural racism” contributes to social and environmental conditions that affect psychosis risk.
“Black and Latino people suffer disproportionately from psychosis risk factors, at the neighborhood level and at the individual level, in large part as a result of structural racism,” study investigator Deidre M. Anglin, PhD, associate professor, department of psychology, City College of New York (N.Y.), told reporters attending a press briefing.
The social environment, which, for minorities, involves disadvantage and discrimination, may account for this increased psychosis risk, perhaps even more so than genetics, she said. Structural racism “is a critical public health threat,” Dr. Anglin added.
The findings were presented at the virtual American Psychiatric Association annual meeting and were simultaneously published online May 3 in The American Journal of Psychiatry.
Perpetual disadvantage
Dr. Anglin and colleagues examined U.S.-based evidence connecting characteristics of social environments with outcomes across the psychosis continuum – from psychotic experiences to schizophrenia.
Citing numerous studies, the researchers highlighted three key areas that reflect social and environmental conditions that may affect psychosis risk, and that disproportionately affect minorities. These were neighborhood factors, trauma in a U.S. context, and racial disparities during the prenatal and perinatal periods.
The data that were related to neighborhoods revealed “just how much racism has historically structured U.S. neighborhoods in ways that generationally perpetuate disadvantage for racially minoritized communities,” said Dr. Anglin.
“This happens through inequitable access to resources, such as health care, clean air, education, [and] employment, but also in terms of disproportionate exposure to environmental toxins and stressors,” she said.
These neighborhood factors are associated with cumulative stress that may be linked to heightened risk for psychosis, the investigators noted.
U.S. studies show that rates of adverse childhood experiences, such as abuse and emotional and physical neglect, are higher among racial and ethnic minorities.
Police victimization and gun violence disproportionately affect racial minorities and create what the investigators call “a unique type of collective trauma” in the United States. They note that Black men have a 1 in 1,000 chance of being victims of lethal force by police over their lifetimes. By comparison, White men have a 39 in 100,000 chance.
One study of a diverse sample from four large U.S. urban centers showed that those who self-reported different types of police victimization were more likely to report psychotic experiences. Another study showed that greater exposure to gun violence fatalities, regardless of police involvement, was positively associated with psychotic experiences.
Obstetric complications
A variety of obstetric complications, including infection, maternal inflammation, and stress, have been associated with increased risk for psychotic disorders in U.S. samples.
“What we saw emerge from the literature is that Black women in the U.S. are at substantially increased risk for many of these obstetrical complications compared to White women, and this is not necessarily explained by socioeconomic status,” said Dr. Anglin.
Neighborhood- and individual-level factors appear to affect the disparity in these outcomes. A recent study revealed that exposure to environmental contaminants such as air pollution is associated with higher rates of preterm birth and low birth weight differentially in Black mothers compared with other mothers, “possibly as a result of an interaction between prenatal stress and contaminants,” the investigators noted.
Research also indicates that Black women are more likely to have lower levels of cortisol during the second trimester of pregnancy compared with women of other racial and ethnic groups. Cortisol is essential for fetal growth. Evidence links lower cortisol levels in later stages of pregnancy with decreased fetal growth in individuals who develop schizophrenia.
, compared with White women of the same socioeconomic status.
Such findings “highlight a complex picture” involving maternal cortisol levels and other stress biomarkers, “potentially leading to poor birth outcomes and subsequent risk for psychotic disorders in adulthood,” the investigators noted.
The researchers call for the dismantling of structural racism and the social policies and norms it shapes. They also recommend changes in health care policy and in the approach to early intervention for psychosis among Black and other racially-minoritized groups.
“Altogether, the current evidence suggests the need to identify, address, and tackle the social determinants deeply ingrained in U.S. society, in tandem with empowering the most marginalized communities,” the researchers wrote.
“We recommend that the field of psychiatry devote considerably more effort to addressing structural racism and social determinants of psychosis in funding priorities, training, and intervention development,” they added.
Dr. Anglin suggests that mental health providers use what she called a “cultural formulation interview” that takes a person’s environmental and social context into consideration. Studies show that incorporating this into clinical practice helps reduce misdiagnosis of mental illness in Black populations, she said.
Call to action
Commenting on the findings in an interview, Ned H. Kalin, MD, editor of The American Journal of Psychiatry and professor and chair of the department of psychiatry, University of Wisconsin, Madison, said the study was well done and serves as a “call to action” to address the impact of structural racism on mental health issues and psychiatric diseases.
The article highlights the need for “collecting better data” on structural racism, said Dr. Kalin. “We know it’s a big issue, but we can’t even quantitate it, so we need some fundamental measures to use as a benchmark as we move forward, as we try to make change.”
He noted that racism “is so embedded in one’s experience and in our society that we sort of don’t even think about it as a trauma.”
In psychiatry, for example, trauma is often thought of as a loss or a traumatic event. “We don’t typically think of trauma as an experience that pervades one’s entire life,” but that needs to change, he said. “At the individual level and in the doctor’s office, being sensitive to and aware of these issues is absolutely critical.”
Dr. Anglin and Dr. Kalin have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social and economic disparities are linked to an increased risk for psychosis in Black and Latino communities, new research shows.
Results of a literature review of social and economic disparities in mental illness suggest that “structural racism” contributes to social and environmental conditions that affect psychosis risk.
“Black and Latino people suffer disproportionately from psychosis risk factors, at the neighborhood level and at the individual level, in large part as a result of structural racism,” study investigator Deidre M. Anglin, PhD, associate professor, department of psychology, City College of New York (N.Y.), told reporters attending a press briefing.
The social environment, which, for minorities, involves disadvantage and discrimination, may account for this increased psychosis risk, perhaps even more so than genetics, she said. Structural racism “is a critical public health threat,” Dr. Anglin added.
The findings were presented at the virtual American Psychiatric Association annual meeting and were simultaneously published online May 3 in The American Journal of Psychiatry.
Perpetual disadvantage
Dr. Anglin and colleagues examined U.S.-based evidence connecting characteristics of social environments with outcomes across the psychosis continuum – from psychotic experiences to schizophrenia.
Citing numerous studies, the researchers highlighted three key areas that reflect social and environmental conditions that may affect psychosis risk, and that disproportionately affect minorities. These were neighborhood factors, trauma in a U.S. context, and racial disparities during the prenatal and perinatal periods.
The data that were related to neighborhoods revealed “just how much racism has historically structured U.S. neighborhoods in ways that generationally perpetuate disadvantage for racially minoritized communities,” said Dr. Anglin.
“This happens through inequitable access to resources, such as health care, clean air, education, [and] employment, but also in terms of disproportionate exposure to environmental toxins and stressors,” she said.
These neighborhood factors are associated with cumulative stress that may be linked to heightened risk for psychosis, the investigators noted.
U.S. studies show that rates of adverse childhood experiences, such as abuse and emotional and physical neglect, are higher among racial and ethnic minorities.
Police victimization and gun violence disproportionately affect racial minorities and create what the investigators call “a unique type of collective trauma” in the United States. They note that Black men have a 1 in 1,000 chance of being victims of lethal force by police over their lifetimes. By comparison, White men have a 39 in 100,000 chance.
One study of a diverse sample from four large U.S. urban centers showed that those who self-reported different types of police victimization were more likely to report psychotic experiences. Another study showed that greater exposure to gun violence fatalities, regardless of police involvement, was positively associated with psychotic experiences.
Obstetric complications
A variety of obstetric complications, including infection, maternal inflammation, and stress, have been associated with increased risk for psychotic disorders in U.S. samples.
“What we saw emerge from the literature is that Black women in the U.S. are at substantially increased risk for many of these obstetrical complications compared to White women, and this is not necessarily explained by socioeconomic status,” said Dr. Anglin.
Neighborhood- and individual-level factors appear to affect the disparity in these outcomes. A recent study revealed that exposure to environmental contaminants such as air pollution is associated with higher rates of preterm birth and low birth weight differentially in Black mothers compared with other mothers, “possibly as a result of an interaction between prenatal stress and contaminants,” the investigators noted.
Research also indicates that Black women are more likely to have lower levels of cortisol during the second trimester of pregnancy compared with women of other racial and ethnic groups. Cortisol is essential for fetal growth. Evidence links lower cortisol levels in later stages of pregnancy with decreased fetal growth in individuals who develop schizophrenia.
, compared with White women of the same socioeconomic status.
Such findings “highlight a complex picture” involving maternal cortisol levels and other stress biomarkers, “potentially leading to poor birth outcomes and subsequent risk for psychotic disorders in adulthood,” the investigators noted.
The researchers call for the dismantling of structural racism and the social policies and norms it shapes. They also recommend changes in health care policy and in the approach to early intervention for psychosis among Black and other racially-minoritized groups.
“Altogether, the current evidence suggests the need to identify, address, and tackle the social determinants deeply ingrained in U.S. society, in tandem with empowering the most marginalized communities,” the researchers wrote.
“We recommend that the field of psychiatry devote considerably more effort to addressing structural racism and social determinants of psychosis in funding priorities, training, and intervention development,” they added.
Dr. Anglin suggests that mental health providers use what she called a “cultural formulation interview” that takes a person’s environmental and social context into consideration. Studies show that incorporating this into clinical practice helps reduce misdiagnosis of mental illness in Black populations, she said.
Call to action
Commenting on the findings in an interview, Ned H. Kalin, MD, editor of The American Journal of Psychiatry and professor and chair of the department of psychiatry, University of Wisconsin, Madison, said the study was well done and serves as a “call to action” to address the impact of structural racism on mental health issues and psychiatric diseases.
The article highlights the need for “collecting better data” on structural racism, said Dr. Kalin. “We know it’s a big issue, but we can’t even quantitate it, so we need some fundamental measures to use as a benchmark as we move forward, as we try to make change.”
He noted that racism “is so embedded in one’s experience and in our society that we sort of don’t even think about it as a trauma.”
In psychiatry, for example, trauma is often thought of as a loss or a traumatic event. “We don’t typically think of trauma as an experience that pervades one’s entire life,” but that needs to change, he said. “At the individual level and in the doctor’s office, being sensitive to and aware of these issues is absolutely critical.”
Dr. Anglin and Dr. Kalin have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social and economic disparities are linked to an increased risk for psychosis in Black and Latino communities, new research shows.
Results of a literature review of social and economic disparities in mental illness suggest that “structural racism” contributes to social and environmental conditions that affect psychosis risk.
“Black and Latino people suffer disproportionately from psychosis risk factors, at the neighborhood level and at the individual level, in large part as a result of structural racism,” study investigator Deidre M. Anglin, PhD, associate professor, department of psychology, City College of New York (N.Y.), told reporters attending a press briefing.
The social environment, which, for minorities, involves disadvantage and discrimination, may account for this increased psychosis risk, perhaps even more so than genetics, she said. Structural racism “is a critical public health threat,” Dr. Anglin added.
The findings were presented at the virtual American Psychiatric Association annual meeting and were simultaneously published online May 3 in The American Journal of Psychiatry.
Perpetual disadvantage
Dr. Anglin and colleagues examined U.S.-based evidence connecting characteristics of social environments with outcomes across the psychosis continuum – from psychotic experiences to schizophrenia.
Citing numerous studies, the researchers highlighted three key areas that reflect social and environmental conditions that may affect psychosis risk, and that disproportionately affect minorities. These were neighborhood factors, trauma in a U.S. context, and racial disparities during the prenatal and perinatal periods.
The data that were related to neighborhoods revealed “just how much racism has historically structured U.S. neighborhoods in ways that generationally perpetuate disadvantage for racially minoritized communities,” said Dr. Anglin.
“This happens through inequitable access to resources, such as health care, clean air, education, [and] employment, but also in terms of disproportionate exposure to environmental toxins and stressors,” she said.
These neighborhood factors are associated with cumulative stress that may be linked to heightened risk for psychosis, the investigators noted.
U.S. studies show that rates of adverse childhood experiences, such as abuse and emotional and physical neglect, are higher among racial and ethnic minorities.
Police victimization and gun violence disproportionately affect racial minorities and create what the investigators call “a unique type of collective trauma” in the United States. They note that Black men have a 1 in 1,000 chance of being victims of lethal force by police over their lifetimes. By comparison, White men have a 39 in 100,000 chance.
One study of a diverse sample from four large U.S. urban centers showed that those who self-reported different types of police victimization were more likely to report psychotic experiences. Another study showed that greater exposure to gun violence fatalities, regardless of police involvement, was positively associated with psychotic experiences.
Obstetric complications
A variety of obstetric complications, including infection, maternal inflammation, and stress, have been associated with increased risk for psychotic disorders in U.S. samples.
“What we saw emerge from the literature is that Black women in the U.S. are at substantially increased risk for many of these obstetrical complications compared to White women, and this is not necessarily explained by socioeconomic status,” said Dr. Anglin.
Neighborhood- and individual-level factors appear to affect the disparity in these outcomes. A recent study revealed that exposure to environmental contaminants such as air pollution is associated with higher rates of preterm birth and low birth weight differentially in Black mothers compared with other mothers, “possibly as a result of an interaction between prenatal stress and contaminants,” the investigators noted.
Research also indicates that Black women are more likely to have lower levels of cortisol during the second trimester of pregnancy compared with women of other racial and ethnic groups. Cortisol is essential for fetal growth. Evidence links lower cortisol levels in later stages of pregnancy with decreased fetal growth in individuals who develop schizophrenia.
, compared with White women of the same socioeconomic status.
Such findings “highlight a complex picture” involving maternal cortisol levels and other stress biomarkers, “potentially leading to poor birth outcomes and subsequent risk for psychotic disorders in adulthood,” the investigators noted.
The researchers call for the dismantling of structural racism and the social policies and norms it shapes. They also recommend changes in health care policy and in the approach to early intervention for psychosis among Black and other racially-minoritized groups.
“Altogether, the current evidence suggests the need to identify, address, and tackle the social determinants deeply ingrained in U.S. society, in tandem with empowering the most marginalized communities,” the researchers wrote.
“We recommend that the field of psychiatry devote considerably more effort to addressing structural racism and social determinants of psychosis in funding priorities, training, and intervention development,” they added.
Dr. Anglin suggests that mental health providers use what she called a “cultural formulation interview” that takes a person’s environmental and social context into consideration. Studies show that incorporating this into clinical practice helps reduce misdiagnosis of mental illness in Black populations, she said.
Call to action
Commenting on the findings in an interview, Ned H. Kalin, MD, editor of The American Journal of Psychiatry and professor and chair of the department of psychiatry, University of Wisconsin, Madison, said the study was well done and serves as a “call to action” to address the impact of structural racism on mental health issues and psychiatric diseases.
The article highlights the need for “collecting better data” on structural racism, said Dr. Kalin. “We know it’s a big issue, but we can’t even quantitate it, so we need some fundamental measures to use as a benchmark as we move forward, as we try to make change.”
He noted that racism “is so embedded in one’s experience and in our society that we sort of don’t even think about it as a trauma.”
In psychiatry, for example, trauma is often thought of as a loss or a traumatic event. “We don’t typically think of trauma as an experience that pervades one’s entire life,” but that needs to change, he said. “At the individual level and in the doctor’s office, being sensitive to and aware of these issues is absolutely critical.”
Dr. Anglin and Dr. Kalin have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Avoid presumptions with LGBTQ+ patients
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
FROM SHM CONVERGE 2021